An adequate immune response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is crucial to not only clear the virus but also prevent tissue immunopathology. Because children generally experience a milder course of coronavirus disease 2019 (COVID-19) than adults, it is important to characterize the immune responses to SARS-CoV-2 in children. In an analysis of 91 children (3–11 years old) and 154 adults (20–71 years old), including 35 and 81 SARS-CoV-2 seropositive participants, respectively, Dowell et al. [1]. showed that COVID-19 convalescent children had more robust humoral immune responses to SARS-CoV-2 and endemic human coronaviruses (hCoVs) than convalescent adults. Notably, antibodies cross-reactive to beta-hCoVs were specific for the S2 domain of the spike protein, which is highly conserved among hCoVs, but not for the S1 domain; these cross-reactive antibodies contribute to the higher SARS-CoV-2-specific titer in children. This finding was emphasized by the lower titers of four hCoV-specific antibodies in seronegative children than in adults. Spike-specific T-cell responses were also higher in children, and even SARS-CoV-2-seronegative children showed prominent cellular immune responses to alpha- and beta-hCoVs. SARS-CoV-2-specific T-cell responses in children showed a differential cytokine response with markedly reduced production of IL-2, suggesting a more highly differentiated functional response in children than in adults. Indeed, at 6 months after primary infection, the majority of spike-specific CD8+ T cells in children had an IL-2−IFN-γ+TNF+ phenotype. Moreover, the stronger adaptive response in children was maintained for at least 6 months after COVID-19 and exhibited broad activity against numerous variants of concern.
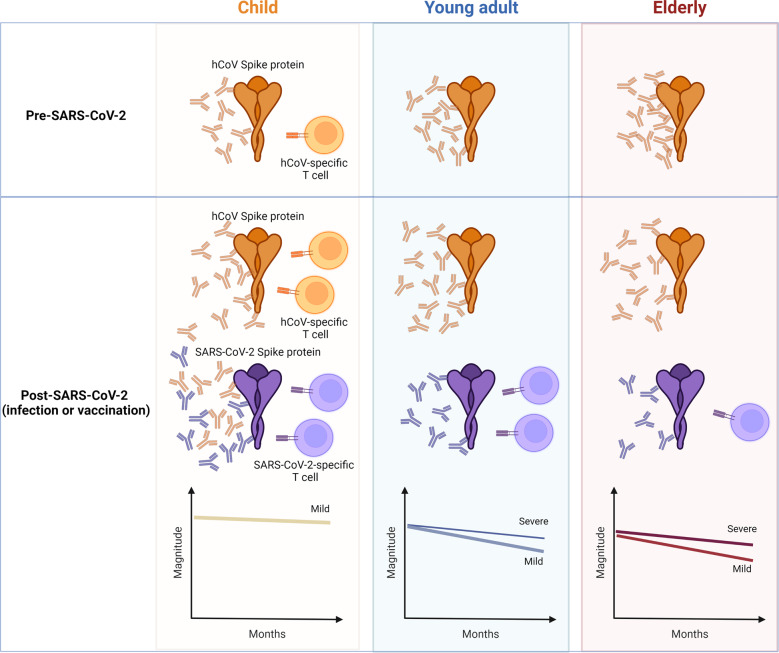
Although we have little data on humoral and cellular immune responses according to age in COVID-19 convalescent adults, there is evidence that the immune response and effectiveness of COVID-19 vaccination are lower in aged adults than in young adults [2]. The results reported by Dowell et al. complete the spectra of humoral and cellular immune responses to SARS-CoV-2 and hCoV in SARS-CoV-2 seronegative or seropositive children, young adults, and elderly people (Fig. 1). hCoV-specific antibody levels tend to be lower in SARS-CoV-2 seronegative children than in adults, whereas hCoV-specific SARS-CoV-2-cross-reactive T cells are abundant in children [1, 3]. In addition, compared to elderly people, young adults have a greater T-cell response to hCoV, and these T cells can cross-react with SARS-CoV-2. Moreover, after SARS-CoV-2 infection or vaccination, humoral and cellular immune responses to SARS-CoV-2 and hCoV are greater in children than in young adults or elderly people. Furthermore, these responses decline more rapidly in elderly people than in young adults or children [1, 2]. Severe COVID-19 is more frequent in elderly people than in young adults, and the magnitude of adaptive responses tends to be greater and more durable in those who have experienced severe COVID-19 [4, 5].
Fig. 1.
Model of adaptive immunity to SARS-CoV-2 according to age. Before SARS-CoV-2 infection, children have more robust and persistent hCoV spike-specific humoral and cellular immune responses that cross-react with SARS-CoV-2 than young adults and elderly people. After SARS-CoV-2 infection, the magnitude of the adaptive response to SARS-CoV-2 is greater and more durable in children than in young adults or elderly people. Image created using Biorender.com
The risk of SARS-CoV-2 reinfection is lower in children than in adults [6], which is in agreement with the robust and sustained humoral and cellular immune responses in convalescent children. However, these data raise questions about the optimal regimen for additional vaccination in COVID-19 convalescent children. In adults, COVID-19 vaccination is routinely recommended for those who have had COVID-19 because one dose of an mRNA vaccine elicits broad humoral and cellular immunity in COVID-19 convalescent adults [7]. Immune responses following an additional vaccination in children and the necessity for this additional intervention should be evaluated.
The relationship of the magnitude of immunity to SARS-CoV-2 with the severity of COVID-19 differs between children and adults. Adaptive responses are greater in COVID-19 convalescent adults who had severe illness than in those who had mild disease [4, 5]. In contrast, Dowell et al. reported that children had stronger immune responses than adults, although children tended to experience milder illness. Notably, it is inadequate to explain the clinical severity of COVID-19 by the magnitude of the SARS-CoV-2-specific immune response in convalescent samples without considering comorbidities or pre-existing or acute-phase immune responses. However, it is plausible that the high-level immune response in convalescent adults who had severe disease comprises bystander activation [8], whereas the response in convalescent children is mainly specific to SARS-CoV-2.
Several immunological theories could explain the differing severity of COVID-19 in children and adults. These hypotheses include reduced respiratory tract expression of angiotensin converting enzyme 2 receptor in children compared with adults [9], a potent and transient antiviral innate immune response, and low turnover rates of T cells and natural killer cells in children [10]. A greater abundance of hCoV-reactive SARS-CoV-2 cross-reactive CD4+ T cells in children has also been suggested [3]. In addition, prominent humoral and cellular immune responses in convalescent samples could be immunological features associated with milder illness in children.
In conclusion, Dowell et al. reported for the first time robust and sustained humoral and cellular immune responses with spike-specific cross-reactivity with hCoVs in COVID-19 convalescent children. The high-level immune response in convalescent children may be associated with the observed differences in clinical severity between children and adults. If so, these findings have important implications for future COVID-19 vaccination strategies for children.
Funding
This work was supported in part by the Creative-Pioneering Researchers Program through Seoul National University (to HRK); Samsung Research Funding and Incubation Center of Samsung Electronics (SRFC-TC2003-02); and the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (RF- 2021M3A9I2080496).
Competing interests
The authors declare no competing interests.
References
- 1.Dowell AC, Butler MS, Jinks E, Tut G, Lancaster T, Sylla P, et al. Children develop robust and sustained cross-reactive spike-specific immune responses to SARS-CoV-2 infection. Nat Immunol. 2022;23:40–9. doi: 10.1038/s41590-021-01089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collier DA, Ferreira I, Kotagiri P, Datir RP, Lim EY, Touizer E, et al. Age-related immune response heterogeneity to SARS-CoV-2 vaccine BNT162b2. Nature. 2021;596:417–22.. doi: 10.1038/s41586-021-03739-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loyal L, Braun J, Henze L, Kruse B, Dingeldey M, Reimer U, et al. Cross-reactive CD4(+) T cells enhance SARS-CoV-2 immune responses upon infection and vaccination. Science. 2021;374:eabh1823. doi: 10.1126/science.abh1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choe PG, Kim Y, Chang E, Kang CK, Kim NJ, Cho NH, et al. Kinetics of neutralizing antibody responses against SARS-CoV-2 Delta Variant in patients infected at the beginning of the pandemic. J Korean Med Sci. 2022;37:e67. doi: 10.3346/jkms.2022.37.e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kang CK, Kim M, Lee S, Kim G, Choe PG, Park WB, et al. Longitudinal analysis of human memory T-Cell response according to the severity of illness up to 8 months after severe acute respiratory syndrome coronavirus 2 infection. J Infect Dis. 2021;224:39–48. doi: 10.1093/infdis/jiab159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anna AM, Helen C, Stowe J, Seghezzo G, Simmons R, Lacy J, et al. Risk of SARS-CoV-2 reinfections in children: prospective national surveillance, January 2020 to July 2021, England. medRxiv. 2021. 10.1101/2021.12.10.21267372.
- 7.Goel RR, Apostolidis SA, Painter MM, Mathew D, Pattekar A, Kuthuru O, et al. Distinct antibody and memory B cell responses in SARS-CoV-2 naive and recovered individuals following mRNA vaccination. Sci Immunol. 2021;6:eabi6950. doi: 10.1126/sciimmunol.abi6950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuri-Cervantes L, Pampena MB, Meng W, Rosenfeld AM, Ittner CAG, Weisman AR, et al. Comprehensive mapping of immune perturbations associated with severe COVID-19. Sci Immunol. 2020;5:eabd7114. doi: 10.1126/sciimmunol.abd7114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Filippatos F, Tatsi EB, Michos A. Immune response to SARS-CoV-2 in children: a review of the current knowledge. Pediatr Investig. 2021;5:e12283. doi: 10.1002/ped4.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu W, Yang L, Li X, Sun M, Zhang A, Qi S, et al. Early immune responses and prognostic factors in children with COVID-19: a single-center retrospective analysis. BMC Pediatr. 2021;21:181. doi: 10.1186/s12887-021-02561-y. [DOI] [PMC free article] [PubMed] [Google Scholar]