Abstract
Objective
To systematically catalogue review studies on digital health to establish extent of evidence on quality healthcare and illuminate gaps for new understanding, perspectives and insights for evidence-informed policies and practices.
Methods
We systematically searched PubMed database using sensitive search strings. Two reviewers independently conducted two-phase selection via title and abstract, followed by full-text appraisal. Consensuses were derived for any discrepancies. A standardized data extraction tool was used for reliable data mining.
Results
A total of 54 reviews from year 2014 to 2021 were included with notable increase in trend of publications. Systematic reviews constituted the majority (61.1%, (37.0% with meta-analyses)) followed by scoping reviews (38.9%). Domains of quality being reviewed include effectiveness (75.9%), accessibility (33.3%), patient safety (31.5%), efficiency (25.9%), patient-centred care (20.4%) and equity (16.7%). Mobile apps and computer-based were the commonest (79.6%) modalities. Strategies for effective intervention via digital health included engineering improved health behaviour (50.0%), better clinical assessment (35.1%), treatment compliance (33.3%) and enhanced coordination of care (24.1%). Psychiatry was the discipline with the most topics being reviewed for digital health (20.3%).
Conclusion
Digital health reviews reported findings that were skewed towards improving the effectiveness of intervention via mHealth applications, and predominantly related to mental health and behavioural therapies. There were considerable gaps on review of evidence on digital health for cost efficiency, equitable healthcare and patient-centred care. Future empirical and review studies may investigate the association between fields of practice and tendency to adopt and research the use of digital health to improve care.
Keywords: Digital health, systematic mapping, quality healthcare, mHealth, technology-enhanced
Introduction
Digital health has shifted the paradigm of quality medical care. In the literature, digital health is diversely defined. From a review of 1527 papers, the seminal study by Fatehi et al. 1 finds 95 unique definitions of digital health, yet common to these definitions is digital intervention that examines the provision of healthcare rather than the use of the technology itself. Empowered by the industrial revolution 4.0, digital health invigorates applications of digital technology that changes the landscape of conventional medical practice. As a result, there is an increasing interest to capitalize digital health to improve the quality of healthcare.
To understand how digital health may improve healthcare quality, this study adopts six domains of quality as being defined by the consensus of experts; 2 patient safety, access to healthcare, effective treatment, efficient use of resources, equity of care across subgroups of populations and patient-centred care. The judgement among these experts were in coherence with the following descriptions of quality care from the World Health Organization (WHO). 3 (pp. 9–10) Patient safety relates to the delivery of care which minimizes risks and harms. Effective treatment denotes improved health outcomes to patients and community. Efficiency indicates optimum use of resources that avoid waste. Equitable healthcare concerns on consistent care quality across different subgroup of patient population. Quality of access refers to the delivery of care that is timely, geographically reasonable and appropriate to the medical need. Lastly, patient-centred approach emphasizes care that considers individual patient's preferences, aspirations and the cultures of the community. Therefore, reviewing the notion of quality from these domains provides a multifaceted approach to understand digital health and its roles to improve quality healthcare.
This understanding is important because the literature has reported innovative digital technology contributes towards quality healthcare in various ways. For example, Rahman et al. 4 reported the use of Vis-Screen mobile application to widen population-based screening for visual impairment and blindness. They raised concern that there was a lack of awareness among certain group of population, especially those who were disadvantaged in terms of economy, education and remote areas of residence. In these population, late presentation of ophthalmologic conditions hindered timely intervention, resulting in dire consequences to the quality of life. 4 Similarly, Yang et al. 5 innovated digital neuroradiology imaging database to enhance retrospective research and prospective clinical trials in the field of radiology, neurosurgery, neurology, rehabilitation and others, for patients with brain tumour. The likely contribution on clinical care from application of this technology is reflected by Othman et al. 6 who reported 386 new cases of primary brain tumour were registered within the period of 2013 to 2018 in a neurosurgery department of a tertiary hospital in Malaysia. The gravity of impact on quality care is further magnified by the potential similar findings among tertiary medical centres around the world. Thus, this variety of contributions indicate the rising interest, research and adoption of digital health for quality healthcare.
Paradoxically, the exponential rise of digital health adoption over the last two decades may have created a challenge to establish the extent of impact from digital health on quality healthcare. 7 Challenges associated with digital health include ethical concern on information security, acceptability on new practice, and whether the technology really is practical and feasible to be implemented in real practice. 8 In 13 November 2018, these challenges had prompted the European Union to sanction a public hearing, followed by an official report by expert panel on effective ways of investing in health (EXPH) to assess the impact of digital transformation on health service. 9 In their summary finding, the 14-member expert panel highlighted broad perspectives should be taken in making the decision to adopt, employ or invest new digital health services. 9 Therefore, aligning the evidence with the need of practice, policy and research may depart from eliciting the extent of evidence with the broader aspects of healthcare.
In response, we are conducting this systematic mapping of review studies to gain a wide-ranging perspective on evidence related to the digital health and quality medical care. A systematic mapping is also known as a scoping review as described by Arksey and O’Malley.10,11(pp. 48–49) However, systematic mapping does not appraise the quality of the selected study and consequently does not analyze the results of the selected studies. Instead, a mapping review focuses on systematic cataloguing of selected studies to derive new insight and understanding on the breadth, purpose and trend of research activities on the topic of interest. 12 The importance of systematic mapping is increasingly recognized in the context of providing multi-faceted aspects of evidence including the literature descriptions of an intervention at different places, contexts, time and fields of practice. 13 These broad perspectives of evidence may prove useful and important for complicated evidence-informed policy decision because every institution is unique in its experience, expertise and resources for healthcare quality improvement.
Therefore, this study adopts systematic mapping design as a robust methodological approach to establish the extent of review evidence on digital health for quality healthcare. The following sections of this study will outline the objective, methodology and results of this review. We will then narratively discuss the findings before concluding with the key findings for policies and practices.
Objective
To our knowledge, there is yet a study that reviews the evidence of review studies on digital health and aspects of quality medical care. The objective of this study is to systematically map these review studies to establish six endpoints: (1) general characteristics of review studies on digital health; (2) trend of research activities by year publication; (3) the aim and objective of digital health for quality medical care; (4) approaches to improve the effectiveness of intervention via digital health; (5) type and frequency of digital health interventions; and (6) predominant disciplines of medical practice and their topics for digital health.
Engaging with users of review study
Engaging key stakeholders allows a review study to gain users’ perspectives to help navigate clearer aims and goals that are relevant and meaningful to inform policy and practice. 14 However, this approach was not adopted due to practical challenges related to the COVID-19 lockdown period during the conduct of this study. Alternatively, the objectives of this review were derived through informal engagement with local key stakeholders. This informal engagement was achieved through one reviewer (HMY) who is currently a member of board of director of Universiti Sultan Zainal Abidin (UniSZA) teaching hospital, and another reviewer (RAM) who was a member of UniSZA centre of academic quality. Objectives (4), (5) and (6) were added following both authors’ experience as policymakers and regular engagement with various stakeholders.
Methods
Search strategy
We began by performing rapid synthesis of evidence with data mining via few keywords in PubMed databases such as ‘digital health’ and ‘medicine’. 15 This exercise served as preliminary measures of exploring research activities in the fields of interest, thus guided a more targeted search by indicating arbitrary boundaries of review that was within the time and practical constraints of this study. 16 Consequently, we derived three conceptual frameworks to guide structured searching for studies on digital health on quality medical care: digital health, medicine and review study.
Conducted in the PubMed database, we designed search strings for each conceptual framework to be based on title/abstract and MeSH term. The final Boolean search strings for this study were conducted on 2 June 2021.
Study selection criteria
Following rapid review of evidence, we developed criteria to define the focus and boundaries of this mapping review. The selection criteria were summarized in Table 1.
Table 1.
Criteria for study selection.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population | Studies of quality healthcare that include medical professionals were accepted. | |
| Language | Studies were conducted in English | |
| Study design | Studies were either systematic review, systematic mapping, or scoping review | Original studies, review protocols, literature reviews, and review of review studies (overview, meta-review or umbrella review) |
| Intervention | Studies were researching the use of digital technology to improve patient care. | Reviews that were mainly focusing on:
|
| Comparison | Studies with or without comparison of interventions were accepted | |
| Outcome | Studies reported results that feature any domain of quality care as its main finding or as one of the main findings. | |
| Timeframe | All publication dates were accepted | Duplicates of the same study |
Selecting studies
Selections were conducted by two independent reviewers (MSI and YIAB). Reviewers initially rejected irrelevant studies based on title and abstract. If there was any doubt for exclusion, studies were accepted for the full text screening. All discrepancies between reviewers were resolved by consensus.
Extracting studies
All title and abstract of included studies were imported into reference manager Endnote 20. Then all details of the final included studies were extracted into a standardized data mining template in Microsoft Excel with structure as shown in Supplemental Appendix 1.
Quality appraisal and search for grey literature
Both quality appraisal and search for grey literature were not applicable for this study which aimed to systematically catalogue the research activities to achieve broad perspectives on the evidence in this field. 17 Consequently, the results of the selected reviews were presented in the appendix section (Supplemental Appendix 2). This approach was adopted as a measure of good practice to avoid misleading the readers that the included reviews had been critically appraised. 18
Data analysis
PRISMA flowchart 19 for the selection process and systematic mapping of all included reviews based on standardized data extraction tool were constructed. Data were analyzed and narratively summarized using descriptive statistics in tables or graphs for each objective of the study. Descriptive statistics were computed using Microsoft Excel 20 while Microsoft Power BI 21 was used for visualization of spatial data.
Results
Search and selection
The structured searching via search strings based on conceptual frameworks returned 4545 studies regarding digital health, 2,709,890 articles concerning medicine, and 199,138 publications on review study. The final Boolean search operation revealed a total of 155 studies that were relevant for all three conceptual frameworks. Table 2 provides summary of the structured search strategy used in this study.
Table 2.
Results of the structured searching.
| No. | Conceptual framework | Search string | Number of returned publications |
|---|---|---|---|
| #1 | Digital health | (digital health[Title/Abstract]) OR (digital health[MeSH Terms]) | 4545 |
| #2 | Medicine | ((((((medicine[Title/Abstract])) OR (medical[Title/Abstract])) OR (doctor[Title/Abstract])) OR (medicine[MeSH Terms])) OR (medical[MeSH Terms])) OR (doctor[MeSH Terms]) | 2,709,890 |
| #3 | Review study | (((((systematic review[Title/Abstract]) OR (scoping review[Title/Abstract])) OR (systematic mapping[Title/Abstract])) OR (systematic review[MeSH Terms])) OR (scoping review[MeSH Terms])) OR (systematic mapping[MeSH Terms]) | 199,138 |
| #4 | Final search | ((#1) AND (#2)) AND (#3) | 155 |
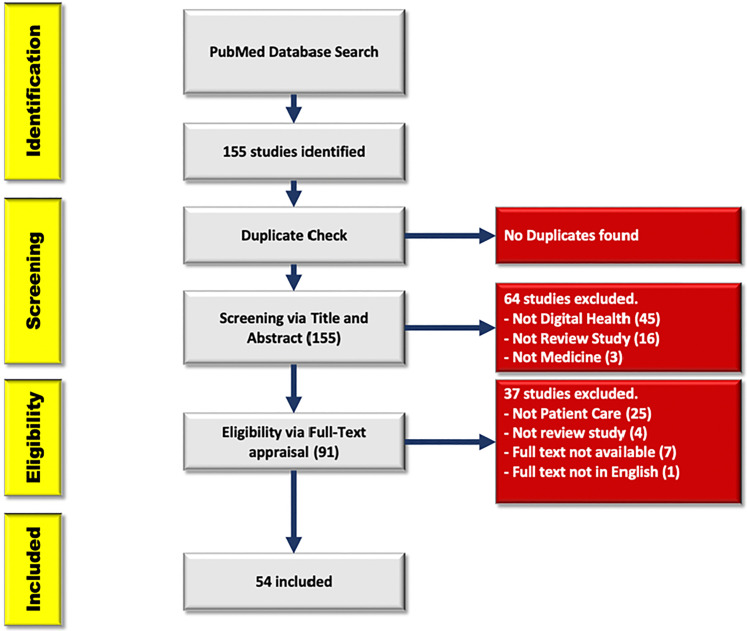
From these 155 studies, no duplications were found. Subsequently, 64 studies were removed during first stage of selection via title and abstract. Further 37 studies were excluded following second stage selection by full text appraisal. Figure 1 summarizes the PRISMA flow diagram 19 for the final 54 reviews for data extraction.
Figure 1.
PRISMA flow diagram 19 of the selection process.
Data mapping of included reviews
Mapping of data by standardized data extraction tool for all 54 reviews established the extent of review evidence to answer all six endpoints of this study. Table 3 provides results of data mapping conducted in this study.
Table 3.
Data mapping for 54 reviews on digital health for quality healthcare.
| No | Author | Type of review * | Topic of review | No. of studies | Main field of discipline | Digital health identified in the review | Domain of quality medical care | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Effective intervention | |||||||||||||||||||||||||||||
| Mobile apps * | Computer-based * | Sensor-based technology | Electronic-Record-based | A.I. * | Telemedicine * | Wearable device | SMS | Game Consoles | Internet of Thing (IoT) | AR/VR * | Endoscope-equipped smartphone | Electronic Medication Container | Videocassette | Telephone Consult | Patient Safety | Efficient use of resources | Access to healthcare | Patient- centred Care | Equity | Improving Health Behaviour | Treatment compliance | Enhanced Clinical Assessment | Better Care Coordination | ||||||
| 1 | Aapro et al. 22 | Sys.R | Supportive care in Oncology | 52 | Oncology | X | X | X | X | X | X | X | X | X | |||||||||||||||
| 2 | Robbins et al. 23 | Sys.R | Healthy Aging | 51 | Multidisciplinary | X | X | X | X | X | X | X | X | ||||||||||||||||
| 3 | Slattery et al. 24 | Sys.R + MA | Chronic Pain | 30 | Multidisciplinary | X | X | X | X | X | X | ||||||||||||||||||
| 4 | El Morr & Layal, 25 | Sys.R | Intimate Partner Violence | 25 | Multidisciplinary | X | X | X | X | X | X | ||||||||||||||||||
| 5 | Beleigoli et al. 26 | Sys.R + MA | Obesity | 11 | Multidisciplinary | X | X | X | X | ||||||||||||||||||||
| 6 | Davies et al. 27 | Sys.R + MA | Depression, Anxiety, and psychological well-being | 17 | Psychiatry | X | |||||||||||||||||||||||
| 7 | Biagianti et al. 28 | Sys.R | Psychosis | 8 | Psychiatry | X | X | X | X | ||||||||||||||||||||
| 8 | Rose et al. 29 | Sys.R + MA | Adolescent health - Diet and healthy behaviour | 27 | Psychiatry | X | X | X | X | X | |||||||||||||||||||
| 9 | Lau et al. 30 | Sys.R + MA | Youth with chronic illness | 16 | Psychiatry | X | X | X | |||||||||||||||||||||
| 10 | Gandrup et al. 31 | Sys.R | Remote symptom monitoring | 12 | Multidisciplinary | X | X | X | X | X | X | X | |||||||||||||||||
| 11 | Rollin et al. 32 | Sys.R | Melanoma | 5 | Multidisciplinary | X | X | X | X | X | X | X | X | ||||||||||||||||
| 12 | Sharma et al. 33 | Sys.R + MA | Renal transplantation | 18 | Renal medicine | X | X | X | X | X | |||||||||||||||||||
| 13 | Farnood et al. 34 | Sys.R | Online self-diagnosing | 25 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 14 | Escriva Boulley et al. 35 | Sys.R | Care for patients with cancer | 23 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 15 | Zhou & Parmanto, 36 | Sys.R | Rehabilitation in underserved areas | 10 | Rehabilitation medicine | X | X | X | X | X | X | X | X | ||||||||||||||||
| 16 | Yadav et al. 37 | Sys.R + MA | Fragility fracture recovery | 15 | Multidisciplinary | X | X | X | X | X | X | X | X | X | |||||||||||||||
| 17 | Robinson et al. 38 | Sys.R | Health Behavior and support for patients undergoing elective surgery | 18 | Multidisciplinary | X | X | X | X | X | X | X | X | ||||||||||||||||
| 18 | Gunasekeran et al. 39 | Sc.R | COVID-19 public health responses | 247 | Public Health | X | X | X | X | X | X | X | X | X | X | X | |||||||||||||
| 19 | Milne-Ives et al. 40 | Sys.R + MA | Physical Activity, Diet, Drug and Alcohol use. Mental Health | 52 | Psychological medicine | X | X | ||||||||||||||||||||||
| 20 | Stogios et al. 41 | Sys.R + MA | Hypertension | 17 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 21 | Wang et al. 42 | Sys.R + MA | Rehabilitation after Total Knee or Hip Replacement | 19 | Rehabilitation medicine | X | X | X | X | X | X | X | X | X | X | X | X | ||||||||||||
| 22 | Choukou et al. 43 | Sc.R | Remote care during COVID-19 | 6 | Multidisciplinary | X | X | X | X | X | X | X | X | ||||||||||||||||
| 23 | Kemp et al. 44 | Sc.R | Mental health | 37 | Psychological Medicine | X | X | X | X | X | X | X | |||||||||||||||||
| 24 | Forbes et al. 45 | Sys.R | Supportive care for prostate cancer survivor | 16 | Multidisciplinary | X | X | X | X | X | X | X | X | ||||||||||||||||
| 25 | Lee et al. 46 | Sc.R | Tuberculosis | 145 | Multidisciplinary | X | X | X | X | X | X | X | X | X | |||||||||||||||
| 26 | Liu et al. 47 | Sys.R + MA | Stroke | 13 | Neurology | X | X | ||||||||||||||||||||||
| 27 | Cao et al. 48 | Sc.R | STI and HIV | 21 | Multidisciplinary | X | X | X | X | X | X | X | X | X | X | ||||||||||||||
| 28 | Widmer et al. 49 | Sys.R + MA | Cardiovascular disease (general) | 51 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 29 | Rhodes et al. 50 | Sys.R + MA | Diet, Physical Activity and Weigh Gain in Pregnancy | 11 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 30 | Bergin et al. 51 | Sc.R | Mental health for children and young people | 30 | Psychiatry | X | X | X | X | X | X | ||||||||||||||||||
| 31 | Nanah & Bayoumi, 52 | Sys.R | effective communication in neurosurgical care | 13 | Neurosurgery | X | X | X | X | X | X | X | X | X | X | ||||||||||||||
| 32 | Tornivuori et al. 53 | Sys.R + MA | Transition of care among adolescent with chronic illness | 12 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 33 | Tully et al. 54 | Sc.R | Paediatric Weight Management | 42 | Paediatric | X | X | X | |||||||||||||||||||||
| 34 | Hewitt et al. 55 | Sys.R + MA | Musculoskeletal conditions | 19 | Multidisciplinary | X | X | ||||||||||||||||||||||
| 35 | Bempong et al. 56 | Sc.R | Infectious disease control | 82 | Multidisciplinary | X | X | X | X | X | X | ||||||||||||||||||
| 36 | Robotham et al. 57 | Sys.R + MA | Clinic Attendance | 25 | Multidisciplinary | X | X | X | |||||||||||||||||||||
| 37 | Seppen et al. 58 | Sc.R | Rheumatoid arthritis | 10 | Rheumatology | X | X | X | X | X | X | X | |||||||||||||||||
| 38 | Wang et al. 59 | Sys.R + MA | mental health and quality of life among cancer patients | 7 | Psychiatry | X | X | X | X | X | X | ||||||||||||||||||
| 39 | Nwolise et al. 60 | Sys.R | Preconception care women with diabetes | 12 | Multidisciplinary | X | X | X | |||||||||||||||||||||
| 40 | Triantafyllidis et al. 61 | Sys.R | Childhood obesity | 17 | Multidisciplinary | X | X | X | X | X | X | ||||||||||||||||||
| 41 | Brigden et al. 62 | Sys.R | Children with chronic condition | 17 | Multidisciplinary | X | X | X | X | X | X | X | X | X | |||||||||||||||
| 42 | Li et al. 63 | Sys.R + MA | adverse drug reaction reporting | 13 | Multidisciplinary | X | X | X | X | ||||||||||||||||||||
| 43 | Taj et al. 64 | Sc.R | Health Behaviour | 631 | Psychological Medicine | X | X | X | X | X | X | ||||||||||||||||||
| 44 | Tilahun et al. 65 | Sc.R | Neglected tropical diseases | 6 | Infectious Disease | X | X | X | X | X | X | X | X | X | X | ||||||||||||||
| 45 | Ngwatu et al. 66 | Sys.R | Tuberculosis | 6 | Multidisciplinary | X | X | X | X | ||||||||||||||||||||
| 46 | Patel et al. 67 | Sys.R + MA | Obesity | 15 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 47 | Jones et al. 68 | Sc.R | PTSD | 38 | Psychiatry | X | X | X | X | X | X | X | X | ||||||||||||||||
| 48 | Batra et al. 69 | Sys.R | Mental Health | 18 | Psychiatry | X | X | X | X | X | X | X | X | ||||||||||||||||
| 49 | Nicholl et al. 70 | Sys.R + MA | Low Back Pain | 6 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 50 | Austin et al. 71 | Sys.R | Anticoagulation therapy | 27 | Multidisciplinary | X | X | X | X | X | |||||||||||||||||||
| 51 | Godinho et al. 72 | Sys.R | Patient-centred care service delivery | 39 | Multidisciplinary | X | X | X | X | X | X | X | X | X | X | X | |||||||||||||
| 52 | Jiang et al. 73 | Sys.R | Cardiovascular diseases | 14 | Multidisciplinary | X | X | X | X | X | X | ||||||||||||||||||
| 53 | Yin et al. 74 | Sc.R | Inflammatory Bowel Disease | 68 | Gastroenterology | X | X | X | X | X | |||||||||||||||||||
| 54 | Tighe et al. 75 | Sys.R | Noncommunicable disease | 7 | Multidisciplinary | X | X | X | X | X | X | X | |||||||||||||||||
Notes. Sys.R + MA: systematic review with meta-analyses; Sys,R: systematic review without meta-analyses; Sc.R: scoping review; AR: augmented reality; VR: virtual reality.
Mobile apps exclude telemedicine. Computer-based include web-based program, emails and offline use of computer program. Artificial intelligence include use of Big Data. AI-based robotics and prediction modelling. Telemedicine include remote video monitoring.
Endpoints
Characteristics of review studies on digital health
This study identified 13 scoping reviews, 20 systematic reviews with meta-analyses and 21 systematic reviews without meta-analyses. From the 54 reviews, institutions of the main author for the reviews were reported from 15 countries; United Kingdom (16), United States (7), Australia (7), Canada (5), Switzerland (4), China (4), Ireland (2), Netherlands (2), and one each for Brazil, Singapore, France, Turkey, Finland, Greece, Ethiopia (Figure 2).
Figure 2.
Review studies on digital health by the countries and regions.
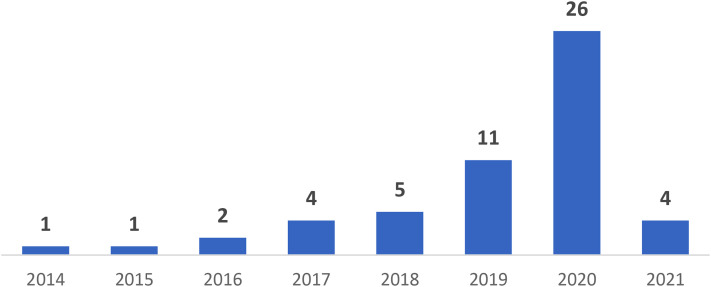
Publication year
There was an increasing number of reviews from one publication in the year 2014 to 26 articles for the year 2020. Figure 3 displays the number of reviewed articles by year of publication.
Figure 3.
Simple bar chart displaying the number of included reviews by year of publication (n = 54).
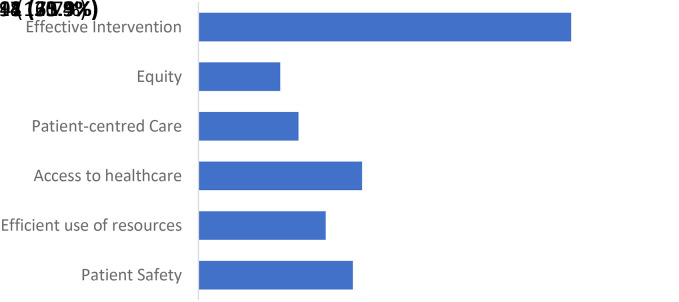
Domains of quality care
Digital health had been reviewed to deliver all six domains of quality healthcare. From the 54 reviews, evidence was mostly prevalent on the aspect of effective intervention (75.9%). Additionally, there were comparable extent of evidence on digital health for accessibility (33.3%), patient safety (31.5%) and efficiency (25.9%). However, there were considerably less number of reviews on digital health for patient-centred care (20.4%) and equitable healthcare (16.7%). Figure 4 summarizes the number of reviews on digital health by domains of quality of care.
Figure 4.
Bar chart presenting the number of articles reporting the different domains of quality medical care (n = 54).
Approaches for effective intervention
Digital health had been reviewed to deliver a more effective intervention via four distinct approaches. The targets of intervention included improving health behaviour (50.0%), enhancing clinical assessment (35.1%), supporting medication compliance or treatment engagement (33.3%) and strengthening coordination of care (24.1%) (Figure 5).
Figure 5.
Bar chart illustrating the frequency of reviews by reported approaches to improve the effectiveness of health intervention (n = 54).
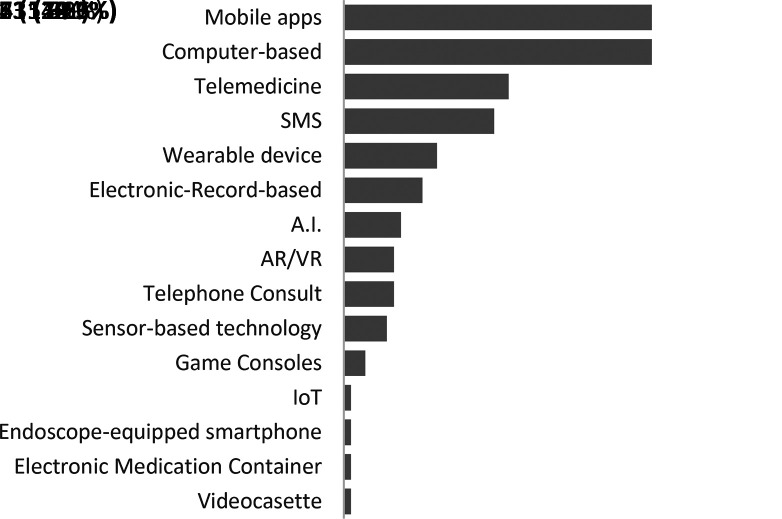
Types of digital health interventions
The data mapping also revealed 15 unique categories of digital health for quality healthcare. Mobile apps and computer-based programs were the most reported digital health intervention. Videocassette, electronic medication container, endoscope-equipped smartphone and IoT each were least applied. Figure 6 presents 15 distinct digital applications used for health interventions reported in the 54 reviews.
Figure 6.
Bar chart providing the information of 15 distinct digital health interventions and the number of reviews reporting their use to improve quality healthcare (n = 54).
Predominant disciplines of medical practice and their topics
Most topic of reviews on digital health for quality healthcare were multidisciplinary in nature (32). However, for single main field of discipline, topics related to psychiatric care emerged as the commonest (11). Table 4 shows predominant disciplines being addressed by the digital health reviews and their topics.
Table 4.
Predominant disciplines being addressed by the digital health reviews and their topics (n = 54).
| No. | Main discipline | Number of reviews | Topic of review | ||
|---|---|---|---|---|---|
| 1 | Multidisciplinary | 32 | Healthy aging Chronic pain Intimate partner violence Obesity (2 reviews) Remote symptom monitoring Melanoma Online self-diagnosing Care for patients with cancer Fragility fracture recovery Health behaviour and support for patients undergoing elective surgery |
Hypertension Remote care during COVID-19 Supportive care for prostate cancer survivor STI and HIV Diet, physical activity and weigh gain in pregnancy Transition of care among adolescent with chronic illness Musculoskeletal conditions Infectious disease control Clinic Attendance Noncommunicable disease |
Preconception care women with diabetes Childhood obesity Children with chronic condition Adverse drug reaction reporting Tuberculosis (2 reviews) Low back pain Anticoagulation therapy Patient-centred care service delivery Cardiovascular diseases (2 reviews) |
| 2 | Psychiatry | 11 | Depression, anxiety, and psychological well-being Psychosis Adolescent health - Diet and healthy behaviour Youth with chronic illness |
Mental health for children and young people Mental health and quality of life among cancer patients PTSD |
Physical Activity, Diet, Drug and alcohol use and mental health Mental health – General (2 reviews) Health behaviour |
| 3 | Rehabilitation care | 2 | Rehabilitation in underserved areas | Rehabilitation after total knee or hip replacement | |
| 4 | Oncology | 1 | Supportive care in oncology | ||
| 5 | Nephrology | 1 | Renal transplantation care | ||
| 6 | Public Health | 1 | COVID-19 public health responses | ||
| 7 | Neurology | 1 | Stroke | ||
| 8 | Neurosurgery | 1 | Effective communication in neurosurgical care | ||
| 9 | Paediatric | 1 | Paediatric weight management | ||
| 10 | Rheumatology | 1 | Rheumatoid arthritis | ||
| 11 | Infectious disease | 1 | Neglected tropical diseases | ||
| 12 | Gastroenterology | 1 | Inflammatory bowel disease | ||
Discussion
To the best of our knowledge, this is the first study to systematically search, select and map review studies on digital health for quality healthcare. A total of 54 reviews are included, ranged from the year 2014 to 2021 with increasing trend till the end of 2020 (Graph 1). From these reviews, a total of 15 distinct digital health interventions are identified (Graph 4) with findings which encapsulate all six domains of quality healthcare (Graph 2), 12 identified group of practices (graph 5), with 51 unique topics of healthcare (Table 3). Therefore, the systematic mapping of compilations of review studies on digital health create new evidence, insight and understanding on quality healthcare which otherwise would have been impossible to derive from individual review.
Effective intervention
The new perspective is evident on the use of digital health primarily to deliver more effective intervention especially via improved health behaviour. For example, to improve diet and physical activities among adolescents, Rose, Barker 29 reported 15 studies were employing web-based program, four were using short messaging system (SMS), three were using gaming approach, and one each was adopting email and other digital platform. All these technologies were primarily used as a medium to deliver educational intervention by providing information and step-by-step guide on how to achieve and maintain healthy diet and physical activities. Similarly, Milne-Ives et al. 40 found a total of 52 randomized controlled trials (RCTs) which targeted the use of mobile apps to drive changes in health behaviour related to diet, physical activities, alcohol and mental health. In a slightly different context, Stogios et al. 41 identified 17 RCTs which investigate the use of digital-based counselling for behaviour change to reduce systolic blood pressure (SBP). Although each review focuses on unique topic of care, all 21 reviews share similar findings of consistent strategy which capitalized the intimate digital technology engagement among mass population to engineer behaviour change for favourable clinical outcomes.
Similar strategy for effective intervention has been extended for technology-enhanced clinical assessment with heightened treatment compliance and engagement. For example, to determine how digital health aids the screening, diagnosis and management of intimate partner violence (IPV), El Morr and Layal 25 have researched 16 RCTs and nine non-RCTs; four pre-post design studies, two cross-sectional studies, two prospective studies and one diagnostic case-control study. The research interest was centred on elucidating the evidence on how the use of desktop computer, laptop, tablet and phone could assist women with IPV to initiate contact and subsequent access to help and care. 25 In comparison, the scoping review on tuberculosis control by Lee et al. 46 identified a total of 43 primary studies which employ various adherence-technologies such as video-observed therapy to encourage patients’ compliance on medication. Likewise, Batra et al. 69 investigated 18 studies which report the use of smart electronic pill container and personal digital record which can provide cues and alerts to improve treatment compliance in hospital setting among patients with serious mental health illness. Thus, the varying intricacy and practices denote how dynamic application of digital health could push the boundaries of conventional approach to improve assessment and treatment compliance.
Setting a new height of more effective intervention is further exemplified in the coordination of complex care. An insightful review by Yadav et al. 37 had compiled evidence from 15 studies from the year 2003 to 2016 on the use of digital health to enhance care on patients with fragility fracture. They reported digital health has been employed at various aspects of care including assisting recovery, education and compliance, treatment engagement, risk reduction for secondary prevention, and communication with the treating team. Yet, common to these aspects of care was the use of digital technology to systematically stage, organize and execute varying duty of care. 37 The tasks include the delivery of digital-based educational package, scheduled phone call by registered nurses, electronic reminder to the treating physician, and systematic collection of clinical history, test results, progress, previous and current treatment regimen for osteoporosis including bisphosphonates and alternatives such as calcitonin and hormone replacement raloxifene. 37 In a more recent context, the scoping review by Gunasekeren et al. 39 has analyzed 247 studies to understand the use of digital health to coordinate the COVID-19 public health responses. Artificial intelligence, telemedicine and big data constitute the main technology being employed. Interestingly, the surge of technology-enhanced coordinated response was justified by the unprecedented scale of impact from the pandemic. Despite the 247 studies were only being conducted since the time of the pandemic in late 2019, 76 the volume of publication of the primary studies in a short period of time highlighted strong commitment for new strategies to address the evolving challenges of care. Therefore, the emerging needs of practice appeared had invigorated the adoption of digital health for effective care coordination and potentially more efficient health intervention.
Other domains of quality healthcare
Unfortunately, complicated aspects of care may have hindered reviews from concluding the use of digital health for cost efficiency. For example, in reviewing the use of digital health for anticoagulation therapy, Austin, Barras 71 reported one study on the use of computerized physician order entry (CPOE) for enoxaparin injection. Yet, deducing cost-effectiveness of digital health for anticoagulation therapy such as CPOE was limited due to scarce availability of primary studies. 71 For similar reason, most reviews which explicitly reported results on cost-effectiveness was reporting this aspect of quality care only as peripheral findings with limited depth to derive a concrete aggregation of results.22,29,36,39,45,52,65 In comparison, Jiang et al. 73 was focusing on the cost effectiveness of employing digital health for cardiovascular diseases (CVDs). All 15 studies identified in the review reported predominant use of telemedicine and wearable devices to achieve cost-efficiency. Yet, heterogeneity of the included studies had limited their conclusion on these digital health to deliver higher quality-adjusted lifeyears or improved clinical outcomes at a lower cost than the standard care. 73 Therefore, despite a huge volume of empirical research and review studies on digital health, the multifaceted aspects of cost-effectiveness may have incurred complex challenges resulting in the gaps of evidence to establish the magnitude of impact, the mechanism and the fidelity of implementation on digital health for cost-efficient healthcare.
Nonetheless, the lack of concrete evidence on cost-efficiency does not negate the strong research interest on accessible, safe and patient-centred care through digital health. For example, Rollin et al. 32 have reviewed five studies on the use of digital health for melanoma care in rural areas and remote communities of Australia. The use of telemedicine has been attributed to improve early detection of skin lesion, facilitate patients’ decision-making, reduced their stress, and empower communication and education. This is in addition of being convenient and save the time for travel. The use of telemedicine has brought fundamental access to quality melanoma care, in addition to reduce the disparity between care in rural and urban areas. 32 Likewise, Godinho et al. 72 have reviewed 39 studies on the use of mHealth to deliver multiple aspects of patient-oriented care including accessibility, equitable care and timely intervention which minimizes risks and harms. The comprehensive review found the use of mHealth such as text messages, mobile apps, phone call and video communication for people-centred care have primarily been used for community-based health issues. These issues include medication compliance, lifestyle activities, diabetes, CVDs and smoking cessation. 72 In these studies, mHealth enhances quality care by enabling patients to bypass gatekeepers for a direct access to healthcare, increasing affordability, empower governance of care, more robust evaluation on safety and strengthening the scheduling and navigation of services. 72 Thus, adoption of digital health for quality healthcare may not only be reactively motivated by the emerging needs of care, but also proactively committed via ongoing determination to set a new benchmark of quality on existing practice.
Trend of review activities on digital health
This motivation is reflected by the large number in each type of reviews. The 13 scoping reviews and 21 systematic reviews without meta-analyses provide meaningful shortcut evidence to the literature. 11 (p. 22) Under the same theme or topic of interest, these reviews illuminate the breadth, purpose and extent of research activities while establish what is known and gaps of evidence. 12 In contrast, the 20 systematic reviews with meta-analyses vigorously search, select, appraise research quality and aggregate evidence from varying contexts and fields of practice to deduce with statistical certainty on the effectiveness of the digital health intervention of interest. 77 Therefore, the increasing number of review studies reflects an escalating motivation to harvest new understanding from these cluster of research to attain deeper insight, broader perspectives and more robust information for decision making.
As a result, the increasing volume of reviews and their diversity in objectives, context, types and topics of interest reflect the heightened interests to establish evidence-informed policies and practices. This trend of reviews is consistent with the increasing trend in the original studies related to the digital health. Compiling digital health research from 2000 until 2018, the review by Taj et al. 64 reported an exponential growth of publications since 2009 attributable to the revolution in smartphone innovation. Supporting this evidence is the result of this study which shows smartphone-based intervention is the most prominent digital health being employed for quality care. Mobile apps, phone calls, video conference and telemedicine and web-based intervention are categories of digital health which can all be delivered via smartphones. Interestingly, smartphones have been available for mostly corporate users since 1993. 78 It is likely the transition of technology users from a niche market to mass population may have served as the key factor that explains the impact and motivation to aggregate research for evidence in this field.
Consequently, the popular smartphone-based digital health to improve health behaviour may elucidate psychiatry as the single field of medical practice most featured in this study. The intrinsic association between favourable change of behaviour and mental health issues may have influenced many aspects of psychiatric care. These aspects include depression, dietary issue, adolescent mental health, substance abuse disorder, psychotic disorder, anxiety and general mental health conditions which made multiple appearance as the focus of reviews on digital health.27–30,40,44,51,64 Cognitive behavioural therapy, mental health examination, timely risk assessment, regular consultations and many other managements of psychiatric patient can directly be enhanced via digital health. Hence, it is likely this association has driven strong advocacy to review digital health to improve clinical outcomes among patients in psychiatric care. This connection also suggests a strong association between research on digital technology, health behaviour and the nature of field of practice.
Suggestion for future direction of reviews on digital health studies
There are notable gaps of evidence on the use of digital health for equitable healthcare, which is the least domain of quality being reviewed (Figure 4). Equitable healthcare addresses reliable services against varying sociodemographic factors such as ethnicity, religion, gender, income and geographic location. 79 Hence, improving equitable care transgress beyond mere improving accessibility. These concerns were highlighted by Bergin et al. 51 whose review reported studies among children on mental health commonly did not include ethnicity and socio-economic status when investigating issue of access to care. Furthermore, improving access and equitable care may be achieved without any change to the routine treatment protocol. Unlike introducing a new strategy, there is less burden of proof to substantiate the effectiveness and safety profile of existing treatments. In contrast, digital health may eliminate or minimize various factors which have disadvantaged certain subgroup of population from otherwise receive a quality healthcare. This is in addition to the surge of technology-users over the last few decades. Therefore, expanding the aggregative and configurative review evidence of digital health for equitable and accessible healthcare, from this aspect, would prove meaningful and impactful due to the scale of target population.
Limitations
There are several limitations of this study. Firstly, the notion of quality is hugely debated, and it is possible that some aspects of quality is not adequately represented in this study. For example, Bate et al. 80 proposed that quality improvement needs to be viewed from social movement approach which comprise both programmatic ‘top-down’ and internally driven ‘bottom-up’ approaches. Grol, 81 in contrast, emphasized the change of culture as a precursor to initiate the culture of change. Tenets of these change of culture include the promotion of reflective practitioners, the power of peers, and patients as partners instead of mere client. 81 Loffler 82 meanwhile insightfully articulated the notion of quality that are essentially evolutionary, rather than static and fragmented in domains. The arguments rewind back to the history of quality from the public sector that transitioned from quality being understood as meeting the expected norms and routines, into effective in meeting the purpose, and finally in fulfilling and exceeding clients’ satisfaction. Understanding the notion of quality from these lenses of perspectives may illuminate unique insight on the roles and evidence of digital health to improve quality care. Nonetheless, expanding the philosophical context of quality and evidence of reviews on digital health require more resources that is beyond the scope of this study.
Secondly, categories of interest are inherently overlap. For example, telemedicine has been referred as remote communication either via voice, or video or both. 36 Yet, these features have also been reported as mobile apps in other reviews.40,43 To be transparent, whenever there is an overlap between descriptions of digital health intervention, this mapping study consistently catalogue based on how the intervention was described by the review. Therefore, the systematic mapping remains robust and transparent despite possible slight variations due to inherent overlapping spectrum of types of digital health and practices.
Conclusion
This study has systematically searched, selected and catalogued review studies on digital health and quality care. Table 5 summarizes key considerations from this study for policy and practice. Majority of reviews describe improved health behaviour, enhanced assessment, treatment compliance and better coordination as the main approach of quality improvement via digital health. Topics related to psychiatry and smartphone-based intervention are the most featured field of practice and the type of digital health respectively. Future studies may investigate the association between field of practice and tendency to adopt and research the use of digital health to improve care. Further reviews may also aggregate evidence on how digital health exerts broader impact on quality care especially in the domain of cost effectiveness and equitable healthcare.
Table 5.
Summary of considerations for policy and practice.
| 1 | Smartphone-based intervention is the commonest digital health for quality healthcare. |
| 2 | Digital health is mainly researched to attain more effective health intervention through improved health behaviour, better medication compliance or treatment engagement, more comprehensive clinical assessment, and enhanced coordination of care. |
| 3 | More empirical and review of evidence is necessary to better-inform the use of digital health for cost-efficient and equitable healthcare. |
| 4 | Most review of evidence on the use of digital health focus on topics related to psychiatric care. |
| 5 | Technology-enhanced quality healthcare may be benefited from research on the association between fields of health practices and the tendency to adopt or research digital health to improve care. |
| 6 | Complex policy decision-making for technology-enhanced quality healthcare may be benefited from the wide-ranging perspectives of evidence via methodologically robust and transparent mapping of digital health interventions at various time, contexts, fields of practice, categories of technology and types of evidence for all six domains of quality healthcare. |
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076221085810 for Digital health for quality healthcare: A systematic mapping of review studies by Mohd Salami Ibrahim, Harmy Mohamed Yusoff, Yasrul Izad Abu Bakar, Myat Moe Thwe Aung, Mohd Ihsanuddin Abas and Ras Azira Ramli in Digital Health
Supplemental material, sj-docx-2-dhj-10.1177_20552076221085810 for Digital health for quality healthcare: A systematic mapping of review studies by Mohd Salami Ibrahim, Harmy Mohamed Yusoff, Yasrul Izad Abu Bakar, Myat Moe Thwe Aung, Mohd Ihsanuddin Abas and Ras Azira Ramli in Digital Health
Acknowledgement
The Author MSI wishes to acknowledge the valuable teaching and training during ‘Systematic reviews: diversity, design and debate’ module from EPPI-Centre, University College London, class of 2017. Experience and skills acquired from the course are pivotal during the conduct of this mapping study. We also thank Mr Afiq Nasri Othman from Infostructure and Network Management Centre, UniSZA, for helping with spatial data visualization via Microsoft Power BI.
Footnotes
Conflict of interest: The authors have no conflicts of interest to declare.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Contributorship: All authors make authorship contributions including conceptualization, expertise, technicalities, preparation of the initial draft, review and revision of the final version of this study.
Ethical approval: None required.
Guarantor: None.
ORCID iDs: Mohd Salami Ibrahim https://orcid.org/0000-0001-5798-7801
Ras Azira Ramli https://orcid.org/0000-0002-7098-5656
Supplemental material: Supplementary materials (Appendix 1 &Appendix 2) for this article is available online.
References
- 1.Fatehi F, Samadbeik M, Kazemi A. What is digital health? Review of definitions. Stud Health Technol Inform 2020; 375: 67–71. DOI: 10.3233/SHTI200696 [DOI] [PubMed] [Google Scholar]
- 2.Dorning H. Consensus on quality, http://www.qualitywatch.org.uk/consensus-quality (2015, accessed 16 January 2017).
- 3.WHO. Quality of care: a process for making strategic choices in health systems, http://www.who.int/management/quality/assurance/QualityCare_B.Def.pdf (2006, accessed 16 January 2017).
- 4.Rahman S, Mutalib A, Baig A, et al. A pilot study on the validation of vis-screen mobile application for vision test J ASIAN Behav Stud 2020; 5: 1. [Google Scholar]
- 5.Yang GL, Tan YF, Loh SC, et al. Neuroradiology imaging database: using picture archive and communication systems for brain tumour research. Singapore Med J 2007; 48: 342–346. [PubMed] [Google Scholar]
- 6.Othman AK, Udin N, Shab MS, et al. Demographic study of brain tumour in a neurosurgical department in Terengganu, Malaysia. Med J Malaysia 2020; 75: 705–709. [PubMed] [Google Scholar]
- 7.Mohd Faeiz P, Siti Norazlina J. Digital transformation of healthcare and medical education, within, and beyond pandemic COVID-19. Asian J Med Biomed 2020; 4. DOI: 10.37231/ajmb.2020.4.2.363. [DOI] [Google Scholar]
- 8.Abu Bakar YI, Hassan A, Yusoff MSB, et al. A scoping review of effective teaching strategies in surface anatomy. Anat Sci Educ 2022; 15: 166–177. DOI: 10.1002/ase.2067. [DOI] [PubMed] [Google Scholar]
- 9.European Commission. Assessing the impact of digital transformation of health services, https://ec.europa.eu/health/sites/default/files/expert_panel/docs/022_digitaltransformation_en.pdf (2019, accessed 20 June 2021).
- 10.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8: 19–32. [Google Scholar]
- 11.Gough D. An introduction to systematic reviews. Edited by David Gough, Sandy Oliver, James Thomas [Kindle Version]. London: Sage, 2012. [Google Scholar]
- 12.Gough D, Thomas J. Commonality and diversity in reviews. In: David Gough SO, Thomas J. (eds) An Introduction to systematic reviews. London: Sage, 2012, pp. 43–70. [Google Scholar]
- 13.James KL, Randall NP, Haddaway NR. A methodology for systematic mapping in environmental sciences. Environ Evidence 2016; 5: 7. [Google Scholar]
- 14.Rees R, Oliver S. Stakeholder perspectives and participation in reviews. In: David Gough SO, Thomas J. (eds) An introduction to systematic reviews. London: Sage, 2012, pp. 19–41. [Google Scholar]
- 15.Booth A, Sutton A, Papaioannou D. Systematic approaches to a successful literature review. 2nd ed. Los Angeles: Sage, 2016. [Google Scholar]
- 16.Oliver S, Sutcliffe K. Describing and analysing studies. In: David Gough SO, Thomas James. (ed) An introduction to systematic reviews. London: Sage, 2012, pp. 123–142. [Google Scholar]
- 17.Gough D, Oliver S, Thomas J. Learning from research: systematic reviews for informing policy decisions. Alliance Useful Evidence 2013; 1: 38. [Google Scholar]
- 18.Rees R. Systematic review: diversity, design and debate: workshop 2 - activity 5&6. UK: UCL, 2017. [Google Scholar]
- 19.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J 2021; 372: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Microsoft Coorporation. Microsoft Excel, https://office.microsoft.com/excel (2018).
- 21.Microsoft Coorporation. Microsoft Power BI, https://powerbi.microsoft.com/en-us/desktop/ (2018).
- 22.Aapro M, Bossi P, Dasari A, et al. Digital health for optimal supportive care in oncology: benefits, limits, and future perspectives. Support Care Cancer 2020; 28: 4589–4612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robbins TD, Lim Choi Keung SN, Arvanitis TN. E-health for active ageing; A systematic review. Maturitas 2018; 114: 34–40. [DOI] [PubMed] [Google Scholar]
- 24.Slattery BW, Haugh S, O’Connor L, et al. An evaluation of the effectiveness of the modalities used to deliver electronic health interventions for chronic pain: systematic review with network meta-analysis. J Med Internet Res 2019; 21: e11086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El Morr C, Layal M. Effectiveness of ICT-based intimate partner violence interventions: a systematic review. BMC Public Health 2020; 20: 1372. DOI: 10.1186/s12889-020-09408-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beleigoli AM, Andrade AQ, Cançado AG, et al. Web-based digital health interventions for weight loss and lifestyle habit changes in overweight and obese adults: systematic review and meta-analysis. J Med Internet Res 2019; 21: e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davies EB, Morriss R, Glazebrook C. Computer-delivered and web-based interventions to improve depression, anxiety, and psychological well-being of university students: a systematic review and meta-analysis. J Med Internet Res 2014; 16: e130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biagianti B, Quraishi SH, Schlosser DA. Potential benefits of incorporating peer-to-peer interactions into digital interventions for psychotic disorders: a systematic review. Psychiatr Serv 2018; 69: 377–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rose T, Barker M, Maria Jacob C, et al. A systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. J Adolesc Health: Off Publ Soc Adolesc Med 2017; 61: 669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lau N, Waldbaum S, Parigoris R, et al. Ehealth and mHealth psychosocial interventions for youths with chronic illnesses: systematic review. JMIR Pediatr Parent 2020; 3: e22329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gandrup J, Ali SM, McBeth J, et al. Remote symptom monitoring integrated into electronic health records: a systematic review. J Am Med Inf Assoc: JAMIA 2020; 27: 1752–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rollin A, Ridout B, Campbell A. Digital health in melanoma posttreatment care in rural and remote Australia: systematic review. J Med Internet Res 2018; 20: e11547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharma V, Piscoran O, Summers A, et al. The use of health information technology in renal transplantation: a systematic review. Transplant Rev (Orlando) 2021; 35: 100607. [DOI] [PubMed] [Google Scholar]
- 34.Farnood A, Johnston B, Mair FS. A mixed methods systematic review of the effects of patient online self-diagnosing in the ‘smart-phone society’ on the healthcare professional-patient relationship and medical authority. BMC Med Inform Decis Mak 2020; 20: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Escriva Boulley G, Leroy T, Bernetière C, et al. Digital health interventions to help living with cancer: a systematic review of participants’ engagement and psychosocial effects. Psychooncology 2018; 27: 2677–2686. [DOI] [PubMed] [Google Scholar]
- 36.Zhou L, Parmanto B. Reaching people with disabilities in underserved areas through digital interventions: systematic review. J Med Internet Res 2019; 21: e12981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yadav L, Haldar A, Jasper U, et al. Utilising digital health technology to support patient-healthcare provider communication in fragility fracture recovery: systematic review and meta-analysis. Int J Environ Res Public Health 2019; 16: 1–22. DOI: 10.3390/ijerph16204047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Robinson A, Oksuz U, Slight R, et al. Digital and mobile technologies to promote physical health behavior change and provide psychological support for patients undergoing elective surgery: meta-ethnography and systematic review. JMIR Mhealth Uhealth 2020; 8: e19237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gunasekeran DV, Tseng R, Tham YC, et al. Applications of digital health for public health responses to COVID-19: a systematic scoping review of artificial intelligence, telehealth and related technologies. NPJ Digit Med 2021; 4: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Milne-Ives M, Lam C, De Cock C, et al. Mobile apps for health behavior change in physical activity, diet, drug and alcohol use, and mental health: systematic review. JMIR Mhealth Uhealth 2020; 8: e17046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stogios N, Kaur B, Huszti E, et al. Advancing digital health interventions as a clinically applied science for blood pressure reduction: a systematic review and meta-analysis. Can J Cardiol 2020; 36: 764–774. [DOI] [PubMed] [Google Scholar]
- 42.Wang X, Hunter DJ, Vesentini G, et al. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord 2019; 20: 06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Choukou MA, Taha A, Qadeer A, et al. Digital health technology for remote care in response to the COVID-19 pandemic: a scoping review. Eur Rev Med Pharmacol Sci 2021; 25: 3386–3394. [DOI] [PubMed] [Google Scholar]
- 44.Kemp J, Zhang T, Inglis F, et al. Delivery of compassionate mental health care in a digital technology-driven age: scoping review. J Med Internet Res 2020; 22: e16263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Forbes CC, Finlay A, McIntosh M, et al. A systematic review of the feasibility, acceptability, and efficacy of online supportive care interventions targeting men with a history of prostate cancer. J Cancer Surviv 2019; 13: 75–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee Y, Raviglione MC, Flahault A. Use of digital technology to enhance tuberculosis control: scoping review. J Med Internet Res 2020; 22: e15727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu S, Feng W, Chhatbar PY, et al. Mobile health as a viable strategy to enhance stroke risk factor control: a systematic review and meta-analysis. J Neurol Sci 2017; 378: 140–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cao B, Bao H, Oppong E, et al. Digital health for sexually transmitted infection and HIV services: a global scoping review. Curr Opin Infect Dis 2020; 33: 44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Widmer RJ, Collins NM, Collins CS, et al. Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clin Proc 2015; 90: 469–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rhodes A, Smith AD, Chadwick P, et al. Exclusively digital health interventions targeting diet, physical activity, and weight gain in pregnant women: systematic review and meta-analysis. JMIR Mhealth Uhealth 2020; 8: e18255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bergin AD, Vallejos EP, Davies EB, et al. Preventive digital mental health interventions for children and young people: a review of the design and reporting of research. NPJ Digit Med 2020; 3: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nanah A, Bayoumi AB. The pros and cons of digital health communication tools in neurosurgery: a systematic review of literature. Neurosurg Rev 2020; 43: 835–846. [DOI] [PubMed] [Google Scholar]
- 53.Tornivuori A, Tuominen O, Salanterä S, et al. A systematic review on randomized controlled trials: coaching elements of digital services to support chronically ill adolescents during transition of care. J Adv Nurs 2020; 76: 1293–1306. [DOI] [PubMed] [Google Scholar]
- 54.Tully L, Burls A, Sorensen J, et al. Mobile health for pediatric weight management: systematic scoping review. JMIR Mhealth Uhealth 2020; 8: e16214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hewitt S, Sephton R, Yeowell G. The effectiveness of digital health interventions in the management of musculoskeletal conditions: systematic literature review. J Med Internet Res 2020; 22: e15617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bempong NE, Ruiz De Castañeda R, Schütte S, et al. Precision global health - the case of Ebola: a scoping review. J Glob Health 2019; 9: 010404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Robotham D, Satkunanathan S, Reynolds J, et al. Using digital notifications to improve attendance in clinic: systematic review and meta-analysis. BMJ Open 2016; 6: e012116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seppen BF, den Boer P, Wiegel J, et al. Asynchronous mHealth interventions in rheumatoid arthritis: systematic scoping review. JMIR Mhealth Uhealth 2020; 8: e19260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang Y, Lin Y, Chen J, et al. Effects of Internet-based psycho-educational interventions on mental health and quality of life among cancer patients: a systematic review and meta-analysis. Support Care Cancer 2020; 28: 2541–2552. [DOI] [PubMed] [Google Scholar]
- 60.Nwolise CH, Carey N, Shawe J. Preconception care education for women with diabetes: a systematic review of conventional and digital health interventions. J Med Internet Res 2016; 18: e291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Triantafyllidis A, Polychronidou E, Alexiadis A, et al. Computerized decision support and machine learning applications for the prevention and treatment of childhood obesity: a systematic review of the literature. Artif Intell Med 2020; 104: 101844. [DOI] [PubMed] [Google Scholar]
- 62.Brigden A, Anderson E, Linney C, et al. Digital behavior change interventions for younger children with chronic health conditions: systematic review. J Med Internet Res 2020; 22: e16924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li R, Zaidi STR, Chen T, et al. Effectiveness of interventions to improve adverse drug reaction reporting by healthcare professionals over the last decade: a systematic review. Pharmacoepidemiol Drug Saf 2020; 29: –8. [DOI] [PubMed] [Google Scholar]
- 64.Taj F, Klein MCA, van Halteren A. Digital health behavior change technology: bibliometric and scoping review of two decades of research. JMIR Mhealth Uhealth 2019; 7: e13311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tilahun B, Gashu KD, Mekonnen ZA, et al. Mapping the role of digital health technologies in the case detection, management, and treatment outcomes of neglected tropical diseases: a scoping review. Trop Med Health 2021; 49: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ngwatu BK, Nsengiyumva NP, Oxlade O, et al. The impact of digital health technologies on tuberculosis treatment: a systematic review. Eur Respir J 2018; 51: 1–11. DOI: 10.1183/13993003.01596-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Patel ML, Wakayama LN, Bass MB, et al. Motivational interviewing in eHealth and telehealth interventions for weight loss: a systematic review. Prev Med 2019; 126: 105738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jones C, Miguel-Cruz A, Smith-MacDonald L, et al. Virtual trauma-focused therapy for military members, veterans, and public safety personnel with posttraumatic stress injury: systematic scoping review. JMIR Mhealth Uhealth 2020; 8: e22079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Batra S, Baker RA, Wang T, et al. Digital health technology for use in patients with serious mental illness: a systematic review of the literature. Med Devices (Auckl) 2017; 10: 237–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nicholl BI, Sandal LF, Stochkendahl MJ, et al. Digital support interventions for the self-management of low back pain: a systematic review. J Med Internet Res 2017; 19: e179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Austin J, Barras M, Sullivan C. Interventions designed to improve the safety and quality of therapeutic anticoagulation in an inpatient electronic medical record. Int J Med Inform 2020; 135: 104066. [DOI] [PubMed] [Google Scholar]
- 72.Godinho MA, Jonnagaddala J, Gudi N, et al. Mhealth for integrated people-centred health services in the western pacific: a systematic review. Int J Med Inform 2020; 142: 104259. [DOI] [PubMed] [Google Scholar]
- 73.Jiang X, Ming WK, You JH. The cost-effectiveness of digital health interventions on the management of cardiovascular diseases: systematic review. J Med Internet Res 2019; 21: e13166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yin AL, Hachuel D, Pollak JP, et al. Digital health apps in the clinical care of inflammatory bowel disease: scoping review. J Med Internet Res 2019; 21: e14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tighe SA, Ball K, Kensing F, et al. Toward a digital platform for the self-management of noncommunicable disease: systematic review of platform-like interventions. J Med Internet Res 2020; 22: e16774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.WHO and China. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) official report, World Health Organization, Geneva, Switzerland, 16–24 February 2020. [Google Scholar]
- 77.Thomas J, Harden A, Newman M. Synthesis: combining results systematically and appropriately. In: Gough D, Oliver S, Thomas J. (eds) An introduction to systematic reviews. London: Sage, 2012, pp. 179–226. [Google Scholar]
- 78.Sarwar M, Soomro T. Impact of smartphone’s on society. Eur J Sci Res 2013; 98: 216-226. [Google Scholar]
- 79.Mayberry RM, Nicewander DA, Qin H, et al. Improving quality and reducing inequities: a challenge in achieving best care. Proc (Baylor Univ Med Cent) 2006; 19: 103–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bate SP, Robert G, Bevan H. The next phase of healthcare improvement: what can we learn from social movements? Qual Saf Health Care 2004; 13: 62–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Richard PTM Gro. Quality improvement in primary care: A change of culture, towards a culture of change. Eur J Gen Pract 2004; 10(2): 43-44. DOI: 10.3109/13814780409094230. [DOI] [PubMed] [Google Scholar]
- 82.Loffler E. Defining quality in public administration. In: NISPAcee conference, Riga, Latvia: Working Group on Better Quality Administration for the Public, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076221085810 for Digital health for quality healthcare: A systematic mapping of review studies by Mohd Salami Ibrahim, Harmy Mohamed Yusoff, Yasrul Izad Abu Bakar, Myat Moe Thwe Aung, Mohd Ihsanuddin Abas and Ras Azira Ramli in Digital Health
Supplemental material, sj-docx-2-dhj-10.1177_20552076221085810 for Digital health for quality healthcare: A systematic mapping of review studies by Mohd Salami Ibrahim, Harmy Mohamed Yusoff, Yasrul Izad Abu Bakar, Myat Moe Thwe Aung, Mohd Ihsanuddin Abas and Ras Azira Ramli in Digital Health