Highlights
-
•
Hospitalized patients were older in Wave 2 Bthan in Wave 1.
-
•
Hospitalized patients were more likely to be male in Wave 1 than in Wave 2.
-
•
Coronavirus disease 2019 was more severe in Wave 2 than in Wave 1.
Abbreviations: COVID-19, Coronavirus disease 2019; HP, Hospitalized Patients; NHP, Non-hospitalized patients; SARS-CoV-2, Severe acute respiratory syndrome coronavirus-2; HTN, Hypertension; DM, Diabetes mellitus
Abstract
Introduction
Uganda was affected by two major waves of coronavirus disease 2019 (COVID-19). The first wave during late 2020 and the second wave in late April 2021. This study compared epidemiologic characteristics of hospitalized (HP) and non-hospitalized patients (NHP) with COVID-19 during the two waves of COVID-19 in Uganda.
Methods
Wave 1 was defined as November–December 2020, and Wave 2 was defined as April–June 2021. In total, 800 patients were included in this study. Medical record data were collected for HP (200 for each wave). Contact information was retrieved for NHP who had polymerase-chain-reaction-confirmed COVID-19 (200 for each wave) from laboratory records; these patients were interviewed by telephone.
Findings
A higher proportion of HP were male in Wave 1 compared with Wave 2 (73% vs 54%; P=0.0001). More HP had severe disease or died in Wave 2 compared with Wave 1 (65% vs 31%; P<0.0001). NHP in Wave 2 were younger than those in Wave 1, but this difference was not significant (mean age 29 vs 36 years; P=0.13). HP were significantly older than NHP in Wave 2 (mean age 48 vs 29 years; P<0.0001), but not Wave 1 (mean age 48 vs 43 years; P=0.31).
Interpretation
Demographic and epidemiologic characteristics of HP and NHP differed between and within Waves 1 and 2 of COVID-19 in Uganda.
Research in context.
Evidence before this study
PubMed was searched for research articles published in English from 21 March 2020 to 28 April 2021 using the terms ‘SARS-CoV-2’ [severe acute respiratory syndrome coronavirus-2], ‘COVID-19’ [coronavirus disease 2019], ‘wave’, ‘hospitalization’, ‘mortality’ and/or ‘variants’. In total, 45 articles were found on these topics. The SARS-CoV-2 Delta variant has been shown to be more transmissible and associated with more severe disease than earlier SARS-CoV-2 variants (Fisman and Tuite, 2021, Sheikh et al., 2021). At the time this study was conducted, little was known about the Delta variant; however, media reports suggested that it might cause more severe disease in younger people (CNN, 2021;UN, 2021).
Added value of this study
The second wave of SARS-CoV-2 infections in Uganda was caused primarily by the Delta variant, while the first wave was caused by a mixture of non-Delta variants (CDC, 2021). In the present study, infections in Waves 1 and 2 in Uganda differed across several indicators. Hospitalized patients were more likely to be male in Wave 1 than in Wave 2. Non-hospitalized patients were younger in Wave 2 than in Wave 1. Increasing age was strongly associated with hospitalization during Wave 2, but was only marginally associated with hospitalization in Wave 1. A higher proportion of hospitalized patients had severe disease and died in Wave 2 than in Wave 1.
Implications of all available data
Different SARS-CoV-2 variants may have differing epidemiologic characteristics. The study findings emphasize the need to study and understand the epidemiologic characteristics of each SARS-CoV-2 variant independently to ensure that messaging and preparedness are tailored appropriately in each wave.
Alt-text: Unlabelled box
Background
Uganda reported its first case of COVID-19 on 21 March 2020 (WHO, 2020). After several months with few confirmed cases, cases began to increase in August 2020, and a large wave of cases swept through the country in late 2020 (Kadowa, 2020). The number of cases waned in early 2021, but a resurgence began in April 2021. The second wave peaked in June 2021 and continued through mid-August 2021. It grew more quickly than the first wave, and challenged the capacity of the healthcare system (Blair, 2021; Bugembe et al., 2021). The first Delta variant sequences in Uganda were detected in mid-April 2021. From mid-May to early September 2021, nearly all SARS-CoV-2 isolates sequenced in Uganda were the Delta variant (Bugembe et al., 2021).
In March 2021, shortly before the start of the second wave in Uganda, the country launched a mass COVID-19 vaccination programme using the AstraZeneca vaccine ChAdOx1-S (Africa News, 2021; VOA News, 2021a). However, vaccine uptake was slow, and as of June 2021, only 750,000 of the 44 million people in Uganda had been vaccinated (713,000 had received the first dose of vaccine, 36,000 had received both doses of vaccine).
Like many areas of the world, Uganda has been affected by misinformation about COVID-19, frequently spread through social media. Mistrust and suspicion surrounded the rollout of COVID-19 vaccines in the country (Kasozi et al., 2020; Samarasekera, 2021), and social media messages about the dangers of vaccination were rampant during the rollout, including reports that younger (CNN, 2021; UN, 2021), fully vaccinated people were dying in hospitals. There was an urgent need to gather data about the epidemiologic characteristics and vaccination status of patients in the second wave, both to support evidence-based public communication, and to provide relevant, current data about infections in Uganda. As such, this study compared the epidemiologic characteristics of hospitalized patients (HP) and non-hospitalized patients (NHP), including vaccination status, diagnosed during the first and second waves of COVID-19 in Uganda.
Methods
Study design and setting
This study included HP from the two highest-volume referral hospitals in Uganda: Mulago Hospital in Kampala and Entebbe Grade B Hospital in Entebbe. NHP from throughout the country were also included.
Study timing
The study procedures took place in May–June 2021. The study periods were defined as ‘Wave 1’ (November–December 2020) and ‘Wave 2’ (April–June 2021). Although neither of these periods fully encompassed the waves of interest, the Wave 1 period was selected to cover the months during which the highest number of patients were identified. The Wave 2 period was selected to include all patients with confirmed infection from April 2021 to the start of this investigation.
Sample size
The sample size needed to identify a difference of 5 years in mean age between patients in each study group was calculated. At 80% power and 95% confidence, and with a standard deviation of 15 years, 200 patients were needed in each group (HP in Wave 1, HP in Wave 2, NHP in Wave 1, and NHP in Wave 2), representing a total of 800 patients.
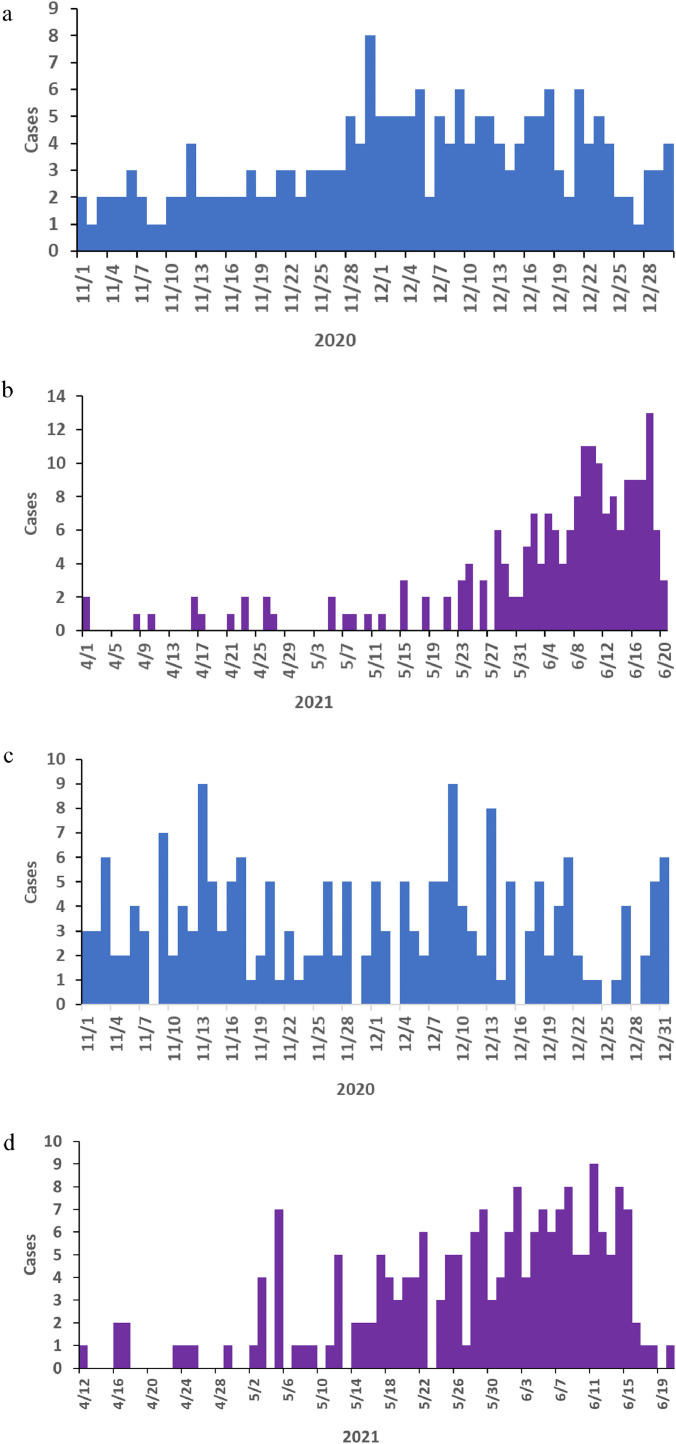
In each of the two hospitals, demographic and clinical data were collected for 100 HP in Wave 1 and 100 HP in Wave 2, representing a total of 400 HP. In addition, data were collected for 200 NHP in Wave 1 and 200 NHP in Wave 2 (Figs. 1a–d).
Figure 1.
(a) Distribution of sample-taking dates for non-hospitalized patients in Wave 1 included in this study, Uganda. (b) Distribution of sample-taking dates for non-hospitalized patients in Wave 2 included in this study, Uganda. (c) Distribution of admission dates for hospitalized patients in Wave 1 included in this study, Uganda. (d) Distribution of admission dates for hospitalized patients in Wave 2 included in this study, Uganda.
Patient selection
For HP, all patient files were separated in each hospital for the periods of interest and sorted by date, then sampled systematically using a sampling interval to reach 100 patients from each hospital in each wave.
For NHP, case patients were identified from the national case line list. While the national case line list included patients from all areas of Uganda, the majority of confirmed cases identified in Uganda [14,646/22,768 (64%) from 1 November to 30 December 2020, and 23,791/32,477 (73%) from 1 April to 20 June 2021 (when this study was started)] were from the Greater Kampala Metropolitan Area. A sampling frame was created for each wave, and 200 NHP were selected per wave using a random number generator.
Data collection
Data were abstracted from hospital records for HP. Contact information for NHP was retrieved from the national case line list, and these individuals were interviewed by telephone to collect demographic and clinical information. Any patient who was contacted and found to have been hospitalized (n=8) was excluded from the study and replaced on a random basis.
Definitions
Patient disease status was categorized as asymptomatic, mild/moderate, severe/critical, or died. Asymptomatic cases comprised patients with no symptoms of COVID-19. Mild/moderate disease included patients with symptoms but without shortness of breath during clinical assessments; where clinical assessments were available, mild/moderate disease was defined as patients with symptoms but with oxygen saturation (SpO2) >94% on atmospheric air. Severe/critical disease was defined as patients with SpO2 <94% on room air, ratio of arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FiO2) <300, >30 breaths/min, lung infiltrates >50%, respiratory failure, septic shock and/or multiple organ dysfunction. Deaths were counted only among patients hospitalized for COVID-19 who died before recovery. Full vaccination was defined as receipt of two doses of vaccine at least 14 days before onset of illness or positive test result.
Data analysis
Mean and interquartile range were calculated for continuous variables, and frequencies and odds ratios with 95% confidence intervals. Between- and within-wave statistics were compared using a two-sample t-test. Mean age was compared using the independent samples t-test. Logistic regression was used to assess the factors associated with hospitalization and death for patients with COVID-19. Data were analysed using Epi Info Version 7.2.
Results
Characteristics of hospitalized and non-hospitalized patients with COVID-19 in study population, Uganda, November–December 2020 and April–June 2021
Among 400 HP, 255 (64%) were male. The mean age was 46 years (range 0–98 years). Nearly half (n=182, 46%) of HP had an underlying condition, with hypertension being the most common (n=108, 27%). Among 400 NHP, 219 (55%) were male. The mean age was 32 years (range 0–82 years).
The majority of HP (167/200,84%) and NHP (179/200, 90%) in Wave 2 were admitted or had their samples taken, respectively, during the third week of May 2021 or later (Figs. 1a–d). Starting from the third week of May 2021 through to at least the last week of July 2021, 246/255 (96%) of SARS-CoV-2 isolates sequenced in Uganda were identified as the Delta variant.
Within-wave differences in hospitalized and non-hospitalized patients, Waves 1 and 2 of COVID-19, Uganda, 2020–2021
In Wave 1, HP were more likely to be male than NHP (73% vs 58%; P=0.002), but in Wave 2, HP and NHP were equally likely to be male (54% vs 52%; P=0.69) (Table 1). HP were significantly older than NHP in Wave 2 (mean age 48 vs 29 years; P=0.0001), but not in Wave 1 (mean age 48 vs 43 years; P=0.31). As vaccines only became available in March 2021, only patients in Wave 2 had received any doses of vaccine. No patients were fully vaccinated at the onset of illness (Table 2).
Table 1.
Characteristics of hospitalized patients (HP) and non-hospitalized patients (NHP) with coronavirus disease 2019 within and between Waves 1 and 2, Uganda, 2020–2021.
| Wave 1 | Within Wave 1 | Wave 2 | Within Wave 2 | Between Wave 1 HP and Wave 2 HP | Between Wave 1 NHP and Wave 2 NHP | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | HP(n=200) n (%) | NHP(n=200) n (%) | P-values | HPa (n=200)n (%) | NHP (n=200)n (%) | P-values | P-values | P-values | n | ||||
| Sex | |||||||||||||
| Male | 147 | (73)b | 116 | (58) | 0.002 | 108 | (54)c | 103 | (52) | 0.69 | 0.0001 | 0.23 | 474 |
| Female | 53 | (27)b | 84 | (42) | 0.002 | 92 | (46)c | 97 | (48) | 0.69 | 0.0001 | 0.23 | 326 |
| Age (years) | |||||||||||||
| 0–5 | 2 | (1) | 7 | (3) | 0.15 | 3 | (2) | 4 | (2) | 0.41 | 0.41 | 0.15 | 17 |
| 6–19 | 3 | (2) | 16 | (8) | 0.02 | 3 | (2)b | 35 | (17) | <0.0001 | 0.41 | 0.01 | 57 |
| 20–34 | 60 | (30) | 71 | (35) | 0.13 | 40 | (20)b | 106 | (53) | <0.0001 | 0.03 | 0.002 | 277 |
| 35–54 | 90 | (45) | 77 | (40) | 0.54 | 78 | (39)b | 48 | (24) | 0.003 | 0.31 | 0.006 | 293 |
| ≥55 | 45 | (22) | 29 | (14) | 0.04 | 74 | (37)b | 7 | (4) | <0.0001 | 0.002 | 0.0002 | 154 |
Two HP in Wave 2 were missing age data.
Significant at P<0.05 within waves.
Significant at P<0.05 between waves.
Table 2.
Comparison of disease severity, and clinical characteristics of hospitalized patients (HP) and non-hospitalized patients (NHP) with coronavirus disease 2019 in Waves 1 and 2, Uganda, 2020–2021.
| Characteristics | Wave 1 | Wave 2 | Vaccination status between HP and NHP in Wave 2 | Between Wave 1 HP and Wave 2 HP | Between Wave 1 NHP and Wave 2 NHP | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HP (n=200)n (%) | NHP (n=200)n (%) | HP (n=200)n (%) | NHP (n=200)n (%) | P-values | P-values | P-values | ||||||
| Infection severity | ||||||||||||
| Asymptomatic | 36 | (18) | 99 | (49) | 20 | (10) | 82 | (41) | NA | 0.02 | 0.11 | 237 |
| Mild/moderate | 102 | (51) | 101 | (51) | 49 | (25) | 118 | (59) | NA | 0.02 | 0.11 | 370 |
| Severe/critical | 50 | (25) | 0 | (0) | 78 | (39) | 0 | (0) | NA | 0.002 | Undefined | 128 |
| Died | 12 | (6) | 0 | (0) | 53 | (26) | 0 | (0) | NA | <0.0001 | Undefined | 65 |
| Vaccination status | ||||||||||||
| Unvaccinated | 200 | (100) | 200 | (100) | 189 | (94) | 180 | (90) | 0.14 | NA | NA | 769 |
| One dose | 0 | (0) | 0 | (0) | 9 | (5) | 17 | (9) | 0.12 | NA | NA | 26 |
| Two doses | 0 | (0) | 0 | (0) | 2 | (1) | 3 | (1) | 1.00 | NA | NA | 5 |
| Two doses + 14 daysa | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) | Undefined | NA | NA | 0 |
Fully vaccinated.
Comparison of hospitalized patients between Waves 1 and 2 of COVID-19, Uganda, 2020–2021
HP were more often male than female in both waves (Table 1). However, in Wave 1, HP were more likely to be male than HP in Wave 2 (73% vs 54%; P<0.0001). HP were asymptomatic about half as often in Wave 2 as in Wave 1 (10% vs 18%; P=0.02), and died more than four times as often in Wave 2 (26% vs 6%; P<0.0001) (Table 2).
Comparison of non-hospitalized patients between Waves 1 and 2 of COVID-19 infection, Uganda, 2020–2021
While NHP were more likely to be male than female in both Waves 1 and 2, the difference in the proportion of males between waves was not significant (58% male in Wave 1 vs 52% in Wave 2; P=0.23) (Table 1). NHP were younger in Wave 2 than in Wave 1, but this difference was not significant (mean age 29 vs 36 years; P=0.13). A non-significantly higher proportion of NHP had any symptoms in Wave 2 compared with Wave 1 (59% vs 51%; P=0.11) (Table 2).
Characteristics of hospitalization and death among patients in Waves 1 and 2, Uganda, 2020–2021
Male sex was associated with two-fold increased odds of hospitalization in Wave 1 (P<0.001), but not in Wave 2 (P=0.62) (Table 3). Male sex was associated with two-fold increased odds of death in Wave 2 (P=0.04) but not in Wave 1 (P=0.9) (Table 4). Being aged 6–19 years was associated with reduced odds of hospitalization in both Waves 1 and 2, compared with being aged 20–34 years. Being aged ≥55 years was associated with 28-fold increased odds of hospitalization in Wave 2 (P<0.0001), but was only associated with two-fold increased odds of hospitalization in Wave 1 (P=0.05). Hypertension and diabetes were more strongly associated with hospitalization in both waves than age, although there was an additive effect of age, hypertension and diabetes in increasing the odds of hospitalization in Wave 2 (Table 3). Among the 31 partially vaccinated patients in Wave 2, there was no significant association with risk of hospitalization (P=0.10). Increasing age was associated with increased mortality in both waves (P<0.0001), even among patients without comorbidities (P=0.002) (Table 4).
Table 3.
Characteristics associated with hospitalization among patients in Waves 1 and 2, Uganda, 2020–2021.
| Characteristics | Wave 1 |
Wave 2 |
Wave 1 |
Wave 2 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HP (n=200)n (%) | NHP (n=200)n (%) | HP (n=200)n (%) | NHP (n=200)n (%) | OR | (95% CI) | P-values | OR | (95% CI) | P-values | |||||
| Sex | ||||||||||||||
| Female | 53 | (27) | 84 | (42) | 92 | (46) | 97 | (48) | 1.00 | (REF) | 1.00 | (REF) | ||
| Male | 147 | (73) | 116 | (58) | 108 | (54) | 103 | (52) | 2.0 | (1.3–3.1) | 0.001 | 1.1 | (0.7–1.6) | 0.62 |
| Age (years) | ||||||||||||||
| 0–5 | 3 | (2) | 7 | (4) | 3 | (2) | 4 | (2) | 0.5 | (0.1–2.0) | 0.34 | 1.9 | (0.4–9.3) | 0.38 |
| 6–19 | 3 | (2) | 16 | (8) | 3 | (2) | 35 | (18) | 0.2 | (0.1–0.8) | 0.02 | 0.2 | (0.07–0.8) | 0.02 |
| 20–34 | 60 | (30) | 71 | (36) | 40 | (20) | 106 | (53) | 1.00 | (REF) | 1.00 | (REF) | ||
| 35–54 | 90 | (45) | 77 | (40) | 78 | (39) | 48 | (24) | 1.4 | 0.9–2.2 | 0.17 | 4.3 | (2.6–7.2) | <0.0001 |
| ≥55 | 44 | (23) | 29 | (15) | 74 | (37) | 7 | (4) | 1.8 | (1.0–3.2) | 0.05 | 28 | (12–66) | <0.0001 |
| Comorbidities | ||||||||||||||
| None | 121 | (61) | 170 | (85) | 97 | (49) | 187 | (94) | 1.00 | (REF) | 1.00 | (REF) | ||
| HTN alone | 35 | (22) | 14 | (8) | 37 | (28) | 7 | (4) | 3.5 | (1.8–6.8) | 0.0002 | 10.2 | (4.4–23.7) | <0.0001 |
| DM alone | 9 | (7) | 6 | (3) | 11 | (10) | 2 | (1) | 2.1 | (0.7–6.1) | 0.16 | 10.3 | (2.3–47.4) | 0.003 |
| HTN and DM alone | 15 | (8) | 0 | (0) | 21 | (11) | 0 | (0) | 43.5 | (2.6–734) | 0.009 | 83 | (4.9–1379) | 0.002 |
| Any other comorbidities | 20 | (14) | 10 | (5) | 34 | (26) | 4 | (2) | 2.8 | (1.3–6.2) | 0.01 | 16.3 | (5.7–47.5) | <0.0001 |
| Age and comorbidities | ||||||||||||||
| <55 years/none | 105 | (53) | 155 | (78) | 64 | (32) | 182 | (91) | 1.00 | (REF) | 1.00 | (REF) | ||
| <55 years/HTN alone | 22 | (17) | 5 | (3) | 15 | (19) | 6 | (3) | 6.5 | (2.3–17.6) | 0.0003 | 7.1 | (2.6–19.1) | 0.0001 |
| <55 years/HTN and DM alone | 6 | (3) | 0 | (0) | 9 | (5) | 0 | (0) | 19.1 | (1.1–343) | 0.04 | 54.8 | (3.1–936) | 0.006 |
| <55 years/other comorbidities | 23 | (12) | 11 | (6) | 36 | (18) | 5 | (3) | 3.1 | (1.4–6.6) | 0.004 | 20.5 | (7.7–54.4) | <0.0001 |
| ≥55 years/none | 16 | (16) | 15 | (8) | 31 | (16) | 5 | (3) | 1.6 | (0.7–3.3) | 0.23 | 18 | (6.6–47.5) | <0.0001 |
| ≥55 years/HTN alone | 13 | (7) | 9 | (5) | 21 | (11) | 1 | (1) | 2.1 | (0.9–5.2) | 0.09 | 59.7 | (7.9–452) | 0.0001 |
| ≥55 years/HTN and DM alone | 9 | (5) | 0 | (0) | 12 | (6) | 0 | (0) | 28.0 | (1.6–486) | 0.02 | 70.7 | (4.1–1211) | 0.003 |
| ≥55 years/other comorbidities | 6 | (3) | 5 | (3) | 7 | (4) | 1 | (1) | 1.8 | (0.5–6.0) | 0.36 | 20.0 | (2.4–164) | 0.006 |
| Vaccination status | ||||||||||||||
| Unvaccinated | 200 | (100) | 200 | (100) | 189 | (94) | 180 | (90) | NA | NA | 1.00 | (REF) | ||
| One dose | 0 | (0) | 0 | (0) | 9 | (5) | 17 | (9) | NA | NA | 0.50 | (0.21–1.2) | 0.11 | |
| Two dosesa | 0 | (0) | 0 | (0) | 2 | (1) | 3 | (1) | NA | NA | 0.63 | (0.10–3.8) | 0.62 | |
| Any doses | 0 | (0) | 0 | (0) | 11 | (6) | 20 | (10) | NA | NA | 0.52 | (0.24–1.1) | 0.10 | |
HP, hospitalized patients; NHP, non-hospitalized patients; HTN, hypertension; DM, diabetes mellitus; OR, odds ratio; CI, confidence interval.
None of these patients had completed 14 days after vaccination before illness onset
Note: Where zeroes in cells interfered with obtaining an interpretable odds ratio, 0.5 was added to all cells.
Table 4.
Characteristics associated with death among hospitalized patients with coronavirus disease 2019 in Waves 1 and 2, Uganda, 2020–2021.
| Characteristics | Wave 1 |
Wave 2 |
Wave 1 |
Wave 2 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Died (n=12)n (%) | Survived (n=188)n (%) | Died (n=53)n (%) | Survived (n=147)n (%) | OR | (95% CI) | p | OR | (95% CI) | P | |||||
| Sex | ||||||||||||||
| Female | 3 | (25) | 50 | (27) | 18 | (33) | 74 | (50) | 1.00 | (REF) | 1.00 | (REF) | ||
| Male | 9 | (75) | 138 | (73) | 35 | (67) | 73 | (50) | 1.1 | (0.3–4.2) | 0.9 | 2.0 | (1.0–3.8) | 0.04 |
| Age (years) | ||||||||||||||
| <55 | 2 | (17) | 154 | (82) | 19 | (36) | 105 | (72) | 1.00 | (REF) | 1.00 | (REF) | ||
| ≥55 | 10 | (83) | 34 | (18) | 34 | (65) | 40 | (28) | 22.6 | (4.7–108) | <0.0001 | 4.7 | (2.4–9.2) | <0.0001 |
| Comorbidities | ||||||||||||||
| None | 4 | (33) | 117 | (62) | 21 | (38) | 76 | (52) | 1.00 | (REF) | 1.00 | (REF) | ||
| Hypertension | 4 | (33) | 31 | (16) | 14 | (27) | 23 | (16) | 3.8 | (0.8–15.9) | 0.07 | 2.2 | (1.0–5.0) | 0.06 |
| Diabetes | 1 | (20) | 8 | (6) | 2 | (9) | 9 | (10) | 3.7 | (0.4–36.7) | 0.3 | 0.8 | (0.2–4.0) | 0.8 |
| Hypertension and diabetes | 2 | (33) | 13 | (10) | 11 | (34) | 10 | (12) | 4.5 | (0.8–27) | 0.07 | 4.0 | (1.5–10.6) | 0.004 |
| Other comorbidities | 1 | (20) | 0 | (0) | 5 | (19) | 29 | (28) | 78.3 | (2.8–2202) | 0.01 | 0.6 | (0.2–1.8) | 0.4 |
| Age and co-morbidities | ||||||||||||||
| <55 years/none | 1 | (9) | 104 | (55) | 8 | (15) | 56 | (38) | 1.00 | (REF) | 1.00 | (REF) | ||
| <55 years/hypertension | 0 | (0) | 28 | (21) | 4 | (8) | 11 | (7) | 1.2 | (0.1–31.9) | 0.9 | 2.5 | (0.7–9.9) | 0.17 |
| <55 years/other comorbidities | 2 | (17) | 27 | (14) | 4 | (8) | 32 | (22) | 7.7 | (0.7–88.1) | 0.10 | 0.9 | (0.2–3.1) | 0.83 |
| ≥55 years/none | 3 | (27) | 13 | (7) | 13 | (25) | 18 | (12) | 24.0 | (2.3–248) | 0.007 | 5.1 | (1.8–14.1) | 0.002 |
| ≥55 years/hypertension | 4 | (33) | 9 | (5) | 10 | (19) | 12 | (8) | 46.0 | (4.7–459) | 0.001 | 5.8 | (1.9–17.9) | 0.002 |
| ≥55 years/other comorbidities | 1 | (19) | 5 | (3) | 2 | (4) | 5 | 93 (3) | 20.8 | (1.1–383) | 0.04 | 2.8 | (0.5–16.9) | 0.2 |
| Vaccination status | ||||||||||||||
| Unvaccinated | NA | NA | NA | NA | 49 | (94) | 139 | (95) | NA | NA | 1.00 | (REF) | ||
| Partially vaccinated | NA | NA | NA | NA | 3 | (6) | 8 | (5) | NA | NA | 1.1 | (0.27–4.2) | 0.92 | |
OR, odds ratio; CI, confidence interval.
Where zeros in cells interfered with obtaining an interpretable OR, 0.5 was added to all cells.
Discussion
This study found that the first and second waves of COVID-19 in Uganda, caused by distinct SARS-CoV-2 variants, differed across epidemiologic metrics. HP were more often male in Wave 1 than in Wave 2. NHP in Wave 2 were younger than those in Wave 1, while HP were older. Age was strongly associated with hospitalization in Wave 2 but not in Wave 1, and disease was more severe in Wave 2. Older age was associated with death in both Waves 1 and 2, but the strength of association was much stronger in Wave 1. These findings indicate that new SARS-CoV-2 variants may have different epidemiologic characteristics from previous variants, and should be studied independently to ensure that messaging and preparedness are tailored appropriately in each wave.
The sex bias in COVID-19 has been well described, and it is generally accepted that males with COVID-19 are at increased risk of severe disease and death compared with females (Peckham et al., 2020; Gomez et al., 2021; Viveiros et al., 2021). Innate and adaptive immune responses have been suggested to be responsible for the ‘female advantage’ with COVID-19 (Pradhan and Olsson, 2020), as have sex hormones (Chakravarty et al., 2020). However, in the present study, this association of sex with hospitalization group was only true for patients in Wave 1, and not Wave 2. In addition, despite the association between male sex and hospitalization in Wave 1, male sex was only associated with death in Wave 2. This might be due to the relatively small number of deaths among HP in Wave 1 compared with Wave 2.
Hypertension and diabetes were strongly associated with hospitalization in both waves. In part, this may be a result of national recommendations around clinical management of patients with COVID-19 in Uganda (National Guidelines for COVID-19, 2020). Throughout the pandemic, patients with asymptomatic SARS-CoV-2 infection in Uganda, and those with underlying conditions predisposing them to more severe disease, have been encouraged to attend hospital for observation (Kirenga et al., 2020). This is largely due to challenges with obtaining rapid access to advanced health care in some areas of Uganda (Dowhaniuk, 2021). However, this practice became less common after home-based care for patients with COVID-19 was established in late 2020 (Independent News, 2020). Due to this, identification of the association between underlying conditions and death is likely to be more appropriate as a metric of disease severity in this setting than their association with hospitalization. Despite this, while hypertension was associated with a greater proportion of deaths in both waves, only the combination of hypertension and diabetes in Wave 2 was significantly associated with death. Systematic reviews have identified that both hypertension and diabetes are modestly associated with death (De Almeida-Pititto, 2020). The sample size in the present study may have been insufficient to detect an association between these underlying diseases and hypertension in Wave 1, if it existed.
National and social media reports in Uganda during the second wave often stated that more young people were being hospitalized than in the previous wave (CNN, 2021). In addition, media reports elsewhere have suggested that younger people may be more affected by the Delta variant than by previous variants (Bloomberg, 2021; Carolina Press, 2021; Healthline, 2021; UN, 2021). The present data did not substantiate reports of more severe disease among younger patients with the Delta variant. In contrast, this study found that the median age of HP was older in Wave 2 than in Wave 1, while the mean age of NHP was younger in Wave 2 than in Wave 1. The increases in the proportion of younger NHP in Wave 2 coincided with the reopening of schools in Uganda. All schools in Uganda closed in March 2020 to attempt to reduce the impact of the pandemic. In October 2020, schools and educational institutions were reopened for ‘candidates and finalists’ (students in the last year of their level) at boarding schools to allow them to graduate (boarding schools are common in Uganda, especially after primary school level). Although some school-associated outbreaks were reported in Uganda in late 2020 (Independent News, 2021), there were relatively few. Starting in March 2021, immediately before the inception of the second wave of COVID-19 in Uganda, universities reopened and ‘semi-candidate’ classes were restarted. At this time, reports of outbreaks in schools began to increase markedly (Emmanuel, 2021), with nearly 1000 cases in 43 schools reported by mid-June 2021. Following school holiday closures in late April 2021, when parents went to retrieve their children from boarding schools and universities that had closed for the holiday, cases were also reported among family members (Emmanuel, 2021; University World News, 2021). Anecdotally, children returning home often infected their parents. This is plausible as the cause of an increase in the proportion of cases in the school-aged group, as well as in cases in their parents’ age groups (Dispatch, 2021).
HP in Wave 2 were twice as likely to have severe or critical disease or die compared with those in Wave 1; this has also been noted in studies in Scotland (Sheikh et al., 2021). This may be attributed, in part, to the older age of patients in Wave 2, who may have had more comorbidities or weaker immune responses compared with HP in Wave 1, as reported in the April 2020 survey, and in two meta-analysis studies (Kasozi et al., 2020, Singhal et al., 2021). However, some studies suggest that it may reflect a different pathogenesis of the Delta variant compared with earlier variants (Bager et al., 2021, Twohig et al., 2022). One recent study suggested that the Delta variant is associated with two-fold increased risk of hospitalization and increased risk of severe illness among people with co-morbidities, possibly due to increased viral load (Sheikh et al., 2021).
In Uganda, the COVID-19 vaccine only became available between Waves 1 and 2, and only the AstraZeneca vaccine was available to the public (Africa News, 2021). While people receiving the vaccine were initially requested to wait 30 days between doses, this was later modified to 3 months, partly due to vaccine shortages (Guardian, 2021). As a result, no patients in Wave 2 (HP or NHP) were fully vaccinated at the onset of illness. Since this study was conducted, it has been shown that, with a single dose, many vaccines are less effective against the COVID-19 Delta variant compared with other variants (Amirthalingam et al., 2021). This study found a protective but non-significant association between partial vaccination and hospitalization. However, the partially vaccinated population comprised a very small proportion of the overall Wave 2 population, primarily due to low vaccination rates in Uganda at the time. Further investigation of this issue should be conducted as soon as possible to provide additional data about the impact of the vaccine in Uganda.
This study had some limitations. First, because of the rapid nature of the study, only two hospitals, both in the Greater Kampala Metropolitan Area, were included. These hospitals often treat the most severe cases of COVID-19, and thus these data cannot be extrapolated to all HP. In addition, HP and NHP were selected from different sites, which may have resulted in confounding that is difficult to control, particularly with regard to age: people living in Greater Kampala Metropolitan Area may be younger, on average, than people from other areas of the country. However, this would have biased results towards the null, as HP were found to be older, rather than younger, than NHP. In addition, patients at referral hospitals in Kampala and Entebbe may live in any area of Uganda. Unfortunately, data on the district of residence of most patients were not available, so the authors were unable to make a direct comparison with regard to this variable. Second, there were secular changes between Waves 1 and 2 that may have had an impact on care-seeking. Specifically, widespread publicity about the cost of hospitalization during Wave 1 may have dissuaded some people from seeking hospitalization in Wave 2 (VOA News, 2021b). Third, home-based care in Uganda only began in late 2020, and was more well established in Wave 2 than in Wave 1. Before home-based care was established, all ‘high-risk’ people with confirmed SARS-CoV-2 infection, regardless of disease severity, were encouraged to attend hospital for observation in case their situation deteriorated rapidly. While this was still in place in Wave 2, home-based care may have been used increasingly for such patients. This could account, in part, for differences in the frequency of asymptomatic or mild infection among HP in Waves 1 and 2. Fourth, the burden of cases in Wave 2 was greater than in Wave 1, and differences in the quality of care due to overwhelmed health facilities cannot be ruled out. The cause of death was not investigated among cases who died, so it was not possible to evaluate whether or not issues such as oxygen shortages may have been more common in one wave compared with the other. Fifth, sequencing data on the specific patients in the sample were not available, and it was not possible to confirm how many of the patients in Wave 2 (HP or NHP) were infected with the Delta variant. Selection of SARS-CoV-2 isolates for sequencing in Uganda has been non-systematic, and samples in different sequencing periods have come from different areas of Uganda. While most of the patients in Wave 2 in this study who were hospitalized or had samples taken after the third week of May 2021 (comprising 84% of HP and 90% of NHP in this study) were almost certainly infected with the Delta variant, it is not possible to estimate the proportion that were infected with the Delta variant before that time. Finally, the sample size was powered to detect differences in ages of HP and NHP, and thus this study was not powered to identify specific clinical differences of importance. Despite these limitations, the body of data included in this article adds to the limited data available on the Delta variant of COVID-19. Additional data in larger studies are critical to supplement the data in this paper.
Conclusion
Demographic and epidemiologic characteristics of HP and NHP differed between and within the first and second waves of the COVID-19 pandemic in Uganda. New waves and variants of COVID-19 may not reflect the same characteristics as previous waves, and should be studied independently.
Acknowledgments
Ethical approval
This investigation was conducted in response to a public health emergency and was therefore determined to be non-research. The Uganda Ministry of Health gave the directive and approval to investigate rumours on hospitalization of vaccinated COVID-19 patients. Verbal consent was obtained from HP, NHP and next-of-kin for deceased patients. This activity was reviewed by the Centers for Disease Control and Prevention (CDC) and was conducted consistent with applicable federal law and CDC policy (see, for example, 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.).
Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the US CDC.
Author contributions
SE, RN, EJN and HTN contributed to the medical records review and abstraction. SE, JRH, BK, DK and AAR contributed to the study design and refining the methods of analysis. SE, GA, EJN, HTN, RN and JRH contributed to data analysis, and creation of tables and figures. SE and JRH contributed to data interpretation and initial drafting of the manuscript. MA, WM, RN, EJN, HTN, GA, BK, DK, AAR and JRH reviewed the final draft of the manuscript. SE, AAR and JRH verified the underlying data. All authors confirm that they had full access to all the data in the study and accept responsibility to submit for publication.
Conflict of interest statement
None declared.
Funding
Uganda Public Health Fellowship Programme is funded by US CDC, Uganda. No other funding was obtained for this data analysis and the development of this manuscript.
Data sharing
The dataset analysed for the manuscript is available upon request from the corresponding author.
Acknowledgments
The authors wish to acknowledge the Public Health Fellowship Program and the Ministry of Health, Uganda for implementation support; Makerere University School of Public Health for support and oversight; and US CDC, Uganda for financial support. The authors also wish to thank Mulago and Entebbe Grade B Hospitals for the medical records of HP with COVID-19.
References
- Africa News. Uganda starts COVID-19 vaccinations. 2021. Available at: https://www.africanews.com/2021/03/10/uganda-starts-covid-19-vaccinations//(accessed 26 July 2021).
- Amirthalingam G, Bernal JL, Andrews N, Whitaker H, Gower C, Stowe J, et al. Serological responses and vaccine effectiveness for extended COVID-19 vaccine schedules in England. Nat Commun. 2021;12:7217. doi: 10.1038/s41467-021-27410-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bager P, Wohlfahrt J, Fonager J, Rasmussen M, Albertsen M, Michaelsen T, et al. Risk of hospitalisation associated with infection with SARS-CoV-2 lineage B.1.1.7 in Denmark: an observational cohort study. Lancet Infect Dis. 2021;21:1507–1517. doi: 10.1016/S1473-3099(21)00290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair T. Variants in Africa: recommendations for preventing an enduring pandemic. 2021. Available at: https://institute.global/advisory/variants-africa-recommendations-preventing-enduring-pandemic (accessed 30 July 2021).
- Bloomberg. What makes Delta the most disruptive virus variant. 2021. Available at: https://www.bloomberg.com/news/articles/2021-07-23/what-makes-delta-the-most-disruptive-virus-variant-quicktake (accessed 16 August 2021).
- Bugembe DL, Phan M, Ssewanyana I, Semanda P, Nansumba H, Dhaala B, et al. Emergence and spread of a SARS-CoV-2 lineage A variant (A.23.1) with altered spike protein in Uganda. Nat Microbiol. 2021;6:1094–1101. doi: 10.1038/s41564-021-00933-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carolina Press. Covid-19 Delta variant affects younger, unvaccinated populations in NC. 2021. Available at: https://carolinapublicpress.org/47324/covid-19-delta-variant-affects-younger-unvaccinated-populations-in-north-carolina/(accessed 22 August 2021).
- CDC. ITF COVID-19 dashboard Uganda country summary 2021. 2021. Available at: https://app.powerbigov.us/groups/me/apps/8498de59-7f3f-4db4-87fd-49ec8a7565f5/reports/5aba1540-acec-45b5-99ec-cb474020748f/ReportSectiona5e351a0e201faef04f4 (accessed 8 January 2022).
- Chakravarty D, Nair SS, Hammouda N, Ratnani P, Gharib Y, Wagaskar V, et al. Sex differences in SARS-CoV-2 infection rates and the potential link to prostate cancer. Commun Biol. 2020;3:374. doi: 10.1038/s42003-020-1088-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CNN . 2021. Young people suffer most in Uganda's second wave as country grapples with severe vaccine shortages.https://edition.cnn.com/2021/06/11/africa/uganda-vaccines-second-wave-cmd-intl/index.html Available at: accessed 26 July 2021. [Google Scholar]
- De Almeida-Pititto B, Dualib PM, Zajdenverg L, Rodrigues Dantas J, Dias de Souza F, Rodacki M, et al. Severity and mortality of COVID 19 in patients with diabetes, hypertension and cardiovascular disease: a meta-analysis. Diabetol Metab Syndr. 2020;12:75. doi: 10.1186/s13098-020-00586-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dispatch. Over 800 COVID-19 positive cases reported in schools across Uganda. 2021. Available at: https://www.dispatch.ug/2021/05/28/over-800-covid-19-positive-cases-reported-in-schools-across-uganda/(accessed 13 November 2021).
- Dowhaniuk N. Exploring country-wide equitable government health care facility access in Uganda. Int J Equity Health. 2021;20:38. doi: 10.1186/s12939-020-01371-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmanuel O. Museveni closes down schools, suspends gatherings as Coronavirus cases rise. 2021. Available at: https://eyeradio.org/museveni-closes-down-schools-suspends-gatherings-as-coronavirus-cases-rise/(accessed 28 July 2021).
- Fisman DN, Tuite AR. Evaluation of the relative virulence of novel SARS-CoV-2 variants: a retrospective cohort study in Ontario, Canada. CMAJ. 2021;193:E1619–E1625. doi: 10.1503/cmaj.211248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guardian. Ugandan minister blames west for Covid vaccine shortage. 2021. Available at: https://www.theguardian.com/world/2021/jul/11/ugandan-minister-blames-west-for-countrys-covid-vaccine-shortage (accessed 16 August 2021).
- Gomez JM, Du-Fay-de-Lavallaz J, Fugar S, Sarau A, Simmons JA, Clark B, et al. Sex differences in COVID-19 hospitalization and mortality. J Womens Health. 2021;30:646–653. doi: 10.1089/jwh.2020.8948. [DOI] [PubMed] [Google Scholar]
- Healthline. Young people make up biggest group of newly hospitalized COVID-19 patients. 2021. Available at: https://www.healthline.com/health-news/young-people-make-up-biggest-group-of-newly-hospitalized-covid-19-patients (accessed 18 September 2021).
- Independent News. Health ministry releases COVID-19 home care guidelines. 2020. Available at: https://www.independent.co.ug/health-ministry-releases-covid-19-home-care-guidelines/(accessed 7 November 2021).
- Independent News. Health Ministry baffled by reports of COVID-19 cases in schools. 2021. Available at: https://www.independent.co.ug/health-ministry-baffled-by-reports-of-covid-19-cases-in-schools/(accessed 29 July 2021).
- Kadowa I. Using evidence and analysis for an adaptive health system response to COVID-19 in Uganda. 2020. Available at: https://www.equinetafrica.org/sites/default/files/uploads/documents/Uganda%20COVID-19%20Rep%202020.pdf (accessed 26 August 2021).
- Kasozi KI, MacLeod E, Ssempijja F, Mahero M.W, Matama K, Musoke G, et al. Misconceptions on COVID-19 risk among Ugandan men: results from a rapid exploratory survey, April 2020. Front Public Health. 2020;8:416. doi: 10.3389/fpubh.2020.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirenga B, Muttamba W, Kayongo A, Nsereko C, Siddharthan T, Lusiba J, et al. Characteristics and outcomes of admitted patients infected with SARS-CoV-2 in Uganda. BMJ Open Respir Res. 2020;7 doi: 10.1136/bmjresp-2020-000646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Guidelines for COVID-19. 2020. Available at: https://elearning.idi.co.ug/covid-19/wp-content/uploads/2020/08/nationalguidelines-for-COVID-19-secondedition.pdf, (accessed 26 August 2021).
- Peckham H, Gruijter N, Raine C, Radziszewska A, Ciurtin C, Wedderburn L, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11:6317. doi: 10.1038/s41467-020-19741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradhan A, Olsson PE. Sex differences in severity and mortality from COVID-19: are males more vulnerable? Biol Sex Differ. 2020;11:53. doi: 10.1186/s13293-020-00330-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samarasekera U. Feelings towards COVID-19 vaccination in Africa. Lancet Infect Dis. 2021;21:324. doi: 10.1016/S1473-3099(21)00082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh A, McMenamin J, Taylor B, Robertson C, Public Health Scotland, EAVE II Collaborators SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet. 2021;397:2461–2462. doi: 10.1016/S0140-6736(21)01358-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singhal S, Kumar P, Singh S, Saha S, Dey A. Clinical features and outcomes of COVID-19 in older adults: a systematic review and meta-analysis. BMC Geriatr. 2021;21:321. doi: 10.1186/s12877-021-02261-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UN. Delta variant drives Africa COVID threat to ‘whole new level´: WHO warns; ‘dominant’ in Europe by August. 2021. Available at: https://turkey.un.org/en/134283-delta-variant-drives-africa-covid-threat-whole-new-level-who-warns-dominant-europe-august (accessed 3 December 2021).
- University World News . 2021. Universities close again amid surge in COVID cases.https://www.universityworldnews.com/post.php?story=20210616062256305 Available at: accessed 20 November 2021. [Google Scholar]
- Twohig K, Nyberg T, Zaidi A, Thelwall S, Sinnathamby MA, Aliabadi S, et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: a cohort study. Lancet Infect Dis. 2022;22:35–42. doi: 10.1016/S1473-3099(21)00475-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viveiros A, Rasmuson J, Mulvagh J, Yip CY, Norris C, Oudit G. Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones. Am J Physiol Heart Circ Physiol. 2021;320:H296–H304. doi: 10.1152/ajpheart.00755.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VOA News. Uganda to begin nationwide COVID vaccinations Wednesday. 2021a. Available at: https://www.voanews.com/a/covid-19-pandemic_uganda-begin-nationwide-covid-vaccinations-wednesday/6203067.html (accessed 26 July 2021).
- VOA News. Court orders Ugandan Government to regulate COVID-19 treatment costs. 2021b. Available at: https://www.voanews.com/a/covid-19-pandemic_court-orders-ugandan-government-regulate-covid-19-treatment-costs/6208003.html (accessed 18 November 2021).
- WHO. COVID-19 in the WHO African Region. 2020. Available at: https://www.afro.who.int/health-topics/coronavirus-covid-19 (accessed 5 December 2021).