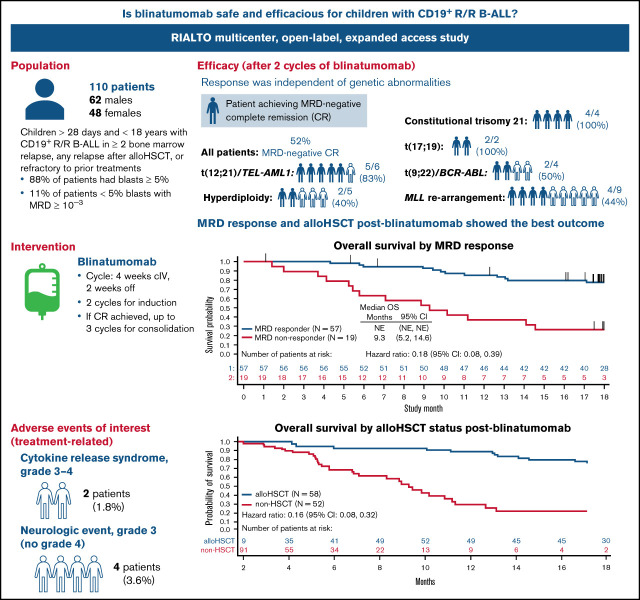
Key Points
Blinatumomab was associated with low incidence of grade 3 or 4 cytokine release syndrome (n = 2; 1.8%) and neurologic events (n = 4; 3.6%).
The best blinatumomab outcomes were seen in patients achieving CR with no MRD who received alloHSCT, independent of genetic abnormalities.
Visual Abstract
Abstract
The safety and efficacy of blinatumomab, a CD3/CD19-directed bispecific molecule, were examined in an open-label, single-arm, expanded access study (RIALTO). Children (>28 days and <18 years) with CD19+ relapsed/refractory B-cell precursor acute lymphoblastic leukemia (R/R B-ALL) received up to 5 cycles of blinatumomab by continuous infusion (cycle: 4 weeks on/2 weeks off). The primary end point was incidence of adverse events. Secondary end points included complete response (CR) and measurable residual disease (MRD) response within the first 2 cycles and relapse-free survival (RFS), overall survival (OS), and allogeneic hematopoietic stem cell transplant (alloHSCT) after treatment. At final data cutoff (10 January 2020), 110 patients were enrolled (median age, 8.5 years; 88% had ≥5% baseline blasts). A low incidence of grade 3 or 4 cytokine release syndrome (n = 2; 1.8%) and neurologic events (n = 4; 3.6%) was reported; no blinatumomab-related fatal adverse events were recorded. The probability of response was not affected by the presence of cytogenetic/molecular abnormalities. Median OS was 14.6 months (95% confidence interval [CI]: 11.0-not estimable) and was significantly better for MRD responders vs MRD nonresponders (not estimable vs 9.3; hazard ratio, 0.18; 95% CI: 0.08-0.39). Of patients achieving CR after 2 cycles, 73.5% (95% CI: 61.4%-83.5%) proceeded to alloHSCT. One-year OS probability was higher for patients who received alloHSCT vs without alloHSCT after blinatumomab (87% vs 29%). These findings support the use of blinatumomab as a safe and efficacious treatment of pediatric R/R B-ALL. This trial was registered at www.clinicaltrials.gov as #NCT02187354.
Introduction
Relapsed or refractory B-cell precursor acute lymphoblastic leukemia (R/R B-ALL) is an aggressive malignancy associated with an unsatisfactory patient outcome. Among children with ALL, more than 98% achieve complete remission (CR) with frontline treatment, but 15% to 20% of patients ultimately relapse.1,2 With standard-of-care chemotherapy, 70% to 98% of first-relapse patients achieve a second CR, depending on the patient risk stratification group.3 Pediatric patients with second or third bone marrow relapse have even poorer outcomes, with only 44% and 27%, respectively, achieving a subsequent CR.4 Achievement of a negative measurable residual disease (MRD) CR correlates with a better probability of event-free survival (EFS) after hematopoietic stem cell transplant (HSCT), because several previously published studies demonstrated that the risk of disease relapse after transplantation is higher in patients with MRD positivity before HSCT than in patients without detectable MRD.5,6 The 5-year disease-free survival rate for patients achieving a second CR ranges between 40% and 50%, depending on patient risk characteristics.3,7-9
Despite improved survival with current risk-adapted treatment regimens, therapeutic approaches using agents with novel mechanisms of action are needed to improve the unsatisfactory outcomes for children with R/R B-ALL. Among these innovative therapeutic options, tisagenlecleucel, a chimeric antigen receptor (CAR) T-cell product, was approved for the treatment of R/R B-ALL in patients up to 25 years of age.10 The approval was based on the outcomes of a single-cohort, multicenter, phase 2 study of tisagenlecleucel (n = 75) that demonstrated an overall remission rate of 81% in pediatric and young adult patients with B-ALL in second or later bone marrow relapse, in bone marrow relapse after allogeneic HSCT (alloHSCT), or refractory to other treatments who received the treatment, although on an intention-to-treat analysis, this value decreased to 66%.11
Blinatumomab is a BiTE® (bispecific T-cell engager) immuno-oncology therapy that activates CD3+ cytotoxic T cells to kill CD19+ B cells. Blinatumomab has demonstrated efficacy and safety in R/R B-ALL in children, adolescents and young adults (AYA), and adults.12-15 In a phase 3 randomized controlled trial of 108 children with high-risk first-relapse B-ALL, treatment with blinatumomab compared with chemotherapy as the third consolidation block before alloHSCT resulted in superior EFS at a median of 22.4 months of follow-up (69% vs 43%), increased MRD remission (90% vs 54%), and was associated with a higher rate of alloHSCT (89% vs 70%).14 In a phase 3 randomized controlled trial by the Children’s Oncology Group, treatment of children and AYAs with high- or intermediate-risk first-relapse B-ALL with blinatumomab vs chemotherapy for 2 cycles following reinduction therapy resulted in increased 2-year overall survival (OS; 71% vs 58%), higher MRD remission (75% vs 32%), and a higher rate of alloHSCT (70% vs 43%).15
The purpose of this expanded access study (RIALTO) was to determine the incidence of treatment-emergent and treatment-related adverse events (TEAEs and TRAEs, respectively) in children with B-ALL in second or later bone marrow relapse, in bone marrow relapse after alloHSCT, or refractory to other treatments. Key efficacy outcomes were also examined, including incidence rate of CR and MRD response within 2 cycles of blinatumomab, relapse-free survival (RFS), OS, incidence rate of alloHSCT, and 100-day mortality after alloHSCT. We previously described findings of the primary analysis16; herein the final follow-up data are presented.
Materials and methods
Study design, oversight, and participants
In this multicenter, open-label, expanded access study, investigators at 16 centers in Europe and the United States (supplemental Table 1) enrolled 110 patients from January 2015 to July 2018. Eligible children were older than 28 days and younger than 18 years at enrollment, with CD19+ R/R B-ALL with second or greater bone marrow relapse (defined as M3 marrow [≥25% morphologic blasts], M2 marrow [≥5% but <25% morphologic blasts], or M1 marrow [<5% morphologic blasts] but with MRD ≥10−3), any bone marrow relapse after alloHSCT, or refractory to prior treatments. Prior treatment with blinatumomab was allowed, provided that the leukemic cells were still CD19+, and the patient was neither refractory nor intolerant to blinatumomab. Exclusion criteria included presence of clinically relevant central nervous system (CNS) pathology, such as epilepsy, seizure, paresis, aphasia, stroke, severe brain injuries, dementia, cerebellar disease, organic brain syndrome, psychosis, with the exception of CNS leukemia that is well controlled with intrathecal therapy; chemotherapy within 2 weeks, radiotherapy within 4 weeks, or immunotherapy within 6 weeks; grade 2 to 4 active acute graft-versus-host disease (GVHD) or active chronic GVHD requiring systemic treatment; and immunosuppressive agents to prevent or treat GVHD within 2 weeks before blinatumomab treatment except for topical corticosteroids.
The trial protocol was approved by an independent ethics committee or institutional review board at each participating center. Patients above the age of 12 years provided assent to participate in the study.
Treatment
Eligible patients received blinatumomab by continuous IV infusion in a 6-week cycle (4 weeks on, 2 weeks off) for up to 5 cycles (2 induction cycles and 3 consolidation cycles). Only patients achieving CR (as defined by M1 marrow) after induction could receive up to 3 consolidation cycles of blinatumomab. For patients with M3 marrow, the initial dose of blinatumomab was 5 μg/m2 per day for the first 7 days, then escalated to 15 μg/m2 per day starting on day 8 (week 2) to day 29 (week 4) of the first cycle, and remained at this dose for all subsequent cycles. For patients with M2 marrow or M1 marrow with MRD ≥10−3, blinatumomab was administered at 15 μg/m2 per day for each cycle. To prevent first-dose adverse events (AEs), dexamethasone was administered at a dose up to 24 mg per day for up to 4 days before the start of blinatumomab treatment. Patients who achieved CR after the first cycle of blinatumomab could undergo alloHSCT.
Outcomes
The primary end points were the incidences of TEAEs and TRAEs. Secondary end points included achievement of CR and MRD response within 2 cycles of blinatumomab, RFS, OS, rate of alloHSCT, and 100-day mortality after alloHSCT.
Assessments
A TEAE is defined as any AE occurring between the start of the first infusion of blinatumomab until 30 days after the end of the infusion. A TRAE is an AE that is deemed treatment related by the investigator. Subject incidence rates of TEAEs and TRAEs were tabulated and summarized by system organ class and preferred term using MedDRA version 22.1 and graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events, v4.03. Serious AEs included events that were fatal, life threatening, required hospitalization or prolonged hospitalization, resulted in disability or incapacity, congenital anomaly or birth defect, or were other medically important events.
Bone marrow aspirate or biopsy was performed at screening, on day 29 of each treatment cycle with blinatumomab, and at every 6-month follow-up. CR was subclassified into 3 groups: CR, CRh, and CRi. CR was defined as <5% bone marrow blasts, no evidence of disease, and full recovery of peripheral blood counts (platelets > 100 × 109/L and absolute neutrophil count > 1.0 × 109/L). CRh was defined as CR with partial recovery of peripheral blood counts (platelets > 50 × 109/L but ≤100 × 109/L and/or absolute neutrophil count > 0.5 × 109/L but ≤1.0 × 109/L). CRi was defined as CR without full or incomplete recovery of peripheral blood counts.
MRD was assessed by either polymerase chain reaction or multicolor flow cytometry. No patients had both MRD assessments. MRD response was defined as conversion of MRD ≥ 10−3 to MRD < 10−4.
Statistical analysis
The statistical reporting of this study was descriptive, with no formal statistical testing requiring a specific sample size. Percentages of patients achieving CR, MRD response, or receiving alloHSCT were each summarized with an exact binomial 95% confidence interval (CI). RFS was calculated for patients achieving CR as the date when CR was first detected to the first date when one of the following RFS events occurred: hematologic relapse, extramedullary relapse, or death from any cause. OS was defined from the start of blinatumomab infusion until death. Survival after alloHSCT was defined from the time of transplant until death. Time-to-event end points were estimated through the Kaplan-Meier method. The Simon-Makuch method was used to examine the association of transplant with time-to-event endpoints. Cumulative incidence function was used to estimate the cumulative incidence of transplant-related mortality adjusting for relapse as a competing risk. Any death occurring without any documented evidence of a relapse after alloHSCT was assumed to be transplant related.
Results
Patient population and treatment
A total of 110 patients were enrolled in this open-label, single-arm, expanded access international study between January 2015 and July 2018, with the last patient ending study on 10 January 2020 (data cutoff date). The patients’ median age was 8.5 (range, 0.4–17) years, 56.4% of patients were males, and 88.2% had ≥5% blasts at baseline (Table 1). Concerning disease history, 55% were in second or further relapse, 40% had relapsed after alloHSCT, 15% had primary refractory disease, and 21% were refractory to reinduction therapy. Thirty-two patients (29.1%) had a recurrent genetic abnormality, the most common being MLL rearrangement (18 patients; 16.4%). Four patients (3.6%) had constitutional trisomy 21. All patients received at least 1 infusion of blinatumomab; 43 patients (39.1%) completed 2 cycles, 14 (12.7%) completed 3 cycles, 6 (5.5%) completed 4 cycles, and 5 (4.5%) completed 5 cycles of blinatumomab. The most frequently reported reasons for ending blinatumomab were protocol-specified criteria (56 patients; 50.9%) and disease progression (26 patients; 23.6%). Of the 56 patients whose treatment was ended for protocol-specific reasons, 34 (60.7%) received alloHSCT, 10 (17.9%) had hematologic or extramedullary relapse subsequent to CR, 9 (16.1%) had >25% blast in the bone marrow at the end of cycle 1, and 3 (5.4%) failed to achieve a CR within the first 2 cycles.
Table 1.
Demographics and baseline characteristics
| Characteristic | All patients (N = 110) |
|---|---|
| Age, median (range), y | 8.5 (0.4-17.0) |
| Age group, y, n (%) | |
| 0-1 | 13 (12) |
| 2-6 | 31 (28) |
| 7-17 | 66 (60) |
| Sex, n (%) | |
| Male | 62 (56) |
| Blast category, n (%) | |
| <5% with MRD ≥ 10−3 | 12 (11) |
| 5%-49% | 55 (50) |
| ≥50% | 42 (38) |
| Unknown | 1 (1) |
| Recurrent genetic abnormalities,* n (%) | |
| MLL rearrangement | 18† (16) |
| t(9;22)/BCR-ABL | 5 (5) |
| t(17;19) | 2 (2) |
| t(12;21)/TEL-AML1 | 9 (8) |
| Hypo/hyperdiploidy | 1 (1)/6 (5) |
| Other | 12 (11) |
| Constitutional trisomy 21 (Down syndrome), n (%) | 4 (4) |
| Prior therapy, n (%) | |
| alloHSCT | 45‡ (41) |
| Blinatumomab | 5 (5) |
| Disease history, n (%) | |
| Primary refractory disease | 17 (15) |
| Refractory to reinduction therapy | 23 (21) |
| Second or further relapse | 61 (55) |
| Relapse after alloHSCT | 44 (40) |
More than 1 type of genetic abnormality may have been selected for the same patient.
Includes 5 patients <1 year old.
Forty-four of these patients relapsed after alloHSCT; 1 patient did not relapse.
Safety
The summary of TEAEs and TRAEs remained unchanged between the primary16 and final analysis (Table 2). The most frequently reported TEAEs and TRAEs and those of grade ≥ 3 are listed in supplemental Tables 2 to 5. Treatment-emergent and treatment-related neurologic events were reported in 46 patients (41.8%) and 22 patients (20.0%), respectively. The most frequently reported (≥2 patients) treatment-related neurologic events were headache (11 patients; 10.0%), tremor (6 patients; 5.5%), seizure (4 patients; 3.6%), and ataxia, depressed level of consciousness, and dizziness (2 patients each; 1.8%; supplemental Table 6). Six patients (5.5%) experienced a grade 3 neurologic event, with a median time to resolution of 2.0 days (range, 1-35 days). The neurologic event was blinatumomab related for 4 patients (2, headache; 1, seizure; 1, depressed level of consciousness) and unrelated for 2 patients (1, agitation; 1, right trigeminal nerve disorder). No patients experienced a grade 4 neurologic event, and no neurologic events were fatal. Treatment-emergent and treatment-related cytokine release syndrome (CRS) were reported for 22 patients (20.0%) and 18 patients (16.4%), respectively, of which none were fatal. Two patients experienced grade ≥ 3 treatment-related CRS (1, grade 3; 1, grade 4) that resolved with a median time of 6.5 days (range, 4-9 days). Nine patients had a fatal TEAE; these deaths were considered a result of disease progression and were not blinatumomab related. Seven patients discontinued blinatumomab because of at least 1 TEAE, with 4 patients discontinuing because of a TRAE. The most frequently reported (≥2 patients) TEAE leading to blinatumomab discontinuation was depressed level of consciousness (n = 2; 1.8%).
Table 2.
Subject incidence of TEAEs and TRAEs in all 110 patients treated with blinatumomab
| TEAE | TRAE | |||
|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | |
| Patients reporting AEs | ||||
| Any grade | 109 (99.1) | 95.0-100.0 | 81 (73.6) | 64.4-81.6 |
| Grade 3 | 71 (64.5) | 54.9-73.4 | 29 (26.4) | 18.4-35.6 |
| Grade 4 | 31 (28.2) | 20.0-37.6 | 3 (2.7) | 0.6-7.8 |
| Serious | 50 (45.5) | 35.9-55.2 | 21 (19.1) | 12.2-27.7 |
| Fatal | 9 (8.2) | 3.8-15.0 | 0 | 0 |
| Leading to treatment discontinuation | 7 (6.4) | 2.6-12.7 | 4 (3.6) | 1.0-9.0 |
| Serious | 6 (5.5) | 2.0-11.5 | 4 (3.6) | 1.0-9.0 |
| Fatal | 2 (1.8)] | 0.2-6.4 | 0 | 0 |
| Leading to treatment interruption | 25 (22.7) | 15.3–31.7 | 18 (16.4) | 10.0-24.6 |
| Serious | 17 (15.5) | 9.3–23.6 | 11 (10.0) | 5.1-17.2 |
| Fatal | 3 (2.7) | 0.6-7.8 | 0 | 0 |
Retreatment data (treated as cycle 2) for 1 patient is included. Adverse events coded using MedDRA version 22.1. Severity graded using CTCAE v4.03.
Efficacy
CR and MRD response.
CR and MRD responses within 2 cycles of blinatumomab were reported in the primary analysis.16 Overall, 57 of 110 patients (52%) achieved CR with MRD response. Herein, the CR and MRD responses were examined in high-risk patients with poor-risk molecular/cytogenetic abnormalities or genetic disorders at baseline. These high-risk patients achieved high rates of CR with MRD response (Table 3). In particular, CR with MRD was achieved by 4 patients with constitutional trisomy 21 and by 2 patients with t(17;19)/TCF3-HLF. Among 18 patients with MLL rearrangements, CR with MRD response was achieved by 4 patients, and 2 patients showed CR without MRD response. Seven patients progressed during blinatumomab treatment and 2 patients showed stable disease. Two patients did not complete at least 1 cycle of blinatumomab, and therefore, no response data within the first 2 cycles were assessed. In the last patient with MLL rearrangement, bone marrow assessment was not performed because of the poor health condition of the patient after the first blinatumomab cycle. Among 5 patients with t(9;22)/BCR-ABL, CR with MRD was achieved in 2 patients, and 2 patients showed CR without MRD; progressive disease was observed in 1 patient. High rates of CR with MRD response were also recorded in patients with low-risk genetic abnormalities: 5 of 6 responders with t(12;21)/TEL-AML1 and 2 of 4 responders with hyperdiploidy also showed MRD response (Table 3).
Table 3.
Best responses after first 2 cycles of blinatumomab treatment in patients with high-risk and low-risk genetic abnormalities
| n (%) | |
|---|---|
| High-risk genetic abnormalities | |
| Constitutional trisomy (n = 4) | |
| CR with MRD | 4 (100) |
| t(17;19)/TCF3-HLF (n = 2) | |
| CR with MRD | 2 (100) |
| MLL rearrangement (n = 18) | |
| CR with MRD | 4 (22) |
| CR without MRD | 2 (11) |
| PD | 7 (39) |
| SD | 2 (11) |
| Noncompletion of at least 1 blinatumomab cycle | 2 (11) |
| Inevaluable* | 1 (6) |
| t(9;22)/BCR-ABL (n = 5) | |
| CR with MRD | 2 (40) |
| CR without MRD | 2 (40) |
| PD | 1 (20) |
| Low-risk genetic abnormalities | |
| t(12;21)/TEL-AML1 (n = 9) | |
| CR with MRD | 5 (56) |
| CR without MRD | 1 (11) |
| Noncompletion of at least 1 blinatumomab cycle | 2 (22) |
| PD | 1 (11) |
| Hyperdiploidy (n = 6) | |
| CR with MRD | 2 (33) |
| CR without MRD | 2 (33) |
| PD | 2 (33) |
PD, progressive disease; SD, stable disease.
Bone marrow assessment was not performed because of poor health of the patient after the first blinatumomab cycle.
RFS.
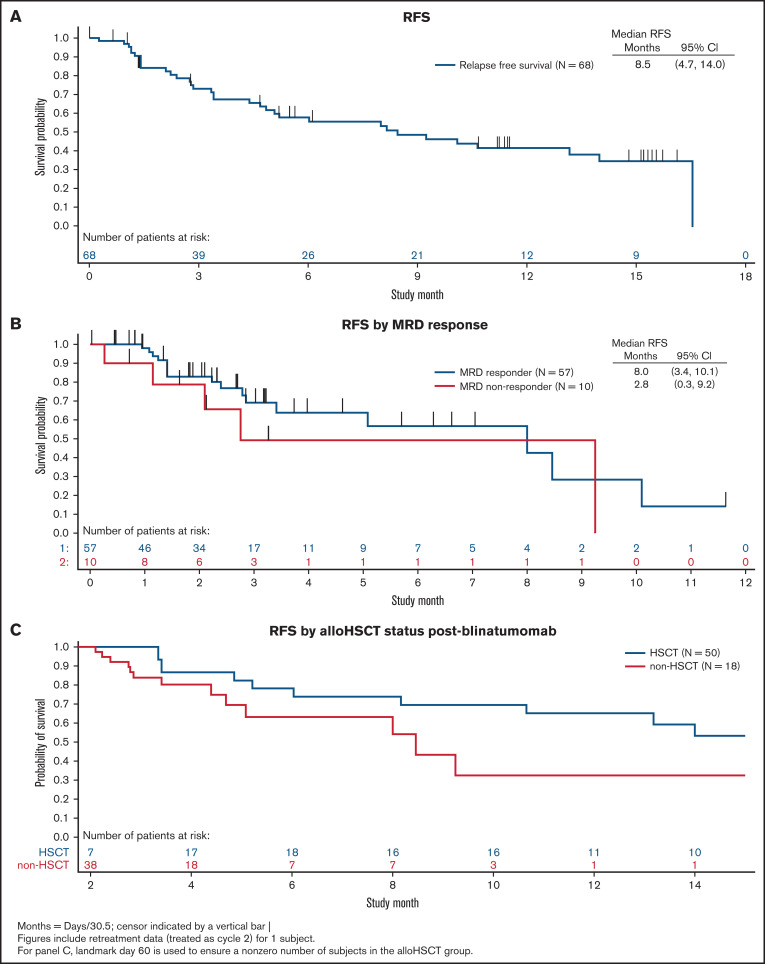
The median follow-up time for RFS was 11.5 months (range, 0.0-16.3 months). The median RFS was 8.5 months (95% CI: 4.7-14.0 months) among patients achieving CR within the first 2 cycles of blinatumomab (Figure 1A). At the end of the study, 34 patients were in continuous remission.
Figure 1.
Relapse-free survival. (A) RFS was calculated relative to the date of bone marrow aspiration when CR was detected for the first time to the event date (date of the bone marrow aspiration at which hematologic relapse was first detected, the date of the diagnosis on which the hematologic or extramedullary relapse was documented, or the date of death because of any cause, whichever occurred earlier). (B) RFS was analyzed according to MRD response using the Kaplan-Meier method. (C) RFS was analyzed according to alloHSCT status after blinatumomab using a Simon-Makuch 71-day landmark analysis..
RFS was analyzed according to MRD response using the Kaplan-Meier method (Figure 1B). The median RFS for MRD responders (n = 57) was 8.0 months (95% CI: 3.4-10.1 months). The median RFS for MRD nonresponders (n = 10) was 2.8 months (95% CI: 0.3-9.2 months).
RFS was analyzed according to alloHSCT status after blinatumomab using a Simon-Makuch 60-day landmark analysis (Figure 1C). This analysis showed a trend toward improved RFS for patients who did receive alloHSCT after blinatumomab treatment compared with patients who did not. At 12 months, the probability of survival was 70% for patients who received alloHSCT after blinatumomab compared with 30% survival for patients who had not received alloHSCT after blinatumomab.
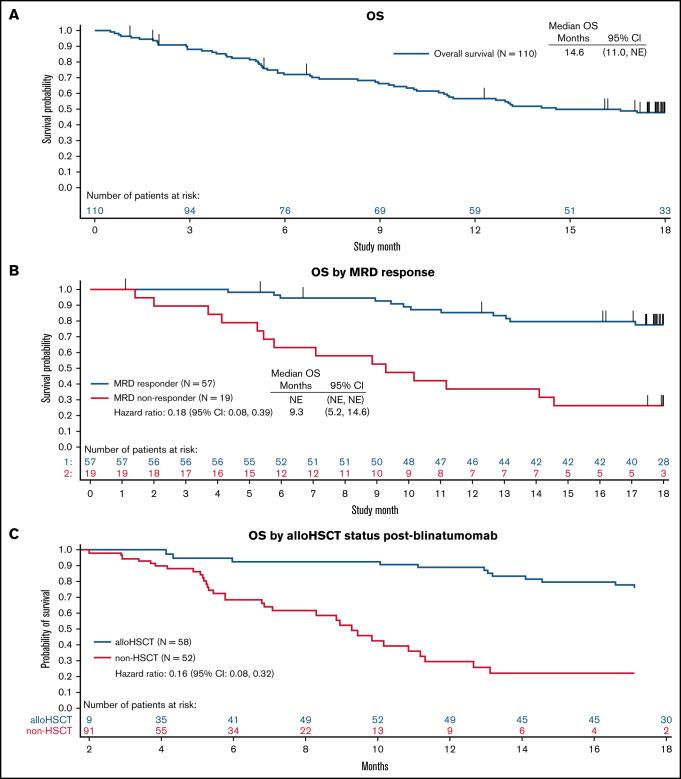
OS.
OS was censored at 18 months because only a subgroup of nontransplanted patients was followed beyond 18 months. The median OS was 14.6 months (95% CI: 11.0 months-not estimable; Figure 2A). The median OS for MRD responders (n = 57) was not estimable, whereas that for MRD nonresponders (n = 19) was 9.3 months (95% CI: 5.2-14.6 months; Figure 2B).
Figure 2.
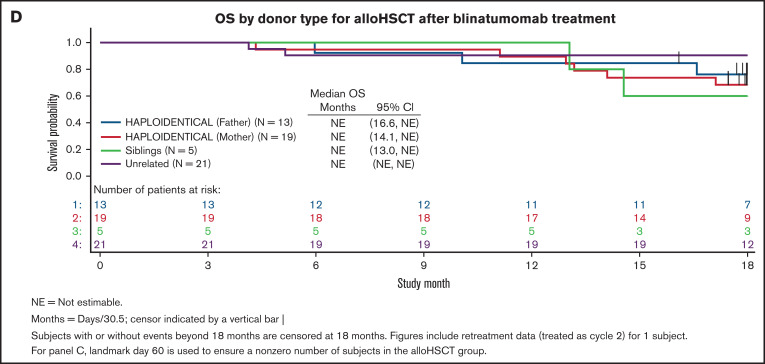
OS was censored at 18 months because only a subgroup of nontransplanted patients was followed beyond 18 months. (A) OS was defined from the start of blinatumomab infusion until death. (B) OS was analyzed according to MRD response using the Kaplan-Meier method. (C) OS was analyzed according to alloHSCT status after blinatumomab using a Simon-Makuch 60-day landmark analysis. (D) OS was analyzed according to donor type for alloHSCT after blinatumomab treatment. Vertical bars indicate censoring.
OS was analyzed according to alloHSCT status after blinatumomab using a Simon-Makuch 60-day landmark analysis (Figure 2C). The Simon-Makuch analysis showed improved OS for patients who did receive alloHSCT after blinatumomab compared with patients who did not (hazard ratio, 0.16; 95% CI: 0.08-0.32). The 1-year OS probability was 87% for patients who received alloHSCT after blinatumomab compared with 29% for patients who had not received alloHSCT. Patients obtaining MRD-negative CR and given alloHSCT showed the best outcome (supplemental Figure 1).
OS was analyzed according to donor type for alloHSCT after blinatumomab treatment (Figure 2D). At the 18-month Kaplan-Meier analysis, OS did not differ across all donor types (haploidentical father, haploidentical mother, siblings, and unrelated) used.
alloHSCT.
Of the 110 patients in this trial, 58 received alloHSCT any time after the first blinatumomab infusion (supplemental Table 7). A total of 17 (15.5%), 32 (29.1%), 6 (5.5%), 1 (0.9%), and 2 (1.8%) patients received alloHSCT after 1, 2, 3, 4, and 5 cycles of blinatumomab, respectively. For patients who achieved a CR within the first 2 cycles of blinatumomab (n = 68), most patients proceeded to alloHSCT (73.5%; 50 of 68; 95% CI: 61.4%-83.5%; Table 4). For patients who had not achieved a CR within the first 2 cycles (n = 25), most patients did not proceed to alloHSCT (76.0%; 19 of 25; 95% CI: 54.9%-90.6%). Likewise, for patients who achieved an MRD response within the first 2 cycles of blinatumomab (n = 57), most patients proceeded to alloHSCT (77.2%; 44 of 57; 95% CI: 64.2%-87.3%; Table 4). For patients without MRD response within the first 2 cycles (n = 19), only 42.1% of patients proceeded to alloHSCT (8 of 19; 95% CI: 20.3%-66.5%).
Table 4.
Patients with/without alloHSCT after blinatumomab
| Patients treated with blinatumomab (N = 110) | ||
|---|---|---|
| n | 95% CI | |
| Patients with/without alloHSCT after blinatumomab, by CR within the first 2 cycles | ||
| Patients with alloHSCT, n (%) | 56 (50.9) | |
| Patients with CR, n (%) | 68 (61.8) | |
| alloHSCT after CR, n (%)* | 50 (73.5) | 61.4-83.5 |
| No alloHSCT after CR, n (%)* | 18 (26.5) | 16.5-38.6 |
| Patients without CR, n (%) | 25 (22.7) | |
| alloHSCT, n (%)† | 6 (24.0) | 9.4-45.1 |
| No alloHSCT, n (%)† | 19 (76.0) | 54.9-90.6 |
| Patients with/without alloHSCT after blinatumomab, by MRD response within the first 2 cycles | ||
| Patients with alloHSCT, n (%) | 52 (47.3) | |
| Patients with MRD response, n (%) | 57 (51.8) | |
| alloHSCT after MRD response, n (%)‡ | 44 (77.2) | 64.2-87.3 |
| No alloHSCT after MRD response, n (%)‡ | 13 (22.8) | 12.7-35.8 |
| Patients without MRD response, n (%) | 19 (17.3) | |
| alloHSCT, n (%)§ | 8 (42.1) | 20.3-66.5 |
| No alloHSCT, n (%)§ | 11 (57.9) | 33.5-79.7 |
| Patients with alloHSCT after blinatumomab, by tumor burden at baseline | ||
| Patients with <5% blasts and MRD ≥ 10−3 (N = 11)ǁ | 9 (82) | 48.2-97.7 |
| Patients with ≥5% blasts (N = 58)¶ | 36 (62) | 48.4-74.5 |
Percentage based on 68 patients with CR.
Percentage based on 25 patients without CR.
Percentage based on 57 patients with MRD response.
Percentage based on 19 patients without MRD response.
N is based on the number of patients with <5% blasts and MRD ≥ 10−3 at baseline who achieved CR within the first 2 cycles of blinatumomab.
N is based on the number of patients with ≥5% blasts at baseline who achieved CR within the first 2 cycles of blinatumomab.
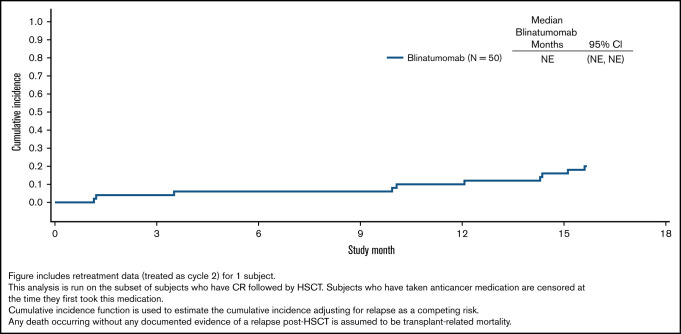
The transplant-related mortality at 1 year after alloHSCT was 10.0% (95% CI: 3.58%-20.35%). Furthermore, the cumulative incidence of transplant-related mortality for patients who achieved the best response in first 2 cycles is shown in Figure 3. In particular, the 100-day cumulative incidence of mortality after alloHSCT for patients who achieved CR within the first 2 cycles of blinatumomab was 4.0% (95% CI: 1.0%-15.1%). The proportion of patients who received alloHSCT was inversely proportional to the leukemia burden. For patients with <5% blasts and MRD ≥ 10−3 at baseline, 82% (9 of 11; 95% CI: 48.2%-97.7%) proceeded to alloHSCT after blinatumomab treatment compared with 62% of patients (36 of 58; 95% CI: 48.4%-74.5%) with ≥5% blasts at baseline (Table 4).
Figure 3.
Cumulative incidence of transplant-related mortality for patients who achieved best response in the first 2 cycles.
Discussion
In this final analysis of the open-label, single-arm, expanded access study (RIALTO), the safety and efficacy of blinatumomab for the treatment of children with R/R B-ALL were determined. Overall, the safety and efficacy from this final analysis were consistent with that reported for the primary analysis; no additional new safety signals were reported.16 One key finding of this study is that a very low incidence of grade ≥ 3 CRS and grade 3 neurologic toxicities occurred with blinatumomab treatment. Only 2 patients (1.8%) experienced grade ≥ 3 treatment-related CRS (1, grade 3; 1, grade 4) that resolved quickly (median resolution time, 6.5 days). Only six patients (5.5%) experienced a grade 3 neurologic event (4 patients; 3.6%; blinatumomab related) that resolved quickly (median resolution time, 2.0 days). No patients experienced a grade 4 neurologic event, and no neurologic events were fatal. Overall, temporary discontinuation of treatment was the most frequently implemented strategy for addressing blinatumomab-related toxicities. In particular, dosing was interrupted if patients experienced a blinatumomab-related grade 2 clinically relevant neurologic event, grade ≥ 2 CRS, tumor lysis syndrome, or disseminated intravascular coagulation or coagulopathy, or any clinically relevant event of grade ≥ 3. After resolution to a minimum of grade 1, blinatumomab was restarted at 5 μg/m2 per day for at least 7 days before increasing to 15 μg/m2 per day. Notably, a low incidence of grade ≥ 3 CRS and neurologic events was also recorded in children with high-risk first-relapse B-ALL treated with blinatumomab, with no patients experiencing grade ≥ 3 CRS and only 3 patients (5.6%) with neurologic events of grade 3 or 4.14 Similar findings were reported for children and AYAs with high- or intermediate-risk first-relapse B-ALL treated with blinatumomab, with only 1 patient (1%) experiencing grade ≥ 3 CRS and 1 patient (1%) experiencing a grade ≥ 3 neurologic event (ie, seizure), of which none were fatal, and both cases were reversible.15 In this study, the proportion of patients experiencing grade ≥ 3 CRS and neurotoxicity AEs was lower than that observed in the phase 1/2 study of blinatumomab in pediatric patients with R/R B-ALL.13 This finding can be attributed to a greater proportion of patients with less than 50% bone marrow blasts at baseline enrolled in this study (61%) compared with that in patients enrolled in the phase 1/2 study of blinatumomab (26%).13 Collectively, these studies demonstrate a good safety profile of blinatumomab for the treatment of R/R B-ALL, especially in the presence of a limited leukemia burden.
High-risk patients with poor-risk molecular/cytogenetic features or genetic disorders at baseline achieved high rates of CR and MRD response after 2 cycles of blinatumomab. All patients with constitutional trisomy 21 or t(17;19) and approximately half of patients with t(9;22)/BCR-ABL or an MLL rearrangement achieved CR with an MRD response. Of the MRD-negative responders with MLL rearrangement, 1 patient was <1 year old, a high-risk age group. This finding is consistent with other studies showing that the efficacy of blinatumomab is not affected by the presence of high-risk genetic abnormalities, unlike chemotherapy.14,17,18
Children with R/R B-ALL who proceeded to alloHSCT after treatment with blinatumomab had better OS compared with those who did not proceed to alloHSCT (87% vs 29% survival probability at 12 months). The cumulative incidence of transplant-related mortality in these children was particularly low, and the probability of OS was similar in patients transplanted from either an HLA-identical donor or an HLA-haploidentical relative, confirming that, nowadays, the outcome of patients given alloHSCT is much more influenced by the state of molecular remission (ie, MRD-negative CR) than by the type of donor.19 Blinatumomab thus serves as an effective bridge to alloHSCT in these patients with multiple R/R B-ALL.
Blinatumomab is highly efficacious in achieving CR and eliminating persistent MRD in both children and adults with R/R B-ALL. In this RIALTO study, 63% of children (69 of 110) achieved CR within the first 2 cycles of blinatumomab; 83% of these responders also achieved MRD response.16 In the primary analysis, the median RFS and OS were 8.5 and 13.1 months, respectively.16 Although the median RFS was same in the final analysis, median OS increased to 14.6 months, thereby indicating that blinatumomab offered benefit in terms of both salvage therapy and in prolonging survival in children with R/R B-ALL. In a phase 3 randomized controlled trial in children with high-risk first-relapse B-ALL, 93% of patients with persistent MRD at baseline achieved MRD response with 1 cycle of blinatumomab administered as the third consolidation block before alloHSCT compared with 24% of patients treated with chemotherapy.14 At the median follow-up time for OS (19.5 months), the median OS for children treated with blinatumomab had not been met.14 High MRD response likewise was seen in children and AYAs with high- or intermediate-risk first-relapse B-ALL treated with blinatumomab.15 In the phase 3 TOWER study, 44% of adult patients with R/R B-ALL achieved CR within the first 2 cycles of blinatumomab, and persistent MRD was eliminated in 76% of these responders.12 In adults, in the TOWER study, the median OS was 7.7 months for patients treated with blinatumomab, which was significantly longer than that in the chemotherapy arm (4.0 months). In the BLAST study enrolling adults with molecularly resistant B-ALL, persistent MRD was eliminated in 78% of patients.20 Furthermore, because of a higher proportion of patients with reduced tumor burden at baseline in this study compared with that in patients enrolled in the phase 1/2 study of blinatumomab in pediatric patients with R/R B-ALL, we documented a higher CR rate than that recorded in the phase 1/2 study.13 Overall, these findings indicated that the benefit derived from treatment with blinatumomab is inversely associated with leukemia burden.
CAR T-cell therapy is a novel form of immunotherapy that has led to promising results in the treatment of children and adults with ALL.21 Although excellent remission rates have been achieved using approved CAR T-cell therapies in the treatment of hematologic malignancies, they have been associated with very high incidences of CRS (42%-93%).11,22-25 In this study, the CRS rates were very low compared with those observed with approved CAR T-cell therapies. Moreover, in 10% to 15% of patients, an adequate number of CAR T cells cannot be manufactured. A recent study analyzing real-word data on patients with R/R B-ALL treated with tisagenlecleucel reported a probability of EFS of 40% at 2 years. This finding indicates that a substantial number of patients failed from benefit of the approach in the long term.
The limitations of this study include the lack of a chemotherapy comparator arm and the assessment of outcomes by investigators instead of an independent central review. Furthermore, it was observed that the efficacy of blinatumomab was unaffected by the presence of high-risk genetic abnormalities. However, this finding was demonstrated in a limited number of patients enrolled at a small number of study centers, thus reducing our ability to draw firm conclusions from the data. Finally, because of the nature of expanded access programs such as the current study, there might be many eligible patients globally who could be identified as potential candidates for treatment. However, some of these patients are excluded to achieve economic and operational feasibility.
Overall, data of patients included in the RIALTO trial support the use of blinatumomab as rescue therapy in children with R/R B-ALL, including those with molecularly resistant disease. Blinatumomab can have particular value in fragile children, such as those with Down syndrome, and in those patients carrying poor-risk molecular/cytogenetics features (including TCF3-HLF–positive B-ALL).10
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
This study was funded by Amgen, Inc. Medical writing support was provided by Liz Leight, an employee of Amgen Inc., and Advait A. Joshi of Cactus Life Sciences (part of Cactus Communications), which was funded by Amgen, Inc.
Authorship
Contribution: All authors and the sponsor (Amgen Inc.) participated in the conception and design of the trial and the analysis and interpretation of data; patient data were collected by F.L., P.B., S.J., P.-G.S., J.-P.B., R.H., B.B, C.R., and C.C.-S; the authors drafted the manuscript in collaboration with a medical writer; and all the authors approved the manuscript for submission and vouch for the accuracy and completeness of the data and the fidelity of the trial to the protocol.
Conflict-of-interest disclosure: F.L. reports advisory board membership for Amgen, Novartis, Bellicum Pharmaceutical, and Neovii and is on the speakers’ bureau for Amgen, Novartis, Miltenyi, Medac, Jazz Pharmaceutical, Gilead, Sanofi, and Takeda outside the submitted work. G.Z., N.M., and W.N.K. are employed by Amgen. G.Z. has patents 20190300609 and 20130323247 licensed. P.B. reports advisory board membership for Novartis, Celgene, Bristol-Myers Squibb, Amgen, Medac, and Servier; research funding from Medac, Riemser, and Neovii; is on the speakers’ bureau for Novartis, Miltenyi, Jazz, Riemser, and Amgen; and reports patents and royalties from Medac. P.-G.S. reports advisory board membership for Novartis and Bellicum outside the submitted work. B.B. reports advisory board membership for Amgen outside the submitted work. C.R. reports advisory board memberships for Amgen, Pfizer, Novartis, Celgene, EUSA Pharma, Roche, and Genentech and speaker honoraria from Amgen, Pfizer, and Roche. The remaining authors declare no competing financial interests.
Correspondence: Franco Locatelli, Department of Pediatric Hematology and Oncology, IRCCS Ospedale Pediatrico Bambino Gesù, Piazza Sant'Onofrio 4, 00165 Rome, Italy; e-mail: franco.locatelli@opbg.net.
References
- 1.Hunger SP, Mullighan CG. Acute lymphoblastic leukemia in children. N Engl J Med. 2015;373(16):1541-1552. [DOI] [PubMed] [Google Scholar]
- 2.Pui CH, Yang JJ, Hunger SP, et al. Childhood acute lymphoblastic leukemia: progress through collaboration. J Clin Oncol. 2015;33(27):2938-2948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Locatelli F, Schrappe M, Bernardo ME, Rutella S. How I treat relapsed childhood acute lymphoblastic leukemia. Blood. 2012;120(14):2807-2816. [DOI] [PubMed] [Google Scholar]
- 4.Ko RH, Ji L, Barnette P, et al. Outcome of patients treated for relapsed or refractory acute lymphoblastic leukemia: a Therapeutic Advances in Childhood Leukemia Consortium study. J Clin Oncol. 2010;28(4):648-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruggeri A, Michel G, Dalle JH, et al. Impact of pretransplant minimal residual disease after cord blood transplantation for childhood acute lymphoblastic leukemia in remission: an Eurocord, PDWP-EBMT analysis. Leukemia. 2012;26(12):2455-2461. [DOI] [PubMed] [Google Scholar]
- 6.Lovisa F, Zecca M, Rossi B, et al. Pre- and post-transplant minimal residual disease predicts relapse occurrence in children with acute lymphoblastic leukaemia. Br J Haematol. 2018;180(5):680-693. [DOI] [PubMed] [Google Scholar]
- 7.Malempati S, Gaynon PS, Sather H, La MK, Stork LC; Children’s Oncology Group . Outcome after relapse among children with standard-risk acute lymphoblastic leukemia: Children’s Oncology Group study CCG-1952. J Clin Oncol. 2007;25(36):5800-5807. [DOI] [PubMed] [Google Scholar]
- 8.Hunger SP, Raetz EA. How I treat relapsed acute lymphoblastic leukemia in the pediatric population. Blood. 2020;136(16):1803-1812. [DOI] [PubMed] [Google Scholar]
- 9.Tallen G, Ratei R, Mann G, et al. Long-term outcome in children with relapsed acute lymphoblastic leukemia after time-point and site-of-relapse stratification and intensified short-course multidrug chemotherapy: results of trial ALL-REZ BFM 90. J Clin Oncol. 2010;28(14):2339-2347. [DOI] [PubMed] [Google Scholar]
- 10.O’Leary MC, Lu X, Huang Y, et al. FDA approval summary: tisagenlecleucel for treatment of patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia. Clin Cancer Res. 2019;25(4):1142-1146. [DOI] [PubMed] [Google Scholar]
- 11.Maude SL, Laetsch TW, Buechner J, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378(5):439-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kantarjian H, Stein A, Gökbuget N, et al. Blinatumomab versus chemotherapy for advanced acute lymphoblastic leukemia. N Engl J Med. 2017;376(9):836-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von Stackelberg A, Locatelli F, Zugmaier G, et al. Phase I/phase II study of blinatumomab in pediatric patients with relapsed/refractory acute lymphoblastic leukemia. J Clin Oncol. 2016;34(36):4381-4389. [DOI] [PubMed] [Google Scholar]
- 14.Locatelli F, Zugmaier G, Rizzari C, et al. Effect of blinatumomab vs chemotherapy on event-free survival among children with high-risk first-relapse b-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325(9):843-854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown PA, Ji L, Xu X, et al. Effect of postreinduction therapy consolidation with blinatumomab vs chemotherapy on disease-free survival in children, adolescents, and young adults with first relapse of B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325(9):833-842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Locatelli F, Zugmaier G, Mergen N, et al. Blinatumomab in pediatric patients with relapsed/refractory acute lymphoblastic leukemia: results of the RIALTO trial, an expanded access study [corrections published in Blood Cancer J. 2021;11:173 and Blood Cancer J. 2021;11:28]. Blood Cancer J. 2020;10(7):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mouttet B, Vinti L, Ancliff P, et al. Durable remissions in TCF3-HLF positive acute lymphoblastic leukemia with blinatumomab and stem cell transplantation. Haematologica. 2019;104(6):e244-e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forero-Castro M, Montaño A, Robledo C, et al. Integrated genomic analysis of chromosomal alterations and mutations in B-cell acute lymphoblastic leukemia reveals distinct genetic profiles at relapse. Diagnostics (Basel). 2020;10(7):E455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bertaina A, Zecca M, Buldini B, et al. Unrelated donor vs HLA-haploidentical α/β T-cell- and B-cell-depleted HSCT in children with acute leukemia. Blood. 2018;132(24):2594-2607. [DOI] [PubMed] [Google Scholar]
- 20.Gökbuget N, Dombret H, Bonifacio M, et al. Blinatumomab for minimal residual disease in adults with B-cell precursor acute lymphoblastic leukemia [correction published in Blood. 2019;133(24):2625]. Blood. 2018;131(14):1522-1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holstein SA, Lunning MA. CAR T-cell therapy in hematologic malignancies: a voyage in progress. Clin Pharmacol Ther. 2020;107(1):112-122. [DOI] [PubMed] [Google Scholar]
- 22.Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017; 377(26):2531-2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raje N, Berdeja J, Lin Y, et al. Anti-BCMA CAR T-cell therapy bb2121 in relapsed or refractory multiple myeloma. N Engl J Med. 2019;380(18):1726-1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang M, Munoz J, Goy A, et al. KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2020;382(14): 1331-1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254):839-852. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.