Abstract
Dyslipidemia, characterized by a high level of lipids (cholesterol, triglycerides, or both), can increase the risk of developing and progressing atherosclerosis. As atherosclerosis progresses, the number and severity of aterial plagues increases with greater risk of myocardial infarction, a major contributor to cardiovascular mortality. Atherosclerosis progresses in four phases, namely endothelial dysfunction, fatty streak formation, lesion progression and plaque rupture, and eventually thrombosis and arterial obstruction. With greater understanding of the pathological processes underlying atherosclerosis, researchers have identified that lipoproteins play a significant role in the development of atherosclerosis. In particular, apolipoprotein B (apoB)-containing lipoproteins have been shown to associate with atherosclerosis. Oxidized low-density lipoproteins (ox-LDLs) also contribute to the progression of atherosclerosis whereas high-density lipoproteins (HDL) contribute to the removal of cholesterol from macrophages thereby inhibiting the formation of foam cells. Given these known associations, lipoproteins may have potential as biomarkers for predicting risk associated with atherosclerotic plaques or may be targets as novel therapeutic agents. As such, the rapid development of drugs targeting lipoprotein metabolism may lead to novel treatments for atherosclerosis. A comprehensive review of lipoprotein function and their role in atherosclerosis, along with the latest development of lipoprotein targeted treatment, is timely. This review focuses on the functions of different lipoproteins and their involvement in atherosclerosis. Further, diagnostic and therapeutic potential are highlighted giving insight into novel lipoprotein-targetted approaches to treat atherosclerosis.
Keywords: atherosclerosis, dyslipidemia, lipoproteins, HDL, LDL
1. Introduction
Atherosclerosis is one of the most common causes of cardiovascular disease (CVD), leading to about 7.2 million deaths each year [1], and the American Heart Association has reported that the prevalence of atherosclerosis will increase by 18% by 2030 [1]. Risk factors for atherosclerosis include dyslipidemia, hypertension, obesity, smoking, diabetes, abnormal glucose tolerance, age, gender, and family history. Of these, recent research has suggested that dyslipidemia is one of the main risk factors contributing to the incidence and progression of atherosclerosis. Dyslipidemia is a common condition characterized by high plasma levels of cholesterol, triglycerides, or both [2] and measurement of plasma cholesterol and triglycerides levels are reliable diagnostic markers of dyslipidemia. Triglycerides and cholesterol are major lipids in the blood that are transported by lipoproteins and have different physiological functions. Triglycerides are a key source of calories (energy) throughout the body and also store excess heat. Cholesterol is an essential structural constituent of cell membranes and is an essential constituent of some hormones (e.g., steroid hormones). In healthy people, when levels of glycerides/cholesterol increase within the blood, cells such as hepatocytes secrete lipoproteins that play an essential role in lipid transport, metabolism, and storage. Binding of lipids to the lipoproteins facilitates a rebalance of lipid metabolism and returns circulating levels of unbound glycerides/cholesterol to more normal levels. Lipoproteins are classified into five categories based on their density and size, namely very-low-density lipoprotein (VLDLs), low-density lipoproteins (LDLs), intermediate-density lipoproteins (IDLs), high-density lipoproteins (HDLs), and chylomicrons (CM). The various lipoproteins bind different proportions of triglycerides and cholesterol and are associated with different types of apolipoproteins [3]. The unique composition of each lipoprotein determines its specific function in maintaining the balance of lipid metabolism [4]. The various lipoproteins work together cohesively to maintain healthy vasculature, including the coroanary arteries. However, with prolonged dyslipidemia, the lipoproteins fail to maintain healthy lipid metabolism, resulting in sustained high levels of cholesterol and triglycerides and accelerated accumulation of lipids in atherosclerotic plaque, thereby exacerbating atherosclerosis.
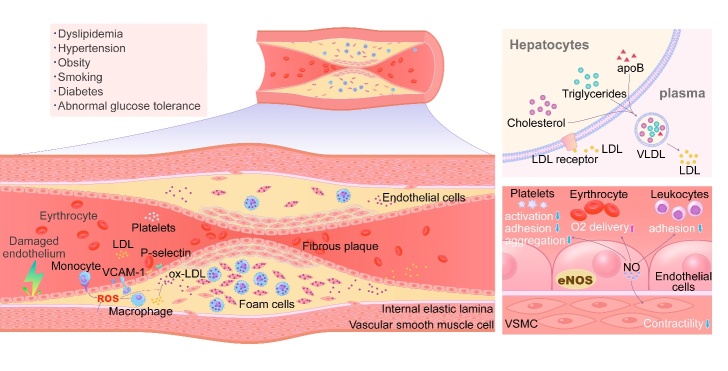
Multiple steps are involved in the pathogenesis of atherosclerosis, including lipid infiltration, endothelial damage, inflammatory response, platelet aggregation, and thrombosis (Fig. 1). Endothelial damage is considered the first step preceding the formation of atherosclerotic plaque. A key function of endothelial cells is to prevent adhesion in the vasculature. Endothelial dysfunction is induced by conditions such as hypertension, metabolic syndrome, smoking and physical inactivity, resulting in senescence and apoptosis of endothelial cells [5]. Abnormal or damaged endothelium increases expression of inflammatory factors like adhesion molecules with enhanced permeability, resulting in increased numbers of lipid particles penetrating the intima and sequential accumulation of lipid within the sub-intima. Lipoproteins continue to enter into the subintimal space and subendothelium, either through transcytosis, or via gap junctions and other processes [5]. Infiltration of lipoproteins, particularly LDL, contributes to the development of atherosclerosis. LDL often enters and accumulates in subendothelium of the vascular wall via transcytosis (promoted by inflammatory factors such as tumour necrosis factor α (TNF-α)). LDL then undergoes oxidative modification induced by vascular smooth muscle cells (SMCs), monocytes, and endothelial cells, resulting in the formation of oxidized LDL (ox-LDL) [6]. Ox-LDL further aggravates endothelial damage and stimulates endothelial cells to produce molecules such as E-selectin or P-selectin, promoting the migration of circulating monocytes towards the vascular wall [7]. Ox-LDL stimulation of endothelium also induces expression of monocyte chemoattractant protein-1 (MCP-1) resulting in monocytes being attracted and traversing the endothelial intercellular gap, entering the sub-intimal space of the vascular wall and accumulating at the lesion site [8]. Similarly, TNF-α stimulates endothelial cells to express interferon-gamma-induced protein 10 (IP-10) which then participates in the collection and migration of lymphocytes from blood into the arterial wall. Both vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1) are secreted by endothelial cells and facilitate capture of monocytes by damaged endothelium. Monocytes accumulating in the damaged endothelium proliferate further signals, promoting increased migration of monocytes to the lesion site resulting in further adhesion of monocytes and lymphocytes to endothelial cells with progressive migration into sub-intimal space, thereby facilitating a vicious cycle. Simultaneously, under the influence of mitogen-responsive nuclear factors, SMCs of the arterial media layers also migrate into the sub-intimal space through the fenestrated pores in the internal elastic lamina [9]. Monocytes transform into macrophages and, together with SMCs, take up ox-LDL by a variety of mechanisms, resulting in the formation of foam cells. Monocyte-derived macrophages engulf ox-LDL via a number of scavenger receptors (SRs) including CD36 receptors, and Fc receptors (FcRγs) which are implicated in the formation of monocyte-derived foam cells. Meanwhile, SMC-derived macrophages can engulf ox-LDL via lipoprotein lipase (LPL) receptors, leading to the formation of muscle-derived foam cells. Taken together, ox-LDL is the main contributor to the formation of foam cells, and foam cell formation is a key early event in atherosclerotic plaque development [3]. Interestingly, modified LDLs are exclusively captured by the macrophage scavenger receptor system, and ox-LDL production is not controlled by a feedback mechanism, thus resulting in an unlimited uptake [3]. The early atherosclerotic plaque then progresses to intimal thickening and narrowing of the vascular lumen, eventually resulting in vessel occlusion with thrombus formation with resultant clinical symptoms and adverse outcomes.
Figure 1.
Summary of the mechanism of atherogenesis. Triglycerides, cholesterols and apoB comprise VLDLs in liver, which are secreted into the circulation. Most of the triglycerides are removed by lipoprotein lipase leading to the VLDLs’ transformation into LDLs. In normal metabolism, LDLs are removed from circulation via LDL receptors on the surface of hepatocytes. However, when the excessive secretion of lipoproteins by the liver and/or ineffective clearance of plasma LDLs occurs, the level of plasma LDL elevates. Furthermore, various risk factors (including dyslipidemia, hyper-tension, obesity, smoking, diabetes, and abnormal glucose tolerance, etc.) stimulates endothelial cells resulting in endothelial damage. Compared with intact endothelium, NO production is deficient in impaired endothelial, which induces platelet aggregation, endothelial-leukocyte interactions and thrombosis. Moreover, damaged endothelium has increased permeability for lipid particles, which accelerates lipid deposition in the sub-intima. Damaged vascular endothelial cells could express VCAM-1, ICAM-1, MCP-1 and IP-10, which attract monocytes and lymphocytes, and leads to the consequential infiltration into the sub-intimal space. Simultaneously, SMCs derived from the arterial media layers also migrate into the sub-intimal space through the membrane pores in the internal elastic lamina. All of these accelerate the formation of foam cells and the process of atherosclerotic.
Understanding of functional role of lipoproteins in atherosclerosis has progressed in recent decades. In addition, new therapeutics have been developed and trialled targeting lipoproteins as treatment for atherosclerosis. Thus, a comprehensive review of lipoproteins’ function and their role in atherosclerosis, along with the latest development of lipoprotein targeted treatment, is timely. In this review, we summarise the different types of lipoproteins and their functions. We then outline the process of atherosclerosis development elucidating key links between lipoproteins and atherosclerosis. Lastly, we discuss the development of lipoprotein targeted treatment of atherosclerosis, including progress on novel delivery platforms for lipoprotein-based therapeutics. Together, this will provide insight to understanding new strategies for clinical management of atherosclerosis.
2. Apolipoprotein B (apoB)-containing lipoproteins in atherosclerosis
2.1 LDL
LDL particles are the main compartment storing serum lipids in the human body [10]. They are composed of free triacylglycerols, cholesterol, phospholipids, cholesteryl esters, and apoB [3], and act as the main transporters of cholesterol in human blood [3]. During normal metabolism, LDLs are removed from circulation via LDL receptors on the surface of hepatocytes [11]. However, when excessive secretion of lipoproteins by the liver and/or ineffective clearance of plasma LDL occurs, circulating levels of LDL rise [12]. Several studies have identified that raised plasma LDL levels results in the initiation and development of atherosclerotic plaques. This increases the risk of atherosclerosis-associated disease and contributes to the burden of cardiovascular disease [13-16]. Generally, a combination of VLDL, LDL, lipoprotein (a) and chylomicrons all contribute to the amount of cholesterol deposited in the arterial wall, and hence progression of atherogenesis. Of note, all of these particles contain apolipoprotein B (apoB). Overexpression of ARL15, a member of the Adenosine diphosphate-Ribosylation Factor (ARF) family, in the liver of mouse models has also been shown to lead to hypercholesterolemia via increasing apoB level. Hypercholesterolemia is a major risk factor contributing to atherosclerosis. Despite the fact that approximately 90% of apoB particles in circulation are resident in LDL particles [17], apoB is of increasing interest in atherosclerosis research, due to its ability to predict the atherogenic risk, which is more accurate than other markers such as LDL-C and HDL-C [18]. Mendelian randomized trials have revealed that the clinical benefits of cholesteryl ester transfer protein (CETP) inhibitors reflect the decrease in circulating LDL particles that are determined by apoB, rather than LDL-C [19, 20]. Another study showed that genetic variants mimicking LDL-C-lowering and triglyceride-lowering therapies play a role in decreasing atherosclerotic cardiovascular disease (ASCVD) risk for similar changes in apoB levels, despite the fact that plasma LDL-C and triglyceride levels showed different patterns of change [21]. These findings strongly suggest that ASCVD risk is correlated to the total apoB levels rather than lipid contents per se. As a result, the European Society of Cardiology/European Atherosclerosis Society 2019 guidelines for the management of dyslipidemia recommended measurement of apoB levels to estimate ASCVD risk and to assess the clinical benefits of using lipid-lowering therapy [22].
Aside from its role as a biomarker for diagnosis and prognosis of ASCVD risk, apoB may also have therapeutic potential for treatment of atherosclerosis. Lipid-lowering therapies (targeting LDL-cholesterol, HDL-cholesterol, total cholesterol, and triglycerides) are the current mainstream treatment paradigm for lowering ASCVD risk. Examples include strategies to upregulate LDL receptors, thus reducing LDL clearance and hence LDL-C, using agents such as ezetimibe, statins, and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors [11]. Such treatments are effective in many patients and can reduce major coronary event rates by ~30% [23]. However, because multiple pathological processes are in play in atherosclerosis, many patients still experience atherosclerosis complications despite successfully decreasing their cholesterol levels. Studies have shown that for some patients with elevated triglyceride levels and low LDL-C levels, therapy that targets management of apoB levels is a viable alternative. For example, John et al. demonstrated that antisense inhibition of apoB led to reductions of <50% apoB and <35% LDL-C levels in humans, suggesting targeting apoB as a potential new treatment strategy to reduce cardiovascular risk [24]. A recent study suggests that measurement of apoB should be included to guide the optimal treatment of patients [11]. ESC/EAS 2019 guidelines state that apoB analysis is recommended as secondary lipid analysis for risk evaluation, especially for patients who have high TG levels, diabetes mellitus, obesity, metabolic syndrome or very low LDL-C levels [22]. For patients at very-high, high and moderate CVD risk, the apoB level should be <65 mg/dL, <80 mg/dL and <100mg/dL respectively [25, 26]. It is also proposed that clinicians should consider the apoB lipoprotein lowering strategy to complement existing clinical practice for atherosclerosis treatment [11].
2.2 Triglyceride-rich lipoproteins
Multiple lines of evidence indicate that high levels of LDL and cholesterol contribute to atherosclerosis, whilst increased levels of HDL reduce the risk of developing atherosclerosis. However, there is no consensus on the atherogenic potential of elevated plasma triglycerides (TGs) and the triglyceride-rich lipoproteins (TRLs; including VLDL and chylomicrons) [27, 28].
TGs are transported in plasma by VLDLs, chylomicrons and their remnants created during metabolism [29]. Lipoprotein lipase (LPL) is a key tissue enzyme, expressed in heart, skeletal muscle and adipose tissue, that participates in the clearance of TRLs. LPL hydrolyzes TRLs in plasma, producing VLDL remnants (including chylomicron remnants and IDL) and high concentrations of lipolytic products such as oxidized free fatty acids [30]. Oxidized free fatty acids can increase expression of inflammatory cytokines and interleukins leading to endothelial inflammation [31-33]. There is some evidence that TRLs may be more atherogenic than LDL, and TRL cholesterol, rather than TGs, may directly promote atherosclerosis development [34, 35]. This may relate to larger volumes of TLR with chylomicrons (75-450 nm diameter) and VLDL (60-80 nm diameter) being the largest lipoprotein particles with greater capacity to carry more cholesterol than the smaller LDLs (18-25 nm diameter) [34].
TRLs and their remnants can upregulate the endothelial expression of ICAM-1 and VCAM-1 [36, 37], which facilitates endothelial monocyte adhesion and the transendothelial migration of leukocytes to the lesion site, leading to the exaggerated inflammatory responses [38]. They can also increase ROS production, resulting in cellular injury and death, and increase vascular endothelial permeability [33, 39]. Furthermore, TRLs and their remnants amplify the coagulation cascade by upregulating the expression of plasminogen activator inhibitor-1 and plasminogen activator inhibitor-1 antigen, while supporting the prothrombinase complex assembly, promoting platelet aggregation and thrombus formation [40]. TRL remnants can also accumulate on atheroprotective HDL particles [41], impairing their atheroprotective effect and impairing coronary vasodilation [42]. Taken together, TRLs and their remnants likely play key roles by multiple mechanisms to facilitate endothelial dysfunction thereby promoting atherogenesis.
2.3 A promising target: lipoprotein A
Lipoprotein a (Lp(a)), first discovered by Berg et al. (1963), is a circulating lipoprotein produced by the liver that is associated with atherosclerosis. Given the similarity of Lp(a) to LDL it may act in similar fashion to induce atherogenesis [43]. Lp(a) structure closely resembles a very large apo(a) protein linked via lysine pockets with apoB-100. Lp(a) promotes development of atherosclerosis by triggering endothelial dysfunction, inducing smooth muscle proliferation, and promoting macrophage foam cell formation [43]. A strong correlation has been reported between increased Lp(a) levels, particularly >50 mg/dL, and cardiovascular events including peripheral arterial disease, aortic stenosis, ischemic stroke, and myocardial infarction [44-48]. To date, no drugs targeting Lp(a) have been clinically approved. Statins have minimal effect on Lp(a) levels, and in fact Lp(a) levels increased in some patients. Similarly, nicotinic acid (niacin), estrogen, and PCSK9 inhibitors only reduce Lp(a) by small degrees (20% to 30%). With the estimated level required for significant reduction of Lp(a) being >50%, existing drugs fall to meet this threshold. There remains an opportunity to develop new drugs targeting Lp(a) that may meet this therapeutic threshold.
Despite increasing awareness of the importance of Lp(a), the measurement of Lp(a) still lacks standardization. Furthermore, specific mechanisms of action of Lp(a) in atherosclerosis remain elusive. Taken together, accumulating evidence indicates that Lp(a) could play a role as a biomarker in atherosclerosis diagnosis and may yet prove a novel therapeutic target.
3. Ox-LDL
3.1 The function of Ox-LDL in atherosclerosis
The natural course of atherosclerosis in both human and experimental animal models of hypercholesterolemia show that LDLs are highly susceptible to oxidative damage by oxygen radicals. LDL undergoes many changes in chemical composition after oxidation, including the generation of lipid peroxides and oxysterols, the degradation of apoB, and the transformation of LDL lipid components from phosphatidylcholine to lysophosphatidylcholine (lysoPC) [49, 50]. LysoPC, the lipid component of ox-LDL, is a significant intermediate product of LDL oxidation and the major active component of ox-LDL [51, 52]. LysoPC can enhance oxidative stress, induce inflammatory reactions, interfere with endothelial cell function and reduce plaque stability, possesses pro-atherosclerotic effect and participates in all stages of atherosclerosis. Under normal conditions, native LDL contains very low levels lysoPC with normal plasma levels being 12~166 μmol/L [53-55]. During oxidation of LDL, about 40% phosphatidylcholine can be transformed to lysoPC through two different pathways. The first and main route is activated secretory phospholipase A2 (sPLA2), an acute-phase protein, that can hydrolyze the fatty acid on the second carbon of LDL phosphatidylcholine, thereby making phosphatidyl-choline which transforms to lysoPC. Secondly, lecithin cholesterol acyltransferase (LCAT) can transfer fatty acid on the phosphatidylcholine, inducing related cholesterol and lysoPC formation. The emergence of oxidized LDL (ox-LDL) in atherosclerotic plaques serves as the starting point for the “oxidation hypothesis of atherosclerosis.” Taken together, ox-LDL is a collective term for heterogeneous oxidative changes in LDL lipid moieties [56].
High levels of ox-LDL are generally considered a high-risk factor for a cardiovascular events due to its central role in atherosclerotic plaque formation. Gao et al. (2017) reported that the incremental level of ox-LDL in the serum was correlated to the elevated risk of cardiovascular events in nested case-control studies, 10 case-cohort studies, and 11 prospective cohort studies on the relationship between ox-LDL and ASCVD [57]. Further studies have elucidated the role of ox-LDLs in the pathogenesis of atherosclerosis, especially their capability to promote inflammatory responses [49, 58, 59], inducing the loss of inherent antioxidant function in the body. For example, ox-LDLs trigger the activation of macrophages via Toll-like receptor-4 (TLR4) as well as accelerate reactive oxygen species (ROS) production and inflammatory cytokine oxidation [60].
Several studies have demonstrated that ox-LDLs can interact with multiple cell types (such as fibroblasts, SMCs, endothelial cells, macrophages and platelets,) and affect their normal physiological functions through various signalling pathways. For example, ox-LDLs can stimulate the abnormal proliferation, migration and collagen synthesis of vascular SMCs and fibroblasts via LOX-1, the receptor for ox-LDL, causing the fibrous hyperplastic pathological change of atherosclerotic arterial walls [61]. Furthermore, ox-LDL can stimulate endothelial cells to produce cytokines, including MCP-1, VCAM-1 and ICAM-1 and p-selectin. These cytokines can attract circulating monocytes in the blood to the damaged endothelium, which aggravates inflammatory cell infiltration of endothelial cells, further exacerbating endothelium damage. In normal physiological states, endothelium can take in L-arginine and produce a basal level of nitric oxide (NO) via a unique isoform of NO synthase (eNOS), catalyzing L-arginine and converting into L-citrulline and NO [62]. NO produced by endothelial cells can diffuse quickly via the endothelial plasma membrane to activate guanylate cyclase in several cell types present in the blood (such as platelets, leukocytes and SMCs). Activated guanylate cyclase in platelets can inhibit platelet activation, adhesion, and aggregation. Activated guanylate cyclase in leukocytes reduce their adhesion, and in SMCs can regulate vasorelaxation and dephosphorylation of the myosin light chain. Moreover, NO can also interact with hemoglobin in erythrocytes to enhance oxygen delivery to tissues [63]. However, ox-LDL can reduce the uptake of L-arginine by endothelial cells, thereby reducing the NO formation. Therefore, the vascular protective function of NO in injured endothelium is decreased to varying degrees or lost completely, which results in lipid deposition, inflammatory cell infiltration, platelet aggregation and thrombosis, accelerating the process of atherogenesis. Fei et al. showed that ox-LDL can induce NF-κB p65 phosphorylation and activate caspase 3, resulting in endothelial cell apoptosis [64]. Cao et al. showed that ox-LDL induces RAW264.7 macrophage-derived foam cell formation, promotes cell lipid accumulation, and induces a senescence phenotype with a reduced number of live cells [65].
Taken together, ox-LDLs interact with a variety of cells impacting normal physiological functions through multiple pathways, which promotes atherosclerosis development. As such, ox-LDLs are considered as key link in atherosclerotic plaque formation.
3.2 Novel direction for atherosclerosis diagnosis and treatment: targeting ox-LDL
Atherosclerotic plaques with high ox-LDL levels are at greater risk of rupture [66]. For this reason, ox-LDL may have potential as a marker of the “vulnerable plaque,” particularly relevant in targeted diagnostic imaging of atherosclerosis and in targeting delivery of therapeutic agents [56].
Coronary angiography visualizing radio-opaque contrast injected into coronary arteries under fluoroscopic is the most common technique to identify clinically significant plaque. However, angiography only identifies presence of plaque with no ability to assess vascular remodelling or plaque components [56]. A number of molecular probes have been developed to visualize ox-LDL in arteries [56]. IK17, the first human-derived single-chain variable fragment (scFv) antibody fragment with high specificity for oxidation-specific epitopes (OSEs) on ox-LDL, enhances imaging capability of atherosclerotic plaque. IK17 has hypoimmunogenic characteristics due to its small size, lack of fragment crystallizable (Fc) regions and as it is derived from human mononuclear mRNA antibody libraries rather than a murine source [67]. IK17 can be bonded with manganese and gadolinium in micelles to enhance the resolution of magnetic resonance imaging (MRI), resulting in high-quality imaging with specific uptake in atherosclerotic lesions in experimental animals [68]. Li et al. reported an alternative strategy with liposomes conjugated with LOX-1, an ox-LDL scavenger receptor, which are used to detect atherosclerotic lesions by single-photon emission computerized tomography (SPECT) and MRI [69].
Ox-LDL also has potential to target delivery of therapeutic nanoparticles to atherosclerotic lesions. There are few reports of targeted drug delivery to the atherosclerotic plaque, however none, to date, have directly targeted ox-LDL. Duivenvoorden et al. used HDL nanoparticles containing lipophilic simvastatin to target atherosclerotic lesions in apo E-knock-out mice. Their nanoparticles accumulated in atherosclerotic plaques, decreased lesion size on MRI, and reduced inflammation as measured in vivo by fluorescence molecular tomography with computed tomography (FMT-CT) and ex vivo by immunohistochemical analysis [70].
Despite some promise of targeting ox-LDL in preclinical studies, challenges to clinical translation remain, including identifying the most appropriate hybrid imaging targets, the safety and immunogenicity of molecular probes, and the selection of targeted drugs. There remains need for more studies.
4. HDL in atherosclerosis: A double-edged sword
4.1. HDL potentially inhibits the development of atherosclerosis
HDL is synthesized in the liver and small intestine and it formation entails production of key protein components of HDL such as apoA-I and apoA-II, acquisition of lipid and the assembly process. Although enterocytes and hepatocytes have been reported to produce apoA-I, the exact contribution of this source to overall plasma apoA-I in humans is unclear. ApoA-I synthesis by cells results in a lipid-poor form, necessitating the acquisition of free cholesterol and PLs via the ABCA1 pathway to form nascent HDL. Nascent HDL recruits more lipid from peripheral tissue and lipoproteins, which then produces cholesteryl ester produced via cholesterol acyltransferase, eventually leading to assembly of mature HDL. The liver also produces apoA-II, leading to the formation of HDL with both apoA-I and apoA-II [71].
Understanding the interactions between HDL and vascular cells has progressed over recent decades. HDL promotes endothelium and NO-dependent relaxation in wild-type but not SR-BI-knockout mice demonstrating that circulating HDL binds to the scavenger receptor BI expressed in endothelium, resulting in the simulation of eNOS [72, 73]. HDL-stimulated NO secretion may be regulated by the HDL-associated lysophospholipids sphingosylphosphorylcholine (SPC), sphingosine-1-phosphate (S1P), and lysosulfatide (LSF).
Anti-atherogenic properties of HDL particles are mainly facilitated by reverse cholesterol transport (RCT), a catabolic mechanism transferring cholesterol from peripheral tissues to the liver for excretion. Anti-inflammatory and antioxidant effects of HDL are essential for vascular protection [3]. Current clinical guidelines state that serum HDL level < 40 mg/dL are a risk for heart attack and stroke [51], whilst a healthy level for HDL is >60mg/dL, highlighting the positive role HDL plays in protection from atherosclerosis.
HDLs are highly heterogeneous resulting in various subtypes of HDL. Some sub-types of HDL demonstrate multiple antiatherogenic effects including transport of cholesterol from the arterial wall to the liver and anti-inflammatory, anti-infectious, antioxidative, anti-apoptotic, antithrombotic and vasodilatory actions [74]. However, the inherent heterogeneity of HDL results in variable results when reporting the impact of HDLs during atherosclerosis development. Johansson et al. reported that HDLs can be grouped into large (9.4 to14 nm), medium (8.2 to 9.4 nm) and small (7.3 to 8.2 nm) HDL particles but notes limitations of precision of measurement for each of these subpopulations [75]. They showed that large HDL particles (9.4 to14nm) are inversely related to coronary disease risk [75]. In contrast, other studies have shown that only the small diameter particles (7.3 to 8.2 nm) with disk-like or mature spherical HDLs can effectively remove cholesterol and enhance the antioxidant and anti-inflammatory functions whilst the larger-diameter HDLs are less effective [76, 77]. Further studies are needed to clarify the role of sub-types and different sized HDLs in the development of atherosclerosis. Despite these discrepancies, it is generally accepted that HDL particles have anti-atherogenic effects. Other beneficial effects include HDLs ability to reduce generation of endothelial adhesion molecules (Von Willebrand factor, and platelet-activating factor), and promote vasorelaxation and endothelium proliferation through stimulating endothelium to produce prostacyclin and nitric oxide (NO), thereby reducing inflammatory cell infiltration and maintaining stabilization of endothelial cells [78]. HDL can also inhibit the production of lipid hydroperoxides that play a major role in oxidizing phospho-lipids and cholesterol [79]. In addition, HDL contains several antioxidant enzymes, including paraoxonase (PON) or platelet-activating factor acetyl-hydrolase (PAF-AH). These enzymes can reduce the formation of ox-LDL, leading to the reduced deposition of ox-LDLs in vessel walls [80, 81]. Furthermore, the antioxidant activity of HDL promotes cholesterol efflux, which alleviates atherosclerosis progress [82].
Several studies have demonstrated that HDLs anti-atherogenic properties are strongly associated with its structural components, including apolipoprotein A-I (apoA-I), apolipoprotein J (apoJ), apolipoprotein E (apoE), PON, glutathione peroxidase, and PAF-AH. ApoA-I, a fundamental protein of HDL, exhibits multiple antioxidant functions. ApoA-I assists in the discharge of cholesterol from vascular macrophages and peripheral tissues via interacting with the ATP-binding cassette (ABC) A1 transporter (ABCA1) [83]. ApoA-I also collects and removes LDL lipid hydroperoxides and peroxides that could oxidize the phospholipids portion of LDLs, thus slowing down the progression of artherosclerosis by reducing ox-LDL [84-86]. ApoA-I can also bind with cholesteryl ester transfer protein (CETP) and trigger lecithin-cholesterol acetyltransferase (LCAT) to promote the RCT process to accelerate peripheral cholesterols back to the liver, thereby achieving its anti-atherosclerotic effects [87]. LCAT can also convert the nascent discoidal-shaped HDL into a mature spherical-shaped HDL particle.
Apolipoprotein A-II (apoA-II) is the second most abundant major apolipoprotein of HDL, but its specific function remains unclear. ApoA-II knock-in rabbits (without apoA-I) showed resistance to the development of atherosclerosis, when compared to wild-type rabbits (that have apoA-I only) demonstrating that apoA-II may inhibit progression of atherosclerosis. This may be related to apoA-II ability to increase plasma HDL-C and reduce triglycerides and atherogenic lipoproteins levels [88]. Results of this study suggests targeting apoA-II may be a new strategy for treatment of atherosclerosis.
ApoE is another key component of HDL exhibiting vascular protection. It has been reported as the most abundant protein in HDL isolated from atherosclerotic lesions [89], indicating an important role of apoE in atherosclerosis pathophysiology. Song et al. reported that, compared to normal controls, apoE knockout mice produce less HDL in the liver with significantly reduced expression and translation of RCT-related genes (ApoA-I and ABCA1), which may lead to the insufficient clearance of peripheral cholesterol, resulting in accelerated development of atherosclerosis [90]. Similarly, Kypreos et al. reported that apoE promotes HDL biogenesis by interacting with ABCA1, independently of apoA-I in mice [91]. When compared to HDL without apoE, apoE enriched HDL is active in size expansion and contraction and is cleared rapidly from the circulation [92]. HDL size expansion likely reflects cholesterol absorption, the primary lipid constituent of the HDL core. Conversely, HDL size contraction mainly results from selective cholesterol ester liver uptake through interacting with lipoprotein lipase (LPL) and hepatic lipase (HL) to generate prebeta-1 HDL as well as increased clearance rates from the circulation [92]. These pathways and key metabolic steps in RCT to protect against atherosclerosis, are not observed for HDL without apoE.
ApoJ, also known as clusterin (CLU), is a multifunctional protein. It is involved in a variety of physiological processes relevant to lipid transportation and vascular SMC differentiation, immune system regulation, oxidative stress, cell adhesion, apoptotic cell death, cell-cycle regulation and tissue remodelling [93]. Importantly, apoJ prevents the development of atherosclerosis. Like apoA-I and apoE, apoJ promotes RCT from peripheral tissues to the liver and accelerates phospholipid and cholesterol export from macrophage-foam cells, the hallmark cell type of atherosclerotic lesions [94, 95].
HDL surfaces have enzymes such as PAF-AH, LCAT [96], PON, and glutathione phospholipid peroxidase (GPX) [82], which all play significant roles in antioxidation. PAF-AH is a member of the lipoprotein-relevant phospholipase A2 family, and its activity is essential to the hydrolysis of bioactive lipids (e.g., PAF oxidized phospholipids and PAF) that are involved in the pathogenesis of atherosclerosis [97]. HDL-associated PAF-AH decreases the production of ox-LDL by decreasing LDL oxidation, thus slowing down the development of atherosclerosis [82]. Vasilis et al. found that HDL-associated PAF-AH activity in individuals with hypercholesterolemia was significantly increased compared with normolipidemic individuals. In normolipidemic individuals, PAF-AH is mainly related to apoB-containing lipoproteins (e.g., as VLDL, LDL, and IDL), with <20% present in HDL, but in hypercholesterolemia PAF-AH activity distribution between LDL and HDL is altered [98]. Gradient ultracentrifugation studies revealed that increased PAF-AH activity in hypercholesterolemia is because of the increasing level of plasma LDL and associated with each LDL subfraction, notably, small density LDL-5. LCAT also facilitates the metabolism of oxidatively modified phospholipids, especially those oxidatively modified phospholipids that generate during LDL oxidation, resulting in an enhanced anti-atherosclerotic effect. LCAT also plays a major role in maintaining normal HDL levels and structures. It catalyzes the transformation of prebeta HDL into mature alpha HDL, representing the majority of HDL components in the plasma [99, 100]. PON, a calcium-dependent enzyme of relevance to HDL [101], can also inhibit LDL oxidation and LDL-induced monocyte chemotactic activity to protect HDL against oxidation, resulting in the antiatherosclerotic effect [102]. Studies show that individuals with low PON activity are exposed to elevated oxidative stress [103], leading to the excess production of ROS that aggravates the atherosclerotic endothelial injury, ox-LDL formation, and lipid deposition, which promotes the atherosclerosis development process. PON can also stimulate the efflux of HDL-mediated macrophage cholesterol using the ABC A1 transporter to mediate atherosclerotic lesions [104]. Lastly, GPX inhibits hydroperoxides of phospholipids and cholesteryl esters associated with intact lipoproteins and efficiently eradicates free radicals in the body, protecting endothelium against oxidative damage and reducing lipid infiltration, thereby alleviating atherosclerosis pathological changes to some extent [105].
4.2. Dysfunctional HDL facilitates the development of atherosclerosis
It is traditionaly believed that the increasing levels of HDL could reduce the risk of developing atherosclerosis. New evidence suggests that the level of HDL and the risk of the developing atherosclerosis has a positive correlation, and that raising HDL levels can increase the risk of developing atherosclerosis. The 2006 ILLUMINATE clinical trial used Torcetrapib, a novel selective cholesteryl ester transfer protein (CETP) inhibitor, to improve HDL plasma levels in patients with ASCVD, and showed that the all-cause mortality increased with elevated HDL levels [106]. Navab et al. showed that elevated plasma HDL levels might contribute to aggressive development of atherosclerosis in animal models [80]. Other studies support the hypothesis that HDL may not always be anti-atherosclerotic [107, 108]. Thus, specific mechanisms of HDL require further study. Contradictary results noted above may relate to the newly discovered dysfunctional HDL that results from the alteration of structure and function secondary to oxidative modifications. In addition, heterogeneity of the HDL structure and components, including presence or not of proteins such as apoC-III, likely contributes to its variable function and effects on development of atherosclerosis.
4.2.1 Oxidative modification of HDL
A number of pathways produce dysfunctional HDL including copper oxidation of HDL. Copper-oxidized HDL stimulates ROS pathways to enhance inflammation, promote apoptosis of endothelial cells, and induce the oxidation of apoproteins [82, 109-111], all of which can increase the risk of developing atherosclerosis. Oxidative modifications of HDL occur via a variety of other enzymatic pathways. Several members of the matrix metalloproteinase (MMP) family can cleave apoA-I of HDL to disrupt cholesterol efflux from foam cells [112]. Myeloperoxidase (MPO) produced by activated phagocytes is another common enzyme found in atherosclerotic lesions [113]. MPO acts on HDL, reducing the anti-atherosclerosis properties of HDL. In contrast to copper oxidation of HDL, MPO likely oxidises HDL via hypochlorous acid (HOCl), but the exact mechanism requires clarification [114]. MPO-modified HDL inhibits cholesterol-efflux by disrupting HDL binding to the scavenger Receptor-BI (SR-BI) [115]. MPO also generates tyrosyl radicals that lead to lipid peroxidation and lipoprotein cross-linking [87], thereby reducing the RCT capacity of normal HDLs and promoting cholesterol deposition in the sub-intimal space [116]. MPO can also bind to the endothelium and directly consume NO produced by endothelial cells, impacting NO signalling and results in impaired endothelial function [87].
Other enzymes that alter HDL and disrupt cholesterol efflux include tryptase, chymase, endothelial lipase, and polymorphonuclear (PMN)-derived enzymes. Tryptase and chymase are both derived from mast cells and have similar mechanisms of action. Tryptase can hydrolyze apoA-I in HDL particles, thus impairing apoA-I-mediated cholesterol efflux from foam cells [87, 117]. Similarly, chymase degrades the apolipoproteins of HDL, resulting in the oxidation of HDL, which leads to the reduction of cholesterol efflux through ABC A1 transporter [118]. Endothelial lipase impairs cholesterol efflux by elevating non-esterified fatty acids and lysophosphatidylcholine [119]. Meanwhile, the elastase derived from PMN damages cholesterol-efflux by producing ROS species [120]. Acute-phase proteins, including serum amyloid A protein (SAA) and sPLA2, can also play a major role in the formation of dysfunctional HDL. SAA binds to HDL, causing impaired access of HDL to the plasma membrane, thereby decreasing cholesterol efflux [121]. SAA can also block HDL-relevant enzymes such as PON and PAF-AH, nullifying their ability to resist LDL oxidation [122]. sPLA2 hydrolyses HDL phospholipids, resulting in disrupted cholesterol efflux [123].
Patients with type 1 diabetes often have severe atherosclerosis despite the increased levels of HDL [124]. This may be related to increased glycation promoting ROS production, oxidation, and inhibition of NO system, causing the HDL structural alterations and functional disorders. Ferretti et al. examined the effect of incubating HDL under hyperglycaemic conditions on lipid composition and PON activity and showed that modification of the polarity of glycated HDL affects HDL-associated PON activity, which may contribute to the accelerated atherosclerosis progression in diabetic patients [125]. Hedrick et al. incubated human HDL (5 mg protein) with or without 25 mmol/l glucose in vitro and found that in vitro glycated HDL did not inhibit monocyte adhesion induced by ox-LDL to human endothelium and caused a 40% reduction in PON activity. They also found a 40% reduction in PON activity in patients with Type II (non-insulin-dependent) diabetes mellitus and atherosclerosis compared with non-diabetic subjects. Based on these results, they propose that dysfunctional glycated HDL could contribute to the accelerated development of atherosclerosis in Type II diabetes patients [126].
Taken together, multiple pathways can form dysfunctional HDL, but studies are limited to in vitro and animal studies. Thus, the significance of HDL modifications in the human health and disease remains unclear.
4.2.2 Certain intrinsic components of HDL may possess pro-atherogenic properties
Despite the generally accepted role of HDL in inhibiting or slowing atherosclerosis, some components of HDL may accelerate atherosclerosis. Apolipoprotein C-III (apoC-III) is an example as Allyson et al. (2018) have shown that, compared with HDL lacking apoC-III, HDL with apoC-III is associated with a higher risk of CVD. HDL containing apoE generally protects against cardiovascular risk, but apoC-III in HDL negates the beneficial effect of apoE on HDL metabolism and relation to cardiovascular disease [92].
5. Cutting-edge therapeutic approaches that target lipoprotein metabolism
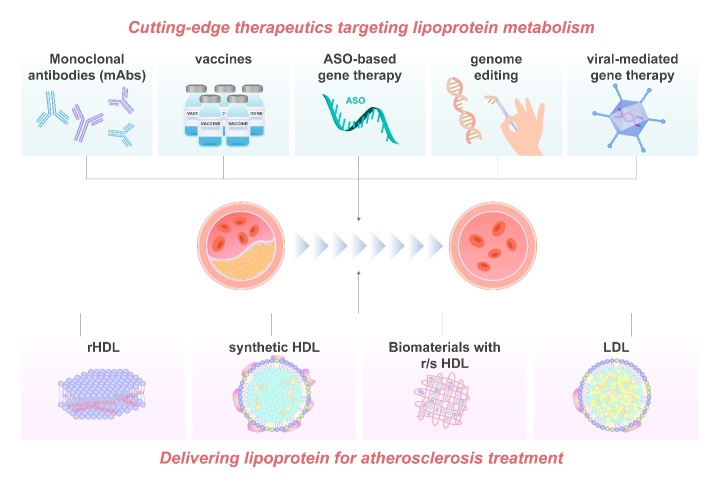
In order to improve efficacy and safety and to achieve more precise and targeted delivery of existing treatments, interest is growing in new strategies targetting lipoprotein metabolism. A number of lipid-lowering therapies have FDA approval and are in routine clinical practice with other promising agents in pre-clinical or clinical trials [127]. Figure 2 and Table 1 summarize cutting-edge therapies and delivery strategies targeting lipoprotein metabolism to treat atherosclerosis.
Figure 2.
Summary of targeting and delivering therapies on atherosclerosis treatment. To resolve the limitations in the efficacy and safety of existing treatment methods of atherosclerosis, biological drugs with improved targeting are currently being explored. One of the most promising directions is to target lipoprotein metabolism. Monoclonal antibodies (mAbs), vaccines, antisense oligonucleotide (ASO)-based gene therapy, genome/base editing technologies and viral-mediated gene therapy are all cutting-edge therapeutic approaches that target lipoprotein metabolism. Another advanced therapy strategy is to delivery natural or synthetic lipoproteins for the treatment of atherosclerosis. Reconstituted (r) HDL has been widely accepted as an ideal drug delivery vehicle, because of their nano-size, unique cellular uptake mechanism via a non-endocytic pathway. Synthetic HDL (sHDL), using a nanoparticle template to tailor the structure and the chemical composition of the HDLs, is featured with improved size, shape and surface chemistry and with less batch-to-batch variation. Biomaterials combined with r/s HDL may have enhanced therapeutic efficacy. LDL could be applied as a vesicle to delivery targeted therapeutic drugs.
Table 1.
Cutting-edge therapeutic approaches that target lipoprotein metabolism.
| Category | Strategy | Target | Method | Models | Therapeutic effect | Refs. |
|---|---|---|---|---|---|---|
| mAbs | PCKS9 | PCKS9 silencing | In vitro and apoliporotein E knockout mice | (1) proinflammatory cytokine downregulation (2) TLR4/NF-ĸβ inhibition |
[129] | |
| Alirocumab | APOE*3Leiden.CETP mice. | (1) decreasing the lipid component of non-culprit plaques (2) stabilize plaque |
[130, 132] | |||
| Alirocumab | Clinical trial | (1) reduced mortality (2) reduced risk of stroke and myocardial infarction (MI) |
[131] | |||
| Bocociziumab | Parallel and randomized clinical trials | (1) reduced the LDL levels in most patients with hyperlipidemia at 3 months | [133] | |||
| Evolocumab | Clinical trials | (1) reduce the cholesterol levels by an average of 0.7mmol/l (2) reduce the risk of cardiovascular events |
[135] | |||
| ANGPTL3 | Evinacumab | Phase 2 clinical trial | (1) 49% reduction in LDL-C (2) <80% reduction in triglycerides |
[143] | ||
| Evinacumab | Clinical trial | (1) benefit for patients with LDL receptor mutations (2) 34% reduction in LDL-C of patients with biallelic null LDL receptor mutations |
[144] | |||
| Vaccine | Cholesterol lowering | PCKS9 | Inclisiran | Phase III clinical trial | (1) inhibition of PCKS9 (2) 50% reduction in LDL-C (3) injection-site adverse events |
[155, 156] |
| Peptide based AT04A | APOE*3Leiden.CETP mice | (1) reduction in plasma lipids (2) decreased inflammatory response (3) diminished atherosclerotic lesions |
[157] | |||
| ApoC3 | ISIS 304801 (Antisense DNA) | Clinical trial | (1) decrease in triglyceride levels | [158] | ||
| VLPs | Mice | (1) reduction in plasma lipid level | [159] | |||
| CETP | Rabbit | (1) 24% reduction in LDL-C (2) 39.6% reduction of atherosclerotic lesions |
[160] | |||
| CETi-1 | Phase I clinical trial | (1) insignificant reduction in HDL | [161] | |||
| Antigen-inducing | HSP65 | Lactococcus lactis | LDL receptor deficient mice | (1) upregulation of IL10 (2) downregulation of IFN-γ (3) atheroprotection |
[163] | |
| HSP60 | Porphyromonas gingivalis | Hyperlipidaemia (Apoeshl) mice | (1) increase in IL-10 (2) reduction in CRP, MCP-1. Ox-LDL (3) inhibition in atherosclerotic lesion formation |
[164] | ||
| Ox-LDL | Hypercholesterolemia rabbits | (1) reduction in atherosclerotic lesion size (2) increase in ox-LDL antibodies |
[152] | |||
| LDL ox-LDL |
Hypercholesterolemia rabbits | (1) ox-LDL antibodies increase in both LDL and ox-LDL immunized rabbits (2) 74% reduction in atherosclerotic lesions in LDL immunized rabbit (3) 48% reduction in lesions in ox-LDL immunized rabbit |
[153] | |||
| ox-LDL LDL |
Hypercholesterolemia rabbits | (1) 58% reduction in the neointial area in ox-LDL immunized rabbit (2) 19% reduction in the neointimal area in LDL immunized rabbit (3) reduced T cells and ox-LDL in ox-LDL immunized rabbit |
[165] | |||
| MDA-LDL | Apo-E-deficient mice | (1) upregulation of MDA-LDL antibodies (2) reduced lesion size at the aortic sinus |
[166] | |||
| ApoB-100 | P210 | ApoE-Null Mice | (1) 60% reduction in atherosclerotic lesion (2) increase in collagen content of subvalvular lesions |
[168] | ||
| P45, P74 | ApoE deficient mice | (1) P45 reduced the atherosclerosis by 48% and reduced the macrophage in lesion by 33% (2) P74 decrease the lesion by 3% and macrophage content by 39% |
[170] | |||
| Multitarget | Apob-100 HSP60 |
P45 and Chylamydophia pneumonia | Ldlr-/-mice | (1) reducing lesion size wihouth Cpn infection (2) downregulation of cellular infiltration, and inflammatory cytokine/chemokine section |
[172] | |
| Gene-therapy | ASO based | ApoB mRNA | Mipomersen | Clinical trials | (1) 24.7% reduction in LDL-C (2) adverse effects: flu like side effect, liver steatosis, injection site reaction |
[173] |
| Apo(a) mRNA | IONIS-APO(a)-LRX | Clinical trials | (1) 71.6% reduction in Lp(a) level | [178] | ||
| AKCEA-APO(a)-LRx (TQJ230) | Clinical trial Phase III | 80% reduction in Lp(a) level | [179] | |||
| ApoC3 mRNA | Volanesorsen | Phase III clinical trial | 77% decrease in triglycerides | [180] | ||
| ANGPTL3 | IONIS-ANGPTL3-LRX | Phase II clinical trial | (1) 33.2-63.1% reduction in triglycerides (2) 1.3-32.9% reduction in LDL-C (3) 27.9-60% reduction in VLDL-C |
[181] | ||
| Viral mediated | LPL | Glybera (AAV1) | Clinical trial | (1) reduced pancreatitis events (2) decreased acute abdominal pain events associated with panceratitis (3) discontinued |
[185] | |
| LDLR | AAV8 | Humanized mouse models of familial hypercholesterolemia | Significant reduction in LDL-C level | [188] | ||
| Humanized mouse model of familial hypercholesterolemia | (1) reduction in plasma cholesterol and non-HD-C level (2) 87% reduction in lesions after 3 months (3) significant remodelling of lesion |
[187] | ||||
| Phase I clinical trial | (1) limited toxicity and no signification upregulation of pro-inflammatory cytokines | [189] | ||||
| ApoA-I | HD-Ad | Apo E-deficient mice | (1) upregulation of APOA-I expression and HDL-C (2) reduction in lesion size |
[191] | ||
| Rabbit | (1) 70% reduction in plasm cholesterol (2) 208% reduction in VACM-1 expression (3) 30% reduction in macrophage content (4) reduction in lesion size, lipid content and ICAM-1 expression |
[192] | ||||
| Hyperlipidemic rabbits | (1) apoA-I mRNA expression (2) reduction in lesion size, lipid/macrophage content (3) downregulation of adhesion molecule expression |
[193] | ||||
| Hyperlipidemic rabbits | (1) 30% reduction in intimal lesion volume (2) 23-32% reduction in intimal lipid, macrophage and SMCs contents (3) 36% reduction in VACM-1 expression (4) downregulation of ICAM-1, MCP-1 and TNF-α |
[194] | ||||
| Genome/base editing | LD-R | AAV-8 mediated CRISPER/Cas 9 | Adult mice | (1) development of hypercholesterolemia adds atherosclerosis | [201, 202] | |
| PCKS9 | S. pyogenes Cas9 in adenoviral vector | Mice | (1) decrease in PCSK9 level (2) increase in hepatic LDL receptor level (3) 35-40% reduction in serum cholesterol levels |
[203] | ||
| aureus Cas9 in AAV | Mice | (1) over 40% gene modification (2) reduction in PCSK9 and cholesterol levels |
[204, 205] | |||
| Streptococcus pyogenes Cas9 | Mice | reduced peptides, decreased indels and no chromosomal translocation in addition to reduced TC levels | [203] | |||
| ANGPTL3 | Mice | (1) 56% reduction in triglycerides (2) a 51% decrease in LDL-C |
[207] |
5.1. Monoclonal antibodies (mAbs)
Monoclonal antibodies (mAbs), targeting PCSK9, angiopoietin-like protein 3(ANGPTL3), angiopoietin-like protein 4(ANGPTL4), ApoC3, and ApoB-100 peptides, are the dominant lipid-lowering medications in current pre-clinical and clinical research.
The most popular of these targets, PCSK9, is produced by the liver and targets the LDL-receptor (LDLR) on the surface of hepatocytes, resulting in the inhibition of LDL clearance and increased LDL levels. When PCSK9 is inhibited, LDLs recycle to the cell surface, with improved clearance from circulation. Therefore, loss-of-function mutations of PCSK9 have relevance to decreased LDL levels and reduced CHD risk [128]. PCSK9 inhibitors also regulate inflammatory responses by downregulating the expression of pro-inflammatory cytokines. In particular, the TLR4/NF-ĸB pathway is associated with PCSK9 induced pro-inflammatory cytokines such as IL-6, IL-1, TNF-α, IFN-γ and MCP-1 [129]. PCSK9 mABs have also been demonstrated to stabilize plaque via decreasing the lipid component of non-culprit plaques [130-132]. Current clinically available PCSK9 inhibitors include bococizumab, evolocumab, alirocumab, and LY3015014 (LY) [131], which all mediate LDL levels and prevent or slow the development of ASCHD and other CVDs. Bocociziumab has been shown in six parallel randomized control trials to significantly reduce LDL levels in most patients with hyperlipidemia at 3 months [133]. Both bococizumab and alirocumab showed improved reduction of Lp(a) compared with statins [121, 134]. Evolocumab reduced cholesterol levels by an average of 0.7mmol/l, significantly reducing cardiovascular event rates with median follow-up of 2.2 years [135]. Several clinical trials of evolocumab or alirocumab administered to patients with recent acute coronary syndrome (ACS) or stable ASCVD and receiving maximum tolerated statin therapy showed reduced risk of stroke and myocardial infarction (MI) [136, 137]. Taken together, PCSK9 inhibitors are recommended as additional or alternative therapy in patients with complete statin intolerance ASCVD and familial hypercholesterolemia (FH) with persistent hypercholesterolemia [138-140].
ANGPTL3 was demonstrated as playing a key role in lipid metabolism by studies in a group of strain KK obese mice, where ANGPTL3 was associated with hyperinsulinemia and hyperglycemia [141]. ANGPTL3 gene plays an important role in modulating TC, LDL, HDL levels by inhibiting lipoprotein lipase (LPL) and endothelial lipase (EL) activities via its coiled-coil region [142]. In phase 2 clinical trials, evinacumab, an ANGPTL3 inhibitor, reduced LDL-C by 49% and decreased triglycerides up to 80% [143]. Evinacumab is particularly beneficial for patients with LDL receptor mutations, as its effects to reduce LDL-C are independent of LDL receptors as demonstrated by a 34% reduction in LDL-C of patients with biallelic null LDL receptor mutations [144]. Thus, evinacumab is suitable for patients with severe heterozygous familial hypercholesterolemia.
ANGPTL4, an endogenous inhibitor of LPL, can modulate LDL, HDL, and reduce the risk of coronary atherosclerosis. Interestingly, ANGPTL4 glycoprotein shares 31% of the same amino acid sequence with ANGPTL3, and both genes have an identical modular structure [145]. However, the transcriptional regulation of the two genes is different. ANGPTL3 is regulated by LXRs and HNF1α [146]; meanwhile, ANGPTL4 is regulated by feeding and fasting [147]. That being said, both genes inhibit LPL activity and increase TG levels. However, the specific role of ANGPTL4 in atherosclerosis progression is controversial. Aryal et al. reported that the inhibition of ANGPTL4 in haematopoetic cells can improve monocyte expansion and promote foam cell formation via CD36 upregulation and ABCA1 localization reduction, resulting in the progression of atherosclerosis [148]. Similarly, ANGPTL4 reduces the inflammatory responses and decreases the number of immune cells (monocytes and macrophages) accumulating in the atherosclerotic plaque in ANGPTL4 TG E3L mice, indicating the upregulation of ANGPTL4 expression can prevent or slow the progression of atherosclerosis [149]. In contrast, Adachi et al. found that the inhibition of ANGPTL4 enhanced lipid metabolism and reduced foam cell formation, resulting in the protection against atherosclerosis in ApoE-/- ANGPTL4-/- mice [150]. Nevertheless, evidence indicates that ANGPTL4 does play a vital in atherosclerosis development, but the mechanism requires clarification. There are no clinical drugs targeting ANGPTL4 to date, but it may offer potential as a target in future.
Taken together, mAbs based drugs offer clinical utility due to their ease of administration, therapeutic efficacy and synergy in working with statins. However, certain limitations of mAbs therapies impede further downstream commercialisation. As an example, the PCSK9i bococizumab was suspended in 2016 due to unsatisfactory safety and efficacy in phase III trials. In addition, mAb therapies such as PCSK9i have issues with affordability and availability.
5.2. Vaccine
Atherosclerosis can be considered a chronic inflammatory condition due to the involvement of monocytes, macrophages and T lymphocytes in atherosclerotic plaque formation. Vaccines against specific antigens effectively target the immune response in a number of autoimmune diseases including atherosclerosis [151]. Palinski et al. (1995) first demonstrated the administration of malondialdehyde (MDA)-modified lysine effectively generated high titers of antibodies resulting in reduced atherosclerotic burden [152]. Ameli et al. showed antibodies against LDL and ox-LDL decreased atherosclerotic lesions by 74% and 48%, respectively in a rabbit model [153]. Since those early reports, increasing numbers of studies have shown vaccination against a number of targets, including cholesterol, active immunization against plaque antigens and multitarget strategies, can effectively treat atherosclerosis [154].
As seen with mAb therapy, a key target for immunization is PCSK9. Inclisiran, a siRNA-based drug to inhibit the expression of PCSK9, has shown efficacy in phase III trials that enrolled over 3000 patients with ASCVD and 482 patients with familial hypercholesterolemia [155, 156]. Other vaccines, including a peptide-based vaccine and AT04A, targeting PCSK9 have shown promise in preclinical animal models. Another target for lowering cholesterol is apolipoprotein CIII (apoC3) [157]. Antisense DNA that targets apoC3 successfully decreased triglyceride levels (TG) in patients with hypertriglyceridemia [158]. A virus like particle-based vaccination strategy targeting apoC3 has shown promise in reducing TG levels in mice [159]. Vaccine-induced CETP inhibition has been shown to reduce aortic lesions in a rabbit model [160]. However, phase I clinical trials of the CETP vaccine did not lower HDL levels as expected [161].
As plaque-associated antigen-induced immunogenic responses play a vital role in atherogenesis, autoantigens could be targeted to prevent atherosclerosis. Heat-Shock proteins (HSPs) are a popular target due to their role in inhibiting the denaturation or loss of function of proteins when cells are under stress. HSP60 expression increases in endothelial cells when atherosclerotic risk factors are present [162]. Oral immunization against HSP65 was developed to downregulate expression of HSP65 leading to upregulation of IL-10 [163]. A vaccine against HSP 60 was atheroprotective in spontaneously hyperlipidemic (Apoeshl) mice [164]. Further HSP based immunization targets are being developed with LDL, oxLDL and apoB based vaccines being tested preclinically. A vaccine against oxLDL administered to hypercholesterolemic rabbits reduced atherosclerotic lesions associated with upregulation of ox-LDL antibodies [152]. LDL based vaccines also achieved atheroprotection in rabbits and mice [153, 165, 166]. Identifying immunogenic epitopes is essential to effective vaccination. Comparison of apoB based peptides to human apoB-100 identified 102 different apoB like peptides that could be a target for immunization [167]. Numerous other studies have targeted immunization against peptides such as native p143, p210 [168], p2 [169] and MD-modified p45 and p47 [170].
Multitarget strategies use more than one vaccine simultaneously, either targeting a single pathogen through multiple serotypes or to target multiple pathogens [171]. As an example, Lu et al. used a mixture of apoB (p45), HSP60, and Chylamydophia pneumonia as a multitarget vaccine in Ldlr-/-mice. This promoted a significant Treg response resulting in improved atheroprotection compared to a single vaccine [172].
Overall, vaccines raised to atherogenic-related antigens exhibit unique advantages, but further studies are required to focus on durability of immunization, efficacy, safety and side effects.
5.3 Gene-based therapy
The recent success in mRNA-based vaccine strategies for COVID-19 shines a light on the potential of gene-based therapies. Through downregulation or upregulation of specific gene expression, such therapies may present a new paradigm for treatment of atherosclerosis.
5.3.1 Antisense oligonucleotide (ASO)-based gene therapy
Synthetic single-stranded DNA or RNA oligonucleotides combined with a specific complementary mRNA species have been applied to promote degradation of the specific complementary mRNA (ribonuclease H1-dependent class) or to disrupt its translation or splicing (steric-blocker class). This has been trialled for ASOs targeting apoB, apoC3, ANGPTL3, Lp(a), and PCSK9.
Mipomersen, the first FDA (2013) cardiovascular ASO drug to be approved by, targets the coding region of the apoB mRNA and reduces LDL levels in patient’s intolerant of statin therapy and at high risk of CVD, and in homozygous/heterozygous FH patients with pre-existing CHD [173-175]. In a Phase III clinical trial, 26-week treatment with mipomersen demonstrated a 24.7% decrease in LDL-C level (NCT00607373). However, severe adverse effects including flu-like symptoms, increased risk of liver steatosis and injection site reaction resulted in mipomersen being withdrawn from the market in 2019 [176-177].
Another ASO based drug, IONIS-APO(a)-LRX, targets Apo(a) mRNA resulting in cleavage and inhibition of Lp(a). Given the absence of other clinically approved therapies that lower Lp(a), this new drug shows promise in reducing Lp(a) levels and preventing the development of atherosclerosis. Weekly injection of 300mg IONIS-APO(a)-LRX, reduced Lp(a) levels by 71.6% [178]. A second-generation ASO targeting Lp(a), AKCEA-APO(a)-LRx, also named TQJ230, demonstrates high efficacy and specificity to reduce Lp(a) levels [179]. Weekly administration (20 mg) reduced Lp(a) levels 80% with improved therapeutic effect. This drug is now in Phase III clinical trial.
Volanesorsen targets mRNA for apoC, the lipoprotein that inhibits LPL, removes hepatic TCL, and contributes to hypertriglyceridemia. In a Phase 3 trial, weekly injections of 300 mg Volanesoren reduced triglycerides by 77% without notable side effects [180].
IONIS-ANGPTL3-LRX, an ASO targeting the ANGPTL3 gene, in Phase I clinical trial showed significant reduction in triglycerides (33.2-63.1%), LCL-C (1.3-32.9%) and VLDL-C levels (27.9-60%) [181]. The drug has progressed to Phase II trial.
A significant challenge for ASOs is optimizing precise targeted delivery. Prakash et al. proposed conjugating ASOs to N-acetyl galactosamine (GalNAc), a high-affinity ligand for the hepatocyte-specific asialoglycoprotein receptor, which enhanced delivery to hepatocytes by 10-fold [182]. A large number of other conjugated moieties are also being explored [183].
5.3.2 Viral-mediated gene therapy
Aside from ASOs reviewed above, viral mediated gene therapies, delivering DNA coded to interfere with transcription in order to compensate for abnormal genes and improve the expression of beneficial proteins, have also been developed for treatment of atherosclesis [184]. Adeno-associated viruses (AAVs), the most common viral vectors, are highly effective for transfection and can transduce both dividing and non-dividing somatic cells. Their simple structures and good safety profiles make them ideal vehicles for gene-based therapies.
Glybera®, the first gene therapy product targeting atheroscletosis, is an AAV1 vector carrying an intact copy of LPL aimed at reversing the severe hyper-triglyceridemia-causing LPL deficiency [185]. However, it was discontinued two years later on financial grounds [186]. A recombinant AAV8 vector containing a mouse or human LDLR transgene given to mouse models of FH resulted in stable dose-dependent reduction in non-HDL-c and TC, with decreased inflammatory cell infiltration and atherosclerotic plaque formation, and favourable plaque remodelling [187-189]. The vector is well tolerated when delivered at clinically relevant doses to mouse and rhesus macaque [189, 190] and it is now undergoing early clinical trial for efficacy and safety (NCT02651675).
Helper-dependent adenoviral vectors (HDAd) lack all viral coding sequences, and hence overcome the disadvantage of the high immunogenicity of other vectors. HDAd vector expressing apoA1, the primary protein of HDL, given to rabbits and mice results in significant reduction of atherosclerotic lesions with negative hepatotoxicity [191-194].
Despite progress in viral-mediated gene therapy, challenges remain. These include dominant mutations, unintended effects on neighbouring genes, risk of insertional mutagenesis, the size limitation of viral vectors and low efficacy of removing targeted genetic material [195]. Although the molecular targets overlap with other strategies, technical advantages and safety profile of viral-mediated methods can have benefits over other strategies for some targets [196]. There is also growing interest in the therapeutic potential of apolipoprotein mimetic peptides [197, 198].
5.3.3 Genome/base editing technologies
Whereas viral-mediated gene therapy is based on a gene replacement principle, genome/base editing aims to modify DNA segments, including insertion, deletion, or replacement, in order to achieve permanent targeted DNA modifications [199]. The most extensively used tool in atherosclerosis is the CRISPR (clustered regularly interspaced short palindromic repeats)/Cas9 system to target genes such as PCSK9, ANGPTL3, apoB, and LDLR.
Genome editing is often categorised as germline or somatic gene editing. Germline editing, used in the embryonic phase resulting in the gene alteration to the offspring, has some ethical concerns as highlighted by the recent report of genetically edited girls for HIV immunization [200]. In contrast, somatic gene editing is restricted to the adult organism without transfer into the next generation.
Jarrett et al. was the first to apply this technology to atherosclerosis, using AAV8-mediated CRISPR/Cas 9 to disrupt the LD-R gene in adult mice, resulting in the development of hypercholesterolemia and atherosclerosis [201,202]. Subsequently others have investigated the potential of gene editing for treatment of atherosclerosis. Inhibition of PCKS9 in mice using S. pyogenes Cas9 in AAV and aureus Cas9 in AAV resulted in a 90% reduction of PCKS9 associated with reduced cholesterol levels and limited off-target effects [203-205]. Carreras et al. showed that targeted editing of PCSK9 in the humanized mouse model induced liver-specific expression of human PCSK9 and decreased both protein and plasma total cholesterol (TC) levels resulting in a human-like hypercholesterolemia phenotype [206]. In the same model, PCSK9 base editing reduced peptides, decreased internal deletions (indels) with no chromosomal translocation and further reduced TC levels compared to genome editing, indicating that base editing may be safer and a more precise method [206]. In principle, base editing of PCSK9 avoids double-strand DNA breaks, reduces the chance of off-targeting indels and enhances on-target indels. Base editing to disrupt ANGPTL3 gene using CRISPR-Cas 9 resulted in a 56% reduction in triglycerides and a 51% decrease in LDL-C [207].
Taken together, genome/base editing technologies show potential for treatment of ASCVD. However, issues to be addressed prior to clinical translation include off-target activity, the large size of Cas, insufficient indel and homology direct repair efficiency and immune responses [208]
6. Advancements in strategies for delivering lipoproteins
6.1 HDL
6.1.1 rHDL
Recombinase HDLs (rHDL) are the discoidal HDLs resulting from the bond between apoA-1 and phospholipids and consequential self-assembly. They incorporate a hydrophobic core, due to lipid bilayer formation from the hydrophilic part of the amphiphilic apoA-1 α-helices, and an aqueous tail, due to the hydrophilic portions of the amphiphilic apoA-1 α-helices. rHDL is often produced through dialysis-based synthesis where apoA-1, phospholipids and sodium cholate or other detergent are placed together, resulting in the self-assembly [209]. An alternative approach is sonication of apoA-1 with phospholipids, followed by centrifugation [210]. A recently developed microfluidic system has also been employed to synthesize rHDL in a high throughput manner, where phospholipid and a hydrophobic payload are deposited into an apoA-1 buffer, resulting in suspension formation of a phospholipid, which is then homogenized through a microfluidizer high-shear processor [211].
Direct injection of rHDL can reduce inflammation and the development of atherosclerosis in preclinical models. A recent clinical trial demonstrated a 4.2% reduction in atheroma volume 5 weeks after intravenous injection of the rHDL Apo A1Milano [212]. In patients with acute coronary syndrome, although atheroma volumes were not significantly reduced 5 weeks after infusion of rHDLs compared to placebo, there were improvements in plaque characterization and coronary scores [213]. Shaw et al. showed that rHDL injection reduces expression of inflammatory markers such as TNFα and CD11bm and reduced lipid accumulation in atherosclerotic lesions [214]. Taken together, rHDL shows therapeutic potential as a treatment for atherosclerosis.
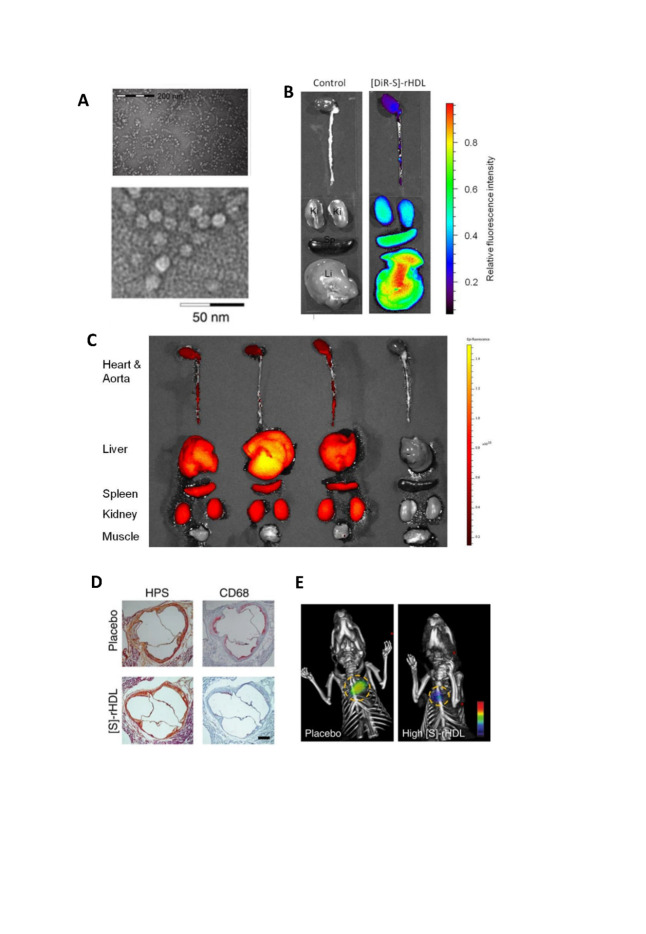
rHDL is widely accepted as a drug delivery vehicle due to its nano-size and unique cellular uptake mechanism via a non-endocytic pathway which results in improved therapeutic effect [215,216]. Furthermore, the hydrophobic core of lipoproteins can be loaded with hydrophobic drugs which are estimated to represent 40% of new therapeutic agents [217]. Simuvastatin loaded rHDL ([S]-rHDL) is a novel therapeutic for atherosclerosis [70] (Fig. 3). Statins have commonly been used to reduce LDL-cholesterol levels, but their effect is often limited to the liver. By incorporating HDL nanoparticles, the statin can penetrate the atherosclerotic plaque even when injected intravenously. Within a week of high dose [S]-rHDL, significant reductions in plaque area are observed, along with reduced number of positive macrophages. Rather than inhibiting monocyte recruitment, [S]-rHDL inhibits macrophages proliferation, together with suppression of inflammation within local macrophages. Combination treatment with [S]-rHDL injection and oral statin shows added benefit over either treatment alone [218].
Figure 3.
The strutural features of reconstituted high-density lipoprotein (rHDL) that promote targeted treatment. (A) Negative staining TEM image showed the typical disk-like morphology of rHDL. (B) Mice were intravenously injected with [DiR-S]-rHDL nanoparticles [rHDL fabricated with stain], and organs were imaged with NIRF 24 hours after the injection. Liver has the highest retention of DiR, followed by spleen, and kidney has the lowest retention. (C) Three mice were intravenously injected with [DiR-S]-rHDL (left three) and one control mouse was not injected (on the right). Organs were imaged with NIRF 24 hours after the injection. While heart, aorta, liver, spleen, and kidney tissue all took up nanoparticles, muscle tissue did not. (D)Typical histology images of the aortic sinus area from a mouse in the placebo group and a mouse in the high-dose [S]-rHDL group show that the mean plaque area is similar, while the plaque macro-phage content is notably smaller in the [S]-rHDL group. (E) FMT-CT molecular im-aging of protease activity revealed that high-dose [S]-rHDL treatment significantly reduced the inflammation levels in the aortic roots of live apoE-KO mice with advanced atherosclerosis as compared with placebo. The yellow circles indicate the aortic root area. All figures were cited from reference [70].
Challenges remain for this treatment strategy, including attaining sufficient Apo AL donor levels, the labor-intensive isolation process and some degree of insufficiency of the intravenous infusion delivery approach [219].
6.1.2 Biomaterials and synthetic HDLs
Advances are being made by using new biomaterials in the fabrication process for rHDL to improve efficacy. Hyaluronic acid (HA) has been used to encapsulate rHDL in an attempt to reduce undesirable accumulation within the liver and improve delivery to the plaque [220]. HA can reduce binding between rHDL and the SR-BI in the liver, and promote precise targeting of CD44 in plaques. HA-LT (lovastatin)-rHDL accumulates in the plaque at twice the rate compared to LT-rHDL not encapsulated with HA. Furthermore, the HA-LT-rHDL treatment group exhibited minimal macrophage activation and matrix metalloproteinase expression along with reduced atherosclerotic lesion size.
Synthetic HDL (sHDL), also known as a spherical HDL biomimetic, uses a nanoparticle template to tailor the structure and the chemical composition of HDLs, resulting in an improved consistency in size, shape and surface chemistry with less batch-to-batch variation [219]. Thaxton et al. developed sHDLs using gold nanoparticles as the core (HDL-AuNPs), similar to rHDL [221]. HDL-AuNPs bind well to cholesterol (Kd=3.8nM), which is comparable to cholesterol acceptors such as serum-derived apoA-1 and rHDL. Zhang et al. synthesized an sHDL named florescent nanocarriers (FCNs) [222]. FCNs contain DMPC, cholesterol oleate, drug, fluorescent dye and DiR-BOA. Similar to rHDL, the hydrophobic core of FCNs effectively load Dir-BOA. FCNs can bypass endosomal sequestration, due to the SR-B1 uptake. Epidermal growth factor receptor (EGFR) has also been conjugated to FCNs, allowing the EGFR-mediated endocytosis with an extended half-life (13.6 h) and targeted delivery [223].
PLGA is another material used as a nanoparticle template for sHDL synthesis. An advanced sHDL consisting of a PLGA core, a lipid bilayer structure, and HA (PLGA-HDL-HA NPs) have been developed to encapsulate simvastatin resulting in a slow-release profile [224]. Incorporating HA reduced binding to the liver, and the lipid bilayer facilitated removal of cholesterol from macrophages. In the atherosclerotic New Zealand rabbit model, sHDLs accumulated within plaque via the CD44 pathway, rather than via the liver, and were taken up by macrophages via SR-BI mediated endocytosis, resulting in improved efficacy to prevent the development of atherosclerosis. Similarly, atorvastatin (AT), has been loaded into PLAG-HDL-HA NPs with dextran sulphate to increase delivery efficiency. This enhanced cholesterol efflux and inhibited the ox-LDL take up of macrophages [225]. Further development of PLGA-HDL-HA NPs drug by incorporating apoA-1 and HA-DOPE can target macrophage and ECs sequentially. AT and lectin-like ox LDL receptor-1 small interfering ribonucleic acid were loaded into the NPs, increasing therapeutic effect [216].
Another dual-targeting strategy was developed to improve the anti-atherosclerotic effects. An adenosine triphosphate (ATP)-responsive ternary core was used, and scavenger receptor A (SR-A) was loaded to promote ATP production resulting in the accelerated release of SA-A siRNA. Dual targeting was achieved by incorporating apoA-1 and phosphatidylserine to target SR-BI and CD36 receptors. In vivo studies demonstrated a 3.3-fold increase in accumulation of NPs in the plaque, resulting in 65.8% plaque reduction [227].
ApoA-1 mimetic peptides have gained popularity recenty years to fabricate sHDL NPs in order reduce cost and production time compared to using apoA-I extract. sHDL NPs using synthetic apoA-1 mimetic peptides showed improved cholesterol efflux [228] and diminished the atherosclerotic lesion by 50% through oral administration in Ldlr-/- mouse model [229].
6.2. LDL
6.2.1 LDL
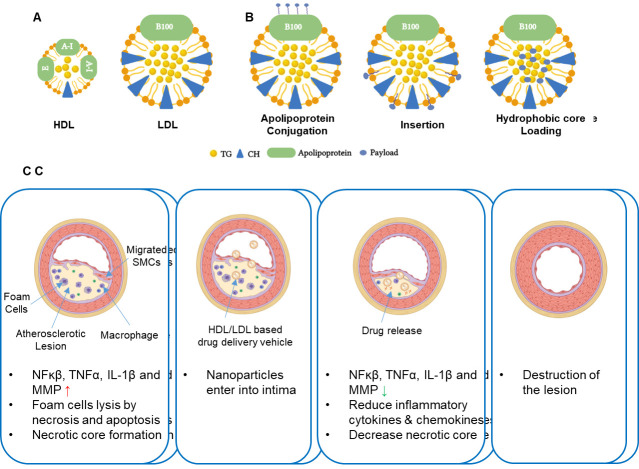
Due to the high prevalence of the LDLr on malignant cells and macrophages, LDL is another potential delivery vehicle [230]. LDL has several advantages including a long half-life in the circulation, high loading capacity, improved cell uptake efficiency and penetration, and the potential for multiple loading strategies [231].
As with HDLs, the hydrophobic core of LDL facilitates drug loading. Dexamethasone has been incorporated into LDL resulting in improved delivery efficiency to plaques and slows the development of atherosclerosis in a mouse model [232, 233]. In addition to direct loading into the hydrophobic core, conjugation is also used to load drugs into LDL. Modified LDL with covalent bonds to apolipoprotein and pre-loaded with amino acid groups, including tyrosine, lysine, arginine and cysterine, has been used for in vivo imaging [234-236]. Modifying apolipoprotein leads to inactivation of ApoB-100 [237]. The insertion strategy utilizes the non-covalent bonding between pre-load and phospholipid layer through weak interaction such as van der Waals forces [215]. The pre-loaded drug often requires an amphiphilic structure to improve success of insertion [238].
Given its role in foam cell transformation and atherosclerotic development, ox-LDL is an ideal delivery vehicle for targeted delivery. Ox-LDL loading with dexamethasone palmitate effectively inhibits foam cell formation and significantly reduces accumulation of cholesteryl esters [239]. In contrast, LDL based carriers may aggravate disease progression due to the presence of apoB (pro-atherogenic molecules). The synthetic process of LDL is challenging and complex due to the large size of apoB, significantly limiting its potential [240]. LDL based delivery systems should be further investigated [231].
6.2.2 LDL mimicking particle
LDL mimic particles (LMP) should be considered as an alternative carrier. Compared to native LDL based carriers, LMP can be synthesized in large quantities, with minimal potential pathogen infection [241, 242]. LMPs are often synthesized using commercial phospholipids without the inclusion of ApoB-100 proteins. Kim et al. synthesized an LMP with cholesteryl oleate and triolein as the core and cholesterol and DC-Cholesterol as the surface structure. Paclitaxel was loaded in LMP at the reconstitution stage [243]. However, LMP normally requires certain LDL receptor-binding domains or specific ligands modification for targeted delivery. For example, Nikanjam et al. synthesised LMP that possessed a lipid-binding motif and ApoB-100 LDLR binding motif to target glioblastoma with LDLR expression [241]. One key characterisctics of LMP is the ability to regulate LDLR expression. Dox has been loaded into LMPs modified with ApoB-100 and supplemented with mevastatin or simvastatin, resulting in the upregulation of LDLR expression [244].
A number of studies have demonstrated atheroprotective effects of LMPs. Synthetic cholesteryl-core LMPs loaded with paclitaxel administered to LDLR knockout mice on a 1% cholesterol diet resulted in reduced atherosclerotic lesions, including a 14% reduction in wall area and a 22% reduction in stenosis [245]. In a similar study, cholesteryl-core based LMPs loaded with paclitaxel, were injected into rabbits fed a high cholesterol diet. These LMPs showed significant atheroprotection, demonstrated by a reduction in intima, lesion extension and number of macrophages in the intima [246]. Carmustine has also been loaded into cholesteryl-core LMPs and reduced the lesion size by 90% and inhibited the accumulation of macrophages, T cells and vascular SMCs at the intima in a rabbit model [247].
Amphiphilic sugar-based molecules (AMs) have been used to synthesize ox-LMPs, which have similar charge and hydrophobicity to ox-LDL. AMs can bind with scavenger receptors. Tian et al. synthesized ox-LMP from amphiphilic polymers with alkyl chains on mucic acid binding to hydrophilic PEG chains, resulting in the self-assembly into ox-LMP [248]. The same group showed that one rotationally restricted carboxylic acid within AMs adequately inhibits THP-A human macrophage take up of ox-LDL [249]. Lewis et al. synthesized ox-LMPs using AM micelles and serum-stable PEG nanoparticles which bound with MSR1 and CD 36, which decreased ox-LDL accumulation and foam cell formation [250]. Petersen reported that AMs based nanoparticles downregulated the expression of scavenger receptors, SRA and CD 63, leading to the transformation of atherogenic macrophages to athero-resistant phenotype [251].
Taken together, the recent advances in HDL and LDL based drug delivery systems showcase the potential for these novel therapies to treat atherosclerosis (Fig. 4). Long-term cytotoxicity and therapeutic effects as well the clinically relevant dosing need to be fully evaluated in preclinical large animal models, before translation to clinical studies.
Figure 4.
HDL and LDL based nano carriers. (A) the structure of HDL and LDL [252]. (B) Three strategies to fabricate rHDL [253]; and (C) HDL/LDL based nano carriers for atherosclerosis treatment [254]. All figures are recreated using Biorender.
7. Conclusions and future perspective
Liproproteins remain an increasing focus of research due to their close association with atherosclerosis. Extensive studies have shown that apoB-containing lipoproteins facilitate the development of atherosclerosis. HDL generally displays anti-atherogenic properties, whilst dysfunctional HDL may promote the development of atherosclerosis. Studies highlighting novel diagnosis and other biomarker indications and treatment strategies targeting lipoprotein metabolism demonstrate increasing potential for clinical translation. However, key challenges remain. The growing understanding of heterogeneity of structure and function of lipoproteins has complicated elucidation of exact mechamisms underlying lipoprotein contributions to atherosclerosis. More work is required to develop precise and readily available diagnostic markers and to identify drugs with appropriately targeted efficacy. Most knowledge to date is based on in vitro cellular studies and animal models. Predicting which of the promising strategies explored to date will translate to the clinic is not yet clear and requires further investigation.
Acknowledgments
We thank for the permission from the Springer Nature to allow us to reuse the images related rHDL in Figure 3. This work was supported by National Nature Science Foundation of China (No. 81800267, 81870328, 82170281, U2004203), Henan Medical Science and Technology Joint Building Program (No.2018020002), Henan Thousand Talents Program (No. ZYQR201912131), Henan Province Youth Talent Promoting Project (No. 2020HYTP051), Excellent Youth Science Foundation of Henan Province (202300410362), University of Otago Health Science Postdoctoral Fellowship, New Zealand Ministry of Business, Innovation and Employment (MBIE) Science Whitinga Fellowship (21-UOO-006), National Heart Foundation of New Zealand (1891-project grant, 1896-Research Fellowship) and New Zealand Health Research Council (Explorer grant-19/779).
Footnotes
Conflicts of interest
The authors declare no conflict of interest.
References
- [1].Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. (2018). Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation, 137:e67-e492. [DOI] [PubMed] [Google Scholar]
- [2].Kemal A, Teshome MS, Ahmed M, Molla M, Malik T, Mohammed J, et al. (2020). Dyslipidemia and Associated Factors Among Adult Patients on Antiretroviral Therapy in Armed Force Comprehensive and Specialized Hospital, Addis Ababa, Ethiopia. HIV AIDS (Auckl), 12:221-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Arnao V, Tuttolomondo A, Daidone M, Pinto A (2019). Lipoproteins in Atherosclerosis Process. Curr Med Chem, 26:1525-1543. [DOI] [PubMed] [Google Scholar]
- [4].Sacks FM, Brewer HB (2014). Petar Alaupovic: The father of lipoprotein classification based on apolipoprotein composition. Arterioscler Thromb Vasc Biol, 34:1111-1113. [DOI] [PubMed] [Google Scholar]
- [5].Rajendran P, Rengarajan T, Thangavel J, Nishigaki Y, Sakthisekaran D, Sethi G, et al. (2013). The vascular endothelium and human diseases. Int J Biol Sci, 9:1057-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Brea D, Roquer J, Serena J, Segura T, Castillo J (2012). Oxidative stress markers are associated to vascular recurrence in non-cardioembolic stroke patients non-treated with statins. BMC Neurol, 12:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Gerhardt T, Ley K (2015). Monocyte trafficking across the vessel wall. Cardiovasc Res, 107:321-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Navab M, Imes SS, Hama SY, Hough GP, Ross LA, Bork RW, et al. (1991). Monocyte transmigration induced by modification of low density lipoprotein in cocultures of human aortic wall cells is due to induction of monocyte chemotactic protein 1 synthesis and is abolished by high density lipoprotein. J Clin Invest, 88:2039-2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gorski DH, Walsh K (1995). Mitogen-responsive nuclear factors that mediate growth control signals in vascular myocytes. Cardiovasc Res, 30:585-592. [PubMed] [Google Scholar]
- [10].Hines KM, Alvarado G, Chen X, Gatto C, Pokorny A, Alonzo F, et al. (2020). Lipidomic and Ultrastructural Characterization of the Cell Envelope of Staphylococcus aureus Grown in the Presence of Human Serum. mSphere, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ference BA, Kastelein JJP, Catapano AL (2020). Lipids and Lipoproteins in 2020. JAMA, 324:595-596. [DOI] [PubMed] [Google Scholar]
- [12].Lougheed M, Steinbrecher UP (1996). Mechanism of uptake of copper-oxidized low density lipoprotein in macrophages is dependent on its extent of oxidation. J Biol Chem, 271:11798-11805. [DOI] [PubMed] [Google Scholar]
- [13].Chou CC, Wang CP, Chen JH, Lin HH (2019). Anti-Atherosclerotic Effect of Leaf Polyphenols against Tumor Necrosis Factor-alpha-Induced Abnormal Vascular Smooth Muscle Cell Migration and Proliferation. Antioxidants (Basel), 8:620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Anderson KM, Castelli WP, Levy D (1987). Cholesterol and mortality. 30 years of follow-up from the Framingham study. JAMA, 257:2176-2180. [DOI] [PubMed] [Google Scholar]
- [15].Martin MJ, Hulley SB, Browner WS, Kuller LH, Wentworth D (1986). Serum cholesterol, blood pressure, and mortality: implications from a cohort of 361,662 men. Lancet, 2:933-936. [DOI] [PubMed] [Google Scholar]
- [16].Stancu CS, Toma L, Sima AV (2012). Dual role of lipoproteins in endothelial cell dysfunction in atherosclerosis. Cell Tissue Res, 349:433-446. [DOI] [PubMed] [Google Scholar]
- [17].Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. (2017). Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J, 38:2459-2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sniderman AD, Thanassoulis G, Glavinovic T, Navar AM, Pencina M, Catapano A, et al. (2019). Apolipoprotein B Particles and Cardiovascular Disease: A Narrative Review. JAMA cardiology, 4:1287-1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ference BA, Kastelein JJP, Ginsberg HN, Chapman MJ, Nicholls SJ, Ray KK, et al. (2017). Association of Genetic Variants Related to CETP Inhibitors and Statins With Lipoprotein Levels and Cardiovascular Risk. JAMA, 318:947-956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bowman L, Hopewell JC, Chen F, Wallendszus K, Stevens W, Collins R, et al. (2017). Effects of Anacetrapib in Patients with Atherosclerotic Vascular Disease. N Engl J Med, 377:1217-1227. [DOI] [PubMed] [Google Scholar]
- [21].Ference BA, Kastelein JJP, Ray KK, Ginsberg HN, Chapman MJ, Packard CJ, et al. (2019). Association of Triglyceride-Lowering LPL Variants and LDL-C-Lowering LDLR Variants With Risk of Coronary Heart Disease. JAMA, 321:364-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].(2019). 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis, 290:140-205. [DOI] [PubMed] [Google Scholar]
- [23].Maron DJ, Fazio S, Linton MF (2000). Current perspectives on statins. Circulation, 101:207-213. [DOI] [PubMed] [Google Scholar]
- [24].Kastelein JJP, Wedel MK, Baker BF, Su J, Bradley JD, Yu RZ, et al. (2006). Potent reduction of apolipoprotein B and low-density lipoprotein cholesterol by short-term administration of an antisense inhibitor of apolipoprotein B. Circulation, 114:1729-1735. [DOI] [PubMed] [Google Scholar]
- [25].Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. (2020). 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J, 41:111-188. [DOI] [PubMed] [Google Scholar]
- [26].Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen M-R, Wiklund O, et al. (2011). ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J, 32:1769-1818. [DOI] [PubMed] [Google Scholar]
- [27].Austin MA (1989). Plasma triglyceride as a risk factor for coronary heart disease. The epidemiologic evidence and beyond. Am J Epidemiol, 129:249-259. [DOI] [PubMed] [Google Scholar]
- [28].Grundy SM, Vega GL (1988). Hypertriglyceridemia: causes and relation to coronary heart disease. Semin Thromb Hemost, 14:149-164. [DOI] [PubMed] [Google Scholar]
- [29].Do R, Willer CJ, Schmidt EM, Sengupta S, Gao C, Peloso GM, et al. (2013). Common variants associated with plasma triglycerides and risk for coronary artery disease. Nat Genet, 45:1345-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Toth PP (2016). Triglyceride-rich lipoproteins as a causal factor for cardiovascular disease. Vasc Health Risk Manag, 12:171-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Sun C, Alkhoury K, Wang YI, Foster GA, Radecke CE, Tam K, et al. (2012). IRF-1 and miRNA126 modulate VCAM-1 expression in response to a high-fat meal. Circ Res, 111:1054-1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Gower RM, Wu H, Foster GA, Devaraj S, Jialal I, Ballantyne CM, et al. (2011). CD11c/CD18 expression is upregulated on blood monocytes during hypertriglyceridemia and enhances adhesion to vascular cell adhesion molecule-1. Arterioscler Thromb Vasc Biol, 31:160-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wang L, Gill R, Pedersen TL, Higgins LJ, Newman JW, Rutledge JC (2009). Triglyceride-rich lipoprotein lipolysis releases neutral and oxidized FFAs that induce endothelial cell inflammation. J Lipid Res, 50:204-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Rosenson RS, Davidson MH, Hirsh BJ, Kathiresan S, Gaudet D (2014). Genetics and causality of triglyceride-rich lipoproteins in atherosclerotic cardiovascular disease. J Am Coll Cardiol, 64:2525-2540. [DOI] [PubMed] [Google Scholar]
- [35].Nordestgaard BG, Varbo A (2014). Triglycerides and cardiovascular disease. Lancet, 384:626-635. [DOI] [PubMed] [Google Scholar]
- [36].Doi H, Kugiyama K, Oka H, Sugiyama S, Ogata N, Koide SI, et al. (2000). Remnant lipoproteins induce proatherothrombogenic molecules in endothelial cells through a redox-sensitive mechanism. Circulation, 102:670-676. [DOI] [PubMed] [Google Scholar]
- [37].Wang YI, Bettaieb A, Sun C, DeVerse JS, Radecke CE, Mathew S, et al. (2013). Triglyceride-rich lipoprotein modulates endothelial vascular cell adhesion molecule (VCAM)-1 expression via differential regulation of endoplasmic reticulum stress. PloS one, 8:e78322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Hua S (2013). Targeting sites of inflammation: intercellular adhesion molecule-1 as a target for novel inflammatory therapies. Front Pharmacol, 4:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Hadi HAR, Carr CS, Al Suwaidi J (2005). Endothelial dysfunction: cardiovascular risk factors, therapy, and outcome. Vasc Health Risk Manag, 1:183-198. [PMC free article] [PubMed] [Google Scholar]
- [40].Olufadi R, Byrne CD (2006). Effects of VLDL and remnant particles on platelets. Pathophysiol Haemost Thromb, 35:281-291. [DOI] [PubMed] [Google Scholar]
- [41].Kones R (2013). Molecular sources of residual cardiovascular risk, clinical signals, and innovative solutions: relationship with subclinical disease, undertreatment, and poor adherence: implications of new evidence upon optimizing cardiovascular patient outcomes. Vasc Health Risk Manag, 9:617-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Zheng XY, Liu L (2007). Remnant-like lipoprotein particles impair endothelial function: direct and indirect effects on nitric oxide synthase. J Lipid Res, 48:1673-1680. [DOI] [PubMed] [Google Scholar]
- [43].Marcovina SM, Koschinsky ML (2003). Evaluation of lipoprotein(a) as a prothrombotic factor: progress from bench to bedside. Curr Opin Lipidol, 14:361-366. [DOI] [PubMed] [Google Scholar]
- [44].Erqou S, Thompson A, Di Angelantonio E, Saleheen D, Kaptoge S, Marcovina S, et al. (2010). Apolipoprotein(a) isoforms and the risk of vascular disease: systematic review of 40 studies involving 58,000 participants. J Am Coll Cardiol, 55:2160-2167. [DOI] [PubMed] [Google Scholar]
- [45].Erqou S, Kaptoge S, Perry PL, Di Angelantonio E, Thompson A, White IR, et al. (2009). Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA, 302:412-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Laschkolnig A, Kollerits B, Lamina C, Meisinger C, Rantner B, Stadler M, et al. (2014). Lipoprotein (a) concentrations, apolipoprotein (a) phenotypes, and peripheral arterial disease in three independent cohorts. Cardiovasc Res, 103:28-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Hopewell JC, Seedorf U, Farrall M, Parish S, Kyriakou T, Goel A, et al. (2014). Impact of lipoprotein(a) levels and apolipoprotein(a) isoform size on risk of coronary heart disease. J Intern Med, 276:260-268. [DOI] [PubMed] [Google Scholar]
- [48].Capoulade R, Chan KL, Yeang C, Mathieu P, Bossé Y, Dumesnil JG, et al. (2015). Oxidized Phospholipids, Lipoprotein(a), and Progression of Calcific Aortic Valve Stenosis. J Am Coll Cardiol, 66:1236-1246. [DOI] [PubMed] [Google Scholar]
- [49].Witztum JL, Steinberg D (1991). Role of oxidized low density lipoprotein in atherogenesis. J Clin Invest, 88:1785-1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Kugiyama K, Kerns SA, Morrisett JD, Roberts R, Henry PD (1990). Impairment of endothelium-dependent arterial relaxation by lysolecithin in modified low-density lipoproteins. Nature, 344:160-162. [DOI] [PubMed] [Google Scholar]
- [51].Esterbauer H, Jürgens G, Quehenberger O, Koller E (1987). Autoxidation of human low density lipoprotein: loss of polyunsaturated fatty acids and vitamin E and generation of aldehydes. J Lipid Res, 28:495-509. [PubMed] [Google Scholar]
- [52].Parthasarathy S, Steinbrecher UP, Barnett J, Witztum JL, Steinberg D (1985). Essential role of phospholipase A2 activity in endothelial cell-induced modification of low density lipoprotein. Proc Natl Acad Sci U S A, 82:3000-3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Kugiyama K, Sakamoto T, Misumi I, Sugiyama S, Ohgushi M, Ogawa H, et al. (1993). Transferable lipids in oxidized low-density lipoprotein stimulate plasminogen activator inhibitor-1 and inhibit tissue-type plasminogen activator release from endothelial cells. Circ Res, 73:335-343. [DOI] [PubMed] [Google Scholar]
- [54].Wisnieski BJ, Williams RE, Fox CF (1973). Manipulation of fatty acid composition in animal cells grown in culture. Proc Natl Acad Sci U S A, 70:3669-3673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Liu SY, Lu X, Choy S, Dembinski TC, Hatch GM, Mymin D, et al. (1994). Alteration of lysophosphatidylcholine content in low density lipoprotein after oxidative modification: relationship to endothelium dependent relaxation. Cardiovasc Res, 28:1476-1481. [DOI] [PubMed] [Google Scholar]
- [56].Hartley A, Haskard D, Khamis R (2019). Oxidized LDL and anti-oxidized LDL antibodies in atherosclerosis - Novel insights and future directions in diagnosis and therapy<sup/>. Trends Cardiovasc Med, 29:22-26. [DOI] [PubMed] [Google Scholar]
- [57].Gao S, Zhao D, Wang M, Zhao F, Han X, Qi Y, et al. (2017). Association Between Circulating Oxidized LDL and Atherosclerotic Cardiovascular Disease: A Meta-analysis of Observational Studies. Can J Cardiol, 33:1624-1632. [DOI] [PubMed] [Google Scholar]
- [58].Murohara T, Kugiyama K, Ohgushi M, Sugiyama S, Ohta Y, Yasue H (1994). LPC in oxidized LDL elicits vasocontraction and inhibits endothelium- dependent relaxation. Am J Physiol, 267:H2441-H2449. [DOI] [PubMed] [Google Scholar]
- [59].Quinn MT, Parthasarathy S, Steinberg D (1988). Lysophosphatidylcholine: a chemotactic factor for human monocytes and its potential role in atherogenesis. Proc Natl Acad Sci U S A, 85:2805-2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Choi SH, Sviridov D, Miller YI (2017). Oxidized cholesteryl esters and inflammation. Biochim Biophys Acta Mol Cell Biol Lipids, 1862:393-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Kattoor AJ, Kanuri SH, Mehta JL (2019). Role of Ox-LDL and LOX-1 in Atherogenesis. Curr Med Chem, 26:1693-1700. [DOI] [PubMed] [Google Scholar]
- [62].Doll J, Bürkle F, Neide A, Tsitlakidis S, Bruckner T, Schmidmaier G, et al. (2020). Contrast-enhanced ultrasound for determining muscular perfusion after oral intake of L-citrulline, L-arginine, and galloylated epicatechines: A study protocol. Medicine (Baltimore), 99:e22318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Gimbrone MA, García-Cardeña G (2016). Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ Res, 118:620-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Lin F, Pei L, Zhang Q, Han W, Jiang S, Lin Y, et al. (2018). Ox-LDL induces endothelial cell apoptosis and macrophage migration by regulating caveolin-1 phosphorylation. J Cell Physiol, 233:6683-6692. [DOI] [PubMed] [Google Scholar]
- [65].Cao H, Jia Q, Yan L, Chen C, Xing S, Shen D (2019). Quercetin Suppresses the Progression of Atherosclerosis by Regulating MST1-Mediated Autophagy in ox-LDL-Induced RAW264.7 Macrophage Foam Cells. Int J Mol Sci, 20:6093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].van Dijk RA, Kolodgie F, Ravandi A, Leibundgut G, Hu PP, Prasad A, et al. (2012). Differential expression of oxidation-specific epitopes and apolipoprotein(a) in progressing and ruptured human coronary and carotid atherosclerotic lesions. J Lipid Res, 53:2773-2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Tsimikas S (2002). Noninvasive imaging of oxidized low-density lipoprotein in atherosclerotic plaques with tagged oxidation-specific antibodies. Am J Cardiol, 90:22L-27L. [DOI] [PubMed] [Google Scholar]
- [68].Briley-Saebo KC, Nguyen TH, Saeboe AM, Cho Y-S, Ryu SK, Volkova ER, et al. (2012). In vivo detection of oxidation-specific epitopes in atherosclerotic lesions using biocompatible manganese molecular magnetic imaging probes. J Am Coll Cardiol, 59:616-626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Li D, Patel AR, Klibanov AL, Kramer CM, Ruiz M, Kang B-Y, et al. (2010). Molecular imaging of atherosclerotic plaques targeted to oxidized LDL receptor LOX-1 by SPECT/CT and magnetic resonance. Circ Cardiovasc Imaging, 3:464-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Duivenvoorden R, Tang J, Cormode DP, Mieszawska AJ, Izquierdo-Garcia D, Ozcan C, et al. (2014). A statin-loaded reconstituted high-density lipoprotein nanoparticle inhibits atherosclerotic plaque inflammation. Nat Commun, 5:3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Rader DJ (2006). Molecular regulation of HDL metabolism and function: implications for novel therapies. J Clin Invest, 116:3090-3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Yuhanna IS, Zhu Y, Cox BE, Hahner LD, Osborne-Lawrence S, Lu P, et al. (2001). High-density lipoprotein binding to scavenger receptor-BI activates endothelial nitric oxide synthase. Nat Med, 7:853-857. [DOI] [PubMed] [Google Scholar]
- [73].Li XA, Titlow WB, Jackson BA, Giltiay N, Nikolova-Karakashian M, Uittenbogaard A, et al. (2002). High density lipoprotein binding to scavenger receptor, Class B, type I activates endothelial nitric-oxide synthase in a ceramide-dependent manner. J Biol Chem, 277:11058-11063. [DOI] [PubMed] [Google Scholar]
- [74].Assmann G, Nofer JR (2003). Atheroprotective effects of high-density lipoproteins. Annu Rev Med, 54:321-341. [DOI] [PubMed] [Google Scholar]
- [75].Rosenson RS, Brewer HB, Chapman MJ, Fazio S, Hussain MM, Kontush A, et al. (2011). HDL measures, particle heterogeneity, proposed nomenclature, and relation to atherosclerotic cardiovascular events. Clin Chem, 57:392-410. [DOI] [PubMed] [Google Scholar]
- [76].Kontush A, Chapman MJ (2006). Antiatherogenic small, dense HDL--guardian angel of the arterial wall? Nat Clin Pract Cardiovasc Med, 3:144-153. [DOI] [PubMed] [Google Scholar]
- [77].Barter P, Kastelein J, Nunn A, Hobbs R (2003). High density lipoproteins (HDLs) and atherosclerosis; the unanswered questions. Atherosclerosis, 168:195-211. [DOI] [PubMed] [Google Scholar]
- [78].Norata GD, Catapano AL (2005). Molecular mechanisms responsible for the antiinflammatory and protective effect of HDL on the endothelium. Vasc Health Risk Manag, 1:119-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Navab M, Hama SY, Cooke CJ, Anantharamaiah GM, Chaddha M, Jin L, et al. (2000). Normal high density lipoprotein inhibits three steps in the formation of mildly oxidized low density lipoprotein: step 1. J Lipid Res, 41:1481-1494. [PubMed] [Google Scholar]
- [80].Navab M, Hama SY, Hough GP, Subbanagounder G, Reddy ST, Fogelman AM (2001). A cell-free assay for detecting HDL that is dysfunctional in preventing the formation of or inactivating oxidized phospholipids. J Lipid Res, 42:1308-1317. [PubMed] [Google Scholar]
- [81].Nofer JR, Kehrel B, Fobker M, Levkau B, Assmann G, von Eckardstein A (2002). HDL and arteriosclerosis: beyond reverse cholesterol transport. Atherosclerosis, 161:1-16. [DOI] [PubMed] [Google Scholar]
- [82].Link JJ, Rohatgi A, de Lemos JA (2007). HDL cholesterol: physiology, pathophysiology, and management. Curr Probl Cardiol, 32:268-314. [DOI] [PubMed] [Google Scholar]
- [83].Ansell BJ, Fonarow GC, Fogelman AM (2007). The paradox of dysfunctional high-density lipoprotein. Curr Probl Cardiol, 18:427-434. [DOI] [PubMed] [Google Scholar]
- [84].Navab M, Ananthramaiah GM, Reddy ST, Van Lenten BJ, Ansell BJ, Fonarow GC, et al. (2004). The oxidation hypothesis of atherogenesis: the role of oxidized phospholipids and HDL. J Lipid Res, 45:993-1007. [DOI] [PubMed] [Google Scholar]
- [85].Navab M, Berliner JA, Subbanagounder G, Hama S, Lusis AJ, Castellani LW, et al. (2001). HDL and the inflammatory response induced by LDL-derived oxidized phospholipids. Arterioscler Thromb Vasc Biol, 21:481-488. [DOI] [PubMed] [Google Scholar]
- [86].Navab M, Hama SY, Anantharamaiah GM, Hassan K, Hough GP, Watson AD, et al. (2000). Normal high density lipoprotein inhibits three steps in the formation of mildly oxidized low density lipoprotein: steps 2 and 3. J Lipid Res, 41:1495-1508. [PubMed] [Google Scholar]
- [87].Norata GD, Pirillo A, Catapano AL (2006). Nutr Metab Cardiovasc Dis. Nutrition, metabolism, and cardiovascular diseases : NMCD, 16:371-386. [DOI] [PubMed] [Google Scholar]
- [88].Koike T, Koike Y, Yang D, Guo Y, Rom O, Song J, et al. (2021). Human apolipoprotein A-II reduces atherosclerosis in knock-in rabbits. Atherosclerosis, 316:32-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Vaisar T, Pennathur S, Green PS, Gharib SA, Hoofnagle AN, Cheung MC, et al. (2007). Shotgun proteomics implicates protease inhibition and complement activation in the antiinflammatory properties of HDL. J Clin Invest, 117:746-756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Song G, Liu J, Zhao Z, Yu Y, Tian H, Yao S, et al. (2011). Simvastatin reduces atherogenesis and promotes the expression of hepatic genes associated with reverse cholesterol transport in apoE-knockout mice fed high-fat diet. Lipids Health Dis, 10:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Kypreos KE, Zannis VI (2007). Pathway of biogenesis of apolipoprotein E-containing HDL in vivo with the participation of ABCA1 and LCAT. Biochem J, 403:359-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Morton AM, Koch M, Mendivil CO, Furtado JD, Tjønneland A, Overvad K, et al. (2018). Apolipoproteins E and CIII interact to regulate HDL metabolism and coronary heart disease risk. JCI insight, 3:e98045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Yang N, Qin Q (2015). Apolipoprotein J: A New Predictor and Therapeutic Target in Cardiovascular Disease? Chinese medical journal, 128:2530-2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Bettuzzi S (2009). Conclusions and perspectives. Adv Cancer Res, 105:133-150. [DOI] [PubMed] [Google Scholar]
- [95].Gelissen IC, Hochgrebe T, Wilson MR, Easterbrook-Smith SB, Jessup W, Dean RT, et al. (1998). Apolipoprotein J (clusterin) induces cholesterol export from macrophage-foam cells: a potential anti-atherogenic function? Biochem J, 331:231-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Liu M, St Clair RW, Subbaiah PV (1998). Impaired function of lecithin:cholesterol acyltransferase in atherosclerosis-susceptible White Carneau pigeons: possible effects on metabolism of oxidized phospholipids. J Lipid Res, 39:245-254. [PubMed] [Google Scholar]
- [97].Kudo I, Murakami M (2002). Phospholipase A2 enzymes. Prostaglandins Other Lipid Mediat, 68- 69:3-58. [DOI] [PubMed] [Google Scholar]
- [98].Tsimihodimos V, Karabina S-AP, Tambaki AP, Bairaktari E, Miltiadous G, Goudevenos JA, et al. (2002). Altered distribution of platelet-activating factor- acetylhydrolase activity between LDL and HDL as a function of the severity of hypercholesterolemia. J Lipid Res, 43:256-263. [PubMed] [Google Scholar]
- [99].Tosheska Trajkovska K, Topuzovska S (2017). High-density lipoprotein metabolism and reverse cholesterol transport: strategies for raising HDL cholesterol. Anatol J Cardiol, 18:149-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Rye KA, Barter PJ (2004). Formation and metabolism of prebeta-migrating, lipid-poor apolipoprotein A-I. Arterioscler Thromb Vasc Biol, 24:421-428. [DOI] [PubMed] [Google Scholar]
- [101].Watson AD, Berliner JA, Hama SY, La Du BN, Faull KF, Fogelman AM, et al. (1995). Protective effect of high density lipoprotein associated paraoxonase. Inhibition of the biological activity of minimally oxidized low density lipoprotein. J Clin Invest, 96:2882-2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Mackness MI, Arrol S, Durrington PN (1991). Paraoxonase prevents accumulation of lipoperoxides in low-density lipoprotein. FEBS letters, 286:152-154. [DOI] [PubMed] [Google Scholar]
- [103].Aviram M, Rosenblat M, Bisgaier CL, Newton RS, Primo-Parmo SL, La Du BN (1998). Paraoxonase inhibits high-density lipoprotein oxidation and preserves its functions. A possible peroxidative role for paraoxonase. J Clin Invest, 101:1581-1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Rosenblat M, Vaya J, Shih D, Aviram M (2005). Paraoxonase 1 (PON1) enhances HDL-mediated macrophage cholesterol efflux via the ABCA1 transporter in association with increased HDL binding to the cells: a possible role for lysophosphatidylcholine. Atherosclerosis, 179:69-77. [DOI] [PubMed] [Google Scholar]
- [105].Sattler W, Maiorino M, Stocker R (1994). Reduction of HDL- and LDL-associated cholesterylester and phospholipid hydroperoxides by phospholipid hydroperoxide glutathione peroxidase and Ebselen (PZ 51). Arch Biochem Biophys, 309:214-221. [DOI] [PubMed] [Google Scholar]
- [106].Doggrell SA (2008). The failure of torcetrapib: is there a case for independent preclinical and clinical testing? Expert Opin Pharmacother, 9:875-878. [DOI] [PubMed] [Google Scholar]
- [107].Kastelein JJP, van Leuven SI, Burgess L, Evans GW, Kuivenhoven JA, Barter PJ, et al. (2007). Effect of torcetrapib on carotid atherosclerosis in familial hypercholesterolemia. N Engl J Med, 356:1620-1630. [DOI] [PubMed] [Google Scholar]
- [108].Ansell BJ, Fonarow GC, Fogelman AM (2006). High-density lipoprotein: is it always atheroprotective? Curr Atheroscler Rep, 8:405-411. [DOI] [PubMed] [Google Scholar]
- [109].Nakajima T, Origuchi N, Matsunaga T, Kawai S, Hokari S, Nakamura H, et al. (2000). Localization of oxidized HDL in atheromatous plaques and oxidized HDL binding sites on human aortic endothelial cells. Ann Clin Biochem, 37:179-186. [DOI] [PubMed] [Google Scholar]
- [110].Matsunaga T, Hokari S, Koyama I, Harada T, Komoda T (2003). NF-kappa B activation in endothelial cells treated with oxidized high-density lipoprotein. Biochem Biophys Res Commun, 303:313-319. [DOI] [PubMed] [Google Scholar]
- [111].Nagano Y, Arai H, Kita T (1991). High density lipoprotein loses its effect to stimulate efflux of cholesterol from foam cells after oxidative modification. Proc Natl Acad Sci U S A, 88:6457-6461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Lindstedt L, Saarinen J, Kalkkinen N, Welgus H, Kovanen PT (1999). Matrix metalloproteinases-3, -7, and -12, but not -9, reduce high density lipoprotein-induced cholesterol efflux from human macrophage foam cells by truncation of the carboxyl terminus of apolipoprotein A-I. Parallel losses of pre-beta particles and the high affinity component of efflux. J Biol Chem, 274:22627-22634. [DOI] [PubMed] [Google Scholar]
- [113].Daugherty A, Dunn JL, Rateri DL, Heinecke JW (1994). Myeloperoxidase, a catalyst for lipoprotein oxidation, is expressed in human atherosclerotic lesions. J Clin Invest, 94:437-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Bergt C, Reicher H, Malle E, Sattler W (1999). Hypochlorite modification of high density lipoprotein: effects on cholesterol efflux from J774 macrophages. FEBS letters, 452:295-300. [DOI] [PubMed] [Google Scholar]
- [115].Marsche G, Hammer A, Oskolkova O, Kozarsky KF, Sattler W, Malle E (2002). Hypochlorite-modified high density lipoprotein, a high affinity ligand to scavenger receptor class B, type I, impairs high density lipoprotein-dependent selective lipid uptake and reverse cholesterol transport. J Biol Chem, 277:32172-32179. [DOI] [PubMed] [Google Scholar]
- [116].Suc I, Brunet S, Mitchell G, Rivard G-E, Levy E (2003). Oxidative tyrosylation of high density lipoproteins impairs cholesterol efflux from mouse J774 macrophages: role of scavenger receptors, classes A and B. J Clin Invest, 116:89-99. [DOI] [PubMed] [Google Scholar]
- [117].Judström I, Jukkola H, Metso J, Jauhiainen M, Kovanen PT, Lee-Rueckert M (2010). Mast cell-dependent proteolytic modification of HDL particles during anaphylactic shock in the mouse reduces their ability to induce cholesterol efflux from macrophage foam cells ex vivo. Atherosclerosis, 208:148-154. [DOI] [PubMed] [Google Scholar]
- [118].Lee M, Lindstedt LK, Kovanen PT (1992). Mast cell-mediated inhibition of reverse cholesterol transport. Arterioscler Thromb, 12:1329-1335. [DOI] [PubMed] [Google Scholar]
- [119].Gauster M, Oskolkova OV, Innerlohinger J, Glatter O, Knipping G, Frank S (2004). Endothelial lipase-modified high-density lipoprotein exhibits diminished ability to mediate SR-BI (scavenger receptor B type I)-dependent free-cholesterol efflux. Biochem J, 382:75-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Pirillo A, Ghiselli G (2000). Enhanced macrophage uptake of elastase-modified high-density lipoproteins. Biochem Biophys Res Commun, 271:386-391. [DOI] [PubMed] [Google Scholar]
- [121].Han CY, Tang C, Guevara ME, Wei H, Wietecha T, Shao B, et al. (2016). Serum amyloid A impairs the antiinflammatory properties of HDL. J Clin Invest, 126:796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Van Lenten BJ, Hama SY, de Beer FC, Stafforini DM, McIntyre TM, Prescott SM, et al. (1995). Anti-inflammatory HDL becomes pro-inflammatory during the acute phase response. Loss of protective effect of HDL against LDL oxidation in aortic wall cell cocultures. J Clin Invest, 96:2758-2767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Ishimoto Y, Yamada K, Yamamoto S, Ono T, Notoya M, Hanasaki K (2003). Group V and X secretory phospholipase A(2)s-induced modification of high-density lipoprotein linked to the reduction of its antiatherogenic functions. Biochim Biophys Acta, 1642:129-138. [DOI] [PubMed] [Google Scholar]
- [124].Chen YD, Jeng CY, Reaven GM (1987). HDL metabolism in diabetes. Diabetes Metab Rev, 3:653-668. [DOI] [PubMed] [Google Scholar]
- [125].Ferretti G, Bacchetti T, Marchionni C, Caldarelli L, Curatola G (2001). Effect of glycation of high density lipoproteins on their physicochemical properties and on paraoxonase activity. Acta Diabetol, 38:163-169. [DOI] [PubMed] [Google Scholar]
- [126].Hedrick CC, Thorpe SR, Fu MX, Harper CM, Yoo J, Kim SM, et al. (2000). Glycation impairs high-density lipoprotein function. Diabetologia, 43:312-320. [DOI] [PubMed] [Google Scholar]
- [127].Valanti EK, Dalakoura-Karagkouni K, Siasos G, Kardassis D, Eliopoulos AG, Sanoudou D (2021). Advances in biological therapies for dyslipidemias and atherosclerosis. Metabolism, 116:154461. [DOI] [PubMed] [Google Scholar]
- [128].Cohen JC, Boerwinkle E, Mosley TH, Hobbs HH (2006). Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. The New England journal of medicine, 354:1264-1272. [DOI] [PubMed] [Google Scholar]
- [129].Tang ZH, Peng J, Ren Z, Yang J, Li TT, Li TH, et al. (2017). New role of PCSK9 in atherosclerotic inflammation promotion involving the TLR4/NF-κB pathway. Atherosclerosis, 262:113-122. [DOI] [PubMed] [Google Scholar]
- [130].Rosenson RS, Hegele RA, Fazio S, Cannon CP (2018). The Evolving Future of PCSK9 Inhibitors. J Am Coll Cardiol, 72:314-329. [DOI] [PubMed] [Google Scholar]
- [131].Kühnast S, van der Hoorn JWA, Pieterman EJ, van den Hoek AM, Sasiela WJ, Gusarova V, et al. (2014). Alirocumab inhibits atherosclerosis, improves the plaque morphology, and enhances the effects of a statin. J Lipid Res, 55:2103-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [132].Ota H, Omori H, Kawasaki M, Hirakawa A, Matsuo H (2021). Clinical impact of PCSK9 inhibitor on stabilization and regression of lipid-rich coronary plaques: a near-infrared spectroscopy study. Eur Heart [J] Cardiovasc Imaging. [DOI] [PubMed] [Google Scholar]
- [133].Ridker PM, Tardif JC, Amarenco P, Duggan W, Glynn RJ, Jukema JW, et al. (2017). Lipid-Reduction Variability and Antidrug-Antibody Formation with Bococizumab. N Engl J Med, 376:1517-1526. [DOI] [PubMed] [Google Scholar]
- [134].O'Donoghue ML, Fazio S, Giugliano RP, Stroes ESG, Kanevsky E, Gouni-Berthold I, et al. (2019). Lipoprotein(a), PCSK9 Inhibition, and Cardiovascular Risk. Circulation, 139:1483-1492. [DOI] [PubMed] [Google Scholar]
- [135].Hadjiphilippou S, Ray KK (2017). Evolocumab and clinical outcomes in patients with cardiovascular disease. J R Coll Physicians Edinb, 47:153-155. [DOI] [PubMed] [Google Scholar]
- [136].Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. (2017). Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med, 376:1713-1722. [DOI] [PubMed] [Google Scholar]
- [137].Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. (2018). Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N Engl J Med, 379:2097-2107. [DOI] [PubMed] [Google Scholar]
- [138].Orringer CE, Jacobson TA, Saseen JJ, Brown AS, Gotto AM, Ross JL, et al. (2017). Update on the use of PCSK9 inhibitors in adults: Recommendations from an Expert Panel of the National Lipid Association. J Clin Lipidol, 11:880-890. [DOI] [PubMed] [Google Scholar]
- [139].Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Daly DD, DePalma SM, et al. (2017). 2017 Focused Update of the 2016 ACC Expert Consensus Decision Pathway on the Role of Non-Statin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol, 70:1785-1822. [DOI] [PubMed] [Google Scholar]
- [140].Landmesser U, Chapman MJ, Stock JK, Amarenco P, Belch JJF, Borén J, et al. (2018). 2017 Update of ESC/EAS Task Force on practical clinical guidance for proprotein convertase subtilisin/kexin type 9 inhibition in patients with atherosclerotic cardiovascular disease or in familial hypercholesterolaemia. Eur Heart J, 39:1131-1143. [DOI] [PubMed] [Google Scholar]
- [141].Shimizugawa T, Ono M, Shimamura M, Yoshida K, Ando Y, Koishi R, et al. (2002). ANGPTL3 decreases very low density lipoprotein triglyceride clearance by inhibition of lipoprotein lipase. J Biol Chem, 277:33742-33748. [DOI] [PubMed] [Google Scholar]
- [142].Lupo MG, Ferri N (2018). Angiopoietin-Like 3 (ANGPTL3) and Atherosclerosis: Lipid and Non-Lipid Related Effects. J Cardiovasc Dev Dis, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Ahmad Z, Banerjee P, Hamon S, Chan KC, Bouzelmat A, Sasiela WJ, et al. (2019). Inhibition of Angiopoietin-Like Protein 3 With a Monoclonal Antibody Reduces Triglycerides in Hypertriglyceridemia. Circulation, 140:470-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Gaudet D, Gipe DA, Pordy R, Ahmad Z, Cuchel M, Shah PK, et al. (2017). ANGPTL3 Inhibition in Homozygous Familial Hypercholesterolemia. N Engl J Med, 377:296-297. [DOI] [PubMed] [Google Scholar]
- [145].Ruscica M, Zimetti F, Adorni MP, Sirtori CR, Lupo MG, Ferri N (2020). Pharmacological aspects of ANGPTL3 and ANGPTL4 inhibitors: New therapeutic approaches for the treatment of atherogenic dyslipidemia. Pharmacol Res, 153:104653. [DOI] [PubMed] [Google Scholar]
- [146].Inukai K, Nakashima Y, Watanabe M, Kurihara S, Awata T, Katagiri H, et al. (2004). ANGPTL3 is increased in both insulin-deficient and -resistant diabetic states. Biochem Biophys Res Commun, 317:1075-1079. [DOI] [PubMed] [Google Scholar]
- [147].Kersten S, Mandard S, Tan NS, Escher P, Metzger D, Chambon P, et al. (2000). Characterization of the fasting-induced adipose factor FIAF, a novel peroxisome proliferator-activated receptor target gene. J Biol Chem, 275:28488-28493. [DOI] [PubMed] [Google Scholar]
- [148].Aryal B, Rotllan N, Araldi E, Ramírez CM, He S, Chousterman BG, et al. (2016). ANGPTL4 deficiency in haematopoietic cells promotes monocyte expansion and atherosclerosis progression. Nat Commun, 7:12313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [149].Georgiadi A, Wang Y, Stienstra R, Tjeerdema N, Janssen A, Stalenhoef A, et al. (2013). Overexpression of angiopoietin-like protein 4 protects against atherosclerosis development. Arterioscler Thromb Vasc Biol, 33:1529-1537. [DOI] [PubMed] [Google Scholar]
- [150].Adachi H, Fujiwara Y, Kondo T, Nishikawa T, Ogawa R, Matsumura T, et al. (2009). Angptl 4 deficiency improves lipid metabolism, suppresses foam cell formation and protects against atherosclerosis. Biochem Biophys Res Commun, 379:806-811. [DOI] [PubMed] [Google Scholar]
- [151].Amirfakhryan H (2020). Vaccination against atherosclerosis: An overview. Hellenic J Cardiol, 61:78-91. [DOI] [PubMed] [Google Scholar]
- [152].Palinski W, Miller E, Witztum JL (1995). Immunization of low density lipoprotein (LDL) receptor-deficient rabbits with homologous malondialdehyde-modified LDL reduces atherogenesis. Proc Natl Acad Sci U S A, 92:821-825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [153].Ameli S, Hultgårdh-Nilsson A, Regnström J, Calara F, Yano J, Cercek B, et al. (1996). Effect of immunization with homologous LDL and oxidized LDL on early atherosclerosis in hypercholesterolemic rabbits. Arterioscler Thromb Vasc Biol, 16:1074-1079. [DOI] [PubMed] [Google Scholar]
- [154].Nettersheim FS, De Vore L, Winkels H (2020). Vaccination in Atherosclerosis. Cells, 9:2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Ray KK, Wright RS, Kallend D, Koenig W, Leiter LA, Raal FJ, et al. (2020). Two Phase 3 Trials of Inclisiran in Patients with Elevated LDL Cholesterol. N Engl J Med, 382:1507-1519. [DOI] [PubMed] [Google Scholar]
- [156].Raal FJ, Kallend D, Ray KK, Turner T, Koenig W, Wright RS, et al. (2020). Inclisiran for the Treatment of Heterozygous Familial Hypercholesterolemia. N Engl J Med, 382:1520-1530. [DOI] [PubMed] [Google Scholar]
- [157].Landlinger C, Pouwer MG, Juno C, van der Hoorn JWA, Pieterman EJ, Jukema JW, et al. (2017). The AT04A vaccine against proprotein convertase subtilisin/kexin type 9 reduces total cholesterol, vascular inflammation, and atherosclerosis in APOE*3Leiden.CETP mice. Eur Heart J, 38:2499-2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Gaudet D, Alexander VJ, Baker BF, Brisson D, Tremblay K, Singleton W, et al. (2015). Antisense Inhibition of Apolipoprotein C-III in Patients with Hypertriglyceridemia. N Engl J Med, 373:438-447. [DOI] [PubMed] [Google Scholar]
- [159].Lindquist IE, Crossey E, Amar M, Remaley A, Chackerian B (2017). A VACCINE-BASED STRATEGY FOR REDUCING CARDIOVASCULAR DISEASE RISK FACTORS. J Am Coll Cardiol, 69:1783. [Google Scholar]
- [160].Rittershaus CW, Miller DP, Thomas LJ, Picard MD, Honan CM, Emmett CD, et al. (2000). Vaccine-induced antibodies inhibit CETP activity in vivo and reduce aortic lesions in a rabbit model of atherosclerosis. Arterioscler Thromb Vasc Biol, 20:2106-2112. [DOI] [PubMed] [Google Scholar]
- [161].Davidson MH, Maki K, Umporowicz D, Wheeler A, Rittershaus C, Ryan U (2003). The safety and immunogenicity of a CETP vaccine in healthy adults. Atherosclerosis, 169:113-120. [DOI] [PubMed] [Google Scholar]
- [162].Grundtman C, Kreutmayer SB, Almanzar G, Wick MC, Wick G (2011). Heat shock protein 60 and immune inflammatory responses in atherosclerosis. Arterioscler Thromb Vasc Biol, 31:960-968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].Jing H, Yong L, Haiyan L, Yanjun M, Yun X, Yu Z, et al. (2011). Oral administration of Lactococcus lactis delivered heat shock protein 65 attenuates atherosclerosis in low-density lipoprotein receptor-deficient mice. Vaccine, 29:4102-4109. [DOI] [PubMed] [Google Scholar]
- [164].Hagiwara M, Kurita-Ochiai T, Kobayashi R, Hashizume-Takizawa T, Yamazaki K, Yamamoto M (2014). Sublingual vaccine with GroEL attenuates atherosclerosis. J Dent Res, 93:382-387. [DOI] [PubMed] [Google Scholar]
- [165].Nilsson J, Calara F, Regnstrom J, Hultgardh-Nilsson A, Ameli S, Cercek B, et al. (1997). Immunization with homologous oxidized low density lipoprotein reduces neointimal formation after balloon injury in hypercholesterolemic rabbits. J Am Coll Cardiol, 30:1886-1891. [DOI] [PubMed] [Google Scholar]
- [166].George J, Afek A, Gilburd B, Levkovitz H, Shaish A, Goldberg I, et al. (1998). Hyperimmunization of apo-E-deficient mice with homologous malondialdehyde low-density lipoprotein suppresses early atherogenesis. Atherosclerosis, 138:147-152. [DOI] [PubMed] [Google Scholar]
- [167].Fredrikson GN, Hedblad B, Berglund G, Alm R, Ares M, Cercek B, et al. (2003). Identification of immune responses against aldehyde-modified peptide sequences in apoB associated with cardiovascular disease. Arterioscler Thromb Vasc Biol, 23:872-878. [DOI] [PubMed] [Google Scholar]
- [168].Fredrikson GN, Söderberg I, Lindholm M, Dimayuga P, Chyu K-Y, Shah PK, et al. (2003). Inhibition of atherosclerosis in apoE-null mice by immunization with apoB-100 peptide sequences. Arterioscler Thromb Vasc Biol, 23:879-884. [DOI] [PubMed] [Google Scholar]
- [169].Khalil DN, Smith EL, Brentjens RJ, Wolchok JD (2016). The future of cancer treatment: immunomodulation, CARs and combination immunotherapy. Nat Rev Clin Oncol, 13:273-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [170].Fredrikson GN, Andersson L, Söderberg I, Dimayuga P, Chyu K-Y, Shah PK, et al. (2005). Atheroprotective immunization with MDA-modified apo B-100 peptide sequences is associated with activation of Th2 specific antibody expression. Autoimmunity, 38:171-179. [DOI] [PubMed] [Google Scholar]
- [171].Ellis RW, Brown KR (1997). Combination vaccines. Adv Pharmacol, 39:393-423. [DOI] [PubMed] [Google Scholar]
- [172].Lu X, Xia M, Endresz V, Faludi I, Szabo A, Gonczol E, et al. (2012). Impact of multiple antigenic epitopes from ApoB100, hHSP60 and Chlamydophila pneumoniae on atherosclerotic lesion development in Apob(tm2Sgy)Ldlr(tm1Her)J mice. Atherosclerosis, 225:56-68. [DOI] [PubMed] [Google Scholar]
- [173].Raal FJ, Santos RD, Blom DJ, Marais AD, Charng M-J, Cromwell WC, et al. (2010). Mipomersen, an apolipoprotein B synthesis inhibitor, for lowering of LDL cholesterol concentrations in patients with homozygous familial hypercholesterolaemia: a randomised, double-blind, placebo-controlled trial. Lancet, 375:998-1006. [DOI] [PubMed] [Google Scholar]
- [174].Stein EA, Dufour R, Gagne C, Gaudet D, East C, Donovan JM, et al. (2012). Apolipoprotein B synthesis inhibition with mipomersen in heterozygous familial hypercholesterolemia: results of a randomized, double-blind, placebo-controlled trial to assess efficacy and safety as add-on therapy in patients with coronary artery disease. Circulation, 126:2283-2292. [DOI] [PubMed] [Google Scholar]
- [175].Thomas GS, Cromwell WC, Ali S, Chin W, Flaim JD, Davidson M (2013). Mipomersen, an apolipoprotein B synthesis inhibitor, reduces atherogenic lipoproteins in patients with severe hypercholesterolemia at high cardiovascular risk: a randomized, double-blind, placebo-controlled trial. J Am Coll Cardiol, 62:2178-2184. [DOI] [PubMed] [Google Scholar]
- [176].Reeskamp LF, Kastelein JJP, Moriarty PM, Duell PB, Catapano AL, Santos RD, et al. (2019). Safety and efficacy of mipomersen in patients with heterozygous familial hypercholesterolemia. Atherosclerosis, 280:109-117. [DOI] [PubMed] [Google Scholar]
- [177].Akdim F, Tribble DL, Flaim JD, Yu R, Su J, Geary RS, et al. (2011). Efficacy of apolipoprotein B synthesis inhibition in subjects with mild-to-moderate hyperlipidaemia. Eur Heart J, 32:2650-2659. [DOI] [PubMed] [Google Scholar]
- [178].Viney NJ, van Capelleveen JC, Geary RS, Xia S, Tami JA, Yu RZ, et al. (2016). Antisense oligonucleotides targeting apolipoprotein(a) in people with raised lipoprotein(a): two randomised, double-blind, placebo-controlled, dose-ranging trials. Lancet, 388:2239-2253. [DOI] [PubMed] [Google Scholar]
- [179].Tsimikas S, Karwatowska-Prokopczuk E, Gouni-Berthold I, Tardif J-C, Baum SJ, Steinhagen-Thiessen E, et al. (2020). Lipoprotein(a) Reduction in Persons with Cardiovascular Disease. N Engl J Med, 382:244-255. [DOI] [PubMed] [Google Scholar]
- [180].Gaudet D, Digenio A, Alexander V, Arca M, Jones A, Stroes E, et al.The approach study: a randomized, double-blind, placebo-controlled, phase 3 study of volanesorsen administered subcutaneously to patients with familial chylomicronemia syndrome (FCS). Atherosclerosis, 263:e10-e10. [Google Scholar]
- [181].Graham MJ, Lee RG, Brandt TA, Tai LJ, Fu W, Peralta R, et al. (2017). Cardiovascular and Metabolic Effects of ANGPTL3 Antisense Oligonucleotides. N Engl J Med, 377:222-232. [DOI] [PubMed] [Google Scholar]
- [182].Prakash TP, Graham MJ, Yu J, Carty R, Low A, Chappell A, et al. (2014). Targeted delivery of antisense oligonucleotides to hepatocytes using triantennary N-acetyl galactosamine improves potency 10-fold in mice. Nucleic Acids Res, 42:8796-8807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [183].Benizri S, Gissot A, Martin A, Vialet B, Grinstaff MW, Barthélémy P (2019). Bioconjugated Oligonucleotides: Recent Developments and Therapeutic Applications. Bioconjug Chem, 30:366-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [184].Wang D, Gao G (2014). State-of-the-art human gene therapy: part II. Gene therapy strategies and clinical applications. Discov Med, 18:151-161. [PMC free article] [PubMed] [Google Scholar]
- [185].Haddley K (2013). Alipogene tiparvovec for the treatment of lipoprotein lipase deficiency. Drugs of today (Barcelona, Spain : 1998), 49:161-170. [DOI] [PubMed] [Google Scholar]
- [186].Senior M (2017). After Glybera's withdrawal, what's next for gene therapy? Nat Biotechnol, 35:491-492. [DOI] [PubMed] [Google Scholar]
- [187].Kassim SH, Li H, Vandenberghe LH, Hinderer C, Bell P, Marchadier D, et al. (2010). Gene therapy in a humanized mouse model of familial hypercholesterolemia leads to marked regression of atherosclerosis. PloS one, 5:e13424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [188].Kassim SH, Li H, Bell P, Somanathan S, Lagor W, Jacobs F, et al. (2013). Adeno-associated virus serotype 8 gene therapy leads to significant lowering of plasma cholesterol levels in humanized mouse models of homozygous and heterozygous familial hypercholesterolemia. Hum Gene Ther, 24:19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [189].Greig JA, Limberis MP, Bell P, Chen SJ, Calcedo R, Rader DJ, et al. (2017). Nonclinical Pharmacology/Toxicology Study of AAV8.TBG.mLDLR and AAV8.TBG.hLDLR in a Mouse Model of Homozygous Familial Hypercholesterolemia. Hum Gene Ther Clin Dev, 28:28-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [190].Greig JA, Limberis MP, Bell P, Chen SJ, Calcedo R, Rader DJ, et al. (2017). Non-Clinical Study Examining AAV8.TBG.hLDLR Vector-Associated Toxicity in Chow-Fed Wild-Type and LDLR Rhesus Macaques. Hum Gene Ther Clin Dev, 28:39-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [191].Pastore L, Belalcazar LM, Oka K, Cela R, Lee B, Chan L, et al. (2004). Helper-dependent adenoviral vector-mediated long-term expression of human apolipoprotein A-I reduces atherosclerosis in apo E-deficient mice. Gene, 327:153-160. [DOI] [PubMed] [Google Scholar]
- [192].Wacker BK, Dronadula N, Zhang J, Dichek DA (2017). Local Vascular Gene Therapy With Apolipoprotein A-I to Promote Regression of Atherosclerosis. Arterioscler Thromb Vasc Biol, 37:316-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [193].Flynn R, Qian K, Tang C, Dronadula N, Buckler JM, Jiang B, et al. (2011). Expression of apolipoprotein A-I in rabbit carotid endothelium protects against atherosclerosis. Mol Ther, 19:1833-1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [194].Wacker BK, Dronadula N, Bi L, Stamatikos A, Dichek DA (2018). Apo A-I (Apolipoprotein A-I) Vascular Gene Therapy Provides Durable Protection Against Atherosclerosis in Hyperlipidemic Rabbits. Arterioscler Thromb Vasc Biol, 38:206-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [195].Wang D, Tai PWL, Gao G (2019). Adeno-associated virus vector as a platform for gene therapy delivery. Nat Rev Drug Discov, 18:358-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [196].Valanti EK, Dalakoura-Karagkouni K, Siasos G, Kardassis D, Eliopoulos AG, Sanoudou D (2021). Advances in biological therapies for dyslipidemias and atherosclerosis. Metabolism, 116:154461. [DOI] [PubMed] [Google Scholar]
- [197].Ditiatkovski M, Palsson J, Chin-Dusting J, Remaley AT, Sviridov D (2017). Apolipoprotein A-I Mimetic Peptides: Discordance Between In Vitro and In Vivo Properties-Brief Report. Arterioscler Thromb Vasc Biol, 37:1301-1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [198].Leman LJ (2015). The potential of apolipoprotein mimetic peptides in the treatment of atherosclerosis. Clin Lipidol, 10:215-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [199].Pickar-Oliver A, Gersbach CA (2019). The next generation of CRISPR-Cas technologies and applications. Nat Rev Mol Cell Biol, 20:490-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [200].Cyranoski D, Ledford H (2018). Genome-edited baby claim provokes international outcry. Nature, 563:607-608. [DOI] [PubMed] [Google Scholar]
- [201].Jarrett KE, Lee C, De Giorgi M, Hurley A, Gillard BK, Doerfler AM, et al. (2018). Somatic Editing of Ldlr With Adeno-Associated Viral-CRISPR Is an Efficient Tool for Atherosclerosis Research. Arterioscler Thromb Vasc Biol, 38:1997-2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [202].Nishita M, Park SY, Nishio T, Kamizaki K, Wang Z, Tamada K, et al. (2017). Ror2 signaling regulates Golgi structure and transport through IFT20 for tumor invasiveness. Sci Rep, 7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [203].Ding Q, Strong A, Patel KM, Ng SL, Gosis BS, Regan SN, et al. (2014). Permanent alteration of PCSK9 with in vivo CRISPR-Cas9 genome editing. Circ Res, 115:488-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [204].Thakore PI, Kwon JB, Nelson CE, Rouse DC, Gemberling MP, Oliver ML, et al. (2018). RNA-guided transcriptional silencing in vivo with S. aureus CRISPR-Cas9 repressors. Nat Commun, 9:1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Ran FA, Cong L, Yan WX, Scott DA, Gootenberg JS, Kriz AJ, et al. (2015). In vivo genome editing using Staphylococcus aureus Cas9. Nature, 520:186-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [206].Carreras A, Pane LS, Nitsch R, Madeyski-Bengtson K, Porritt M, Akcakaya P, et al. (2019). In vivo genome and base editing of a human PCSK9 knock-in hypercholesterolemic mouse model. BMC Biol, 17:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [207].Chadwick AC, Evitt NH, Lv W, Musunuru K (2018). Reduced Blood Lipid Levels With In Vivo CRISPR-Cas9 Base Editing of ANGPTL3. Circulation, 137:975-977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [208].Doudna JA (2020). The promise and challenge of therapeutic genome editing. Nature, 578:229-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [209].Jonas A (1986). Reconstitution of high-density lipoproteins. Methods Enzymol, 128:553-582. [DOI] [PubMed] [Google Scholar]
- [210].Ritter MC, Scanus AM (1977). Role of apolipoprotein A-I in the structure of human serum high density lipoproteins. Reconstitution studies. J Biol Chem, 252:1208-1216. [PubMed] [Google Scholar]
- [211].Kim Y, Fay F, Cormode DP, Sanchez-Gaytan BL, Tang J, Hennessy EJ, et al. (2013). Single step reconstitution of multifunctional high-density lipoprotein-derived nanomaterials using microfluidics. ACS nano, 7:9975-9983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [212].Dudley-Brown S (2004). A shot of good cholesterol: synthetic HDL, a new intervention for atherosclerosis. J Cardiovasc Nurs, 19:421-424. [DOI] [PubMed] [Google Scholar]
- [213].Tardif J-C, Grégoire J, L'Allier PL, Ibrahim R, Lespérance J, Heinonen TM, et al. (2007). Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA, 297:1675-1682. [DOI] [PubMed] [Google Scholar]
- [214].Shaw JA, Bobik A, Murphy A, Kanellakis P, Blombery P, Mukhamedova N, et al. (2008). Infusion of reconstituted high-density lipoprotein leads to acute changes in human atherosclerotic plaque. Circ Res, 103:1084-1091. [DOI] [PubMed] [Google Scholar]
- [215].Sabnis N, Nair M, Israel M, McConathy WJ, Lacko AG (2012). Enhanced solubility and functionality of valrubicin (AD-32) against cancer cells upon encapsulation into biocompatible nanoparticles. Int J Nanomedicine, 7:975-983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [216].Ng KK, Lovell JF, Zheng G (2011). Lipoprotein-inspired nanoparticles for cancer theranostics. Acc Chem Res, 44:1105-1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [217].Farokhzad OC, Langer R (2009). Impact of nanotechnology on drug delivery. ACS nano, 3:16-20. [DOI] [PubMed] [Google Scholar]
- [218].Tang J, Lobatto ME, Hassing L, van der Staay S, van Rijs SM, Calcagno C, et al. (2015). Inhibiting macrophage proliferation suppresses atherosclerotic plaque inflammation. Sci Adv, 1:e1400223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [219].Damiano MG, Mutharasan RK, Tripathy S, McMahon KM, Thaxton CS (2013). Templated high density lipoprotein nanoparticles as potential therapies and for molecular delivery. Adv Drug Deliv Rev, 65:649-662. [DOI] [PubMed] [Google Scholar]
- [220].Liu L, He H, Zhang M, Zhang S, Zhang W, Liu J (2014). Hyaluronic acid-decorated reconstituted high density lipoprotein targeting atherosclerotic lesions. Biomaterials, 35:8002-8014. [DOI] [PubMed] [Google Scholar]
- [221].Thaxton CS, Daniel WL, Giljohann DA, Thomas AD, Mirkin CA (2009). Templated spherical high density lipoprotein nanoparticles. J Am Chem Soc, 131:1384-1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [222].Zhang Z, Chen J, Ding L, Jin H, Lovell JF, Corbin IR, et al. (2010). HDL-mimicking peptide-lipid nanoparticles with improved tumor targeting. Small, 6:430-437. [DOI] [PubMed] [Google Scholar]
- [223].Zhang Z, Cao W, Jin H, Lovell JF, Yang M, Ding L, et al. (2009). Biomimetic nanocarrier for direct cytosolic drug delivery. Angew Chem Int Ed Engl, 48:9171-9175. [DOI] [PubMed] [Google Scholar]
- [224].Zhang M, He J, Jiang C, Zhang W, Yang Y, Wang Z, et al. (2017). Plaque-hyaluronidase-responsive high-density-lipoprotein-mimetic nanoparticles for multistage intimal-macrophage-targeted drug delivery and enhanced anti-atherosclerotic therapy. Int J Nanomedicine, 12:533-558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [225].Zhao Y, Jiang C, He J, Guo Q, Lu J, Yang Y, et al. (2017). Multifunctional Dextran Sulfate-Coated Reconstituted High Density Lipoproteins Target Macrophages and Promote Beneficial Antiatherosclerotic Mechanisms. Bioconjug Chem, 28:438-448. [DOI] [PubMed] [Google Scholar]
- [226].Zhao Y, Gao H, He J, Jiang C, Lu J, Zhang W, et al. (2018). Co-delivery of LOX-1 siRNA and statin to endothelial cells and macrophages in the atherosclerotic lesions by a dual-targeting core-shell nanoplatform: A dual cell therapy to regress plaques. J Control Release, 283:241-260. [DOI] [PubMed] [Google Scholar]
- [227].Jiang C, Qi Z, He W, Li Z, Tang Y, Wang Y, et al. (2019). Dynamically enhancing plaque targeting via a positive feedback loop using multifunctional biomimetic nanoparticles for plaque regression. J Control Release, 308:71-85. [DOI] [PubMed] [Google Scholar]
- [228].Zhao Y, Imura T, Leman LJ, Curtiss LK, Maryanoff BE, Ghadiri MR (2013). Mimicry of high-density lipoprotein: functional peptide-lipid nanoparticles based on multivalent peptide constructs. J Am Chem Soc, 135:13414-13424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [229].Guo Y, Yuan W, Yu B, Kuai R, Hu W, Morin EE, et al. (2018). Synthetic High-Density Lipoprotein-Mediated Targeted Delivery of Liver X Receptors Agonist Promotes Atherosclerosis Regression. EBioMedicine, 28:225-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [230].Thaxton CS, Rink JS, Naha PC, Cormode DP (2016). Lipoproteins and lipoprotein mimetics for imaging and drug delivery. Adv Drug Deliv Rev, 106:116-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [231].Zhu C, Xia Y (2017). Biomimetics: reconstitution of low-density lipoprotein for targeted drug delivery and related theranostic applications. Chem Soc Rev, 46:7668-7682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [232].Tauchi Y, Zushida L, Chono S, Sato J, Ito K, Morimoto K (2001). Effect of dexamethasone palmitate-low density lipoprotein complex on cholesterol ester accumulation in aorta of atherogenic model mice. Biol Pharm Bull, 24:925-929. [DOI] [PubMed] [Google Scholar]
- [233].Tauchi Y, Takase M, Zushida I, Chono S, Sato J, Ito K, et al. (1999). Preparation of a complex of dexamethasone palmitate-low density lipoprotein and its effect on foam cell formation of murine peritoneal macrophages. J Pharm Sci, 88:709-714. [DOI] [PubMed] [Google Scholar]
- [234].Jamil (1996). Methods in Enzymology, Volume 263, Plasma Lipoproteins, Part C, Quantitation. Edited by Bradley William A, Gianturco Sandra H, and Segrest Jere P. Academic Press, San Diego, 1995. 373 pp., $80.00. Anal Biochem, 238: 104-105. [DOI] [PubMed] [Google Scholar]
- [235].Versluis AJ, van Geel PJ, Oppelaar H, van Berkel TJ, Bijsterbosch MK (1996). Receptor-mediated uptake of low-density lipoprotein by B16 melanoma cells in vitro and in vivo in mice. Br J Cancer, 74:525-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [236].Lees RS, Garabedian HD, Lees AM, Schumacher DJ, Miller A, Isaacsohn JL, et al. (1985). Technetium-99m low density lipoproteins: preparation and biodistribution. J Nucl Med, 26:1056-1062. [PubMed] [Google Scholar]
- [237].Glickson JD, Lund-Katz S, Zhou R, Choi H, Chen IW, Li H, et al. (2008). Lipoprotein nanoplatform for targeted delivery of diagnostic and therapeutic agents. Mol Imaging, 7:101-110. [PubMed] [Google Scholar]
- [238].Jasanada F, Urizzi P, Souchard JP, Gaillard FL, Favre G, Nepveu F (1996). Indium-111 Labeling of Low Density Lipoproteins with the DTPABis(stearylamide): Evaluation as a Potential Radiopharmaceutical for Tumor Localization. Bioconjug Chem, 7:72-81. [DOI] [PubMed] [Google Scholar]
- [239].Tauchi Y, Zushida L, Yokota M, Chono S, Sato J, Ito K, et al. (2000). Inhibitory effect of dexamethasone palmitate-low density lipoprotein complex on low density lipoprotein-induced macrophage foam cell formation. Biol Pharm Bull, 23:466-471. [DOI] [PubMed] [Google Scholar]
- [240].Busatto S, Walker SA, Grayson W, Pham A, Tian M, Nesto N, et al. (2020). Lipoprotein-based drug delivery. Adv Drug Deliv Rev, 159:377-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [241].Harisa GI, Alanazi FK (2014). Low density lipoprotein bionanoparticles: From cholesterol transport to delivery of anti-cancer drugs. Saudi Pharm J, 22:504-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [242].Nikanjam M, Gibbs AR, Hunt CA, Budinger TF, Forte TM (2007). Synthetic nano-LDL with paclitaxel oleate as a targeted drug delivery vehicle for glioblastoma multiforme. J Control Release, 124:163-171. [DOI] [PubMed] [Google Scholar]
- [243].Kim J-H, Kim Y, Bae KH, Park TG, Lee JH, Park K (2015). Tumor-targeted delivery of paclitaxel using low density lipoprotein-mimetic solid lipid nanoparticles. Mol Pharm, 12:1230-1241. [DOI] [PubMed] [Google Scholar]
- [244].Kopecka J, Campia I, Olivero P, Pescarmona G, Ghigo D, Bosia A, et al. (2011). A LDL-masked liposomal-doxorubicin reverses drug resistance in human cancer cells. J Control Release, 149:196-205. [DOI] [PubMed] [Google Scholar]
- [245].D Lima A, Hua N, C Maranhão R, A Hamilton J (2017). Evaluation of atherosclerotic lesions in cholesterol-fed mice during treatment with paclitaxel in lipid nanoparticles: a magnetic resonance imaging study. J Biomed Res, 31:116-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [246].Freitas SCMP, Tavares ER, Silva BMO, Meneghini BC, Kalil-Filho R, Maranhão RC (2018). Lipid core nanoparticles resembling low-density lipoprotein and regression of atherosclerotic lesions: effects of particle size. Braz J Med Biol Res, 51:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [247].Daminelli EN, Martinelli AEM, Bulgarelli A, Freitas FR, Maranhão RC (2016). Reduction of Atherosclerotic Lesions by the Chemotherapeutic Agent Carmustine Associated to Lipid Nanoparticles. Cardiovasc Drugs Ther, 30:433-443. [DOI] [PubMed] [Google Scholar]
- [248].Lu T, Yam L, Nan Z, Tat H, Uhrich KE (2004). Amphiphilic Scorpion-like Macromolecules: Design, Synthesis, and Characterization. Macromolecules, 37:538-543. [Google Scholar]
- [249].Iverson NM, Sparks SM, Demirdirek B, Uhrich KE, Moghe PV (2010). Controllable inhibition of cellular uptake of oxidized low-density lipoprotein: structure-function relationships for nanoscale amphiphilic polymers. Acta Biomater, 6:3081-3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [250].Lewis DR, Petersen LK, York AW, Zablocki KR, Joseph LB, Kholodovych V, et al. (2015). Sugar-based amphiphilic nanoparticles arrest atherosclerosis in vivo. Proc Natl Acad Sci U S A, 112:2693-2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [251].Petersen LK, York AW, Lewis DR, Ahuja S, Uhrich KE, Prud'homme RK, et al. (2014). Amphiphilic nanoparticles repress macrophage atherogenesis: novel core/shell designs for scavenger receptor targeting and down-regulation. Mol Pharm, 11:2815-2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [252].Thaxton CS, Rink JS, Naha PC, Cormode DP (2016). Lipoproteins and lipoprotein mimetics for imaging and drug delivery. Adv Drug Deliv Rev, 116-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [253].Zhu C, Xia Y (2017). Biomimetics: reconstitution of low-density lipoprotein for targeted drug delivery and related theranostic applications. Chem Soc Rev, 46:7668-7682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [254].Pillai SC, Borah A, Jacob EM, Kumar DS (2021). Nanotechnological approach to delivering nutraceuticals as promising drug candidates for the treatment of atherosclerosis. Drug Deliv, 28:550-568. [DOI] [PMC free article] [PubMed] [Google Scholar]