Abstract
Nonalcoholic fatty liver disease (NAFLD) can develop in lean individuals. Despite a better metabolic profile, the risk of disease progression to hepatic inflammation, fibrosis, and decompensated cirrhosis in the lean is similar to that in obesity-related NAFLD and lean individuals may experience more severe hepatic consequences and higher mortality relative to those with a higher body mass index (BMI). In the absence of early symptoms and abnormal laboratory findings, lean individuals are not likely to be screened for NAFLD or related comorbidities; however, given the progressive nature of the disease and the increased risk of morbidity and mortality, a clearer understanding of the natural history of NAFLD in lean individuals, as well as efforts to raise awareness of the potential health risks of NAFLD in lean individuals, are warranted. In this review, we summarize available data on NAFLD prevalence, clinical characteristics, outcomes, and mortality in lean individuals and discuss factors that may contribute to the development of NAFLD in this population, including links between dietary and genetic factors, menopausal status, and ethnicity. We also highlight the need for greater representation of lean individuals in NAFLD-related clinical trials, as well as more studies to better characterize lean NAFLD, develop improved screening algorithms, and determine specific treatment strategies based on underlying etiology.
Keywords: NAFLD, NASH, Lean, Nonobese, BMI, Prevalence, Clinical outcomes, Menopause, Choline deficiency, Genetic variation, Metabolic syndrome
Introduction
Nonalcoholic fatty liver disease (NAFLD) is a chronic, progressive condition that arises from intrahepatic fat accumulation in the absence of monogenic metabolic disorders, infections, steatogenic medications, or significant alcohol consumption [1]. Since it was first described in 1980 [2], NAFLD has become the most common liver disease in Western populations [3, 4]. NAFLD is also recognized as a common chronic disease worldwide, affecting ~ 24% of the population [5], with a growing prevalence [6, 7]. In the United States, nonalcoholic steatohepatitis (NASH), a severe form of NAFLD characterized by hepatic inflammation and often accompanied by fibrosis, is the major cause of chronic liver disease and is emerging as the most common indication for liver transplantation [8].
Obesity is a risk factor for the development of NAFLD [9, 10] and the prevalence of NAFLD increases in parallel with BMI [11]. Nevertheless, NAFLD is not inextricably linked with obesity, as many individuals with obesity maintain normal intrahepatic content, while a significant number of lean individuals develop NAFLD, even in the absence of insulin resistance, type 2 diabetes (T2D), and related metabolic comorbidities [10]. Early observations by Bellentani et al. [12] noted a NAFLD prevalence of 16% in normal weight individuals enrolled in the Dionysos Study. One of the first studies in nonobese Asian populations reported a NAFLD prevalence > 23%, and many of the same characteristics observed in NAFLD patients with obesity, including male sex, higher BMI, older age, hyperuricemia, and elevated metabolic markers, were also common among nonobese patients [13–15]. Vos et al. [16] described the presence of NAFLD in nonobese individuals (BMI < 30 kg/m2) as a new clinical entity and defined it as “lean-NAFLD”. However, because body weight is not a component of the diagnostic criteria for NAFLD, and describing NAFLD itself as lean is imprecise, “NAFLD in lean individuals” has been suggested as a more accurate description of this condition [17]. In agreement, we utilize this terminology here.
Although NAFLD in lean individuals is not uncommon, the pathophysiology of the disease in lean patients remains poorly characterized. While some characteristics of NAFLD are shared among individuals in obese and lean BMI groups, not all lean individuals with NAFLD have metabolic antecedents that predispose to hepatic dysfunction. In these individuals, factors such as dietary composition, lifestyle factors, and genetic susceptibility may contribute to the development of NAFLD. Despite potentially distinct etiologies, NAFLD in lean individuals appears to follow a disease progression similar to that in patients with overweight or obesity, indicating that the absence of excess corporeal adiposity does not confer protection against hepatic inflammation, fibrosis, or decompensated cirrhosis. As discussed in the following sections, some studies have even reported more severe histological presentation and higher mortality in NAFLD patients with normal BMI compared to higher BMI groups.
Because NAFLD is a clinically silent disease in most cases, the absence of early signs and symptoms, coupled with normal laboratory and anthropometric measures, likely blind clinicians to the presence of NAFLD in lean individuals. However, lean NAFLD patients are at risk for progression to severe liver disease and possibly even increased mortality, warranting efforts to promote awareness of NAFLD in lean individuals. In this review, we summarize the literature on NAFLD prevalence, characteristics, outcomes, and mortality in lean individuals and discuss factors that may contribute to the development of NAFLD in this patient population. We also address clinical strategies for the screening and management of NAFLD in lean individuals based on suspected etiologies.
Prevalence of NAFLD in lean individuals
The prevalence of NAFLD in lean individuals has been estimated almost exclusively using BMI as the sole criterion to describe body habitus. The international definition for normal BMI is defined as < 25 kg/m2. However, in Asians and Pacific Islanders, a BMI of < 23 kg/m2 is used due to the occurrence of visceral adiposity and risk of developing comorbidities, such as T2D and cardiovascular disease, at a lower BMI than that found in Europeans [18]. Using these thresholds to define lean individuals, a comprehensive survey of available studies based on BMI cut-offs of < 25 kg/m2 (< 23 kg/m2 for Asians) for lean individuals indicates that the prevalence of NAFLD ranges from 5 to 34% (Table 1). Of note, there is significant heterogeneity among these studies, which vary by geography, method of NAFLD determination, design, sample size, and comparison group. For example, the assignment of NAFLD was based on a number of different methods including liver biopsy, abdominal ultrasonography, computed tomography, liver function tests (i.e., hepatic transaminases), magnetic resonance imaging, controlled attenuation parameter, and several indices. Some studies were population-based, while others were hospital-based or located at a tertiary care clinic. Sample sizes ranged from 39 to more than 10,000, with the majority of studies emanating from South and East Asia. Comparator groups were either lean NAFLD compared to all lean or lean NAFLD compared to all NAFLD.
Table 1.
Prevalence of NAFLD in individuals with normal BMI
| Study | Country | Setting | Method | N | Comparison | Prev (%) |
|---|---|---|---|---|---|---|
| European/North American | ||||||
| Bellentani et al. [12] | Italy | Population-based | USa | 67 | Lean NAFLD/all lean | 16.4 |
| Yououssi et al. [26] | USA | Population-based | US | 4457 | Lean NAFLD/all lean | 7.4 |
| Margariti et al. [29] | Greece | Tertiary clinic | US or biopsy | 162 | Lean NAFLD/all NAFLD | 11.7 |
| Chiloiro et al. [141] | Italy | Population-based | US | 2946 | Lean NAFLD/all lean | 8.1 |
| Cruz et al. [142] | USA | Hospital-based | Biopsy | 1090 | Lean NAFLD/all NAFLD | 11.5 |
| Denkmayr et al. [31] | Austria | Tertiary clinic | Biopsy | 466 | Lean NAFLD/all NAFLD | 15.9 |
| Hagström et al. [36] | Sweden | Hospital-based | Biopsy | 646 | Lean NAFLD/all NAFLD | 19.0 |
| Golabi et al. [37] | USA | Population-based | US or IONb | 5375 | Lean NAFLD/all lean i | 10.8 |
| Alferink et al. [143] | Netherlands | Population-based | US | 3882 | Lean NAFLD/all NAFLD | 9.9 |
| Zou et al. [38] | USA | Population-based | USFLIc | 4711 | Lean NAFLD/all NAFLD | 4.9 |
| Ahmed et al. [27] | USA | Hospital-based | Biopsy or imaging | 4834 | Lean NAFLD/all NAFLD | 8.6 |
| Younes et al. [33] | Multisite | Tertiary clinic | Biopsy | 1339 | Lean NAFLD/all NAFLD | 14.1 |
| Middle Eastern | ||||||
| Akyuz et al. [144] | Turkey | Hospital-based | US or biopsy | 483 | Lean NAFLD/all NAFLD | 7.6 |
| Lankarani et al. [145] | Iran | Population-based | US | 819 | Lean NAFLD/all NAFLD | 16.4 |
| South Asian | ||||||
| Singh et al. [15] | India | Tertiary clinich | US | 39 | Lean NAFLD/all NAFLD | 17.9 |
| Das et al. [146] | India | Population-based | US and CTd | 164 | Lean NAFLD/all NAFLD | 31.7 |
| Kumar et al. [147] | India | Hospital-based | US | 205 | Lean NAFLD/all NAFLD | 13.2 |
| Bhat et al. [148] | India | Tertiary clinic | US and LFTe | 150 | Lean NAFLD/all NAFLD | 15.3 |
| Singh et al. [149] | India | Tertiary clinic | US | 632 | Lean NAFLD/all NAFLD | 15.9 |
| Alam et al. [150] | Bangladesh | Population-based | US | 2782 | Lean NAFLD/all NAFLD | 14.5 |
| Niriella et al. [108] | Sri Lanka | Population-based | US | 936 | Lean NAFLD/all NAFLD | 12.8 |
| Rahman et al. [151] | Bangladesh | Population-based | US | 1305 | Lean NAFLD/all NAFLD | 4.1 |
| Choudhary et al. [152] | India | Tertiary clinich | Biopsy | 157 | Lean NAFLD/all lean | 33.5 |
| East Asian | ||||||
| Kim et al. [14] | Korea | Population-basedh | US | 460 | Lean NAFLD/all lean | 16.1 |
| Hsiao et al. [153] | Taiwan | Hospital-based | US | 16,309 | Lean NAFLD/all lean | 32.1 |
| Goh et al. [154] | Malaysia | Hospital-basedh | US | 1621 | Lean NAFLD/all NAFLD | 10.6 |
| Feng et al. [155] | China | Hospital-basedh | US | 731 | Lean NAFLD/all lean | 18.3 |
| Fukuda et al. [156] | Japan | Population-basedh | US | 4629 | Lean NAFLD/all lean | 4.6 |
| Wang et al. [157] | China | Population-based | US | 4899 | Lean NAFLD/all lean | 12.7 |
| Yoshitaka et al. [158] | Japan | Hospital-basedh | US | 1647 | Lean NAFLD/all NAFLD | 22.1 |
| Shao et al. [159] | China | Hospital-based | US and MRI | 1509 | Lean NAFLD/all NAFLD | 20.2 |
| Wang [160] | Japan | Hospital-basedh | US | 10,064 | Lean NAFLD/ all lean | 5.4 |
| Meta-analysis | ||||||
| Ye et al. [20] | Multinational | Multiple | US, CT, MRIf, CAPg, FLIh, HISi, LPAIj, or biopsy | 63,017 | Lean NAFLD/all lean | 10.6 |
| Shi et al. [21] | Multinational | Population-basedh | US | 55,936 | Lean NAFLD/all lean | 10.2 |
Normal BMI: < 25 kg/m2 for non-Asians; < 23 kg/m2 for Asians
aUS: abdominal ultrasonography
bION: index of NASH
cUSFLI: US fatty liver index
dCT: computed tomography
eLFT: liver function tests (i.e., hepatic transaminases)
fMRI: magnetic resonance imaging
gCAP: controlled attenuation parameter
hFLI: fatty liver index
iHIS: hepatic steatosis index
jLPAI: liver-spleen attenuation index
hRecruited from population of apparently healthy individuals or health checkup program
The highest NAFLD prevalence rates (e.g., > 30%) were observed in India, and were based on estimates obtained from community-based populations, indicating a lower degree of bias compared to studies in which participants were recruited from hospitals or tertiary liver clinics. This increased prevalence, coupled with observations that lean, healthy, sedentary, non-smoking Asian-Indian men have a three- to fourfold increased prevalence of insulin resistance associated with a twofold increase in hepatic fat content compared to Eastern Asian, Black, Caucasian, and Hispanic men [19], suggests that this lean population may be at particular risk for NAFLD due to yet-to-be-identified factors.
In addition to the individual studies in Table 1, a comprehensive meta-analysis using data from 84 studies (n = 10,530,308) found that within the NAFLD population, 19.2% (95% Confidence Interval [CI] 15.9–23.0) of participants were lean [20]. However, in the general population (23 studies; n = 113,394), comprising all individuals regardless of NAFLD status, only 5.1% (95% CI 3.7–7.0) had NAFLD in the presence of normal BMI. Among the lean population (19 studies; n = 49,503), 10.6% (95% CI 7.8–14.1) had NAFLD. The authors noted high heterogeneity among the results, although in general, European countries appeared to have the highest, and Asian countries the lowest, prevalence of NAFLD in nonobese individuals. In a similar analysis of 21 studies (N = 55,936), Shi et al. [21] estimated an overall NAFLD prevalence rate of 10.2% (95% CI 7.6–13.6%) in lean populations, also noting significant heterogeneity. Data from the Global NAFLD/NASH Registry comprising data from 18 countries found that approximately 8% of the patients were lean, based on BMI, and exhibited fewer components of the metabolic syndrome, fewer comorbidities, and less cirrhosis [22]. The year in which data were collected and sample size significantly impacted estimates of NAFLD prevalence, but BMI cut-off, region of study, population source, and method of diagnosis also exerted nonsignificant effects on the observed heterogeneity. Like obesity-associated NAFLD [6], the prevalence of NAFLD in lean individuals is also increasing. In studies with data collected before 2000, the prevalence was 5.6%, but from 2001 to 2010, and after 2011, rates were estimated at ~ 11.0% and 12.6%, respectively, reflecting the trend of increasing prevalence in the overall population [23].
Several groups have estimated NAFLD prevalence in nonobese populations using combined normal and overweight BMI groups (i.e., < 30 kg/m2 [< 25 kg/m2 in Asians]). In China, a population study comprising 911 individuals recruited from the census database of the Hong Kong government reported a NAFLD prevalence of 19.3% in nonobese subjects [24]. In a cross-sectional study of individuals receiving health checkups in Japan, NAFLD prevalence in nonobese individuals was estimated at 15.2% [25]. NAFLD prevalence in nonobese, nondiabetic Belgians undergoing biopsy for chronic liver disease was 2.8% (50/1777) [16]. Estimates in nonobese populations are similar to those found in lean populations (Table 1), revealing potential limitations of BMI cut-off for NAFLD screening in the general population.
Clinical characteristics, outcomes, and mortality of lean individuals with NAFLD
Clinical characteristics
A number of studies have compared clinical characteristics between lean and non-lean NAFLD cohorts. An early study by Vos et al. [16] observed the presence of NASH and fibrosis in 61% and 55% of the lean group, respectively. Relative to healthy controls, these individuals were less insulin sensitive and had higher triglyceride levels. However, these observations were based on a BMI cut-off < 30 kg/m2 for lean individuals and a relatively small sample size (31 “lean” and 48 obese individuals with NAFLD and eight healthy controls), thereby, limiting the conclusions to be drawn.
A survey of available studies indicates that, in general, lean individuals with NAFLD have a more favorable metabolic profile compared to those with a higher BMI (Table 2). Measures of metabolic markers such as waist circumference, triglyceride levels, fasting plasma glucose, HDL-C (high-density lipoprotein-cholesterol), adiponectin levels, and Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) appear to be intermediate between lean individuals without NAFLD and those with both NAFLD and obesity (Table 2). Many studies report a male dominance and younger age relative to the non-lean group. Multivariate analysis of data from the National Health and Nutrition Examination Survey III (NHANES III) showed that lean individuals with NAFLD were more commonly Hispanic with T2D and hypertension compared to lean control individuals without liver disease, but relative to individuals with overweight or obesity, NAFLD in lean individuals was independently associated with younger age, female sex, and a lower prevalence of insulin resistance and hypercholesterolemia [26]. Among NAFLD patients living in Olmstead County (Minnesota), female predominance (66.9%) and a higher proportion of Asian and African American individuals (13.2%) were found in lean individuals compared to overweight (47.2%; 6.5%) and obese (56.1%; 7.4%) groups [27]. Feldman et al. [28] reported lower serum levels of lysophosphatidylcholines and phosphatidylcholines and higher levels of glutamate in lean individuals with NAFLD relative to lean healthy controls, but no differences in level of physical activity or frequency of fast-food consumption were observed between the two weight groups. In this study, lean individuals with NAFLD had levels of severely impaired glucose tolerance almost identical to those in found in NAFLD patients with obesity, and ~ 30% were diagnosed with T2D. Glucose homeostasis thus appears to be abnormal in some lean subjects with NAFLD, confirming data suggesting that the accumulation of liver fat may be of particular importance to the development of insulin resistance and diabetes even in the absence of obesity [28].
Table 2.
Characteristics and mortality associated with NAFLD in lean individuals
| Study | Country | Agea | BMI | ALT (U/L)a | AST (U/L)a | Metabolic profile and related characteristicsb | Mortality | F/Uc |
|---|---|---|---|---|---|---|---|---|
| European/North American | ||||||||
| Younossi et al. [26] | USA | 41.9 ± 1.2 | 22.2 ± 0.16 | 18.0 ± 0.16 | 21.5 ± 0.16 | Younger, female predominance, lower ALT, AST, HOMA score, platelet count, lower frequency of visceral obesity, insulin resistance, T2D, hypercholesteremia, and hypertension | – | – |
| Margariti et al. [29] | Greece | 44 ± 16 | NA | 92 (17–164) | 45 (18–121) | Higher ALT and AST, less comorbidities, smaller waist circumference, lower liver stiffness measures | – | – |
| Cruz et al. [142] | USA | NA | 23.1 ± 1.7 | NA | NA | Male predominance, non-Caucasian, lower ALT levels and HOMA, lower prevalence of T2D, hypertension, hypertriglyceridemia, low-HDL-C, central obesity, and metabolic syndrome, lower degree of steatosis and less advanced fibrosis, more severe lobular inflammation | Higher overall mortality than non-lean NAFLD patients | 11.1 ± 6.8 |
| Feldman et al. [28] | Austria | 61 (12)d | 23.6 (1.8)d | 21.0 (14.0)d | 22.0 (10.5)d | Waist circumference, ALT, GGT, TG, HDL-C, FPG, adiponectin levels, and HOMA-IR intermediate between lean healthy and NAFLD with obesity | – | – |
| Fracanzani et al. [30] | Italy | 46 ± 13 | 23 ± 2 | 64 ± 42 | 41 ± 27 | Less prevalence of hypertension, diabetes, and metabolic syndrome, NASH, fibrosis of F2 or higher, carotid plaques and significantly thinner carotid intima-media | – | – |
| Denkmayr et al. [31] | Austria | 48.7 ± 14.8 | 23.1 ± 1.5 | 60.0 ± 36.4 | 43.0 ± 26.9 | Less components of metabolic syndrome, higher rate of cirrhosis | – | – |
| Bernhardt et al. [161] | Germany | NA | 23.8 (23.0–24.7) | 26.0 ± 7.1 | 26.4 ± 3.0 | Higher serum ferritin, hemoglobin, hematocrit, and mean corpuscular hemoglobin concentration, lower levels of soluble transferrin receptor, high HOMA-IR, TC, LDL-C, and TG, comparable to NAFLD patients with obesity | – | – |
| Hagstrom et al. [36] | Sweden | 51.4 ± 13.4 | 23.1 ± 2.7 | 72 ± 47 | 44 ± 25 | Older, lower transaminase levels, lower stages of fibrosis, and lower prevalence of NASH at baseline; increased risk for severe liver disease | Similar overall mortality as non-lean NAFLD patients | 19.9 |
| Golabi et al. [37] | USA | 50.9 ± 1.3 | NA | NA | NA | Older, more likely to be Hispanic, had lower income, and had reported poorer health and more comorbiditiese | Higher risk for all cause and CV mortality compared to lean controls | 17.8 |
| Feldman et al. [162] | Austria | 47.6 ± 14.5 | 23.0 ± 1.5 | 54.6 ± 35.5 | 47.6 ± 24.8 | Higher likelihood of dying from liver-related causes compared NAFLD patients with overweight or obesity; higher proportion with cirrhosis; less features of metabolic syndrome | Similar overall mortality as NAFLD patients with obesity | 8.4 |
| Ahmed et al. [27] | USA | 51.5 ± 18.0 | 22.5 ± 2.0 | NA | NA | Female predominance, higher proportion of Asian and African Americans, lower risk of metabolic comorbidities; same risk of cirrhosis and decompensation, malignancy, and cardiovascular events as non-lean NAFLD patients | Higher risk for all-cause mortality compared to NAFLD patients with obesity | 6.4 |
| Younes et al. [33] | USA | 45 (36, 55)d | 29.8 (26.5, 34.5)d | 59 (41, 88)d | 38 (28, 54)d | Younger, male predominance, less steatosis, lobular inflammation, ballooning and advanced liver fibrosis | Same mortality risk as non-lean NAFLD patients | 7.7 |
| Middle Eastern | ||||||||
| Akyuz et al. [144] | Turkey | 41.2 ± 11.8 | 23.6 ± 1.3 | 82 ± 46 | 49 ± 38 | Younger, lower blood pressure, higher hemoglobin, lower prevalence of metabolic syndrome, and less severe hepatic fibrosis | – | – |
| Lankarani et al. [145] | Iran | 49.8 ± 13.9 | NA | NA | NA | Lower waist circumference, TG levels, and prevalence of metabolic syndrome | – | – |
| South Asian | ||||||||
| Kumar et al. [147] | India | 38 ± 15.4 | 21.3 ± 1.9 | 45 (11–217) | 38 (23–180) | Similar metabolic profile as overweight group, but lower than obese group, lower prevalence of fibrosis in lean individuals, but similar prevalence of NASH | – | – |
| Bhat et al. [148] | India | 39.9 ± 7.4 | 21.7 ± 1.3 | 69.9 ± 29.8 | NA | Lower HOMA-IR, similar levels of fasting and 2 h glucose and lipid levels | – | – |
| Niriella et al. [108] | Sri Lanka | 35.6 ± 6.4 | NA | NA | NA | Male predominance, lower prevalence of hypertension and central obesity, similar prevalence of other metabolic comorbidities as non-lean group | – | – |
| Choudhary et al. [152] | India | 33.5 ± 10.4 | 21.3 ± 1.2 | 33.4 ± 11.7 | 26.6 ± 7.5 | Younger age, lower ALT, TGs, fasting glucose, LDL-C, higher HDL-C than non-lean group | – | – |
| East Asian | ||||||||
| Kim et al. [14] | Korea | 51.6 ± 9.7 | 23.4 ± 1.3 | 31.9 ± 19.0 | 23.5 ± 7.7 | Male predominance, higher BMI, WC, WHR, uric acid, fasting blood glucose, insulin, ASP, ALT, HOMA-IR compared to lean controls; no differences in metabolic variables compared to overweight group | – | – |
| Feng et al. [155] | China | 48.2 ± 10.5 | 22.7 ± 1.1 | 21.6 ± 11.9 | 21.1 ± 9.3 | Male predominance, higher BMI and blood pressure, and greater likelihood of having diabetes, metabolic syndrome, and hypertension compared to lean controls; lower levels of blood glucose, blood pressure, hyperlipidemia, IR, blood cell count and HGB than non-lean NAFLD patients | – | – |
| Fukuda [156] | Japan | 42.6 ± 7.6 | 21.8 ± 0.9 | 25 (19, 36) | 19 (15, 23) | Male predominance, higher incidence of T2D, ALT, AST, HbA1c, FPG, and TG compared to overweight group without NAFLD and lean control group | – | 12.8 |
| Wang et al. [157] | China | 43 (32–58) | 21.6 (20.2–22.8) | 16.1 ± 12.3 | 20.3 ± 8.0 | Male predominance | – | – |
| Yoshitaka et al. [158] | Japan | 50.0 ± 7.9 | 22.0 ± 0.7 | 30.2 ± 15.9 | 21.1 ± 6.1 | Higher blood pressure, triglycerides, fasting plasma glucose, uric acid, ALT, AST, and GGT, lower HDL-C, higher risk of incident CVD relative to lean controls | – | – |
| Shao et al. [159] | China | 44.7 ± 11.9 | 21.6 ± 1.2 | 24 (19, 35) | 25 (20, 32) | Lower WC, WHR, blood pressure, ALT, AST, fasting insulin, HOMA-IR, atherosclerosis index, liver fat content, and liver stiffness compared to nonlean group with NAFLD | ||
| Wang [160] | Japan | 45.6 ± 8.3 | 21.7 ± 1.1 | 16.2 ± 11.5 | 17.2 ± 8.4 | Male predominance, older age, higher BMI, WC, smoking status, FPG, HbA1c, TG, blood pressure, hepatic transaminases, and risk of incident T2D, and lower HDL-C compared to lean control group | ||
| Meta-analyses | ||||||||
| Sookoian and Pirola [34] | Multi | NA | NA | NA | NA | Lower fibrosis score, less risk for NASH, and lower NAFLD activity compared to NAFLD patients with obesity | – | – |
BMI: < 25 kg/m2 for non-Asians; < 23 kg/m2 for Asians
NA information not available
aMean (standard deviation) unless indicated otherwise
bCompared to NAFLD patients with obesity, unless noted otherwise
cAverage follow-up in years
dMedian (interquartile rang [IQR])
eCompared to lean non-NAFLD controls
Despite the better metabolic profile generally observed in lean individuals with NAFLD relative to those with obesity, the risk of disease progression to NASH is comparable to that experienced in NAFLD patients with overweight or obesity. In 56 Greek subjects with liver biopsy-documented NAFLD, the severity of inflammation and fibrosis did not differ between weight groups and NASH prevalence in lean individuals was 50% (compared to 68.8% in the non-lean NAFLD group) [29]. Another study found that 42% of lean Italian NAFLD patients had NASH, of which 42.3% had a fibrosis score of 2 or higher [30]. In lean Austrians with NAFLD, rates of portal inflammation, lobular inflammation, hepatocyte ballooning, perisinusoidal and periportal fibrosis, and NASH were similar between lean and non-lean groups [31, 32], although the proportion of lean individuals with cirrhosis was significantly higher compared to non-lean groups (11% vs. 2–3%) [32]. In NHANES III participants, individuals with normal BMI had the same risk of cirrhosis and decompensation, malignancy, and cardiovascular events as those in the overweight and obese categories, indicating that in these individuals, a normal BMI does not confer protection against progression or severity of liver dysfunction in the context of NAFLD [27].
In contrast, a multinational study found that lean subjects with NAFLD had significantly less steatosis, lobular inflammation, ballooning, and advanced liver fibrosis compared to the non-lean group, although 50% and 10% of lean individuals displayed mild/moderate fibrosis and advanced fibrosis, respectively [33]. Findings from meta-analyses studies were in agreement with a more favorable metabolic profile and milder disease progression in lean individuals with NAFLD. Sookoian and Pirola [34] reported that lean NAFLD patients showed less severe histological features than NAFLD patients with overweight or obesity and were less likely to have NASH. However, 33% of lean individuals with NAFLD had NASH, and it should be noted that in this analysis, all but one of the studies in Asian populations failed to use the BMI cut-off point of < 23 kg/m2, and therefore, included overweight individuals in the estimates. Shi et al. [21] found that lean and nonobese NAFLD patients were predominantly male and had a significantly lower rate of hypertension, lower waist circumference, lower levels of fasting plasma glucose, triglycerides, and uric acid, and higher levels of HDL-C compared to NAFLD patients with obesity. No significant differences were observed between these two groups with respect to diabetes prevalence, age, and levels of total cholesterol and low-density lipoprotein-cholesterol (LDL-C), suggesting that lean/nonobese NAFLD patients may have a risk for developing metabolic diseases similar to NAFLD patients with obesity. Alam et al. observed that lean and non-lean NAFLD patients had similar characteristics and shared common risk factors [35].
Outcomes and mortality
Few studies have investigated differences in outcomes and mortality between lean and non-lean individuals with NAFLD (Table 2). Lean Swedish patients with NAFLD, despite a better prognostic profile at baseline, including a lower prevalence of NASH and advanced fibrosis, showed an increased risk for development of severe liver disease during follow-up compared to patients with a higher BMI, even after adjustment for age and fibrosis stage at baseline [36]. This unexpected finding may indicate that the lean individuals in this study experienced a faster rate of fibrosis progression relative to patients with a higher BMI. In a cohort of 1339 NAFLD patients from Australia, Italy, Spain, and the United Kingdom, followed for a median period of 7.6 years, new onset diabetes, cardiovascular events, extrahepatic cancers, liver-related events, and hepatocellular carcinoma (HCC) occurred in 6.2%, 7.3%, 4.7%, 8.9%, and 1.0% of lean individuals, respectively [33]. The incidence of these complications, as well as overall survival, were not significantly different between normal and high BMI groups.
Using data from the NHANES III with a median follow-up period of 17.8 years, Golabi et al. [37] reported that the weighted, unadjusted all-cause mortality was significantly higher in lean individuals with NAFLD compared to lean individuals without NAFLD (40.9% vs. 17.9%, P < 0.001). In lean NAFLD patients, the unadjusted hazard ratio (HR) for all-cause mortality was 2.44 (95% CI 1.77–3.37), which remained significant after adjusting for demographic variables, metabolic components, and primary comorbidities. Likewise, weighted unadjusted cardiovascular mortality was also significantly higher in lean individuals with NAFLD (15.1% vs. 3.7%, P < 0.001), showing a 238% increased risk of cardiovascular mortality, following adjustment. In 299 Austrian NAFLD patients (38 lean, 165 overweight, and 93 obese) over a follow-up period of 8.4 years, lean individuals had a lower overall mortality compared to overweight patients, but a mortality rate similar to NAFLD patients with obesity [32]. Notably, in this population, lean patients had a significantly higher mortality rate from liver-related causes compared to the overweight (11% vs. 4%) and obese groups (11% vs. 4%). In NAFLD patients from Olmstead County, the normal BMI group had a higher risk of death relative to the high BMI group [27]. The most common causes of death in the normal BMI group were malignancy (25.7%), cardiovascular event (21.6%), and infection (13.5%). In contrast to the findings reported by Feldman et al. [32], who reported significantly higher numbers of fatal liver-related events in the lean BMI group compared to higher BMI groups, mortality due to hepatic events was significantly lower in the normal BMI group (1.4%) compared to the obese BMI group (10.4%), but similar to the overweight BMI group (2.0%), and no significant differences in mortality from cardiovascular events or malignancy were observed among the three groups. A recent study by Zou et al. [38] found that lean NAFLD patients had the highest 15-year cumulative all-cause mortality (76.3%) compared to nonobese NAFLD patients (51.7%), NAFLD patients with obesity (27.2%), and individuals without NAFLD (20.7%). The analysis revealed similar patterns related to cardiovascular disease (16.9% vs. 5.6% vs. 8.8%, respectively, P = 0.0013).
Combined, these studies indicate that despite lower adiposity, less severe dyslipidemia, and lower levels of hepatic transaminases, lean individuals with NAFLD are at similar or greater risk as those with higher BMI for cardiovascular disease, malignancy, progressive liver disease, and increased all-cause mortality associated with NAFLD. The reason(s) for this relative increase in risk has not yet been characterized and may likely depend on the underlying pathogenesis of NAFLD in lean individuals.
Possible causes of NAFLD in lean individuals
Recent epidemiological and clinical studies have identified a number of factors that may contribute to the development of NAFLD in the absence of excess adiposity (Fig. 1). The main classes of these factors include environmental determinants, of which the role of dietary composition has been the best studied, genetic susceptibility, endocrine dysfunction, and metabolic derangement. Some of these factors are known to interact with one another to modulate NAFLD risk, oftentimes in the presence of increasing visceral adiposity, regardless of BMI, suggesting a common metabolic pathway that underlies NAFLD development in all individuals regardless of body habitus.
Fig. 1.
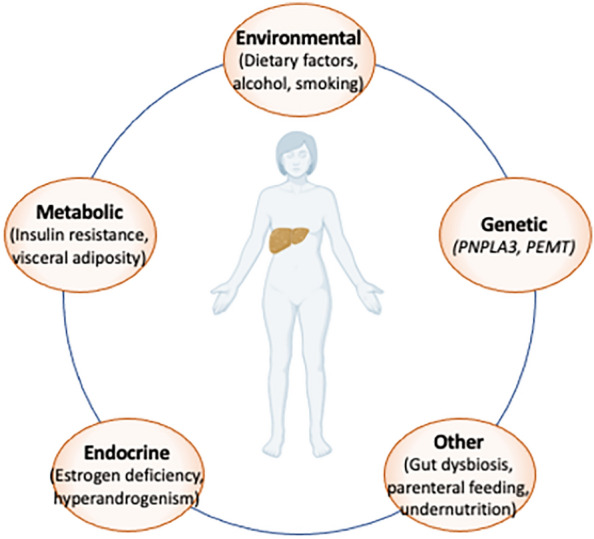
Potential contributors to NAFLD in lean individuals. Despite the same pathological findings in the liver, the factors that contribute to NAFLD and subsequent progression NASH in lean individuals are not yet well-characterized relative to those with obesity-related NAFLD. However, a number of factors that likely influence risk of NAFLD development and progression, even in the absence of excess adiposity, have been postulated in the recent literature. The majority of these risk factors fall into environmental, endocrine, genetic, and metabolic origins. Most of these factors are also expected to interact with one another, as well as other, as-yet-undefined factors, to further modulate NAFLD risk
Environmental factors
Excessive intakes of sucrose, refined carbohydrates, saturated fats, and animal protein are generally regarded as major factors in the development of NAFLD [39–44]. In particular, regular consumption of sugar-sweetened beverages is strongly associated with NAFLD in adults [39, 45–47] and children [48]. In adults, soft drink consumption predicts NAFLD, even following adjustment for dietary composition and physical activity level [47]. Soft drink consumption in NAFLD patients with no risk factors for metabolic syndrome was three times higher than in healthy controls and was significantly associated with the presence of fatty liver [49].
Fructose is a monosaccharide that, together with glucose, forms sucrose (table sugar). Regular dietary fructose consumption induces hepatic de novo lipogenesis and endoplasmic stress, impairs fatty acid oxidation, depletes beneficial microbial species in the gut [50], and promotes hepatic inflammation through the generation of both uric acid and gut-derived endotoxins [51–55]. Due to the constellation of these metabolic effects, dietary fructose may indirectly promulgate hepatic insulin resistance, an important factor in the development of NAFLD [52]. The relationship between dietary fructose and NAFLD is an area of active investigation [56–63]. For example, in adults with NAFLD, daily fructose consumption was associated with higher fibrosis stage [64], while in children, high fructose intake was independently associated with NASH [65].
Thus far, dietary interventions for NAFLD have been limited to non-lean individuals. In a comparison of fat- and carbohydrate-restricted diets in adults with obesity and NAFLD, only the latter led to significant reductions in hepatic fat fraction [66]. Interestingly, the carbohydrate-restricted group also exhibited significantly greater reductions in insulin resistance, abdominal fat mass, and body fat mass compared to the fat-restricted group [66]. Eight weeks of sugar restriction in adolescent males with NAFLD yielded significant decreases in hepatic fat fraction, mean body weight, and mean levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), and total cholesterol [67]. Reduced liver fat was independent of changes in weight or measures of adiposity [67]. Similarly, isocaloric substitution of starch for sugar over a period of 9 days resulted in reduced levels of liver fat, visceral adipose tissue, fractional de novo lipogenesis, and insulin resistance in children with obesity who reported habitually high (> 50 g/day) sugar consumption [68]. The strongest effects of a low fructose, low glycemic index, and low glycemic load diet on metabolic parameters were observed in children with NASH, who also had the highest reported dietary intakes of fructose at baseline, compared to children with NAFLD, and healthy controls [69]. Consistent with these results, current EASL guidelines now recommend a Mediterranean diet with avoidance of processed foods and added fructose for individuals with NAFLD [3].
Some dietary components have been associated with NAFLD in lean individuals. Deprivation of choline, an essential nutrient for human health [70], for 3 weeks in healthy male volunteers resulted in increased ALT activity [71]. Extended depletion of choline for up to 42 days resulted in significant liver dysfunction in men and postmenopausal women [72–74]. Postmenopausal women from the NASH Clinical Research Network study with low dietary choline intake had worse fibrosis (OR 3.37; p = 0.002) after adjusting for age, race, obesity, triglycerides, alcohol, and steroid use [75]. In normal-weight Chinese women, higher dietary choline intake was associated with a lower risk of NAFLD [76]. The Adequate Intake (AI) for choline is 550 mg/day for men and 425 mg/day for women, although analyses of dietary patterns reveal that the vast majority of individuals do not achieve these levels [76–78]. Because choline is present at more abundant levels in animal-derived foods, vegetarians and vegans may have a greater risk of deficiency, and therefore a higher risk of NAFLD due to inadequate intake [77, 78].
In the choline biosynthesis pathway, phosphatidylethanolamine N-methyltransferase (PEMT) catalyzes the formation of phosphatidylcholine, which is required for the secretion of VLDL (very low-density lipoprotein-cholesterol) in the liver [79]. PEMT−/− mice fed a diet high in fat and sucrose rapidly develop hepatic steatosis, inflammation, and fibrosis; dietary choline supplementation ameliorated liver damage in these animals [80–84]. In humans, hepatic PEMT expression was observed to be lower in NASH patients compared to NAFLD patients, and was significantly correlated with platelet counts, which decline in tandem with progression of fibrosis [80]. Lower hepatic PEMT expression was also associated with lower BMI [80], in keeping with the demonstration that PEMT−/− mice are protected from high fat diet-induced obesity and insulin resistance [84, 85]. Because the PEMT gene is regulated by estrogen [86, 87], the detrimental impact of choline deficiency may be exacerbated following the menopausal transition, consistent with findings from choline depletion [73, 88] and observational studies [75]. Together, findings from human and mouse studies suggest that choline deficiency, whether due to low PEMT expression or inadequate dietary intake, may be related to the development of NAFLD and a susceptibility toward progressive disease specifically in lean individuals.
Other environmental factors that may modulate NAFLD include alcohol consumption and cigarette smoking. The diagnostic criteria for NAFLD requires the absence of significant alcohol consumption, although there is not yet a global consensus among professional societies on what level is considered “significant”. In the United States, alcohol limits for men and women are 294 g/week and 196 g/week, respectively [89], while in Europe and Asia, limits are 210 g/week (men)/140 g/week (women) [3] and 140 g/week (men)/70 g/week (women) [3, 90, 91], respectively. However, a retrospective study using prospectively recorded data found that French NAFLD patients who consumed more than 7 units/week (i.e., 56 g) experienced a significantly higher mortality than those consuming less, and conversely, alcohol consumption of less than 1 unit/week (8 g) was significantly associated with improved survival in NAFLD patients [92]. In the NAFLD population, alcohol consumption in excess of 7 units of alcohol/week significantly increased the probability of death from cardiovascular causes and was associated with a significantly higher rate of overall complications, as well as cardiovascular- and cancer-related complications [92]. Moderate alcohol consumption (30 g/day for men and 20 g/day for women) has also been associated with worse fibrosis in NAFLD [93]. Other large and multiethnic studies have likewise reported a significant relationship between low-to-moderate alcohol consumption and increased mortality and morbidity risk [94–96]. Interestingly, alcohol consumption worsens liver disease in individuals with obesity. A BMI > 30 kg/m2 was found to double the hepatoxicity of alcohol [97] and synergistically increase the risk of HCC [98]. The role of modest alcohol consumption and NAFLD in lean individuals has not yet been investigated.
Cigarette smoking is associated with NAFLD onset [99], progression to fibrosis, and increased risk for severe liver disease [100–102]. In Chinese men with a history of heavy smoking and moderate alcohol consumption, NAFLD risk was 85% higher compared to individuals who neither drank nor smoke [103].
Genetic susceptibility
Obesity is the strongest independent risk factor for NAFLD, even after adjusting for age, sex, total cholesterol, triglycerides, HDL, LDL, glucose, uric acid, homocysteine, creatinine, AST, ALT, and hypertension [11]. However, even in the presence of severe obesity and the corresponding chronic caloric excess, some individuals do not develop NAFLD. Conversely, the relationship between risk of NAFLD and BMI is J-shaped, with risk increasing below BMI of 19 from a nadir [11]. These data suggest that there are putative NAFLD susceptibility and/or protective factors that can modify the effects of BMI, particularly genetic variation [104]. The single nucleotide variant (SNV) resulting in the I148M substitution (rs738409) in the patatin-like phospholipase domain-containing protein 3 gene (PNPLA3) is the major genetic risk factor for NAFLD known to date [105]. In addition to PNPLA3, variants in MBOAT7 (membrane- bound O-acyltransferase domain-containing 7) and TM6SF2 (trans-membrane 6 superfamily antigen 2) have been associated with NAFLD [106]. Most genetic association studies have been performed in individuals with classical obesity-related NAFLD and few data are available from lean populations.
In a study of 904 community dwelling Japanese participants, in whom the prevalence of NAFLD was 12.4%, 41.4% and 59.1% in lean, overweight, and obese groups, the PNPLA3 rs738409 risk genotype (GG) increased NAFLD risk in lean subjects by more than twofold compared with overweight and obese participants [107]. No differences in risk were found for the MBOAT7 or TM6SF2 NAFLD risk alleles after stratifying by BMI. In a study of 187 Austrian participants, Feldman et al. [28] observed a higher rate of PNPLA3 risk alleles in lean individuals with NAFLD compared with the lean control group, with a frequency comparable to NAFLD patients with obesity. In addition, a significantly greater proportion of lean individuals with NAFLD carried the rs58542926 risk allele (4%), relative to non-lean NAFLD patients (0.3%). In Italian patients with lean NAFLD, the only variable associated independently with NASH and a fibrosis score ≥ 2 was the presence of the rs738409 (PNPLA3) risk allele [30]. The rs738409 risk genotype was also associated with NAFLD in lean individuals in a Sri Lankan population [108] and nonobese Japanese subjects [109]. A recent study found the highest NAFLD risk increase among carriers of the rs738409 risk genotype in 529 lean subjects (OR 6.04, 95% CI [2.62, 13.91]), compared with 162 and 213 individuals with overweight (OR 3.43, 95% CI [1.06, 11.14]) and obesity (OR 2.51, 95% CI [0.93, 6.78]), respectively [110]. Other groups have not found evidence for statistically significant differences for NAFLD risk alleles in PNPLA3 and TM6SF2 between weight groups [31, 111].
A risk genotype (AA) at the V175M variant (rs7946) in PEMT, which results in a partial loss of PEMT activity, was 1.7-fold higher in individuals with NAFLD compared to normal controls [112]. Additional PEMT variants (rs12325817, rs4646343, and rs3761088) were associated with developing liver dysfunction in response to a choline-depleted diet [88]. Two other PEMT variants, rs1531100 and rs4646365, increased liver damage risk in postmenopausal women [88]. Variants in genes from the choline biosynthesis pathway, namely choline kinase A, moderated the effects of a low choline diet [88], while a genetic signature comprised of variants in the choline and 1-carbon metabolism pathways were associated with severity of hepatic steatosis [113]. Using an unbiased exome sequencing approach in a discovery set of two lean NAFLD patients and six lean controls, only rs7946 (PEMT) and rs2290532 in oxysterol-binding protein-related protein 10 (OSBPL10) were found to be associated with NAFLD [114]. Genotyping in a validation cohort of 191 lean individuals with NAFLD and 105 lean controls revealed a threefold higher risk of NAFLD in carriers of the rs7946 risk genotype, but no significant differences were found for the OSBPL10 variant.
Lipodystrophies are a group of heterogeneous rare genetic disorders characterized by the common phenotype of deficient adipose tissue without nutritional deprivation or increased metabolism [115]. The inability to store lipids as fat leads to several adverse complications including NAFLD and liver fibrosis, which can lead to cirrhosis. Pathogenic variants in several genes can cause familial partial lipodystrophies including peroxisome proliferator-activated receptor gamma (PPARG), lamin A/C (LMNA), perilipin 1 (PLIN1), hormone-sensitive lipase (LIPE), cell death-inducing DFFA-like effector C (CIDEC), and Akt murine thymoma viral oncogene homolog 2 (AKT2) [116]. Hepatic steatosis is an almost universal finding in these individuals, suggesting that NAFLD in lean individuals may be a type of ectopic fat deposition similar to lipodystrophy. Genetic evidence supports such a mechanism. A polygenic risk score associated with insulin resistance and decreased adiposity in the lower extremities, both of which are features of lipodystrophy, has been reported [117]. Subsequently, Chen et al. [118] determined that the lipodystrophy polygenic risk score was associated with NAFLD, increased liver fibrosis, and decreased lower extremity fat mass.
Other factors
NAFLD can develop against the backdrop of endocrine disturbances, often by exacerbating hormone-related metabolic alterations. For example, women are at high risk of developing NAFLD and NASH following the menopausal transition [119], likely due to the loss of protection conferred by estrogens, in combination with sub-clinical disturbances in metabolic parameters prior to menopause, such as mild to moderate levels of adiposity, dyslipidemia, and impaired glucose tolerance. Hyperandrogenism is also associated with hepatic steatosis and fibrosis in women, independent of insulin resistance and adiposity [120, 121], although increased circulating testosterone levels in middle-aged women are associated with higher visceral adiposity [122]. Hyperthyroidism-induced NAFLD is regarded as a distinct disease entity [123] and thyroid hormone supplementation improves liver dysfunction [124]. To date, no studies have specifically focused on the role of endocrine factors in NAFLD risk in lean individuals, although many changes in hormonal levels are accompanied by increasing visceral adiposity, which yields ramifications for NAFLD susceptibility, even in lean individuals.
There is some evidence suggesting that high dietary fat or fructose intake in animals can synergistically enhance the effects of estrogen deficiency, leading to exaggerated effects on hepatocellular injury [125, 126]. Similarly, interactions between choline deficiency and hormonal status may modulate NAFLD risk. For example, postmenopausal women had significantly worse fibrosis compared to premenopausal women, although both groups had similarly low levels of choline intake [75]. As noted above, reduced endogenous production of estrogen results in diminished PEMT expression, which may lead a greater susceptibility to the development of NAFLD in postmenopausal women with chronic states of choline deficiency [86, 87].
Other potential etiologies of NAFLD in lean individuals include those related to the gut dysbiosis, parenteral nutrition, undernutrition, and specific steatogenic medications. These have been discussed in detail elsewhere [127–131].
Screening and clinical management of NAFLD in lean individuals: outstanding questions
Despite the prevalence and adverse outcomes associated with NAFLD in normal weight individuals, there are no global consensus guidelines for NAFLD screening, nor is screening in the general population recommended by any professional societies. As shown in Table 3, practice guidance statements developed by the American Association for the Study of Liver Diseases (AASLD), and intended for use by physicians and other health professionals [89], do not recommend routine screening for NAFLD in high-risk groups (i.e., T2D or obesity) due to the uncertain evidence supporting diagnostic tests, treatment options, and the long-term benefits or cost-effectiveness of screening. Some specialists in the United States recommend screening individuals at risk of developing liver disease, such as those older than 50 years and with T2D or metabolic syndrome, using liver function tests and abdominal ultrasound in a primary care setting and imaging or prediction algorithms to assess the presence of fibrosis and subsequent diagnosis of NASH and staging of fibrosis [132].
Table 3.
Summary of AASLD practice guidelines for the screening, evaluation, and treatment of NAFLD [89]
| Screening | Routine Screening for NAFLD in high-risk groups attending primary care, diabetes, or obesity clinics is not advised because of uncertainties surrounding diagnostic tests and treatment options, along with lack of knowledge related to long-term benefits and cost-effectiveness of screening |
| There should be a high index of suspicion for NAFLD and NASH in patients with type 2 diabetes | |
| Systematic screening of family members for NAFLD is not recommended | |
| Evaluation | Patients with unsuspected hepatic steatosis detected on imaging who have symptoms or signs attributable to liver disease or have abnormal liver chemistries should be evaluated as though they have suspected NAFLD and worked up accordingly |
| Patients with incidental hepatic steatosis detected on imaging who lack any liver-related symptoms or signs and have normal liver biochemistries should be assessed for metabolic risk factors (e.g., obesity, diabetes mellitus, or dyslipidemia) and alternate causes for hepatic steatosis, such as significant alcohol consumption or medications | |
| When evaluating a patient with suspected NAFLD, it is essential to exclude competing etiologies for steatosis and coexisting common chronic liver disease | |
| In patients with suspected NAFLD, persistently high serum ferritin, and increased iron saturation, especially in the context of homozygote or heterozygote C282Y HFE mutation, a liver biopsy should be considered | |
| High serum titers of autoantibodies in association with other features suggestive of autoimmune liver disease (> 5 upper limit of normal aminotransferases, high globulins, or high total protein to albumin ratio) should prompt a work-up for autoimmune liver disease | |
| Initial evaluation of patients with suspected NAFLD should carefully consider the presence of commonly associated comorbidities such as obesity, dyslipidemia, insulin resistance or diabetes, hypothyroidism, polycystic ovary syndrome, and sleep apnea | |
| Treatment | Weight loss generally reduces hepatic steatosis, achieved either by hypocaloric diet alone or in conjunction with increased physical activity. A combination of a hypocaloric diet (daily reduction by 500–1000 kcal) and moderate-intensity exercise is likely to provide the best likelihood of sustaining weight loss over time |
| Weight loss of at least 3–5% of body weight appears necessary to improve steatosis, but a greater weight loss (7–10%) is needed to improve the majority of the histopathological features of NASH, including fibrosis | |
| Pharmacological treatments, such as pioglitazone and Vitamin E, aimed primarily at improving liver disease should generally be limited to those with biopsy-proven NASH and fibrosis. Bariatric surgery can be considered in otherwise eligible obese individuals with NAFLD or NASH |
A review of current international guidelines has recently been published [133]. In contrast to the AASLD, European and Asian guidelines recommend that screening be considered for groups considered at risk for developing NAFLD, including patients with obesity and T2D [3, 90, 91]. With respect to lean individuals, guidelines for NAFLD screening become less clear. Many guidelines acknowledge the importance of NAFLD in lean individuals, especially those of Asian ancestry or who exhibit features of metabolic syndrome [3, 90, 134]. The development and distribution of consistent screening and risk assessment guidelines will be critical to ensure optimal clinical management for all NAFLD patients [133]. Knowledge of disease etiology, screening, detection methods, and consensus guidelines are becoming increasingly important for adequate clinical care of both lean and obese NAFLD patients, especially for primary care physicians, who are the providers in the best position to make an initial diagnosis.
Most of the guidelines do not directly address screening and treatment of NAFLD in lean individuals. There are thus many questions that arise when considering the screening and clinical management of NAFLD in this patient population. For example, is visceral adiposity, rather than the overall amount of body fat, more relevant for NAFLD pathogenesis in lean individuals than it is in those with higher BMI? If so, are there better alternatives to the use of BMI as a marker for adiposity for NAFLD screening? Some investigators have argued that waist circumference is a more accurate representation of body fat distribution and a better method with which to identify individuals at higher risk of developing cardiometabolic disease [135]. However, despite the relative simplicity and low financial cost, implementation of waist circumference measurements as a standard measure of adiposity in primary care faces systemic obstacles, and in many settings, would require problematic process reconfiguration. However, obtaining waist circumference measurements may be clinically significant for lean individuals, who, despite having a normal BMI, may have some degree of visceral adiposity and consequently, an increased risk for NAFLD.
A major question is whether NAFLD in lean individuals represents a distinct clinicopathological entity requiring specific management, as suggested by many researchers [16, 27, 31, 32, 36, 136], or is it a sub-phenotype of classical obesity-associated NAFLD that will respond to the current approach of weight loss and control of insulin resistance, hypertension, and hyperlipidemia [17]? Certainly, many of the same factors that increase susceptibility to NAFLD are shared between normal weight and overweight individuals. Further, even among normal weight individuals, those with NAFLD appear to have slightly worse metabolic features. For example, Kim et al. [14] observed significant differences in sex, waist circumference, triglyceride level, and logarithm HOMA-IR between normal weight subjects with and without NAFLD. These differences in clinical and laboratory measures between normal weight individuals with or without NAFLD were comparable to those observed between overweight individuals with or without NAFLD, suggesting that in this cohort, NAFLD in lean individuals is a clinical entity similar to obesity-related NAFLD [14]. However, the risk of insulin resistance, hypertriglyceridemia, hyperuricemia, and central obesity in NAFLD patients compared with those without NAFLD was higher in lean individuals than those with overweight.
Lean individuals with NAFLD have also been found to respond to diet and lifestyle modifications typically utilized in the treatment of obesity-related NAFLD. In one study, loss of only 5% of initial body weight was demonstrated to result in remission of NAFLD in 75% of individuals [137]. Likewise, a 5% reduction in weight in 35 NAFLD patients (14 lean and 21 with obesity) yielded significant improvements in ALT and AST levels, hepatic steatosis, and liver stiffness [138]. In this intervention, NAFLD was resolved in 57.1% of lean individuals [138]. Combined, these data suggest that lifestyle modifications and weight loss are appropriate to reduce NAFLD, at least in some lean individuals. More research to determine whether reductions in central obesity, through a nutritional regimen and exercise, are appropriate therapeutic approaches in lean individuals with NAFLD.
It will also be important to determine whether therapeutics under investigation for classical obesity-related NAFLD will also be effective in lean NAFLD patients. Clinical trials addressing the potential effectiveness of drugs such as SGLT2 (sodium–glucose transport protein 2) inhibitors, GLP-1 (glucagon-like peptide 1) receptor agonists, obeticholic acid, pioglitazone, or saroglitazar in lean individuals with NAFLD are urgently needed [139].
Despite the similarities in NAFLD across the BMI spectrum, there may be cases in which NAFLD in lean individuals represents a distinct disease entity, and here, interventions that specifically address the pathophysiological triggers must be developed and tested. In these cases, the etiology and pathogenesis of NAFLD may inform the most appropriate treatment strategy. More studies to identify potential genetic factors that specifically contribute to NAFLD without obesity (or are masked by the presence of obesity) and uncover interactions with lifestyle factors that modulate their impact would provide a deeper understanding of disease risk in lean individuals. The role of various dietary factors or specific macronutrient composition as significant contributors to NAFLD risk in lean individuals remains largely unexplored. Many research studies have consistently demonstrated a link between liver dysfunction and choline deficiency, which has the unusual phenotype of resistance to diet-induced obesity, but are there other micronutrients that contribute to NAFLD, and if so, do they interact with functional genetic variants, as observed between choline and PEMT SNVs? Finally, there may be additional, as-yet unknown environmental factors, including herbal supplements, that contribute to the development of NAFLD in lean individuals.
Recent efforts to apply data-driven cluster analysis identified five distinct subtypes of diabetes, showing distinct patient characteristics and differential risk for diabetic complications [140]. This level of stratification of patients with a notably heterogeneous disease may lead to more focused treatment strategies instead of a one-size-fits-all approach, which represents the current state of diabetes care. We envision the application of similar cluster analysis to identify a spectrum of individuals from those who may have relatively mild NAFLD with little chance of progression to those who are on a rapid trajectory to advanced disease with severe complications. Such stratification may also lead to specific treatment strategies.
Going forward it will be important to assess the variance in NAFLD prevalence in lean populations, according to different ancestries, ethnicities, and geographies, and determine risk factors that may be more important for some groups than for others. Knowledge of the long-term consequences of NAFLD in the lean and the rate and severity of progression to NASH compared to classical obesity-associated NAFLD will also be important for the development of precise treatment strategies.
Conclusions
It is not uncommon for lean individuals to develop NAFLD and NASH, despite a healthier metabolic phenotype than that observed in classical obesity-related NAFLD. We posit that NAFLD develops in lean individuals due to a distinct array of contributing etiologies, including dietary composition, genetic susceptibility, and hormonal status. In the absence of suspicious laboratory findings, lean individuals are not likely to be screened for NAFLD, nor for metabolic diseases associated with NAFLD. Awareness of menopausal status, genetic factors, ethnicity, dietary factors (especially added sugar, refined carbohydrates, and saturated fat/cholesterol), choline deficiency, and alcohol consumption patterns may be of value in assessing NAFLD risk in lean individuals.
Much more work is needed not only to address the questions raised above, but also to promote greater awareness among practitioners about the potential health risks associated with NAFLD in lean individuals. Efforts aimed at the development of screening algorithms that are less dependent on BMI and hepatic transaminase levels, implementation of more precise treatment strategies based on underlying pathoetiology, and inclusion of lean individuals in NAFLD-related clinical trials are necessary to reduce the burden of NAFLD in this patient group. Further, additional studies to characterize the lean NAFLD population and identify factors that modulate NAFLD risk in the absence of clinically significant metabolic dysfunction are urgently needed. Finally, recognition that NAFLD in some lean individuals may resemble classical obesity-related NAFLD, while in others, it may represent a distinct clinical entity, provides a foundation by which different strategies for clinical management can be devised. Early detection, combined with the appropriate steps to mitigate NAFLD through lifestyle modifications and clinical interventions, may effectively prevent the progression to NASH in lean individuals.
Acknowledgements
Not applicable.
Abbreviations
- NAFLD
Nonalcoholic fatty liver disease
- BMI
Body mass index
- NASH
Nonalcoholic steatohepatitis
- CI
Confidence interval
- HDL-C
High-density lipoprotein-cholesterol
- HOMA-IR
Homeostatic Model Assessment for Insulin Resistance
- NHANES III
National Health and Nutrition Examination Survey III
- LDL-C
Low-density lipoprotein-cholesterol
- HCC
Hepatocellular carcinoma
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- GGT
Gamma-glutamyl transferase
- AI
Adequate Intake
- PEMT
Phosphatidylethanolamine N-methyltransferase
- VLDL
Very low-density lipoprotein-cholesterol
- SNV
Single nucleotide variant
- PNPLA3
Patatin-like phospholipase domain-containing protein 3 gene
- MBOAT7
Membrane-bound O-acyltransferase domain-containing 7
- TM6SF2
Trans-membrane 6 superfamily antigen 2
- OR
Odds ratio
- AASLD
Association for the Study of Liver Diseases
- SGLT2
Sodium–glucose transport protein 2
- GLP-1
Glucagon-like peptide 1
Authors’ contributions
JKD conceived the paper, JKD and GSG contributed to the writing and editing of the manuscript. Both authors read and approved the final manuscript.
Funding
This study was supported by the National Institutes of Health (R01 DK107735, R01 DK120890).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Johanna K. DiStefano, Email: jdistefano@tgen.org
Glenn S. Gerhard, Email: gsgerhard@temple.edu
References
- 1.Vos MB, Abrams SH, Barlow SE, Caprio S, Daniels SR, Kohli R, et al. NASPGHAN clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children: recommendations from the expert committee on NAFLD (ECON) and the North American society of pediatric gastroenterology, hepatology and nutrition (NASPGHAN) J Pediatr Gastroenterol Nutr. 2017;64(2):319–334. doi: 10.1097/MPG.0000000000001482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55(7):434–438. [PubMed] [Google Scholar]
- 3.European Association for the Study of the L, European Association for the Study of D, European Association for the Study of O. EASL–EASD–EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–402. [DOI] [PubMed]
- 4.Younossi ZM, Blissett D, Blissett R, Henry L, Stepanova M, Younossi Y, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577–1586. doi: 10.1002/hep.28785. [DOI] [PubMed] [Google Scholar]
- 5.Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 6.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 7.Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123–133. doi: 10.1002/hep.29466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141(4):1249–1253. doi: 10.1053/j.gastro.2011.06.061. [DOI] [PubMed] [Google Scholar]
- 9.Fabbrini E, Sullivan S, Klein S. Obesity and nonalcoholic fatty liver disease: biochemical, metabolic, and clinical implications. Hepatology. 2010;51(2):679–689. doi: 10.1002/hep.23280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yilmaz Y, Younossi ZM. Obesity-associated nonalcoholic fatty liver disease. Clin Liver Dis. 2014;18(1):19–31. doi: 10.1016/j.cld.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Fan R, Wang J, Du J. Association between body mass index and fatty liver risk: a dose-response analysis. Sci Rep. 2018;8(1):15273. doi: 10.1038/s41598-018-33419-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bellentani S, Saccoccio G, Masutti F, Croce LS, Brandi G, Sasso F, et al. Prevalence of and risk factors for hepatic steatosis in northern Italy. Ann Intern Med. 2000;132(2):112–117. doi: 10.7326/0003-4819-132-2-200001180-00004. [DOI] [PubMed] [Google Scholar]
- 13.Chen CH, Huang MH, Yang JC, Nien CK, Yang CC, Yeh YH, et al. Prevalence and risk factors of nonalcoholic fatty liver disease in an adult population of Taiwan: metabolic significance of nonalcoholic fatty liver disease in nonobese adults. J Clin Gastroenterol. 2006;40(8):745–752. doi: 10.1097/00004836-200609000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Kim HJ, Kim HJ, Lee KE, Kim DJ, Kim SK, Ahn CW, et al. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Intern Med. 2004;164(19):2169–2175. doi: 10.1001/archinte.164.19.2169. [DOI] [PubMed] [Google Scholar]
- 15.Singh SP, Nayak S, Swain M, Rout N, Mallik RN, Agrawal O, et al. Prevalence of nonalcoholic fatty liver disease in coastal eastern India: a preliminary ultrasonographic survey. Trop Gastroenterol. 2004;25(2):76–79. [PubMed] [Google Scholar]
- 16.Vos B, Moreno C, Nagy N, Fery F, Cnop M, Vereerstraeten P, et al. Lean non-alcoholic fatty liver disease (Lean-NAFLD): a major cause of cryptogenic liver disease. Acta Gastroenterol Belg. 2011;74(3):389–394. [PubMed] [Google Scholar]
- 17.Albhaisi S, Chowdhury A, Sanyal AJ. Non-alcoholic fatty liver disease in lean individuals. JHEP Rep. 2019;1(4):329–341. doi: 10.1016/j.jhepr.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Consultation WE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 19.Petersen KF, Dufour S, Feng J, Befroy D, Dziura J, Dalla Man C, et al. Increased prevalence of insulin resistance and nonalcoholic fatty liver disease in Asian-Indian men. Proc Natl Acad Sci USA. 2006;103(48):18273–18277. doi: 10.1073/pnas.0608537103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ye Q, Zou B, Yeo YH, Li J, Huang DQ, Wu Y, et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(8):739–752. doi: 10.1016/S2468-1253(20)30077-7. [DOI] [PubMed] [Google Scholar]
- 21.Shi Y, Wang Q, Sun Y, Zhao X, Kong Y, Ou X, et al. The prevalence of lean/nonobese nonalcoholic fatty liver disease: a systematic review and meta-analysis. J Clin Gastroenterol. 2020;54(4):378–387. doi: 10.1097/MCG.0000000000001270. [DOI] [PubMed] [Google Scholar]
- 22.Younossi ZM, Yilmaz Y, Yu ML, Wai-Sun Wong V, Fernandez MC, Isakov VA, et al. Clinical and patient-reported outcomes from patients with nonalcoholic fatty liver disease across the world: data from the global non-alcoholic steatohepatitis (NASH)/non-alcoholic fatty liver disease (NAFLD) registry. Clin Gastroenterol Hepatol. 2021 doi: 10.1016/j.cgh.2021.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Ge X, Zheng L, Wang M, Du Y, Jiang J. Prevalence trends in non-alcoholic fatty liver disease at the global, regional and national levels, 1990–2017: a population-based observational study. BMJ Open. 2020;10(8):e036663. doi: 10.1136/bmjopen-2019-036663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wei JL, Leung JC, Loong TC, Wong GL, Yeung DK, Chan RS, et al. Prevalence and severity of nonalcoholic fatty liver disease in non-obese patients: a population study using proton-magnetic resonance spectroscopy. Am J Gastroenterol. 2015;110(9):1306–1314. doi: 10.1038/ajg.2015.235. [DOI] [PubMed] [Google Scholar]
- 25.Nishioji K, Sumida Y, Kamaguchi M, Mochizuki N, Kobayashi M, Nishimura T, et al. Prevalence of and risk factors for non-alcoholic fatty liver disease in a non-obese Japanese population, 2011–2012. J Gastroenterol. 2015;50(1):95–108. doi: 10.1007/s00535-014-0948-9. [DOI] [PubMed] [Google Scholar]
- 26.Younossi ZM, Stepanova M, Negro F, Hallaji S, Younossi Y, Lam B, et al. Nonalcoholic fatty liver disease in lean individuals in the United States. Medicine. 2012;91(6):319–327. doi: 10.1097/MD.0b013e3182779d49. [DOI] [PubMed] [Google Scholar]
- 27.Ahmed OT, Gidener T, Mara KC, Larson JJ, Therneau TM, Allen AM. Natural history of nonalcoholic fatty liver disease with normal body mass index: a population-based study. Clin Gastroenterol Hepatol. 2021 doi: 10.1016/j.cgh.2021.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feldman A, Eder SK, Felder TK, Kedenko L, Paulweber B, Stadlmayr A, et al. Clinical and metabolic characterization of lean caucasian subjects with non-alcoholic fatty liver. Am J Gastroenterol. 2017;112(1):102–110. doi: 10.1038/ajg.2016.318. [DOI] [PubMed] [Google Scholar]
- 29.Margariti A, Deutsch M, Manolakopoulos S, Tiniakos D, Papatheodoridis GV. The severity of histologic liver lesions is independent of body mass index in patients with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2013;47(3):280–286. doi: 10.1097/MCG.0b013e31826be328. [DOI] [PubMed] [Google Scholar]
- 30.Fracanzani AL, Petta S, Lombardi R, Pisano G, Russello M, Consonni D, et al. Liver and cardiovascular damage in patients with lean nonalcoholic fatty liver disease, and association with visceral obesity. Clin Gastroenterol Hepatol. 2017;15(10):1604–1611. doi: 10.1016/j.cgh.2017.04.045. [DOI] [PubMed] [Google Scholar]
- 31.Denkmayr L, Feldman A, Stechemesser L, Eder SK, Zandanell S, Schranz M, et al. Lean patients with non-alcoholic fatty liver disease have a severe histological phenotype similar to obese patients. J Clin Med. 2018;7(12):562. doi: 10.3390/jcm7120562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feldman A, Wernly B, Strebinger G, Eder SK, Zandanell S, Niederseer D, et al. Liver-related mortality is increased in lean subjects with non-alcoholic fatty liver disease compared to overweight and obese subjects. J Gastrointest Liver Dis. 2021;30(3):366–373. doi: 10.15403/jgld-3622. [DOI] [PubMed] [Google Scholar]
- 33.Younes R, Govaere O, Petta S, Miele L, Tiniakos D, Burt A, et al. Caucasian lean subjects with non-alcoholic fatty liver disease share long-term prognosis of non-lean: time for reappraisal of BMI-driven approach? Gut. 2021;71(2):382–390. doi: 10.1136/gutjnl-2020-322564. [DOI] [PubMed] [Google Scholar]
- 34.Sookoian S, Pirola CJ. Systematic review with meta-analysis: the significance of histological disease severity in lean patients with nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2018;47(1):16–25. doi: 10.1111/apt.14401. [DOI] [PubMed] [Google Scholar]
- 35.Alam S, Eslam M, Skm Hasan N, Anam K, Chowdhury MAB, Khan MAS, et al. Risk factors of nonalcoholic fatty liver disease in lean body mass population: a systematic review and meta-analysis. JGH Open. 2021;5(11):1236–1249. doi: 10.1002/jgh3.12658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hagstrom H, Nasr P, Ekstedt M, Hammar U, Stal P, Hultcrantz R, et al. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: a long-term follow-up study. Hepatol Commun. 2018;2(1):48–57. doi: 10.1002/hep4.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Golabi P, Paik J, Fukui N, Locklear CT, de Avilla L, Younossi ZM. Patients with lean nonalcoholic fatty liver disease are metabolically abnormal and have a higher risk for mortality. Clin Diabetes. 2019;37(1):65–72. doi: 10.2337/cd18-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zou B, Yeo YH, Nguyen VH, Cheung R, Ingelsson E, Nguyen MH. Prevalence, characteristics and mortality outcomes of obese, nonobese and lean NAFLD in the United States, 1999–2016. J Intern Med. 2020;288(1):139–151. doi: 10.1111/joim.13069. [DOI] [PubMed] [Google Scholar]
- 39.Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, Webb M, Blendis L, Halpern Z, et al. Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): a population based study. J Hepatol. 2007;47(5):711–717. doi: 10.1016/j.jhep.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 40.Cortez-Pinto H, Jesus L, Barros H, Lopes C, Moura MC, Camilo ME. How different is the dietary pattern in non-alcoholic steatohepatitis patients? Clin Nutr. 2006;25(5):816–823. doi: 10.1016/j.clnu.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 41.Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, et al. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology. 2003;37(4):909–916. doi: 10.1053/jhep.2003.50132. [DOI] [PubMed] [Google Scholar]
- 42.Agius L. High-carbohydrate diets induce hepatic insulin resistance to protect the liver from substrate overload. Biochem Pharmacol. 2013;85(3):306–312. doi: 10.1016/j.bcp.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 43.Colak Y, Tuncer I, Senates E, Ozturk O, Doganay L, Yilmaz Y. Nonalcoholic fatty liver disease: a nutritional approach. Metab Syndr Relat Disord. 2012;10(3):161–166. doi: 10.1089/met.2011.0145. [DOI] [PubMed] [Google Scholar]
- 44.Parry SA, Hodson L. Influence of dietary macronutrients on liver fat accumulation and metabolism. J Investig Med. 2017;65(8):1102–1115. doi: 10.1136/jim-2017-000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DiStefano JK. Fructose-mediated effects on gene expression and epigenetic mechanisms associated with NAFLD pathogenesis. Cell Mol Life Sci. 2020;77(11):2079–2090. doi: 10.1007/s00018-019-03390-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ouyang X, Cirillo P, Sautin Y, McCall S, Bruchette JL, Diehl AM, et al. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J Hepatol. 2008;48(6):993–999. doi: 10.1016/j.jhep.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Assy N, Nasser G, Kamayse I, Nseir W, Beniashvili Z, Djibre A, et al. Soft drink consumption linked with fatty liver in the absence of traditional risk factors. Can J Gastroenterol. 2008;22(10):811–816. doi: 10.1155/2008/810961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DiStefano JK, Shaibi GQ. The relationship between excessive dietary fructose consumption and paediatric fatty liver disease. Pediatr Obes. 2020;16:e12759. doi: 10.1111/ijpo.12759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abid A, Taha O, Nseir W, Farah R, Grosovski M, Assy N. Soft drink consumption is associated with fatty liver disease independent of metabolic syndrome. J Hepatol. 2009;51(5):918–924. doi: 10.1016/j.jhep.2009.05.033. [DOI] [PubMed] [Google Scholar]
- 50.Jones RB, Alderete TL, Kim JS, Millstein J, Gilliland FD, Goran MI. High intake of dietary fructose in overweight/obese teenagers associated with depletion of Eubacterium and Streptococcus in gut microbiome. Gut Microbes. 2019;10(6):712–719. doi: 10.1080/19490976.2019.1592420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vos MB, Lavine JE. Dietary fructose in nonalcoholic fatty liver disease. Hepatology. 2013;57(6):2525–2531. doi: 10.1002/hep.26299. [DOI] [PubMed] [Google Scholar]
- 52.Softic S, Stanhope KL, Boucher J, Divanovic S, Lanaspa MA, Johnson RJ, et al. Fructose and hepatic insulin resistance. Crit Rev Clin Lab Sci. 2020;57(5):308–322. doi: 10.1080/10408363.2019.1711360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Russo E, Leoncini G, Esposito P, Garibotto G, Pontremoli R, Viazzi F. Fructose and uric acid: major mediators of cardiovascular disease risk starting at pediatric age. Int J Mol Sci. 2020;21(12):4479. doi: 10.3390/ijms21124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Parks EJ, Skokan LE, Timlin MT, Dingfelder CS. Dietary sugars stimulate fatty acid synthesis in adults. J Nutr. 2008;138(6):1039–1046. doi: 10.1093/jn/138.6.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chong MF, Fielding BA, Frayn KN. Mechanisms for the acute effect of fructose on postprandial lipemia. Am J Clin Nutr. 2007;85(6):1511–1520. doi: 10.1093/ajcn/85.6.1511. [DOI] [PubMed] [Google Scholar]
- 56.Alwahsh SM, Gebhardt R. Dietary fructose as a risk factor for non-alcoholic fatty liver disease (NAFLD) Arch Toxicol. 2017;91(4):1545–1563. doi: 10.1007/s00204-016-1892-7. [DOI] [PubMed] [Google Scholar]
- 57.Basaranoglu M, Basaranoglu G, Sabuncu T, Senturk H. Fructose as a key player in the development of fatty liver disease. World J Gastroenterol. 2013;19(8):1166–1172. doi: 10.3748/wjg.v19.i8.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.DiNicolantonio JJ, Subramonian AM, O'Keefe JH. Added fructose as a principal driver of non-alcoholic fatty liver disease: a public health crisis. Open Heart. 2017;4(2):e000631. doi: 10.1136/openhrt-2017-000631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jegatheesan P, De Bandt JP. Fructose and NAFLD: the multifaceted aspects of fructose metabolism. Nutrients. 2017;9(3):230. [Google Scholar]
- 60.Jensen T, Abdelmalek MF, Sullivan S, Nadeau KJ, Green M, Roncal C, et al. Fructose and sugar: a major mediator of non-alcoholic fatty liver disease. J Hepatol. 2018;68(5):1063–1075. doi: 10.1016/j.jhep.2018.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lim JS, Mietus-Snyder M, Valente A, Schwarz JM, Lustig RH. The role of fructose in the pathogenesis of NAFLD and the metabolic syndrome. Nat Rev Gastroenterol Hepatol. 2010;7(5):251–264. doi: 10.1038/nrgastro.2010.41. [DOI] [PubMed] [Google Scholar]
- 62.Ter Horst KW, Serlie MJ. Fructose consumption, lipogenesis, and non-alcoholic fatty liver disease. Nutrients. 2017;9(9):981. doi: 10.3390/nu9090981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wiernsperger N, Geloen A, Rapin JR. Fructose and cardiometabolic disorders: the controversy will, and must, continue. Clinics. 2010;65(7):729–738. doi: 10.1590/S1807-59322010000700013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abdelmalek MF, Suzuki A, Guy C, Unalp-Arida A, Colvin R, Johnson RJ, et al. Increased fructose consumption is associated with fibrosis severity in patients with nonalcoholic fatty liver disease. Hepatology. 2010;51(6):1961–1971. doi: 10.1002/hep.23535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mosca A, Nobili V, De Vito R, Crudele A, Scorletti E, Villani A, et al. Serum uric acid concentrations and fructose consumption are independently associated with NASH in children and adolescents. J Hepatol. 2017;66(5):1031–1036. doi: 10.1016/j.jhep.2016.12.025. [DOI] [PubMed] [Google Scholar]
- 66.Goss AM, Dowla S, Pendergrass M, Ashraf A, Bolding M, Morrison S, et al. Effects of a carbohydrate-restricted diet on hepatic lipid content in adolescents with non-alcoholic fatty liver disease: a pilot, randomized trial. Pediatr Obes. 2020;15(7):e12630. doi: 10.1111/ijpo.12630. [DOI] [PubMed] [Google Scholar]
- 67.Schwimmer JB, Ugalde-Nicalo P, Welsh JA, Angeles JE, Cordero M, Harlow KE, et al. Effect of a low free sugar diet vs usual diet on nonalcoholic fatty liver disease in adolescent boys: a randomized clinical trial. JAMA. 2019;321(3):256–265. doi: 10.1001/jama.2018.20579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schwarz JM, Noworolski SM, Erkin-Cakmak A, Korn NJ, Wen MJ, Tai VW, et al. Effects of dietary fructose restriction on liver fat, de novo lipogenesis, and insulin kinetics in children with obesity. Gastroenterology. 2017;153(3):743–752. doi: 10.1053/j.gastro.2017.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mager DR, Iniguez IR, Gilmour S, Yap J. The effect of a low fructose and low glycemic index/load (FRAGILE) dietary intervention on indices of liver function, cardiometabolic risk factors, and body composition in children and adolescents with nonalcoholic fatty liver disease (NAFLD) JPEN J Parenter Enteral Nutr. 2015;39(1):73–84. doi: 10.1177/0148607113501201. [DOI] [PubMed] [Google Scholar]
- 70.Zeisel SH, da Costa KA. Choline: an essential nutrient for public health. Nutr Rev. 2009;67(11):615–623. doi: 10.1111/j.1753-4887.2009.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zeisel SH, Da Costa KA, Franklin PD, Alexander EA, Lamont JT, Sheard NF, et al. Choline, an essential nutrient for humans. FASEB J. 1991;5(7):2093–2098. [PubMed] [Google Scholar]
- 72.Fischer LM, da Costa KA, Kwock L, Galanko J, Zeisel SH. Dietary choline requirements of women: effects of estrogen and genetic variation. Am J Clin Nutr. 2010;92(5):1113–1119. doi: 10.3945/ajcn.2010.30064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fischer LM, daCosta KA, Kwock L, Stewart PW, Lu TS, Stabler SP, et al. Sex and menopausal status influence human dietary requirements for the nutrient choline. Am J Clin Nutr. 2007;85(5):1275–1285. doi: 10.1093/ajcn/85.5.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kohlmeier M, da Costa KA, Fischer LM, Zeisel SH. Genetic variation of folate-mediated one-carbon transfer pathway predicts susceptibility to choline deficiency in humans. Proc Natl Acad Sci USA. 2005;102(44):16025–16030. doi: 10.1073/pnas.0504285102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Guerrerio AL, Colvin RM, Schwartz AK, Molleston JP, Murray KF, Diehl A, et al. Choline intake in a large cohort of patients with nonalcoholic fatty liver disease. Am J Clin Nutr. 2012;95(4):892–900. doi: 10.3945/ajcn.111.020156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yu D, Shu XO, Xiang YB, Li H, Yang G, Gao YT, et al. Higher dietary choline intake is associated with lower risk of nonalcoholic fatty liver in normal-weight Chinese women. J Nutr. 2014;144(12):2034–2040. doi: 10.3945/jn.114.197533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim S, Fenech MF, Kim PJ. Nutritionally recommended food for semi- to strict vegetarian diets based on large-scale nutrient composition data. Sci Rep. 2018;8(1):4344. doi: 10.1038/s41598-018-22691-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wallace TC, Blusztajn JK, Caudill MA, Klatt KC, Natker E, Zeisel SH, et al. Choline: the underconsumed and underappreciated essential nutrient. Nutr Today. 2018;53(6):240–253. doi: 10.1097/NT.0000000000000302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Noga AA, Zhao Y, Vance DE. An unexpected requirement for phosphatidylethanolamine N-methyltransferase in the secretion of very low density lipoproteins. J Biol Chem. 2002;277(44):42358–42365. doi: 10.1074/jbc.M204542200. [DOI] [PubMed] [Google Scholar]
- 80.Nakatsuka A, Matsuyama M, Yamaguchi S, Katayama A, Eguchi J, Murakami K, et al. Insufficiency of phosphatidylethanolamine N-methyltransferase is risk for lean non-alcoholic steatohepatitis. Sci Rep. 2016;6:21721. doi: 10.1038/srep21721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhu X, Song J, Mar MH, Edwards LJ, Zeisel SH. Phosphatidylethanolamine N-methyltransferase (PEMT) knockout mice have hepatic steatosis and abnormal hepatic choline metabolite concentrations despite ingesting a recommended dietary intake of choline. Biochem J. 2003;370(Pt 3):987–993. doi: 10.1042/BJ20021523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Waite KA, Cabilio NR, Vance DE. Choline deficiency-induced liver damage is reversible in Pemt(−/−) mice. J Nutr. 2002;132(1):68–71. doi: 10.1093/jn/132.1.68. [DOI] [PubMed] [Google Scholar]
- 83.Vance DE. Physiological roles of phosphatidylethanolamine N-methyltransferase. Biochim Biophys Acta. 2013;1831(3):626–632. doi: 10.1016/j.bbalip.2012.07.017. [DOI] [PubMed] [Google Scholar]
- 84.Jacobs RL, Zhao Y, Koonen DP, Sletten T, Su B, Lingrell S, et al. Impaired de novo choline synthesis explains why phosphatidylethanolamine N-methyltransferase-deficient mice are protected from diet-induced obesity. J Biol Chem. 2010;285(29):22403–22413. doi: 10.1074/jbc.M110.108514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wan S, van der Veen JN, Bakala N'Goma JC, Nelson RC, Vance DE, Jacobs RL. Hepatic PEMT activity mediates liver health, weight gain, and insulin resistance. FASEB J. 2019;33(10):10986–10995. doi: 10.1096/fj.201900679R. [DOI] [PubMed] [Google Scholar]
- 86.Resseguie ME, da Costa KA, Galanko JA, Patel M, Davis IJ, Zeisel SH. Aberrant estrogen regulation of PEMT results in choline deficiency-associated liver dysfunction. J Biol Chem. 2011;286(2):1649–1658. doi: 10.1074/jbc.M110.106922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Resseguie M, Song J, Niculescu MD, da Costa KA, Randall TA, Zeisel SH. Phosphatidylethanolamine N-methyltransferase (PEMT) gene expression is induced by estrogen in human and mouse primary hepatocytes. FASEB J. 2007;21(10):2622–2632. doi: 10.1096/fj.07-8227com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.da Costa KA, Corbin KD, Niculescu MD, Galanko JA, Zeisel SH. Identification of new genetic polymorphisms that alter the dietary requirement for choline and vary in their distribution across ethnic and racial groups. FASEB J. 2014;28(7):2970–2978. doi: 10.1096/fj.14-249557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American association for the study of liver diseases. Hepatology. 2018;67(1):328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 90.Wong VW, Chan WK, Chitturi S, Chawla Y, Dan YY, Duseja A, et al. Asia-Pacific working party on non-alcoholic fatty liver disease guidelines 2017—part 1: definition, risk factors and assessment. J Gastroenterol Hepatol. 2018;33(1):70–85. doi: 10.1111/jgh.13857. [DOI] [PubMed] [Google Scholar]
- 91.Chitturi S, Wong VW, Chan WK, Wong GL, Wong SK, Sollano J, et al. The Asia-Pacific working party on non-alcoholic fatty liver disease guidelines 2017—part 2: management and special groups. J Gastroenterol Hepatol. 2018;33(1):86–98. doi: 10.1111/jgh.13856. [DOI] [PubMed] [Google Scholar]
- 92.Decraecker M, Dutartre D, Hiriart JB, Irles-Depe M, Marraud des Grottes H, Chermak F, et al. Long-term prognosis of patients with alcohol-related liver disease or non-alcoholic fatty liver disease according to metabolic syndrome or alcohol use. Liver Int. 2021;42(2):350–362. doi: 10.1111/liv.15081. [DOI] [PubMed] [Google Scholar]
- 93.Chang Y, Cho YK, Kim Y, Sung E, Ahn J, Jung HS, et al. Nonheavy drinking and worsening of noninvasive fibrosis markers in nonalcoholic fatty liver disease: a cohort study. Hepatology. 2019;69(1):64–75. doi: 10.1002/hep.30170. [DOI] [PubMed] [Google Scholar]
- 94.Hajifathalian K, Torabi Sagvand B, McCullough AJ. Effect of alcohol consumption on survival in nonalcoholic fatty liver disease: a national prospective cohort study. Hepatology. 2019;70(2):511–521. doi: 10.1002/hep.30226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Aberg F, Puukka P, Salomaa V, Mannisto S, Lundqvist A, Valsta L, et al. Risks of light and moderate alcohol use in fatty liver disease: follow-up of population cohorts. Hepatology. 2020;71(3):835–848. doi: 10.1002/hep.30864. [DOI] [PubMed] [Google Scholar]
- 96.Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, Castellanos M, Aller-de la Fuente R, Metwally M, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018;155(2):443–457.e17. doi: 10.1053/j.gastro.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 97.Hart CL, Morrison DS, Batty GD, Mitchell RJ, Davey Smith G. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ. 2010;340:c1240. doi: 10.1136/bmj.c1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Loomba R, Yang HI, Su J, Brenner D, Barrett-Connor E, Iloeje U, et al. Synergism between obesity and alcohol in increasing the risk of hepatocellular carcinoma: a prospective cohort study. Am J Epidemiol. 2013;177(4):333–342. doi: 10.1093/aje/kws252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Okamoto M, Miyake T, Kitai K, Furukawa S, Yamamoto S, Senba H, et al. Cigarette smoking is a risk factor for the onset of fatty liver disease in nondrinkers: a longitudinal cohort study. PLoS ONE. 2018;13(4):e0195147. doi: 10.1371/journal.pone.0195147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zein CO, Unalp A, Colvin R, Liu YC, McCullough AJ, Nonalcoholic Steatohepatitis Clinical Research N Smoking and severity of hepatic fibrosis in nonalcoholic fatty liver disease. J Hepatol. 2011;54(4):753–759. doi: 10.1016/j.jhep.2010.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jung HS, Chang Y, Kwon MJ, Sung E, Yun KE, Cho YK, et al. Smoking and the risk of non-alcoholic fatty liver disease: a cohort study. Am J Gastroenterol. 2019;114(3):453–463. doi: 10.1038/s41395-018-0283-5. [DOI] [PubMed] [Google Scholar]
- 102.Bjorkstrom K, Franzen S, Eliasson B, Miftaraj M, Gudbjornsdottir S, Trolle-Lagerros Y, et al. Risk factors for severe liver disease in patients with type 2 diabetes. Clin Gastroenterol Hepatol. 2019;17(13):2769–2775.e4. doi: 10.1016/j.cgh.2019.04.038. [DOI] [PubMed] [Google Scholar]
- 103.Liu P, Xu Y, Tang Y, Du M, Yu X, Sun J, et al. Independent and joint effects of moderate alcohol consumption and smoking on the risks of non-alcoholic fatty liver disease in elderly Chinese men. PLoS ONE. 2017;12(7):e0181497. doi: 10.1371/journal.pone.0181497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Meroni M, Longo M, Tria G, Dongiovanni P. Genetics is of the essence to face NAFLD. Biomedicines. 2021;9(10):1359. doi: 10.3390/biomedicines9101359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40(12):1461–1465. doi: 10.1038/ng.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Martin K, Hatab A, Athwal VS, Jokl E, Piper HK. Genetic contribution to non-alcoholic fatty liver disease and prognostic implications. Curr Diab Rep. 2021;21(3):8. doi: 10.1007/s11892-021-01377-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lin H, Wong GL, Whatling C, Chan AW, Leung HH, Tse CH, et al. Association of genetic variations with NAFLD in lean individuals. Liver Int. 2021;42(1):149–160. doi: 10.1111/liv.15078. [DOI] [PubMed] [Google Scholar]
- 108.Niriella MA, Kasturiratne A, Pathmeswaran A, De Silva ST, Perera KR, Subasinghe S, et al. Lean non-alcoholic fatty liver disease (lean NAFLD): characteristics, metabolic outcomes and risk factors from a 7-year prospective, community cohort study from Sri Lanka. Hepatol Int. 2019;13(3):314–322. doi: 10.1007/s12072-018-9916-4. [DOI] [PubMed] [Google Scholar]
- 109.Honda Y, Yoneda M, Kessoku T, Ogawa Y, Tomeno W, Imajo K, et al. Characteristics of non-obese non-alcoholic fatty liver disease: effect of genetic and environmental factors. Hepatol Res. 2016;46(10):1011–1018. doi: 10.1111/hepr.12648. [DOI] [PubMed] [Google Scholar]
- 110.Lin H, Wong GL, Whatling C, Chan AW, Leung HH, Tse CH, et al. Association of genetic variations with NAFLD in lean individuals. Liver Int. 2022;42(1):149–160. doi: 10.1111/liv.15078. [DOI] [PubMed] [Google Scholar]
- 111.Younes R, Caviglia GP, Govaere O, Rosso C, Armandi A, Sanavia T, et al. Long-term outcomes and predictive ability of non-invasive scoring systems in patients with non-alcoholic fatty liver disease. J Hepatol. 2021;75(4):786–794. doi: 10.1016/j.jhep.2021.05.008. [DOI] [PubMed] [Google Scholar]
- 112.Song J, da Costa KA, Fischer LM, Kohlmeier M, Kwock L, Wang S, et al. Polymorphism of the PEMT gene and susceptibility to nonalcoholic fatty liver disease (NAFLD) FASEB J. 2005;19(10):1266–1271. doi: 10.1096/fj.04-3580com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Corbin KD, Abdelmalek MF, Spencer MD, da Costa KA, Galanko JA, Sha W, et al. Genetic signatures in choline and 1-carbon metabolism are associated with the severity of hepatic steatosis. FASEB J. 2013;27(4):1674–1689. doi: 10.1096/fj.12-219097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bale G, Vishnubhotla RV, Mitnala S, Sharma M, Padaki RN, Pawar SC, et al. Whole-exome sequencing identifies a variant in phosphatidylethanolamine N-methyltransferase gene to be associated with lean-nonalcoholic fatty liver disease. J Clin Exp Hepatol. 2019;9(5):561–568. doi: 10.1016/j.jceh.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Brown RJ, Araujo-Vilar D, Cheung PT, Dunger D, Garg A, Jack M, et al. The diagnosis and management of lipodystrophy syndromes: a multi-society practice guideline. J Clin Endocrinol Metab. 2016;101(12):4500–4511. doi: 10.1210/jc.2016-2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Akinci B, Onay H, Demir T, Savas-Erdeve S, Gen R, Simsir IY, et al. Clinical presentations, metabolic abnormalities and end-organ complications in patients with familial partial lipodystrophy. Metabolism. 2017;72:109–119. doi: 10.1016/j.metabol.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 117.Lotta LA, Gulati P, Day FR, Payne F, Ongen H, van de Bunt M, et al. Integrative genomic analysis implicates limited peripheral adipose storage capacity in the pathogenesis of human insulin resistance. Nat Genet. 2017;49(1):17–26. doi: 10.1038/ng.3714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chen VL, Wright AP, Halligan B, Chen Y, Du X, Handelman SK, et al. Body composition and genetic lipodystrophy risk score associate with nonalcoholic fatty liver disease and liver fibrosis. Hepatol Commun. 2019;3(8):1073–1084. doi: 10.1002/hep4.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.DiStefano JK. NAFLD and NASH in postmenopausal women: implications for diagnosis and treatment. Endocrinology. 2020;161(10):bqaa134. doi: 10.1210/endocr/bqaa134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cai J, Wu CH, Zhang Y, Wang YY, Xu WD, Lin TC, et al. High-free androgen index is associated with increased risk of non-alcoholic fatty liver disease in women with polycystic ovary syndrome, independent of obesity and insulin resistance. Int J Obes. 2017;41(9):1341–1347. doi: 10.1038/ijo.2017.116. [DOI] [PubMed] [Google Scholar]
- 121.Petta S, Ciresi A, Bianco J, Geraci V, Boemi R, Galvano L, et al. Insulin resistance and hyperandrogenism drive steatosis and fibrosis risk in young females with PCOS. PLoS ONE. 2017;12(11):e0186136. doi: 10.1371/journal.pone.0186136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Janssen I, Powell LH, Kazlauskaite R, Dugan SA. Testosterone and visceral fat in midlife women: the study of women’s health across the nation (SWAN) fat patterning study. Obesity. 2010;18(3):604–610. doi: 10.1038/oby.2009.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lonardo A, Ballestri S, Mantovani A, Nascimbeni F, Lugari S, Targher G. Pathogenesis of hypothyroidism-induced NAFLD: evidence for a distinct disease entity? Dig Liver Dis. 2019;51(4):462–470. doi: 10.1016/j.dld.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 124.Okosieme O, Gilbert J, Abraham P, Boelaert K, Dayan C, Gurnell M, et al. Management of primary hypothyroidism: statement by the British thyroid association executive committee. Clin Endocrinol. 2016;84(6):799–808. doi: 10.1111/cen.12824. [DOI] [PubMed] [Google Scholar]
- 125.Riant E, Waget A, Cogo H, Arnal JF, Burcelin R, Gourdy P. Estrogens protect against high-fat diet-induced insulin resistance and glucose intolerance in mice. Endocrinology. 2009;150(5):2109–2117. doi: 10.1210/en.2008-0971. [DOI] [PubMed] [Google Scholar]
- 126.Ohashi K, Munetsuna E, Yamada H, Ando Y, Yamazaki M, Taromaru N, et al. High fructose consumption induces DNA methylation at PPARalpha and CPT1A promoter regions in the rat liver. Biochem Biophys Res Commun. 2015;468(1–2):185–189. doi: 10.1016/j.bbrc.2015.10.134. [DOI] [PubMed] [Google Scholar]
- 127.Allard JP. Other disease associations with non-alcoholic fatty liver disease (NAFLD) Best Pract Res Clin Gastroenterol. 2002;16(5):783–795. doi: 10.1053/bega.2002.0330. [DOI] [PubMed] [Google Scholar]
- 128.Paquot N, Delwaide J. Fatty liver in the intensive care unit. Curr Opin Clin Nutr Metab Care. 2005;8(2):183–187. doi: 10.1097/00075197-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 129.Lee G, You HJ, Bajaj JS, Joo SK, Yu J, Park S, et al. Distinct signatures of gut microbiome and metabolites associated with significant fibrosis in non-obese NAFLD. Nat Commun. 2020;11(1):4982. doi: 10.1038/s41467-020-18754-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gibiino G, Sartini A, Gitto S, Binda C, Sbrancia M, Coluccio C, et al. The other side of malnutrition in inflammatory bowel disease (IBD): non-alcoholic fatty liver disease. Nutrients. 2021;13(8):2772. doi: 10.3390/nu13082772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Satapathy SK, Kuwajima V, Nadelson J, Atiq O, Sanyal AJ. Drug-induced fatty liver disease: an overview of pathogenesis and management. Ann Hepatol. 2015;14(6):789–806. doi: 10.5604/16652681.1171749. [DOI] [PubMed] [Google Scholar]
- 132.Pandyarajan V, Gish RG, Alkhouri N, Noureddin M. Screening for nonalcoholic fatty liver disease in the primary care clinic. Gastroenterol Hepatol. 2019;15(7):357–365. [PMC free article] [PubMed] [Google Scholar]
- 133.Schattenberg JM, Anstee QM, Caussy C, Bugianesi E, Popovic B. Differences between current clinical guidelines for screening, diagnosis and management of nonalcoholic fatty liver disease and real-world practice: a targeted literature review. Expert Rev Gastroenterol Hepatol. 2021;15(11):1253–1266. doi: 10.1080/17474124.2021.1974295. [DOI] [PubMed] [Google Scholar]
- 134.Fan JG, Wei L, Zhuang H, National Workshop on Fatty L. Alcoholic Liver Disease CSoHCMA. Fatty Liver Disease Expert Committee CMDA guidelines of prevention and treatment of nonalcoholic fatty liver disease (2018, China) J Dig Dis. 2019;20(4):163–173. doi: 10.1111/1751-2980.12685. [DOI] [PubMed] [Google Scholar]
- 135.Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Waist circumference and cardiometabolic risk: a consensus statement from shaping America’s health: association for weight management and obesity prevention; NAASO, the obesity society; the American society for nutrition; and the American diabetes association. Diabetes Care. 2007;30(6):1647–1652. doi: 10.2337/dc07-9921. [DOI] [PubMed] [Google Scholar]
- 136.Chen F, Esmaili S, Rogers GB, Bugianesi E, Petta S, Marchesini G, et al. Lean NAFLD: a distinct entity shaped by differential metabolic adaptation. Hepatology. 2020;71(4):1213–1227. doi: 10.1002/hep.30908. [DOI] [PubMed] [Google Scholar]
- 137.Zelber-Sagi S, Lotan R, Shlomai A, Webb M, Harrari G, Buch A, et al. Predictors for incidence and remission of NAFLD in the general population during a seven-year prospective follow-up. J Hepatol. 2012;56(5):1145–1151. doi: 10.1016/j.jhep.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 138.Hamurcu Varol P, Kaya E, Alphan E, Yilmaz Y. Role of intensive dietary and lifestyle interventions in the treatment of lean nonalcoholic fatty liver disease patients. Eur J Gastroenterol Hepatol. 2020;32(10):1352–1357. doi: 10.1097/MEG.0000000000001656. [DOI] [PubMed] [Google Scholar]
- 139.Kuchay MS, Martinez-Montoro JI, Choudhary NS, Fernandez-Garcia JC, Ramos-Molina B. Non-alcoholic fatty liver disease in lean and non-obese individuals: current and future challenges. Biomedicines. 2021;9(10):1346. doi: 10.3390/biomedicines9101346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ahlqvist E, Storm P, Karajamaki A, Martinell M, Dorkhan M, Carlsson A, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018;6(5):361–369. doi: 10.1016/S2213-8587(18)30051-2. [DOI] [PubMed] [Google Scholar]
- 141.Chiloiro M, Caruso MG, Cisternino AM, Inguaggiato R, Reddavide R, Bonfiglio C, et al. Ultrasound evaluation and correlates of fatty liver disease: a population study in a Mediterranean area. Metab Syndr Relat Disord. 2013;11(5):349–358. doi: 10.1089/met.2012.0169. [DOI] [PubMed] [Google Scholar]
- 142.Cruz ACD, Bugianesi E, George J, Day CP, Liaquat H, Charatcharoenwitthaya P, et al. 379 characteristics and long-term prognosis of lean patients with nonalcoholic fatty liver disease. Gastroenterology. 2014;146(5):S-909. [Google Scholar]
- 143.Alferink LJ, Kiefte-de Jong JC, Erler NS, Veldt BJ, Schoufour JD, de Knegt RJ, et al. Association of dietary macronutrient composition and non-alcoholic fatty liver disease in an ageing population: the Rotterdam study. Gut. 2019;68(6):1088–1098. doi: 10.1136/gutjnl-2017-315940. [DOI] [PubMed] [Google Scholar]
- 144.Akyuz U, Yesil A, Yilmaz Y. Characterization of lean patients with nonalcoholic fatty liver disease: potential role of high hemoglobin levels. Scand J Gastroenterol. 2015;50(3):341–346. doi: 10.3109/00365521.2014.983160. [DOI] [PubMed] [Google Scholar]
- 145.Lankarani KB, Ghaffarpasand F, Mahmoodi M, Lotfi M, Zamiri N, Heydari ST, et al. Non alcoholic fatty liver disease in southern Iran: a population based study. Hepat Mon. 2013;13(5):e9248. doi: 10.5812/hepatmon.9248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Das K, Das K, Mukherjee PS, Ghosh A, Ghosh S, Mridha AR, et al. Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology. 2010;51(5):1593–1602. doi: 10.1002/hep.23567. [DOI] [PubMed] [Google Scholar]
- 147.Kumar R, Rastogi A, Sharma MK, Bhatia V, Garg H, Bihari C, et al. Clinicopathological characteristics and metabolic profiles of non-alcoholic fatty liver disease in Indian patients with normal body mass index: do they differ from obese or overweight non-alcoholic fatty liver disease? Indian J Endocrinol Metab. 2013;17(4):665–671. doi: 10.4103/2230-8210.113758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bhat G, Baba CS, Pandey A, Kumari N, Choudhuri G. Insulin resistance and metabolic syndrome in nonobese Indian patients with non-alcoholic fatty liver disease. Trop Gastroenterol. 2013;34(1):18–24. doi: 10.7869/tg.2012.86. [DOI] [PubMed] [Google Scholar]
- 149.Singh SP, Kar SK, Panigrahi MK, Misra B, Pattnaik K, Bhuyan P, et al. Profile of patients with incidentally detected nonalcoholic fatty liver disease (IDNAFLD) in coastal eastern India. Trop Gastroenterol. 2013;34(3):144–152. doi: 10.7869/tg.118. [DOI] [PubMed] [Google Scholar]
- 150.Alam S, Fahim SM, Chowdhury MAB, Hassan MZ, Azam G, Mustafa G, et al. Prevalence and risk factors of non-alcoholic fatty liver disease in Bangladesh. JGH Open. 2018;2(2):39–46. doi: 10.1002/jgh3.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Rahman MM, Kibria MG, Begum H, Haque M, Sultana N, Akhter M, et al. Prevalence, risk factors and metabolic profile of the non-obese and obese non-alcoholic fatty liver disease in a rural community of South Asia. BMJ Open Gastroenterol. 2020;7(1):e000535. doi: 10.1136/bmjgast-2020-000535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Choudhary NS, Saraf N, Saigal S, Duseja A, Gautam D, Rastogi A, et al. Nonalcoholic fatty liver in lean individuals: clinicobiochemical correlates of histopathology in 157 liver biopsies from healthy liver donors. J Clin Exp Hepatol. 2021;11(5):544–549. doi: 10.1016/j.jceh.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Hsiao PJ, Kuo KK, Shin SJ, Yang YH, Lin WY, Yang JF, et al. Significant correlations between severe fatty liver and risk factors for metabolic syndrome. J Gastroenterol Hepatol. 2007;22(12):2118–2123. doi: 10.1111/j.1440-1746.2006.04698.x. [DOI] [PubMed] [Google Scholar]
- 154.Goh SC, Ho EL, Goh KL. Prevalence and risk factors of non-alcoholic fatty liver disease in a multiracial suburban Asian population in Malaysia. Hepatol Int. 2013;7(2):548–554. doi: 10.1007/s12072-012-9359-2. [DOI] [PubMed] [Google Scholar]
- 155.Feng RN, Du SS, Wang C, Li YC, Liu LY, Guo FC, et al. Lean-non-alcoholic fatty liver disease increases risk for metabolic disorders in a normal weight Chinese population. World J Gastroenterol. 2014;20(47):17932–17940. doi: 10.3748/wjg.v20.i47.17932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Fukuda T, Hamaguchi M, Kojima T, Hashimoto Y, Ohbora A, Kato T, et al. The impact of non-alcoholic fatty liver disease on incident type 2 diabetes mellitus in non-overweight individuals. Liver Int. 2016;36(2):275–283. doi: 10.1111/liv.12912. [DOI] [PubMed] [Google Scholar]
- 157.Wang L, Guo J, Lu J. Risk factor compositions of nonalcoholic fatty liver disease change with body mass index in males and females. Oncotarget. 2016;7(24):35632–35642. doi: 10.18632/oncotarget.9691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Yoshitaka H, Hamaguchi M, Kojima T, Fukuda T, Ohbora A, Fukui M. Nonoverweight nonalcoholic fatty liver disease and incident cardiovascular disease: a post hoc analysis of a cohort study. Medicine. 2017;96(18):e6712. doi: 10.1097/MD.0000000000006712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Shao C, Ye J, Li F, Feng S, Wang W, Zhong B. Different predictors of steatosis and fibrosis severity among lean, overweight and obese patients with nonalcoholic fatty liver disease. Dig Liver Dis. 2019;51(10):1392–1399. doi: 10.1016/j.dld.2019.02.019. [DOI] [PubMed] [Google Scholar]
- 160.Wang L. Ultrasound-diagnosed nonalcoholic fatty liver disease independently predicts a higher risk of developing diabetes mellitus in nonoverweight individuals. Acad Radiol. 2019;26(7):863–868. doi: 10.1016/j.acra.2018.08.019. [DOI] [PubMed] [Google Scholar]
- 161.Bernhardt P, Kratzer W, Schmidberger J, Graeter T, Gruener B, Group ES Laboratory parameters in lean NAFLD: comparison of subjects with lean NAFLD with obese subjects without hepatic steatosis. BMC Res Notes. 2018;11(1):101. doi: 10.1186/s13104-018-3212-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Feldman A, Denkmayr L, Strasser M, Ruhaltinger S, Strebinger G, Huber-Schönauer U, et al. Liver-related mortality and morbidity of lean NAFLD is higher compared to overweight and obese NAFLD patients. J Hepatol. 2017;66(1):S149. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


