Abstract
Suicide, a common cause of death in adolescents, is linked to internalizing and externalizing symptoms. These associations are pronounced amongst adolescents who use substances. But these relationships are complex. For example, sex differences are present in association with internalizing/externalizing symptoms as well as differences in suicidality. A rarely explored factor that may account for this complexity as a moderator is callous-unemotional traits. The present study examines associations of internalizing and externalizing in relation to suicidality in the context of callous-unemotional traits amongst adolescents in substance use treatment. Additionally, sex differences were explored. A sample of 317 adolescents (13–18; 16.05±1.22) in treatment for substance use completed measures for internalizing, externalizing, and suicidal symptoms. The main result suggested the presence of CU traits attenuated the positive association between internalizing and a latent suicidality factor. This novel result contextualizes the association between transdiagnostic symptoms and suicidality. Assessing CU traits in the presence of internalizing symptoms may be an important component of understanding suicide risk amongst adolescents in treatment for substance use.
Keywords: Adolescent, Suicide, Internalizing, Externalizing, Callous-unemotional traits
Multiple lines of research support that male and female youth with internalizing and externalizing symptoms have an increased likelihood of suicidality (i.e., attempts and ideation; [For longitudinal meta-analysis see: 1]. Internalizing symptoms account for 61% of the variance for suicidal ideation and attempts [2]. Externalizing symptoms also predict suicide attempts [3]. Both internalizing and externalizing symptoms have a higher prevalence amongst adolescents in substance use treatment [4] and have a stronger association with suicide amongst adolescents who use substances [5, 6]. But there are clear gender differences. For example, prevalence of internalizing conditions are higher in females [7] whereas externalizing symptoms are greater in males [8, 9]. The link between internalizing symptoms and suicidality is greater in females [2] and these associations between males and female hold for adolescent samples in substance use treatment [6]. This line of research demonstrates internalizing and externalizing symptoms account for heterogeneity in suicidality as well as differences between genders. But less is known about whether these associations are different in the presence of other factors.
A factor that may moderate this relationship is callous-unemotional (CU) traits, which is defined by a persistent lack of empathy, guilt, and remorse [10]. Prevalence of CU traits is around 7% of community youth and 32% of adolescents diagnosed with conduct disorder [11]. CU traits are commonly co-morbid with internalizing and externalizing symptoms, which compound behavioral risks across multiple domains [12] such as greater substance use in adolescents; in turn, substance use associates with greater levels of CU traits [e.g., 13, 14]. Suicidality is a greater risk in those with a phenotype of aggression and antisocial behavior [15, 16]. However, CU traits may be protective from suicide because, suicidality involves internally focused rather than externally focused negative affect [17] and those with higher levels of CU traits may be more callous to socialization factors contributing to suicidality [18]. Although rarely examined, CU traits may act as a moderator between suicidality and both internalizing and externalizing symptoms.
We find only one prior study including CU traits when examining suicidality. A study by Javdani, Sadeh [18] found internalizing symptoms (depression) positively associated with suicidality, but CU traits were shown to be protective of suicidal behavior in females. Although these findings are intriguing, weakness included examining internalizing symptoms without accounting for externalizing symptoms, and modeling internalizing symptoms with CU traits so they competed for variance. Inferences on suicidality may be improved by modeling internalizing and externalizing symptoms in one model with CU traits as a moderator. And given the higher prevalence of mortality [e.g., 19], internalizing, and externalizing symptoms in adolescents who use substances, examining samples with higher levels of substance use, such as those in substance use disorder treatment, is critical. Finally, the available literature examines outcomes of either suicide attempts or ideation separately when, given that suicide assessments examine both ideation and past attempts to assess a latent construct of suicidality [20], inferences can be improved by fitting these associations in one model. Here, we address these methodological gaps to advance this line of research.
The present study expands prior research by examining internalizing and externalizing symptoms association with suicidality (including attempts and ideation) with CU traits as a moderator amongst adolescents in treatment for substance use disorders. As reported above, adolescents that use substances demonstrate patterns in suicidality that are similar but more pronounced, therefore we expect to find similar patterns amongst our proposed sample of adolescents in substance use treatment. Externalizing is positively associated with suicide attempts in general population samples; thus, we expect CU traits to moderate the association between externalizing symptoms and suicidality in these adolescent patients. Internalizing positively associates with both suicidal ideation and attempts in general population samples; thus, we expect CU traits to moderate the association between internalizing symptoms with suicidality in these adolescent patients. And, because females differ from males on the associations between internalizing and externalizing symptoms with suicidality [2, 3] as well as because CU traits having a higher prevalence in males [e.g. 21] we expect to see differences in these associations by gender.
Methods
Sample
The current sample was drawn from a larger genetics study approved by Colorado Multiple Institutional Review Board. The study recruited from two large metropolitan adolescent substance use disorder treatment programs (a university-based treatment program and a community hospital-based program). Participants were selected from the larger study if they were (1) adolescents aged 13–18 years old; (2) a participant in one of the clinical programs for substance use disorders; (3) estimated full-scale IQ >= 80; (4) for subjects 17 years of age or younger, valid written consent from parent or guardian, together with assent from the subject, or for subjects 18 years of age, consent from the subject. Participants were excluded if (1) they had a history of psychosis; (2) obvious intoxication at time of interview; (3) current risk of suicide, violence, or fire setting that would interfere with evaluation or to endanger evaluators (though no subject was excluded from the study based on this criterion); and (4) insufficient English skills. This resulted in a sample of 317 adolescent patients (ages 13–18; 16.05±1.22) that were predominantly male (20% female) and White (58%). Demographics listed in Table 1.
Table 1.
Descriptives
| M±SD (min-max) or N (%) | |
|---|---|
|
| |
| Age | 16.05±1.22(13–18) |
| Sex | |
| Male | 253(80%) |
| Female | 65(20%) |
| Race | |
| American Indian | 8(3%) |
| Asian | 1(0.5%) |
| Black | 64(20%) |
| Hispanic | 26(8%) |
| Pacific Islander | 2(0.5%) |
| White | 184(58%) |
| Other | 32(10%) |
| Other diagnoses (lifetime) | |
| Major depression | 68(21%) |
| General anxiety | 45(14%) |
| PTSD | 0(0%) |
| ADHD | 76(24%) |
| Conduct disorder | 178(56%) |
| Oppositional defiant disorder | 104(33%) |
Measures
From the large battery of assessments completed in the parent project, this study utilizes data from the following.
Diagnostic Interview Schedule for Children [DISC; 22].
Adolescents underwent a fully structured diagnostic interview with the child version of the DISC. The DISC consists of several modules for various psychiatric conditions and symptoms. For associations of interest for the present study, we used modules assessing depression, anxiety, oppositional defiant disorder, and conduct disorder. These modules were used to examine internalizing symptoms (depression [19 items] and anxiety [12 items] modules), externalizing symptoms (conduct disorder [19 items] and opposition [12 items] modules) and suicidality (subset of depression module [4 items]). Suicidality indicators covered suicidal ideation, suicide attempts, and suicide planning. The procedures for ascertaining these variables are describes in the analysis section.
Inventory of Callous-Unemotional Traits [ICU; 23].
The ICU is a 24-item comprehensive assessment of callous-unemotional (CU) traits consisting of three subscales: uncaring, unemotional, and callousness. Items such as “I do not show my emotions to others” are rating on a four-point Likert scale from 0 (Not at all true) to 3 (definitely true) where higher scores indicate greater levels of CU traits. The ICU has a confirmed factor structure and demonstrates convergent and divergent validity [24].
Control variables.
Because post-traumatic stress disorder (PTSD) is known to associate with internalizing, externalizing and suicide [25], we used DISC PTSD module overall score as a control, which indicated the number of traumatic events a participant has experienced. We also controlled for age and gender reported on the DISC. Similarly, substance use is associated with internalizing, externalizing, and suicidality [26]. Thus, we also controlled for overall substance use disorder symptoms measured by the Composite International Diagnostic Interview–Substance Abuse Module (CIDI-SAM) [27]. The CIDI-SAM assesses substance abuse and dependence on 10 substances including: alcohol, nicotine, hallucinogens, cocaine, amphetamines, opioids, PCP, sedatives, cannabis, and inhalants. The present analysis used a summary score for substance abuse and dependence for all 10 substances.
Analysis
All analyses were conducted with R software [Version 4.02; 28] using the ‘lavaan’ package for structural equation modeling [29] and two-tailed tests with a p-value < 0.05 defined significance. Prior to analysis, we tested assumptions of our data including distribution normality of residuals, autocorrelation, and multicollinearity. We found two variables from the DISC conduct disorder module that were highly correlated (ycd008= “held someone up or attacked someone to steal” and ycd009= “threatened someone in order to steal”; r=.76) and determined these items would be best fit as correlated error terms in the depression measure used in the final analysis. Assumptions for multivariate normality were met, thus maximum likelihood estimation was deemed appropriate.
Missing data analysis.
We assessed data missingness with the Visualization and Imputation of Missing Values ‘VIF’ package in R [30]; and conducted test for Missing Completely at Random (MCAR) described by Jamshidian and Jalal [31] using the ‘MissMech’ package in R [32]. This MCAR test quantitates homoscedasticity and normality with the missing data using the Hawkins [33] test statistic. Then we tested for systematic reasons for missing values by creating a dichotomous variable for missing values (missing = 1 and not missing = 0) and conducting chi-square or t tests to quantitate any explanations for missing values present [34].
Only 3.8% of data were missing, most of which were from a single item on the depression scale used for suicidality (3.5%). The test for MCAR indicated we could not rule out MCAR (p= 0.69). Follow up analyses found no systematic reasons for the missing values in the data; thus, we did not include any ancillary variables into our analysis. Because the indicators for the measures used in the present study are < 5 indicators they are best handled with the weighted least squares mean and variance adjusted estimator (WLSMV) within the structural equation modeling (SEM) framework [35, 36]. WLSMV can produce unbiased estimates and retain missing values without dropping cases [37].
Identifying internalizing and externalizing symptom dimensions.
A principal components analysis (PCA) was used to reduce the number of internalizing and externalizing items into distinct symptom dimensions using a varimax rotation. Items included in the PCA were from the depression, conduct, oppositional defiant, and anxiety modules of the DISC that were all rated on the same scale (0–2) and relevant for the construct being assessed (e.g., items asking age of symptom onset were omitted). A total of 62 items were included (19 depression, 19 conduct, 12 oppositional defiant, 12 anxiety) comprising internalizing and externalizing dimensions. We randomly sampled 50% of our sample to conduct the PCA and used the remaining 50% to confirm a latent factor structure for analysis. We determined the number of factors by examining a scree plot using the criteria that a factor had to account for at least 7% of additional variance for inclusion [38]. We report on the PCA with the number of factors identified to assess if the factor solution chosen was adequate. As suggested by Comrey and Lee [39], items with factor loadings > 0.55 were considered good fit and retained and used to confirm latent factor structure.
The PCA identified two factors that accounted for 24% of the variance. Given that one construct consisted of items from the conduct and oppositional defiant modules and the other consisted of depression and anxiety modules, these factors represented internalizing and externalizing constructs. A third factor was not apparent in the scree plot and did not contribute significant variance (Δ < 4%) so we retained the two-factor solution. The internalizing construct consisted of ten items and the externalizing construct consisted of five items. The PCA on two factors revealed an adequate solution (X2 = 3097.26, p < 0.001, RMSR = 0.06, diagonal value fit = 0.82) with factor proportional variance of 13% and 11% for internalizing and externalizing factors, respectively (Table 2, Supplementary Figure 1). There were no cross loadings between factors.
Table 2.
PCA loadings
| Item | Internalizing | Externalizing | Item | Internalizing | Externalizing | Item | Internalizing | Externalizing |
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| ymd001 | 0.554 | 0.008 | yga003 | 0.381 | 0.061 | ycd021 | 0.220 | 0.569 |
| ymd002 | 0.533 | 0.024 | yga004 | 0.336 | −0.230 | ycd022 | 0.008 | 0.347 |
| ymd003 | 0.602 | 0.330 | yga005 | 0.342 | 0.078 | ycd023 | 0.027 | 0.376 |
| ymd004 | 0.290 | 0.237 | yga023 | 0.477 | 0.087 | ycd025 | 0.039 | 0.425 |
| ymd005 | 0.445 | 0.101 | yga024 | 0.592 | 0.019 | ycd026 | 0.170 | 0.646 |
| ymd006 | 0.247 | −0.052 | yga025 | 0.481 | 0.043 | ycd027 | 0.036 | 0.434 |
| ymd007 | 0.409 | 0.108 | yga026 | 0.425 | −0.065 | ycd028 | 0.124 | 0.505 |
| ymd008 | 0.489 | 0.177 | yga027 | 0.330 | 0.080 | ycd029 | −0.018 | 0.506 |
| ymd009 | 0.233 | 0.231 | yga028 | 0.304 | 0.093 | yod001 | 0.248 | 0.271 |
| ymd010 | 0.583 | 0.116 | yga029 | 0.350 | 0.104 | yod002 | −0.030 | 0.427 |
| ymd011 | 0.484 | 0.133 | ycd001 | 0.129 | 0.342 | yod003 | 0.118 | 0.377 |
| ymd012 | 0.562 | 0.113 | ycd002 | −0.018 | 0.444 | yod004 | 0.165 | 0.260 |
| ymd013 | 0.623 | 0.223 | ycd003 | 0.054 | 0.547 | yod005 | 0.153 | 0.416 |
| ymd014 | 0.424 | 0.264 | ycd004 | 0.058 | 0.315 | yod006 | 0.305 | 0.396 |
| ymd015 | 0.660 | 0.064 | ycd007 | 0.118 | 0.394 | yod007 | 0.609 | 0.183 |
| ymd016 | 0.670 | −0.073 | ycd008 | −0.114 | 0.549 | yod008 | 0.546 | 0.169 |
| ymd017 | 0.639 | 0.004 | ycd009 | −0.095 | 0.558 | yod009 | 0.428 | 0.243 |
| ymd018 | 0.539 | 0.150 | ycd012 | 0.082 | 0.251 | yod010 | 0.250 | 0.528 |
| ymd019 | 0.472 | 0.253 | ycd018 | −0.003 | 0.360 | yod011 | 0.182 | 0.540 |
| yga001 | 0.383 | −0.006 | ycd019 | −0.094 | 0.639 | yod012 | 0.130 | 0.413 |
| yga002 | 0.330 | −0.126 | ycd020 | 0.133 | 0.574 | |||
Confirmatory factor analyses.
We then conducted confirmatory factor analysis (CFA) on measures prior to fitting the full model. We assessed measure models based on Hu and Bentler [40] criteria for good fit (CFI and TLI ≥ 0.95 and RMSEA ≤ 0.06). If there were issues with model fit, we first removed items with loadings < 0.55, for consistency with the PCA criteria, before reevaluating model fit. Internalizing and externalizing CFA’s were conducted on a subset of the data separate from the dataset the PCA was conducted (i.e., the test subset described above). The suicidality and CU traits measures were confirmed on the entire dataset.
Internalizing and externalizing.
The initial fit of the internalizing measure did not meet a priori criteria (CFI = 0.888, TLI = 0.851, RMSEA = 0.087) and evaluating loadings revealed five items did not load well (Table 3). After removing these items, the internalizing measure fit the data well (CFI = 0.996, TLI = 0.991, RMSEA = 0.33). This final measure had adequate reliability (α= 0.71), so we used this five-item measure in our final analysis (Table 3, Table 4). The initial fit of the externalizing measure fit the data well (CFI = 0.100, TLI = 0.101, RMSEA < 0.001) without additional modifications (Table 3, Table 4). The five-item externalizing measure had adequate reliability (α= 0.73), so we used it in our final model.
Table 3.
CFA loadings
| Measure: | Internalizing |
Externalizing |
Suicidality |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model: | Initial |
Final |
Final |
Final |
||||||
| Items | loading | P Value | loading | P Value | Items | loading | P Value | Items | loading | P Value |
|
| ||||||||||
| Ymd001 | 0.47 | < 0.001 | -- | -- | ycd009 | 0.54 | < 0.001 | ymd020 | 0.54 | < 0.001 |
| Ymd003 | 0.50 | < 0.001 | -- | -- | ycd019 | 0.55 | < 0.001 | ymd021 | 0.75 | < 0.001 |
| Ymd010 | 0.47 | < 0.001 | -- | -- | ycd020 | 0.67 | < 0.001 | ymd022 | 0.58 | < 0.001 |
| Ymd013 | 0.56 | < 0.001 | 0.55 | < 0.001 | ycd021 | 0.72 | < 0.001 | ymda9y | 0.74 | < 0.001 |
| Ymd015 | 0.61 | < 0.001 | 0.62 | < 0.001 | ycd026 | 0.55 | < 0.001 | |||
| Ymd016 | 0.57 | < 0.001 | 0.58 | < 0.001 | ||||||
| Ymd017 | 0.55 | < 0.001 | 0.55 | < 0.001 | ||||||
| Yga024 | 0.57 | < 0.001 | 0.61 | < 0.001 | ||||||
| Yod007 | 0.47 | < 0.001 | -- | -- | ||||||
Table 4.
Measure CFA Model Fits
| Model | X2(df) | CFI | TLI | RMSEA | Cronbach’s alpha |
|---|---|---|---|---|---|
|
| |||||
| Internalizing | |||||
| Initial Model | 90.69(27) | 0.888 | 0.851 | 0.087 | -- |
| Final Model | 12.54(5) | 0.996 | 0.991 | 0.033 | 0.712 |
| Externalizing | |||||
| Final Model | 8.181(5) | 1.000 | 1.001 | 0.000 | 0.725 |
| Suicidality | |||||
| Final Model | 12.42(2) | 0.991 | 0.973 | 0.052 | 0.687 |
| Callous-Unemotional Traits | |||||
| Final model* | 395.85(181) | 0.927 | 0.907 | 0.059 | 0.690 |
= measure replicated previous literature CFA fit
Suicidality.
The suicidality measure consisted of four items involving a subset of the depression module. Items addressed suicidal plans, thoughts, and attempts. The initial theoretical model met a priori criteria for good fit (CFI = 0.991, TLI = 0.973, RMSEA = 0.052) without additional modifications and had adequate reliability (α= 0.69).
Callous-Unemotional traits.
For the Inventory of Callous-Unemotional Traits (ICU) we fit the model confirmed by Kimonis, Frick [24] including the model specification, items for latent factors, and correlated residuals. In this original paper, the ICU did not meet criteria for good fit specified a priori here; thus, we used this as a reference for what to expect with the current factor structure. Our current analysis replicated the previously confirmed the ICU structure (CFI= 0.927, TLI= 0.907, RMSEA= 0.059) with adequate reliability (α = 0.69). All the above measures were appropriate for use in the formal analysis.
Structural equation modeling.
An SEM was fit to test the study’s hypotheses. Given that the ICU factor structure was replicated in the current sample, we parceled the three ICU subscales to estimate the CU traits latent structure in order to improve estimation of model fit and moderating terms by reducing the number of parameters [41]. We then calculated moderating terms using the R package ‘semTools’ [42] for residual centering to eliminate nonessential multicollinearity proposed by Little, Card [43] that uses every indicator combination.
Model estimation was evaluated for adequate fit using criteria of both TLI and CFI ≥ 0.90, and RMSEA ≤ 0.06 [40, 44]. Seven influential outliers were detected using Cook’s D cutoff criteria (D(i) > 4/n; [45] that was calculated with the R package “influence.SEM” [46]. These outliers were removed from proceeding analyses and figures. We modeled moderating terms of internalizing and externalizing symptoms with CU traits associating with suicidality latent factor. We also considered estimating separate parameters for males and females using a multigroup SEM approach and probed for differences in the magnitude of regression parameters using a likelihood ratio test. Moderating term effects were tested using 1000 bootstrap resamples and then modeled by calculating the − 1SD, mean SD, and +1SD of ICU for significant moderating effects observed in the model.
Results
The model fit the data well (X2(1142)= 1130.31, CFI = 1.00, TLI= 1.020, RMSEA= 0.057) without re-specification, accounted for 72% of the variance in latent suicidality (R2= 0.715). Results indicate internalizing symptoms were associated with higher suicidality (γ= 0.87, p< 0.001), but that, after controlling for other factors, the presence of callous unemotional traits changed this relationship (γ= − 0.11, p= 0.049) (Table 5, Figure 1, Figure 2). Modeling moderating effects suggest all paths were significant and positive (−1SD β= 0.92, p< 0.001; μ β= 0.87, p< 0.001; +1SD β= 0.81, p< 0.001). Externalizing had no significant direct association with suicidality or moderating effect.
Table 5.
Structural Equation Model Results (n= 310)
| Unstandardized Estimate | Standard Error | Standardized Estimate | Z score | P value | Bootstrapped 95% CI |
||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
|
| |||||||
| Suicidal (R2=0.715) | |||||||
| Externalizing | 0.220 | 0.247 | 0.105 | 0.889 | 0.374 | −0.265 | 0.704 |
| Internalizing | 0.868* | 0.127 | 0.686 | 6.82 | <0.001 | 0.618 | 1.117 |
| CU traits | −0.049 | 0.03 | −0.188 | −1.65 | 0.099 | −0.106 | 0.009 |
| CU traits*Internalizing | −0.111* | 0.057 | −0.234 | −1.967 | 0.049 | −0.143 | −0.095 |
| CU traits*Externalizing | 0.028 | 0.132 | 0.018 | 0.213 | 0.831 | −0.028 | 0.114 |
| Age | 0.074 | 0.044 | 0.12 | 1.691 | 0.091 | −0.012 | 0.159 |
| Gender | −0.457* | 0.135 | −0.269 | −3.381 | 0.001 | −0.723 | −0.192 |
| PTSD | 0.041 | 0.022 | 0.111 | 1.872 | 0.061 | −0.001 | 0.084 |
| Substance Use | −0.009 | 0.038 | −0.022 | −0.23 | 0.818 | −0.082 | 0.065 |
| Moderation: CU*Internalizing | |||||||
| CU −1 SD | 0.924* | 0.132 | 0.803 | 7.001 | <0.001 | 0.665 | 1.182 |
| CU mean SD | 0.869* | 0.127 | 0.687 | 6.824 | <0.001 | 0.619 | 1.118 |
| CU +1 SD | 0.814* | 0.129 | 0.571 | 6.319 | <0.001 | 0.561 | 1.066 |
Model Fit: Chi-square(df)= 1130.312(1142); CFI = 1.000; TLI= 1.020; RMSEA= 0.057
CU = Callous-Unemotional traits
p<.05
Figure 1.
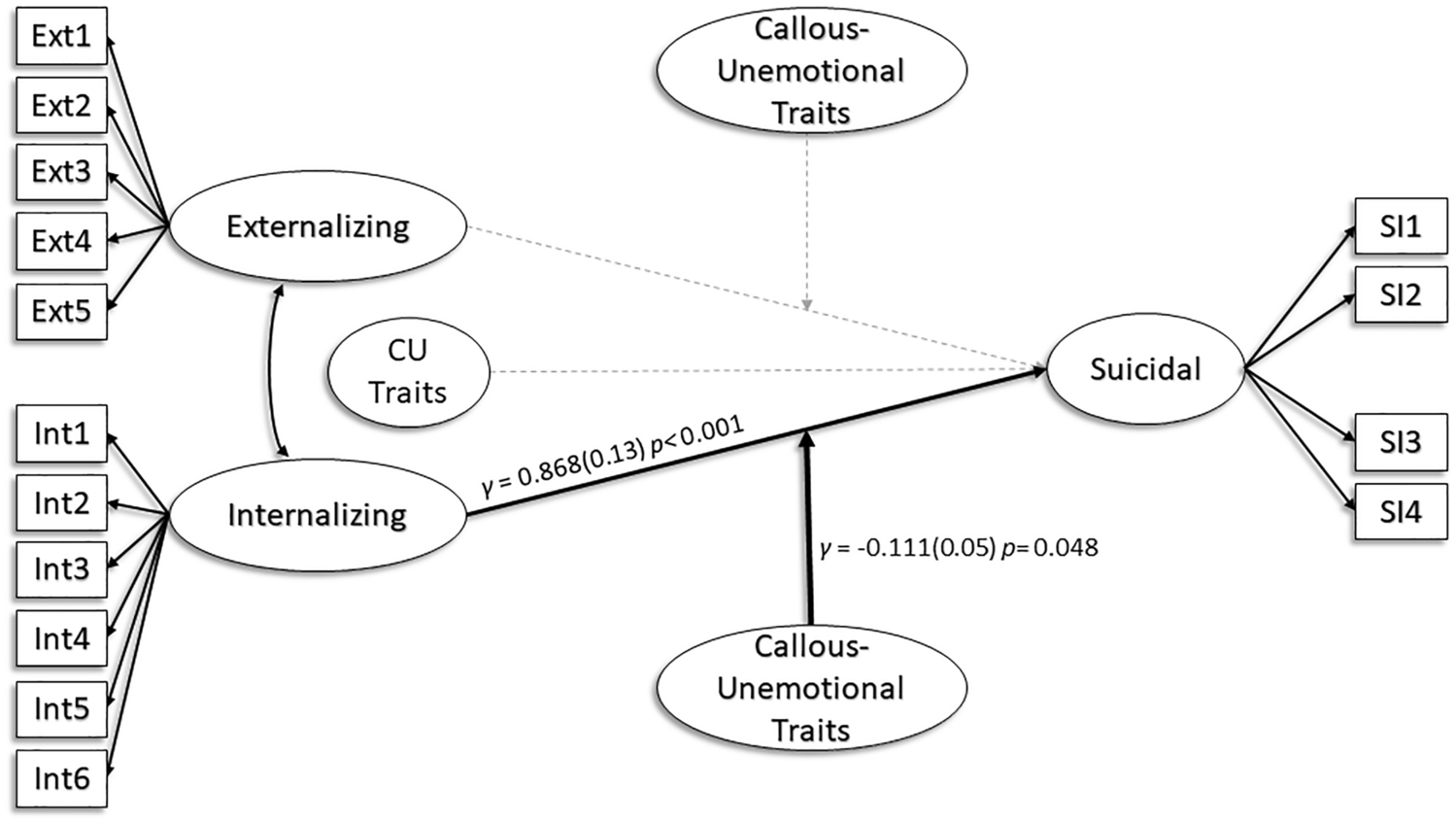
Description of structural equation model. Solid lines indicate significant paths and dotted lines indicate insignificant paths.
Figure 2.
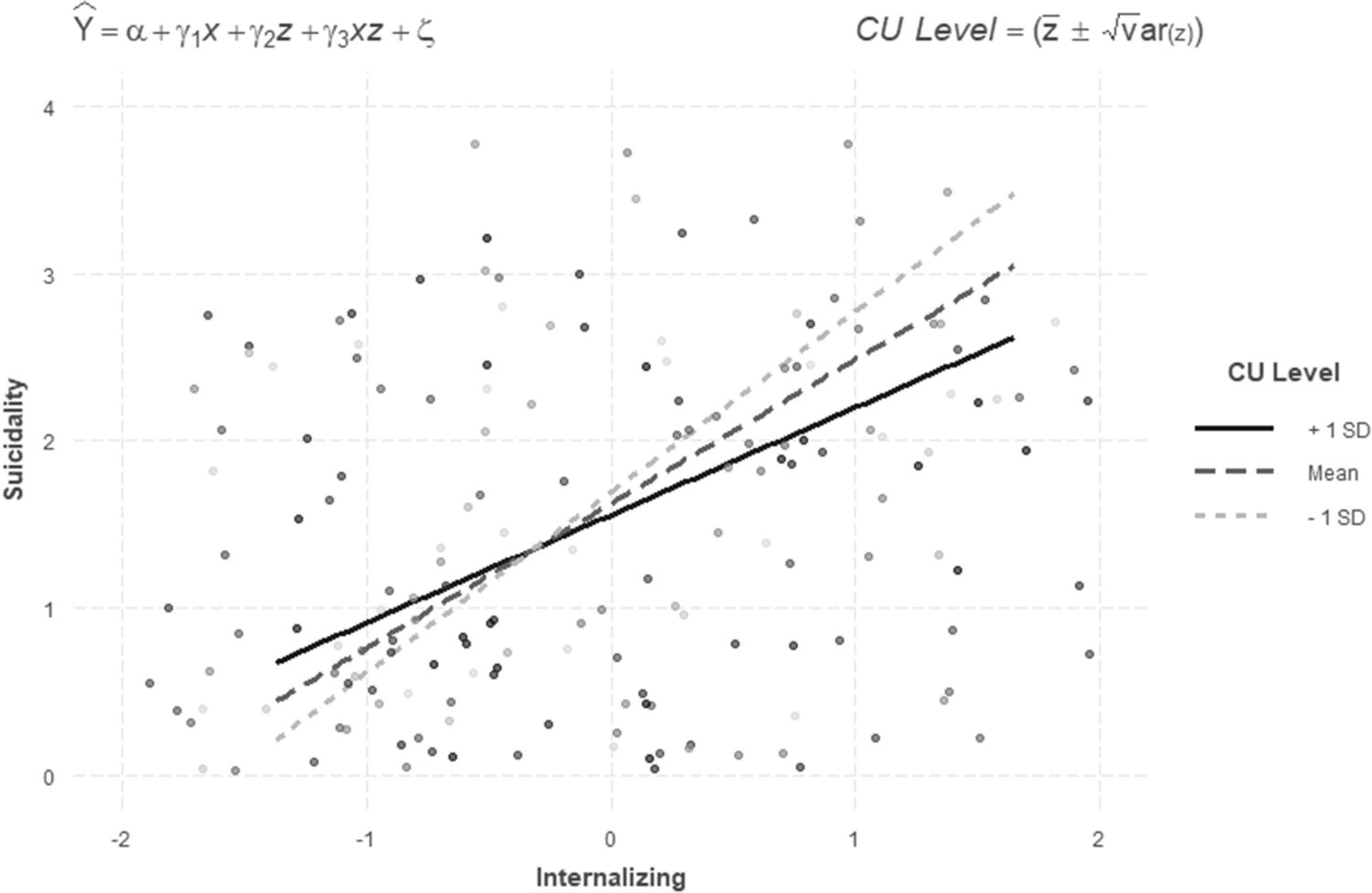
Depiction of moderating effect of callous-unemotional (CU) traits on internalizing in relatoin to suicidality.
Gender and control effects.
For gender, females associated with greater suicidality when reference to males (γ= − 0.46, p= 0.001). Multigroup comparisons were unable to be examined because configural invariance across genders was not established (X2(2132) = 5131.51, CFI = 0.682, TLI= 0.619, RMSEA= 0.095). Overall control variables did not significantly predict suicidality.
Other Null Results.
All other control variables were not significant. These included PTSD symptoms, age, and substance use (see Table 5).
Discussion
The present analysis provides evidence that CU traits moderates the association between internalizing symptoms and suicidality. Externalizing symptoms did not significantly associate with suicidality. Females were more likely than males to greater suicidality. These results compliment and extend previous work [1–8] by characterizing internalizing and externalizing symptoms association with suicidality in the presence of CU traits.
Internalizing positively associated with suicidality after controlling for other covariates, and this association was attenuated in the presence of CU traits. The literature supports internalizing symptoms positive association with suicidal ideation and attempts [e.g., 1, 2]; but the finding that CU traits moderates this association is a novel contribution. It is plausible the attenuation of this association is a result of CU traits callous disregard for feelings of others also applies to oneself. For example, adolescents with CU traits may be more callous toward themselves and their own emotional experiences [e.g. 47, 48]. It may be that CU traits protect against general suicidality due to less reactivity to internalizing symptoms when present. Another consideration is that CU traits associate with externalizing negative affect during emotions like fear [e.g. 49] whereas suicidality associates with internalized negative affect [17]. It may be this redirection of negative affect protects from general suicidality. Suicide in adolescents is a complex issue and this finding future contextualizes this complexity.
Externalizing did not associate with suicidality as expected and CU traits did not interact with this association. CU traits is often comorbid with externalizing conditions [50] and is a specifier for the externalizing condition conduct disorder [51]. Thus, it is possible the interaction of these symptoms may not have accounted for variance beyond externalizing.
Gender differences were present for the latent construct of suicidality. This is well supported in the literature. For example, females have higher rates of suicidal ideation and attempts but males have higher rates of serious suicidal attempts and suicide completions [52, 53]. Overall, gender differences in the latent construct of suicide are well supported in the literature and the current finding adds specificity when considering CU traits and transdiagnostic symptoms.
Limitations.
The present results must be interpreted under some limitations. First, data were from a cross-sectional dataset and we cannot determine causality. Next, the suicidality measure was derived from a depression module of the DISC. However, because criteria for internalizing and depression associate with suicidal ideation and assessing suicide involves the same line of questioning, it is probable suicidal assessments border on internalizing and depressive symptoms. Males and females had disparate sample sizes and the current results need to be confirmed in samples with greater proportion of females. And finally, the internalizing and externalizing measures were derived from separate partitions of one sample. It may be that these measures only describe the current sample of adolescents in substance use disorder treatment and testing with other substance using adolescents is necessary to confirm.
Conclusions.
The present findings have implications for improving models of suicidality in adolescents in substance use disorder treatment. Specifically, CU traits attenuates internalizing symptoms association with suicidality. Practically, assessing callous-unemotional traits when conducting a suicide assessment for youth in substance use treatment may be an important consideration. For research, it is important to consider CU traits when examining suicidality in adolescents to future parse these complex associations. This line of research has promise to improve our understanding of suicidal behavior in adolescents with higher levels of substance use.
Summary
Suicide is linked with internalizing and externalizing symptoms and has even stronger links in adolescents who use substances; however, a relatively unexplored factor with a higher prevalence amongst adolescents who use substances that plausibly moderates suicidality is callous-unemotional (CU) traits. The present study extends research on adolescent suicidality by examining CU traits as a moderator for the association between internalizing and externalizing symptoms association with suicidality. We recruited 317 adolescents (ages 13–18; 16.05±1.22) in substance use treatment. Participants completed measures for CU traits (Inventory of Callous-Unemotional Traits) and symptom measures for internalizing, externalizing, and suicidality (Diagnostic Interview Schedule for Children). A structural equation model was used to estimate measurement and structural paths between these variables, including CU traits as a moderator. Results revealed that increased in internalizing associated with higher suicidality and the presence of CU traits attenuated this relationship. This novel finding contextualizes the association between transdiagnostic symptoms and suicidality; and that assessing CU traits in the presence of internalizing may be an important component of understanding suicide risk amongst adolescents in treatment for substance use.
Supplementary Material
Supplementary Figure 1. Depiction of PCA loadings for internalizing and externalizing symptoms.
Acknowledgments
Drew E Winters, PhD. was supported by a training grant from National Institutes of Mental Health, T32MH015442
Christian Hopfer was supported by two grants from National Institute on Drug abuse DA032555 and DA042755
References
- 1.Soto-Sanz V, et al. , Internalizing and externalizing symptoms and suicidal behaviour in young people: a systematic review and meta-analysis of longitudinal studies. Acta Psychiatr Scand, 2019. 140(1): p. 5–19. [DOI] [PubMed] [Google Scholar]
- 2.Piqueras JA, et al. , What is the Role of Internalizing and Externalizing Symptoms in Adolescent Suicide Behaviors? Int J Environ Res Public Health, 2019. 16(14). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verona E, Sachs-Ericsson N, and Joiner TE Jr, Suicide attempts associated with externalizing psychopathology in an epidemiological sample. American Journal of Psychiatry, 2004. 161(3): p. 444–451. [DOI] [PubMed] [Google Scholar]
- 4.Chan Y-F, Dennis ML, and Funk RR, Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of substance abuse treatment, 2008. 34(1): p. 14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Esposito-Smythers C and Spirito A, Adolescent substance use and suicidal behavior: a review with implications for treatment research. Alcohol Clin Exp Res, 2004. 28(5 Suppl): p. 77s–88s. [DOI] [PubMed] [Google Scholar]
- 6.Ramchand R, et al. , A prospective investigation of suicide ideation, attempts, and use of mental health service among adolescents in substance abuse treatment. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors, 2008. 22(4): p. 524–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ford DE and Erlinger TP, Depression and C-Reactive Protein in US Adults: Data From the Third National Health and Nutrition Examination Survey. Archives of Internal Medicine, 2004. 164(9): p. 1010–1014. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, et al. , Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of general psychiatry, 1994. 51(1): p. 8–19. [DOI] [PubMed] [Google Scholar]
- 9.Newman DL, et al. , Psychiatric disorder in a birth cohort of young adults: prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. Journal of consulting and clinical psychology, 1996. 64(3): p. 552. [PubMed] [Google Scholar]
- 10.Frick PJ and White SF, Research review: The importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. Journal of child psychology and psychiatry, 2008. 49(4): p. 359–375. [DOI] [PubMed] [Google Scholar]
- 11.Kahn RE, et al. , The effects of including a callous-unemotional specifier for the diagnosis of conduct disorder. Journal of child psychology and psychiatry, and allied disciplines, 2012. 53(3): p. 271–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fanti KA and Kimonis E, Heterogeneity in externalizing problems at age 3: Association with age 15 biological and environmental outcomes. Developmental psychology, 2017. 53(7): p. 1230. [DOI] [PubMed] [Google Scholar]
- 13.Sakai JT, et al. , Imaging decision about whether to benefit self by harming others: Adolescents with conduct and substance problems, with or without callous-unemotionality, or developing typically. Psychiatry Research: Neuroimaging, 2017. 263(Supplement C): p. 103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Winters DE, et al. , Systematic review and meta-analysis of socio-cognitive and socio-affective processes association with adolescent substance use. Drug and Alcohol Dependence, 2020: p. 108479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bukstein O, et al. , Risk factors for completed suicide among adolescents with a lifetime history of substance abuse: a case-control study. Acta Psychiatrica Scandinavica, 1993. 88(6): p. 403–408. [DOI] [PubMed] [Google Scholar]
- 16.Goldston DB, et al. , Suicide attempts among formerly hospitalized adolescents: A prospective naturalistic study of risk during the first 5 years after discharge. Journal of the American Academy of Child & Adolescent Psychiatry, 1999. 38(6): p. 660–671. [DOI] [PubMed] [Google Scholar]
- 17.Burke TA, et al. , Cognitive Risk and Protective Factors for Suicidal Ideation: A Two Year Longitudinal Study in Adolescence. Journal of abnormal child psychology, 2016. 44(6): p. 1145–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Javdani S, Sadeh N, and Verona E, Suicidality as a function of impulsivity, callous– unemotional traits, and depressive symptoms in youth. Journal of Abnormal Psychology, 2011. 120(2): p. 400–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Border R, et al. , Independent predictors of mortality in adolescents ascertained for conduct disorder and substance use problems, their siblings and community controls. Addiction, 2018. 113(11): p. 2107–2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Posner K, et al. , Factors in the assessment of suicidality in youth. CNS spectrums, 2007. 12(2): p. 156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fragkaki I, Cima M, and Meesters C, The association between callous–unemotional traits, externalizing problems, and gender in predicting cognitive and affective morality judgments in adolescence. Journal of youth and adolescence, 2016. 45(9): p. 1917–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shaffer D, et al. , NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 2000. 39(1): p. 28–38. [DOI] [PubMed] [Google Scholar]
- 23.Frick PJ, The inventory of callous-unemotional traits. Unpublished rating scale, 2004. [Google Scholar]
- 24.Kimonis ER, et al. , Assessing callous–unemotional traits in adolescent offenders: Validation of the Inventory of Callous–Unemotional Traits. International journal of law and psychiatry, 2008. 31(3): p. 241–252. [DOI] [PubMed] [Google Scholar]
- 25.Chou P-H, Ito M, and Horikoshi M, Associations between PTSD symptoms and suicide risk: A comparison of 4-factor and 7-factor models. Journal of Psychiatric Research, 2020. [DOI] [PubMed] [Google Scholar]
- 26.Yuodelis-Flores C and Ries RK, Addiction and suicide: a review. The American journal on addictions, 2015. 24(2): p. 98–104. [DOI] [PubMed] [Google Scholar]
- 27.Cottler LB, Robins LN, and Helzer JE, The reliability of the CIDI-SAM: a comprehensive substance abuse interview. British journal of addiction, 1989. 84(7): p. 801–814. [DOI] [PubMed] [Google Scholar]
- 28.R Core Team, R: A language and environment for statistical computing. R Foundation for Statistical Computing. 2021, Vienna, Austria: URL https://www.R-project.org/. [Google Scholar]
- 29.Rosseel Y, Lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 2012. 48(2): p. 1–36. [Google Scholar]
- 30.Kowarik A and Templ M, Imputation with the R Package VIM. Journal of Statistical Software, 2016. 74(7): p. 1–16. [Google Scholar]
- 31.Jamshidian M and Jalal S, Tests of homoscedasticity, normality, and missing completely at random for incomplete multivariate data. Psychometrika, 2010. 75(4): p. 649–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mortaza J, Siavash J, and Camden J, MissMech: An R Package for Testing Homoscedasticity, Multivariate Normality, and Missing Completely at Random (MCAR). Journal of Statistical Software, 2014. 56(6): p. 1–31. [Google Scholar]
- 33.Hawkins DM, A new test for multivariate normality and homoscedasticity. Technometrics, 1981. 23(1): p. 105–110. [Google Scholar]
- 34.Little RJA and Rubin DB, Statistical Analysis with Missing Data. 2019: Wiley. [Google Scholar]
- 35.Bovaird JA and Koziol NA, Measurement models for ordered-categorical indicators, in Handbook of structural equation modeling, R.H.H. (Ed.), Editor. 2012, The Guilford Press. p. 495–511. [Google Scholar]
- 36.Rhemtulla M, Brosseau-Liard PÉ, and Savalei V, When can categorical variables be treated as continuous? A comparison of robust continuous and categorical SEM estimation methods under suboptimal conditions. Psychological methods, 2012. 17(3): p. 354. [DOI] [PubMed] [Google Scholar]
- 37.Asparouhov T and Muthén B Weight least squared estimation with missing data. 2010; Available from: https://www.statmodel.com/download/GstrucMissingRevision.pdf
- 38.MacCallum RC, et al. , Sample size in factor analysis: The role of model error. Multivariate behavioral research, 2001. 36(4): p. 611–637. [DOI] [PubMed] [Google Scholar]
- 39.Comrey AL and Lee HB, A first course in factor analysis. 2013: Psychology press. [Google Scholar]
- 40.Hu L.t. and Bentler PM, Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal, 1999. 6(1): p. 1–55. [Google Scholar]
- 41.Little TD, et al. , Why the items versus parcels controversy needn’t be one. Psychological methods, 2013. 18(3): p. 285–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jorgensen TD, et al. , semTools: Useful tools for structural equation modeling. R package version 0.5–1, 2018. [Google Scholar]
- 43.Little TD, et al. , Structural equation modeling of mediation and moderation with contextual factors. Modeling contextual effects in longitudinal studies, 2007. 1: p. 207–230. [Google Scholar]
- 44.Mulaik SA, et al. , Evaluation of goodness-of-fit indices for structural equation models. Psychological bulletin, 1989. 105(3): p. 430. [Google Scholar]
- 45.Cook RD and Weisberg S, Residuals and influence in regression. 1982: New York: Chapman and Hall. [Google Scholar]
- 46.Pastore M and Altoe G, influence.SEM: Case Influence in Structural Equation Models. R Foundation for Statistical Computing, 2018. [Google Scholar]
- 47.Berg JM, et al. , The Inventory of Callous and Unemotional Traits: A constructvalidational analysis in an at-risk sample. Assessment, 2013. 20(5): p. 532–544. [DOI] [PubMed] [Google Scholar]
- 48.Morley RH, Violent criminality and self-compassion. Aggression and Violent Behavior, 2015. 24: p. 226–240. [Google Scholar]
- 49.Cardinale EM, et al. , Externalizing behavior severity in youths with callous-unemotional traits corresponds to patterns of amygdala activity and connectivity during judgments of causing fear. Dev Psychopathol, 2018. 30(1): p. 191–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Herpers PC, et al. , Callous–unemotional traits as a cross-disorders construct. Social psychiatry and psychiatric epidemiology, 2012. 47(12): p. 2045–2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders. 5th ed. 2013, Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- 52.Allison S, et al. , Gender differences in the relationship between depression and suicidal ideation in young adolescents. Australian & New Zealand Journal of Psychiatry, 2001. 35(4): p. 498–503. [DOI] [PubMed] [Google Scholar]
- 53.Freeman A, et al. , A cross-national study on gender differences in suicide intent. BMC Psychiatry, 2017. 17(1): p. 234. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. Depiction of PCA loadings for internalizing and externalizing symptoms.


