Abstract
The design of N95 filtering facepiece respirators (FFRs) continues to pose usability concerns for healthcare workers, which have been exacerbated by the COVID-19 pandemic. The aim of this study was to develop a holistic model to guide mask design improvement. Dental students (n = 38) with experience wearing N95 FFRs participated in a randomized wear trial of three alternative protective masks. A mixed methods survey was used to examine usability of individual mask design components, the relationship of facial/head area to mask features, and overall mask design. Survey results indicated MNmask v1 demonstrated higher usability in seal confidence (M = 3.46), while MNmask v2 performed higher in satisfactory fit (M = 3.50). Design components of nose wire and head/neck bands were the most problematic, while conditions of skin irritation and tight/loose fit created an unfavorable wear experience. To consider healthcare workers’ needs in improving the usability of protective masks, a model is presented to consider characteristics of fit, comfort, material, and design.
Keywords: Remote usability, Mask design improvement, Holistic mask design approach, N95 filtering facepiece respirators, Healthcare workers, COVID-19
1. Introduction
N95 filtering facepiece respirators (FFRs) continue to be a significant design challenge. Healthcare workers’ (HCWs) usability concerns are widely reported in and outside of past infectious disease outbreaks (Baig et al., 2010; Beckman et al., 2013), and have resurfaced following the emergence of the novel coronavirus disease 2019 (COVID-19). At the beginning of the COVID-19 pandemic, the infectious nature of the disease necessitated an unprecedented level of N95 FFR use to adequately protect those against infection from inhalation of viral particles and transmission of the virus on the frontline. HCWs across the globe took to social media to share their bruised and reddened faces after weeks of wearing FFRs on extended shifts, which highlighted the urgent need to improve the design of N95 FFRs.
As a component of personal protective equipment (PPE), N95 FFRs are designed to be securely fitted to the face with at least 95% filtering efficiency to prevent inhalation of airborne particles of <0.3 μm per the National Institute for Occupational Safety and Health (NIOSH, 1996) standard 42 CFR Part 84. Successful FFR design is dependent on holistically evaluating the interactive system of human factors and ergonomics including people, their abilities (physical, physiological, psychological, and social), and environments (Dul et al., 2012). Usability is an important measure to evaluate mask performance and user well-being; however, in review of the literature, effective research methods and tools to understand usability are lacking. Moreover, there is a limited understanding of the interaction of mask components and their effect on performance and user satisfaction. Without an approach to evaluating the usability of components, it is a challenge to create new, innovative mask designs. There is a need for a design model for evaluating components of N95 FFRs to work toward mask design improvement.
2. Background
2.1. Previous usability studies of N95 FFRs
Previous studies have concluded there is a need to improve the design of N95 FFRs to increase adherence, comfort, and tolerability (Baig et al., 2010; Locatelli et al., 2014). Usability problems reported by healthcare workers include discomfort (Bryce et al., 2008; Baig et al., 2010; Or et al., 2018), breathing difficulties (Baig et al., 2010; Beckman et al., 2013), skin irritation (Baig et al., 2010; Locatelli et al., 2014), tightness (Locatelli et al., 2014; Or et al., 2018), poor fit and effective seal (Locatelli et al., 2014), heat and moisture buildup (Baig et al., 2010; Beckman et al., 2013; Or et al., 2018), and speech intelligibility (Baig et al., 2010; Beckman et al., 2013). Additionally, several studies have developed new respirators to test the usability compared to standard NIOSH-approved N95 FFRs (Radonovich et al., 2019; Suen et al., 2020). The majority of usability criteria are measured quantitatively through closed answer survey responses utilizing yes/no questions, Likert scale, or visual analogue scale. In contrast, Locatelli et al. (2014) used a qualitative method of focus group discussion with HCWs to code themes related to FFR usability. Other studies have used qualitative methods, but these are not exclusive to PPE design, and concentrate on the HCW experience during a pandemic (Corley et al., 2010; Hoernke et al., 2021).
2.2. Reports of N95 FFR usability concerns during the COVID-19 pandemic
The need to improve the usability and design of N95 FFRs has been documented by HCWs during the COVID-19 pandemic (Law, 2020; Hu et al., 2020; Lan et al., 2020; Yuan et al., 2021; Chan et al., 2021; Hignett et al., 2021; O'Kelly et al., 2021; Jiang et al., 2021; Purushothaman et al., 2021; Williams et al., 2021; Ong et al., 2020; Rahne et al., 2021; Isaacs, 2021; Ruskin et al., 2021). Reported side effects, injuries, and usability issues became more extreme and exacerbated during the pandemic due to increased use of N95 FFRs. Table 1 contains a summary of mask wear issues commonly cited during the COVID-19 pandemic. However, many of these reported issues can be mitigated with a strong respiratory protection program in place per 29 CFR 1910. 134, which includes training to achieve a proper fit and user seal check (OSHA, 2004).
Table 1.
Mask wear issues commonly cited during COVID-19.
| Mask Wear Issues During COVID-19 | Description | Reference |
|---|---|---|
| Skin conditions and injuries | Pressure ulcers, scarring, itchiness, acne, rash, bruising |
Law (2020) Hu et al. (2020) Lan et al. (2020) Yuan et al. (2021) |
| Fit | Loose-fitting, tight-fitting, low confidence in mask seal, poor fit because of wrong size available |
Chan et al. (2021) Hignett et al. (2021) O'Kelly et al. (2021) |
| Physical discomfort | Sensation of pressure/tightness, difficulty breathing, heat/moisture buildup, odor, sweating |
Jiang et al. (2021) Purushothaman et al. (2021) Yuan et al. (2021) |
| Side effects | Headaches, dizziness, dehydration, heat stress, nausea, fatigue |
Williams et al. (2021) Ong et al. (2020) Yuan et al. (2021) |
| Task interference | Difficulty donning and doffing, reduced speech intelligibility, interference with patient communication |
Rahne et al. (2021) Isaacs (2021) Ruskin et al. (2021) |
2.3. The design of FFRs
While a quantitative survey method is effective in providing generalized usability responses from HCWs, previous studies fail to provide enough details regarding usability to improve mask design. Through examining usability studies prior to the COVID-19 pandemic against HCW experience during the pandemic, it is evident that the usability of FFRs failed to significantly improve. Mask design is complex and requires rigorous scientific evaluation of materials to ensure the filtering media meets minimum material standards set by NIOSH (1996) under 42 CFR Part 84. However, the task of evaluating components in terms of usability, comfort, and fit is not well-researched.
At minimum, traditional FFRs consist of filtering media tested to NIOSH (1996) standards (42 CFR Part 84), the ability to create a seal on the face through a nose wire or similar apparatus conforming to the nose, and two stretchable bands that wrap around the head and secure the mask to the face. N95 FFRs typically cover half of the face, including the mouth, nose, chin, cheeks, and a portion of the head. The comfort of straps and nose wire, and the size and shape of the filtering media have been mentioned in previous studies as needing improvement (Locatelli et al., 2014; Or et al., 2018; Radonovich et al., 2019; Suen et al., 2020), but the details of comfort in relation to specific components and facial zones have not been specified.
For design purposes, mask usability needs to be understood in the context of the body-product relationship. The fit and function of a mask are interrelated, where poor mask fit in one area of the face can cause poor fit in other areas, or disturb the mask seal. There is a need to evaluate all areas of both the body (head) and the product (mask) independently and as a whole to address the complexities of fit, comfort, and usability in future FFR design innovation.
3. Purpose
The purpose of this research was to explore a holistic approach in evaluating the usability of emergency-use protective masks and their components for application of mask design improvement. Drawing from a remote usability study of emergency-use protective face masks carried out in March 2021, this research aimed to extend knowledge in the methods for evaluating the usability of masks in relation to design components and facial and head zones. We believe that a usability analysis of mask components and fit location can reveal considerations for improving holistic mask design and user safety and well-being.
4. Methods and materials
4.1. Study design
This study used a repeated measures, mixed methods design to evaluate the comparative usability of three emergency-use protective face masks. Due to pandemic conditions, and to ensure the safety of participants, a procedure was developed to conduct usability testing remotely. Ethical approval for this study was obtained by the University of Minnesota Institutional Review Board.
4.2. Masks
In the spring of 2020, an interdisciplinary team of researchers at the University of Minnesota assembled to address the rising critical shortages of N95 FFRs. An iterative process of designing, prototyping, and testing followed to develop MNmasks, emergency-use protective face masks to be utilized in crises when the recommended alternatives of N95 FFRs are not available (Griffin et al., 2022). MNmasks feature a simple fabrication process where specialized machinery and an experienced workforce are not required. The masks are quickly assembled by hand using components sourced from non-endangered supply chains, which includes commercially available air filter media and non-traditional components such as rubber bands, foam, and staples. For this study, two models of MNmasks were included for usability testing. MNmask v1 is an earlier model developed in spring 2020 and MNmask v2 is an updated model to achieve better fit developed over fall and winter 2020–21.
Table 2, Table 3 describe the style and component characteristics of the three masks tested. In addition, the performance of the three masks were tested to determine quantitative fit factor and filtration efficiency (Table 4 ). Fit tests for the three masks were conducted with a convenience sample of participants (n = 9) following OSHA (2004) protocol 29 CFR 1910.134 with the PortaCount Pro + Respirator Fit Tester 8038 (TSI Inc., Shoreview, MN, USA). The sample size was limited due to pandemic restrictions, and further testing will be included in a future publication. Filtration tests of mask media were conducted using the method of fractional filtration efficiency over a particle size range between 0.03 and 1.0 μm (Ou et al., 2020). A limitation of this study is the absence of an N95 FFR for comparison. N95 models commonly used in healthcare, such as the 3M 1860, 1860S or 1870+ (3M Company, St. Paul, MN, USA) are suitable for comparison; however, N95 FFRs were still in short supply at the time of study data collection. In lieu of an N95, a KN95 model that is not NIOSH-approved was selected as an alternative (FDA, 2020).
Table 2.
Style description of masks.
| MNmask v1 | MNmask v2 | KN95 | |
|---|---|---|---|
 |
 |
 |
|
| Size range | S, M/L | S, M/L | One-size |
| Style description | Emergency-use face mask featuring a heat-sealed pouch design, foam interior lining for fit and comfort, internal nose wire, and a versatile head/neck band for a proper seal. | Emergency-use face mask featuring a folded pouch design, foam interior lining for fit and comfort, internal nose wire, and an adjustable head/neck band system to prevent breaks in seal for various face shapes and sizes. | Non-medical use only KN95 mask featuring a flat-fold design with heat sealed elastic ear loops and an external nose clip for a proper seal. |
| Certification | FDA issued EUAa Not NIOSH approved |
FDA issued EUA Not NIOSH approved |
Chinese Standard GB2626-2006 Tested |
EUA: Emergency Use Authorization.
Table 3.
Component description of masks.
| MNmask v1 | MNmask v2 | KN95 | |
|---|---|---|---|
| Filter media: Provides two-way protection of harmful particles breathed in and breathed out. |
Cummins Industries: EX101 |
Cummins Industries: EX101 |
4-ply non-woven polypropylene, melt-blown filter inner layers |
| Nose wire: Secures the seal around the nose bridge. |
Bedford Industries: Plastic coated double wire strip (internal) |
Adhesive-backed aluminum strip (internal) | Adhesive-backed aluminum strip (external) |
| Foam: Provides a cushion for fit and comfort. |
Vinyl, closed cell, pressure to compress 25%: 4 psi Placement: lines inside edge of full perimeter, ⅛” thick x ¾” wide |
Vinyl, closed cell, pressure to compress 25%: 4 psi Placement: lines inside edge of full perimeter, ⅛” thick x ½” wide upper; ¾” wide lower |
N/A |
| Bands: Anchors mask to fit securely around the nose, cheeks, and underneath chin. |
Non-latex rubber band | Nylon paracord (head) and elastic string cord (neck) with plastic cord lock toggles | Round elastic ear loops |
Table 4.
Performance of masks.
| MNmask v1 | MNmask v2 | KN95 | ||
|---|---|---|---|---|
| Fit factor (n = 9) | Pass rate | 2 out of 9 | 7 out of 9a | 0 out of 9b |
| Mean (S.D.) | 93.32 (141.35) | 438.00 (436.15) | 4.86 (2.15) | |
| Filtration efficiency (particle size range 0.03–1.0 μm) | >95% | >95% | 88%–94% | |
See Griffin et al. (2022) for further information.
Reflects the score of an improved modification to nose wire durability and band fit.
Reflects the score of a similar KN95 mask (GB2626-2006 certified) tested for another publication.
4.3. Participants and setting
Participants were recruited via convenience sampling through coordination with an accredited dental education program in the midwest region of the United States. A group of 38 dental students enrolled in this study. This population met the inclusion criteria requirements of HCWs with experience wearing N95 FFRs in the clinical setting. Exclusion criteria included participants with a beard or a history of respiratory complications due to potential interference with mask seal and the breathing resistance of FFRs, respectively. Written informed consent was obtained prior to enrollment, and participation was voluntary.
The researchers coordinated with dental education instructors to test students in the classroom setting without interruption to their studies. Mask kits were delivered to the testing site, and were handed out to students on the first day of testing. All communication with participants was conducted remotely over a secure video conferencing platform and was projected at the front of the classroom to provide instruction for the wear trials.
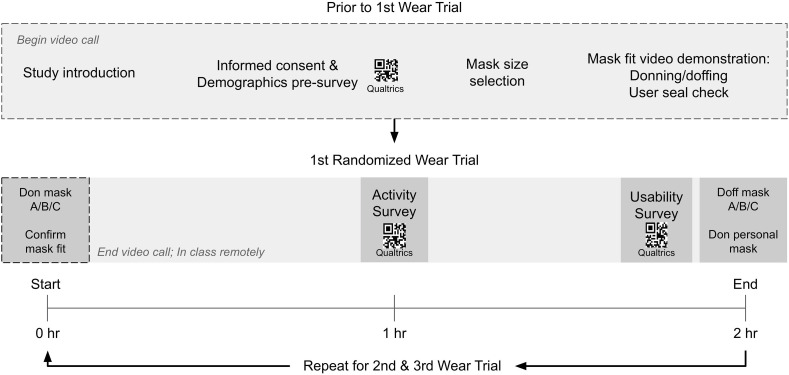
4.4. Data collection
Each mask wear trial was completed during a scheduled class meeting time of 2 h. The researchers coordinated with four instructors to conduct three usability sessions in consecutive class meeting times over the course of three weeks. In total, 12 usability sessions were completed for all participants to test each of the three masks. Throughout the procedure, the order of masks was randomized to minimize the impact of bias.
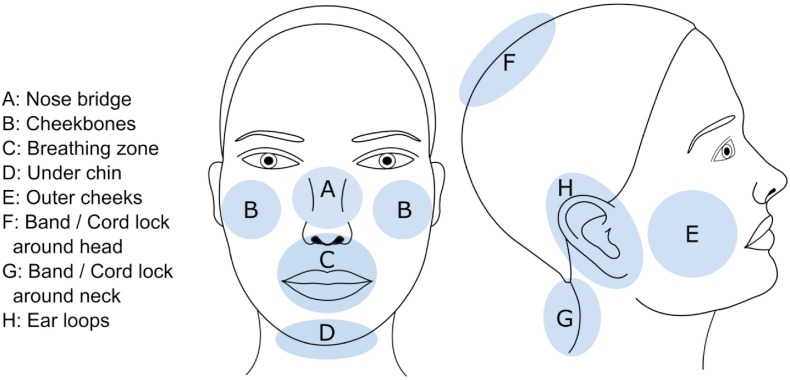
A survey instrument was designed using Qualtrics survey platform (Qualtrics LLC, Provo, UT, USA) and was administered via mobile by scanning a QR code. The surveys had three parts: 1) a demographics pre-survey; 2) an activity survey to measure the performance of the masks; and 3) a usability survey to measure subjective evaluation of wear experience criteria. An essential section of the usability survey was the evaluation of mask wear issues determined by facial and head zones (Fig. 1 ). Four usability criteria referenced in the literature were selected to test in these zones. In addition, two open-ended questions were designed at the end of the survey to reveal details of participants’ mask wear experience. Written responses were optional and prompted reflections on mask design complications and suggestions for improvement. These survey items were designed to integrate multiple methods of data collection to aid in uncovering why usability concerns were occurring, and where, in order to evaluate specific mask design components in the body-product relationship. The activity survey and the remaining sections of the usability survey will be discussed in a future publication. Table 5 provides an overview of the activity and usability survey items and their reference.
Fig. 1.
Facial and head zones used to guide the usability evaluation.
Table 5.
Overview of survey design and items.
| Surveys (Qualtrics link) | Measures | Reference | |
|---|---|---|---|
| Activity Survey | Breathing comfort: Normal breathing; Deep breathing; Moderate activity (walking); Intense activity (high knees) | 1, very uncomfortable; 5, very comfortable |
Locatelli et al. (2014),OSHA (2004) |
| Stability: Open/close mouth; Head side to side; Bend forward; Head up and down | 1, very poor; 5, excellent |
OSHA (2004) Suen et al. (2020) |
|
| Usability Survey | Subjective discomfort: In-mask heat; In-mask humidity; In-mask odor; Dizziness; Headache; Pressure on nose | 1, severe; 5, none |
Li et al. (2005) Locatelli et al. (2014),Loibner et al. (2019) Suen et al. (2020) Viscusi et al. (2011) |
| Wear efficiency: Donning; Doffing | 1, very difficult; 5, very easy |
Pompeii et al. (2020) Viscusi et al. (2011) |
|
| Speech intelligibility: Subjective comparison to previous masks | 1, very poor; 5, excellent | Suen et al. (2020) | |
| Localized evaluation with zones: Instability (shifting); Fit; Seal confidence; Comfort |
Instability: 1, always; 5, never Fit: 1, very loose; 5, very tight Seal confidence: 1, not confident at all; 5, completely confident Comfort: 1, very uncomfortable; 5, very comfortable |
Lee et al. (2018) Locatelli et al. (2014) Suen et al. (2020) |
|
| Overall: Fit; Comfort; Ease of use; Satisfaction | 5-star rating |
Lee et al. (2018) Suen et al. (2020) Viscusi et al. (2011) |
|
| Qualitative feedback: 1. Did you experience any irritation while wearing this mask? If yes, please describe. 2. When evaluating the mask design, is there anything you would suggest that needs improvement? For example, consider the following components: nose wire, elastic straps, plastic toggle adjusters, foam, etc. |
Open-ended |
Baig et al. (2010) Viscusi et al. (2011) |
|
Prior to the start of the first mask wear trial, participants completed the demographics pre-survey after indicating informed consent. Next, participants received instructions for choosing the best-fitting mask (S or M/L for MNmasks) according to past experience fitting N95 FFRs. A video followed, demonstrating the proper donning and doffing method and the procedure to achieve a secure fit using a positive pressure user seal check. After all masks were secured over the nose and mouth, the researchers confirmed understanding of the wear trial procedures, and then signed off from the video call. Remotely, participants continued to wear masks for the next 2 h (the duration of the class). At a halfway point as determined by the instructor, participants completed the activity survey. At the end of class, participants completed the final usability survey. To conclude the wear trial, participants doffed the tested mask and exchanged for their personal mask. While this may have introduced influence bias, participants would inevitably compare the test masks to their personal mask; however, this is irrelevant, as the objective of the study was to compare and contrast the three test masks. This procedure repeated for the subsequent two masks in the following class meeting times (Fig. 2 ).
Fig. 2.
Flowchart of randomized mask wear trial procedure.
4.5. Data analysis
Descriptive statistics were used to describe the demographics and background characteristics of the participants. Survey responses were also analyzed using descriptive statistics to report mean and standard deviation on a 5-point Likert scale. The differences between mask usability were analyzed using one-way ANOVA with Tukey's multiple comparison test for post-hoc analysis at 95% confidence level. A statistical significance was accepted at p < .05. All statistical analyses of mean, standard deviation, and significance were performed using Qualtrics reports and SPSS Statistics version 26 (IBM Corp, Armonk, NY, USA). Qualitative feedback of the two open-ended survey questions were examined using thematic analysis to identify regular patterns of meaning. Following Braun and Clarke's (2006) six-phase approach, the process of thematic analysis included: 1) careful reading and re-reading of all participant responses, 2) inserting initial codes of highlighted statements, 3) collapsing initial codes into emerging themes, 4) reviewing potential themes to confirm representation of the entire dataset, 5) assigning names to final themes, and 6) producing a report of final themes and supporting statements. While only one author independently coded responses, two other authors read and re-read participant responses to ensure final themes aligned with their own analysis. To ensure unified analysis across mixed methods, all data were analyzed in the context of usability according to the defined facial and head zones (Fig. 1).
5. Results
5.1. Participant background and demographics
Thirty-eight dental students participated in this study. Ten participants were removed from the sample for incomplete return of surveys, such as missing responses or incorrect selection of the mask to be tested for a particular wear trial. The sample for data analysis consisted of 28 female dental hygiene and dental assisting students with ages ranging 18–34 years and self-reporting as White (92.9%), Hispanic (3.6%), and Other (3.6%). The students had varied experience wearing respiratory PPE in the clinical setting. The average experience wearing a surgical mask was 6–12 months, while the average experience wearing an N95 FFR was 0–6 months. For a typical day in the clinic, participants estimated the average length of time an N95 FFR is worn without removal was 2–4 h.
5.2. Subjective evaluation of usability criteria by facial and head zones
Frequency of mask instability. If the mask fit is not stable, gaps in the mask seal may occur and compromise user safety. Participants differentiated the instability of the three masks by examining whether or not the mask felt stable or unstable across the zones of the face and head, using the five-point scale. Overall zones revealed significantly higher stability for MNmasks (p < .001, Table 6 ). Meanwhile, the KN95 had consistently lower scores in stability, as participants perceived the mask to shift throughout all zones of the face and head. The KN95 mask scored an overall mean frequency of 2.14. MNmask v1 was rated with a more stable fit than MNmask v2 in all areas, apart from the band around the head. Here, MNmask v2's paracord band was perceived to be more stable than MNmask v1's rubber band, as evidenced by a mean of 3.21 compared to 2.86. However, MNmask v2's adjustable cord lock was found to be less stable than the paracord band.
Table 6.
Frequency of mask instability.
| How often did the mask shift and require re-adjusting in the facial and head areas designated? (1: Always; 2: Often; 3: Sometimes; 4: Rarely; 5: Never) | ||||
|---|---|---|---|---|
| MNmask v1 |
MNmask v2 |
KN95 |
F | |
| Mean (S.D.) | Mean (S.D.) | Mean (S.D.) | ||
| Nose bridge | 3.21 (1.18) A | 2.61 (1.32) AB | 2.18 (1.26) B | 4.671* |
| Cheekbones | 2.89 (1.32) A | 2.25 (1.18) AB | 1.79 (1.01) B | 6.010** |
| Breathing zone | 2.86 (1.30) A | 2.21 (1.15) AB | 1.71 (0.84) B | 7.168** |
| Under chin | 2.79 (1.45) | 2.68 (1.26) | 2.25 (1.27) | 1.231 |
| Outer cheeks | 2.61 (1.26) A | 2.25 (1.24) AB | 1.68 (0.85) B | 4.606* |
| Band around head | 2.86 (1.36) | 3.21 (1.26) | – | – |
| Band around neck | 2.82 (1.49) | 2.07 (1.22) | – | – |
| Cord lock around head | – | 2.86 (1.30) | – | – |
| Cord lock around neck | – | 2.00 (1.16) | – | – |
| Ear loops | – | – | 1.57 (0.78) | – |
| Overall | 3.39 (1.01) A | 3.07 (1.10) A | 2.14 (0.87) B | 11.381*** |
*p<.05, **p<.01, ***p<.001.
Alphabet is the result of post hoc tests (A > B).
Degree of mask fit. The perceived fit of the three masks were examined across the face zones in terms of being very loose (1), somewhat loose (2), satisfactory fit (3), somewhat tight (4), and very tight (5). Overall, MNmask v1 had a significantly tight fit (M = 4.43, p < .001), while the KN95 mask had the loosest fit (M = 2.71, Table 7 ). The fit of MNmask v1's rubber band around the head and neck was perceived to be a contributing factor of tightness, and all zones associated in the tension of the straps followed closely in high scores of tight fit, apart from the breathing zone. Meanwhile, the KN95's lower mean scores of fit at the nose bridge (M = 2.50) and under chin (M = 2.57) reveal complications with the mask's sizing and shape in those hard-to-fit areas of the face. For MNmask v2, the fit was rated at or above satisfactory in all but the nose bridge area where the fit was rated below satisfactory (M = 2.86). The tightest zone of fit was under the chin (M = 3.64), where there was a paracord band.
Table 7.
Degree of mask fit.
| Please evaluate your experience of fit according to the designated facial and head areas. (1: Very loose; 2: Somewhat loose; 3: Satisfactory fit; 4: Somewhat tight; 5: Very tight) | ||||
|---|---|---|---|---|
| MNmask v1 |
MNmask v2 |
KN95 |
F | |
| Mean (S.D.) | Mean (S.D.) | Mean (S.D.) | ||
| Nose bridge | 4.39 (0.82) A | 2.86 (1.16) B | 2.50 (1.02) B | 26.955*** |
| Cheekbones | 4.36 (0.72) A | 3.32 (1.07) B | 2.64 (0.81) C | 26.020*** |
| Breathing zone | 3.54 (1.09) A | 3.04 (0.94) AB | 2.75 (0.78) B | 4.771* |
| Under chin | 4.25 (0.99) A | 3.64 (1.04) A | 2.57 (0.86) B | 20.861*** |
| Outer cheeks | 4.39 (0.72) A | 3.36 (0.93) B | 2.82 (0.76) C | 26.214*** |
| Band around head | 4.43 (0.68) | 3.43 (0.90) | – | – |
| Band around neck | 4.43 (0.56) | 3.29 (0.65) | – | – |
| Cord lock around head | – | 3.21 (0.90) | – | – |
| Cord lock around neck | – | 3.18 (0.76) | – | – |
| Ear loops | – | – | 3.04 (0.73) | – |
| Overall | 4.43 (0.62) A | 3.50 (0.68) B | 2.71 (0.75) C | 42.206*** |
*p<.05, **p<.01, ***p<.001.
Alphabet is the result of post hoc tests (A > B > C).
Level of confidence in mask seal. The wearer's confidence in the mask seal was examined to understand how well they thought the mask was protecting them and to connect the wearer's perception of mask fit with their confidence in the seal. Although there were no significant differences between the masks, the mean values reveal considerations for design improvement. MNmask v1 was perceived to have the tightest fit, and was also rated with the highest confidence in mask seal (M = 3.46, Table 8 ). This was followed by MNmask v2 (M = 3.32), and the KN95 (M = 3.07.) Out of all of the zones, users rated the seal at the nose bridge the worst for all three masks. MNmask v2's system of nose wire and adjustable band running across the nose bridge was rated with lower seal confidence than the performance of a single nose wire in MNmask v1 and the KN95. Conversely, the seal at the outer cheeks for all masks had consistently higher confidence scores.
Table 8.
Level of confidence in mask seal.
| What is your level of confidence in the seal of the mask to avoid leakage according to the facial areas designated? (1: Not confident at all; 2: Slightly confident; 3: Somewhat confident; 4: Fairly confident; 5: Completely confident) | ||||
|---|---|---|---|---|
| MNmask v1 |
MNmask v2 |
KN95 |
F | |
| Mean (S.D.) | Mean (S.D.) | Mean (S.D.) | ||
| Nose bridge | 3.14 (1.22) | 2.68 (1.28) | 3.07 (1.25) | 1.079 |
| Cheekbones | 3.79 (0.94) | 3.21 (1.24) | 3.36 (1.23) | 1.826 |
| Breathing zone | 3.64 (0.97) | 3.29 (0.96) | 3.43 (1.27) | 0.756 |
| Under chin | 3.71 (0.96) | 3.50 (0.98) | 3.32 (1.39) | 0.821 |
| Outer cheeks | 3.96 (0.87) | 3.57 (1.12) | 3.50 (1.24) | 1.434 |
| Overall | 3.46 (0.98) | 3.32 (0.97) | 3.07 (1.31) | 0.889 |
Perception of mask comfort. The comfort of the three masks was evaluated by participants in terms of the facial and head zones, as well as overall comfort. The KN95 mask overall had significantly higher comfort than MNmasks (M = 3.89, p < .001), while users found MNmask v1 to be the least comfortable mask (M = 2.61, Table 9 ). These findings are consistent with the perception of the KN95 having the loosest fit and MNmask v1 having the tightest fit, as one expects a correlation between discomfort and the tight fit of the mask required to achieve a secure face seal. Zones that were perceived to have the least amount of comfort include the band around the head for MNmask v1 (rubber band) and MNmask v2 (adjustable paracord), and the under chin area for MNmask v2 and the KN95.
Table 9.
Perception of mask comfort.
| Please evaluate your experience of comfort according to the designated facial and head areas. (1: Very uncomfortable; 2: Uncomfortable; 3: Neutral; 4: Comfortable; 5: Very comfortable) | ||||
|---|---|---|---|---|
| MNmask v1 |
MNmask v2 |
KN95 |
F | |
| Mean (S.D.) | Mean (S.D.) | Mean (S.D.) | ||
| Nose bridge | 2.57 (1.37) B | 3.00 (1.00) AB | 3.86 (0.99) A | 8.976*** |
| Cheekbones | 2.68 (1.36) B | 2.93 (0.80) B | 4.04 (0.87) A | 13.012*** |
| Breathing zone | 2.86 (1.33) B | 3.18 (0.85) B | 4.00 (0.85) A | 8.799*** |
| Under chin | 2.75 (1.43) B | 2.64 (0.89) B | 3.64 (1.17) A | 5.789** |
| Outer cheeks | 2.71 (1.33) B | 2.86 (1.03) B | 3.93 (0.92) A | 9.699*** |
| Band around head | 2.25 (1.35) | 2.68 (0.93) | – | – |
| Band around neck | 2.39 (1.35) | 3.04 (0.82) | – | – |
| Cord lock around head | – | 2.64 (0.85) | – | – |
| Cord lock around neck | – | 3.04 (0.82) | – | – |
| Ear loops | – | – | 3.89 (1.01) | – |
| Overall | 2.61 (1.29) B | 2.71 (0.70) B | 3.89 (0.94) A | 13.568*** |
*p<.05, **p<.01, ***p<.001.
Alphabet is the result of post hoc tests (A > B > C).
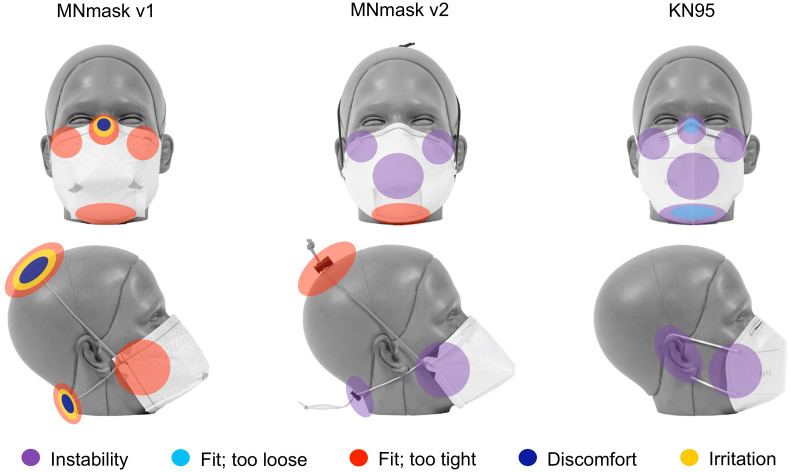
Overall mask usability results. The overall mask usability results were examined holistically by combining the significant negative scores from quantitative feedback and the recurring themes of mask wear issues from qualitative feedback. These results are summarized in Fig. 3 to highlight the most prominent mask usability concerns overall. For each mask, major usability concerns were color-coded in the corresponding facial and head zone according to instability, fit, discomfort, and irritation. Overall evaluation revealed the fit of MNmask v1 was significantly tight with discomfort and irritation most associated with the nose/nose wire and the head and neck/bands. MNmask v2 had overall concerns of instability at the cheekbones, cheeks, and neck, and a tight fit at the head and under chin due to the adjustable paracord band system. The KN95 mask had overall usability concerns of instability throughout all zones of the mask, which is related to the loose fit of the mask and its components at the nose and under chin.
Fig. 3.
Summary of the most prominent mask usability concerns according to quantitative and qualitative survey results.
5.3. Participants’ qualitative feedback
The feedback from the two open-ended questions regarding mask irritation and suggestions for mask design improvement were assigned to facial/head zone and component, and then summarized into themes and supporting statements. These findings complement the metrics of the subjective evaluation to reveal a richer understanding of mask usability. As evidence for considerations in the future design of protective masks, the main themes and supporting statements are listed in Table 10 .
Table 10.
Holistic approach to evaluating usability to inform future protective mask design.
| Zone/Component | Qualitative Feedback (Themes and Supporting Statements) | Future Design Considerations | |
|---|---|---|---|
| Nose/Nose wire | -Irritation -Pressure -Tight -Sore -Difficulty breathing -Poor malleability |
“Redness on bridge of nose …” “Very tight around nose. Nose still sore after doffing the mask.” “The nose band mostly closed off my nose forcing me to breathe out of my mouth.” “… could never get the wire to fit my nose correctly.” “… would not seal around my nose …” |
Nose wires should be tested to relieve pressure and conform to the nose comfortably and securely. Material property considerations: strength, malleability, thickness |
| Head & Neck/Bands | -Discomfort -Irritation -Tight -Stuck in hair -Slipping on hair |
“The elastic was very irritating.” “The rubber bands are very uncomfortable and get wrapped in hair.” “The plastic toggle adjusts and straps were very very uncomfortable.” “… upper cord to stay more on the top of the head.” |
Bands should be tested to relieve pressure on the head and neck. Bands must not interfere with hair in donning and doffing. Material property considerations: tension, slippage, thickness, elasticity, contour to head, relationship to hair types |
| Ears/Ear loops | -Sore -Loose |
“… made my ears hurt.” “… tighter ear loops or adjustable ear loops.” |
Ear loops should be tested to reduce pulling and rubbing behind the ears. However, ear loops do not guarantee a secure mask seal. Material property considerations: adjustability, elasticity, material softness |
| Chin/Foam | -Itchy -Tight -Irritation -Difficulty breathing |
“… tight on my chin.” “Itchy and irritating under the chin.” “It really hurt under my chin/neck. Felt like it was digging into my airway.” |
Chin foam should be tested to fit comfortably under the chin and secure the mask seal without breathing interference. Material property considerations: moisture-wicking, position, material softness |
| Cheeks & Cheekbones/Foam | -Irritation -Sticky/sweat |
“… rash around cheeks.” “The foam strips after a period of time stick to the face and become irritating.” “… the foam, it starts to get sweaty.” |
Cheek foam should be tested to aid in mask seal, cushion pressure impact, and limit effects of heat and moisture retention. Material property considerations: moisture-wicking, shape retention, temperature regulating, material softness |
| Face/Filter media | -Irritation -Itchy -Difficulty breathing |
“Itchy on face and irritated after.” “… very hard to breathe in. The mask collapsed on itself when I breathed in and expanded when I breathed out.” |
Filter media should be tested for standard filtration efficiency, breathing resistance, and biocompatibility, while considering ways to prevent fiber abrasion. Material property considerations: skin-friendly, material softness and texture, breathability, fiber breakdown |
| Overall mask design | -Unpleasant appearance -Poor fit -Side effects -Tight -Hot |
“The mask is very big and bulky and I do not like that feeling or look.” “It's comfortable … just too big for my face. Felt like it was always hitting my eyes …” “Make a bigger size, m/L was still pretty tight on most people and gave me a bad headache.” “… very uncomfortable and tight and hot.” |
All interrelated components of mask design should be considered in their effect on fit, discomfort, and mask wear experience. Design considerations: aesthetics, unobtrusive shape, size selection, secure and comfortable fit, temperature regulating |
While participants overall preferred the KN95 mask to MNmask v1 and MNmask v2, the areas where the KN95 mask scored lower were supported by comments noting the mask's large size and loose components – “Felt like it was always hitting my eyes, [and] could never get the wire to fit my nose correctly.” To improve the KN95 design, there was a desire to have adjustability of the ear loops and greater malleability of the nose wire to conform to the face. In addition to fit concerns, participants noted the ear loops of the KN95 caused pressure behind the ears after 2 h of wear – “… made my ears hurt.”
Qualitative feedback of MNmask v1 and MNmask v2 expanded on the lower ratings in comfort to reveal usability issues with components such as the bands, foam, and nose wire. For MNmask v1, there were concerns with the rubber band, which was difficult to don and doff with long hair and was perceived as tight – “The elastic was very irritating.” Despite the design intention of the foam to provide comfort, participants commented on sensations of humidity and irritation – “The foam strips after a period of time stick to the face and become irritating.” Further, comments about the plastic nose wire in MNmask v1 suggest it is too rigid. This caused nose soreness, difficulty breathing, and a poor seal around the bridge of the nose. At the time MNmask v1 was developed, supply chains were disrupted. Consequently, some of the sourced components were unrefined, which prompted the development of MNmask v2 to address these problems after material shortages began to recover. New components introduced new problems, but to a lesser frequency.
The primary usability concern of MNmask v2 were the paracord bands. While participants were able to adjust the bands to customize fit, the cylindrical shape of the cord caused slippage on the top of the head and the plastic cord locks were a source of discomfort – “The plastic toggle adjusts and straps were very very uncomfortable.” Participants also experienced irritation with the cord's design to cinch under the chin to prevent breaks in seal during movement – “It really hurt under my chin/neck. Felt like it was digging into my airway.” These issues reflect the lower scores in mask instability and comfort where the bands and their affiliated zones are concerned. The change to an aluminum nose wire for MNmask v2 (see Table 3) improved comfort by allowing the wire to more smoothly conform to the nose bridge. Pressure and soreness were noted less frequently, with MNmask v2 scoring the best mean fit at the nose out of all three masks.
6. Discussion
The critical shortages of masks throughout the COVID-19 pandemic heightened usability concerns of the N95 FFR through extreme cases of repeated use and prolonged wear. To explore a holistic approach for mask design improvement, this study evaluated the usability of emergency-use protective face masks by facial and head zone, component, and overall design. This study corroborates previous N95 FFR usability studies to report unfavorable characteristics of mask designs; however, the applied methods in usability evaluation discussed here provide a model for moving toward mask design improvement. The sections that follow discuss recent mask usability concerns occurring throughout the pandemic, and relates these to the associated zone of the face and head, and mask design component. Each section concludes with considerations in improving the design and testing of protective mask design.
Nose wire and nose discomfort. N95 FFRs place a considerable amount of pressure on certain areas of the face to maintain a tight seal. In this study, the nose bridge was a recurring zone where discomfort was experienced. With the exception of the loose fit of the KN95, MNmasks v1 and v2 were rated as tight-fitting and sensations of nose soreness occurred from friction and shear forces of the mask against the skin. Participants found the nose wires were rigid, causing redness, bruising, and pinching. This finding corroborates Locatelli et al. (2014) and Kim et al. (2015), which found the nose wire in N95 FFRs pinched the nose, leading some HCW participants to experience difficulty breathing. Further, the nose bridge is a cartilaginous and bony prominence of the face, which is at risk for pressure-related injuries such as sores, scarring, or bruising due to combined factors of pressure, friction, and moisture (Darlenski and Tsankov, 2020). Throughout the pandemic, reports of nose bridge injuries proliferated as a result of prolonged pressure duration (Hu et al., 2020; Jiang et al., 2021). Future testing of nose wire components should consider ways to increase malleability to prevent pinching, and reduce shear and friction forces across the nose to relieve pressure.
Bands and head and neck discomfort. The bands of the mask, which act as tethering devices to secure a tight seal, may also negatively impact the overall face and areas of the head and neck. If the bands are secured tightly and masks are worn for a prolonged period, the straps may cause headaches and facial pain due to impeded lymphatic flow in the face (Szeinuk et al., 2000). MNmasks v1 and v2 were designed to replicate the material and performance quality of N95 elastic headbands; however, non-traditional components were used in light of the supply shortages. The survey and open-ended responses revealed participants found these straps were uncomfortable, unstable, and tight-fitting on the head and neck. In particular, the non-latex rubber band caused hair pulling and the cord locks of the paracord bands contributed to pressure. The ear loops of the KN95 also caused soreness despite the loose fit.
These findings confirm Ong et al. (2020), which found a correlation between the location of discomfort and the associated head bands of the N95 FFR. In a sample of 128 HCWs reporting N95-related headaches during COVID-19, pain, pressure, or compression was experienced at the sides of the head (94.5%), lower neck (41.4%), and above the ears (71.9%). While pandemic conditions may have worsened symptoms, our study agrees with Locatelli et al. (2014), which concluded there is a need to improve the material softness, stability, and elasticity of straps to improve comfort and tolerability.
Foam and chin and cheekbones discomfort. The chin and cheekbones are additional bony prominences of the face subject to friction and shear forces of tight-fitting masks. As reports of facial irritation and pressure injury at these affected areas have increased, a number of preventative measures such as the application of barrier creams and wound dressings have been proposed (Lansang et al., 2020; Pacis et al., 2020). However, there is conflicting evidence regarding whether these measures compromise the mask seal (Cuddigan et al., 2020). MNmasks v1 and v2 were designed with a full inner perimeter of closed cell foam to relieve pressure on the face, which was validated in fit testing to prevent breaks in the mask seal. Despite this, participants in the study continued to experience symptoms of pressure at the cheekbones and chin. Another concern that arose was the foam's retention of exhaled moisture. Unpleasant sensations of sweating, stickiness, and itching were expressed by participants. These findings suggest future design considerations should consider methods to cushion the mask-face contact area to improve seal and comfort, while prioritizing materials with moisture-wicking properties.
Filter material and skin discomfort. A final mask usability concern in this study was skin irritation of the face. In qualitative feedback, participants noted symptoms of rash, skin indentations, and itching, which have been widely reported with N95 FFRs (Lan et al., 2020; Yuan et al., 2021). The epidermis is a thin and delicate layer of skin, and in cases of prolonged wear, irritant contact dermatitis (ICD) is found to be the common cause of skin irritation due to factors of friction, pressure, and moisture (Yu et al., 2021). Less common is allergic contact dermatitis (ACD), however, sensitivities to mask materials may still occur (Hornbeck et al., 2020). N95 FFR filter media is composed of nonwoven polypropylene that is biocompatible and poses a low risk for ACD (Yu et al., 2021). The alternative filter media used in MNmasks v1 and v2 is similarly composed of composite thermoplastic polymers, and underwent the same performance and safety testing standards as N95 FFRs (Ou et al., 2020). Current evidence of skin irritation and potential sensitivity to mask materials from this study, as well as past N95 FFR studies, points to the need for future testing of respirator filter media. A closer inspection of the role of filter media in contributing to skin irritation through combinations of heat, moisture, friction, and fiber breakdown is needed. Considerations should include methods to relieve fiber abrasion, prevent filter media contact with the skin, and increased testing of skin sensitivity to material texture and fiber breakdown.
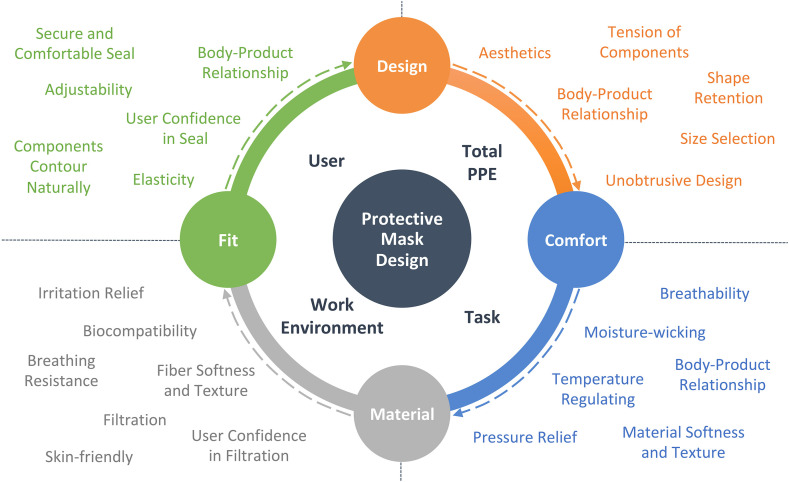
6.1. Application
The qualitative feedback from MNmask v1, MNmask v2, and the KN95 mask has been synthesized into a holistic approach to inform mask design improvement in Table 10. By leveraging usability research that focuses on the relationship of facial and head zone to mask component, an understanding of where and why mask usability problems occur may be better understood. Informed by human factors (Dul et al., 2012) and ecological systems theory (Bronfenbrenner, 1992), a holistic model of protective mask design brings this study's findings into application (Fig. 4 ). These resources may be beneficial to those involved in mask development by providing a framework to holistically evaluate mask usability.
Fig. 4.
Holistic model of protective mask design.
6.2. Limitations
Given the national PPE shortages and university restrictions, we were not able to compare NIOSH-approved N95 FFRs with the masks tested here. Other limitations include convenience sampling and a small sample size. The final sample of 28 dental students may not be representative of the total U.S. healthcare population according to demographics (including age), healthcare specializations, and experience wearing N95 FFRs. While the physical absence of a researcher during the study could be considered a limitation, the remote usability evaluation and method prevented the bias of influence by eliminating the presence of the researcher. In addition, it was not possible to collect participants’ fit factor scores due to remote testing, which may have provided further understanding of the usability of the masks with comparison to mask function. Despite these limitations, the outcome proved successful in overcoming the challenges of conducting this study remotely during the COVID-19 pandemic.
7. Conclusion and future research
The 2009 H1N1 influenza pandemic established a need for expanded N95 FFR design and research efforts (Baig et al., 2010; Radonovich et al., 2019; Suen et al., 2020). The COVID-19 pandemic has created unprecedented circumstances surrounding the usability of masks and a renewed effort to improve mask usability for HCWs. This study evaluated the usability of emergency-use protective face masks to explore a holistic approach in improving mask design development. While the findings can only discuss the masks evaluated here, the design considerations for mask components and the affiliated facial/head zone may be applied broadly to N95 FFRs.
The purpose of the holistic model for mask design and evaluation is to provide an applied method in evaluating usability from a human factors lens. The interrelationships of the user, their environment, and the mask requires components to be evaluated separately and holistically to advance PPE design and safety. While research and design has primarily concentrated on filtration media in the past, an equal attention to holistic mask design is necessary to move design innovation in favor of HCWs’ needs. The results from this method can be used to improve mask design, comfort, and performance to increase tolerability and compliance to respiratory PPE requirements.
Further research is ongoing to optimize the design of MNmasks as emergency-use protective face masks. In addition, studies are in progress to compare MNmask usability to N95 FFRs and other general use masks. Current research has been expanded to include fit testing and 3D face scanning to evaluate fit and filtration performance, as well as reaching wider populations of HCWs in testing. This will allow greater understanding of mask usability in examining the body-product relationship across various users while working toward mask design improvement.
Funding
This work was supported by the National Institutes of Health's National Center for Advancing Translational Sciences [grant UL1TR002494]; and the University of Minnesota Institute for Engineering and Medicine. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health's National Center for Advancing Translational Sciences.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank Cummins Inc. for their generous material donation and the Center for Filtration Research for their support in testing mask filter media. A special thanks also to Jessica Arnold for her support in the development of mask designs and the dental education instructors for facilitating study procedures in-person while the authors were remote.
References
- Baig A.S., Knapp C., Eagan A.E., Radonovich L.J. Health care workers' views about respirator use and features that should be included in the next generation of respirators. Am. J. Infect. Control. 2010;38(1):18–25. doi: 10.1016/j.ajic.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckman S., Materna B., Goldmacher S., Zipprich J., D'Alessandro M., Novak D., Harrison R. Evaluation of respiratory protection programs and practices in California hospitals during the 2009-2010 H1N1 influenza pandemic. Am. J. Infect. Control. 2013;41(11):1024–1031. doi: 10.1016/j.ajic.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Bronfenbrenner U. In: Six Theories of Child Development: Revised Formulations and Current Issues. Vasta R., editor. Jessica Kingsley Publishers; 1992. Ecological systems theory; pp. 187–249. [Google Scholar]
- Bryce E., Forrester L., Scharf S., Eshghpour M. What do healthcare workers think? A survey of facial protection equipment user preferences. J. Hosp. Infect. 2008;68(3):241–247. doi: 10.1016/j.jhin.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Chan J.K., Yep K.H., Magarey S., Keon-Cohen Z., Acheson M. Fit testing disposable P2/N95 respirators during COVID-19 in Victoria, Australia: fit check evaluation, failure rates, and a survey of healthcare workers. COVID. 2021;1(Issue 1):83–96. doi: 10.3390/covid1010007. [DOI] [Google Scholar]
- Corley A., Hammond N.E., Fraser J.F. The experiences of health care workers employed in an Australian intensive care unit during the H1N1 Influenza pandemic of 2009: a phenomenological study. Int. J. Nurs. Stud. 2010;47(5):577–585. doi: 10.1016/j.ijnurstu.2009.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuddigan J., Black J., Deppisch M., Pittman J., Sonenblum S., Tescher A. 2020. NPIAP Position Statements on Preventing Injury with N95 Masks. National Pressure Injury Advisory Panel.https://cdn.ymaws.com/npiap.com/resource/resmgr/position_statements/Mask_Position_Paper_FINAL_fo.pdf [Google Scholar]
- Darlenski R., Tsankov N. COVID-19 pandemic and the skin: what should dermatologists know? Clin. Dermatol. 2020;38(6):785–787. doi: 10.1016/J.CLINDERMATOL.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dul J., Bruder R., Buckle P., Carayon P., Falzon P., Marras W.S., Wilson J.R., van der Doelen B. A strategy for human factors/ergonomics: developing the discipline and profession. Ergonomics. 2012;55(4):377–395. doi: 10.1080/00140139.2012.661087. [DOI] [PubMed] [Google Scholar]
- Griffin L., Yu M., Cloet A., Arnold S., Carlson N., Hillmyer M., Ou Q., Pei C., Cao Q., Pui D., Franklin R., Durfee W. Protective masks utilizing nonendangered components. J. Med. Dev. Trans. ASME. 2022;16(1) doi: 10.1115/1.4053720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hignett S., Welsh R., Banerjee J. Human factors issues of working in personal protective equipment during the COVID-19 pandemic. Anaesthesia. 2021;76(1):134–135. doi: 10.1111/ANAE.15198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoernke K., Djellouli N., Andrews L., Lewis-Jackson S., Manby L., Martin S., Vanderslott S., Vindrola-Padros C. Frontline healthcare workers' experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal. BMJ Open. 2021;11(1) doi: 10.1136/bmjopen-2020-046199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornbeck, A., Cichowicz, J. K., Kilinc-Balci, S., Rottach, D., Pollard, J., & Boyles, H. L. (2020, August 14). Skin Irritation from Prolonged Use of Tight-Fitting Respirators. NIOSH Science Blog.https://blogs.cdc.gov/niosh-science-blog/2020/08/04/skin-irritation-respirators/.
- Hu K., Fan J., Li X., Gou X., Li X., Zhou X. The adverse skin reactions of health care workers using personal protective equipment for COVID-19. Medicine. 2020;99(24) doi: 10.1097/MD.0000000000020603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs K. 2021. March 1). How PPE for COVID-19 Impacts Patient Communication. RDH Magazine.https://www.rdhmag.com/infection-control/article/14189079/how-personal-protective-equipment-ppe-for-covid19-impacts-patient-communication [Google Scholar]
- Jiang Q., Liu Y., Song S., Wei W., Bai Y. Association between N95 respirator wearing and device-related pressure injury in the fight against COVID-19: a multicentre cross-sectional survey in China. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-041880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.H., Roberge R.J., Powell J.B., Shaffer R.E., Ylitalo C.M., Sebastian J.M. Pressure drop of filtering facepiece respirators: how low should we go? Int. J. Occup. Med. Environ. Health. 2015;28(1):71–80. doi: 10.13075/ijomeh.1896.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan J., Song Z., Miao X., Li H., Li Y., Dong L., Yang J., An X., Zhang Y., Yang L., Zhou N., Li J., Cao J.J., Wang J., Tao J. Skin damage among health care workers managing coronavirus disease-2019. J. Am. Acad. Dermatol. 2020;82(5):1215–1216. doi: 10.1016/J.JAAD.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansang P., Orrell K.A., Tran J., Chen T. Skin damage prevention strategies during COVID-19: assessing their effect on N95 mask seal integrity. J. Cutan. Med. Surg. 2020;24(6):646–647. doi: 10.1177/1203475420943861. [DOI] [PubMed] [Google Scholar]
- Law, T. (2020, March 22). Health Care Workers Around the World Are Sharing Bruised, Exhausted Selfies after Hard Days Treating COVID-19 Patients. Time.https://time.com/5807918/health-care-workers-selfies-coronavirus-covid-19/.
- Lee W., Yang X., Jung D., Park S., Kim H., You H. Ergonomic evaluation of pilot oxygen mask designs. Appl. Ergon. 2018;67:133–141. doi: 10.1016/j.apergo.2017.10.003. [DOI] [PubMed] [Google Scholar]
- Li Y., Tokura H., Guo Y.P., Wong A.S.W., Wong T., Chung J., Newton E. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int. Arch. Occup. Environ. Health. 2005;78:501–509. doi: 10.1007/s00420-004-0584-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locatelli S.M., LaVela S.L., Gosch M. Health care workers' reported discomfort while wearing filtering face-piece respirators. Workplace Health & Saf. 2014;62(9):362–368. doi: 10.3928/21650799-20140804-03. [DOI] [PubMed] [Google Scholar]
- Loibner M., Hagauer S., Schwantzer G., Berghold A., Zatloukal K. Limiting factors for wearing personal protective equipment (PPE) in a health care environment evaluated in a randomised study. PLoS One. 2019;14(1) doi: 10.1371/journal.pone.0210775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health NIOSH. (1996). NIOSH Guide to the Selection and Use of Particulate Respirators Certified under 42 CFR 84 (NIOSH Publication No. 96-101). Cincinnati, OH: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. https://www.cdc.gov/niosh/docs/96-101/.
- Occupational Safety and Health Administration . 2004. Fit Testing Procedures (Mandatory)https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134AppA 29 CFR 1910.134 App A. [Google Scholar]
- O'Kelly E., Arora A., Pirog S., Ward J., Clarkson P.J. Comparing the fit of N95, KN95, surgical, and cloth face masks and assessing the accuracy of fit checking. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0245688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong J.J.Y., Bharatendu C., Goh Y., Tang J.Z.Y., Sooi K.W.X., Tan Y.L., Tan B.Y.Q., Teoh H.L., Ong S.T., Allen D.M., Sharma V.K. Headaches associated with personal protective equipment – a cross-sectional study among frontline healthcare workers during COVID-19. Headache. 2020;60(5):864–877. doi: 10.1111/head.13811. [DOI] [PubMed] [Google Scholar]
- Or P.P.L., Chung J.W.Y., Wong T.K.S. A study of environmental factors affecting nurses' comfort and protection in wearing N95 respirators during bedside procedures. J. Clin. Nurs. 2018;27(7–8):e1477–e1484. doi: 10.1111/jocn.14268. [DOI] [PubMed] [Google Scholar]
- Ou Q., Pei C., Kim S.C., Abel E., Pui D.Y.H. Evaluation of decontamination methods for commercial and alternative respirator and mask materials – view from filtration aspect. J. Aerosol Sci. 2020;150 doi: 10.1016/j.jaerosci.2020.105609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacis M., Azor-Ocampo A., Burnett E., Tanasapphaisal C., Coleman B. Prophylactic dressings for maintaining skin integrity of healthcare workers when using N95 respirators while preventing contamination due to the novel coronavirus: a quality improvement project. J. Wound, Ostomy Cont. Nurs. 2020;47(6):551–557. doi: 10.1097/WON.0000000000000713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompeii L.A., Kraft C.S., Brownsword E.A., Lane M.A., Benavides E., Rios J., Radonovich L.J. Training and fit testing of health care personnel for reusable elastomeric half-mask respirators compared with disposable N95 respirators. JAMA. 2020;323(18):1849–1852. doi: 10.1001/jama.2020.4806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purushothaman P.K., Priyangha E., Vaidhyswaran R. Effects of prolonged use of facemask on healthcare workers in tertiary care hospital during COVID-19 pandemic. Indian J. Otolaryngol. Head Neck Surg. 2021;73(1):59–65. doi: 10.1007/S12070-020-02124-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radonovich L.J., Wizner K., LaVela S.L., Lee M.L., Findley K., Yorio P. A tolerability assessment of new respiratory protective devices developed for health care personnel: a randomized simulated clinical study. PLoS One. 2019;14(1) doi: 10.1371/journal.pone.0209559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahne T., Fröhlich L., Plontke S., Wagner L. Influence of surgical and N95 face masks on speech perception and listening effort in noise. PLoS One. 2021;16(7) doi: 10.1371/JOURNAL.PONE.0253874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruskin K.J., Ruskin A.C., Musselman B.T., Harvey J.R., Nesthus T.E., O'Connor M. COVID-19, personal protective equipment, and human performance. Anesthesiology. 2021;134(4):518–525. doi: 10.1097/ALN.0000000000003684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suen L.K.P., Guo Y.P., Ho S.S.K., Au-Yeung C.H., Lam S.C. Comparing mask fit and usability of traditional and nanofibre N95 filtering facepiece respirators before and after nursing procedures. J. Hosp. Infect. 2020;104(3):336–343. doi: 10.1016/j.jhin.2019.09.014. [DOI] [PubMed] [Google Scholar]
- Szeinuk J., Beckett W.S., Clark N., Hailoo W.L. Medical evaluation for respirator use. Am. J. Ind. Med. 2000;37:142–157. doi: 10.1002/(SICI)1097-0274(200001)37:1<142::AID-AJIM11>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- U.S. Food and Drug Administration FDA. (2020, October 15). FDA Reissues Emergency Use Authorization for Certain Non-NIOSH-approved Filtering Face-Piece Respirators Manufactured in China.https://www.fda.gov/news-events/press-announcements/fda-reissues-emergency-use-authorization-certain-non-niosh-approved-filtering-face-piece-respirators.
- Viscusi D.J., Bergman M.S., Novak D.A., Faulkner K.A., Palmiero A., Powell J., Shaffer R.E. Impact of three biological decontamination methods on filtering facepiece respirator fit, odor, comfort, and donning ease. J. Occup. Environ. Hyg. 2011;8(7):426–436. doi: 10.1080/15459624.2011.585927. [DOI] [PubMed] [Google Scholar]
- Williams, J., Cichowicz, J. K., Hornbeck, A., Pollard, J., & Snyder, J. (2021, October 14). The Physiological Burden of Prolonged PPE Use on Healthcare Workers during Long Shifts. NIOSH Science Blog. https://blogs.cdc.gov/niosh-science-blog/2020/06/10/ppe-burden/.
- Yu J., Chen J.K., Mowad C.M., Reeder M., Hylwa S., Chisolm S., Dunnick C.A., Goldminz A.M., Jacob S.E., Wu P.A., Zippin J., Atwater A.R. Occupational dermatitis to facial personal protective equipment in health care workers: a systematic review. J. Am. Acad. Dermatol. 2021;84(2):486–494. doi: 10.1016/J.JAAD.2020.09.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan N., Yang W.-X., Lu J.-L., Lv Z.-H. Investigation of adverse reactions in healthcare personnel working in Level 3 barrier protection PPE to treat COVID-19. Postgrad. Med. 2021;97(1148):351–354. doi: 10.1136/postgradmedj-2020-137854. [DOI] [PMC free article] [PubMed] [Google Scholar]