Abstract
Presently, nanocarriers (NCs) have gained huge attention for their structural ability, good biocompatibility, and biodegradability. The development of effective NCs with stimuli-responsive properties has acquired a huge interest among scientists. When developing drug delivery NCs, the fundamental goal is to tackle the delivery-related problems associated with standard chemotherapy and to carry medicines to the intended sites of action while avoiding undesirable side effects. These nanocarriers were able of delivering drugs to tumors through regulating their pH, temperature, enzyme responsiveness. With the use of nanocarriers, chemotherapeutic drugs could be supplied to tumors more accurately that can equally encapsulate and deliver them. Material carriers for chemotherapeutic medicines are discussed in this review keeping in viewpoint of the structural properties and targeting methods that make these carriers more therapeutically effective, in addition to metabolic pathways triggered by drug-loaded NCs. Largely, the development of NCs countering to endogenous and exogenous stimuli in tumor regions and understanding of mechanisms would encourage the progress for tumor therapy and precision diagnosis in future.
Graphical Abstract
Keywords: Cancer therapy, Smart drug delivery, Functional nanocarriers, Stimulus-responsive drug release
Where are we today with cancer therapeutics?
Cancers are a group of diseases that are caused by the uncontrolled development of malignant cells, which can infiltrate tissues and spread to other regions of the body. According to the World Health Organization, cancer-related fatalities accounted for nearly 10 million deaths in 2020, and the incidence of cancer is expected to increase rapidly to 28.4 million new cases in 2040 [1]. The most common cancer-related death includes breast, lung, colon and rectum, prostate, skin (non-melanoma), and stomach cancers. Fortunately, the death rate has been reduced drastically by advances in our understanding of tumor biology and the development of improved diagnostic equipment and therapies.
Current oncological treatments and new therapies: an overview
Several core strategies exist for treating cancer, including surgical intervention, chemotherapy, and radiation therapy, as well as a combination of these techniques. Conventional chemotherapy works primarily by interfering with the genetic material and cell division of cancer cells; however, this approach is non-selective and damages even the healthy cells, thereby resulting in severe side effects and a high mortality rate. In addition, hydrophobic drugs have poor accessibility that reduces the final drug dosage delivered to the tumor tissues, meaning that higher doses must be administered systematically. However, this can lead to severe toxicity in normal tissues and increase the chances of multiple drug resistance (MDR) where cancer cells can evade chemotherapies by developing resistance against cytotoxic drugs immediately after therapy. Therefore, novel drug delivery systems that can enhance specific targeting and reduce adverse side effects in cancer tissues are urgently required. These shortcomings of conventional chemotherapy have prompted the development of smart monitored nanocarrier (NCs)-based drug delivery systems that allow targeted drug release at specific sites and reduce toxicity [2–5] with enhanced penetration [6].
The correlation between drug delivery and nanoparticles (NPs) was first described by Paul Ehrlich [7] using the magic bullet concept, while Speiser et al. [8] were the first to report the regulated sustained release of drugs using a bead polymerization technique. Also, some engineered bioinspired synthetic and cellular systems towards design of nanomedicine platforms for the treatment of cancer [9]. In recent years, an increasing number of studies have investigated tumor biology and reported the construction of NCs using versatile materials, such as inorganic carriers, lipids [10], proteins [11], and polymeric micelles [12, 13]. This has led to the development of NC-based drug delivery systems that can deliver chemotherapeutics into the tumor microenvironment on demand. Compared to conventional chemotherapeutics, NCs like liposomes, micelles, and nanoparticles have a variety of advantageous features for use in clinical cancer therapy. For instance, NCs can have a high selective accumulation rate in the tumor microenvironment via the enhanced permeability and retention (EPR) effect [14], which improves treatment efficiency by reducing toxicity in normal tissues. Moreover, active targeted delivery can be achieved using NCs loaded with chemotherapeutic agents and conjugated to molecules that bind to receptors that are overexpressed on cancer cells.
In this review, we highlight various NCs-based drug delivery systems and discuss the targeted mechanisms via which they improve the therapeutic index of chemotherapeutic drugs. In addition, we discuss several endogenous and exogenous stimuli-responsive drug release studies in the context of present-day NCs development, in addition, the metabolic pathways and mechanisms induced by drug-loaded NCs.
NCs used for drug delivery in cancer therapy
Several innovative drug delivery strategies are currently being used to treat cancer, and novel cancer therapies have been developed using an array of nanomaterials, including organic and inorganic particles, and synthetically produced lipids, proteins, and polymers. The delivery of drugs encapsulated in NCs offers several advantages over the direct administration of refined chemotherapeutic drugs. These include enhanced drug delivery, protection of the encapsulated drugs against degradation in the bloodstream, targeted drug delivery, efficient treatment with reduced systemic toxicity, improved drug solubility, and enhanced pharmacodynamic and pharmacokinetic drug properties [13, 15–18].
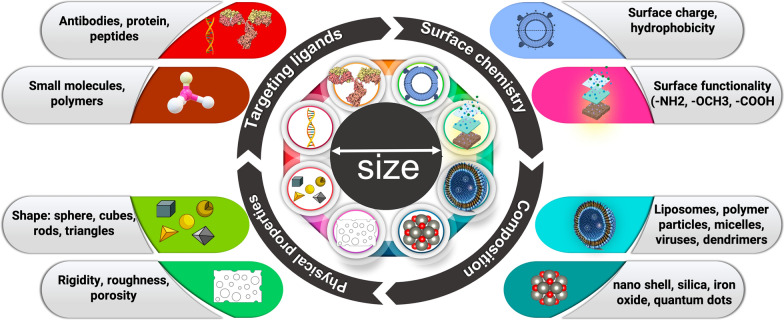
NPs have a small diameter of 1–100 nm and a high surface area to volume ratio, which significantly affects their biological activities and allows them to bind, absorb, and transport drugs, DNA, RNA, proteins, and detection molecules. The therapeutic efficacy of NCs are based on the efficiency of nano-drug delivery used in medical treatments which are controlled predominantly by their size, shape, and surface [19]. To date, a remarkable variety of drug delivery NCs have been developed with different sizes, molecules, conformations, and surface physicochemical characteristics (Fig. 1). It is noteworthy that conventional NCs are unspecific, unstable, shows reduced biocompatibility, low permeability, retention effect, drug resistance, and high toxicity due to several barriers encountered during circulation or abnormal vascular networks in tumor microenvironment [20]. However, the targeted stimuli-responsive NCs are precise, shows high stability, biocompatibility, enhanced permeability, shows reduced toxicity and retention effect i.e., exhibit smart behaviors at biological environments. Moreover, in conventional NCs the drug delivery is not targeted and the doesn’t show enhanced permeability and retention (EPR) effect to the tumor site, in contrast, delivery of drugs encapsulated in targeted stimuli responsive NCs offers several advantages over the direct administration of refined chemotherapeutic drugs and reduction of side effects that improves therapeutic efficacy [13, 15, 16].
Fig. 1.
Intracellular applications of nanocarriers designed using different materials. The type and functionality of the nanocarrier are controlled by its shape, size, and targeting ligands, leading to high maneuverability and target-specific drug delivery
Here, firstly we discuss the main types of NCs that have been used as drug delivery systems in the treatment of cancer (Tables 1 and 2).
Table 1.
Inorganic drug delivery NCs in cancer therapy
| Material | Description of carrier | Material advantage | Specificity | Refs. |
|---|---|---|---|---|
| CNT | Anti-P-glycoprotein antibody functionalized CNT-doxorubicin | Defeats multidrug resistance | Leukemia cells | [31] |
| CNT | Multi-walled CNT decorated with guanidinylated dendritic molecular transporters | Efficient DOX delivery | Prostate cancer cells | [32] |
| CNT | PEG-CNT complex | Mitochondrial targeting | Lung cancer cells | [33] |
| Layered double hydroxide NPs | Co-delivery of 5-fluorouracil and siRNAs | Prevents drug resistance and enhances cancer treatment | Various cancer cells | [34] |
| Layered double hydroxide NPs | Raloxifene intercalated into the interlayer gallery of LDH host | Improves therapeutic efficacy, reduction of adverse side effects | Solid tumors | [35] |
| Iron oxide NPs | Phospholipid-PEG-coated superparamagnetic iron oxide NPs | Chemotherapy and hyperthermia treatment | Solid cancers | [36] |
| Magnetic NPs | Pluronic F127-anchored iron oxide NPs | Active and passive delivery of hydrophobic drugs | Folate-positive cancer cells | [37] |
| Magnetic NPs | Chitosan-coated superparamagnetic iron oxide NPs | Doxorubicin delivery | Ovarian cancer cells | [38] |
| Mesoporous silica NPs | Azobenzene-modified mesoporous silica for NIR-triggered anticancer drug delivery | Drug release rate can be controlled by varying the intensity and/or time | Solid tumor | [39] |
| Mesoporous silica NPs | Hyaluronic acid-capped mesoporous Silica NPs | Site-selective, controlled-release delivery | MDA-MB-231 and NIH3T3 cells | [40] |
| QDs | Riboflavin-tageting graphene quantum dots-PEG-benzofuran | High potency, improved dispersibility | Laryngeal, lung and colorectal cancer cells | [2] |
| QDs | Hyaluronic acid/ferrocene (Fc)-anchored nitrogen-doped graphene QDs (Fc-GQD-HA) | Selective binding to CD44 receptors, redox-based drug delivery | Diverse range of cancer cells | [41] |
| QDs | Hederagenin anchored black phosphorus QDs encapsulated with platelet membrane | Mono-dispersive capacity, elevated drug-loading | In vivo application | [42] |
CNT carbon nanotubes; NPs nanoparticles; QDs quantum dots; LDH layered double hydroxides; PEG polyethylglycol
Table 2.
Organic drug delivery NCs in cancer therapy
| Material | Description of carrier | Material advantage | Specificity | Refs. |
|---|---|---|---|---|
| Liposomes | Liposomal doxorubicin | Improved delivery to site of disease; decrease in systemic toxicity of free drug | Ovarian cancer; multiple myeloma | [99] |
| Liposomes | Liposomal daunorubicin | Improved delivery to tumor site; lower systemic toxicity arising from side effects | Karposi’s sarcoma | [100] |
| Liposomes | Genistein and plumbagin encapsulated nanoliposomes | Inhibition of cell metabolism | In vitro and in vivo prostate cancer | [101] |
| Liposomes | Folate-conjugated bovine serum albumin bound paclitaxel NPs | Increased solubility, cellular uptake; targeted specificity | Prostate cancer cells | [102] |
| Protein-based | Alpha mangostin loaded crosslinked silk fibroin-based NPs | Physicochemically stable, increased the drug's solubility | Colorectal and breast cancer | [85] |
| Protein-based | Noscapine-loaded human serum albumin NPs | High drug-loading efficiency (85–96%) and delivery of maximum quantity of drug to the tumor site | Breast cancer cells | [103] |
| Protein-based | Plasmid cDNA (pGL3) polyethyleneimine (PEI)-coated HSA NPs | Enhance endosomal escape | In vitro gene delivery application | [104] |
| Micelles | Polymeric methoxy-PEG-poly(D,L-lactide) micelle formulation of paclitaxel | Improved delivery to site of disease; decrease in systemic toxicity of free drug | Breast cancer; ovarian cancer | [91] |
| Micelles | Folate-PEG/Hyd-curcumin/C18-g-polysuccinimide | pH sensitive drug release | Colon cancer | [105] |
| Micelles | PEGylated prodrug nano-micelles | Glucose-sensitive | In vitro and in vivo anticancer activity | [106] |
| Polymeric Micelles | CD44v6-targeted polymeric micelles (PM) loaded with niclosmide | Increase drug safety | Efficacy against colorectal stem cells | [107] |
| Self-assembly | Aptamer-tethered DNA assembly | Stronger targeting ability, higher cellular uptake | Cancer cell imaging | [108] |
| Self-assembly | DNA-aptamer conjugated RNA-triple helix hydrogel | Efficient cellular uptake and enhanced nuclease resistance with superior biocompatibility | Triple negative breast cancer detection and treatment | [109] |
| Self-assembly | Folate-modified MPEG-PCL | Improved bioavailability, low toxicity, sustained drug release | Colorectal cancer mice model | [110] |
| Self-assembly | Folate receptor-targeted β-cyclodextrin (β-CD) | Biosafety, bioavailability, and improve curcumin drug loading capacity | Cervical cancer, fibroblast cells | [111] |
Inorganic NCs
Inorganic NCs have proven to be highly useful in cancer therapy owing to their high surface area to volume ratio and easy conjugation with various cancer drugs. In addition, biocompatibility, low toxicity, and the ability to control drug release have facilitated the use of inorganic NCs, such as mesoporous silica NCs (MSNCs), gold NCs (AuNCs) [21], magnetic NCs (MNCs), carbon nanotube NCs (CNT-NCs), graphene oxide and quantum dots (QDs), as drug carriers (Fig. 2) [22].
Fig. 2.
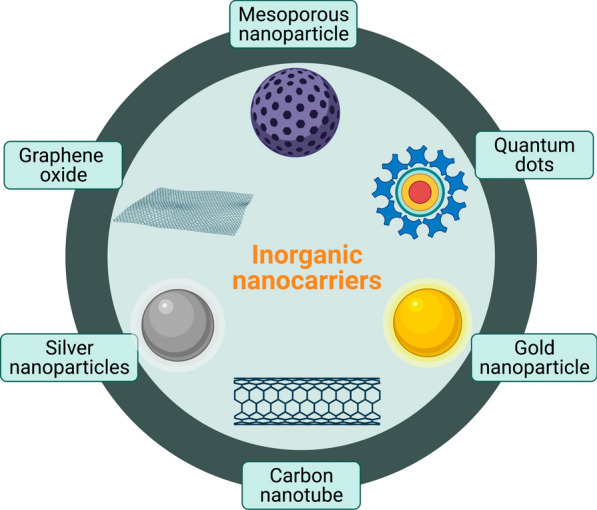
Examples of inorganic nanocarriers. Mesoporous nanoparticles are silica nanoparticles with overall diameter of < 1 μm and pores diameter from 2 to 50 nm. Quantum dots are colloidal fluorescent semiconductor nanocrystals (2–10 nm). Silver and gold nanoparticles (1–100 nm) have high surface area, tunable optical, and are non-toxic. Carbon nanotubes consist of coaxial graphite sheets (< 100 nm) rolled up cylindrical. Graphene oxide is single atomic layer of carbon, consist of thickness 1 nm. Figure has been created using Biorender
Mesoporous silica NCs
MSNCs have a variety of unique characteristics that make them appealing NCs, including a highly porous structure and adsorption capacity, tunable particle size, easy functionalization, excellent biocompatibility, and the potential to act as a physiological container to protect drugs against dysfunction or denaturation [23]. In addition, the pore diameter of some MSNCs can be controlled to regulate drug encapsulation ratios and the release kinetics, allowing anticancer medicines to be delivered in a tailored manner and discharged on time to promote cellular uptake without being released before reaching the intended target site. MSNCs can also adsorb various hydrophobic drugs and thus act as ubiquitous intracellular drug carriers by transporting them across the cell membrane. Moreover, MSNCs can simultaneously adsorb both hydrophilic and hydrophobic drugs for targeted drug delivery. For instance, Chan et al. synthesized phenyl-exMSN-PEG + TA (NTT2_131), which was anchored simultaneously with hydrophilic doxorubicin (DOX) and phobic JM15 anticancer drugs [24]. Moreover, MSNCs have the ability to target the tumor site through both active and passive mechanisms, such as the EPR effect and the evasion of reticuloendothelial system (RES) clearance [25]. Furthermore, the surface of MSNCs can be functionalized with specific ligands, such as hyaluronic acid or transferrin, to target specific tumors or be coated with proteins, enzymes, and magnetic nanoparticles, which function as homing devices. Together, the intracellular absorption, pharmacokinetics, and tissue distribution patterns of MSNCs throughout the targeting process can be significantly altered by regulating the particle size and surface of MSNCs.
Gold nanocarriers
AuNCs have been used as anticancer agents in photothermal therapy (PTT) owing to their excellent ability to convert light into heat [26]. The therapeutic potential of AuNCs is determined by their size, shape, surface plasmon resonance (SPR), and surface biochemistry [27]. Basically, size and shape of nanoparticles are important parameter that effects cellular uptake and site-specific drug delivery from the synthesized system. It was also noticed that the smaller particles infused into the deep layers of tissues while the 100–200 nm particles stayed on the surface [28], that additionally signifies better bioavailability of small sized gold NPs. The particle size also affect the blood concentration along with circulation time. Moreover, their benign nature and excellent surface functionalization properties make AuNCs effective anticancer drug carriers. The surface functionalization of AuNCs with anticancer drugs can improve their anticancer efficacy via the combined effect of the nanoparticle–drug conjugate on tumor cells, while anchoring with a specific antibody can improve their target specificity [29]. Furthermore, the surface modification of Au NPs with a pH-sensitive material can allow them to specifically target tumor cells, which have a lower pH than normal cells. Chaudhari et al. [30] investigated the metabolic pathways and mechanisms induced by methotrexate (MTX)-AuNC in breast cancer cells. MTX-AuNC targeting the folate receptor, demonstrated considerable uptake by the breast cancer cells, as well as substantial down-regulation of the anti-apoptotic gene and up-regulation of pro-apoptotic genes [30].
Magnetic NCs
MNCs have recently received a lot of interest owing to their immense potential as heat regulators for treating hyperthermia as well as their ability to transport drugs in a targeted manner, which can reduce systemic effects [43]. In addition, MNC-based cancer therapies have novel features that are not observed in traditional approaches, such as minimal toxicity and controlled drug release. The behavior of MNCs is predominantly affected by their hydrodynamic diameter, surface chemistry, and magnetic properties. Surface chemistry is crucial for preventing clearance by the RES and improving half-life within the blood circulation. For example, researchers have modified the surface of MNCs with neutral and hydrophilic ligands, such as PEG or P(S/V-COOH) polymers, and reported an improvement in their circulatory half-life from minutes to months [44]. Anchoring the surfaces of MNCs with new ligands has facilitated targeted drug delivery, and the anchoring of single or multiple drugs on MNCs has recently been studied to improve anticancer drug efficacy. The stability and biocompatibility of MNCs can be optimized by anchoring them with organic or inorganic compounds, which can improve the efficacy of anti-cancer chemotherapy and gene therapy [45]. It is worth to mention that MNCs, offers a suitable tool for cancer treatment and diagnosis due to their unique features which distinguish them from other NCs. These can act through magnetic drug targeting, making them therapy magnetically responsive, therefore it can be controlled inside the human body by external magnets, and eventually absorbed into tumor tissues. Their utilization in magnetic resonance imaging (MRI) delivers a high divergence for generating the most detailed imaging. Such as, magnetic iron oxide NPs widely applied for lung MRI due to their good magnetization and biocompatibility as well as their appropriate drug uptake and subsequent release [46]. Similarly, water-dispersible PEI-conjugated iron oxide NPs have been also exploited for MRI-based cancer imaging [47].
Carbon nanotube NCs
Carbon nanotubes (CNTs) are long cylindrical structures with flexible NCs characteristics that have sparked interest as drug delivery molecules owing to their unique biological, physical, and chemical capabilities [48]. Indeed, CNTs have been used to deliver anticancer drugs, such as DOX, paclitaxel, methotrexate, and small interfering RNAs (siRNAs), to treat a range of malignancies.
The developing siRNA technology merged with chemotherapy has presented significant rationale in cancer therapies. The main challenges in the fabrication of siRNA/chemotherapeutic drug co-loaded NPs are specific targeted delivery, sufficient cargo protection, and site-specific release [49]. CNTs are a popular multifunctional drug delivery system owing to their large surface area, high adsorption capacity, durability, ease of functionalization, an exceptionally high length-to-diameter ratio, and excellent intracellular absorption [50]. In addition, the surface characteristics of CNTs can be readily altered using covalent/noncovalent crosslinking, making them a favorable nanomaterial. The hydrophobicity of CNTs leads to π–π stacking interactions with a variety of drugs and medicinal compounds, including those with an aromatic ring such as anthracyclines; however, CNTs have a low solubility that makes them ineffective drug delivery molecules. The solubility of CNTs can be improved by surface functionalization with various molecules using covalent/noncovalent bonding and electrostatic forces to make them more hydrophilic, thus altering their biocompatibility profile [51, 52].
Quantum dots NCs (0-D)
Quantum dots (QDs) s are uniform spherical (0-D) NCs with very small sizes of 1–10 nm [53]. These fluorescent particles have exceptional physio-chemical characteristics, including a very large surface area, biocompatibility, highly customizable photoluminescence, strong signal brightness, and high photostability. These features have inspired researchers to use QDs as potential NCs for targeted and traceable drug delivery systems, to monitor intracellular processes in real time, and for in vivo molecular imaging. However, the hydrophobicity, easy agglomeration, and high adsorption affinity of QDs for the surrounding impurities make them poor candidates for therapeutic applications. Fortunately, these shortcomings can be avoided by coating QDs with ionic species or layering them with ligand shells [54]. For instance, imaging probes, smaller hydrophobic or hydrophilic drugs, and targeting agents can be embedded between the inorganic core and the amphiphilic polymer coating layer [55, 56].
2D-materials NCs
2D materials have excessive light photodynamic and heat conversion proficiency, therefore they retain various benefits in biomedical applications. These characteristics provide them high potentials in medicine fields, including imaging [57], sensing [58] and therapy [59, 60]. In the meantime, 2D materials exhibited a challenging capability in drug delivery with various advantages. One of the exclusive crucial features of 2D materials is the lamella organization, that offers the huge surface space for high drug loading efficiency [61]. Yu et al. synthesized a reduced GO nanocomposite modified with a polydopamine (PDA). They coated the dopamine-modified rGO surface with antiarrhythmic peptide 10 which limit tumor development about more than 95% while used with radiotherapy [62]. This innovative drugs possesses several abilities, such as large surface area, excellent biocompatibility, and a high drug loading capacity. Moreover, these NCs confirmed subsequent pH responsiveness and drug release. As stated by Xing et al. injectable hydrogel made of black phosphorous nanosheets and cellulose exhibits noteworthy antitumor activity in contrast to PTT. Interestingly, these nanoscale hydrogel platform is non-toxic and 100% biocompatible as confirmed by both in vitro and in vivo studies [63].
Organic nanocarriers
Organic NCs have been studied for decades and contain a diverse range of components. They are biocompatible, have low drug loading capacity and the drug molecules are encapsulated or conjugated.
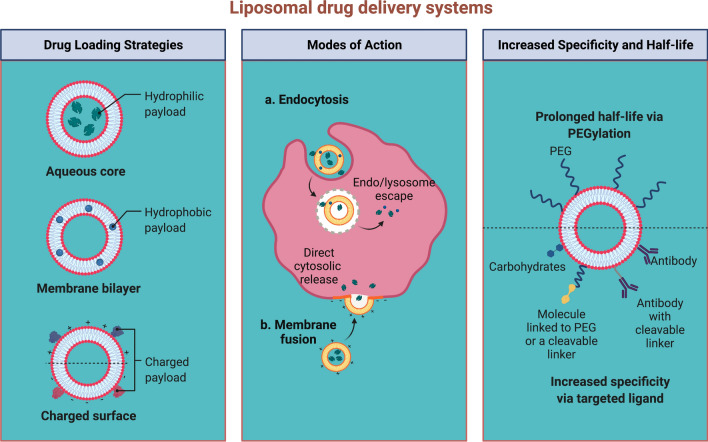
Liposomes NCs
Liposomes are made up of an exterior lipid layer and a core that contains either hydrophobic or hydrophilic medications; they were the first nano-scale drugs to be licensed for clinical use [64]. Liposomes can be modified to perform a variety of tasks by altering the lipid layer structure; for instance, the lipid layer can be altered to mimic the biophysical properties of living cells [65], which can improve the efficiency of targeted drug delivery [66]. The inner aqueous core of liposomes can be loaded with amphiphilic drugs using various techniques, such as the ammonium sulfate gradient method [67]. However, standard liposomes are rapidly eliminated from the bloodstream and can be detected by opsonin proteins, leading to phagocytosis and destruction by macrophages. To overcome this issue, surface-modified liposomes have been developed that can be grafted with monoclonal antibodies, glycoproteins, carbohydrates, vitamins, antibodies, and peptides to actively target cancer cells (Fig. 3).
Fig. 3.
Schematic representation of the different types of liposomal drug delivery systems. A Conventional liposomes consist of a lipid bilayer surrounding aqueous compartments, composed of phospholipids and cholesterol unmodified B PEGylated liposomes have a hydrophilic polymer coating (PEG) on the surface of the liposome that modifies in vivo characteristics and behavior via steric stabilization. C Ligand-targeted liposomes can affect specific targets via ligands attached to the surface or terminal end of the attached PEG chains. D Theranostic liposomes are a single system consisting of a nanoparticle, a targeting element, an imaging component, and a therapeutic component. Figure has been created using Biorender
Similarly, Najlah et al. developed stealth liposomes by modifying the surface coating of a hydrophilic lipid polymer derivative of PEG [68]. This modification was shown to improve the efficacy of the encapsulated drugs by prolonging their circulation in the blood and reducing their elimination [69].Unfortunately, the reliability of the PEGylated liposomes decreases upon systemic injection, which may prolong their circulation in the blood; therefore, novel PEG-dendron phospholipids have been developed to produce super-stealth liposomes. In vitro studies have shown that ligand-targeted liposomes can promote the internalization of liposome-drug conjugates via prostate-specific membrane antigens on the targeted cell [10]. Decades of liposome research have facilitated the development of liposomes that are a suitable platform for the in vivo administration of various anti-cancer drugs, including docetaxel [70], and nucleic acids [71]. Indeed, liposomes are now increasingly being used to treat breast [72] and prostate [73, 74] cancers. In addition, more liposome-based medicines are currently in clinical trials for cancer therapy [75, 76].
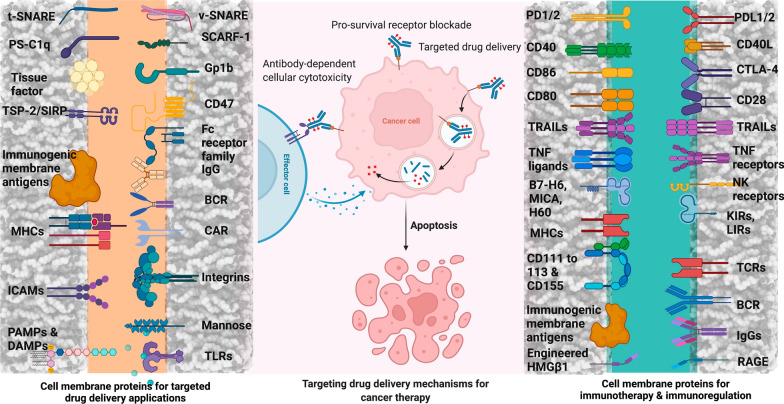
Protein-based NCs
Proteins are essential macromolecules that possess unique functions and characteristics in biological materials and manufacturing field; therefore, they are utilized as a starting material for the synthesis of NCs (Fig. 4) [77, 78].
Fig. 4.
Potential cell surface proteins and their complementary receptors for use in targeted-drug delivery applications. t-SNARE/v-SNARE target snap receptor/vesicle snap receptor; PS phosphatidylserine; C1q complement component 1q; SCARF-1 scavenger receptor class-F, member-1; Gp1b glycoprotein-Ib; TSP-2 thrombospondin-2; SIRPα signal regulatory protein α; CD cluster of differentiation; ICAM intercellular adhesion molecule; LFA-1 lymphocyte function-associated antigen-1; MAC-1 macrophage adhesion ligand-1; VLA very late antigen; PAMP pathogen associated molecular pattern; DAMP damage-associated molecular pattern; PD-1/PD-2 programmed cell death protein-1/programmed cell death protein-2; PD-L1/PD-L2 programmed death-ligand-1/programmed death-ligand-2; CTLA-4 cytotoxic t-lymphocyte-associated protein-4; TRAIL tumor necrosis factor-related apoptosis-inducing ligand; TNF tumor necrosis factor; B7-H6 B7 homolog 6; MIC MHC class I polypeptide-related sequence; H60 histocompatibility protein-60; NKp natural cytotoxicity triggering receptor; NKG natural killer cell granule protein; KIR killer-cell immunoglobulin-like receptor; LIR leukocyte immunoglobulin-like receptor; HMGβ1 high-mobility group protein β1; RAGE receptor for advanced glycation end products. Figure has been created using Biorender
Since protein-based NCs display good biodegradability and low toxicity, they are used to carry both pharmaceuticals and nutraceuticals [79]. Additionally, protein NCs have high stability, are non-antigenic, can be metabolized, and it is easy to synthesize their particles, modify their surface, and monitor their size [11]. Owing to their promising characteristics, protein NCs have been used for a variety of targeted uses, such as cancer therapy [80, 81], pulmonary delivery [82], and vaccine delivery [83]. Protein NCs can be incorporated into biodegradable polymers in a monolithic particle structure, such as a microsphere [84], to allow controlled and sustained drug release and can be produced using proteinaceous materials such as silk protein fibroin [85], bovine [86], human serum albumin [87], and gliadin [88].
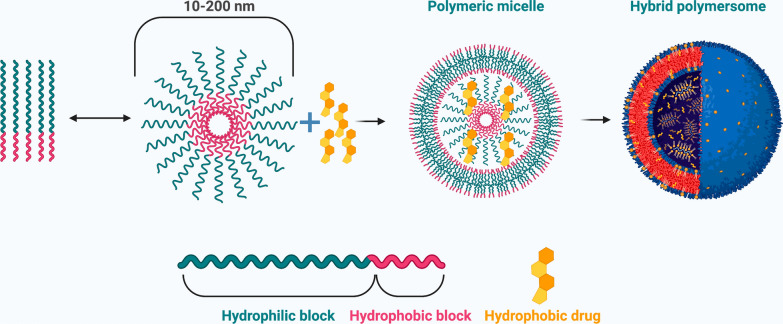
Micelles NCs
Micelles are spherical nanosized structures that are formed via the self-assembly of amphiphilic block copolymers that have both hydrophilic and hydrophobic portions in aqueous solution, thus forming a hydrophobic core and a hydrophilic shell, known as polymeric micelle (Fig. 5) [89, 90]. Micelles can be formed intrinsically at specific concentrations (critical micelle concentration (CMC) and temperatures. For instance, if the solvent portion is hydrophilic and its concentration exceeds the CMC, the polar region of the co-polymer is drawn toward the solvent, whereas the hydrophobic region is repelled from the solvent [12]. In polymeric micelles, the hydrophobic core serves as a reservoir site for the incorporation of hydrophobic drugs, while the hydrophilic shell stabilizes the core and keeps the polymer and drug intact, making micelles a suitable candidate for intravenous administration. Genexol-PM [PEG-poly(D,L-lactide)-paclitaxel] was the first cremophor-free polymeric micelle to contain paclitaxel and was shown to have no adverse reactions and a good toxicity profile in advanced refractory cancers [91].
Fig. 5.
Schematic representation of polymeric micelles. Self-assembly of di-block copolymers into a polymeric micelle takes place above the critical aggregation concentration. The hydrophobic drug is encapsulated into the hydrophobic core. Figure has been created using Biorender
Self-assembled drug NCs
The spontaneous organization of molecules into ordered geometric structures is known as molecular self-assembly and provides both inorganic and organic structures with unique qualities via non-covalent interactions. The spontaneity, versatility, inexpensiveness, and simplicity of self-assembly mean that it is extensively used for designing nanoscale biomaterials [92] and has various biomedical applications, including drug delivery, tissue engineering, and regenerative medicine. Self-assembled NCs such as micelles, polymeric NPs, liposomes, and CNTs have been shown to improve drug delivery, prolong blood circulation, control drug release kinetics, impart molecular targeting, improve tumor accumulation [93] and bioavailability, allow proper encapsulation, and protect the drug from the external milieu [94]. Ultimately, these self-assembled NCs help to overcome physiological barriers in vivo during drug delivery.
Supramolecules
Supramolecules are molecular assemblies that are held together by electrostatic interactions, metal coordination, hydrophobic attractions, host–guest interactions, and van der Waals forces [95]. Also, supramolecular compounds are easy to realize the “Lego-like” construction of NCs, which have excellent editability. These interactions provide the NCs with stability in body fluids and improve their characteristics, including durability, sustained release, and transport efficiency. Accordingly, supramolecules are used as drug carriers for targeted anticancer delivery systems [96]. Indeed, the side effects of anticancer drugs, such as DOX, on normal cells can be controlled by using amphiphiles to generate supramolecular aggregates for cancer therapy [97].DOX-anchored supramolecular polymersomes circulate in the bloodstream for a longer time, and in vivo experiments have demonstrated their superior antitumor efficacy against malignant HeLa cells with decreased cytotoxicity [98].
Stimuli-responsive NCs drug release
In recent decades, the development of novel polymers has prompted the study of smart stimuli-responsive drug delivery systems [112, 113]. Wei et al. proposed that stimuli-responsive nanomedicines determine noteworthy benefits via their adaptive transition application during drug delivery cascade [114]. A number of literature suggests that stimuli-responsive materials improve their pre-designed functions in response to the tumor microenvironment (TME) or intracellular signals, for instance conversion of the surface charge, PEG deshielding, exposure of tumor-targeting ligand, and controlled drug release [115–117]. It is broadly known that the TME has distinctive physiological characteristics such as acidic pH [118], hypoxia [119], and induction of certain enzymes [120]. Overall, the NCs might response to exogenous stimuli, including temperature, magnetic field, light etc., and endogenous stimuli, including pH, ATP, H2O2, enzyme, redox-potential, and hypoxia etc., although the stimuli might be emerged in TME or inside cancer cells (Fig. 6) [121].
Fig. 6.
Schematic illustration of drug release. In response to either internal (pH, redox, enzyme) or external (thermo, magnetic field, light) stimuli. Figure has been created using Biorender
Endogenous stimuli
Also known as an intrinsic stimuli, endogenous stimuli include changes in the internal pH levels, enzyme activity, redox activity, hypoxic conditions of the body.
pH-responsive NCs
Tumor cells primarily generate energy by enhancing glycolysis and then fermenting lactic acid in the cytosol, which is known as the Warburg effect [122]. The increased acid production results in an acidic pH in and around the cancer cells compared to that in normal cells, which is why pH has been established as an effective physiological property for targeted and controllable drug delivery by pH-responsive NCs [123, 124]. To achieve targeted and site-specific drug delivery, pH-responsive NCs exploit pH gradients in the physiological milieu [125]. The normal physiological pH is neutral (7.0–7.4), whereas the pH of the tumor microenvironment is highly acidic due to high metabolic activity and inadequate perfusion [126]. The main feature of pH-triggered NCs is their transition from hydrophobic to hydrophilic in response to acidic pH levels, which can alter their size or behavior. For instance, Tang et al. reported pH-sensitive NC systems based on reversibly ionizable carboxylic groups that undergo protonation and deprotonation due to changes in pH, leading to NC swelling, rupture, and drug release [127].
Several pH-responsive materials have been used for controlled drug delivery, including curcumin-loaded pH-sensitive N-naphthyl-N,O-succinyl chitosan polymeric micelles that were developed for colon-targeted drug delivery and exhibited pH-dependent release kinetics in colorectal cancer cells [128]. In addition, Ishida et al. [69] synthesized various pH-sensitive sterically-stabilized liposomes composed of DOPE/HSPC/CHEMS/CHOL/mPEG2000-DSPE. These liposomes enhanced drug retention and pH-sensitivity, increased the blood retention time of encapsulated DOX, and targeted antigens on cancer cells to allow controlled drug release in the acidic tumor microenvironment [69]. Unfortunately, tumor cells can still become resistant to anticancer drugs delivered by NCs, thus compromising their therapeutic efficacy. To address this issue, Guo et al. [129] developed a novel dual pH-sensitive micelle NC, PEO-b-P(DMAEMA-co-MAEBA) combined with a specific inhibitor (A01) of the TMEM16A ion channel, which is overexpressed in lung adenocarcinoma tissue. These micelles released A01 into the surrounding weakly acidic microenvironment of lung adenocarcinoma cells but were also internalized by the cells and entered their endosome-lysosome compartments, where they inhibited TMEM16A and MAPK signaling. pH-sensitive self-assembled drug carriers have also been extensively used. For instance, Song et al. synthesized biodegradable pH-responsive PEGylated DOX micelles that self-assemble in aqueous solutions via esterification and Schiff base reactions [130]. These NCs had a high drug payload and an excellent pH-responsive controlled drug release profile, as well as rapid prodrug internalization and enhanced antitumor activity against MCF-7 cancer cells. Interestingly, Chen et al. prepared a nature-inspired pH-responsive organic–inorganic hybrid capped mesoporous silica NPs based on biomineralization mechanism having low toxicity, enhanced cellular uptake and efficient drug release [131]. In another study, a group of researchers established a cRGD-decorated pH-responsive polyion complex micelle for DOX intracellular targeted delivery to enhance tumor inhibition and decrease cytotoxicity [132].
Redox-responsive NCs
Glutathione sulfhydryl (GSH) is a tripeptide compound in which glutamic acid is conjugated through its side chain to the N-terminus of cysteinylglycine. Since GSH levels are fourfold higher in cancer cells than in normal cells [133], it is used to produce redox-responsive NCs. In particular, GSH cleaves the disulfide bond of NCs in cancer cells, leading to controlled redox-driven drug release [134].
Various redox-responsive drug delivery systems have been reported in recent years, including liposome, micelle, nanogel, and prodrug-based systems. Redox-responsive liposomes initiate drug release in the presence of GSH (reducing agents) via disulfide linker reduction or liposome membrane destabilization. For instance, Chi et al. [135] synthesized a novel Chol-SS-mPEG/HA liposome (conjugated with PEG via disulfide linkages) that displayed cytoplasmic drug release triggered by GSH due to PEG de-protection and liposome agglomeration. In another study, Yin et al. [136] prepared chitooligosaccharides (COS) conjugated with cholesterol through a disulfide linker, wherein linker reduction caused COS removal, liposome instability, and rapid drug release. Micelle-based drug delivery systems are often used because of their ease of administration, enhanced circulation time when PEGylated, high structural stability, good hydrophobic drug encapsulation, and ability to respond to the external environment [137]. Micelles assembled using disulfide linkages are redox-responsive, as they can be cleaved in the presence of GSH (or a reductive environment). Sun et al. prepared redox-responsive amphiphilic glycan conjugates by linking heparosan with deoxycholic acid via disulfide bonds [138]. When the micelles reached cancer cell cytosol, they rapidly disassembled and released the drug. Similarly, Kang et al. [139] developed a redox-responsive system by linking gambogic acid with poly(amido amine)s via amide bonds, which self-assembled into micelles. The presence of disulfide bonds in a reductive environment led to rapid disassembly and release of the encapsulated drugs.
Although disulfide bonds are the main component when designing redox-responsive NCs, diselenide bonds can be used to prepare mesoporous silica-based NPs [140]. For instance, controlled drug release can be achieved using albumin or myoglobin by conjugating them to mesoporous silica-based NPs via diselenide bonds, which yields an NC that is highly responsive to GSH and H2O2 [141]. In addition, Lei et al. developed a novel intrinsic redox-responsive metal–organic framework carrier using iron, aluminum, or zirconium as metal nodes and 4,4-dithiobisbenzoic acid (4,4-DTBA) as the organic ligand [142].
Enzyme-responsive NCs
Upregulation of several enzymes are linked to the pathophysiology of many diseases, including infection, inflammation, and cancer. Since most of the enzymes are present in similar concentrations in both cancerous and normal cells [143], these NCs cannot be used for intracellular drug release; however, enzyme-cleavable peptides can be used to generate enzyme-triggered NC deshielding, which can ultimately allow the drug to be released. Enzyme-triggered NCs can be prepared by modifying the NC surface, which can respond to the biocatalytic reaction of enzymes that are overexpressed in the extracellular microenvironment of cancer cells. Such as, matrix metalloproteinases (MMPs) and hyaluronidases (HAs) are the extracellular enzymes that are mostly upregulated in tumors [144, 145]. The upregulation of these extracellular enzymes can be used to trigger NCs for reduction of their size and surface ligand exposure for tumor infiltration. It is well-stated that cathepsin and legumain showed overexpression in several cancer cells [157–161]. Legumain is the endopeptidase which specifically cleaves linkers containing asparagine or aspartic acid residues which are upregulated in the various cancer cells lysosomal compartments. For instance, Liu et al. [162] developed a legumain cleavable liposome consisting of alanine-alanine-asparagine substrate linked to cell penetrating peptides (trans-activating factor) carrying doxorubicin. In another study, Cai et al. [146] developed an enzyme-responsive colon-specific delivery system based on hollow mesoporous silica spheres conjugated with biodegradable chitosan via cleavable azo bonds and encapsulating DOX. This NCs system displayed enzyme-responsive drug release in the presence of colonic enzymes.
Hypoxia-responsive NCs
In solid tumors, the poor vascularization system is possibly to form low oxygen level (hypoxia), that plays a critical role in cancer progression, including distant metastasis [147]. Consequently, many approaches have been employed for treatment of hypoxic tumors, primarily including rising the oxygen level and by means of hypoxia activatable drugs, etc. [119]. Till date, different types of nanocarriers have been designed for the drug delivery system to hypoxic tumors [148], such as silica nanoparticles [149], liposomes [150], layer-by-layer nanoparticles [151], polymeric micelles [152], nanovesicles [153], polymersomes [154], and albumin nanoparticles [155] (Table 3).
Table 3.
List of representative hypoxia-responsive NCs [112]
| Nanocarriers | Magnetic-responsive strategy/materials | Cargos | Applications |
|---|---|---|---|
| Liposomes | The prodrug of banoxantrone dihydrochloride (AQ4N) could be activated in hypoxic environment caused by PDT | Ce6, AQ4N | Cancer therapy |
| Silica nanoquencher | Azo monomer; cell-penetrating poly(disulfide)s (CPD) coated silica nanoquencher (BS-qNP) (CPD-protein@BS-qNP) | Antibody (Cetuximab), fluorescent dye | Hypoxia-triggered protein release and fluorescence imaging |
| Upconversion nanoparticles (UCNPs) | Oxygen indicator [Ru(dpp)3]2+Cl2 for hypoxia detection as UCNPs provided the excitation light of [Ru(dpp)3]2+Cl2 by upconversion process at 980 nm | [Ru(dpp)3]2+Cl2, UCNPs | Imaging hypoxic regions or oxygen changes in cells and zebrafish |
| Nanoparticles | The photosensitizer of ICG-mediated PTT induced hypoxia, which then activated the prodrug of TPZ | TPZ, ICG | Tumor therapy by PDT and chemotherapy |
| Nanoparticles | The shift from hydrophobic to hydrophilic of 2-nitroimidazole that grafted to polymers in light-activated hypoxia | Doxorubicin, light-sensitive polymer | Hypoxia-triggered drug release, tumor |
| Nanoparticles | PEG-azo(azobenzene)-PEI-DOPE block copolymer | siRNA | siRNA delivery and tumor RNAi |
| Nanoparticles | Layer-by-layer nanoparticles with a pH-sensitive layer for targeting of tumor hypoxia | Sulfonated polystyrene beads or carboxylated quantum dots | Systemic tumor targeting |
| Cancer cell membrane coated MOFs | The porphyrinic MOFs could generate toxic ROS for PDT and cause hypoxic regions for activating TPZ | Porphyrinic metal organic framework, TPZ | Tumor targeted PDT and chemotherapy |
| Nanovesicles | The light irradiation of Ce6 induced hypoxia for oxidation bioreduction of 2-nitroimidazole in polymers and activation of TPZ | Ce6, TPZ | Tumor fluorescence imaging and therapy |
| Polymeric micelles | The metronidazole (MN) grafted in polymers could change hydrophobicity in hypoxic conditions for drug release | Doxorubicin | Tumor chemotherapy and radiotherapy |
| Polymersomes | The PLA (polylactic acid)-azobenzene-PEG is sensitive to hypoxia | Gemcitabine, hypoxia-sensitive dye “Image-iT” | Tumor imaging and drug delivery |
| Albumin nanoparticles | With hypoxia-sensitive azobenzene linker to covalently bridge photosensitizer Ce6-conjugated HSA and oxaliplatin prodrug-conjugated HSA | Oxaliplatin prodrug, Ce6 | Tumor chemotherapy and photodynamic therapy |
| Mesoporous silica nanoparticles | The Ce6-dopped mesoporous silica nanoparticles were decorated with PEG and glycol chitosan by hypoxia-sensitive azobenzene linker | Oligonucleotide (CpG), Ce6 | Cancer immunotherapy |
| Solid-state sensors | Iodide-substituted difluoroboron dibenzoylmethane-poly(lactic acid) [BF2dbm(I)PLA] solid-state sensor material | BF2dbm(I)PLA | Tumor hypoxia optical imaging |
| Polymeric probes | Poly(N-vinylpyrrolidone)-conjugated iridium-(III) complex (Ir-PVP) and poly(ε-caprolactone)-b-poly(N-vinylpyrrolidone) (PCL-PVP) nanoparticles | Iridium (III) complex | Optical imaging of tumor and metastasis |
| Polymer hybrid CaP nanoparticles | Tumor pH-triggered release of Mn2+ from CaP to boost higher contrast enhancement in hypoxic tumor regions | Mn2+ | MR imaging of solid tumors, hypoxia and metastasis |
Tumor-metabolite responsive NCs
In tumor cells, metabolic reprogramming changes the metabolic pathways to encounter their unquenchable craving for nutrient and energy. In this regard, tumor-associated metabolites are generally valued in estimating tumor incidence and advancement timely. Insufficient nutrient supply fluctuates cancer energy metabolism, in this case lactic acid (extracellular metabolite) declines the pH of the tumor microenvironment. Fruehauf et al. mentioned that the oxamate-functionalized NPs proficiently sequestered lactate dehydrogenase (LDH) to make an OxNP–protein complex. This effort validates a great concept for tuning NPs sensitivity via conjugation with a fundamental protein to aim a particular metabolite of cancer disease [156].
Exogenous stimuli
When trigger stimuli are caused by external factors, such as a change in temperature, ultrasound, or light responsiveness, they are known as exogenous stimuli. In this system, contrast agents are employed to visualize NCs retention in cancer cells.
Temperature responsive NCs
Thermo responsive NCs use temperature changes as the trigger to release their cargo, as they can change their hydrophilic and hydrophobic balance, solubility, or structural features in response to a particular temperature. These NCs show a low critical solution temperature (LCST), below which the constituents of a mixture are misciblee [157]. Thermoresponsive polymers with an LCST are promising candidates for drug delivery, as are stimuli-responsive hydrogels that can prevent drug degradation and display rapid on/off switching [158, 159]. Hydrogels can be injected as viscous liquids and become jellified under physiological conditions. For instance, Tipa et al. [160] synthesized a biocompatible and injectable thermo-responsive hydrogel that was jellified in situ at 28 °C and injected with a 5 N force. The hydrogel contained clay NPs whose interlaminar spaces were intercalated with methylene blue (MB) for controlled release with enhanced encapsulation efficiency. Notably, the Pluronic hydrogel demonstrated controlled long-term MB release. Similarly, Ahsan et al. [161] formulated a thermosensitive chitosan-based, cross-linked injectable hydrogel for the sustained delivery of disulfiram to cancer cells as a long-term cancer therapy, and found that the drug-loaded hydrogels allowed greater cellular uptake than the free drugs.
Graphene oxide (GO) has a high ratio of surficial functional groups that permits the modification of bioactive molecules, as well has high dispersibility in aqueous conditions; however, its applications are limited by non-targeted and uncontrolled drug release. To overcome these limitations, Kazempour et al. modified GO with biodegradable and hydrophilic polymeric components, such as poly(N-vinylcaprolactam) (PNVCL) and poly(glycolic acid), which conferred pH and temperature sensitivity to allow the effective loading and release of oxaliplatin in MCF-7 cells [162]. Similarly, Farjadian et al. synthesized smart temperature-and pH-responsive NCs based on a random copolymer of poly(N-isopropylacrylamide-co-acrylamide) [163]. The presence of a hydrophilic group in acrylamide increased the LCST to 37 °C (close to body temperature) and ultimately made the structure suitable for drug delivery. This structure was further modified with hydrazine and conjugated to DOX via a Schiff base linkage (acid-cleavable bond) to make NCs responsive to heat and pH.
Given that hyperthermia increases the temperature of body tissues to as high as 113 °C and increases the sensitivity of cancer cells to chemotherapeutics, combining these two effects as thermo-chemotherapy could enhance the efficacy of cancer therapy. Mirrahimi et al. [164] developed a novel multifunctional nanocomplex, consisting of an alginate nanogel loaded with cisplatin and AuNPs, for combined therapy. In vivo thermometry studies showed that under 532 nm laser irradiation, the temperature increased and exerted a higher thermal dose due to the optical absorption characteristics of AuNPs; this finding indicated that these NCs suppressed tumor growth due to their thermo-responsive behavior.
Light-responsive NCs
Various NCs can respond to light and have the potential to adjust the irradiation wavelength, power, and affecting area [165]; therefore, light-responsive NCs have recently been developed for targeted controlled drug delivery. NCs can be sensitive to any form of light, including ultraviolet, visible, or near-infrared, which can also affect biological systems such as cancer cells or tumors. By controlling the range of irradiation, light-responsive tumor therapies can be precisely conducted to minimize or avoid negative effects on normal cells. Polyplexes [166], polymeric micelles [167], liposomes [168], nanogels [169], and nanorods [170] have all been exploited as light-responsive NCs using materials such as gold nanocomposites, CNTs, graphene, and organic molecules.
NCs can undergo conformational changes in response to light via the structural conversion of light-sensitive molecules. For instance, UV–Vis-responsive photoswitching NCs have exhibited potential for loading with drugs, including DOX, docetaxel, and paclitaxel, for cancer therapy [171]. However, UV–Vis has a short wavelength, which limits the application of these NCs. Therefore, NIR light-responsive NCs may be more appropriate for controlled drug delivery [172]. Fan et al. [173] synthesized photo-responsive degradable hollow mesoporous organo silica NCs for anti-cancer drug delivery. The NCs were based on singlet oxygen (1O2)-responsive bridged organoalkoxysilanes [from a 9, 10-dialkoxy-anthracene (DN)-based precursor] and wrapped with graphene oxide QDs. Upon irradiation, the these QDs generated 1O2, leading to the cleavage of 1O2-responsive bridges, NCs degradation, and the release of the anticancer drug.
Ultrasound-responsive NCs
High-frequency waves, named as ultrasound might affect NCs for the controlled drug release at tumor sites. Currently, it has been considerably applied in the various biomedical applications, for instance gene delivery and imaging-guided drugs. It can initiate the release of the drugs via the heat produced from cavitation phenomena [174]. The ultrasound-responsive nanocarriers might be used for tumor ultrasound imaging, which is considerably safe, cost-effective and commonly applied in clinics. The gas and perfluoropentane incorporated NCs [175], which could generate gas (e.g., CO2) in biological atmosphere [176], have exhibited tumor-site specific imaging at great intensity. Besides, the ultrasound-responsive property might be used for boosting the intracellular delivery of siRNA or DNA in tumors [177]. Nevertheless, the huge size of ultrasound-responsive NCs can limit their penetration within tumor tissues, due to the weak penetration [178]. In general, the drug-loaded ultrasound-sensitive NCs might be used for tumor therapy [179] as well as theranostics [180].
Mechanisms of targeting stimuli responsive NCs to tumor site
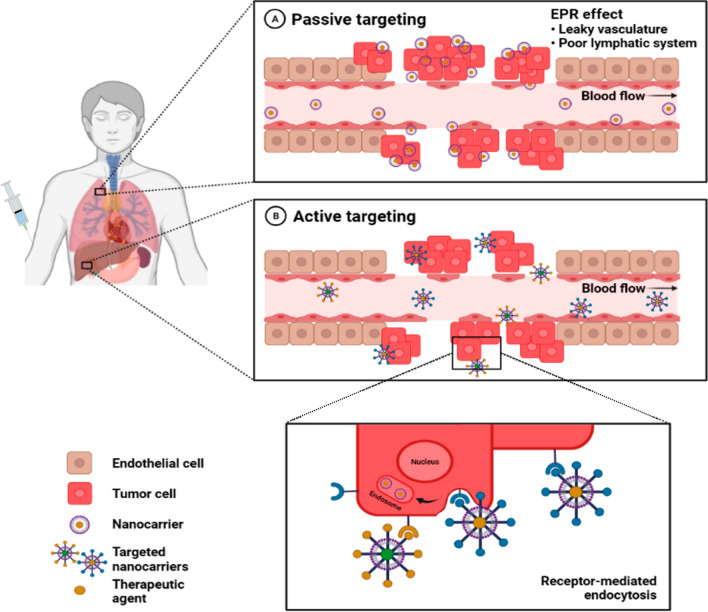
Cancer cell specificity is an important feature of NCs for drug delivery because it improves their therapeutic efficacy while sparing normal cells from damage. However, NCs can only reach cancer cells if they deceive the body's own defense system. There are two mechanisms of targeted drug delivery: passive and active targeting (Fig. 7) [181]. Both of these methods aim to prevent contact between normal cells and harmful chemicals, reduce negative dose-limiting consequences, and prevent the development of drug-resistant malignant cells.
Fig. 7.
Mechanisms of targeting NCs to tumors. A Passive targeting by nanomedicines is due to the enhanced permeability and retention (EPR) effect, which involves their extravasation from leaky tumor vasculature and poor lymphatic drainage. B Active targeting is achieved by functionalizing nanomedicines with targeting ligands that recognize tumor cell receptors, which increases cell specificity and uptake. Figure has been created using Biorender
Passive targeting
Compared to normal cells, rapidly developing malignant cells put higher stress on the endothelium of blood vessels, resulting in the formation of new vessels or the depletion of existing vessels. During this process, pores are formed on cancer cells, allowing the adsorbed macromolecules or NCs to enter the newly formed vessels [182]. Inadequate lymphatic drainage within tumors prevents the NCs from leaving, thereby enabling them to discharge the loaded drugs into the cancer cells. This phenomenon is known as the EPR effect and is an important factor for passive targeting [125]. This effect is influenced by the diameter of NPs; studies have shown that smaller NPs have a higher permeation but do not spill into regular channels [183], whereas micro molecules are preferentially removed by immune defense systems [184]. Interstitial fluid pressure (IFP) is another obstacle to the effective deposition of drug-loaded nanocarriers in solid tumors [185]; however, successful NCs alterations can bypass biological obstacles. At first, passively targeted NCs moved the clinic several years back with the agreement of PEGylated liposomal doxorubicin (DOXIL™) [186]. There are numerous studies regarding passive targeting by lipid NPs also. For instance, sclareol-SLNs with an typical particle size of 88 nm, has disclosed considerably growth inhibition effect on lung cancer cells along with a sustained drug release when compared to the free drug alone [187]. Conjugation of curcumin with solid lipid NPs is additional report for passive targeting of osteocarcoma cancer tissues with extremely higher tissue availability [188]. In contrast, for passive targeting of melanoma and glioblastoma, temozolomide-SLN exhibited maximum inhibition in proliferation with low toxicity in normal counterparts when compared to temozolomide without solid lipid NPs [189].
A variety of NPs are now being used in clinical trials, including Genexol-PM™ in Korea and ProLindac™ and Opaxio™ in the United States [190]. Awada et al. and Burris et al. have also validated the standards and/or therapeutic efficacy of a variety of other NCs in clinical trials, including AZD2811, NK911, and CPX-1 [191, 192]. Though, many of these NCs basically change the toxicological profile, or drug solubility, some have also presented substantial survival advantages and improved therapeutic efficacy as stated in clinical reports. One case is Abraxane™ which established notably greater response rates as compared to standard paclitaxel treatment in a phase III trial conducted in breast cancer patients with metastasis [193].This findings is tremendously promising for this field which opens up innovative prospects in employing NCs as smart delivery vehicles for various drugs. Unfortunately, passive targeting has several drawbacks, including non-specific drug distribution, restriction of the EPR effect, and varying blood vessel permeability across tumors [194].
Active targeting
Active targeting approaches are considerably more complicated than the passive approaches. It is remarkable that the active targeting is critical for the drug and gene delivery to the site of interest and thereby augments the therapeutic efficacy and restricts side effects on the normal tissues. Active targeting is able to improve the amount of drug delivered to the target tumor cell compared passively targeted NCs. Following accumulation in the tumor site, the drug competence may be even augmented by the active targeting. This is accomplished via the decoration of the NCs surfaces with ligands which could bind to overexpressed receptors in tumor cells [181]. This strategies will expand the affinities of the NCs for the tumor cell surface to improve the drug penetration capability. To ensure that the drugs are released at a specific location at a predetermined ratio, the binding of NCs ligands to cancer cell receptors causes receptor-mediated endocytosis, which allows the NCs to effectively deliver the therapeutic drugs. Consequently, active targeting is specifically tailored toward the transport of macromolecular drugs, such as proteins and siRNAs. Targeting ligands include proteins (antibodies and fragments), nucleic acids (aptamers), and other peptides, vitamins, and carbohydrates [195]. The ligands attach to receptors on targeted cells, among which the most common are the transferrin receptor, folate receptor, glycoproteins, and epidermal growth factor receptor. Bartlett et al. demonstrated that the active targeting of nucleic acids into cells may also be used to silence luciferase beacons targeting the transferrin receptor in neuroblastoma xenografts [196]. Although there are currently no commercially available active targeting NCs on the market, clinical trials are under way for NCs based on liposome-targeted and polymeric NPs. For instance, MBP-426, MCC-465, SGT53, MM-302, BIND-014, CALEA-01, cetuximad-decorated Doxil/Caelyx liposomes, and a retroviral vector are currently in phase I/II clinical studies for primary therapeutic targets, including EGF, Tf-R, PSMA, the surface of gastric cancer cells, and HER-2 [191, 192].
In general, crossing the tumor endothelium is a fundamental footstep in the expedition of NPs from the administration region to diseased tissues. Earlier literature proposed that the vascular barrier of tumor blood vessels is compromised [197]. It is believed that compared to healthy blood vessels, tumor blood vessels could demonstrate certain pathological features that affect NPs activity throughout accumulation inside tumor tissues [198] concisely, systemically controlled NPs could transport from the tumor blood vessel lumen via the endothelial spaces into the tumor interstitial area [197]. This is the central mechanism for both active and passive NPs targeting [199].
Challenges and future prospects
As nanotechnology and innovative functional materials have advanced, so has interest in polymer and hybrid-based nanocarriers for drug delivery. Developing nanocarriers for the delivery of pharmaceuticals has long been a focus of many scientists. Despite substantial advances with hybrid nanocarriers, polymer-based nanocarriers have had a lot of success in clinical studies. While in circulation in the blood, nanocarriers must (1) prevent early leakage of therapeutic agents, (2) possess targeting ability so that therapeutic agents may aggregate at tumor sites and decrease severe side effects on healthy tissues, show biocompatibility, and (3) demonstrate degradability.
There has been a surge in interest in nanocarriers due to a variety of factors including their biodegradability, biocompatibility, physiological medium stability, and structural instability in malignancies. Polymer or hybrid-based nanocarriers with stimuli-responsive properties have required a great deal of effort to create effectively. They were able to change their pH, enzyme, thermal, and ultrasonic responsiveness to deliver medications to tumors. It is possible to deliver chemotherapy chemicals to tumors more accurately owing to nanocarriers, which both encapsulate and distribute the chemicals in a targeted manner. To improve the therapeutic efficacy of hybrid-based nanocarriers, these nanocarriers have also been used in imaging. Hybrid nanocarriers, which are being developed at a rapid pace, are anticipated to stimulate a combination of diagnostic and therapeutic in the area of cancer therapy. Researchers have proven that theragnostic hybrid nanocarriers with theragnostic capabilities may be utilized to correctly cure cancer in the future. To date, the hybrid-based nanocarriers’ therapeutic efficacy has been improved by using these nanocarriers in imaging. Nanocarriers that combine diagnostic and therapeutic capabilities are anticipated to be encouraged by the rapid development of hybrid nanocarriers. Hybrid nanocarriers with theragnostic capabilities may be employed to correctly treat cancer in the future as previously predicted.
A few issues remain in the design of nanocarriers containing stimuli-responsive polymer or hybrid materials. Although progress has been made in the development of stable nanocarriers in a healthy medium and stable nanocarriers at tumor locations, it is still challenging to accomplish. The discovery of novel hybrid-based nanocarriers, despite significant progress, continues to impede the development of nanomedicines. Nanocarriers have also been overdesigned in recent decades to integrate many functionalities into a single molecule in order to create a multifunctional nanomedicine. Nanocarriers that are too complicated to be used in clinical trials are generally the result of over-engineering. Nature is always guided by the simplest and most cost-effective rules of operation. Polymer or hybrid nanocarriers that can be synthesized economically and at large scale will thus be the most beneficial. In the end, these issues and obstacles will encourage biomedical scientists to better decipher the relationships between the nanocarriers structural and functional aspects and to enhance nanocarrier design. Consequently, experts from a variety of fields will be better able to realize the promise of stimuli-responsive nanocarriers for cancer treatment if they work together.
Conclusion
In this review, we have provided a broad overview of various materials that can be used as drug delivery NCs for cancer therapy, as well as stimuli-based drug delivery systems and the different mechanisms of targeting. Due to their unique characteristics, clinicians have been able to use drug delivery NCs as monotherapies or as adjuncts to current treatments in order to enhance therapeutic efficacy (Table 4). Although some of these systems have failed in clinical trials, numerous new and intriguing materials are currently under development and display tremendous potential, indicating that new therapeutic alternatives may soon be available. In particular, stimuli-sensitive NCs provide high specificity as well as various desirable drug delivery functions, including regulated release, tumor accumulation, and better diagnostic and therapeutic efficacy.
Table 4.
List of NCs used in clinics or in clinical trials [200]
| Products | Drug | Nanocarrier | Application |
|---|---|---|---|
| In clinics | |||
| ADI-PEG 20 | Arginine deaminase | Polymeric | Hepatocellular carcinoma |
| Doxil | Doxorubicin | Polymeric | Leukemia, lymphoma, and carcinoma |
| AP5280 | Platinum | Polymeric | Solid tumors |
| DepoCyt | Cytarabine | Liposomal | Lymphomatous meningitis |
| MAG-CPT | Camptothecin | Polymeric | Solid tumors |
| Visudyne | Verteporfin | Liposomal | Macular degeneration |
| Oncaspar | L-Asparaginase | Polymeric | Lymphoblastic leukemia |
| Pegasys | Interferon alfa-2a | Polymeric | Hepatitis B and hepatitis C |
| Clinical trials | |||
| PNU166945 | Paclitaxel | Polymeric | Solid tumors |
| Lipoplatin | Cisplatin | Liposomal | Non-small cell lung cancer |
| XMT-1001 | Camptothecin | Polymeric | Gastric cancer and lung cancer |
| Onco-TCS | Vincristine | Liposomal | Relapsed non-Hodgkin lymphoma |
| OSI-211 | Lurotecan | Liposomal | Head, neck, and ovarian cancer |
| SPI-077 | Cisplatin | Liposomal | Head, lung, and neck cancer |
| PEG-SN38 | Irinotecan derivate | Polymeric | Solid tumors and breast cancer |
| Livatag | Doxorubicin | Polymeric | Liver cancer |
| NKTR-105 | Docetaxel | Polymeric | Solid tumors and ovarian cancer |
| Paclical | Paclitaxel | Polymeric | Breast, lung, and ovarian cancer |
| PEG-docetaxel | Docetaxel | Polymeric | Solid tumors |
Acknowledgements
Not applicable.
Abbreviations
- NCs
Nanocarriers
- MDR
Multiple Drug Resistance
- NPs
Nanoparticles
- EPR
Enhanced Permeability and Retention
- MSNCs
Mesoporous Silica NCs
- AuNCs
Gold (Au) NCs
- MNCs
Magnetic NCs
- CNNCs
Carbon Nanotube NCs
- QDs
Quantum Dots
- DOX
Doxorubicin
- RES
Reticulo Endothelial System
- PTT
Photothermal Therapy
- SPR
Surface Plasmon Resonance
- PEG
PolyEthylene Glycol
- FA
Folic Acid
- IO
Iron Oxide
- CIO
Chitosan-coated Iron Oxide
- CNTs
Carbon Nanotubes
- siRNAs
small interfering RNAs
- MWCNTs
Multi-Walled CNTs
- RF
Riboflavin
- ROS
Reactive Oxygen Species
- Fc
Ferrocene
- TUNEL
Terminal deoxyribonucleotide transferase-mediated dUTP Nick-End-Labeling
- DNR
Daunorubicin
- PLGA
Poly (Lactic-co-Glycolic Acid)
- PLL
Poly-L-Lysine
- Tf
Transferrin
- FNPs
Fibroin Nanoparticles
- PEI
PolyEthyleneImine
- SPARC
Secreted Protein, Acidic, and Rich in Cysteine
- BSA
Bovine Serum Albumin
- HSA
Human Serum Albumin
- FRα
Folate Receptor alpha
- BID
BH3 Interacting Domain
- Bcl-2
B-cell lymphoma 2
- BAX
Bcl-2-associated X
- TRAIL
Tumor necrosis factor-Related Apoptosis-Inducing Ligand
- CMC
Critical Micelle Concentration
- RAP
Rapamycin
- WOG
Wogonin
- VEGF
Vascular Endothelial Growth Factor
- CSCs
Cancer Stem Cells
- Fab
Antibody fragment
- cur
Curcumin
- GSH
Glutathione SulfHydryl
- COS
Chito Oligo Saccharides
- LCST
Low Critical Solution Temperature
- MB
Methylene Blue
- GO
Graphene Oxide
- PNVCL
Poly(N-VinylCaproLactam)
- mio
Magnetic Iron Oxide
- GOQDs
Graphene Oxide QDs
- IFP
Interstitial Fluid Pressure
Authors’ contributions
NK-conceptualization, writing original draft; SBB, SKN-writing; PKP, NK, NKK, EHC-writing, review and editing; NK, PKP-illustrations, EHC, NK, NKK-supervision and funding resources. All authors read and approved the final manuscript.
Funding
This study was also supported by the National Research Foundation (NRF) of Korea, funded by the Korea government (NRF-2021R1C1C1013875, 2021R1A6A1A03038785 and 2021R1F1A1055694).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Neha Kaushik and Shweta B. Borkar contributed equally in this work
Contributor Information
Neha Kaushik, Email: neha.bioplasma@suwon.ac.kr.
Nagendra Kumar Kaushik, Email: kaushik.nagendra@kw.ac.kr.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Iannazzo D, Pistone A, Celesti C, Triolo C, Patané S, Giofré SV, et al. A smart nanovector for cancer targeted drug delivery based on graphene quantum dots. Nanomaterials. 2019;9:1–17. doi: 10.3390/nano9020282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanadgol N, Wackerlig J. Developments of smart drug-delivery systems based on magnetic molecularly imprinted polymers for targeted cancer therapy: a short review. Pharmaceutics. 2020;12:1–31. doi: 10.3390/pharmaceutics12090831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yao Y, Zhou Y, Liu L, Xu Y, Chen Q, Wang Y, et al. Nanoparticle-based drug delivery in cancer therapy and its role in overcoming drug resistance. Front Mol Biosci. 2020;7:1–14. doi: 10.3389/fmolb.2020.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kutova OM, Guryev EL, Sokolova EA, Alzeibak R, Balalaeva IV. Targeted delivery to tumors: Multidirectional strategies to improve treatment efficiency. Cancers. 2019 doi: 10.3390/cancers11010068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ding J, Chen J, Gao L, Jiang Z, Zhang Y, Li M, et al. Engineered nanomedicines with enhanced tumor penetration. Nano Today. 2019;29:100800. [Google Scholar]
- 7.Kreuter J. Nanoparticles-a historical perspective. Int J Pharm. 2007;331:1–10. doi: 10.1016/j.ijpharm.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 8.Khanna SC, Jecklin T, Speiser P. Bead polymerization technique for sustained-release dosage form. J Pharm Sci. 1970;59:614–8. doi: 10.1002/jps.2600590508. [DOI] [PubMed] [Google Scholar]
- 9.Chen Z, Wang Z, Gu Z. Bioinspired and Biomimetic Nanomedicines. Acc Chem Res. 2019;52:1255–64. doi: 10.1021/acs.accounts.9b00079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patil Y, Shmeeda H, Amitay Y, Ohana P, Kumar S, Gabizon A. Targeting of folate-conjugated liposomes with co-entrapped drugs to prostate cancer cells via prostate-specific membrane antigen (PSMA) Nanomed Nanotechnol Biol Med. 2018;14:1407–16. doi: 10.1016/j.nano.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Lohcharoenkal W, Wang L, Chen YC, Rojanasakul Y. Protein nanoparticles as drug delivery carriers for cancer therapy. Biomed Res Int. 2014 doi: 10.1155/2014/180549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cagel M, Tesan FC, Bernabeu E, Salgueiro MJ, Zubillaga MB, Moretton MA, et al. Polymeric mixed micelles as nanomedicines: achievements and perspectives. Eur J Pharm Biopharm. 2017;113:211–28. doi: 10.1016/j.ejpb.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 13.Masood F. Polymeric nanoparticles for targeted drug delivery system for cancer therapy. Mater Sci Eng C. 2016;60:569–78. doi: 10.1016/j.msec.2015.11.067. [DOI] [PubMed] [Google Scholar]
- 14.Xin Y, Yin M, Zhao L, Meng F, Luo L. Recent progress on nanoparticle-based drug delivery systems for cancer therapy. Cancer Biol Med. 2017;14:228–241. doi: 10.20892/j.issn.2095-3941.2017.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahato R. Nanoemulsion as targeted drug delivery system for cancer therapeutics. J Pharm Sci Pharmacol. 2017;3:83–97. [Google Scholar]
- 16.Narayanaswamy R, Torchilin VP. Hydrogels and their applications in targeted drug delivery. Molecules. 2019;24:603. doi: 10.3390/molecules24030603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deshpande PP, Biswas S, Torchilin VP. Current trends in the use of liposomes for tumor targeting. Nanomedicine. 2013;8:1509–1528. doi: 10.2217/nnm.13.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang G, Gao S, Tian R, Miller-Kleinhenz J, Qin Z, Liu T, et al. Theranostic hyaluronic acid-iron micellar nanoparticles for magnetic-field-enhanced in vivo cancer chemotherapy. ChemMedChem. 2018;13:78–86. doi: 10.1002/cmdc.201700515. [DOI] [PubMed] [Google Scholar]
- 19.Bahrami B, Hojjat-Farsangi M, Mohammadi H, Anvari E, Ghalamfarsa G, Yousefi M, et al. Nanoparticles and targeted drug delivery in cancer therapy. Immunol Lett. 2017;190:64–83. doi: 10.1016/j.imlet.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 20.Zhou Y, Chen X, Cao J, Gao H. Overcoming the biological barriers in the tumor microenvironment for improving drug delivery and efficacy. J Mater Chem B. 2020;8:6765–81. doi: 10.1039/d0tb00649a. [DOI] [PubMed] [Google Scholar]
- 21.Li W, Cao Z, Liu R, Liu L, Li H, Li X, et al. AuNPs as an important inorganic nanoparticle applied in drug carrier systems. Artif Cells Nanomed Biotechnol. 2019;47:4222–33. doi: 10.1080/21691401.2019.1687501. [DOI] [PubMed] [Google Scholar]
- 22.Nejati K, Dadashpour M, Gharibi T, Mellatyar H, Akbarzadeh A. Biomedical applications of functionalized gold nanoparticles: a review. J Clust Sci. 2021 [Google Scholar]
- 23.Zhao W, Wang H, Wang H, Han Y, Zheng Z, Liu X, et al. Light-responsive dual-functional biodegradable mesoporous silica nanoparticles with drug delivery and lubrication enhancement for the treatment of osteoarthritis. Nanoscale. 2021;13:6394–6399. doi: 10.1039/d0nr08887k. [DOI] [PubMed] [Google Scholar]
- 24.Chan Hardy Wai Hong (New Taipei City), Mou Chung-Yuan (Taipei City), Wu Cheng-Hsun (Hsinchu City), Wu Si-Han (Taoyuan City), Chen Yi-Ping Chen (Keelung City) Zhang Rong-Lin (Pingtung City). Drug delivery by pore-modified mesoporous silica nanoparticles. 2021.01.20 https://patents.justia.com/patent/20210015757#history.
- 25.Narayan R, Nayak UY, Raichur AM, Garg S. Mesoporous silica nanoparticles: a comprehensive review on synthesis and recent advances. Pharmaceutics. 2018;10:1–49. doi: 10.3390/pharmaceutics10030118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ali HR, Selim SA, Aili D. Effects of macrophage polarization on gold nanoparticle-assisted plasmonic photothermal therapy. RSC Adv. 2021;11:25047–25056. doi: 10.1039/d1ra03671h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bakeer AM, Hassanen EI, Korany RMS. Cisplatin-conjugated gold nanoparticles-based drug delivery system for targeting hepatic tumors. J Biochem Mol Toxicol. 2021 doi: 10.1002/jbt.22722. [DOI] [PubMed] [Google Scholar]
- 28.Sonavane G, Tomoda K, Sano A, Ohshima H, Terada H, Makino K. In vitro permeation of gold nanoparticles through rat skin and rat intestine: effect of particle size. Colloids Surfaces B Biointerfaces. 2008;65:1–10. doi: 10.1016/j.colsurfb.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 29.Tao Y, Chan HF, Shi B, Li M, Leong KW. Light: a magical tool for controlled drug delivery. Adv Funct Mater. 2020;30:1–28. doi: 10.1002/adfm.202005029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chaudhari R, Patel P, Meghani N, Nasra S, Kumar A. Fabrication of methotrexate-loaded gold nanoconjugates and its enhanced anticancer activity in breast cancer. 3 Biotech. 2021;11:1–13. doi: 10.1007/s13205-021-02718-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li R, Wu R, Zhao L, Wu M, Yang L, Zou H. P-glycoprotein antibody functionalized carbon nanotube overcomes the multidrug resistance of human leukemia cells. ACS Nano. 2010;4:1399–1408. doi: 10.1021/nn9011225. [DOI] [PubMed] [Google Scholar]
- 32.Lyra KM, Kaminari A, Panagiotaki KN, Spyrou K, Papageorgiou S, Sakellis E, et al. Multi-walled carbon nanotubes decorated with guanidinylated dendritic molecular transporters: an efficient platform for the selective anticancer activity of doxorubicin. Pharmaceutics. 2021 doi: 10.3390/pharmaceutics13060858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim SW, Kyung Lee Y, Yeon Lee J, Hee Hong J, Khang D. PEGylated anticancer-carbon nanotubes complex targeting mitochondria of lung cancer cells. Nanotechnology. 2017;28:465102. doi: 10.1088/1361-6528/aa8c31. [DOI] [PubMed] [Google Scholar]
- 34.Li L, Gu W, Chen J, Chen W, Xu ZP. Co-delivery of siRNAs and anti-cancer drugs using layered double hydroxide nanoparticles. Biomaterials. 2014;35:3331–3339. doi: 10.1016/j.biomaterials.2013.12.095. [DOI] [PubMed] [Google Scholar]
- 35.Senapati S, Thakur R, Verma SP, Duggal S, Mishra DP, Das P, et al. Layered double hydroxides as effective carrier for anticancer drugs and tailoring of release rate through interlayer anions. J Control Release. 2016;224:186–98. doi: 10.1016/j.jconrel.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 36.Maier-Hauff K, Ulrich F, Nestler D, Niehoff H, Wust P, Thiesen B, et al. Efficacy and safety of intratumoral thermotherapy using magnetic iron-oxide nanoparticles combined with external beam radiotherapy on patients with recurrent glioblastoma multiforme. J Neurooncol. 2011;103:317–324. doi: 10.1007/s11060-010-0389-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hiremath CG, Heggnnavar GB, Kariduraganavar MY, Hiremath MB. Co-delivery of paclitaxel and curcumin to foliate positive cancer cells using Pluronic-coated iron oxide nanoparticles. Prog Biomater. 2019;8:155–68. doi: 10.1007/s40204-019-0118-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Javid A, Ahmadian S, Saboury AA, Kalantar SM, Rezaei-Zarchi S. Chitosan-coated superparamagnetic iron oxide nanoparticles for doxorubicin delivery: synthesis and anticancer effect against human ovarian cancer cells. Chem Biol Drug Des. 2013;82:296–306. doi: 10.1111/cbdd.12145. [DOI] [PubMed] [Google Scholar]
- 39.Liu J, Bu W, Pan L, Shi J. NIR-triggered anticancer drug delivery by upconverting nanoparticles with integrated azobenzene-modified mesoporous silica. Angew Chemie. 2013;125:4471–4475. doi: 10.1002/anie.201300183. [DOI] [PubMed] [Google Scholar]
- 40.Chen Z, Li Z, Lin Y, Yin M, Ren J, Qu X. Bioresponsive hyaluronic acid-capped mesoporous silica nanoparticles for targeted drug delivery. Chem A Eur J. 2013;19:1778–83. doi: 10.1002/chem.201202038. [DOI] [PubMed] [Google Scholar]
- 41.Campbell E, Hasan MT, Gonzalez-Rodriguez R, Truly T, Lee BH, Green KN, et al. Graphene quantum dot formulation for cancer imaging and redox-based drug delivery. Nanomed Nanotechnol Biol Med. 2021 doi: 10.1016/j.nano.2021.102408. [DOI] [PubMed] [Google Scholar]
- 42.Shang Y, Wang Q, Wu B, Zhao Q, Li J, Huang X, et al. Platelet-membrane-camouflaged black phosphorus quantum dots enhance anticancer effect mediated by apoptosis and autophagy. ACS Appl Mater Interfaces. 2019;11:28254–28266. doi: 10.1021/acsami.9b04735. [DOI] [PubMed] [Google Scholar]
- 43.Fatimah I, Fadillah G, Yudha SP. Synthesis of iron-based magnetic nanocomposites: a review. Arab J Chem. 2021;14:103301. [Google Scholar]
- 44.Arami H, Khandhar A, Liggitt D, Krishnan KM. In vivo delivery, pharmacokinetics, biodistribution and toxicity of iron oxide nanoparticles. Chem Soc Rev. 2015;44:8576–8607. doi: 10.1039/c5cs00541h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rayegan A, Allafchian A, Abdolhosseini Sarsari I, Kameli P. Synthesis and characterization of basil seed mucilage coated Fe3O4 magnetic nanoparticles as a drug carrier for the controlled delivery of cephalexin. Int J Biol Macromol. 2018;113:317–28. doi: 10.1016/j.ijbiomac.2018.02.134. [DOI] [PubMed] [Google Scholar]
- 46.Laurent S, Forge D, Port M, Roch A, Robic C, Vander Elst L, et al. Magnetic iron oxide nanoparticles: synthesis, stabilization, vectorization, physicochemical characterizations, and biological applications. Chem Rev. 2008;108:2064–110. doi: 10.1021/cr068445e. [DOI] [PubMed] [Google Scholar]
- 47.Yang J, Luo Y, Xu Y, Li J, Zhang Z, Wang H, et al. Conjugation of iron oxide nanoparticles with RGD-modified dendrimers for targeted tumor MR imaging. ACS Appl Mater Interfaces. 2015;7:5420–8. doi: 10.1021/am508983n. [DOI] [PubMed] [Google Scholar]
- 48.Debnath SK, Srivastava R. Drug delivery with carbon-based nanomaterials as versatile nanocarriers: progress and prospects. Front Nanotechnol. 2021;3:1–22. [Google Scholar]
- 49.Sun J, Ogunnaike EA, Jiang X, Chen Z. Nanotechnology lights up the antitumor potency by combining chemotherapy with siRNA. J Mater Chem B. 2021;9:7302–17. doi: 10.1039/d1tb01379c. [DOI] [PubMed] [Google Scholar]
- 50.Sajjadi M, Nasrollahzadeh M, Jaleh B, Soufi GJ, Iravani S. Carbon-based nanomaterials for targeted cancer nanotherapy: recent trends and future prospects. J Drug Target. 2021;29:716–41. doi: 10.1080/1061186X.2021.1886301. [DOI] [PubMed] [Google Scholar]
- 51.Figarol A, Pourchez J, Boudard D, Forest V, Tulliani JM, Lecompte JP, et al. Biological response to purification and acid functionalization of carbon nanotubes. J Nanoparticle Res. 2014 [Google Scholar]
- 52.Jha R, Singh A, Sharma PK, Fuloria NK. Smart carbon nanotubes for drug delivery system: a comprehensive study. J Drug Deliv Sci Technol. 2020;58:101811. [Google Scholar]
- 53.Molaei MJ. Carbon quantum dots and their biomedical and therapeutic applications: a review. RSC Adv. 2019;9:6460–6481. doi: 10.1039/c8ra08088g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ghanbari N, Salehi Z, Khodadadi AA, Shokrgozar MA, Saboury AA. Glucosamine-conjugated graphene quantum dots as versatile and pH-sensitive nanocarriers for enhanced delivery of curcumin targeting to breast cancer. Mater Sci Eng C. 2021;121:111809. doi: 10.1016/j.msec.2020.111809. [DOI] [PubMed] [Google Scholar]
- 55.Gidwani B, Sahu V, Shukla SS, Pandey R, Joshi V, Jain VK, et al. Quantum dots: prospectives, toxicity, advances and applications. J Drug Deliv Sci Technol. 2021;61:102308. [Google Scholar]
- 56.Zhao MX, Zhu BJ. The research and applications of quantum dots as nano-carriers for targeted drug delivery and cancer therapy. Nanoscale Res Lett. 2016 doi: 10.1186/s11671-016-1394-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen H, Liu T, Su Z, Shang L, Wei G. 2D transition metal dichalcogenide nanosheets for photo/thermo-based tumor imaging and therapy. Nanoscale Horizons. 2018;3:74–89. doi: 10.1039/c7nh00158d. [DOI] [PubMed] [Google Scholar]
- 58.Tang X, Du A, Kou L. Gas sensing and capturing based on two-dimensional layered materials: overview from theoretical perspective. WIREs Comput Mol Sci. 2018 [Google Scholar]
- 59.Jin J, Guo M, Liu J, Liu J, Zhou H, Li J, et al. Graphdiyne nanosheet-based drug delivery platform for photothermal/chemotherapy combination treatment of cancer. ACS Appl Mater Interfaces. 2018;10:8436–42. doi: 10.1021/acsami.7b17219. [DOI] [PubMed] [Google Scholar]
- 60.Liu Z, Chen H, Jia Y, Zhang W, Zhao H, Fan W, et al. A two-dimensional fingerprint nanoprobe based on black phosphorus for bio-SERS analysis and chemo-photothermal therapy. Nanoscale. 2018;10:18795–804. doi: 10.1039/c8nr05300f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peng L, Mei X, He J, Xu J, Zhang W, Liang R, et al. Monolayer nanosheets with an extremely high drug loading toward controlled delivery and cancer theranostics. Adv Mater. 2018;30:1707389. doi: 10.1002/adma.201707389. [DOI] [PubMed] [Google Scholar]
- 62.Yu J, Lin Y-H, Yang L, Huang C-C, Chen L, Wang W-C, et al. Improved anticancer photothermal therapy using the bystander effect enhanced by antiarrhythmic peptide conjugated dopamine-modified reduced graphene oxide nanocomposite. Adv Healthc Mater. 2017;6:1600804. doi: 10.1002/adhm.201600804. [DOI] [PubMed] [Google Scholar]
- 63.Xing C, Chen S, Qiu M, Liang X, Liu Q, Zou Q, et al. Conceptually novel black phosphorus/cellulose hydrogels as promising photothermal agents for effective cancer therapy. Adv Healthc Mater. 2018;7:1701510. doi: 10.1002/adhm.201701510. [DOI] [PubMed] [Google Scholar]
- 64.Zylberberg C, Matosevic S. Pharmaceutical liposomal drug delivery: a review of new delivery systems and a look at the regulatory landscape. Drug Deliv. 2016;23:3319–3329. doi: 10.1080/10717544.2016.1177136. [DOI] [PubMed] [Google Scholar]
- 65.Lemière J, Carvalho K, Sykes C. Cell-sized liposomes that mimic cell motility and the cell cortex. Methods Cell Biol. 2015;128:271–285. doi: 10.1016/bs.mcb.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 66.Hua S, Wu SY. The use of lipid-based nanocarriers for targeted pain therapies. Front Pharmacol. 2013;4:1–7. doi: 10.3389/fphar.2013.00143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bolotin EM, Cohen R, Bar LK, Emanuel N, Ninio S, Danilo DL, et al. Ammonium sulfate gradients for efficient and stable remote loading of amphipathic weak bases into liposomes and ligandoliposomes. J Liposome Res. 1994;4:455–479. [Google Scholar]
- 68.Najlah M, Suliman AS, Tolaymat I, Kurusamy S, Kannappan V, Elhissi AMA, et al. Development of injectable PEGylated liposome encapsulating disulfiram for colorectal cancer treatment. Pharmaceutics. 2019;11:1–16. doi: 10.3390/pharmaceutics11110610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ishida T, Okada Y, Kobayashi T, Kiwada H. Development of pH-sensitive liposomes that efficiently retain encapsulated doxorubicin (DXR) in blood. Int J Pharm. 2006;309:94–100. doi: 10.1016/j.ijpharm.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 70.Wang Q, Alshaker H, Böhler T, Srivats S, Chao Y, Cooper C, et al. Core shell lipid-polymer hybrid nanoparticles with combined docetaxel and molecular targeted therapy for the treatment of metastatic prostate cancer. Sci Rep. 2017;7:1–8. doi: 10.1038/s41598-017-06142-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen Y, Zhu X, Zhang X, Liu B, Huang L. Nanoparticles modified with tumor-targeting scFv deliver siRNA and miRNA for cancer therapy. Mol Ther. 2010;18:1650–6. doi: 10.1038/mt.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tang B, Peng Y, Yue Q, Pu Y, Li R, Zhao Y, et al. Design, preparation and evaluation of different branched biotin modified liposomes for targeting breast cancer. Eur J Med Chem. 2020 doi: 10.1016/j.ejmech.2020.112204. [DOI] [PubMed] [Google Scholar]
- 73.Li N, Xie X, Hu Y, He H, Fu X, Fang T, et al. Herceptin-conjugated liposomes co-loaded with doxorubicin and simvastatin in targeted prostate cancer therapy. Am J Transl Res. 2019;11:1255–1269. [PMC free article] [PubMed] [Google Scholar]
- 74.Rommasi F, Esfandiari N. Liposomal nanomedicine: applications for drug delivery in cancer therapy. Nanoscale Res Lett. 2021 doi: 10.1186/s11671-021-03553-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yang B, Song B, Shankar S, Guller A, Deng W. Recent advances in liposome formulations for breast cancer therapeutics. Cell Mol Life Sci. 2021;78:5225–43. doi: 10.1007/s00018-021-03850-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Qiu N, Ma Y, Zhao X, An L, Liu J, Li X. Application of liposome-based drug co-delivery system for the reversal of multidrug resistance in cancer treatment. J Nat Med Res. 2020;1:1–11. [Google Scholar]
- 77.Verma D, Gulati N, Kaul S, Mukherjee S, Nagaich U. Protein based nanostructures for drug delivery. J Pharm. 2018;2018:1–18. doi: 10.1155/2018/9285854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yaman S, Chintapula U, Rodriguez E, Ramachandramoorthy H, Nguyen KT. Cell-mediated and cell membrane-coated nanoparticles for drug delivery and cancer therapy. Cancer Drug Resist. 2020;3:879–911. doi: 10.20517/cdr.2020.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jacob J, Haponiuk JT, Thomas S, Gopi S. Biopolymer based nanomaterials in drug delivery systems: a review. Mater Today Chem. 2018;9:43–55. [Google Scholar]
- 80.Hao L, Zhou Q, Piao Y, Zhou Z, Tang J, Shen Y. Albumin-binding prodrugs via reversible iminoboronate forming nanoparticles for cancer drug delivery. J Control Release. 2021;330:362–71. doi: 10.1016/j.jconrel.2020.12.035. [DOI] [PubMed] [Google Scholar]
- 81.Rochani AK, Balasubramanian S, Girija AR, Maekawa T, Kaushal G, Sakthi KD. Heat shock protein 90 (Hsp90)-inhibitor-luminespib-loaded-protein-based nanoformulation for cancer therapy. Polymers. 2020 doi: 10.3390/polym12081798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mottaghitalab F, Kiani M, Farokhi M, Kundu SC, Reis RL, Gholami M, et al. Targeted delivery system based on gemcitabine-loaded silk fibroin nanoparticles for lung cancer therapy. ACS Appl Mater Interfaces. 2017;9:31600–31611. doi: 10.1021/acsami.7b10408. [DOI] [PubMed] [Google Scholar]
- 83.Sahoo N, Sahoo RK, Biswas N, Guha A, Kuotsu K. Recent advancement of gelatin nanoparticles in drug and vaccine delivery. Int J Biol Macromol. 2015;81:317–31. doi: 10.1016/j.ijbiomac.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 84.Pal K, Roy S, Parida PK, Dutta A, Bardhan S, Das S, et al. Folic acid conjugated curcumin loaded biopolymeric gum acacia microsphere for triple negative breast cancer therapy in invitro and invivo model. Mater Sci Eng C. 2019;95:204–16. doi: 10.1016/j.msec.2018.10.071. [DOI] [PubMed] [Google Scholar]
- 85.Pham DT, Saelim N, Tiyaboonchai W. Alpha mangostin loaded crosslinked silk fibroin-based nanoparticles for cancer chemotherapy. Colloids Surfaces B Biointerfaces. 2019;181:705–13. doi: 10.1016/j.colsurfb.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 86.Jithan A, Madhavi K, Madhavi M, Prabhakar K. Preparation and characterization of albumin nanoparticles encapsulating curcumin intended for the treatment of breast cancer. Int J Pharm Investig. 2011;1:119. doi: 10.4103/2230-973X.82432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Saleh T, Soudi T, Shojaosadati SA. Aptamer functionalized curcumin-loaded human serum albumin (HSA) nanoparticles for targeted delivery to HER-2 positive breast cancer cells. Int J Biol Macromol. 2019;130:109–16. doi: 10.1016/j.ijbiomac.2019.02.129. [DOI] [PubMed] [Google Scholar]
- 88.Mathew MS, Vinod K, Jayaram PS, Jayasree RS, Joseph K. Improved bioavailability of curcumin in gliadin-protected gold quantum cluster for targeted delivery. ACS Omega. 2019;4:14169–14178. doi: 10.1021/acsomega.9b00917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yadav HKS, Almokdad AA, Shaluf SIM, Debe MS. Polymer-based nanomaterials for drug-delivery carriers. Nanocarriers Drug Deliv. 2019 [Google Scholar]
- 90.Ghezzi M, Pescina S, Padula C, Santi P, Del Favero E, Cantù L, et al. Polymeric micelles in drug delivery: an insight of the techniques for their characterization and assessment in biorelevant conditions. J Control Release. 2021;332:312–36. doi: 10.1016/j.jconrel.2021.02.031. [DOI] [PubMed] [Google Scholar]
- 91.Kim TY, Kim DW, Chung JY, Shin SG, Kim SC, Heo DS, et al. Phase I and pharmacokinetic study of Genexol-PM, a Cremophor-free, polymeric micelle-formulated paclitaxel, in patients with advanced malignancies. Clin Cancer Res. 2004;10:3708–3716. doi: 10.1158/1078-0432.CCR-03-0655. [DOI] [PubMed] [Google Scholar]
- 92.Yadav S, Sharma AK, Kumar P. Nanoscale self-assembly for therapeutic delivery. Front Bioeng Biotechnol. 2020;8:1–24. doi: 10.3389/fbioe.2020.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang Z, Chen J, Little N, Lu J. Self-assembling prodrug nanotherapeutics for synergistic tumor targeted drug delivery. Acta Biomater. 2020;111:20–8. doi: 10.1016/j.actbio.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Varma LT, Singh N, Gorain B, Choudhury H, Tambuwala MM, Kesharwani P, et al. recent advances in self-assembled nanoparticles for drug delivery. Curr Drug Deliv. 2020;17:279–91. doi: 10.2174/1567201817666200210122340. [DOI] [PubMed] [Google Scholar]
- 95.Zhou J, Rao L, Yu G, Cook TR, Chen X, Huang F. Supramolecular cancer nanotheranostics. Chem Soc Rev. 2021;50:2839–91. doi: 10.1039/d0cs00011f. [DOI] [PubMed] [Google Scholar]
- 96.Kawakami K, Ebara M, Izawa H, Sanchez-Ballester NM, Hill JP, Ariga K. Supramolecular approaches for drug development. Curr Med Chem. 2012;19:2388–2398. doi: 10.2174/092986712800269254. [DOI] [PubMed] [Google Scholar]
- 97.Chen J, Zhang Y, Meng Z, Guo L, Yuan X, Zhang Y, et al. Supramolecular combination chemotherapy: a pH-responsive co-encapsulation drug delivery system. Chem Sci. 2020;11:6275–6282. doi: 10.1039/d0sc01756f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yu G, Yu W, Shao L, Zhang Z, Chi X, Mao Z, et al. Fabrication of a targeted drug delivery system from a pillar [5] arene-based supramolecular diblock copolymeric amphiphile for effective cancer therapy. Adv Funct Mater. 2016;26:8999–9008. [Google Scholar]
- 99.Von Hoff DD, Mita MM, Ramanathan RK, Weiss GJ, Mita AC, Lorusso PM, et al. Phase I study of PSMA-targeted docetaxel-containing nanoparticle BIND-014 in patients with advanced solid tumors. Clin Cancer Res. 2016;22:3157–3163. doi: 10.1158/1078-0432.CCR-15-2548. [DOI] [PubMed] [Google Scholar]
- 100.Mross K, Niemann B, Massing U, Drevs J, Unger C, Bhamra R, et al. Pharmacokinetics of liposomal doxorubicin (TLC-D99; Myocet) in patients with solid tumors: An open-label, single-dose study. Cancer Chemother Pharmacol. 2004;54:514–524. doi: 10.1007/s00280-004-0825-y. [DOI] [PubMed] [Google Scholar]
- 101.Yuan SY, Yuan Y, Shi X, Yuan CY. Improved drug delivery and anti-tumor efficacy of combinatorial liposomal formulation of genistein and plumbagin by targeting Glut1 and Akt3 proteins in mice bearing prostate tumor. Colloids Surfaces B Biointerfaces. 2020;190:110966. doi: 10.1016/j.colsurfb.2020.110966. [DOI] [PubMed] [Google Scholar]
- 102.Zhao D, Zhao X, Zu Y, Li J, Zhang Y, Jiang R, et al. Preparation, characterization, and in vitro targeted delivery of folate-decorated paclitaxel-loaded bovine serum albumin nanoparticles. Int J Nanomed. 2010;5:669–677. doi: 10.2147/ijn.s12918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sebak S, Mirzaei M, Malhotra M, Kulamarva A, Prakash S. Human serum albumin nanoparticles as an efficient noscapine drug delivery system for potential use in breast cancer: preparation and in vitro analysis. Int J Nanomed. 2010;5:525–532. doi: 10.2147/ijn.s10443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Langiu M, Dadparvar M, Kreuter J, Ruonala MO. Human serum albumin-based nanoparticle-mediated in vitro gene delivery. PLoS ONE. 2014;9:1–7. doi: 10.1371/journal.pone.0107603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Le TT, Kim D. Folate-PEG/Hyd-curcumin/C18-g-PSI micelles for site specific delivery of curcumin to colon cancer cells via Wnt/β-catenin signaling pathway. Mater Sci Eng C. 2019;101:464–71. doi: 10.1016/j.msec.2019.03.100. [DOI] [PubMed] [Google Scholar]
- 106.Zhang HY, Yong SC, Adu-Frimpong M, Nan YJ, Ming XX. Glutathione-sensitive PEGylated curcumin prodrug nanomicelles: preparation, characterization, cellular uptake and bioavailability evaluation. Int J Pharm. 2019;555:270–9. doi: 10.1016/j.ijpharm.2018.11.049. [DOI] [PubMed] [Google Scholar]
- 107.Andrade F, Rafael D, Vilar-Hernández M, Montero S, Martínez-Trucharte F, Seras-Franzoso J, et al. Polymeric micelles targeted against CD44v6 receptor increase niclosamide efficacy against colorectal cancer stem cells and reduce circulating tumor cells in vivo. J Control Release. 2021;331:198–212. doi: 10.1016/j.jconrel.2021.01.022. [DOI] [PubMed] [Google Scholar]
- 108.Sun S, Xiao QR, Wei J, Wei YY, Wang Y, Gao PC, et al. Bioinspired DNA self-assembly for targeted cancer cell imaging and drug delivery. Colloids Surfaces A Physicochem Eng Asp. 2020;585:124182. [Google Scholar]
- 109.Ding L, Li J, Wu C, Yan F, Li X, Zhang S. A self-assembled RNA-triple helix hydrogel drug delivery system targeting triple-negative breast cancer. J Mater Chem B. 2020;8:3527–33. doi: 10.1039/c9tb01610d. [DOI] [PubMed] [Google Scholar]
- 110.Hu Y, He Y, Ji J, Zheng S, Cheng Y. Tumor targeted curcumin delivery by folate-modified MPEG-PCL self-assembly micelles for colorectal cancer therapy. Int J Nanomed. 2020;15:1239–1252. doi: 10.2147/IJN.S232777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hong W, Guo F, Yu N, Ying S, Lou B, Wu J, et al. A novel folic acid receptor-targeted drug delivery system based on curcumin-loaded β-cyclodextrin nanoparticles for cancer treatment. Drug Des Devel Ther. 2021;15:2843–2855. doi: 10.2147/DDDT.S320119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mi P. Stimuli-responsive nanocarriers for drug delivery, tumor imaging, therapy and theranostics. Theranostics. 2020;10:4557–4588. doi: 10.7150/thno.38069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bruneau M, Bennici S, Brendle J, Dutournie P, Limousy L, Pluchon S. Systems for stimuli-controlled release: materials and applications. J Control Release. 2019;294:355–71. doi: 10.1016/j.jconrel.2018.12.038. [DOI] [PubMed] [Google Scholar]
- 114.Wei L, Chen J, Ding J. Sequentially stimuli-responsive anticancer nanomedicines. Nanomedicine. 2021;16:261–4. doi: 10.2217/nnm-2021-0019. [DOI] [PubMed] [Google Scholar]
- 115.Danhier F, Feron O, Préat V. To exploit the tumor microenvironment: passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J Control Release. 2010;148:135–46. doi: 10.1016/j.jconrel.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 116.Torchilin VP. Multifunctional, stimuli-sensitive nanoparticulate systems for drug delivery. Nat Rev Drug Discov. 2014;13:813–27. doi: 10.1038/nrd4333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hammond PT. Building biomedical materials layer-by-layer. Mater Today. 2012;15:196–206. [Google Scholar]
- 118.Webb BA, Chimenti M, Jacobson MP, Barber DL. Dysregulated pH: a perfect storm for cancer progression. Nat Rev Cancer. 2011;11:671–7. doi: 10.1038/nrc3110. [DOI] [PubMed] [Google Scholar]
- 119.Brown JM, Wilson WR. Exploiting tumour hypoxia in cancer treatment. Nat Rev Cancer. 2004;4:437–47. doi: 10.1038/nrc1367. [DOI] [PubMed] [Google Scholar]
- 120.de la Rica R, Aili D, Stevens MM. Enzyme-responsive nanoparticles for drug release and diagnostics. Adv Drug Deliv Rev. 2012;64:967–78. doi: 10.1016/j.addr.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 121.Raza A, Rasheed T, Nabeel F, Hayat U, Bilal M, Iqbal HMN. Endogenous and exogenous stimuli-responsive drug delivery systems for programmed site-specific release. Molecules. 2019;24:1–21. doi: 10.3390/molecules24061117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Warburg O. On the origin of cancer cells. Science. 1956;123:309–14. doi: 10.1126/science.123.3191.309. [DOI] [PubMed] [Google Scholar]
- 123.Gao W, Chan JM, Farokhzad OC. pH-responsive nanoparticles for drug delivery. Mol Pharm. 2010;7:1913–20. doi: 10.1021/mp100253e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Balamurali V, Pramodkuma TM, Srujana N, Venkatesh MP, Gupta NV, Krishna KL, et al. pH sensitive drug delivery systems: a review. Am J Drug Discov Dev. 2010;1:24–48. [Google Scholar]
- 125.Liu M, Du H, Zhang W, Zhai G. Internal stimuli-responsive nanocarriers for drug delivery: design strategies and applications. Mater Sci Eng C. 2017;71:1267–80. doi: 10.1016/j.msec.2016.11.030. [DOI] [PubMed] [Google Scholar]
- 126.Swietach P, Vaughan-Jones RD, Harris AL, Hulikova A. The chemistry, physiology and pathology of pH in cancer. Philos Trans R Soc B Biol Sci. 2014 doi: 10.1098/rstb.2013.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Tang H, Zhao W, Yu J, Li Y, Zhao C. Recent development of pH-responsive polymers for cancer nanomedicine. Molecules. 2019 doi: 10.3390/molecules24010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Woraphatphadung T, Sajomsang W, Rojanarata T, Ngawhirunpat T, Tonglairoum P, Opanasopit P. Development of chitosan-based pH-sensitive polymeric micelles containing curcumin for colon-targeted drug delivery. AAPS PharmSciTech. 2018;19:991–1000. doi: 10.1208/s12249-017-0906-y. [DOI] [PubMed] [Google Scholar]
- 129.Guo S, Qiu L, Chen Y, Wang X, Ma B, Qu C, et al. TMEM16A-inhibitor loaded pH-responsive nanoparticles: a novel dual-targeting antitumor therapy for lung adenocarcinoma. Biochem Pharmacol. 2020;178:114062. doi: 10.1016/j.bcp.2020.114062. [DOI] [PubMed] [Google Scholar]
- 130.Song J, Xu B, Yao H, Lu X, Tan Y, Wang B, et al. Schiff-linked PEGylated doxorubicin prodrug forming pH-responsive nanoparticles with high drug loading and effective anticancer therapy. Front Oncol. 2021;11:1–10. doi: 10.3389/fonc.2021.656717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chen Z, Li Z, Lin Y, Yin M, Ren J, Qu X. Biomineralization inspired surface engineering of nanocarriers for pH-responsive, targeted drug delivery. Biomaterials. 2013;34:1364–71. doi: 10.1016/j.biomaterials.2012.10.060. [DOI] [PubMed] [Google Scholar]
- 132.Zheng P, Liu Y, Chen J, Xu W, Li G, Ding J. Targeted pH-responsive polyion complex micelle for controlled intracellular drug delivery. Chinese Chem Lett. 2020;31:1178–82. [Google Scholar]
- 133.Zhang Y, Xing Y, Xian M, Shuang S, Dong C. Folate-targeting and bovine serum albumin-gated mesoporous silica nanoparticles as a redox-responsive carrier for epirubicin release. New J Chem. 2019;43:2694–701. [Google Scholar]
- 134.Xiao D, Jia HZ, Zhang J, Liu CW, Zhuo RX, Zhang XZ. A dual-responsive mesoporous silica nanoparticle for tumor-triggered targeting drug delivery. Small. 2014;10:591–598. doi: 10.1002/smll.201301926. [DOI] [PubMed] [Google Scholar]
- 135.Chi Y, Yin X, Sun K, Feng S, Liu J, Chen D, et al. Redox-sensitive and hyaluronic acid functionalized liposomes for cytoplasmic drug delivery to osteosarcoma in animal models. J Control Release. 2017;261:113–25. doi: 10.1016/j.jconrel.2017.06.027. [DOI] [PubMed] [Google Scholar]
- 136.Yin X, Chi Y, Guo C, Feng S, Liu J, Sun K, et al. Chitooligosaccharides modified reduction-sensitive liposomes: enhanced cytoplasmic drug delivery and osteosarcomas-tumor inhibition in animal models. Pharm Res. 2017;34:2172–2184. doi: 10.1007/s11095-017-2225-0. [DOI] [PubMed] [Google Scholar]
- 137.Movassaghian S, Merkel OM, Torchilin VP. Applications of polymer micelles for imaging and drug delivery. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2015;7:691–707. doi: 10.1002/wnan.1332. [DOI] [PubMed] [Google Scholar]
- 138.Sun C, Li X, Du X, Wang T. Redox-responsive micelles for triggered drug delivery and effective laryngopharyngeal cancer therapy. Int J Biol Macromol. 2018;112:65–73. doi: 10.1016/j.ijbiomac.2018.01.136. [DOI] [PubMed] [Google Scholar]
- 139.Kang Y, Lu L, Lan J, Ding Y, Yang J, Zhang Y, et al. Redox-responsive polymeric micelles formed by conjugating gambogic acid with bioreducible poly(amido amine)s for the co-delivery of docetaxel and MMP-9 shRNA. Acta Biomater. 2018;68:137–153. doi: 10.1016/j.actbio.2017.12.028. [DOI] [PubMed] [Google Scholar]
- 140.Gisbert-garzar M. Redox-responsive mesoporous silica nanoparticles for cancer treatment: recent updates. Nanomaterials. 2021 doi: 10.3390/nano11092222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Yan H, Dong J, Huang X, Du X. Protein-gated upconversion nanoparticle-embedded mesoporous silica nanovehicles via diselenide linkages for drug release tracking in real time and tumor chemotherapy. ACS Appl Mater Interfaces. 2021;13:29070–29082. doi: 10.1021/acsami.1c04447. [DOI] [PubMed] [Google Scholar]
- 142.Lei B, Wang M, Jiang Z, Qi W, Su R, He Z. Constructing redox-responsive metal-organic framework nanocarriers for anticancer drug delivery. ACS Appl Mater Interfaces. 2018;10:16698–706. doi: 10.1021/acsami.7b19693. [DOI] [PubMed] [Google Scholar]
- 143.Andresen TL, Thompson DH, Kaasgaard T. Enzyme-triggered nanomedicine: drug release strategies in cancer therapy (invited review) Mol Membr Biol. 2010;27:353–363. doi: 10.3109/09687688.2010.515950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.McAtee CO, Barycki JJ, Simpson MA. Emerging roles for hyaluronidase in cancer metastasis and therapy. 2014. pp. 1–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lafleur MA, Drew AF, de Sousa EL, Blick T, Bills M, Walker EC, et al. Upregulation of matrix metalloproteinases (MMPs) in breast cancer xenografts: a major induction of stromal MMP-13. Int J Cancer. 2005;114:544–54. doi: 10.1002/ijc.20763. [DOI] [PubMed] [Google Scholar]
- 146.Cai D, Han C, Liu C, Ma X, Qian J, Zhou J, et al. Chitosan-capped enzyme-responsive hollow mesoporous silica nanoplatforms for colon-specific drug delivery. Nanoscale Res Lett. 2020 doi: 10.1186/s11671-020-03351-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Keith B, Simon MC. Hypoxia-inducible factors, stem cells, and cancer. Cell. 2007;129:465–72. doi: 10.1016/j.cell.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Liu Y, Jiang Y, Zhang M, Tang Z, He M, Bu W. Modulating hypoxia via nanomaterials chemistry for efficient treatment of solid tumors. Acc Chem Res. 2018;51:2502–11. doi: 10.1021/acs.accounts.8b00214. [DOI] [PubMed] [Google Scholar]
- 149.Im S, Lee J, Park D, Park A, Kim Y-M, Kim WJ. Hypoxia-triggered transforming immunomodulator for cancer immunotherapy via photodynamically enhanced antigen presentation of dendritic cell. ACS Nano. 2019;13:476–88. doi: 10.1021/acsnano.8b07045. [DOI] [PubMed] [Google Scholar]
- 150.Liu H-M, Zhang Y-F, Xie Y-D, Cai Y-F, Li B-Y, Li W, et al. Hypoxia-responsive ionizable liposome delivery siRNA for glioma therapy. Int J Nanomed. 2017;12:1065–83. doi: 10.2147/IJN.S125286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Poon Z, Chang D, Zhao X, Hammond PT. Layer-by-layer nanoparticles with a pH-sheddable layer for in vivo targeting of tumor hypoxia. ACS Nano. 2011;5:4284–92. doi: 10.1021/nn200876f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhen J, Tian S, Liu Q, Zheng C, Zhang Z, Ding Y, et al. Nanocarriers responsive to a hypoxia gradient facilitate enhanced tumor penetration and improved anti-tumor efficacy. Biomater Sci. 2019;7:2986–95. doi: 10.1039/c9bm00461k. [DOI] [PubMed] [Google Scholar]
- 153.Qian C, Feng P, Yu J, Chen Y, Hu Q, Sun W, et al. Anaerobe-inspired anticancer nanovesicles. Angew Chemie. 2017;129:2632–7. doi: 10.1002/anie.201611783. [DOI] [PubMed] [Google Scholar]
- 154.Kulkarni P, Haldar MK, Karandish F, Confeld M, Hossain R, Borowicz P, et al. Tissue-penetrating, hypoxia-responsive echogenic polymersomes for drug delivery to solid tumors. Chem A Eur J. 2018;24:12490–4. doi: 10.1002/chem.201802229. [DOI] [PubMed] [Google Scholar]
- 155.Yang G, Phua SZF, Lim WQ, Zhang R, Feng L, Liu G, et al. A hypoxia-responsive albumin-based nanosystem for deep tumor penetration and excellent therapeutic efficacy. Adv Mater. 2019;31:1901513. doi: 10.1002/adma.201901513. [DOI] [PubMed] [Google Scholar]
- 156.Fruehauf KR, Kim TI, Nelson EL, Patterson JP, Wang S-W, Shea KJ. Metabolite responsive nanoparticle-protein complex. Biomacromolecules. 2019;20:2703–12. doi: 10.1021/acs.biomac.9b00470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Pasparakis G, Tsitsilianis C. LCST polymers: thermoresponsive nanostructured assemblies towards bioapplications. Polymer. 2020;211:123146. [Google Scholar]
- 158.Castillo-Henríquez L, Castro-Alpízar J, Lopretti-Correa M, Vega-Baudrit J. Exploration of bioengineered scaffolds composed of thermo-responsive polymers for drug delivery in wound healing. Int J Mol Sci. 2021;22:1–25. doi: 10.3390/ijms22031408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hogan KJ, Mikos AG. Biodegradable thermoresponsive polymers: applications in drug delivery and tissue engineering. Polymer. 2020;211:123063. [Google Scholar]
- 160.Tipa C, Cidade MT, Vieira T, Silva JC, Soares PIP, Borges JP. A new long-term composite drug delivery system based on thermo-responsive hydrogel and nanoclay. Nanomaterials. 2021;11:1–22. doi: 10.3390/nano11010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ahsan A, Farooq MA, Parveen A. Thermosensitive chitosan-based injectable hydrogel as an efficient anticancer drug carrier. ACS Omega. 2020;5:20450–20460. doi: 10.1021/acsomega.0c02548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kazempour M, Edjlali L, Akbarzadeh A, Davaran S, Farid SS. Synthesis and characterization of dual pH-and thermo-responsive graphene-based nanocarrier for effective anticancer drug delivery. J Drug Deliv Sci Technol. 2019;54:101158. [Google Scholar]
- 163.Farjadian F, Ghasemi S, Andami Z, Tamami B. Thermo-responsive nanocarrier based on poly(N-isopropylacrylamide) serving as a smart doxorubicin delivery system. Iran Polym J. 2020;29:197–207. [Google Scholar]
- 164.Mirrahimi M, Abed Z, Beik J, Shiri I, Shiralizadeh Dezfuli A, Mahabadi VP, et al. A thermo-responsive alginate nanogel platform co-loaded with gold nanoparticles and cisplatin for combined cancer chemo-photothermal therapy. Pharmacol Res. 2019;143:178–85. doi: 10.1016/j.phrs.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 165.Yan L, Li X. Biodegradable stimuli-responsive polymeric micelles for treatment of malignancy. Curr Pharm Biotechnol. 2016;17:227–236. doi: 10.2174/138920101703160206142821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Nomoto T, Fukushima S, Kumagai M, Machitani K, Arnida Y, Matsumoto Y, et al. Three-layered polyplex micelle as a multifunctional nanocarrier platform for light-induced systemic gene transfer. Nat Commun. 2014 doi: 10.1038/ncomms4545. [DOI] [PubMed] [Google Scholar]
- 167.Yen HC, Cabral H, Mi P, Toh K, Matsumoto Y, Liu X, et al. Light-induced cytosolic activation of reduction-sensitive camptothecin-loaded polymeric micelles for spatiotemporally controlled in vivo chemotherapy. ACS Nano. 2014;8:11591–11602. doi: 10.1021/nn504836s. [DOI] [PubMed] [Google Scholar]
- 168.Luo D, Carter KA, Razi A, Geng J, Shao S, Giraldo D, et al. Doxorubicin encapsulated in stealth liposomes conferred with light-triggered drug release. Biomaterials. 2016;75:193–202. doi: 10.1016/j.biomaterials.2015.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Khatun Z, Nurunnabi M, Nafiujjaman M, Reeck GR, Khan HA, Cho KJ, et al. A hyaluronic acid nanogel for photo-chemo theranostics of lung cancer with simultaneous light-responsive controlled release of doxorubicin. Nanoscale. 2015;7:10680–10689. doi: 10.1039/c5nr01075f. [DOI] [PubMed] [Google Scholar]
- 170.Yang G, Sun X, Liu J, Feng L, Liu Z. Light-responsive, singlet-oxygen-triggered on-demand drug release from photosensitizer-doped mesoporous silica nanorods for cancer combination therapy. Adv Funct Mater. 2016;26:4722–4732. [Google Scholar]
- 171.Tong R, Chiang HH, Kohane DS. Photoswitchable nanoparticles for in vivo cancer chemotherapy. Proc Natl Acad Sci USA. 2013;110:19048–19053. doi: 10.1073/pnas.1315336110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Timko BP, Arruebo M, Shankarappa SA, McAlvin JB, Okonkwo OS, Mizrahi B, et al. Near-infrared-actuated devices for remotely controlled drug delivery. Proc Natl Acad Sci USA. 2014;111:1349–1354. doi: 10.1073/pnas.1322651111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Fan J, Zhang Z, Wang Y, Lin S, Yang S. Photo-responsive degradable hollow mesoporous organosilica nanoplatforms for drug delivery. J Nanobiotechnol. 2020;18:1–14. doi: 10.1186/s12951-020-00642-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chen W-T, Kang S-T, Lin J-L, Wang C-H, Chen R-C, Yeh C-K. Targeted tumor theranostics using folate-conjugated and camptothecin-loaded acoustic nanodroplets in a mouse xenograft model. Biomaterials. 2015;53:699–708. doi: 10.1016/j.biomaterials.2015.02.122. [DOI] [PubMed] [Google Scholar]
- 175.Li C, Zhang Y, Li Z, Mei E, Lin J, Li F, et al. Light-responsive biodegradable nanorattles for cancer theranostics. Adv Mater. 2018;30:1706150. doi: 10.1002/adma.201706150. [DOI] [PubMed] [Google Scholar]
- 176.Wang X, Niu D, Li P, Wu Q, Bo X, Liu B, et al. Dual-enzyme-loaded multifunctional hybrid nanogel system for pathological responsive ultrasound imaging and T 2 -weighted magnetic resonance imaging. ACS Nano. 2015;9:5646–56. doi: 10.1021/nn5068094. [DOI] [PubMed] [Google Scholar]
- 177.Carson AR, McTiernan CF, Lavery L, Grata M, Leng X, Wang J, et al. Ultrasound-targeted microbubble destruction to deliver siRNA cancer therapy. Cancer Res. 2012;72:6191–9. doi: 10.1158/0008-5472.CAN-11-4079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cabral H, Matsumoto Y, Mizuno K, Chen Q, Murakami M, Kimura M, et al. Accumulation of sub-100 nm polymeric micelles in poorly permeable tumours depends on size. Nat Nanotechnol. 2011;6:815–23. doi: 10.1038/nnano.2011.166. [DOI] [PubMed] [Google Scholar]
- 179.Vandenbroucke RE, Lentacker I, Demeester J, De Smedt SC, Sanders NN. Ultrasound assisted siRNA delivery using PEG-siPlex loaded microbubbles. J Control Release. 2008;126:265–73. doi: 10.1016/j.jconrel.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 180.Wang Z, He Q, Zhao W, Luo J, Gao W. Tumor-homing, pH- and ultrasound-responsive polypeptide-doxorubicin nanoconjugates overcome doxorubicin resistance in cancer therapy. J Control Release. 2017;264:66–75. doi: 10.1016/j.jconrel.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 181.Attia MF, Anton N, Wallyn J, Omran Z, Vandamme TF. An overview of active and passive targeting strategies to improve the nanocarriers efficiency to tumour sites. J Pharm Pharmacol. 2019;71:1185–1198. doi: 10.1111/jphp.13098. [DOI] [PubMed] [Google Scholar]
- 182.Hossen S, Hossain MK, Basher MK, Mia MNH, Rahman MT, Uddin MJ. Smart nanocarrier-based drug delivery systems for cancer therapy and toxicity studies: a review. J Adv Res. 2019;15:1–18. doi: 10.1016/j.jare.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Carita AC, Eloy JO, Chorilli M, Lee RJ, Leonardi GR. Recent advances and perspectives in liposomes for cutaneous drug delivery. Curr Med Chem. 2017;25:606–635. doi: 10.2174/0929867324666171009120154. [DOI] [PubMed] [Google Scholar]
- 184.Qiang H, Li J, Wang S, Feng T, Cai H, Liu Z, et al. Distribution of systemically administered nanoparticles during acute pancreatitis: effects of particle size and disease severity. Pharmazie. 2021;76:180–188. doi: 10.1691/ph.2021.0156. [DOI] [PubMed] [Google Scholar]
- 185.Onzi G, Guterres SS, Pohlmann AR, Frank LA. Passive targeting and the enhanced permeability and retention (EPR) effect. ADME Encycl. Cham: Springer International Publishing; 2021. pp. 1–13. [Google Scholar]
- 186.Barenholz Y. Doxil®—The first FDA-approved nano-drug: lessons learned. J Control Release. 2012;160:117–34. doi: 10.1016/j.jconrel.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 187.Hamishehkar H, Bahadori MB, Vandghanooni S, Eskandani M, Nakhlband A, Eskandani M. Preparation, characterization and anti-proliferative effects of sclareol-loaded solid lipid nanoparticles on A549 human lung epithelial cancer cells. J Drug Deliv Sci Technol. 2018;45:272–80. [Google Scholar]
- 188.Dhule SS, Penfornis P, Frazier T, Walker R, Feldman J, Tan G, et al. Curcumin-loaded γ-cyclodextrin liposomal nanoparticles as delivery vehicles for osteosarcoma. Nanomed Nanotechnol Biol Med. 2012;8:440–51. doi: 10.1016/j.nano.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Clemente N, Ferrara B, Gigliotti C, Boggio E, Capucchio M, Biasibetti E, et al. Solid lipid nanoparticles carrying temozolomide for melanoma treatment. Preliminary in vitro and in vivo studies. Int J Mol Sci. 2018;19:255. doi: 10.3390/ijms19020255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Patel JK, Patel AP, Pathak YV. Passive targeting of nanoparticles to cancer BT—surface modification of nanoparticles for targeted drug delivery. Cham: Springer International Publishing; 2019. pp. 125–43. [Google Scholar]
- 191.Chithrani BD, Ghazani AA, Chan WCW. Determining the size and shape dependence of gold nanoparticle uptake into mammalian cells. Nano Lett. 2006;6:662–668. doi: 10.1021/nl052396o. [DOI] [PubMed] [Google Scholar]
- 192.Tang F, Li L, Chen D. Mesoporous silica nanoparticles: synthesis, biocompatibility and drug delivery. Adv Mater. 2012;24:1504–1534. doi: 10.1002/adma.201104763. [DOI] [PubMed] [Google Scholar]
- 193.Gradishar WJ, Tjulandin S, Davidson N, Shaw H, Desai N, Bhar P, et al. Phase III trial of nanoparticle albumin-bound paclitaxel compared with polyethylated castor oil-based paclitaxel in women with breast cancer. J Clin Oncol. 2005;23:7794–803. doi: 10.1200/JCO.2005.04.937. [DOI] [PubMed] [Google Scholar]
- 194.Sriraman SK, Aryasomayajula B, Torchilin VP. Barriers to drug delivery in solid tumors. Tissue Barriers. 2014;2:e29528-1–10. doi: 10.4161/tisb.29528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Ahmad A, Khan F, Mishra RK, Khan R. Precision cancer nanotherapy: evolving role of multifunctional nanoparticles for cancer active targeting. J Med Chem. 2019;62:10475–10496. doi: 10.1021/acs.jmedchem.9b00511. [DOI] [PubMed] [Google Scholar]
- 196.Bartlett DW, Su H, Hildebrandt IJ, Weber WA, Davis ME. Impact of tumor-specific targeting on the biodistribution and efficacy of siRNA nanoparticles measured by multimodality in vivo imaging. Proc Natl Acad Sci USA. 2007;104:15549–15554. doi: 10.1073/pnas.0707461104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Hobbs SK, Monsky WL, Yuan F, Roberts WG, Griffith L, Torchilin VP, et al. Regulation of transport pathways in tumor vessels: role of tumor type and microenvironment. Proc Natl Acad Sci. 1998;95:4607–12. doi: 10.1073/pnas.95.8.4607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature. 2000;407:249–57. doi: 10.1038/35025220. [DOI] [PubMed] [Google Scholar]
- 199.Rosenblum D, Joshi N, Tao W, Karp JM, Peer D. Progress and challenges towards targeted delivery of cancer therapeutics. Nat Commun. 2018;9:1410. doi: 10.1038/s41467-018-03705-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Zhao X, Bai J, Yang W. Stimuli-responsive nanocarriers for therapeutic applications in cancer. Cancer Biol Med. 2021;18:319–35. doi: 10.20892/j.issn.2095-3941.2020.0496. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.