Abstract
Inpatient falls are frequently reported incidents in hospitals around the world. The recent COVID-19 pandemic has further exacerbated the risk. With the rising importance of human factors and ergonomics (HF&E), a fall prevention programme was introduced by applying HF&E principles to reduce inpatient falls from a systems engineering perspective. The programme was conducted in an acute public hospital with around 750 inpatient beds in Hong Kong. A hospital falls review team (the team) was formed in June 2020 to plan and implement the programme. The ‘Define, Measure, Analyse, Improve and Control’ (DMAIC) method was adopted. Improvement actions following each fall review were implemented. Fall rates in the ‘pre-COVID-19’ period (January–December 2019), ‘COVID-19’ period (January–June 2020) and ‘programme’ period (July 2020–August 2021) were used for evaluation of the programme effectiveness. A total of 120, 85 and 142 inpatient falls in the ‘pre-COVID-19’, ‘COVID-19’ and ‘programme’ periods were reviewed, respectively. Thirteen areas with fall risks were identified by the team where improvement actions applying HF&E principles were implemented accordingly. The average fall rates were 0.476, 0.773 and 0.547 per 1000 patient bed days in these periods, respectively. The average fall rates were found to be significantly increased from the pre-COVID-19 to COVID-19 periods (mean difference=0.297 (95% CI 0.068 to 0.526), p=0.009), which demonstrated that the COVID-19 pandemic might have affected the hospitals fall rates, while a significant decrease was noted between the COVID-19 and programme periods (mean difference=−0.226 (95% CI −0.449 to –0.003), p=0.047), which proved that the programme in apply HF&E principles to prevent falls was effective. Since HF&E principles are universal, the programme can be generalised to other healthcare institutes, which the participation of staff trained in HF&E in the quality improvement team is vital to its success.
Keywords: human factors, patient safety, quality improvement, risk management
Problem
Inpatient falls are frequently reported incidents in hospitals around the world. Studies showed that falls of hospitalised patients could be as high as 3.44 falls per 1000 patient days in the USA and 6.63 falls per 1000 occupied bed days in the UK.1 2 Regardless of injuries, most patients who fall would have increased length of hospital stay leading to increased medical costs.3 Patients and relatives may also lodge complaints bringing up litigation issues about hospital services and staff competence and as a result affecting the reputation of the hospital and their trust with staff.4
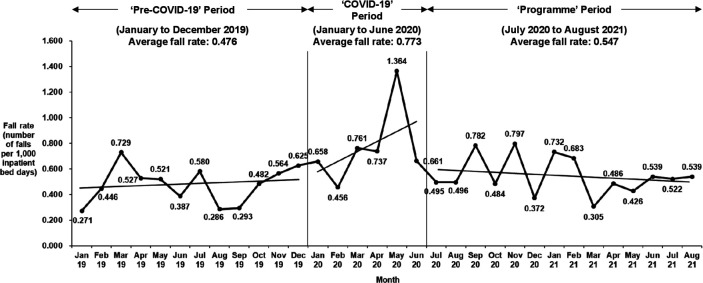
The average inpatient fall rate in the hospital of this study was 0.630 per 1000 patient bed days from January 2019 to June 2020. Since the COVID-19 pandemic had been affecting the healthcare services of Hong Kong since January 2020, further analysis found the fall rate before the COVID-19 pandemic was 0.476 (the ‘pre-COVID-19’ period from January to December 2019) and since the COVID-19 pandemic was 0.773 (the ‘COVID-19’ period from January to June 2020 before the introduction of the quality improvement programme). This indicated that the COVID-19 pandemic might have an effect in increasing falls in the hospital.
The hospital management was concerned about the increased fall rates, which might increase patients’ length of stay and affect the capacity to admit other patients in need. The hospital’s reputation would also be affected when patient complaints were brought to media reports. In this regard, a falls review team (the team) was formed in June 2020 to introduce a quality improvement programme aiming to reduce inpatient falls.
The objective of this programme was to apply HF&E principles to reduce inpatient falls by applying a systems engineering approach. The existing gaps in falls prevention by reviewing past inpatient falls were reviewed and interventions for quality improvement were proposed and carried out by the team.
Background
About 20%–30% of falls are preventable.4 Many researches have been analysing the risk factors of inpatient falls.4 5 In general, they can be divided into intrinsic and extrinsic factors. Intrinsic factors are related to the patient’s physical states and conditions including fall history, age, mobility, mental status, medication use and intention to seek assistance, while extrinsic factors are related to the external environment surrounding the patient that include the use of bed rails, walking aids, footwear, the access to items and toilet location.6 7 The overall risk of an inpatient fall is affected by all these variables. Also, the recent COVID-19 pandemic has exacerbated patient safety risks including falls. Though there were no abundant validated research data on evaluating the consequence of COVID-19 to falls, there had been reports of experiences in increased falls during the COVID-19 period.8–11
Traditionally, falls prevention strategies including fall risk screening and assessment, patient education, provision of walking aids and bed rails are some common ones to name.6 12 It is not uncommon to see that these falls prevention interventions are implemented in a bundle in healthcare institutions since single intervention is not effective to prevent falls.4 13 Also, the interventions’ effectiveness is limited by the patients’ judgement and cooperation, the misalignment of their perception on the risk of fall and their worsening illnesses, as well as the latent systems factors including staffing, environment, equipment and workflow design.14 15 All these factors behind affect the effectiveness of falls prevention intervention resulting in falls remaining to be a difficult problem to treat.
Human factors and ergonomics (HF&E) has become a more widely adopted discipline in healthcare.16 It has been applied to improve patient safety in different areas including medication safety, infection control, medical equipment design and surgical safety.17–20 HF&E is a scientific and evidence-based profession that aims to enhance human performance by understanding the capabilities and limitations of humans and the interactions between humans and surrounding systems. HF&E uses a systems engineering approach to examine the design to the tools, software, furniture, workplaces and environments and improve human performance and prevent incidents. A human factors specialist applies various HF&E principles, for example, systems thinking, action hierarchy and product design principles, and skills and techniques, for example, task analysis, workload analysis and anthropometric measurements, to investigate use errors and designs flaws and support improvements at the systems level.16 21 It is believed that HF&E can be applied to falls prevention by using the previous principles and techniques to identify different design flaws of the system and implement improvement actions to prevent falls.
Measurement
The public healthcare services in Hong Kong is governed by the Hong Kong Hospital Authority (HA). The hospital involved in this quality improvement programme was one of the HA acute hospitals, which had around 750 inpatient beds and was located in the northwest region of Hong Kong.
The performance of inpatient falls was measured by the incident rates reported to the HA Advance Incident Reporting System (AIRS) by wards. The AIRS is an electronic system that all staff in HA can report incidents voluntarily. As a requirement of the nursing management, ward staff have to report all falls to the AIRS, which allows a more accurate database of falls for the team for evaluation.
The fall rates (number of falls per 1000 patient bed days) of the hospital from January 2019 to June 2020 were used as the baseline data. Since the COVID-19 pandemic had been affecting the healthcare services of Hong Kong since January 2020, the baseline data were divided into ‘pre-COVID-19’ period (from January to December 2019) and ‘COVID-19’ period (from January to June 2020) to examine whether the COVID-19 pandemic had any effects on the fall rates. The effectiveness of the programme was evaluated by comparing the fall rates between the pre-programme period (‘pre-COVID-19’ and ‘COVID-19’ periods) and the ‘programme' period (from July 2020 to August 2021).
One-way analysis of variance with post hoc tests and χ2 test or Fisher’s exact test were used to evaluate if there were any changes in fall rates and demographics of falls in the three periods, respectively. Statistical significance was considered when the p value was less than 0.05. The data were analysed using SPSS V.26.
Design
The hospital falls review team was formed in June 2020 to plan and introduce the falls prevention programme. The team composed of geriatrician, nurses, physiotherapists, occupational therapist, human factors specialist (a hospital patient safety officer chartered in HF&E) and administrators. The team was led by the geriatrician, while other members provided advice on falls prevention from their professional aspects and supported the implementation of interventions. The human factors specialist supported the team to focus its observations, discussion and actions on the systems perspective instead of solely the staff or patient factors. The administrators supported the coordination of fall visits and regular team meetings, documented the observations and discussion made between the team and frontline staff during the visits and performed data analysis.
The common quality improvement model Plan, Do, Study, Act (PDSA) cycle was not used in this programme because this programme adopted a continuous improvement process that improvement actions were taken immediately after reviewing each fall. While problems identified in different falls were complex, and the improvement actions were implemented swiftly across all wards in the hospital, the use of the PDSA model would become complicated to the team at both the operational and planning levels.22 It was not practical to evaluate the effectiveness of a single improvement action as several actions were often implemented at the same time which their effectiveness was reflected in the overall fall rates. As such, the team had adopted the Six Sigma improvement model of ‘Define, Measure, Analyse, Improve and Control’ (DMAIC) to ensure a structured methodology was in place in the programme.
A retrospective analysis of 120 and 85 falls occurred in the hospital in the ‘pre-COVID-19’ and ‘COVID-19’ periods, respectively, was conducted by the team. Case detail of falls reported to the AIRS was analysed. Also, to facilitate the team in understanding the ward environment, additional visits were conducted separately to examine the environmental, equipment and task design. The observations were categorised according to the Framework on Interventions for Inpatient Falls (the framework) illustrated by Hignett, an expert in human factors.6 This framework provided clear and structured descriptions of elements on fall assessment and prevention that matched with the existing fall preventive measures carrying out in the hospital. The analysis results were categorised into five areas based on the domains of the framework, namely ‘assessment’, ‘communication’, ‘monitoring’, ‘patient’ and ‘environment’.
Strategy
The falls prevention programme was commenced in July 2020. At the initial stage, all observations with areas for improvement identified in the retrospective analysis were discussed by the team for possible interventions and standardisation across all clinical departments.
For falls occurred after the programme commencement, when an inpatient fall in the hospital was reported to the AIRS, a senior nursing officer (to provide clinical and nursing advice), the human factors specialist (to provide HF&E advice) and an administrator (to record the observations) from the team conducted a short visit for about 10–15 min to the ward on the incident day or the next working day. The elements on each category of the framework was used by the visiting members as quick prompts of areas to inspect. The visiting members reviewed and discussed with ward staff about the fall preventive measures applied on the patient. The visit reviewed the patient records related to falls prevention and postfall management (eg, whether the fall screening on admission was appropriate, the communication among staff was adequate, the advice by physiotherapist or occupational therapist was followed), the incident location of the patient fallen, and the design and usability of any falls prevention equipment (eg, if the fall alarm mat was properly used). The team also interviewed the fallen patient (if the patient had not been discharged and was in stable physical and mental conditions) to learn about the fall detail like the movement or activity during the fall. The gaps between the observations and the hospital falls prevention and management policy were identified. Immediate feedback for any quick fix would be provided by the visiting members to the ward managers for consideration in their departmental meetings.
The team also conducted special visits to inpatient wards (both in service and under renovation) to assess the equipment, environmental and workflow design on falls prevention when requested by clinical departments.
All observations of each fall in the fall visits would be summarised into a ‘fall summary’ for discussion in the team’s monthly meetings through a multidisciplinary approach. The team discussed all falls and ‘fall summaries’ to decide whether each fall was preventable. A preventable fall indicated that there were opportunities for systems improvement and vice versa for non-preventable ones. The departmental representatives in the team would also share their work progress and concerns in the meetings. The observations from the special visits were also followed.
All proposed interventions at the ward level were discussed with the ward managers, and implementation would be conducted if deemed to be feasible. Interventions that were hospital wide, required support from the hospital management, or required a long-term planning, were discussed in the Hospital Liaison Committee, chaired by the hospital chief executive, as well as other senior staff meetings. Follow-up ward visits were conducted by the team and reported in subsequent team meetings to monitor the implementation progresses of each intervention.
Results
A total of 120, 85 and 142 inpatient falls in the ‘pre-COVID-19’, ‘COVID-19’ and ‘programme’ periods were reviewed, respectively. Thirteen areas of observations were identified by the Team. Each observation with its associated fall risk, the actions taken and the HF&E knowledge areas applied on each intervention were summarised in online supplemental table 1. When reviewing the falls, the team adopted a systems approach such that most actions taken were believed to be generalisable to other departments or wards in the hospital. For example, in ‘Assessment’, the team reviewed the patients’ hospital fall screening forms and found in some falls that nurses had difficulty in knowing whether patients had recent fall histories, which might be caused by the lack of communication with patients or carers and the lack of clear documentation in the previous clinical notes. In this regard, this observation was shared in hospital committees’ meetings for further deliberation. The department representatives subsequently could remind their ward nurses to enhance the checking of patient’s previous fall history in their daily routine. All actions were agreed by the team before implementation.
bmjoq-2021-001696supp001.pdf (146.3KB, pdf)
The monthly and average fall rates in the ‘pre-COVID-19’, ‘COVID-19’ and ‘programme’ periods were shown in figure 1. The average fall rates were 0.476, 0.773 and 0.547 per 1000 patient bed days in the three periods, respectively. The average fall rates were found to be significantly increased from the ‘pre-COVID-19’ to ‘COVID-19’ periods (mean difference=0.297 (95% CI 0.068 to 0.526), p=0.009), while a significant decrease was noted between the ‘COVID-19’ and ‘programme’ periods (mean difference=−0.226 (95% CI −0.449 to –0.003), p=0.047). Table 1 summarised the demographics of falls in the three periods. The authors believed that the insignificant differences in the profiles might indicate that the changes in fall rates were likely caused by the COVID-19 pandemic effect and the falls prevention programme effectiveness. More researches to study the relationship between the intrinsic factors of patients and the COVID-19 pandemic effect on falls would be required in the future.
Figure 1.
Trend of fall rates in the hospital.
Table 1.
Demographics of falls in ‘pre-COVID-19’, ‘COVID-19’ and ‘programme’ periods
| ‘Pre-COVID-19’ period | ‘COVID-19’ period | ‘Programme’ period | P value* | ||
| January–December 2019 | January–June 2020 | July 2020–August 2021 | |||
| n (%) | n (%) | n (%) | |||
| Sex | Male | 70 (58) | 52 (61) | 84 (59) | 0.918 |
| Female | 50 (42) | 33 (39) | 58 (41) | ||
| Age group | 0–30 | 5 (4) | 2 (2) | 6 (4) | 0.956 |
| 31–50 | 9 (8) | 5 (6) | 9 (6) | ||
| 51–70 | 41 (34) | 31 (36) | 44 (31) | ||
| >70 | 65 (54) | 47 (55) | 83 (58) | ||
| Time of fall | 00:01–06:00 | 30 (25) | 23 (27) | 29 (20) | 0.506 |
| 06:01–12:00 | 28 (23) | 24 (28) | 35 (25) | ||
| 12:01–18:00 | 27 (23) | 23 (27) | 37 (26) | ||
| 18:01–00:00 | 35 (29) | 15 (18) | 41 (29) | ||
| Specialty of underlying clinical problem | Medical | 65 (54) | 49 (58) | 93 (65) | 0.345 |
| Surgical | 42 (35) | 25 (29) | 34 (24) | ||
| Emergency medicine | 13 (11) | 11 (13) | 15 (11) | ||
| Fall risk | Low risk | 54 (45) | 46 (55) | 59 (42) | 0.126 |
| High risk | 66 (55) | 37 (45) | 83 (58) | ||
| Location of fall | Patient bedside | 88 (74) | 69 (81) | 115 (81) | 0.815 |
| Patient cubicle | 3 (3) | 1 (1) | 3 (2) | ||
| Ward toilet | 15 (13) | 6 (7) | 9 (6) | ||
| Ward common Area | 11 (9) | 7 (8) | 13 (9) | ||
| Others | 3 (3) | 2 (2) | 2 (1) | ||
*Significant difference is considered when the p value is less than 0.05.
Lessons and limitations
The falls prevention programme demonstrated that HF&E principles could be applied to falls prevention. The actions taken in a bundled approach focused on the systems that the work system was strengthened and became more robust. The application of HF&E principles helps focusing the organisational factors and supporting human performance in the sociotechnical systems that good design is key instrument to success.23
From the HF&E perspective, the safety hierarchy model was an important principle to apply. The safety hierarchy model helped to identify stronger corrective actions, for example, architectural changes, equipment usability enhancement and standardisation, that modify the design of the work system, have a higher tendency to prevent incident recurrence and are more sustainable. However, weak actions like warnings, checking and trainings that tend to modify human behaviour are less effective.24 Although strong actions usually require higher cost and time to complete, the costs invested might be able to turn into savings over time.24 25 Therefore, aiming for the stronger actions was the key targets for improvement in the falls prevention programme. The team experienced that some interventions, for example, ward renovation and product design modification, required multidisciplinary support like the facilities management on hospital facility enhancement and may take time in terms of years to complete as they require longer consultation and planning processes to ensure the final design meets staff’s expectation and can be practically implemented. Balancing the time required to examine the outcome of these ‘long-term’ work, the ‘programme’ period was therefore selected to be 1 year long as an initial review of outcomes. Follow-up evaluations of the programme effectiveness should be considered.
Fostering a patient safety culture is another important HF&E principle to practice. The introduction of patient safety programmes is an effective means to achieve this, in particular strong leadership is the most crucial factor for the falls prevention programme to be successful.26 The formation of the team with multidisciplinary members of supervisory roles demonstrated leadership and commitment of the hospital to reduce inpatient falls. It was believed that the fall visits could enhance frontline staff’s awareness on falls prevention and management that professional advice was given by the visiting members. A follow-up survey to study the perception of frontline staff on the fall visits at the ward level is beneficial. The fall visits also allowed the visiting members to understand what had happened and made prompt and precise advice while frontline staff could directly express their concerns and difficulties to the team. This brought an opportunity for the team to examine the variations between work-as-imagined (what was expected to happen) and work-as-done (what actually happened) so that the interventions were down to earth and easier to be accepted by frontline staff.27 An example was the improved communication with patients in isolation rooms. Patients’ needs should be addressed promptly, and staff should approach them before they have fall-prone activities (work-as-imagined). In the fall visits, it was found that ward staff could not promptly talk to these patients because there was no active intercom system linked to the isolation rooms. The staff had to spend time to put on personal protective equipment before entering the isolation rooms (work-as-done), which patients might have left their bed before the staff entered the isolation rooms.15 Therefore, the team liaised with the hospital facilities management unit to replace the intercom system to enhance the communication process. This improvement demonstrated the importance of understanding human behaviour and examining the work-as-imagined and work-as-done in preventing falls.
With the advancement in technology, fall prediction systems and prevention devices become popular in falls prevention. Motion detectors, floor or bed alarm mats and prediction models are the latest innovations to date.6 28–32 These technologies help enhance work performance by supporting patient monitoring and predicting patients’ behaviour so that staff can promptly attend to patients when they are at risk of fall.32 Nevertheless, they have to be carefully evaluated in terms of usability, efficiency and user satisfaction.28–31 For example, in the falls prevention programme, patients eligible for using bed alarm mats had to be cautiously selected because if they were applied on patients requiring walking assistance who could go to toilet by himself or herself, the frequent false alarms would induce disturbance to staff. The staff might feel fatigue and eventually ignore the alarms when they find most patients did not require any assistance. The decision making in selecting the best eligible patients might also increase their cognitive workload that, in turn, reduce their willingness to use the mats.32 Further HF&E researches on how the design of user interface, display and workflow affects the workload and user experience should be conducted.
Traditionally, fall risk screening by using tools like Morse Fall Scale is the first step in fall prevention.4 33 How to ensure an accuracy and effective fall screening is a difficult challenge. The knowledge and compliance of nurses and their clinical judgement would affect the accuracy and increase the probability of underestimating or overestimating fall risks.34 35 The problem with an underestimated fall risk would lead to inadequate support including subsequent assessment for differential diagnosis and individualised care plan they need.36 Also, when patients are identified to be at high fall risk, staff tend to focus their attention and resources in monitoring these patients. On the other side of the coin, low fall risk patients become the blind spot area on falls prevention.35 37 Before commencing the falls prevention programme, only patients who fell and had severe injuries like fractures were visited by nursing staff. These led to an incomplete understanding of each fall and reduced learning opportunities for systems improvement. The falls prevention programme strengthened the analysis from selected cases to all falls so that fall preventive measures could be more generic and applicable to all patients in the hospital.
This study also evaluated if the COVID-19 pandemic had affected the effectiveness of fall preventive measures in the hospital. Although there were only 6-month data, the team believed that the increase in fall rates in the ‘COVID-19’ period might be caused by factors such as poorer morbidity of patients, more stringent infection control requirements (eg, more time is required for donning personal protective equipment), increased dependency from patients, lack of line of sight due to assignment of patients in isolation rooms, reduced frequency in ward rounds, limited patient contact time, restrictions on visiting, increased staff absence and elevated work stress.8 11 38 39 The comparison of fall rates between the ‘COVID-19’ and ‘programme’ periods aimed to balance out the effects of these factors as falls in both periods were within the COVID-19 pandemic timeframe. From the results, the significant reduction of fall rates between the ‘COVID-19’ and ‘programme’ periods proved that the falls prevention programme was successful in preventing inpatient falls. Nevertheless, confounding factors that might have affected the fall rates over the time have to be taken into account, including changes in clinical practice and staff’s resilience during the COVID-19 pandemic.40–43
This programme had some limitations. First, it was conducted in a single acute hospital. Whether the improvement actions are effective to prevent falls in other hospitals has to be further evaluated. However, since HF&E principles are universal and evidence based,18 20 the framework concepts are believed to be generalisable to other healthcare institutes. The team acknowledged that staff who was trained in HF&E are vital to properly evaluate the gaps and identify systems improvement actions throughout the programme. Second, only the fall rates were used as an outcome measure for evaluating the programme effectiveness. Understanding the perception of ward staff on the fall visits and workload of the team would be beneficial to evaluate the programme effectiveness in another angle. Third, the programme was introduced during the COVID-19 pandemic. The team believed that the fall rates might have been affected by the pandemic effect that further quantitative analysis is required to assess the actual effectiveness of the programme when the pandemic has gone down.
Conclusion
HF&E is a scientific and evidence-based discipline. It is proven to be useful in enhancing patient safety including falls. This report demonstrated how HF&E principles can be applied to assess and improve the design of the systems to prevent inpatient falls in a falls prevention programme. The results showed significant reduction of falls after the programme was commenced. Since HF&E principles are universal, it is believed that the programme applying HF&E principles can be generalised to other healthcare institutes, which the involvement of staff who have been trained in HF&E to conduct assessment, provide professional advice and implement interventions at the systems level is vital to the success.
Acknowledgments
The authors would like to thank the members of the falls review team in supporting this programme and Dr. Angus Chu, Chairperson of New Territories West Cluster Falls and Restraint Management Committee, in providing his valuable advice on falls prevention.
Footnotes
Contributors: YK was the guarantor of the study. YK and ML designed the quality improvement programme. YK conducted the analysis and wrote the manuscript. YK and ML approved the final manuscript. The hospital statistician had been consulted for data analysis and interpretation.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Approval from Research Ethics Committee, New Territories West Cluster, Hong Kong Hospital Authority, was obtained (reference no.: NTWC/REC/21050).
References
- 1.Royal College of physicians . National audit of inpatient falls: audit report. London, 2015. [Google Scholar]
- 2.Staggs VS, Mion LC, Shorr RI. Assisted and unassisted falls: different events, different outcomes, different implications for quality of hospital care. Jt Comm J Qual Patient Saf 2014;40:358–64. 10.1016/S1553-7250(14)40047-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morello RT, Barker AL, Watts JJ, et al. The extra resource burden of in-hospital falls: a cost of falls study. Med J Aust 2015;203:367. 10.5694/mja15.00296 [DOI] [PubMed] [Google Scholar]
- 4.Morris R, O'Riordan S. Prevention of falls in hospital. Clin Med 2017;17:360–2. 10.7861/clinmedicine.17-4-360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Najafpour Z, Godarzi Z, Arab M, et al. Risk factors for falls in hospital in-patients: a prospective nested case control study. Int J Health Policy Manag 2019;8:300–6. 10.15171/ijhpm.2019.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hignett S. Technology and building design initiatives in interventions to reduce the incidence and injuries of elderly in-patient falls. HERD 2010;3:93–105. [DOI] [PubMed] [Google Scholar]
- 7.Gu Y-Y, Balcaen K, Ni Y, et al. Review on prevention of falls in hospital settings. Chin Nur Research 2016;3:7–10. 10.1016/j.cnre.2015.11.002 [DOI] [Google Scholar]
- 8.De La Cámara Miguel Ángel, Jiménez-Fuente A, Pardos AI. Falls in older adults: the new pandemic in the post COVID-19 era? Med Hypotheses 2020;145:110321. 10.1016/j.mehy.2020.110321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adelman JS, Gandhi TK. COVID-19 and patient safety: time to TAP into our investment in high reliability. J Patient Saf 2021;17:331–3. 10.1097/PTS.0000000000000843 [DOI] [PubMed] [Google Scholar]
- 10.Liang S-C, Wei P-C, Ma H-L, et al. Higher fall rate of admitted patients during the ongoing COVID-19 epidemic: is it coincidence or not? J Patient Saf 2021;17:e45–6. 10.1097/PTS.0000000000000794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.HSJ . Covid pressures linked to increased fall rates and patient deaths [Internet] UK. Available: https://www.hsj.co.uk/patient-safety/covid-pressures-linked-to-increased-fall-rates-and-patient-deaths/7029440.article?adredir=1 [Accessed 21 June 2021].
- 12.Heng H, Jazayeri D, Shaw L, et al. Hospital falls prevention with patient education: a scoping review. BMC Geriatr 2020;20:140. 10.1186/s12877-020-01515-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sutton D, Windsor J, Husk J. A care bundle approach to falls prevention. Nurs Times 2014;110:21–3. [PubMed] [Google Scholar]
- 14.Wolf L, Hignett S. Are patients at risk for falling?…not if you ask them. Proceedings 19th Triennial Congress of the IEA. Melbourne, Australia, 2015. [Google Scholar]
- 15.Hignett S, Wolf L. Reducing inpatient falls: Human Factors & Ergonomics offers a novel solution by designing safety from the patients' perspective. Int J Nurs Stud 2016;59:A1–3. 10.1016/j.ijnurstu.2016.02.007 [DOI] [PubMed] [Google Scholar]
- 16.Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf 2014;23:196–205. 10.1136/bmjqs-2013-001812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carayon P, Wetterneck TB, Cartmill R, et al. Characterising the complexity of medication safety using a human factors approach: an observational study in two intensive care units. BMJ Qual Saf 2014;23:56–65. 10.1136/bmjqs-2013-001828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gurses AP, Tschudy MM, McGrath-Morrow S, et al. Overcoming COVID-19: what can human factors and ergonomics offer? J Patient Saf Risk Manag 2020;25:49–54. 10.1177/2516043520917764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donchin Y. Resuscitation trolleys: human factors engineering. Qual Saf Health Care 2002;11:393. 10.1136/qhc.11.4.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O'Connor P, Reddin C, O'Sullivan M, et al. Surgical checklists: the human factor. Patient Saf Surg 2013;7:14. 10.1186/1754-9493-7-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chartered Institute of Ergonomics and Human Factors . Human factors for health and social care white paper. UK: London, 2018. [Google Scholar]
- 22.Reed JE, Card AJ. The problem with Plan-Do-Study-Act cycles. BMJ Qual Saf 2016;25:147–52. 10.1136/bmjqs-2015-005076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carayon P, Schoofs Hundt A, Karsh B-T, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care 2006;15 Suppl 1:i50–8. 10.1136/qshc.2005.015842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hibbert PD, Thomas MJW, Deakin A, et al. Are root cause analyses recommendations effective and sustainable? an observational study. Int J Qual Health Care 2018;30:124–31. 10.1093/intqhc/mzx181 [DOI] [PubMed] [Google Scholar]
- 25.Reiling J, Hughes RG, Murphy MR. The Impact of Facility Design on Patient Safety. In: Hughes RG, ed. Patient safety and quality: an evidence-based Handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality (US), 2008. [PubMed] [Google Scholar]
- 26.Weaver SJ, Lubomksi LH, Wilson RF, et al. Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:369–74. 10.7326/0003-4819-158-5-201303051-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Catchpole K, Neyens DM, Abernathy J, et al. Framework for direct observation of performance and safety in healthcare. BMJ Qual Saf 2017;26:1015–21. 10.1136/bmjqs-2016-006407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun R, Sosnoff JJ. Novel sensing technology in fall risk assessment in older adults: a systematic review. BMC Geriatr 2018;18:14. 10.1186/s12877-018-0706-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carayon P, Hoonakker P. Human factors and usability for health information technology: old and new challenges. Yearb Med Inform 2019;28:071–7. 10.1055/s-0039-1677907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parsons R, Cramb SM, McPhail SM. Clinical prediction models for hospital falls: a scoping review protocol. BMJ Open 2021;11:e051047. 10.1136/bmjopen-2021-051047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rajagopalan R, Litvan I, Jung T-P. Fall prediction and prevention systems: recent trends, challenges, and future research directions. Sensors 2017;17:2509. 10.3390/s17112509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mileski M, Brooks M, Topinka JB, et al. Alarming and/or alerting device effectiveness in reducing falls in long-term care (LTC) facilities? A systematic review. Health Care 2019;7:51. 10.3390/healthcare7010051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Watson BJ, Salmoni AW, Zecevic AA. The use of the Morse fall scale in an acute care hospital. Clin Nurs Stud 2016;4:32–40. 10.5430/cns.v4n2p32 [DOI] [Google Scholar]
- 34.Vassallo M, Poynter L, Sharma JC, et al. Fall risk-assessment tools compared with clinical judgment: an evaluation in a rehabilitation ward. Age Ageing 2008;37:277–81. 10.1093/ageing/afn062 [DOI] [PubMed] [Google Scholar]
- 35.Lee Y-S, Choi E-J, Kim Y-H, et al. Factors influencing falls in high- and low-risk patients in a tertiary hospital in Korea. J Patient Saf 2020;16:e376–82. 10.1097/PTS.0000000000000593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quigley PA. Evidence levels: applied to select fall and fall injury prevention practices. Rehabil Nurs 2016;41:5–15. 10.1002/rnj.253 [DOI] [PubMed] [Google Scholar]
- 37.Mion LC, Chandler AM, Waters TM, et al. Is it possible to identify risks for injurious falls in hospitalized patients? Jt Comm J Qual Patient Saf 2012;38:408–AP3. 10.1016/S1553-7250(12)38052-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thatrimontrichai A, Weber DJ, Apisarnthanarak A. Mental health among healthcare personnel during COVID-19 in Asia: a systematic review. J Formos Med Assoc 2021;120:1296–304. 10.1016/j.jfma.2021.01.023 [DOI] [PubMed] [Google Scholar]
- 39.Camicia ME, Cournan MC, Rye J. COVID-19 and inpatient rehabilitation nursing care: lessons learned and implications for the future. Rehabil Nur 2021;46:187–96. 10.1097/RNJ.0000000000000337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baskin RG, Bartlett R. Healthcare worker resilience during the COVID-19 pandemic: an integrative review. J Nurs Manag 2021;29:2329–42. 10.1111/jonm.13395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Kock JH, Latham HA, Leslie SJ, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 2021;21:104. 10.1186/s12889-020-10070-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manchia M, Gathier AW, Yapici-Eser H, et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: a critical review across waves. Eur Neuropsychopharmacol 2022;55:22–83. 10.1016/j.euroneuro.2021.10.864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barbash IJ, Kahn JM. Fostering Hospital Resilience-Lessons from COVID-19. JAMA 2021;326:693–4. 10.1001/jama.2021.12484 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2021-001696supp001.pdf (146.3KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.