Abstract
Object:
The Affordable Care Act expanded Medicaid eligibility in many states, improving access to some forms of elective healthcare in the United States. Whether this effort increased access to elective spine surgical care is unknown. This study’s objective was to evaluate the impact of Medicaid expansion under the Affordable Care Act on the volume and payer mix of elective spine surgery in the United States.
Methods
This study evaluated elective spine surgeries using all-payor state inpatient databases from 2011–2016 from 10 states that did and four states that did not expand Medicaid access in 2014. Adult patients aged 18 to 64 years undergoing elective spine surgery were included. We used a quasi-experimental difference-in-difference design to evaluate the impact of Medicaid expansion on hospital procedure volume and payer mix, independent of any time-dependent trends. Subgroup analyses were conducted that stratified results by cervical fusion, thoracolumbar fusion, and non-instrumented surgery.
Results:
We identified 218,648 surgeries in 10 Medicaid expansion states and 118,693 in 4 non-expansion states. Medicaid expansion was associated with a 17% (95% CI 2%-35%; p=0.03) increase in mean hospital spine surgical volume, and a 23% (95% CI −0.3%-52%; p=0.054) increase in Medicaid volume. Privately insured surgical volumes did not change significantly (incidence rate ratio=1.13; 95% CI −5%-34%; p=0.18). The rise in Medicaid volumes led to a shift in payer mix, with the proportion of Medicaid patients rising by 6.0 percentage points (95% CI 4.1–7.0; p<0.001), and the proportion of private payers decreasing by 6.7 percentage points (95% CI 4.5–8.8; p<0.001). While the magnitude of the effects varied, these trends were similar across procedure subgroups.
Conclusion:
Medicaid expansion under the Affordable Care Act was associated with an economically and statistically significant increase in spine surgery volume and the proportion of surgical patients with Medicaid insurance, indicating improved access to care.
Keywords: access to healthcare, health service research, spine surgery, Medicaid, patient protection and affordable care act, administrative data research
Introduction:
In an attempt to expand healthcare access, the United States Congress passed the Patient Protection and Affordable Care Act (ACA) in 2010, representing the largest overall change to health insurance in the United States since the establishment of Medicaid and Medicare.1 Among other provisions, the ACA provided federal support for states to expand their Medicaid programs to increase coverage.1 Since the ACA was passed, more than 20 million Americans have gained health insurance, with the majority of the new coverage being in the form of increased access to Medicaid.2 Nonetheless, both the impact and legality of the ACA continue to be the subject of ongoing debate and litigation,3 highlighting the importance of studying the effects of Medicaid expansion on healthcare delivery.
A large body of evidence has demonstrated positive effects associated with Medicaid expansion, including improved access to care and healthcare quality across a variety of conditions.4 Although many of these studies have focused on access to medical care,5–8 there is growing evidence suggesting that Medicaid expansion also improved access to some forms of elective surgical care.6,8–10 For elective orthopedic disease, evidence has been more limited. For example, one study in New York state found increased use of a variety of orthopedic procedures following Medicaid expansion,9 and Medicaid expansion was associated with improved access to joint arthroplasty.6 Nonetheless, other studies have shown that Medicaid patients face ongoing barriers to access elective orthopedic care.11
Ensuring access to degenerative spine care is a particularly important priority, given that degenerative spine disease is among the most common and disabling health conditions in the United States and worldwide.12,13 However, there is sparse evidence describing the impact of Medicaid expansion under the ACA on access to spine surgical care. Preliminary investigations evaluating healthcare reform in Massachusetts yielded mixed results regarding the extent to which Medicaid expansion influenced spine surgery access and quality.14 For example, one investigation found that rates of surgical intervention for cervical spine fractures were unchanged after health reform, but several markers of quality improved.15
Given these limited and inconclusive results, focused attention is needed to identify the extent to which the ACA impacted access to spine care, particularly for elective surgeries where physicians may have more discretion in determining whether to offer a surgery based on patient insurance status. Consequently, the objective of this study was to evaluate the impact of the ACA on elective spine surgical care, including both treatment rates and payer mix. As a secondary objective, we evaluated the extent to which the impact of Medicaid expansion varied by specific procedure type.
Material and Methods:
Study Dataset
Data for this study came primarily from State Inpatient Databases (SID) provided by the Healthcare Cost and Utilization Project supported by the Agency for Healthcare Research and Quality. The SID are administrative billing databases that included all discharges from non-federal hospitals in participating states.16 We used the SID from the following selection of geographically and socially diverse states: Arizona, Arkansas, Colorado, Florida, Iowa, Maryland, Nebraska, New Jersey, Nevada, New York, Wisconsin, Washington, and Vermont. In addition, we obtained Missouri inpatient discharge data from the Hospital Industry Data Institute (HIDI; Missouri Hospital Association, Jefferson City, MO). Together, these sources provided comprehensive information on all non-federal discharges in ten states that did and four states that did not expand Medicaid access in 2014.
Patient Selection
We included patients between 18 and 64 years who underwent elective spine surgery in participating states between 2011 and 2016. We excluded patients with Medicare and other (e.g. military, worker’s compensation, and other government) insurance coverage, as these populations would not be expected to benefit from Medicaid expansion. In the overall analysis, we included patients who underwent spinal fusion, cervical arthroplasty, or non-instrumented surgery (laminectomy and/or discectomy). We also conducted subgroup analyses in patients who underwent cervical spine fusion, thoracolumbar or lumbosacral fusion, or non-instrumented spine surgery. The cervical arthroplasty group was not analyzed independently due to its small size. The complete list of International Classification of Diseases (ICD)-9 and ICD-10 codes used to identify the population of interest is shown in E-Table 1 in the online-only Appendix.
To restrict the analysis to only elective operations, we excluded patients who had a diagnosis of spinal trauma or spinal cord injury, neoplasm, cauda equina syndrome, or infection, along with patients who underwent fracture repair. In addition, we excluded patients who were admitted from the emergency department or transferred from another hospital.
Exposure, Outcome, and Confounder Assignment
The exposure in this analysis was expansion of Medicaid insurance under the ACA. Expansion states included AZ, AR, CO, IA, MD, NJ, NV, NY, WA, and VT, which all expanded Medicaid eligibility on January 1, 2014.17 Non-expansion states included FL, MO, NE, and WI, though MO and NE chose to expand Medicaid eligibility after the analysis period. The pre-expansion period was 2011–2013, and the post-expansion period was 2014–2016. The primary outcomes were the mean overall and Medicaid hospital procedure volume per capita, along with the proportion of elective spine surgeries covered by Medicaid or private insurance. Per capita volume calculations were based on United States Census estimates each year, therefore accounting for any inconsistency in population changes across states during the study period.18 We also evaluated rates of uninsured (i.e. self-pay) cases as secondary outcomes, although conclusions are limited by the very low case prevalence of uninsured elective spine procedures.
Four states did not have data available for all study years. In particular, data were not available for year 2016 for CO, IA, NV, or WA, or for years 2011–2012 for WI. To avoid bias resulting from sudden changes in observed volume across years, these states were not included in analyses of hospital volume, which were restricted to states containing data for all years (AZ, AR, FL, MD, MO, NE, NJ, NY, VT). While MO included data for all years, it did not independently identify uninsured patients, which limited comparisons among payer subgroups. Consequently, MO was not included in analyses of payor mix changes. The number of patients per year contributed by state to each analysis is summarized in E-Table 2. Finally, to substantiate that our findings reflected the impact of Medicaid expansion, we also conducted a sensitivity analysis to evaluate changes in other payer (e.g. Medicare, military) procedure volumes, as these groups should not have experienced a significant change.
We considered patient age, race, comorbidity status, median income of home zip code, residence in a rural location, and state-level disability rates as potential confounders with the Medicaid outcome. Comorbidities were defined using a composite score based on the Elixhauser comorbidity index.19 Median income of home zip code, divided into quartiles by state, was generally captured in the SID. In instances when this variable was missing, we used median income data for zip code provided by the University of Michigan.20 Rural versus non-rural status was defined based on rural-urban commuting area (RUCA) codes, defined based on patient FIPS county codes when available or zip codes in other cases.21,22 Disability data were provided by the Social Security Office of Retirement and Disability Policy.23
Statistical Analysis
To evaluate the impact of Medicaid expansion under the ACA, we used a difference-in-difference quasi-experimental design. This design leverages comparisons between two groups experiencing the same time-dependent trends, other than a policy exposure (i.e., Medicaid expansion) applied only to one group and only in select time periods—before vs. after the 2014 expansion. Using this exposure, we could evaluate pre-post changes in Medicaid insurance coverage attributable to Medicaid expansion, independent of any background changes common to the all states.24
A difference-in-difference analysis assumes that although the groups being compared may have differed in levels of the outcome prior to intervention, they had the same (i.e. “parallel”) trend prior to intervention.25 We investigated this assumption graphically and statistically by testing for a significant group-time interaction in the pre-implementation period. The difference-in-difference analysis also assumes that major influences on the outcome occurring during or after the policy intervention will have an equal impact on both intervention and control groups (i.e. “common shocks”). While not directly testable, we did not identify any major health coverage changes impacting the states analyzed during the study period, apart from the ACA. Additionally, while some expansion states did have minor variations in how they met the ACA provisions,17 all adhered to the general specifications of expanding Medicaid eligibility, justifying their analysis as a single exposure group.
To evaluate changes in procedure volumes, we used negative binomial models producing incidence rate ratios (IRR) due to over-dispersion in the data. To evaluate change in payer mixes, we used linear probability models. All models included state-level expansion status, exposure period, an interaction between those terms, as well as potential confounding variables listed above. We also included variables for state and year fixed effects. The model interaction term between exposure period and expansion status captures the impact of Medicaid expansion, independent of other variables in the model. We used generalized estimating equations to account for state-level clustering impacting the standard errors. All analyses were conducted using complete case analysis, and significance was set as p < 0.05. All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). The authors’ Institutional Review Board (IRB) determined this study did not constitute human subjects research. Therefore, neither IRB approval nor informed consent was needed.
Results:
During the study period, we identified a total of 337,341 elective spine surgeries meeting inclusion criteria, including 218,648 surgeries in Medicaid expansion states and 118,693 in non-expansion states. In total, 48,538 (14.4%) surgeries had Medicaid insurance coverage. The most common surgery type in both exposure groups and study periods was thoracolumbar fusion (n=138,542, 41.1%), followed by cervical spine fusion (n=123,927, 36.7%), non-instrumented surgery (n=71,632, 21.2%) and cervical arthroplasty (n=3,240, 1.0%).The mean age (49.9 years) and proportion female (53%) were very similar between expansion and non-expansion states during both the pre- and post-expansion period. The proportion of non-White patients and mean comorbidity index were slightly higher in expansion (23.6% and 4.0) compared to non-expansion (19.2% and 3.2) states during both study periods. By comparison, the proportion rural was higher in non-expansion states (33.1% vs. 26.9%). As discussed in more detail below, expansion states had a higher proportion of Medicaid patients and a lower proportion of privately insured patients than non-expansion states, proportions that shifted during the study period. The population demographic characteristics for both expansion and non-expansion states are summarized by study period in Table 1.
Table 1:
Demographic characteristics of patients treated in expansion and non-expansion states. IQR=interquartile range.
| Characteristic | Expansion States | Non-expansion states | ||
|---|---|---|---|---|
| Pre-expansion | Post-expansion | Pre-expansion | Post-expansion | |
| Age in years, mean (IQR) | 49.5 (43–58) | 50.2 (44–58) | 49.6 (43–58) | 50.5 (44–58) |
| Gender, n (%) | ||||
| Male | 55,038 (46.4) | 47,036 (47.0) | 28,096 (46.4) | 27,201 (46.8) |
| Female | 63,497 (53.6) | 53,061 (53.0) | 32,519 (53.7) | 30,868 (53.2) |
| Missing | NR | 15 (0.01) | NR | NR |
| Race, n (%) | ||||
| Non-White | 26,506 (22.4) | 25,142 (25.1) | 11,246 (18.6) | 11,511 (19.8) |
| White | 92,028 (77.6) | 74,970 (74.9) | 49,369 (81.5) | 46,567 (80.2) |
| Insurance status, n (%)* | ||||
| Private | 100,914 (85.1) | 78,007 (77.9) | 39,684 (89.5) | 40,002 (88.6) |
| Medicaid | 15,570 (13.1) | 20,497 (20.5) | 3,728 (8.4) | 4,661 (10.3) |
| Uninsured | 2,052 (1.7) | 1,608(1.6) | 947 (2.1) | 502 (1.1) |
| Median income of home zip code, n (%) | ||||
| 1st (lowest) quartile | 25,468 (21.5) | 23,110 (23.1) | 12,957 (21.4) | 12,084 (20.8) |
| 2nd quartile | 29,116 (24.6) | 24,577 (24.6) | 15,378 (25.4) | 14,979 (25.8) |
| 3rd quartile | 30,961 (26.1) | 26,037 (26.0) | 16,499 (27.2) | 26,080 (27.7) |
| 4th (highest) quartile | 32,463 (27.4) | 26,082 (26.1) | 15,765 (26.0) | 14,881 (25.6) |
| Missing | 528 (0.45) | 306 (0.31) | 16 (0.03) | 54 (0.09) |
| Elixhauser comorbidity index, mean (IQR) | 3.9 (0–7) | 4.1 (0–7) | 3.2 (0–5) | 3.3 (0–6) |
| Rural zip code, n (%) | 28,158 (23.8) | 25,666 (25.6) | 20,904 (34.5) | 19,520 (33.6) |
| Missing | 11,930 (10.1) | 6,770 (6.8) | 22 (0.04) | 32 (0.06) |
| Procedure type, n (%) | ||||
| Cervical fusion | 42,857 (36.2) | 37,367 (37.3) | 22,352 (36.9) | 21,351 (36.8) |
| Cervical arthroplasty | 638 (0.54) | 964 (0.96) | 765 (1.3) | 873 (1.5) |
| Thoracolumbar fusion | 46,249 (39.0) | 42,697 (42.7) | 24,743 (40.8) | 24,853 (42.8) |
| Non-instrumented surgery | 28,792 (24.3) | 19,084 (19.1) | 12,755 (21.0) | 11,001 (18.9) |
Excluded data from MO, where the proportion of uninsured patients was not reported.
NR= not reported due to not reaching the HCUP minimum threshold of 10 events per cell.
To test for heterogeneity in socioeconomic status among Medicaid patients in each exposure group, we specifically evaluated the median income of home zip code for Medicaid patients (E-Table 3). As shown in the table, the median income of home zip code was generally similar across exposure groups. However, expansion states did have a slightly higher proportion of patients living in zip codes with the lowest income (40.8% vs. 36.5% in the pre-expansion period). The distribution of median income of home zip codes changed little in the post-expansion period.
There were no notable deviations from the parallel trends assumption in the pre-expansion period, consistent with the lack of a statistically significant difference in trends between expansion and non-expansion states in the pre-expansion period (E-Tables 2–3). In other words, there was no evidence for significant differences in trends for payor mix or volume by payor between expansion and non-expansion states from 2011 to 2014.
Trends in overall procedure volume as well as the procedure volume for specific payers are shown in Figure 1 and E-Figures 1–3. From 2011–2016, the mean hospital volume per quarter-year decreased from 0.24 surgeries to 0.20 surgeries per 100,000 residents in non-expansion states. By comparison, in expansion states there was a negligible change in surgery rates per quarter-year (0.33 in both periods). This difference led to a significant 17% relative increase in elective spine surgical volume associated with Medicaid expansion (95% CI 2%-35%; p=0.03). The magnitude and significance of the impact of Medicaid expansion on surgical volume varied by procedure type. There was a statistically significant 24% (95% CI 4%-48%; p=0.02) and 15% (95% CI 0.5%-31%; p=0.04) increase in cervical and thoracolumbar fusion volumes. By comparison, there was a smaller, not significant effect of Medicaid expansion on non-instrumented surgeries (IRR 1.09; 95% CI 0.97–1.21; p=0.15), where both expansion and non-expansion states had decreased volume in the post-expansion period (E-Figure 1; Table 2).
Figure 1:
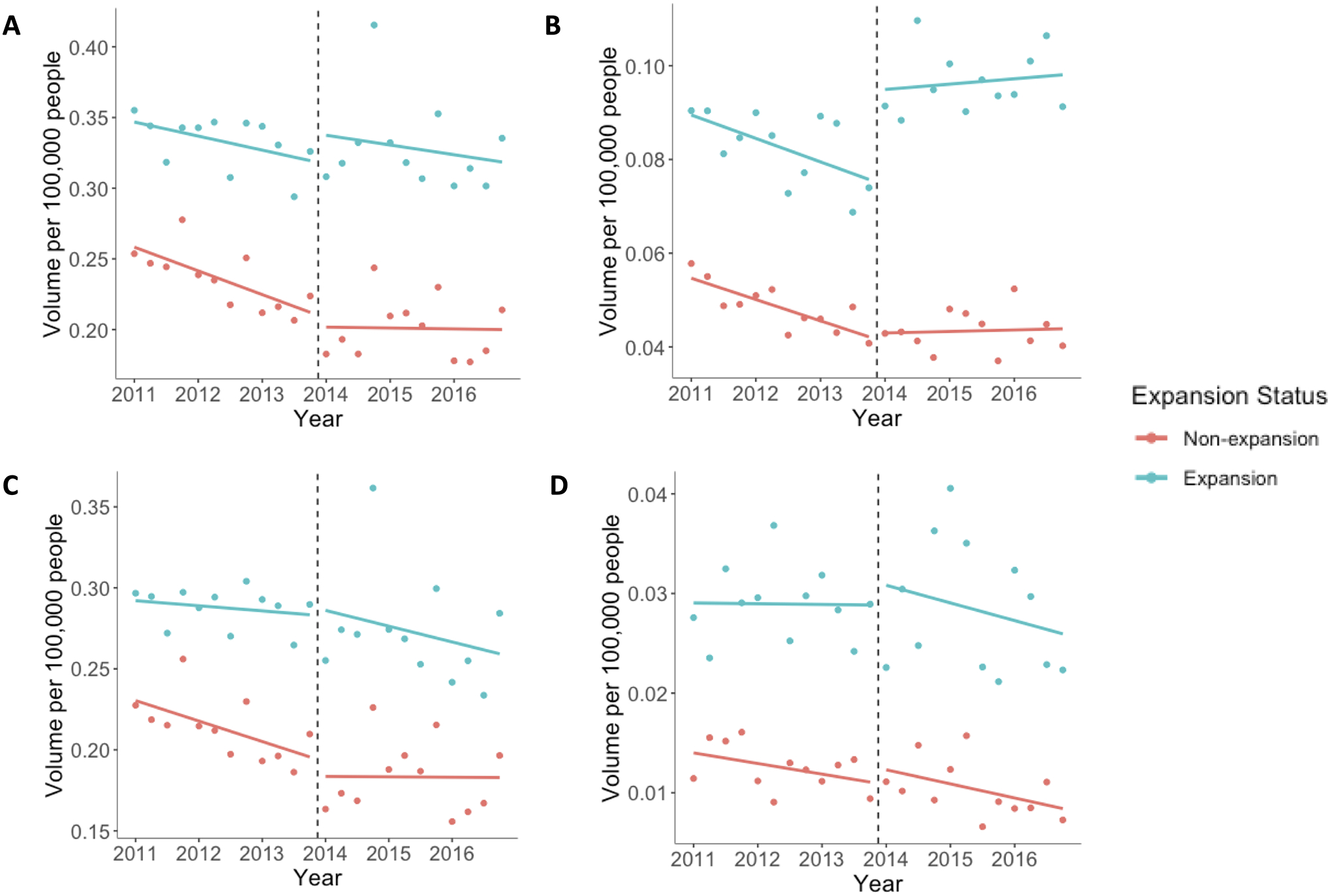
Changes in procedure volume according to payer type. Individual data points are displayed by quarter-year. The vertical dashed line indicates the time of Medicaid expansion in 2014. A) changes in overall volume, B) changes in Medicaid surgical volume, C) changes in privately insured surgical volume, D) changes in uninsured surgical volume.
Table 2:
Impact of Medicaid expansion on mean hospital elective spine surgical volume per quarter-year. Adjusted incidence rate ratios (with 95% CI) are shown for all elective surgeries, and also separated by surgery type.
| Overall | Medicaid | Private | Uninsured | |
|---|---|---|---|---|
| All surgeries | 1.17 (1.02–1.35)* | 1.23 (−0.3–52) | 1.13 (0.95–1.34) | 1.31 (0.91–1.88) |
| Cervical spine fusion | 1.24 (1.04–1.48)* | 1.09 (0.88–1.36) | 1.23 (0.99–1.52) | 1.24 (0.97–1.59) |
| Thoracolumbar fusion | 1.15 (1.005–1.31)* | 1.34 (1.05–1.70)* | 1.12 (0.95–1.32) | 1.29 (1.17–1.43) ** |
| Non-instrumented surgery | 1.09 (0.97–1.21) | 1.19 (1.04–1.37)* | 1.04 (0.91–1.20) | 1.16 (0.95–1.43) |
<0.05,
< 0.01
Analyses are adjusted for state and year fixed effects, state-level disability rates, as well as mean hospital values for patient age, gender, and comorbidity index.
The increase in overall elective spine volume associated with Medicaid expansion was largely driven by a 23% increase in Medicaid surgical volume (95% CI −0.3%-52%; p=0.054). While privately insured surgical volumes decreased across the 2011–2016 study period, the relative rates of privately insured surgeries did not change significantly in association with Medicaid expansion in 2014 (IRR=1.13; 95% CI −5%-34%; p=0.18). Uninsured (i.e., self-pay) procedures accounted for less than 2% of overall volume, and there was a non-significant change in the uninsured procedure volume (IRR=1.31; 95% CI 0.92–1.88; p=0.14) associated with Medicaid expansion. While all procedure subgroups saw relative increases in Medicaid procedure volumes associated with Medicaid expansion, the magnitude and significance of these changes varied. For example, the change in Medicaid volumes ranged from a 9% (95% CI −12%-36%; p=0.41) increase for cervical fusions to a 34% (95% 5%-70%; p=0.02) increase for thoracolumbar fusion. These changes in overall, Medicaid, privately insured, and uninsured procedure volumes are summarized in Table 2. Finally, the sensitivity analysis indicated Medicaid expansion status was not associated with a significant change in procedure volume for other payer types, such as military or Medicare insurance (IRR 1.09; 95% CI 0.97–1.24; p=0.15).
The disproportionate increase in Medicaid surgical volumes compared to privately insured surgical volumes led to a shift in payer mix. Therefore, Medicaid expansion in 2014 was associated with a statistically significant 6.0 percentage point (95% CI 4.1–7.0; p < 0.001) increase in the proportion of patients with Medicaid coverage (Figure 2). This effect was generally similar across procedure subgroups (range 5.9–6.2). This change was closely mirrored by the 6.7 percentage point (95% CI 4.5–8.8; p <0.001) decrease in the proportion of surgeries with private insurance. As shown in Figure 2, the impact of Medicaid expansion on payer mix gradually increased in the post-expansion period, with the proportion of Medicaid patients increasing and the proportion of privately insured patients decreasing from 2014–2016. Medicaid expansion was associated with a small and not significant change in the proportion of patients without insurance coverage (0.7 percentage points; 95% CI −0.3–1.7; p=0.17). The complete summary of the changes in payer mix is shown in Table 3 and E-Figures 4–5.
Figure 2:
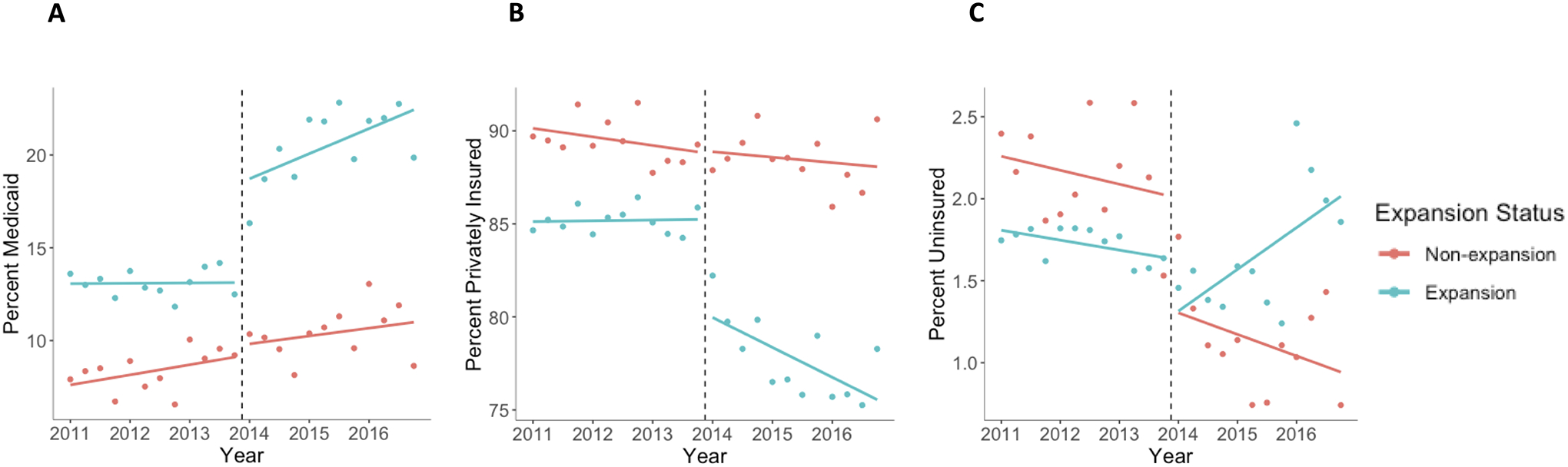
Changes in payer mix during the analysis period. Individual data points are displayed by quarter-year. The vertical dashed line indicates the time of Medicaid expansion in 2014. A) changes in proportion of Medicaid patients, B) changes in proportion of privately insured patients, C) changes in proportion uninsured.
Table 3:
Impact of Medicaid expansion on payor mix of elective spine surgery. The difference-in-difference estimate (with 95% CI) is shown for change in probability of Medicaid, private insurance, and uninsured payer type.
| Medicaid | Private | Uninsured | |
|---|---|---|---|
| All elective surgeries | 6.0 (4.1–7.0)** | −6.7 (−8.8 – −4.5)** | 0.7 (−0.3–1.7) |
| Cervical spine fusion | 6.2 (3.9–8.6)** | −7.2 (−9.5 – −4.9)** | 1.0 (−0.1–2.2) |
| Thoracolumbar spine fusions | 5.9 (4.2–7.6)** | −6.5 (−8.2 – −4.7)** | 0.6 (−0.1 – 1.2) |
| Non-instrumented surgery | 6.1 (4.0–8.2)** | −7.2 (−9.9 – −4.5)** | 0.7 (−1.2–1.8) |
< 0.05;
<0.01
Estimates are adjusted for state and year fixed effects, patient age, race, comorbidity index, median income of home zip code, rural zip code, and state-level disability rates.
Discussion:
To our knowledge this is the first focused assessment of the impact of Medicaid expansion under the ACA on elective spine surgical volumes and payer mix. Our primary results indicated that the ACA was associated with a 17% increase in overall elective surgical volume, which was driven primarily by a 23% increase in Medicaid surgical volume. There was no significant change in volume of privately insured surgeries or patients with other (e.g. military, Medicare) insurance. Increases in Medicaid surgical volume also led to a change in payer mix, with Medicaid expansion states experiencing a 6.0 percentage point increase in the proportion of patients with Medicaid coverage. Although the magnitude and statistical significance of these changes varied, the results were generally consistent across subgroups of different procedure types. In both study groups and treatment periods, uninsured (i.e., self-pay) patients were a small minority of those treated, and our results did not indicate that Medicaid expansion was associated a significant change in access for these patients.
Our finding that Medicaid expansion led to a significant expansion in access to elective spine care is somewhat surprising in light of previous evidence demonstrating major barriers to spine care for Medicaid patients. For example, one study found Medicaid patients had to travel approximately three times farther than privately insured to find a provider who would offer elective lumbar spine surgical care.26 Other studies have found Medicaid patients had success rates below 1% making appointments for elective lumbar spine care.27,28 While such results would suggest that Medicaid expansion would have had a negligible impact on elective spine practice, these limited case series may not provide a generalizable perspective on population trends.
One explanation for our findings is that the increase in Medicaid surgeries was generally restricted to patients with higher spine disease severity (e.g. more severe myelopathy or deformity) who either did not pursue or were not offered surgery prior to Medicaid expansion. While not directly testable using billing data, this theory is consistent with previous studies indicating that Medicaid patients have worse deformity than privately insured patients at the time of presentation and scoliosis surgery.29,30 The notion that treatment access was concentrated among patients with severely disabling disease is also supported by comparisons to other orthopedic conditions. For example, spine disease is typically more disabling than other orthopedic pathologies,31 such as hip and knee disease. Reflecting this difference, we observed a notably larger shift in Medicaid payer mix following Medicaid expansion (6.0%) than has been shown previously for hip and knee arthroplasty (1.5%).6
Beyond orthopedic conditions, the impact of Medicaid expansion on elective spine surgical care should be interpreted within the context of the broader surgical and economic literature. We observed an overall increase in elective spine surgical volume of 17%, similar to rate changes found in studies evaluating major general surgery procedures, including gastric bypass surgery (8%), paraesophageal hernia or reflux disease surgery (17%), cancer surgeries (12%), hernia repair (16%), and vascular surgery (20%).8,32–34 While each of these conditions differs with regard to the urgency of treatment and the likely unmet demand among uninsured patients, the impact of Medicaid expansion was similar. These findings suggest that observed changes in procedural volume may partly reflect the degree to which surgeons balance new Medicaid demand with maintaining privately insured volumes, a tradeoff which appears to bear similarity across a variety of major health conditions. Finally, given estimates of fusion surgeries alone leading to approximately $13 billion in costs in the United States in 2011,35 a 17% change in spine surgery volume is likely to have important economic significance.36
By leveraging a large and representative dataset, this study provides novel insights about the impact of Medicaid expansion on one of the most common surgeries performed in the United States. Moreover, by examining several endpoints and patient subgroups using a robust statistical approach, these results support a detailed examination of the policy effects. This study also has limitations. The most important limitation is that the study datasets only included inpatient surgeries. Given the growing role of outpatient elective spine surgery,37 a disproportionate shift to outpatient surgeries in non-expansion versus Medicaid expansion states could have impacted our results. However, several lines of evidence suggest that such patterns should not undermine our conclusions. First, the shift to outpatient surgery has been far more pronounced for non-instrumented than fusion surgeries.38 For fusion surgeries, and lumbar fusion in particular, existing evidence suggests that the vast majority of surgeries occurred in the inpatient setting during the study period.38–41 The consistency of our findings across procedure subgroups make it unlikely that consideration of ambulatory practices would impact these results. Second, previous studies have not found a marked change in ambulatory surgeries associated with the timing of Medicaid expansion in 2014.38,42,43 Finally, previous evidence suggests that the shift to ambulatory surgeries has occurred in similar proportions across states and geographic regions, making a differential impact associated with Medicaid expansion status unlikely.44,45
Another limitation is that despite including a larger sample of states than many comparable studies,6–8 our sample size still limited our ability to test for heterogeneity in effects across states, such as variations related to individual state expansion strategies.17 Finally, the study dataset did not allow us to investigate the exact mechanisms leading to the observed changes, such as increased imaging and referral rates by primary care physicians versus changes in decision-making among spine surgeons. Such questions may be explored by future researchers using other data sources that incorporate relevant data elements.
Conclusions:
Medicaid expansion under the ACA was associated with an economically significant increase in overall spine surgery volumes and volume of Medicaid surgeries. Along with an increase in the proportion of surgical patients with Medicaid insurance, these results support the hypothesis that Medicaid expansion increased access to elective spine surgery, likely offering improved quality of life to a subset of the population previously unable to access treatment. Future work should use alternative datasets to identify the mechanisms leading to the observed changes in practice, including examining changes in both imaging practices and outpatient referral rates.
Supplementary Material
Acknowledgment:
The authors thank Ms. Joanna Reale for her assistance with database programming.
Disclosures:
Dr. Ray reports: stock/equity in Acera surgical; consulting support from Depuy/Synthes, Globus, and Nuvasive; royalties from Depuy/Synthes, Nuvasive, Acera surgical. Dr. Olsen reports grants from Merck, Pfizer, and Sanofi Pasteur, along with consulting fees from Pfizer. No authors have any conflicts of interest.
Funding:
This work and the Center for Administrative Data Research were supported by the Washington University Institute of Clinical and Translational Sciences which is, in part, supported by the NIH/National Center for Advancing Translational Sciences (NCATS), CTSA grant #UL1 TR002345. The Center for Administrative Data Research is also supported in part by Grant Number R24 HS19455 through the Agency for Healthcare Research and Quality (AHRQ). JKG was supported by funding from the Agency for Healthcare Research and Quality (1F32HS027075-01A1) and the Thrasher Research Fund (#15024).
References:
- 1.Blumenthal D, Abrams M, Nuzum R. The Affordable Care Act at 5 Years. N Engl J Med. 2015;373(16):1580. [DOI] [PubMed] [Google Scholar]
- 2.Frean M, Gruber J, Sommers BD. Disentangling the ACA’s Coverage Effects - Lessons for Policymakers. N Engl J Med. 2016;375(17):1605–1608. [DOI] [PubMed] [Google Scholar]
- 3.Keith K The ACA At The Supreme Court And Beyond: A review of upcoming challenges and developments involving the Affordable Care Act. Health Aff (Millwood). 2020;39(4):554–555. [DOI] [PubMed] [Google Scholar]
- 4.Mazurenko O, Balio CP, Agarwal R, Carroll AE, Menachemi N. The effects of Medicaid expansion under the ACA: a systematic review. Health Aff (Millwood). 2018;37(6):944–950. [DOI] [PubMed] [Google Scholar]
- 5.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance. JAMA Intern Med. 2016;176(10):1501–1509. [DOI] [PubMed] [Google Scholar]
- 6.Dy CJ, Brown DS, Maryam H, Keller MR, Olsen MA. Two-State Comparison of Total Joint Arthroplasty Utilization Following Medicaid Expansion. J Arthroplasty. 2019;34(4):619–625.e611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ellimoottil C, Miller S, Ayanian JZ, Miller DC. Effect of insurance expansion on utilization of inpatient surgery. JAMA Surg. 2014;149(8):829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin S, Brasel KJ, Chakraborty O, Glied SA. Association Between Medicaid Expansion and the Use of Outpatient General Surgical Care Among US Adults in Multiple States. JAMA surgery. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williamson TR, Paoli AR, Hutzler L, Zuckerman J, Bosco JI. Access to Elective Orthopaedic Surgery After the Affordable Care Act Medicaid Expansion: The New York State Experience. JAAOS - Journal of the American Academy of Orthopaedic Surgeons. 2020;28(4):e158–e163. [DOI] [PubMed] [Google Scholar]
- 10.Crocker AB, Zeymo A, Chan K, et al. The Affordable Care Act’s Medicaid expansion and utilization of discretionary vs. non-discretionary inpatient surgery. Surgery. 2018;164(6):1156–1161. [DOI] [PubMed] [Google Scholar]
- 11.Marrero CE, Igbokwe LI, Leonardi C. Access to Orthopedic Care post Medicaid Expansion Through the Affordable Care Act. J Natl Med Assoc. 2019;111(2):148–152. [DOI] [PubMed] [Google Scholar]
- 12.HCUP. HCUP Fast Stats. Healthcare Cost and Utilization Project (HCUP). www.hcup-us.ahrq.gov/faststats/national/inpatientcommonprocedures.jsp. Agency for Healthcare Research and Quality; Published 2019. Accessed 2019 December 29, 2019. [PubMed] [Google Scholar]
- 13.Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. The Lancet. 2018;391(10137):2356–2367. [DOI] [PubMed] [Google Scholar]
- 14.Blucher JA, Schoenfeld AJ. Changes in the care of spine surgical patients following health reform in Massachusetts: A review of the literature. Paper presented at: Seminars in Spine Surgery2019. [Google Scholar]
- 15.Schoenfeld AJ, Wahlquist TC, Bono CM, Lehrich JL, Power RK, Harris MB. Changes in the care of patients with cervical spine fractures following health reform in Massachusetts. Injury. 2015;46(8):1545–1550. [DOI] [PubMed] [Google Scholar]
- 16.Agency for Healthcare Research and Quality. Introduction to the HCUP State Inpatient Databases (SID). In: (HCUP) HCaUP, ed: Agency for Healthcare Research and Quality; 2019. [Google Scholar]
- 17.KFF. Status of State Action on the Medicaid Expansion Decision. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. KFF; Published 2021. Accessed 2021 February 15, 2021. [Google Scholar]
- 18.State Population Totals and Components of Change: 2010–2019. https://www.census.gov/data/tables/time-series/demo/popest/2010s-state-total.html. United States Census Bureau; Published 2019. Accessed 2020 September 21, 2020. [Google Scholar]
- 19.Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data. Med Care. 2017;55(7):698–705. [DOI] [PubMed] [Google Scholar]
- 20.Institute for Social Research. Zip Code Characteristics: Mean and Median Household Income. https://www.psc.isr.umich.edu/dis/census/Features/tract2zip/. Michigan Population Studies Center; Published 2020. Accessed August 8, 2020. [Google Scholar]
- 21.Rural Health Research Center. RUCA Data Zip Code RUCA Approximation. https://depts.washington.edu/uwruca/ruca-approx.php. Rural Health Research Center; Published 2020. Accessed August 8, 2020. [Google Scholar]
- 22.United States Department of Agriculture. Rural-Urban Commuting Area Codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. United States Department of Agriculture, Economic Research Service; Published 2019. Accessed August *, 2020. [Google Scholar]
- 23.SSA Fiscal Year Disability Claim Data. https://www.ssa.gov/disability/data/ssa-sa-fywl.htm#FieldI. Social Security Administration; Published 2020. Accessed August 27, 2020. [Google Scholar]
- 24.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401–2402. [DOI] [PubMed] [Google Scholar]
- 25.Ryan AM, Burgess JF Jr., Dimick JB. Why We Should Not Be Indifferent to Specification Choices for Difference-in-Differences. Health Serv Res. 2015;50(4):1211–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weiner BK, Black KP, Gish J. Access to spine care for the poor and near poor. Spine J. 2009;9(3):221–224. [DOI] [PubMed] [Google Scholar]
- 27.Anandasivam NS, Wiznia DH, Kim CY, Save AV, Grauer JN, Pelker RR. Access of Patients With Lumbar Disc Herniations to Spine Surgeons: The Effect of Insurance Type Under the Affordable Care Act. Spine (Phila Pa 1976). 2017;42(15):1179–1183. [DOI] [PubMed] [Google Scholar]
- 28.Segal DN, Grabel ZJ, Shi WJ, Gottschalk MB, Boden SD. The impact of insurance coverage on access to orthopedic spine care. Journal of Spine Surgery. 2018;4(2):260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fletcher ND, Lazarus DE, Desai MJ, Patel NN, Bruce RW Jr. Medicaid insurance is associated with larger curves in patients who require scoliosis surgery. Surgery. 2015;57(60.6):15.17. [PubMed] [Google Scholar]
- 30.Russell T, Dharia A, Folsom R, et al. Healthcare disparities in adolescent idiopathic scoliosis: the impact of socioeconomic factors on Cobb angle. Spine Deformity. 2020:1–7. [DOI] [PubMed] [Google Scholar]
- 31.Fontal JAB, Granell JB, Olmo JG, Busquets RR, Prats FP, Leal CV. Evaluation of health-related quality of life in patients candidate for spine and other musculoskeletal surgery. Eur Spine J. 2013;22(5):1002–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eguia E, Cobb AN, Kothari AN, et al. Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries. Ann Surg. 2018;268(4):584–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eguia E, Baker MS, Chand B, Sweigert PJ, Kuo PC. The impact of the affordable care act (ACA) Medicaid Expansion on access to minimally invasive surgical care. The American Journal of Surgery. 2020;219(1):15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eguia E, Baker MS, Bechara C, Shames M, Kuo PC. The Impact of the Affordable Care Act Medicaid Expansion on Vascular Surgery. Ann Vasc Surg. 2020;66:454–461.e451. [DOI] [PubMed] [Google Scholar]
- 35.Weiss AJ, Elixhauser A, Andrews RM. Statistical Brief# 180. Overview of Hospital Stays in the United States. 2014. [PubMed] [Google Scholar]
- 36.Office of the General Counsel. Rulemaking and Guidance Procedures. In: Education Do, ed2020. [Google Scholar]
- 37.DelSole EM, Makanji HS, Kurd MF. Current trends in ambulatory spine surgery: a systematic review. J Spine Surg. 2019;5(Suppl 2):S124–S132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Idowu OA, Boyajian HH, Ramos E, Shi LL, Lee MJ. Trend of Spine Surgeries in the Outpatient Hospital Setting Versus Ambulatory Surgical Center. Spine (Phila Pa 1976). 2017;42(24). [DOI] [PubMed] [Google Scholar]
- 39.Blaginykh E, Alvi MA, Goyal A, et al. Outpatient Versus Inpatient Posterior Lumbar Fusion for Low-Risk Patients: An Analysis of Thirty-Day Outcomes From the National Surgical Quality Improvement Program. World Neurosurg. 2020;142:e487–e493. [DOI] [PubMed] [Google Scholar]
- 40.Arshi A, Wang C, Park HY, et al. Ambulatory anterior cervical discectomy and fusion is associated with a higher risk of revision surgery and perioperative complications: an analysis of a large nationwide database. Spine J. 2018;18(7):1180–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martin CT, D’Oro A, Buser Z, et al. Trends and Costs of Anterior Cervical Discectomy and Fusion: a Comparison of Inpatient And Outpatient Procedures. The Iowa orthopaedic journal. 2018;38:167–176. [PMC free article] [PubMed] [Google Scholar]
- 42.Soffin EM, Beckman JD, Beathe JC, Girardi FP, Liguori GA, Liu J. Trends in Ambulatory Laminectomy in the USA and Key Factors Associated with Successful Same-Day Discharge: A Retrospective Cohort Study. HSS Journal ®. 2020;16(1):72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weiss HK, Yamaguchi JT, Garcia RM, Hsu WK, Smith ZA, Dahdaleh NS. Trends in National Use of Anterior Cervical Discectomy and Fusion from 2006 to 2016. World Neurosurg. 2020;138:e42–e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arshi A, Park HY, Blumstein GW, et al. Outpatient Posterior Lumbar Fusion: A Population-Based Analysis of Trends and Complication Rates. Spine (Phila Pa 1976). 2018;43(22):1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baird EO, Egorova NN, McAnany SJ, Qureshi SA, Hecht AC, Cho SK. National Trends in Outpatient Surgical Treatment of Degenerative Cervical Spine Disease. Global Spine Journal. 2014;4(3):143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


