Abstract
Gavin Yamey and colleagues say that a new, urgent push for global vaccine equity could help avert suffering and deaths, protect economies, and prevent new virus variants
During the covid-19 pandemic, we have seen the best of international collective action and its limits. Global scientific cooperation drove the development of safe, highly effective covid-19 vaccines in under one year.1 Yet we have also witnessed global vaccine inequity,2 in which low and middle income countries have “limited supply and limited vaccine brand options.”3
With the omicron wave dissipating, several well vaccinated high income nations with stockpiles of covid-19 vaccines are rushing to declare the pandemic over, reminding us of how things unfolded with tuberculosis, malaria, and HIV/AIDS in the past. But the pandemic is not over and 2.8 billion people remain completely unvaccinated. Now is the time to recommit to, and further invest in, equitable and effective country led vaccination campaigns.
In this paper, we briefly examine how global vaccine inequity arose, lay out a renewed case for urgently ramping up our commitment to vaccine equity, and propose principles to ensure no one is left behind in the quest to vaccinate the world.
What caused global vaccine inequity?
Vaccination coverage varies starkly by country income level. Although over 11 billion vaccine doses have been administered, nearly 70% of them benefited high and upper middle income countries.4 As of 19 March 2022, 79% of people in high income countries had received at least one dose of a covid-19 vaccine, compared with just 14% in low income countries.4 Primary vaccination and booster coverage have been highly regressive (fig 1).
Fig 1.
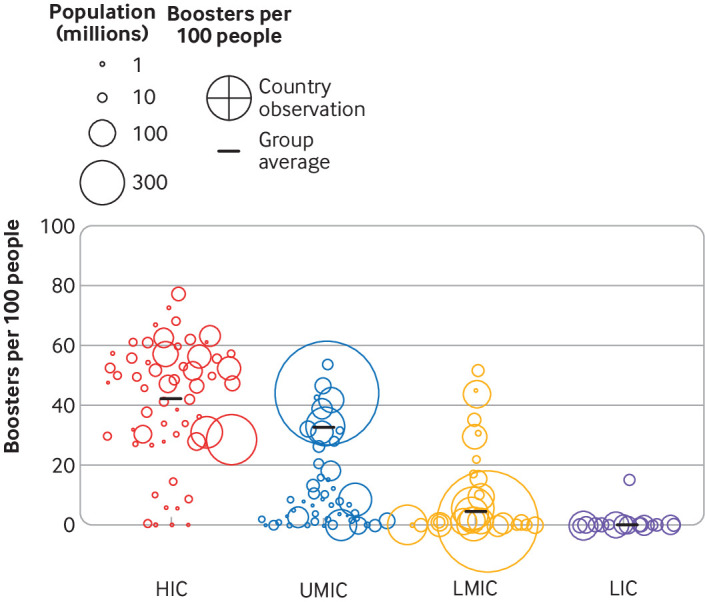
Booster coverage of total population, by income. Country observations (centre points) of boosters per 100 people by income group and total population size (area) with group averages (lines). HIC=high income countries; UMIC=upper middle income countries; LMIC=lower middle income countries; LIC=low income countries. Source: https://pandem-ic.com/booster-coverage-of-population-by-country-income-and-population-size/
What caused such inequity? We use Wouter and colleagues’ framework to briefly summarise inequitable access to covid-19 vaccines across four dimensions: vaccine production, allocation, affordability, and deployment.5
Vaccine production
High income countries quickly pre-ordered huge numbers of doses from companies such as BioNTech/Pfizer that overcame early manufacturing scale-up challenges relatively quickly.6 In contrast, low and middle income countries, as well as the Covid-19 Vaccines Global Access (Covax) facility that purchased doses for distribution in these countries (box 1), largely relied on initial purchases from Astra Zeneca, Janssen, and Novavax, which were slower to overcome manufacturing scale-up challenges.
Box 1. Covax.
The Covax facility was formally launched in June 2020, aiming to supply covid-19 vaccines to all countries worldwide. Covax hoped to be able to vaccinate all health workers, elderly people, and high risk populations in every country by the end of 2021, which would constitute about 20% of the global population.
Covax was “designed to stand on two legs.”7 The first was the self-financing leg: high income and upper middle income countries would buy doses through Covax for their own populations. Initially, they would be able to purchase enough doses to vaccinate 20% of their populations, though Covax later raised the ceiling to 50% to attract more high income and upper middle income country purchases. The incentive for these nations to buy doses from Covax, rather than only through bilateral deals with vaccine manufacturers, was as an insurance mechanism. If a high income country’s bilateral deals were unsuccessful (that is, the candidates failed in trials), the country would still have access to vaccine doses from the wide portfolio of around a dozen Covax candidates. The second leg was aimed at the 92 countries that are low income or lower middle income countries—doses for these nations would be paid for largely by donor funding through an advanced market commitment.
Covax hoped that a huge number of high and lower middle income countries would buy doses through the facility, which would have given Covax massive buying power to invest in research and development, fund manufacturing at risk, drive prices down through pooled purchases, and ensure that some of the supply would go to low income and lower middle income countries. However, in the end most high income and upper middle income nations largely bypassed Covax: “About 3 dozen rich nations ended up buying most of their doses by way of direct deals with vaccine companies rather than through the Covax pool.”8 Its supply projections were overly optimistic. It was not transparent about the contracts it made with companies and the prices it paid.7 Most high income and upper middle income nations that pledged to donate doses to Covax have not met their pledges. An independent review of Covax found “insufficient inclusion and meaningful engagement” of low and middle income countries and civil society in developing the mechanism.9 Nevertheless, Covax has to date delivered nearly 1.2 billion doses to the 92 nations participating in the Covax advanced market commitment.
Additionally, low and middle income countries did not have manufacturing capacities in place at the beginning of the pandemic, with notable exceptions (for example, China, Cuba, and India).10 While there has been some investment in vaccine manufacturing in low and middle income countries since the pandemic began—such as the US Development Finance Corporation investment in Biological E in India and the Carlos Slim Foundation’s investment in vaccine manufacturing in Mexico and Argentina—these take time to stand up manufacturing capabilities and cannot solve the immediate crisis. Vaccine companies and high income nations were reluctant to share vaccine patents and technology with vaccine manufacturers in less wealthy countries and with multilateral initiatives that aim to boost vaccine equity, though there has been some voluntary licensing to manufacturers in low and middle income countries.
Allocation
To try to ensure fair global vaccine allocation, Gavi, the Vaccine Alliance, the Coalition for Epidemic Preparedness, and the World Health Organization launched Covax, a “first-of-its kind ‘buyers pool’ in which richer nations can collectively purchase vaccines, fund vaccine development and manufacturing and ensure that some of the supply will go to poorer countries.”8 Covax also uses foreign aid to buy doses for distribution to 92 lower middle income and low income countries.
Covax has undoubtedly procured vaccines for people who would otherwise not have had access, but as an allocation mechanism it faced an array of challenges, some of its own making and others outside its control (box 1). High income and upper middle income nations largely bypassed Covax, buying huge numbers of doses directly from vaccine companies, and Covax struggled to raise necessary financing, leaving it at the back of the queue when it came to purchasing doses.8
The case of Latin America illustrates the allocation problems faced by low and middle income countries.11 Even with resources to buy vaccine doses, the lack of capacity for negotiations caused delays in vaccination (for example, Peru was able to start vaccinating only in March 2021). High public trust in vaccines has allowed the region to catch up,12 but the delays caused a huge number of deaths that could have been averted.
Affordability
The wide variation and lack of transparency in vaccine prices across countries and companies contributed to inequity.13 In 2021, when the European Union was paying $3.50 (£2.70; €3.20) per dose of the Oxford-AstraZeneca vaccine, South Africa was being charged $5.25 and Uganda was being charged $7. Many low and middle income countries had to take out loans to procure vaccines for their populations while high covid-19 vaccine prices have led to huge profits for industry.14 The lack of transparency around vaccine prices and terms of contracts, including indemnity, has been a barrier to countries being able to negotiate and buy vaccines even when resources were available—a problem that was particularly acute for Latin America.15
Deployment
Cross country differences in health systems, including vaccine supply chains, data infrastructure, and health workforce, contributed to global vaccine inequity. For example, many covid-19 vaccines need ultra-cold chains and expire quickly once removed from storage.5
Vaccine hesitancy also varied across countries.16 While vaccine uptake is high in many regions of low and middle income countries, complex social factors drive hesitancy for some communities. For example, “a history of colonial medical and vaccine research abuse in Africa diminishes trust in current vaccines.”17 Scarcity and unpredictability of vaccine supply also complicated building vaccine confidence.17 18 19
Renewed case for vaccine equity
Covid-19 vaccines are very safe and effective, particularly at reducing hospitalisation and death. Nations with high vaccine coverage have greatly weakened the link between cases and death. It is unjust that people in high income and upper middle income nations have been protected from illness, hospitalisation, and death while those in low and lower middle income countries are being left behind. While the global omicron surge led to large numbers of people worldwide getting infected and surviving, leaving them with a degree of immunity, infection induced immunity is not as robust and durable as being up to date with vaccination; nor does it provide the same protection against future variants.20 21 22 23 24
It is a myth to believe that high income countries have been harder hit by the pandemic and thus “deserve” to have hoarded the lion’s share of the vaccine supply. Figure 2 shows that estimates of excess deaths per capita have been substantial worldwide, with lower middle income countries—not high income countries—having the highest rates. In terms of share, low and middle income countries currently account for 63% of cumulative reported covid-19 mortality. When under-reporting and other factors are considered, excess mortality estimates suggest this share could be as high as 87%.25
Fig 2.
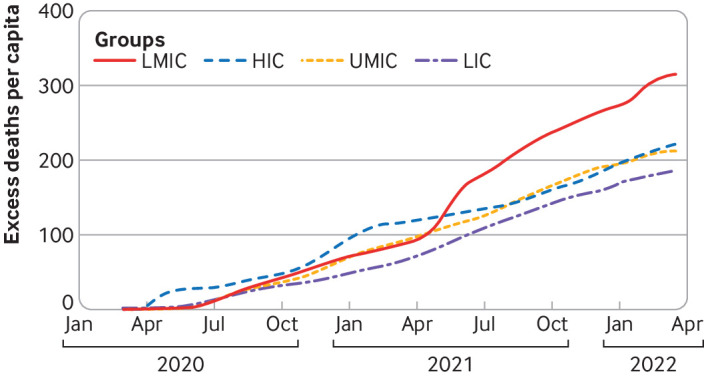
Cumulative estimated excess deaths since the start of the pandemic per 100 000 people. HIC=high income countries; UMIC=upper middle income countries; LMIC=lower middle income countries; LIC=low income countries. Mid-point estimates of excess death model by The Economist. Source: https://pandem-ic.com/cumulative-estimated-excess-deaths-per-capita-by-income/
Low and middle income countries also bear the highest burden of endemic infectious diseases, such as HIV and tuberculosis, and have had to redirect resources usually used to tackle these diseases towards covid-19 control. The pandemic is hindering progress towards controlling these other diseases in addition to worsening social determinants such as poverty.26
Vaccinating everyone in low and middle income countries could avert a huge number of deaths. Savinkina and colleagues estimate that giving two doses of mRNA vaccine to everyone in low income countries and lower middle income countries would cost $35.5bn and avert 1.3 million deaths from covid-19.27 Three doses would cost $61.2bn and avert 1.5 million deaths from covid-19. To put these costs into perspective, the International Monetary Fund estimates the economic losses caused by covid-19 will be $13.8tn from 2020 to 2024.28
Global vaccine inequity undermines the economic recovery and social and political stability of low and middle income countries. Sub-Saharan Africa will suffer the greatest economic losses from covid-19 as a proportion of gross domestic product.29 An April 2021 analysis by the United Nations Development Programme found that if vaccination rates in low income countries had been the same as those in high income countries, low income countries would have added $38bn to their gross domestic product forecast for 2021.30 A United Nations Counter-Terrorism Committee study concluded: “Pandemic-related economic hardships (including rising unemployment, poverty, growing inequality, and food insecurity) are potential drivers for an increased terrorist threat.”31
Given the economic interdependency of countries, high income nations are also harmed economically by their own vaccine nationalism. Çakmakli and colleagues estimate that high income countries will bear 13-49% of the global economic losses arising from vaccine inequity, through factors such as interruption of global supply chains and reduced exports to low and middle income countries.32
Achieving global vaccine equity is an urgent priority to reduce the risk of future SARS-CoV-2 variants. The uncontrolled spread of SARS-CoV-2 in unvaccinated populations is a risk factor for new variants, as seen with the emergence of the delta and omicron variants.29 The recent delta/omicron surge led to a huge escalation in cases compared with previous surges (fig 3), creating fertile ground for the development of new variants. Vaccination reduces the risk of infection and transmission, even against the highly transmissible omicron variant. For example, with a booster dose, vaccine efficacy against infection with omicron approaches 70%, akin to the efficacy of influenza vaccines.33
Fig 3.
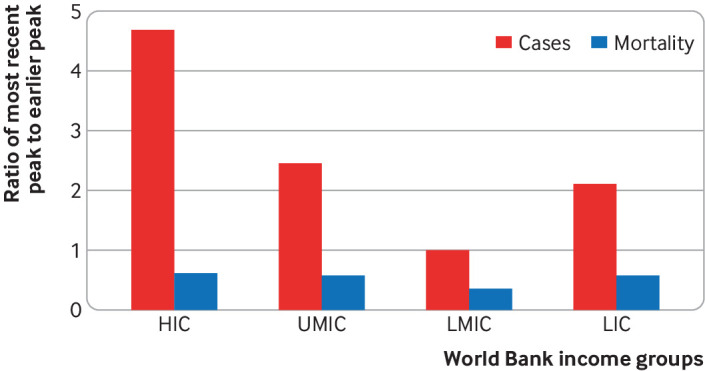
Ratio of the peak in cases and mortality rates for the current omicron/delta surge versus previous waves prior to 1 November 2021. Peaks calculated for daily weekly trailing averages of newly confirmed cases and deaths per 100 000 people. HIC=high income countries; UMIC=upper middle income countries; LMIC=lower middle income countries; LIC=low income countries. Source: https://pandem-ic.com/the-scale-of-the-omicron-escalation/
We cannot assume the next variant will be less severe than omicron. Preventing the emergence of new variants is our best strategy, requiring equitable access to vaccines, new antiviral drugs, and rapid tests. Equitable access to vaccines must mean equitable access to a full course, including boosters. Since vaccine effectiveness wanes around 4-6 months after completing two doses of an mRNA vaccine or one dose of J&J vaccine,34 the best protected are those who had a booster—they are considered “up to date” on vaccination. For high risk populations, further boosters will probably be needed.
Equity among different populations within countries of all income levels is increasingly important. In the United States, for example, black and Hispanic populations have been vaccinated at lower rates compared with the white population,35 and vaccination coverage is much lower in rural than in urban areas.36 These types of sub-national disparities are common worldwide.
How we can vaccinate the world and be better prepared
The world is not on course to reach the WHO target of 70% of people in all countries vaccinated by mid-2022. Yet vaccine equity remains critical to end the pandemic. How can it be achieved?
Firstly, empowering national sovereignty so that countries determine their own priorities and targets is a critical dimension of the path forward in vaccinating the world. Such national sovereignty is embedded in recent guidance on boosters issued by both Africa CDC and WHO’s Strategic Advisory Group of Experts on Immunization.34 37 For many nations, reaching the highest risk groups, including marginalised populations, is their key priority. They may prioritise vaccinating all older people and health workers for full vaccination (including boosters).
Secondly, in the short term, there is an important role for more bilateral donations (provided the doses are not close to expiration) and donations to Covax. The COVID GAP project estimated in November 2021 that at the end of 2021, the Group of 7 (G7) and EU countries had 834 million excess doses, even after accounting for boosters, child vaccinations, and contingencies; these should have been donated or diverted well before the end of the year.38
Hundreds of millions of doses were delivered to low and middle income countries in November and December 2021, as donor countries scrambled to meet their donation targets. Unfortunately, more than 100 million of these doses were rejected by recipient countries in December alone, primarily because the expiration dates were too close to allow for in-country distribution.39 In addition to accelerating pledged donations, G7 and EU countries should also “queue shift” expected deliveries—that is, defer delivery of contracted vaccine doses to prioritise delivery to the African Union, Covax, and countries with unfulfilled bilateral contracts. Covax has shifted from delivering doses to Africa once they are available to delivering them timed with when the country wants them, which should also help to support country led vaccination campaigns.40
Thirdly, urgent, intensified financial and operational support to low and middle income countries is needed for their own national vaccination programmes. Vaccine supply must be made “consistent and predictable.”41 Donors, multilateral banks, and others must also tackle health systems bottlenecks, including political context, in-country planning and financing, health workforce, supply chain constraints, and data systems.
Fourthly, a trickle-down charity model—in which high income and upper middle income nations donate doses to lower middle income and low income nations—is not a fair or sustainable way to achieve vaccine equity. We need a revitalised push towards vaccine self-reliance and decentralised bottom-up manufacturing worldwide, which would be accelerated by the sharing of vaccine intellectual property and technology transfer, financing, workforce development, and regulatory support. The case of Latin America has also shown how critical it is to strengthen capabilities for negotiation and improve transparency on prices and contracts.
WHO’s covid mRNA vaccine hub in South Africa is one potential way forward. The hub is a partnership between Afrigen (a biotech company), Biovac (a vaccine manufacturer), universities, and Africa CDC. It recently announced it had developed “its own version of an mRNA shot, based on the publicly available data on the composition of the Moderna covid-19 vaccine, which will be tested in the coming months.”42 Six African nations have been tapped to receive mRNA vaccine technology from the hub.43
Many other efforts are under way to manufacture mRNA vaccines in sub-Saharan Africa—for example, the Kenyan government is partnering with Moderna to build a vaccine manufacturing facility,44 a South African company (NantSA) is launching a vaccine plant,45 and Moderna plans to ship modular mRNA vaccine factory kits.46
Some low and middle income countries, such as China, Cuba, and India, have invested in their own covid-19 vaccine development and production and have achieved impressive vaccination coverage. In Cuba, for example, as of 19 March 2022, 94% of the population had received at least one dose of a home grown vaccine, 87% were fully vaccinated, and 54% were boosted (several Chinese and Indian vaccines have WHO emergency use listing, unlike Cuba’s vaccines).4 47 South-South collaborations and technology transfer could pave the way for current and future pandemic responses.
Fifthly, regional initiatives will become increasingly important in increasing vaccine coverage in low and middle income countries. Examples include the African Union African Vaccine Acquisition Trust, which is leading pooled procurement efforts for member states, and the Asia Pacific Vaccine Access Facility.
Finally, work is ongoing to develop new variant specific vaccines and nasal vaccines that could potentially provide sterilising immunity. Unless we take steps now to ensure a fair, transparent global allocation process, global inequities will continue for access to these tools, as they have for new covid-19 treatments, such as monoclonal antibodies and tablets such as Paxlovid.
We are at a pivotal moment in the covid-19 pandemic. Without a recommitment to global equity for vaccines and other covid-19 counter measures, coupled with stronger actions and accountability, many more people will die needlessly, and all countries will increase their own future health and economic risks. Prematurely “moving on” from the pandemic, however attractive the short term implications, would be a moral failure from which the world will not easily recover.
Key messages.
Covid-19 vaccine access is inequitable: around 8 in 10 people in high income countries have received at least one vaccine dose compared with just 1 in 10 in low income countries
Such global inequity has been caused by vaccine development and production being concentrated in high income nations, hoarding of doses by such nations, high vaccine prices, and challenges in deploying vaccines in resource poor settings
Even as rich nations are “moving on” and declaring the pandemic over, the public health, moral, and economic case for vaccine equity, including to reduce the chances of future waves or variants, remains powerful and undiminished
We can vaccinate the world through more robust donations, timed specifically to when low and middle income countries request them; strengthened capabilities for distribution, delivery, and demand generation; and decentralised “bottom-up” manufacturing worldwide, accelerated by shared vaccine intellectual property and technology transfer
Competing interests: GY was a member of the covid-19 vaccine development taskforce hosted by the World Bank, and participated as an unpaid academic adviser in the consultation process that led to the launch of Covax. He has received grant funding from WHO; Gavi, the Vaccine Alliance; and the Bill and Melinda Gates Foundation. He is a funding member of Amnesty International, which is one of the members of the People’s Vaccine Alliance. PG participated as a member of the Data Safety and Monitoring Board for a phase 3 double blind, randomised, placebo controlled clinical trial for the evaluation of efficacy and safety in health professionals of the adsorbed vaccine covid-19 (inactivated) produced by Sinovac (study implemented by BUTANTAN in Brazil). FH is a member of the People’s Vaccine Alliance and serves on the advisory group of Resolve to SAVE Lives. WM has received research funding from WHO and the Bill and Melinda Gates Foundation. KKM was a member of the covid-19 vaccine development taskforce hosted by the World Bank and has received funding from WHO and the Bill and Melinda Gates Foundation. MP is an adviser to non-profit organisations such as the Bill and Melinda Gates Foundation, WHO, Stop TB Partnership, and Foundation for Innovative New Diagnostics; he has no financial or industry disclosures. SS has no competing interests. PS has contributed to this article in a personal capacity unconnected to his duties as an employee of the World Bank Group and has provided analytical and other inputs based on the data analytics resource pandem-ic.com that he also developed in a personal capacity. AT has received research funding through Duke University and Duke affiliated non-profit Innovations in Healthcare from Bill and Melinda Gates Foundation, The Rockefeller Foundation, USAID, Grand Challenges Canada, and Pfizer Foundation. KU has received research funding through Duke University and Duke affiliated non-profit Innovations in Healthcare from Bill and Melinda Gates Foundation, The Rockefeller Foundation, USAID, Grand Challenges Canada, Amgen, AstraZeneca, Bayer, Johnson and Johnson Foundation, Medtronic, Pfizer, Pfizer Foundation, Takeda, and Vynamic. He has served as unpaid adviser for the Hewlett Foundation and Africa CDC, and has received an honorarium from Weber Shandwick.
This article is part of a series commissioned by The BMJ for the World Innovation Summit for Health (WISH) 2022. The BMJ commissioned, edited, and made the decisions to publish. The series, including open access fees, is funded by WISH.
References
- 1.Glassman A, Kenny C, Yang G. Covid-19 vaccine development and rollout in historical perspective. Center for Global Development. Feb 2022. Report no 607. https://www.cgdev.org/publication/covid-19-vaccine-development-and-rollout-historical-perspective
- 2.Byanyima W. A global vaccine apartheid is unfolding. People’s lives must come before profit. Guardian 2021 Jan 29. https://www.theguardian.com/global-development/2021/jan/29/a-global-vaccine-apartheid-is-unfolding-peoples-lives-must-come-before-profit
- 3. Sheel M, McEwen S, Davies SE. Brand inequity in access to COVID-19 vaccines. Lancet Reg Health West Pac 2022;18:100366. 10.1016/j.lanwpc.2021.100366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ritchie H, Mathieu E, Rodés-Guirao L, et al. Coronavirus vaccinations (COVID-19). Our World in Data 2020. https://ourworldindata.org/covid-vaccinations
- 5. Wouters OJ, Shadlen KC, Salcher-Konrad M, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet 2021;397:1023-34. 10.1016/S0140-6736(21)00306-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duke Global Health Innovation Center. Vaccine purchases. Launch & Scale Speedometer. https://launchandscalefaster.org/covid-19/vaccinepurchases
- 7. Usher AD. A beautiful idea: how COVAX has fallen short. Lancet 2021;397:2322-5. 10.1016/S0140-6736(21)01367-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yamey G. Rich countries should tithe their vaccines. Nature 2021;590:529-529. 10.1038/d41586-021-00470-9 [DOI] [PubMed] [Google Scholar]
- 9.Naively ambitious’: How COVAX failed on its promise to vaccinate the world. Goldhill O, Furneaux R, Davies M. Stat News 2021 Oct 8. https://www.statnews.com/2021/10/08/how-covax-failed-on-its-promise-to-vaccinate-the-world/
- 10.Duke Global Health Innovation Center. Vaccine manufacturing. Launch & Scale Speedometer. https://launchandscalefaster.org/covid-19/vaccinemanufacturing
- 11.Rosati A. Vaccine delays leave Latin America’s economies in the mud. Bloomberg 2021 Feb 23. https://www.bloomberg.com/news/articles/2021-02-23/vaccine-delays-threaten-economies-hardest-hit-by-pandemic
- 12.How South America became a global leader in covid-19 vaccination. El País 2022 Jan 13. https://english.elpais.com/usa/2022-01-13/how-south-america-became-a-global-leader-in-covid-19-vaccination.html
- 13.UNICEF. Covid-19 vaccine market dashboard. https://www.unicef.org/supply/covid-19-vaccine-market-dashboard
- 14. Sung M, Huang Y, Duan Y, Liu F, Jin Y, Zheng Z. Pharmaceutical industry’s engagement in the global equitable distribution of covid-19 vaccines: corporate social responsibility of EUL vaccine developers. Vaccines (Basel) 2021;9:1183. 10.3390/vaccines9101183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Phelan AL, Eccleston-Turner M, Rourke M, Maleche A, Wang C. Legal agreements: barriers and enablers to global equitable COVID-19 vaccine access. Lancet 2020;396:800-2. 10.1016/S0140-6736(20)31873-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel) 2021;9:160. 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mutombo PN, Fallah MP, Munodawafa D, et al. COVID-19 vaccine hesitancy in Africa: a call to action. Lancet Glob Health 2022;10:e320-1. 10.1016/S2214-109X(21)00563-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cascini F, Pantovic A, Al-Ajlouni Y, Failla G, Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. EclinicalMedicine 2021;40:101113. 10.1016/j.eclinm.2021.101113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mallapaty S. Researchers fear growing COVID vaccine hesitancy in developing nations. Nature 2022;601:174-5. 10.1038/d41586-021-03830-7 [DOI] [PubMed] [Google Scholar]
- 20.Bozio CH. Laboratory-confirmed COVID-19 among adults hospitalized with COVID-19–like illness with infection-induced or mRNA vaccine-induced SARS-CoV-2 immunity—Nine States, January–September 2021. Centers for Disease Control and Prevention 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7044e1.htm [DOI] [PMC free article] [PubMed]
- 21.Cavanaugh AM. Reduced risk of reinfection with SARS-CoV-2 after COVID-19 vaccination—Kentucky, May–June 2021. Centers for Disease Control and Prevention. 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7032e1.htm [DOI] [PMC free article] [PubMed]
- 22.Assis R, Jain A, Nakajima R, et al. Distinct SARS-CoV-2 antibody responses elicited by natural infection and mRNA vaccination. bioRvix 2021:2021.04.15.440089. [Preprint] 10.1101/2021.04.15.440089. [DOI] [PMC free article] [PubMed]
- 23.Kavanagh K. Natural immunity vs super immunity: only a covid-19 vaccination away. Infection Control Today. 2021. https://www.infectioncontroltoday.com/view/covid-19-booster-policy-in-flux-from-super-immunity-to-3-dose-discussions
- 24.Röltgen K, Nielsen SCA, Silva O, et al. Immune imprinting, breadth of variant recognition, and germinal center response in human SARS-CoV-2 infection and vaccination. Cell 2022 Jan 25. https://www.sciencedirect.com/science/article/pii/S0092867422000769 [DOI] [PMC free article] [PubMed]
- 25.Schellekens P, Gill I. COVID-19 is a developing country pandemic. Future development. Brookings Institution. 2021. https://www.brookings.edu/blog/future-development/2021/05/27/covid-19-is-a-developing-country-pandemic/. Updated: https://pandem-ic.com/the-global-mortality-distribution-reported-versus-excess-deaths/
- 26. Mao W, Ogbuoji O, Watkins D, et al. Achieving global mortality reduction targets and universal health coverage: The impact of COVID-19. PLoS Med 2021;18:e1003675. 10.1371/journal.pmed.1003675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Savinkina A, Bilinski A, Fitzpatrick MC, et al. Model-based estimates of deaths averted and cost per life saved by scaling-up mRNA COVID-19 vaccination in low and lower-middle income countries in the COVID-19 omicron variant era [Preprint]. medRixiv 2022. https://www.medrxiv.org/content/10.1101/2022.02.08.22270465v1 10.1101/2022.02.08.22270465 [DOI] [PMC free article] [PubMed]
- 28.Gopinath G. A disrupted global recovery. IMG Blog. 9 Mar 2022. https://blogs.imf.org/2022/01/25/a-disrupted-global-recovery/
- 29.Andersen H. The global cost of vaccine inequity. Tony Blair Institute for Global Change. 2021. https://institute.global/advisory/global-cost-vaccine-inequity
- 30.UNDP Data Futures Platform. Impact of vaccine inequity on economic recovery. https://data.undp.org/vaccine-equity/impact-of-vaccine-inequity-on-economic-recovery/
- 31.Counter-terrorism Committee Executive Directorate. Update on the impact of the COVID-19 pandemic on terrorism, counter-terrorism and countering violent extremism. United Nations Security Council. Jun 2021. https://www.un.org/securitycouncil/ctc/content/update-impact-covid-19-pandemic-terrorism-counter-terrorism-and-countering-violent-extremism
- 32.Çakmaklı C, Demiralp S, Kalemli-Özcan Ṣ, Yeşiltaş S, Yıldırım MA. The economic case for global vaccinations: An epidemiological model with international production networks. National Bureau of Economic Research. Jan 2021. Working paper series. Report no 28395. https://www.nber.org/papers/w28395
- 33. Tseng HF, Ackerson BK, Luo Y, et al. Effectiveness of mRNA-1273 against SARS-CoV-2 omicron and delta variants. [Preprint]. medRxiv 2022. p. 2022.01.07.22268919. https://www.medrxiv.org/content/10.1101/2022.01.07.22268919v3 [DOI] [PMC free article] [PubMed]
- 34.WHO Strategic Advisory Group of Experts on Immunization updates recommendations on boosters, COVID-19 vaccines for children. PAHO/WHO. 2022 Jan 21. https://www.paho.org/en/news/21-1-2022-who-strategic-advisory-group-experts-immunization-updates-recommendations-boosters
- 35.Chhibber A, Kharat A, Duong K, et al. Strategies to minimize inequity in COVID-19 vaccine access in the US: Implications for future vaccine rollouts. Lancet Regional Health–Americas 2022 Mar 1. https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(21)00134-4/fulltext [DOI] [PMC free article] [PubMed]
- 36.Saelee R. Disparities in COVID-19 vaccination coverage between urban and rural counties-United States, December 14, 2020-January 31, 2022. Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/mmwr/volumes/71/wr/mm7109a2.htm [DOI] [PMC free article] [PubMed]
- 37.Guidance on administration of COVID-19 vaccine boosters in Africa. Africa CDC. Feb 2022. https://africacdc.org/download/guidance-on-administration-of-covid-19-vaccine-boosters-in-africa/
- 38.Boyer B, Taylor A, Edson G, Merson M, McClellan M, Udayakumar K. Holding the world to account: urgent actions needed to close gaps in the global COVID-19 response. Duke Global Health Innovation Center, COVID Collaborative. 2021 Nov 18. https://covid19gap.org/assets/publications/Holding-the-World-to-Account-COVID-GAP-11-18-21.pdf
- 39.Guarascio F. Poorer nations reject over 100 mln COVID-19 vaccine doses as many near expiry. Reuters 2022 Jan 14. https://www.reuters.com/business/healthcare-pharmaceuticals/more-than-100-million-covid-19-vaccines-rejected-by-poorer-nations-dec-unicef-2022-01-13/
- 40.Payne D. Africa CDC to ask world to pause covid-19 vaccine donations. POLITICO 2022 Feb 22. https://www.politico.com/news/2022/02/22/africa-asks-covid-vaccine-donation-pause-00010667
- 41.Boyer B, Edson G, Lindstrand A, et al. From airports to arms: new insights and urgent recommendations to accelerate global covid-19 vaccinations. Duke Global Health Innovation Center, COVID Collaborative 2021 Dec 23. https://covid19gap.org/assets/publications/COVID-GAP-From-Airports-to-Arms.pdf
- 42.World Health Organization. South Africa’s mRNA hub progress is foundation for self-reliance. WHO 2022 Feb 11. https://www.who.int/news/item/11-02-2022-south-africa-s-mrna-hub-progress-is-foundation-for-self-reliance
- 43.Schnirring L. 2022. WHO: Africa mRNA vaccine hub expands to 6 nations. CIDRAP News 2022 Feb 18. https://www.cidrap.umn.edu/news-perspective/2022/02/who-africa-mrna-vaccine-hub-expands-6-nations
- 44.Khandekar A. Moderna to build mRNA vaccine manufacturing facility in Kenya. Reuters 2022 Mar 8. https://www.reuters.com/business/healthcare-pharmaceuticals/moderna-build-mrna-vaccine-manufacturing-facility-kenya-2022-03-07/
- 45.Roelf W. Billionaire Soon-Shiong opens new vaccine plant in South Africa. Reuters 2022 Jan 19. https://www.reuters.com/world/africa/billionaire-soon-shiong-opens-new-vaccine-plant-south-africa-2022-01-19/
- 46.Burger L. BioNTech to ship mRNA vaccine factory kits to Africa. Reuters 2022 Feb 16. https://www.reuters.com/business/healthcare-pharmaceuticals/biontech-ship-mrna-vaccine-factory-kits-africa-2022-02-16/
- 47.Craven J. COVID-19 vaccine tracker. Regulatory Affairs Professionals Society. 2022. https://www.raps.org/news-and-articles/news-articles/2020/3/covid-19-vaccine-tracker


