Abstract
Simple Summary
The Solanaceae family is one of the most important arable and economic families in the world. In addition, it includes a wide range of valuable active secondary metabolites of species with biological and medical properties. This literature review focuses on the assessment of the anticancer properties of the extracts and pure compounds, and the synergistic effects with chemotherapeutic agents and nanoparticles from various species of the Solanaceae family, as well as their potential molecular mechanisms of action in in vitro and in vivo studies in various types of tumours.
Abstract
Many of the anticancer agents that are currently in use demonstrate severe side effects and encounter increasing resistance from the target cancer cells. Thus, despite significant advances in cancer therapy in recent decades, there is still a need to discover and develop new, alternative anticancer agents. The plant kingdom contains a range of phytochemicals that play important roles in the prevention and treatment of many diseases. The Solanaceae family is widely used in the treatment of various diseases, including cancer, due to its bioactive ingredient content. The purpose of this literature review is to highlight the antitumour activity of Solanaceae extracts—single isolated compounds and nanoparticles with extracts—and their synergistic effect with chemotherapeutic agents in various in vitro and in vivo cancer models. In addition, the biological properties of many plants of the Solanaceae family have not yet been investigated, which represents a challenge and an opportunity for future anticancer therapy.
Keywords: anticancer potential, apoptosis, cytotoxic effect, in vitro and in vivo studies, plant extracts, pure compounds, Solanaceae
1. Introduction
Cancer is arguably one of the most dangerous diseases for civilization, affecting all people, regardless the their origin, age or social status. Cancer is also one of the most common causes of death after cardiovascular diseases in developed countries. Statistics show that about 20 million new cases were diagnosed in the world in 2020, and as many as 10 million people died as a result of cancer [1]. Apart from the genetic determinants of the development of cancer (e.g., the presence of typical gene mutations), the most common causes of cell transformation are lifestyle factors (e.g., radiation exposure, smoking, poor diet, alcohol consumption, occupational factors or environmental contamination). Gender and age are also of great importance in the development of neoplastic diseases, and have a significant influence on cancer incidence and mortality [2,3,4,5]. Tumour development and progression are complex, involving factors in the cancer cells themselves like abnormally excessive proliferation as well as multidimensional interactions between other cells and tissues in the body. These cells can also cause angiogenesis, and are capable of dividing indefinitely and metastasizing. As such, rapid and correct diagnosis increases the chances of successful treatment [6,7].
Statistics show that one in six deaths in the world today is caused by cancer, and about 70% of these deaths occur in low- and middle-income people [8]. The problem of increased cancer incidence around the world has led to an increasing search for new compounds that are ideally toxic to cancer cells but not to normal cells. As the currently used chemotherapeutic agents show relatively high toxicity towards both neoplastic cells and normal cells [9,10,11], there is great interest in the identification of new compounds of natural origin with specific activity against different cancer types. The anticancer properties of plants have been recognised for centuries. About 60% of the drugs currently used to treat cancer were originally isolated from nature, with the plant kingdom being the most important source. The intensive development of phytochemistry and isolation methods of plant-derived compounds eventually led to the development of a number of anticancer drugs [12].
A considerable variety and number of plants are known to have medicinal properties [13,14,15]. An estimated 70,000 plant species, from algae to trees, have been used for medicinal purposes [16]. The National Cancer Institute (NCI) has studied approximately 35,000 plant species for potential anticancer effects. Among them, about 3000 plant species showed reproducible anticancer activity [8]. While the bioactive principles from these plants can be obtained traditionally by extraction from various natural sources, they can be produced more efficiently using various biotechnological tools. The range of secondary metabolites known to exhibit anticancer properties is chemically broad, with the predominant groups being alkaloids, terpenoids and polyphenols [17,18].
Both pure compounds and extracts of plant origin show cytotoxic effects by inducing apoptosis in cancer cells [19,20,21,22,23,24]. Secondary metabolites, either used per se or as nanoparticles in targeted therapy, have also been found to have numerous effects on cancer, both in vitro and in vivo; they also appear to interact with chemotherapeutic agents, thus positively or negatively affecting their efficacy, and to protect normal cells against the adverse effects of anticancer therapies [25,26,27].
One family of plants commonly included in the diet is the Solanaceae. It is one of the largest plant families, and its genus—Solanum—is the richest in edible species, including potatoes (Solanum tuberosum), tomatoes (Solanum lycopersicum) and eggplants (Solanum melongena); in addition, peppers are widely-consumed vegetables which are included in the related genus Capsicum [28,29]. The Solanum genus contains a range of phenolic, alkaloid, saponin, terpene and lipid compounds; as such, it has frequently been used for medicinal purposes. Many of the alkaloids from the Solanum genus are particularly interesting because they have demonstrated extensive antirheumatic, antimicrobial, antioxidant and antitumour effects, in the latter case against several types of cancer [30,31].
The present study displays selected general issues including medicinal plants in cancer treatment, nanotechnology and plant compounds in the fight against cancer, the synergy between chemotherapeutic agents and plant compounds in cancer therapy, and the Solanaceae family’s general characteristics and application. Moreover, the reports discussed the functional properties of extracts or compounds isolated from Solanaceae species that are known to exert selective anticancer activity in vitro and in vivo, as well as their synergistic effects when used in combination with chemotherapeutic agents. In some cases, the extracts were formulated by using nanoparticle-based delivery systems. The studies also address the molecular and cellular mechanisms involved in the death of cancer cells.
2. Inclusion and Exclusion Criteria
This research papers included in this review focused on in vitro and in vivo studies of plant extracts or isolated compounds from the Solanaceae family administered per se, or in combination with chemotherapeutics. In certain studies, the potential mechanisms of antitumour activity were discussed. Only research articles published in peer-reviewed journals were selected. Studies in which the isolated compounds of interest were synthesized or purchased, rather than being derived from plant material, were excluded. In addition, studies that did not specify the extraction and/or purification methodology of a bioactive compound were also excluded.
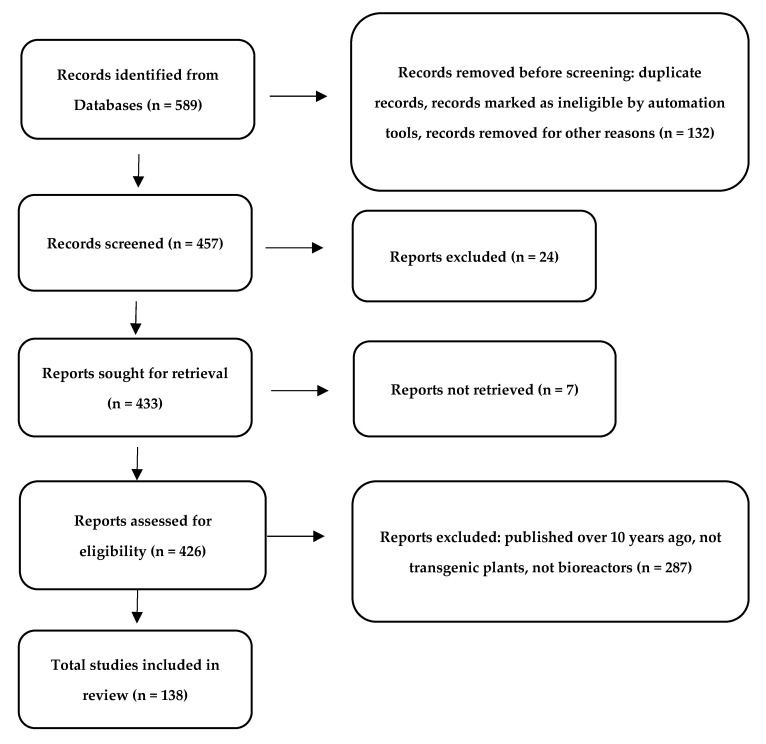
The present literature review was carried out using the following electronic databases: MedLars Online International Literature, PubMed, SCOPUS, and Web of Science. First, the medical subject headings (MeSH) were defined using “Solanaceae”, “plant extract”, “plant-derived compounds”, “cancer cell lines”, “anticancer effect”, ‘’chemotherapeutic with combination of plant extracts’’, and ‘’nanoparticles with plant extracts’’ as descriptive terms. The same strategy was used for all of the databases, with adaptations, as appropriate. The data presented in the tables were published in the period 2015–2021 (Figure 1).
Figure 1.
PRISMA flow diagram demonstrating the screening method for the article [32].
3. Medicinal Plants in Cancer Treatment
Phytotherapy is believed to have originated with the Sumerian and Chinese civilizations over four thousand years ago, and became particularly prominent in ancient Egypt. The first plant to be used against cancer may have been Trifolium pratense: Dioscurides reported its use in the treatment of neoplasms in De Materia Medica, together with an extract of Colchicum autumnale known to have anticancer properties, which were attributed to its colchicine content. Elsewhere, Avicenna also mentions the use of Ricinus communis, Atropa belladonna, Urtica dioica, Narcissus poeticus, Scrophularia nodosa and Ecbalium elaterium. Currently, the rapid development of phytochemistry has allowed the discovery of new compounds with potential medical properties [6,33,34,35,36,37,38]. Other families of great medical importance include the Poaceae, Fabaceae, Apiaceae, Lamiaceae, Brassicaceae, Papaveraceae, Plantaginaceae, and Solananceae, etc. [39,40]. For example, in the Poaceae, Oryza sativa exerts anticancer effects due the presence of anthocyanins and some phenols, e.g., tricin, which can be used to treat breast cancer [41]. In turn, Arachis hypogaea, of the Fabaceae family, has demonstrated efficacy in the treatment of colon, prostate and breast cancer, which was associated with its β-sitosterol and sterol content [42]. In addition, Senna obtusifolia extract, which is rich in betulinic acid, showed cytotoxic effects in human glioblastoma U87MG and leukemic NALM6 cells [19,43]. Daucus carota, a member of the Apiaceae family, contains bioactive carotenoids (beta-carotene and lutein), polyacetylenes, falcarindiol and falcarindiol-3-acetate, which may be effective in the treatment of leukemia [44]. In addition, Leonurus sibiricus or Leonotis nepetifolia, of the Lamiaceae, containing phenolic acids and flavonoids, were found to demonstrate cytotoxic effects against breast, leukemia, and human glioblastoma cancer cell lines [21,24,45]. In the Brassicaceae, Brassica oleracea exerts anticancer effects which have been attributed to the presence of sulforaphane, which can be used to decrease prostate specific antigen (PSA) levels [46]. In addition, alkaloid-rich Papaver somniferum extract was proved to have a cytotoxic effect against various cancer cell lines [47]. In turn, Plantago lanceolata extract, of the Plantaginaceae, has demonstrated a cytotoxic effect against several breast cancer cell lines, which has been associated with its flavonoid glycosides content [48]. Patients with benign prostatic hyperplasia treated with Solanum lycopersicum (of the Solanaceae family) with Serenoa repens, lycopene and bromelain exhibited an improvement in their lower urinary tract symptom-related quality of life [49].
The drugs used in anticancer therapy are mainly based on limiting the division of pathological cells and inducing apoptosis. The currently used anticancer cytostatic agents most often induce programmed cell death, damaging DNA. The use of natural compounds with potential anticancer activity seems interesting due to the fact that it may open up new possibilities for their use in the development of more effective methods of cancer therapy. Their antitumour activity is often based on a complex mechanism including antioxidant activity, carcinogen inactivation, antiproliferation, cell cycle arrest, the induction of apoptosis and differentiation, the inhibition of angiogenesis, and the abolition of multidrug resistance [50,51,52,53].
Cancer treatment modalities are generally based on combinations of chemotherapy, radiotherapy, surgery, hormone therapy, immunotherapy and targeted drug therapy. Chemotherapy is an important option in the treatment of cancer, and plant-derived chemotherapeutic agents have contributed significantly to advances in its development [54,55,56,57,58,59,60,61,62,63]. A number of clinically-applied agents from plant sources were standard ingredients in many anticancer therapies, including vinblastine, vincristine (Catharanthus sp.), paclitaxel (Taxus sp.), camptothecin derivatives (Camptotheca sp.) and podophyllotoxins (Podophyllum sp.) [9,63,64,65,66,67]. Currently, vincristine encapsulated in liposomes is approved for the treatment of acute lymphoblastic leukemia, while protein-bound paclitaxel particles are approved for the treatment of non-small cell lung cancer, according to a Food and Drug Administration (FDA) report [68]. It is noteworthy that, in some cases, their use is associated with various side effects that might limit their broad clinical use [69].
Plant compounds generally suffer from low bioavailability and hydrophobicity issues, which have been addressed with the use of recently discovered nanomaterials, many of which may also be of natural origin. Nanoparticle application has led to the increase of the concentration of the drug in neoplastic cells with particular receptors on their surface [70,71,72,73,74]. A nanoparticle consists of a drug on the inside, and a so-called “ligand”—i.e., a molecule designed to bind to a tumour cell receptor—on the outside. After binding to the receptor, the nanoparticles are absorbed into the cell and the drug is released. Compounds of plant origin (pure compounds or extracts) have been used in combination with nanoparticles and with chemotherapeutic agents in adjunctive therapies [75,76].
However, it should be noted that plant preparations have more complicated and unpredictable interactions with drugs than would be expected between two conventional drugs due to the numerous active compounds found in the plant raw materials. This may be due to the fact that compounds of plant origin may influence the pharmacokinetics and pharmacodynamics of the anticancer drugs used. As a consequence, toxic drug effects may be observed or treatment efficacy may be reduced [77,78,79,80]. So far, numerous studies have highlighted the positive effects deriving from the co-administration of drugs with plant extracts. For example, Hussain et al. reported a synergistic effect between cisplatin and Aloe vera extract on MCF-7 and HeLa cancer cell lines, suggesting that the plant extract may increase the therapeutic efficacy of conventional anticancer drugs [81]. In addition, Senna obtusifolia extract was found to have a synergistic effect in combination with doxorubicin [43].
4. Nanotechnology and Plant Compounds in the Fight against Cancer
The advance of modern technology has brought new products and research techniques which have driven significant scientific progress. Nanotechnologies have successfully entered everyday life, and are increasingly used in medical sciences. Many common devices are based on the achievements of modern nanotechnology, such as energy-efficient and powerful electronic devices, versatile nanocoatings, and new-generation cosmetics [82,83,84]. In its simplest definition, nanotechnology is a “nano-scale technology”, i.e., a technology in the size range 1–100 nm. For a better understanding of these sizes, the nanometer scale (nm) is one billionth of a meter, or three to five atoms wide: less than one tenth of a micrometer in at least one dimension.
The latest scientific achievements may turn out to be effective treatments for diseases that have been troubling people for centuries, among which cancer is still a challenging and often unresolved issue. In the past, the detection of neoplastic diseases was possible only after the appearance of specific symptoms, generally in an advanced stage of the disease, and even in the presence of distant metastases. A more complete view of pathologically-changed tissues can be obtained by biopsy; however, this method has many limitations, and carries the risk of complications [85,86]. In response, highly-sensitive non-invasive methods of detecting neoplastic diseases have been developed, most of which rely heavily on nanotechnology [87].
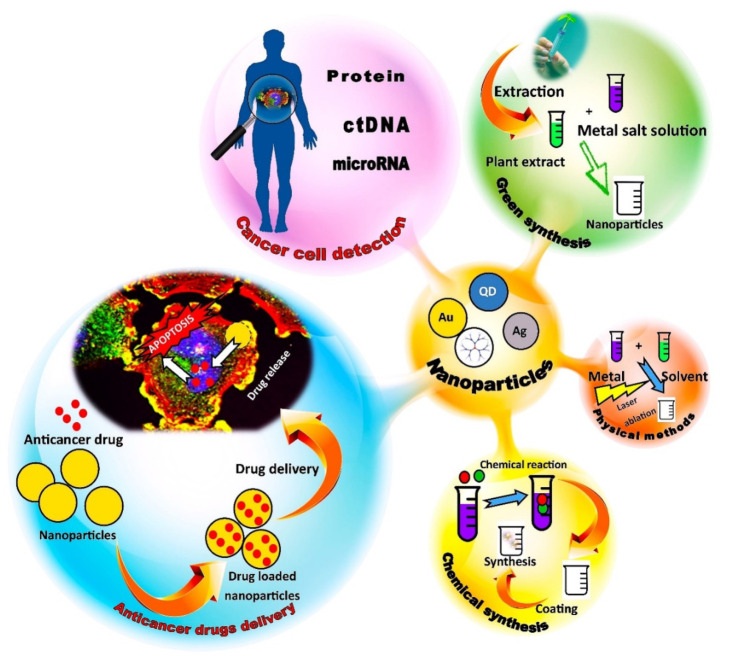
In fact, nanomaterials are widely used in the diagnosis and treatment of different types of cancer due to the possibility of precisely controlling their shapes, sizes and specific physical properties. Nanoparticles can also serve as carriers of anticancer drugs to specific cells [88], and nanomaterial-based devices used to detect the proteins or nucleic acids of cancer cells can provide an early indication of disease or monitor the effectiveness of therapy. Such biomarkers can be detected in body fluids such as blood, saliva and urine. One such group of tumour biomarkers are proteins. A number of biomarkers are routinely tested in clinical practice—PSA (prostate cancer), CEA (colorectal cancer), CA-125 (ovarian cancer), ER (breast cancer), AFP (liver cancer) and CA 19-9 (pancreatic cancer)—and nanosensors can be successfully used to detect them [89,90,91,92,93,94]. The most frequently used nanoparticles in the diagnosis of cancer diseases are gold nanoparticles, nanoshells and quantum dots [95,96].
Nanoparticles such as micelles, dendrimers, quantum dots, liposomes and carbon nanotubes can also be used in the treatment of neoplastic diseases. Traditional chemotherapeutics include alkylating agents and antibiotics that induce damage to the DNA of cancer cells. Topoisomerase or mitosis inhibitors are also used [97]. Many of these therapeutics are highly effective, but they often demonstrate a lack of specificity, resulting in severe side effects [98]. There is a clear need for new methods allowing for the effective and specific targeting of neoplastic cells. One potential strategy that has received much attention over the past few years involves the use of nanoparticles [99,100,101], as well as those based on a combination of modern nanotechnology with a rich arsenal of compounds of natural origin with anticancer properties [102,103,104,105,106].
The nanoparticles themselves are typically obtained by electrospraying, evaporation–condensation, laser ablation or pyrolysis, or high-energy ball milling. They can also be obtained chemically by chemical vapor synthesis, the sol-gel method, hydrothermal synthesis, microemulsion technique, or polyol synthesis [107,108]. It is worth emphasizing that physical methods sometimes have an advantage over chemical methods due to the lack of danger of solvent contamination in the prepared thin films, and due to the uniformity of the synthesized nanoparticle distribution [109]. However, these synthesis methods are often complicated and require strictly controlled temperature, pH and pressure conditions, as well as specialized equipment, and often environmentally-hazardous reagents containing heavy metals [110]. Hence, many research teams are interested in the biological synthesis of nanoparticles, which should offer weak contamination with toxic agents, the customization of desired properties, repeatability and easy scalability [111,112].
Among the various biological systems used for this purpose, plants deserve special attention because plant cells may contain a wide range of bioactive compounds with potential anticancer properties. One study examined the antitumour potential of Nepeta deflersiana extract in silver nanoparticles (ND-AgNPs) against human cervical cancer (HeLa) cells, as well as the influence of cytotoxic concentrations of ND-AgNP on markers of oxidative stress, reactive oxygen species (ROS) production, mitochondrial membrane potential, cell cycle arrest, and apoptosis/necrosis. It was found that the cytotoxicity of the tested particles was concentration dependent, and that the treatment was associated with a significant increase in ROS and lipid peroxidation, and a decrease in matrix metalloproteinases (MMPs) and glutathione levels. The cell cycle analysis and apoptosis/necrosis assay data showed that ND-AgNP induced SubG1 arrest and apoptotic/necrotic cell death [113]. Gomathi et al. examined the potential for silver nanoparticles to be biosynthesized in the fruit shell of Tamarindus indica. Here, too, the plant extract acts as a reducing and stabilizing agent for silver nanoparticles. These nanoparticles proved to be cytotoxic to MCF-7 cell lines; hence, they could be considered as potential therapeutic agents in the treatment of human breast cancer [114].
Because plants from the Solanaceae family produce a number of compounds with proven or potential anticancer activity, they may well be used on a large scale as the basis for new systems for the biosynthesis of nanoparticles exhibiting anticancer activity. Combined with the extremely rapid technological progress, this may be the starting point for the development and implementation of completely new and more effective methods of fighting cancer. The general scheme of the synthesis and application of nanoparticles in cancer diagnosis and treatment is presented in Figure 2.
Figure 2.
General scheme of the synthesis and application of nanoparticles in cancer diagnosis and treatment.
5. Synergy between Chemotherapeutic Agents and Plant Compounds in Cancer Therapy
Despite its many side effects, chemotherapy remains the most popular treatment for cancer. Although many chemotherapeutic compounds are of plant origin (e.g., paclitaxel, camptothecin, colchicine, vincristine, and podophyllotoxin, etc.), being either synthetic or isolated directly from plants, they have considerable side effects. Moreover, their low water solubility, poor penetration into target cells, limited therapeutic potential and toxic side effects may limit the suitability of these natural agents for the treatment of cancer [9,11,63,115,116,117]. Therefore, new phytochemical anticancer agents require substantial evidence of efficacy from appropriate preclinical trials before their approval for use in patients [79,118,119,120,121]. It is also possible to chemically modify the molecule and improve its properties [122].
One new therapeutic strategy which is based on the synergistic action between chemotherapeutic agents and plant compounds intends to overcome these shortcomings. Synergy comes from the Greek word “synergos”, which means “working together”, and is broadly defined as the interaction of two or more compounds or other factors to produce a combined effect greater than the sum of their separate parts [123,124]. Synergistic effects are believed to arise from synergistic multi-target effects, the modulation of pharmacokinetic or physicochemical effects, interference with resistance mechanisms, or elimination and neutralization potentials [125,126,127,128]. Studies show that a secondary compound or plant extract—such as essential oil derivatives, polyphenol derivatives or terpenoid derivatives—may be capable of removing or neutralizing the toxic effects or side effects of a drug [123,129,130,131].
6. Solanaceae Family—General Characteristics and Application
The Solanaceae (nightshades) are considered to be the third most economically-important family in the plant kingdom after the Poaceae and the Fabaceae. They are also one of the most significant families of trees, shrubs and herbs, with great floristic, phytochemical and ethnobotanical importance, with over 90 genera comprising 3000–4000 species spread all over the world. Almost half of these belong to the large and varied genus Solanum. It is distributed in all continents except Antarctica, with the greatest diversity being observed in Central and South America [132,133,134,135,136]. In addition to Solanum, the leading genera of the Solanaceae family include Atropa, Datura, Capsicum, Nicotiana, Lycium, Hyoscyamus, Lycopersicon, Withania and Petunia. This single-genus hyper-diversity is remarkable in angiosperms, making Solanum interesting from an evolutionary point of view, as well as for its usefulness to humans (Figure 3).
Figure 3.
Selected examples of species from the Solanaceae family exhibiting anticancer activity, such as Solanum tuberosum, Capsicum annuum, Solanum melongena, Lycopersicon esulentum, Nicotiana tabacum, Datura stramonium and Lycium barbarum.
The representatives of the Solanaceae vary extremely in regards to their habit, distribution and morphology, with an astonishing variety of flowers and fruits. The flowers are usually radially symmetrical, with five united sepals, five united petals, five stamens inserted on the tube. The ovary is positioned superior. It consists of two united carpels with the partition walls often present, but more obvious in wild species than domestics. The leaves are alternate, or rarely opposite, and are usually simple. The fruit is a two-chambered capsule called a berry [28,29,137,138,139,140,141,142,143]. In addition to a wide range of other uses (e.g., traditional medicine, traditional culture, pharmacology, and ornamental horticulture), the species of the Solanaceae are of great importance as food crops around the world. In 2020, the global areas cultivated with four basic species— potatoes, tomatoes, aubergines and capsicums (chilies and green peppers)—were 16.5, 5.1, 1.9 and 2.1 million hectares, with productions of 359.1, 186.8, 56.6 and 36.1 million tons, respectively [144]. Moreover, from a biotechnological point of view, species from the seven genera of the Solanaceae have become the subject of genetic research as model plants and/or because of their importance as crops. Model plants include cultivated tomatoes and their wild relatives (genus Solanum, former genus Lycopersicon), tobacco (genus Nicotiana), and species of petunias (genus Petunia) [29,142,143]
The Solanaceae are also known to possess a diverse range of biologically-active compounds that can be used to benefit human health, such as phenolics, alkaloids, saponins, terpenes and lipids. However, toxic alkaloids such as tropane alkaloids or glycoalkaloids are of particular interest because of their reported antimicrobial, anti-rheumatic and antioxidant activities [145]. They have also demonstrated antitumour activity against several types of cancer, including prostate, breast and colon cancer [146,147]. Tropane alkaloids such as atropine, hyoscyamine and scopolamine have a characteristic bicyclic structure, and particularly high concentrations have been found in Datura stramonium, Datura ferox and Datura innoxia. Atropine is a racemic mixture of two enantiomeric forms of hyoscyamine, with the L-enantiomeric form being the active one. Scopolamine, which acts as an antagonist at both the peripheral and central muscarinic receptors, is the most valuable member of a group known as the tropane alkaloids [143,147,148]. This group is highly diverse, being formed from a tropane skeleton, which is highly prone to modification. Tropane alkaloids are found in all plant parts, with the highest concentrations in roots and seeds. Their levels vary according to their species, season, location, and plant organ. From a pharmacological standpoint, they are well known as potent anticholinergic agents, meaning that they inhibit neurological signals from the endogenous neurotransmitter acetylcholine. The symptoms of an overdose may include a dry mouth, ataxia, dilated pupils, convulsions, urinary retention, hallucinations, coma, and death [140,147,149].
Glycoalkaloids are produced in more than 350 plant species, particularly those of the Solanaceae and Liliaceae families. They are a group of glycosidic derivatives of nitrogen-containing steroids consisting of a cholestane skeleton with a carbohydrate moiety of one to five monosaccharides attached at the 3-OH position [150]. Arguably, the most significant glycoalkaloids are α-solanine and α-chaconin, which are contained in potatoes (Solanum tuberosum); solasonin and solamargine, in eggplants (Solanum melongena); and α-tomatin and dehydrotomatin, which are spirosolan-type glycoalkaloids found in tomato plants (Lycopersicon esculentum) [151].
7. Anticancer Effect and Potential Mechanisms of Action of Plant Extracts from the Solanaceae Family
Thanks to their wide range of active substances, plant extracts exert a variety of effects on cancer cells, with some of them having been reported to have inhibitory effects on cell proliferation [152]. Indeed, a number of in vitro and in vivo studies have found extracts from Solanaceae family members to also have strong anticancer properties.
In the Solanum genus, a Solanum lycopersicum leaf extract was shown to exhibit potential antitumour properties against breast cancer cells by modulating the expression of genes associated with cancer growth and progression [153]. In addition, a Solanum lyratum extract taken from the whole plant exhibited a proapoptotic effect against human osteosarcoma epithelial cells. The apoptosis induction took place through a number of routes: the increase of reactive oxygen and nitrogen species production; the decrease of mitochondrial membrane potential; the release of cytochrome c; the activation of caspase 3, 8 and 9; the increase of the level of proapoptotic proteins, including Bax; and the decrease of the level of anti-apoptotic proteins, including Bcl-2 [154]. Solanum nigrum fruit extract has also been found to decrease viability by the induction of apoptosis and cell cycle arrest at the G2/M phase in prostate cancer cells [155], and to inhibit the proliferation, migration and invasion of glioma cells by the induction of their apoptosis [156].
Extracts of Withania species are also indicated to have specific cytotoxic properties against cancer cells. Withania somnifera leaf extract was found to have cytotoxic effects against human osteosarcoma, fibrosarcoma and lung cancer epithelial cells, and to activate tumour suppressor proteins including p53 [157]. Similarly, extracts from different parts of Withania coagulans were found to bestow antiproliferative properties and NFκB pathway induction [158].
In addition, Capsicum annuum seed extract has been shown to inhibit the migration of lung cancer and breast cancer cells by downregulating metalloproteinases MMP-2 and MMP-9, and increasing E-cadherin expression [159]. Furthermore, leaf and shoot extracts of Nicotiana glauca exhibit cytotoxic properties against lung cancer and prostate cancer cells, and demonstrate anti-angiogenic properties in vivo by inhibiting microvessel formation [160].
Recent reports on the anticancer properties of plant extracts in the Solanaceae family are listed in Table 1.
Table 1.
In vitro anticancer effect of plant extracts from the Solanaceae family and their potential mechanisms of action.
| Name of the Species | Part of the Plant | Type of Solvent | Class of Compounds/Compounds Identified in Extract/Fraction | Cancer Cell Lines | Activity/Mechanism/Effect | Ref. |
|---|---|---|---|---|---|---|
| Athenaea velutina Sendtn. | leaves | dichloromethane: methanol (1:1) | phenolic compounds and flavonoids |
MCF-7, HepG2, B16-F10 | Cytotoxic (IC50 values in the range of 1.56–200 μg/mL) (MTT test); inhibition of migration, adhesion, invasion and cell colony formation. | [161] |
| Capsicum annuum L. | red pericarp | water/methanol | capsianoside derivatives | HCT116, PC-3 | Cytotoxic (IC50 = 51 μg/mL and 60 μg/mL) (MTT test) | [162] |
| Capsicum annuum L. | fruits | ethanol | carotenoids, chlorophyll, polyphenols, tannins, and flavonoids | Calu6 | Cytotoxic | [163] |
| Solanum betaceum Cav. | fruits | ethanol | phenolics | HepG2, MDA-MB-231 | Cytotoxic (IC50 values in the range of 30–80 μg/mL) (MTT test) | [164] |
| Datura innoxia Mill. | leaves | water | phenolic and flavonoid contents | K562 | Cytotoxic (IC50 = 0.6 mg/mL) (MTT test); antiproliferative activity by interaction with DNA and histones | [165] |
| Datura stramonium L., Datura inoxia Mill. | leaves | ethyl acetate | rutin, gallic acid, catechin, apigenin and caffeic acid | PC-3, MDA-MB 231, MCF-7 | Cytotoxic (IC50 < 3 μg/mL) (MTT assay); anti-tumour activity (evaluation of haematological, biochemical and histological) | [166] |
| Hyoscyamus reticulatus L., Hyoscyamus tenuicaulis Schönb.-Tem. Lycium shawii Roem. & Schult. and Solanum luteum L. | shoots, leaves, stems |
dichloromethane | - | MOLT-4 | Cytotoxic (IC50 values in the range of 35.5–>50 μg/mL) (MTT test) | [167] |
| Ipomoea batatas (L.) Lam. | root tubers and leaves | methanol/trifluoroacetic acid (TFA), ethanol/TFA, methanol/TFA/water, and ethanol/TFA/water | anthocyanins | MCF-7, HCT-116, and HeLa | Antiproliferative properties | [168] |
| Lycium barbarum L. | fruits (Goji berries) | ethanol | - | T47D | Cytotoxic (IC50 = 0.75 mg/mL) (MTT test); induction of apoptosis by changes of the apoptotic protein expression (increase in pro-apoptotic proteins and a decrease in anti-apoptotic proteins) | [169] |
| Lycium barbarum L. | fruits | - | phenolics | HepG2 | Cytotoxic (18%, at 1600 μg/mL) (MTT test) | [170] |
| Lycium barbarum L. | fruits | methanol/ethyl acetate/petroleum ether | zeaxanthin-rich extract | BJ HEP, A375 | Cytotoxic (IC50 = 75.15 and 85.06 μM for BJ HEP, 62.36 and 92.59 μM for A375) | [171] |
| Lycium barbarum L. | water | pectin-free, polysaccharides fraction |
MCF-10A, MCF-7, HER2, MDA-MB-231 | Cytotoxic 1000 μg/mL (MTT test) | [172] | |
| Lycium barbarum L. | fruits | - | carotenoids | Caco-2 cells | Effect (range from 6.5 to 92.8%) (MTT test) | [173] |
| Lycium barbarum L., Lycium ruthenicum Murr | fruits | ethyl acetate | phenolics flavonoids, carotenoids | MDA | Cytotoxic (EC50 = 4.08 mg/mL); apoptosis via modulating cell cycle arrest, cell apoptosis, and the p53 signalling pathway | [174] |
| Lycium chinense Mill. | fruit (Goji berries) | ethanol | - | LS180 | Cytotoxic (MTT test) | [175] |
| Lycium europaeum L. | fruit | methanol | phenolic, flavonoids, anthocyanins, carotenoids, lycopens, and condensed tannins content | A549, PC12 | Cytotoxic (MTT assay), morphological changes and induction of apoptosis by caspase 3/7 activation | [176] |
| Lycopersicon esculentum Mill. | leaves | hydromethanol, acetone and alkaloid extracts | phenolic compounds, pigments, and alkaloids | AGS | Cytotoxic (IC50 values in the range of 9–171 μg/ mL) | [177] |
| Nicotiana glauca Graham | leaves | ethanol | palmitic acid and scopoletin | CCL-136 | Anti-proliferative effect and induction of apoptosis by changes in mitochondrial and nuclear morphology | [178] |
| Nicotiana glauca Graham | stem | n-hexane | beta-sitosterol, stigmasterol, campesterol, D-alpha-tocopherol, scopoletin, 3,7,11,15-tetramethyl-2-hexadecen-1-ol, Bicyclo[3.1.1]heptanes |
MCF-7 | Cytotoxic (IC50 = 17.98 μg/mL) (MTT test); induction of apoptosis by changes in mitochondrial membrane potential, chromatin condensation and cytoplasmic shrinkage | [179] |
| Physalisalkekengi L. | fruit | chloroform | physalin D | HeLa MCF-7, A431 | Growth inhibition | [180] |
| Physalis angulata L. | leaves | ethanol | - | SKOV3, HL-60 | Cytotoxic (IC50 in the range of 18–375 μg/mL) (MTS test) | [181] |
| Physalis peruviana L. | fruit | ethanol, isopropanol | ursolic acid, rosmarinic acid, gallic acid, quercetin, and epicatechin | HeLa | Cytotoxic (IC50 = 60.48 μg/mL) (Resazurin Reduction) | [182] |
|
Solanum aculeastrum Dunal |
whole plant | methanol | solamargine and solanine | SH-SY5Y | Cytotoxic (IC50 = 10.72 μg/mL) (sulforhodamine B (SRB) colorimetric assay) | [183] |
| Solanum capsicoides All. | seeds | methanol | carpesterol | K562 | Cytotoxic (U251 GI50 = 24.7 μg/mL, MCF-7 GI50 = 27.1 μg/mL, 786-0 GI50 = 25.8 μg/mL, OVCAR-03 GI50 = 24.0 μg/mL, and K562 GI50 = 32.0 μg/mL) (Toxicity Estimation Software Tool (TEST) software) | [184] |
| Solanum chacoense Bitter. | leaves, tubers | methanol | phenolic acids and volatile compounds | MCF-7 | Cytotoxic (IC50 values in the range of 132.9–390.7 μg/mL) (MTT test); induction of apoptosis by changes in expression of proliferation- and apoptosis-related genes (overexpression Bax¸ down-regulation Bcl-2) | [185] |
| Solanum incanum L. | whole plant | acid base precipitation followed by the different ratios of ethanol/H2 O extraction (according to the patents—US patent 7,078,063, EU patent 1,058,334, and Japan patent 3,940,928) | solamargine | B16 | Cytotoxic (IC50 in the range of 2.91–6.85 μg/mL) (MTT test); induction of apoptosis by DNA damage and activation of caspase 9; G0/G1 cell cycle arrest | [186] |
| Solanum incanum L. | fruit | water | - | HCT-116 | Cytotoxic (IC50 = 23.35 μg/mL) (Sulphorhodamine B test); ultrastructural changes (loss of the surface microvilli, mitochondrial damage, formation of autophagic vacuoles, nuclear shrinkage, chromatin condensation and nucleolar changes) |
[187] |
|
Solanum incanum L., Solanum schimperianum Hochst, Solanum nigrum L., Physalis lagascae Roem. & Schult. and Withania somnifera (L.) Dunal |
leaves | methanol | hydroxycinnamic acid amides, steroid alkaloids, steroidal glycoalkaloid fractions | MCF-7, MDA-MB-231, HT-29, HTC-116 | Cytotoxic (IC50 values in the range of μg/mL and 1.29–19.83 μg/mL) (MTT test) | [188] |
| Solanum lycopersicum L. | fruit | methanol | phenolic, ascorbic acids and flavonoid content | HepG2, HeLa | Cytotoxic (IC50 values in the range of 156–212 μg/mL) (MTT test) | [189] |
| Solanum lycopersicum L. | fruit | ethanol/water | carotenoids, phenolics, sterol content, fatty acid | HT-29 | Cytotoxic (IC50 = 150 μg/mL) (MTT test) | [190] |
| Solanum lycopersicum L. | leaves | ethanol | - | A549, HeLa | Cytotoxic (IC50 < 31.25 μg/mL) (MTT); significant caspase-3 activity | [191] |
| Solanum lyratum Thunb. | whole plant | chloroform | - | HSC-3, SAS, CAL-27 | Cytotoxic (IC50 values in the range of 40–80 μg/mL); induction of apoptosis (in extrinsic- and intrinsic-dependent pathways) by changing levels of the proteins p21, p16, CDK2 and CDK6, and cyclins D1 and E. It also promotes proapoptotic proteins Bax and Bad and inhibits anti-apoptotic proteins Bcl-2 and Bcl-xl, promotes ROS and Ca2þ production, decreases mitochondrial membrane potential, increases NO production |
[192] |
| Solanum nigrum L. | whole plant | water | alkaloids, glycosides, flavonoids, polyphenols terpenoids, and saponins | A-375 | Cytotoxic | [193] |
| Solanum nigrum L. | whole plant | water | - | MCF-7 | Cytotoxic (IC50 = 100 μg/mL) (crystal violet staining assay) induction of apoptosis by activation of caspase-3 and loss of mitochondrial integrity. It also inhibited EMT (cancer cell metastasis and migration) by downregulating ZEB1, N-cadherin, and vimentin | [194] |
| Solanum nigrum L. | leaves | water | - | SCC-4 | Cytotoxic (IC50 = 150 μg/mL) (crystal violet staining assay); induction of apoptosis by increasing ROS production, activating caspase-9 and caspase-3, alleviating the inhibition of glucose uptake and loss of mitochondrial integrity | [195] |
| Solanum nigrum L. | fruit | ethanol | phenolic and flavonoid compounds | MCF-7 | Cytotoxic (IC50 value = 40.77 μg/mL) (MTT assay); arrest the cell cycle in the S phase and continued to the G2/M phase | [196] |
| Solanum nigrum L. | whole plants | water | - | HepG2 | Cytotoxic (MTT test); inhibits the proliferation and AKT/mTOR pathway | [197] |
| Solanum paniculatum L. | fruit | ethanol | carotenoids, phenolic compounds | MCF-7 | Cytotoxic (IC50 value = 1.87–30 μg/mL) | [198] |
|
Solanum schimperianum Hochst. ex A.Rich Solanum villosum Mill. Solanum coagulans Forssk. Solanum glabratum Dunal., Solanum incanum L., Solanum nigrum L. |
aerial parts | ethanol | rutin | HepG2, HEK293, MCF-7 | Cytotoxic (IC50 values in the range of 20.4–30.1 μg/mL) (MTT assay) | [199] |
| Solanum sessiliflorum Dunal | pulp/seed | ethanol | caffeic and gallic acids, beta-carotene, catechin, quercetin, and rutin | MCF-7, HT-29 | Cytotoxic (IC50 values in the range of 3–>30 μg/mL) (MTT assay) | [200] |
| Solanum tuberosum L. | tuber, peels, flesh, flowers | water | - | HT-29 | Cytotoxic (IC50 values in the range of 7.2–14.4 mg/ mL) (MTS test); induction of apoptosis by upregulation of caspase-3 protease activity | [201] |
| Solanum tuberosum L. | tubers | water | polyphenol and anthocyanin-rich | U937 | Cytotoxic; expression of specific apoptotic agents, such as caspase 8, 9, 3, and poly (ADP-ribose) polymerase (PARP) | [202] |
| Solanum tuberosum L. | peels | ethanol/water | caffeic, caffeoylquinic acid, O-glycosylated flavonol derivatives and polyamine derivatives | NCI-H460, MCF-7, HepG2, and HeLa |
Cytotoxic (GI50 values in the range of 51–365 μg/mL) | [203] |
| Withania coagulans (Stocks) Dunal | roots, leaves, leaf stalk, and fruit | methanol | flavonoid and phenolic content, myricetin, quercetin, gallic acid, hydroxybenzoic acid | HeLa, MCF-7, RD, RG2 | Cytotoxic (IC50 values in the range of 0.96 μg/mL–6.69 μg/mL (Presto Blue cell metabolic test) | [204] |
| Withania coagulans (Stocks) Dunal | fruits | methanol | withaferin A | MDA-MB-231 | Cytotoxic (IC50 = 40 mg/mL) (MTT assay) | [205] |
| Withania somnifera (L.) Dunal | root | water | - | A375 | Cytotoxic (IC50 = 350 μg/mL) (MTT test); induction of morphological changes (apoptotic body and nuclear blebbing) and DNA fragmentation | [206] |
| Withania somnifera (L.) Dunal | leaves | water | - | HepG2 | Cytotoxic (IC50 = 5.0 mg/mL)(MTT test); induction of apoptosis by caspase-3, -8 and -9 activation | [207] |
| Withania somnifera (L.) Dunal | roots and leaves | water, ethanol, metanol (various methods of extraction and maceration) | withanoside V, withanoside IV, 12-deoxywithastramonolide, withanolide A, and withaferin A | HeLa | Cytotoxic (IC50 = 10 mg/mL) (MTT test) | [208] |
| Withania somnifera (L.) Dunal | roots | ethanol/water | alkaloids, carbohydrates, phytosterols and phenolics | A549 | Cytotoxic (IC50 = 99.7 μg/mL) (MTT test); anticancer activity via antioxidant, apoptotic, autophagy and angiogenesis inhibition mechanisms | [209] |
| Withania somnifera (L.) Dunal | roots | - | withaferin A, whitanolide, withanolide B | Jurkat | Proapoptotic mechanism involves intracellular Ca2+ accumulation and the generation of reactive oxygen species | [210] |
| Withania somnifera (L.) Dunal | leaves | water | - | C6 glioma | Activation of multiple pro-apoptotic pathways, leading to suppression of cyclin D1, Bcl-xl, and p-Akt | [211] |
| Withania somnifera (L.) Dunal | stems | methanol, ethanol, water | withaferin A | MDA-MB-231 | Cytotoxic (IC50 values of 30 and 37 μg/mL) (MTT test) | [212] |
8. Anticancer Effect and Potential Mechanisms of Action of Pure Compounds Isolated from the Solanaceae Family
Although plants and natural extracts are very important sources of biologically-active compounds, the study of their isolated products can provide a starting point for the development of new drug candidates with unique structures and mechanisms of action. Indeed, many of the secondary metabolites produced by the Solanaceae have been found to be of medical importance, with effects on cancer cells [13].
For example, solajiangxins H, solajiangxins I and 7-hydroxylsolajiangxin I isolated from whole plant extracts of Solanum lyratum show cytotoxic effect against intestinal cancer cells [213]. Solanum aculeastrum, containing steroidal glycosides, showed antitumour activity against various cancer cell lines, including lung, colon and cervical cancer cells [214]. In turn, Shieh et al. demonstrated the time- and dose-dependent inhibition of cell viability in α-tomatine-treated non-lung cancer cells [215]. The steroidal alkaloid soladulcidine, isolated from Solanum dulcamara, and ten of its derivatives were shown to have significant antiproliferative effects against prostate cancer cells [216]. In addition, 35 withanolides and withaferin A from the roots and leaves of Withania somnifera have demonstrated efficacy against a wide range of cell lines [217,218]. Withawrightolide and four other withanolides derived from the aerial parts of Datura wrightii were similarly found to exhibit cytotoxic properties against glioma cells [219]. In addition, Physalis peruviana seed extract induced apoptosis in HeLa cells [220].
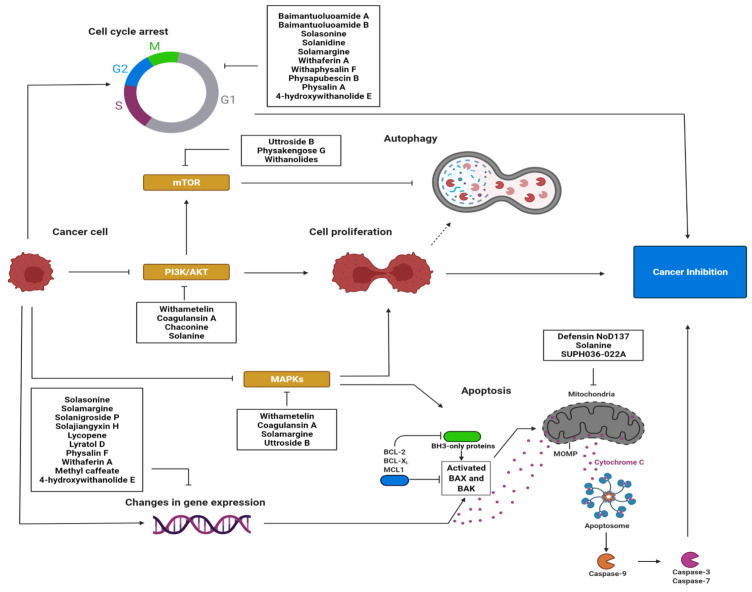
In particular, secondary metabolites of the Solanaceae family are known to induce apoptosis in various types of cancer cells by activating different signalling pathways. These differences may result from both chemical structure of the compounds and specific sensitivity of cancer cells. Such compounds with antiproliferative properties commonly affect processes associated with the cell cycle, gene expression, signal transduction pathways, changes in the mitochondrial membrane, metabolic pathways, and autophagy [31].
The cell cycle is an important mechanism that determines cell proliferation. Alkaloids such as baimantuoluoamide A and baimantuoluoamide B inhibit cyclin-dependent kinase 4 (CDK4) activity, and glycoalkaloids such as solasonine, solanidine, and solamargine induce cycle arrest in the S phase. Arrest in the G2/M phase is induced by solamargine and withaferin A [24]. Withaphysalin F—isolated from the leaves of Acnistus arborescens—also has anti-proliferative properties and the ability to arrest the cell cycle in the G2/M phase, which has been attributed to the inhibition of tubulin polymerization and the induction of DNA fragmentation [221].
The compounds also influence gene expression. For example, withaferin A is known to inhibit transcription factors such as MYB and C/EBPβ [31]. In addition, solasonine, β1-solasonine, solamargine and solanigroside P isolated from the aerial part of Solanum nigrum show antiproliferative properties against gastric cancer cells, and can induce apoptosis by altering gene expression, such as by increasing Bax expression, decreasing Bcl-2 expression, and activating caspase-3 [222]. Lycopene, a carotenoid found commonly in Solanum lycopersicum, was found to regulate the expression of various apoptosis-related proteins and genes—such as caspase-3, caspase-8, Bax, Bax:Bcl-2 and Bcl-xL—among breast cancer cells [223]. Furthermore, physalin F derived from the whole plant Physalis minima has cytotoxic effects and induces the apoptosis of breast cancer cells through caspase-3 activation and DNA fragmentation [224]. In turn, solamargine increased the expression of p53, Bax and Bcl-2 in U2OS and K562/A02 cells on the mRNA and protein levels, and the mRNA expression and promoter activity of EP4, as well as the protein expression of SP1 and NF-κB subunit p65 in lung cancer cell lines [225].
In addition, they can also inhibit various signalling pathways that may be responsible for cell growth and proliferation. For example, withanolide S5 inhibits receptor tyrosine kinases, withametelin and coagulansin A downregulate the Mitogen-Activated Protein Kinase (MAPK) pathway and the phosphatidylinositol-3-kinase (PI3K) pathway, and 4β-hydroxywithanolide E targets the Wnt/β-catenin pathway. Solamargine suppresses the phosphorylation of Akt [225]. In addition, withaferin A inhibits colon cancer by inhibiting Notch-1 signalling, as indicated by the downregulation of Notch-1 targets including Hes-1 and Hey-1; it also inhibits its cross-talk with the Akt/mTOR pathway, thus suggesting the Notch-Akt-mTOR axis as a therapeutic target in colon cancer [226]. Furthermore, α-chaconine and α-solanine reduce the expression and activity of the Akt and ERα signalling pathways in human endometrial carcinoma cells [227]. In addition, arabinogalactan upregulates two of the three MAPK cascades, including c-jun N-terminal kinase (JNK) and p38 kinases, and downregulates the third based on extracellular signal-regulated kinases (ERK), and scopoletin demonstrates a strong binding affinity with vascular endothelial growth factor (VEGFA), which is involved in signalling [31].
Solanaceae-isolated compounds may also induce apoptosis by influencing the mitochondrial membrane. Defensin (NoD173), for example, permeates the mitochondrial outer membrane, resulting in the potential collapse of the membrane, followed by the release of cytochrome c and the activation of caspases. In turn, α-solanine was found to induce mitochondrial mediated apoptosis by opening pores and inducing the release of cytochrome c and Smac from mitochondria into the cytosol, further activating caspase-9 and decreasing the mitochondrial membrane potential [228].
They may also alter metabolic pathways: physapubescin I blocks kidney-type glutaminase, an enzyme involved in ATP production. Its downregulation may inhibit the growth and proliferation of cancer cells. Finally, physapubescin B is known to activate autophagy via mTORC1 inhibition, while physapubenolide downregulates key proteins involved in the process [31].
Recent reports on the anticancer properties of pure compounds isolated from plants from the Solanaceae family are listed in Table 2.
Table 2.
In vitro anticancer effect of pure compounds isolated from the Solanaceae family, and their potential mechanisms of action.
| Name of the Species | Part of the Plant | Compounds/Fraction | Cancer Cell Lines | Activity/Mechanism/Effect | Ref. |
|---|---|---|---|---|---|
|
Brugmansia suaveolens (Humb. & Bonpl. ex Willd.) Bercht. & J.Presl |
leaves | SUPH036-022A | MCF7, A549 | Cytotoxic (MTT test) and induction of apoptosis by loss of mitochondrial integrity and increase of ROS | [229] |
| Capsicum annuum L. | pericarp | polyphenolic content | U937 | Cytotoxic (Trypan blue assay) | [230] |
| Capsicum chinenses L. | fruits | capsaicin and dihydrocapsaicin | SH-SY5Y | Cytotoxic (IC50 = 69.75 μg/mL) (Trypan blue assay) | [231] |
| Datura innoxia Mill. | aerial parts | dinnoxolide A, 21,27-dihydroxy-1-oxowitha-2,5,24-trienolide, daturamalakin B, withametelin | U251 and SK-LU-1 | Cytotoxic (IC50 values in the range of 1.2–19.6 μM) (SRB assay) | [232] |
| Datura inoxia Mill. | leaves | phytosterol, rinoxiaB | HCT 15 | Cytotoxic (IC50 = 4 μM), apoptotic effects by targeting BAX/Bcl2 pathway | [233] |
| Datura metel L. | seeds | indole alkaloids, daturametelindoles A–D |
SGC-7901, Hepg2, MCF-7 | Cytotoxic (IC50 values in the range of 6.73–47.63 μM/mL) (MTT test) | [234] |
| Datura metel L. | whole plants | steroidal saponins (metelosides A–E) | HepG2, MCF-7, and SK-Mel-2 | Cytotoxic (SRB assay) | [235] |
| Lycium ruthenicum Murray | fruits | petunidin 3-O-[6-O-(4-O-(trans-p-coumaroyl)-α-l-rhamnopyranosyl)-β-d-glucopyranoside]-5-O-[β-d-glucopyranoside] | DU-145 | Cytotoxic (IC50 = 361.58 μg/mL) (MTT test), apoptosis through the ROS/PTEN/PI3K/Akt/caspase 3 signalling pathway | [236] |
| Lycium shawii Roem. & Schult | whole plant | aloe emodin, dehydrocostus lactone costunolide, lyciumate, aloe emodine 11-O-rhamnoside, emodin-8-O-β-d-glucoside and lyciuma | MDA-MB-231 | Cytotoxic (IC50 values in the range of >72 μg/mL) (MTT test) | [237] |
| Physalis alkekengi var. franchetii Mast. | aerial parts | physalin A | A549 | Cytotoxic (IC50 = 28.4 μM/mL) (MTT test); cell cycle arrest in the G2/M phase and increase of ROS | [238] |
| Physalis alkekengi var. franchetii Mast. | - | physakengose G | U-2OS, HOS | Cytotoxic (MTT test), increase of lysosome dysfunction, induction of apoptosis (mitochondrial-dependent pathway) and inhibition of mTOR signalling | [239] |
| Physalis alkekengi var. franchetii Mast. | calyx | withanolides | A549, K562 | Cytotoxic (IC50 value in the range of 1.9–4.3 μM/mL) (MTT test); induction of apoptosis by suppressing the PI3K/Akt/mTOR signalling pathway | [240] |
| Physalis angulata L. | stems and leaves | physangulatins A−N; withaphysalin Y;withaphysalin Z | C4-2B, 22Rvl, 786-O, A-498, ACHN, A375-S2 | Cytotoxic (IC50 values in the range of 0.18–11.59 μM/mL) (MTT test) | [241] |
| Physalis angulata L. | stems and leaves | physalins and analogues (physalins V-IX, 16,24-cyclo-13, 14-seco withanolides) | C4-2B, 22Rv1, 786-O, A-498, ACHN, A375-S2 | Cytotoxic (IC50 values in the range of 0.24–3.17 μM/mL) (MTT test) | [242] |
| Physalis angulata L. | whole plant | physalin B, physalin F | HL60, A549, HeLa, HuCCA-1, HepG2, MDA-MB-231), T47-D), S102, H69AR, MRC-5 | Cytotoxic (IC50 values in the range of 0.76–11.92 μM/mL) (MTT, XTT test) | [243] |
| Physalis angulata L. | aerial parts | withanolide | MG-63, HepG-2, MDAMB-231 | Cytotoxic (IC50 values in the range of 3.50–15.74 μM/mL) | [244] |
| Physalis angulata L. | whole plant | withanolides | A549, HeLa and p388 | Cytotoxic (IC50 values in the range of 1.91–>30 μM/mL) (MTT test); apoptosis-inducing activity by flow cytometric analysis | [245] |
| Physalis crassifolia Benth. | fruits | 17β-Hydroxy-18-acetoxywithanolides | LNCaP, PC-3M, MCF-7, NCI-H460 and SF-268 | Cytotoxic (IC50 values in the range of 0.12–>5.0 μM/mL) (AlamarBlue) | [246] |
| Physalis ixocarpa Lam. | fruits | ixocarpalactone A | SW1990, MCF-7, HeLa | Cytotoxic (IC50 values in the range of 3.22–7.51 μM/mL) (CCK-8 assay); induction of apoptosis by inhibition of PHGDH | [247] |
| Physalis minima L. | whole plant | withanolides | A549, SMMC-7721, MCF-7 | Cytotoxic (IC50 value in the range of 40.01–82.17 μM/mL) (MTT test) | [248] |
| Physalis minima L. | whole plant | 5, 6-β-epoxywithanolides | A549, SMMC-7721, MCF-7 | Cytotoxic (IC50 values in the range of 31.25–80.14 μM/mL) (MTT test) | [249] |
| Physalis minima L. | aerial parts | withanolide E, withaperuvin C, 4b-hydroxywithanolide E, 28-hydroxywithaperuvin C, physaperuvin G, and 4-deoxywithaperuvin | HepG2, SK-LU-1, and MCF7 | Cytotoxic (IC50 in the range of 0.051–0.86 μg/mL) | [250] |
| Physalis minima L. | aerial parts | physaminilides HeK, withanolides | A375 | Cytotoxic (IC50 values in the range of 1.2–7.5 μM/mL) (MTT assay) | [251] |
| Physalis peruviana L. | seeds | perulactones I–L, 17-deoxy-23β-hydroxywithanolide E, 23βhydroxywithanolide E, 4-deoxyphyperunolide A, 7β-hydroxywithanolide F, 7βhydroxy-17-epi-withanolide K, 24,25-dihydro-23β,28-dihydroxywithanolide G, and 24,25-dihydrowithanolide E, withanolides | LNCaP, 22Rv1 ACHN, M14, SK-MEL-28 | Cytotoxic (IC50 values in the range of 0.11–> 2 μM/mL) (MTS assay) | [252] |
| Physalis peruviana L. | aerial parts | 4-hydroxywithanolide E | HT-29, HCT116, Caco-2 | Cytotoxic (IC50 = 0.84 μM/mL) (CCK-8); cell cycle arrest in the G0/G1 phase (at low concentrations) and induction of apoptosis (at higher concentrations) by changes in apoptosis-related proteins and genes and histone modification | [253] |
| Physalis philadelphica Lam. | aerial parts | 7-epi-philadelphicalactone A; withaphysacarpin philadelphicalactone C, ixocarpalactone A |
LNCaP, ACHN, UO-31, M14,SK-MEL-28 | Cytotoxic (IC50 values in the range of 0.06–>10 uM/mL) (MTS assay) | [254] |
| Physalis pubescens L. | Fruits | physapubescin B | SKOV3, HepG2, MDA-MB-231, PC-3, Du145 | Cytotoxic (IC50 values in the range of 1.85–16.05 μM) (MTT test); cell cycle arrest in the G2/M phase (associated with reduced Cdc25C levels and increased levels of CyclinB1, p21 as well as p-Cdk1) |
[255] |
| Physalis pubescens L. | stems and leaves | physapubescin E physapubside A physapubside B physapubescin F physapubside C physapubescin G physapubescin H physapubescin I and two withanolides |
C4-2B, 22Rvl, 786-O, A-498, ACHN, Caki-2, A375-S2, A375 | Cytotoxic (IC50 values in the range of 0.17–5.30 μM/mL) (MTT test) | [256] |
| Physalis pubescens L. | fruits | physapubescin B | ES-2, A2780, A2780/TR | Induction of apoptosis and cell-cycle arrest | [257] |
| Physalis pubescens L. | fruits | physapubescin I | SW1990 | Cytotoxic (IC50 in the range of 2.06–5.04 μM/mL) | [258] |
| Salpichroa scandens Dammer | aerial parts | salpichrolides A, C, D, G, M, S, T, and 2,3-dihydrosalpichrolide B and derivatives | LNCaP, PC-3, MCF-7, T47D | Cytotoxicity (IC50 values in the range of 29.97–64.91 μM/mL) (MTS assay) | [259] |
| Solanum capsicoides All. | seeds | carpesterol | U251, MCF-7, 786-0, OVCAR 03, K562 | Cytotoxic (GI50 values in the range of 24.0–226.3 μg/mL) | [184] |
|
Solanum incanum L., Solanum schimperianum Hochst, Solanum nigrum L., Physalis lagascae Roem. & Schult. and Withania somnifera (L) Dunal |
leaves | steroidal glycoalkaloid fractions | MCF-7,MDA-MB-231, HT-29, HTC-116 | Cytotoxic (IC50 values in the range of 1.29–>50 μg/mL) (MTT test) | [188] |
| Solanum lycopersicum L. | different parts | α-tomatine | CT-26 | Inhibition of tumour growth and induction of apoptosis through caspase-independent signalling pathways | [260] |
| Solanum lyratum Thunb | whole plant | sesquiterpenoids including solajiangxin H and lyratol D | MCF-7, HCT-8, A549, SGC-7901, BEL-7402) | Cytotoxicity (IC50 value in the range of 4.8–5.9 μg/mL) (CCK-8); induction of apoptosis (mitochondrial-dependent pathway) by changes in apoptosis-related proteins | [261] |
| Solanum lyratum Thunb. | whole plant | steroidal compounds | SGC-7901, BEL-7402 | Cytotoxic (IC50 value in the range of 0.39–71.89 μmol/mL) (MTT test) | [262] |
| Solanum melongena L. | fruit peels | solasonine; solasodine; solamargine |
Huh7, HepG2 | Cytotoxic (IC50 values in the range of 9.6–91.8 μM/mL) (SRB assay); cell cycle arrest in S-phase, induction of apoptosis, | [263] |
| Solanum melongena L. | sepals | melongenamides H-I | HeLa, Ishikawa and MGC-803 | Cytotoxic (IC50 values in the range of 15.3–32.1 μM/mL) (CCK8 assay) | [264] |
| Solanum nigrum L. | whole plant | degalactotigonin, solasodine, O-acetyl solasodine, and soladulcoside A | PANC1, MIA-PaCa2, A549, NCI-H1975, and NCI-H1299 | Cytotoxic (IC50 values in the range of 2.9–>30) (Cell Migration Assay),; induces apoptosis and cell cycle arrest via inhibiting the EGFR signalling pathways | [265] |
| Solanum nigrum L. | fruits | solaoiacid | A549 | Cytotoxic (IC50 = 2.3 μmol/mL (MTT assay) | [266] |
| Solanum nigrum L. | fruits | alkaloid glycosides | HL-60, U-937, Jurkat, K562, and HepG2 | Cytotoxic (IC50 values in the range of 2.72–39.19 μM/mL) (MTT assay) | [267] |
| Solanum nigrum L. | leaves | uttroside B | HepG2 | Cytotoxic (IC50 = 0.5 μM) (MTT test); induction of apoptosis by down-regulating the activation of MAPK and mTOR pathways | [268] |
| Solanum nigrum L. | - | degalactotigonin | different lines of osteosarcoma cells | Cytotoxic (IC50 values in the range of 12.91–31.46 μM/mL) (MTT test); induction of apoptosis, suppression of migration and invasion by repression of the Hedgehog/Gli1 pathway through GSK3b inactivation. | [269] |
| Solanum nigrum L. | fruits | solanine A; 7a-OH khasianine, 7a-OH solamargine; 7a-OH solasonine |
MGC803, HepG2, SW480 | Cytotoxic (IC50 values in the range of 6.00–9.25 μM/mL) (SRB assay) | [270] |
| Solanum septemlobum Bunge | whole plant | septemlobin D and 11,12-O-isopropylidenesolajiangxin F | P-388, HONE-1 and HT-29 | Cytotoxic (IC50 values in the range of 3.0–7.3 μM/mL) (MTT test) | [271] |
| Solanum torvum Swartz. | Fruits | methyl caffeate | MCF-7 | Cytotoxic (IC50 = 0.62 μM/mL) (MTT test); induction of apoptosis by caspase activation via cytochrome c release from mitochondria. Further, increased DNA fragmentation, apoptotic body and changes in apoptosis-related proteins (Bcl-2, Bid and Bax) | [272] |
| Withania adpressa Coss. | leaves | glycowithanolide named wadpressine, withanolide F, withaferin A, coagulin L and nicotiflorin | MM-CSCs, RPMI 8226 | Cytotoxic (IC50 values in the range of 0.1–>20 μM/mL) (MTT test) | [273] |
| Withania somnifera (L.) Dunal | roots | withasilolides A−F, withanone | A549, SK-OV-3, SK-MEL-2, and HCT-15 | Cytotoxic (IC50 values in the range of <10.0 μM/mL) (SRB assay) | [274] |
| Withania somnifera (L.) Dunal | leaves | withaferin A and its derivatives | PANC-1, DU145, MCF7 | Cytotoxic (IC50 values in the range of 1.1–>25 μM/mL) | [275] |
| Withania somnifera (L.) Dunal | roots | protein fraction | MBA-MB-435, MDA-MB-231, T47D, MCF-7, HCT-116, A549 | Cytotoxic (IC50 = 92 μg/mL) (MTT test); induction of apoptosis by decrease of the mitochondrial membrane potential levels, promotion of the reactive oxygen species production, changes in apoptosis-related proteins regulation and caspases-3 activation. Further, cell cycle arrest in G2/M-phase. | [276] |
| Withania somnifera (L.) Dunal | roots and leaves | withanoside V, withanoside IV, 12-deoxywithastramonolide, withanolide A, and withaferin A | HeLa | Cytotoxic (IC50 value in the range of 3.2 to 7.7 μM/mL) (MTT test) | [208] |
The mechanisms of action described in the text and included in Table 2 are presented in Figure 4.
Figure 4.
Schematic diagram presenting the potential anticancer effect of compounds from the Solanaceae family through the induction of apoptosis and the activation of signalling pathways in cancer cells (created using BioRender).
9. Anticancer Effect and Potential Mechanisms of Action of Nanoparticles in Combination with Plant Extracts from the Solanaceae Family
Plant-based nanomaterial synthesis has been growing in popularity. The approach is more environmentally friendly than chemical or physical methods, and many studies have reported that it yields nanoparticles with improved pharmacological properties [277]. Regarding extracts from the Solanaceae, the available data indicate that silver nanoparticles generated by Datura inoxia exert significant antiproliferative effect against lung cancer cells. They also induce apoptosis cell cycle arrest and inhibit DNA synthesis [278]. Recent reports on the anticancer properties of nanoparticles using extracts from the Solanaceae family are listed in Table 3.
Table 3.
Anticancer effect of nanoparticles in combination with plant extracts from the Solanaceae family, and their potential mechanisms of action.
| Name of the Species | Part of the Plant | Type of Solvent/Active Compounds | Type of Nanoparticles | Cancer Cell Lines | Activity/Mechanism/Effect | Ref. |
|---|---|---|---|---|---|---|
| Atropa acuminate Royle ex Lindl. | leaves | water/total phenolic, flavonoid and tannin | Ag | HeLa | Cytotoxic (IC50 = 5.418 μg/mL) (MTT test) | [279] |
| Lycium chinense Mill. | fruits | water | Au, Ag |
MCF 7 | Cytotoxic (MTT test) | [280] |
| Lycopersicon esculentum L. | fruits | benzene/lycopene | Ag, Au, Fe | COLO320DM, HT29 and HeLa | Cytotoxic (MTT test) | [281] |
| Solanum elaeagnifolium Cav. | leaves | water | Ag-AgO-Ag2O | A-549 | Cytotoxic (IC50 = 67.09 μg/mL) (MTT test) | [282] |
| Solanum incanum L. | leaves | water | Ag-NPs | HepG2, MCF-7 | Cytotoxic (IC50 values in the range of 21.76–129.9 μg/mL) (MTT test) | [283] |
| Solanum lycocarpum A.St.-Hil. | fruits | glycoalkaloids | NP-AE | RT4 | Cytotoxic (2D model: IC50 = 4.18 μg/mL, 3D model: three-fold higher than in 2D cell culture) (2D—the neutral red assay, 3D—CellTiter-Glo®3D); induction of apoptosis by cell cycle arrest | [284] |
| Solanum lycocarpum L. | fruits | ethanol-soluble fraction glycoalkaloids, solamargine and solasonine | AE-loaded folate-targeted nanoparticles | MDA-MB-231, RT4 | Folate-conjugated polymeric nanoparticles are potential carriers for targeted glycoalkaloidic extract delivery to bladder cancer cells (2D model: IC50 = 3.78 μg/mL, 3D model: 7.7 μg/mL) (2D model—Neutral Red Uptake assay, 3D model: CellTiter-Glo®3D) | [285] |
| Solanum lycopersicum L. | tomato’s pomase | ethyl acetate/lycopene | lycopene-NPs | MCF-7, HCT-116, HepG2, | Cytotoxic (IC50 in the range of 72.40–92.54 μg/mL) (MTT test) | [286] |
| Solanum muricatum L. | leaves | water | Ag | HeLa | Cytotoxic (IC50 = 37.5 μg/mL) (MTT assay) | [287] |
| Solanum trilobatum L. | unripe fruits | water | Ag | MCF7 | Cytotoxic (MTT test); induction of apoptosis by changes in expression of proliferation- and apoptosis-related genes (overexpression Bax¸ down-regulation Bcl-2), and activation of caspases 3 and 9 | [288] |
| Solanum trilobatum L. | leaves | water | Mn-Ag co-doped FeO | MCF-7, HeLa | Cytotoxic (IC50 value in the range of 37.11–60.49 μg/mL) (MTT test) | [289] |
| Solanum xanthocarpum Schrad. & Wendl | leaves | water | Au | C666-1 | Cytotoxic (MTT test); triggering cell death by autophagy and apoptosis (mitochondrial-dependent pathway) | [290] |
| Withania somnifera L. | leaves | water/total flavonoid, phenolic and tannin | Se | A549 | Cytotoxic (IC50 = 25 μg/mL) (MTT test) | [291] |
| Withania somnifera L. | leaves | water/phenolic, flavonoid and tannin | Zn | HEP2, PC3, MCF-7, HCT-116, | Cytotoxic (IC50 value in the range of 19.17–88.3 7 μg/mL) (MTT test) | [292] |
10. Synergistic Effect of Chemotherapeutic Drugs and Plant Extracts from the Solanaceae Family
The occurrence of drug resistance indicates the need to search for new chemotherapeutic agents and improved combinations of them. Combined anticancer therapy uses drugs that target different pathways, as this can result in improved cytotoxicity for the cancer cell, with both additive and synergistic effects [293]. Synergy can also be observed between conventional drugs and chemical compounds and extracts, and some plant-derived compounds have been found to improve the effeciency of anticancer therapy [124]. For example, Solanum nigrum leaf extract has been found to enhance the effect of cisplatin, doxorubicin, docetaxel and 5-fluorouracil, resulting in the induction of intestinal cancer cell autophagy through the accumulation of microtubule-associated proteins [294]. Moreover, whole-plant Solanum nigrum extract has intensified the effect of doxorubicin in the suppression of the growth of HeLa [295] and breast cancer cells [296]. Recent reports on the synergistic properties of extracts from the Solanaceae family and anticancer drugs are listed in Table 4.
Table 4.
Anticancer synergistic effect of chemotherapeutic drugs and plant extracts from the Solanaceae family.
| Name of the Species | Part of the Plant | Type of Slovent or Fraction or Compound | Chemotherapeutic Drugs | Cancer Cell Lines | Activity/Mechanism/Effect | Ref. |
|---|---|---|---|---|---|---|
| Capsicum frutescens L. | - | capsaicin | doxorubicin | Caco-2 and CEM/ADR 5000 | Enhancement of the doxorubicin cytotoxicity in cancer cells and chemosensitizing activity (inhibition of P-glycoprotein activity) | [297] |
| Lycium barbarum L. | fruits | water | doxorubicin | MCF-7, MDA-MB-231 | Enhancement of the doxorubicin cytotoxicity in cancer cells | [298] |
| Solanum cernuum Vell. | leaves | cernumidine | cisplatin | T24, RT4, 5637 | Enhancement of the cisplatin cytotoxicity in cancer cells. Inhibition of cell migration, down-regulation of MMP-2/9 and p-ERK1/2, increase EGFR activity. Furthermore, down-regulation of Bcl-2, up-regulation of Bax and reduction of the mitochondrial membrane potential | [299] |
| Solanum incanum L. | extract—according to the patent (US patent 7,078,063, EU patent 1,058,334, and Japan patent 3,940,928) SR-T100 |
extract containing solamargine | cisplatin, paclitaxel | ES2, TOV-21G, IGROV1, A2780, A2780CP70, ov2008 and ov2008CP20 | Suppression of C/EBPβ and COL11A1 expression and its promoter activity | [300] |
| Solanum nigrum L. | leaves | water | cisplatin, doxorubicin | Hep3B, HepJ5 | Induction of caspase-7 and accumulation of microtubule associated protein-1 light chain-3 A/1B II | [301] |
| Solanum nigrum L. | leaves | water | cisplatin, doxorubicin, docetaxel | ES-2, SKOV-3, OVCAR-3 | Induction of caspase-3 and accumulation of microtubule associated protein-1 light chain-3 A/1B II | [302] |
| Solanum nigrum L. | unripe fruit | glycoside fraction (methanol) | doxorubicin | NCI/ADR-RES | Overcoming doxorubicin resistance by inhibiting the JAK-STAT3 signalling pathway by downregulation of JAK1, STAT3, pSTAT3, and Mdr1 expression. Furthermore, the cell growth suppression was proven to be apoptotic, based on results obtained from DNA fragmentation, annexin V apoptosis assay and PARP cleavage analysis.” | [303] |
11. Anticancer Effect in In Vivo Studies of Compounds of the Solanaceae Family
Due to due to their high content of bioactive compounds, Solanaceae family members have also been used in a number of in vivo studies. This review categorizes in vivo studies as extracts, pure compounds, nanoparticle extracts and chemotherapeutic extracts. For example, Wu et al. showed that SR-T100—extracted from Solanum incanum (solamargine alkaloid)—caused all papillomas (35/35) and 27 of the 30 UVB-induced microinvasive squamous cell carcinoma in hairless mice to disappear within 10 weeks of the daily use of topical SR-T100 [304]. In other studies, Wu et al. found that Solanum incanum extract (SR-T100) paclitaxel and cisplatin inhibited the growth of A2780CP70 cells in mouse xenografts, compared to the vehicle control, and that the combination of cisplatin and SR-T100 was more effective than either treatment alone. The authors suspect that SR-T100 may represent a potential therapeutic adjunct to chemotherapy for ovarian cancer treatment [300]. Furthermore, Solanum lyratum aerial part extract was found to significantly inhibit the growth of S180 sarcoma in mice in vivo, and to increase the proliferation of splenocytes, natural killer cells and cytotoxic T cells, as well as interleukin 2 and interferon-γ, by splenocytes. The authors propose that the extract exhibits its anti-tumour effects through its immunomodulatory properties [305]. Solasodine and rhamnosyl glycosides isolated from Solanum sodomaeum were found to demonstrate antitumour properties in a mouse model [306].
In turn, Deng et al. revealed that the fraction from Lycium barbarum polysaccharide could reduce immunotoxicity and enhance the antitumour activity of doxorubicin in mice. The results showed that Lycium barbarum polysaccharide did not protect against the bodyweight loss caused by doxorubicin, but it promoted the recovery of bodyweight starting at day 5 after doxorubicin treatment in tumour-free mice. Lycium barbarum polysaccharide also improved peripheral blood lymphocyte counts, promoted cell cycle recovery in bone marrow cells, and restored the cytotoxicity of natural killer cells. Furthermore, in H22 tumour-bearing mice, Lycium barbarum polysaccharide enhanced the antitumour activity of doxorubicin, and improved the peripheral blood lymphocyte counts and the cytotoxicity of splenocytes [307]. Diwanay et al. noted that the alkaloid-free polar fraction of Withania somnifera resulted in protection towards cyclophosphamide-induced myelo- and immunoprotection, as was evident from the significant increase in white cell counts and hemagglutinating and hemolytic antibody titers. Treatment with these candidate drugs may be important in the development of adjunctive therapy with anticancer chemotherapy [308].
The anticancer and radio-sensitizing efficacy of a Withania somnifera extract/Gadolinium III oxide nanocomposite (WSGNC) was also investigated in mice. WSGNC treatment combined with γ-radiation led to a significant decrease in the solid Ehrlich carcinoma size and weight in mice; this was associated with a significant decrease in mitochondrial enzyme activities, glutathione content and superoxide dismutase (SOD) activity, as well as a significant increase in caspase-3 activity, malondialdehyde concentration and DNA fragmentation in cancer tissues. The authors indicate that WSGNC can be considered as a radio-sensitizer and an anticancer modulator, suggesting a possible role in the reduction of the radiation exposure dose during radiotherapy [309]. Further studies are presented in the Table 5.
Table 5.
In vivo anticancer effect of plant extracts and pure compounds from the Solanaceae family and their potential mechanisms of action.
| Name of The Species | Part of the Plant | Type of Solvent | Class of Compounds/Compounds Identified in Extract/Fraction | Potential Mechanism of Action | Ref. |
|---|---|---|---|---|---|
| Athenaea velutina Sendtn. | leaves | dichloromethane: methanol (1:1) | phenolic compounds and flavonoids | Suppression of the development of pulmonary melanomas following the intravenous injection of melanoma cells to C57BL/6 mice | [161] |
| Datura stramonium L., Datura inoxia Mill. | leaves | ethyl acetate | rutin, gallic acid, catechin, apigenin and caffeic acid | Alleviative effects in benzene induced leukaemia in Sprague Dawley rats | [166] |
| Physalis alkekengi L. | aerial parts | hydro alcoholic | - | Tumour progression on the 28 ER+ BC BALB/c mice animal model (the tumour size among the different doses of extract lose to 0.6 mm was in the greatest dimension with dosage of 10 mg/kg) | [310] |
| Physalis ixocarpa Lam. | fruits | - | ixocarpalactone A | Inhibition of the tumour growth in a SW1990 xenograft mouse model with low toxicities, suggesting its potential therapeutic application in pancreatic cancer treatment | [247] |
| Physalis pubescens L. | fruits | - | physapubescin B | Antitumour efficacy in human prostate cancer PC3 xenograft in nude mice | [255] |
| Solanum incanum L. | whole plant SR-T100 |
acid base precipitation followed by the different ratios of ethanol/H2 O extraction (according to the patents—US patent 7,078,063, EU patent 1,058,334, and Japan patent 3,940,928) | solamargine | Extract SR-T100-treated C57BL/6 mice, the tumour burden of lung metastases was significantly reduced compared to that in control mice | [186] |
| Solanum incanum L. | whole plant SR-T100 |
acid base precipitation followed by the different ratios of ethanol/H2 O extraction (according to the patents—US patent 7,078,063, EU patent 1,058,334, and Japan patent 3,940,928) | solamargine | Animal experiments showed that all papillomas (35/35) and 27 of 30 UVB-induced microinvasive SCCs in hairless SKH-hr1 female mouse mice disappeared within 10 weeks after once-daily application of topical SR-T100 extract | [304] |
| Solanum lycopersicum L. | different parts | - | α-tomatine | Intraperitoneally administered α-tomatine (5 mg/kg body weight) also markedly inhibited growth of the tumour using CT-26 cancer cells without causing body and organ weight changes. The reduced tumour growth in the BALB/c mice by 38% after 2 weeks was the result of increased caspase-independent apoptosis associated with increased nuclear translocation of AIF and decreased surviving expression in tumour tissues. | [260] |
| Solanum nigrum L. | fruits | methanol | rutin, solasonine, quercetin and solamargine | Reduction of the growth and infiltration of C6 glioma tissue and suppressed the proliferation of tumour cells in Wistar rats brain | [311] |
| Solanum nigrum L. | stems | - | polysaccharide fraction (SN-ppF3) | Tumour suppression mechanisms observed in SN-ppF3-treated mice were most probably due through enhancing the host immune response | [312] |
| Solanum nigrum L. | leaves | - | uttroside B | Drastic inhibition of tumour growth produced by uttroside B in NOD-SCID mice bearing human liver cancer xenografts demonstrates the chemotherapeutic efficacy of uttroside B | [268] |
| Solanum nigrum L. | - | - | degalactotigonin | Degalactotigonin injected intraperitoneally after tumour inoculation, significantly decreased the volume of osteosarcoma xenografts in athymic nude (nu/nu) mice model and dramatically diminished the occurrence of osteosarcoma xenograft metastasis to the lungs | [269] |
| Withania somnifera L. | leaves | water | ASH-WEX extract | Reduced the intracranial tumour volumes in vivo and suppressed the tumour-promoting proteins p-nuclear factor kappa B (NF-κB), p-Akt, vascular endothelial growth factor in the albino rat model of orthotopic glioma allograft | [211] |
12. Conclusions and Future Perspectives
Cancer is a devastating disease, and the currently available treatments for patients are generally associated with undesirable adverse effects. The use of medicinal plants to manage or arrest the carcinogenic process provides an additional strategy that can be used alongside treatments with canonical drugs. Many plant-derived bioactive compounds have achieved favorable results in clinical studies, and their tumouricidal properties against various cancers are under investigation.
This literature review evaluated the anticancer properties of natural products from the Solanaceae family. They were grouped in terms of extracts, pure compounds, nanoparticles with extracts, and chemotherapeutic agents with extracts, and their potential mechanisms of action were given. Although all of the studies found the extracts to demonstrate strong in vitro and in vivo anticancer activity in cancer cell lines and animal models, more research is needed in order to elucidate their specific mechanisms of action, and to determine their potential for cancer prevention and treatment.
Plants of the Solanaceae family are widely discussed due to their multi-directional activity. Multiple in vitro studies have been reported with promising results. On the other hand, the anti-tumour potential of the secondary metabolites from Solanaceae is also quite clear. In addition, nanotechnology techniques can enhance their action and eliminate negative effects on normal cells. Thus, plants of the Solanaceae family should be tested further in order to better elucidate their therapeutic potential not only in in vitro and in vivo studies but also in clinical applications. However, the study of these plants should not limit the study of the plethora of anticancer plants, some of which are still unexplored. Research is needed in order to elucidate the antitumour mechanism of action of many already studied and unexplored plants.
Author Contributions
Conceptualization, P.S. and T.K.; investigation, P.S., T.K., K.G. and A.M.-S.; writing—original draft preparation, P.S., T.K. and A.M.-S.; writing—review and editing, M.B., J.P., S.H., M.M. and P.R.; visualization, T.K., P.S. and A.M.-S.; supervision, T.Ś., J.S. and J.P. All authors have read and agreed to the published version of the manuscript.
Funding
The work was supported by the Medical University of Lodz, 503/3-012-01/503-31-001-19-00, 503/3-012-01/503-90-000.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Golemis E.A., Scheet P., Beck T.N., Scolnick E.M., Hunter D.J., Hawk E., Hopkins N. Molecular mechanisms of the preventable causes of cancer in the United States. Genes Dev. 2018;32:868–902. doi: 10.1101/gad.314849.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parsa N. Environmental factors inducing human cancers. Iran. J. Public Health. 2012;41:1–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Wu S., Zhu W., Thompson P., Hannun Y.A. Evaluating intrinsic and non-intrinsic cancer risk factors. Nat. Commun. 2018;9:3490. doi: 10.1038/s41467-018-05467-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anand P., Kunnumakara A.B., Sundaram C., Harikumar K.B., Tharakan S.T., Lai O.S., Sung B., Aggarwal B.B. Cancer is a preventable disease that requires major lifestyle changes. Pharm. Res. 2008;25:2097–2116. doi: 10.1007/s11095-008-9661-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 7.Feitelson M.A., Arzumanyan A., Kulathinal R.J., Blain S.W., Holcombe R.F., Mahajna J., Marino M., Martinez-Chantar M.L., Nawroth R., Sanchez-Garcia I., et al. Sustained proliferation in cancer: Mechanisms and novel therapeutic targets. Semin. Cancer Biol. 2015;35:S25–S54. doi: 10.1016/j.semcancer.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Cancer. 2022. [(accessed on 5 January 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer.
- 9.Lichota A., Gwozdzinski K. Anticancer activity of natural compounds from plant and marine environment. Int. J. Mol. Sci. 2018;19:3533. doi: 10.3390/ijms19113533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Senapati S., Mahanta A.K., Kumar S., Maiti P. Controlled drug delivery vehicles for cancer treatment and their performance. Signal Transduct. Target. Ther. 2018;3:7. doi: 10.1038/s41392-017-0004-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X., Zhang H., Chen X. Drug resistance and combating drug resistance in cancer. Cancer Drug Resist. 2019;2:141–160. doi: 10.20517/cdr.2019.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newman D.J., Cragg G.M. Natural products as sources of new drugs over the 30 years from 1981 to 2010. J. Nat. Prod. 2012;75:311–335. doi: 10.1021/np200906s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dehelean C.A., Marcovici I., Soica C., Mioc M., Coricovac D., Iurciuc S., Cretu O.M., Pinzaru I. Plant-derived anticancer compounds as new perspectives in drug discovery and alternative therapy. Molecules. 2021;26:1109. doi: 10.3390/molecules26041109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koparde A.A., Doijad R.C., Magdum C.S. Pharmacognosy—Medicinal Plants. IntechOpen Limited; London, UK: 2019. Natural Products in Drug Discovery. [Google Scholar]
- 15.Veeresham C. Natural products derived from plants as a source of drugs. J. Adv. Pharm. Technol. Res. 2012;3:200–201. doi: 10.4103/2231-4040.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pan S.Y., Litscher G., Gao S.H., Zhou S.F., Yu Z.L., Chen H.Q., Zhang S.F., Tang M.K., Sun J.N., Ko K.M. Historical perspective of traditional indigenous medical practices: The current renaissance and conservation of herbal resources. Evid. Based Complement. Altern. Med. 2014;2014:525340. doi: 10.1155/2014/525340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gordaliza M. Natural products as leads to anticancer drugs. Clin. Transl. Oncol. 2007;9:767–776. doi: 10.1007/s12094-007-0138-9. [DOI] [PubMed] [Google Scholar]
- 18.Alamgir A.N.M. Progress in Drug Research. Volume 74. Springer; Berlin/Heidelberg, Germany: 2018. Biotechnology, in vitro production of natural bioactive compounds, herbal preparation, and disease management (treatment and prevention) pp. 585–664. [Google Scholar]
- 19.Kowalczyk T., Sitarek P., Merecz-Sadowska A., Szyposzyńska M., Spławska A., Gorniak L., Bijak M., Śliwiński T. Methyl jasmonate effect on betulinic acid content and biological properties of extract from Senna obtusifolia transgenic hairy roots. Molecules. 2021;26:6208. doi: 10.3390/molecules26206208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kowalczyk T., Sitarek P., Toma M., Rijo P., Domínguez-Martín E., Falcó I., Sánchez G., Śliwiński T. Enhanced Accumulation of Betulinic Acid in Transgenic Hairy Roots of Senna obtusifolia Growing in the Sprinkle Bioreactor and Evaluation of Their Biological Properties in Various Biological Models. Chem. Biodivers. 2021;18:e2100455. doi: 10.1002/cbdv.202100455. [DOI] [PubMed] [Google Scholar]
- 21.Kowalczyk T., Merecz-Sadowska A., Rijo P., Isca V.M.S., Picot L., Wielanek M., Śliwiński T., Sitarek P. Preliminary phytochemical analysis and evaluation of the biological activity of Leonotis nepetifolia (L.) r. br transformed roots extracts obtained through rhizobium rhizogenes-mediated transformation. Cells. 2021;10:1242. doi: 10.3390/cells10051242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sitarek P., Merecz-Sadowska A., Śliwiński T., Zajdel R., Kowalczyk T. An in vitro evaluation of the molecular mechanisms of action of medical plants from the Lamiaceae family as effective sources of active compounds against human cancer cell lines. Cancers. 2020;12:2957. doi: 10.3390/cancers12102957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Śliwiński T., Sitarek P., Skała E., Isca V.M.S., Synowiec E., Kowalczyk T., Bijak M., Rijo P. Diterpenoids from Plectranthus spp. As potential chemotherapeutic agents via apoptosis. Pharmaceuticals. 2020;13:123. doi: 10.3390/ph13060123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sitarek P., Synowiec E., Kowalczyk T., Śliwiński T., Skała E. An in vitro estimation of the cytotoxicity and genotoxicity of root extract from Leonurus sibiricus L. overexpressing AtPAP1 against different cancer cell lines. Molecules. 2018;23:2049. doi: 10.3390/molecules23082049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao C.Y., Cheng R., Yang Z., Tian Z.M. Nanotechnology for cancer therapy based on chemotherapy. Molecules. 2018;23:826. doi: 10.3390/molecules23040826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheng Z., Li M., Dey R., Chen Y. Nanomaterials for cancer therapy: Current progress and perspectives. J. Hematol. Oncol. 2021;14:85. doi: 10.1186/s13045-021-01096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sanna V., Pala N., Sechi M. Targeted therapy using nanotechnology: Focus on cancer. Int. J. Nanomed. 2014;9:467–483. doi: 10.2147/IJN.S36654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Samuels J. Biodiversity of food species of the Solanaceae family: A preliminary taxonomic inventory of subfamily Solanoideae. Resources. 2015;4:277–322. doi: 10.3390/resources4020277. [DOI] [Google Scholar]
- 29.Gebhardt C. The historical role of species from the Solanaceae plant family in genetic research. Theor. Appl. Genet. 2016;129:2281–2294. doi: 10.1007/s00122-016-2804-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guzmán Ceferino J., Contreras Ezquivel J.C., Aguilar González C.N., López López L.I., Solís Salas L.M., Sierra Rivera C.A., Durán Mendoza T., Silva Belmares S.Y. Bioactive compounds derived from metabolism of Solanaceae with medicinal effects. Acad. J. Med. Plants. 2016;4 doi: 10.15413/ajmp.2016.0XXX. [DOI] [Google Scholar]
- 31.Nkwe D.O., Lotshwao B., Rantong G., Matshwele J., Kwape T.E., Masisi K., Gaobotse G., Hefferon K., Makhzoum A. Anticancer mechanisms of bioactive compounds from Solanaceae: An update. Cancers. 2021;13:4989. doi: 10.3390/cancers13194989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Petrovska B.B. Historical review of medicinal plants’ usage. Pharmacogn. Rev. 2012;6:1–5. doi: 10.4103/0973-7847.95849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Magowska A. Historia farmacji według Zbigniewa Beli. Stud. Hist. Sci. 2018;17:583–599. doi: 10.4467/2543702XSHS.18.023.9343. [DOI] [Google Scholar]
- 35.Yin M., Zhang Y., Li H. Advances in research on immunoregulation of macrophages by plant polysaccharides. Front. Immunol. 2019;10:145. doi: 10.3389/fimmu.2019.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Phillipson J.D. Phytochemistry and medicinal plants. Phytochemistry. 2001;56:237–243. doi: 10.1016/S0031-9422(00)00456-8. [DOI] [PubMed] [Google Scholar]
- 37.Jaradat N., Qneibi M., Hawash M., Al-Maharik N., Qadi M., Abualhasan M.N., Ayesh O., Bsharat J., Khadir M., Morshed R., et al. Assessing Artemisia arborescens essential oil compositions, antimicrobial, cytotoxic, anti-inflammatory, and neuroprotective effects gathered from two geographic locations in Palestine. Ind. Crop. Prod. 2022;176:114360. doi: 10.1016/j.indcrop.2021.114360. [DOI] [Google Scholar]
- 38.Hawash M., Kahraman D.C., Olgac A., Ergun S.G., Hamel E., Cetin-Atalay R., Baytas S.N. Design and synthesis of novel substituted indole-acrylamide derivatives and evaluation of their anti-cancer activity as potential tubulin-targeting agents. J. Mol. Struct. 2022;1254:132345. doi: 10.1016/j.molstruc.2022.132345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Street R.A., Prinsloo G. Commercially important medicinal plants of South Africa: A review. J. Chem. 2013;2013:1–16. doi: 10.1155/2013/205048. [DOI] [Google Scholar]
- 40.Anand U., Jacobo-Herrera N., Altemimi A., Lakhssassi N. A comprehensive review on medicinal plants as antimicrobial therapeutics: Potential avenues of biocompatible drug discovery. Metabolites. 2019;9:258. doi: 10.3390/metabo9110258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hui C., Bin Y., Xiaoping Y., Long Y., Chunye C., Mantian M., Wenhua L. Anticancer activities of an anthocyanin-rich extract from black rice against breast cancer cells in vitro and in vivo. Nutr. Cancer. 2010;62:1128–1136. doi: 10.1080/01635581.2010.494821. [DOI] [PubMed] [Google Scholar]
- 42.Awad A.B., Chan K.C., Downie A.C., Fink C.S. Peanuts as a source of β-sitosterol, a sterol with anticancer properties. Nutr. Cancer. 2000;36:238–241. doi: 10.1207/S15327914NC3602_14. [DOI] [PubMed] [Google Scholar]
- 43.Kowalczyk T., Sitarek P., Toma M., Picot L., Wielanek M., Skała E., Śliwiński T. An extract of transgenic Senna obtusifolia L. Hairy roots with overexpression of PgSS1 gene in combination with chemotherapeutic agent induces apoptosis in the leukemia cell line. Biomolecules. 2020;10:510. doi: 10.3390/biom10040510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zaini R., Clench M.R., Le Maitre C.L. Bioactive chemicals from carrot (Daucus carota) juice extracts for the treatment of leukemia. J. Med. Food. 2011;14:1303–1312. doi: 10.1089/jmf.2010.0284. [DOI] [PubMed] [Google Scholar]
- 45.Sitarek P., Kowalczyk T., Santangelo S., Białas A.J., Toma M., Wieczfinska J., Śliwiński T., Skała E. The Extract of Leonurus sibiricus Transgenic Roots with AtPAP1 Transcriptional Factor Induces Apoptosis via DNA Damage and Down Regulation of Selected Epigenetic Factors in Human Cancer Cells. Neurochem. Res. 2018;43:1363–1370. doi: 10.1007/s11064-018-2551-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alumkal J.J., Slottke R., Schwartzman J., Cherala G., Munar M., Graff J.N., Beer T.M., Ryan C.W., Koop D.R., Gibbs A., et al. A phase II study of sulforaphane-rich broccoli sprout extracts in men with recurrent prostate cancer. Investig. New Drugs. 2015;33:480–489. doi: 10.1007/s10637-014-0189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Güler D.A., Aydın A., Koyuncu M., Parmaksız İ., Tekin Ş. Anticancer Activity of Papaver somniferum. J. Turk. Chem. Soc. Sect. A Chem. 2016;3:349–366. doi: 10.18596/jotcsa.43273. [DOI] [Google Scholar]
- 48.Alsaraf K.M., Mohammad M.H., Al-Shammari A.M., Abbas I.S. Selective cytotoxic effect of Plantago lanceolata L. against breast cancer cells. J. Egypt. Natl. Cancer Inst. 2019;31:10. doi: 10.1186/s43046-019-0010-3. [DOI] [PubMed] [Google Scholar]
- 49.Lambertini L., Di Maida F., Tellini R., Bisegna C., Valastro F., Grosso A.A., Scelzi S., Del Giudice F., Ferro M., Pirola G.M., et al. Impact of the Treatment of Serenoa repens, Solanum lycopersicum, Lycopene and Bromelain in Combination with Alfuzosin for Benign Prostatic Hyperplasia. Results from a Match-Paired Comparison Analysis. Uro. 2021;1:228–237. doi: 10.3390/uro1040025. [DOI] [Google Scholar]
- 50.Ricci M.S., Zong W.-X. Chemotherapeutic Approaches for Targeting Cell Death Pathways. Oncologist. 2006;11:342–357. doi: 10.1634/theoncologist.11-4-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pan S.T., Li Z.L., He Z.X., Qiu J.X., Zhou S.F. Molecular mechanisms for tumour resistance to chemotherapy. Clin. Exp. Pharmacol. Physiol. 2016;43:723–737. doi: 10.1111/1440-1681.12581. [DOI] [PubMed] [Google Scholar]
- 52.Mansoori B., Mohammadi A., Davudian S., Shirjang S., Baradaran B. The different mechanisms of cancer drug resistance: A brief review. Adv. Pharm. Bull. 2017;7:339–348. doi: 10.15171/apb.2017.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Reuvers T.G.A., Kanaar R., Nonnekens J. DNA damage-inducing anticancer therapies: From global to precision damage. Cancers. 2020;12:2098. doi: 10.3390/cancers12082098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang H., Oo Khor T., Shu L., Su Z.-Y., Fuentes F., Lee J.-H., Tony Kong A.-N. Plants vs. Cancer: A Review on Natural Phytochemicals in Preventing and Treating Cancers and Their Druggability. Anticancer Agents Med. Chem. 2012;12:1281–1305. doi: 10.2174/187152012803833026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Demain A.L., Vaishnav P. Natural products for cancer chemotherapy. Microb. Biotechnol. 2011;4:687–699. doi: 10.1111/j.1751-7915.2010.00221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Michalkova R., Mirossay L., Gazdova M., Kello M., Mojzis J. Molecular mechanisms of antiproliferative effects of natural chalcones. Cancers. 2021;13:2730. doi: 10.3390/cancers13112730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kubczak M., Szustka A., Rogalińska M. Molecular Targets of Natural Compounds with Anti-Cancer Properties. Int. J. Mol. Sci. 2021;22:13659. doi: 10.3390/ijms222413659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Singh D., Kumar A., Bhatia A., Singh H., Kukreja S., Singh B., Arora S., Arora R. Pharmacotherapeutic Botanicals for Cancer Chemoprevention. Springer; Singapore: 2020. Role of Phytochemicals in Modulating Signaling Cascades in Cancer Cells. [Google Scholar]
- 59.Bhagwat A.S., Vakoc C.R. Targeting Transcription Factors in Cancer. Trends Cancer. 2015;1:53–65. doi: 10.1016/j.trecan.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li W.W., Li V.W., Hutnik M., Chiou A.S. Tumor angiogenesis as a target for dietary cancer prevention. J. Oncol. 2012;2012:879623. doi: 10.1155/2012/879623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.DeVita V.T., Chu E. A history of cancer chemotherapy. Cancer Res. 2008;68:8643–8653. doi: 10.1158/0008-5472.CAN-07-6611. [DOI] [PubMed] [Google Scholar]
- 62.Pan L., Chai H.B., Kinghorn A.D. Discovery of new anticancer agents from higher plants. Front. Biosci. Sch. 2012;4:142–156. doi: 10.2741/s257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cragg G.M., Pezzuto J.M. Natural Products as a Vital Source for the Discovery of Cancer Chemotherapeutic and Chemopreventive Agents. Med. Princ. Pract. 2016;25:41–59. doi: 10.1159/000443404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee C.-T., Huang Y.-W., Yang C.-H., Huang K.-S. Drug Delivery Systems and Combination Therapy by Using Vinca Alkaloids. Curr. Top. Med. Chem. 2015;15:1491–1500. doi: 10.2174/1568026615666150414120547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Denis J.N., Greene A.E., Guénard D., Guéritte-Voegelein F., Mangatal L., Potier P. A highly efficient, practical approach to natural taxol. J. Am. Chem. Soc. 1988;110:5917–5919. doi: 10.1021/ja00225a063. [DOI] [Google Scholar]
- 66.Volkmann R., Danishefsky S., Eggler J., Solomon D.M. A Total Synthesis of dl-Camptothecin. J. Am. Chem. Soc. 1971;93:5576–5577. doi: 10.1021/ja00750a045. [DOI] [Google Scholar]
- 67.Ardalani H., Avan A., Ghayour-Mobarhan M. Podophyllotoxin: A novel potential natural anticancer agent. Avicenna J. Phytomed. 2021;7:285–294. [PMC free article] [PubMed] [Google Scholar]
- 68.FDA Approved Drugs. [(accessed on 8 February 2022)]. Available online: https://www.centerwatch.com/directories/1067-fda-approved-drugs.
- 69.Madariaga-Mazón A., Hernández-Alvarado R.B., Noriega-Colima K.O., Osnaya-Hernández A., Martinez-Mayorga K. Toxicity of secondary metabolites. Phys. Sci. Rev. 2019;4:20180116. doi: 10.1515/psr-2018-0116. [DOI] [Google Scholar]
- 70.Seca A.M.L., Pinto D.C.G.A. Plant secondary metabolites as anticancer agents: Successes in clinical trials and therapeutic application. Int. J. Mol. Sci. 2018;19:263. doi: 10.3390/ijms19010263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Atanasov A.G., Waltenberger B., Pferschy-Wenzig E.M., Linder T., Wawrosch C., Uhrin P., Temml V., Wang L., Schwaiger S., Heiss E.H., et al. Discovery and resupply of pharmacologically active plant-derived natural products: A review. Biotechnol. Adv. 2015;33:1582–1614. doi: 10.1016/j.biotechadv.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Blanco E., Shen H., Ferrari M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat. Biotechnol. 2015;33:941–951. doi: 10.1038/nbt.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Patra J.K., Das G., Fraceto L.F., Campos E.V.R., del Rodriguez-Torres M.P., Acosta-Torres L.S., Diaz-Torres L.A., Grillo R., Swamy M.K., Sharma S., et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018;16:71. doi: 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jeevanandam J., Barhoum A., Chan Y.S., Dufresne A., Danquah M.K. Review on nanoparticles and nanostructured materials: History, sources, toxicity and regulations. Beilstein J. Nanotechnol. 2018;9:1050–1074. doi: 10.3762/bjnano.9.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Muhamad N., Plengsuriyakarn T., Na-Bangchang K. Application of active targeting nanoparticle delivery system for chemotherapeutic drugs and traditional/herbal medicines in cancer therapy: A systematic review. Int. J. Nanomed. 2018;13:3921–3935. doi: 10.2147/IJN.S165210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mohajerani A., Burnett L., Smith J.V., Kurmus H., Milas J., Arulrajah A., Horpibulsuk S., Kadir A.A. Nanoparticles in construction materials and other applications, and implications of nanoparticle use. Materials. 2019;12:3052. doi: 10.3390/ma12193052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gurley B.J. Pharmacokinetic herb-drug interactions (part 1): Origins, mechanisms, and the impact of botanical dietary supplements. Planta Med. 2012;78:1478–1489. doi: 10.1055/s-0031-1298273. [DOI] [PubMed] [Google Scholar]
- 78.Yingchoncharoen P., Kalinowski D.S., Richardson D.R. Lipid-based drug delivery systems in cancer therapy: What is available and what is yet to come. Pharmacol. Rev. 2016;68:701–787. doi: 10.1124/pr.115.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Iqbal J., Abbasi B.A., Mahmood T., Kanwal S., Ali B., Shah S.A., Khalil A.T. Plant-derived anticancer agents: A green anticancer approach. Asian Pac. J. Trop. Biomed. 2017;7:1129–1150. doi: 10.1016/j.apjtb.2017.10.016. [DOI] [Google Scholar]
- 80.Seely D., Oneschuk D. Interactions of natural health products with biomedical cancer treatments. Curr. Oncol. 2008;15((Suppl. S2)):s109.es81–s109.es86. [PMC free article] [PubMed] [Google Scholar]
- 81.Hussain A., Sharma C., Khan S., Shah K., Haque S. Aloe vera inhibits proliferation of human breast and cervical cancer cells and acts synergistically with cisplatin. Asian Pac. J. Cancer Prev. 2015;16:2939–2946. doi: 10.7314/APJCP.2015.16.7.2939. [DOI] [PubMed] [Google Scholar]
- 82.Hutchison J.E. The road to sustainable nanotechnology: Challenges, progress and opportunities. ACS Sustain. Chem. Eng. 2016;4:5907–5914. doi: 10.1021/acssuschemeng.6b02121. [DOI] [Google Scholar]
- 83.Fytianos G., Rahdar A., Kyzas G.Z. Nanomaterials in cosmetics: Recent updates. Nanomaterials. 2020;10:979. doi: 10.3390/nano10050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Manikanika, Kumar J., Jaswal S. Role of nanotechnology in the world of cosmetology: A review. Proc. Mater. Today. 2021;45:3302–3306. doi: 10.1016/j.matpr.2020.12.638. [DOI] [Google Scholar]
- 85.Riche M., Amelot A., Peyre M., Capelle L., Carpentier A., Mathon B. Complications after frame-based stereotactic brain biopsy: A systematic review. Neurosurg. Rev. 2021;44:301–307. doi: 10.1007/s10143-019-01234-w. [DOI] [PubMed] [Google Scholar]
- 86.Ding X.F., Luan Y., Lu S.M., Zhou G.C., Huang T.B., Zhu L.Y., Guo C.H. Risk factors for infection complications after transrectal ultrasound-guided transperineal prostate biopsy. World J. Urol. 2021;39:2463–2467. doi: 10.1007/s00345-020-03454-y. [DOI] [PubMed] [Google Scholar]
- 87.Zhang Y., Li M., Gao X., Chen Y., Liu T. Nanotechnology in cancer diagnosis: Progress, challenges and opportunities. J. Hematol. Oncol. 2019;12:137. doi: 10.1186/s13045-019-0833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mu W., Chu Q., Liu Y., Zhang N. A Review on Nano-Based Drug Delivery System for Cancer Chemoimmunotherapy. Nano-Micro Lett. 2020;12:142. doi: 10.1007/s40820-020-00482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Xu L., Lee J.R., Hao S., Ling X.B., Brooks J.D., Wang S.X., Gambhir S.S. Improved detection of prostate cancer using a magneto-nanosensor assay for serum circulating autoantibodies. PLoS ONE. 2019;14:e0221051. doi: 10.1371/journal.pone.0221051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhou Y., Chen S., Luo X., Chai Y., Yuan R. Ternary Electrochemiluminescence Nanostructure of Au Nanoclusters as a Highly Efficient Signal Label for Ultrasensitive Detection of Cancer Biomarkers. Anal. Chem. 2018;90:10024–10030. doi: 10.1021/acs.analchem.8b02642. [DOI] [PubMed] [Google Scholar]
- 91.Omer W.E., Abdelbar M.F., El-Kemary N.M., Fukata N., El-Kemary M.A. Cancer antigen 125 assessment using carbon quantum dots for optical biosensing for the early diagnosis of ovarian cancer. RSC Adv. 2021;11:31047–31057. doi: 10.1039/D1RA05121K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li J., Guan X., Fan Z., Ching L.M., Li Y., Wang X., Cao W.M., Liu D.X. Non-invasive biomarkers for early detection of breast cancer. Cancers. 2020;12:2767. doi: 10.3390/cancers12102767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kim D.H., Oh H.G., Park W.H., Jeon D.C., Lim K.M., Kim H.J., Jang B.K., Song K.S. Detection of alpha-fetoprotein in hepatocellular carcinoma patient plasma with graphene field-effect transistor. Sensors. 2018;18:4032. doi: 10.3390/s18114032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chang C.W., Chen P.H., Wang S.H., Hsu S.Y., Hsu W.T., Tsai C.C., Wadekar P.V., Puttaswamy S., Cheng K.H., Hsieh S., et al. Fast detection of tumor marker CA 19-9 using AlGaN/GaN high electron mobility transistors. Sens. Actuators B Chem. 2018;267:191–197. doi: 10.1016/j.snb.2018.04.008. [DOI] [Google Scholar]
- 95.Chaturvedi V.K., Singh A., Singh V.K., Singh M.P. Cancer Nanotechnology: A New Revolution for Cancer Diagnosis and Therapy. Curr. Drug Metab. 2018;20:416–429. doi: 10.2174/1389200219666180918111528. [DOI] [PubMed] [Google Scholar]
- 96.Lombardo D., Kiselev M.A., Caccamo M.T. Smart Nanoparticles for Drug Delivery Application: Development of Versatile Nanocarrier Platforms in Biotechnology and Nanomedicine. J. Nanomater. 2019;2019:3702518. doi: 10.1155/2019/3702518. [DOI] [Google Scholar]
- 97.Bukowski K., Kciuk M., Kontek R. Mechanisms of multidrug resistance in cancer chemotherapy. Int. J. Mol. Sci. 2020;21:3233. doi: 10.3390/ijms21093233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pearce A., Haas M., Viney R., Pearson S.A., Haywood P., Brown C., Ward R. Incidence and severity of self-reported chemotherapy side effects in routine care: A prospective cohort study. PLoS ONE. 2017;12:e0184360. doi: 10.1371/journal.pone.0184360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Aghebati-Maleki A., Dolati S., Ahmadi M., Baghbanzhadeh A., Asadi M., Fotouhi A., Yousefi M., Aghebati-Maleki L. Nanoparticles and cancer therapy: Perspectives for application of nanoparticles in the treatment of cancers. J. Cell. Physiol. 2020;235:1962–1972. doi: 10.1002/jcp.29126. [DOI] [PubMed] [Google Scholar]
- 100.Sharma A., Goyal A.K., Rath G. Recent advances in metal nanoparticles in cancer therapy. J. Drug Target. 2018;26:617–632. doi: 10.1080/1061186X.2017.1400553. [DOI] [PubMed] [Google Scholar]
- 101.Beik J., Khateri M., Khosravi Z., Kamrava S.K., Kooranifar S., Ghaznavi H., Shakeri-Zadeh A. Gold nanoparticles in combinatorial cancer therapy strategies. Coord. Chem. Rev. 2019;387:299–324. doi: 10.1016/j.ccr.2019.02.025. [DOI] [Google Scholar]
- 102.Dinparvar S., Bagirova M., Allahverdiyev A.M., Abamor E.S., Safarov T., Aydogdu M., Aktas D. A nanotechnology-based new approach in the treatment of breast cancer: Biosynthesized silver nanoparticles using Cuminum cyminum L. seed extract. J. Photochem. Photobiol. B Biol. 2020;208:111902. doi: 10.1016/j.jphotobiol.2020.111902. [DOI] [PubMed] [Google Scholar]
- 103.Eid A.M., Hawash M. Biological evaluation of Safrole oil and Safrole oil Nanoemulgel as antioxidant, antidiabetic, antibacterial, antifungal and anticancer. BMC Complement. Med. Ther. 2021;21:159. doi: 10.1186/s12906-021-03324-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Feng T., Wei Y., Lee R.J., Zhao L. Liposomal curcumin and its application in cancer. Int. J. Nanomed. 2017;12:6027–6044. doi: 10.2147/IJN.S132434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Santos A.C., Pereira I., Magalhães M., Pereira-Silva M., Caldas M., Ferreira L., Figueiras A., Ribeiro A.J., Veiga F. Targeting Cancer Via Resveratrol-Loaded Nanoparticles Administration: Focusing on In Vivo Evidence. AAPS J. 2019;21:57. doi: 10.1208/s12248-019-0325-y. [DOI] [PubMed] [Google Scholar]
- 106.Herdiana Y., Wathoni N., Shamsuddin S., Muchtaridi M. α-Mangostin Nanoparticles Cytotoxicity and Cell Death Modalities in Breast Cancer Cell Lines. Molecules. 2021;26:5119. doi: 10.3390/molecules26175119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jamkhande P.G., Ghule N.W., Bamer A.H., Kalaskar M.G. Metal nanoparticles synthesis: An overview on methods of preparation, advantages and disadvantages, and applications. J. Drug Deliv. Sci. Technol. 2019;53:101174. doi: 10.1016/j.jddst.2019.101174. [DOI] [Google Scholar]
- 108.Barkat M.A., Harshita, Beg S., Naim M.J., Pottoo F.H., Singh S.P., Ahmad F.J. Current Progress in Synthesis, Characterization and Applications of Silver Nanoparticles: Precepts and Prospects. Recent Pat. Antiinfect. Drug Discov. 2017;13:53–69. doi: 10.2174/1574891X12666171006102833. [DOI] [PubMed] [Google Scholar]
- 109.Pal G., Rai P., Pandey A. Green Synthesis, Characterization and Applications of Nanoparticles. Elsevier; Amsterdam, The Netherlands: 2019. Green synthesis of nanoparticles: A greener approach for a cleaner future; pp. 1–26. [DOI] [Google Scholar]
- 110.Salem S.S., Fouda A. Green Synthesis of Metallic Nanoparticles and Their Prospective Biotechnological Applications: An Overview. Biol. Trace Elem. Res. 2021;199:344–370. doi: 10.1007/s12011-020-02138-3. [DOI] [PubMed] [Google Scholar]
- 111.Das R.K., Pachapur V.L., Lonappan L., Naghdi M., Pulicharla R., Maiti S., Cledon M., Dalila L.M.A., Sarma S.J., Brar S.K. Biological synthesis of metallic nanoparticles: Plants, animals and microbial aspects. Nanotechnol. Environ. Eng. 2017;2:18. doi: 10.1007/s41204-017-0029-4. [DOI] [Google Scholar]
- 112.Garg D., Sarkar A., Chand P., Bansal P., Gola D., Sharma S., Khantwal S., Surabhi, Mehrotra R., Chauhan N., et al. Synthesis of silver nanoparticles utilizing various biological systems: Mechanisms and applications—A review. Prog. Biomater. 2020;9:81–95. doi: 10.1007/s40204-020-00135-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Al-Sheddi E.S., Farshori N.N., Al-Oqail M.M., Al-Massarani S.M., Saquib Q., Wahab R., Musarrat J., Al-Khedhairy A.A., Siddiqui M.A. Anticancer potential of green synthesized silver nanoparticles using extract of Nepeta deflersiana against human cervical cancer cells (HeLA) Bioinorg. Chem. Appl. 2018;2018:9390784. doi: 10.1155/2018/9390784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gomathi A.C., Xavier Rajarathinam S.R., Mohammed Sadiq A., Rajeshkumar S. Anticancer activity of silver nanoparticles synthesized using aqueous fruit shell extract of Tamarindus indica on MCF-7 human breast cancer cell line. J. Drug Deliv. Sci. Technol. 2020;55:101376. doi: 10.1016/j.jddst.2019.101376. [DOI] [Google Scholar]
- 115.Greenwell M., Rahman P.K.S.M. Medicinal Plants: Their Use in Anticancer Treatment. Int. J. Pharm. Sci. Res. 2015;6:4103–4112. doi: 10.13040/IJPSR.0975-8232.6(10).4103-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wei Q.Y., He K.M., Chen J.L., Xu Y.M., Lau A.T.Y. Phytofabrication of nanoparticles as novel drugs for anticancer applications. Molecules. 2019;24:4246. doi: 10.3390/molecules24234246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Vimala K., Kannan S. Phyto-drug conjugated nanomaterials enhance apoptotic activity in cancer. Adv. Protein Chem. Struct. Biol. 2021;125:275–305. doi: 10.1016/bs.apcsb.2020.12.003. [DOI] [PubMed] [Google Scholar]
- 118.Schirrmacher V. From chemotherapy to biological therapy: A review of novel concepts to reduce the side effects of systemic cancer treatment (Review) Int. J. Oncol. 2019;54:407–419. doi: 10.3892/ijo.2018.4661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lewandowska U., Gorlach S., Owczarek K., Hrabec E., Szewczyk K. Synergistic interactions between anticancer chemotherapeutics and phenolic compounds and anticancer synergy between polyphenols. Postepy Hig. Med. Dosw. 2014;68:528–540. doi: 10.5604/17322693.1102278. [DOI] [PubMed] [Google Scholar]
- 120.Garcia-Oliveira P., Otero P., Pereira A.G., Chamorro F., Carpena M., Echave J., Fraga-Corral M., Simal-Gandara J., Prieto M.A. Status and challenges of plant-anticancer compounds in cancer treatment. Pharmaceuticals. 2021;14:157. doi: 10.3390/ph14020157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Choudhari A.S., Mandave P.C., Deshpande M., Ranjekar P., Prakash O. Phytochemicals in cancer treatment: From preclinical studies to clinical practice. Front. Pharmacol. 2020;10:1614. doi: 10.3389/fphar.2019.01614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hawash M., Jaradat N., Bawwab N., Salem K., Arafat H., Hajyousef Y., Shtayeh T., Sobuh S. Design, synthesis, and biological evaluation of phenyl-isoxazole-carboxamide derivatives as anticancer agents. Heterocycl. Commun. 2020;27:133–141. doi: 10.1515/hc-2020-0134. [DOI] [Google Scholar]
- 123.Segen J. Concise Dictionary of Modern Medicine. University of Michigan; Ann Arbor, MI, USA: 2006. [Google Scholar]
- 124.Pezzani R., Salehi B., Vitalini S., Iriti M., Zuñiga F.A., Sharifi--Rad J., Martorell M., Martins N. Synergistic effects of plant derivatives and conventional chemotherapeutic agents: An update on the cancer perspective. Medicina. 2019;55:110. doi: 10.3390/medicina55040110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Imming P., Sinning C., Meyer A. Drugs, their targets and the nature and number of drug targets. Nat. Rev. Drug Discov. 2006;5:821–834. doi: 10.1038/nrd2132. [DOI] [PubMed] [Google Scholar]
- 126.Butterweck V., Jürgenliemk G., Nahrstedt A., Winterhoff H. Flavonoids from Hypericum perforatum show antidepressant activity in the forced swimming test. Planta Med. 2000;66:3–6. doi: 10.1055/s-2000-11119. [DOI] [PubMed] [Google Scholar]
- 127.Hemaiswarya S., Kruthiventi A.K., Doble M. Synergism between natural products and antibiotics against infectious diseases. Phytomedicine. 2008;15:639–652. doi: 10.1016/j.phymed.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 128.Rasool M., Iqbal J., Malik A., Ramzan H.S., Qureshi M.S., Asif M., Qazi M.H., Kamal M.A., Chaudhary A.G.A., Al-Qahtani M.H., et al. Hepatoprotective effects of Silybum marianum (silymarin) and Glycyrrhiza glabra (glycyrrhizin) in combination: A possible synergy. Evid. Based Complement. Altern. Med. 2014;2014:641597. doi: 10.1155/2014/641597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Gautam N., Mantha A.K., Mittal S. Essential oils and their constituents as anticancer agents: A mechanistic view. Biomed. Res. Int. 2014;2014:154106. doi: 10.1155/2014/154106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mileo A.M., Miccadei S. Polyphenols as Modulator of Oxidative Stress in Cancer Disease: New Therapeutic Strategies. Oxid. Med. Cell. Longev. 2016;2016:6475624. doi: 10.1155/2016/6475624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ramos-Esquivel A., Víquez-Jaikel A., Fernández C. Potential drug-drug and herb-drug interactions in patients with cancer: A prospective study of medication surveillance. J. Oncol. Pract. 2017;13:e613–e620. doi: 10.1200/JOP.2017.020859. [DOI] [PubMed] [Google Scholar]
- 132.Knapp S., Bohs L., Nee M., Spooner D.M. Solanaceae—A model for linking genomics with biodiversity. Comp. Funct. Genomics. 2004;5:285–291. doi: 10.1002/cfg.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Echeverría-Londoño S., Särkinen T., Fenton I.S., Purvis A., Knapp S. Dynamism and context-dependency in diversification of the megadiverse plant genus Solanum (Solanaceae) J. Syst. Evol. 2020;58:767–782. doi: 10.1111/jse.12638. [DOI] [Google Scholar]
- 134.Tetenyi P. A Chemotaxonomic Classification of the Solanaceae. Ann. Mo. Bot. Gard. 1987;74:600. doi: 10.2307/2399328. [DOI] [Google Scholar]
- 135.Knapp S., Nee M., Symon D.E., Lester R.N., Jessop J.P. In Solanaceae IV. Advances in Biology and Utilization. R. Bot. Gard. Kew. 2000;55:763. doi: 10.2307/4118799. [DOI] [Google Scholar]
- 136.Sucha L., Tomsik P. The Steroidal Glycoalkaloids from Solanaceae: Toxic Effect, Antitumour Activity and Mechanism of Action. Planta Med. 2016;82:379–387. doi: 10.1055/s-0042-100810. [DOI] [PubMed] [Google Scholar]
- 137.Ashfaq S., Ahmad M., Zafar M., Sultana S., Bahadur S., Ahmed S.N., Gul S., Nazish M. Pollen morphology of family solanaceae and its taxonomic significance. An. Acad. Bras. Cienc. 2020;92:e20181221. doi: 10.1590/0001-3765202020181221. [DOI] [PubMed] [Google Scholar]
- 138.Ghatak A., Chaturvedi P., Paul P., Agrawal G.K., Rakwal R., Kim S.T., Weckwerth W., Gupta R. Proteomics survey of Solanaceae family: Current status and challenges ahead. J. Proteomics. 2017;169:41–57. doi: 10.1016/j.jprot.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 139.Motti R. The Wild Solanums Genomes. Springer; Cham, Switzerland: 2021. The Solanaceae Family: Botanical Features and Diversity; pp. 1–9. [Google Scholar]
- 140.Shah V.V., Shah N.D., Patrekar P.V. Medicinal plants from solanaceae family. Res. J. Pharm. Technol. 2013;6:143–151. [Google Scholar]
- 141.Kaunda J.S., Zhang Y.-J. The Genus Solanum: An Ethnopharmacological, Phytochemical and Biological Properties Review. Nat. Prod. Bioprospect. 2019;9:77–137. doi: 10.1007/s13659-019-0201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kumara M. Solanum Alkaloids and their Pharmaceutical Roles: A Review. J. Anal. Pharm. Res. 2015;3:00075. doi: 10.15406/japlr.2016.03.00075. [DOI] [Google Scholar]
- 143.Mesas C., Fuel M., Martínez R., Prados J., Melguizo C., Porres J.M. In vitro evidence of the antitumor capacity of Solanaceae and Cucurbitaceae in colon cancer: A systematic review. Crit. Rev. Food Sci. Nutr. 2021;19:1–22. doi: 10.1080/10408398.2021.1900058. [DOI] [PubMed] [Google Scholar]
- 144.Food and Agriculture Data. [(accessed on 5 January 2022)]. Available online: https://www.fao.org/faostat/en/#home.
- 145.Gutiérrez-Grijalva E.P., López-Martínez L.X., Contreras-Angulo L.A., Elizalde-Romero C.A., Heredia J.B. Plant-Derived Bioactives: Chemistry and Mode of Action. Springer; Singapore: 2020. Plant alkaloids: Structures and bioactive properties. [Google Scholar]
- 146.Jerzykiewicz J. Alkaloids of Solanaceae (nightshade plants) Postepy Biochem. 2007;53:280–286. [PubMed] [Google Scholar]
- 147.Chowański S., Adamski Z., Marciniak P., Rosiński G., Büyükgüzel E., Büyükgüzel K., Falabella P., Scrano L., Ventrella E., Lelario F., et al. A review of bioinsecticidal activity of Solanaceae alkaloids. Toxins. 2016;8:60. doi: 10.3390/toxins8030060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kohnen-Johannsen K.L., Kayser O. Tropane alkaloids: Chemistry, pharmacology, biosynthesis and production. Molecules. 2019;24:796. doi: 10.3390/molecules24040796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Huang J.P., Wang Y.J., Tian T., Wang L., Yan Y., Huang S.X. Tropane alkaloid biosynthesis: A centennial review. Nat. Prod. Rep. 2021;38:1634–1658. doi: 10.1039/D0NP00076K. [DOI] [PubMed] [Google Scholar]
- 150.Roddick J.G. Steroidal glycoalkaloids: Nature and consequences of bioactivity. Adv. Exp. Med. Biol. 1996;404:277–297. doi: 10.1007/978-1-4899-1367-8_25. [DOI] [PubMed] [Google Scholar]
- 151.Friedman M. Potato glycoalkaloids and metabolites: Roles in the plant and in the diet. J. Agric. Food Chem. 2006;54:8655–8681. doi: 10.1021/jf061471t. [DOI] [PubMed] [Google Scholar]
- 152.Solowey E., Lichtenstein M., Sallon S., Paavilainen H., Solowey E., Lorberboum-Galski H. Evaluating medicinal plants for anticancer activity. Sci. World J. 2014;2014:721402. doi: 10.1155/2014/721402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Amid A., Chik W.D.W., Jamal P., Hashim Y.Z.H.Y. Microarray and quantitative PCR analysis of gene expression profiles in response to treatment with tomato leaf extract in MCF-7 breast cancer cells. Asian Pac. J. Cancer Prev. 2012;13:6319–6325. doi: 10.7314/APJCP.2012.13.12.6319. [DOI] [PubMed] [Google Scholar]
- 154.Lin Y.T., Huang A.C., Kuo C.L., Yang J.S., Lan Y.H., Yu C.C., Huang W.W., Chung J.G. Induction of cell cycle arrest and apoptosis in human osteosarcoma U-2 OS cells by Solanum lyratum extracts. Nutr. Cancer. 2013;65:469–479. doi: 10.1080/01635581.2013.757627. [DOI] [PubMed] [Google Scholar]
- 155.Akbar N., Thakur V.S., Yunus M., Mahdi A.A., Gupta S. Selective cell cycle arrest and induction of apoptosis in human prostate cancer cells by a polyphenol-rich extract of Solanum nigrum. Int. J. Mol. Med. 2012;29:277–284. doi: 10.3892/ijmm.2011.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Nieto-Sampedro M., Valle-Argos B., Gómez-Nicola D., Fernández-Mayoralas A., Nieto-Díaz M. Inhibitors of glioma growth that reveal the tumour to the immune system. Clin. Med. Insights Oncol. 2011;5:265–314. doi: 10.4137/CMO.S7685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wadhwa R., Singh R., Gao R., Shah N., Widodo N., Nakamoto T., Ishida Y., Terao K., Kaul S.C. Water Extract of Ashwagandha Leaves Has Anticancer Activity: Identification of an Active Component and Its Mechanism of Action. PLoS ONE. 2013;8:e77189. doi: 10.1371/annotation/b7059f27-5970-4734-8601-9913adcce984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Haq I.U., Mirza B., Kondratyuk T.P., Park E.J., Burns B.E., Marler L.E., Pezzuto J.M. Preliminary evaluation for cancer chemopreventive and cytotoxic potential of naturally growing ethnobotanically selected plants of Pakistan. Pharm. Biol. 2013;51:316–328. doi: 10.3109/13880209.2012.728612. [DOI] [PubMed] [Google Scholar]
- 159.Kim H.A., Kim M.S., Kim S.H., Kim Y.K. Pepper seed extract suppresses invasion and migration of human breast cancer cells. Nutr. Cancer. 2014;66:159–165. doi: 10.1080/01635581.2014.853814. [DOI] [PubMed] [Google Scholar]
- 160.Hassan L.E.A., Khadeer Ahamed M.B., Abdul Majid A.S., Baharetha H.M., Muslim N.S., Nassar Z.D., Abdul Majid A.M.S. Correlation of antiangiogenic, antioxidant and cytotoxic activities of some Sudanese medicinal plants with phenolic and flavonoid contents. BMC Complement. Altern. Med. 2014;14:406. doi: 10.1186/1472-6882-14-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Almeida A.A., Lima G.D.A., Simão M.V.R.C., Moreira G.A., Siqueira R.P., Zanatta A.C., Vilegas W., Machado-Neves M., Bressan G.C., Leite J.P.V. Screening of plants from the Brazilian Atlantic Forest led to the identification of Athenaea velutina (Solanaceae) as a novel source of antimetastatic agents. Int. J. Exp. Pathol. 2020;101:106–121. doi: 10.1111/iep.12351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Chilczuk B., Marciniak B., Stochmal A., Pecio Ł., Kontek R., Jackowska I., Materska M. Anticancer Potential and Capsianosides Identification in Lipophilic Fraction of Sweet Pepper (Capsicum annuum L.) Molecules. 2020;25:3097. doi: 10.3390/molecules25133097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kim H.G., Bae J.H., Jastrzebski Z., Cherkas A., Heo B.G., Gorinstein S., Ku Y.G. Binding, Antioxidant and Anti-proliferative Properties of Bioactive Compounds of Sweet Paprika (Capsicum annuum L.) Plant Foods Hum. Nutr. 2016;71:129–136. doi: 10.1007/s11130-016-0550-9. [DOI] [PubMed] [Google Scholar]
- 164.Mutalib M.A., Ali F., Othman F., Ramasamy R., Rahmat A. Phenolics profile and anti-proliferative activity of Cyphomandra Betacea fruit in breast and liver cancer cells. Springerplus. 2016;5:2105. doi: 10.1186/s40064-016-3777-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Chamani E., Ebrahimi R., Khorsandi K., Meshkini A., Zarban A., Sharifzadeh G. In vitro cytotoxicity of polyphenols from Datura innoxia aqueous leaf-extract on human leukemia K562 cells: DNA and nuclear proteins as targets. Drug Chem. Toxicol. 2020;43:138–148. doi: 10.1080/01480545.2019.1629588. [DOI] [PubMed] [Google Scholar]
- 166.Nasir B., Baig M.W., Majid M., Ali S.M., Khan M.Z.I., Kazmi S.T.B., Haq I.U. Preclinical anticancer studies on the ethyl acetate leaf extracts of Datura stramonium and Datura inoxia. BMC Complement. Med. Ther. 2020;20:188. doi: 10.1186/s12906-020-02975-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Mirzaei H.H., Firuzi O., Baldwin I.T., Jassbi A.R. Cytotoxic activities of different Iranian Solanaceae and Lamiaceae plants and bioassay-guided study of an active extract from Salvia lachnocalyx. Nat. Prod. Commun. 2017;12:1563–1566. doi: 10.1177/1934578X1701201009. [DOI] [Google Scholar]
- 168.Vishnu V.R., Renjith R.S., Mukherjee A., Anil S.R., Sreekumar J., Jyothi A.N. Comparative Study on the Chemical Structure and In Vitro Antiproliferative Activity of Anthocyanins in Purple Root Tubers and Leaves of Sweet Potato (Ipomoea batatas) J. Agric. Food Chem. 2019;67:2467–2475. doi: 10.1021/acs.jafc.8b05473. [DOI] [PubMed] [Google Scholar]
- 169.Wawruszak A., Czerwonka A., Okła K., Rzeski W. Anticancer effect of ethanol Lycium barbarum (Goji berry) extract on human breast cancer T47D cell line. Nat. Prod. Res. 2016;30:1993–1996. doi: 10.1080/14786419.2015.1101691. [DOI] [PubMed] [Google Scholar]
- 170.Ceccarini M.R., Vannini S., Cataldi S., Moretti M., Villarini M., Fioretti B., Albi E., Beccari T., Codini M. In Vitro Protective Effects of Lycium barbarum Berries Cultivated in Umbria (Italy) on Human Hepatocellular Carcinoma Cells. Biomed. Res. Int. 2016;2016:7529521. doi: 10.1155/2016/7529521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Cenariu D., Fischer-Fodor E., Țigu A.B., Bunea A., Virág P., Perde-Schrepler M., Toma V.A., Mocan A., Berindan-Neagoe I., Pintea A., et al. Zeaxanthin-Rich Extract from Superfood Lycium barbarum Selectively Modulates the Cellular Adhesion and MAPK Signaling in Melanoma versus Normal Skin Cells In Vitro. Molecules. 2021;26:333. doi: 10.3390/molecules26020333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Georgiev K.D., Slavov I.J., Iliev I.A. Antioxidant Activity and Antiproliferative Effects of Lycium barbarum’s (Goji berry) Fractions on Breast Cancer Cell Lines. Folia Med. 2019;61:104–112. doi: 10.2478/folmed-2018-0053. [DOI] [PubMed] [Google Scholar]
- 173.Juan-García A., Montesano D., Mañes J., Juan C. Cytoprotective effects of carotenoids-rich extract from Lycium barbarum L. on the beauvericin-induced cytotoxicity on Caco-2 cells. Food Chem. Toxicol. 2019;133:110798. doi: 10.1016/j.fct.2019.110798. [DOI] [PubMed] [Google Scholar]
- 174.Xiong L., Deng N., Zheng B., Lic T., Liu R.H. Goji berry (Lycium spp.) extracts exhibit antiproliferative activity via modulating cell cycle arrest, cell apoptosis, and the p53 signaling pathway. Food Funct. 2021;12:6513–6525. doi: 10.1039/D1FO01105G. [DOI] [PubMed] [Google Scholar]
- 175.Kwaśnik P., Lemieszek M.K., Rzeski W. Impact of phytochemicals and plant extracts on viability and proliferation of NK cell line NK-92—A closer look at immunomodulatory properties of goji berries extract in human colon cancer cells. Ann. Agric. Environ. Med. 2021;28:291–299. doi: 10.26444/aaem/133801. [DOI] [PubMed] [Google Scholar]
- 176.Ghali W., Vaudry D., Jouenne T., Marzouki M.N. Lycium europaeum fruit extract: Antiproliferative activity on A549 human lung carcinoma cells and PC12 rat adrenal medulla cancer cells and assessment of its cytotoxicity on cerebellum granule cells. Nutr. Cancer. 2015;67:637–646. doi: 10.1080/01635581.2015.1017054. [DOI] [PubMed] [Google Scholar]
- 177.Figueiredo-González M., Valentão P., Pereira D.M., Andrade P.B. Further insights on tomato plant: Cytotoxic and antioxidant activity of leaf extracts in human gastric cells. Food Chem. Toxicol. 2017;109:386–392. doi: 10.1016/j.fct.2017.09.018. [DOI] [PubMed] [Google Scholar]
- 178.Musso F., Pronsato L., Milanesi L., Vasconsuelo A., Faraoni M.B. Pharmacognosy non-polar extracts of Nicotiana glauca (Solanaceae) induce apoptosis in human rhabdomyosarcoma cells. Rodriguesia. 2020;7:8363690. doi: 10.1590/2175-7860202071047. [DOI] [Google Scholar]
- 179.Tabana Y.M., Dahham S.S., Ahmed Hassan L.E. In Vitro Anti-Metastatic and Antioxidant Activity of Nicotiana glauca Fraction Against Breast Cancer Cells. Adv. Biol. Res. 2015;9:95–102. doi: 10.5829/idosi.abr.2015.9.2.9521. [DOI] [Google Scholar]
- 180.Laczkó-Zöld E., Forgó P., Zupkó I., Sigrid E., Hohmann J. Isolation and quantitative analysis of physalin d in the fruit and calyx of Physalis alkekengi L. Acta Biol. Hung. 2017;68:300–309. doi: 10.1556/018.68.2017.3.7. [DOI] [PubMed] [Google Scholar]
- 181.Hidayat T., Priyandoko D., Perdana F.S., Insan A.M. Hernawati Cytotoxicity effects of leaf extracts of Ciplukan (Physalis angulata; Solanaceae) on human blood and ovary cancer cell lines. J. Phys. Conf. Ser. 2019;1280:022009. doi: 10.1088/1742-6596/1280/2/022009. [DOI] [Google Scholar]
- 182.Mier-Giraldo H., Díaz-Barrera L.E., Delgado-Murcia L.G., Valero-Valdivieso M.F., Cáez-Ramírez G. Cytotoxic and Immunomodulatory Potential Activity of Physalis peruviana Fruit Extracts on Cervical Cancer (HeLa) and Fibroblast (L929) Cells. J. Evid. Based Complement. Altern. Med. 2017;22:777–787. doi: 10.1177/2156587217718751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Burger T., Mokoka T., Fouché G., Steenkamp P., Steenkamp V., Cordier W. Solamargine, a bioactive steroidal alkaloid isolated from Solanum aculeastrum induces non-selective cytotoxicity and P-glycoprotein inhibition. BMC Complement Altern. Med. 2018;18:137. doi: 10.1186/s12906-018-2208-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Petreanu M., Guimarães Á.A.A., Broering M.F., Ferreira E.K., Machado I.D., Gois A.L.T., de Carvalho J.E., Monache F.D., Niero R., Santin J.R. Antiproliferative and toxicological properties of methanolic extract obtained from Solanum capsicoides All. seeds and carpesterol. Naunyn. Schmiedebergs. Arch. Pharmacol. 2016;389:1123–1131. doi: 10.1007/s00210-016-1275-x. [DOI] [PubMed] [Google Scholar]
- 185.Cruceriu D., Diaconeasa Z., Socaci S., Socaciu C., Balacescu O., Rakosy-Tican E. Extracts of the Wild Potato Species Solanum chacoense on Breast Cancer Cells: Biochemical Characterization, In Vitro Selective Cytotoxicity and Molecular Effects. Nutr. Cancer. 2021;73:630–641. doi: 10.1080/01635581.2020.1761407. [DOI] [PubMed] [Google Scholar]
- 186.Yu S., Sheu H.M., Lee C.H. Solanum incanum extract (SR-T100) induces melanoma cell apoptosis and inhibits established lung metastasis. Oncotarget. 2017;8:103509–103517. doi: 10.18632/oncotarget.21508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Al-Emam A., Al-Shraim M., Eid R., Alfaifi M., Al-Shehri M., Moustafa M.F., Radad K. Ultrastructural changes induced by Solanum incanum aqueous extract on HCT 116 colon cancer cells. Ultrastruct. Pathol. 2018;42:255–261. doi: 10.1080/01913123.2018.1447623. [DOI] [PubMed] [Google Scholar]
- 188.Fadl Almoulah N., Voynikov Y., Gevrenova R., Schohn H., Tzanova T., Yagi S., Thomas J., Mignard B., Ahmed A.A.A., El Siddig M.A., et al. Antibacterial, antiproliferative and antioxidant activity of leaf extracts of selected Solanaceae species. S. Afr. J. Bot. 2017;112:368–374. doi: 10.1016/j.sajb.2017.06.016. [DOI] [Google Scholar]
- 189.Raiola A., Del Giudice R., Monti D.M., Tenore G.C., Barone A., Rigano M.M. Bioactive compound content and cytotoxic effect on human cancer cells of fresh and processed yellow tomatoes. Molecules. 2016;21:33. doi: 10.3390/molecules21010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Ramos-Bueno R.P., Romero-González R., González-Fernández M.J., Guil-Guerrero J.L. Phytochemical composition and in vitro anti-tumour activities of selected tomato varieties. J. Sci. Food Agric. 2017;97:488–496. doi: 10.1002/jsfa.7750. [DOI] [PubMed] [Google Scholar]
- 191.Alper M., Güneş H. Cytotoxic Potential of Solanum lycopersicum Leaves Extract on Different Human Cell Lines. BSEU J. Sci. 2020;7:544–552. doi: 10.35193/bseufbd.682245. [DOI] [Google Scholar]
- 192.Chiu C.H., Chou Y.C., Lin J.P., Kuo C.L., Lu H.F., Huang Y.P., Yu C.C., Lin M.L., Chung J.G. Chloroform Extract of Solanum lyratum Induced G0/G1 Arrest via p21/p16 and Induced Apoptosis via Reactive Oxygen Species, Caspases and Mitochondrial Pathways in Human Oral Cancer Cell Lines. Am. J. Chin. Med. 2015;43:1453–1469. doi: 10.1142/S0192415X15500822. [DOI] [PubMed] [Google Scholar]
- 193.Ling B., Michel D., Sakharkar M.K., Yang J. Evaluating the cytotoxic effects of the water extracts of four anticancer herbs against human malignant melanoma cells. Drug Des. Dev. Ther. 2016;10:3563–3572. doi: 10.2147/DDDT.S119214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Lai Y.J., Tai C.J., Wang C.W., Choong C.Y., Lee B.H., Shi Y.C., Tai C.J. Anti-cancer activity of Solanum nigrum (AESN) through suppression of mitochondrial function and epithelial-mesenchymal transition (EMT) in breast cancer cells. Molecules. 2016;21:553. doi: 10.3390/molecules21050553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Uen W.C., Lee B.H., Shi Y.C., Wu S.C., Tai C.J., Tai C.J. Inhibition of aqueous extracts of Solanum nigrum (AESN) on oral cancer through regulation of mitochondrial fission. J. Tradit. Complement. Med. 2018;8:220–225. doi: 10.1016/j.jtcme.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Churiyah C., Ningsih S., Firdayani F. The Cytotoxic, Apoptotic Induction, and Cell Cycle Arrest Activities of Solanum nigrum L. Ethanolic Extract on MCF-7 Human Breast Cancer Cell. Asian Pac. J. Cancer Prev. 2020;21:3735–3741. doi: 10.31557/APJCP.2020.21.12.3735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Yang M.Y., Hung C.H., Chang C.H., Tseng T.H., Wang C.J. Solanum nigrum Suppress Angiogenesis-Mediated Tumor Growth Through Inhibition of the AKT/mTOR Pathway. Am. J. Chin. Med. 2016;44:1273–1288. doi: 10.1142/S0192415X16500713. [DOI] [PubMed] [Google Scholar]
- 198.Ferraz A.P.C.R., Sussulini A., Garcia J.L., Costa M.R., Francisqueti-Ferron F.V., Ferron A.J.T., Silva C.C.V.D.A., Corrente J.E., Manfio V.M., Namba V., et al. Hydroethanolic Extract of Solanum paniculatum L. Fruits Modulates ROS and Cytokine in Human Cell Lines. Oxid. Med. Cell. Longev. 2020;2020:7240216. doi: 10.1155/2020/7240216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Alajmi M.F., Alam P., Rehman M.T., Husain F.M., Khan A.A., Siddiqui N.A., Hussain A., Kalam M.A., Parvez M.K. Interspecies Anticancer and Antimicrobial Activities of Genus Solanum and Estimation of Rutin by Validated UPLC-PDA Method. Evid. Based Complement. Alternat. Med. 2018;2018:6040815. doi: 10.1155/2018/6040815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Dos Santos Montagner G.F.F., Barbisan F., Ledur P.C., Bolignon A., De Rosso Motta J., Ribeiro E.E., De Souza Praia R., Azzolin V.F., Cadoná F.C., Machado A.K., et al. In Vitro Biological Properties of Solanum sessiliflorum (Dunal), an Amazonian Fruit. J. Med. Food. 2020;23:978–987. doi: 10.1089/jmf.2019.0193. [DOI] [PubMed] [Google Scholar]
- 201.Zuber T., Holm D., Byrne P., Ducreux L., Taylor M., Kaiser M., Stushnoff C. Optimization of in vitro inhibition of HT-29 colon cancer cell cultures by Solanum tuberosum L. extracts. Food Funct. 2015;6:72–83. doi: 10.1039/C4FO00649F. [DOI] [PubMed] [Google Scholar]
- 202.De Masi L., Bontempo P., Rigano D., Stiuso P., Carafa V., Nebbioso A., Piacente S., Montoro P., Aversano R., D’Amelia V., et al. Comparative Phytochemical Characterization, Genetic Profile, and Antiproliferative Activity of Polyphenol-Rich Extracts from Pigmented Tubers of Different Solanum tuberosum Varieties. Molecules. 2020;25:233. doi: 10.3390/molecules25010233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Sampaio S.L., Petropoulos S.A., Dias M.I., Pereira C., Calhelha R.C., Fernandes Â., Leme C.M.M., Alexopoulos A., Santos-Buelga C., Ferreira I.C.F.R., et al. Phenolic composition and cell-based biological activities of ten coloured potato peels (Solanum tuberosum L.) Food Chem. 2021;363:130360. doi: 10.1016/j.foodchem.2021.130360. [DOI] [PubMed] [Google Scholar]
- 204.Maqsood M., Qureshi R., Ikram M., Ahmad M.S., Jabeen B., Asi M.R., Khan J.A., Ali S., Lilge L. In vitro anticancer activities of Withania coagulans against HeLa, MCF-7, RD, RG2, and INS-1 cancer cells and phytochemical analysis. Integr. Med. Res. 2018;7:184–191. doi: 10.1016/j.imr.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Ahmad R., Fatima A., Srivastava A.N., Khan M.A. Evaluation of apoptotic activity of Withania coagulans methanolic extract against human breast cancer and Vero cell lines. J. Ayurveda Integr. Med. 2017;8:177–183. doi: 10.1016/j.jaim.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Halder B., Singh S., Thakur S.S. Withania somnifera root extract has potent cytotoxic effect against human malignant melanoma cells. PLoS ONE. 2015;10:e0137498. doi: 10.1371/journal.pone.0137498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Ahmed W., Mofed D., Zekri A.R., El-Sayed N., Rahouma M., Sabet S. Antioxidant activity and apoptotic induction as mechanisms of action of Withania somnifera (Ashwagandha) against a hepatocellular carcinoma cell line. J. Int. Med. Res. 2018;46:1358–1369. doi: 10.1177/0300060517752022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Nile S.H., Nile A., Gansukh E., Baskar V., Kai G. Subcritical water extraction of withanosides and withanolides from ashwagandha (Withania somnifera L) and their biological activities. Food Chem. Toxicol. 2019;132:110659. doi: 10.1016/j.fct.2019.110659. [DOI] [PubMed] [Google Scholar]
- 209.Sajida, Prabhu A. Anti-angiogenic, apoptotic and matrix metalloproteinase inhibitory activity of Withania somnifera (ashwagandha) on lung adenocarcinoma cells. Phytomedicine. 2021;90:153639. doi: 10.1016/j.phymed.2021.153639. [DOI] [PubMed] [Google Scholar]
- 210.Turrini E., Calcabrini C., Sestili P., Catanzaro E., de Gianni E., Diaz A.R., Hrelia P., Tacchini M., Guerrini A., Canonico B., et al. Withania somnifera Induces Cytotoxic and Cytostatic Effects on Human T Leukemia Cells. Toxins. 2016;8:147. doi: 10.3390/toxins8050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Kataria H., Kumar S., Chaudhary H., Kaur G. Withania somnifera Suppresses Tumor Growth of Intracranial Allograft of Glioma Cells. Mol. Neurobiol. 2016;53:4143–4158. doi: 10.1007/s12035-015-9320-1. [DOI] [PubMed] [Google Scholar]
- 212.Srivastava A.N., Ahmad R., Khan M.A. Evaluation and Comparison of the In Vitro Cytotoxic Activity of Withania somnifera Methanolic and Ethanolic Extracts against MDA-MB-231 and Vero Cell Lines. Sci. Pharm. 2015;84:41–59. doi: 10.3797/scipharm.1507-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Li G.S., Yao F., Zhang L., Yue X.D., Dai S.J. New sesquiterpenoid derivatives from Solanum lyratum and their cytotoxicities. J. Asian Nat. Prod. Res. 2014;16:129–134. doi: 10.1080/10286020.2013.839664. [DOI] [PubMed] [Google Scholar]
- 214.Koduru S., Grierson D.S., Van De Venter M., Afolayan A.J. Anticancer activity of steroid alkaloids isolated from Solanum aculeastrum. Pharm. Biol. 2007;45:613–618. doi: 10.1080/13880200701538690. [DOI] [Google Scholar]
- 215.Shieh J.M., Cheng T.H., Shi M.D., Wu P.F., Chen Y., Ko S.C., Shih Y.W. α-Tomatine Suppresses Invasion and Migration of Human Non-Small Cell Lung Cancer NCI-H460 Cells Through Inactivating FAK/PI3K/Akt Signaling Pathway and Reducing Binding Activity of NF-κB. Cell Biochem. Biophys. 2011;60:297–310. doi: 10.1007/s12013-011-9152-1. [DOI] [PubMed] [Google Scholar]
- 216.Zha X.M., Zhang F.R., Shan J.Q., Chen Y.K., Zhang Y.H., Liu J., Sun H. Bin Synthesis and in vitro antitumor activities of novel soladulcidine derivatives. J. China Pharm. Univ. 2010;41:493–498. [Google Scholar]
- 217.Yang Z., Garcia A., Xu S., Powell D.R., Vertino P.M., Singh S., Marcus A.I. Withania somnifera Root Extract Inhibits Mammary Cancer Metastasis and Epithelial to Mesenchymal Transition. PLoS ONE. 2013;8:e75069. doi: 10.1371/journal.pone.0075069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Zhang H., Samadi A.K., Cohen M.S., Timmermann B.N. Antiproliferative withanolides from the solanaceae: A structure-activity study. Pure Appl. Chem. 2012;84:1353–1367. doi: 10.1351/PAC-CON-11-10-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Zhang H., Bazzill J., Gallagher R.J., Subramanian C., Grogan P.T., Day V.W., Kindscher K., Cohen M.S., Timmermann B.N. Antiproliferative withanolides from Datura wrightii. J. Nat. Prod. 2013;76:445–449. doi: 10.1021/np300766p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Çakir Ö., Pekmez M., Çepni E., Candar B., Fidan K. Evaluation of biological activities of Physalis peruviana ethanol extracts and expression of Bcl-2 genes in HeLa cells. Food Sci. Technol. 2014;34:422–430. doi: 10.1590/fst.2014.0060. [DOI] [Google Scholar]
- 221.Rocha D.D., Balgi A., Maia A.I.V., Pessoa O.D., Silveira E.R., Costa-Lotufo L.V., Roberge M., Pessoa C. Cell cycle arrest through inhibition of tubulin polymerization by withaphysalin F, a bioactive compound isolated from Acnistus arborescens. Investig. New Drugs. 2012;30:959–966. doi: 10.1007/s10637-011-9649-x. [DOI] [PubMed] [Google Scholar]
- 222.Ding X., Zhu F., Yang Y., Li M. Purification, antitumor activity in vitro of steroidal glycoalkaloids from black nightshade (Solanum nigrum L.) Food Chem. 2013;141:1181–1186. doi: 10.1016/j.foodchem.2013.03.062. [DOI] [PubMed] [Google Scholar]
- 223.Takeshima M., Ono M., Higuchi T., Chen C., Hara T., Nakano S. Anti-proliferative and apoptosis-inducing activity of lycopene against three subtypes of human breast cancer cell lines. Cancer Sci. 2014;105:252–257. doi: 10.1111/cas.12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Ooi K.L., Tengku Muhammad T.S., Sulaiman S.F. Physalin F from Physalis minima L. triggers apoptosis-based cytotoxic mechanism in T-47D cells through the activation caspase-3- and c-myc-dependent pathways. J. Ethnopharmacol. 2013;150:382–388. doi: 10.1016/j.jep.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 225.Chen Y.Q., Tang Q., Wu J.J., Zheng F., Yang L.J., Hann S.S. Inactivation of PI3-K/Akt and reduction of SP1 and p65 expression increase the effect of solamargine on suppressing EP4 expression in human lung cancer cells. J. Exp. Clin. Cancer Res. 2015;34:154. doi: 10.1186/s13046-015-0272-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Koduru S., Kumar R., Srinivasan S., Evers M.B., Damodaran C. Notch-1 inhibition by withaferin-A: A therapeutic target against colon carcinogenesis. Mol. Cancer Ther. 2010;9:202–210. doi: 10.1158/1535-7163.MCT-09-0771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Arslan A.K.K., Yerer M.B. α-Chaconine and α-Solanine inhibit RL95-2 endometrium cancer cell proliferation by reducing expression of Akt (Ser473) and ERα (Ser167) Nutrients. 2018;10:672. doi: 10.3390/nu10060672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Yi Y.J., Jia X.H., Wang J.Y., Chen J.R., Wang H., Li Y.J. Solanine induced apoptosis and increased chemosensitivity to adriamycin in t-cell acute lymphoblastic leukemia cells. Oncol. Lett. 2018;15:7383–7388. doi: 10.3892/ol.2018.8229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Kumar S., Gupta A., Saini R.V., Kumar A., Dhar K.L., Mahindroo N. Immunomodulation-mediated anticancer activity of a novel compound from Brugmansia suaveolens leaves. Bioorg. Med. Chem. 2020;28:115552. doi: 10.1016/j.bmc.2020.115552. [DOI] [PubMed] [Google Scholar]
- 230.Mokhtar M., Soukup J., Donato P., Cacciola F., Dugo P., Riazi A., Jandera P., Mondello L. Determination of the polyphenolic content of a Capsicum annuum L. extract by liquid chromatography coupled to photodiode array and mass spectrometry detection and evaluation of its biological activity. J. Sep. Sci. 2015;38:171–178. doi: 10.1002/jssc.201400993. [DOI] [PubMed] [Google Scholar]
- 231.Ayariga J.A., Abugri D.A., Griffin G.D. Capsaicin and dihydrocapsaicin extracted from Capsicum chinenses de- crease cell viability of neuroblastoma SH-SY5Y cells in vitro. Preprints. 2021:2021100438. doi: 10.20944/preprints202110.0438.v1. [DOI] [Google Scholar]
- 232.Maldonado E., Ramírez-Apan T., Martínez M. Cytotoxic withanolides from Datura innoxia. Z. Naturforsch. C J. Biosci. 2020;76:251–255. doi: 10.1515/znc-2020-0265. [DOI] [PubMed] [Google Scholar]
- 233.Gajendran B., Durai P., Varier K.M., Chinnasamy A. A novel phytosterol isolated from Datura inoxia, RinoxiaB is a potential cure colon cancer agent by targeting BAX/Bcl2 pathway. Bioorg. Med. Chem. 2019;28:115242. doi: 10.1016/j.bmc.2019.115242. [DOI] [PubMed] [Google Scholar]
- 234.Liu Y., Jiang H.B., Liu Y., Algradi A.M., Naseem A., Zhou Y.Y., She X., Li-Li , Yang B.Y., Kuang H.X. New indole alkaloids from the seeds of Datura metel L. Fitoterapia. 2020;146:104726. doi: 10.1016/j.fitote.2020.104726. [DOI] [PubMed] [Google Scholar]
- 235.Mai N.T., Cuc N.T., Anh H.L.T., Nhiem N.X., Tai B.H., Van Minh C., Quang T.H., Kim K.W., Kim Y.-C., Oh H., et al. Steroidal saponins from Datura metel. Steroids. 2017;121:1–9. doi: 10.1016/j.steroids.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 236.Li Z.L., Mi J., Lu L., Luo Q., Liu X., Yan Y.M., Jin B., Cao Y.L., Zeng X.X., Ran L.W. The main anthocyanin monomer of Lycium ruthenicum Murray induces apoptosis through the ROS/PTEN/PI3K/Akt/caspase 3 signaling pathway in prostate cancer DU-145 cells. Food Funct. 2021;12:1818–1828. doi: 10.1039/D0FO02382E. [DOI] [PubMed] [Google Scholar]
- 237.Ur Rehman N., Halim S.A., Khan M., Hussain H., Yar Khan H., Khan A., Abbas G., Rafiq K., Al-Harrasi A. Antiproliferative and Carbonic Anhydrase II Inhibitory Potential of Chemical Constituents from Lycium shawii and Aloe vera: Evidence from In Silico Target Fishing and In Vitro Testing. Pharmaceuticals. 2020;13:94. doi: 10.3390/ph13050094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Kang N., Jian J.F., Cao S.J., Zhang Q., Mao Y.W., Huang Y.Y., Peng Y.F., Qiu F., Gao X.M. Physalin A induces G2/M phase cell cycle arrest in human non-small cell lung cancer cells: Involvement of the p38 MAPK/ROS pathway. Mol. Cell. Biochem. 2016;415:145–155. doi: 10.1007/s11010-016-2686-1. [DOI] [PubMed] [Google Scholar]
- 239.Lin H., Zhang C., Zhang H., Xia Y.Z., Zhang C.Y., Luo J., Yang L., Kong L.Y. Physakengose G induces apoptosis via EGFR/mTOR signaling and inhibits autophagic flux in human osteosarcoma cells. Phytomedicine. 2018;42:190–198. doi: 10.1016/j.phymed.2018.03.046. [DOI] [PubMed] [Google Scholar]
- 240.Sun Y., Guo T., Zhang F.B., Wang Y.N., Liu Z., Guo S., Li L. Isolation and characterization of cytotoxic withanolides from the calyx of Physalis alkekengi L. var franchetii. Bioorg. Chem. 2020;96:103614. doi: 10.1016/j.bioorg.2020.103614. [DOI] [PubMed] [Google Scholar]
- 241.Sun C.P., Qiu C.Y., Yuan T., Nie X.F., Sun H.X., Zhang Q., Li H.X., Ding L.Q., Zhao F., Chen L.X., et al. Antiproliferative and Anti-inflammatory Withanolides from Physalis angulata. J. Nat. Prod. 2016;79:1586–1597. doi: 10.1021/acs.jnatprod.6b00094. [DOI] [PubMed] [Google Scholar]
- 242.Sun C.P., Qiu C.Y., Zhao F., Kang N., Chen L.X., Qiu F. Physalins V-IX, 16,24-cyclo-13,14-seco withanolides from Physalis angulata and their antiproliferative and anti-inflammatory activities. Sci. Rep. 2017;7:4057. doi: 10.1038/s41598-017-03849-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Boonsombat J., Chawengrum P., Mahidol C., Kittakoop P., Ruchirawat S., Thongnest S. A new 22,26-seco physalin steroid from Physalis angulata. Nat. Prod. Res. 2020;34:1097–1104. doi: 10.1080/14786419.2018.1550766. [DOI] [PubMed] [Google Scholar]
- 244.Gao C., Li R., Zhou M., Yang Y., Kong L., Luo J. Cytotoxic withanolides from Physalis angulata. Nat. Prod. Res. 2018;32:676–681. doi: 10.1080/14786419.2017.1338281. [DOI] [PubMed] [Google Scholar]
- 245.Meng Q., Fan J., Liu Z., Li X., Zhang G., Zhang Y., Sun Y., Li L., Hua E. Cytotoxic Withanolides from the Whole Herb of Physalis angulata L. Molecules. 2019;24:1608. doi: 10.3390/molecules24081608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Xu Y., Bunting D.P., Liu M.X., Bandaranayake H.A., Gunatilaka A.A.L. 17β-Hydroxy-18-acetoxywithanolides from Aeroponically Grown Physalis crassifolia and Their Potent and Selective Cytotoxicity for Prostate Cancer Cells. J. Nat. Prod. 2016;79:821–830. doi: 10.1021/acs.jnatprod.5b00911. [DOI] [PubMed] [Google Scholar]
- 247.Zheng M., Guo J., Xu J., Yang K., Tang R., Gu X., Li H., Chen L. Ixocarpalactone A from dietary tomatillo inhibits pancreatic cancer growth by targeting PHGDH. Food Funct. 2019;10:3386–3395. doi: 10.1039/C9FO00394K. [DOI] [PubMed] [Google Scholar]
- 248.Wu J., Li X., Zhao J., Wang R., Xia Z., Li X., Liu Y., Xu Q., Khan I.A., Yang S. Anti-inflammatory and cytotoxic withanolides from Physalis minima. Phytochemistry. 2018;155:164–170. doi: 10.1016/j.phytochem.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 249.Wu J., Zhang T., Si J., Xu Q., Gu Y., Yang S., Zou Z. Five new 5,6-β-epoxywithanolides from Physalis minima. Fitoterapia. 2020;140:104413. doi: 10.1016/j.fitote.2019.104413. [DOI] [PubMed] [Google Scholar]
- 250.Le Canh V.C., Le Ba V., Thi Hai Yen P., Le Thi L., Thi Thuy Hoai P., Huu Dat T.T., Thao D.T., Bach L.G., Kim Y.H., Tuan Anh H.L. Identification Of Potential Cytotoxic Inhibitors From Physalis minima. Nat. Prod. Res. 2021;35:2082–2085. doi: 10.1080/14786419.2019.1650360. [DOI] [PubMed] [Google Scholar]
- 251.Zhang M., Jiang B., He X., Cao S., Ding L., Kang N., Chen L., Qiu F. New cytotoxic withanolides from Physalis minima. Fitoterapia. 2020;146:104728. doi: 10.1016/j.fitote.2020.104728. [DOI] [PubMed] [Google Scholar]
- 252.Xu Y.M., Wijeratne E.M.K., Babyak A.L., Marks H.R., Brooks A.D., Tewary P., Xuan L.J., Wang W.Q., Sayers T.J., Gunatilaka A.A.L. Withanolides from Aeroponically Grown Physalis peruviana and Their Selective Cytotoxicity to Prostate Cancer and Renal Carcinoma Cells. J. Nat. Prod. 2017;80:1981–1991. doi: 10.1021/acs.jnatprod.6b01129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Park E.J., Sang-Ngern M., Chang L.C., Pezzuto J.M. Induction of cell cycle arrest and apoptosis with downregulation of Hsp90 client proteins and histone modification by 4β-hydroxywithanolide E isolated from Physalis peruviana. Mol. Nutr. Food Res. 2016;60:1482–1500. doi: 10.1002/mnfr.201500977. [DOI] [PubMed] [Google Scholar]
- 254.Xu Y.M., Wijeratne E.M.K., Brooks A.D., Tewary P., Xuan L.J., Wang W.Q., Sayers T.J., Gunatilaka A.A.L. Cytotoxic and other withanolides from aeroponically grown Physalis philadelphica. Phytochemistry. 2018;152:174–181. doi: 10.1016/j.phytochem.2018.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Ding W., Hu Z., Zhang Z., Ma Q., Tang H., Ma Z. Physapubescin B Exhibits Potent Activity against Human Prostate Cancer In Vitro and In Vivo. J. Agric. Food Chem. 2015;63:9504–9512. doi: 10.1021/acs.jafc.5b03045. [DOI] [PubMed] [Google Scholar]
- 256.Xia G., Li Y., Sun J., Wang L., Tang X., Lin B., Kang N., Huang J., Chen L., Qiu F. Withanolides from the stems and leaves of Physalis pubescens and their cytotoxic activity. Steroids. 2016;115:136–146. doi: 10.1016/j.steroids.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 257.Zhao X., Huang L., Xu W., Chen X., Shen Y., Zeng W., Chen X. Physapubescin B inhibits tumorgenesis and circumvents taxol resistance of ovarian cancer cells through STAT3 signaling. Oncotarget. 2017;8:70130–70141. doi: 10.18632/oncotarget.19593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Yang K.Y., Wu C.R., Zheng M.Z., Tang R.T., Li X.Z., Chen L.X., Li H. Physapubescin I from husk tomato suppresses SW1990 cancer cell growth by targeting kidney-type glutaminase. Bioorg. Chem. 2019;92:103186. doi: 10.1016/j.bioorg.2019.103186. [DOI] [PubMed] [Google Scholar]
- 259.Basso A.V., Leiva González S., Barboza G.E., Careaga V.P., Calvo J.C., Sacca P.A., Nicotra V.E. Phytochemical Study of the Genus Salpichroa (Solanaceae), Chemotaxonomic Considerations, and Biological Evaluation in Prostate and Breast Cancer Cells. Chem. Biodivers. 2017;14 doi: 10.1002/cbdv.201700118. [DOI] [PubMed] [Google Scholar]
- 260.Kim S.P., Nam S.H., Friedman M. The tomato glycoalkaloid α-tomatine induces caspase-independent cell death in mouse colon cancer CT-26 cells and transplanted tumors in mice. J. Agric. Food Chem. 2015;63:1142–1150. doi: 10.1021/jf5040288. [DOI] [PubMed] [Google Scholar]
- 261.Chen M., Wu J., Zhang X.X., Wang Q., Yan S.H., Wang H.D., Liu S.L., Zou X. Anticancer activity of sesquiterpenoids extracted from Solanum lyratum via the induction of Mitochondria-Mediated apoptosis. Oncol. Lett. 2017;13:370–376. doi: 10.3892/ol.2016.5404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Yun-Ling X.U., Jia L.V., Wei-Fang W.A.N.G., Yue L.I.U., Ya-Juan X.U., Tun-Hai X.U. New steroidal alkaloid and furostanol glycosides isolated from Solanum lyratum with cytotoxicity. Chin. J. Nat. Med. 2018;16:499–504. doi: 10.1016/S1875-5364(18)30085-2. [DOI] [PubMed] [Google Scholar]
- 263.Fekry M.I., Ezzat S.M., Salama M.M., Alshehri O.Y., Al-Abd A.M. Bioactive glycoalkaloides isolated from Solanum melongena fruit peels with potential anticancer properties against hepatocellular carcinoma cells. Sci. Rep. 2019;9:1746. doi: 10.1038/s41598-018-36089-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Zhao D.Y., Liu Y., Yin X., Li X.M., Pan J., Guan W., Yang B.Y., Kuang H.X. Two new alkaloids from the sepals of Solanum melongena L. Nat. Prod. Res. 2021;35:3569–3577. doi: 10.1080/14786419.2020.1713126. [DOI] [PubMed] [Google Scholar]
- 265.Tuan Anh H.L., Tran P.T., Thao D.T., Trang D.T., Dang N.H., Van Cuong P., Kiem P.V., Minh C.V., Lee J.H. Degalactotigonin, a Steroidal Glycoside from Solanum nigrum, Induces Apoptosis and Cell Cycle Arrest via Inhibiting the EGFR Signaling Pathways in Pancreatic Cancer Cells. BioMed Res. Int. 2018;2018:3120972. doi: 10.1155/2018/3120972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Shi F., Wang C., Wang L., Song X., Yang H., Fu Q., Zhao W. Preparative isolation and purification of steroidal glycoalkaloid from the ripe berries of Solanum nigrum L. by preparative HPLC-MS and UHPLC-TOF-MS/MS and its anti-non-small cell lung tumors effects in vitro and in vivo. J. Sep. Sci. 2019;42:2471–2481. doi: 10.1002/jssc.201801165. [DOI] [PubMed] [Google Scholar]
- 267.Xiang L., Wang Y., Yi X., He X. Steroidal alkaloid glycosides and phenolics from the immature fruits of Solanum nigrum. Fitoterapia. 2019;137:104268. doi: 10.1016/j.fitote.2019.104268. [DOI] [PubMed] [Google Scholar]
- 268.Nath L.R., Gorantla J.N., Thulasidasan A.K.T., Vijayakurup V., Shah S., Anwer S., Joseph S.M., Antony J., Veena K.S., Sundaram S., et al. Evaluation of uttroside B, a saponin from Solanum nigrum Linn, as a promising chemotherapeutic agent against hepatocellular carcinoma. Sci. Rep. 2016;6:36318. doi: 10.1038/srep36318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Zhao Z., Jia Q., Wu M.S., Xie X., Wang Y., Song G., Zou C.Y., Tang Q., Lu J., Huang G., et al. Degalactotigonin, a natural compound from Solanum nigrum L., inhibits growth and metastasis of osteosarcoma through GSK3β inactivation-mediated repression of the Hedgehog/gli1 pathway. Clin. Cancer Res. 2018;24:130–144. doi: 10.1158/1078-0432.CCR-17-0692. [DOI] [PubMed] [Google Scholar]
- 270.Gu X.Y., Shen X.F., Wang L., Wu Z.W., Li F., Chen B., Zhang G.L., Wang M.K. Bioactive steroidal alkaloids from the fruits of Solanum nigrum. Phytochemistry. 2018;147:125–131. doi: 10.1016/j.phytochem.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 271.Zhang L., Lin H.-Q., Li G.-S., Yue X.-D., Dai S.-J. New sesquiterpenoid derivatives from Solanum septemlobum with cytotoxicities. Nat. Prod. Res. 2015;29:1889–1893. doi: 10.1080/14786419.2015.1010164. [DOI] [PubMed] [Google Scholar]
- 272.Balachandran C., Emi N., Arun Y., Yamamoto Y., Ahilan B., Sangeetha B., Duraipandiyan V., Inaguma Y., Okamoto A., Ignacimuthu S., et al. In vitro anticancer activity of methyl caffeate isolated from Solanum torvum Swartz. fruit. Chem. Biol. Interact. 2015;242:81–90. doi: 10.1016/j.cbi.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 273.Ben Bakrim W., El Bouzidi L., Nuzillard J.M., Cretton S., Saraux N., Monteillier A., Christen P., Cuendet M., Bekkouche K. Bioactive metabolites from the leaves of Withania adpressa. Pharm. Biol. 2018;56:505–510. doi: 10.1080/13880209.2018.1499781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Kim S., Yu J.S., Lee J.Y., Choi S.U., Lee J., Kim K.H. Cytotoxic Withanolides from the Roots of Indian Ginseng (Withania somnifera) J. Nat. Prod. 2019;82:765–773. doi: 10.1021/acs.jnatprod.8b00665. [DOI] [PubMed] [Google Scholar]
- 275.Yoneyama T., Arai M.A., Sadhu S.K., Ahmed F., Ishibashi M. Hedgehog inhibitors from Withania somnifera. Bioorg. Med. Chem. Lett. 2015;25:3541–3544. doi: 10.1016/j.bmcl.2015.06.081. [DOI] [PubMed] [Google Scholar]
- 276.Dar P.A., Mir S.A., Bhat J.A., Hamid A., Singh L.R., Malik F., Dar T.A. An anti-cancerous protein fraction from Withania somnifera induces ROS-dependent mitochondria-mediated apoptosis in human MDA-MB-231 breast cancer cells. Int. J. Biol. Macromol. 2019;135:77–87. doi: 10.1016/j.ijbiomac.2019.05.120. [DOI] [PubMed] [Google Scholar]
- 277.Selvakesavan R.K., Franklin G. Prospective application of nanoparticles green synthesized using medicinal plant extracts as novel nanomedicines. Nanotechnol. Sci. Appl. 2021;14:179–195. doi: 10.2147/NSA.S333467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Gajendran B., Chinnasamy A., Durai P., Raman J., Ramar M. Biosynthesis and characterization of silver nanoparticles from Datura inoxia and its apoptotic effect on human breast cancer cell line MCF7. Mater. Lett. 2014;122:98–102. doi: 10.1016/j.matlet.2014.02.003. [DOI] [Google Scholar]
- 279.Rajput S., Kumar D., Agrawal V. Green synthesis of silver nanoparticles using Indian Belladonna extract and their potential antioxidant, anti-inflammatory, anticancer and larvicidal activities. Plant Cell Rep. 2020;39:921–939. doi: 10.1007/s00299-020-02539-7. [DOI] [PubMed] [Google Scholar]
- 280.Chokkalingam M., Singh P., Huo Y., Soshnikova V., Ahn S., Kang J., Mathiyalagan R., Kim Y.J., Yang D.C. Facile synthesis of Au and Ag nanoparticles using fruit extract of Lycium chinense and their anticancer activity. J. Drug Deliv. Sci. Technol. 2019;49:308–315. doi: 10.1016/j.jddst.2018.11.025. [DOI] [Google Scholar]
- 281.Shejawal K.P., Randive D.S., Bhinge S.D., Bhutkar M.A., Todkar S.S., Mulla A.S., Jadhav N.R. Green synthesis of silver, iron and gold nanoparticles of lycopene extracted from tomato: Their characterization and cytotoxicity against COLO320DM, HT29 and Hella cell. J. Mater. Sci. Mater. Med. 2021;32:19. doi: 10.1007/s10856-021-06489-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Barwant M., Ugale Y., Ghotekar S., Basnet P., Nguyes V.-H., Pansambal S., Murthy A., Pham T.-H., Bilal M., Oza R., et al. Plant-Mediated Biological Synthesis of Ag-Ago- Ag2O Nanocomposites Using Leaf Extracts of Solanum Elaeagnifolium for Antioxidant, Anticancer, and DNA Cleavage Activities. [(accessed on 10 March 2022)]. Available online: https://assets.researchsquare.com/files/rs-973781/v1/e3654371-3edd-4957-9399-1bb661d71fa3.pdf?c=1637245890.
- 283.Lashin I., Fouda A., Gobouri A.A., Azab E., Mohammedsaleh Z.M., Makharita R.R. Antimicrobial and in vitro cytotoxic efficacy of biogenic silver nanoparticles (Ag--nps) fabricated by callus extract of Solanum incanum L. Biomolecules. 2021;11:341. doi: 10.3390/biom11030341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Miranda M.A., Marcato P.D., Carvalho I.P.S., Silva L.B., Ribeiro D.L., Amaral R., Swiech K., Bastos J.K., Paschoal J.A.R., dos Reis R.B., et al. Assessing the cytotoxic potential of glycoalkaloidic extract in nanoparticles against bladder cancer cells. J. Pharm. Pharmacol. 2019;71:1520–1531. doi: 10.1111/jphp.13145. [DOI] [PubMed] [Google Scholar]
- 285.Miranda M.A., Silva L.B., Carvalho I.P.S., Amaral R., de Paula M.H., Swiech K., Bastos J.K., Paschoal J.A.R., Emery F.S., dos Reis R.B., et al. Targeted uptake of folic acid-functionalized polymeric nanoparticles loading glycoalkaloidic extract in vitro and in vivo assays. Colloids Surf. B Biointerfaces. 2020;192:111106. doi: 10.1016/j.colsurfb.2020.111106. [DOI] [PubMed] [Google Scholar]
- 286.Ahmed H.A., Salama Z.A., Salem S.H., Aly H.F., Nassrallah A., Abou-Elella F., Aboul-Enein A.M. Lycopene Nanoparticles Ameliorate The Antioxidants, Antimicrobial And Anticancer Potencies Of Tomato Pomace. Egypt. J. Chem. 2021;64:3739–3749. doi: 10.21608/ejchem.2021.71766.3583. [DOI] [Google Scholar]
- 287.Gorbe M., Bhat R., Aznar E., Sancenón F., Marcos M.D., Herraiz F.J., Prohens J., Venkataraman A., Martínez-Máñez R. Rapid Biosynthesis of Silver Nanoparticles Using Pepino (Solanum muricatum) Leaf Extract and Their Cytotoxicity on HeLa Cells. Materials. 2016;9:325. doi: 10.3390/ma9050325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Ramar M., Manikandan B., Marimuthu P.N., Raman T., Mahalingam A., Subramanian P., Karthick S., Munusamy A. Synthesis of silver nanoparticles using Solanum trilobatum fruits extract and its antibacterial, cytotoxic activity against human breast cancer cell line MCF 7. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2015;140:223–228. doi: 10.1016/j.saa.2014.12.060. [DOI] [PubMed] [Google Scholar]
- 289.Vandhana T., Clement Lourduraj A.J. Biogenic synthesis of Mn-Ag co-doped FeO (Fe1-2xMnxAgx) nanoparticles: As an effective disinfectant and anticancer agent. Inorg. Chem. Commun. 2020;112:107712. doi: 10.1016/j.inoche.2019.107712. [DOI] [Google Scholar]
- 290.Zhang P., Wang P., Yan L., Liu L. Synthesis of gold nanoparticles with Solanum xanthocarpum extract and their in vitro anticancer potential on nasopharyngeal carcinoma cells. Int. J. Nanomed. 2018;13:7047–7059. doi: 10.2147/IJN.S180138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Alagesan V., Venugopal S. Green Synthesis of Selenium Nanoparticle Using Leaves Extract of Withania somnifera and Its Biological Applications and Photocatalytic Activities. Bionanoscience. 2019;9:105–116. doi: 10.1007/s12668-018-0566-8. [DOI] [Google Scholar]
- 292.Dhabian S.Z., Jasim R.S. Anticancer and Antioxidant activity of the Greenly synthesized Zinc nanoparticles composites using Aqueous extract of Withania somnifera plant. Egypt. J. Chem. 2021;64:5561–5574. doi: 10.21608/ejchem.2021.75114.3686. [DOI] [Google Scholar]
- 293.Mohan L. Alternative Medicine—Update. IntechOpen Limited; London, UK: 2021. Plant-Based Drugs as an Adjuvant to Cancer Chemotherapy. [Google Scholar]
- 294.Tai C.J., Wang C.K., Tai C.J., Lin Y.F., Lin C.S., Jian J.Y., Chang Y.J., Chang C.C. Aqueous extract of Solanum nigrum leaves induces autophagy and enhances cytotoxicity of cisplatin, doxorubicin, docetaxel, and 5-fluorouracil in human colorectal carcinoma cells. Evid. Based Complement. Altern. Med. 2013;2013:514719. doi: 10.1155/2013/514719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Sarmoko S., Putri D.D.P., Puspitasari E., Anindyajati A., Meiyanto E. Combination of Leunca Herb Ethanolic Extract and Doxorubicin Suppresses HeLa Cells’ Growth. Indones. J. Cancer Chemoprev. 2011;2:281–285. doi: 10.14499/indonesianjcanchemoprev2iss3pp281-285. [DOI] [Google Scholar]
- 296.Anindyajati A., Sarmoko S., Putri D.D.P., Hermawan A., Meiyanto E. Combination of Solanum nigrum L. Herb Ethanolic Extract and Doxorubicin Performs Synergism on T47D Breast Cancer Cells. Indones. J. Cancer Chemoprev. 2010;1:78. doi: 10.14499/indonesianjcanchemoprev1iss2pp78-84. [DOI] [Google Scholar]
- 297.Li H., Krstin S., Wang S., Wink M. Capsaicin and piperine can overcome multidrug resistance in cancer cells to doxorubicin. Molecules. 2018;23:557. doi: 10.3390/molecules23030557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Georgiev K.D., Slavov I.J., Iliev I.A. Synergistic Growth Inhibitory Effects of Lycium barbarum (Goji berry) Extract with Doxorubicin against Human Breast Cancer Cells. J. Pharm. Pharmacol. Res. 2019;3:51–58. doi: 10.26502/jppr.0020. [DOI] [Google Scholar]
- 299.Miranda M.A., Mondal A., Sachdeva M., Cabral H., Neto Y.A.A.H., Khan I., Groppo M., McChesney J.D., Bastos J.K. Chemosensitizing Effect of Cernumidine Extracted from Solanum cernuum on Bladder Cancer Cells in Vitro. Chem. Biodivers. 2019;16:e1900334. doi: 10.1002/cbdv.201900334. [DOI] [PubMed] [Google Scholar]
- 300.Wu Y.H., Chiu W.T., Young M.J., Chang T.H., Huang Y.F., Chou C.Y. Solanum incanum extract downregulates aldehyde dehydrogenase 1-mediated stemness and inhibits tumor formation in ovarian cancer cells. J. Cancer. 2015;6:1011–1019. doi: 10.7150/jca.12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Wang C.K., Lin Y.F., Tai C.J., Wang C.W., Chang Y.J., Choong C.Y., Lin C.S., Tai C.J., Chang C.C. Integrated Treatment of Aqueous Extract of Solanum nigrum -Potentiated Cisplatin- and Doxorubicin-Induced Cytotoxicity in Human Hepatocellular Carcinoma Cells. Evid. Based Complement. Altern. Med. 2015;2015:675270. doi: 10.1155/2015/675270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Tai C.J., Wang C.W., Chen C.L., Wang C.K., Chang Y.J., Jian J.Y., Lin C.S., Tai C.J. Cisplatin-, Doxorubicin-, and Docetaxel-Induced Cell Death Promoted by the Aqueous Extract of Solanum nigrum in Human Ovarian Carcinoma Cells. Integr. Cancer Ther. 2015;14:546–555. doi: 10.1177/1534735415588826. [DOI] [PubMed] [Google Scholar]
- 303.Jagadeeshan S., David D., Jisha S., Manjula S., Asha Nair S. Solanum nigrum Unripe fruit fraction attenuates Adriamycin resistance by down-regulating multi-drug resistance protein (Mdr)-1 through Jak-STAT pathway. BMC Complement. Altern. Med. 2017;17:370. doi: 10.1186/s12906-017-1872-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Wu C.H., Liang C.H., Shiu L.Y., Chang L.C., Lin T.S., Lan C.C.E., Tsai J.C., Wong T.W., Wei K.J., Lin T.K., et al. Solanum incanum extract (SR-T100) induces human cutaneous squamous cell carcinoma apoptosis through modulating tumor necrosis factor receptor signaling pathway. J. Dermatol. Sci. 2011;63:83–92. doi: 10.1016/j.jdermsci.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 305.Liu S.H., Shen X.H., Wei X.F., Mao X.H., Huang T. Immunomodulatory activity of butanol extract from Solanum lyratum in tumor-bearing mice. Immunopharmacol. Immunotoxicol. 2011;33:100–106. doi: 10.3109/08923973.2010.483520. [DOI] [PubMed] [Google Scholar]
- 306.Cham B.E., Chase T.R. Solasodine rhamnosyl glycosides cause apoptosis in cancer cells. Do they also prime the immune system resulting in long-term protection against cancer? Planta Med. 2012;78:349–353. doi: 10.1055/s-0031-1298149. [DOI] [PubMed] [Google Scholar]
- 307.Deng X., Luo S., Luo X., Hu M., Ma F., Wang Y., Zhou L., Huang R. Fraction From Lycium barbarum Polysaccharides Reduces Immunotoxicity and Enhances Antitumor Activity of Doxorubicin in Mice. Integr. Cancer Ther. 2018;17:860–866. doi: 10.1177/1534735417753544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Diwanay S., Chitre D., Patwardhan B. Immunoprotection by botanical drugs in cancer chemotherapy. J. Ethnopharmacol. 2004;90:49–55. doi: 10.1016/j.jep.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 309.Abdallah N.M., Noaman E., Eltahawy N.A., Badawi A.M., Kandil E., Mansour N.A., Mohamed H.E. Anticancer and radiosensitization efficacy of nanocomposite Withania somnifera extract in mice bearing tumor cells. Asian Pac. J. Cancer Prev. 2016;17:4367–4375. [PubMed] [Google Scholar]
- 310.Jasim G.A., Ghasemian A. The therapeutic efficacy of Physalis alkekengi hydro alcoholic extract on estrogen receptor-positive breast cancer mice model in an autophagy manner. Syst. Rev. Pharm. 2020;11:118–122. doi: 10.34172/jsums.2020.29. [DOI] [Google Scholar]
- 311.Li J.H., Li S.Y., Shen M.X., Qiu R.Z., Fan H.W., Li Y. Bin Anti-tumor effects of Solanum nigrum L. extraction on C6 high-grade glioma. J. Ethnopharmacol. 2021;274:114034. doi: 10.1016/j.jep.2021.114034. [DOI] [PubMed] [Google Scholar]
- 312.Razali F.N., Sinniah S.K., Hussin H., Zainal Abidin N., Shuib A.S. Tumor suppression effect of Solanum nigrum polysaccharide fraction on Breast cancer via immunomodulation. Int. J. Biol. Macromol. 2016;92:185–193. doi: 10.1016/j.ijbiomac.2016.06.079. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.