Abstract
Purpose
This study aimed at investigating five dimensions of the psychological impact (post-traumatic stress symptoms (PTSS), anxiety, depression, sleep disturbance or profession-related burnout) of COVID-19 on healthcare workers (HCW) in China.
Methods
Studies that evaluated at least one of the five target dimensions of the psychological impact of COVID-19 on HCW in China were included. Studies with no data of our interest were excluded. Relevant Databases were searched from inception up to June 10, 2020. Preprint articles were also included. The methodological quality was assessed using the checklist recommended by AHRQ. Both the rate of prevalence and the severity of symptoms were pooled. The protocol was registered in PROSPERO (CRD42020197126) on July 09, 2020.
Results
We included 44 studies with a total of 65,706 HCW participants. Pooled prevalence rates of moderate to severe PTSS, anxiety, depression, and sleep disturbances were 27% (95% CI 16%-38%), 17% (13–21%), 15% (13–16%), and 15% (7–23%), respectively; while the prevalence of mild to severe level of PTSS, anxiety, and depression was estimated as 31% (25–37%), 37% (32–42%) and 39% (25–52%). Due to the lack of data, no analysis of profession-related burnout was pooled. Subgroup analyses indicated higher prevalence of moderate to severe psychological impact in frontline HCW, female HCW, nurses, and HCW in Wuhan.
Conclusion
About a third of HCW in China showed at least one dimension of psychological symptoms during the COVID-19 pandemic, whereas the prevalence of moderate and severe syndromes was relatively low. Studies on profession-related burnout, long-term impact, and the post-stress growth are still needed.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00127-022-02264-4.
Keywords: COVID-19, Psychological impact, Mental health, Stress, Chinese healthcare workers
Introduction
The coronavirus disease 2019 (COVID-19) outbreak has rapidly spread worldwide and posed a serious public health threat. However, when the outbreak was firstly noticed in November 2019 in Wuhan, the capital of Hubei province in China, no one ever knew about this disease and the public panicked. All of the sudden, healthcare workers (HCW) in China experienced a tremendous increase in both physical workload and psychological stress [1]. Learning lessons from several past viral epidemics, such as the severe acute respiratory syndrome (SARS) and the Ebola virus disease, frontline HCW had greater levels of both acute or post-traumatic stress and general psychological distress [2]. Therefore, the mental health of HCW should be examined in COVID-19.
Fortunately, the psychological impact of COVID-19 on HCW from China has already been noticed and assessed. Generally, an increased prevalence of mental illnesses, such as post-traumatic stress disorder (PTSD), depression, and anxiety disorders was indicated, but the prevalence rates varied greatly by different studies. Several systematic reviews and meta-analyses were also conducted. Among them, a review carried out by Pappa et al. showed that the prevalence of depression, anxiety, and insomnia was 23.2%, 22.8%, and 38.9%, respectively [3]. However, the review only covered studies published in the early stages of COVID-19. A more recent meta-analysis showed that the prevalence of anxiety and depression in HCW was similar to the general public yet lower than patients with pre-existing conditions and a COVID-19 infection [4]. Nevertheless, it did not account for the fact that the criteria for case definition varied between the studies, and the pooled results could not distinguish those with only mild or subclinical syndromes from those with more severe symptoms and in need of professional help. In addition, even though most studies included were conducted in China, no paper published in Chinese was included in these systematic reviews. Moreover, the severity of psychological impact as reflected by continuous variables were never included.
Therefore, a systematic review and meta-analysis encompassing the most recent studies both published in English and Chinese is needed to investigate the psychological impact of COVID-19 on HCW in China. Besides anxiety and depression, we took more dimensions into account, such as post-traumatic stress symptoms (PTSS), sleep disturbances and profession-related burnout. Additionally, this review examined the prevalence of psychological problems by varying degrees of severity. Subsequently, subgroup analyses were conducted for gender, occupational group, location (Wuhan vs. Hubei other than Wuhan vs. other provinces), and previous working experience (frontline HCW who were defined as caring for people with confirmed or suspected COVID-19 vs. non-frontline HCW).
Methods
The review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [5]. The review protocol was registered in the international prospective register of systematic reviews (PROSPERO) (CRD42020197126) on July 09, 2020.
Data sources
Relevant records that were published until June 10, 2020 were searched in the databases of Medline, PsycINFO, EMBASE, the Cochrane Library (including Cochrane Database of Systematic Reviews), and main Chinese databases including Sinomed, the China National Knowledge Infrastructure (CNKI), and WanFang data. Preprint articles published on Medrxiv and SSRN servers, as well as the Google Scholar, and the daily updated WHO COVID-19 database were also included. The search strategy for Medline was provided in the supplementary materials. The language was restricted to English, Chinese or German. Furthermore, the reference lists from reviewed articles were searched to identify and retrieve relevant articles.
Inclusion and exclusion criteria
We included studies that evaluated the psychological impact of COVID-19 on HCWs in China, which ought to include at least one of the following five target dimensions: PTSS, anxiety, depression, sleep disturbance or profession-related burnout. To be included into the meta-analysis, studies should use measurements that were proved to be valid to measure at least one of our target dimensions. Therefore, studies were excluded if they only measured general distress using tools of the General Health Questionnaire (GHQ-12) [6], or used non-validated self-designed questionnaire [7] or one single question of “what has been your mental attitude since COVID-19 outbreak” [8].
In order to ensure the study quality, we only included Chinese articles that were published in journals which are incorporated in the Chinese Science Citation Database (CSCD).
Both cross-sectional studies and interventional studies aligning with our criteria would be included, provided that, for the latter, the baseline level of psychological impact was extractable. Surveys investigating both HCW and other populations were included only if the data on HCW could be extracted separately.
Studies with neither data of our interest nor extractable data were excluded. When papers contained post-hoc analyses of an already included study, data was combined into one data set [9–12].
Study quality assessment
The methodological quality of the included studies was assessed using an 11-item checklist recommended by Agency for Healthcare Research and Quality (AHRQ) [13]. An item was scored ‘0’ if it was answered ‘NO’ or ‘UNCLEAR’; if it was answered ‘YES’, then the item scored ‘1’. Article quality was assessed as follows: low quality = 0–3; moderate quality = 4–7; high quality = 8–11.
Measurements
Primary outcomes include the prevalence of moderate to severe psychological impact, i.e. its five dimensions, PTSS, anxiety, depression, sleep disturbances, and profession-related burnout. The secondary outcomes include the prevalence of mild to severe psychological impact, and the severity of the psychological impact which were reflected through continuous variables.
The severities of each dimension were defined according to the validated cut-off values of each measure.
Data extraction
Data extraction was then independently carried out by three authors (NNX, YP and JL). To compute the prevalence rate, both the number of confirmed cases and the total amount of participants was extracted. For primary outcomes of the prevalence of moderate to severe cases, only participants who indicated symptoms above the cut-off for moderate symptoms were classified as burdened. Participants with no or mild symptoms were classified as not burdened. Continuous outcomes were analysed using the number of participants, the mean, and the standard deviation (STD). Missing STD values were calculated from reported confidence intervals (CI), standardized errors (SE), or p values. When none of the above data were reported, study authors were contacted via e-mail for further information.
As some studies report the prevalence rates of mild, moderate, severe symptoms plus the mean and STD of the same scales, these studies were included in the pooled analyses for both primary and secondary outcomes.
Data synthesis and statistical analysis
Statistical heterogeneity was tested using the I2 statistic and the natural approximate chi-square test [14]. I2 values above 50% indicated high heterogeneity. High heterogeneity was indicated by p values smaller than 0.10. The random effects model was used for heterogeneous data. The rate of prevalence was pooled by the inverse variance method. For continuous data, because of the variance in measurements across studies, the reported values were first transformed into the standardized values with a range from 0 to 100, according to the possible ranges of each questionnaire. Then the standardized values were pooled and compared between different subgroups. The likelihood of significant publication bias was assessed by both Begg’s test and Egger’s test. In addition, funnel plots were provided as a visual tool for publication bias. The Stata (15.1) [15] and the metan package [14] was used for statistical analyses.
Subgroup analyses
Subgroup analyses were planned a priori to investigate potential moderators influencing the psychological distress of HCW, and thereby, to assess the sources of high heterogeneity. Therefore, both primary and secondary outcomes were compared by frontline HCW (yes/ no), gender, occupation and work location. Subgroup analysis was performed when there were at least two comparisons included. Further meta-analysis was performed in different subgroups. Meta-regressions were not performed here due to the partially small number of studies.
Sensitivity analyses
Sensitivity analyses were conducted to test the reliability of primary outcomes, which were performed by excluding studies with low quality both individually and altogether.
Results
Characteristics of included studies
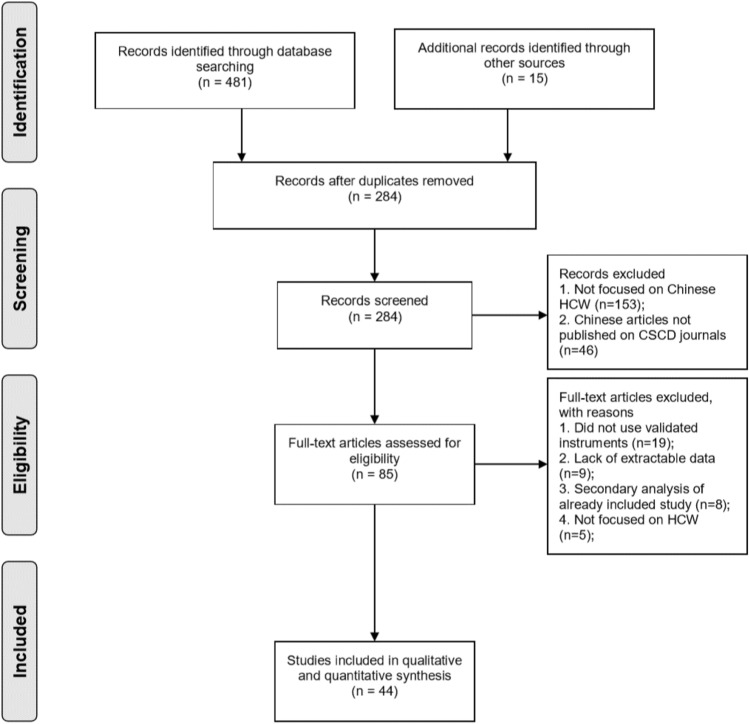
Overall, 85 full text articles were obtained and assessed for eligibility (Fig. 1). Of these, 44 studies met the inclusion criteria for the review, and were included in the meta-analysis [10, 11, 16–57].
Fig. 1.
PRISMA Flow diagram of the study selection process
44 studies with a total of 65,706 participants were included (see Table 1), with 76.7% being women. Apart from the studies that did not report the specific occupation of HCW, a total of 19,316 (33.0%) doctors, 35,644 (60.9%) nurses and 3552 (6.1%) technicians and administrative staff were investigated. As shown in Table 1, most studies were conducted from early to mid-February, at the height of the COVID-19 epidemic in China. Regarding the locations of the studies, 12 were conducted in Wuhan city, 3 in Hubei province, 16 in other provinces in China, and another 13 at multiple centres nationwide or in unknown areas. Twenty-four of the included studies were published in English, whereas the remaining 20 studies were published in Chinese. No articles in German were identified.
Table 1.
Overview of the characteristics of included studies (organized by regions)
| Author | Date (in 2020) | Sample size | Response rate (%) | HCW subgroup (%) | Female (%) | Age (SD) | Prevalence of psychological impact** (%) | Quality score (AHRQ) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Doctor | Nurse | Others | PTSS | Anxiety | Depression | Insomnia | |||||||
| Region: Wuhan city | |||||||||||||
| Du 2020 | 2.13–2.17 | 134 | 43.2 | 35.1 | 41.0 | 23.9 | 60.5 | 36.0 (8.1) | – | 20.1* | 12.7* | – | 5 |
| Jiang 2020 | 1.27–2.1 | 175 | UNK | – | 100 | – | 100 | 31.7 (5.9) | – | – | – | – | 5 |
| Li 2020a | 2.8–2.11 | 205 | UNK | – | 100 | – | 85.4 | UNK | 50.7 | – | – | – | 6 |
| Li 2020b | Jan–Feb | 66 | 100 | – | 100 | – | 77.3 | UNK | – | – | – | – | 5 |
| Li 2020c | UNK | 121 | 100 | – | 100 | – | 89.3 | 30.3 (5.4) | – | – | – | – | 5 |
| Li 2020d | 2.8–2.15 | 4369 | 88.2 | 13.3 | 77.4 | 9.3 | 100 | UNK | 31.6 | 25.2 | 14.2 | – | 6 |
| Li 2020e | 2.17–2.21 | 526 | UNK | – | 100 | – | 85.6 | 29.5 (5.0) | – | – | – | – | 3 |
| Mo 2020 | 2.21 | 180 | 85.7 | UNK | UNK | UNK | 90.0 | 32.7 (6.5) | – | – | – | – | 5 |
| Wang 2020 | UNK | 112 | UNK | UNK | UNK | UNK | 76.8 | 34.3 (6.1) | – | – | – | – | 2 |
| Xu 2020a | UNK | 41 | UNK | – | 100 | – | 90.2 | 31.3 (2.5) | – | – | – | – | 4 |
| Yuan 2020 | 2.7–2.20 | 309 | 85.6 | 43.7 | 48.5 | 7.8 | 76.4 | 34.0 (8.9) | – | – | – | – | 4 |
| Zhu 2020b | 2.8–2.10 | 5062 | 77.1 | 19.8 | 67.5 | 12.7 | 85.0 | UNK | 29.8 | 24.1 | 13.4 | – | 8 |
| Region: other cities in the Hubei province | |||||||||||||
| Qi 2020 | Feb | 1306 | UNK | UNK | UNK | UNK | 80.4 | 33.1 (8.4) | – | – | – | 71.7* | 7 |
| Xing 2020 | 1.22 | 40 | UNK | – | 100 | – | 95.0 | 31.4 (7.3) | – | – | – | – | 4 |
| Xu 2020b | 2.9 | 42 | 100 | – | 100 | – | 100 | UNK | – | 35.7 | – | – | 5 |
| Region: outside of the Hubei province | |||||||||||||
| Cai 2020 | 2.1–2.7 | 1521 | UNK | 33.6 | 35.9 | 11.9 | 75.5 | UNK | – | – | – | – | 3 |
| Cao 2020 | UNK | 37 | 100 | 43.2 | 56.8 | – | 78.4 | 32.8 (9.6) | – | – | 18.9 | – | 4 |
| Chen 2020 | UNK | 206 | 93.7 | 84.0 | 16.0 | 69.5 | 34.0(8.9) | – | 0.5 | – | – | 3 | |
| Deng 2020a | UNK | 60 | UNK | 30.0 | 70.0 | – | 86.7 | 32.2 (8.0) | – | – | – | – | 3 |
| Deng 2020b | Jan | 68 | 100 | UNK | UNK | UNK | 66.2 | UNK | – | – | – | – | 3 |
| Huang 2020a | 2.7–2.14 | 230 | 93.5 | 30.4 | 69.6 | – | 81.3 | 32.6 (6.2) | 27.4* | 7.0 | – | – | 6 |
| Liang 2020 | 2.3–2.21 | 59 | UNK | 39.0 | 61.0 | – | UNK | UNK | – | – | – | – | 2 |
| Liu 2020a | 2.1–2.18 | 1097 | 100 | – | 100 | – | 98.3 | 29.0 (5.9) | – | 3.5 | 9.7 | 2.8 | 3 |
| Luo 2020 | 2.10–2.20 | 171 | 91.9 | UNK | UNK | UNK | 76.0 | UNK | – | 15.2 | 17.5 | – | 6 |
| Pu 2020 | UNK | 867 | UNK | – | 100 | – | 95.6 | 30.8 (7.1) | 19.3 | – | – | – | 3 |
| Sheng 2020 | UNK | 92 | 96.8 | – | 100 | – | 93.5 | 21.3 (1.0) | – | – | – | 17.4* | 4 |
| Tian 2020 | 4.6–4.10 | 845 | 79.9 | 23.2 | 76.8 | – | 84.5 | 35.5 (6.7) | – | 20.7* | 45.6* | 27.0* | 4 |
| Wu 2020a | UNK | 106 | 94.6 | – | 100 | – | 80.2 | 30.8 (4.5) | – | 29.3 | – | 64.2* | 4 |
| Wu 2020b | UNK | 120 | UNK | UNK | UNK | UNK | 74.2 | 33.7 (12.2) | – | – | – | – | 3 |
| Yin 2020 | 2.3–2.5 | 1266 | UNK | UNK | UNK | UNK | 74.7 | 35.2 (7.8) | – | 11.7 | 10.2 | – | 8 |
| Zhu 2020a | 2.1–2.29 | 165 | 100 | 47.9 | 52.1 | – | 83.0 | 34.2 (8.1) | – | 20.0* | 44.2* | – | 6 |
| Region: multiple centers nationwide or unknown | |||||||||||||
| Guo 2020 | 2.18–2.20 | 11,118 | UNK | 30.3 | 53.1 | 16.6 | 74.8 | UNK | – | 5.0 | 13.5 | – | 3 |
| Huang 2020b | 2.3–2.17 | 2250 | UNK | UNK | UNK | UNK | UNK | UNK | – | 35.6 | 19.8 | 23.6 | 4 |
| Huangfu 2020 | UNK | 326 | 100 | – | 100 | – | 100 | 28.6 (12.2) | – | – | – | – | 3 |
| Lai 2020 | 1.29–2.3 | 1257 | 68.7 | 39.2 | 60.8 | – | 76.7 | UNK | 35.0 | 12.3 | 14.8 | 7.8 | 6 |
| Liu 2020b | 2.10–2.20 | 512 | 85.4 | UNK | UNK | UNK | 84.6 | UNK | – | 2.1 | – | – | 4 |
| Liu 2020c | 2.17–2.24 | 4679 | UNK | 39.6 | 60.4 | – | 82.3 | 35.9 (9.0) | – | 5.2 | 19.8 | – | 4 |
| Lv 2020 | UNK | 7071 | UNK | 52.2 | 47.8 | – | 71.2 | UNK | – | 35.6* | 37.0* | 35.2* | 3 |
| Song 2020 | 2.28–3.18 | 14,825 | UNK | 41.1 | 58.9 | – | 64.3 | 34.0 (8.2) | 7.3 | – | 15.2 | – | 3 |
| Sun 2020 | 1.31–2.4 | 442 | UNK | 12.0 | 78.7 | 9.3 | 83.3 | UNK | – | – | – | – | 5 |
| Xiao 2020a | Jan–Feb | 180 | 81.8 | 45.6 | 54.4 | – | 71.7 | 32.3 (4.9) | – | 36.7 | – | 31.7 | 4 |
| Xiao 2020b | 1.28 | 958 | UNK | 39.5 | 37.5 | 23.1 | 67.2 | UNK | – | 54.1* | 57.3* | – | 2 |
| Zhang 2020a | 2.19–3.6 | 927 | UNK | UNK | UNK | UNK | 73.1 | UNK | – | 13.0 | 12.2 | 10.5 | 3 |
| Zhang 2020b | 1.29–2.3 | 1563 | UNK | 29.0 | 63.0 | 8.0 | 82.7 | UNK | 37.4 | 12.9 | 17.2 | – | 5 |
AHRQ Agency for Healthcare Research and Quality, HCW healthcare workers, PTSS post-traumatic stress symptoms, UNK unknown
Prevalence of psychological impact**: the prevalence of moderate to severe level of burden was presented if available; if not, the prevalence of mild to severe level of burden was used with a mark of *. For all studies with no prevalence indicated, only the severity data was available and extracted
The total quality score is added up from all applicable items (potential range: 0–11). Item 1: source of information defined; Item 2: clear criteria for exposed and exposed subjects; Item 3: time period for identifying patients indicated; Item 4: whether or not subjects were consecutive if not population-based indicated; Item 5: whether subjective components of study were masked to other aspects of the status of the participants indicated; Item 6: quality assurance for assessments undertaken; Item 7: patient exclusions from analysis explained; Item 8: confounding assessment or/and control described; Item 9: missing data handling explained (if existent); Item 10: response rates and completeness of data collection indicated; Item 11: expected follow-up clarified (if any)
All selected articles were assessed for methodological quality. According to the criteria of AHRQ, only two studies were of high quality, 26 studies were of moderate quality, and 16 studies were of low quality (see Table 1 and detailed information in Supplementary Table 1).
All assessment tools and the according cut-off values employed to measure the psychological impact are listed in Table 2.
Table 2.
Overview of the measurements employed to assess the psychological impact of COVID-19 on HCW in China
| Measurements | Prevalence criteriaa | Studies | ||
|---|---|---|---|---|
| PTSS | At least Moderate | At least mild | ||
| Impact of Event Scale- Revised (IES-R) | ≥ 26 | ≥ 9 | Lai 2020; Li 2020b; Sun 2020a; Zhang 2020b; Zhu 2020b | |
| PTSD Checklist Civilian Version (PCL-C) | > 38 | NA | Li 2020a; Wu 2020b | |
| Post-Traumatic Stress Disorder Self-Rating Scale (PTSD-SS) | NA | 50 | Huang 2020b | |
| PTSD Checklist for DSM-5 (PCL-5) | > 38 | > 33 | Song 2020 | |
| Triage Assessment Form (TAF) | ≥ 13 | NA | Pu 2020 | |
| Stanford Acute Stress Reaction Questionnaire (SASRQ) | Severity only | Xiao 2020a | ||
| Vicarious Traumatization Questionnaire (VTQ) | Severity only | Li 2020e | ||
| Anxiety | ||||
| Zung Self-Rating Anxiety Scale (SAS) | ≥ 60 | ≥ 50 | Chen 2020a; Guo 2020; Huang 2020b; Liang 2020; Liu 2020a; Liu 2020d; Mo 2020; Pu 2020; Sheng 2020; Wu 2020a; Wu 2020b; Xiao 2020a; Xu 2020; Zhu 2020a | |
| Generalized Anxiety Disorder 7-item (GAD-7) | ≥ 10 | ≥ 5 | Huang 2020a; Lai 2020; Li 2020b; Li 2020d; Liu 2020c; Luo 2020b; Lv 2020; Tian 2020; Zhang 2020a; Zhang 2020b; Zhu 2020b | |
| Symptom Checklist 90; Anxiety subscale (SCL-90) | Severity only | Cai 2020b; Deng 2020b; Huangfu 2020; Jiang 2020; Wang 2020b; Xing 2020; Xu 2020 | ||
| Hamilton Anxiety Rating Scale (HAM-A) | ≥ 21 | ≥ 14 | Li 2020c | |
| Stress-related Questions associated with the H1N1 event; Anxiety subscale | Severity only | Deng 2020a | ||
| Beck Anxiety Inventory (BAI) | NA | ≥ 8 | Du 2020 | |
| Hospital Anxiety and Depression Scale; Anxiety subscale (HADS) | NA | ≥ 8 | Xiao 2020b | |
| Depression | ||||
| Patient Health Questionnaire 9-item (PHQ-9) | ≥ 10 | ≥ 5 | Cao 2020; Lai 2020; Li 2020b; Li 2020d; Liu 2020c; Luo 2020b; Lv 2020; Tian 2020; Zhang 2020a; Zhang 2020b; Zhu 2020b | |
| Symptom Checklist 90; Depression subscale (SCL-90) | Severity only | Cai 2020b; Deng 2020b; Huangfu 2020; Jiang 2020; Wang 2020b; Xing 2020; Xu 2020 | ||
| Zung Self-Rating Depression Scale (SDS) | ≥ 60 | ≥ 50 | Guo 2020; Liang 2020; Liu 2020d; Sheng 2020; Wu 2020a; Zhu 2020a | |
| Center for Epidemiology Studies Depression Scale (CES-D) | > 28 | Huang 2020a; Song 2020 | ||
| Beck Depression Inventory (BDI-II) | NA | ≥ 14 | Du 2020 | |
| Hospital Anxiety and Depression Scale; Depression subscale (HADS) | NA | ≥ 8 | Xiao 2020b | |
| Sleep disturbance | ||||
| Pittsburgh Sleep Quality Index (PSQI) | ≥ 11 | ≥ 6 | Huang 2020a; Li 2020d; Qi 2020; Sheng 2020; Wu 2020a; Wu 2020b; Xiao 2020 | |
| Insomnia Severity Index (ISI) | ≥ 15 | ≥ 8 | Lai 2020; Liu 2020c; Lv 2020; Tian 2020; Zhang 2020a; Zhang 2020b | |
| Athens Insomnia Scale (AIS) | NA | > 6 | Qi 2020 | |
| Profession-related burnoutb | ||||
| Maslach Burn-out Inventory (MBI) | NA | Cao 2020; Wu 2020c | ||
| Stress-related questions associated with the H1N1 event; Burnout subscale | Severity only | Deng 2020a | ||
PTSS post-traumatic stress symptoms, NA not applicable
aData extraction was conducted separately for the primary outcome (% prevalence for at least moderate symptoms), and for the secondary outcomes (% prevalence for at least mild symptoms; Severity of symptoms). Studies with pertinent information for at least one outcome were included in the meta-analysis. Studies which indicated data for both primary outcomes and secondary outcomes were both included in the respective pooled analyses
bProfession-related burnout was not pooled since the original papers did not report the prevalence rates, or the case definition used did not align with the common criteria
Primary outcome: prevalence of moderate to severe levels of psychological impact
PTSS
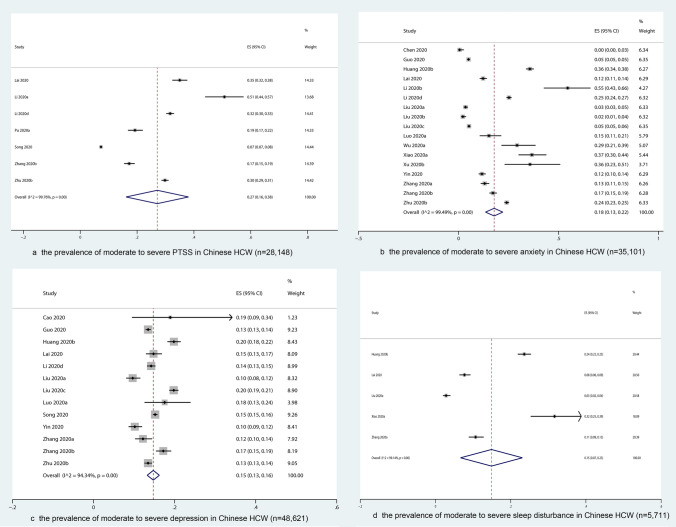
Seven studies with 28,148 participants measured the prevalence of moderate to severe PTSS (Fig. 2a). The overall prevalence was 27% (95% CI 16–38%) with substantial heterogeneity (I2 = 99.8%, p = 0.02).
Fig. 2.
The prevalence of moderate to severe psychological impact on the whole sample of Chinese HCW
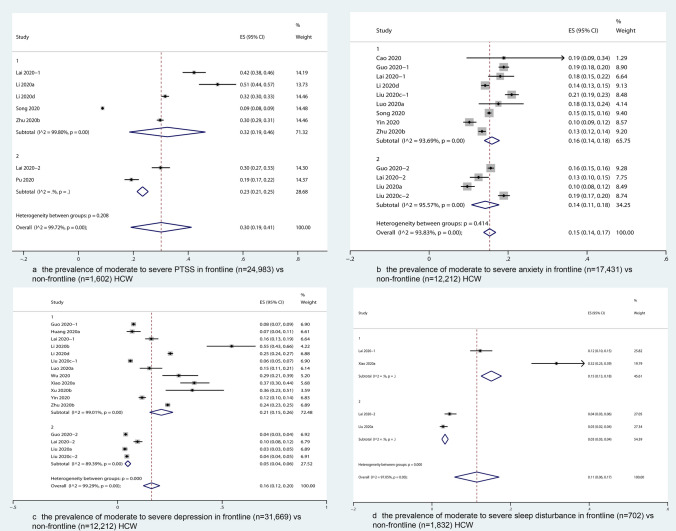
Among them, six studies (seven subgroups) reported the prevalence for frontline and non-frontline HCWs separately. Subgroup analysis showed that the prevalence of moderate to severe PTSS was higher in frontline [32% (95% CI 19–46%)] than non-frontline HCW [23% (95% CI 21–25%)] (Fig. 3a).
Fig. 3.
The prevalence of moderate to severe psychological impact on frontline vs. non-frontline HCW
Additional subgroup analyses showed that the prevalence of moderate to severe PTSS was significantly higher in female [33% (95% CI 31–35%)] than male HCW [22% (95% CI 20–25%)], was significantly higher in nurses [34% (95% CI 28–40%)] than technicians or others [22% (95% CI 20–25%)], and was significantly higher in HCW from Wuhan [36% (95% CI 32–41%)] than those from other provinces in China [21% (95% CI 18–23%)] (Supplementary Figs. 1–3).
The difference between gender, occupations and locations could partly account for the large heterogeneity (p < 0.01).
Anxiety
Resulting from 18 studies with 34,793 participants, the overall prevalence of moderate to severe anxiety was estimated as 17% (95% CI 13–21%) (Fig. 2b).
Subgroup analysis showed that the prevalence of moderate to severe anxiety was higher in frontline [21% (95% CI 15–26%)] than non-frontline participants [5% (95% CI 4–6%)] (Fig. 3b), and higher in HCW from Wuhan [25% (95% CI 20–30%)] than from other cities in the Hubei province [9% (95% CI 6–13%)], and other provinces in China [10% (95% CI 5–14%)], but was comparable in female and male participants, as well as in nurses, doctors, and technicians (Supplementary Figs. 4–6).
The difference between positions (frontline vs. non-frontline) and locations could partly account for the large heterogeneity within the whole sample (p < 0.01).
Depression
The prevalence of moderate to severe level of depression was estimated as 15% (95% CI 13–16%) (k = 13, n = 48,621) (Fig. 2c).
Subgroup analysis showed that the prevalence of moderate to severe depression was comparable between frontline and non-frontline HCW (Fig. 3c), and between female and male HCW. In contrast, the prevalence was significantly higher in nurses [17% (95% CI 14–21%)] than technicians or others [11% (95% CI 8–13%)], and significantly higher in HCW from Wuhan [14% (95% CI 13–16%)] than those from other provinces in China [11% (95% CI 9–13%)] (Supplementary Figs. 7–9).
Only the differences between locations could partly account for the heterogeneity (p = 0.04).
Sleep disturbance
The overall prevalence of moderate to severe sleep disturbance was estimated as 15% (95% CI 7–23%, k = 5, n = 5,711) with substantial heterogeneity (I2 = 99.1%, p = 0.01) (Fig. 2d). As indicated in Fig. 3d, sleep disturbance was significantly more severe among frontline [15% (95% CI 13–18%)] than non-frontline HCW [3% (95% CI 3–4%)]. Such subgroup difference could partly account for the heterogeneity (p < 0.01). Due to the lack of data, no subgroup analysis on gender, occupational group* and location was conducted.
Secondary outcomes: prevalence of mild to severe levels of psychological impact
The prevalence of mild to severe PTSS was not pooled due to the lack of data. The prevalence of mild to severe levels of anxiety, depression and sleep disturbances was estimated as 31% (95% CI 25–37%), 37% (95% CI 32–42%) and 39% (95% CI 25–52%), respectively (Supplementary Figs. 10–12).
Secondary outcomes: severity of psychological impact
Reflected by continuous data, the psychological impact was pooled and compared between different subgroups. Take the pooled ES of both frontline and non-frontline HCW for an example, on a standardized range between 0 and 100, all dimensions of psychological impact, including PTSS [SMD = 37.0 (95% CI 28.2–45.8)], anxiety (SMD = 43.7 (95% CI 39.6–47.8)], depression [SMD = 37.4 (95% CI 29.4–45.5)], and sleep disturbances [SMD = 36.2 (95% CI 25.1–47.3)] fall into a mild to moderate range.
Severity of psychological impact in frontline vs. non-frontline HCW
We found no significant differences between frontline and non-frontline HCW regarding the severity of PTSS, anxiety, and depression. However, sleep disturbance was more severe in frontline HCWs [SMD = 43.2 (95% CI 33.1–53.3) vs. 25.5 (95% CI 14.8–36.2)] (Supplementary Figs. 13–16).
Severity of psychological impact in female vs. male HCW
Based on the pooled ES, no significant differences were found between female and male HCW in terms of the severity of PTSS, anxiety, depression, as well as sleep disturbances (Supplementary Figs. 17–20).
Severity of psychological impact on HCWs with different occupations
Due to the lack of data, comparisons were only conducted between doctors and nurses. Our results indicate that the severity of PTSS, anxiety, depression, and sleep disturbance appear more severe in nurses, although no significant difference were given (Supplementary Figs. 21–24).
Psychological impact on HCWs from different locations
As the pooled ES showed, the severity of PTSS and sleep disturbance of HCW in Wuhan seemed to be higher than those from other provinces in China, but no significant difference was detected (Supplementary Figs. 25–26).
Interestingly, both levels of anxiety [SMD = 49.4 (95% CI 43.1–55.7)] and depression [SMD = 44.8 (95% CI 40.9–48.8)] were significantly higher in HCW from other cities in the Hubei province than in those from Wuhan [SMD = 32.8 (95% CI 24.0–41.5] and 28.2 (95% CI 20.2–36.2)] (Supplementary Figs. 27–28).
Sensitivity analyses
By excluding all studies with low methodological quality, the prevalence of moderate to severe PTSS, anxiety, depression, and sleep disturbance was slightly higher, which was estimated as 32% (95% CI 26–39%), 21% (95% CI 15–27%), 16% (95% CI 14–18%), and 21% (95% CI 8–34%). The heterogeneity within each outcome remained substantial, with the I2 lowered by 0–1.6%.
Publication bias
Results from Egger’s test showed potential publication bias concerning the prevalence of moderate to severe PTSS (p = 0.009), anxiety (p = 0.003), and depression (p < 0.001), but the Begg’s test did not reveal risk of publication bias in the prevalence of PTSS (p = 0.23). Neither test indicated potential risk in the prevalence of sleep disturbances (p = 0.254 and 0.221), or the severity of PTSS (p = 0.640 and 0.436), anxiety (p = 0.079 and 0.315), depression (p = 0.616 and 0.767) or sleep disturbances (p = 0.366 and 0.734) as reflected in continuous data. Funnel plots were provided in the Supplementary Figs. 29–36.
Discussion
This systematic review and meta-analysis focused on the psychological burden of HCW in China during the COVID-19 pandemic. Compared to other reviews [3, 4, 58–60], this review covers a longer period until June 2020 and has included good quality studies in Chinese language. Additionally, this study distinguished between differing severities of psychological problems and synthesized data measured with continuous scales.
Summary of the main findings
Forty-four studies with a total of 65,706 HCW were included. The period of studies spanned the end of January to early April 2020, at the height of the COVID-19 epidemic in China. Despite the great heterogeneity of the studies, there is strong evidence that about a third of the clinic staff showed at least one dimension of psychological symptoms. More pronounced symptoms like moderate and severe level of PTSS, anxiety, depression, and sleep disturbances, were found in 27%, 17%, 15%, and 15% of the participants examined, respectively.
Comparison with other reviews and studies in other countries
Compared with results of the latest China mental health survey [61], the psychological burden was significantly elevated. However, the increased values differed little from the values reported for the general population in China in the above-mentioned months [4, 62, 63].
Compared to studies from other countries: a multi-centered study in Singapore and India investigated frontline HCW. In this study, only 2.2% were screened positive for moderate to extremely-severe stress, 8.7% for anxiety, and 5.3% for depression. However, the prevalence of physical discomforts was as high as 33.4% [64]. It was speculated that somatic symptoms were used to represent emotions in this situation. A study conducted during an early peak of COVID-19 in New York City also found very high positive screens for psychological symptoms as follows: 57% for acute stress, 48% for depressive symptoms, and 33% for anxiety symptoms [65].
In addition, after the data of our meta-analysis were collected, similar studies were piled up and have provided further evidence in professional-related burnout and post-traumatic growth. For example, a study showed that the burnout thresholds in disengagement and exhaustion were met by 79.7% and 75.3% of respondents [66]. Another large-scale survey of frontline nurses in China reported that 13.3% of them experienced trauma, and 39.3% experienced post-traumatic growth [67]. In a tertiary hospital of a highly burdened area of north-east Italy, 38.3% HCW showed high emotional exhaustion and 46.5% showed low professional efficacy [68].
Relevance of key subgroups
Similar to our results considering the prevalence of psychological burden, previous evidence from China, Germany, and worldwide has shown that mental problems were more pronounced in female participants, nurses, and frontline health professionals, especially those in the departments for infectious diseases, fever clinics and intensive care units, which was in line with their exposure level and proximity to COVID-19 patients [3, 10, 58].
However, contrary to our expectations, the subgroup comparison results differed between the binary and the continuous outcomes, i.e. reflected by continuous data, basically all subgroups were comparable, and that HCW in the Hubei province even had higher levels of anxiety and depression than those in Wuhan city. One possible explanation was that since most HCW did not have severe symptoms, so that the effect sizes from higher percentages of confirmed cases were diluted. Such results also remind us to not neglect the mental health of “non-frontline” healthcare providers. In addition, during that period, it is possible that Wuhan got most of the assistance at the very beginning, and healthcare providers in other cities of the Hubei province, like Huanggang city, were suffering under more severe anxiety and depression [69].
Comparisons with other viral epidemics
Similar to the COVID-19, several viral epidemics have occurred in the past 20 years, such as the SARS, the A/H1N1 influenza pandemic, the Middle East respiratory syndrome (MERS), and the Ebola virus disease. According to a review, in these large-scale viral outbreaks, HCW at high risks of exposure also had greater levels of both acute or posttraumatic stress (OR 1.71) and psychological distress (OR 1.74) [2]. Another similar review found that 11–73.4% of HCW reported PTSS during outbreaks, whereas depressive symptoms were reported in 27.5–50.7%, insomnia symptoms in 34–36.1%, and severe anxiety symptoms in 45% of HCW [70].
Compared with these results, our findings on the prevalence of psychological symptoms, especially the moderate and severe cases, in HCW from China under the COVID-19 were at the lower end. A possible explanation for the lower psychological distress of HCW in China could be the relatively low mortality rate, the quick control of the epidemic in China and available experiences acquired from previous pandemics, like the SARS in 2003.
Interventions and lessons learnt
In response to the crisis, as early as Jan 27, 2020, the National Health Commission of China published a national guideline of psychological crisis intervention for COVID-19 to provide multifaceted psychological protection of the mental health of medical workers [71]. Mental health experts across the country responded quickly to form psychosocial crisis intervention teams, and offered both online and face-to-face psychological counseling, hotline services, and online platforms with psychological self-help information, such as mindfulness and relaxation techniques [69]. Based on previous experiences, they were also expected to look after the needs of teams that were newly formed in the course of the Corona-related restructuring or that have come into conflict situations due to stress overload.
However, the implementation of psychological intervention services encountered obstacles, as Chen et al. pointed out [72]. Even though medical staff showed signs of psychological distress, they denied problems and refused psychological help. Therefore, interventions were adjusted to focus more on fulfilling their basic needs, such as providing more places to rest, guaranteeing food and daily living supplies [72]. According to existing evidence, prevention efforts such as screening for mental health problems should be provided in a proper way [73].
In some studies, psychological support demonstrated protective effects. For example, the Balint group, which was developed by Michael and Enid Balint, is a small group of clinicians who meet regularly to discuss cases from their practices, with a focus on the doctor–patient relationships. In Iran, the Balint groups were found to help healthcare workers to better cope with psychosocial stressors by improving participants' insight into their experience and by facilitating group learning on the doctor-patient relationships [74].
Limitations
Our review has several limitations. First, we only focused on studies conducted in China. Future reviews with studies from other countries that are affected by the virus at a later time period may show different exposure profiles. In particular, different health care systems will have an influence on the severity of mental stress and coping strategies. Second, the heterogeneity of the studies was high, perhaps due to the different assessment scales and its respective cut-off scores. We have tried to compensate for this heterogeneity by differentiating the moderate and severe cases from other subclinical symptoms, as well as by examining the severity reflected through continuous data. Subgroup analyses were also carried out and revealed that the frontline work, gender, occupation, and location could partly explain the high heterogeneity among the different studies. Third, even though we tried to include more high-quality studies by setting criteria for the journals in which they were published, the methodological quality of most studies was assessed as being moderate, and even low. For one, given the special background, most of the studies were carried out online so that no response rate could be provided, and the representative of the sample could not be guaranteed. Moreover, risk factors were seldom inquired, such as previous mental disorders or stressful live events, which could be the confounding factors of the current psychological distress. In addition, we did not set a criterion for the minimum time period when assessing the study quality, even though the AHRQ checklist was used to assess whether the study period was reported. It is also one of our limitations that we did not look up the subsequent studies that have referenced the studies included. Last, our analyses showed that a publication bias was likely, pertaining to the prevalence of PTSS, anxiety, and depression.
Future research directions
Future high-quality research remains necessary to explore the impact of COVID-19 on profession-related burnout of HCW, its long-term impact, and post-stress or post-traumatic growth, i.e., the positive psychological change experienced after the struggle with COVID-19, such as to identify meaning in interpersonal relationships, to change priorities, and to have a richer spiritual life.
To improve the methodological quality, researchers should pay further attention when designing the study, and should especially consider how to improve the representativeness of the sample, and the validity and reliability of assessment tools, and how to assess and control for potential confounding factors more sufficiently.
Conclusions
In summary, during the COVID-19 pandemic, an increased level of anxiety, depression, sleep disorders, and PTSS symptoms was detected among healthcare professionals in China. Among them, about a third showed at least mild symptoms, while moderate and severe syndromes were relatively low. Despite the low severity of the symptoms, these subsyndromal disorders should be detected and treated in time to prevent the development of complex disorders such as PTSD and to prevent the chronification of depression, anxiety and sleep disorders. In the future, high-quality studies on profession-related burnout, long-term impacts and the post-stress growth are still needed.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are grateful for the help of Chuanzhu Lv, Xingyue Song, Yan Lv, Ningxi Yang, Zhou Zhu and Jinfeng Miao, and Zhaorui Liu and Chao Ma by providing relevant data for the research through contacting by e-mail.
Funding
Open Access funding enabled and organized by Projekt DEAL. The research was funded by the National Natural Science Foundation of China (no. 81800482).
Availability of data and material
Available at request.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Not required.
References
- 1.Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Ng CH. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ (Clin Res Ed) 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—a systematic review and meta-analysis. Psychiatry Res. 2020;291:113190. doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 6.Dai Y, Hu G, Xiong H, Qiu H, Yuan X (2020) Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. 10.1101/2020.03.03.20030874(medRxiv:2020.2003.2003.20030874)
- 7.Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, Zhuang Q. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 During the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit. 2020;26:e924171. doi: 10.12659/msm.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jin Y-H, Huang Q, Wang Y-Y, Zeng X-T, Luo L-S, Pan Z-Y, Yuan Y-F, Chen Z-M, Cheng Z-S, Huang X, Wang N, Li B-H, Zi H, Zhao M-J, Ma L-L, Deng T, Wang Y, Wang X-H. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID-19 infected healthcare workers in a tertiary acute care hospital in Wuhan: a cross-sectional survey. Mil Med Res. 2020;7(1):24. doi: 10.1186/s40779-020-00254-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, Yao L, Bai H, Cai Z, Xiang Yang B, Hu S, Zhang K, Wang G, Ma C, Liu Z. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: who will be the high-risk group? Psychol Health Med. 2020 doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- 13.Viswanathan M, Berkman ND, Dryden DM, Hartling L (2013) AHRQ Methods for effective health care. in: assessing risk of bias and confounding in observational studies of interventions or exposures: further development of the RTI Item Bank. Agency for Healthcare Research and Quality (US), Rockville (MD) [PubMed]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clin Res Ed) 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.StataCorp. 2017. Stata statistical software: release 15. collegestation, TX: StataCorp LLC
- 16.Li G, Miao J, Wang H, Xu S, Sun W, Fan Y, Zhang C, Zhu S, Zhu Z, Wang W. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J Neurol Neurosurg Psychiatry. 2020 doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- 17.Sun D, Yang D, Li Y, Zhou J, Wang W, Wang Q, Lin N, Cao A, Wang H, Zhang Q. Psychological impact of 2019 novel coronavirus (2019-nCoV) outbreak in health workers in China. Epidemiol Infect. 2020 doi: 10.1017/S0950268820001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, Du H, Li R, Kang L, Su M, Zhang J, Liu Z, Zhang B. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychol. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, Miao J, Zhang C, Yang Y, Sun W, Zhu S, Fan Y, Chen Y, Hu J, Liu J, Wang W. COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine. 2020;24:100443. doi: 10.1016/j.eclinm.2020.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen J, Min M, Yin G, Luo J, Chen F, Ren J, Gong W. Survey of the psychological status and associated factors of healthcare workers in Qingbai district of Chengdu during the COVID-19. Shandong Med. 2020;60(09):70–72. [Google Scholar]
- 21.Deng R, Chen F, Liu S, Yuan L, Song J. Influencing factors for psychological stress of healthcare workers in COVID-19 isolation wards. Chin J Infect Control. 2020;19(3):256–261. doi: 10.12138/j.issn.1671-9638.20206395. [DOI] [Google Scholar]
- 22.Deng S. A survey on the psychological status of healthcare providers in Yongchuan hospital affiliated to Chongqing Medicial University, one of the designated hospitals for noval coronavirus pneumonia. Basic Cin Med. 2020;40(5):1–3. [Google Scholar]
- 23.Huang J, Han M, Luo T, Ren A, Zhou X. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Chin J Ind Hyg Occup Dis. 2020;38(3):192–195. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- 24.Huangfu M, Fu X, Wang L, Huang N (2020) Investigation on psychological stress of frontline nurses in novel coronavirus pneumonia prevention and control (online first). Chongqing Med 1–6
- 25.Jiang X, Tan X. Investigation of mental health status among front-line nurses during the epidemic of coronavirus disease 2019. J Nurs Sci. 2020;35(07):75–77. [Google Scholar]
- 26.Li C, Mi Y, Chu J, Zhu L, Zhang Z, Liang L, Liu L. Investigation and analysis of post-traumatic stress disorder in front-line nursing staff during the COVID-19. J Nurs. 2020;35(07):615–618. [Google Scholar]
- 27.Li R, Xiong Z, Liu L, Zong S, Li H. Prevalence of anxiety and influencing factors in frontline nurses combating the COVID-19 epidemic: an analysis based on a survey from the first batch of designated hospitals for COVID-19 treatment in Wuhan. Pract J Card Cereb Pneumal Vasc Dis. 2020;28(03):19–23. [Google Scholar]
- 28.Li X, Lei Y, Hu D, Deng X. The construction of the three-level intervention system of psychological crisis of first-line nurses in the designated hospital of COVID-19. J Nurs. 2020;35:1–4. [Google Scholar]
- 29.Liu X, Cheng Y, Wang M, Pan Y, Guo H, Jiang R, Wang Q. Psychological state of nursing staff in a large scale of general hospital during COVID-19 epidemic. Chin J Nosocomiol. 2020;30(11):1634–1639. [Google Scholar]
- 30.Luo Q, Yan C, Zhang D, Deng S, Zhou L, Mai W, Ning Y, He H, Zhang S, Li Y, Nong F, Liao Y, Li A, Wu Y, Ge J, Zhong Y, Hu Y, Li F, Peng H. Investigation and mental health status of frontline medical staff in COVID-19 treatment hospital in Guangdong province. Guangdong Med J. 2020;41:1–7. [Google Scholar]
- 31.Pu J, li G, Cao L, Wu Y, Xu L (2020) Investigation and analysis of the psychological status of the clinical nurses in a class A hospital facing the novel coronavirus pneumonia (online first). Chongqing Med 1–6
- 32.Sheng X, Liu F, Zhou J, Liao R. Psychological status and sleep quality of nursing interns during the outbreak of COVID-19. J South Med Univ. 2020;40(3):346–350. doi: 10.12122/j.issn.1673-4254.2020.03.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang J, Cheng Y, Zhou Z, Jiang A, Guo J, Chen Z, Wan Q. Psychological status of Wuhan medical staff in fighting against COVID-19. Med J Wuhan Univ. 2020;41(4):547–550. [Google Scholar]
- 34.Wu J, Rong X, Chen F, Diao Y, Chen D, Jing X, Gong X. Investigation on sleep quality of first-line nurses in fighting against corona virus disease 2019 and its influencing factors. Chin Nurs Res. 2020;34(4):558–562. doi: 10.12102/j.issn.1009-6493.2020.04.107. [DOI] [Google Scholar]
- 35.Xing L, Ren Z, Zhou Y, Peng J, Gao S. Psychological intervention for first-line nurses battling coronavirus disease 2019. J Nurs Sci. 2020;35(8):17–19. [Google Scholar]
- 36.Xu M, Zhang Y. psychological survey of first clinical firstline support nurses fighting against pneumonia caused by a 2019 noval coronavirus infection. Chin Nurs Res. 2020;34(3):368–370. doi: 10.12102/j.issn.1009-6493.2020.03.002. [DOI] [Google Scholar]
- 37.Xu Y. Survey of the psychological status of the first batch of miltary healthcare workers assisted Wuhan city and the advice for prevention. Mil Med Sci. 2020;44(4):313–315. [Google Scholar]
- 38.Yin J, Wu X, Ma W, Xu J, Wei P, Dang X, Li Y. Psychological investigation and analysis on medical care personnel in designated hospitals of Coronavirus disease 2019. Med Philos. 2020;41(08):38–42. [Google Scholar]
- 39.Yuan H, Luo L, Wu J, Hu D, Lei K, Huang J (2020) Mental health status and coping strategies among medical staff during outbreak of coronavirus disease 2019 (online first)] Med J Wuhan Univ 1–6
- 40.Cai W, Lian B, Song X, Hou T, Deng G, Li H. A cross-sectional study on mental health among health care workers during the outbreak of corona virus disease 2019. Asian J Psychiatry. 2020;51:102111. doi: 10.1016/j.ajp.2020.102111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cao J, Wei J, Zhu H, Duan Y, Geng W, Hong X, Jiang J, Zhao X, Zhu B. A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 outbreak. Psychother Psychosom. 2020 doi: 10.1159/000507453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, Liu B, Zhang M, Yin Y, Qin J, Bouey J, Zhao M, Li X. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. 2020 doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guo J, Liao L, Wang B, Li X, Guo L, Gu Y (2020) Psychological effects of COVID-19 on hospital staff: a national cross-sectional survey of China mainland—manuscript draft
- 44.Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, Bi J, Zhan G, Xu X, Wang L, Zhou Q, Zhou C, Pan Y, Liu S, Zhang H, Yang J, Zhu B, Hu Y, Hashimoto K, Jia Y, Wang H, Wang R, Liu C, Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. 2020;133:110102. doi: 10.1016/j.jpsychores.2020.110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, Cheng ASK. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect. 2020;148:e98. doi: 10.1017/s0950268820001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu Z, Han B, Jiang R, Huang Y, Ma C, Wen J, Zhang T, Wang Y, Chen H, Ma Y (2020) Mental health status of doctors and nurses during COVID-19 epidemic in China
- 48.Lv Y, Yao H, Xi Y, Zhang Z, Zhang Y, Chen J, Li J, Li J, Wang X, Luo GQ. Social support protects Chinese medical staff from suffering psychological symptoms in COVID-19 defense. SSRN Electron J. 2020 doi: 10.2139/ssrn.3559617. [DOI] [Google Scholar]
- 49.Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, Qin M, Huang H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020 doi: 10.1111/jonm.13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Qi J, Xu J, Li BZ, Huang JS, Yang Y, Zhang ZT, Yao DA, Liu QH, Jia M, Gong DK, Ni XH, Zhang QM, Shang FR, Xiong N, Zhu CL, Wang T, Zhang X. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 2020;72:1–4. doi: 10.1016/j.sleep.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, Yan S, Lv C. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tian T, Meng F, Pan W, Zhang S, Cheung T, Ng CH, Li XH, Xiang YT. Mental health burden of frontline health professionals in screening and caring the imported COVID-19 patients in China during the pandemic. Psychol Med. 2020 doi: 10.1017/S0033291720002093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. 2020;26:e924085. doi: 10.12659/msmbr.924085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. doi: 10.12659/msm.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xiao X, Zhu X, Fu S, Hu Y, Li X, Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J Affect Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, Min BQ, Tian Q, Leng HX, Du JL, Chang H, Yang Y, Li W, Shangguan FF, Yan TY, Dong HQ, Han Y, Wang YP, Cosci F, Wang HX. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020 doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, Li W, Xiao S. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psychol. 2020;11:386. doi: 10.3389/fpsyt.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bohlken J, Schömig F, Lemke MR, Pumberger M, Riedel-Heller SG. COVID-19 pandemic: stress experience of healthcare workers—a short current review. Psychiatry Prax. 2020;47(4):190–197. doi: 10.1055/a-1159-5551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med. 2020;21(5):1059–1066. doi: 10.5811/westjem.2020.7.48684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—a review. Asian J Psychiatry. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, Yu Y, Kou C, Xu X, Lu J, Wang Z, He S, Xu Y, He Y, Li T, Guo W, Tian H, Xu G, Xu X, Ma Y, Wang L, Wang L, Yan Y, Wang B, Xiao S, Zhou L, Li L, Tan L, Zhang T, Ma C, Li Q, Ding H, Geng H, Jia F, Shi J, Wang S, Zhang N, Du X, Du X, Wu Y. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–224. doi: 10.1016/s2215-0366(18)30511-x. [DOI] [PubMed] [Google Scholar]
- 62.Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020;15(4):e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, Choo FN, Tran B, Ho R, Sharma VK, Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, Yeo LLL, Ahmad A, Ahmed Khan F, Napolean Shanmugam G, Sharma AK, Komalkumar RN, Meenakshi PV, Shah K, Patel B, Chan BPL, Sunny S, Chandra B, Ong JJY, Paliwal PR, Wong LYH, Sagayanathan R, Chen JT, Ying Ng AY, Teoh HL, Tsivgoulis G, Ho CS, Ho RC, Sharma VK. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S, Birk JL, Brodie D, Cannone DE, Chang B, Claassen J, Cornelius T, Derby L, Dong M, Givens RC, Hochman B, Homma S, Kronish IM, Lee SAJ, Manzano W, Mayer LES, McMurry CL, Moitra V, Pham P, Rabbani L, Rivera RR, Schwartz A, Schwartz JE, Shapiro PA, Shaw K, Sullivan AM, Vose C, Wasson L, Edmondson D, Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tan BYQ, Kanneganti A, Lim LJH, Tan M, Chua YX, Tan L, Sia CH, Denning M, Goh ET, Purkayastha S, Kinross J, Sim K, Chan YH, Ooi SBS. Burnout and associated factors among health care workers in singapore during the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21(12):1751–1758.e1755. doi: 10.1016/j.jamda.2020.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen R, Sun C, Chen JJ, Jen HJ, Kang XL, Kao CC, Chou KR. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nurs. 2021;30(1):102–116. doi: 10.1111/inm.12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lasalvia A, Amaddeo F, Porru S, Carta A, Tardivo S, Bovo C, Ruggeri M, Bonetto C. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. 2021;11(1):e045127. doi: 10.1136/bmjopen-2020-045127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Huang J, Liu F, Teng Z, Chen J, Zhao J, Wang X, Wu R. Care for the psychological status of frontline medical staff fighting against COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, Di Pierro R, Madeddu F, Calati R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. 2020;22(8):43. doi: 10.1007/s11920-020-01166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, Wang Y, Hu J, Lai J, Ma X, Chen J, Guan L, Wang G, Ma H, Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14. doi: 10.1016/s2215-0366(20)30047-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, He L, Sheng C, Cai Y, Li X, Wang J, Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/s2215-0366(20)30078-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 74.Kiani Dehkordi M, Sakhi S, Gholamzad S, Azizpour M, Shahini N. Online Balint groups in healthcare workers caring for the COVID-19 patients in Iran. Psychiatry Res. 2020;290:113034. doi: 10.1016/j.psychres.2020.113034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Available at request.
Not applicable.