Abstract
Background
Arthropod-borne viruses (arboviruses) impose a major health and economic burden on human populations globally, with mosquitoes serving as important vectors. Measuring the ability of a mosquito population to transmit an arbovirus is important in terms of evaluating its public health risk. In the laboratory, a variety of methods are used to estimate arboviral transmission by mosquitoes, including indirect methods involving viral detection from mosquito saliva collected by forced salivation. The accuracy of indirect methods to estimate arbovirus transmission to live animal hosts has not been fully evaluated.
Methods
We compared three commonly used proxies of arboviral transmission, namely, the presence of virus in mosquito legs, in salivary glands (SG) and in saliva collected in capillary tubes using forced salivation, with direct transmission estimates from mosquitoes to suckling mice. We analyzed five vector-virus combinations, including Aedes aegypti infected with chikungunya virus, West Nile virus and Zika virus; Culex quinquefasciatus infected with West Nile virus; and Aedes triseriatus infected with La Crosse virus.
Results
Comparatively, the methods of detecting virus infection in mosquito legs and in SG were equally accurate in predicting transmission. Overall, the presence of virus in mosquito legs was a more accurate predictor of transmission than the commonly implemented viral detection method using forced salivation into a capillary tube, and was subject to less technical variation.
Conclusions
These results suggest that, in general, forced salivation methods tend to underestimate virus transmission, and they provide confidence in the use of mosquito leg screens to evaluate the transmission potential of a mosquito population.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s13071-022-05198-7.
Keywords: Arbovirus, Transmission, Vector, Proxy, Saliva
Background
Arthropod-borne viruses (arboviruses) impose a major public health burden on affected populations and are on the rise in both tropical and temperate regions of the world. In recent decades, chikungunya virus (CHIKV), West Nile virus (WNV) and Zika virus (ZIKV) have spread to new geographic regions, driving research on the vector competence of local mosquito populations for these and other invasive arboviruses. Vector competence is defined as the ability of an arthropod to acquire, maintain and transmit the pathogen to a vertebrate host during the blood-feeding process. In the laboratory, a variety of methods are used to estimate arboviral transmission by a mosquito vector. Direct in vivo methods involve exposing laboratory animals to infected vectors, which allows mosquitoes to engage in the natural blood-feeding process that is required for arbovirus transmission. However, in vivo methods are rarely used today due to high costs, requirements for personnel training, appropriate husbandry and containment facilities and animal permits [1]. Furthermore, the use of vertebrate hosts for these studies is limited to the availability of competent animal models for the arbovirus under study [1]. More frequently, transmission is estimated by indirect in vitro methods, which are more accessible and cost-effective but can be labor-intensive. Among the in vitro methods in current use, the capillary method of forced salivation is the most widely used assay, involving imobilization of individual mosquitoes and subsequent harvesting of their saliva for arboviral testing by inserting their proboscis in a finely drawn capillary tube or pipette tip. Another approach is to simply screen the peripheral tissues (legs, salivary glands [SG] and/or head tissue) for arbovirus infection with the underlying assumption that these measures of disseminated infection are equivalent to virus transmission [2–4].
The complexity involved in the experimental design of vector competence trials complicates comparisons across studies [5]. Nevertheless, it is worth noting that these studies often report sharp declines in the percentage of mosquitoes transmitting virus after developing a disseminated virus infection [6–9]. This could imply either a strong SG infection or an escape barrier in these vectors [10], or perhaps this is an artifact of the techniques used to assess arbovirus transmission. For example, Aedes aegypti and Aedes albopictus often demonstrate poor vector competence for CHIKV, DENV, and ZIKV in the laboratory, even though they are known to serve as efficient vectors for these arboviruses in nature [5, 11, 12]. These studies have relied on forced salivation techniques to demonstrate virus transmission, which does not allow mosquitoes to probe or feed naturally.
The indirect methods used to estimate arbovirus transmission by mosquitoes have not been fully validated, despite their widespread use in vector competence studies. In a study by Styer et al. [13], mosquitoes were found to deliver approximately 600-fold more WNV after probing on mice than recovered by a forced salivation technique (the capillary method), suggesting that some methods may underestimate arbovirus transmission to live animal hosts. Accordingly, to explore this possibility further, we compared three commonly used proxies of arboviral transmission (indirect methods), namely, the presence of virus in legs, SG and saliva, with direct transmission estimates from mosquitoes to suckling mice (“true transmission rate”) to determine the most informative and efficient proxy for arbovirus transmission in five vector–virus combinations.
Methods
Mosquito species
Mosquitoes were reared from eggs in plastic trays, and larvae were fed as needed with either TetraMin® tropical flakes (Tetra GmbH, Melle, Germany) or a 2% solution of 3:2 liver powder and brewer's yeast mix. Adults were kept in 30 × 30 × 30-cm cages and provided with a 10% sucrose solution ad libidum on a cotton ball. The Ae. aegypti Orlando (ORL) colony was obtained from the Agricultural Research Service of the US Department of Agriculture (USDA ARS, Gainesville, FL, USA), originally derived from field-collected mosquitoes from Orlando Florida in 1952 (Gloria-Soria et al. [14]). The Aedes triseriatus colony originated from mosquitoes collected in Waterford, CT (USA) in 1992. The Culex quinquefasciatus colony was established from mosquitoes originally purchased from Benzon Research Inc. (Carlisle, PA, USA) and is believed to have originally been derived from mosquitoes in northern Florida.
Virus strains
CHIKV LR2006-OPY1 (GenBank accession no. KT449801.1) was obtained from the World Reference Center for Arboviruses at the University of Texas Medical Branch, Galveston, TX (USA). This strain was originally isolated from serum of a patient returning from La Réunion Island in 2006, and passed five times on Vero cell culture, once in suckling mice and once in C6/36 cells. WNV 2741-99 was isolated from Culex pipiens collected in Greenwich, CT (USA) in 1999 and was passaged 4 times on Vero cells. ZIKV MR766 (GenBank accession no. MW143022.1) was obtained from The Arbovirus Reference Collection from the Centers of Disease Control (Fort Collins, CO, USA). This strain was originally isolated from a sentinel rhesus monkey in 1947 at Zika Forest, Entebbe, Uganda, and repeatedly passed in mice, twice on Vero cell culture and once on C6/36 cell culture. La Crosse virus (LACV) 78V-8853 strain was isolated in 1978 from an Ae. triseriatus mosquito from Rochester, MN (USA) and passaged once on Vero cells, twice on suckling mice and twice more on Vero cells.
Experimental infections
Intrathoracic inoculation
Female mosquitoes aged 6 to 10 days were inoculated intrathoracically with 69 nl of a virus solution prepared from a frozen viral stock to contain approximately 17 plaque-forming units (PFU) of the virus. Females were incubated at 28 °C and a 14:10 (light:dark) cycle, with free access to a 10% sugar solution from a cotton ball, for the extrinsic incubation period (EIP) described in Table 1.
Table 1.
Details of the intrathoracic inoculation experiment
| Mosquito species | Virus | Virus strain | PFU | EIP (days) | IIP (days) | References |
|---|---|---|---|---|---|---|
| Aedes aegypti [ORL] | CHIKV | L006-OPY1 | 17.2 | 6 | 3 | [15, 34–36] |
| Aedes aegypti [ORL] | ZIKV | MR766 | 17 | 10 | 6 | [16, 36–38] |
| Aedes aegypti [ORL] | WNV | 2741-99 | 16.8 | 10 | 6 | [19, 37, 38] |
| Culex quinquefasciatus | WNV | 2741-99 | 16.8 | 7 and 10 | 6 | [19, 37, 38] |
| Aedes triseriatus | LACV | 78V-8853 | 18.1 | 7 | 3 | [18] |
EIP, Extrinsic incubation period (days of mosquito incubation post-infection); IIP, intrinsic incubation period (days of suckling mice incubation post-infection); for other abbreviations, see Abbreviations section
Oral infections
Female mosquitoes aged 6 to 10 days were sorted into meshed pint cups and deprived of sugar 24 h prior to the experiment. On the day of the experiment, mosquitoes were offered an infectious blood meal consisting of a 1:1 mix of freshly grown virus culture and defibrinated sheep’s blood (HemoStat Labs, Dixon, CA, USA). The viral culture was obtained by inoculating a confluent monolayer of Ae. albopictus C6/36 cells into a T25 flask containing 100 ul of CHIKV stock virus, followed by a 3-day incubation; the culture was harvested on the day of the experiment to prepare the mix. The blood meal was warmed at 37 °C for 45 min in an artificial membrane system lined with hog sausage casing. Fully engorged mosquitoes were retained and incubated for 12 and 15 days at 28 °C under a 14:10 (light:dark) cycle, with free access to a 10% sugar solution provided on a cotton ball.
Transmission estimates
Immunocompetent suckling mice have been shown to develop systemic infection and viremia upon exposure to CHIKV [15], ZIKV [16, 17], LACV [18] and WNV [19]. In this study we used infection developed in post-exposure suckling mice as the “true arbovirus transmission rate” and compared this rate to transmission estimates based on mosquito tissue/saliva proxies. Litters of suckling mice (mixed sex) from pregnant CD-1 mice were obtained from the Charles River Laboratories (Wilmington, MA, USA). Procedures for handling and care of animals were approved by and performed under the Animal Care and Use Committee at The Connecticut Agricultural Experiment Station (protocol no. P28-17). Suckling mice were tattooed to track individual mice from each litter. Individual mosquitoes were randomly assigned to individual suckling mice after the corresponding EIP had elapsed (Table 1). Each mosquito was allowed to feed on a restrained mouse placed on top of a screened cage at 28 °C. Following feeding, the legs and wings of engorged mosquitoes were removed. Saliva was collected from mosquitoes by inserting their proboscis into P20 microcapillary gel-loading tips containing 5 ul of a 1:1 solution of 50% sucrose:fetal bovine serum for 1 h at room temperature. The tip contents were expelled into a tube with 50 ul of PBS-G (phosphate-buffered saline, 30% heat-inactivated rabbit serum, 0.5% gelatin). It should be noted that Miller et al. [20] have recently demonstrated that blood-feeding immediately prior to forced salivation does not affect arbovirus expectoration. SG were dissected. Abdomens, legs and SG were independently homogenized in 200 µl of PBS-G in a 2-ml microcentrifuge tube using Copperhead copper beads (Crosman Corp., Boomfield, NY, USA) and a Mixer Mill 400 (Retsch GmbH, Haan, Germany) for 30–60 s at 24 Hz. All samples were stored at − 80 °C until RNA extraction.
Mice were kept in a Thoren cage rack system (Thoren Caging Systems Inc., Hazleton, PA, USA) with HEPA filtration under a 12:12 (light:dark) cycle and observed daily until they displayed illness symptoms or for a maximum number of days after exposure, corresponding to the intrinsic incubation period (IIP) reported in Table 1. At that point, mice were euthanized, and one hind limb and brain tissue were collected, homogenized in 500 µl of PBS-G (as described above) and stored at − 80 °C until RNA extraction.
Mosquito viral dissemination after IT injection was confirmed by testing the mosquito legs via real-time PCR (RT-PCR). Infection by oral feeding was confirmed by testing the mosquito abdomen by the same method. The ability of the mosquito to achieve viral transmission was assessed via four parameters: (i) detection of virus in mosquito legs; (ii) detection of virus in mosquito SG; (iii) detection of virus in mosquito saliva; and (iv) development of systemic infection of exposed suckling mice.
Virus detection
We maximized our ability to detect the presence of arboviruses in the samples by screening for RNA viral copies via RT-PCR. This detection method is more sensitive than quantifying infectious particles via plaque assay because for every arboviral infectious particle there are at least 102–104 more RNA viral particles [20–22].
RNA was extracted from 50 ul of the homogenized tissue and saliva solution using the KingFisher™ Flex Purification System (Thermo Fisher Scientific, Waltham, MA, USA) with the Mag-Bind ® Viral DNA/RNA Kit (Omega Bio-Tek, Norcross, GA, USA) and eluted in a final volume of 50 µl of 1/10X TE buffer (Tris–EDTA). A 2-μl aliquot of this eluate was then used in each 10 µl RT-PCR reaction. Presence of virus was determined in duplicate with the I-Taq™ Universal probes 1-Step-Kit (BioRad Laboratories, Hercules, CA, USA), using primers and probes described in Additional file 1: Table S1. Samples were only thawed once. Results were analyzed with the BioRad CFX Maestro™ Software for Mac 1.1. v.4.1.2 (BioRad Laboratories) using a baseline of 100. A mosquito was considered infected if viral RNA was detected in the abdomen and considered to have a disseminated infection if the legs were positive. A cycle threshold (Ct) cut-off value < 37 was used in the RT-PCR assays to consider a sample positive for WNV, LACV and ZIKV, and a Ct value < 35 was used for CHIKV; these cut-off values were based on the detection limit of our assay, established from standard curves (Additional file 1: Supplementary information; Fig. S1; Table S2).
Statistical analyses
Proportions of positive samples were compared using a Fisher exact test [23] applying the Holm correction for multiple testing [24], as implemented by the prop.fisher.test() function in the fmsb v.0.7.1 package [25] from R v. 4.0.3. [26]. Graphs were generated in R v. 4.0.3. [26] and 95% binomial confidence intervals for each proportion were calculated with the prop.test() function available in the software core stats package. A Welch two-sample t-test was used to compare the accuracy of legs and saliva to predict transmission.
Results
Evaluation of transmission proxies in mosquitoes with disseminated infections
We examined the accuracy of salivary glands and saliva as proxies for arboviral transmission in multiple mosquito-virus pairings using mosquitoes infected by intrathoracic (IT) inoculation. This approach was utilized to ensure viral dissemination at the time of the transmission assay. After the corresponding EIP elapsed (Table 1), mosquitoes were allowed to feed on suckling mice, and the presence of arbovirus in legs, salivary glands and saliva was determined. The presence of virus in legs was used to confirm dissemination. The “true transmission rate” was based on the percentage of suckling mice that developed infection within the IIP, and the accuracy of each transmission proxy was determined by comparing this value to the proportion of positive samples derived from SG and saliva.
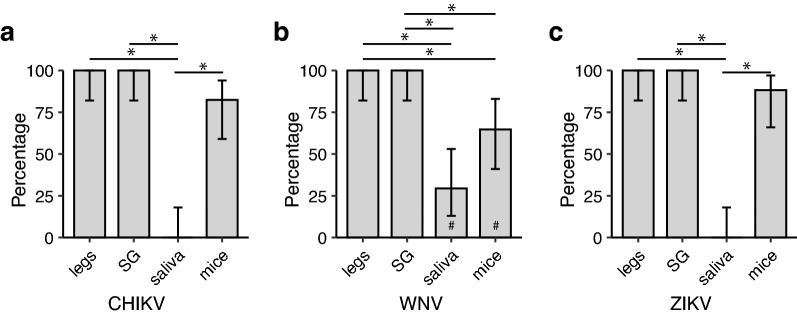
We first estimated transmission of three arboviruses (CHIKV, ZIKV, and WNV) by Ae. aegypti. All mosquito legs tested were positive for the corresponding injected virus, confirming dissemination (Fig. 1). The brain and/or hind limb from 82.4% (14/17) of suckling mice tested positive for CHIKV after being fed upon by infected Ae. aegypti (Fig. 1a). Examination of the proxies revealed a positivity rate of 100% (17/17) and 0% (0/17) for the salivary glands and saliva, respectively (Fig. 1a). Statistical analysis revealed no significant difference in the infection rates of SG and mice (P = 0.68) whereas the positivity of saliva collected by forced salivation significantly differed from the infection rates in mice (P < 0.001).
Fig. 1.
Transmission rate estimated for Aedes aegypti mosquitoes injected with three different arboviruses, based on sample type. a CHIKV (N = 17), b WNV (N = 18/#17), c ZIKV (N = 17). Error bars represent the 95% binomial confidence intervals. Asterisks (*) indicate significant comparisons based on a Fisher exact [23] test after Holm correction for multiple testing [24]. Abbreviations: CHIKV, Chikungunya virus; SG, salivary glands; WNV, West Nile Virus; ZIKV, Zika virus
While Ae. aegypti is not considered a vector for WNV, studies have demonstrated its competency in the laboratory and, thus, it was utilized to further evaluate transmission proxy accuracy. Infected Ae. aegypti transmitted WNV to 61.1% of exposed mice (11/17; Fig. 1b). As with CHIKV, all SG were positive (100%, 18/18), yet the proportion of mosquitoes with WNV in saliva secretions was 27.8% (5/17) (Fig. 1b). Based on these findings, the results for the SG significantly overestimated transmission events when compared to the infection rates in mice (P = 0.03). Conversely, the percentage of positive saliva samples was lower than that of WNV-positive mice, but this difference was not statistically different (P = 0.17) (Fig. 1b).
Aedes aegypti transmitted ZIKV to 88.3% of exposed mice (15/17) (Fig. 1c), with all of the SG and none of the saliva secretions testing positive (Fig. 1c). Statistically, ZIKV transmission was better estimated from the positivity of SG (P = 1.00) than from positive saliva (P < 0.001).
Since Ae. aegypti is not the natural vector of WNV, we performed transmission assays on Cx. quinquefasciatus mosquitoes, a major vector of WNV in North America, inoculated intrathoracically. All Cx. quinquefasciatus with disseminated infection also had positive SG (100%; Fig. 2) at 7- and 10-days post-infection (dpi). Despite our efforts, we only recorded six out of 16 mosquitoes either probing or feeding on the mice. All mice exposed to WNV became infected (100%; Fig. 2). WNV was detected in 63.2% (24/38) and 72.7% (24/33) of the saliva samples 7 and 10 dpi, respectively (Fig. 2). Estimates of transmission rate using saliva were not significantly different from the transmission rate observed in suckling mice at dpi 10 (P = 1.00), nor were the estimates based on SG (P = 1.00). However, due to the low numbers of exposed mice, these results should be interpreted with caution.
Fig. 2.
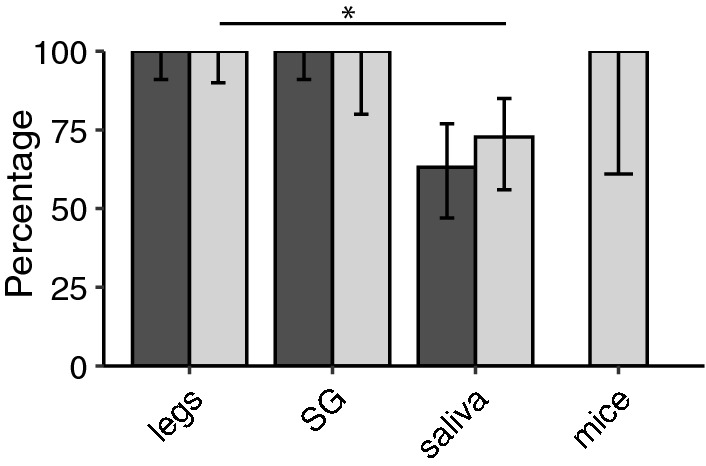
Transmission rate estimated for Culex quinquefasciatus mosquitoes injected with WNV, based on sample type at 7 dpi (dark-gray bars; N = 38) and 10 dpi (light-gray bars; N = 33†). †SG were only dissected from 15 out of the 33 mosquitoes at 10 dpi and that only 6 mice were successfully exposed to WNV. Error bars represent the 95% binomial confidence intervals. Asterisks (*) indicate significant comparisons at 10 dpi based on a Fisher exact [23] test after Holm correction for multiple testing [24]. Abbreviations: dpi, Days post-infection
We further evaluated transmission proxy accuracy utilizing a member of the family Peribunyaviridae (LACV) and Ae. triseriatus mosquitoes. High transmission rates were observed in suckling mice fed upon by LACV-infected Ae. triseriatus (16/17, 94.1%). All SG of disseminated mosquitoes were positive (100%), while 47.1% (8/17) of the saliva samples were positive for LACV (Fig. 3). Positivity of SG better reflected LACV transmission to suckling mice than saliva (P = 1.00 and P = 0.0264, respectively) in this system.
Fig. 3.
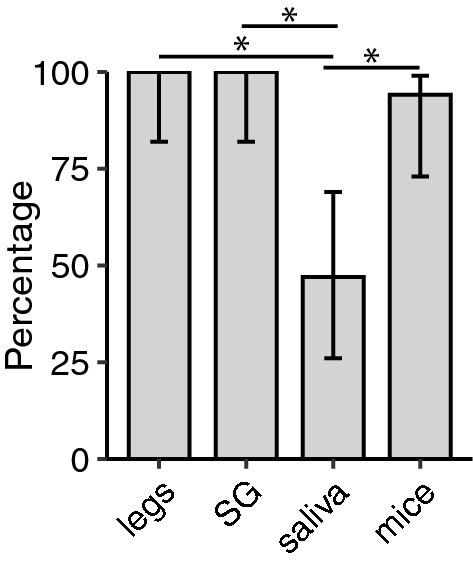
Transmission rate estimated for Aedes triseriatus mosquitoes injected with LACV based on sample type (N = 17). Error bars represent the 95% binomial confidence intervals. Asterisks (*) indicate significant comparisons based on a Fisher exact [23] test after Holm correction for multiple testing [24]. Abbreviations: LACV, La Crosse virus
Influence of infection route on transmission proxies
Since IT inoculation of arboviruses bypasses the midgut barriers to infection and thus does not follow the natural infection route, we tested whether infection route influenced the accuracy of transmission proxies by orally infecting Ae. aegypti with CHIKV. The infection status and transmission capacity of mosquitoes fed with a CHIKV-infected blood meal were determined at 12 and 15 dpi. Only fully fed mosquitoes were used for the analysis. Infection rate, estimated from the presence of virus in bodies, was 52.9% (9/17) at 12 dpi and reached 100% by 15 dpi (18/18). All mosquitoes with CHIKV-positive legs had CHIKV-positive SG. Among the infected mosquitoes (positive bodies), 88.9% (8/9) developed disseminated infections at 12 dpi and 83.3% (15/18) at 15 dpi. From the suckling mice that were fed upon by a mosquito with a disseminated infection, 62.5% (5/8) became infected from mosquitoes with a 12-day EIP and 80% (12/15) from mosquitoes with a 15-day EIP (Fig. 4). The percentage of suckling mice that became infected by a mosquito was not statistically different from positivity based on legs or SG at 12 dpi (P = 0.6) or 15 dpi (P = 0.6724). No positive saliva was detected at 12 dpi, and only one sample was positive for CHIKV at 15 dpi. The positivity of saliva was not statistically different to that of suckling mice at day 12 EIP (P = 0.1025) but it was significantly different at day 15 EIP (P < 0.001).
Fig. 4.
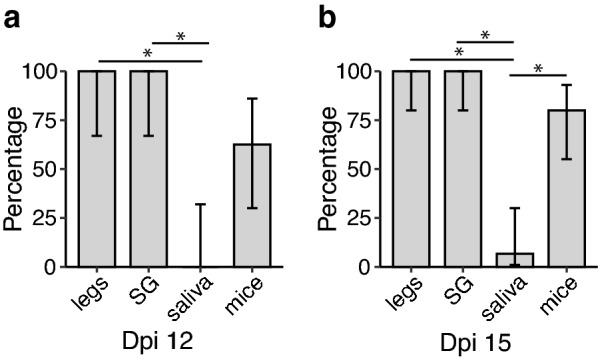
Transmission rate estimated for orally infected Ae. aegypti mosquitoes with CHIKV based on sample type after 12 dpi (N = 8) (a) and 15 dpi (N = 15) (b). Error bars represent the 95% binomial confidence intervals. Asterisks (*) indicate significant comparisons based on a Fisher exact [23] test after Holm correction for multiple testing [24]
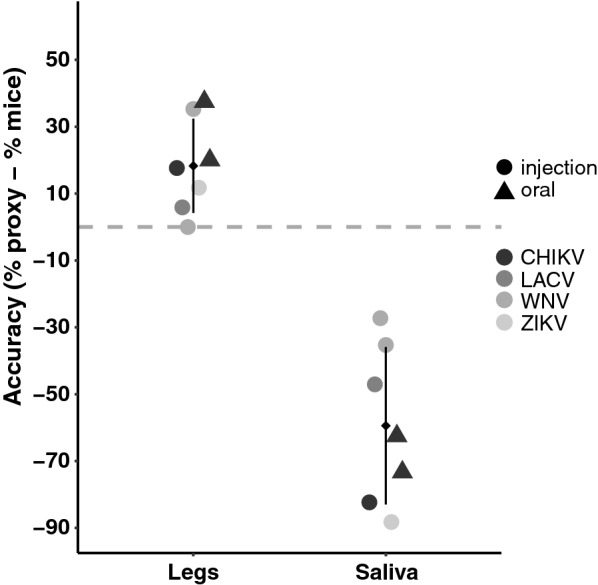
Accuracy of transmission proxies
Across all vector-virus pairs assayed, SG infection status was identical to that of legs, independently of infection route (all pairwise comparisons P = 1.00). The presence of virus in legs (and thus of SG) more closely reflected direct transmission values to suckling mice, overestimating transmission by an average of 18.29 ± 14.09% (Fig. 5). In comparison, transmission estimated from virus positivity in saliva underestimated transmission by 59.43 ± 23.55% (Fig. 5). The difference in accuracy was significant (Welch t-test, P < 0.001) and the pattern was observed regardless of the mode of infection (IT inoculation vs oral feed).
Fig. 5.
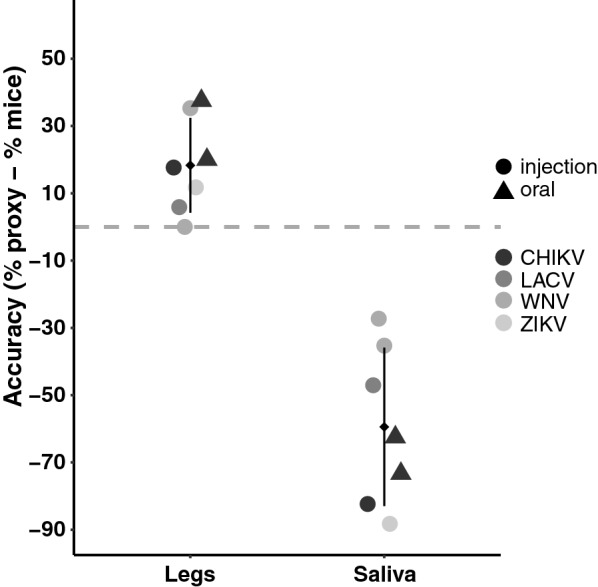
Accuracy of proxies relative to direct virus transmission estimates to suckling mice. Vertical axis shows the difference in the percentage of transmission estimated between the proxy and the mice infections. Different shades of gray represent the different viruses. Experiments from intrathoracic injection are indicated by the larger circles and oral infections by triangles. Mean and standard deviation of the proxy are indicated by the small diamond and attached vertical line, respectively
Discussion
Accurately assessing the ability of a mosquito population to transmit a pathogen is critical to determining its potential to serve as a disease vector. In the laboratory, this is achieved by performing forced salivation on individual mosquitoes, having mosquitoes feed on susceptible vertebrate hosts or assaying peripheral tissues, such as legs, heads and/or SG, for virus infection. In recent years, due to the cost and increasing restrictions on the use of vertebrates, forced salivation has become the accepted method for assaying transmission potential, despite a lack of empirical data demonstrating its accuracy at predicting transmission.
Forced salivation techniques lack standardization, and our data suggest that in our set-up, they misrepresent arboviral transmission to vertebrate hosts. In these techniques, mosquitoes may be anesthetized by cold, CO2 or triethylamine, following which their proboscises are immersed in one of many possible saliva collection diluents (sugar, virus media, FBS, or immersion oil). Smith et al. [27] reported no differences in Venezuelan equine encephalitis virus titers between saliva collected in mineral oil or fetal bovine serum (FBS) media. Miller et al. [20] consistently found the same was true for CHIKV and ZIKV but noted that saliva collected in mineral oil was more often positive for virus than that collected in FBS media [20]. Each of these variables can impact mosquito physiology and the salivation process in different ways and may account for observed inter-study variability. This was demonstrated in three studies examining Ae. aegypti transmission rates via forced salivation, in which 0% to approximately 45% of ZIKV-exposed mosquitoes were reported to have detectable virus in saliva following a 14-day EIP [28–30]. Such discrepancies may be attributed to differences between mosquito and virus strains, or suggest variation in forced salivation techniques. While the goal of this study was not to discriminate different forced salivation techniques, we did find that forced salivation in general underrepresents the transmission potential of an arbovirus when compared to feeding on live animals.
Direct feeding on laboratory animals is the gold standard for assessing arbovirus transmission because it most accurately recapitulates the biological and physiological conditions associated with natural transmission events. Previous studies have shown that suckling outbred mice are a reliable animal model for CHIKV, WNV, ZIKV and LACV [15–19], as they develop viremia and severe disease and mortality often accompany infection [31]. We are thus confident that the direct transmission rates we observed for these pathogens accurately reflect their transmission potential. Nevertheless, although direct mosquito feeding can be highly sensitive for assessing arbovirus transmission, it is dependent on the availability of a suitable animal model, limiting the utility of this approach for many arboviruses.
Alternative approaches to estimate virus transmission by mosquitoes involve testing head/SG tissue via PCR assay, immunofluorescence assay (IFA) or virus titration. In this study we examined SG tissue by PCR assay as another proxy for transmission and found that it overestimated direct transmission rates to mice, but that was closer to direct transmission rates than were those estimated from forced salivation. The positivity of SG was identical to that in legs in this system, despite our efforts to rinse the SG after dissection. A possible explanation is that contamination of the SG by the surrounding hemolymph may have inflated the number of positive SG samples recorded and that this parameter may not reflect an actual SG infection, but rather the attachment of virus particles to the exterior of this tissue. Had we performed IFA, infection rates from SG may have been in closer agreement with the direct feeding results. Nevertheless, these results suggest that dissemination rate (as measured from the legs) may be a good proxy for transmission, without the need of time-consuming and technically challenging dissection of SG.
The poor performance of saliva collected via capillary tubes as proxy for transmission was observed regardless of the mode of infection. While we are aware that infection via IT injection does not reflect a natural route of infection, the focus of this work was to measure the effectiveness of different methods to estimate transmission rate once infection becomes established. We relied on IT inoculations for the bulk of the studies to increase the sample size of our treatments and minimize the use of vertebrates. By using IT injections, we were able to bypass any potential midgut infection and/or escape barriers, thus ensuring that all the mosquitoes tested had a disseminated infection. We further investigated whether our results were dependent on the mode of infection by performing both IT and oral infections with Ae. aegypti and CHIKV. A longer EIP was considered for the oral infection, since IT inoculation is known to reduce EIP [15, 27, 29, 30]. The data from the oral infections supports our findings that forced salivation methods significantly underestimate transmission in this system. In these experiments, detection of virus in saliva proved more difficult in Ae. aegypti than for the other two species tested, regardless of the virus. Studies have reported low transmission for CHIKV and ZIKV in the Ae. aegypti ORL strain, relative to other strains [32, 33], and we cannot discard the possibility that our results may reflect, in part, an overall lower competence level of this particular colony.
The lack of accuracy of forced salivation to reflect arboviral transmission likely results from low viral saliva titers during the early stages of transmission that fall below assay detection thresholds [20, 22], within-population variability in viral expectoration [22] further influenced by differences in vector-virus pairings [27] and/or the possibility that mosquitoes may re-ingest their saliva during forced salivation, as they do during an artificial blood feed [20]. Moreover, there is evidence that SG respond differently following acquisition of a sugar meal and a blood meal [39]. Consequently, saliva collected during forced salivation may not accurately mimic the saliva expectorated during blood-feeding. The interplay of all these variables, further amplified by the lack of standardization of forced salivation techniques across laboratories caution against the use of saliva as a proxy for transmission without prior knowledge of the system investigated.
Conclusions
Our results suggest that virus positivity of legs or SG (dissemination rate) are overall more accurate predictors of arboviral transmission than detection of virus from saliva collected using the commonly implemented forced salivation technique and are subject to less technical variation. However, a leg-only approach for estimating transmission rates may not be appropriate for all studies. When examining the competency of a new virus–vector pairing, multiple approaches for estimating transmission rate should be implemented to explore the possibility that a SG infection barrier or escape barrier exists. Moreover, the use of legs as transmission proxy should be utilized judicially when examining EIP. Based on the kinetics of infection, the hemolymph/legs will become infected prior to transmission; therefore, studies assessing transmission through the use of legs alone may report shortened EIPs.
Supplementary Information
Additional file 1: Text S1. Titration of viral stock solutions. Table S1. Sequence of primers and probes (5’ to 3’) used for viral detection in the RT-PCR assay. Table S2. Limit of detection of RT-PCR assay. Figure S1. RT-PCR standard curves for chikungunya (a), Zika (b), La Crosse (c) and West Nile (d) viruses.
Acknowledgements
We would like to thank J.J. Shepard, and T. Petruff for help in rearing the mosquito colonies and A. Bransfield and M.J. Misencik for support in the BSL3 lab.
Abbreviations
- CHIKV
Chikungunya virus
- EIP
Extrinsic incubation period
- IIP
Intrinsic incubation period
- IT
Intrathoracic inoculation
- LACV
La Crosse virus
- ORL
Aedes aegypti Orlando strain
- PFU
Plaque-forming units
- SG
Salivary glands
- WNV
West Nile virus
- ZIKV
Zika virus
Authors' contributions
AG-S contributed to experimental design, conducted all experiments, collected and analyzed data and drafted the manuscript. DEB contributed to the experimental design and data analyses, and reviewed manuscript drafts. PMA contributed to the experimental design, conducted experiments and collected data and reviewed manuscript drafts. All authors read and approved the final manuscript.
Funding
This publication was funded the Cooperative Agreement U01CK000509, funded by the Center for Disease Control and Prevention. Its content is solely the responsibility of the authors and do not necessarily represent the official views of the Center for Disease Control and Prevention or the Department of Health and Human Services. The funding agency did not participate in the design of the study, collection, analysis, or interpretation of data.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Declarations
Ethics approval and consent to participate
Procedures for handling and care of animals were approved by and performed under the Animal Care and Use Committee at The Connecticut Agricultural Experiment Station (protocol no. P28-17).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
A. Gloria-Soria, Email: andrea.gloria-soria@ct.gov
D. E. Brackney, Email: doug.brackney@ct.gov
P. M. Armstrong, Email: philip.armstrong@ct.gov
References:
- 1.Reynolds ES, Hart CE, Hermance ME, Brining DL, Thangamani S. An overview of animal models for arthropod-borne viruses. Comp Med. 2017;67:232–241. [PMC free article] [PubMed] [Google Scholar]
- 2.Armstrong PM, Rico-Hesse R. Efficiency of dengue serotype 2 virus strains to infect and disseminate in Aedes aegypti. Am J Trop Med Hyg. 2003;68:539–544. doi: 10.4269/ajtmh.2003.68.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li MI, Wong PSJ, Ng LC, Tan CH. Oral susceptibility of Singapore Aedes (Stegomyia) aegypti (Linnaeus) to Zika virus. PLOS Negl Trop Dis. 2012;6:e1792. doi: 10.1371/journal.pntd.0001792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moncayo AC, Fernandez Z, Ortiz D, Diallo M, Sall A, Hartman S, et al. Dengue emergence and adaptation to peridomestic mosquitoes. Emerg Infect Dis. 2004;10:1790–1796. doi: 10.3201/eid1010.030846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azar SR, Weaver SC. Vector competence: what has Zika virus taught us? Viruses. 2019;11:867. doi: 10.3390/v11090867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ciota AT, Bialosuknia SM, Zink SD, Brecher M, Ehrbar DJ, Morrissette MN, et al. Effects of Zika virus strain and Aedes mosquito species on vector competence. Emerg Infect Dis. 2017;23:1110–1117. doi: 10.3201/eid2307.161633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia-Luna SM, Weger-Lucarelli J, Rückert C, Murrieta RA, Young MC, Byas AD, et al. Variation in competence for ZIKV transmission by Aedes aegypti and Aedes albopictus in Mexico. PLOS Negl Trop Dis. 2018;12:e0006599. doi: 10.1371/journal.pntd.0006599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gloria-Soria A, Payne AF, Bialosuknia SM, Stout J, Mathias N, Eastwood G, et al. Vector competence of Aedes albopictus populations from the Northeastern United States for Chikungunya, Dengue, and Zika Viruses. Am J Trop Med Hyg. 2021;104:1123–1130. doi: 10.4269/ajtmh.20-0874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryckebusch F, Berthet M, Missé D, Choumet V. Infection of a French population of Aedes albopictus and of Aedes aegypti (Paea Strain) with Zika Virus reveals low transmission rates to these vectors’ saliva. Int J Mol Sci. 2017;18:2384. doi: 10.3390/ijms18112384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanchez-Vargas I, Olson KE, Black WC. The genetic basis for salivary gland barriers to arboviral transmission. Insects. 2021;12:73. doi: 10.3390/insects12010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azar SR, Roundy CM, Rossi SL, Huang JH, Leal G, Yun R, et al. Differential vector competency of Aedes albopictus populations from the Americas for Zika virus. Am J Trop Med Hyg. 2017;97:330–339. doi: 10.4269/ajtmh.16-0969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roundy CM, Azar SR, Rossi SL, Huang JH, Leal G, Yun R. Variation in Aedes aegypti mosquito competence for Zika virus transmission. Emerg Infect Dis. 2017;23:625–632. doi: 10.3201/eid2304.161484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Styer LM, Kent KA, Albright RG, Bennett CJ, Kramer LD, Bernard KA. Mosquitoes inoculate high doses of West Nile virus as they probe and feed on live hosts. PLoS Pathog. 2007;3:132. doi: 10.1371/journal.ppat.0030132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gloria-Soria A, Soghigian J, Kellner D, Powell JR. Genetic diversity of laboratory strains and implications for research: the case of Aedes aegypti. PLoS Negl Trop Dis. 2019;13:0007930. doi: 10.1371/journal.pntd.0007930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Couderc T, Chrétien F, Schilte C, Disson O, Brigitte M, Guivel-Benhassine F, et al. A mouse model for Chikungunya: young age and inefficient type-I interferon signaling are risk factors for severe disease. PLoS Pathog. 2008;4:29. doi: 10.1371/journal.ppat.0040029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu J, Liu X, Ke C, Wu Q, Lu W, Qin Z, et al. Effective suckling C57BL/6, Kunming, and BALB/c mouse models with remarkable neurological manifestation for Zika virus infection. Viruses. 2017;9:165. doi: 10.3390/v9070165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yadav PD, Kumar V, Kumar S, Mote CS, Majumdar TD, Gokhale M, et al. Zika virus pathogenesis in infant mice after natural transmission by the bite of infected mosquitoes. Intervirology. 2017;60:227–234. doi: 10.1159/000486841. [DOI] [PubMed] [Google Scholar]
- 18.Paulson SL, Grimstad PR, Craig GB. Midgut and salivary gland barriers to La Crosse virus dissemination in mosquitoes of the Aedes triseriatus group. Med Vet Entomol. 1989;3:113–123. doi: 10.1111/j.1365-2915.1989.tb00485.x. [DOI] [PubMed] [Google Scholar]
- 19.Sudeep AB, Mandar P, Ghodke YK, George RP, Gokhale MD. Vector competence of two Indian populations of Culex quinquefasciatus (Diptera: Culicidae) mosquitoes to three West Nile virus strains. J Vector Borne Dis. 2015;52:185. [PubMed] [Google Scholar]
- 20.Miller MR, Sorensen MR, Markle ED, Clarkson TC, Knight AL, Savran MJ, et al. Characterizing and quantifying arbovirus transmission by Aedes aegypti using forced salivation and analysis of bloodmeals. Insects. 2021;12:304. doi: 10.3390/insects12040304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aaskov J, Buzacott K, Thu HM, Lowry K, Holmes EC. Long-term transmission of defective RNA viruses in humans and Aedes mosquitoes. Science. 2006;311:236–238. doi: 10.1126/science.1115030. [DOI] [PubMed] [Google Scholar]
- 22.Mayton EH, Hernandez HM, Vitek CJ, Christofferson RC. A method for repeated, longitudinal sampling of individual Aedes aegypti for transmission potential of arboviruses. Insects. 2021;12:292. doi: 10.3390/insects12040292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher RA. Statistical methods for research workers. The logic of inductive inference. J Royal Stat Soc Ser A. 1935;98:39–54. [Google Scholar]
- 24.Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 25.Nakazawa M. fmsb: Functions for medical statistics book with some demographic data. R package version 0.7.1. https://CRAN.R-project.org/package=fmsb. Accessed 18 Dec 2021.
- 26.R Core Team. R: A language and environment for statistical computing. 2016. Vienna: R Foundation for Statistical Computing. https://www.r-project.org. Accessed 18 Dec 2021.
- 27.Smith DR, Carrara AS, Aguilar PV, Weaver SC. Evaluation of methods to assess transmission potential of Venezuelan equine encephalitis virus by mosquitoes and estimation of mosquito saliva titers. Am J Trop Med Hyg. 2005;73:33–39. [PubMed] [Google Scholar]
- 28.Weger-Lucarelli J, Rückert C, Chotiwan N, Nguyen C, Garcia Luna SM, Fauver JR, et al. Vector competence of American mosquitoes for three strains of Zika virus. PLoS Negl Trop Dis. 2016;10:e0005101. doi: 10.1371/journal.pntd.0005101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gutiérrez-Bugallo G, Boullis A, Martinez Y, Hery L, Rodríguez M, Bisset JA, et al. Vector competence of Aedes aegypti from Havana, Cuba, for dengue virus type 1, chikungunya, and Zika viruses. PLOS Negl Trop Dis. 2020;14:e0008941. doi: 10.1371/journal.pntd.0008941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan KK, Auguste AJ, Brewster CC, Paulson SL. Vector competence of Virginia mosquitoes for Zika and Cache Valley viruses. Parasit Vectors. 2020;13:188. doi: 10.1186/s13071-020-04042-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karabatsos N, editor. International catalogue of arboviruses, including certain other viruses of vertebrates. San Antonio: American Society of Tropical Medicine and Hygiene for the Subcommittee on Information Exchange of the American Committee on Arthropod-borne Viruses. 1985.
- 32.Alto BW, Wiggins K, Eastmond B, Velez D, Lounibos LP, Lord CC. Transmission risk of two chikungunya lineages by invasive mosquito vectors from Florida and the Dominican Republic. PLoS Negl Trop Dis. 2017;11:e0005724. doi: 10.1371/journal.pntd.0005724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Uraki R, Hastings AK, Gloria-Soria A, Powell JR, Fikrig E. Altered vector competence in an experimental mosquito-mouse transmission model of Zika infection. PLoS Negl Trop Dis. 2018;12:e0006350. doi: 10.1371/journal.pntd.0006350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dubrulle M, Mousson L, Moutailler S, Vazeille M, Failloux AB. Chikungunya virus and Aedes mosquitoes: saliva is infectious as soon as two days after oral infection. PLoS ONE. 2009;4:e5895. doi: 10.1371/journal.pone.0005895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arias-Goeta C, Mousson L, Rougeon F, Failloux AB. Dissemination and transmission of the E1–226V variant of chikungunya virus in Aedes albopictus are controlled at the midgut barrier level. PLoS ONE. 2013;8:e57548. doi: 10.1371/journal.pone.0057548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robison A, Young MC, Byas AD, Rückert C, Ebel GD. Comparison of chikungunya virus and Zika virus replication and transmission dynamics in Aedes aegypti mosquitoes. Am J Trop Med Hyg. 2020;103:869. doi: 10.4269/ajtmh.20-0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sardelis MR, Turell MJ, Dohm DJ, O'Guinn ML. Vector competence of selected North American Culex and Coquillettidia mosquitoes for West Nile virus. Emerg Infect Dis. 2001;7:1018. doi: 10.3201/eid0706.010617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McGee CE, Shustov AV, Tsetsarkin K, Frolov IV, Mason PW, Vanlandingham DL, et al. Infection, dissemination, and transmission of a West Nile virus green fluorescent protein infectious clone by Culex pipiens quinquefasciatus mosquitoes. Vector-Borne Zoonotic Diseases. 2010;10:267–274. doi: 10.1089/vbz.2009.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marinotti O, James AA, Ribeiro JC. Diet and salivation in female Aedes aegypti mosquitoes. J Insect Physiol. 1990;36:545–548. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Text S1. Titration of viral stock solutions. Table S1. Sequence of primers and probes (5’ to 3’) used for viral detection in the RT-PCR assay. Table S2. Limit of detection of RT-PCR assay. Figure S1. RT-PCR standard curves for chikungunya (a), Zika (b), La Crosse (c) and West Nile (d) viruses.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.