Abstract
Background
In Ethiopia, cervical cancer ranked as the second leading cause of female cancer and also stands as the most common cancer among women aged from 15 to 44 years old. Hence, this study aimed to assess knowledge, attitude, and practice toward cervical cancer screening among women attending health facilities in central Ethiopia.
Methods
Institutional-based cross-sectional study was conducted among 420 study participants. Data were collected using an interviewer-administered questionnaire. The collected data were entered into EPI data 3.1 and exported to SPSS version 23 for analysis. Binary and multivariate logistic regressions were used to identify factors associated with knowledge, attitude, and practice of cervical cancer screening. Odds ratio (OR) with 95% CI and a P-value < .05 were used to declare statistical significance.
Results
Half, 50.7% of study participants had good knowledge. Less than half, 46.1% had a positive attitude toward cervical cancer screening. Only 6.3% of women have been screened for cervical cancer. Diploma and above education (AOR: 2.22, 95% CI: 1.32, 6.157), no idea about cervical cancer curable at an early stage (AOR: 6.23, 95% CI: 6.23 (2.77, 15.13) were significantly associated with knowledge of cervical cancer screening. Diploma and above education (AOR: 0.37, 95% CI: 0.19, 0.74) and multiple sexual partners (AOR: 0.18, 95% CI: 0.05, 0.62) were factors associated with a negative attitude toward cervical cancer screening. Positive attitude about cervical cancer screening (AOR: 2.37, 95% CI: 1.91, 6.20) was significantly associated with the practice of being screened.
Conclusions
Cervical cancer screening knowledge and attitudes were moderate, but practice was low. Educational status, considering cervical cancer is not curable at an early stage and not having an idea about its curability at an early stage, was significantly associated with knowledge of cervical cancer screening. Sexual partner status and educational status showed significant association with an attitude toward cervical cancer screening and having a positive attitude toward cervical cancer screening were significantly associated with the practice of cervical cancer screening. Health professionals need to disseminate cervical cancer screening information and offer cervical cancer treatment during health-care appointments.
Keywords: cervical cancer, HPV, knowledge, attitude, practice, screening, women
Background
Cervical cancer occurs when abnormal cells in the lining of the cervix grow in an uncontrolled way and is caused by Human papillomavirus (HPV).1,2 Worldwide, cervical cancer is the second most common health problem in women. It is estimated that over the next 12 years (2018-2030) the number of annual cervical cancer incidence and death is expected to increase from 570,000 to 700,000 and 311,000 to 400,000, respectively. 3 In Ethiopia, cervical cancer also ranks the second leading cause of female cancer and also stands as the most common cancer among women aged from 15 to 44 years old. 4
Early diagnosis, effective screening, and treatment programs can reduce cervical cancer.5-7 By 2030, it was proposed by WHO that globally, 90% of girls fully vaccinated with the HPV vaccine by age 15; 70% of women are screened with a high-performance test by 35 years of age and 45 years; and 90% of women identified with the cervical disease receive treatment. 8 The Ethiopian Federal Ministry of health in collaboration with pathfinder international has also started the program of cervical cancer screening in 2010 to reduce the morbidity and mortality caused by cervical cancer. 9
Existing evidence indicate that geographical status, lack of access to screening services, socio-economic and demographic characteristics, poor attitude toward the disease and screening, lack of knowledge and educational level are factors influencing cervical cancer screening.10,11
The rate of the prevalence of cervical cancer varies from place to place. 12 For instance, the rate of cervical cancer in developed countries is 5 per 100,000 women, whereas 25/100,000 in developing countries. The annual prevalence of newly diagnosed cases and death from cervical cancer in Ethiopia is 35.9 and 22.6 per 100,000 women, respectively. 13 In low and middle-income countries like Ethiopia, cervical cancer accounts for approximately 90% of deaths from cancer. 6 The highest mortality rates due to cervical cancer occur in Eastern, Western, and Southern part of the sub-Saharan African countries which is 25.3/100000, 24/100000, 14.8/100000, respectively. 14 In the Africa region, cervical cancer accounts for 22% of all female cancers, and also 34 out of every 100000 and 23 out of 100000 women are diagnosed with and die from cervical cancer, respectively. 15
However, despite the fact that increasing awareness has an important role to increase and strengthen the demand for cervical cancer screening services, 16 in Ethiopia, knowledge, attitude, and practice of cervical cancer screening is not well-known.17,18 Therefore, this study aimed to assess knowledge, attitude, and practice toward cervical cancer screening among women attending health facilities in Ambo town, central Ethiopia.
Methods
Study Design, Period, and Area
An institutional-based cross-sectional study was conducted from August to September 2020 in Ambo town, central Ethiopia. Ambo town is located 114 km to the West of Addis Ababa, the capital. 19 In the town, there were one General Hospital, one Referral Hospital, and two Health centers which provide health services for the community. The study was conducted in all health facilities available in the town. All of the health facilities in the town give preventive and curative cares for mothers including cervical cancer screening. According to the national population and housing census of 2007, the estimated number of women of childbearing age was (15-49) was 18,379. 20
Source and Study Population
The source populations were all women aged 18-49 years of age attending health facilities in Ambo town and the study populations were randomly selected women. Women of 18-49 years age who attended antenatal care, Family Planning, Postnatal care, and other Outpatient Departments (OPDs) were included; however, women with known mental illness, in labor, or who were seriously sick (those who had postpartum hemorrhage and uterine rupture) were excluded from the study.
Sample Size Determination
The sample size was determined using the single population proportion formula and by considering 45.5% of prevalence of favorable attitude toward cervical cancer screening from a previous study conducted in Wolaita Zone, Ethiopia, 21 at the confidence interval 95% and margin of error 5%. After adding 10% non-response rate, the final sample size was 420.
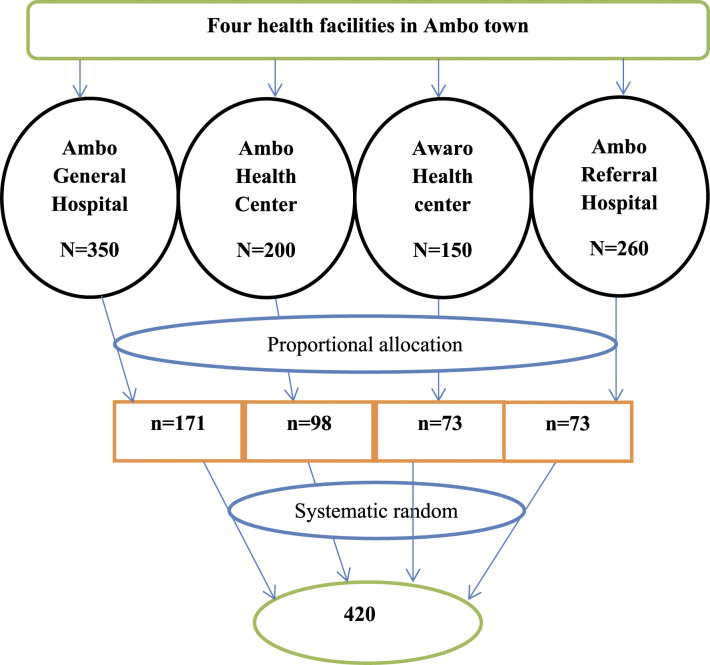
Sampling Procedure
The study was conducted in all health facilities available in Ambo town (two Hospitals and two Health centers). The study participants were proportionally allocated to each health facility based on the average number of women of 18-49 years flow during the last 3 months prior to the study. A systematic random sampling technique was used to select the study participants among those eligible clients (Figure 1).
Figure 1.
Schematic representation of the sampling technique among women attending town health facilities in Ambo, 2020.
Data Collection Methods, Tool, and Procedures
Interviewer-administered structured questionnaire was adapted from a previous study 22 for data collection. The questionnaire contained socio-demographic characteristics, knowledge, attitude, and practice of cervical cancer screening of women. The questionnaire was prepared in English and translated to Afan Oromo and translated back to the English language by the language experts to check the consistency. Data were collected using face-to-face interviews. Four female BSC nurses and two BSC Public health professionals were recruited for data collection and supervision, respectively.
Operational Definitions
Knowledge of cervical cancer: was assessed by using 11 items questions that give maximum of 11 points and a minimum of 0 points. The cumulative mean score of knowledge of participants about cervical cancer was estimated using the mean score to classify into good knowledge (those respondents who scored above the mean) and poor knowledge (those respondents who scored below the mean score on the knowledge question). 23
We examined the attitude with a Likert scale and 7 satisfaction items. The following rating method was used: strongly disagree = 1, disagree = 2, neutral = 3, agree = 4, and strongly agree = 5. The responses were totaled to produce a total score. The mean score was then computed. Those who scored the mean or above were considered to have a good attitude toward cervical cancer screening, whereas those who scored below the mean were judged to have a negative attitude toward cervical cancer screening. 21
Poor Practice refers to respondents who have never been screened for cervical cancer, whereas Good Practice refers to respondents who have been screened for cervical cancer at least once. 21
Data Quality Control and Management
Three days of training was given for data collectors and supervisors on the objectives of the study, data collection tools, procedure as well as on how to maintain the confidentiality of the respondents. The questionnaire was pretested using 5% at Guder Hospital which is outside the study area. Close supervision was also made every day at the end of data collection.
Data Processing and Analysis
Data were checked for completeness, coded, and entered into EPI data version 3.1 and then, exported to SPSS version 23 for analysis. The results were presented using texts, frequencies, percentages, and graphs. Binary logistic regression at a P-value of < .25 was used to identify candidate variables for multivariate logistic regression analysis. 24 Hosmer and Lemeshow goodness was used to check model goodness and the P-value of the model fitness test was .880. Multicollinearity was checked by Variance Inflation Factor (VIF). All the candidate variables were entered into multivariate logistic regression analysis. Finally, OR with 95% CI and P-value < .05 were used to declare significant association.
Results
Socio-Demographic Characteristics of the Respondents
A total of 414 women participated in this study yielding a response rate of 98.6%. One hundred and seventy, (41.10%) of the respondents were in 20-25 age groups. Six in ten, (61.4%) of the study participants were married. Regarding educational status, 33.3% completed high school. Nearly all (95.2%) of the respondents have single sexual partner during their lifetime (Table 1).
Table 1.
Socio-Demographic Characteristics of Women Attending Health Facilities in Ambo Town, 2020.
| Variables | Number | Percent |
|---|---|---|
| Age Category in years | ||
| <20 | 46 | 11.11 |
| 20-24 | 170 | 41.10 |
| 25-29 | 90 | 21.74 |
| 30-34 | 59 | 14.25 |
| ≥35 | 49 | 11.80 |
| Educational status | ||
| No formal education | 54 | 13.0 |
| Elementary | 121 | 29.2 |
| High school | 138 | 33.3 |
| Diploma and above | 101 | 24.4 |
| Residence | ||
| Urban | 322 | 77.8 |
| Rural | 92 | 22.2 |
| Marital status | ||
| Currently married | 254 | 61.4 |
| Living together/Cohabiting | 74 | 17.9 |
| Never married | 61 | 14.7 |
| Others a | 25 | 6 |
| Number of lifetime sexual partner | ||
| Single | 394 | 95.2 |
| Multiple | 20 | 4.8 |
awidowed, divorced/separated.
Knowledge About Cervical Cancer Screening
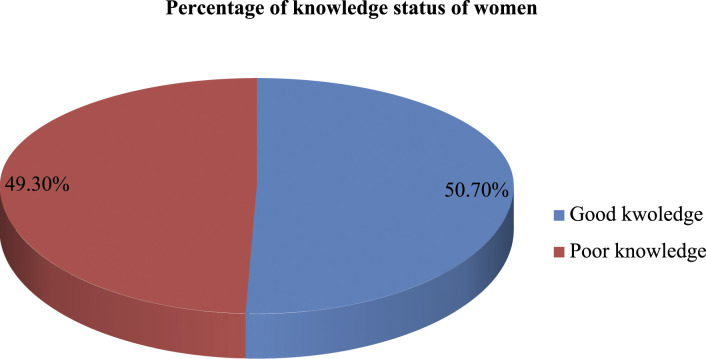
Out of the 414 respondents, 68.8% reported that they heard about cervical cancer. Of 414 respondents, 45.2% did not know the sign and symptoms of cervical cancer and 49% did not know the risk factors for cervical cancer. Of all respondents, 45.9% did not know how one can prevent cervical cancer and only 26.1% responded that cervical cancer can be cured at an early stage. Only 72.2% of women knew cervical screening methods (Table 2). Nearly half, (50.7%) of the study participants had good knowledge while 49.3% had poor knowledge of cervical cancer screening (Figure 2).
Table 2.
Knowledge About Prevention, Treatment and Screening Modalities of Cervical Cancer Among Women Attending Health Facilities in Ambo Town, 2020.
| Variables, n = 414 | Number | Percent |
|---|---|---|
| Have you heard about cervical cancer | ||
| Yes | 285 | 68.8 |
| No | 129 | 31.2 |
| Source of information about cervical cancer | ||
| Media | 149 | 52.3 |
| Written materials | 8 | 2.8 |
| Health workers | 38 | 13.3 |
| Family, friends, neighbor | 60 | 21.1 |
| Religious leaders | 10 | 3.5 |
| Teachers | 20 | 7 |
| What are the symptoms of cervical cancer | ||
| Vaginal bleeding | 85 | 20.5 |
| Vaginal foul-smelling discharges | 133 | 32.1 |
| Do not know | 196 | 47.4 |
| What are the risk factors of cervical cancer | ||
| Having multiple sexual partners | 73 | 17.6 |
| Early sexual intercourse | 83 | 20.0 |
| Acquiring HPV virus | 27 | 6.5 |
| Cigarette smoking | 20 | 4.8 |
| Do not know | 211 | 50.9 |
| How can person prevent cervical cancer | ||
| Avoid multiple sexual partners | 80 | 19.3 |
| Avoid early sexual intercourse | 96 | 23.2 |
| Quit smoking | 17 | 4.1 |
| Through vaccination of HPV vaccine | 30 | 7.2 |
| Do not know | 191 | 46.1 |
| Avoid multiple sexual partners | 80 | 19.3 |
| Cervical cancers can cure at early stage | ||
| Yes | 108 | 26.1 |
| No | 194 | 46.9 |
| Don’t know | 112 | 27.1 |
| How can someone have treated of the cervical cancer | ||
| Herbal remedies | 24 | 5.8 |
| Surgery | 66 | 15.9 |
| Drugs | 196 | 47.3 |
| Radiotherapy | 37 | 8.9 |
| don’t know | 91 | 22 |
| How is the cost of treatment for cervical cancer screening in this country? | ||
| It is free of charge | 44 | 10.6 |
| It is reasonably priced | 62 | 15.0 |
| It is moderately expensive | 45 | 10.9 |
| It is very expensive | 141 | 34.1 |
| Don’t know | 122 | 29.5 |
| How frequent is screening for cervical cancer screening | ||
| Once every year | 105 | 25.4 |
| Once every 3 years | 83 | 20.0 |
| Once every 5 years | 19 | 4.6 |
| Don’t know | 207 | 50.0 |
| Who should be screened for cervical cancer? | ||
| Women of 25 years and above | 192 | 46.4 |
| Prostitutes | 78 | 18.8 |
| Elderly women | 144 | 34.7 |
| Screening procedure | ||
| Visual inspection of the cervix with acetic acid | 35 | 8.5 |
| Pap smear | 28 | 6.8 |
| Biopsy | 44 | 10.6 |
| Don’t know | 299 | 72.2 |
Figure 2.
Knowledge status of women attending health facilities in Ambo town towards cervical cancer, 2020.
Attitudes of Respondents Toward Cervical Cancer Screening
This study revealed that only 46.1% of study participants had positive attitude toward cervical cancer screening (Figure 2). Of the 414 participants, 48.6% of them agreed that cervical cancer is highly prevalent in Ethiopia. Less than a quarter of the study participants strongly agreed that all females can acquire cervical cancer. About one-fourth (25.8%) of the participants agreed that the precancerous cervical cancer screening methods can help to prevent cervical cancer.
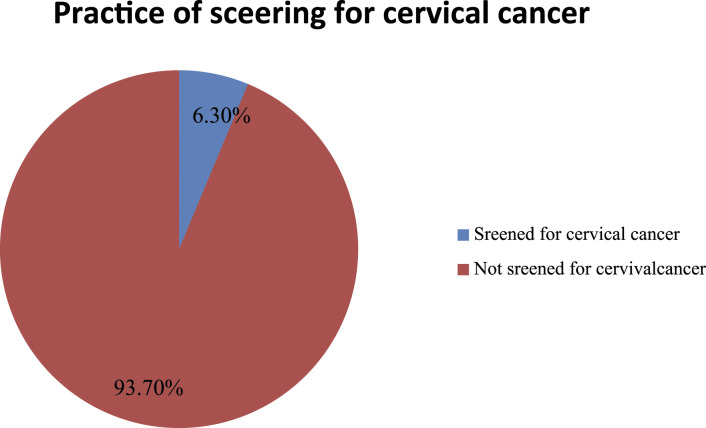
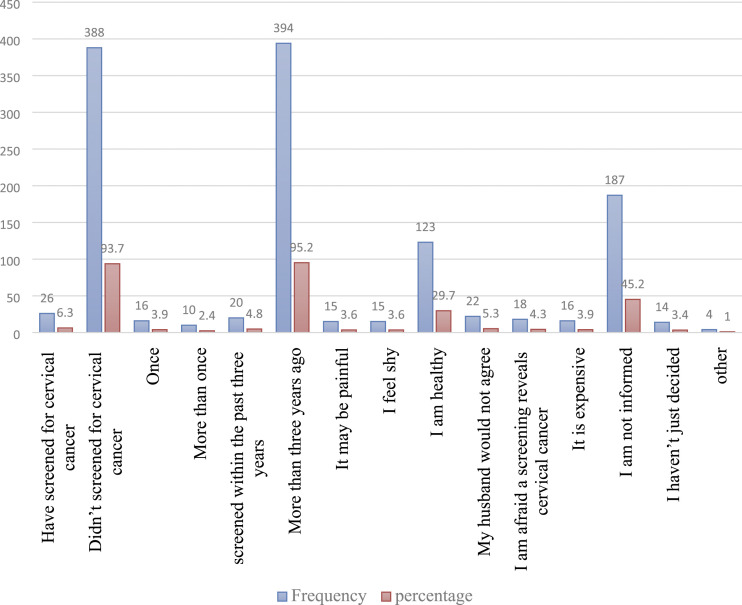
Practice Toward Cervical Cancer Screening
Only 6.3% of respondents have been screened for cervical cancer at least once before the survey day (Figure 2). Among those who have been screened, 3.9% stated that they have been screened once since they become sexually active and 95.2% have undergone their last screening before 3 years. For those who have not been screened, the most commonly reported reasons were lack of information for the procedure and thinking they were healthy (Figures 3 and 4).
Figure 3.
Percentages of practice cervical cancer screening of women attending health facilities in Ambo town 2020.
Figure 4.
Cervical cancer screening practice among women attending family planning clinic in Ambo town public health facilities 2020.
Factors Associated With the Knowledge, Attitude, and Practice of Cervical Cancer Screening
Bivariate logistic regression analysis was done for each impendent variable. Those variables with P-value < .25 in bivariate analysis and those variables with no collinearity were entered into multivariate regression analysis.
The result from multiple logistic regression showed that women who had primary education were around 8 times more likely to have good knowledge of cervical cancer screening than those who had no formal education (AOR: 7.94, 95% CI: 3.698, 26.71). The odds of having good knowledge of cervical cancer screening was 3.32-fold higher among women who attended secondary education compared to those who had no formal education (AOR: 3.32, 95% CI: 1.5, 7.33). The odds of having good knowledge of cervical cancer screening was 2.22-fold higher among women who attended diploma and above education compared to those who had no formal education (AOR: 2.22, 95% CI: 1.32, 6.157). The odds of good knowledge of cervical cancer was 2.26-fold higher among women who negatively responded about the early curability of cervical cancer compared to their counterparts (AOR: 2.26, 95% CI: 1.46, 7.28). Women who did not know about the early curability of cervical cancer had good knowledge of cervical cancer (AOR: 6.23, 95% CI: 6.23 (2.77, 15.13). Women who attended high school education were 51% less likely to have a negative attitude toward cervical cancer than those who had no formal education (AOR: 0.49, 95% CI: 0.26, 0.95). Women who had diploma and above educational status were 63% less likely to have negative attitude toward cervical cancer than their counterparts (AOR: 0.37, 95% CI: 0.19, 0.74). Women who had multiple sexual partners were 82% less likely to have a negative attitude toward cervical cancer than those who had a single sexual partner (AOR: 0.18, 95% CI: 0.05, 0.62). The odds of screening for cervical cancer was 2.37-fold higher among women who had positive attitude compared to their counterparts (AOR: 2.37, 95% CI: 1.91, 6.20) (Table 3).
Table 3.
Factors Associated With Knowledge, Attitude, and Practice of Cervical Cancer Screening, Among Women Attending Public Health Facilities in Ambo Town, Central Ethiopia Ambo, 2020.
| Variables | Knowledge of Cervical Cancer Screening | COR (CI = 95%) | AOR (CI = 95%) | |
| Poor Knowledge | Good Knowledge | |||
| Education level | ||||
| No education | 17 | 37 | 1 | 1 |
| Primary (1-8) | 51 | 70 | 9.90 (4.44, 21.82) | 7.94 (3.70, 26.71) |
| Secondary (9-12) | 67 | 71 | 3.73 (1.87, 7.45) | 3.32 (1.50, 7.33) |
| Diploma and above | 69 | 32 | 2.86 (1.44, 5.69) | 2.22 (1.32, 6.18) |
| Can cervical cancers cure at early stage | ||||
| Yes | 78 | 30 | 1 | 1 |
| No | 94 | 100 | 2.77 (1.67, 4.59) | 2.26 (1.46, 7.28) |
| Don’t know | 32 | 80 | 6.50 (3.61,11.70) | 6.23 (2.767, 15.13) |
| Attitude of cervical cancer screening | ||||
| Poor attitude | Positive attitude | |||
| Education level | ||||
| No formal education | 21 | 33 | 1 | 1 |
| Elementary | 64 | 57 | 0.57 (0.30, 1.09) | 0.52 (0.27, 1.02) |
| High school | 76 | 62 | 0.52 (0.27, .99) | 0.49 (0.26,0.95) |
| Diploma and above | 62 | 39 | 0.40 (0.20, 0.79) | 0.37 (0.19,0.74) |
| Number of sexual partners | ||||
| Single | 206 | 188 | 1 | |
| Multiple | 17 | 3 | 0.19 (0.06,0.9.67) | 0.18 (0.05,0.62) |
| Practice toward cervical cancer screening | ||||
| Good | Poor | |||
| Attitude score | ||||
| Poor Attitude | 18 | 205 | 1 | 1 |
| Positive Attitude | 8 | 183 | 2.01 (0.85, 4.73) | 2.37 (1.91, 6.20) |
Discussion
In the current study, 50.7% have good knowledge about cervical cancer screening. This finding comparable with studies conducted in Hossaina, 18 Wolaita Zone, and Ethiopia. 21 It is somewhat higher than studies from North West, Ethiopia, 25 Gabon, 26 and Tanzania. 27 This difference can be due to participants’ lack of information during the reception of different reproductive health services including family planning service and the variation in study setting.
Nearly two-thirds, (68.8%) have heard about cervical cancer. This result is lower than finding from Tanzania 28 and Yemen 29 where 83.1% and 80.6% heard about cervical cancer, respectively. This discrepancy can be due to low awareness creation level, variation in sample size, and educational interventional strategies between the study areas.
Near to half, 47.3% of women thought that cervical cancer could be treated by chemical therapy as one of the most common treatment options. This is, in contrast, to studies in Yemen 29 and Tanzania where the respondents which indicated that surgical (35.6%) and Radiotherapy (70.8%) 28 as a treatment option for cervical cancer.
About 46.1% of the study participants had good attitude toward cervical cancer screening. This finding is higher compared to the results from Hossaina, 34.8%, 11 and Wolaita, 45.5%, 21 of the participants who had favorable attitudes regarding cervical cancer screening. The extent of information supplied on the necessity of cervical cancer screening, which plays a critical role in increasing respondents’ health-seeking behavior, might be one reason for the disparities.
Only 6.3% of the respondents have been screened for cervical cancer before the survey. The finding was lower than a study conducted in Hossaina, 9.9%; 11 Wolaita,77.1%; 21 and Tanzania,14.3%. 28 This disparity might be attributed to variations in the research environment and the respondents’ socio-demographic variables.
The respondents’ educational status was significantly associated with their knowledge of cervical cancer screening. This finding is in line with studies conducted in Addis Ababa, 30 Hossaina, 11 Wolaita, 21 Tanzania, 28 and Bhopal 23 . This might be because educated individuals read more, follow health experts’ recommendations, and learn more about their health issues, such as cervical cancer.
Furthermore, compared to their peers, individuals who responded negatively and did not know about the early curability of cervical cancer were more likely to have inadequate awareness of cervical cancer screening. The finding contradicts previous research from Gondar 31 and Adama 32 towns that found no significant link. The disparity is attributable to variations in the study populations as well as disparities in socio-demographic variables.
A positive attitude was found to be associated with the practice of cervical cancer screening. This finding differs from the findings of the Wolaita, 21 Hossaina, 11 and Tanzania 28 where attitude did not show an association with cervical cancer screening practice. This is due to differences in the respondents’ socio-economic and demographic factors. This study further indicated that formal education is significantly associated with attitudes toward cervical cancer screening. This result is similar to studies from Wolaita zone, 21 India (48), and Nepal 33 where Education was significantly associated with attitude regarding cervical cancer screening. This could be due to the fact that educated people are more confident that makes them develop a positive attitude toward their health-seeking behavior.
The finding from this study showed that those participants who have a history of multiple sexual partners were more likely to have a positive attitude toward cervical cancer screening. A number of studies have addressed the association between having multiple sexual partners and the risk of getting cervical cancer. The lifetime number of sexual partners is significantly associated with a risk chance of acquiring cervical cancer. 34 Research conducted in Turkey regarding the risk factors for cervical cancer among women in the reproductive age group implied that having multiple sexual partners was less likely associated with cervical cancer. 35 This is because those who have multiple sexual partners suspect themselves of STIs, cervical cancer and develop a positive attitude toward cervical cancer screening.
The finding from this study also indicated that women who have multiple lifetime sexual partners have positive attitudes compared to their counterparts. But this finding is not similar to a study conducted in Adama. 32 The variance is attributable to variations in the study populations as well as differences in the respondents’ socio-demographic variables. This study revealed that those women who have a positive attitude were more likely to undergo the screening practice toward cervical cancer. A similar result was shown by the finding from Adama women with positive attitudes were more likely to go for cervical cancer screening. 32 This is could be due those who have positive attitude may also have good knowledge, accept counseling of health professionals, and implement screening practice.
Limitation the Study
This is a cross-sectional study; hence, it is not possible to differentiate cause and effect between dependent and independent variables. Lack of qualitative study which helps in assessing the in-depth unforeseen information is also the limitation of this study.
Conclusion
The results of this study indicated that cervical cancer screening knowledge and attitudes were moderate, but practice was low. This indicates the existing gap that needs more education so as to connect knowledge with attitude as well as to uplift the regular practice of cervical cancer screening for eligible women. Factors like educational level and beliefs related to the early curability of cervical cancer were significantly associated with knowledge. Having multiple lifetime sexual partners and educational status showed significant association with Attitude regarding cervical cancer whereas having a positive attitude about cervical cancer was associated with practice toward cervical cancer screening practice. Health education and awareness creation regarding cervical cancer should be created and implemented at public health facilities. Moreover, there is a need to disseminate cervical cancer screening information and offer cervical cancer treatment during health-care appointments.
Acknowledgments
The authors acknowledge the Rift valley University Department of Public health, all health facilities from where data were collected, data collectors, supervisors, and study participants for their nice cooperation.
Appendix
Abbreviations and acronyms
- HIV
Human Immune virus
- HPV
Human papillomavirus
- STI
Sexually transmitted infection
- SPSS
Statistical package for social science
- VIA
Visual inspection of cervix with acetic acid.
Footnotes
Authors Contributions: Tulu Gebisa, Elias Teferi Bala, and Berhanu Senbeta Deriba contributed significantly to substantial to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Moreover, they participated in drafting the work or revising it critically for important intellectual content.
Tulu Gebisa, Elias Teferi Bala, and Berhanu Senbeta Deriba approved the final version to be published. They agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval and Consent to Participate: This study was conducted in accordance with the Declaration of Helsinki. The study protocol and methodology was approved by the Ethical Review Committee of Rift Valley University. Permission to collect data was obtained from managements of health facilities. Written consent was obtained from every study participant after explaining the objective and purpose of the study. Privacy and confidentiality of the respondents were also strictly maintained. Health education on the importance of cervical cancer screening was given to all respondents.
Data sharing Statement: The data supporting this study cannot publicly available at present time. It will be made available from the corresponding author on a reasonable request.
ORCID iD
Berhanu Senbeta Deriba https://orcid.org/0000-0002-4282-1427
References
- 1.Santesso N, Mustafa RA, Schünemann HJ, et al. World Health Organization Guidelines for treatment of cervical intraepithelial neoplasia 2–3 and screen‐and‐treat strategies to prevent cervical cancer. Int J Gynecol Obstet. 2016;132(3):252-258. [DOI] [PubMed] [Google Scholar]
- 2.Onah OT, Unamba B, Anyaogu C, et al. Evaluation of diets served to cancer patients in oncology ward of university of Nigeria teaching hospital, Ituku/Ozalla, Enugu State. Pakistan J Nutr. 2016;15(2):104. [Google Scholar]
- 3.Mailhot Vega RB, Balogun OD, Ishaq OF, Bray F, Ginsburg O, Formenti SC. Estimating child mortality associated with maternal mortality from breast and cervical cancer. Cancer. 2019;125(1):109-117. [DOI] [PubMed] [Google Scholar]
- 4.Teka B, Gizaw M, Ruddies F, et al. Population‐based human papillomavirus infection and genotype distribution among women in rural areas of South Central Ethiopia. Int J Cancer. 2021;148(3):723-730. [DOI] [PubMed] [Google Scholar]
- 5.Koh W-J, Abu-Rustum NR, Bean S, et al. Cervical cancer, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2019;17(1):64-84. [DOI] [PubMed] [Google Scholar]
- 6.Simms KT, Steinberg J, Caruana M, et al. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020–99: a modelling study. Lancet Oncol. 2019;20(3):394-407. [DOI] [PubMed] [Google Scholar]
- 7.Vora C, Gupta S. Targeted therapy in cervical cancer. Esmo Open. 2019;3(Suppl 1):e000462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arbyn M, Gultekin M, Morice P, et al. The European response to the WHO call to eliminate cervical cancer as a public health problem. Int J Cancer. 2020;148(2):277-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santesso N, Schünemann H, Blumenthal P, et al. World Health Organization Guidelines: Use of cryotherapy for cervical intraepithelial neoplasia. Int J Gynecol Obstet. 2012;118(2):97-102. [DOI] [PubMed] [Google Scholar]
- 10.Döbrőssy L, Kovács A, Budai A. Inequalities in cervical screening practices. Orv Hetil. 2015;156(24):955-963. [DOI] [PubMed] [Google Scholar]
- 11.Aweke YH, Ayanto SY, Ersado TL. Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: Community-based cross-sectional study. PLoS One. 2017;12(7):e0181415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Draft W. Global Strategy Towards Eliminating Cervical Cancer as a Public Health Problem. Geneva, Switzerland: WHO; 2019. [Google Scholar]
- 13.Asseffa NA. Cervical cancer: Ethiopia’s outlook. J Gynecol Womens Health. 2017;5(2):555660. [Google Scholar]
- 14.Ntekim A. Cervical cancer in sub Sahara Africa. Topics on cervical cancer with an advocacy for prevention. 2012;4:54-59. [Google Scholar]
- 15.Black E, Richmond R. Prevention of cervical cancer in Sub-Saharan Africa: The advantages and challenges of HPV vaccination. Vaccines. 2018;6(3):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tarekegn AA, Mengistu MY, Mirach TH. Health professionals’ willingness to pay and associated factors for cervical cancer screening program at College of Medicine and Health Sciences, University of Gondar, Northwest Ethiopia. PLoS One. 2019;14(4):e0215904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Segni MT, Demissie HF, Tadesse DM, Amdemichael R, Mamo YT, Worku A. Level of knowledge and associated factor toward cervical cancer among women age (21-64) years visiting health facilities in gulele sub-city addis Ababa Ethiopia. J Pancreas. 2017;18(1):44-48. [Google Scholar]
- 18.Gebreegziabher M, Asefa NG, Berhe S. Factors affecting the practices of cervical cancer screening among female nurses at Public Health Institutions in Mekelle Town, Northern Ethiopia, 2014: A Cross-Sectional Study. J Cancer Res. 2016;2016(2):1-7. [Google Scholar]
- 19.Deriba BS, Bulto GA, Bala ET. Nutritional-related predictors of anemia among pregnant women attending antenatal care in central Ethiopia: An unmatched case-control study. BioMed Research International. 2020;2020:8824291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Office of Ambo town Health office Health Management Information System Annual Report of June 2020. Unpublished; 2020:890-912.
- 21.Tekle T, Wolka E, Nega B, Kumma WP, Koyira MM. Knowledge, attitude and practice towards cervical cancer screening among women and associated factors in hospitals of wolaita zone, Southern Ethiopia. Cancer Manag Res. 2020;12:993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tadesse A. Knowledge, Attitude and Practice towards Screening for Cervical Cancer Among Adama University Female Students. Ethiopia: Adama; 2014. [Google Scholar]
- 23.Bansal AB, Pakhare AP, Kapoor N, Mehrotra R, Kokane AM. Knowledge, attitude, and practices related to cervical cancer among adult women: A hospital-based cross-sectional study. J Nat Sci Biol Med. 2015;6(2):324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sperandei S. Understanding logistic regression analysis. Biochem Med: Biochem Med. 2014;24(1):12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Getahun F, Mazengia F, Abuhay M, Birhanu Z. Comprehensive knowledge about cervical cancer is low among women in Northwest Ethiopia. BMC Cancer. 2013;13(1):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Islam JY, Khatun F, Alam A, et al. Knowledge of cervical cancer and HPV vaccine in Bangladeshi women: A population based, cross-sectional study. BMC Women's Health. 2018;18(1):1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lyimo FS, Beran TN. Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: Three public policy implications. BMC Public Health. 2012;12(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mabelele MM, Materu J, Ng’ida FD, Mahande MJ. Knowledge towards cervical cancer prevention and screening practices among women who attended reproductive and child health clinic at Magu district hospital, Lake Zone Tanzania: A cross-sectional study. BMC Cancer. 2018;18(1):565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abdul-Aziz M. Knowledge, attitude and practice towards cervical cancer among reproductive health clients at the University of Science & Technology Hospital-Sana’a in Yemen. Yemeni Journal for Medical Sciences. 2012;6. [Google Scholar]
- 30.Shiferaw S, Addissie A, Gizaw M, et al. Knowledge about cervical cancer and barriers toward cervical cancer screening among HIV‐positive women attending public health centers in Addis Ababa city, Ethiopia. Cancer medicine. 2018;7(3):903-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mengesha A, Messele A, Beletew B. Knowledge and attitude towards cervical cancer among reproductive age group women in Gondar town, North West Ethiopia. BMC Publ Health. 2020;20(1):209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kassa R, Gurmessa T, Lemma T, Abebe W. Cervical cancer and screening method: Knowledge, attitude and practice among women living in adama town. J Women's Health Care. 2019;8(458):2167. [Google Scholar]
- 33.Thapa N, Maharjan M, Petrini MA, et al. Knowledge, attitude, practice and barriers of cervical cancer screening among women living in mid-western rural, Nepal. Journal of gynecologic oncology. 2018;29(4):e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cancer ICoESoC . Cervical carcinoma and sexual behavior: Collaborative reanalysis of individual data on 15,461 women with cervical carcinoma and 29,164 women without cervical carcinoma from 21 epidemiological studies. Cancer Epidemiol Biomark Prev. 2009;18(4):1060. [DOI] [PubMed] [Google Scholar]
- 35.Sogukpinar N, Saydam BK, Can HO, et al. Assessment of cervical cancer risk in women between 15 and 49 years of age: case of Izmir. Asian Pac J Cancer Prev APJCP. 2013;14(3):2119-2125. [DOI] [PubMed] [Google Scholar]