Accessibility to ‘virtual’ cardiac rehabilitation (VCR) whether at home or elsewhere can play a key role in limiting the effects of barriers known to influence whether patients enroll, participate, adhere, and complete center-based CR [1], [2], [3], [4], [5]. The ample amount of evidence supporting the safety and effectiveness of various types of VCR for improving cardiorespiratory fitness and cardiovascular risk factors over the short-to-middle term also does not appear to depend on whether an asynchronous (i.e., without real-time monitoring by healthcare providers) or synchronous service model is used [2,5]. However, despite the notable evidence suggesting VCR should be included as an option for standard of care, in the United States (US) the Centers for Medicare & Medicaid Services (CMS) has not committed to supporting an indefinite presence of the Hospital without Walls initiative for delivering CR services beyond the ongoing Public Health Emergency (PHE) period [2,6]. There is also an equivocal understanding of the potential real-world financial implications to both institutions and patients associated with a VCR model that could be successful in increasing CR utilization, but while also being based on the same CMS rules and regulations governing traditional center-based CR. The financial impact to Medicare and direct out-of-pocket costs incurred by beneficiaries caused by unplanned and unknown levels of VCR utilization and expenditures has yet to be forecasted at either state (e.g., Ohio) or national levels. There may be reasons to worry about both the immediate reality and long-term financial sustainability of the classical center-based CR delivery and billing model translated to a predominant virtual environment. More than ever before, there is unprecedented reason to look to innovate and consider other emerging digital health services, such as remote physiologic monitoring (RPM) [7], for translating the progressive concepts of VCR into a contemporary, cost-effective, and sustainable service for Medicare beneficiaries of all socioeconomic backgrounds.
For calendar years (CY) 2021–2022, CMS updated the Physician Fee Schedule (PFS) and payment policies for RPM services described by Current Procedural Terminology (CPT) codes 99453, 99454, 99457, 99458, and 99091 (see Supplement Table for full code descriptions) [6,7]. We have interpreted these CPT codes as being directly applicable and appropriate for describing possible future annual expenditures at both state and national levels impacted by different levels of VCR utilization amongst Medicare fee-for-service (FFS) beneficiaries ≥65 years of age. On an annual basis, these adults are likely to be ideal candidates for meeting the medical requirements supporting the need for both RPM and CR. Patients within this age sector are not only known to represent a major portion of Medicare FFS beneficiaries meeting CMS eligibility criteria for enrollment in center-based CR under §410.49(b), but most of these individuals are also likely to meet the reasonable medical necessity threshold required to access RPM services by demonstrating multiple chronic conditions [7], [8], [9].
Data focusing on CY 2018 Medicare FFS beneficiaries and center-based CR in the US represents the most up-to-date publically accessible information on performance and quality metrics reflecting CR eligibility, participation, sessions completed, and program completion at both national and individual state levels [8,9]. Therefore, in order to use the latest PFS payment policies to forecast crude direct cost-of-service expenditures representing different levels of future VCR uptake via traditional center-based CR claims policies (CPT codes 93797/98) as compared with billing rules linked to RPM services, we performed cost calculations having to assume census trends in the CY 2018 Medicare FFS beneficiary data would be similarly observed for CY 2021–2022 [7], [8], [9]. We also chose to calculate costs assuming RPM and CR eligible beneficiaries who initiate and complete VCR would do so in an exact three month timeframe since this ideal delivery window represents the most cost-conservative number of weeks an enrollee could be expected to meet the key quality measure of achieving the recommended dose of 36 CR sessions [10]. We did not see it to be clinically helpful to generate forecasts reflecting the maximal allowable observation period (i.e., ≤36 weeks) for completing 36 sessions since CR of this prolonged duration should only occur in extenuating circumstances.
Also relevant to understanding our final cost estimates, none of our forecasts included the additional impact of indirect expenditures associated with key technological resources typical of studies demonstrating VCR efficacy [5]. At the very minimum, Medicare FFS beneficiaries enrolling in VCR could be expected to need access to current generation wearable health technology (e.g., heart rate monitor, accelerometer, etc.), electronic medical record connected data transmittal software/cloud services, and web-based heart health education resources. For VCR approaches largely emphasizing synchronous delivery of care methodology, above-and-beyond technological expenses can be expected to closely follow the CMS requirement of live interactive video and audio streaming capabilities, which is a problematic stipulation included in the current Hospital without Walls initiative [6,7,11]. This level of technological requirement incorrectly assumes fixed terrestrial broadband-grade streaming capacity is readily attainable and/or affordable for Medicare FFS beneficiaries on a national level. The basic-to-advanced technological resource need and availability scaled to the size of the US CR eligible patient population are largely unknown. Nevertheless, current Medicare policy does note that there is no requirement that the digital device used for RPM services needs to be cleared as a medical device by the FDA or meet a specific set of technological standards for monitoring exercise physiologic data; although, submitting claims using CPT codes 99453, 99454, 99457, 99458, and 99091 assumes the selected wearable electronic device meets the general definition of a medical device as described in section 201(h) of the Federal, Food, Drug and Cosmetic Act [7].
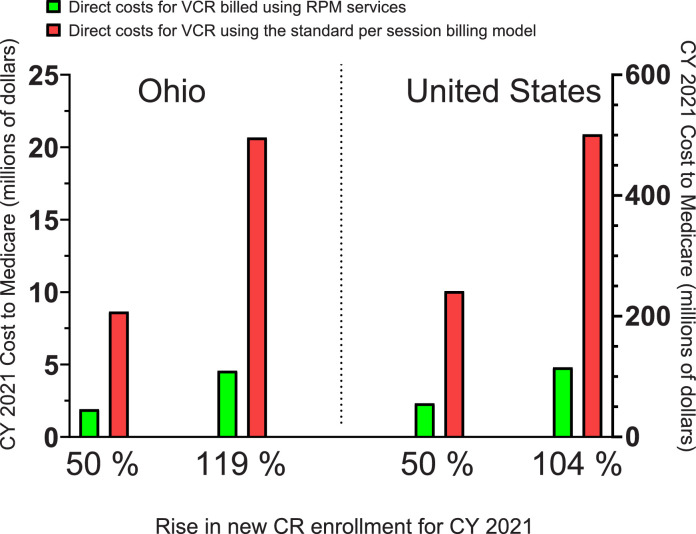
When interpreting our forecasted VCR expenditures illustrated in our Fig. 1, it is important to evaluate not only what effect different levels of VCR uptake could have on annual Medicare costs at state and national levels, but also the marked differences in direct cost-of-service between the two different approaches to VCR. Our forecasts suggest annual gross expenditures for a VCR approach adopting RPM service billing policies could be at least four-fold less than a service based on per session billing standards using CPT codes 93797/98. The per beneficiary cost of VCR via RPM services could be as low as $655.64 and 420 minutes of CR staff time-effort, most of which could be reflective of an asynchronous delivery approach. These would-be per enrollee dollar and staff time-effort costs are in stark contrast to those expected for VCR based on classical per session billing. Our forecasts place those per enrollee expenditure totals in the range of $2,852 to $4,178 and at least 1474 to 2160 minutes of CR staff time-effort associated with the direct supervision of 25 to 36 sessions in a one patient- to- one staff member ratio. This mostly synchronous approach to VCR is not particularly cost effective at the institutional level given center-based CR currently allows for as high as a 5:1 patient- to- staff member ratio.
Fig. 1.
Forecasted calendar year (CY) 2021 direct cost-of-service expenditures for virtual cardiac rehabilitation (VCR) among Medicare fee-for-service (FFS) beneficiaries equal to or greater than 65 years of age for the entire United States (US) or Ohio alone. Initially, CY 2018 data focused on Medicare FFS beneficiaries and center-based CR quality metrics reflective of national and Ohio level CR eligibility, enrollment, sessions, and program completion were used to forecast CY 2021 Medicare expenditures associated with a 50% rise in new CR participation via VCR. Theoretical 119% and 104% increases in new VCR enrollment in CY 2021 for Ohio and the US, respectively, represent what proportional rise in VCR participation would be needed in order to achieve 70% enrollment in CR out of all those who are eligible. Forecasted direct costs for VCR using per session billing refers to the use of CPT codes 93797/98, which are traditionally billed for during center-based CR. Details on the cost breakdown of VCR using CPT codes for remote physiologic monitoring (RPM) services can be viewed in the Supplement Table.
By increasing national CR enrollment via ‘virtual’ participation with the hopes of achieving the 70% enrollment goal of the Million Hearts initiative originally targeted for CY 2022 or shortly thereafter [1], our forecast predicts this would require as much as a 104% rise (n = 175,765) in new enrollment above the total number of participants (∼169,359) [8] recorded for center-based CR in CY 2018 (Fig. 1). This enrollment figure would be accompanied by direct out-of-pocket costs incurred by enrollees totaling at least $100 million if cost calculations are conservatively based on the lowest CY 2021–2022 co-pay rate of $23.22/session and the average number of CR sessions completed (24.6) in CY 2018 for the entire US [8,11]. If VCR enrollees were to be fully compliant in completing the standard dose of 36 exercise sessions, total direct out-of-pocket costs incurred by beneficiaries could swell further to at least $146 million.
As technology evolves and cultivates increasing demand for routine digital and virtual health services, traditional center-based medical specialties such as CR will be presented with new opportunities to expand boundaries of service accessibility, utilization, and delivery. Our forecasts highlight that an innovative, cost-effective, and contemporary approach to VCR is urgently needed if we are to largely rely on the virtual health pathway to fill the major gap required to achieve the national 70% participation goal for CR by the year 2022 or shortly thereafter [1]. Making CR, whether center-based or virtual, an accessible, cost-effective, and sustainable reality for the beneficiaries who historically make up a largest proportion of those eligible for center-based CR will require that patient level expenditures be taken more seriously as a barrier to care and addressed in radically progressive Medicare policy given socioeconomic status is a proven powerful predictor of whether a patient participates, adheres, and completes CR [1,2].
Funding
None.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
References
- 1.Ades PA, Keteyian SJ, Wright JS, et al. Increasing cardiac rehabilitation participation from 20 to 70%: a road map from the Million hearts cardiac rehabilitation collaborative. Mayo Clin Proc. 2017;92(2):234–242. doi: 10.1016/j.mayocp.2016.10.014. Paper presented at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American association of cardiovascular and pulmonary rehabilitation, the American heart association, and the American college of cardiology. Circulation. 2019;140(1):e69–e89. doi: 10.1161/CIR.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 3.Chindhy S, Taub PR, Lavie CJ, Shen J. Current challenges in cardiac rehabilitation: strategies to overcome social factors and attendance barriers. Expert Rev Cardiovasc Ther. 2020;18(11):777–789. doi: 10.1080/14779072.2020.1816464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babu AS, Arena R, Ozemek C, Lavie CJ. COVID-19: a time for alternate models in cardiac rehabilitation to take centre stage. Can J Cardiol. 2020;36(6):792–794. doi: 10.1016/j.cjca.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson L, Sharp GA, Norton RJ, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6(6) doi: 10.1002/14651858.CD007130.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services (CMS) Health and Human Services (HHS). Waivers during Public Health Emergency (PHE), CMS Guidance to Delivering CR/ICR/PR Using Home as a Provider-Based Department (PBD). Vol 86 Federal Register 64996 (19 November 2021), pp. 65244-65250 (https://www.govinfo.gov/app/details/FR-2021-11-19/2021-23972): Office of the Federal Register, National Archives and Records Administration; 2021:65244-65250.
- 7.Centers for Medicare & Medicaid Services (CMS) Health and Human Services (HHS). Medicare Program; CY 2021 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies; Medicare Shared Savings Program Requirements; Medicaid Promoting Interoperability Program Requirements for Eligible Professionals; Quality Payment Program; Coverage of Opioid Use Disorder Services Furnished by Opioid Treatment Programs; Medicare Enrollment of Opioid Treatment Programs; Electronic Prescribing for Controlled Substances for a Covered Part D Drug; Payment for Office/Outpatient Evaluation and Management Services; Hospital IQR Program; Establish New Code Categories; Medicare Diabetes Prevention Program (MDPP) Expanded Model Emergency Policy; Coding and Payment for Virtual Check-in Services Interim Final Rule Policy; Coding and Payment for Personal Protective Equipment (PPE) Interim Final Rule Policy; Regulatory Revisions in Response to the Public Health Emergency (PHE) for COVID–19; and Finalization of Certain Provisions from the March 31st, May 8th and September 2nd Interim Final Rules in Response to the PHE for COVID–19. Vol 85 Federal Register 84472 (28 December 2020), pp. 84472-85377 (https://www.govinfo.gov/content/pkg/FR-2020-12-28/pdf/2020-26815.pdf): Office of the Federal Register, National Archives and Records Administration; 2021:84472-85377.
- 8.Centers for Disease Control and Prevention. Interactive atlas of heart disease and stroke. http://nccd.cdc.gov/DHDSPAtlas, Accessed August 5, 2021 (http://nccd.cdc.gov/DHDSPAtlas).
- 9.Centers for Medicare & Medicaid Services. Multiple chronic conditions. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/MCC_Main, Accessed August 5, 2021 (https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/MCC_Main).
- 10.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American college of cardiology/American heart association task force on performance measures. J Am Coll Cardiol. 2018;71(16):1814–1837. doi: 10.1016/j.jacc.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 11.American Association of Cardiovascular Pulmonary Rehabilitation. Reimbursement update. Medicare 2021 final physician and hospital outpatient regulations and payment rates. https://www.aacvpr.org/Portals/0/Docs/Advocacy/Reimbursement%20Updates/2021/1.06.21%20AACVPR%20Reimbursement%20Update.pdf?ver=2021-01-19-101211-627, Accessed August 5, 2021 (https://www.aacvpr.org/Portals/0/Docs/Advocacy/Reimbursement%20Updates/2021/1.06.21%20AACVPR%20Reimbursement%20Update.pdf?ver=2021-01-19-101211-627).