Abstract
Thoracic outlet syndrome (TOS) is defined as compression of neurovascular components passing the thoracic outlet. While neurologic compression is the most common form, rare cases of arterial comprssion could result in concerning cerebral thromboembolic events. Here we present a 15-year-old female with repeated left hemiparesis and radiologic signs of cerebrovascular accident (CVA) in right middle cerebral artery. Further investigations revealed stenosis of the right subclavian artery, saccular aneurysm, and occlusion of the right brachial artery which suggested the diagnosis of arterial TOS. Based on this report, we present this diagnosis as a rare but important cause of CVA, especially in young patients.
Keywords: Arterial thoracic outlet syndrome, Left hemiparesis, Radiologic, Neurovascular
Abbreviations: TOS, thoracic outlet syndrome; CVA, cerebrovascular accident; NIHSS, national health Institute of stroke scale; MCA, middle cerebral artery
Introduction
Thoracic outlet syndrome (TOS) is a broad term referring to a set of disorders with distinct etiologies that lead to compression of neurovascular components passing through and around the thoracic outlet [1]. Thoracic outlet anatomy is defined by a bony circle consisting sternum in front, first rib in lateral side and vertebra posteriorly, additionally the clavicle provides a superior margin for it [2]. The subclavian artery and vein pass through this outlet, while the brachial plexus runs over the top of this area [2].
TOS has congenital or acquired types and is divided into 3 categories: arterial, venous, and neurogenic, based on etiology [3]. Arterial TOS is the rarest and account for only 1%-2% of TOS cases. Cervical ribs are a common cause of TOS, and given the possibility of subclavian artery compression, they have been particularly associated with arterial TOS in a way that they are present in up to 85% of patients [4]. Arterial TOS common presentations range from asymptomatic findings to limb ischemia, and stenosis of arteries. Some studies have reported post-stenotic aneurysms and cerebral thromboembolic events as a rare but important complications of arterial TOS [5], [6], [7], [8], [9]. Left untreated, they can result in severe morbidity. Here, we present a case of multiple common carotid embolic stroke in a young teenager.
Case presentation
A 15-year-old girl with a history of COVID-19 infection 4 months ago was admitted to the hospital with a sudden onset of left hemiparesis, vertigo, and dysarthria. These symptoms started 8 hours before the admission and were alleviated before reaching the hospital. The patient reported intermittent paresthesia and numbness of the left upper limb, which started last year. On the physical exam, the muscle strength of the upper, and lower limbs were both 3:5 on the Medical Research Council (MRC) manual muscle testing grading system [10]. She had mild left hemifacial paresis, and on the National Health Institute of Stroke Scale (NIHSS), she was scored 8.
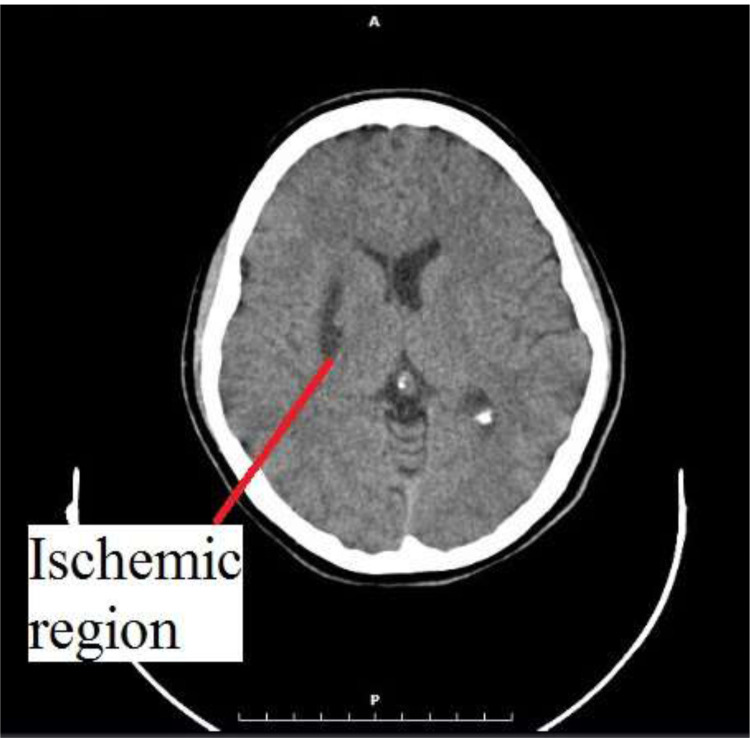
Due to the delay in hospitalization, the golden time was elapsed, and she did not receive recombinant tissue plasminogen activator for thrombolysis. Brain CT scan raised suspicion for temporal ischemia (Fig. 1).
Fig. 1.
Initial brain CT scan suggestive of temporal ischemia.
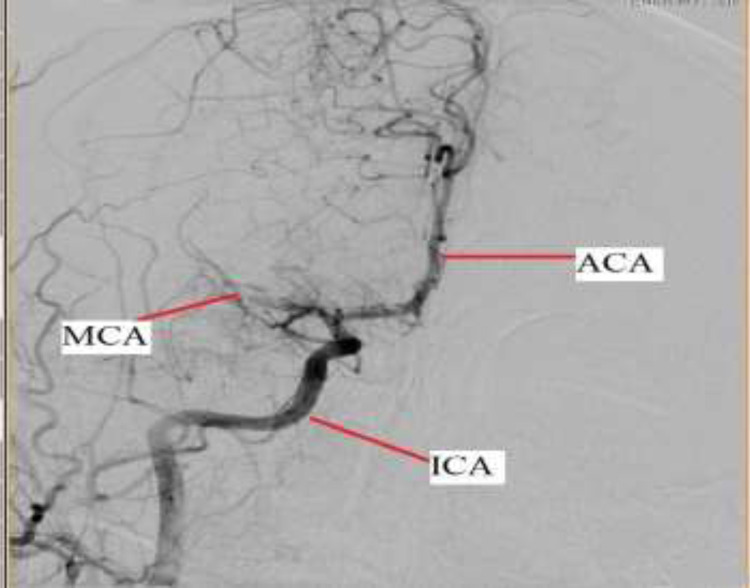
She underwent mechanical thrombectomy in which an occlusion in the right middle cerebral artery (MCA) due to a fresh clot was seen and eliminated (Figs. 2 and 3).
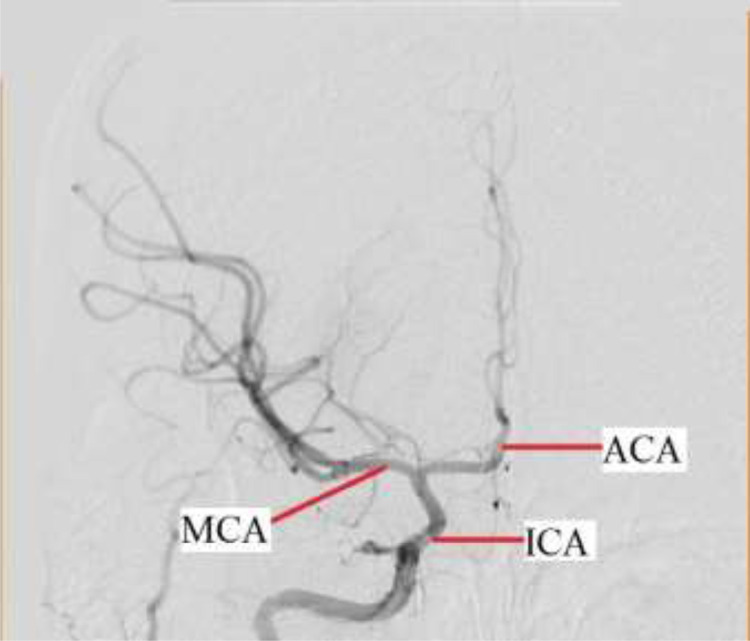
Fig. 2.
Brain angiography after first stroke and before treatment. Middle cerebral artery occlusion is clearly visible. MCA, middle cerebral artery, ACA, anterior cerebral artery, ICA, internal carotid artery.
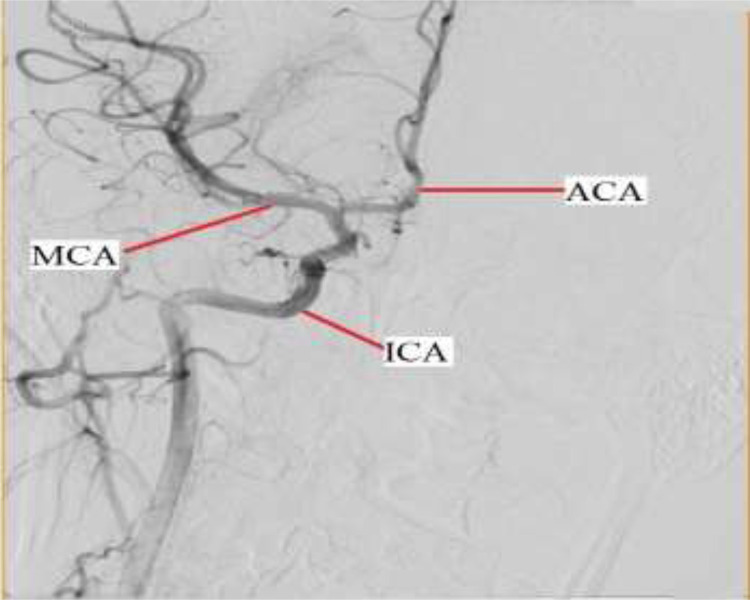
Fig. 3.
Post-treatment brain angiography after first stroke. Reperfusion is evident in middle cerebral artery.MCA, middle cerebral artery, ACA, anterior cerebral artery, ICA, internal carotid artery.
A few hours after the procedure, the muscle force of both affected limbs improved and changed to 4:5; also, dysarthria and facial paresis ameliorated relatively. After that, cardiologic workup, COVID-19 PCR, and vasculitis tests were performed, which did not reveal any pathologic findings. Besides, cervical color-doppler ultrasonography showed no arterial nor venous abnormality. Two days later, the patient's symptoms disappeared, and she was discharged with aspirin 325 mg daily, rosuvastatin 80 mg daily, and pantoprazole 40 mg daily.
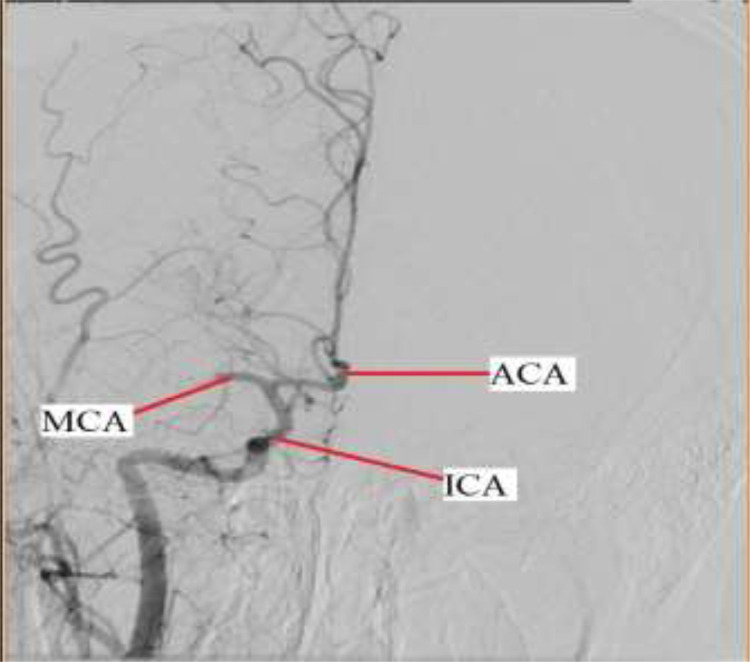
Two weeks later, and while playing basketball, the same symptoms but with more severe characteristics recurred. This time, the muscle strength was 0:5 for both upper and lower left limbs; the patient also had mild dysarthria, left hemifacial paresis, upward plantar reflex, and the calculated NIHSS was ten. Brain CT scan showed a hypodense area in the left basal ganglia. Once again, mechanical thrombectomy was performed, and another occlusion in the right MCA was detected (Figs. 4 and 5).
Fig. 4.
Brain angiography after second stroke and before treatment. Middle cerebral artery is again obstructed. MCA, middle cerebral artery, ACA, anterior cerebral artery, ICA, internal carotid artery.
Fig. 5.
Post-treatment brain angiography after second stroke. Middle cerebral artery occlusion is resolved. MCA, middle cerebral artery, ACA, anterior cerebral artery, ICA, internal carotid artery.
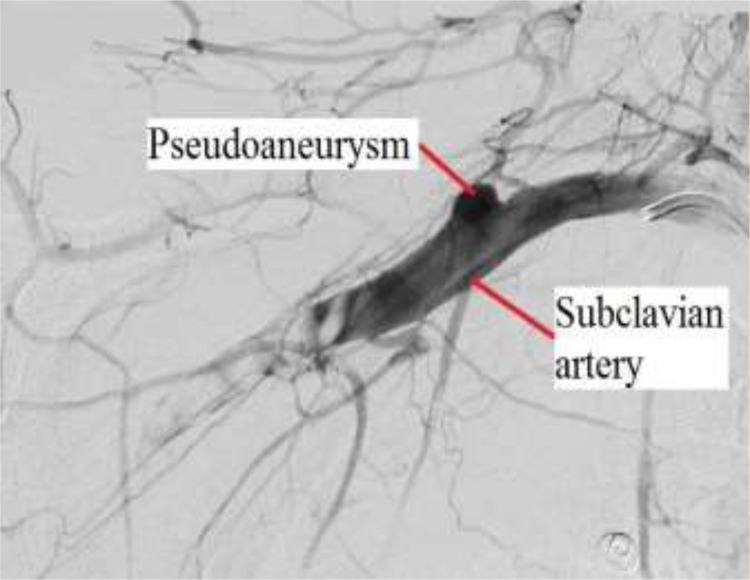
After the occluded artery was reopened, the symptoms resolved, and NIHSS reached zero. We found that the right upper limb was pulseless during the admission, and the blood pressure between the right and left sides was different (right brachial artery systolic blood pressure: 70 mm Hg and left: 120 mm Hg). In addition, her right upper limb was ischemic (Rutherford-Fontaine stage: IIA). A CT angiography was performed to rule out Takayasu's arteritis and examine other vascular abnormalities. It exhibited mild stenosis of the right subclavian artery, saccular aneurysm right after that, and occlusion of the right brachial artery due to a massive fresh clot (Fig. 6).
Fig. 6.
Subclavian artery angiography revealing pseudoaneurysm formation and artery occlusion.
Adson's test and Roos stress test were performed with a suspicion for TOS. Based on the clinical presentations and examination results, patient was diagnosed with TOS, and was treated with heparin infusion to resolve the clot. The patient became a candidate for emergent TOS surgery and right subclavian, axillary, brachial, radial, and ulnar thrombectomy. However, it was decided that operation should be performed after 3-6 months of anticoagulation therapy and organization of the thrombosis.
Further workups showed heterozygote plasminogen activator inhibitor 4G and/or 5G polymorphism and heterozygote methylenetetrahydrofolate reductase C677T polymorphism in this patient. Due to these coagulation factors disorder and 2 life-threatening thrombosis, indefinite anticoagulation therapy with warfarin was indicated, with an INR goal between 2.5, and 3.5.
Discussion
Trauma, repetitive motions and muscle hypertrophy, and anatomic variations such as cervical ribs are some factors that may give rise to TOS [11]. While neurogenic TOS is more common in females, arterial TOS has an equal distribution between genders [3]. Embolic stroke as a rare result of arterial TOS, which is not that common itself, has been long known, and its first hints in literature dates back to 1884 [12]. To date, this condition has not been systematically reviewed. In a review by Meumann et al [6]., 33 patients with stroke or transient ischemic attack associated with subclavian artery disease were identified. In this review, cervical ribs were seen in 26 (78%) patients, the median age among them was 21, and 50% were male. A majority of them (81%) were symptomatic before the occurrence of stroke. In a similar study by Palmer et al [13]., 19 cases were described in which 56% were male, and the mean age was 26.6. In all of these cases, prior signs, and symptoms of limb ischemia were present. As demonstrated above, this problem is mainly seen in young adults.
The prolonged subclavian artery compression by a cervical rib or any other abnormality can lead to intimal damage and, subsequently, atheroma formation. These chronic intimal changes result in turbulent blood flow, which propagates thromboembolic events. In addition, in some cases, post stenosis aneurysms form, and furthers the possibility of thrombosis. In this context, thrombosis is most often present distal to the compression site, but retrograde thrombosis, and central nervous ischemia are still possible[14,15]. Retrograde advancement and formation of thrombosis into the vertebral or common carotid arteries or brief retrograde blood flow in the subclavian artery have been suggested as 2 main explanations for this phenomenon [5,6].
In our case, both thromboembolic events were right-sided, and happened after physical activity. Furthermore, in the second mechanical thrombectomy and angiography, a clot was also observed in the right external carotid artery. No other arterial or venous thrombosis was diagnosed in any other region. These factors suggest TOS as the most probable cause of strokes. As to why the patient's vertebral artery, being more proximal to the compression site, was not thrombosed, it should be noted that given the large emboli in the upper limb and the patient's hypoplastic artery, it was not possible for the clots to pass through and common carotid artery got involved.
Despite the scarcity of arterial TOS, its consequences are more severe, and morbid than neurogenic or venous TOS. After diagnosis, immediate thrombolysis followed by surgical decompression of the thoracic outlet should be performed to alleviate symptoms, and prevent future recurrence. Nevertheless, if thrombectomy is not possible or the artery is compromised, bypass graft is the alternative [14]. Given the serious complications, all physicians should consider arterial TOS, especially in young patients with cervical ribs, pulselessness, different blood pressures across the limbs, and cerebrovascular strokes.
Authors contributions
SHA,FA,MGH,NMKH,BSL,AS,BA, and PD participated the wrote up the draft of the manuscript, helped revise the draft, and approved it. The authors read and approved the final manuscript.
Patient consent
Written informed consent was obtained from the patient family for publication of this case report and accompanying images.
Funding
We have no funding sources to declare.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient family for publication of this case report and accompanying images.
Footnotes
Acknowledgments: Not applicable.
Competing Interests: The authors declare that they have no competing interests
References
- 1.Ferrante MA, Ferrante ND. The thoracic outlet syndromes: Part 1. Overview of the thoracic outlet syndromes and review of true neurogenic thoracic outlet syndrome. Muscle Nerve. 2017;55(6):782–793. doi: 10.1002/mus.25536. [DOI] [PubMed] [Google Scholar]
- 2.Urschel HC. Anatomy of the thoracic outlet. Thorac Surg Clin. 2007;17(4):511–520. doi: 10.1016/j.thorsurg.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB, et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther. 2019;8(1):5–18. doi: 10.1007/s40122-019-0124-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hussain MA, Aljabri B, Al-Omran M. Vascular thoracic outlet syndrome. Semin Thorac Cardiovasc Surg. 2016;28(1):151–157. doi: 10.1053/j.semtcvs.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Celier A, Chabay S, Maurizot A, Cochennec F, Stanciu D, Pico F. Posterior cerebral artery stroke by reverse flow embolism in thoracic outlet syndrome - a case report. BMC Neurol. 2020;20(1):229. doi: 10.1186/s12883-020-01797-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meumann EM, Chuen J, Fitt G, Perchyonok Y, Pond F, Dewey HM. Thromboembolic stroke associated with thoracic outlet syndrome. J Clin Neurosci. 2014;21(5):886–889. doi: 10.1016/j.jocn.2013.07.030. [DOI] [PubMed] [Google Scholar]
- 7.al-Hassan HK, Abdul Sattar M, Eklof B. Embolic brain infarction: a rare complication of thoracic outlet syndrome. A report of two cases. J Cardiovasc Surg (Torino) 1988;29(3):322–325. [PubMed] [Google Scholar]
- 8.Nishibe T, Kunihara T, Kudo FA, Adachi A, Shiiya N, Murashita T, et al. Arterial thoracic outlet syndrome with embolic cerebral infarction. Report of a case. Panminerva Med. 2000;42(4):295–297. [PubMed] [Google Scholar]
- 9.Lee TS, Hines GL. Cerebral embolic stroke and arm ischemia in a teenager with arterial thoracic outlet syndrome: a case report. Vasc Endovascular Surg. 2007;41(3):254–257. doi: 10.1177/1538574407299780. [DOI] [PubMed] [Google Scholar]
- 10.Compston A. Aids to the investigation of peripheral nerve injuries. Medical Research Council: Nerve Injuries Research Committee. His Majesty's Stationery Office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O'Brien for the Guarantors of Brain. Saunders Elsevier: 2010; pp. [8] 64 and 94 Figures. Brain. 2010 Oct;133(10):2838-44. doi: 10.1093/brain/awq270. PMID: 20928945. [DOI] [PubMed]
- 11.Ferrante MA, Ferrante ND. The thoracic outlet syndromes: Part 2. The arterial, venous, neurovascular, and disputed thoracic outlet syndromes. Muscle Nerve. 2017;56(4):663–673. doi: 10.1002/mus.25535. [DOI] [PubMed] [Google Scholar]
- 12.Gould AP. Vol. 17. Trans Clin Soc London; London: 1884. A case of spreading obliterative arteritis; p. 95. [Google Scholar]
- 13.Palmer OP, Weaver FA. Bilateral cervical ribs causing cerebellar stroke and arterial thoracic outlet syndrome: a case report and review of the literature. Ann Vasc Surg. 2015;29(4):840.e1–840.e4. doi: 10.1016/j.avsg.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Daniels B, Michaud L, Sease JrF, Cassas KJ, Gray BH. Arterial thoracic outlet syndrome. Curr Sports Med Rep. 2014;13(2):75–80. doi: 10.1249/JSR.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 15.Bains RD, Platt J, MacGregor D, Borschel GH. Atypical thoracic outlet syndrome and reverse flow thromboembolism. Pediatr Neurol. 2014;51(3):453–456. doi: 10.1016/j.pediatrneurol.2014.04.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.