Abstract
The delivery of monetary incentives contingent on verified abstinence is an effective treatment for alcohol use disorder. However, incentive cost has often been cited as a barrier to delivering this type of treatment. In the present randomized parallel groups trial, we systematically replicated a previous trial we conducted that employed remote alcohol monitoring and incentive delivery to promote abstinence from alcohol, but with the additional requirement for participants to partially self-fund their abstinence incentives. Treatment-seeking participants with alcohol use disorder (n = 92) who met inclusion criteria (n = 36) were randomized to either a Contingent or Noncontingent group (n = 18 each). Those not meeting inclusion criteria included 15 participants who agreed to the deposit requirement but failed to make the deposit payment. The Contingent group received nearly immediate monetary incentives each day they remotely provided negative breathalyzer samples. The Noncontingent group received matched incentives each day they successfully provided samples independent of alcohol content. Days abstinent in the Contingent group were 86%, which was significantly higher than the 44% recorded in the Noncontingent group, corresponding to an odds ratio of 8.2. Exploratory analyses revealed that the deposit requirement prevented participation in those with lower incomes and those with greater alcohol use. These results support the efficacy of this remotely deliverable alcohol abstinence reinforcement incentive intervention with a deposit requirement. However, the requirement to provide a monetary deposit to self-fund abstinence incentives may prevent those with greater alcohol use and/or those experiencing extreme poverty from participating in the intervention.
Keywords: alcohol use disorder, contingency management, incentives, poverty, deposit contracts
Lifetime prevalence of DSM-5 alcohol use disorder in the United States is 29%, but only 20 to 24% of people with alcohol use disorder ever seek treatment (Grant et al., 2015; Hasin et al., 2007). This leaves over 20% of the US adult population – 10s of millions of people – with untreated alcohol use disorder at some point in their lives. The most prevalent reasons given for not seeking treatment relate to an inability or unwillingness (e.g., due to stigmatization) to attend traditional in-person treatment (Cohen et al., 2007). Additionally, situational factors such as the COVID-19 pandemic, rural location, disability, or poverty can impair access to treatment services that rely on in-person interactions among providers and clients.
Contingency management is a highly efficacious treatment that reduces drug use (Higgins et al., 2008). In contingency management treatments, a tangible reward (e.g., money) is provided contingent upon a bout of verified treatment success (e.g., 24 hours of abstinence from the target drug). Among those with alcohol use disorder (Bobova et al., 2009; Mitchell et al., 2005; Petry, 2001) or another drug use disorder (Bickel & Marsch, 2001), delayed outcomes have relatively little control over behavior. Immediately available reinforcers, such as those in contingency management interventions, are more likely to promote positive behavior than the delayed health or social gains associated with abstinence (Koffarnus et al., 2011). We recently reported on a remote version of this protocol that used mobile breathalyzers, cell phones, and reloadable debit cards to remotely monitor alcohol use and incentivize abstinence with no in-person contact with participants during the intervention (Koffarnus et al., 2018). In this intervention, the active treatment group who received financial incentives contingent on negative breathalyzer submissions achieved 85% days of the 21-day intervention period abstinent, significantly and substantially more than the 38% days abstinent of the control group who received incentives for submissions independent of alcohol use (Cohen’s d effect size = 1.7).
The incentive costs associated with contingency management interventions have been shown to be a cost-effective treatment component (Sindelar et al., 2007), supporting the funding of such incentives as a component of clinical care. Despite this, one proposed alternate method of reducing the funding burden of these incentive costs is deposit contracts, which consist of up-front money supplied by the participant (Bickel et al., 2014). The participant earns the deposit back by succeeding in treatment, with the possibility of earning additional funds beyond the deposit with continued success. Contracts work as a “precommitment strategy” (Rachlin & Green, 1972) in that they move the decision point for engaging in substance use from the time that drugs are present and available to a point in time days or weeks prior to availability, increasing the likelihood of making and committing to the delayed rewards associated with abstinence. Theoretically, by agreeing ahead of time to forfeit money by drinking, the alcohol user changes the consequences of alcohol use from a possibility of delayed negative consequences to a relatively immediate negative financial consequence. Also, people are more sensitive to monetary losses than gains (Green & Myerson, 2004; Kahneman & Tversky, 1979). Self-funded deposit contracts may increase incentive effectiveness by encouraging participants to think of these incentives as reversing the “loss” of the deposit contract instead of as gain supplied by the treatment provider. Deposit contracts have been used in a number of contingency management interventions for smoking cessation and weight loss, demonstrating the effectiveness of self-funded incentives to promote behavior change and the willingness of some participants to deposit money toward their treatment (Bowers et al., 1987; Elliott & Tighe, 1968; John et al., 2011; Paxton, 1980, 1981, 1983; Volpp et al., 2008; Winett, 1973).
The present randomized parallel groups trial was designed to evaluate the effectiveness and acceptability of a remotely delivered contingency management intervention with a deposit contract requirement to partially fund the cost of the monetary incentives to be earned in the intervention. Our first primary hypothesis was that this deposit contract variant of this intervention would be effective at incentivizing abstinence from alcohol. Our second primary goal was to assess acceptability of this intervention and determine if the deposit contracts reduced costs. Furthermore, we kept all major design elements the same as our previous trial without deposit contracts (Koffarnus et al., 2018) so that we could both demonstrate the reproducibility of these results and make exploratory comparisons among these two trials. Specifically, the current trial allowed us to draw conclusions about the impact of the deposit contract requirement on the demographics of study inclusion rates.
Method
Study Design
This randomized parallel trial was split into two phases: a 7-day Monitoring Only phase and a 21-day Treatment phase. Participants also completed six in-lab assessment sessions which occurred immediately prior to the Monitoring Only phase; immediately after the Treatment phase; and 1 month, 2 months, 3 months, and 6 months following the end of the Treatment phase.
Participants
Participants were recruited from the community surrounding Roanoke, VA, primarily with advertisements in public places and with targeted advertisements on websites such as Facebook.com and Craigslist.com. Eligible participants were at least 18 years of age, met DSM 5 criteria for alcohol use disorder, did not meet DSM criteria for other substance use disorder (excluding caffeine, marijuana, and nicotine), scored below 23 on the Alcohol Withdrawal Symptom Checklist (Pittman et al., 2007), indicated a willingness to provide a $75 monetary deposit to be held in an incentive fund, and expressed a desire to cut down or quit drinking. All participants provided written informed consent and this protocol was monitored by the Virginia Tech Institutional Review Board (#14–715) and registered with clinicaltrials.gov (NCT04182022).
Procedures
Monitoring Only phase.
During this phase, participants were asked to provide daily self-reports of previous-day drinking and current withdrawal symptoms via cell phone text message (see Supplemental Figure S1 for the content of these messages). This occurred for 7 days with no other study intervention taking place. The first of these days was the consent session during which participants were guided through the process. Each day, participants were asked to report how many alcoholic drinks they consumed the previous day and their current alcohol withdrawal symptom severity. We asked them about the previous day alcohol use instead of the current day to best capture all drinks consumed each day without inconsistent response times complicating the measurement. Participants were allowed to report this information at any time throughout the day but were encouraged through prompts to do so in the morning to increase the likelihood of accurate recall of previous day use. Participants received a reminder to report their previous-day drinking with text messages, followed by a phone call if they did not contact us by early evening. For completing this daily self-report, participants received a $1 adherence incentive. If a participant reported any withdrawal symptoms (≥2 on a scale from 0 [no symptoms] to 9 [severe symptoms]), research staff called them and administered the Alcohol Withdrawal Symptom Checklist (Pittman et al., 2007). If their score on this assessment indicated clinically significant withdrawal symptoms, they were put in contact with the study physician to determine if any medical intervention was necessary. The purpose for this baseline period was to verify that recent alcohol use met patterns of heavy drinking and to determine if participants would respond to text message prompts. At the end of this phase, participants who indicated patterns of at least two heavy-drinking episodes (≥4 drinks in one day for women, ≥5 drinks for men) and successfully reported their level of drinking as requested on 5 of the 6 days following consent were invited to continue in the study.
Randomization and masking.
At the end of the Monitoring Only phase, eligible participants were randomly assigned to either the Contingent or Noncontingent group (even allocation ratio between groups) with a computerized algorithm that biased the random assignment to balance the groups on current alcohol use (average drinks per day during baseline period), alcohol use history (years of self-reported heavy drinking), and current use of outside treatment resources (measured with the Treatment Services Review, (McLellan, Alterman, et al., 1992). The first two participants to enroll in the study were assigned to the Contingent group to accommodate the yoking procedure (see group descriptions below). Participants and research staff were not aware of the participants’ group assignment during the Monitoring Only phase because group assignment had not yet occurred at this point, but because knowledge of abstinence reinforcement contingencies and incentive schedule was an integral part of the intervention, they were not masked during the Treatment phase. Additionally, at the point of randomization, participants completed a second consent session where they were provided with a detailed explanation of the contingencies relevant to their own group. Contingencies for the other group were not described to participants. All other information provided to participants was the same for both groups, which included instruction to consider the first day of the Treatment phase as their ‘quit date’.
$75 participant-funded deposit.
During the second consent session when it was determined that participants met eligibility criteria to proceed to the Treatment phase, a $75 deposit was collected from participants. Participants were informed of this requirement in all advertisements, during screening, and during both consent sessions. Participants had to indicate they were willing to provide this deposit during both consent sessions to continue with the study. Participants were allowed to fund this deposit with cash, a personal check, with a personal debit card (including the payment card we supplied them to deliver study incentives), or any combination of these. Credit card payments or third-party payments were not accepted. At this point in the study, participants who completed all scheduled study requirements had earned $52 in compensation, so a minimum of an additional $23 was required from the participants personal funds if they saved their study compensation and used it toward the deposit requirement. Participants who were unable to provide the deposit but expressed a desire to continue study participation were allowed up to one week to ‘pause’ the study and attempt to save the funds. Participants who still did not provide the deposit after this week were discontinued from the study. Deposit payments were held in a fund separate from the primary study fund, and the first $75 in incentives earned by the participant following the deposit payment were paid to them from their own deposit.
Treatment phase.
Both groups were exposed to the same treatment events, but the consequence for breathalyzer screens differed by group. The treatment period consisted of 21 consecutive days with three remote breathalyzer screens per day. During this 21-day period as they did during the baseline period, participants self-reported their previous-day alcohol use and current withdrawal symptoms daily in response to a text message and/or phone call. Participants were provided with a prepaid cell phone (if necessary) at the beginning of the study and a breathalyzer at the beginning of the Treatment phase.
Breathalyzer monitoring.
Alcohol use during the Treatment phase was monitored remotely with thrice daily breathalyzer screens with a Soberlink (Soberlink Healthcare, LLC, Cypress, CA, USA) SL2 breathalyzer. During breathalyzer assessments, a picture was automatically taken of the user, which was compared to a reference picture taken at the onset of the Treatment phase. The breathalyzer automatically uploaded the breathalyzer results and the picture of the user to a centralized, secure website where the data were available to research staff. Research staff monitored these results, verified that the picture matched a reference picture for that participant if not approved by automatic facial recognition, and informed the participant via text message of the consequences of the breathalyzer screen (see Supplemental Figure S1 for the content of these messages). No images were unable to be recognized by either automatic facial recognition or manual recognition by research staff, and text-message feedback was sent as soon as possible after submissions were received and typically within a 2-hour window post submission.
All participants completed breathalyzer assessments 3 times per day for 21 days. Participants chose these times each day with guidance from research staff. Participants were asked to choose an assessment time shortly after they usually awaken, shortly before they go to bed at night, and once throughout the day. Chosen times could be between 5:00 am and midnight and had to be separated by at least 6 hours. This ensured that the first and last screens each day were at least 12 hours apart and the screens were distributed throughout the waking hours. Participants were reminded via text message when a sample was to be collected, and samples were accepted up to 15 minutes before the scheduled time and 60 minutes after the scheduled time. Both groups received a $1 adherence incentive payment for each breathalyzer result submitted within the allowed 75-minute submission period, regardless of the result of that test. This payment was to encourage participants to complete screens, even if they had consumed alcohol that day.
Contingent group.
Participants in the Contingent group earned incentive payments based on the results of the breathalyzer screens. Any BrAC reading ≥ 0.02% or a missed submission was considered a positive indicator of alcohol use. A participant that submitted three on-time negative samples in a given day earned an abstinence incentive payment that escalated in value with each day of negative results. The first day a participant recorded all negative samples, s/he received an abstinence incentive payment of $5. For each subsequent day of negative samples, this daily payment increased by $1 to a maximum daily payment of $25 if no alcohol use was recorded for all 21 days. In addition, the participant received a $5 bonus for every third consecutive day of negative samples. A participant who never recorded a positive sample and never missed a screen earned $350 in abstinence incentive payments over three weeks. If a positive sample was recorded, the participant received no breath-sample payments that day other than the $1 adherence incentive for each submitted sample and their escalating pay schedule was reset to the base rate of $5. If, after a positive sample, the participant recorded three consecutive days of negative samples, their contingency payment reverted back to the value it was before being reset. This escalating system of payments with bonuses and pay resets for positive samples was based on previous contingency management interventions where it was shown to be more highly effective (Roll & Higgins, 2000; Roll et al., 1996), including our (Koffarnus et al., 2018) and others’ studies of alcohol use (Barnett et al., 2011), and remote monitoring of smoking (Dallery & Raiff, 2011).
Noncontingent group.
Like the Contingent group, the Noncontingent group was required to submit 3 breathalyzer samples per day and received a $1 adherence incentive for each submitted sample. They also received incentive payments, but the payments received were not contingent on their breathalyzer results. Instead, Noncontingent participants were yoked to a completed participant in the Contingent group and received a payment equal to the payment the Contingent participant would have received on that study day if s/he submitted negative samples. This way, both groups experienced the same payment schedule with the same likelihood of pay increases, bonuses, and pay resets, isolating the contingency tying the payments to breathalyzer results for comparison between the groups.
Remote delivery of payments.
To allow for incentive payments that were both convenient and rapidly available, we delivered payments to participants with reloadable prepaid debit cards through Greenphire® ClinCard® (King of Prussia, PA, USA). As payments were earned during the course of the study, additional funds were added to the account for that participant. Funds were immediately available when added and research staff sent participants a text message notifying them of payments when they were added (see Supplemental Figure S1 for the content of these messages).
Assessment sessions.
Assessment sessions included various behavioral assessments and questionnaires related to alcohol use and associated cognitive processes and were repeated at the study consent, the day after the treatment phase ended, and at 1-, 2-, 3-, and 6-month post-treatment follow-ups. The time-line follow-back (TLFB) assessment (Sobell & Sobell, 1992) was used to assess daily drinking quantity for the 30 days preceding each assessment session. The Alcohol Use Disorder Identification Test (AUDIT) (Saunders et al., 1993) was used to assess alcohol use disorder risk factors, the Treatment Services Review (McLellan, Alterman, et al., 1992) assessed use of treatment resources including professional counseling and attendance at groups such as Alcoholics Anonymous, and the Addiction Severity Index-lite (ASI-lite) (McLellan, Kushner, et al., 1992) assessed medical, legal, employment, psychiatric, and social factors related to substance use. The 5-question adjusting delay discounting task (Koffarnus & Bickel, 2014) was used to determine participants’ monetary delay discounting rate, a measure of impulsive decision making that is often associated with substance use disorders and treatment outcomes (Bickel et al., 2014; Koffarnus et al., 2013).
Outcome variables and data analyses
The primary measure of alcohol use during the intervention period was alcohol use measured by the Soberlink breathalyzer 3 times per day. This outcome was coded as a trichotomous variable once per day as either positive (at least one positive screen throughout the day), negative (all three screens submitted on time and negative), or missing (at least one missing screen with any submitted screens recorded as negative). This variable was also analyzed with any missing samples treated as positive. Data were analyzed in a generalized logistic model with main effects of group and study day and an autoregressive(1) working correlation matrix. Generalized estimating equations (GEE) were used to accommodate intra-subject correlation inherent in repeated measurements (Liang & Zeger, 1986). As a secondary measure of alcohol use, we also analyzed the daily self-reports of previous-day drinks. These data were analyzed as above with generalized linear regression. Additional variables measured with generalized linear or logistic regression as above include breathalyzer adherence (missing versus submitted BrAC samples) and daily self-reported withdrawal symptoms on a 0 to 9 scale.
Additional measures of alcohol use were collected during the three assessment sessions. The TLFB assessment (mean drinks per day) and AUDIT score were each compared across assessment session, group, and for a session by group interaction in generalized linear or logistic regression using GEE. These aforementioned measures collected at the post-treatment assessment session were compared between groups with multivariate general linear regression, and participant characteristics were compared between groups with independent t tests or Fisher’s exact tests as appropriate. Participant characteristics associated with the likelihood of participants paying the $75 deposit were analyzed in a binary logistic regression model. All analyses were conducted in SPSS 26 (IBM Analytics) and GraphPad Prism 8 with alpha set at 0.05.
Results
A total of 92 participants were recruited from the community surrounding Roanoke, VA from December 2016 through December 2018 (Figure 1). Sixteen were excluded after the initial assessment session for failing to meet inclusion criteria, 5 withdrew from the study, and 3 were terminated for violating policies (e.g., attempted theft, consuming alcohol on premises). One participant failed to meet the requirement to respond to text messages on 5 monitoring days, 16 participants were excluded for failing to meet drinking criteria during the monitoring phase, and 15 met all inclusion criteria but were not able to provide the $75 deposit at the time of group assignment, leaving 36 participants randomized into a study arm and included in final data analyses. The 56 participants not randomized to a study arm were more likely to be male, African American, older, and heavier drinkers (see Supplemental Table S1). This final sample size was determined with a power analysis (Liu & Liang, 1997) with 80% power to detect an effect size observed in previous work (Koffarnus et al., 2011).
Figure 1:
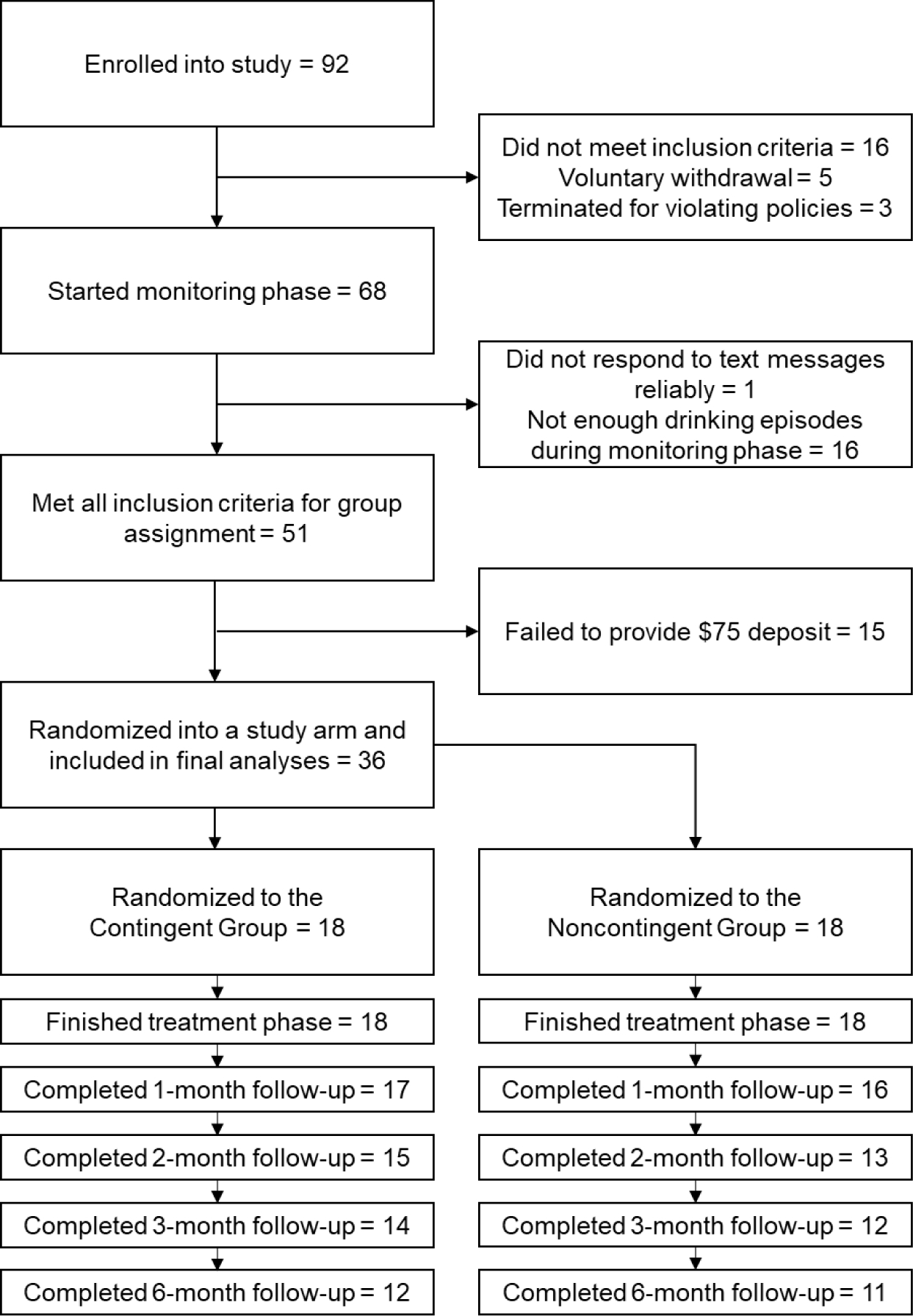
CONSORT Diagram Depicting Participant Inclusion and Exclusion
Participant characteristics for randomized participants are shown in Table 1. No group differences were detected on any characteristic variable including gender, race, age, monthly income, AUDIT score, drinks per day as measure by the TLFB, Treatment Services Review score, years of heavy drinking as assessed by the ASI-lite, heavy drinking days self-reported during the Monitoring Only phase, or monetary delay discounting rate. Along with drinks per day during the Monitoring Only phase, Treatment Services Review score and years of heavy drinking were used as group stratification variables.
Table 1.
Characteristics of participants randomized to a study group.
| Contingent (n=18) | Noncontingent (n=18) | Statistic | |
|---|---|---|---|
| Gender | 10 female (56%), 8 male (44%) | 11 female (61%), 7 male (39%) | Fisher’s exact p = 1.0 |
| Race | 2 African American (11%), 15 White (83%), 1 other race (6%) | 1 African American (6%), 15 White (83%), 2 other race (11%) | Fisher’s exact p = 1.0 |
| Age | 36.1 (SD = 9.9) | 39.2 (SD = 14.6) | t(34) = 0.76, p = .5 |
| Monthly Individual Income a | US$1823 (SD = US$1260; median = US$1550) | US$1687 (SD = US$1625; median = US$1250 | t(34) = 0.58, p = .6 |
| AUDIT | 21.2 (SD = 6.6) | 22.2 (SD = 5.6) | t(34) = 0.49, p = .6 |
| Drinks per day prior to study onset b | 3.9 (SD = 2.3) | 4.2 (SD = 3.3) | t(34) = 0.36, p = .7 |
| Treatment Services Review alcohol score | 0.8 (SD = 1.0) | 0.7 (SD = 0.7) | t(34) = 0.59, p = .6 |
| Years of heavy drinking c | 13.1 (SD = 7.0) | 12.5 (SD = 8.2) | t(34) = 0.24, p = .8 |
| ASI-lite Alcohol Composite c | 0.47 (SD = 0.17) | 0.56 (SD = 0.20) | t(34) = 1.46, p = .2 |
| Heavy drinking days self-reported in Monitoring phase | 4.1 (SD = 1.5) | 4.5 (SD = 1.6) | t(34) = 0.86, p = .4 |
| $1000 Delay Discounting Log(ED50) | 1.89 (SD = 0.84) | 2.39 (SD = 0.63) | t(34) = 2.02, p = .051 |
Note.
Income was square-root-transformed prior to group comparison to normalize the distributions.
30-day average preceding the consent session from the Timeline Follow-Back assessment.
From the Addiction Severity Index-lite.
Throughout the 21-day treatment phase, participants were asked to submit three remote breathalyzer assessments per day. The primary abstinence outcome was the percent days abstinent from these breathalyzer submissions (i.e., all three samples were submitted on time and were negative for alcohol). Mean percent days abstinent reached 86% (SD = 20%) in the Contingent group, which was significantly higher than the 44% (SD = 34%) in the Noncontingent group (Figure 2 top; χ2 = 17.33, p < .001). This difference corresponds to an odds ratio (OR) of 8.2 (95% CI = 3.0 to 22.1). No main effect of treatment day on daily abstinence was observed (χ2 = 2.49, p = .1). Results were similar if all missing samples were considered positive, with mean percent days abstinent with no missing samples of 83% (SD = 23%) in the Contingent group and 42% (SD = 33%) in the Noncontingent group. This resulted in a significant effect of group (χ2 = 14.98, p < .001, OR = 6.6 [95% CI = 2.5 to 17.2) and no significant effect of treatment day (χ2 = 0.67, p = .4).
Figure 2:
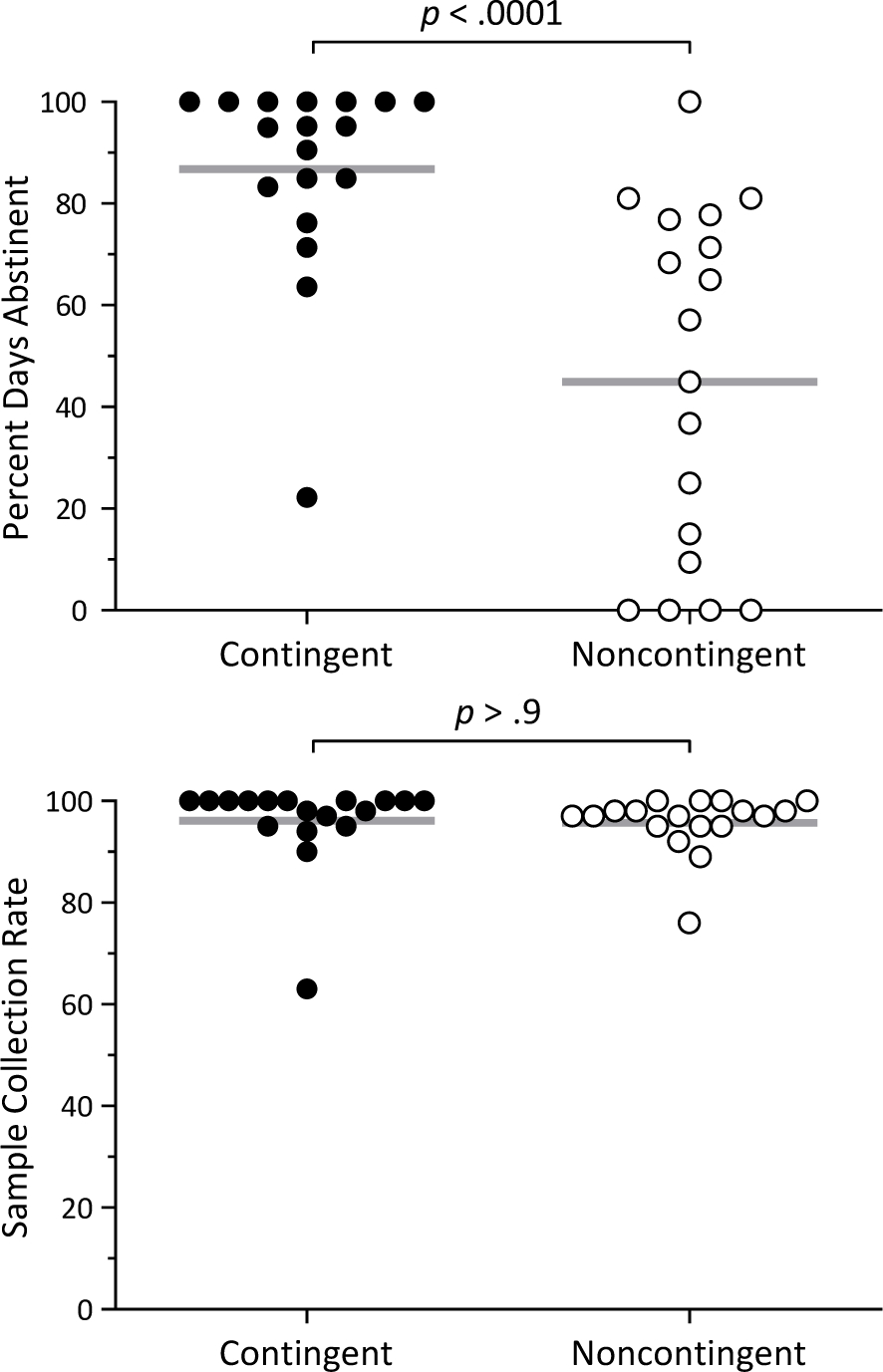
Remote Breathalyzer Results
Note. Abstinence and individual sample collection rate results from the thrice-daily remote breathalyzer assessments during the Treatment phase. Percent days abstinent was significantly higher in the Contingent group (top), and the collection rate was similarly high in both groups (bottom).
One of the primary goals of this study was to establish the feasibility of remotely assessing abstinence from alcohol, with our primary measure of this being adherence to the scheduled breathalyzer assessments. Adherence was high in both groups, with an overall sample collection rate of 95.7% of requested samples submitted and all but two participants having greater than an 80% collection rate (Figure 2 bottom). Collection rate did not differ between groups (χ2 = 0.00, p > 0.9), but a significant tendency for collection rate to decrease as the 21-day treatment phase progressed was detected (χ2 = 46.40, p < .001; OR = 1.08 [95% CI = 1.06 to 1.10]).
Previous-day drinks per day and withdrawal symptoms rated on a zero to nine scale were collected daily via text message prompts sent to each participant. The effects of treatment group (Contingent versus Noncontingent), Phase (Monitoring only versus Treatment), study day, and the interaction of Group and Phase were assessed with each of these self-reported measures with general linear regression and GEE to control for repeated measurements. On drinks per day (Figure 3 top), an overall main effect of Phase (χ2 = 31.30, p < .001) and a significant Group by Phase interaction (χ2 = 4.82, p = .03) was observed. Pairwise comparisons revealed a significant difference between the groups in the Treatment phase only (p = .01) with no difference in the monitoring phase (p = .4) and no main effect of study day (χ2 = 1.19, p = .3) or overall main effect of Group (χ2 = 3.15, p = .08).
Figure 3:
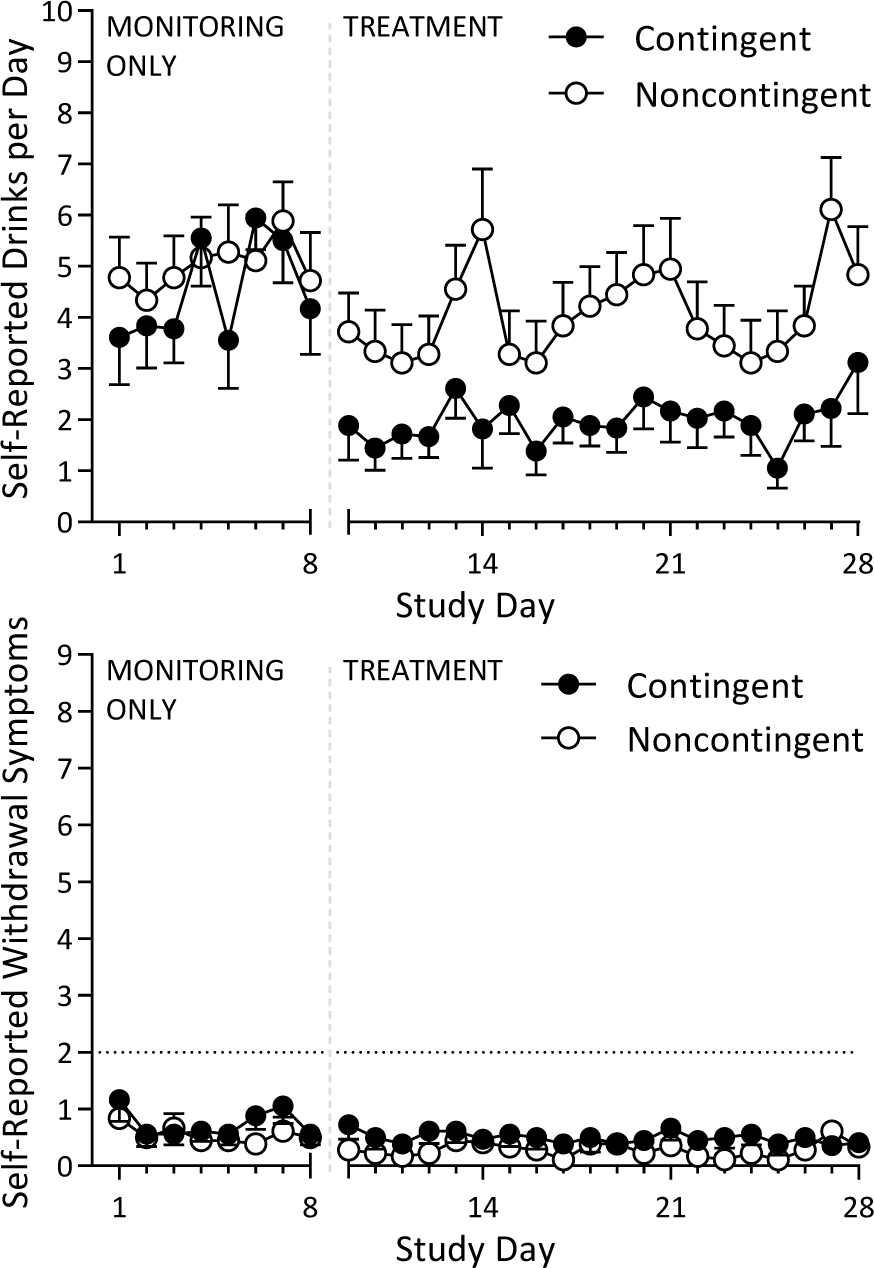
Daily Participant Self-Reports
Note. Daily self-reports of drinks per day and withdrawal symptoms collected throughout the Monitoring Only and Treatment phases. Drinks per day were significantly lower in the Contingent group during the Treatment phase only (top), and withdrawal symptoms were similarly low throughout the study in both groups (bottom).
Daily reports of previous-day withdrawal symptoms indicated minimal withdrawal symptoms throughout the study in both groups (Figure 3 bottom) with no instances of withdrawal symptoms concerning enough to warrant in-person medical evaluation. No main effect of Group (χ2 = 1.67, p = .2) or Day (χ2 = 2.57, p = .1) was detected, nor was there a Group by Phase interaction (χ2 = 0.24, p = .6). An overall significant effect of study Phase indicated that self-reported withdrawal symptoms were less in the Intervention phase independent of group (χ2 = 4.38, p = .04).
Secondary outcome variables that we were not necessarily powered to assess in this relatively small feasibility study included three measures of alcohol use and dependence that were collected at each of the assessment sessions. The TLFB (Figure 4 top) contained retrospective recall of alcohol use prior to the study consent session, during the 21 active-intervention days (collected at the end of treatment assessment session) and for the 30 days prior to each of the four extended post-intervention follow-up sessions. A treatment effect on self-reported drinks per day was indicated by a significant Session by Group interaction between the consent and end-of-treatment assessments (χ2 = 4.86, p = .03). Self-reported drinking in the Contingent group remained low during the extended follow-up sessions, but this was not significantly different from the Noncontingent group, a trend which may have been exasperated by missed assessment sessions disproportionately likely to be seen in participants with higher rates of drinking behavior. Self-reported drinks per day analyzed as a function of proportion of days with heavy drinking from the daily self-reports (treatment phase) and TLFB (all other timepoints) data reported showed a similar pattern. A treatment effect on proportion of days with heavy drinking was indicated by a significant Session by Group interaction between the consent and treatment phase (χ2 = 8.33, p = .004) and overall effect of session (χ2 = 7.70, p = .006), but no significant difference during the follow-up sessions.
Figure 4:
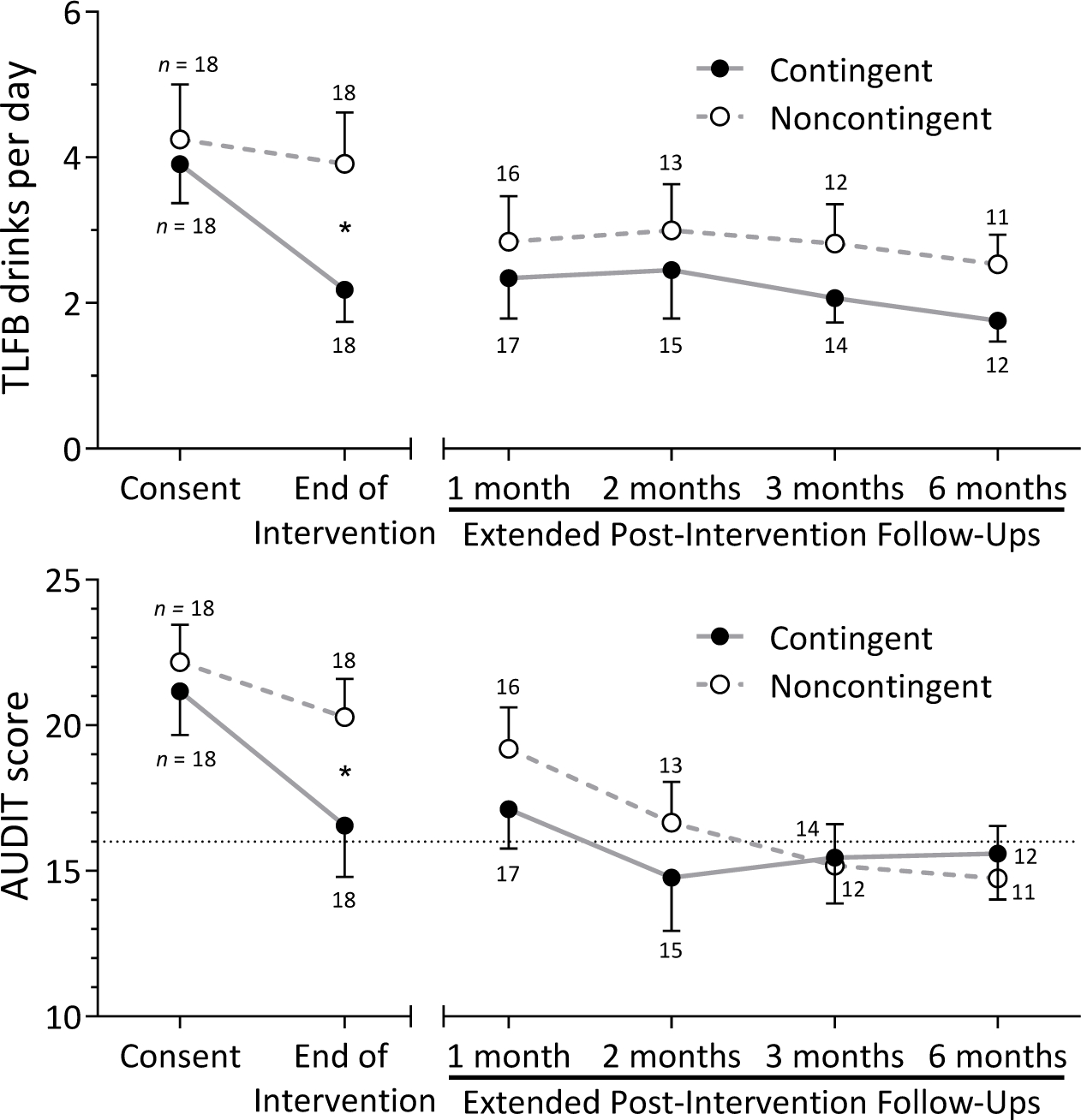
Alcohol Use Quantity and Problems
Note. Indicators of alcohol use quantity as measured by the Timeline Follow-back assessment (top) and problems associated with alcohol use as measured by the AUDIT assessment (bottom). Numeric labels near points indicate the number of participants to complete an assessment and asterisks indicate a significant treatment effect between groups (p < .05).
Symptoms of alcohol use disorder were assessed with the AUDIT at each assessment session (Figure 4 bottom). AUDIT scores were similar between groups at the consent session, but differences emerged by the end of the treatment. This pattern resulted in a significant group by session interaction between these two sessions (χ2 = 3.99, p = .046). AUDIT scores during the extended follow-up sessions were relatively low in both groups among those participants who attended those sessions.
Participants completed a custom questionnaire at the end of the Treatment phase with questions grouped into the categories of overall satisfaction, treatment effectiveness, and the ease of use of treatment components (Figure 5). One participant in the Contingent group and two participants in the Noncontingent group did not complete this questionnaire due to computer error. Both groups were satisfied overall with the approach, with no significant differences in ratings by group in the general assessment of the approach overall. In the treatment effectiveness category of questions, the Noncontingent group rated the components approximately ‘somewhat’ effective, with the Contingent group giving ratings significantly higher for their satisfaction with the ability of the treatment to help them reduce their alcohol use (F1,31 = 2.47, p = .04) and marginally higher for the overall category (F1,31 = 1.70, p = .06). Participants rated the various components of the treatment approach between ‘somewhat easy’ and ‘very easy’ with no significant differences between the groups for any question.
Figure 5:
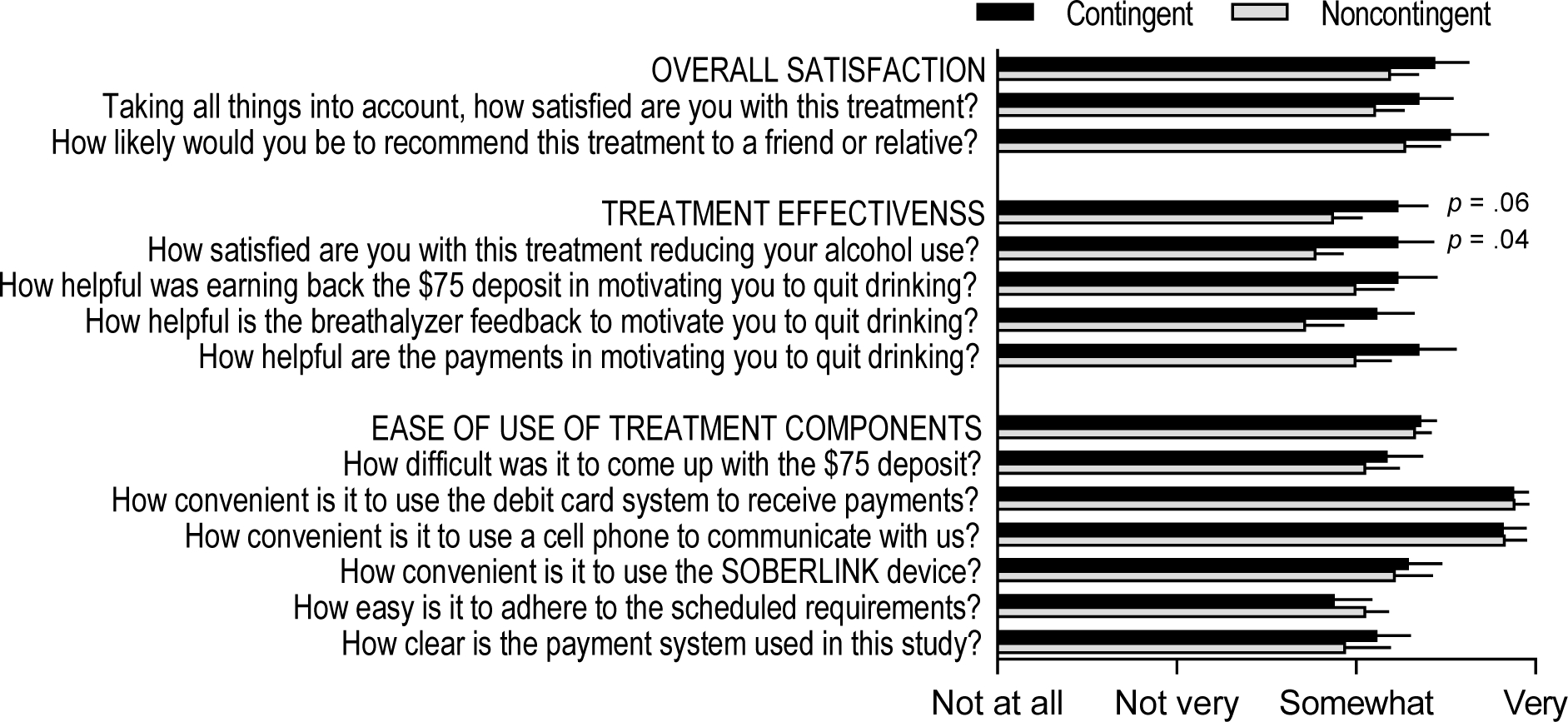
Participant Ratings of Treatment Acceptability
The 15 participants who met all inclusion criteria but were unable to provide the $75 deposit after the Monitoring Only phase were compared to the 36 participants randomized into a study arm in Table 2. Simple group comparisons without factoring in covariance among characteristics suggested that participants who did not pay the deposit were more likely to be male, be African American, have a lower monthly income, have a higher monetary delay discounting rate, and trended toward more self-reported drinks per day prior to the study. However, many of these characteristics were correlated with one another, so we conducted a logistic regression to determine which characteristics were most reliably associated with ability to pay the deposit. In this model containing all variables listed in Table 2 (income was square-root transformed, discounting rate was log-transformed, and race dichotomized to white versus nonwhite), only income (χ2 = 7.2, p = .007) and drinks per day prior to study onset (χ2 = 5.8, p = .02) were significantly associated with likelihood of paying the deposit. All other variables were not significantly associated with paying the deposit after accounting for these.
Table 2.
Characteristics Associated with Paying the $75 Deposit
| Paid Deposit (n = 36) | Did Not Pay Deposit (n = 15) | Group Comparison Without Covariances | Logistic Model Predicting Payment | |
|---|---|---|---|---|
| Gender | 21 female (58%), 15 male (42%) | 3 female (20%), 12 male (80%) | Fisher’s exact p = .02 | χ2 = 1.13, p = .3 |
| Race | 3 African American (8%), 30 White (83%), 3 other race (8%) | 8 African American (53%), 7 White (47%), 0 other race (0%) | Fisher’s exact p = .001 | χ2 = 1.56, p = .2 |
| Age | 37.6 (SD = 12.4) | 41.3 (SD = 12.0) | t(49) = 0.98, p = .3 | χ2 = 0.07, p = .8 |
| Monthly Individual Income a | US$1755 (SD = US$1435; median = US$1500) | US$587 (SD = US$604; median = US$300 | t(49) = 2.99, p = .004 | χ2 = 7.24, p = .007 |
| AUDIT | 21.7 (SD = 6.0) | 24.5 (SD = 5.3) | t(49) = 1.60, p = .1 | χ2 = 0.41, p = .5 |
| Drinks per day prior to study onset b | 4.1 (SD = 2.8) | 7.0 (SD = 5.0) | t(17.9) = 2.10, p = .05 d | χ2 = 5.77, p = .02 |
| Treatment Services Review alcohol score | 0.8 (SD = 2.0) | 0.5 (SD = 0.5) | t(49) = 0.93, p = .4 | χ2 = 1.12, p = .3 |
| Years of heavy drinking c | 12.8 (SD = 7.5) | 17.9 (SD = 13.5) | t(17.7) = 1.39, p = .2 d | χ2 = 1.66, p = .2 |
| ASI-lite Alcohol Composite c | 0.52 (SD = 0.19) | 0.49 (SD = 0.17) | t(34) = 0.51, p = .6 | χ2 = 0.99, p = .3 |
| Heavy drinking days self-reported in Monitoring phase | 4.3 (SD = 1.5) | 4.8 (SD = 1.9) | t(49) = 1.02, p = .3 | χ2 = 0.92, p = .3 |
| $1000 Delay Discounting Log(ED50) | 2.14 (SD = 0.77) | 1.42 (SD = 0.68) | t(49) = 3.13, p = .003 | χ2 = 1.84, p = .2 |
Note.
Income was square-root-transformed prior to group comparison to normalize the distributions.
30-day average preceding the consent session from the Timeline Follow-Back assessment.
From the Addiction Severity Index-lite.
Levene’s test for equality of variances failed, unequal variances assumed in t test.
Discussion
The primary goals of this study were to assess the efficacy and acceptability of this remote monitoring and abstinence incentive approach we have previously shown to be effective (Koffarnus et al., 2018) with the addition of a deposit contract requirement wherein participants would prefund $75 of their abstinence incentives prior to the intervention phase. We think this study advances the literature through 1) the comparison of these results to our earlier results without deposit contracts (Koffarnus et al., 2018) as there are few direct comparisons of deposit contracts in the literature with other procedures remaining constant (see Halpern et al. (2015) for another recent example); 2) demographic comparisons of those who did and did not pay the deposit, highlighting potential inequities with this requirement; and 3) as a demonstration of the robustness and replicability of these procedures. This protocol with the deposit requirement was associated with a large treatment effect (Chen et al., 2010) for our primary outcome of breathalyzer results during the active treatment phase, and did not appear to have noticeably greater or less effectiveness than our previous trial (Koffarnus et al., 2018). While it is likely that some participants were able to consume small amounts of alcohol undetected with our breathalyzer schedule (see Koffarnus et al., 2018 for an in-depth discussion), self-reported alcohol use also demonstrated a significant treatment effect corresponding to breath alcohol readings. As we have previously reported, breath alcohol readings, retrospective TLFB recall of use, and daily self-reports of use tend to have acceptable rates of concordance without absent a major change in use patterns (Kaplan & Koffarnus, 2019). Ratings of acceptability were also positive among those enrolled in the trial, with marginally higher ratings of effectiveness in the Contingent group. Like our previous trial, all alcohol withdrawal symptoms were in an acceptable range and did not hinder the ability to deliver this type of intervention remotely in this population. Overall, results from this trial among those participants who paid the deposit were highly similar to those results from our previous trial without the deposit requirement. The consistent effectiveness of contingency management interventions has been reported previously (Higgins et al., 2008), and this replicability across time and setting is a strength of contingency management in general and this remotely delivered approach specifically.
One highly notable outcome of this trial that differentiates it from our previous trial concerns the participant population that was able to complete the full protocol. Our participant recruitment methods consisted of physical and online community advertisements and yielded a participant population with alcohol use disorder, but otherwise not wildly discordant from the demographics of Roanoke, VA. The compensation information and the $75 deposit requirement was prominently displayed in all advertisements, was covered in detail in the IRB-approved informed consent form, and was verbally explained to participants during the consent session. All participants were aware of the deposit requirement before expressing interest in and consenting to participate in this research study, and we likely never heard from any participants who found this deposit requirement unappealing. Our participant population therefore includes only those individuals who felt that the $75 deposit requirement was acceptable, and this randomized trial does not provide a good basis to determine the overall acceptability of this type of intervention in the general population.
Despite not being able to draw conclusions about the overall population-level acceptableness of deposit contracts, however, we can draw interesting conclusions among those in this group of community adults with alcohol use disorder who were sufficiently motivated to participate in this trial that they agreed to the deposit requirement. Of these participants, a substantial portion (29%) were not able to pay the $75 deposit when prompted to do so, and due to how our pre-determined protocol was written, were excluded from the remainder of the study at this point. We did not predict this degree of non-payment, especially considering participants were allowed to use the ~$50 of study compensation earned at this point toward their deposit. These participants reported that they did not fail to pay the deposit due to a change of heart about study participation, but they simply did not have the $75 available to them, often having already spent the previously earned study compensation. Our logistic model predicting who paid the $75 deposit revealed that drinks per day consumed prior to the trial onset and monthly income significantly predicted deposit payment. Notably, monetary delay discounting rate, a measure of self-control that is often associated with substance use disorder treatment outcomes (Bickel et al., 2014; Koffarnus et al., 2013), was higher in the group that did not pay the deposit but was not significantly predictive after accounting for income and drinks per day. Deposit contracts are sometimes discussed as a means to fund monetary incentives in contingency management interventions, but our research suggests that a deposit requirement may prevent lower income individuals with a greater drinking intensity from accessing this treatment approach. Even though our deposit requirement was relatively modest at $75, the median monthly income of those individuals unable to pay the deposit was $300. With this income, our deposit requirement was 25% of the monthly income for this group. In addition to an effective drug use disorder intervention, contingency management is often touted as an effective anti-poverty invention (Silverman et al., 2016; Silverman et al., 2018; Silverman et al., 2019). Procedural requirements such as deposit contracts should therefore be employed cautiously considering they may exclude individuals experiencing poverty from participating.
If self-funding of incentives is associated with undesirable exclusions of lower income and more frequent drinkers, alternate funding mechanisms are required. Despite evidence that financial incentives delivered in a contingency management treatment are cost effective (Sindelar et al., 2007), the up-front cost of incentives is a large contributor to hesitant attitudes of providers to use contingency management with their patients (Benishek et al., 2010; Rash et al., 2012). However, exposure to the procedure can shift attitudes toward support of financial incentives as worthwhile (Kirby et al., 2012), and over the past few decades there has been considerable momentum toward the use of incentives to promote behavioral change with the incentives funded as an intervention cost like any other cost-effective treatment component. For example, in response to the continued evidence showing it to be an effective treatment, the United States Veterans Administration implemented contingency management treatment for substance use nationwide (Petry et al., 2014). As an approved substance use treatment method, Veterans Administration physicians may prescribe contingency management to patients with a substance use disorder. This type of funding model allows all eligible patients to receive this efficacious treatment, including those experiencing poverty. The impact of future dissemination efforts for interventions employing financial incentives could be maximized by working with the health care industry to develop reimbursement mechanisms for financial incentives as a mode of treatment.
Contingent incentives are highly effective at promoting abstinence from alcohol with or without a participant-funded monetary deposit requirement when delivered as part of a remote monitoring protocol. However, even modest participant-funded deposits may prevent those with greater levels of alcohol use and/or those experiencing extreme poverty from receiving this treatment approach. Remote monitoring approaches such as this have great potential to deliver treatment to those with significant barriers to accessing in-person treatment, but deposit contracts may be counterproductive to the goal of reaching this population.
Supplementary Material
Public significance statement:
In the present clinical trial, treatment-seeking adults with alcohol use disorder were randomized to receive remotely delivered monetary incentives if they abstained from alcohol use or to a control condition where incentives were received regardless of alcohol use. Results indicated that this intervention was associated with lower rates of alcohol use and alcohol-related problems. Due to a requirement that participant self-fund a portion of their incentives at treatment onset, this intervention was not accessible to some lower income individuals.
Disclosures and Acknowledgements
Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under award number R21 AA023605 to MNK. 100% of this research was supported by federal money with no financial or nonfinancial support from nongovernmental sources. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding source did not have a role in writing this manuscript or in the decision to submit it for publication. All authors had full access to the data in this study and the corresponding author had final responsibility for the decision to submit these data for publication. Portions of this manuscript have been previously reported at the following scientific conferences: College on Problems of Drug Dependence, University of Kentucky Substance Use Research Day, American Psychological Association, and Research Society on Alcoholism.
MNK designed the experiment, collected the data, analyzed the data, interpreted the data, and drafted the manuscript. ASK monitored participant safety, assisted with study design, data collection, and data interpretation. BAK assisted with data analysis and interpretation. EMC assisted with data collection and interpretation. All authors read and approved the final version of the manuscript.
MNK, BAK, and EMC have no known conflicts of interest to disclose. ASK has no conflicts of interest to disclose related to this project, but has received other research support from the following in the past 5 years: Sunovian, Pfizer, Curemark, Roche, Allergan, Gilead, Takeda, and Liva Nova.
References
- Barnett NP, Tidey J, Murphy JG, Swift R, & Colby SM (2011). Contingency management for alcohol use reduction: A pilot study using a transdermal alcohol sensor. Drug and Alcohol Dependence, 118(2–3), 391–399. 10.1016/j.drugalcdep.2011.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benishek LA, Kirby KC, Dugosh KL, & Padovano A (2010). Beliefs about the empirical support of drug abuse treatment interventions: A survey of outpatient treatment providers. Drug and Alcohol Dependence, 107(2–3), 202–208. 10.1016/j.drugalcdep.2009.10.013 [DOI] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, & Murphy JG (2014). The behavioral economics of substance abuse disorders: Reinforcement pathologies and their repair. Annual Review of Clinical Psychology, 10(1), 641–677. 10.1146/annurev-clinpsy-032813-153724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, & Marsch LA (2001). Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction, 96(1), 73–86. 10.1046/j.1360-0443.2001.961736.x [DOI] [PubMed] [Google Scholar]
- Bobova L, Finn PR, Rickert ME, & Lucas J (2009). Disinhibitory psychopathology and delay discounting in alcohol dependence: Personality and cognitive correlates. Experimental and Clinical Psychopharmacology, 17(1), 51–61. 10.1037/A0014503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers TG, Winett RA, & Frederiksen LW (1987). Nicotine fading, behavioral contracting, and extended treatment: effects on smoking cessation. Addictive Behaviors, 12(2), 181–184. 10.1016/0306-4603(87)90024-4 [DOI] [PubMed] [Google Scholar]
- Chen H, Cohen P, & Chen S (2010). How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics—Simulation and Computation, 39(4), 860–864. 10.1080/03610911003650383 [DOI] [Google Scholar]
- Cohen E, Feinn R, Arias A, & Kranzler HR (2007). Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 86(2–3), 214–221. 10.1016/j.drugalcdep.2006.06.008 [DOI] [PubMed] [Google Scholar]
- Dallery J, & Raiff BR (2011). Contingency management in the 21st century: Technological innovations to promote smoking cessation. Substance Use & Misuse, 46(1), 10–22. 10.3109/10826084.2011.521067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott R, & Tighe T (1968). Breaking the cigarette habit: Effects of a technique involving threatened loss of money. The Psychological Record, 18(4), 503–513. 10.1007/BF03393800 [DOI] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, & Huang B (2015). Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA psychiatry, 72(8), 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green L, & Myerson J (2004). A discounting framework for choice with delayed and probabilistic rewards. Psychological Bulletin, 130(5), 769–792. 10.1037/0033-2909.130.5.769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern SD, French B, Small DS, Saulsgiver K, Harhay MO, Audrain-McGovern J, Loewenstein G, Brennan TA, Asch DA, & Volpp KG (2015). Randomized trial of four financial-incentive programs for smoking cessation. The New England Journal of Medicine, 372, 2108–2117. 10.1056/NEJMoa1414293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, & Grant BF (2007). Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States - Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 64(7), 830–842. 10.1001/archpsyc.64.7.830 [DOI] [PubMed] [Google Scholar]
- Higgins ST, Silverman K, & Heil SH (2008). Contingency management in substance abuse treatment. Guilford Press. [Google Scholar]
- John LK, Loewenstein G, Troxel AB, Norton L, Fassbender JE, & Volpp KG (2011). Financial incentives for extended weight loss: A randomized, controlled trial. Journal of General Internal Medicine, 26(6), 621–626. 10.1007/s11606-010-1628-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahneman D, & Tversky A (1979). Prospect theory: An analysis of decision under risk. Econometrica, 47(2), 263–291. 10.2307/1914185 [DOI] [Google Scholar]
- Kaplan BA, & Koffarnus MN (2019). Timeline followback self-reports underestimate alcohol use prior to successful contingency management treatment. Alcohol and Alcoholism, 54(3), 258–263. 10.1093/alcalc/agz031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KC, Carpenedo CM, Stitzer ML, Dugosh KL, Petry NM, Roll JM, Saladin ME, Cohen AJ, Hamilton J, & Reese K (2012). Is exposure to an effective contingency management intervention associated with more positive provider beliefs? Journal of Substance Abuse Treatment, 42(4), 356–365. 10.1016/j.jsat.2011.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, & Bickel WK (2014). A 5-trial adjusting delay discounting task: accurate discount rates in less than one minute. Experimental and Clinical Psychopharmacology, 22(3), 222–228. 10.1037/a0035973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Bickel WK, & Kablinger AS (2018). Remote alcohol monitoring to facilitate incentive-based treatment for alcohol use disorder: A randomized trial. Alcoholism: Clinical and Experimental Research, 42(12), 2423–2431. 10.1111/acer.13891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Jarmolowicz DP, Mueller ET, & Bickel WK (2013). Changing delay discounting in the light of the competing neurobehavioral decision systems theory: a review. Journal of the Experimental Analysis of Behavior, 99(1), 32–57. 10.1002/jeab.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Wong CJ, Diemer K, Needham M, Hampton J, Fingerhood M, Svikis DS, Bigelow GE, & Silverman K (2011). A randomized clinical trial of a Therapeutic Workplace for chronically unemployed, homeless, alcohol-dependent adults. Alcohol and Alcoholism, 46(5), 561–569. 10.1093/alcalc/agr057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, & Zeger SL (1986). Longitudinal data-analysis using generalized linear-models. Biometrika, 73(1), 13–22. 10.1093/biomet/73.1.13 [DOI] [Google Scholar]
- Liu GH, & Liang KY (1997). Sample size calculations for studies with correlated observations. Biometrics, 53(3), 937–947. 10.2307/2533554 [DOI] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D, & Obrien CP (1992). A New Measure of Substance-Abuse Treatment - Initial Studies of the Treatment Services Review. Journal of Nervous and Mental Disease, 180(2), 101–110. 10.1097/00005053-199202000-00007 [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, & Argeriou M (1992). The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment, 9(3), 199–213. 10.1016/0740-5472(92)90062-s [DOI] [PubMed] [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, & Boettiger CA (2005). Impulsive responding in alcoholics. Alcoholism: Clinical and Experimental Research, 29(12), 2158–2169. 10.1097/01.alc.0000191755.63639.4a [DOI] [PubMed] [Google Scholar]
- Paxton R (1980). The effects of a deposit contract as a component in a behavioural programme for stopping smoking. Behaviour Research and Therapy, 18(1), 45–50. 10.1016/0005-7967(80)90068-6 [DOI] [PubMed] [Google Scholar]
- Paxton R (1981). Deposit contracts with smokers: varying frequency and amount of repayments. Behaviour Research and Therapy, 19(2), 117–123. 10.1016/0005-7967(81)90035-8 [DOI] [PubMed] [Google Scholar]
- Paxton R (1983). Prolonging the effects of deposit contracts with smokers. Behaviour Research and Therapy, 21(4), 425–433. 10.1016/0005-7967(83)90012-8 [DOI] [PubMed] [Google Scholar]
- Petry NM (2001). Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology (Berl), 154(3), 243–250. 10.1007/s002130000638 [DOI] [PubMed] [Google Scholar]
- Petry NM, DePhilippis D, Rash CJ, Drapkin M, & McKay JR (2014). Nationwide dissemination of contingency management: the Veterans Administration initiative. The American Journal on Addictions, 23(3), 205–210. 10.1111/j.1521-0391.2014.12092.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittman B, Gueorguieva R, Krupitsky E, Rudenko AA, Flannery BA, & Krystal JH (2007). Multidimensionality of the alcohol withdrawal symptom checklist: A factor analysis of the alcohol withdrawal symptom checklist and CIWA-Ar. Alcoholism: Clinical and Experimental Research, 31(4), 612–618. 10.1111/j.1530-0277.2007.00345.x [DOI] [PubMed] [Google Scholar]
- Rachlin H, & Green L (1972). Commitment, choice and self-control. Journal of the Experimental Analysis of Behavior, 17(1), 15–22. 10.1901/jeab.1972.17-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash CJ, Petry NM, Kirby KC, Martino S, Roll J, & Stitzer ML (2012). Identifying provider beliefs related to contingency management adoption using the contingency management beliefs questionnaire. Drug and Alcohol Dependence, 121(3), 205–212. 10.1016/j.drugalcdep.2011.08.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, & Higgins ST (2000). A within-subject comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. Drug & Alcohol Dependence, 58(1), 103–109. 10.1016/s0376-8716(99)00073-3 [DOI] [PubMed] [Google Scholar]
- Roll JM, Higgins ST, & Badger GJ (1996). An experimental comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. Journal of Applied Behavior Analysis, 29(4), 495–505. 10.1901/jaba.1996.29-495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, Delafuente JR, & Grant M (1993). Development of the Alcohol-Use Disorders Identification Test (Audit) - Who collaborative project on early detection of persons with harmful alcohol consumption. Addiction, 88(6), 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Silverman K, Holtyn AF, & Jarvis BP (2016). A potential role of anti-poverty programs in health promotion. Preventive Medicine, 92, 58–61. 10.1016/j.ypmed.2016.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Holtyn AF, & Subramaniam S (2018). Behavior analysts in the war on poverty: Developing an operant antipoverty program. Experimental and Clinical Psychopharmacology, 26(6), 515. 10.1037/pha0000230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Holtyn AF, & Toegel F (2019). The utility of operant conditioning to address poverty and drug addiction. Perspectives on Behavior Science, 42(3), 525–546. 10.1007/s40614-019-00203-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sindelar J, Elbel B, & Petry NM (2007). What do we get for our money? Cost-effectiveness of adding contingency management. Addiction, 102(2), 309–316. 10.1111/j.1360-0443.2006.01689.x [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline follow-back. In Measuring alcohol consumption (pp. 41–72). Springer. [Google Scholar]
- Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, & Loewenstein G (2008). Financial incentive-based approaches for weight loss: a randomized trial. The Journal of the American Medical Association, 300(22), 2631–2637. 10.1001/jama.2008.804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winett RA (1973). Parameters of deposite contracts in the modification of smoking. The Psychological Record, 23(1), 49–60. 10.1007/BF03394136 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


