Abstract
Background:
Functional abdominal pain (FAP) is a common complaint causing several referrals to pediatricians. On the other hand, the most common presentation of hyperuricosuria and also hypercalciuria is chronic/recurrent abdominal pain. Therefore, a hypothesis has been raised; abdominal pain due to hyperuricosuria and/or hypercalciuria may be misdiagnosed as FAP. The current study has aimed to respond to this theory.
Materials and Methods:
This is a case–control study conducted on children diagnosed with FAP based on Rome IV criteria and age-matched normal controls. Blood and random urine samples were taken from healthy children and those with FAP. Random urine samples were examined for calcium, uric acid, oxalate, and creatinine concentrations. Random urine calcium to urine creatinine above 0.2 mg/mg was considered hypercalciuria and random urine uric acid above 0.56 mg/dl, GFR as hyperuricosuria. The data were analyzed using logistic models.
Results:
Hypercalciuric children had a significantly lower chance of FAP (odds ratio [OR] =0.425, 95% confidence interval [CI] =0.204–0.886). Although an inverse association was seen between hyperuricosuria and FAP (OR = 0.693, 95% CI = 0.395–1.214), it was not statistically significant. In stratified analyses by gender for both hyperuricosuria and hypercalciuria, a marginal inverse significant association was seen in male gender (P < 0.1).
Conclusion:
Our study showed that hypercalciuria is significantly in inverse association with FAP but not hyperuricosuria. Therefore, these disorders, particularly hyperuricosuria may not be considered as the possible causes of FAP. Further studies with larger sample size for providing more reliable evidence are recommended.
Keywords: Abdominal pain, children, functional abdominal pain, hypercalciuria, hyperuricosuria, Rome IV
INTRODUCTION
Functional abdominal pain (FAP) is a common complaint which accounts for 0.3%–19% of prevalence among school-aged[1] and <12% among younger than 6-year-old children.[2] In almost 90% of these children, no explanatory organic cause can be identified.[3]
This disorder causes several referrals to pediatricians. A pediatrician from Britain in the early 1900s said: “I know of no symptom which can be more obscure in its causation than colicky abdominal pain in childhood”.[4] Nowadays, this clinical issue is still a great challenge for researchers and pediatricians after more than a century. This lack of obvious etiologic diagnosis for the abdominal pains of children results in several clinical referrals, extensive investigations, excessive costs for diagnostic modalities, noneffective treatments, poor satisfaction, and a significant burden on the health-care system.[5]
Chronic or recurrent abdominal pain, recently known as FAP based on Rome IV diagnostic criteria, affects 8%–25% of children.[6,7] It is responsible for 2%–4% of pediatric clinic referrals[8] and is estimated to occur in 10%–20% of school-aged children and even up to 15% of adolescents.[9]
Based on Rome IV diagnostic criteria, FAP is defined as continuous or episodic abdominal pain without any clue to metabolic, inflammatory, and/or neoplastic etiologies. This pain should be present 25% of the time and be accompanied by one or more of the following symptoms: daily activity limitation and other somatic symptoms such as headache, limb pain, and sleep disturbances.[10]
Hypercalciuria is a common condition occurring in 9% of children. This condition, which is not necessarily accompanied by the higher incidence rate of nephrolithiasis, might be responsible for FAP.[11] It is reported that up to 41% of children with hypercalciuria present recurrent and chronic abdominal pain episodes; therefore, it is hypothesized that hypercalciuria might be one of the underlying factors of FAP.[12]
Hyperuricosuria is another dysfunction that might occur with or without hypercalciuria. It is accompanied by various clinical manifestations, including nephrolithiasis and hematuria, flank, and abdominal pain.[13] As children aged <5 years may present flank pain as abdominal pain, it is suggested that hyperuricosuria might have a role in FAP.[14]
Based on an extensive search in the literature, we found scare studies with small size and controversial findings on the role of hyperuricosuria and hypercalciuria in FAP.[15,16] Therefore, considering the inconsistency in the findings, the current study aimed at determining the association of hypercalciuria and hyperuricosuria with FAP.
METHODS
Study design and setting
This case–control study was conducted from January 2016 to April 2018 on 200 children referred to clinics of training hospitals of Imam Hossein and Amin, affiliated to Isfahan University of Medical Sciences, Isfahan, Iran. Considering type one error rate 5%, statistical power 80%, and odds ratio (OR) =0.43 for the association of hyperuricosuria and/or hypercalciuria with FAP, the total sample size was calculated to be 193. We entered 100 samples per group (a total of 200 samples) in the study.
Inclusion and exclusion criteria
Those children who met the Rome IV criteria for FAP diagnosis[17] with normal reports of the laboratory tests and ultrasonography were included in this study according to the diagnosis of a pediatric gastroenterologist. The following laboratory tests were assessed for all of included children: complete blood count and differentiation, erythrocyte sedimentation rate, aspartate aminotransferase (AST), alanine aminotransferase, amylase, lipase, anti-tissue transglutaminase antibody (anti-TTG antibody) (IgA), total IgA, stool examination, urine analysis, and urine culture.
The exclusion criteria consisted of any abnormal laboratory findings, presence of any organic etiology including inflammatory, metabolic and neoplastic reasons for abdominal pain, and use of any medication affecting calcium and uric acid excretion.
Procedure and assessment of variables
Overall, 100 children with a possible diagnosis of FAP were included by convenient sampling, and an equal number of age-matched controls were recruited from the same clinics among those children referred for complaints other than abdominal pain. They underwent a physical examination and laboratory tests similar to the case group. All of the patients underwent abdominopelvic ultrasonography by an expert radiologist to reduce the interobserver bias.
Blood and random urine samples were obtained from members of both groups. All laboratory tests were performed in the same laboratory, using quantitative Pars Azmun kits (http://www.irancode.ir/Home/PersonalPage?MemberCode=18514andgProduct-orderBy=CombaseName-descandgProduct-page=3). Random urine samples were examined for calcium, uric acid, oxalate, and creatinine concentrations.
Random urine calcium to urine creatinine above 0.2 mg/mg was considered as hypercalciuria.[18]
Above 0.56 mg/dl GFR was defined as hyperuricosuria based on the following formula;[19,20]
Besides, the age (year) and the gender of the participants were recorded.
Ethical considerations
The study protocol was approved by the Isfahan University of Medical Sciences Ethics Committee (Ethics Committee approval number: IR.MUI.REC.1396.3.796). Thus study protocol was explained for cases’ and control’ legal guardians. They all were reassured about the confidentiality of obtained information and requested to sign the informed consent form to participate in the study.
Statistical analyses
Data were presented as mean (standard deviation [SD]) and frequency (%) for numeric and categorical variables. Chi-square and Student's t-test conducted comparisons of variables between the case and control groups for categorical and numeric variables, respectively. Normality of continuous data was evaluated using Kolmogorov–Smirnov test and Q-Q plot. Association between hyperuricosuria and hypercalciuria with FAP was evaluated using binary logistic regression in total sample and separately in boys and girls. Results of logistic regression were reported as ORs and their 95% confidence intervals (CIs) for OR. Data were analyzed by IBM SPSS Statistics (version 20, IBM SPSS Statistics, Armonk, NY, USA). A P < 0.05 was considered statistically significant.
RESULTS
In the first step, we assessed a total of 300 participants. There were 100 dropouts (74 of them did not meet the inclusion criteria, and 36 were unwilling to attend the study). Afterward, 100 participants in each group were assessed for risk factors, and there was no missing information in this step. Finally, data were analyzed on 100 cases and 100 controls [STORBE diagram; Figure 1].
Figure 1.
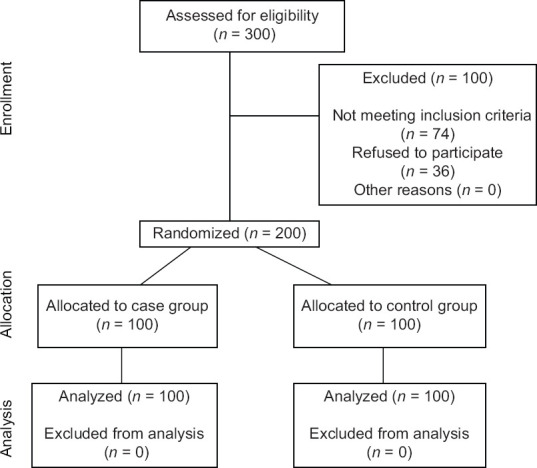
STROBE diagram of participants’ recruitment in case–control study
The man (SD) age of study participants was not significantly different between cases (8 [2.99] years) and controls (7.65 [2.77] years) (P = 0.399). However, a significant difference was observed in terms of gender distribution between cases (17% boys) and control (25% boys) (P = 0.022).
Mean value of urine calcium and hypercalciuria distribution was significantly higher in controls than in cases (26% vs. 13%, P = 0.020). However, the distribution of hyperuricosuria was not significantly different between controls and cases (48.0% vs. 39%, P = 0.199).
However, there were no significant differences between cases and controls in uric acid, urine creatinine, and plasma creatinine (all P > 0.05) [Table 1].
Table 1.
Basic demographic and clinical characteristics of study participants
| Variables | Variable | ||
|---|---|---|---|
|
| |||
| Case | Control | P | |
| Sex: Boys (%) | 50 (25.0) | 34 (17.0) | 0.022 |
| Age | 7.7 (2.7) | 8.0 (3.0) | 0.399 |
| Hypercalciuria (%) | 26 (13.0) | 13 (6.5) | 0.020 |
| Hyperuricosuria (%) | 48 (24.0) | 39 (19.5) | 0.199 |
| Urine calcium | 0.12 (0.10) | 0.17 (0.18) | 0.010 |
| Uric acid | 0.49 (0.22) | 0.58 (0.44) | 0.081 |
| Plasma creatinine | 0.63 (0.10) | 0.61 (0.10) | 0.094 |
| Urine creatinine | 71.8 (49.1) | 84.0 (53.2) | 0.476 |
Continuous and categorical data were reported as mean (SD) and frequency (%). P values resulted from independent samples t-test for continuous and Chi-squared test for categorical data, respectively. SD=Standard deviation
Table 2 presents the results of logistic regression in total sample and separately in both gender for the association of hypercalciuric and hyperuricosuria with FAP. Hypercalciuric children had a significantly lower risk of FAP (OR = 0.425, 95% CI = 0.204–0.886). Although an inverse association was seen between hyperuricosuria and FAP (OR = 0.693, 95% CI = 0.395–1.214), however, it was not statistically significant. In stratified analyses by gender for both hyperuricosuria and hypercalciuria, a marginal inverse significant association was seen in male gender (P < 0.1).
Table 2.
Logistic regression results for the association of hyperuricosuria and hypercalciuria with functional abdominal pain
| Variables | Total sample | Boy | Girl | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| OR | Lowe-upper CI for OR | P | OR | Lower-upper CI for OR | P | OR | Lower-upper CI for OR | P | |
| Hypercalciuria | 0.425 | 0.204-0.888 | 0.022 | 0.275 | 0.072-1.055 | 0.060 | 0.508 | 0.202-1.279 | 0.151 |
| Hyperuricosuria | 0.693 | 0.395-1.214 | 0.20 | 0.441 | 0.178-1.904 | 0.078 | 0.938 | 0.447-1.969 | 0.865 |
OR=Odds ratio; CI=Confidence interval
DISCUSSION
Based on the findings of our case–control study, the distribution of hypercalciuria was significantly higher in controls than in cases, no statistical difference was found in terms of hyperuricosuria between cases and controls.
The hypothesis about the role of idiopathic hypercalciuria/hyperuricosuria on FAP was raised based on the findings of cross-sectional studies assessing idiopathic hypercalciuria/hyperuricosuria that found recurrent/chronic abdominal pain as the most common symptom among children presenting idiopathic hypercalciuria/hyperuricosuria.[12,13,14,15,16,17,18,19,20,21,22]
Further evaluations in these studies showed that abdominal pain among these children might be present without manifestation of urolithiasis.[12,13] On the other hand, as young children, aged under five, might present their flank pain as abdominal pain,[23] this hypothesis about the potential role of hypercalciuria/hyperuricosuria on FAP was underscored.
Various studies showed that hypercalciuria and hyperuricosuria might lead to urolithiasis, which can cause significant abdominal pain and more probability, flank pain.[12,13,14,15,16,17,18,19,20,21,22,23,24] Therefore hypercalciuria and hyperuricosuria were suggested as the underlying etiologies of recurrent and/or chronic abdominal pain. Following mentioned hypothesis, Polito et al. performed a study on the association of urolithiasis with recurrent abdominal pain. Consistent with other studies, they found that imaging may not present urolithiasis at episodes of pain. Therefore, the probability of abdominal pain due to urolithiasis should not be underestimated.[25] It should be acknowledged that hypercalciuric and/or hyperuricosuric children without manifestations of urolithiasis during first imaging assessments may present calculi after 1 to 4 years in further evaluations.[24,25,26]
Limited comparative studies have assessed this association, and most previous studies have just presented the probable role of this association. In contrast, the study of Polito et al. assessed the role of hypercalciuria in recurrent abdominal pain in childhood. In their cross-sectional study, they gathered data of 46 over 3-year-old patients and defined hypercalciuria. They also included 37 normal cases and compared the hypercalciuric state of the two groups. There presented no association between hypercalciuria and recurrent abdominal pain.[27]
Furthermore, in the study of Polito et al.,[19] they did not find a significant association between hypercalciuria and FAP in children.
Another study by Polito investigated appendectomy among children with hypercalciuria/hyperuricosuria. It represented a remarkably higher appendectomy rate among children with hypercalciuria/hyperuricosuria than the control children with normal ranges of calcium and urea urinary excretion. Further investigations showed that the patients’ recurrent abdominal pain was preserved following appendectomy; by a-year therapeutic approaches for hypercalciuria/hyperuricosuria, abdominal pain improved dramatically.[23]
Leslie was another scientist who represented a direct correlation between hypercalciuria and recurrent abdominal pain in children; however, they may not necessarily represent the symptoms of nephrolithiasis or have abnormal urine analysis or ultrasonography.[18]
Study limitations and strengths
The main limitations of our study are the small number of participants studied, without long-term follow-ups. Furthermore, choosing a sample of children referred to clinics of training hospitals of Imam Hossein and Amin restricts the generalizability of the findings to other settings. Future directions are recommended to study a variety of settings for more external validity. The strengths of our study are the novelty in the pediatric age group and conducting complete laboratory and sonographic evaluations for participants. This study is among a limited number of studies assessing the probable role of hypercalciuria/hyperuricosuria on recurrent/chronic abdominal pain among children presenting with FAP. We recommend further studies by considering the probable confounding variables affecting calcium and urea excretion status, such as routine daily regimen. Besides, a longer duration of follow-up is required to provide a more thorough view of hypercalciuria/hyperuricosuria in FAP.
CONCLUSION
Our study showed that hypercalciuria is significantly in inverse association with FAP but not hyperuricosuria. Therefore, these disorders particularly hyperuricosuria may not be considered as the possible causes of FAP. Further studies with larger sample size for providing more reliable evidence are recommended.
Ethics approval and consent to participate
The Institutional Review Board (IRB) of Isfahan University of Medical Sciences approved the study's protocol. Informed consent was obtained from all participants.
Financial support and sponsorship
This study was funded by vice-chancellor for research and technology of Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Imam Hossein and Amin Hospitals of Isfahan University of Medical Sciences’ research deputy for supporting this study.
REFERENCES
- 1.Chitkara DK, Rawat DJ, Talley NJ. The epidemiology of childhood recurrent abdominal pain in Western countries: A systematic review. Am J Gastroenterol. 2005;100:1868–75. doi: 10.1111/j.1572-0241.2005.41893.x. [DOI] [PubMed] [Google Scholar]
- 2.Ramchandani PG, Hotopf M, Sandhu B, Stein A ALSPAC Study Team. The epidemiology of recurrent abdominal pain from 2 to 6 years of age: Results of a large, population-based study. Pediatrics. 2005;116:46–50. doi: 10.1542/peds.2004-1854. [DOI] [PubMed] [Google Scholar]
- 3.Spee LA, Lisman-Van Leeuwen Y, Benninga MA, Bierma-Zeinstra SM, Berger MY. Prevalence, characteristics, and management of childhood functional abdominal pain in general practice. Scand J Prim Health Care. 2013;31:197–202. doi: 10.3109/02813432.2013.844405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korterink J, Devanarayana NM, Rajindrajith S, Vlieger A, Benninga MA. Childhood functional abdominal pain: Mechanisms and management. Nat Rev Gastroenterol Hepatol. 2015;12:159–71. doi: 10.1038/nrgastro.2015.21. [DOI] [PubMed] [Google Scholar]
- 5.Devanarayana NM, Rajindrajith S, Benninga MA. Quality of life and health care consultation in 13 to 18 year olds with abdominal pain predominant functional gastrointestinal diseases. BMC Gastroenterol. 2014;14:150. doi: 10.1186/1471-230X-14-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saps M, Seshadri R, Sztainberg M, Schaffer G, Marshall BM, Di Lorenzo C. A prospective school-based study of abdominal pain and other common somatic complaints in children. J Pediatr. 2009;154:322–6. doi: 10.1016/j.jpeds.2008.09.047. [DOI] [PubMed] [Google Scholar]
- 7.Shelby GD, Shirkey KC, Sherman AL, Beck JE, Haman K, Shears AR, et al. Functional abdominal pain in childhood and long-term vulnerability to anxiety disorders. Pediatrics. 2013;132:475–82. doi: 10.1542/peds.2012-2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campo JV, Bridge J, Ehmann M, Altman S, Lucas A, Birmaher B, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004;113:817–24. doi: 10.1542/peds.113.4.817. [DOI] [PubMed] [Google Scholar]
- 9.Moreno MA, Furtner F, Rivara FP. Functional abdominal pain in children and adolescents. JAMA Pediatr. 2013;167:204. doi: 10.1001/jamapediatrics.2013.1665. [DOI] [PubMed] [Google Scholar]
- 10.Helgeland H, Flagstad G, Grøtta J, Vandvik PO, Kristensen H, Markestad T. Diagnosing pediatric functional abdominal pain in children (4-15 years old) according to the Rome III Criteria: Results from a Norwegian prospective study. J Pediatr Gastroenterol Nutr. 2009;49:309–15. doi: 10.1097/MPG.0b013e31818de3ab. [DOI] [PubMed] [Google Scholar]
- 11.Favus MJ, Zeytinoglu M, Coe FL. Chapter 81 - Idiopathic Hypercalciuria and Nephrolithiasis. In: Feldman D, editor. Vitamin D. Fourth Edition. Academic Press; 2018. pp. 485–05. [Google Scholar]
- 12.Vachvanichsanong P, Malagon M, Moore ES. Recurrent abdominal and flank pain in children with idiopathic hypercalciuria. Acta Paediatr. 2001;90:643–8. [PubMed] [Google Scholar]
- 13.Akl K, Ghawanmeh R. The clinical spectrum of idiopathic hyperuricosuria in children: Isolated and associated with hypercalciuria/hyperoxaluria. Saudi J Kidney Dis Transpl. 2012;23:979–84. doi: 10.4103/1319-2442.100879. [DOI] [PubMed] [Google Scholar]
- 14.Ranabothu S, Bernstein AP, Drzewiecki BA. Diagnosis and management of non-calcium-containing stones in the pediatric population. Int Urol Nephrol. 2018;50:1191–8. doi: 10.1007/s11255-018-1883-0. [DOI] [PubMed] [Google Scholar]
- 15.Malaki M. The role of hypercalciuria in pathogenesis of recurrent abdominal pain. Saudi J Kidney Dis Transpl. 2017;28:664–5. doi: 10.4103/1319-2442.206437. [DOI] [PubMed] [Google Scholar]
- 16.Marzuillo P, Guarino S, Apicella A, La Manna A, Polito C. Why we need a higher suspicion index of urolithiasis in children. J Pediatr Urol. 2017;13:164–71. doi: 10.1016/j.jpurol.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 17.Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Childhood functional gastrointestinal disorders: Child/adolescent. Gastroenterology. 2006;150:1527–37. doi: 10.1053/j.gastro.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leslie SW, Sajjad H. Treasure Island (FL); 2020: Hypercalciuria: StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 19.Kruse K, Kracht U, Kruse U. Reference values for urinary calcium excretion and screening for hypercalciuria in children and adolescents. Eur J Pediatr. 1984;143:25–31. doi: 10.1007/BF00442743. [DOI] [PubMed] [Google Scholar]
- 20.Copelovitch L. Urolithiasis in children: Medical approach. Pediatr Clin North Am. 2012;59:881–96. doi: 10.1016/j.pcl.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demidenko E. Sample size determination for logistic regression revisited. Stat Med. 2007;26:3385–97. doi: 10.1002/sim.2771. [DOI] [PubMed] [Google Scholar]
- 22.Beiraghdar F, Panahi Y, Madani A, Jahani Y. Non calculus signs and symptoms of hyperoxaluria and hyperuricosuria in children: A single experience. Nephro-Urol Mon. 2009;1:137–42. [Google Scholar]
- 23.Polito C, Marte A, La Manna A. Appendectomy in children with hypercalciuria/hyperuricosuria. J Pediatr Urol. 2005;1:279–82. doi: 10.1016/j.jpurol.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 24.La Manna A, Polito C, Marte A, Iovene A, Di Toro R. Hyperuricosuria in children: Clinical presentation and natural history. Pediatrics. 2001;107:86–90. doi: 10.1542/peds.107.1.86. [DOI] [PubMed] [Google Scholar]
- 25.Polito C, Cioce F, Signoriello G, La Manna A. Central/diffuse abdominal perception of urological pain in children. Acta Paediatr. 2006;95:82–5. doi: 10.1080/08035250500325082. [DOI] [PubMed] [Google Scholar]
- 26.Polito C, La Manna A, Cioce F, Villani J, Nappi B, Di Toro R. Clinical presentation and natural course of idiopathic hypercalciuria in children. Pediatr Nephrol. 2000;15:211–4. doi: 10.1007/s004670000433. [DOI] [PubMed] [Google Scholar]
- 27.Polito C, La Manna A, Signoriello G, Marte A. Recurrent abdominal pain in childhood urolithiasis. Pediatrics. 2009;124:e1088–94. doi: 10.1542/peds.2009-0825. [DOI] [PubMed] [Google Scholar]


