Abstract
Background
The novel coronavirus disease 2019 (COVID-19) started in Wuhan, China, in December 2019. It spread widely around the world and was described as a pandemic by the World Health Organization (WHO). The knowledge regarding the mortality rate and risk factors of COVID-19 among the pediatric population is lacking. In this regard, we aimed to report the clinical and laboratory characteristics of deceased pediatric patients with SARS-CoV-2 infection.
Method
This cross-sectional study was conducted in Mofid Children's Hospital, Tehran, Iran, from February 2020 to April 2021. Recorded documents of 59 pediatric patients (under 18 years old) assumed to have COVID-19 who had died in the COVID-19 ward and COVID-19 intensive care unit (ICU) were retrospectively evaluated. All statistical analyses were performed using SPSS software (v. 26.0, Chicago, IL). A P value of less than 0.05 was considered statistically significant.
Results
From 711 COVID-19 definite and suspected patients, 59 children died. Of these deceased pediatric patients, 34 were boys (57.62%) and 25 were girls (42.37%), with a total mean age of 5.6 years. The median length of stay in the hospital was 10 days (range 1–215). 91.52% had underlying comorbidities of which neurological diseases accounted for the largest share. 54 patients were admitted to the ICU and 83.05% of them had intubation during their hospitalization. In addition, the most common reasons for death in our study were related to respiratory and multiorgan failure.
Conclusion
According to our knowledge, we are the first team to report such a thorough study in the field of COVID-19 pediatric mortality in Iran. Mortality was observed in all age groups of children, especially in those with previous comorbidities, specifically neurological disease. Abnormally elevated tests of ESR, CRP, LDH, AST, and ALT as well as the presence of proteinuria and hematuria were found in more than 50% of patients in our investigations, and ICU admission between both definite and suspected groups had significant differences, so monitoring and considering these factors may help to control and reduce the progression of the disease to death.
1. Introduction
The novel coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has received global attention since its first diagnosis in Wuhan, China, in December 2019. Due to the alarming levels of prevalence, severity, and stagnation, this outbreak was described by the World Health Organization as a pandemic [1] and has since emerged as a major public health emergency with global destructive effects [2]. This is the first pandemic caused by the coronavirus [3]. Based on the Lynx Insight Service report on April 2 (Reuters), more than 129.34 million people have been infected with the new coronavirus worldwide and 2,947,927 have died. Since the first cases were identified, infections have been reported in more than 210 countries and territories [4].
Nevertheless, the significant numbers of asymptomatic children (about 25%) [5] and the longer incubation period [6] compared with adults impose a potential threat of silent distribution of the infection. Most pediatric patients represent mild symptoms [7], and few studies worldwide have reported severe forms of COVID-19 in children [8–10]. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is assumed to be rare in children, accounting for 1.7–2% of diagnosed patients [11]. In the pediatric population, the impact of comorbidities, such as chronic kidney diseases, neurological disorders, cardiovascular disease, liver disease, and inborn errors of immunity affecting the interferon pathway (as the most frequent disorders) [12–15] on the outcome of SARS-CoV-2 infection is disputed [16, 17]. Due to the paucity of studies published on pediatric COVID-19 infections [8], including critically ill patients, a better understanding of the mortality rate and risk factors associated with COVID-19 infections in pediatric patients is still lacking.
The objective of this study is to report the clinical and laboratory characteristics of deceased pediatric patients with SARS-CoV-2 infection.
2. Methods
From February 2020 to April 2021, 711 COVID-19-infected patients (477 definite and 234 suspected) were admitted to Mofid Children's Hospital, a referral center in Tehran (capital city of Iran), and we retrospectively evaluated 59 pediatric patients who died with the diagnosis of COVID-19 infection (definite or suspected).
We categorized patients into definite or suspected; cases that met two or more of these criteria were considered suspicious [18]:
A high fever, malaise, or gastrointestinal or respiratory symptoms
Laboratory data with a decrease in white blood cells (WBC) count or lymphocytopenia or an increase in C-reactive protein (CRP)/erythrocyte sedimentation rate (ESR)
Atypical chest imaging, as well as computed tomography (CT) scans
And they are classified as definite if they meet the following criteria [18]:
COVID-19 nucleic acid positivity in blood samples, nasal, and pharyngeal swab samples, as confirmed by RT-PCR
A questionnaire was developed and filled with demographic and laboratory data, length of hospital stay (LOS), underlying comorbidities, clinical manifestations, and outcomes.
The SPSS software (v. 26.0, Chicago, IL) was used for the statistical analyses. Descriptive statistics included means and standard deviation (SD) for normally distributed or medians and interquartile range (IQR) for skewed measures, and proportions for categorical variables. A P value <0.05 was considered statistically significant.
3. Results
This study was conducted between February 2020 and April 2021 on 59 COVID-19 patients (with definite or probable novel coronavirus infection) who died in Mofid Children's Hospital, Tehran, Iran. 34 were males (57.62%) and 25 were females (42.37%), with a total mean age of 5.6 years. Table 1 shows the number of pediatric patients in each age group in total.
Table 1.
Age groups of patients in total children.
| Total age range | Number of children | Percentage |
|---|---|---|
| <1 | 17 | 29 |
| 1–5 | 14 | 24 |
| 5–10 | 13 | 22 |
| 10< | 15 | 25 |
The median days of hospitalization were 10 (range 1–215).
About 89.83% of the study population had underlying medical conditions; 31 patients (52.54%) had only one and 22 (37.29%) had two or more underlying diseases.
In total, patients, in the course of their illness, experienced most of the following symptoms: 52 (88.1%) had respiratory distress, 50 (84.7%) dyspnea, 39 (66.1%) fever, and 27 (45.8%) cough. Also, 39 (66.1%) showed gastrointestinal (GI) manifestation, and 28 (47.5%) showed varying degrees of loss of consciousness in the period of illness.
The most common clinical symptoms seen in our patients are listed in Table 2.
Table 2.
Common symptoms in total patients.
| Symptoms | Percentage | Numbers in total |
|---|---|---|
| Respiratory distress | 88.1 | 59 |
| Dyspnea | 84.7 | 59 |
| Fever | 66.1 | 59 |
| Gastrointestinal | 66.1 | 58 |
| Loss of consciousness | 47.5 | 59 |
| Cough | 45.8 | 58 |
In our study population, at the time of admission with diagnosis or suspicion of COVID-19, 47 (79.7%), patients had either no or mild dehydration and 12 (20.3%) had moderate or severe dehydration; among the latter group, 58.3% (7 patients) had the moderate type and 41.7% (5 patients) showed the severe type of dehydration.
54 patients (91.52% of the study population) were admitted to the ICU, and 49 (83.1%) of them had been intubated during their hospitalization. 51 (86.4%) of cases had chest CT in favor of COVID-19 during their illness.
Based on the mentioned criteria for definite and suspected identification patterns, we had 54 patients that could be considered in these two groups.
34 out of 54 (63%) were known as definite, based on a positive COVID-19 PCR test.
Half of the definite patients (17/34) and 65% of the suspected cases (13/20) were males. In the definite group, the children's mean age was 6.36, and in the suspicious group, this mean number was 4.9 years (Figure 1).
Figure 1.
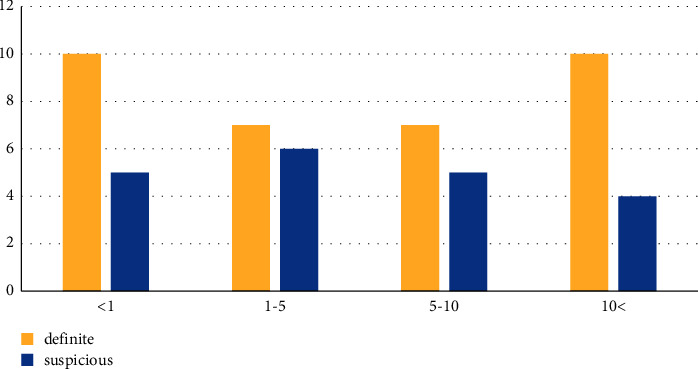
Age chart of the definite and suspicious groups.
The median length of stay (LOS) in definite children was 13.5 days, which was more than 1.5 times the probable one (8 days).
18 (90%) of suspected children and 32 (94.11%) of definite ones had different underlying diseases (Table 3).
Table 3.
Types of underlying diseases in the definite/suspected groups.
| Underlying disease | Definite (%) | Suspected (%) |
|---|---|---|
| Malignancy | 23.53 | 10 |
| PID∗ | 11.76 | 15 |
| Neurologic | 35.29 | 25 |
| Hematologic | 5.88 | 20 |
| Rheumatologic | 11.76 | 0 |
| Respiratory system | 8.82 | 10 |
| Endocrine | 11.76 | 25 |
| Renal | 14.71 | 15 |
| Hepatic | 8.82 | 10 |
| Gastrointestinal | 5.88 | 10 |
| Traumatic | 2.94 | 0 |
| Cardiac | 8.82 | 25 |
∗ Primary immunodeficiency diseases.
In both groups, the mean range of some initial tests, including ESR, LDH, AST (aspartate aminotransferase), ALT (alanine transaminase), and CPK (creatine phosphokinase), was higher than normal.
In Figure 2, we compare the level of tests in the definitive and suspected groups. Statistical analysis shows there was no significant difference between these groups.
Figure 2.
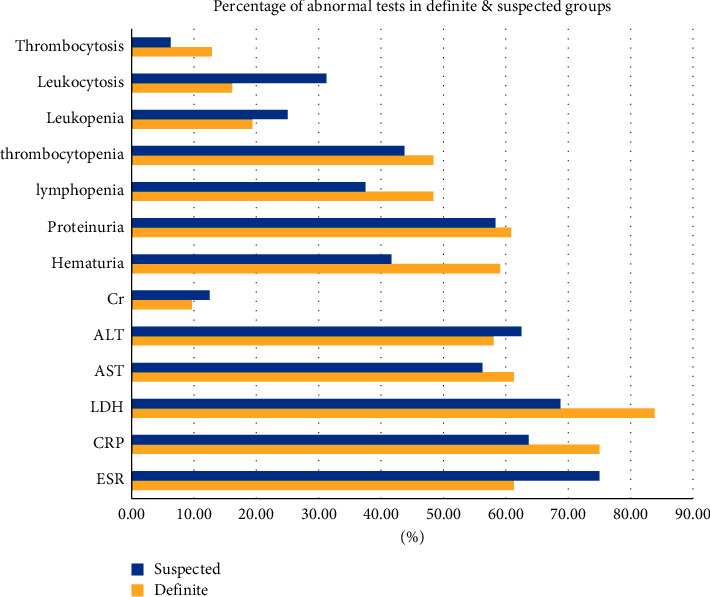
Percentage of abnormal initial tests in the definite and suspected groups.
Also, according to the reference of this hospital, we considered albumin less than 3 abnormal, which after analysis and comparison of the two definite and suspicious groups, no significant difference was found (the mean range of initial albumin in these two groups was 3.51 and 3.14, respectively).
16 (80%) of the suspected group and 33 (97.06%) of the definite group had been admitted to the ICU during their hospitalization (with a PP value of 0.037). 15 (75%) of the first group and 29 (85.3%) of the second one experienced intubation through their confinement.
In the suspected group, 95% of CT scan findings were in favor of COVID-19 while this number was 87.1% in the definitive group.
Except for ICU admission (with a P value of 0.03), in general, no significant relationship was found in P value less than 0.05 between definite and suspicious groups in symptoms and laboratory tests.
The reasons for the death in our total group of pediatric patients are shown in Table 4.
Table 4.
Reasons for death in COVID-19-infected children.
| Reasons for death | Percentage | Numbers in total |
|---|---|---|
| Respiratory | 54.2 | 59 |
| Multiorgan failure | 16.9 | 59 |
| DIC | 13.6 | 59 |
| Septic shock | 8.5 | 59 |
| Sepsis | 6.8 | 59 |
| Shock | 5.1 | 59 |
| CNS | 5.1 | 59 |
| Renal | 3.4 | 59 |
| Hepatic | 1.7 | 59 |
| Cardiac | 1.7 | 59 |
| Hemodynamic | 1.7 | 59 |
4. Discussion
Since the worldwide studies on SARS-CoV-2 mortality in children are limited or information that has been collected is insufficient, according to our evidence, in the field of COVID-19 pediatric mortality in Iran, we are the first group to report such a study with this number of data and variables over a long time.
In the children's group, some recent epidemic study results, such as Dong et al.'s results, suggest that boys are dominant in getting affected by the virus; however, with a slight predominance of boys, there was no significant difference in getting infection between the sexes [10]. Also, in our study, boys were dominant with 57%.
There is a risk of infection and mortality in all age groups of children with COVID-19 infection [19]. From studies of Olivia et al. in the United Kingdom, Philip et al. in New York City, and the CDC, the severity and mortality of COVID-19 were higher in children under age 1 and adolescents [20–22]. In the same way, our study shows the highest number of deaths in the age group under one year, then 10 years and above, after that 1–5 years, and finally 5–10 years, respectively.
From reports at Pernambuco-Brazilian in 2020, on patients under 20 years, based on pediatric age group, the neonates and infants' fatality rate was higher [23]. Also, in reports from Jakarta, Indonesia, in a hospital-based retrospective cohort study, death happened across all age groups, and based on pediatric age-specific mortalities, the highest death percentage in children was for 0–4 years [24].
According to a study by Rutgers researchers, children, adolescents, and young people with underlying comorbidities are more at risk for SARS-CoV-2 severe complications [25]. A significant number of our total COVID-19 patients who died had the underlying disease (91.52%) was observed. In addition, the Aimen et al. pediatric study reported a 7% fatality rate in which they clearly stated the presence of underlying diseases is considerably associated with mortality [26]. In proportion to these statements, children with underlying diseases should be taken care of as much as possible [27].
In France, Oualha et al.'s study on severe and fatal forms of a novel coronavirus in pediatric cases announced that 70% of cases had comorbidities, most of which were neurological ones with 25.92% [8]. In Singh et al.'s cohort study of COVID-19 children mortality, about 11.11% had a neurological underlying illness [28], but in ours, about 33.33% had this condition. However, the presence of underlying cardiac, hematologic, and gastrointestinal diseases in suspected COVID-19 patients who died was higher than in the definitive group, so attention to this issue in the field of care is likely to be helpful. However, in some pediatric studies, such as two case series in China by Wang et al. and in Iran by Rahimzadeh et al., the underlying disease was not present among children diagnosed with COVID-19 [29, 30]. This difference may be due to the severity of the disease in the study population. Our hospital is an excellent multidisciplinary referral center for children, so cases with underlying diseases and COVID-19 infection may be referred here. In addition, in this study, only cases related to deceased children were investigated.
From 171 confirmed children, according to Lu et al. studies, 48.5% showed cough as the most common symptom [31]. Also, in another study, as stated by Wu et al., one-third of 74 COVID-19-infected children had cough and fever during their disease duration [32]. The most common symptoms in our observations were somehow similar to the results of other countries' studies [10, 20, 33–35].
According to the studies, which Harvard University also reported, under hydrated conditions, body temperature regulation, prevention of infection, delivery of nutrients to cells, and proper functioning of organs are established. In order to create balanced hydration and support the body's healthy metabolism, drinking an adequate amount of water continuously is essential. Dehydration is associated with a number of health disorders [36]. It is also expected that suboptimal hydration in the weeks prior to COVID-19 exposure increases the risk of mortality from this infection [37]. In a COVID-19 study from the United States, David and his colleagues reported that one of the most common symptoms for patients who died with MIS-C (after cough, nausea, dyspnea, and loss of appetite) was dehydration (6 of 14, 43%) [38], while in our study, out of 59 patients, 20.3% of children were in the category of moderate and severe dehydration.
From pooled analysis and review of Henry et al. in severe COVID-19 pediatric patients, out of 5 studies, 61.5% of cases had elevated CRP, and also, out of 3 studies, 72.7% presented elevated LDH [39]. We also experienced increased LDH and CRP levels, with a percentage of 78.72 and 71.43, respectively. The elevation of these markers indicates a serious infection or inflammation.
In the New Delhi cohort study, of fatal cases of confirmed SARS-CoV-2 infection in children, 44.4% of them had increased AST and ALT [28], which was similar to our data.
From reviewing several reports, Henry et al. found a normal leukocyte count in 69.2% of pediatric cases and only 3% of cases had lymphopenia [40]. Besides, the Lu et al. study states that lymphopenia was present in just 3.5% of COVID-19-infected children [31]. In another study by Wang et al., 30% of infants showed this abnormal situation [41]. On the contrary, in the Lippi and Plebani study of adult patients, the prevalence of increasing the number of leukocytes during disease progression was noted [42].
In our study, less than 45% of patients had lymphocytopenia and only a limited number of patients had thrombocytosis (10.64%). Leukocytosis also affected less than a quarter of the population. We should consider that our study was done on a poor prognostic group which may be shown differently from other children's COVID-19 case data.
In our study, a significant difference was observed between the two groups of definite and suspicious COVID-19 in the field of ICU admission, which seems reasonable. We noticed that endotracheal intubation was done in most cases, a procedure in which the likelihood of transmitting the virus and infection is very high [43, 44].
Based on our retrospective study in Mofid Children's Hospital, Tehran, Iran, the fatality rate over 14.5 months was 8.29%.
The mortality rate of this novel virus varies from country to country. In Norway, an archival study of over 2.5 months (1 March 2020–15 May 2020) did not report any confirmed SARS-CoV-2-related deaths in children under 20 years of age [45]. From Brazilian reports by Sena et al. in 2020, out of 682 confirmed pediatric cases in the state of Pernambuco, the total mortality rate was 5.6% [23]. According to the American Academy of Pediatrics (APP) and the Association of Children's Hospitals (CHA) in April 2021, in the United States, children diagnosed with COVID-19 account for 13.8% of the total. 1.2 to 3.1% of COVID-19 patients and 0.00–0.21% of COVID-19 deaths are pediatric [46]. Furthermore, patients under the age of 20 accounted for 2.1 percent with a mortality rate of 0.02 percent, according to an analysis of COVID-19 cases confirmed by the Centers for Disease Control and Prevention (CDC), China [47].
According to a study of COVID-19 deaths in children at a hospital in Indonesia, Dewi and her colleagues reported that two of the most common causes of death were acute respiratory distress syndrome and septic shock [48]. However, the priority of our findings as the causes of death was first respiratory diseases and then multiorgan failure which may be due to the high rates of underlying diseases in our study population.
5. Conclusion
According to our information in the field of COVID-19 pediatric mortality in Iran, this is the first original report about the death of children from COVID-19. As a result, children with comorbidities, especially neurological diseases, that are prone to suffer from serious illnesses should receive better care. In addition, children with fever, changes in the level of consciousness, and clinical, gastrointestinal, and respiratory symptoms need more attention. There was a significant difference in the rate of ICU admission between the definite and suspicious groups, and since the most important organs involved in coronavirus disease are the lungs, it seems logical that in our study, the most common causes of death are in the respiratory category.
6. Limitations
As in all other retrospective studies, data were collected from patients' medical files and there were some missing data or some variables did not request at all. We suggest a closer look for other pediatric studies on definite cases who died of COVID-19.
Abbreviations
- MIS-C:
Multisystem inflammatory syndrome in children
- DIC:
Disseminated intravascular coagulation
- ESR:
Erythrocyte sedimentation rate
- CRP:
C-reactive protein
- LDH:
Lactate dehydrogenase
- AST:
Aspartate aminotransferase
- ALT:
Alanine aminotransferase
- RT-PCR:
Real-time reverse-transcriptase polymerase chain reaction.
Data Availability
The data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
References
- 1.Livingston E., Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. 2020. [DOI] [PubMed]
- 2.Adeyinka A., Bailey K., Pierre L., Kondamudi N. COVID 19 infection: pediatric perspectives. Journal of the American College of Emergency Physicians Open . 2021;2(1) doi: 10.1002/emp2.12375.e12375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Geneva, Switzerland: WHO; 2020. Coronavirus Disease (COVID-19). 2020; p. p. 116. Situation Report. [Google Scholar]
- 4.Reuters. FACTBOX-Worldwide Coronavirus Cases Cross 129.34 Million, Death Toll at 2,947,927 . London, UK: Reuters; 2021. https://news.trust.org/item/20210402090114-bcl9v . [Google Scholar]
- 5.Chang T.-H., Wu J.-L., Chang L.-Y. Clinical characteristics and diagnostic challenges of pediatric COVID-19: a systematic review and meta-analysis. Journal of the Formosan Medical Association . 2020;119(5):982–989. doi: 10.1016/j.jfma.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.She J., Liu L., Liu W. COVID‐19 epidemic: disease characteristics in children. Journal of Medical Virology . 2020;92(7):747–754. doi: 10.1002/jmv.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Götzinger F., Santiago-García B., Noguera-Julián A., et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. The Lancet Child & Adolescent Health . 2020;4(9):653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oualha M., Bendavid M., Berteloot L., et al. Severe and fatal forms of COVID-19 in children. Archives de Pediatrie . 2020;27(5):235–238. doi: 10.1016/j.arcped.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ong J. S. M., Tosoni A., Kim Y., Kissoon N., Murthy S. Coronavirus disease 2019 in critically ill children: a narrative review of the literature. Pediatric Critical Care Medicine . 2020;21(7):662–666. doi: 10.1097/pcc.0000000000002376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong Y., Mo X., Hu Y., et al. Epidemiology of COVID-19 among children in China. Pediatrics . 2020;145(6) doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 11.Tsabouri S., Makis A., Kosmeri C., Siomou E. Risk factors for severity in children with coronavirus disease 2019. Pediatric Clinics of North America . 2021;68(1):321–338. doi: 10.1016/j.pcl.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Q., Bastard P., Liu Z., Le Pen J., Moncada-Velez M., Chen J., et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science . 2020;370(6515) doi: 10.1126/science.abd4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahmoudi S., Mehdizadeh M., Shervin Badv R., et al. The coronavirus disease 2019 (COVID-19) in children: a study in an Iranian Children’s referral hospital. Infection and Drug Resistance . 2020;13:2649–2655. doi: 10.2147/idr.s259064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Di Giorgio A., Hartleif S., Warner S., Kelly D. COVID-19 in children with liver disease. Frontiers in Pediatrics . 2021;9:p. 182. doi: 10.3389/fped.2021.616381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alsohime F., Temsah M.-H., Al-Nemri A. M., Somily A. M., Al-Subaie S. COVID-19 infection prevalence in pediatric population: etiology, clinical presentation, and outcome. Journal of Infection and Public Health . 2020 doi: 10.1016/j.jiph.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ogimi C., Englund J. A., Bradford M. C., Qin X., Boeckh M., Waghmare A. Characteristics and outcomes of coronavirus infection in children: the role of viral factors and an immunocompromised state. Journal of the Pediatric Infectious Diseases Society . 2019;8(1):21–28. doi: 10.1093/jpids/pix093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehta N. S., Mytton O. T., Mullins E. W. S., et al. SARS-CoV-2 (COVID-19): what do we know about children? A systematic review. Clinical Infectious Diseases . 2020;71(9):2469–2479. doi: 10.1093/cid/ciaa556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics . 2020;58(4) [Google Scholar]
- 19.Gharehbaghi G., Yousefzadegan S., Javid A., Riazi-Esfahani H., Mousavi A., Mahdavynia S. COVID-19 in children and neonates: a comprehensive review article. Iranian Journal of Pediatrics . 2021;31(1) [Google Scholar]
- 20.CDC COVID-19 Response Team. Coronavirus disease 2019 in children—United States, february 12–april 2, 2020. Morbidity and Mortality Weekly Report . 2020;69(14):p. 422. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Swann O. V., Holden K. A., Turtle L., Pollock L., Fairfield C. J., Drake T. M. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: prospective multicentre observational cohort study. Bmj . 2020;370 doi: 10.1136/bmj.m3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zachariah P., Johnson C. L., Halabi K. C., et al. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a Children’s hospital in New York city, New York. JAMA Pediatrics . 2020;174(10):p. e202430. doi: 10.1001/jamapediatrics.2020.2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sena G. R., Lima T. P. F., Vidal S. A., et al. Clinical characteristics and mortality profile of COVID-19 patients aged less than 20 years old in Pernambuco-Brazil. The American Journal of Tropical Medicine and Hygiene . 2021;104(4):1507–1512. doi: 10.4269/ajtmh.20-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Surendra H., Elyazar I. R., Djaafara B. A., et al. Clinical characteristics and mortality associated with COVID-19 in Jakarta, Indonesia: a hospital-based retrospective cohort study. The Lancet Regional Health-Western Pacific . 2021;9 doi: 10.1016/j.lanwpc.2021.100108.100108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rutgers University. Children face risk for severe complications and death from COVID-19: most of the children admitted to pediatric intensive care units had underlying conditions. ScienceDaily . 2020 http://www.sciencedaily.com/releases/2020/05/200511142153.htm . [Google Scholar]
- 26.Aimen C., Bari A., Rashid J., Alvi Y., Naz F., Rana N., et al. Comorbidity and covid-19 in children-a single center experience. Pakistan Paediatric Journal . 2020;44(4) [Google Scholar]
- 27.Guan W.-J., Ni Z.-Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine . 2020;382(18):1708–1720. doi: 10.1056/nejmoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh A., Saini I., Meena S. K., Gera R. Demographic and clinical profile of mortality cases of COVID-19 in children in New Delhi. Indian Journal of Pediatrics . 2021;88(6):p. 610. doi: 10.1007/s12098-021-03687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang X., Yuan J., Zheng Y., Chen J., Bao Y., Wang Y., et al. Retracted: clinical and epidemiological characteristics of 34 children with 2019 novel coronavirus infection in Shenzhen. Chinese Journal of Pediatrics . 2020;58:p. E008. doi: 10.3760/cma.j.issn.0578-1310.2020.0008. [DOI] [PubMed] [Google Scholar]
- 30.Rahimzadeh G., Ekrami Noghabi M., Kadkhodaei Elyaderani F., et al. COVID-19 infection in Iranian children: a case series of 9 patients. Journal of Pediatrics Review . 2020;8(2):139–144. doi: 10.32598/jpr.8.2.139. [DOI] [Google Scholar]
- 31.Lu X., Zhang L., Du H., et al. SARS-CoV-2 infection in children. New England Journal of Medicine . 2020;382(17):1663–1665. doi: 10.1056/nejmc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu Q., Xing Y., Shi L., Li W., Gao Y., Pan S., et al. Epidemiological and clinical characteristics of children with coronavirus disease. 2019.
- 33.Patel N. A. Pediatric COVID-19: systematic review of the literature. American Journal of Otolaryngology . 2020;41(5) doi: 10.1016/j.amjoto.2020.102573.102573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoang A., Chorath K., Moreira A., et al. COVID-19 in 7780 pediatric patients: a systematic review. EClinicalMedicine . 2020;24 doi: 10.1016/j.eclinm.2020.100433.100433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bellino S., Punzo O., Rota M. C., et al. COVID-19 disease severity risk factors for pediatric patients in Italy. Pediatrics . 2020;146(4) doi: 10.1542/peds.2020-009399. [DOI] [PubMed] [Google Scholar]
- 36.Elmadfa I., Meyer A. L. Patterns of drinking and eating across the European Union: implications for hydration status. Nutrition Reviews . 2015;73(suppl_2):141–147. doi: 10.1093/nutrit/nuv034. [DOI] [PubMed] [Google Scholar]
- 37.Stookey J. D., Allu P. K. R., Chabas D., Pearce D., Lang F. Hypotheses about sub-optimal hydration in the weeks before coronavirus disease (COVID-19) as a risk factor for dying from COVID-19. Medical Hypotheses . 2020;144 doi: 10.1016/j.mehy.2020.110237.110237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCormick D. W., Richardson L. C., Young P. R., et al. Deaths in children and adolescents associated with COVID-19 and MIS-C in the United States. Pediatrics . 2021;148(5) doi: 10.1542/peds.2021-052273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Henry B. M., Benoit S. W., de Oliveira M. H. S., et al. Laboratory abnormalities in children with mild and severe coronavirus disease 2019 (COVID-19): a pooled analysis and review. Clinical Biochemistry . 2020;81 doi: 10.1016/j.clinbiochem.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Henry B. M., Lippi G., Plebani M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clinical Chemistry and Laboratory Medicine . 2020;58(7) doi: 10.1515/cclm-2020-0272. [DOI] [PubMed] [Google Scholar]
- 41.Wang D., Ju X., Xie F., Lu Y., Li F., Huang H., et al. Clinical analysis of 31 cases of 2019 novel coronavirus infection in children from six provinces (autonomous region) of northern China. Zhonghua er ke za zhi . 2020:269–274. doi: 10.3760/cma.j.cn112140-20200225-00138. [DOI] [PubMed] [Google Scholar]
- 42.Lippi G., Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clinical Chemistry and Laboratory Medicine . 2020;58(7):1131–1134. doi: 10.1515/cclm-2020-0198. [DOI] [PubMed] [Google Scholar]
- 43.WHO. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations: Scientific Brief, 27 March 2020 . Geneva, Switzerland: World Health Organization; 2020. [Google Scholar]
- 44.Cao Q., Chen Y.-C., Chen C.-L., Chiu C.-H. SARS-CoV-2 infection in children: transmission dynamics and clinical characteristics. Journal of the Formosan Medical Association . 2020;119(3):670–673. doi: 10.1016/j.jfma.2020.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Størdal K., Bakken I. J., Greve-Isdahl M., Klingenberg C., Helland E., Nystad W., et al. Sars-CoV-2 Hos Barn Og Ungdom I Norge: Påvist Smitte, Sykehusinnleggelser Og Underliggende Tilstander. Tidsskrift for Den norske legeforening . 2020;140 doi: 10.4045/tidsskr.20.0457. [DOI] [PubMed] [Google Scholar]
- 46.Association TAAoPatCsH. Children and COVID-19: state-level data report. 2021. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/
- 47.Surveillances V. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC weekly . 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]
- 48.Dewi R., Kaswandani N., Karyanti M. R., et al. Mortality in children with positive SARS-CoV-2 polymerase chain reaction test: lessons learned from a tertiary referral hospital in Indonesia. International Journal of Infectious Diseases . 2021;107:78–85. doi: 10.1016/j.ijid.2021.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.


