Abstract
Open reading frame 8 (ORF8) shows one of the highest levels of variability among accessory proteins in Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the causative agent of Coronavirus Disease 2019 (COVID-19). It was previously reported that the ORF8 protein inhibits the presentation of viral antigens by the major histocompatibility complex class I (MHC-I), which interacts with host factors involved in pulmonary inflammation. The ORF8 protein assists SARS-CoV-2 in evading immunity and plays a role in SARS-CoV-2 replication. Among many contributing mutations, Q27STOP, a mutation in the ORF8 protein, defines the B.1.1.7 lineage of SARS-CoV-2, engendering the second wave of COVID-19. In the present study, 47 unique truncated ORF8 proteins (T-ORF8) with the Q27STOP mutations were identified among 49,055 available B.1.1.7 SARS-CoV-2 sequences. The results show that only one of the 47 T-ORF8 variants spread to over 57 geo-locations in North America, and other continents, which include Africa, Asia, Europe and South America. Based on various quantitative features, such as amino acid homology, polar/non-polar sequence homology, Shannon entropy conservation, and other physicochemical properties of all specific 47 T-ORF8 protein variants, nine possible T-ORF8 unique variants were defined. The question as to whether T-ORF8 variants function similarly to the wild type ORF8 is yet to be investigated. A positive response to the question could exacerbate future COVID-19 waves, necessitating severe containment measures.
Keywords: ORF8, SARS-CoV-2, COVID-19, Truncated, Intrinsically disordered region, Truncation mutation, Continent distribution
Introduction
The world is proceeding through a very difficult time due to the Coronavirus Disease 2019 (COVID-19), of which the causative agent is the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) (Hu et al., 2021; Yuen et al., 2020; Matheson & Lehner, 2020; Wu et al., 2020; Fontanet et al., 2021). There are nine open reading frames (ORFs), which encode accessory proteins important for the modulation of metabolism in infected host cells and innate immunity evasion via a complicated signalome and an interactome (Ren et al., 2020; Hassan et al., 2021c, 2020b; Díaz, 2020; Stukalov et al., 2021). The ORF8 protein is one of the most rapidly evolving accessory proteins among the beta coronaviruses, not only due to its ability to interfere with host immune response, but also with regards to its several missense mutations detected to date (Li et al., 2020; Zinzula, 2021; Hassan et al., 2021a; Flower et al., 2021). ORF8 directly interacts with major histocompatibility complex class I (MHC-I) both in vitro and in vivo, and is down-regulated, which impairs its ability to carry out antigen presentation and rendering infected cells less sensitive to lysis by cytotoxic T lymphocytes (Zhang et al., 2021). ORF8 suppresses type I interferon antiviral responses and interacts with host factors involved in pulmonary inflammation and fibrogenesis (Zhang et al., 2021; Rashid et al., 2021). From all viral proteomes interacting with human metalloproteome, the ORF8 proteins interact with 10 out of 58 human metalloproteins (Chasapis et al., 2021). Both SARS-CoV-2 and SARS-CoV ORF8 proteins play crucial roles in virus pathophysiological events, and dysregulate the TGF-β pathway, which is involved in the tissue fibrosis (Pereira, 2020). The functional implications of SARS-CoV-2 ORF8 had already gained immense attention and ORF8 is considered an important component of the immune evasion machinery (Li et al., 2020; Pereira, 2020; Mohammad et al., 2020; Alkhansa, Lakkis & El Zein, 2021). The SARS-CoV-2 ORF8 protein has less than twenty percent amino acid sequence homology with the SARS-CoV ORF8 protein, and represents a rapidly evolving viral protein (Flower et al., 2021; Velazquez-Salinas et al., 2020). A molecular framework for understanding the rapid evolution of ORF8, its contributions to COVID-19 pathogenesis, and the potential for its neutralization by antibodies have been supported by the structural analysis of the ORF8 protein (Hachim et al., 2020; Wang et al., 2020a). The crosstalk between SARS-CoV-2 or SARS-CoV infection and the host cell proteome at different levels may enable the identification of distinct and common molecular mechanisms (Zhang et al., 2021). Of note, SARS-CoV-2 ORF8 interacts with a significant number of host proteins related to the endoplasmic reticulum quality control, glycosylation, and extracellular matrix organization, although the mechanism of action of ORF8 concerning those interacting proteins is uncertain (Wang et al., 2020a; Wu et al., 2021).
The clade S, a subtype of SARS-CoV-2, was identified to possess the mutation L84S in the ORF8 protein sequence (Koyama, Platt & Parida, 2020; Mercatelli & Giorgi, 2020; Sengupta, Hassan & Choudhury, 2021). Presently, among many variants of SARS-CoV-2, the lineage B.1.1.7 carries a larger than usual number of genetic changes (Galloway et al., 2021; Ramírez et al., 2021; Frampton et al., 2021). Among many non-synonymous mutations, Q27STOP in the ORF8 protein contributed to the extrapolation of the branch leading to lineage B.1.1.7 (Perchetti et al., 2021; Li et al., 2021). The Q27STOP mutation inactivates the ORF8 protein favoring further downstream mutations, and could be responsible for the increased transmissibility of the B.1.1.7 variant (Galloway et al., 2021; Borges et al., 2021). The B.1.1.7 variant, being more transmissible than the wild-type SARS-CoV-2, was first detected in September 2020 in the UK (Shen et al., 2021; Walensky, Walke & Fauci, 2021). It began to spread rapidly by mid-December and was correlated with a significant increase in the number of SARS-CoV-2 infections in the UK and worldwide.
Functional implications on the immune surveillance due to the ORF8 truncation at position 27 remain unclear (Pereira, 2020). Therefore, it is of utmost importance to gain insight into the functionality of the truncated ORF8 protein variants to comprehend the B.1.1.7 lineage through theoretical and experimental characterization and genomic surveillance worldwide (Davies et al., 2021). The present study aimed at characterizing the unique variations of truncated ORF8 proteins (T-ORF8) due to the Q27STOP mutation. Further, this investigation differentiates a single T-ORF8 variant among 47 distinct unique T-ORF8 variants present in SARS-CoV-2 worldwide, as of May 20th, 2021. Several clusters of the unique T-ORF8 have been identified based on the various bioinformatics features and phylogenetic relationships, along with the emerging variants of the unique T-ORF8.
Data Acquisition and Methods
A total of 49,055 truncated ORF8 protein (T-ORF8) sequences (complete) from five continents (Asia, Africa, Europe, South America, and North America) were downloaded in FASTA format from the National Center for Biotechnology Information (NCBI) database (http://www.ncbi.nlm.nih.gov/). Note that no T-ORF8 protein sequence was found from Oceania. Next, FASTA files were processed in MATLAB 2021a for extracting unique T-ORF8 protein sequences for each continent. Note that only 47 unique T-ORF8 protein sequences were found. Here “unique T-ORF8” refers to a T-ORF8 protein sequence, which is different from other T-ORF8 sequences by the arrangement of amino acids, showing a non-zero Hamming distance from other T-ORF8 sequences. Consequently, the amino acid sequence of a “unique T-ORF8” variant is non-identical to other T-ORF8 sequences.
Derivation of polar/non-polar sequences and associated phylogeny
Every amino acid in a given T-ORF8 sequence was identified as polar (Q) or non-polar (P). Thus, every unique T-ORF8 became a binary sequence with two symbols P and Q. Then, the homology of these sequences was determined using the Clustal Omega web-suite (https://www.ebi.ac.uk/Tools/msa/clustalo/) and then associated with the nearest neighbor phylogenetic relationship among the unique T-ORF8 variants. Further, unique T-ORF8 variants with distinct binary polar/non-polar sequences were extracted (Hassan et al., 2020a; Broome & Hecht, 2000).
Frequency distribution of amino acids and phylogeny
The frequency of each amino acid present in a T-ORF8 sequence was determined using standard bioinformatics routine in Matlab-2021a. For each T-ORF8 protein, a twenty-dimensional frequency-vector considering the frequency of standard twenty amino acids can be obtained. Based on this frequency distribution of amino acids several consequences were drawn. The distance (Euclidean metric) between any two pairs of frequency vectors was calculated for each pair of T-ORF8 sequences. The distance matrix was used to develop a phylogenetic relationship based on the nearest neighbor-joining method using the standard routine in Matlab-2021a (Hassan et al., 2020c; Hassan, Choudhury & Roy, 2021).
Deep phylogenetic analyses
All phylogenetic data preparation and calculations were conducted in MEGA X (Kumar et al., 2018; Stecher, Tamura & Kumar, 2020). For deep phylogeny analyses we used two nucleotide datasets: one composed by the alignment of all 47 truncated ORF 8 sequences in addition to the RATG13 ORF8 as an external group, and a second group using all 47 truncated ORF 8, the RATG13 ORF 8 as well as 66 representative ORF 8 sequences for different Alpha, Beta, Gamma, Delta, Mu, GH/490R and Omicron variants. The phylogeny estimations were inferred by Maximum Likelihood using the Hasegawa-Kishino-Yano model (Hasegawa, Kishino & Yano, 1985). A discrete Gamma distribution was used compute the evolutionary rate differences among sites: four categories +G, parameter = 200.0000 and 500 bootstrap replications (Benvenuto et al., 2020). Furthermore, initial trees were heuristically obtained using Neighbor-Join and BioNJ algorithms with a Maximum Composite Likelihood (MCL) approach.
Amino acid conservation in terms of Shannon’s entropy
The degree of conservation of amino acids embedded in a T-ORF8 protein was obtained by the well-known information-theoretic measure called “Shannon’s entropy (SE)”. For each T-ORF8 protein, Shannon’s entropy of amino acid conservation over the amino acid sequence of T-ORF8 protein was calculated using as described in (Hassan et al., 2020c, 2021b). For a given T-ORF8 sequence of length l (here l = 26), the conservation of amino acids was calculated as follows:
where ; ki represents the number of occurrences of an amino acid si in the T-ORF8 sequence (Strait & Dewey, 1996).
Prediction of molecular and physicochemical properties
Theoretical pI (PI), extinction coefficient (EC), instability index (II), aliphatic index (AI), protein solubility (PS), grand average of hydropathicity (GRAVY), and the number of tiny, small, aliphatic, aromatic, non- polar, polar, charged, basic and acidic residues of all unique T-ORF8 proteins were calculated using the web-servers ’ProtParam’, ’Protein-sol’ and EMBOSS Pepstats (Gasteiger et al., 2005; Hebditch et al., 2017; Madeira et al., 2019).
Intrinsic disorder analysis
All 47 T-ORF8 variants were subjected to the per-residue disorder analysis, for which PONDR® VSL2 algorithm was employed (Obradovic et al., 2005). This tool showed good performance on proteins containing both structure and disorder and was favorably ranked in a recent Critical Assessment of protein Intrinsic Disorder prediction (CAID) experiment (Necci, Piovesan & Tosatto, 2021).
Finding functional motifs
The Eukaryotic Linear Motif (ELM) resource (http://elm.eu.org/) was used for finding functional sites in proteins (Kumar et al., 2020). ELMs (also known as short linear motifs (SLiMs)), are short protein interaction sites, which are commonly found in intrinsically disordered regions of proteins and define a wide range of protein functionality.
Results
All 49,055 unique T-ORF8 protein variants were segregated from a set of available truncated ORF8 protein sequences collected from the NCBI database. Further, variability and commonality of the unique T-ORF8 proteins were analyzed from various quantitative measures as discussed in the methods section.
Characteristics of the unique variants of T-ORF8
The number of total sequences for each continent, the unique truncated ORF8 (T-ORF8) sequences, and their percentages are presented in Table 1. The results showed that 47 unique T-ORF8 proteins among the total of 48,691 were present in North America (Table 1). The unique T-ORF8 variants from Africa, Asia, Europe, and South America were contained in the set of unique T-ORF8 variants available in North America. Additionally, there were seven T-ORF8 with amino acid lengths 22, 24, 40 and 41 available in North America as of May 18, 2021 (Table 2). Note that among the seven T-ORF8 sequences, only five were found to be unique, as mentioned in Table 2. As of May 18, 2021 a single copy of the T-ORF8 proteins of amino acid lengths of 24 and 41 (Table 2) were found. There were two T-ORF8 variants of 41 amino acids available in North America. The most frequent T-ORF8 proteins so far observed, were the T-ORF8 proteins of 26 amino acids. It was observed that the T-ORF8 arose due to truncation at the residue positions 23, 25, 27, 41, and 42 of the 121 amino acid full-length ORF8 protein. We investigated the possible mutations for such truncations. A snapshot of the amino acid residues and their possible mutations with respect to the reference sequence NC 045512 is presented in Fig. S1.
Table 1. Frequency and percentages unique T-ORF8 variants (continent-wise).
| Percentages of the unique T-ORF8 variants on continents | ||||
|---|---|---|---|---|
| Continent | Total T-ORF8 (T) | Unique T-ORF8 (U) | Percentage, continent-wise | Percentage, world-wide |
| Africa | 108 | 1 | 0.926% | 1.96% |
| Asia | 99 | 1 | 1.01% | 1.96% |
| Europe | 156 | 1 | 0.641% | 1.96% |
| South America | 1 | 1 | 100% | 1.96% |
| North America | 48,691 | 47 | 0.096% | 92.16% |
| World-wide | 49,055 | 47 | 0.104% | |
Note:
Here ‘U’ stands for the total number of unique T-ORF8 variants over the total available T-ORF8 sequences, which is denoted by ‘T’.
Table 2. Truncated ORF8 variants of length other than 26 amino acids.
| Accession ID | Length (number of amino acid residues) | Date of collection | Geo-location | Remarks |
|---|---|---|---|---|
| QQX22250.1 | 22 | 20-10-2020 | USA: KS | 2*Identical sequence |
| QQX22346.1 | 22 | 24-09-2020 | USA: MO | |
| QVF74147.1 | 24 | 27-04-2021 | USA: Colorado | Worldwide frequency: 01 |
| QRE01295.1 | 40 | 13-12-2020 | USA: MD | Worldwide frequency: 01 |
| QQX21038.1 | 41 | 30-10-2020 | USA: OK | Worldwide frequency: 01 |
| QLJ58176.1 | 41 | 09-04-2020 | USA | 2*Identical sequence |
| QLJ58236.1 | 41 | 16-04-2020 | USA |
Note that at four positions, 23, 25, 27, and 40, amino acids glutamine (Gln) and cysteine (Cys) were truncated due to mutations at the codon’s first and third positions, respectively. The amino acid valine (Val) was truncated due to three mutations at the third, second, and first positions of the codon ’GUG’. Furthermore, it was observed that the mutations at the positions 23 and 25 were identical (C to U), and the changes of bases were transition mutations; i.e., pyrimidine (purine) to pyrimidine (purine). In contrast, the changes of bases of the truncated mutations at the positions 25 and 41 were transversal mutations; i.e., pyrimidine (purine) to purine (pyrimidine). For position 42, three sequences of mutations were hypothesized, taking place at first, second, and third positions of the codon (GUG); i.e., transition mutations (purine to purine), transversal mutation (pyrimidine to purine), and transversal mutation (purine to pyrimidine), respectively.
The list of unique T-ORF8 sequences of 26 amino acids with their representative accession IDs and sequences is presented in Table S1. Further, it was found that the unique T-ORF8 variants from Africa, Asia, Europe and South America were identical in relation to P15, as illustrated in Table S1. The date of sample collection, geo-location and accession ID of the first identified SARS-CoV-2 containing unique T-ORF8 variants are presented in Table S2.
Based on Table S2, the ORF8 protein sequence P15 was found in 48395 copies of the B.1.17 SARS-CoV-2 lineage in North America. Besides, the P15 variant with the Q27STOP mutation in the B.1.1.7 lineage was found in Africa, Asia, Europe and South America with a frequency of 108, 99, 156, and 1, respectively. None of the other 46 T-ORF8 unique variants was found on any continent, as of May 18, 2021. So, 46 unique T-ORF8 sequences were exclusively found in North America. Therefore, the P15 TORF8 variant is of particular interest for its uniqueness due to its apparent prevalence in most of the B.1.17 lineages of SARS-CoV-2 from North America and other continents.
In Europe, the P15 variant was first detected in two infected patients from Poland on March 15, 2020. In North America, two patients from Maryland were infected with the same SARS-CoV-2 P15 variant on May 27, 2020. After five days of the second occurrence of P15 in North America, one patient from Punjab-Pakistan (Asia) was infected by the P15 SARS-CoV-2 variant. Six months thereafter, the same variant was found in a patient from Ghana, for the first time in Africa. Twenty days after the fifth occurrence in Africa, the P15 variant was identified in Peru (South America) on December 31, 2020
Additionally, the frequency distribution of the T-ORF8 P15 variants across the North American continent is presented in Table 3. It was found that the T-ORF8 P15 variant spread over three geo-locations, Michigan, Florida, and Minnesota, with the highest number of frequencies of 5084, 6884, and 7416, respectively. The P15 variant was found for the first time in Maryland, but the frequency at this geo-location was 1171 on May 14, 2021.
Table 3. Distribution of cumulative frequency of P15 variants across North America.
| Geo-location | Frequency | Geo-location | Frequency | Geo-location | Frequency |
|---|---|---|---|---|---|
| Wyoming | 56 | North Carolina | 776 | Iowa | 141 |
| Wisconsin | 383 | New York | 887 | Indiana | 823 |
| West Virginia | 289 | New Mexico | 250 | Illinois | 1,426 |
| Washington | 83 | New Jersey | 1,815 | Idaho | 85 |
| Virginia | 917 | New Hampshire | 234 | Hawaii | 16 |
| Vermont | 209 | Nevada | 157 | Guam | 7 |
| Utah | 97 | Nebraska | 105 | Georgia | 1,232 |
| Texas | 3,420 | Montana | 25 | Florida | 6,884 |
| Tennessee | 993 | Missouri | 254 | District of Columbia | 61 |
| South Dakota | 86 | Mississippi | 40 | Delaware | 70 |
| South Carolina | 261 | Minnesota | 7,416 | Connecticut | 496 |
| Rhode Island | 339 | Michigan | 5,084 | Colorado | 533 |
| Puerto Rico | 224 | Massachusetts | 2,761 | California | 1,727 |
| Pennsylvania | 3,285 | Maryland | 1,171 | CA, Santa Clara County | 4 |
| Oregon | 166 | Maine | 79 | CA, Humboldt | 20 |
| Okhlahoma | 81 | Louisiana | 223 | Arkansas | 62 |
| Ohio | 1,191 | Kentucky | 145 | Arizona | 290 |
| North Dakota | 13 | Kansas | 100 | Alaska | 65 |
| Alabama | 168 | ||||
| USA | 654 |
There were 18 geo-locations, where the frequency of spread of the P15 variant was found to be less than 100 (Table 3). Among other geo-locations, Guam (US territory located in the Pacific Ocean) and North Dakota, USA, had the least number of patients infected by the B.1.1.7 variant containing the P15 protein. In Guam, according to the NCBI SARS-CoV-2 database, all seven patients were infected by the B.1.1.7 variant containing the P15, within a short period from February 21 to April 11, 2021. Also, in North Dakota, 13 of 16 patients were infected by the same strain of SARS-CoV-2 from February 2, 2021 to April 28, 2021.
The frequency distribution of all T-ORF8 variants across the US is presented in Table 4. It is evident that all 47 unique T-ORF8 variants were detected in 21 different states of the US. The highest number (7) of the unique T-ORF8 variants was detected as a first instance in Pennsylvania within a short period (March 2 to April 20, 2021) (Table 4). The P35 variant was found initially in two states: Rhode Island and Massachusetts on March 20, 2021. Furthermore, it was observed that all T-ORF8 variants other than P15 emerged for the first time from February 12, 2021 to April 28, 2021.
Table 4. Frequency distribution of unique T-ORF8 variants over the USA.
| USA: states | Unique T-ORF8 variants | USA: states | Unique T-ORF8 variants |
|---|---|---|---|
| USA: California | P1, P30, P40 | USA: Missouri | P28 |
| USA: Connecticut | P32, P33 | USA: New Jersey | P10, P41 |
| USA: Florida | P4, P14, P16 | USA: Ohio | P2 |
| USA: Georgia | P21 | USA: North Carolina | P47 |
| USA: Illinois | P18 | USA: Pennsylvania | P7, P17, P19, P20, P23, P27, P39 |
| USA: Kentucky | P36 | USA: Puerto Rico | P24 |
| USA: Louisiana | P31 | USA: Tennessee | P5, P22 |
| USA: Maryland | P15, P26, P29, P34 | USA: Rhode Island | P35 |
| USA: Massachusetts | P35, P42 | USA: Texas | P6, P9, P11, P25 |
| USA: Michigan | P8, P38, P43, P46 | USA: Utah | P45 |
| USA: Minnesota | P3, P12, P13, P37, P44 |
Using the Clustal Omega web-server, an amino acid sequence-based alignment and corresponding phylogenetic tree of the unique T-ORF8 variants are presented in Fig. S2. From the sequence alignment, it was derived that all unique T-ORF8 variants share identical amino acids methionine (Met), lysine (Lys), Gln, serine (Ser), and leucine (Leu) at positions 1, 2, 18, 21, and 22 respectively. Further it was found that T-ORF8 P15 is closest to the ORF8 sequences P13 and P14 (Fig. S2). Note that P15 was placed at the leftmost branch of the phylogenetic tree, which made the sequence P15 distinguishable from the rest of the T-ORF8 variants. The pairs of T-ORF8 variants (P13, P14), (P5, P6), (P33, P45), (P9, P37), (P19, P20), (P35, P36), (P31, P34), (P29, P43), (P27, P42), (P25, P26), (P22, P23), (P21, P40), (P17, P18), (P2, P8), and (P1, P47) were found to be the closest to each other based on the amino acid sequence homology-based phylogeny (Fig. S2).
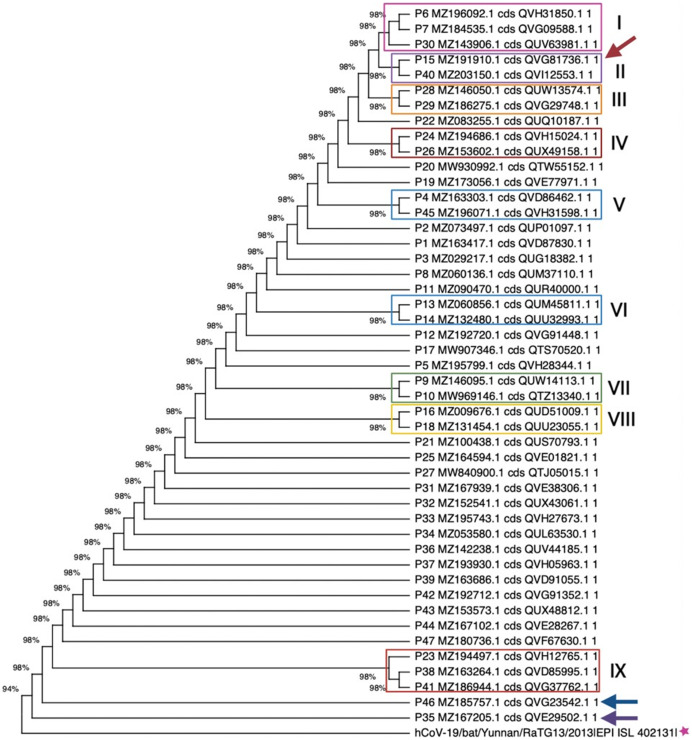
Next, we conducted deep phylogenic analysis. The first nucleotide dataset used for this analysis included the alignment of all 47 truncated ORF8 sequences in addition to the RATG13 ORF8 as an external group. Phylogenic analysis of this group returned a tree (Fig. 1) with the highest log likelihood of −400.62 in an analysis with 48 nucleotide sequences and a total of 83 positions in the final dataset. In addition, Fig. 1 shows nine well-defined monophyletic groups, where the ORF 8 sequences 15 and 40 formed a unique clade in the group II. Based on this tree analysis it can be inferred that at least nine truncated ORF8 variants could be related to a specific SARS-CoV-2 variant and/or a specific variant subtype, in this case more related to de Alpha type. Interestingly, sequences 35 and 46 rooted outside the tree together with the external group ORF8 from the RATG13 genome. In these cases, the sequences 35 and 46 are possibly mutating to the corresponding SARS-CoV-2 start point or they could be related to a subtype with a small viral load and spread.
Figure 1. Maximum likelihood phylogenetic tree for the 47 truncated ORF8, using 500 bootstrap replications and the Hasegawa-Kishino-Yano model.
Nine group clades were found, while sequences 35 and 46 (marine blue and purple arrows, respectively) are phylogenetically near to the RATG13 ORF8 sequence. Sequence 15 is indicated by a red arrow.
In the second dataset there were all 47 truncated ORF8 variants, the RATG13 ORF8, as well as 66 representative ORF8 sequences from different Alpha, Beta, Gamma, Delta, Mu, GH/490R, and Omicron variants. Results of the phylogenetic analysis of this set containing all 47 sequences and different SARS-CoV-2 ORF8 variant representatives are shown in Fig. S3, where the resultant tree presented a highest log likelihood of −430.29.
This analysis involved 114 nucleotide sequences with a total of 81 positions in the final dataset. In this tree, one can find at least 14 group clades, and, as expected, almost all ORF8 variants are grouped together in the group I. The other 47 truncated ORF8 sequences presented similar tree topologies in comparison to the first dataset tree (cf. Figs. 1 and S3). On the other hand, the group IV showed that the sequences 15 and 40 formed a clear clade to the Alpha ORF8, what was expected. Furthermore, these sequences grouped with the ORF8 variant B.1.640, which was described as the new variant IHU found in France in December 2021 (Colson et al., 2021).
Evaluation of intrinsic disorder content of 47 T-ORF8 proteins
Unfortunately, no structural information is available for the truncated forms of ORF8. In fact, although two X-ray structures were reported for the dimeric form of the SARS-CoV-2 ORF8 protein, both of these structures were solved for the ORF8 sequences containing residues 18–121; i.e., they do not include information for more than a half (63%) of the N-terminal region of the full-length ORF8, which constitutes T-ORF8. Furthermore, truncated forms of ORF8 are relatively short to have independently foldable structure. It would be really important to conduct some structural analysis of the truncated ORF8 (e.g., by solution NMR). However, such an analysis could be complicated by the presence of two cysteine residues and by the highly hydrophobic nature of this region showing the mean hydrophobicity of 0.5926, which dramatically exceeds the mean hydrophobicity of typical globular proteins (~0.46 ± 0.05).
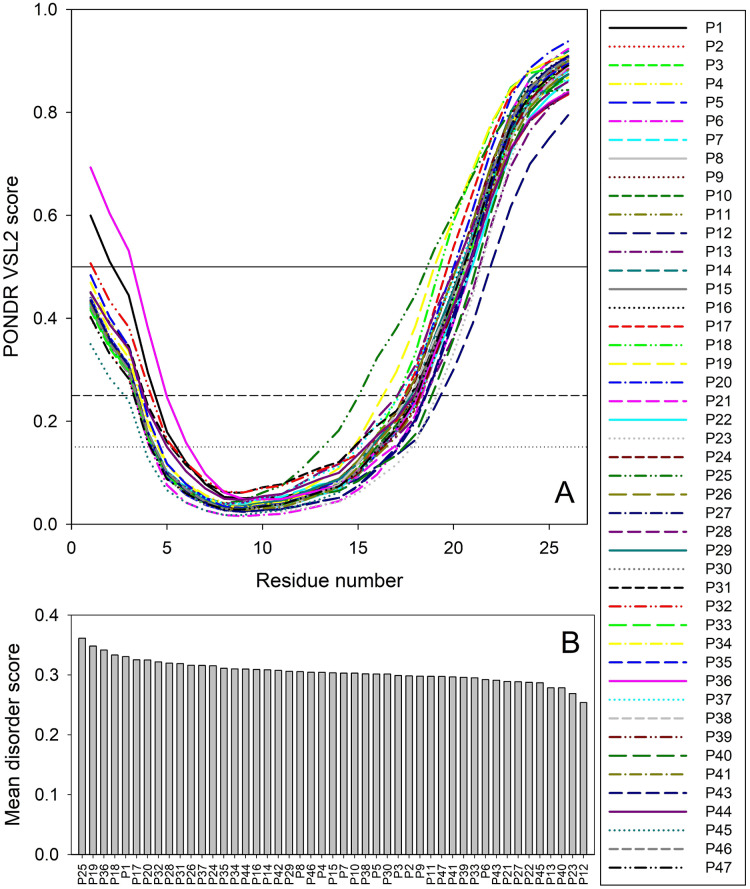
Therefore, to gain some structure-related information for the truncated forms of ORF8, we analyzed the peculiarities of the distribution of per-residue intrinsic disorder predisposition within sequences of the 47 T-ORF8 variants. Since the amino acid sequences of T-ORF8 proteins are shorter than 30 residues, the number of computational tools capable of predicting the intrinsic disorder is limited. In this study, we used the PONDR® VSL2 algorithm. The results of this analysis are shown in Fig. 2. Due to their short length and limited sequence variability, T-ORF8 proteins are characterized by rather featureless disorder profiles, where both N- and C-terminal regions are predicted to have higher levels of intrinsic disorder than the central parts.
Figure 2. Analysis of intrinsic disorder predisposition of 47 T-ORF8 proteins.
(A) Disorder profiles generated using the PONDR-VSL2 disorder predictor. Three thresholds of predicted disorder scores (PDSs) are shown, 0.15, 0.25, and 0.5, which are used for the classification of protein residues as highly disordered (PDS ≥ 0.5), flexible (0.25 ≤ PDS < 0.5), moderately flexible (0.15 ≤ PDS < 0.25) and mostly ordered (PDS < 0.15). B. Ranking of 47 T-ORF8 proteins based on their mean disorder scores.
Most T-ORF8 proteins show rather similar profiles, with the noticeable exceptions of P1 and P36, which show the highest disorder levels in their N-terminal regions. In contrast, P45 presents the least disorder at the N-terminus, P25 the longest and most peculiar disorder distribution in its C-terminal half, P18 and P19 long disorder stretches at their C-termini, and P12 the lowest levels of disorder in the C-terminal region (Fig. 2A). These observations are further supported by Fig. 2B, where the 47 T-ORF8 proteins are ranked based on their mean disorder scores, from the highest to the lowest levels of disorder. However, the vast majority of T-ORF8 proteins (38 of 47) form a rather uniform cluster with the average mean disorder score of 0.304 ± 0.010, whereas P25, P19, P36, P18, and P1 show higher than average and P13, P40, P23, and P12 lower than average levels of disorder.
Table S3 lists potential functional motifs identified in the 47 T-ORF8 variants by ELM resource and shows that all T-ORF8 proteins have several such motifs. Based on their content of functional motifs, T-ORF8 proteins can be grouped into 21 clusters, with three clusters containing 13, 4, and 2 proteins, respectively, and all the remaining being singletons. The common motif found in all T-ORF8 proteins is the N-degron that initiates protein degradation by binding to the UBR-box of N-recognins. A kinase docking motif that mediates interaction towards the ERK1/2 and P38 subfamilies of MAP kinases and a Ser/Thr (serine/threonine) residue phosphorylated by the Plk1 kinase are present in 20 clusters, whereas 17 clusters also include a site for attachment of a fucose residue to a serine. The lowest number of functional motifs (3) is found in 6 proteins (P12, P16, P17, P19, P21, and P40), many of which are characterized by lower mean disorder scores. On the contrary, proteins with the largest number of functional motifs (6 and 7) typically show higher disorder scores. Table S3 shows that truncation might generate functional T-ORF8 variants (or at least variants possessing functional motifs), and that expected functionality of different T-ORF8 proteins can be quite different. It is clear that the results of this computational analysis should be taken with caution, and the functionality of T-ORF8 requires experimental validation.
Variability and commonality of T-ORF8 variants
In the proceeding section, the quantification of unique T-ORF8 variants using various parameters such as polar/non-polar residue sequence homology, amino acid frequency distributions, amino acid conservation through the Shannon entropy, and physicochemical properties is described.
Polarity based variability of T-ORF8 variants
Each unique T-ORF8 variant possessed a binary polar/non-polar sequence and based on the sequence homology of these sequences, a phylogenetic relationship was obtained (Fig. S4). The number of polar and non-polar residues in the unique T-ORF8 variants was found to be almost balanced (50-50 in percentage). Among 26 residue positions of each T-ORF8 variant with the amino acid length of 26 residues, 14 positions (polar residues at positions 1, 5–7, 13 and non-polar residues at positions 2, 17–18, 20–23) remained invariant as illustrated by Table S4. The pairs of unique T-ORF8 variants (P5, P6), (P21, P40), (P4, P33), (P12, P13), (P28, P29), and (P9, P10) were closest to each other (Fig. S4).
Note that, the P15 variant was placed in a single leaf and found to be distant from the other unique ORF8 variants as per polarity-based homology, although P15 was closest to the T-ORF8 variants P13 and P14 based on amino acid homology. Furthermore, it was noticed that only 17 unique T-ORF8 variants possessed unique polar/non-polar sequences (Table S4). The polar/non-polar sequence of each T-ORF8 variant other than P4, P5, P15, and P28 was unique.
Surprisingly, among the total of 47 T-ORF8 variants, there were 28 T-ORF8 variants, which share identical polar/non-polar sequence with that of P15. According to the phylogenetic relationship derived from the unique polar/non-polar sequence homology, the T-ORF8 P15 was found to be closest to P42. Furthermore, the pairs (P13, P25), (P21, P40), and (P5, P30) were found to be close enough to each other (see Fig. S5).
Variability of the frequency distribution of amino acids present in T-ORF8 variants
The frequency of each amino acid present in the unique T-ORF8 variants was enumerated, and consequently, a twenty-dimensional frequency vector was obtained (Table S5). Tryptophan (Trp) was not present in any of the unique T-ORF8 variants. It was noted that the amino acids arginine (Arg), asparagine (Asn), aspartic acid (Asp), proline (Pro), and tyrosine (Tyr) were absent in the T-ORF8 P15. Arg was found with frequency one in the T-ORF8 P17, P39, P19, P22, and P33. In the P14 and P41 sequences, Asn was present with frequency one. Likewise, Asp was found in P38 and P11. Pro with frequency one, was found in the P8 variant only. Tyr was found in the T-ORF8 P20 and P23 variants. The highest frequency of 4 was seen for phenylalanine (Phe) in P3, P16, and P47, Leu in P10, P12, P24, P34, and P35, and threonine (Thr) in P29, P31, P32, and P42.
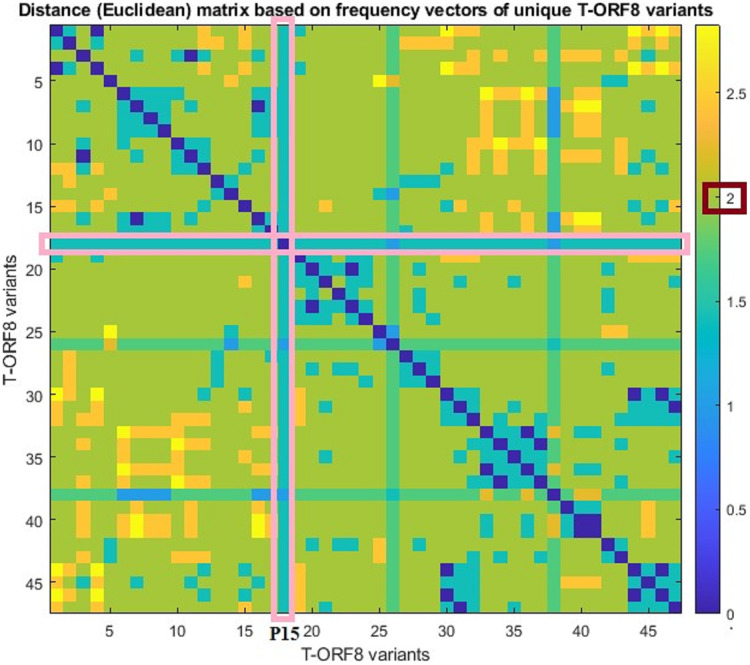
For each pair of frequency vectors corresponding to all unique T-ORF8 variants, Euclidean distances were calculated (Table S6), and the distance matrix in color heat-map is presented in Fig. 3. It was found that the P15 variant is equidistant (1.41) from all other variants except P30 and P40, which are one distance apart from P15. Further, we observed that the distance between any two pairs of T-ORF8 variants is two (light green color) except in a few cases (Fig. S6). Although the amino acid sequences were different, identical frequency vectors were found for the pair of ORF8 variants (P3, P47), (P2, P9), (P6, P13), (P17, P19), (P24, P34), (P24, P35), (P25, P36), (P34, P35), (P29, P42), and (P27, P43).
Figure 3. Pairwise distance matrix of amino acid frequency vectors of the unique T-ORF8 variants.
Based on the distance matrix, all unique T-ORF8 variants were clustered, and the associated phylogeny is presented in Fig. S6. The P15 variant was very close to P22, P23, P33, P40, and P41 according to the phylogenetic relationship depicted in Fig. S6. Other than the pairs of T-ORF8 having identical frequency vectors, it was found that the pairs of the unique T-ORF8 variants (P23, P33), (P14, P30), (P19, P20), and (P31, P32) were close to each other as derived from the phylogenetic relationship (Fig. S6).
Variability of T-ORF8 through Shannon entropy
Shannon entropy (SE) for each unique T-ORF8 variant was calculated using the formula stated in “Deep Phylogenetic Analyses” (Table S7). It was found that the highest and lowest SEs of the 47 unique T-ORF8 proteins were 0.958 and 0.973, respectively. That is, the length of the largest interval is 0.015, which is sufficiently small. Based on SEs of the T-ORF8 proteins a set of clusters were derived (Fig. S7A) SEs of each of the T-ORF8 variants are plotted in Fig. S7B. The largest cluster containing 18 T-ORF8 variants (including the T-ORF8 P15) based on the identical SEs were obtained (Fig. S7).
Molecular and physicochemical informatics of unique T-ORF8 variants
For each unique T-ORF8 variant and complete ORF8 protein, several physicochemical and molecular properties were computed using the web-servers. It was found that the extinction coefficient of all T-ORF8 variants was 125, except for four T-ORF8 variants, P16, P17, P18, and P19, whose extinction coefficient was zero (see Table S8). Further, it was noticed that for P20 and P23, extinction coefficients were found to be significantly higher compared to the others. Instability indices of all the T-ORF8 protein variants were ranging from 45.36 to 95.85 (greater than 40), and consequently they are all unstable. It was observed that the P15 variant had a unique frequency of the various types of residues (Tiny: 10, Small: 12, Aliphatic: 9, Aromatic: 4, Non-polar: 16, Polar: 10, Charged: 3, Basic: 2, Acidic: 1) and none of the other T-ORF8 variants was identical.
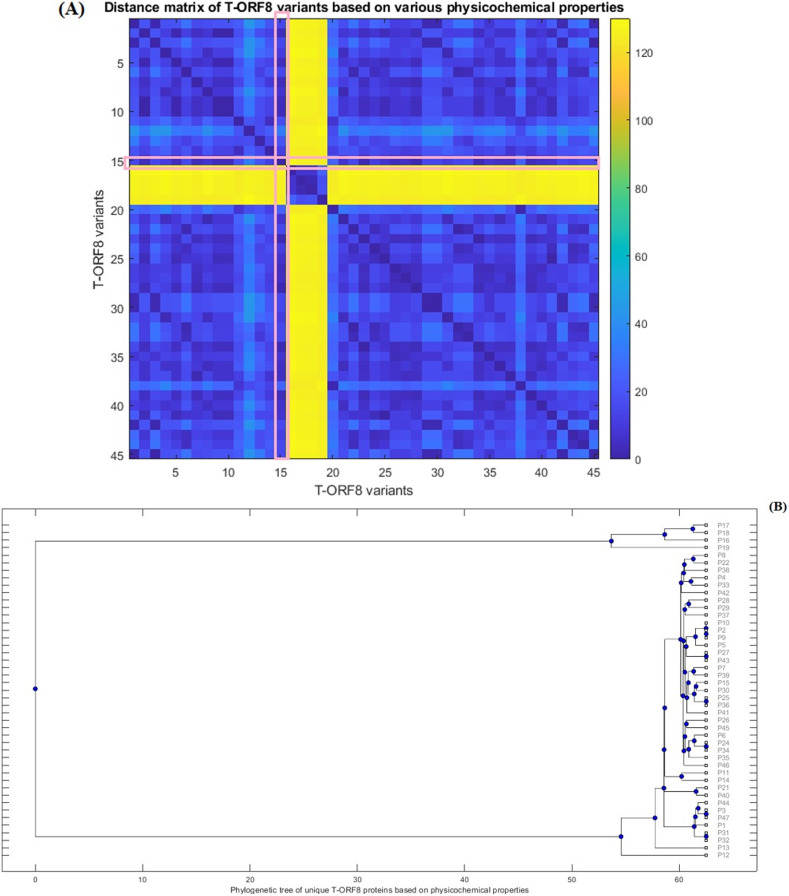
Furthermore, Euclidean distances between every pair of molecular and physicochemical property vectors corresponding to each T-ORF8 variant were computed and a phylogenetic relationship was derived (Fig. 4) based on the distance matrix (Table S9). Note that the property vectors of P20 and P30 were highly distant from the other ORF8 variants due to the huge difference in extinction coefficients (for P20, EC: 1490 and for P30, EC: 1615). So, ignoring these two ORF8 variants, the phylogenetic relationship among the remaining 45 T-ORF8 was derived. It was found that none of the T-ORF8 variants had identical property vectors to the P15 variant. It was further found from the phylogenetic relationship (Fig. 4B) that the pair of unique T-ORF8 variants (P17, P18), (P8, P22), (P4, P33), (P28, P29), (P2, P9), (P27, P43), (P7, P39), (P15, P30), (P25, P36), (P26, P45), (P24, P34), (P11, P14), (P21, P40), (P3, P47), and (P31, P32) were found to be the closest pairs based on the closeness of property vectors. Property vector distances from each 45 unique T-ORF8 variant from the P15 variant are presented in Table S10. In the close vicinity of P15, only the P25, P30, and P36 variants appeared based on the nearness of property vectors (Table S10).
Figure 4. Distance matrix of property vectors and derived phylogenetic tree of 45 T-ORF8 variants.
(A) The distance matrix; (B) phylogenetic tree based on physicochemical properties.
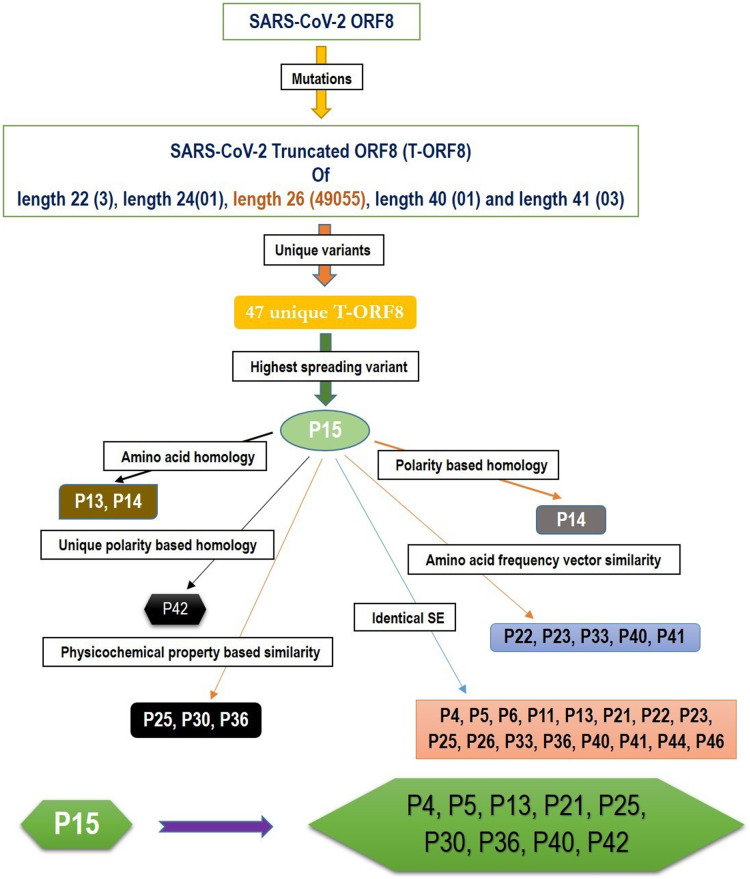
Possible T-ORF8 variants in the likelihood of P15 variant
Based on the amino acid sequence homology and other various features, such as the frequency distribution of amino acids, SE, and physicochemical properties of T-ORF8 variants, a possible cluster of nine unique T-ORF8 variants are derived. A schematic presentation is given in Fig. 5. All these nine unique T-ORF8 variants had unique polar/non-polar sequences as shown in Table S4. In addition to the P15 variant, these possible nine emerging variants are likely to appear in the B.1.1.7 lineage of SARS-CoV-2 in the near future. As of May 22nd, 2021, it was observed that 16 of 17 COVID-19 affected patients from India (mostly from Gujrat), were infected by the B.1.1.7 lineage of SARS-CoV-2 with the P15 variant, and only one patient (Accession: QVO43928) infected on February 28, 2021 with the SARS-CoV-2 strain with the P34 T-ORF8 variant, which had an identical polar/non-polar sequence as that of P15.
Figure 5. A schematic representation of a possible cluster of unique T-ORF8 variants which were residing in the likelihood of P15 variant.
Note: the frequency of each length of T-ORF8 protein was mentioned in parentheses. T-ORF8 variants mentioned in each box were found in the close likelihood of P15 T-ORF8 variants.
Discussion and Concluding Remarks
The ORF8 protein is 121 amino acid long with two genotypes (orf8L and orf8S). It has an Ig-like fold, is highly immunogenic, and interacts with 47 human proteins, 15 of them being drug targets interacting with MHC-I molecules leading to a significant down-regulation of their surface expression on various cell types (Rashid et al., 2021; Gordon et al., 2020; Gamage et al., 2020). As a result, inhibition of ORF8 could boost special immune surveillance and speed up SARS-CoV-2 eradication in vivo (Gamage et al., 2020). ORF8 is not like ORF3a, an ion channel (viroporin), implicated in virion assembly and membrane budding both in SARS-CoV and SARS-CoV-2. In contrast to SARS-CoV, which is not viable when lacking E and ORF3a proteins, and which requires the full-length E and ORF3a proteins for maximal replication and virulence (Barrantes, 2021; Castaño-Rodriguez et al., 2018; Tan et al., 2021), ORF8 in SASR-CoV-2 seems to only have a minor or no impact on the viral life cycle, as the virus can seemingly survive without a functional ORF8 protein, which has been demonstrated by the presence of many mutations and truncations detected in viable SARS-CoV-2 variants (Wang et al., 2020a, 2021). The Q27STOP mutation in the ORF8 protein has been discovered to cause 47 distinct truncated ORF8 variations. Furthermore, other truncated protein variants of different lengths 22, 24, 40, and 41 amino acids, were detected, although the frequency of occurrences of those variants was significantly lower (Table 2). In Colorado, one T-ORF8 variant of the length of 24 amino acids was detected on April 24, 2021, and this variant is likely to spread further in the future. Other truncated ORF8 variants of amino acids lengths of 22, 40, and 41, no longer appeared in new strains of SARS-CoV-2.
An important consequence of the ORF8 truncation is the alterations in the presentation of this protein by the human leukocyte antigen (HLA) complex on the surface of T-cells, which are among the key players in the immune response to viral infection. In fact, the development of the T-cell-based immunity is based on the presentation of short viral peptides on the cell surface by the HLA complex. Activation of killer CD8 T-cells depends on the recognition of viral peptides presented by HLA class I molecules, whereas activation of CD4 T lymphocytes (helper T-cells) is initiated by binding to a complex between viral peptides and HLA class II molecules (Klein & Sato, 2000). Although the major functions of the activated CD8 T-cells are the recognition and elimination of the infected cells, the main function of activated CD4 T-cells is regulation of immunity, including stimulation of antibody generation by B cells and enhancement of CD8 T-cell responses (Klein & Sato, 2000; Swain, McKinstry & Strutt, 2012). The overall importance of the T-cell-based responses in COVID-19 severity and long-term immunity has been documented in multiple reports (Wang et al., 2020b; Shkurnikov et al., 2021; Iturrieta-Zuazo et al., 2020; Bange et al., 2021; Grifoni et al., 2020; Peng et al., 2020; Dan et al., 2021). Therefore, it is not surprising that constant appearance of novel mutations in the SARS-CoV-2 genome can target T-cell epitopes (Agerer et al., 2021; Reynolds et al., 2021). Potential CD8 and CD4 epitopes represent peptides derived from the viral proteins, where 8- to 14-mers and 15- to 20-mers are serving as partners for HLA class I and class II receptors, respectively. The appearance of the premature stop codon in the ORF8 gene encoding the NS8 (ORF8) protein (Q27stop) not only generates the truncated form of this protein due to the deletion of almost 80% of the ORF8 protein, but also eliminates the whole immunopeptidome associated with this part of protein. Therefore, it is likely that such distortion in the immunopeptidome of ORF8 will dramatically affect its immunogenicity. Furthermore, mutations found in T-ORF8 could further modulate T-cell immunity.
Quantitative characteristics of the 47 unique truncated ORF8 protein variants were examined. All 47 T-ORF8 variants were found in North America, and only the P15 T-ORF8 variant was spread to four other continents: Africa, Asia, Europe and South America, until May 22, 2021. In this regard, it is pertinent to raise the question of whether there is any correlation between the spreading of all unique T-ORF8 variants and the epidemiological nature of North America. Within North America, it was reported that one of the top mutations, 27964C>T-(S24L) in the ORF8 protein, has an unusually strong gender dependence (Wang et al., 2021). The spread of the P15 variants over the 57 geo-locations across North America was noticed, and in addition, many patients from Asia, Africa, South America and Europe were infected by the particular B.1.1.7 variant of SARS-CoV-2, which contains the P15 variant. Like in many states of the US, also in the US territory of Guam and in North Dakota, most of the patients were noticed to have contracted the P15 variant of the B.1.1.7 lineage. Consequently, the present trend implies that a much higher spread of this lineage with this particular P15 variant is likely to occur. After Europe, the first case of the B.1.1.7 variant with the T-ORF8 P15 was discovered in Maryland in the US, but although later this strain remained limited in Maryland it spread further to other states, such as Florida and Minnesota (Table 3). Furthermore, this analysis reports a set of nine most likely T-ORF8 variants P4, P5, P13, P21, P25, P30, P36, P40, and P42, which were found to be residing in close vicinity of the P15 ORF8 variant. It was noticed that among 47 unique T-ORF8 variants, 28 of them had identical polar/non-polar sequences to that of the P15 variant. Considering the ability of the P15 variant to spread one can assume that the 28 variants with identical polar/non-polar sequences may spread in the near future and cause third, fourth, and fifth waves of COVID-19. As evidence, one patient from India was infected with SARS-CoV-2 with the P34 variant, which has the same polar/non-polar sequences as the P15 variant, as of May 22, 2021 (NCBI accession: QVO43928). The fact that T-ORF8 is still operating as ORF8, is an open issue that needs to be addressed. Reports try to link these T-ORF8 present in many lineages to COVID-19 severity and/or outcomes, effects that contribute to disease progression if associated with mutations in spike protein (Pereira, 2020; Guthmiller et al., 2021; Nagy, Pongor & Győrffy, 2021). It has also been reported that patients infected with SARS-CoV-2, lacking the majority of ORF8 protein, have a lower risk of aggravation, a conclusion that accrued variants in the spike, ORF8, and ORF3a proteins were associated with improved clinical outcomes (Esper et al., 2021; Young et al., 2020). More recently, SARS-CoV-2 strains were isolated in Washington state (USA), with a stop codon mutation generating a novel truncated and much shorter ORF8 protein, as well as in Hong Kong, which completely lacked ORF8 (gene, protein and antibody), ORF7a, and ORF7b (Esper et al., 2021; DeRonde et al., 2021; Tse et al., 2021). However, the in vitro analysis on Nasal Epithelial cells (NECs) infected with one of these isolates (ORF8-∆382) showed no significant functional differences between the wild type ORF8 and the ORF-∆382 mutant (Gamage et al., 2020). In contrast, Vero-6 cell infected with the same strain (ORF8-∆382) showed significantly higher replicative fitness in vitro than the wild type, while no difference was observed in the patient viral load, indicating that the deletion variant retained its replicative fitness (Su et al., 2020). In any case, the combinatorial clinical effects of T-ORF8 need to be investigated and analyzed in depth. It is necessary to investigate in detail the functions of T-ORF8 and the effects of this protein on inflammation and antigen-presenting ability. Finally, caution should be paid to using ORF8 as a diagnostic marker, as many immunoassay tests depend on antibody potency (Pereira, 2021). A systematic analysis of this protein and its specific antibodies is needed to determine the effects of these mutations/truncations on the diagnostic potential of the anti-ORF8 antibodies.
Supplemental Information
Funding Statement
The authors received no funding for this work.
Additional Information and Declarations
Competing Interests
Vasco Azevedo, Debmalya Barh and Vladimir N Uversky are Academic Editors for PeerJ.
Kenneth Lundstrom is employed by PanTherapeutics.
Author Contributions
Sk. Sarif Hassan conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Vaishnavi Kodakandla performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Elrashdy M. Redwan performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Kenneth Lundstrom conceived and designed the experiments, performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Pabitra Pal Choudhury performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Tarek Mohamed Abd El-Aziz performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Kazuo Takayama performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Ramesh Kandimalla performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Amos Lal performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Ángel Serrano-Aroca performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Gajendra Kumar Azad performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Alaa AA. Aljabali performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Giorgio Palù performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Gaurav Chauhan performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Parise Adadi performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Murtaza Tambuwala performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Adam M. Brufsky performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Wagner Baetas-da-Cruz performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Debmalya Barh performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Vasco Azevedo performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Nikolas G. Bazan performed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Bruno Silva Andrade conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Raner José Santana Silva performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Vladimir N. Uversky conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Data Availability
The following information was supplied regarding data availability:
The data are available in the article and the Supplemental File.
References
- Agerer et al. (2021).Agerer B, Koblischke M, Gudipati V, Montaño-Gutierrez LF, Smyth M, Popa A, Genger JW, Endler L, Florian DM, Mühlgrabner V, Graninger M, Aberle SW, Husa AM, Shaw LE, Lercher A, Gattinger P, Torralba-Gombau R, Trapin D, Penz T, Barreca D, Fae I, Wenda S, Traugott M, Walder G, Pickl WF, Thiel V, Allerberger F, Stockinger H, Puchhammer-Stöckl E, Weninger W, Fischer G, Hoepler W, Pawelka E, Zoufaly A, Valenta R, Bock C, Paster W, Geyeregger R, Farlik M, Halbritter F, Huppa JB, Aberle JH, Bergthaler A. SARS-CoV-2 mutations in MHC-I-restricted epitopes evade CD8 + T cell responses. Science Immunology. 2021;6(57):eabg6461. doi: 10.1126/sciimmunol.abg6461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhansa, Lakkis & El Zein (2021).Alkhansa A, Lakkis G, El Zein L. Mutational analysis of SARS-CoV-2 ORF8 during six months of COVID-19 pandemic. Gene Reports. 2021;23:101024. doi: 10.1016/j.genrep.2021.101024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bange et al. (2021).Bange EM, Han NA, Wileyto P, Kim JY, Gouma S, Robinson J, Greenplate AR, Hwee MA, Porterfield F, Owoyemi O, Naik K, Zheng C, Galantino M, Weisman AR, Ittner CAG, Kugler EM, Baxter AE, Oniyide O, Agyekum RS, Dunn TG, Jones TK, Giannini HM, Weirick ME, McAllister CM, Babady NE, Kumar A, Widman AJ, DeWolf S, Boutemine SR, Roberts C, Budzik KR, Tollett S, Wright C, Perloff T, Sun L, Mathew D, Giles JR, Oldridge DA, Wu JE, Alanio C, Adamski S, Garfall AL, Vella LA, Kerr SJ, Cohen JV, Oyer RA, Massa R, Maillard IP, Maxwell KN, Reilly JP, Maslak PG, Vonderheide RH, Wolchok JD, Hensley SE, Wherry EJ, Meyer NJ, DeMichele AM, Vardhana SA, Mamtani R, Huang AC. CD8+ T cells contribute to survival in patients with COVID-19 and hematologic cancer. Nature Medicine. 2021;27(7):1280–1289. doi: 10.1038/s41591-021-01386-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrantes (2021).Barrantes FJ. Structural biology of coronavirus ion channels. Acta Crystallographica Section D: Structural Biology. 2021;77(Pt 4):391–402. doi: 10.1107/S2059798321001431. [DOI] [PubMed] [Google Scholar]
- Benvenuto et al. (2020).Benvenuto D, Giovanetti M, Salemi M, Prosperi M, De Flora C, Junior Alcantara LC, Angeletti S, Ciccozzi M. The global spread of 2019-nCoV: a molecular evolutionary analysis. Pathogens and Global Health. 2020;114(2):64–67. doi: 10.1080/20477724.2020.1725339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges et al. (2021).Borges V, Sousa C, Menezes L, Gonçalves AM, Picão M, Almeida JP, Vieita M, Santos R, Silva AR, Costa M, Carneiro L. Tracking SARS-CoV-2 VOC 202012/01 (lineage B. 1.1. 7) dissemination in Portugal: insights from nationwide RT-PCR Spike gene drop out data. Eurosurveillance. 2021;26:2100131. doi: 10.2807/1560-7917.ES.2021.26.10.2100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broome & Hecht (2000).Broome BM, Hecht MH. Nature disfavors sequences of alternating polar and non-polar amino acids: implications for amyloidogenesis. Journal of Molecular Biology. 2000;296(4):961–968. doi: 10.1006/jmbi.2000.3514. [DOI] [PubMed] [Google Scholar]
- Castaño-Rodriguez et al. (2018).Castaño-Rodriguez C, Honrubia JM, Gutiérrez-Álvarez J, DeDiego ML, Nieto-Torres JL, Jimenez-Guardeño JM, Regla-Nava JA, Fernandez-Delgado R, Verdia-Báguena C, Queralt-Martín M, Kochan G, Perlman S, Aguilella VM, Sola I, Enjuanes L. Role of severe acute respiratory syndrome coronavirus viroporins E, 3a, and 8a in replication and pathogenesis. mBio. 2018;9(3):e02325. doi: 10.1128/mBio.02325-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chasapis et al. (2021).Chasapis CT, Georgiopoulou AK, Perlepes SP, Bjørklund G, Peana M. A SARS-CoV-2-human metalloproteome interaction map. Journal of Inorganic Biochemistry. 2021;219:111423. doi: 10.1016/j.jinorgbio.2021.111423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colson et al. (2021).Colson P, Delerce J, Burel E, Dahan J, Jouffret A, Fenollar F, Yahi N, Fantini J, La Scola B, Raoult D. Emergence in Southern France of a new SARS-CoV-2 variant of probably Cameroonian origin harbouring both substitutions N501Y and E484K in the spike protein. medRxiv. 2021 doi: 10.1101/2021.12.24.21268174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dan et al. (2021).Dan JM, Mateus J, Kato Y, Hastie KM, Yu ED, Faliti CE, Grifoni A, Ramirez SI, Haupt S, Frazier A, Nakao C, Rayaprolu V, Rawlings SA, Peters B, Krammer F, Simon V, Saphire EO, Smith DM, Weiskopf D, Sette A, Crotty S. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021;371(6529):eabf4063. doi: 10.1126/science.abf4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies et al. (2021).Davies NG, Abbott S, Barnard RC, Jarvis CI, Kucharski AJ, Munday JD, Pearson CAB, Russell TW, Tully DC, Washburne AD, Wenseleers T, Gimma A, Waites W, Wong KLM, van Zandvoort K, Silverman JD, CMMID COVID-19 Working Group; COVID-19 Genomics UK (COG-UK) Consortium. Diaz-Ordaz K, Keogh R, Eggo RM, Funk S, Jit M, Atkins KE, Edmunds WJ. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science. 2021;372(6538):eabg3055. doi: 10.1126/science.abg3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRonde et al. (2021).DeRonde S, Deuling H, Parker J, Chen J. Identification of a novel SARS-CoV-2 strain with truncated protein in ORF8 gene by next generation sequencing. Research Square. 2021;rs.3.rs:413141. doi: 10.21203/rs.3.rs-413141/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz (2020).Díaz J. SARS-CoV-2 molecular network structure. Frontiers in Physiology. 2020;11:870. doi: 10.3389/fphys.2020.00870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esper et al. (2021).Esper FP, Cheng YW, Adhikari TM, Tu ZJ, Li D, Li EA, Farkas DH, Procop GW, Ko JS, Chan TA, Jehi L, Rubin BP, Li J. Genomic epidemiology of SARS-CoV-2 infection during the initial pandemic wave and association with disease severity. JAMA Network Open. 2021;4(4):e217746. doi: 10.1001/jamanetworkopen.2021.7746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flower et al. (2021).Flower TG, Buffalo CZ, Hooy RM, Allaire M, Ren X, Hurley JH. Structure of SARS-CoV-2 ORF8, a rapidly evolving immune evasion protein. Proceedings of the National Academy of Sciences of the United States of America. 2021;118(2):e2021785118. doi: 10.1073/pnas.2021785118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanet et al. (2021).Fontanet A, Autran B, Lina B, Kieny MP, Karim SSA, Sridhar D. SARS-CoV-2 variants and ending the COVID-19 pandemic. Lancet. 2021;397(10278):952–954. doi: 10.1016/S0140-6736(21)00370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frampton et al. (2021).Frampton D, Rampling T, Cross A, Bailey H, Heaney J, Byott M, Scott R, Sconza R, Price J, Margaritis M, Bergstrom M, Spyer MJ, Miralhes PB, Grant P, Kirk S, Valerio C, Mangera Z, Prabhahar T, Moreno-Cuesta J, Arulkumaran N, Singer M, Shin GY, Sanchez E, Paraskevopoulou SM, Pillay D, McKendry RA, Mirfenderesky M, Houlihan CF, Nastouli E. Genomic characteristics and clinical effect of the emergent SARS-CoV-2 B.1.1.7 lineage in London, UK: a whole-genome sequencing and hospital-based cohort study. Lancet Infectious Diseases. 2021;21(9):1246–1256. doi: 10.1016/S1473-3099(21)00170-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway et al. (2021).Galloway SE, Paul P, MacCannell DR, Johansson MA, Brooks JT, MacNeil A, Slayton RB, Tong S, Silk BJ, Armstrong GL, Biggerstaff M, Dugan VG. Emergence of SARS-CoV-2 B.1.1.7 Lineage—United States, December 29, 2020–January 12, 2021. MMWR–Morbidity and Mortality Weekly Report. 2021;70(3):95–99. doi: 10.15585/mmwr.mm7003e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamage et al. (2020).Gamage AM, Tan KS, Chan WOY, Liu J, Tan CW, Ong YK, Thong M, Andiappan AK, Anderson DE, Wang Y, Wang LF. Infection of human Nasal Epithelial Cells with SARS-CoV-2 and a 382-nt deletion isolate lacking ORF8 reveals similar viral kinetics and host transcriptional profiles. PLOS Pathogens. 2020;16(12):e1009130. doi: 10.1371/journal.ppat.1009130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasteiger et al. (2005).Gasteiger E, Hoogland C, Gattiker A, Wilkins MR, Appel RD, Bairoch A. The Proteomics Protocols Handbook. Totowa: Humana Press; 2005. Protein identification and analysis tools on the ExPASy server; pp. 571–607. [Google Scholar]
- Gordon et al. (2020).Gordon DE, Jang GM, Bouhaddou M, Xu J, Obernier K, White KM, O’Meara MJ, Rezelj VV, Guo JZ, Swaney DL, Tummino TA, Hüttenhain R, Kaake RM, Richards AL, Tutuncuoglu B, Foussard H, Batra J, Haas K, Modak M, Kim M, Haas P, Polacco BJ, Braberg H, Fabius JM, Eckhardt M, Soucheray M, Bennett MJ, Cakir M, McGregor MJ, Li Q, Meyer B, Roesch F, Vallet T, Mac Kain A, Miorin L, Moreno E, Naing ZZC, Zhou Y, Peng S, Shi Y, Zhang Z, Shen W, Kirby IT, Melnyk JE, Chorba JS, Lou K, Dai SA, Barrio-Hernandez I, Memon D, Hernandez-Armenta C, Lyu J, Mathy CJP, Perica T, Pilla KB, Ganesan SJ, Saltzberg DJ, Rakesh R, Liu X, Rosenthal SB, Calviello L, Venkataramanan S, Liboy-Lugo J, Lin Y, Huang XP, Liu Y, Wankowicz SA, Bohn M, Safari M, Ugur FS, Koh C, Savar NS, Tran QD, Shengjuler D, Fletcher SJ, O’Neal MC, Cai Y, Chang JCJ, Broadhurst DJ, Klippsten S, Sharp PP, Wenzell NA, Kuzuoglu-Ozturk D, Wang HY, Trenker R, Young JM, Cavero DA, Hiatt J, Roth TL, Rathore U, Subramanian A, Noack J, Hubert M, Stroud RM, Frankel AD, Rosenberg OS, Verba KA, Agard DA, Ott M, Emerman M, Jura N, von Zastrow M, Verdin E, Ashworth A, Schwartz O, d’Enfert C, Mukherjee S, Jacobson M, Malik HS, Fujimori DG, Ideker T, Craik CS, Floor SN, Fraser JS, Gross JD, Sali A, Roth BL, Ruggero D, Taunton J, Kortemme T, Beltrao P, Vignuzzi M, García-Sastre A, Shokat KM, Shoichet BK, Krogan NJ. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature. 2020;583(7816):459–468. doi: 10.1038/s41586-020-2286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grifoni et al. (2020).Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, Rawlings SA, Sutherland A, Premkumar L, Jadi RS, Marrama D, de Silva AM, Frazier A, Carlin AF, Greenbaum JA, Peters B, Krammer F, Smith DM, Crotty S, Sette A. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181(7):1489–1501.e15. doi: 10.1016/j.cell.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guthmiller et al. (2021).Guthmiller JJ, Stovicek O, Wang J, Changrob S, Li L, Halfmann P, Zheng NY, Utset H, Stamper CT, Dugan HL, Miller WD, Huang M, Dai YN, Nelson CA, Hall PD, Jansen M, Shanmugarajah K, Donington JS, Krammer F, Fremont DH, Joachimiak A, Kawaoka Y, Tesic V, Madariaga ML, Wilson PC. SARS-CoV-2 infection severity is linked to superior humoral immunity against the spike. mBio. 2021;12(1):e02940. doi: 10.1128/mBio.02940-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hachim et al. (2020).Hachim A, Kavian N, Cohen CA, Chin AWH, Chu DKW, Mok CKP, Tsang OTY, Yeung YC, Perera RAPM, Poon LLM, Peiris JSM, Valkenburg SA. ORF8 and ORF3b antibodies are accurate serological markers of early and late SARS-CoV-2 infection. Nature Immunology. 2020;21(10):1293–1301. doi: 10.1038/s41590-020-0773-7. [DOI] [PubMed] [Google Scholar]
- Hasegawa, Kishino & Yano (1985).Hasegawa M, Kishino H, Yano T. Dating of the human-ape splitting by a molecular clock of mitochondrial DNA. Journal of Molecular Evolution. 1985;22(2):160–174. doi: 10.1007/BF02101694. [DOI] [PubMed] [Google Scholar]
- Hassan et al. (2021a).Hassan SS, Aljabali AAA, Panda PK, Ghosh S, Attrish D, Choudhury PP, Seyran M, Pizzol D, Adadi P, Abd El-Aziz TM, Soares A, Kandimalla R, Lundstrom K, Lal A, Azad GK, Uversky VN, Sherchan SP, Baetas-da-Cruz W, Uhal BD, Rezaei N, Chauhan G, Barh D, Redwan EM, Dayhoff GW, II, Bazan NG, Serrano-Aroca Á, El-Demerdash A, Mishra YK, Palu G, Takayama K, Brufsky AM, Tambuwala MM. A unique view of SARS-CoV-2 through the lens of ORF8 protein. Computers in Biology and Medicine. 2021a;133(8):104380. doi: 10.1016/j.compbiomed.2021.104380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan et al. (2021b).Hassan SS, Attrish D, Ghosh S, Choudhury PP, Roy B. Pathogenic perspective of missense mutations of ORF3a protein of SARS-CoV-2. Virus Research. 2021b;300(1):198441. doi: 10.1016/j.virusres.2021.198441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan et al. (2021c).Hassan SS, Attrish D, Ghosh S, Choudhury PP, Uversky VN, Aljabali AAA, Lundstrom K, Uhal BD, Rezaei N, Seyran M, Pizzol D, Adadi P, Soares A, Abd El-Aziz TM, Kandimalla R, Tambuwala MM, Azad GK, Sherchan SP, Baetas-da-Cruz W, Lal A, Palù G, Takayama K, Serrano-Aroca Á, Barh D, Brufsky AM. Notable sequence homology of the ORF10 protein introspects the architecture of SARS-CoV-2. International Journal of Biological Macromolecules. 2021c;181(5):801–809. doi: 10.1016/j.ijbiomac.2021.03.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan et al. (2020a).Hassan SS, Choudhury PP, Basu P, Jana SS. Molecular conservation and differential mutation on ORF3a gene in Indian SARS-CoV2 genomes. Genomics. 2020a;112(5):3226–3237. doi: 10.1016/j.ygeno.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan, Choudhury & Roy (2021).Hassan SS, Choudhury PP, Roy B. Rare mutations in the accessory proteins ORF6, ORF7b, and ORF10 of the SARS-CoV-2 genomes. Meta Gene. 2021;28(18):100873. doi: 10.1016/j.mgene.2021.100873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan et al. (2020b).Hassan SS, Choudhury PP, Roy B, Jana SS. Missense mutations in SARS-CoV2 genomes from Indian patients. Genomics. 2020b;112(6):4622–4627. doi: 10.1016/j.ygeno.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan et al. (2020c).Hassan SS, Ghosh S, Attrish D, Choudhury PP, Aljabali AAA, Uhal BD, Lundstrom K, Rezaei N, Uversky VN, Seyran M, Pizzol D, Adadi P, Soares A, El-Aziz TMA, Kandimalla R, Tambuwala MM, Azad GK, Sherchan SP, Baetas-da-Cruz W, Takayama K, Serrano-Aroca Á, Chauhan G, Palu G, Brufsky AM. Possible transmission flow of SARS-CoV-2 based on ACE2 features. Molecules. 2020c;25(24):5906. doi: 10.3390/molecules25245906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebditch et al. (2017).Hebditch M, Carballo-Amador MA, Charonis S, Curtis R, Warwicker J. Protein-Sol: a web tool for predicting protein solubility from sequence. Bioinformatics. 2017;33(19):3098–3100. doi: 10.1093/bioinformatics/btx345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu et al. (2021).Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nature Reviews Microbiology. 2021;19(3):141–154. doi: 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iturrieta-Zuazo et al. (2020).Iturrieta-Zuazo I, Rita CG, García-Soidán A, de Malet Pintos-Fonseca A, Alonso-Alarcón N, Pariente-Rodríguez R, Tejeda-Velarde A, Serrano-Villar S, Castañer-Alabau JL, Nieto-Gañán I. Possible role of HLA class-I genotype in SARS-CoV-2 infection and progression: a pilot study in a cohort of COVID-19 Spanish patients. Clinical Immunology. 2020;219(13):108572. doi: 10.1016/j.clim.2020.108572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein & Sato (2000).Klein J, Sato A. The HLA system. First of two parts. New England Journal of Medicine. 2000;343(10):702–709. doi: 10.1056/NEJM200009073431006. [DOI] [PubMed] [Google Scholar]
- Koyama, Platt & Parida (2020).Koyama T, Platt D, Parida L. Variant analysis of SARS-CoV-2 genomes. Bulletin of the World Health Organization. 2020;98(7):495–504. doi: 10.2471/BLT.20.253591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar et al. (2020).Kumar M, Gouw M, Michael S, Sámano-Sánchez H, Pancsa R, Glavina J, Diakogianni A, Valverde JA, Bukirova D, Čalyševa J, Palopoli N, Davey NE, Chemes LB, Gibson TJ. ELM-the eukaryotic linear motif resource in 2020. Nucleic Acids Research. 2020;48(D1):D296–D306. doi: 10.1093/nar/gkz1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar et al. (2018).Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X: molecular evolutionary genetics analysis across computing platforms. Molecular Biology and Evolution. 2018;35(6):1547–1549. doi: 10.1093/molbev/msy096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2020).Li JY, Liao CH, Wang Q, Tan YJ, Luo R, Qiu Y, Ge XY. The ORF6, ORF8 and nucleocapsid proteins of SARS-CoV-2 inhibit type I interferon signaling pathway. Virus Research. 2020;286(1):198074. doi: 10.1016/j.virusres.2020.198074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2021).Li R, Ma X, Deng J, Chen Q, Liu W, Peng Z, Qiao Y, Lin Y, He X, Zhang H. Differential efficiencies to neutralize the novel mutants B.1.1.7 and 501Y.V2 by collected sera from convalescent COVID-19 patients and RBD nanoparticle-vaccinated rhesus macaques. Cellular & Molecular Immunology. 2021;18(4):1058–1060. doi: 10.1038/s41423-021-00641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madeira et al. (2019).Madeira F, Park YM, Lee J, Buso N, Gur T, Madhusoodanan N, Basutkar P, Tivey ARN, Potter SC, Finn RD, Lopez R. The EMBL-EBI search and sequence analysis tools APIs in 2019. Nucleic Acids Research. 2019;47(W1):W636–W641. doi: 10.1093/nar/gkz268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson & Lehner (2020).Matheson NJ, Lehner PJ. How does SARS-CoV-2 cause COVID-19? Science. 2020;369(6503):510–511. doi: 10.1126/science.abc6156. [DOI] [PubMed] [Google Scholar]
- Mercatelli & Giorgi (2020).Mercatelli D, Giorgi FM. Geographic and genomic distribution of SARS-CoV-2 mutations. Frontiers in Microbiology. 2020;11:1800. doi: 10.3389/fmicb.2020.01800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad et al. (2020).Mohammad S, Bouchama A, Mohammad Alharbi B, Rashid M, Saleem Khatlani T, Gaber NS, Malik SS. SARS-CoV-2 ORF8 and SARS-CoV ORF8ab: genomic divergence and functional convergence. Pathogens. 2020;9(9):677. doi: 10.3390/pathogens9090677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagy, Pongor & Győrffy (2021).Nagy Á, Pongor S, Győrffy B. Different mutations in SARS-CoV-2 associate with severe and mild outcome. International Journal of Antimicrobial Agents. 2021;57(2):106272. doi: 10.1016/j.ijantimicag.2020.106272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Necci, Piovesan & Tosatto (2021).Necci M, Piovesan D, CAID Predictors; DisProt Curators. Tosatto SCE. Critical assessment of protein intrinsic disorder prediction. Nature Methods. 2021;18(5):472–481. doi: 10.1038/s41592-021-01117-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obradovic et al. (2005).Obradovic Z, Peng K, Vucetic S, Radivojac P, Dunker AK. Exploiting heterogeneous sequence properties improves prediction of protein disorder. Proteins-structure Function and Bioinformatics. 2005;61(Suppl 7):176–182. doi: 10.1002/(ISSN)1097-0134. [DOI] [PubMed] [Google Scholar]
- Peng et al. (2020).Peng Y, Mentzer AJ, Liu G, Yao X, Yin Z, Dong D, Dejnirattisai W, Rostron T, Supasa P, Liu C, López-Camacho C, Slon-Campos J, Zhao Y, Stuart DI, Paesen GC, Grimes JM, Antson AA, Bayfield OW, Hawkins DEDP, Ker DS, Wang B, Turtle L, Subramaniam K, Thomson P, Zhang P, Dold C, Ratcliff J, Simmonds P, de Silva T, Sopp P, Wellington D, Rajapaksa U, Chen YL, Salio M, Napolitani G, Paes W, Borrow P, Kessler BM, Fry JW, Schwabe NF, Semple MG, Baillie JK, Moore SC, Openshaw PJM, Ansari MA, Dunachie S, Barnes E, Frater J, Kerr G, Goulder P, Lockett T, Levin R, Zhang Y, Jing R, Ho LP, Cornall RJ, Conlon CP, Klenerman P, Screaton GR, Mongkolsapaya J, McMichael A, Knight JC, Ogg G, Dong T. Oxford Immunology network COVID-19 response T cell consortium; ISARIC4C investigators, broad and strong memory CD4+ and CD8+ T cells induced by SARS-CoV-2 in UK convalescent individuals following COVID-19. Nature Immunology. 2020;21(11):1336–1345. doi: 10.1038/s41590-020-0782-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perchetti et al. (2021).Perchetti GA, Zhu H, Mills MG, Shrestha L, Wagner C, Bakhash SM, Lin MJ, Xie H, Huang ML, Mathias P, Bedford T, Jerome KR, Greninger AL, Roychoudhury P. Specific allelic discrimination of N501Y and other SARS-CoV-2 mutations by ddPCR detects B.1.1.7 lineage in Washington State. Journal of Medical Virology. 2021;93(10):5931–5941. doi: 10.1002/jmv.27155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira (2020).Pereira F. Evolutionary dynamics of the SARS-CoV-2 ORF8 accessory gene. Infection Genetics and Evolution. 2020;85:104525. doi: 10.1016/j.meegid.2020.104525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira (2021).Pereira F. SARS-CoV-2 variants lacking a functional ORF8 may reduce accuracy of serological testing. Journal of Immunological Methods. 2021;488:112906. doi: 10.1016/j.jim.2020.112906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramírez et al. (2021).Ramírez JD, Muñoz M, Patiño LH, Ballesteros N, Paniz-Mondolfi A. Will the emergent SARS-CoV2 B.1.1.7 lineage affect molecular diagnosis of COVID-19? Journal of Medical Virology. 2021;93(5):2566–2568. doi: 10.1002/jmv.26823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashid et al. (2021).Rashid F, Dzakah EE, Wang H, Tang S. The ORF8 protein of SARS-CoV-2 induced endoplasmic reticulum stress and mediated immune evasion by antagonizing production of interferon beta. Virus Research. 2021;296:198350. doi: 10.1016/j.virusres.2021.198350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren et al. (2020).Ren Y, Shu T, Wu D, Mu J, Wang C, Huang M, Han Y, Zhang XY, Zhou W, Qiu Y, Zhou X. The ORF3a protein of SARS-CoV-2 induces apoptosis in cells. Cellular & Molecular Immunology. 2020;17(8):881–883. doi: 10.1038/s41423-020-0485-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds et al. (2021).Reynolds CJ, Pade C, Gibbons JM, Butler DK, Otter AD, Menacho K, Fontana M, Smit A, Sackville-West JE, Cutino-Moguel T, Maini MK, Chain B, Noursadeghi M, Brooks T, Semper A, Manisty C, Treibel TA, Moon JC, Valdes AM, McKnight Áine, Altmann DM, Boyton R, Abbass H, Abiodun A, Alfarih M, Alldis Z, Altmann DM, Amin OE, Andiapen M, Artico J, Augusto Jão B, Baca GL, Bailey SNL, Bhuva AN, Boulter A, Bowles R, Boyton RJ, Bracken OV, O’Brien B, Brooks T, Bullock N, Butler DK, Captur G, Champion N, Chan C, Chandran A, Collier D, Couto de Sousa J, Couto-Parada X, Cutino-Moguel T, Davies RH, Douglas B, Di Genova C, Dieobi-Anene K, Diniz MO, Ellis A, Feehan K, Finlay M, Fontana M, Forooghi N, Gaier C, Gibbons JM, Gilroy D, Hamblin M, Harker G, Hewson J, Heywood W, Hickling LM, Hingorani AD, Howes L, Hughes A, Hughes G, Hughes R, Itua I, Jardim V, Lee W-YJ, Jensen M, Jones J, Jones M, Joy G, Kapil V, Kurdi H, Lambourne J, Lin K-M, Louth S, Maini MK, Mandadapu V, Manisty C, McKnight Áine, Menacho K, Mfuko C, Mills K, Mitchelmore O, Moon C, Moon JC, Munoz-Sandoval D, Murray SM, Noursadeghi M, Otter A, Pade C, Palma S, Parker R, Patel K, Pawarova B, Petersen SE, Piniera B, Pieper FP, Pope D, Prossora M, Rannigan L, Rapala A, Reynolds CJ, Richards A, Robathan M, Rosenheim J, Sambile G, Schmidt NM, Semper A, Seraphim A, Simion M, Smit A, Sugimoto M, Swadling L, Taylor S, Temperton N, Thomas S, Thornton GD, Treibel TA, Tucker A, Veerapen J, Vijayakumar M, Welch S, Wodehouse T, Wynne L, Zahedi D, Chain B. Prior SARS-CoV-2 infection rescues B and T cell responses to variants after first vaccine dose. Science. 2021;30(6549):1418–1423. doi: 10.1126/science.abh1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sengupta, Hassan & Choudhury (2021).Sengupta A, Hassan SS, Choudhury PP. Clade GR and clade GH isolates of SARS-CoV-2 in Asia show highest amount of SNPs. Infection Genetics and Evolution. 2021;89(5):104724. doi: 10.1016/j.meegid.2021.104724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen et al. (2021).Shen X, Tang H, McDanal C, Wagh K, Fischer W, Theiler J, Yoon H, Li D, Haynes BF, Sanders KO, Gnanakaran S, Hengartner N, Pajon R, Smith G, Glenn GM, Korber B, Montefiori DC. SARS-CoV-2 variant B.1.1.7 is susceptible to neutralizing antibodies elicited by ancestral spike vaccines. Cell Host & Microbe. 2021;29(4):529–539.e3. doi: 10.1016/j.chom.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shkurnikov et al. (2021).Shkurnikov M, Nersisyan S, Jankevic T, Galatenko A, Gordeev I, Vechorko V, Tonevitsky A. Association of HLA class I genotypes with severity of coronavirus disease-19. Frontiers in Immunology. 2021;12:641900. doi: 10.3389/fimmu.2021.641900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stecher, Tamura & Kumar (2020).Stecher G, Tamura K, Kumar S. Molecular evolutionary genetics analysis (MEGA) for macOS. Molecular Biology and Evolution. 2020;37(4):1237–1239. doi: 10.1093/molbev/msz312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strait & Dewey (1996).Strait BJ, Dewey TG. The Shannon information entropy of protein sequences. Biophysical Journal. 1996;71(1):148–155. doi: 10.1016/S0006-3495(96)79210-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stukalov et al. (2021).Stukalov A, Girault V, Grass V, Karayel O, Bergant V, Urban C, Haas DA, Huang Y, Oubraham L, Wang A, Hamad MS, Piras A, Hansen FM, Tanzer MC, Paron I, Zinzula L, Engleitner T, Reinecke M, Lavacca TM, Ehmann R, Wölfel R, Jores J, Kuster B, Protzer U, Rad R, Ziebuhr J, Thiel V, Scaturro P, Mann M, Pichlmair A. Multilevel proteomics reveals host perturbations by SARS-CoV-2 and SARS-CoV. Nature. 2021;594(7862):246–252. doi: 10.1038/s41586-021-03493-4. [DOI] [PubMed] [Google Scholar]
- Su et al. (2020).Su YCF, Anderson DE, Young BE, Linster M, Zhu F, Jayakumar J, Zhuang Y, Kalimuddin S, Low JGH, Tan CW, Chia WN, Mak TM, Octavia S, Chavatte JM, Lee RTC, Pada S, Tan SY, Sun L, Yan GZ, Maurer-Stroh S, Mendenhall IH, Leo YS, Lye DC, Wang LF, Smith GJD. Discovery and genomic characterization of a 382-nucleotide deletion in ORF7b and ORF8 during the early evolution of SARS-CoV-2. mBio. 2020;11(4):e01610. doi: 10.1128/mBio.01610-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swain, McKinstry & Strutt (2012).Swain SL, McKinstry KK, Strutt TM. Expanding roles for CD4+ T cells in immunity to viruses. Nature Reviews Immunology. 2012;12(2):136–148. doi: 10.1038/nri3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan et al. (2021).Tan Y, Schneider T, Shukla PK, Chandrasekharan MB, Aravind L, Zhang D. Unification and extensive diversification of M/Orf3-related ion channel proteins in coronaviruses and other nidoviruses. Virus Evolution. 2021;7(1):veab014. doi: 10.1093/ve/veab014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse et al. (2021).Tse H, Lung DC, Wong SC, Ip KF, Wu TC, To KK, Kok KH, Yuen KY, Choi GK. Emergence of a severe acute respiratory syndrome coronavirus 2 virus variant with novel genomic architecture in Hong Kong. Clinical Infectious Diseases. 2021;73(9):1696–1699. doi: 10.1093/cid/ciab198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velazquez-Salinas et al. (2020).Velazquez-Salinas L, Zarate S, Eberl S, Gladue DP, Novella I, Borca MV. Positive selection of ORF1ab, ORF3a, and ORF8 genes drives the early evolutionary trends of SARS-CoV-2 during the 2020 COVID-19 pandemic. Frontiers in Microbiology. 2020;11:550674. doi: 10.3389/fmicb.2020.550674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walensky, Walke & Fauci (2021).Walensky RP, Walke HT, Fauci AS. SARS-CoV-2 variants of concern in the United States-challenges and opportunities. JAMA. 2021;325(11):1037–1038. doi: 10.1001/jama.2021.2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2021).Wang R, Chen J, Gao K, Hozumi Y, Yin C, Wei GW. Analysis of SARS-CoV-2 mutations in the United States suggests presence of four substrains and novel variants. Communications Biology. 2021;4(1):228. doi: 10.1038/s42003-021-01754-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2020a).Wang X, Lam JY, Wong WM, Yuen CK, Cai JP, Au SW, Chan JF, To KKW, Kok KH, Yuen KY. Accurate diagnosis of COVID-19 by a novel immunogenic secreted SARS-CoV-2 orf8 protein. mBio. 2020a;11(5):e02431. doi: 10.1128/mBio.02431-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2020b).Wang Z, Yang X, Zhou Y, Sun J, Liu X, Zhang J, Mei X, Zhong J, Zhao J, Ran P. COVID-19 severity correlates with weaker T-cell immunity, hypercytokinemia, and lung epithelium injury. American Journal of Respiratory and Critical Care Medicine. 2020b;202(4):606–610. doi: 10.1164/rccm.202005-1701LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu et al. (2021).Wu S, Tian C, Liu P, Guo D, Zheng W, Huang X, Zhang Y, Liu L. Effects of SARS-CoV-2 mutations on protein structures and intraviral protein-protein interactions. Journal of Medical Virology. 2021;93(4):2132–2140. doi: 10.1002/jmv.26597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu et al. (2020).Wu D, Wu T, Liu Q, Yang Z. The SARS-CoV-2 outbreak: what we know. International Journal of Infectious Diseases. 2020;94(395):44–48. doi: 10.1016/j.ijid.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young et al. (2020).Young BE, Fong SW, Chan YH, Mak TM, Ang LW, Anderson DE, Lee CY, Amrun SN, Lee B, Goh YS, Su YCF, Wei WE, Kalimuddin S, Chai LYA, Pada S, Tan SY, Sun L, Parthasarathy P, Chen YYC, Barkham T, Lin RTP, Maurer-Stroh S, Leo YS, Wang LF, Renia L, Lee VJ, Smith GJD, Lye DC, Ng LFP. Effects of a major deletion in the SARS-CoV-2 genome on the severity of infection and the inflammatory response: an observational cohort study. Lancet. 2020;396(10251):603–611. doi: 10.1016/S0140-6736(20)31757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen et al. (2020).Yuen KS, Ye ZW, Fung SY, Chan CP, Jin DY. SARS-CoV-2 and COVID-19: the most important research questions. Cell and Bioscience. 2020;10(1):40. doi: 10.1186/s13578-020-00404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2021).Zhang Y, Chen Y, Li Y, Huang F, Luo B, Yuan Y, Xia B, Ma X, Yang T, Yu F, Liu J, Liu B, Song Z, Chen J, Yan S, Wu L, Pan T, Zhang X, Li R, Huang W, He X, Xiao F, Zhang J, Zhang H. The ORF8 protein of SARS-CoV-2 mediates immune evasion through down-regulating MHC-I. Proceedings of the National Academy of Sciences of the United States of America. 2021;118(23):e2024202118. doi: 10.1073/pnas.2024202118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinzula (2021).Zinzula L. Lost in deletion: the enigmatic ORF8 protein of SARS-CoV-2. Biochemical and Biophysical Research Communications. 2021;538(1):116–124. doi: 10.1016/j.bbrc.2020.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The following information was supplied regarding data availability:
The data are available in the article and the Supplemental File.