This cross-sectional study of respondents to the National Survey on Drug Use and Health evaluates rates of medication for opioid use disorder receipt among people with need for treatment as well as associated sociodemographic characteristics.
Key Points
Question
What are the individual characteristics associated with medication for opioid use disorder (MOUD) receipt among people with opioid use disorder treatment need?
Findings
In this cross-sectional study with a weighted sample of 2 206 169 people with treatment need, approximately 1 in 4 (27.8%) reported past-year MOUD use, including no adolescents and only 13.2% of adults 50 years and older. Use of MOUD was low despite high prevalence of past-year health care or criminal legal system contacts.
Meaning
Given that MOUD use was low, these results suggest that cross-system integrated interventions to increase MOUD uptake are needed, especially for younger age groups and older adults.
Abstract
Importance
Medication for opioid use disorder (MOUD) is the criterion standard treatment for opioid use disorder (OUD), but nationally representative studies of MOUD use in the US are lacking.
Objective
To estimate MOUD use rates and identify associations between MOUD and individual characteristics among people who may have needed treatment for OUD.
Design, Setting, and Participants
Cross-sectional, nationally representative study using the 2019 National Survey on Drug Use and Health in the US. Participants included community-based, noninstitutionalized adolescent and adult respondents identified as individuals who may benefit from MOUD, defined as (1) meeting criteria for a past-year OUD, (2) reporting past-year MOUD use, or (3) receiving past-year specialty treatment for opioid use in the last or current treatment episode.
Main Outcomes and Measures
The main outcomes were treatment with MOUD compared with non-MOUD services and no treatment. Associations with sociodemographic characteristics (eg, age, race and ethnicity, sex, income, and urbanicity); substance use disorders; and past-year health care or criminal legal system contacts were analyzed. Multinomial logistic regression was used to compare characteristics of people receiving MOUD with those receiving non-MOUD services or no treatment. Models accounted for predisposing, enabling, and need characteristics.
Results
In the weighted sample of 2 206 169 people who may have needed OUD treatment (55.5% male; 8.0% Hispanic; 9.9% non-Hispanic Black; 74.6% non-Hispanic White; and 7.5% categorized as non-Hispanic other, with other including 2.7% Asian, 0.9% Native American or Alaska Native, 0.2% Native Hawaiian or Pacific Islander, and 3.8% multiracial), 55.1% were aged 35 years or older, 53.7% were publicly insured, 52.2% lived in a large metropolitan area, 56.8% had past-year prescription OUD, and 80.0% had 1 or more co-occurring substance use disorders (percentages are weighted). Only 27.8% of people needing OUD treatment received MOUD in the past year. Notably, no adolescents (aged 12-17 years) and only 13.2% of adults 50 years and older reported past-year MOUD use. Among adults, the likelihood of past-year MOUD receipt vs no treatment was lower for people aged 50 years and older vs 18 to 25 years (adjusted relative risk ratio [aRRR], 0.14; 95% CI, 0.05-0.41) or with middle or higher income (eg, $50 000-$74 999 vs $0-$19 999; aRRR, 0.18; 95% CI, 0.07-0.44). Compared with receiving non-MOUD services, receipt of MOUD was more likely among adults with at least some college (vs high school or less; aRRR, 2.94; 95% CI, 1.33-6.51) and less likely in small metropolitan areas (vs large metropolitan areas, aRRR, 0.41; 95% CI, 0.19-0.93). While contacts with the health care system (85.0%) and criminal legal system (60.5%) were common, most people encountering these systems did not report receiving MOUD (29.5% and 39.1%, respectively).
Conclusions and Relevance
In this cross-sectional study, MOUD uptake was low among people who could have benefited from treatment, especially adolescents and older adults. The high prevalence of health care and criminal legal system contacts suggests that there are critical gaps in care delivery or linkage and that cross-system integrated interventions are warranted.
Introduction
In 2019, 70.6% of the 70 630 drug overdose fatalities in the US involved opioids.1 These premature deaths have been associated with millions of years of life lost, including more than 1.6 million life-years attributed to opioid-related deaths in 2016 alone.2 Opioid-related deaths can be prevented through overdose reversal medication (ie, naloxone)3 and upstream treatment of underlying opioid use disorder (OUD).4 Evidence supporting the effectiveness of medication for OUD (MOUD; ie, methadone, buprenorphine, or naltrexone)5,6,7 is unequivocal, making it the criterion standard OUD treatment. Medication for OUD is associated with reductions in opioid use8 and disorder,9 longer treatment retention,10,11 and substantially reduced opioid-related mortality.7 Despite the strong evidence base, access to MOUD is limited by low facility and clinician uptake12,13,14,15 and persistent stigma surrounding OUD and medication.16,17,18
Current estimates of MOUD use rely on administrative data, such as specialty substance use treatment episodes10,19,20 and insurance or prescription records.12,21,22,23,24,25 These estimates consistently indicate low access to MOUD, particularly among younger age groups,7,12,20,21 pregnant women,22 residents of rural counties,26 adults involved in the criminal legal system,1,27,28 and racial and ethnic minority individuals.23 Studies have described individual and contextual characteristics associated with OUD treatment broadly29,30 but have not examined MOUD specifically owing to a lack of nationally representative data. As a result, knowledge about MOUD use is limited to convenience or clinical samples, which may differ systematically from people with OUD treatment need in the general population.
In 2019, the National Survey on Drug Use and Health (NSDUH) began measuring MOUD use, which for the first time made it possible to obtain nationally representative estimates of MOUD using a community-based sample.31 However, little is known about individual-level characteristics associated with past-year MOUD. This gap is even wider for individuals without medically documented OUD diagnoses because they are often excluded from research using clinical and administrative samples. Examining MOUD among a more expansive sample of people who may need treatment is clinically meaningful because people receiving MOUD may no longer meet OUD criteria or, alternatively, may receive medication without a diagnosis.24,32
This study is the first to our knowledge to estimate past-year MOUD use in a nationally representative community sample of people who may have needed past-year OUD treatment, which included noninstitutionalized people with OUD or who reported treatment for opioids. Building on past studies examining OUD treatment services more generally,29,30 we compared characteristics of people receiving MOUD with those of people receiving non-MOUD services (ie, connected with treatment but not receiving medication) or no treatment at all. We hypothesized that MOUD use would be particularly low among younger age groups20,21 and would be disproportionately distributed by sex, race and ethnicity, and urbanicity, based on previous research.25,29 We also identified points of treatment engagement, describing MOUD among people in contact with the health care and criminal legal systems, to inform interventions aimed at improving treatment access. To our knowledge, this is the first study to quantify MOUD use for the general population with OUD treatment need, providing critical evidence to build a more comprehensive understanding of care access and quality. Findings can inform national efforts needed to increase equitable access to MOUD in the US.
Methods
Data Source
The NSDUH is an annual, nationally representative cross-sectional household survey of people 12 years and older in the US designed to provide estimates of substance use and disorders. The complex survey design captured households in all 50 states, excluding people who were institutionalized or homeless and not in shelters.33 In-person interviews incorporated audio computer-assisted self-interviewing to increase willingness to report sensitive behaviors honestly.33 Drug use disorder measures had moderate validity and reliability (κ = 0.60-0.67).34,35 The NSDUH was approved by the RTI institutional review board.36 In 2019, the total response rate was 45.8%, including 70.5% for screening and 64.9% for weighted interviews.33,36 The Columbia University institutional review board approved this study; the use of deidentified public-use data was not considered human participants research and did not require informed consent beyond what was provided through the NSDUH. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cross-sectional studies.37
Study Sample
The 2019 NSDUH deidentified public-use data included 56 136 people 12 years and older in the US. Inclusion criteria for past-year OUD treatment need were as follows: (1) past-year OUD (ie, past-year Diagnostic and Statistical Manual of Mental Disorders [Fourth Edition]38 heroin or prescription pain reliever abuse or dependence); (2) past-year MOUD (ie, “medication to help reduce or stop your use of [heroin/prescription pain relievers]”), or (3) past-year or current specialty treatment episode for heroin or prescription pain relievers (eMethods in the Supplement, measures 1-4, for wording and question sequence). These criteria adapted the NSDUH “treatment need” definition33 to be OUD-specific, including MOUD. Our final unweighted sample was n = 487. Of all observations not meeting the inclusion criteria, 1.9% were excluded owing to unknown or missing inclusion measure responses (ie, “don’t know,” refused, blank, or “bad data”; eMethods in the Supplement).
Measures
Past-Year MOUD, Non-MOUD Services, or No Treatment
Participants reporting lifetime use of heroin or nonmedical prescription opioids and past-year treatment for drug use were asked about past-year MOUD (eg, buprenorphine, methadone, or naltrexone; eMethods in the Supplement, measure 5). Past-year MOUD indicated using “medication to help reduce or stop your use of [heroin/prescription pain relievers].” Non-MOUD services included reporting past-year treatment for drug use in any setting among those not reporting MOUD. We created a 3-level categorical OUD treatment variable (eMethods in the Supplement, measure 5): past-year MOUD, non-MOUD services (ie, past-year treatment or counseling for drug use but no MOUD), and no treatment (ie, no past-year MOUD or non-MOUD services).
Individual Predisposing, Enabling, and Need Characteristics
We used the Andersen Behavioral Model of Health Services Use39 and previous literature21 to select individual characteristics of clinical interest, as categorized in the public-use NSDUH. Predisposing characteristics included age (12-17, 18-25, 26-34, 35-49, or ≥50 years), sex (male or female), and education (among adults: high school or less or at least some college). Self-reported race and ethnicity included Hispanic/Latinx, non-Hispanic Black, non-Hispanic White, and non-Hispanic other (including Asian, Native American or Alaska Native, Native Hawaiian or Pacific Islander, and/or multiracial). Enabling resources included household income (<$20 000, $20 000-$49 999, $50 000-$74 999, or ≥$75 000), insurance status (any public insurance [eg, Medicaid, the Children’s Health Insurance Program, Medicare, or the Civilian Health and Medical Program of the Uniformed Services or other military insurance], private only, or uninsured or other), and urbanicity (large, small, or nonmetropolitan area). Need variables included OUD (Diagnostic and Statistical Manual of Mental Disorders [Fourth Edition]38 heroin and prescription pain reliever abuse or dependence), any other co-occurring substance use disorder (excluding opioid or tobacco use disorder), and past-year major depressive episode.
Contacts With Health Care and Criminal Legal Systems
Health care contacts included past-year health care use in emergency, inpatient, or outpatient settings. Past-year criminal legal system contacts included any past-year booking, arrests, probation, or parole.
Statistical Analysis
We calculated descriptive statistics for the past-year OUD treatment need sample using survey weights to derive nationally representative estimates, as well as the proportion within each subgroup reporting past-year MOUD, non-MOUD services, or no treatment. Then we fit multinomial regression models to identify the association of predisposing, enabling, and need variables with MOUD, as compared with both non-MOUD services and no drug treatment. We also examined past-year contacts with the health care and criminal legal systems to describe rates of MOUD among people encountering each system. In sensitivity analyses, the model included detailed categories of public insurance and an additional indicator of past-year criminal legal system involvement to examine associations independent of criminal legal contact. All analyses were conducted using svy command estimations in Stata, version 15MP (StataCorp LLC), with standard errors accounting for complex survey data design using Taylor linearization, and a 2-sided P value significance threshold of less than .05.
Results
Among the weighted sample of 2 206 169 people (unweighted, 487) who may have needed OUD treatment (55.5% male; 8.0% Hispanic, 9.9% non-Hispanic Black, 74.6% non-Hispanic White, and 7.5% non-Hispanic other, with other including 2.7% Asian, 0.9% Native American or Alaska Native, 0.2% Native Hawaiian or Pacific Islander, and 3.8% identified as multiracial), 55.1% were aged 35 years or older, 53.7% were publicly insured, 52.2% lived in a large metropolitan area, 56.8% had past-year prescription OUD, and 80.0% had 1 or more co-occurring substance use disorders (percentages are weighted) (Table 1).
Table 1. Sociodemographic Characteristics of Adolescents and Adults With Past-Year OUD Treatment Needa.
| Characteristic | Overall sample of respondents with OUD treatment need | Past-year drug treatment use | P value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Weighted No. | Weighted column % (95% CI) | No treatment | Non-MOUD services | MOUD | |||||
| Weighted No. | Weighted row % (95% CI) | Weighted No. | Weighted row % (95% CI) | Weighted No. | Weighted row % (95% CI) | ||||
| Total (row %) | 2 206 169 | 100.0 | 1 256 838 | 57.0 (50.9-62.8) | 336 580 | 15.3 (12.0-19.2) | 612 750 | 27.8 (22.0-34.3) | NA |
| Predisposing | |||||||||
| Age, y | |||||||||
| 12-17b | 92 081 | 4.2 (2.8-6.1) | 80 829 | 87.8 (72.4-95.2) | 11 252 | 12.2 (4.8-27.6) | 0 | 0 (0-0) | <.001 |
| 18-25b | 251 824 | 11.4 (8.8-14.7) | 154 797 | 61.5 (46.4-74.6) | 41 492 | 16.5 (10.4-25.1) | 55 534 | 22.0 (12.3-36.3) | |
| 26-34b | 646 460 | 29.3 (23.6-35.8) | 264 713 | 41.0 (28.6-54.6) | 108 180 | 16.7 (9.1-28.7) | 273 567 | 42.3 (30.7-54.8) | |
| 35-49b | 699 988 | 31.7 (26.6-37.4) | 342 394 | 48.9 (40.8-57.1) | 141 967 | 20.3 (13.5-29.3) | 215 627 | 30.8 (22.6-40.5) | |
| ≥50b | 515 817 | 23.4 (16.3-32.4) | 414 106 | 80.3 (64.8-90.0) | 33 689 | 6.5 (3.8-11.0) | 68 022 | 13.2 (5.8-27.4) | |
| Sex | |||||||||
| Male | 1 224 910 | 55.5 (49.4-61.5) | 658 927 | 53.8 (45.9-61.5) | 231 657 | 18.9 (14.0-25.0) | 334 326 | 27.3 (20.0-36.0) | .10 |
| Female | 981 259 | 44.5 (38.5-50.6) | 597 911 | 60.9 (52.3-68.9) | 104 923 | 10.7 (6.9-16.2) | 278 425 | 28.4 (21.8-36.0) | |
| Race and ethnicity | |||||||||
| Hispanic | 176 701 | 8.0 (5.8-11.0) | 126 733 | 71.7 (44.2-89.0) | 23 835 | 13.5 (6.5-25.8) | 26 133c | 14.8 (2.9-50.0) | .60 |
| Non-Hispanic | |||||||||
| Black | 219 095 | 9.9 (6.7-14.5) | 138 214 | 63.1 (43.9-78.9) | 38 178 | 17.4 (7.0-37.0) | 42 703 | 19.5 (9.2-36.6) | |
| White | 1 645 196 | 74.6 (68.5-79.8) | 881 641 | 53.6 (46.3-60.8) | 253 883 | 15.4 (11.2-20.8) | 509 672 | 31.0 (23.9-39.1) | |
| Other | 165 178 | 7.5 (4.4-12.4) | 110 251 | 66.8 (41.6-85.0) | 20 684c | 12.5 (4.3-31.1) | 34 243c | 20.7 (7.2-47.0) | |
| Education (≥18 y) | |||||||||
| High school or lessb | 935 320 | 44.2 (37.5-51.2) | 470 296 | 50.3 (42.5-58.1) | 206 670 | 22.1 (15.6-30.3) | 258 354 | 27.6 (20.0-36.8) | .03 |
| Some college or moreb | 1 178 768 | 55.8 (48.8-62.5) | 705 714 | 59.9 (50.8-68.5) | 118 658 | 10.1 (06.0-16.5) | 354 396 | 30.1 (23.2-37.9) | |
| Enabling | |||||||||
| Insurance | |||||||||
| Any publicb | 1 185 665 | 53.7 (46.9-60.4) | 585 286 | 49.4 (40.9-57.9) | 183 580 | 15.5 (11.4-20.8) | 416 799 | 35.2 (26.6-44.8) | .01 |
| Private onlyb | 576 544 | 26.1 (19.7-33.8) | 393 950 | 68.3 (57.7-77.3) | 61 249 | 10.6 (6.1-17.8) | 121 345 | 21.0 (12.3-33.6) | |
| Uninsured/otherb | 443 960 | 20.1 (14.6-27.1) | 277 603 | 62.5 (49.5-74.0) | 91 751 | 20.7 (12.8-31.7) | 74 606 | 16.8 (9.2-28.8) | |
| Income, $ | |||||||||
| 0-19 999 | 736 805 | 33.4 (26.3-41.4) | 321 047 | 43.6 (32.9-54.9) | 138 994 | 18.9 (11.7-28.9) | 276 765 | 37.6 (28.1-48.0) | .09 |
| 20 000-49 999 | 674 355 | 30.6 (24.0-38.0) | 407 270 | 60.4 (48.6-71.1) | 99 968 | 14.8 (8.6-24.3) | 167 117 | 24.8 (15.6-37.1) | |
| 50 000-74 999 | 311 849 | 14.1 (10.3-19.0) | 209 007 | 67.0 (52.3-79.0) | 52 298 | 16.8 (8.2-31.2) | 50 544 | 16.2 (9.8-25.6) | |
| ≥75 000 | 483 160 | 21.9 (15.5-30.0) | 319 514 | 66.1 (50.8-78.7) | 45 321 | 9.4 (3.9-20.9) | 118 325 | 24.5 (13.5-40.2) | |
| Urbanicity | |||||||||
| Large metropolitan | 1 152 707 | 52.2 (46.3-58.1) | 690 354 | 59.9 (52.4-67.0) | 127 075 | 11.0 (6.4-18.5) | 335 278 | 29.1 (22.2-37.1) | .30 |
| Small metropolitan | 754 477 | 34.2 (28.9-40.0) | 394 378 | 52.3 (40.5-63.8) | 165 656 | 22.0 (15.4-30.3) | 194 443 | 25.8 (18.0-35.5) | |
| Nonmetropolitan | 298 985 | 13.6 (9.8-18.4) | 172 106 | 57.6 (38.1-74.9) | 43 849 | 14.7 (7.5-26.6) | 83 029 | 27.8 (14.6-46.4) | |
| Need | |||||||||
| Any OUDb | 1 700 870 | 77.1 (71.3-82.0) | 1 256 838 | 73.9 (67.9-79.1) | 150 072 | 8.8 (6.4-12.0) | 293 959 | 17.3 (12.6-23.3) | <.001 |
| Prescription OUD onlyb | 1 253 326 | 56.8 (51.0-62.5) | 1 049 077 | 83.7 (75.7-89.4) | 77 281 | 6.2 (3.2-11.5) | 126 968 | 10.1 (6.0-16.6) | <.001 |
| Heroin use disorder onlyb | 267 312 | 12.1 (8.9-16.3) | 157 826 | 59.0 (44.1-72.5) | 42 938 | 16.1 (7.2-32.2) | 66 548 | 24.9 (14.5-39.3) | |
| Co-occurring heroin/prescription OUDb | 180 232 | 8.2 (5.4-12.2) | 49 936 | 27.7 (13.8-47.9) | 29 853c | 16.6 (6.0-38.3) | 100 443 | 55.7 (35.2-74.5) | |
| Other co-occurring substance use disorderb | 1 764 273 | 80.0 (73.4-85.3) | 1 183 527 | 67.1 (60.8-72.8) | 219 392 | 12.4 (9.2-16.5) | 361 354 | 20.5 (14.8-27.6) | <.001 |
| Major depressive episode (≥18 y) | 852 697 | 38.6 (32.0-45.8) | 439 950 | 51.6 (41.8-61.3) | 129 214 | 15.2 (9.5-23.3) | 283 534 | 33.2 (24.4-43.4) | .27 |
Abbreviations: MOUD, medication for opioid use disorder; NA, not applicable; OUD, opioid use disorder.
Weighted No. is the survey-weighted sample size; unweighted N = 487; weighted column % indicates survey-weighted column percentage; weighted percentages may not sum to 100 because of rounding. A callout of 18 years and older indicates the characteristic being restricted to adults 18 years and older. Other co-occurring substance use disorder includes 1 or more of the following past-year substance use disorders: alcohol, cannabis, cocaine, hallucinogens, inhalants, methamphetamine, tranquilizers, stimulants, sedatives, and psychedelics. Self-reported race and ethnicity included Hispanic/Latinx, non-Hispanic Black, non-Hispanic White, and non-Hispanic other (eg, Asian, Native American or Alaska Native, Native Hawaiian, Pacific Islander, or multiracial).
Design-based P less than .05 with Rao-Scott adjustment.
Lower bound of confidence interval for weighted sample estimate includes zero.
Only 27.8% of people needing OUD treatment received MOUD in the past year; 57.0% received no treatment, and 15.3% received non-MOUD services (Table 1). Notably, no adolescents (aged 12-17 years) and only 13.2% of adults 50 years and older reported past-year MOUD use. A minority of adults with higher education (30.1%) and high school or less education (27.6%) reported receiving MOUD. Other predisposing characteristics were not statistically associated with treatment status but signaled potential treatment disparities. For example, 14.8% of Hispanic respondents, 19.5% of non-Hispanic Black respondents, and 20.7% of respondents identified as other race and ethnicity reported receiving MOUD, compared with 31.0% of non-Hispanic White people. Insurance was the main enabling resource associated with treatment status. More than one-third of people with public insurance (35.2%) reported receiving MOUD compared with 21.0% with private coverage and 16.8% with no public or private insurance. Need variables were associated with MOUD use, including co-occurring substance use disorders. Overall, 17.3% of people with any OUD reported receiving MOUD, but a gradient was observed by OUD type, with only 10.1% for prescription OUD only, 24.9% for heroin use disorder only, and 55.7% for both heroin and prescription OUD reporting MOUD (percentages are weighted) (Table 1). Among people reporting MOUD, 52.0% did not meet past-year OUD criteria (eTable 1 in the Supplement).
Table 2 shows unadjusted and adjusted multinomial estimates comparing predisposing, enabling, and need characteristics of people receiving MOUD with people receiving no treatment or non-MOUD services. Adolescents were excluded because none reported past-year MOUD (eTable 2 in the Supplement, adult subsample characteristics). In adjusted models, groups less likely to report MOUD included people 50 years and older compared with ages 18 to 25 years (adjusted relative risk ratio [aRRR], 0.14; 95% CI, 0.05-0.41), people identifying as non-Hispanic other compared with people identifying as non-Hispanic White (aRRR, 0.28; 95% CI, 0.08-0.92), women compared with men (aRRR, 0.52; 95% CI, 0.29-0.95), people with private insurance only (aRRR, 0.34; 95% CI, 0.13-0.89) or no/other insurance (aRRR, 0.26; 95% CI, 0.08-0.87) compared with public insurance, and people reporting incomes $50 000 to $74 999 compared with less than $20 000 (aRRR, 0.18; 95% CI, 0.07-0.44). People with some college were more likely to report MOUD than those with high school or less education (aRRR, 2.12; 95% CI, 1.18-3.78). Need characteristics were strongly associated with MOUD, including significantly greater likelihood of MOUD for people with co-occurring heroin and prescription OUD (aRRR, 5.07; 95% CI, 1.50-17.12) and lower likelihood for other co-occurring substance use disorders (aRRR, 0.07; 95% CI, 0.03-0.16). Only 2 characteristics distinguished people receiving MOUD from those receiving non-MOUD services; MOUD was more likely among those with some college compared with lower education (aRRR, 2.94; 95% CI, 1.33-6.51) and less likely for people living in small compared with large metropolitan areas (aRRR, 0.41; 95% CI, 0.19-0.93).
Table 2. Likelihood of Medication for Opioid Use Disorder Among Adults Who May Have Needed OUD Treatmenta.
| Characteristics | MOUD vs no treatment | MOUD vs non-MOUD services | ||
|---|---|---|---|---|
| uRRR (95% CI) | aRRR (95% CI) | uRRR (95% CI) | aRRR (95% CI) | |
| Predisposing | ||||
| Age categories, y | ||||
| 18-25 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 26-34 | 2.88 (1.11-7.50)b | 1.37 (0.42-4.43) | 1.89 (0.67-5.32) | 1.30 (0.42-4.03) |
| 35-49 | 1.76 (0.74-4.15) | 0.84 (0.30-2.35) | 1.13 (0.47-2.71) | 0.75 (0.28-2.05) |
| ≥50 | 0.46 (0.16-1.32) | 0.14 (0.05-0.41)b | 1.51 (0.60-3.79) | 0.86 (0.31-2.42) |
| Race and ethnicity | ||||
| Hispanic | 0.38 (0.06-2.39) | 0.57 (0.14-2.28) | 0.53 (0.09-3.00) | 0.61 (0.15-2.57) |
| Non-Hispanic | ||||
| Black | 0.60 (0.21-1.74) | 0.82 (0.27-2.46) | 0.57 (0.14-2.31) | 0.52 (0.12-2.18) |
| White | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Other | 0.53 (0.13-2.16) | 0.28 (0.08-0.92)b | 0.80 (0.18-3.57) | 0.35 (0.08-1.54) |
| Sex | ||||
| Male | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Female | 0.95 (0.57-1.56) | 0.52 (0.29-0.95)b | 1.87 (0.95-3.69) | 1.77 (0.81-3.85) |
| Education | ||||
| High school or less | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Some college or more | 0.91 (0.57-1.46) | 2.12 (1.18-3.78)b | 2.39 (1.04-5.46)b | 2.94 (1.33-6.51)b |
| Enabling | ||||
| Insurance | ||||
| Any public | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Private only | 0.45 (0.20-1.04) | 0.34 (0.13-0.89)b | 0.87 (0.30-2.51) | 0.89 (0.23-3.40) |
| Uninsured/other | 0.38 (0.18-0.81)b | 0.26 (0.08-0.87)b | 0.34 (0.15-0.79)b | 0.33 (0.11-1.03) |
| Income, $ | ||||
| 0-19 999 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 20 000-49 999 | 0.49 (0.24-1.02) | 0.47 (0.22-1.01) | 0.86 (0.31-2.35) | 0.72 (0.23-2.22) |
| 50 000-74 999 | 0.28 (0.12-0.65)b | 0.18 (0.07-0.44)b | 0.47 (0.15-1.43) | 0.35 (0.09-1.42) |
| ≥75 000 | 0.44 (0.18-1.08) | 0.37 (0.13-1.04) | 1.27 (0.35-4.53) | 0.83 (0.19-3.68) |
| Urbanicity | ||||
| Large metropolitan | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Small metropolitan | 0.98 (0.54-1.80) | 0.95 (0.50-1.79) | 0.45 (0.20-1.03) | 0.41 (0.19-0.93)b |
| Nonmetropolitan | 0.97 (0.37-2.54) | 0.94 (0.32-2.78) | 0.75 (0.25-2.23) | 0.82 (0.26-2.58) |
| Need | ||||
| Co-occurring heroin and prescription OUD | 4.42 (1.61-12.17)b | 5.07 (1.50-17.12)b | 1.94 (0.53-7.08) | 2.31 (0.44-12.18) |
| Other co-occurring substance use disorder | 0.10 (0.04-0.22)b | 0.07 (0.03-0.16)b | 0.81 (0.31-2.11) | 0.64 (0.19-2.13) |
| Major depressive episode | 1.44 (0.79-2.64) | 1.58 (0.84-2.95) | 1.31 (0.64-2.69) | 0.98 (0.45-2.16) |
Abbreviations: aRRR, adjusted relative risk ratio (from the multinomial model with a categorical outcome); MOUD, medication for opioid use disorder; OUD, opioid use disorder; uRRR, unadjusted relative risk ratio.
Weighted N = 2 114 089; unweighted N = 438. Adolescents aged 12 to 17 years were excluded from the model because of collinearity with the outcome. Other co-occurring substance use disorder includes 1 or more of the following past-year substance use disorders: alcohol, cannabis, cocaine, hallucinogens, inhalants, methamphetamine, tranquilizers, stimulants, sedatives, and psychedelics. Self-reported race/ethnicity included Hispanic/Latinx, non-Hispanic Black, non-Hispanic White, and non-Hispanic other (eg, Asian, Native American or Alaska Native, Native Hawaiian, Pacific Islander, or multiracial).
Design-based P < .05.
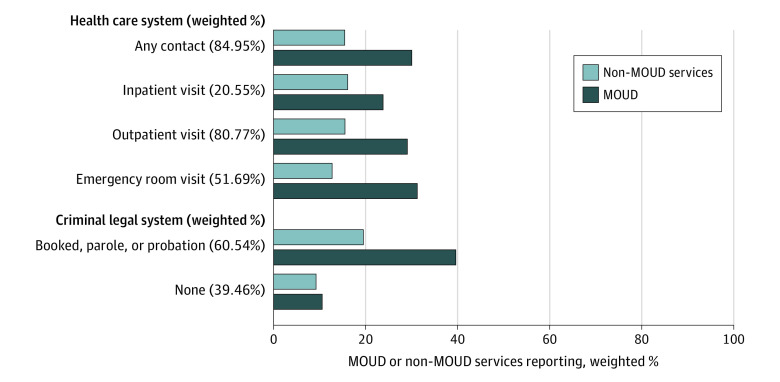
The Figure shows that 85.0% of the sample had past-year health care (ie, 80.8% outpatient, 20.6% inpatient, and 51.7% emergency department settings) or criminal legal system contacts (60.5%). Only a minority of people encountering these systems reported receiving MOUD (health, 29.5%; legal, 39.1%) (percentages are weighted).
Figure. Past-Year Contact With Health Care and Criminal Legal System Contacts and Medication for Opioid Use Disorder (MOUD) Treatment, 2019.
Weighted N = 2 206 169; unweighted N = 487.
Results of sensitivity analyses resembled the main results; criminal legal exposure was strongly associated with receiving MOUD compared with no treatment (aRRR, 3.73; 95% CI, 1.78-7.80; eTable 3 in the Supplement).
Discussion
Our nationally representative cross-sectional study examined MOUD in a community sample of US adolescents and adults in 2019, extending prior studies using administrative data12,40 or examining OUD treatment broadly.29,30 Approximately 1 in 4 people who may have needed OUD treatment reported past-year MOUD. No adolescents received MOUD, and most adults received no drug treatment at all, indicating substantial gaps in access. While past-year OUD signaled clinical need for treatment, only 1 in 6 (17.3%) people with OUD reported receiving MOUD, although this was higher among people with co-occurring heroin and prescription OUD. Beyond clinical need, both predisposing and enabling characteristics were associated with MOUD compared with no treatment, but only education and urbanicity distinguished people receiving MOUD from those receiving non-MOUD services. This is consistent with prior work demonstrating that individual characteristics influence OUD treatment access29 and underscores the importance of key modifiable factors in distinguishing the type of treatment received.
Only adults reported receiving MOUD, consistent with past reports of low MOUD use in adolescents.20,21,41 Buprenorphine is approved by the US Food and Drug Administration for people 16 years and older and is the only medication approved to treat OUD in adolescents.42 Hesitancy about off-label prescribing for ages 12 to 15 years could contribute to underuse of MOUD in this population. Gaps in access could be worsened by specialty facilities with adolescent treatment programs being less likely to provide MOUD than facilities serving adults.43 Our findings support calls for additional MOUD engagement and retention strategies tailored for youths.44,45 Furthermore, older adults were less likely than young adults to receive MOUD, with most receiving no treatment at all. Misconceptions about substance use in older age alongside lower screening/assessment rates46,47 may contribute to the observed low OUD treatment rates.
Medication for OUD was lower among women after accounting for need and enabling characteristics. While this contrasts with previous literature that did not find differences by sex in OUD treatment use patterns more broadly,29 our findings were consistent with past work focused on MOUD.25 Our ability to detect statistical differences by race and ethnicity was limited because most people in the sample identified as non-Hispanic White, but MOUD use appeared racially patterned. Nearly one-third of non-Hispanic White people with OUD treatment need received MOUD, compared with approximately 20% of people identifying as non-Hispanic Black or other non-Hispanic or multiracial groups and 15% of Hispanic people. In contrast, roughly similar proportions of each racial and ethnic group received non-MOUD services, revealing substantial gaps specifically for MOUD access among people of color. In light of evidence showing faster growth in overdose death rates for minoritized groups48 and disparities in MOUD by community-level racial and ethnic composition,49 structural interventions that increase equitable MOUD access and retention are needed.50
Public insurance was an important enabling characteristic associated with MOUD, and sensitivity analyses showed that this association was driven by Medicaid. Therefore, policies that increase Medicaid coverage could be a key population-level strategy to enable MOUD.50 While all 50 states have Medicaid coverage for buprenorphine, as of 2018, only 42 states had Medicaid coverage for methadone.51 Starting in 2020, the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act mandated that Medicaid cover all 3 US Food and Drug Administration–approved medications for OUD, including methadone in certified opioid treatment programs.52 This important change could further increase MOUD in the publicly insured population because removing structural barriers, such as prior authorization policies,53 are important steps to increase MOUD use. The strong association of Medicaid coverage with MOUD could explain, in part, associations between lower income and MOUD, considering Medicaid is the primary source of insurance for low-income individuals in the US. These findings add to evidence highlighting the important role of public insurance in facilitating access to care for marginalized groups. However, our study shows that substantial gaps remain even among publicly insured people, which composed more than half of our sample.
While geography is associated with unequal distribution of MOUD prescribers,54,55 we found no differences by urbanicity for MOUD compared with no treatment. However, living in a small metropolitan area was associated with lower likelihood of MOUD compared with non-MOUD services. Individuals who receive treatment may have greater access to MOUD in urban areas with higher concentrations of prescribers, despite indications of county-level increases in buprenorphine prescribers across all categories of rurality.56 Growth in the number of clinicians with US Drug Enforcement Administration waivers required to prescribe buprenorphine is an important step to improve MOUD access, but more work is needed to increase prescribing rates among qualified clinicians57,58,59,60 and align prescribing practices with clinical guidelines.61
We found that health care and criminal legal system contacts were common, yet most people encountering these systems reported receiving no MOUD, highlighting systemic gaps and continued missed opportunities to increase MOUD uptake. Engaging people in care and initiating MOUD are the first stages in the OUD continuum of care and necessary to achieve the reductions in mortality and adverse opioid-related outcomes associated with MOUD retention.8,25 More than 80% had at least 1 general health care encounter, yet only 30% reported receiving MOUD. In a 2020 study,46 discussions about drug use with health care clinicians were associated with drug treatment use and perceived treatment need, indicating that relatively low-threshold interventions could potentially increase treatment uptake, yet these discussions were rare. Our findings provide further evidence that investments are needed to increase MOUD prescribing and referrals in ambulatory settings. Similarly, more than half of our sample reported a past-year emergency department visit, yet fewer than one-third of them reported receiving MOUD, supporting growing efforts to overcome barriers in implementing hospital-based MOUD induction and warm handoffs to community health care professionals.62,63,64 Consistent with past research,65 we found that criminal legal contact was associated with MOUD above and beyond other need, enabling, or predisposing characteristics. This could reflect mandated treatment or the continued criminalization of people who use drugs without necessarily linking people to treatment services. While we could not distinguish treatment referrals, many reports indicate low MOUD access through criminal legal settings.19,66 Strategies that do not require criminal legal contact to access drug treatment generally and MOUD specifically are needed to reinforce equitable community-based treatment access.
Limitations
This study has limitations. While the NSDUH used audio computer-assisted self-interviewing to increase reporting of sensitive information and reduce social desirability bias, self-reported data may nonetheless underestimate drug use, particularly heroin.67,68,69 Our OUD treatment need inclusion definition was tailored to be OUD-specific, yet we may have missed people owing to data limitations,70 such as individuals with multiple past-year treatment episodes if the last episode treated a different substance. Because most people received no treatment, we expect this would be a small minority. Findings may not generalize to groups excluded from the survey, including institutionalized people in correctional settings who are disproportionately composed of racial and ethnic minoritized groups. Although we could not ascertain OUD treatment need and receipt for nonparticipating individuals, the NSDUH is the only available national data set measuring MOUD, making it an important source for national estimates. Findings should be interpreted alongside other OUD treatment need and MOUD indicators available. In addition, we could not differentiate the type of MOUD (eg, methadone vs buprenorphine) and call for future studies with restricted data access to examine differences by medication type.
Conclusions
Despite strong evidence that medication is the most effective treatment for OUD and high rates of contact with the health care system, all adolescents and most adults with OUD treatment need in this study reported no past-year MOUD use. An important first step in understanding correlates of MOUD use in the general US population, this nationally representative study revealed critical gaps in treatment engagement and MOUD use, suggesting that increased efforts to address barriers to evidence-based care are warranted. Individuals who received MOUD differed from those who received no past-year drug treatment not only in terms of clinical need but also in terms of predisposing and enabling characteristics, highlighting a need for interventions and policies to increase MOUD uptake. Because most people encountered the health care and criminal legal systems, results suggest a need for cross-system integrated interventions to increase MOUD uptake.
eMethods.
eTable 1. Sociodemographic Characteristics of Adults and Adolescents by Past-Year Treatment Utilization, 2019
eTable 2. Sociodemographic Characteristics of Adults Ages 18 and Older With Past-Year OUD Treatment Need, 2019
eTable 3. Likelihood of MOUD Treatment Among Adults With Past-Year OUD Treatment Need, Including Criminal Legal System Exposure
References
- 1.Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013-2019. MMWR Morb Mortal Wkly Rep. 2021;70(6):202-207. doi: 10.15585/mmwr.mm7006a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gomes T, Tadrous M, Mamdani MM, Paterson JM, Juurlink DN. The burden of opioid-related mortality in the United States. JAMA Netw Open. 2018;1(2):e180217-e180217. doi: 10.1001/jamanetworkopen.2018.0217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. doi: 10.1136/bmj.f174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Intern Med. 2018;169(3):137-145. doi: 10.7326/M17-3107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database of Syst Rev. 2014(2):CD002207. doi: 10.1002/14651858.CD002207.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies–tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063-2066. doi: 10.1056/NEJMp1402780 [DOI] [PubMed] [Google Scholar]
- 7.Krawczyk N, Mojtabai R, Stuart EA, et al. Opioid agonist treatment and fatal overdose risk in a state-wide US population receiving opioid use disorder services. Addiction. 2020;115(9):1683-1694. doi: 10.1111/add.14991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samples H, Williams AR, Crystal S, Olfson M. Impact of long-term buprenorphine treatment on adverse health care outcomes In Medicaid. Health Aff (Millwood). 2020;39(5):747-755. doi: 10.1377/hlthaff.2019.01085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wakeman SE, Larochelle MR, Ameli O, et al. Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open. 2020;3(2):e1920622-e1920622. doi: 10.1001/jamanetworkopen.2019.20622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Askari MS, Martins SS, Mauro PM. Medication for opioid use disorder treatment and specialty outpatient substance use treatment outcomes: differences in retention and completion among opioid-related discharges in 2016. J Subst Abuse Treat. 2020;114:108028. doi: 10.1016/j.jsat.2020.108028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Timko C, Schultz NR, Cucciare MA, Vittorio L, Garrison-Diehn C. Retention in medication-assisted treatment for opiate dependence: a systematic review. J Addict Dis. 2016;35(1):22-35. doi: 10.1080/10550887.2016.1100960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hadland SE, Bagley SM, Rodean J, et al. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. JAMA Pediatr. 2018;172(11):1029-1037. doi: 10.1001/jamapediatrics.2018.2143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huhn AS, Hobelmann JG, Strickland JC, et al. Differences in availability and use of medications for opioid use disorder in residential treatment settings in the United States. JAMA Netw Open. 2020;3(2):e1920843-e1920843. doi: 10.1001/jamanetworkopen.2019.20843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGinty EE, Stone EM, Kennedy-Hendricks A, Bachhuber MA, Barry CL. Medication for opioid use disorder: a national survey of primary care physicians. Ann Intern Med. 2020;173(2):160-162. doi: 10.7326/M19-3975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mojtabai R, Mauro C, Wall MM, Barry CL, Olfson M. Medication treatment for opioid use disorders in substance use treatment facilities. Health Aff (Millwood). 2019;38(1):14-23. doi: 10.1377/hlthaff.2018.05162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barry CL, McGinty EE, Pescosolido BA, Goldman HH. Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness. Psychiatr Serv. 2014;65(10):1269-1272. doi: 10.1176/appi.ps.201400140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kennedy-Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, McGinty EE. Social stigma toward persons with prescription opioid use disorder: associations with public support for punitive and public health-oriented policies. Psychiatr Serv. 2017;68(5):462-469. doi: 10.1176/appi.ps.201600056 [DOI] [PubMed] [Google Scholar]
- 18.Stone EM, Kennedy-Hendricks A, Barry CL, Bachhuber MA, McGinty EE. The role of stigma in U.S. primary care physicians’ treatment of opioid use disorder. Drug Alcohol Depend. 2021;221:108627. doi: 10.1016/j.drugalcdep.2021.108627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mantha S, Mauro PM, Mauro CM, Martins SS. State criminal justice policy context and opioid agonist treatment delivery among opioid treatment admissions, 2015. Drug Alcohol Depend. 2020;206:107654. doi: 10.1016/j.drugalcdep.2019.107654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feder KA, Krawczyk N, Saloner B. Medication-assisted treatment for adolescents in specialty treatment for opioid use disorder. J Adolesc Health. 2017;60(6):747-750. doi: 10.1016/j.jadohealth.2016.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olfson M, Zhang VS, Schoenbaum M, King M. Trends in buprenorphine treatment in the United States, 2009-2018. JAMA. 2020;323(3):276-277. doi: 10.1001/jama.2019.18913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krans EE, Kim JY, James AE III, Kelley D, Jarlenski MP. Medication-assisted treatment use among pregnant women with opioid use disorder. Obstet Gynecol. 2019;133(5):943-951. doi: 10.1097/AOG.0000000000003231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donohue JM, Jarlenski MP, Kim JY, et al. ; Medicaid Outcomes Distributed Research Network (MODRN) . Use of medications for treatment of opioid use disorder among US medicaid enrollees in 11 states, 2014-2018. JAMA. 2021;326(2):154-164. doi: 10.1001/jama.2021.7374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gordon AJ, Lo-Ciganic WH, Cochran G, et al. Patterns and quality of buprenorphine opioid agonist treatment in a large medicaid program. J Addict Med. 2015;9(6):470-477. doi: 10.1097/ADM.0000000000000164 [DOI] [PubMed] [Google Scholar]
- 25.Morgan JR, Schackman BR, Leff JA, Linas BP, Walley AY. Injectable naltrexone, oral naltrexone, and buprenorphine utilization and discontinuation among individuals treated for opioid use disorder in a United States commercially insured population. J Subst Abuse Treat. 2018;85:90-96. doi: 10.1016/j.jsat.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haffajee RL, Lin LA, Bohnert ASB, Goldstick JE. Characteristics of US counties with high opioid overdose mortality and low capacity to deliver medications for opioid use disorder. JAMA Netw Open. 2019;2(6):e196373-e196373. doi: 10.1001/jamanetworkopen.2019.6373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matusow H, Dickman SL, Rich JD, et al. Medication assisted treatment in US drug courts: results from a nationwide survey of availability, barriers and attitudes. J Subst Abuse Treat. 2013;44(5):473-480. doi: 10.1016/j.jsat.2012.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bronson J, Stroop J, Zimmer S, Berzofsky M. Drug Use, Dependence, and Abuse Among State Prisoners and Jail Inmates, 2007-2009. Bureau of Justice Statistics, Office of Justice Programs, U.S. Department of Justice; 2017, NCJ 250546. [Google Scholar]
- 29.Wu LT, Zhu H, Swartz MS. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend. 2016;169:117-127. doi: 10.1016/j.drugalcdep.2016.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saloner B, Karthikeyan S. Changes in substance abuse treatment use among individuals with opioid use disorders in the United States, 2004-2013. JAMA. 2015;314(14):1515-1517. doi: 10.1001/jama.2015.10345 [DOI] [PubMed] [Google Scholar]
- 31.Substance Abuse and Mental Health Services Administration . Key Substance Use And Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020. [Google Scholar]
- 32.Mark TL, Dilonardo J, Vandivort R, Miller K. Psychiatric and medical comorbidities, associated pain, and health care utilization of patients prescribed buprenorphine. J Subst Abuse Treat. 2013;44(5):481-487. doi: 10.1016/j.jsat.2012.11.004 [DOI] [PubMed] [Google Scholar]
- 33.Center for Behavioral Health Statistics and Quality . 2019 National Survey on Drug Use and Health: Methodological Summary and Definitions. Substance Abuse and Mental Health Services Administration; 2020. [Google Scholar]
- 34.Jordan BK, Karg RS, Batts KR, Epstein JF, Wiesen C. A clinical validation of the National Survey on Drug Use and Health assessment of substance use disorders. Addict Behav. 2008;33(6):782-798. doi: 10.1016/j.addbeh.2007.12.007 [DOI] [PubMed] [Google Scholar]
- 35.Substance Abuse and Mental Health Services Administration . Reliability of Key Measures in the National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration; 2010. [PubMed] [Google Scholar]
- 36.Center for Behavioral Health Statistics and Quality . 2019 National Survey on Drug Use and Health (NSDUH): Methodological Resource Book, Section 8, Data Collection Final Report. Substance Abuse and Mental Health Services Administration; 2020. [Google Scholar]
- 37.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800-804. doi: 10.1097/EDE.0b013e3181577654 [DOI] [PubMed] [Google Scholar]
- 38.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Publishing, Inc; 1994. [Google Scholar]
- 39.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10. doi: 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- 40.Krawczyk N, Williams AR, Saloner B, Cerdá M. Who stays in medication treatment for opioid use disorder? a national study of outpatient specialty treatment settings. J Subst Abuse Treat. 2021;126:108329. doi: 10.1016/j.jsat.2021.108329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001-2014. JAMA Pediatr. 2017;171(8):747-755. doi: 10.1001/jamapediatrics.2017.0745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Squeglia LM, Fadus MC, McClure EA, Tomko RL, Gray KM. Pharmacological treatment of youth substance use disorders. J Child Adolesc Psychopharmacol. 2019;29(7):559-572. doi: 10.1089/cap.2019.0009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alinsky RH, Hadland SE, Matson PA, Cerda M, Saloner B. Adolescent-serving addiction treatment facilities in the United States and the availability of medications for opioid use disorder. J Adolesc Health. 2020;67(4):542-549. doi: 10.1016/j.jadohealth.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Borodovsky JT, Levy S, Fishman M, Marsch LA. Buprenorphine treatment for adolescents and young adults with opioid use disorders: a narrative review. J Addict Med. 2018;12(3):170-183. doi: 10.1097/ADM.0000000000000388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Camenga DR, Colon-Rivera HA, Muvvala SB. Medications for maintenance treatment of opioid use disorder in adolescents: a narrative review and assessment of clinical benefits and potential risks. J Stud Alcohol Drugs. 2019;80(4):393-402. doi: 10.15288/jsad.2019.80.393 [DOI] [PubMed] [Google Scholar]
- 46.Mauro PM, Samples H, Klein KS, Martins SS. Discussing drug use with health care providers is associated with perceived need and receipt of drug treatment among adults in the United States: we need to talk. Med Care. 2020;58(7):617-624. doi: 10.1097/MLR.0000000000001340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mauro PM, Askari MS, Han BH. Gender differences in any alcohol screening and discussions with providers among older adults in the United States, 2015 to 2019. Alcohol Clin Exp Res. 2021;45(9):1812-1820. doi: 10.1111/acer.14668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Furr-Holden D, Milam AJ, Wang L, Sadler R. African Americans now outpace whites in opioid-involved overdose deaths: a comparison of temporal trends from 1999 to 2018. Addiction. 2021;116(3):677-683. doi: 10.1111/add.15233 [DOI] [PubMed] [Google Scholar]
- 49.Stein BD, Dick AW, Sorbero M, et al. A population-based examination of trends and disparities in medication treatment for opioid use disorders among Medicaid enrollees. Subst Abus. 2018;39(4):419-425. doi: 10.1080/08897077.2018.1449166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Andraka-Christou B. Addressing racial and ethnic disparities in the use of medications for opioid use disorder. Health Aff (Millwood). 2021;40(6):920-927. doi: 10.1377/hlthaff.2020.02261 [DOI] [PubMed] [Google Scholar]
- 51.Substance Abuse and Mental Health Services Administration . Medicaid Coverage of Medication-Assisted Treatment for Alcohol and Opioid Use Disorders and of Medication for the Reversal of Opioid Overdose. Substance Abuse and Mental Health Services Administration; 2018. [Google Scholar]
- 52.Costello AM. Mandatory Medicaid State Plan Coverage of Medication-Assisted Treatment. Centers for Medicare & Medicaid. December 30, 2020. Accessed October 28, 2021. https://www.medicaid.gov/federal-policy-guidance/downloads/sho20005.pdf [Google Scholar]
- 53.Mark TL, Parish WJ, Zarkin GA. Association of formulary prior authorization policies with buprenorphine-naloxone prescriptions and hospital and emergency department use among Medicare beneficiaries. JAMA Netw Open. 2020;3(4):e203132. doi: 10.1001/jamanetworkopen.2020.3132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Andrilla CHA, Moore TE, Patterson DG, Larson EH. Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: a 5-year update. J Rural Health. 2019;35(1):108-112. doi: 10.1111/jrh.12307 [DOI] [PubMed] [Google Scholar]
- 55.Saloner B, Lin L, Simon K. Geographic location of buprenorphine-waivered physicians and integration with health systems. J Subst Abuse Treat. 2020;115:108034. doi: 10.1016/j.jsat.2020.108034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Andrilla CHA, Patterson DG. Tracking the geographic distribution and growth of clinicians with a DEA waiver to prescribe buprenorphine to treat opioid use disorder. J Rural Health. 2022;38(1):87-92. doi: 10.1111/jrh.12569 [DOI] [PubMed] [Google Scholar]
- 57.Abraham AJ, Andrews CM, Harris SJ, Friedmann PD. Availability of medications for the treatment of alcohol and opioid use disorder in the USA. Neurotherapeutics. 2020;17(1):55-69. doi: 10.1007/s13311-019-00814-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thomas CP, Doyle E, Kreiner PW, et al. Prescribing patterns of buprenorphine waivered physicians. Drug Alcohol Depend. 2017;181:213-218. doi: 10.1016/j.drugalcdep.2017.10.002 [DOI] [PubMed] [Google Scholar]
- 59.Jones CM, McCance-Katz EF. Characteristics and prescribing practices of clinicians recently waivered to prescribe buprenorphine for the treatment of opioid use disorder. Addiction. 2019;114(3):471-482. doi: 10.1111/add.14436 [DOI] [PubMed] [Google Scholar]
- 60.Stein BD, Saloner B, Schuler MS, Gurvey J, Sorbero M, Gordon AJ. Concentration of patient care among buprenorphine-prescribing clinicians in the US. JAMA. 2021;325(21):2206-2208. doi: 10.1001/jama.2021.4469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Volkow ND, Jones EB, Einstein EB, Wargo EM. Prevention and treatment of opioid misuse and addiction: a review. JAMA Psychiatry. 2019;76(2):208-216. doi: 10.1001/jamapsychiatry.2018.3126 [DOI] [PubMed] [Google Scholar]
- 62.D’Onofrio G, Edelman EJ, Hawk KF, et al. Implementation facilitation to promote emergency department-initiated buprenorphine for opioid use disorder: protocol for a hybrid type III effectiveness-implementation study (Project ED HEALTH). Implement Sci. 2019;14(1):48. doi: 10.1186/s13012-019-0891-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim HS, Samuels EA. Overcoming barriers to prescribing buprenorphine in the emergency department. JAMA Netw Open. 2020;3(5):e204996-e204996. doi: 10.1001/jamanetworkopen.2020.4996 [DOI] [PubMed] [Google Scholar]
- 64.Kilaru AS, Lubitz SF, Davis J, et al. A state financial incentive policy to improve emergency department treatment for opioid use disorder: a qualitative study. Psychiatr Serv. 2021;72(9):1048-1056. doi: 10.1176/appi.ps.202000501 [DOI] [PubMed] [Google Scholar]
- 65.Cook BL, Alegría M. Racial-ethnic disparities in substance abuse treatment: the role of criminal history and socioeconomic status. Psychiatr Serv. 2011;62(11):1273-1281. doi: 10.1176/ps.62.11.pss6211_1273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Krawczyk N, Picher CE, Feder KA, Saloner B. Only one in twenty justice-referred adults in specialty treatment for opioid use receive methadone or buprenorphine. Health Aff (Millwood). 2017;36(12):2046-2053. doi: 10.1377/hlthaff.2017.0890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Midgette G, Caulkins JP, Reuter P. Pathways to drug prevalence estimation: synthesizing three comments on triangulation. Addiction. 2021;116(10):2615-2616. doi: 10.1111/add.15607 [DOI] [PubMed] [Google Scholar]
- 68.Reuter P, Caulkins JP, Midgette G. Heroin use cannot be measured adequately with a general population survey. Addiction. 2021;116(10):2600-2609. doi: 10.1111/add.15458 [DOI] [PubMed] [Google Scholar]
- 69.Radhakrishnan K. Significance of integration and use of multiple data sources for understanding substance use and mental health disorders. Addiction. 2021;116(10):2611-2613. doi: 10.1111/add.15562 [DOI] [PubMed] [Google Scholar]
- 70.Nesoff ED, Martins SS, Palamar JJ. Caution is necessary when estimating treatment need for opioid use disorder using national surveys. Am J Public Health. 2022;112(2):199-201. doi: 10.2105/AJPH.2021.306624 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Sociodemographic Characteristics of Adults and Adolescents by Past-Year Treatment Utilization, 2019
eTable 2. Sociodemographic Characteristics of Adults Ages 18 and Older With Past-Year OUD Treatment Need, 2019
eTable 3. Likelihood of MOUD Treatment Among Adults With Past-Year OUD Treatment Need, Including Criminal Legal System Exposure