Abstract
A 68-year-old woman was admitted with a persistent cough and dyspnea that had persisted for 4 months prior. Chest computed tomography revealed a tumor protruding from the membranous portion of the trachea. She underwent tumor resection via rigid and flexible bronchoscopy to relieve the symptoms and obtain a diagnosis. After the procedure, she was diagnosed with tracheal liposarcoma. Three months after the procedure, she underwent complete surgical tumor resection. Liposarcoma is a mesenchymal tumor that usually develops in the extremities and the retroperitoneum. Tracheal liposarcoma is extremely rare. To the best of our knowledge, this is only the second reported case.
Keywords: liposarcoma, tracheal liposarcoma, tracheal tumor
Introduction
Primary tracheal tumors are rare, constituting only 2% of all airway malignancies (1). Most arise from the surface epithelium. Most are squamous cell carcinomas, followed by adenoid cystic carcinomas (2). Mesenchymal neoplasms are rare and mostly benign. Primary tracheal liposarcoma is extremely rare, with only one case reported in the relevant literature (in 1979) (3). We herein present the second case.
Case Report
A 68-year-old woman developed severe cough and was diagnosed with bronchial asthma by her general practitioner. She started inhaled budesonide/formoterol fumarate hydrate, but her cough did not improve. Four months later, the cough worsened and she developed dyspnea. Chest computed tomography (CT) revealed a tumor protruding from the membranous portion of the trachea. She was admitted to our hospital to improve her symptoms and confirm the diagnosis.
On physical examination, she had no respiratory failure but had stridor in both the inspiratory and expiratory phases of respiration. Her laboratory data showed no remarkable abnormality. Chest CT revealed a protruding tracheal tumor (10.6×12.2×16.6 mm) from the membranous portion, which almost occluded the tracheal lumen (Fig. 1A-C). There was no evidence of metastasis on CT or gastrointestinal endoscopy.
Figure 1.
Chest CT reveals a tracheal tumor protruding from the membranous portion.
She underwent initial tumor resection using rigid and flexible bronchoscopes under general anesthesia. At bronchoscopy, a protruding tumor was observed at the membranous portion of the trachea. The diameter was almost 11 mm, and it was located approximately 5 cm distal to the vocal cords (Fig. 2). The surface of the tumor was smooth with slight vascular engorgement. The tumor was resected using a high-frequency electric snare and argon plasma coagulation. A pathological examination revealed spindle cell tumor proliferation and atypical mitotic activity with intracellular edema and inflammatory cell infiltration (Fig. 3A, B). Immunohistochemical studies showed that the spindle cells were positive for αSMA (Fig. 3C), vimentin (Fig. 3D), and Ki-67 (approximately 30%), and negative for CD68 (PG-M1), pan-keratin (AE1.3, PCK26), desmin, S100, ALK, CD31, CK OSCAR, calponin, SOX10, EMA, CD117, EBER ISH, and pan-TRK. Fluorescence in situ hybridization (FISH) demonstrated amplification of the MDM2 gene on chromosome 12 (Fig. 2D), and no EWS gene recombination. The pathological diagnosis was a dedifferentiated liposarcoma. Three months later, she underwent total pharyngolaryngectomy, cervical esophagectomy and free jejunal reconstruction. Microscopic examination of the resected specimen revealed a residual tumor in the membranous portion of the trachea, extending to the tracheal lumen (Fig. 4). The margin of the resected tissue was negative. The final diagnosis was tracheal liposarcoma.
Figure 2.
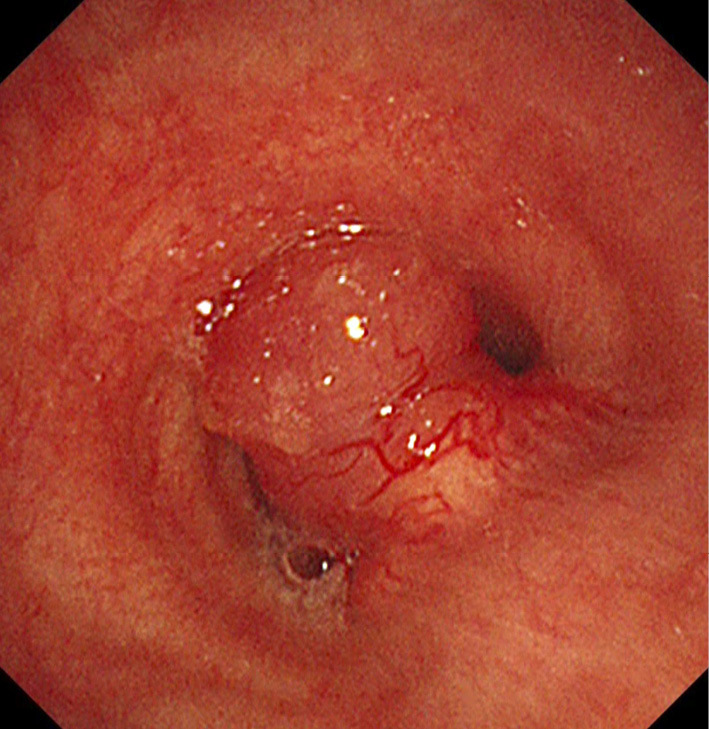
Bronchoscopic view of the tumor obstructing the trachea.
Figure 3.
A, B: Hematoxylin and Eosin staining revealed spindle cell tumor proliferation and atypical mitotic activity with intracellular edema and inflammatory cell infiltration (A ×40), (B ×400). C: Immunohistochemical images of αSMA. D: Immunohistochemical images of vimentin. E: The FISH analysis using probes for MDM2 (red signals) and centromere 12 (green signals) revealed high-level MDM2 amplification. The amplified signals formed a large cluster.
Figure 4.
A, B: The histopathological examination of specimens obtained via total laryngectomy (A ×1.25) (B ×20; the square portion of A). (a) The tracheal lumen, (b) the tumor, (c) tracheal cartilage, (d) the esophageal muscularis propria, (e) the esophageal mucosal epithelium.
Discussion
Liposarcoma is a rare mesenchymal neoplasm, accounting for only 1% of all malignancies (4). Liposarcoma is classified into four subtypes according to the 2019 National Comprehensive Cancer Network classification of liposarcoma: well-differentiated, myxoid, pleomorphic and dedifferentiated. The relative frequency of liposarcoma in various body sites is dependent on the tumor subtype. Dedifferentiated liposarcoma most commonly occurs in the retroperitoneum, followed by the extremities, and the scrotum/spermatic cord. Liposarcoma has been seen in the trachea in some cases but most of these had invaded from the mediastinum, and cases originating in the trachea are extremely rare, with only one reported case in 1979 (3).
In comparison to the previous case (3), our case exhibited certain similarities in terms of symptoms (dyspnea), abnormal chest sounds (wheezing and stridor), and tumor structure (polypoid mass with a smooth surface). However, the pathological diagnoses differed; the earlier tumor was well-differentiated, while the present tumor dedifferentiated. Thus, this is the first case of a dedifferentiated liposarcoma of the trachea.
A dedifferentiated liposarcoma develops when a well-differentiated tumor progresses to (a usually non-lipogenic) sarcoma of variable histological grade. The extent of dedifferentiation is also variable. Both dedifferentiated and well-differentiated liposarcomas are characterized by consistent amplification of MDM2 and CDK4 (12q14-q15). In some cases, a well-differentiated lipomatous component is hard to identify (5). In the present case, no well-differentiated component was evident in either the biopsy or resection specimens. The detection of MDM2 amplification via FISH aided in the diagnosis.
Surgical resection is the treatment of choice. Postoperative chemotherapy and radiotherapy may reduce local recurrence; however, their efficacy is limited (6). The long-term prognosis of tracheal dedifferentiated liposarcoma is unclear, but its tight adhesion to adjacent structures makes it difficult to resect completely or to debulk the tumor. In addition, it has strong potential for metastasis, which is associated with a poor prognosis.
This patient underwent initial tumor resection using rigid and flexible bronchoscopes, which improved her symptoms. After three months, we performed total pharyngolaryngectomy, cervical esophagectomy and free jejunal reconstruction, and the margin of the resected tissue was negative.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We thank Dr. M. Hashimoto of Nagoya Daini Red Cross Hospital for their advice on the pathological diagnosis.
References
- 1.Diaz-Mendoza J, Debiane L, Peralta AR, Simoff M. Tracheal tumors. Curr Opin Pulm Med 25: 336-343, 2019. [DOI] [PubMed] [Google Scholar]
- 2.Macchiarini P. Primary tracheal tumours. Lancet Oncol 7: 83-91, 2006. [DOI] [PubMed] [Google Scholar]
- 3.Van Den Beukel JT, Beukel JT, Wagenaar SJ, Vanderschueren R. Liposarcoma of the trachea. Thorax 34: 817-818, 1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gethin-Jones TL, Evans NR, Morse CR. Surgical management of mediastinal liposarcoma extending from hypopharynx to carina: case report. World J Surg Oncol 8: 13, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dei Tos AP, Marino-Enriquez A, Pedeutour F. Dedifferentiated liposarcoma. In: WHO Classification of Tumours. Soft Tissue and Bone Tumours Vol. 3. 5th ed. Antonescu CR, Blay JV, Bovée JVMG, et al. , Eds. IARC Press, Lyon, 2020: 39-41. [Google Scholar]
- 6.Thway K, Jones RL, Noujaim J, Zaidi S, Miah AB, Fisher C. Dedifferentiated liposarcoma: updates on morphology, genetics, and therapeutic strategies. Adv Anat Pathol 23: 30-40, 2016. [DOI] [PubMed] [Google Scholar]





