Abstract
Spinal epidural lipomatosis (SEL) is a rare pathologic growth of histologically normal nonencapsulated adipose tissue in the epidural space. It can cause myelopathy or radiculopathy. Etiologies include chronic exposure to endogenous or exogenous steroids and obesity. Idiopathic forms are much infrequent. We present a case of lumbar SEL compressing the thecal sac in a 50-year-old female patient.
A 50-year-old female patient presented to our radiology department complaining of lumbar and right lower extremity pain and weakness. Magnetic resonance imaging (MRI) of the lumbo-sacral spine demonstrated severe circumferential compression of the dural sac (from L5 to S1) caused by significant epidural fat hypertrophy (Fig. 1a–c). The compressed thecal sac adopted a “Y” configuration (Fig. 2), a finding characteristic of a grade III Borré et al. spinal epidural lipomatosis (SEL).
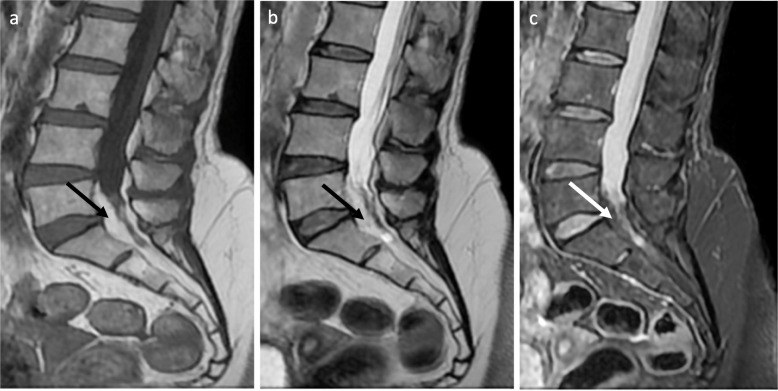
Fig. 1.
Midsagittal T1 (a), T2 (b), and STIR (c) weighted images show a large amount of circumferential epidural fat (black and white arrows) surrounding the dural sac at level L5-S1. No other substantial lumbar spine abnormality is present
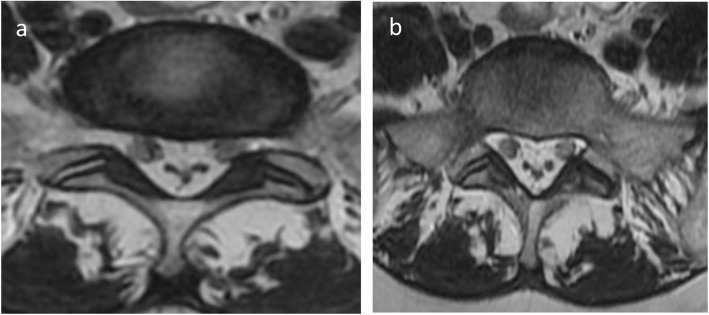
Fig. 2.
Axial T2-weighted images at L5-S1 interspace (a) and S1 superior end plate (b) demonstrate the pathognomonic “Y” shape of the dural sac
SEL is a rare condition characterized by nonencapsulated adipose tissue accumulation in the thoracic or lumbar spinal canal’s epidural space which can cause spinal cord or nerve root compression [1, 2]. It can be due to chronic steroid therapy (55% of cases), obesity (25%), Cushing’s syndrome (3%), or idiopathic (17%) [3]. According to recent studies, SEL should be contemplated as a metabolic syndrome manifestation, alongside increased BMI, abdominal circumference, and visceral and liver fat deposits [4]. To diagnose and grade this condition, MRI is the gold standard imaging modality. Mild (grade I) SEL is asymptomatic, moderate (grade II) SEL is symptomatic in 14.5% of cases, whereas all severe (grade III) SEL cases are symptomatic [1]. Weight loss and/or steroids suspension are efficient therapeutic strategies. When conservative approaches fail, surgical management involving decompressive laminectomy and epidural adipose tissue excision is indicated [5].
Authors' contributions
All authors contributed to the interpretation of data and drafted the manuscript. JEF critically revised the manuscript. All the authors have read and approved the final draft of the manuscript.
Funding
No funding was received.
Availability of data and materials
Data are available on reasonable request from the authors.
Declarations
Ethics approval and consent to participate
Ethical approval is not required for de-identified single case reports based on institutional policies.
Consent for publication
Consent for publication was obtained in accordance with the journal's patient consent policy.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Borré, D. G., Borré, G. E., Aude, F., & Palmieri, G. N. Lumbosacral epidural lipomatosis: MRI grading. Eur Radiol. 2003;13(7):1709–21. 10.1007/s00330-002-1716-4. [DOI] [PubMed]
- 2.Koch CA, Doppman JL, Patronas NJ, Nieman LK, Chrousos GP. Do glucocorticoids cause spinal epidural lipomatosis? When endocrinology and spinal surgery meet. Trends in Endocrinology and Metabolism. 2000;11(3):86–90. doi: 10.1016/s1043-2760(00)00236-8. [DOI] [PubMed] [Google Scholar]
- 3.Fogel GR, Cunningham PY, 3rd, Esses SI. Spinal epidural lipomatosis: case reports, literature review and meta-analysis. Spine Journal. 2005;5(2):202–211. doi: 10.1016/j.spinee.2004.05.252. [DOI] [PubMed] [Google Scholar]
- 4.Ishihara, S., Fujita, N., Azuma, K., Michikawa, T., Yagi, M., Tsuji, T., Takayama, M., Matsumoto, H., Nakamura, M., Matsumoto, M., & Watanabe, K. Spinal epidural lipomatosis is a previously unrecognized manifestation of metabolic syndrome. Spine J. 2019;19(3):493–500. 10.1016/j.spinee.2018.07.022. [DOI] [PubMed]
- 5.Kim, K., Mendelis, J., & Cho, W. Spinal Epidural Lipomatosis: A Review of Pathogenesis, Characteristics, Clinical Presentation, and Management. Global Spine J. 2019;9(6):658–65. 10.1177/2192568218793617. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request from the authors.