Background:
Although abdominally-based free flaps have long been the gold standard, the profunda artery perforator (PAP) flap has emerged as an important alternative option for autologous breast reconstruction. The aim of this study was to directly compare the donor site morbidity of using the PAP versus deep inferior epigastric perforator (DIEP) free flap.
Methods:
We performed a retrospective review of patients undergoing autologous breast reconstruction using a DIEP and/or PAP flap from January 2017 to December 2020. In total, 30 PAP flap patients were matched with 60 DIEP flap patients. Outcomes included donor site wound dehiscence, length of stay, narcotic consumption, and pain scores. Patient-reported outcomes for the thigh versus abdomen were compared using questions derived from the BREAST-Q.
Results:
There was no significant difference in length of stay (P = 0.182), reoperation rates (P = 0.999), flap failure rates (P = 0.999), or donor site complications (P = 0.999). Both groups had similar mean pain scores, maximum pain scores, daily and total narcotic requirements. In comparing the thigh or abdomen as a donor site, there was no difference in frequency of negative symptoms (difficulty with daily activities, discomfort, tightness, and negative impact on ability to work) or satisfaction scores as related to their appearance in and out of clothing and the appearance of the scar.
Conclusions:
The thigh and abdomen are both suitable donor sites for autologous breast reconstruction with similar flap-related and patient-reported outcomes. The ultimate decision regarding whether to use a PAP or DIEP flap for breast reconstruction should be tailored based on patient anatomy and preference.
Takeaways
Question: How does the thigh compare with the abdomen as a donor site for autologous breast reconstruction?
Findings: This was a retrospective review of autologous breast reconstruction patients with the thigh or abdomen as the donor site. Donor site complications and patient-reported outcome measures demonstrated no significant difference between the two sites.
Meaning: The thigh and abdomen are both suitable donor sites for autologous breast reconstruction with similar flap-related and patient-reported outcomes.
INTRODUCTION
Breast reconstruction after mastectomy can significantly improve a patient’s sense of well-being and quality of life. Although implant-based reconstruction remains the most common method, autologous reconstruction has distinct advantages, including a more natural appearance with superior long-term aesthetic results and avoidance of implant-related complications.1 Allen and Treece reported the first case of using the deep inferior epigastric perforator (DIEP) flap for breast reconstruction.2 Since then, the DIEP flap has become the gold standard with a focus on minimizing donor site morbidity and improving overall aesthetics of both the breast and the abdomen.3 However, there has been a recent paradigm shift in using alternative donor sites for patients who are not good candidates for the DIEP flap due to a previous history of abdominal surgery or paucity of abdominal tissue, or patients who prefer to avoid any risk of abdominal wall morbidity.4 As our understanding of perforator flap physiology and imaging techniques have evolved, several additional flaps from the flanks, buttock, and thigh regions have emerged as promising additional options for autologous breast reconstruction.5–7 The profunda artery perforator (PAP) flap in particular has been utilized as an important alternative due to its relatively concealable donor site scar, consistent anatomy, and adequate flap volume.
Despite its rise in popularity, there are limited data on patient satisfaction and donor site outcomes with the PAP flap. In contrast, morbidity associated with an abdominally-based flap has been well-studied with reported rates of postoperative bulge or hernia ranging from 1% to 6%, with a single study reporting a prevalence of 33%.8–10 Despite recent technical modifications to the flap harvest process to minimize permanent adverse outcomes, there remains an impact on abdominal strength and function particularly for physically active patients. With advances in microsurgery, flap success rates in autologous reconstruction in high-volume centers were reported to be near 98%.11 Therefore, evaluation of patient outcomes and satisfaction has moved beyond flap survival to include impact of donor site morbidity.12 The aim of this study was to directly compare the donor site morbidity of using the PAP versus DIEP free flap for autologous breast reconstruction and to evaluate potential differences in patient outcomes.
METHODS
We performed a retrospective review of patients undergoing autologous breast reconstruction using a DIEP or PAP flap at our center from January 2017 to December 2020 following institutional review board approval. A total of 30 patients underwent breast reconstruction using the PAP flap. Sixty patients who underwent the DIEP free flap reconstruction during the same time period were matched to the PAP patient cohort in a two to one ratio based on age, body mass index (BMI), and ASA class. In addition, 17 patients who underwent simultaneous PAP and DIEP free flaps were identified and queried using the second patient-reported outcome questionnaire. Primary endpoints were donor site wound dehiscence, reoperation rates, length of stay, narcotic consumption, and pain scores during the admission. Pain scores were determined by a numerical rating pain scale ranging from 0 (no pain) to 10 (severe pain). Donor site wound dehiscence was defined as any wound requiring dressing changes or debridement. All opioid medications were converted to morphine equivalents to standardize comparison and interpretation. Secondary endpoints included flap-related outcomes including partial or total flap loss. Major complications were defined as complications requiring hospital readmission and/or unplanned return to the operating room.
In addition, two separate questionnaires were designed to assess patient-reported outcomes. The first questionnaire assessed the thigh or the abdomen in patients who had either the PAP or DIEP free flap. (See table, Supplemental Digital Content 1, which displays a patient-reported questionnaire for PAP or DIEP only patients. http://links.lww.com/PRSGO/B974.) Two novel surveys were developed and extrapolated from the BREAST-Q questionnaire specifically focusing on the assessment of patient physical well-being and satisfaction with the donor site. In addition, a separate questionnaire similarly derived from the BREAST-Q was sent to patients who underwent both free DIEP and PAP free flaps for reconstruction to directly compare the two donor sites in the same patient. (See table, Supplemental Digital Content 2, which displays a patient-reported questionnaire for stacked PAP and DIEP patients. http://links.lww.com/PRSGO/B975.) All patients were contacted by e-mail or telephone and invited to participate in the study.
Patient demographics and clinical characteristics were analyzed using IBM SPSS (version 21; IBM Corp., Armonk, N.Y.). Frequencies and proportions were used to summarize the categorical variables. Chi-square or Fisher exact tests and Student t-test were used to test for differences in demographics between the PAP versus DIEP groups. Differences in complications were assessed using the Chi-square or Fisher exact tests. The statistical significance was fixed two-tailed α less than 0.05 for all tests.
RESULTS
A total of 30 patients underwent breast reconstruction using the PAP flap. Sixty patients who underwent the DIEP free flap reconstruction during the same time period were matched based on age, BMI, and ASA class. In addition, 17 patients who underwent simultaneous PAP and DIEP free flaps and queried using the second patient-reported outcome questionnaire. The majority of patients (73.3%) had a BMI less than 30 kg/m2 for both the DIEP and PAP groups. The PAP flap skin paddle was oriented transversely in 17 patients, vertically in nine patients, and “L”-shaped in four patients. There were no significant differences between the PAP versus DIEP flap group in terms of previous radiation, chemotherapy, or laterality of reconstruction (Table 1). Delayed reconstructions were more common in patients who underwent DIEP free flaps (P = 0.012). Average follow-up was 17.1 ± 11.4 months for the PAP flap patients compared with 14.3 ± 8.5 months for the DIEP flap patients.
Table 1.
Demographics (PAP versus DIEP)
| DIEP | PAP | P | |
|---|---|---|---|
| No. patients | 60 | 30 | |
| Age* | 51.4 ± 9.3 | 51.4 ± 9.4 | 0.999 |
| BMI* | 0.999 | ||
| ≤30 | 44 (73.3) | 22 (73.3) | |
| >30 | 16 (26.7) | 8 (26.7) | |
| ASA* | 0.999 | ||
| 2 | 20 (33.3) | 10 (33.3) | |
| 3 | 40 (66.7) | 20 (66.7) | |
| Radiotherapy | 30 (50) | 12 (40) | 0.370 |
| Chemotherapy | 36 (60) | 16 (53.3) | 0.546 |
| Laterality | 0.179 | ||
| Unilateral | 29 (48.3) | 19 (63.3) | |
| Bilateral | 31 (51.7) | 11 (36.7) | |
| Timing of reconstruction | 0 (0) | 1 (3.3) | For 0* |
| Delayed | 35 (58.3) | 8 (26.7) | 0.012 |
| Delayed immediate | 11 (18.3) | 13 (43.3) | |
| Immediate | 14 (23.3) | 8 (26.7) |
*DIEP and PAP cohorts were matched by age, BMI, and ASA status.
There was no significant difference in length of stay (P = 0.182), reoperation rates (P = 0.999), flap failure rates (P = 0.999), or donor site wound complications (P = 0.999) between the two groups (Table 2). None of the reoperations within 30 days was related to a donor site complication. Of the six patients in the PAP group that experienced donor site complications, three patients had a transverse skin paddle, two had a vertical skin paddle, and one patient had an “L”-shaped skin paddle. Both groups had similar mean and maximum pain scores by postoperative day as shown (Table 3). There were no significant differences in narcotic requirements by postoperative day or in total narcotic requirements during the hospitalization.
Table 2.
Clinical Outcomes (PAP versus DIEP)
| DIEP | PAP | P | |
|---|---|---|---|
| Median OR time, min (range) | 503 (270–1086) | 539.5 (150–822) | 0.924 |
| Median LOS, d (range) | 4 (3-6) | 4.7 (3–8.6) | 0.182 |
| Reoperation within 30 days | 4 (6.7) | 2 (6.7) | 0.999 |
| Flap failure | 0 (0) | 0 (0) | 0.999 |
| Donor site wound dehiscence | 12 (20) | 6 (20) | 0.999 |
| Donor site infection | 0 (0) | 1 (3.3) | 0.341 |
Table 3.
Pain Scores and Narcotic Requirements (PAP versus DIEP)
| Variables | DIEP | PAP | P * |
|---|---|---|---|
| Average pain scores by postoperative day | |||
| POD#0 | 2.1(0–7.4) | 2.6(0–9) | 0.325 |
| POD#1 | 2.4(0.3–6.8) | 2.3(0.2–5.7) | 0.710 |
| POD#2 | 1.9(0–6.7) | 2(0.1–5.1) | 0.847 |
| POD#3 | 1.5(0–7.2) | 1.6(0–4.8) | 0.864 |
| POD#4 | 0.9(0–5.7) | 2.2(0–5.2) | 0.313 |
| Max pain score by postoperative day | |||
| POD#0 | 6(0–10) | 6.5(0–10) | 0.689 |
| POD#1 | 6(1–10) | 6(2–10) | 0.839 |
| POD#2 | 5(0–10) | 5(1–10) | 0.554 |
| POD#3 | 4(0–10) | 5(0–10) | 0.493 |
| POD#4 | 4(0–9) | 5(0–8) | 0.164 |
| Narcotic requirements by postoperative day | |||
| POD#0 | 9.5(0–272.8) | 18(0–155.9) | 0.375 |
| POD#1 | 15(0.4–203.8) | 17(10–155.9) | 0.140 |
| POD#2 | 17.5(0.8–92.5) | 26.3(2–137) | 0.284 |
| POD#3 | 21.4(2–85.8) | 23(7.5–101.3) | 0.580 |
| POD#4 | 30(7.5–75) | 25.3(20–60) | 0.880 |
| Total narcotic requirements during hospitalization | 23(1.9–622.1) | 41.8(0–561.4) | 0.630 |
*P values were calculated using Wilcoxon rank sum tests.
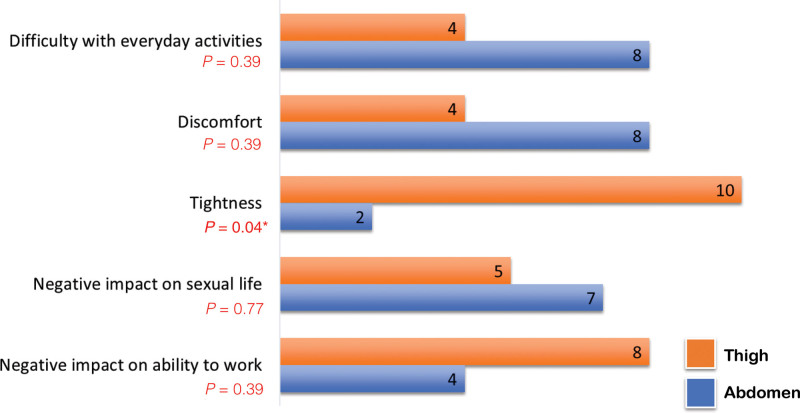
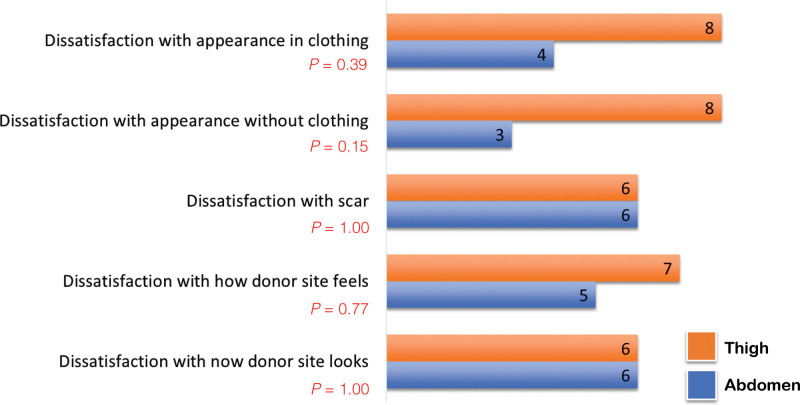
Thirty-eight of 90 patients (19 PAP flap patients and 19 DIEP flap patients) completed the first questionnaire for a response rate of 42.2%. Patients experienced negative thigh or abdomen donor site symptoms with similar frequencies and expressed similar levels of satisfaction for each donor site, with the exception that DIEP flap patients reported a higher frequency of their abdominal incisions having a negative impact on their sexual life compared with the thigh incisions in the PAP flap patients (Tables 4, 5). Twelve of the 17 patients (71%) who had both the PAP and DIEP free flap for reconstruction completed the questionnaire directly comparing the morbidity of the thigh versus abdomen. While tightness was the only donor site symptom significantly more frequently experienced in the thigh compared with the abdomen in these patients (Figs. 1, 2), donor site discomfort in general was two to three times higher in the abdominal donor site group although not statistically significant.
Table 4.
Summary of Donor Site Symptoms Experienced by PAP or DIEP Flap Only Patients (1 = None of the Time, 5 = All of the Time)
| Abdomen, Mean ± SD | Thigh, Mean ± SD | P * | |
|---|---|---|---|
| Difficulty doing everyday activities | 1.63 ± 1.12 | 1.42 ± 0.69 | 0.846 |
| Discomfort | 2.17 ± 1.15 | 1.84 ± 0.96 | 0.409 |
| Tightness | 2.47 ± 1.31 | 2.16 ± 1.26 | 0.462 |
| Negative impact on your sexual life due to incisions? | 2.26 ± 1.41 | 1.42 ± 0.84 | 0.042 * |
| Negative impact on your ability to work? | 1.74 ± 1.33 | 1.32 ± 0.82 | 0.373 |
*P values were calculated using Wilcoxon rank sum tests.
Boldface values indicate P < 0.05.
Table 5.
Summary of Donor Site Satisfaction Scores for PAP or DIEP Flap Only Patients (1 = Very Dissatisfied, 4 = Very Satisfied)
| Abdomen, Mean ± SD | Thigh, Mean ± SD | P * | |
|---|---|---|---|
| Appearance in clothing | 3.32 ± 0.95 | 3.68 ± 0.58 | 0.238 |
| Appearance without clothing | 2.84 ± 0.96 | 3.05 ± 1.18 | 0.323 |
| Appearance of scar | 2.74 ± 1.1 | 2.79 ± 1.08 | 0.892 |
| Feeling of donor site | 2.84 ± 1.01 | 2.95 ± 1.13 | 0.648 |
| Appearance of donor site | 2.79 ± 1.08 | 3.16 ± 1.07 | 0.262 |
*P values were calculated using Wilcoxon rank sum tests.
Fig. 1.
Comparison of donor site symptoms experienced by 12 patients who underwent simultaneous stacked PAP and DIEP flaps for breast reconstruction. Tightness was the only symptom experienced more commonly in the thigh compared with the abdomen.
Fig. 2.
Comparison of donor site satisfaction in 12 patients who underwent simultaneous stacked PAP and DIEP flaps for breast reconstruction. Satisfaction scores when comparing the thigh vs the abdomen were similar.
DISCUSSION
The abdomen remains the preferred choice for autologous breast reconstruction owing to the large amount of available skin and soft tissue, improved abdominal contour, and well-defined vascular anatomy. Several advancements including the transition to total muscle-sparing and now fascial-sparing techniques as well as refinements in perforator selection, and even robotic approaches to reduce the surgical footprint at the donor site have been implemented in attempts to limit the negative effects on abdominal wall function.8,13 Although alternative flaps utilizing other donor sites such as the buttock, thigh, and back region have been introduced for use mainly when the abdomen is not available or as adjunctive procedures for patients who require additional soft tissue, they have remained distant secondary options.14 However, with increasing experience and familiarity with the PAP flap, it has emerged as an important primary option for select patients who wish to avoid the abdomen as a donor site.15
In this study, there was no difference between the DIEP and PAP flap patients in immediate postoperative outcomes, including flap success and return to operating room and rates of donor site complications. Although the DIEP flap has been refined and optimized to maximize surgical success over time and limit donor site morbidity, we demonstrate that the PAP flap is an equally reliable option. In addition, patients with PAP flaps had similar pain scores and narcotic requirements compared with DIEP patients during their index hospital stay. The PAP flap patients are placed on the same enhanced recovery after surgery (ERAS) pathways, and this appears to be similarly effective in reducing opioid consumption and length of hospital stay, as demonstrated in DIEP patients.16 Notably, it is our standard practice to perform a transverse abdominis plane block for all DIEP flap patients with liposomal bupivacaine, which has been demonstrated to significantly decrease postoperative pain.15,17 The PAP flap patients in our cohort also underwent liposomal bupivacaine injection, but as local field infiltration into the harvest site, which may be less effective than the regional transverse abdominis plane block for the abdomen. Nonetheless, the PAP flap patients had similar pain scores and narcotic requirements, which may suggest that the thigh could be a less painful donor site compared with the abdomen. We were not able to capture analgesic requirements post discharge to determine whether patients experience more pain from the abdomen compared with the thigh, as the efficacy of the transverse abdominis plane block disappears.
For patients in whom both the abdomen and thigh are good donor site options, the choice for reconstruction should be based on volume of available tissue at each site, skin resurfacing needs, donor site morbidity, and patient and surgeon preference.18,19 Because fat distribution in patients with the same BMI can differ dramatically based on body habitus, both the thigh and abdomen should be routinely examined in all autologous reconstruction candidates. The DIEP flap in the majority of patients provides a larger amount of skin than the PAP flap. This is an important consideration for delayed reconstruction patients who often require replacement of the majority of the breast skin envelope.20 However, if the PAP and DIEP flaps provide similarly adequate amounts of soft tissue volume and skin surface area, surgeons should consider physical activity preferences and counsel patients on the morbidity of flap harvest from each donor site. Our selection criteria for PAP flaps over DIEP flaps are the following: (1) paucity of abdominal tissue unavailable due to prior surgery (ie, abdominoplasty or lack of suitable abdominal perforators); (2) greater volume of available tissue in thighs compared with the abdomen; (3) strong patient preference to avoid the abdomen as a donor site.
The long-term morbidity of DIEP free flaps is relatively well-known with rates of hernia and bulge ranging anywhere from 1% to 6%.9,21,22 In contrast, preliminary studies demonstrate little to no functional deficits with the PAP flap on lower extremity function with excellent patient satisfaction.23 Our study included a unique cohort of patients who underwent both PAP and DIEP free flap harvest concurrently. Although it was a relatively small sample size of 12 patients, these patients served as their own internal controls and they reported similar levels of negative symptoms and satisfaction for the thigh and the abdomen donor sites. Tightness was one complaint more prevalent in the thighs compared with the abdomen; patients considering the PAP flap should be appropriately counseled about this before surgery. Although our surveys did not undergo the same psychometric analysis and validation process of the BREAST-Q, it demonstrated statistically similar outcomes for both the thigh and the abdomen. In addition, there were several trends that appeared to favor the thigh but were not statistically significant likely due to a type II error from a low sample size. Future studies using validated patient-reported outcome measures should be conducted to corroborate our findings.
The PAP skin paddle can be oriented transversely, vertically or in an “L-shaped” pattern incorporating both a horizontal and vertical component.24 The majority of breast reconstruction patients prefer the transverse pattern due to its less conspicuous scar. However, the transverse scar may lead to sensation of greater tightness especially when sitting, due to its orientation along the skin tension. This should be taken into consideration in patients with minimal skin laxity in the upper thigh region, and weighed against the disadvantages of a much more visible vertical scar in the medial thigh. It is important to note that there was a significant learning curve with the PAP flap harvest in our cohort. Specifically with the transversely oriented flaps, the authors initially designed much wider skin paddles than required, but have since transitioned to smaller flap widths with more beveling of the fat to obtain adequate volume while minimizing the risk of wound dehiscence. Beveling is also important to not miss the most proximal perforator, which has been shown most consistently to be about 7 cm from the gluteal crease and typically lies at the inferior most aspect of the incision.15 Anecdotally, the feeling of tightness appears to improve with time and conservative maneuvers, including stretching and massage. Future studies are needed to elucidate the true impact of this symptom on patient’s return to physical activity and overall sense of well-being.
There are several limitations to our study, including its single-institution, retrospective design with its inherent risk of bias. Given the small nature of our cohort, the patient-reported outcomes analysis was underpowered and any potential differences which may be clinically significant may not have been statistically significant. In addition, we were not able to capture pain levels or narcotic consumption in the postoperative period after discharge. Furthermore, there is currently no validated patient-reported outcome tool equivalent to the BREAST-Q to assess the thigh donor site; however, both of our questionnaires contained items and questions directly derived from the abdominal donor site subscale of the BREAST-Q. Finally, the relatively short follow-up time limits the ability to assess any lasting negative donor site consequences especially related to the abdominal wall such as hernia and bulge.
Ultimately, our experience adds to the growing literature supporting the safety and efficacy of the PAP flap as an alternative to the DIEP flap for autologous breast reconstruction. Furthermore, this is the first study to directly compare donor site outcomes of the thigh versus the abdomen, using both objective measures and patient-reported outcome questionnaires. We demonstrate similar levels of donor site morbidity for the PAP and DIEP flaps with some subtle differences. Given these findings, the PAP flap should be included in the armamentarium for all reconstructive plastic surgeons and the ultimate decision of whether to use a PAP or DIEP flap for breast reconstruction should be tailored based on patient anatomy, lifestyle, and preference.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. [DOI] [PubMed] [Google Scholar]
- 2.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–38. [DOI] [PubMed] [Google Scholar]
- 3.Macadam SA, Bovill ES, Buchel EW, et al. Evidence-based medicine: autologous breast reconstruction. Plast Reconstr Surg. 2017;139:204e–229e. [DOI] [PubMed] [Google Scholar]
- 4.Opsomer D, van Landuyt K. Indications and controversies for nonabdominally-based complete autologous tissue breast reconstruction. Clin Plast Surg. 2018;45:93–100. [DOI] [PubMed] [Google Scholar]
- 5.Arnez ZM, Pogorelec D, Planinsek F, et al. Breast reconstruction by the free transverse gracilis (TUG) flap. Br J Plast Surg. 2004;57:20–26. [DOI] [PubMed] [Google Scholar]
- 6.Tuinder SMH, Beugels J, Lataster A, et al. The lateral thigh perforator flap for autologous breast reconstruction: a prospective analysis of 138 flaps. Plast Reconstr Surg. 2018;141:257–268. [DOI] [PubMed] [Google Scholar]
- 7.Baumeister S, Werdin F, Peek A. The sGAP flap: rare exception or second choice in autologous breast reconstruction? J Reconstr Microsurg. 2010;26:251–258. [DOI] [PubMed] [Google Scholar]
- 8.Chang EI, Chang EI, Soto-Miranda MA, et al. Comprehensive analysis of donor-site morbidity in abdominally based free flap breast reconstruction. Plast Reconstr Surg. 2013;132:1383–1391. [DOI] [PubMed] [Google Scholar]
- 9.Butler DP, Plonczak AM, Reissis D, et al. Factors that predict deep inferior epigastric perforator flap donor site hernia and bulge. J Plast Surg Hand Surg. 2018;52:338–342. [DOI] [PubMed] [Google Scholar]
- 10.Futter CM, Webster MH, Hagen S, et al. A retrospective comparison of abdominal muscle strength following breast reconstruction with a free TRAM or DIEP flap. Br J Plast Surg. 2000;53:578–583. [DOI] [PubMed] [Google Scholar]
- 11.Wade RG, Razzano S, Sassoon EM, et al. Complications in DIEP flap breast reconstruction after mastectomy for breast cancer: A prospective cohort study comparing unilateral versus bilateral reconstructions. Ann Surg Oncol. 2017;24:1465–1474. [DOI] [PubMed] [Google Scholar]
- 12.Grinsell DG, McCoubrey GW, Finkemeyer JP. The deep inferior epigastric perforator learning curve in the current era. Ann Plast Surg. 2016;76:72–77. [DOI] [PubMed] [Google Scholar]
- 13.Macadam SA, Zhong T, Weichman K, et al. Quality of life and patient-reported outcomes in breast cancer survivors: a multicenter comparison of four abdominally based autologous reconstruction methods. Plast Reconstr Surg. 2016;137:758–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myers PL, Nelson JA, Allen RJ, Jr. Alternative flaps in autologous breast reconstruction. Gland Surg. 2021;10:444–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Largo RD, Chu CK, Chang EI, et al. Perforator mapping of the profunda artery perforator flap: anatomy and clinical experience. Plast Reconstr Surg. 2020;146:1135–1145. [DOI] [PubMed] [Google Scholar]
- 16.Offodile AC, II, Gu C, Boukovalas S, et al. Enhanced recovery after surgery (ERAS) pathways in breast reconstruction: systematic review and meta-analysis of the literature. Breast Cancer Res Treat. 2019;173:65–77. [DOI] [PubMed] [Google Scholar]
- 17.Momeni A, Ramesh NK, Wan D, et al. Postoperative analgesia after microsurgical breast reconstruction using liposomal bupivacaine (Exparel). Breast J. 2019;25:903–907. [DOI] [PubMed] [Google Scholar]
- 18.Chu CK, DeFazio M, Largo RD, et al. Bilateral breast reconstruction with profunda artery perforator flaps and immediate implant augmentation. Aesthet Surg J Open Forum. 2020;2:ojz036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jo T, Jeon DN, Han HH. The PAP flap breast reconstruction: a practical option for slim patients. J Reconstr Microsurg. 2022;38:27–33. [DOI] [PubMed] [Google Scholar]
- 20.Phillips BT, Mercier-Couture G, Xue AS, et al. Is tissue expansion worth it? Comparative outcomes of skin-preserving versus delayed autologous breast reconstruction. Plast Reconstr Surg Glob Open. 2020;8:e3217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Espinosa-de-Los-Monteros A, Frias-Frias R, Alvarez-Tostado-Rivera A, et al. Postoperative abdominal bulge and hernia rates in patients undergoing abdominally based autologous breast reconstruction: systematic review and meta-analysis. Ann Plast Surg. 2021;86:476–484. [DOI] [PubMed] [Google Scholar]
- 22.Garvey PB, Salavati S, Feng L, et al. Abdominal donor-site outcomes for medial versus lateral deep inferior epigastric artery branch perforator harvest. Plast Reconstr Surg. 2011;127:2198–2205. [DOI] [PubMed] [Google Scholar]
- 23.Haddock NT, Teotia SS. Consecutive 265 profunda artery perforator flaps: refinements, satisfaction, and functional outcomes. Plast Reconstr Surg Glob Open. 2020;8:e2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunsinger V, Lhuaire M, Haddad K, et al. Medium- and large-sized autologous breast reconstruction using a fleur-de-lys profunda femoris artery perforator flap design: a report comparing results with the horizontal profunda femoris artery perforator flap. J Reconstr Microsurg. 2019;35:8–14. [DOI] [PubMed] [Google Scholar]