Abstract
The circadian clock is an evolutionarily highly conserved endogenous timing program that structures physiology and behavior according to the time of day. Disruption of circadian rhythms is associated with many common pathologies. The emerging field of circadian medicine aims to exploit the mechanisms of circadian physiology and clock–disease interaction for clinical diagnosis, treatment, and prevention. In this Essay, we outline the principle approaches of circadian medicine, highlight the development of the field in selected areas, and point out open questions and challenges. Circadian medicine has unambiguous health benefits over standard care but is rarely utilized. It is time for clock biology to become an integrated part of translational research.
The emerging field of circadian medicine implements and translates findings from clock biology to improve health. Circadian medicine has clear health benefits over standard care but is rarely used owing to a lack of systematic and mechanistic evidence and overarching concepts. This Essay explains the principles of circadian medicine and highlights future approaches to promote its dissemination.
Principles of circadian organization
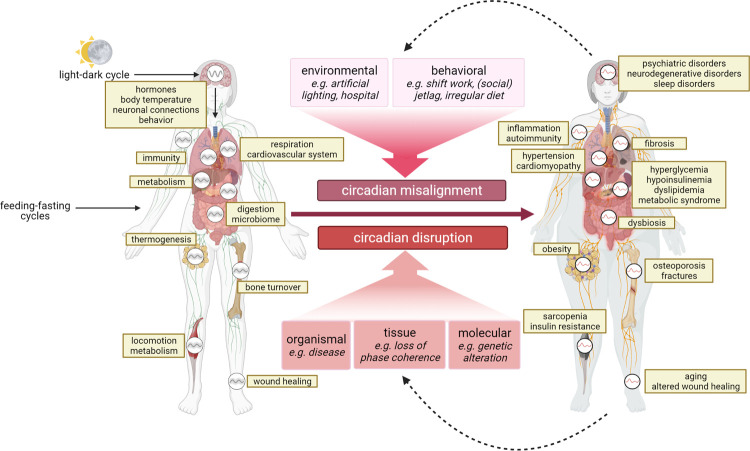
Humans are a rhythmic species. During evolution, they have adapted to environmental cycles such as daily and annual rhythms to be able to anticipate recurring opportunities and challenges. Nearly all physiological processes such as immune responses and energy metabolism—but also many behavioral functions—are temporally modulated by endogenous timing systems. The best-studied biological timer is the so-called circadian clock (from the Latin circa diem meaning “about a day”), a fundamental biological program that is critical to health [1–3]. Circadian rhythm disorders are on the rise in our modern, 24/7 society and occur, for example, during shift work. They are associated with an increased risk of common diseases including psychiatric and neurodegenerative disorders, metabolic and cardiovascular disorders, immune system dysfunction, and some sorts of cancer (Fig 1). Before describing the current state of knowledge about the medical implications of the circadian clock, let us first consider some basic principles of circadian organization.
Fig 1. Circadian misalignment and disruption are associated with disease.
Circadian rhythms are present at the level of the individual cell, tissue, and system and contribute to the optimal temporal coordination of physiological organ functions with environmental entrainment signals (left). It is therefore not surprising that misalignment of endogenous circadian and exogenous environmental cycles, as well as disruption of endogenous circadian rhythmicity is associated with or increases the risk for many diseases (right). Moreover, by contributing to circadian disruption or by altering behavioral rhythms, disease may in turn aggravate pathologies related to dysfunction of the circadian system (created with biorender.com).
Circadian rhythms are ubiquitous and affect almost all biological functions. Prominent examples are sleep–wake and feeding–fasting cycles, but cognitive performance, glymphatic and lymphatic fluid flow, body temperature, insulin sensitivity, glucose metabolism, immune cell trafficking and activity, hormone secretion, blood pressure, heart rate, kidney function, adipose tissue physiology, and many more processes are also affected by circadian rhythms (for recent reviews, see [3,4]). The circadian clock governs molecular and cellular processes at virtually every level of regulation. We know from mouse experiments that between 5% and 20% of all protein-coding genes are rhythmically expressed in each tissue, and nearly half are rhythmic somewhere in the body [5]. This ubiquity of circadian rhythms is reflected at the protein [6] and metabolite levels [7]. Recent data reveal that even the composition of the gut microbiota exhibits prominent circadian rhythms [8]. The ultimate goals of such temporal structuring of physiology and behavior are the anticipation of predictable changes in environmental demands and the temporal segregation of physiologically incompatible processes.
Circadian clocks are cellular entities based on a set of core clock genes and proteins organized in interlocked transcriptional–translational feedback loops (TTFLs). In the core circadian TTFL, the transcription factors CLOCK (circadian locomotor output cycles kaput) and BMAL1 (brain and muscle ANRT-like 1) drive transcription of period (Per1-3) and cryptochrome (Cry1/2) genes during the day. PER and CRY proteins form complexes that negatively feedback on CLOCK/BMAL1 activity during the night, thus shutting down their own transcription. The core TTFL is stabilized by several accessory loops to create self-sustained oscillations that persist even under nonrhythmic environmental conditions. In other words, cycles in sleep and wakefulness, body temperature, and hormone levels are not driven by environmental rhythms such as light–dark cycles but are sustained (with an endogenous, genetically determined period) even in constant environmental conditions. Although this was already well established for rodent clocks at the beginning of the 20th century, it was not until the groundbreaking work of Jürgen Aschoff in the 1960s that the existence of an endogenous clock in humans was unequivocally demonstrated [9]. While being principally self-sustained, circadian clocks and rhythms are synchronized to environmental cycles. This process is called entrainment. It ensures that oscillatory processes stably align with environmental cycles, which means that they always occur at predictable times relative to environmental time cues. The dominant natural time signal (or zeitgeber) for the human circadian clock is light, but food signals can also entrain cellular circadian clocks in peripheral tissues [10]. Temperature rhythms, exercise, and hormones such as cortisol and melatonin can also be applied as zeitgebers, for example, to accelerate realignment of internal and external time after rapid travel across time zones, a process termed jetlag.
In the 1970s, Ron Konopka and Seymour Benzer identified the first clock gene mutants in the fruit fly Drosophila, thus establishing a genetic basis for behavior [11]. With the cloning of the fly period (per) gene in the 1980s, the molecular biology era of chronobiology began [12,13]. The components of the molecular clockwork were successively discovered in different species (in mammals, about a dozen genes are involved) and the molecular mechanism of circadian rhythm generation, the TTFL, was deciphered [14]. Over 25 years later, in 2017, these achievements were acknowledged with the Nobel Prize in Physiology or Medicine for Michael Rosbash, Jeff Hall, and Michael Young.
The human circadian system is hierarchically organized. A master clock resides in the suprachiasmatic nucleus (SCN) of the hypothalamus. It receives information on external light conditions from the eyes via the retinohypothalamic tract [4]. In the retina, light is perceived by rods, cones, and blue-light sensitive ganglion cells expressing the photopigment melanopsin to synchronize the SCN clock with the environment [15]. Through a variety of routes, the SCN synchronizes the many molecular clocks in other brain areas and in peripheral organs [3,4]. Almost every cell in our body harbors its own molecular clockwork. Coupling signals between the SCN and peripheral clocks, as well as between single-cell clocks within a tissue, provides coherence and stable phase relationships within the circadian system. It is believed that the pathological effects of circadian disruptors such as shift work, jetlag, and nocturnal light exposure are the consequence of internal desynchronization (the loss of phase coherence between different tissue clocks) [3].
The expression of circadian rhythms in humans shows large variations. Interactions between genetic disposition, age, sex hormones, and light exposure (intensity, duration, and timing) determines the so-called chronotype [16]. In early and late chronotypes, clock-controlled processes tend to occur early and late, respectively, in relation to the synchronizing environmental cycles. There is a striking age dependency of chronotype: Children on average start as early types but become later and later during puberty, whereas adults become earlier and earlier with increasing age [17]. Chronotype is approximately normally distributed within the population, indicating polygenic traits [18]. Several candidate genes have been identified based on linkage between polymorphisms and chronotypic variance. The best-known example is a variant in the clock gene period 2 (PER2), which causes familial advanced sleep–wake phase syndrome (FASPS) [19].
The circadian system is tightly linked to sleep [20]. Sleep is promoted by a homeostatic process S, which controls sleep pressure as a function of wake time, and antagonized by process C, the circadian regulator of wakefulness. In humans, process C peaks in the afternoon and declines in the evening, opening the sleep window and allowing sleep to begin at a time of high sleep pressure. Sleep-regulating substances and wakefulness-inducing neurotransmitters act on subcortical sleep regulatory centers with strong connections to the SCN, but also to neurons of the stress system. Thus, the onset of sleep is associated with decreased activity of stress systems but is also characterized by darkness, recumbency, and decreases in food intake, locomotion, stimulus processing, and core body temperature. All these factors also act as timing signals for the SCN and peripheral clocks. In consequence, the manipulation of the circadian system always affects sleep and vice versa.
The circadian clock and disease
Fundamental insights from chronobiology have enabled us to understand the relevance of the circadian system for health and disease. It is now widely accepted that a functional and well-aligned circadian clock promotes health, while circadian disruption increases disease risk (Fig 1). Four fundamental insights paved the road leading from chronobiology to circadian medicine.
Disruption of the clock causes pathologies
In rodents, clock function has been experimentally manipulated at different levels and by various methods. The common result of such loss-of-function studies is that disrupting the clock leads to pathology. We refer to in-depth reviews and only list a few examples here. Genetic deletion of the essential clock gene Bmal1 [14] in mice leads to various pathologies, including hyperglycemia, hyperlipidemia, increased inflammation, and premature aging [21]. Bmal1 knockout in various tissues leads to phenotypes such as hypoglycemia and dyslipidemia (in the liver) [22], metabolic inefficiency and impaired triglyceride biosynthesis (in the muscle) [23], obesity (in adipose tissue) [24], or increased inflammation and insulin resistance (in myeloid cells) [25]. Variations of such phenotypes are seen after mutation or depletion of other clock genes. Anatomical ablation of the SCN pacemaker in rodents is associated with changes in intestinal immune cells and microbiota [26], increased adiposity [27], and tumor growth [28]. Exposing mice to a chronodisruptive environment such as repeated shifts in the light–dark cycle (simulating shift work or jetlag) increases mortality in aged animals [29], promotes tumor growth [30] and autoimmune processes [31], and dysregulates inflammatory responses [32].
Epidemiological, genetic, and laboratory studies link the circadian clock to human disease
Circadian disruption due to artificial light, shift work, travels across time zones, and social jetlag (the misalignment of biological and social time) has been linked to a variety of human diseases, ranging from sleep disorders, psychiatric and cardiovascular diseases to systemic chronic inflammation, impaired immune responses against pathogens, higher tumor risk, and worsened reactions to allergens and autoantigens [3]. For example, the large epidemiological Nurses’ Health Study showed that cancer is associated with shift work and circadian rhythm disruption [33]. Shift work further increases the risk of dyslipidemia and hypertension, type 2 diabetes, heart attacks, and multiple sclerosis [34,35]. It disrupts natural rhythms of the gut microbiota, thus increasing the risk of inflammatory bowel disease [36]. Social jetlag is associated with increased alcohol and cigarette consumption [37] and a higher prevalence of obesity [37], diabetes, cardiovascular diseases, and cancer [38]. Genetic association studies indicate a role for clock genes in immune, metabolic, and psychiatric disorders. For example, variants in several clock genes (including BMAL1 and PER2) as well as in the melatonin receptor 1B (MTNR1B) gene are associated with an increased risk of specific metabolic disorders. In laboratory studies in humans, circadian misalignment leads to increased blood pressure, increased ghrelin, and decreased leptin levels, as well as reduced insulin sensitivity in skeletal muscle (for a review, see [39]).
Disease occurrence and symptoms vary with time of day
The circadian clock controls a variety of physiological processes. Thus, it is not surprising that the expression of disease symptoms often also varies with the time of day. Some prominent examples for such rhythms are symptoms in asthma, allergic rhinitis, cancer, arthritis, pain, and depression as well as the incidence of heart attacks, suicidal intent, and peptic ulcers [2]. Epidemiological studies show a steep increase in the incidence of heart attacks and strokes in the morning hours [40]. Patients with rheumatoid arthritis (RA) are particularly affected by joint stiffness and pain in the morning hours, an aftereffect of a nocturnal increase in proinflammatory cytokines [41]. In asthma and allergic rhinitis, inflammatory processes and their symptoms are highest during the second half of the night—likely due to combined direct effects of sleep loss and circadian rhythms on pulmonary and nasal epithelial functions [42]. In neurodegenerative diseases, there are rhythms in mood and emotional volatility. The “sundowning syndrome” in patients with Alzheimer’s disease is a prominent example [43]. These patients are increasingly agitated and emotionally unstable in the late afternoon or evening. On the other hand, the “dawn phenomenon” in patients with diabetes, characterized by abnormally high fasting blood glucose levels due to impaired insulin secretion, is another example for an aggravation of disease symptoms during the morning [44].
Circadian rhythms are disrupted in many pathologies
An overwhelming body of evidence shows that daily rhythms are disrupted in a wide range of diseases. Again, we can only give a few examples here. In patients with neurodegenerative diseases, such as Parkinson’s disease, Alzheimer’s disease, or Huntington’s disease, sleep–wake behavior, melatonin secretion, and clock gene expression rhythms are all disrupted [45]. This holds true for schizophrenia spectrum and several other psychiatric disorders [46]. In patients with autoimmune diseases, daily rhythms in rest–activity, hormone, and cytokine levels, as well as molecular clock rhythms are disrupted [47]. In type 2 diabetes, circadian regulation of insulin secretion is impaired [48] and shifted eating patterns correlate with increased body mass index [49], in line with disrupted gut microbiota rhythms [8].
The triad of circadian medicine
The findings described above have led to the development of circadian medicine. While first successes are becoming apparent, circadian knowledge is still far from being part of routine medical practice (Box 1). Circadian medicine essentially comprises 3 main approaches (Fig 2): using knowledge of physiological rhythms for time-of-day adapted treatment regimens (exploiting the clock); improvement or resynchronization of disrupted rhythms through interventions in the clock (targeting the clock); and development of circadian medicine as part of precision medicine through new diagnostic tools that allow personalized interventions tailored to the chronotype (detecting the clock).
Box 1. A physician’s viewpoint on circadian medicine
The lack of awareness of our internal clock and the processes it controls can easily be linked to the conveniences and challenges of modern societies. Opportunities and 24/7 offerings in cities that never sleep, and the associated work demands, have resulted in a lost sense of physical needs that are less urgent than, for example, the desire to grab a quick bite to eat at a temptingly advertised fast food joint in the middle of the night. Similarly, disciplined adherence to timely or chronomedical medication intake is usually achieved only when the effects of delayed intake are severe (for example, off-times in patients with Parkinson’s disease) or when the adverse effects of postponed nonchronomedical medication intake are severe (for example, insomnia after delayed intake of corticosteroids). Adherence to an individual’s circadian rhythm, along with a healthy, balanced diet, regular physical activity, and healthy sleep, has the inestimable value of having a lasting positive impact on health and healthy aging, but also the challenge of making personal lifestyle choices that can then be translated into personalized therapies as needed. To firmly implement circadian principles in medical practice will require compelling science, clear information that permeates all levels of society, and implementation of knowledge about circadian medicine in the training of medical professionals.
Fig 2. The future of circadian medicine.
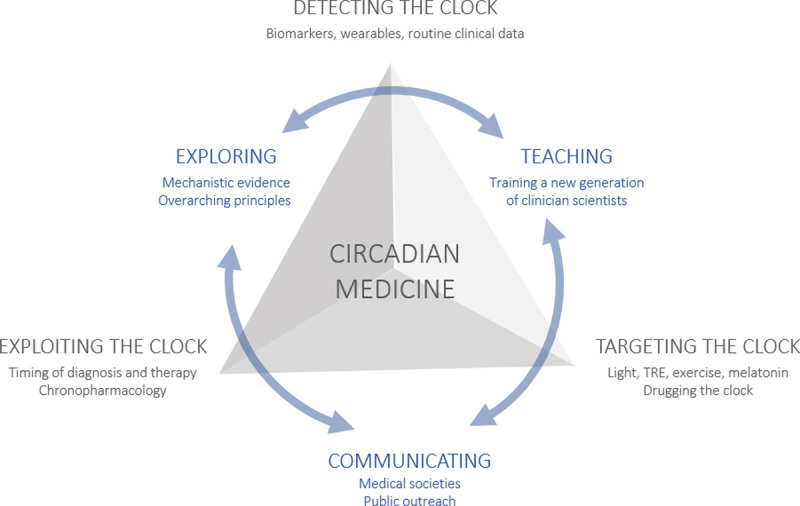
Our vision for the future of circadian medicine is to firmly integrate it into medical guidelines so that, for each patient, the circadian aspect is always taken into consideration and incorporated into the treatment plan as appropriate. Circadian medicine has many facets and to sustain its development, they all need to be advanced. They include treatment and diagnosis at the right time of day (exploiting), realigning and strengthening the circadian system (targeting), and diagnosing the patient’s circadian characteristics to develop personalized treatment plans (detecting). To achieve this goal, more evidence, especially on overarching principles of circadian medicine, needs to be gathered. To do this, on the one hand, we need a transdisciplinary approach to research, but we also need to train a new generation of physicians and communicate our findings more to the public and decision makers. TRE, time-restricted eating.
Exploiting the clock
In most pharmacological studies in which the time of administration is explicitly evaluated for clinical outcome, there is a clear time-of-day dependent variation in drug efficacy or toxicity [2,50–53]. This applies to drugs targeting major common diseases such as hypertension, cancer, asthma, and arthritis. This variation is explained by daily rhythms in pharmacokinetics and pharmacodynamics of most short-lived drugs [2,50,54]. For example, more than 50 years ago, HMG-CoA reductase, a rate-limiting enzyme of cholesterol synthesis, was described as being rhythmically expressed in rat liver. Its inhibitor, simvastatin, was approved some 20 years later for the treatment of hyperlipidemia with an explicit recommendation for the time-of-day to take it (“in the evening”)—one of the first chronopharmacological approvals. Timed immunotherapy in patients with melanoma has proven superior to standard therapy in terms of adverse effects and survival [55]. In RA therapy, application of a modified-release prednisone in the evening (with drug release during the second half of the night) reduces peak nocturnal interleukin-6 levels, thus positively affecting clinical parameters [42]. Such pharmacological studies are still few, although numbers have increased in recent years. Likewise, many surgical interventions can benefit from chronobiological optimization. For example, major adverse cardiovascular events are lower when aortic valve replacement is performed in the afternoon compared with morning surgeries, probably because myocardial tolerance to ischemia-reperfusion is better at this time of day [56]. Circadian effects are also important for disease diagnosis. For example, for the diagnosis of Cushing’s syndrome, which is characterized by hypercortisolemia, cortisol levels should be determined in the evening when endogenous cortisol production is at its trough [57], while adrenal insufficiency should be diagnosed in the morning when cortisol normally peaks [58].
Targeting the clock
Circadian rhythm disruption is not only a symptom, but also a risk factor for many diseases. In consequence, therapeutic approaches aimed at strengthening circadian rhythms may affect disease progression or even prevent disease initiation (Fig 3). Many zeitgebers known to influence the circadian system, such as light, food, melatonin, and exercise, have been used for this purpose [59]. Light therapy is a widely used adjunct therapy in sleep–wake rhythm and psychiatric disorders (such as depression and bipolar disorder [60]), but also in neurodegenerative disorders (such as Alzheimer’s disease and Parkinson’s disease [61]). Time-restricted eating, in which food consumption is limited to a window of 8 to 12 hours per day (without caloric restriction), improves glucose regulation, triglyceride levels, blood pressure, and various quality of life measures [62]. Exercise can phase-shift the human clock in a similar manner to light and enhance circadian amplitude of rest–activity cycles, body temperature, and muscle strength [63]. Furthermore, the circadian system can also be addressed by pharmacological means (“drugging the clock”), not only to strengthen clock rhythms, but also to address specific links between the clock and disease. Recently, several small molecule modulators of core clock function have been developed. They alter clock period, enhance its amplitude, or affect a specific clock component. For example, molecules that stabilize the clock protein cryptochrome 1 (CRY1) improve glucose tolerance in obese mice [64,65], while inhibiting casein kinase 1δ (CK1δ) prolongs clock period and may be used to treat (F)ASPS [66]. Of note, however, none of these molecules has yet been shown to be effective in humans.
Fig 3. Circadian medicine in ICUs.

Critically ill patients frequently exhibit disturbed or absent diurnal rhythms. This is likely to be a result of their illness and sedative measures but could also be related to the often-arrhythmic environment of an ICU (inadequate light exposure, parenteral nutrition, etc.). At the same time, they are arguably the best monitored patients, and vast amounts of routine clinical data are available with time courses for a variety of physiological parameters. We propose evaluating this treasure trove of information much more systematically with data science methods to detect the clock and improving light settings in the ICUs to target the clock. The analysis of clinical source data will help to characterize patients in the ICU in terms of their circadian rhythms, to identify predictors of circadian disruption as well as therapy-based improvements, and to associate circadian rhythms with clinical parameters (for example, delirium). In addition, since current ICUs do not provide adequate light settings, we have implemented a novel concept at Charité –Universitätsmedizin Berlin, consisting of a light ceiling for each experimental ICU bed that extends from the head above the patient to the patient’s feet [67]. Each light ceiling consists of multiple layers of light-emitting diodes designed to target the patient’s circadian clock. ICU, intensive care unit. Photos can be used with kind permission of GRAFT; photo credit is given to Tobias Hein.
Detecting the clock
In humans, the interaction of genetic disposition, age, sex, and light exposure (intensity, duration, and timing) determines the entrained phase, the so-called chronotype [17]. Since the outcome of many therapeutic interventions depends on internal circadian phase, such interventions should be tailored to the individual chronotype. The 2 main prerequisites for successful application of circadian precision medicine are attaining a high degree of accuracy, sensitivity, and reliability of individual circadian phase assessment in clinical practice and a reasonable cost and practical applicability. Chronotype is traditionally determined by questionnaires, actigraphy, or by determining the timing of the evening rise in melatonin levels in blood or saliva [68]. Recently, more practicable biomarkers have been suggested that use single blood or tissue samples instead of time series analyses, which may allow the determination of chronotype in larger cohorts [69]. In addition, we anticipate that wearables and telemedicine will increasingly contribute to circadian diagnostics, prevention, and health maintenance. Future challenges include the use of clinical source data to characterize patients in hospitals with regard to their circadian rhythms (Fig 3), as well as the development of new diagnostic tools for circadian disruption. For example, shift work probably leads to internal desynchronization of tissue clocks, which has been very difficult to measure in animal models and virtually impossible in humans.
Conclusion and open questions
In summary, overwhelming evidence indicates that the circadian clock is essential for health while its disruption causes pathologies [1]. These findings have sparked the development of circadian medicine, and the first successes in this field are becoming apparent. At the same time, in many disease areas, the extent, nature, and mechanism of circadian disruption and the mode of action of chronotherapies have not yet been sufficiently studied and validated. There is a lack of knowledge about the overarching principles of circadian disruption, its diagnosis, and therapy. To unravel these principles, several fundamental questions remain to be answered.
How can circadian clock function and rhythms be measured in clinical settings?
Traditionally, daily rhythms are captured by measuring many data points over one or more 24-hour cycles. In some clinical settings, this is possible (for example, in intensive care units), but for broader application, simpler solutions such as wearables are needed. New biomarkers can already infer circadian phase (chronotype) from a single biosample, but such tests are not yet available for detection of circadian changes in patients. Genetic markers may additionally be used to infer rhythm alterations in certain clinical settings.
How can circadian disruption be defined and quantified?
Many stressors in our modern society can affect circadian rhythms and “circadian disruption” is an umbrella term for very different modes of circadian alterations. Conceptually, one could distinguish at least 3 possible scenarios that are not mutually exclusive. The first is loss of rhythms or reduced rhythm amplitudes. The second is internal desynchronization, for example, different tissue clocks running with altered phase relationships. This is predicted when zeitgebers (such as light and food) are inconsistent (as may be the case with shift work). The third is circadian misalignment, for example, when internal synchrony is maintained but social demands do not match with internal time (such as when school starts too early for adolescents with late chronotypes). A common language is needed, and better tools to qualitatively and quantitatively describe circadian disruption under different conditions.
How does circadian disruption affect disease risk?
How exactly do shift work or other circadian disruptions contribute to a higher risk of diseases? What are the molecular and cellular mediators? How does clock disruption interact with other factors such as sleep loss, a lack of light exposure, increased stress, or unhealthy diets? Experimental protocols that aim to separate the effects of the circadian system from those of other factors are extremely challenging. We predict that in most cases where circadian medicine leads to positive health outcomes, circadian rhythm modulations exert a joint, synergistic influence on behavioral and physiological parameters together with other effectors such as caloric restriction or improved sleep.
How to choose and use the right circadian medicine approach?
To date, there are almost no recommendations or evidence-based guidelines on which type of circadian medicine should be used for which pathology, because evidence on the mechanisms of action is still sparse and no randomized controlled trials have been conducted.
How can chronobiology inform personalized medicine?
People are genetically different with regard to their circadian clocks and downstream physiology. However, the chronotype of patients has so far not had a role in the design of treatment. With simpler diagnostic methods for circadian characterization, this could change, and a truly individualized precision circadian medicine could be established.
In summary, it is becoming increasingly clear that circadian medicine has unambiguous health benefits over standard care. However, it is still far from being part of routine medical practice [70], and to truly advance circadian medicine, coordinated action is needed at different levels (Fig 2). In particular, there is still a lack of systematic and mechanistic evidence and overarching transdisciplinary chronomedical concepts. It is time to fill these gaps in order to make circadian aspects an integral part of translational research and clinical practice.
Acknowledgments
We sincerely apologize to all those colleagues whose important work is not cited because of space limitations.
Abbreviations
- BMAL1
brain and muscle ANRT-like 1
- CK1δ
casein kinase 1δ
- CLOCK
circadian locomotor output cycles kaput
- CRY1
cryptochrome 1
- FASPS
familial advanced sleep–wake phase syndrome
- MTNR1B
melatonin receptor 1B
- RA
rheumatoid arthritis
- SCN
suprachiasmatic nucleus
- TTFL
transcriptional–translational feedback loop
Funding Statement
This work was in part supported by funds from the German Research Foundation (www.dfg.de; TRR186/A17 and KR 1989/12-1 to AK; OS353-10/1 and OS353-11/1 to HO), the European Horizon 2020 program (https://ec.europa.eu/programmes/horizon2020/en/home; CLOCK 846016 to AK's lab), the Michael J. Fox Foundation (www.michaeljfox.org; Foxpark I & II to HO), the German Federal Ministry of Education and Research (BMBF) (www.bmbf.de; Female Professors Program III to TL), Joachim Herz Foundation (www.joachim-herz-stiftung.de/en; Add-On Fellowship for Interdisciplinary Life Sciences to AF). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Allada R, Bass J. Circadian Mechanisms in Medicine. N Engl J Med. 2021;384(6):550–61. doi: 10.1056/NEJMra1802337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cederroth CR, Albrecht U, Bass J, Brown SA, Dyhrfjeld-Johnsen J, Gachon F, et al. Medicine in the Fourth Dimension. Cell Metab. 2019;30(2):238–50. doi: 10.1016/j.cmet.2019.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finger AM, Kramer A. Mammalian circadian systems: Organization and modern life challenges. Acta Physiol (Oxf). 2021;231(3):e13548. doi: 10.1111/apha.13548 [DOI] [PubMed] [Google Scholar]
- 4.Finger AM, Dibner C, Kramer A. Coupled network of the circadian clocks: a driving force of rhythmic physiology. FEBS Lett. 2020;594(17):2734–69. doi: 10.1002/1873-3468.13898 [DOI] [PubMed] [Google Scholar]
- 5.Zhang R, Lahens NF, Ballance HI, Hughes ME, Hogenesch JB. A circadian gene expression atlas in mammals: implications for biology and medicine. Proc Natl Acad Sci U S A. 2014;111(45):16219–24. doi: 10.1073/pnas.1408886111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robles MS, Cox J, Mann M. In-vivo quantitative proteomics reveals a key contribution of post-transcriptional mechanisms to the circadian regulation of liver metabolism. PLoS Genet. 2014;10(1):e1004047. doi: 10.1371/journal.pgen.1004047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dallmann R, Viola AU, Tarokh L, Cajochen C, Brown SA. The human circadian metabolome. Proc Natl Acad Sci U S A. 2012;109(7):2625–9. doi: 10.1073/pnas.1114410109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reitmeier S, Kiessling S, Clavel T, List M, Almeida EL, Ghosh TS, et al. Arrhythmic Gut Microbiome Signatures Predict Risk of Type 2 Diabetes. Cell Host Microbe. 2020;28(2):258–72 e6. doi: 10.1016/j.chom.2020.06.004 [DOI] [PubMed] [Google Scholar]
- 9.Aschoff J. Circadian Rhythms in Man. Science. 1965;148(3676):1427–32. doi: 10.1126/science.148.3676.1427 [DOI] [PubMed] [Google Scholar]
- 10.Damiola F, Le Minh N, Preitner N, Kornmann B, Fleury-Olela F, Schibler U. Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Genes Dev. 2000;14(23):2950–61. doi: 10.1101/gad.183500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Konopka RJ, Benzer S. Clock mutants of Drosophila melanogaster. Proc Natl Acad Sci U S A. 1971;68(9):2112–6. doi: 10.1073/pnas.68.9.2112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bargiello TA, Jackson FR, Young MW. Restoration of circadian behavioural rhythms by gene transfer in Drosophila. Nature. 1984;312(5996):752–4. doi: 10.1038/312752a0 [DOI] [PubMed] [Google Scholar]
- 13.Zehring WA, Wheeler DA, Reddy P, Konopka RJ, Kyriacou CP, Rosbash M, et al. P-element transformation with period locus DNA restores rhythmicity to mutant, arrhythmic Drosophila melanogaster. Cell. 1984;39(2 Pt 1):369–76. doi: 10.1016/0092-8674(84)90015-1 [DOI] [PubMed] [Google Scholar]
- 14.Takahashi JS. Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet. 2017;18(3):164–79. doi: 10.1038/nrg.2016.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lazzerini Ospri L, Prusky G, Hattar S. Mood, the Circadian System, and Melanopsin Retinal Ganglion Cells. Annu Rev Neurosci. 2017;40:539–56. doi: 10.1146/annurev-neuro-072116-031324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roenneberg T, Kantermann T, Juda M, Vetter C, Allebrandt KV. Light and the human circadian clock. Handb Exp Pharmacol. 2013;217:311–31. doi: 10.1007/978-3-642-25950-0_13 [DOI] [PubMed] [Google Scholar]
- 17.Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, et al. Epidemiology of the human circadian clock. Sleep Med Rev. 2007;11(6):429–38. doi: 10.1016/j.smrv.2007.07.005 [DOI] [PubMed] [Google Scholar]
- 18.Kalmbach DA, Schneider LD, Cheung J, Bertrand SJ, Kariharan T, Pack AI, et al. Genetic Basis of Chronotype in Humans: Insights From Three Landmark GWAS. Sleep. 2017;40(2). doi: 10.1093/sleep/zsw048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toh KL, Jones CR, He Y, Eide EJ, Hinz WA, Virshup DM, et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science. 2001;291(5506):1040–3. doi: 10.1126/science.1057499 [DOI] [PubMed] [Google Scholar]
- 20.Foster RG. Sleep, circadian rhythms and health. Interface Focus. 2020;10(3):20190098. doi: 10.1098/rsfs.2019.0098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang G, Chen L, Grant GR, Paschos G, Song WL, Musiek ES, et al. Timing of expression of the core clock gene Bmal1 influences its effects on aging and survival. Sci Transl Med. 2016;8(324):324ra16. doi: 10.1126/scitranslmed.aad3305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pan X, Bradfield CA, Hussain MM. Global and hepatocyte-specific ablation of Bmal1 induces hyperlipidaemia and enhances atherosclerosis. Nat Commun. 2016;7:13011. doi: 10.1038/ncomms13011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dyar KA, Hubert MJ, Mir AA, Ciciliot S, Lutter D, Greulich F, et al. Transcriptional programming of lipid and amino acid metabolism by the skeletal muscle circadian clock. PLoS Biol. 2018;16(8):e2005886. doi: 10.1371/journal.pbio.2005886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paschos GK, Ibrahim S, Song WL, Kunieda T, Grant G, Reyes TM, et al. Obesity in mice with adipocyte-specific deletion of clock component Arntl. Nat Med. 2012;18(12):1768–77. doi: 10.1038/nm.2979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguyen KD, Fentress SJ, Qiu Y, Yun K, Cox JS, Chawla A. Circadian gene Bmal1 regulates diurnal oscillations of Ly6C(hi) inflammatory monocytes. Science. 2013;341(6153):1483–8. doi: 10.1126/science.1240636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Godinho-Silva C, Domingues RG, Rendas M, Raposo B, Ribeiro H, da Silva JA, et al. Light-entrained and brain-tuned circadian circuits regulate ILC3s and gut homeostasis. Nature. 2019;574(7777):254–8. doi: 10.1038/s41586-019-1579-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coomans CP, van den Berg SA, Lucassen EA, Houben T, Pronk AC, van der Spek RD, et al. The suprachiasmatic nucleus controls circadian energy metabolism and hepatic insulin sensitivity. Diabetes. 2013;62(4):1102–8. doi: 10.2337/db12-0507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Filipski E, King VM, Li X, Granda TG, Mormont MC, Liu X, et al. Host circadian clock as a control point in tumor progression. J Natl Cancer Inst. 2002;94(9):690–7. doi: 10.1093/jnci/94.9.690 [DOI] [PubMed] [Google Scholar]
- 29.Davidson AJ, Sellix MT, Daniel J, Yamazaki S, Menaker M, Block GD. Chronic jet-lag increases mortality in aged mice. Curr Biol. 2006;16(21):R914–6. doi: 10.1016/j.cub.2006.09.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu M, Zeng J, Chen Y, Zeng Z, Zhang J, Cai Y, et al. Experimental chronic jet lag promotes growth and lung metastasis of Lewis lung carcinoma in C57BL/6 mice. Oncol Rep. 2012;27(5):1417–28. doi: 10.3892/or.2012.1688 [DOI] [PubMed] [Google Scholar]
- 31.Toth LA, Trammell RA, Liberati T, Verhulst S, Hart ML, Moskowitz JE, et al. Influence of Chronic Exposure to Simulated Shift Work on Disease and Longevity in Disease-Prone Inbred Mice. Comp Med. 2017;67(2):116–26. [PMC free article] [PubMed] [Google Scholar]
- 32.Castanon-Cervantes O, Wu M, Ehlen JC, Paul K, Gamble KL, Johnson RL, et al. Dysregulation of inflammatory responses by chronic circadian disruption. J Immunol. 2010;185(10):5796–805. doi: 10.4049/jimmunol.1001026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I, et al. Night-shift work and risk of colorectal cancer in the nurses’ health study. J Natl Cancer Inst. 2003;95(11):825–8. doi: 10.1093/jnci/95.11.825 [DOI] [PubMed] [Google Scholar]
- 34.Papantoniou K, Massa J, Devore E, Munger KL, Chitnis T, Ascherio A, et al. Rotating night shift work and risk of multiple sclerosis in the Nurses’ Health Studies. Occup Environ Med. 2019;76(10):733–8. doi: 10.1136/oemed-2019-106016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ha M, Park J. Shiftwork and metabolic risk factors of cardiovascular disease. J Occup Health. 2005;47(2):89–95. doi: 10.1539/joh.47.89 [DOI] [PubMed] [Google Scholar]
- 36.Bishehsari F, Voigt RM, Keshavarzian A. Circadian rhythms and the gut microbiota: from the metabolic syndrome to cancer. Nat Rev Endocrinol. 2020;16(12):731–9. doi: 10.1038/s41574-020-00427-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–43. doi: 10.1016/j.cub.2012.03.038 [DOI] [PubMed] [Google Scholar]
- 38.Giuntella O, Mazzonna F. Sunset time and the economic effects of social jetlag: evidence from US time zone borders. J Health Econ. 2019;65:210–26. doi: 10.1016/j.jhealeco.2019.03.007 [DOI] [PubMed] [Google Scholar]
- 39.Mason IC, Qian J, Adler GK, Scheer F. Impact of circadian disruption on glucose metabolism: implications for type 2 diabetes. Diabetologia. 2020;63(3):462–72. doi: 10.1007/s00125-019-05059-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen L, Yang G. Recent advances in circadian rhythms in cardiovascular system. Front Pharmacol. 2015;6:71. doi: 10.3389/fphar.2015.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buttgereit F, Smolen JS, Coogan AN, Cajochen C. Clocking in: chronobiology in rheumatoid arthritis. Nat Rev Rheumatol. 2015;11(6):349–56. doi: 10.1038/nrrheum.2015.31 [DOI] [PubMed] [Google Scholar]
- 42.Buttgereit F, Doering G, Schaeffler A, Witte S, Sierakowski S, Gromnica-Ihle E, et al. Efficacy of modified-release versus standard prednisone to reduce duration of morning stiffness of the joints in rheumatoid arthritis (CAPRA-1): a double-blind, randomised controlled trial. Lancet. 2008;371(9608):205–14. doi: 10.1016/S0140-6736(08)60132-4 [DOI] [PubMed] [Google Scholar]
- 43.Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A. Sundowning and circadian rhythms in Alzheimer’s disease. Am J Psychiatry. 2001;158(5):704–11. doi: 10.1176/appi.ajp.158.5.704 [DOI] [PubMed] [Google Scholar]
- 44.Kashyap S, Bala R, Behl T. Understanding the Concept of Chronotherapeutics in the Management of Diabetes Mellitus. Curr Diabetes Rev. 2021;17(5):e221020187106. doi: 10.2174/1573399816666201022120825 [DOI] [PubMed] [Google Scholar]
- 45.Fifel K, Videnovic A. Circadian and Sleep Dysfunctions in Neurodegenerative Disorders-An Update. Front Neurosci. 2020;14:627330. doi: 10.3389/fnins.2020.627330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cosgrave J, Wulff K, Gehrman P. Sleep, circadian rhythms, and schizophrenia: where we are and where we need to go. Curr Opin Psychiatry. 2018;31(3):176–82. doi: 10.1097/YCO.0000000000000419 [DOI] [PubMed] [Google Scholar]
- 47.Xiang K, Xu Z, Hu YQ, He YS, Wu GC, Li TY, et al. Circadian clock genes as promising therapeutic targets for autoimmune diseases. Autoimmun Rev. 2021;20(8):102866. doi: 10.1016/j.autrev.2021.102866 [DOI] [PubMed] [Google Scholar]
- 48.Stenvers DJ, Scheer F, Schrauwen P, la Fleur SE, Kalsbeek A. Circadian clocks and insulin resistance. Nat Rev Endocrinol. 2019;15(2):75–89. doi: 10.1038/s41574-018-0122-1 [DOI] [PubMed] [Google Scholar]
- 49.Bruzas MB, Allison KC. A Review of the Relationship between Night Eating Syndrome and Body Mass Index. Curr Obes Rep. 2019;8(2):145–55. doi: 10.1007/s13679-019-00331-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ruben MD, Smith DF, FitzGerald GA, Hogenesch JB. Dosing time matters. Science. 2019;365(6453):547–9. doi: 10.1126/science.aax7621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gorbacheva VY, Kondratov RV, Zhang R, Cherukuri S, Gudkov AV, Takahashi JS, et al. Circadian sensitivity to the chemotherapeutic agent cyclophosphamide depends on the functional status of the CLOCK/BMAL1 transactivation complex. Proc Natl Acad Sci U S A. 2005;102(9):3407–12. doi: 10.1073/pnas.0409897102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anafi RC, Francey LJ, Hogenesch JB, Kim J. CYCLOPS reveals human transcriptional rhythms in health and disease. Proc Natl Acad Sci U S A. 2017;114(20):5312–7. doi: 10.1073/pnas.1619320114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Henriksson E, Huber AL, Soto EK, Kriebs A, Vaughan ME, Duglan D, et al. The Liver Circadian Clock Modulates Biochemical and Physiological Responses to Metformin. J Biol Rhythms. 2017;32(4):345–58. doi: 10.1177/0748730417710348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ruan W, Yuan X, Eltzschig HK. Circadian rhythm as a therapeutic target. Nat Rev Drug Discov. 2021;20(4):287–307. doi: 10.1038/s41573-020-00109-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Qian DC, Kleber T, Brammer B, Xu KM, Switchenko JM, Janopaul-Naylor JR, et al. Effect of immunotherapy time-of-day infusion on overall survival among patients with advanced melanoma in the USA (MEMOIR): a propensity score-matched analysis of a single-centre, longitudinal study. Lancet Oncol. 2021. doi: 10.1016/S1470-2045(21)00546-5 [DOI] [PubMed] [Google Scholar]
- 56.Montaigne D, Marechal X, Modine T, Coisne A, Mouton S, Fayad G, et al. Daytime variation of perioperative myocardial injury in cardiac surgery and its prevention by Rev-Erbalpha antagonism: a single-centre propensity-matched cohort study and a randomised study. Lancet. 2018;391(10115):59–69. doi: 10.1016/S0140-6736(17)32132-3 [DOI] [PubMed] [Google Scholar]
- 57.Carroll T, Raff H, Findling JW. Late-night salivary cortisol measurement in the diagnosis of Cushing’s syndrome. Nat Clin Pract Endocrinol Metab. 2008;4(6):344–50. doi: 10.1038/ncpendmet0837 [DOI] [PubMed] [Google Scholar]
- 58.Montes-Villarreal J, Perez-Arredondo LA, Rodriguez-Gutierrez R, Gonzalez-Colmenero AD, Solis RC, Gonzalez-Gonzalez JG, et al. Serum Morning Cortisol as a Screening Test for Adrenal Insufficiency. Endocr Pract. 2020;26(1):30–5. doi: 10.4158/EP-2019-0327 [DOI] [PubMed] [Google Scholar]
- 59.Panda S. The arrival of circadian medicine. Nat Rev Endocrinol. 2019;15(2):67–9. doi: 10.1038/s41574-018-0142-x [DOI] [PubMed] [Google Scholar]
- 60.Bais B, Hoogendijk WJG, Lambregtse-van den Berg MP. Light therapy for mood disorders. Handb Clin Neurol. 2021;182:49–61. doi: 10.1016/B978-0-12-819973-2.00004-6 [DOI] [PubMed] [Google Scholar]
- 61.Liu YL, Gong SY, Xia ST, Wang YL, Peng H, Shen Y, et al. Light therapy: a new option for neurodegenerative diseases. Chin Med J (Engl). 2020;134(6):634–45. doi: 10.1097/CM9.0000000000001301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Adafer R, Messaadi W, Meddahi M, Patey A, Haderbache A, Bayen S, et al. Food Timing, Circadian Rhythm and Chrononutrition: A Systematic Review of Time-Restricted Eating’s Effects on Human Health. Nutrients. 2020;12(12). doi: 10.3390/nu12123770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lewis P, Korf HW, Kuffer L, Gross JV, Erren TC. Exercise time cues (zeitgebers) for human circadian systems can foster health and improve performance: a systematic review. BMJ Open Sport Exerc Med. 2018;4(1):e000443. doi: 10.1136/bmjsem-2018-000443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Deota S, Panda S. New Horizons: Circadian Control of Metabolism Offers Novel Insight Into the Cause and Treatment of Metabolic Diseases. J Clin Endocrinol Metab. 2021;106(3):e1488–e93. doi: 10.1210/clinem/dgaa691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hirota T, Lee JW, St John PC, Sawa M, Iwaisako K, Noguchi T, et al. Identification of small molecule activators of cryptochrome. Science. 2012;337(6098):1094–7. doi: 10.1126/science.1223710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li SS, Dong YH, Liu ZP. Recent Advances in the Development of Casein Kinase 1 Inhibitors. Curr Med Chem. 2021;28(8):1585–604. doi: 10.2174/0929867327666200713185413 [DOI] [PubMed] [Google Scholar]
- 67.Luetz A, Piazena H, Weiss B, Finke A, Willemeit T, Spies C. Patient-centered lighting environments to improve health care in the intensive care unit. Clin Health Prom. 2016;6:5–12. [Google Scholar]
- 68.Reiter AM, Sargent C, Roach GD. Finding DLMO: estimating dim light melatonin onset from sleep markers derived from questionnaires, diaries and actigraphy. Chronobiol Int 2020;37(9–10):1412–24. doi: 10.1080/07420528.2020.1809443 [DOI] [PubMed] [Google Scholar]
- 69.Wittenbrink N, Ananthasubramaniam B, Munch M, Koller B, Maier B, Weschke C, et al. High-accuracy determination of internal circadian time from a single blood sample. J Clin Invest 2018;128(9):3826–39. doi: 10.1172/JCI120874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Selfridge JM, Gotoh T, Schiffhauer S, Liu J, Stauffer PE, Li A, et al. Chronotherapy: Intuitive, Sound, Founded. . .But Not Broadly Applied. Drugs 2016;76(16):1507–21. doi: 10.1007/s40265-016-0646-4 [DOI] [PMC free article] [PubMed] [Google Scholar]