Abstract
There has been a surge in vaccine hesitancy following the Coronavirus pandemic. This study measured the prevalence of and identified factors associated with vaccine hesitancy and social media use. An online survey was administered (n = 1050) between May and July 2021. Chi-square tests were used to examine bivariate associations with vaccine hesitancy (partially vaccinated and unvaccinated participants). Logistic regression was used to identify associations between social media use and vaccine hesitancy. Chi-square tests showed women (69.7% vs 28.2% men, padjusted = .002), African American participants (52.3% vs 17.8% white, padjusted < .001), high school diploma (54.4% vs 38.6% college degree, padjusted < .001), political unaffiliated (15.8% vs 14.5% republican, padjusted < .001), Muslim (10.0% vs 0% Jewish, padjusted < .001), and never married/single (53.9% vs 17.0% married, padjusted < .001) were more likely to be vaccine hesitant. Controlling for all demographic variables (age, race, gender, and education), more frequent use of social media for reading news was associated with lower vaccine hesitancy (OR 0.35, 99% CI 0.20, 0.63, p < 0.001). However, using social media as a source of vaccine information without any other trusted source (health department, doctor, CDC,) was associated with higher odds of being vaccine hesitant (OR 2.00, 99% CI 1.15, 3.46, p = 0.001). People who use social media without referencing trusted sources may be particularly vulnerable to disinformation or vaccine hesitant persons are more likely exposed to non-trusted social media sites as their only information source.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10900-022-01081-9.
Keywords: COVID-19 pandemic, Vaccine hesitancy, Social media, Health disparity, Public health
Introduction
Vaccination has been an essential tool used to fight infectious disease for decades. Diseases such as smallpox and polio have been eradicated after successful worldwide vaccination efforts. In 2019, the COVID-19 virus emerged and has since caused a global pandemic. In response to this crisis, COVID-19 vaccines were developed. Although these vaccines are considered safe, some of the country’s most vulnerable populations (low-income, racial and ethnic minority groups, women and persons without a college degree) responded to these vaccines with distrust [1, 2]. According to the World Health Organization, vaccine hesitancy is indecision, uncertainty, delay and refusal of vaccination despite the availability of vaccination services. Many studies address vaccine hesitancy in general and several factors have been identified in the literature as influencing vaccine hesitancy. These factors include social media, race, gender, age, education, income, family, religion, politics, personal beliefs, trust and experience with the healthcare system [3–7].
Race has consistently been identified as a factor associated with vaccine hesitancy [1, 3, 7]. African Americans in particular distrust the government and the healthcare system [6]. Misinformation about vaccine safety and lack of trust in the healthcare system is also a factor associated with hesitancy even among healthcare workers [7–10]. In fact, a correlation was found between healthcare worker’s belief in vaccine safety and their vaccine recommendations [10]. Other factors such as being female, being younger age, having less education, having lower income, belonging to religious and political groups have all been associated with lower vaccine acceptance rates [1, 2, 7].
Social media use was also identified as a factor influencing vaccine hesitancy [9, 11]. According to Thaker [6], vaccine disinformation is deliberately spread across social media platforms. While most social media sites contain vaccine disinformation and anti-vaccination posts, social media platforms vary in the degree of vaccine disinformation shared with the public [6, 11]. Although vaccine hesitancy existed prior to the COVID-19 pandemic, there has been a recent change in vaccine hesitancy following the Emergency Use Authorizations for the COVID-19 vaccines in the United States [12]. Dube suggests, consuming social media has increased mistrust towards vaccines [12]. Most adults (98%) use social media and it only takes a few minutes of exposure to disinformation on social media to influence vaccine hesitancy. Furthermore, the most vaccine hesitant groups (for COVID-19 vaccines) are frequently the most vulnerable [1, 2, 8]. Therefore, it is imperative for public health officials to understand vaccine hesitancy as it relates to the COVID-19 vaccines and how social media use influences vaccine uptake [6, 11, 13].
This study identified factors associated with vaccine hesitancy, measured activity levels on social media platforms and examined how differences in vaccine information source (family, friends, social media, trusted sources) influence hesitancy. To understand how social media exposure influences vaccine behavior. The objectives of this study were: to measure the prevalence of vaccine hesitancy among vulnerable populations, identify factors associated with vaccine hesitancy among this population, compare activity levels on social media platforms, and determine how vaccine information source (family, friends, social media, trusted sources) influence hesitancy. We hypothesized; (1) More frequent social media use is associated with increased vaccine hesitancy. (2) Vaccine information source will influence vaccine hesitancy (obtaining vaccine information from social media sites will increase vaccine hesitancy).
Methods
The Philadelphia Department of Public Health Division of COVID Containment developed a questionnaire (The Vaccine Hesitancy and Social Media Use Survey). This questionnaire was a modified version of “The PEW Social Media Use 2021” and “The Social Networking Usage Questionnaire” [13, 14]. This questionnaire was administered from mid-May to early July 2021 and data were collected anonymously via a public self-administered online survey through Qualtrics Panels (a third-party survey panels provider) [1, 15]. The survey instrument captured participants’ demographic information, social media use, sources of vaccine information and vaccine hesitancy. Survey quotas based on race, age and gender were established and participants were selected based on demographics that were representative of Philadelphia’s racial and ethnic demographic distribution (African–American 40%; White 35%; Hispanic 15%; Asian 7%; Other 3%), age (at least 50% age 18 to 44), gender (no more than 50% Females) [16].
A total of 4115 survey responses were attempted online. Survey responses that met our quota and inclusion criteria were included for our data analyses (n = 1050). Inclusion criteria were as follows; (1) persons residing in zip codes located in Philadelphia, (2) ≥ 18 years old, and (3) persons who committed to giving their best answers). The rest of the survey responses (n = 3065) were terminated for not meeting our inclusion criteria (listed above) or for failing the Qualtrics quality check. Qualtrics quality check excluded responses for the following: (1) finishing the survey more than two standard deviations from the mean duration and (2) being identified as a possible bot or duplicate responses). Among the 3065 responses that were excluded, 2402 were terminated by our screening questions (65 were over the quota; 2064 were not located inside a Philadelphia zip code; 17 were under 18 years old; 256 did not commit to provide the best answers). A total of 663 were detected and excluded by Qualtrics quality check system (199 duplicate responses; 49 possible bots; 26 speeders; 389 incomplete).
The survey instrument captured participants’ activity on each social media platform (Twitter, Instagram, Facebook, Snapchat, WhatsApp, LinkedIn, Reddit, Nextdoor, Youtube, Pinterest and TikTok), frequency of use (once a day or more/less than once a day), source of vaccine information (Social Media, Health Care Provider, Centers for Disease Control Website (CDC), City of Philadelphia Website, Local News Major News Network, Friends/Family, Other Website, or Other), Social Media use for Reading News (Always, Sometimes, Rarely/Never), and Vaccine hesitancy (unvaccinated, received 1 dose of a 2 dose vaccine and did not schedule a second dose, unvaccinated and not having any plans to get vaccinated). Trusted sources were Health Care Provider, Centers for Disease Control Website (CDC) and the City of Philadelphia Website. Participants were allowed to choose more than one social media platform and more than one vaccine information source. The complete survey is available in the Supplementary Materials (Table S1).
Data Analysis
Chi-square tests of independence were used to assess the relationship between all variables (each demographic variable: gender, race, age, education, political affiliation, religion, household status, etc.; social media use variables) and vaccine hesitancy. All analyses were based on two-sided P-values, which statistical significance define by p < 0.01. When the expected frequencies smaller than five, Fisher’s exact test were applied to examine the statical significance [17]. A total of 33 chi-square tests were calculated; for multiple comparisons corrections, we used the Benjamini–Hochberg procedure to decrease the false positive rate/type I error. To present the results of the Benjamini–Hochberg procedure in simple manner, adjusted p values are reported and shown in Tables 1 and 2 [18].
Table 1.
Demographic, vaccine information source and social media use variables
| Demographic variables | Overall N = 1050 (%)a | Vaccine information sources variables | Overall N = 1051 | |
|---|---|---|---|---|
| Gender | Social media platform | Yes | No | |
| Female | 630 (60.0%) | 601 (61.0%) | 410 (39.0%) | |
| Male | 401 (38.2%) | 830 (79.0%) | 220 (21.0%) | |
| Other | 19 (1.8%) | 812 (77.3%) | 238 (22.7%) | |
| Age | Snapchat | 581 (55.3%) | 469(44.7%) | |
| 18–24 | 279 (26.6%) | Youtube | 966 (92.0%) | 84 (8.0%) |
| 25–34 | 282 (26.9%) | 452 (43.0%) | 598 (57.0%) | |
| 35–44 | 239 (22.8%) | 487 (46.4%) | 563 (53.6%) | |
| 45–54 | 104 (9.9%) | 456 (38.6%) | 645 (61.4%) | |
| 55–64 | 79 (7.5%) | 283 (27.0%) | 767 (73.0%) | |
| 66 or older | 67 (6.4%) | TikTok | 517 (49.2%) | 533 (50.8%) |
| Race and ethnicity | Nextdoor | 167 (15.9%) | 883 (84.1%) | |
| African-American | 392 (37.3%) | Vaccine information source non trusted | ||
| Asian | 63 (6.0%) | Yes | No | |
| White | 328 (31.2%) | Friends | 386 (36.8%) | 664 (63.2%) |
| Hispanic | 251 (23.9%) | Family | 533 (50.8%) | 517(49.2%) |
| Other/unknown | 16 (1.5%) | Social media | 352 (33.5%) | 698 (66.5%) |
| Religion | Major News Networks | 374 (35.6%) | 667 (64.4%) | |
| Agnostic | 28 (2.7%) | Other Website | 65 (6.2%) | 985 (93.8%) |
| Atheist | 30 (2.9%) | Vaccine information source trusted | ||
| Buddhist | 17 (1.6%) | Yes | No | |
| Catholic | 178 (17%) | Health care provider | 514 (49.0%) | 536 (51.0%) |
| Christian | 444 (42.3%) | City of Philadelphia | 276 (26.3%) | 774 (73.7%) |
| Hindu | 6 (0.6%) | CDC website | 325 (31.0%) | 725 (69.0%) |
| Jewish | 29 (2.8%) | Use social media for reading news | ||
| Muslim | 69 (6.6%) | Always | 326 (31.0%) | |
| None | 180 (17.1%) | Sometimes | 489 (46.6%) | |
| Other | 69 (6.6%) | Rarely/never | 235 (22.4%) | |
| Relationship status | Use social media for sharing new ideas | |||
| Divorced | 43 (4.1%) | Always | 317(30.2%) | |
| Married | 257 (24.5%) | Sometimes | 446(42.5%) | |
| Never married/living with someone | 158 (15.0%) | Rarely/never | 287(27.3%) | |
| Never married/single | 438 (41.7%) | Social media frequency of use | ||
| Separated | 37 (3.5%) | Several times a day | 689 (65.6%) | |
| Widowed | 17 (1.6%) | About once a day | 180 (17.1%) | |
| Education | A few times a week | 94 (9.0%) | ||
| High school graduate/trade school/GED | 379 (36.1%) | Every few weeks | 26 (2.5%) | |
| College degree | 469 (44.7%) | Less often | 34 (3.2%) | |
| Master’s degree or above | 202 (19.2%) | I don't know | 27 (2.6%) | |
| Political affiliation | ||||
| Democrat | 522 (49.7%) | |||
| Republican | 230 (21.9%) | |||
| Independent | 172 (16.4%) | |||
| Unaffiliated | 89 (8.5%) | |||
| Other | 37 (3.5%) | |||
This table displays percentages of demographic variables including race, gender, age, religious affiliation, relationship status and education; vaccine information source variables including social media sites, family, friends, other media, and trusted sources (Healthcare provider, CDC, Health department) and frequency of social media use
aThe survey was administered between May and July, 2021 (N = 1050)
Table 2.
Demographic and media variables significantly associated with vaccine hesitancy
| Demographic variables | Hesitancy N = 241 (%)b | No hesitancy N = 809 (%)b | Chi-square test adjusted p valuec | Media & vaccine information sources variables | Hesitancy N = 241 (%)b | No hesitancy N = 809 (%)b | Chi-square test adjusted p valuec | ||
|---|---|---|---|---|---|---|---|---|---|
| Gendera | .002 | Social Media Platform | Use | Do not use | Use | Do not use | |||
| Female | 168 (69.7%) | 462 (57.1%) | 115 (47.7%) | 126 (52.3%) | 525 (64.9%) | 284 (35.1%) | < .001 | ||
| Male | 68 (28.2%) | 333 (41.2%) | 168 (69.7%) | 73 (30.3%) | 644 (79.6%) | 165 (20.4%) | 0.003 | ||
| Other | 5 (2.1%) | 14 (1.7%) | Snapchat | 118(49.0%) | 123(51.0%) | 463(57.2%) | 346(42.8%) | 0.039d | |
| Agea | < .001 | 76 (31.5%) | 165 (68.5%) | 376 (46.5%) | 433 (53.5%) | < .001 | |||
| 18–24 | 92 (38.2%) | 187 (23.1%) | 59 (24.5%) | 182 (75.5%) | 346 (42.8%) | 463 (57.2%) | < .001 | ||
| 25–34 | 63 (26.1%) | 219 (27.1%) | 40 (16.6%) | 201 (83.4%) | 243 (30%) | 566 (70%) | < .001 | ||
| 35–44 | 35 (14.5%) | 204 (25.0%) | Nextdoor | 12 (5%) | 229 (95%) | 155 (19.2%) | 654 (80.8%) | < .001 | |
| 45–54 | 25 (10.4%) | 79 (9.8%) | Vaccine Information Source Non Trusted | Use | Do not use | Use | Do not use | ||
| 55–64 | 13 (5.4%) | 66 (8.2%) | |||||||
| 65 or older | 13 (5.4%) | 54 (6.7%) | Friends | 64 (26.6%) | 177 (73.4%) | 322 (39.8%) | 487 (60.2%) | < .001 | |
| Race and ethnicitya | < .001 | Family | 106 (44.0%) | 135 (56.0%) | 427 (52.8%) | 382 (47.2%) | 0.029d | ||
| African-American | 126 (52.3%) | 266 (32.9%) | Social Media | 104 (43.2%) | 137 (56.8%) | 248 (30.7%) | 561 (69.3%) | < .001 | |
| Asian | 5 (2.1%) | 58 (7.2%) | Major News Networks | 66 (27.4%) | 175 (72.6%) | 308 (38.1%) | 501 (61.9%) | .005 | |
| White | 43 (17.8%) | 285 (35.2%) | Other Website | 25 (10.4%) | 216 (89.6%) | 40 (4.9%) | 769 (95.1%) | 0.005 | |
| Hispanic | 62 (25.7%) | 189 (23.4%) | Vaccine Information Source Trusted | Use | Do not use | Use | Do not use | ||
| Other/unknown | 5 (2.1%) | 11 (1.4%) | |||||||
| Religion | < .001 | Health Care Provider | 92 (38.2%) | 149 (61.8%) | 422 (52.2%) | 387 (47.8%) | < .001 | ||
| Agnostic | 3 (1.2%) | 25 (3.1%) | City of Philadelphia | 29 (12%) | 212 (88%) | 247 (30.5%) | 562 (69.5%) | < .001 | |
| Atheist | 3 (1.2%) | 27 (3.3%) | CDC Website | 51 (21.2%) | 190 (78.8%) | 274 (33.9%) | 535 (66.1%) | < .001 | |
| Buddhist | 0 (0%) | 17 (2.1%) | Use Social Media for Reading News | ||||||
| Catholic | 34 (14.1%) | 144 (17.8%) | Hesitancy n = 241 (%) | No Hesitancy n = 809 (%) | < .001 | ||||
| Christian | 97 (40.2%) | 347 (42.9%) | Always | 49 (20.3%) | 277 (34.2%) | ||||
| Hindu | 1 (0.4%) | 5 (0.6%) | Sometimes | 116 (48.1%) | 373 (46.1%) | ||||
| Jewish | 0 (0%) | 29 (3.6%) | Rarely/Never | 76 (31.5%) | 159 (19.7%) | ||||
| Muslim | 24 (10.0%) | 45 (5.6%) | Use Social Media for Sharing New Ideas | ||||||
| None | 57 (23.7%) | 123 (15.2%) | < .001 | ||||||
| Other | 22 (9.1%) | 47 (5.8%) | Always | 47(19.5%) | 270(33.4%) | ||||
| Relationship status | < .001 | Sometimes | 112(46.5%) | 334(41.3%) | |||||
| Divorced | 10 (4.1%) | 33 (4.1%) | Rarely/never | 82(34.0%) | 205(25.3%) | ||||
| Married | 41 (17.0%) | 316 (39.1%) | |||||||
| Never married/living with someone | 42 (17.4%) | 116 (14.3%) | |||||||
| Never married/single | 130 (53.9%) | 308 (38.1%) | |||||||
| Separated | 13 (5.4%) | 24 (3.0%) | |||||||
| Widowed | 5 (2.1%) | 12 (1.5%) | |||||||
| Education | < .001 | ||||||||
| High school graduate/trade school/GED | 131 (54.4%) | 248 (30.6%) | |||||||
| College degree | 93 (38.6%) | 376 (46.5%) | |||||||
| Master’s degree or above | 17 (7.0%) | 185 (22.9%) | |||||||
| Political affiliation | |||||||||
| Democrat | 100 (41.5%) | 422 (52.2%) | < .001 | ||||||
| Republican | 35 (14.5%) | 195 (24.1%) | |||||||
| Independent | 51 (21.2%) | 121 (15.0%) | |||||||
| Unaffiliated | 38 (15.8%) | 51 (6.3%) | |||||||
| Other | 17 (7.1%) | 20 (2.5%) | |||||||
This table displays the demographic and media variables significantly associated with vaccine hesitancy
The survey was administered between May and July, 2021 (N = 1050)
aThe percentages of Gender, Age, Race and Ethnicity were collected based on quotas similar to the demographic make up of Philadelphia residents as stated in the Methods section
bSome percentages do not sum up to 100 because of rounding
cBased on Benjamin-Hochberg procedure, with adjusted p value < .01 considered significant
dVariables are significant at adjusted p value < .05
Multivariate logistic regression models were built to understand the dynamics between social media use variable and vaccine hesitancy and included the significant variables (gender, race, age, education, social media use) as covariates that were already shown to be related to the outcome (vaccine hesitancy). We considered p < 0.01 to be significant and reported 99% Confidence Interval for odds ratios. Cramer’s V test (a correlation test for categorical variables) was conducted among independent variables to ensure no multicollinearity was observed in the regression models [19]. All results were below 0.28.
Results
Demographic Factors Associated with Vaccine Hesitancy
Overall, several demographic and social media factors were significantly associated with vaccine hesitancy. A chi-square test of independence showed gender, age, race, education level, relationship status, political affiliation, and religious affiliation all had a significant association with vaccine hesitancy (padjusted < 0.001) (See Table 2). A surprising finding was that religious affiliation can have both a negative and a positive correlation to vaccine hesitancy. Participants who identified as Jewish are significantly less likely to be hesitant (padjusted < 0.001). Whereas participants who identified as Muslim other religion or no religious affiliation are significantly more likely to be hesitant (padjusted < 0.001). Receiving vaccine information from friends (padjusted < 0.001) and family were found to be significant (padjusted = 0.029) (See Table 2).
Vaccine Hesitancy and Social Media Use
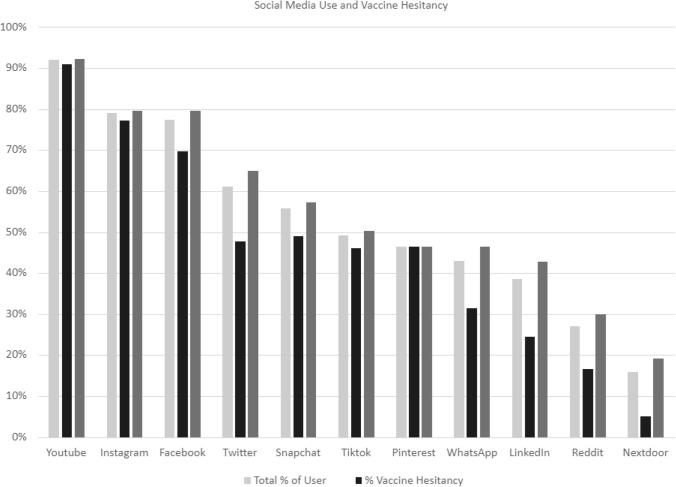
Among the Never Vaxer (NV) hesitancy group “No, I do not want to be vaccinated now or at any-time in the future”, Instagram is the second most widely used platform among the age group 18–34 in both the (NV) and the (SV) “No, I do not want to be vaccinated at this time” group. Among the age group 35 and 54, Facebook was the second most popular platform after YouTube in both the (NV) and in the (SV) groups. Among age 55 or older, YouTube and Facebook remain the most popular platforms in both the NV and SV groups (Figs. 1, 2).
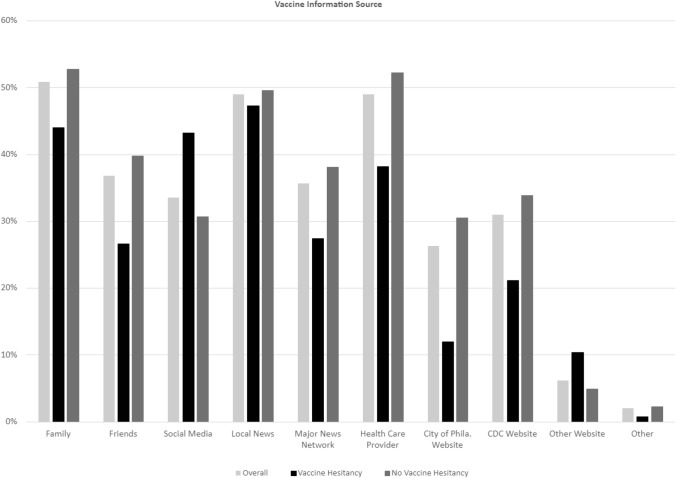
Fig. 1.
Vaccine information. Source This graph shows the relationship between vaccine information source and vaccine hesitancy. Obtaining vaccine information from non-trusted social media sites is predictive of vaccine hesitancy
Fig. 2.
Social media use and vaccine hesitancy. This graph shows the relationship between social media use and vaccine hesitancy
Our results did not support hypothesis number 1. More frequent social media use is associated with increased vaccine hesitancy. Controlling for all demographic variables, more frequent use of social media for reading news was associated with lower odds of being vaccine hesitancy (OR 0.35, 99% CI 0.20, 0.63, p < 0.001). Therefore, the data are not shown. The data does however support hypothesis number 2. Vaccine information source does influence vaccine hesitancy (obtaining vaccine information from non-trusted social media sites will increase vaccine hesitancy), Using social media as a source of vaccine information without any other trusted source (health department, doctor, CDC,) was associated with higher odds of being vaccine hesitant (OR 2.00, 99% CI 1.15, 3.46, p = 0.001) (See Table 3).
Table 3.
Multivariable logistic regression results
| Independent variable | Adjusted odds ratio (99% Confidence Interval) [P Value] | |
|---|---|---|
| Model 1: Use Social Media for Vaccine Information | Model 2: Frequency of Using Social Media for Reading News | |
| Age | ||
| 18–24 | 1 [Reference] | 1 [Reference] |
| 25–34 | 0.79 (0.46, 1.36) [0.270] | 0.87 (0.50, 1.49) [0.495] |
| 35–44 | 0.61 (0.32, 1.14) [0.041] | 0.62 (0.33, 1.16) [0.048] |
| 45–54 | 0.91 (0.44, 1.89) [0.748] | 0.81 (0.39, 1.68) [0.45] |
| 55–64 | 0.54 (0.22, 1.33) [0.078] | 0.44 (0.18, 1.08) [0.018] |
| 65+ | 0.75 (0.30, 1.91) [0.433] | 0.53 (0.21, 1.36) [0.085] |
| Race | ||
| White | 1 [Reference] | 1 [Reference] |
| African American | 1.99 (1.12, 3.52) [0.002] | 2.15 (1.21, 3.82) [0.001] |
| Asian | 0.46 (0.12, 1.74) [0.136] | 0.47 (0.12, 1.79) [0.147] |
| Hispanic | 1.41 (0.75, 2.66) [0.162] | 1.56 (0.82, 2.95) [0.073] |
| Other/unknown | 2.41 (0.51, 11.41) [0.144] | 2.77 (0.58, 13.16) [0.092] |
| Gender | ||
| Female | 1 [Reference] | 1 [Reference] |
| Male | 0.87 (0.55, 1.40) [0.461] | 0.87 (0.54 1.39) [0.447] |
| Other | 0.64 (0.15, 2.66) [0.415] | 0.6 (0.14, 2.61) [0.375] |
| Highest education | ||
| College degree | 1 [Reference] | 1 [Reference] |
| High school degree | 1.72 (1.11, 2.65) [0.001] | 1.7 (1.10, 2.63) [0.002] |
| Master’s or above degree | 0.43 (0.20, 0.90) [0.003] | 0.42 (0.20, 0.89) [0.003] |
| Use social media for vaccine informationa | ||
| Not use social media | 1 [Reference] | |
| Use social media with trusted sources | 1.16 (0.69, 1.93) [0.458] | |
| Use social media alone or with other non-trusted sources | 2 (1.15, 3.46) [0.001] | |
| Using social media for reading news | ||
| Rarely/never | 1 [Reference] | |
| Always | 0.35 (0.20, 0.63) [<0.001] | |
| Sometimes | 0.65 (0.40, 1.07) [0.027] | |
Model 1 examined the association between vaccine hesitancy and social media use for vaccine information while controlling the selected variables constanta; Model 2 examined the association between vaccine hesitancy and the frequency of using social media for reading news while controlling the selected variables constanta (N = 1050)
Predictor Variables used in the regression models include Age, Race, Gender, and Highest Education
aVariables were regrouped into 3 categories (do not use social media, use social media with trusted sources, use social media alone or with other non-trusted sources) to better understand how social media use influences vaccine hesitancy
Discussion
The purpose of this study was to measure the prevalence of vaccine hesitancy among vulnerable populations, identify factors associated with vaccine hesitancy among this population, compare activity levels on social media platforms, and determine how vaccine information source (family, friends, social media, trusted sources) influence s hesitancy. We hypothesized that more frequent social media use is associated with vaccine hesitancy. Our findings did not support this hypothesis. This may be because we had insufficient data to detect an association. Our findings did support hypothesis number 2. Our study found that vaccine information source (non-trusted social media sites) influences vaccine hesitancy. We found that frequenters of non- trusted sites are more likely to be hesitant and visitors of trusted sites such as CDC, PDPH and healthcare providers, are less likely to be hesitant. Our results indicate that social media can be a good source of vaccine information when the information is delivered by someone considered to be a trusted source in the community [8]. Health care providers, health departments and the CDC are considered trusted sources [11]. Trusted social media sites provide accurate fact-based information. Whereas many non-trusted social media sites do not provide factual-information or scientific evidence supporting their claims [11]. Our findings suggest that people who use social media alone without referencing trusted sources may be particularly vulnerable to disinformation or that vaccine hesitant persons are more likely to have been exposed to non-trusted social media sites as their only source of vaccine information. hesitant are especially drawn to social media as their only information source. Furthermore, social media users may engage in confirmation bias by seeking out vaccination information that supports their pre-conceived beliefs. Additional studies reveal that many social media sites contain vaccine disinformation and anti-vaccination posts [11]. Pro and Anti-vaccination social media users are often siloed on social media and anti-vaccination post on social media is often re-posted or re-tweeted more frequently that neutral posts and tweets [11, 20, 21]. Although, the effects of viewing non-factual vaccine information or even vaccine disinformation information on less trust-worthy social media sites appears to be mitigated in better-educated, older, less racially diverse social media users who also view vaccine information on trusted social media sites.
While viewing vaccine information on trusted social media sites may dilute the effects of vaccine disinformation for some, younger adults, African American persons, and less educated cohorts appear to be more susceptible to vaccine disinformation [11] found that some social media users, such as those who are less educated are highly susceptible to social media campaigns. Women, African American persons, persons ages (18–44), less educated persons, those who identify as Muslim, no religious affiliation or other, those who are single never married, single living with someone, or separated and those who are politically unaffiliated are more likely to be hesitant. This finding has important implications. There is a correlation between age and social media use. Over 80% of adults between the ages of 19 and 34 use social media and adults ages 18 to 39 display greater social media use when compared to other age groups [13]. Furthermore, the Household Pulse Survey Covid-19 Vaccination Tracker found that persons aged 25 to 39 display greater vaccine hesitancy for COVID-19 vaccine uptake than any other age group. African American persons have a long history of being victims of systemic racism and of being ignored or exploited by the government and the medical community. This lived experience fuels African American persons’ distrust in the vaccine and is often cited as the reason for hesitancy [8, 22]. Reasons for hesitancy in less educated cohorts may have more to do with health literacy. Some persons may have difficulty understanding the science or navigating the ever- changing COVID-19 guidelines and may be more responsive to less factual emotional appeals on social media [11]. Thus, the need for pro-active simple easy to read social media content about vaccine safety, efficacy, and side effects [11].
While talking with family and friends about vaccines is associated with decreased vaccine hesitancy, being single never married, single living with someone, or separated is associated with increased vaccine hesitancy. In other words, our findings support the notion that social pressure is effective. Family and friends (social pressure) can convince their loved ones to get vaccinated [8]. It may also be the cases that persons who live alone or who are unmarried may experience less social pressure in the home which may explain why they are more likely to be hesitant. Our study also found that politically unaffiliated persons and Independents are more likely to be hesitant. This finding is not supported in the literature. A recent study by Kaiser Family Foundation found that Republicans were more likely to be vaccine hesitant [23]. Persons who identify as Jewish or Buddhist are least likely to be hesitant and persons who identify as Muslim or other religion are more likely to be hesitant. Faith Based Organizations (FBOs) can be effective facilitators in reducing vaccine hesitancy and increasing vaccine uptake because clergy members have significant influence on congregation members’ health behaviors and FBOs provide the type of social support that encourages and significantly improves healthy behaviors [24]. Additional studies demonstrate that most people would like to hear information about vaccine efficacy from scientists and not from lay men or community leaders [11]. Therefore, addressing the concerns that specific communities of faith have about the COVID-19 vaccines is a critical step in the fight to reduce vaccine hesitancy [25–27].
As public health officials if we want to reduce vaccine hesitancy, we must address hesitancy where it occurs. Identifying the specific demographic make-up of vaccine hesitant populations can inform future targeted public health campaigns. Understanding that racial groups are not monolithic and that there is no one size fits all is key. People within the same racial group have different perspectives and motives for hesitancy across other demographics. There is a need to specifically target the reason for hesitancy within each of these subgroups. Lower vaccination rates in African Americans and in low-income communities can increase health inequities and lead to further disparities. Therefore, efforts to combat vaccine hesitancy must be tailored to fit each of these subgroups. Reducing vaccine hesitancy is a necessary step toward reducing health disparities resulting from the COVID-19 virus and achieving health equity [1, 2]. If we can increase vaccine uptake in vulnerable communities, we can move one step closer to achieving herd immunity.
Implications for Policy and Practice
Our research shows several factors are significantly associated with vaccine hesitancy. Age (18 to 34), Women, African American persons, persons without a bachelor’s degree and individuals who use social media for vaccine information are more likely to be hesitant.
Over 93% of the participants surveyed use social media, over 98% of vaccine hesitant participants use social media, and persons aged (18 to 39) use social media more than any other age group.
Based on our study results it imperative that public health entities reduce vaccine hesitancy by mounting targeted campaigns on social media platforms in populations where hesitancy frequently occurs.
Social media platforms vary in the degree of vaccine disinformation shared with the public, therefore, there is a need for proactive communication strategies to respond to misinformation on social media by specifically tailoring communications to each social media platform and its users [11].
There are race-based inequities in the healthcare system [8] and a general mistrust of the government. Thus, sincere long-term efforts should be made to establish trust between the most vulnerable communities, the government and health care system by establishing permanent relationships with community-based organizations that persist after the pandemic.
Study Limitations
The data collection of the study was conducted by a Qualtrics panel survey. That implies our survey may not adequately sample persons with low technological abilities. In addition, our study was cross-sectional and collected at one specific time. Factors influencing vaccine hesitancy may change over time.
Recommendations for Future Studies
We offer the following recommendations to reduce vaccine hesitancy and to increase vaccine equity.
We plan a future study with a larger sample size to better understand how frequency of social media engagement influences vaccine hesitancy.
We also plan a future study examining factors influencing booter hesitancy.
Additional studies are warranted to determine the effect of full FDA approval of the COVID-19 vaccines and the implementation of mandates on vaccine changes the associations observed in our study.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to acknowledge Dr. Hannah Lawman for her guidance and support.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by C-CC, LA and BB. The first draft of the manuscript was written by LAl. All authors LA, FAF, C-CC, and BB commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This project was supported by the Centers for Disease Control and Prevention of the U.S. Department of Health and Human Services as part of a financial assistance award (Grant # NU50CK000521-01) funded by CDC/HHS. The contents are those of the author (S) and do not necessarily represent the official views of, nor the endorsement, by CDC/HHS, or the US Government.
Data Availability
The data that support the findings of this study are available from [The Philadelphia Department of Public Health] but restrictions apply to the availability of these data and are not publicly available. Data are however available from the authors upon reasonable request and with permission of [The Philadelphia Department of Public Health].
Code Availability
Not Applicable.
Declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical Approval
This study was reviewed by The City of Philadelphia Institutional Review Board and was determined to be exempt from Institutional Review Board review based upon the following Federal Regulation that Information…is recorded by the investigator in such a manner that the identity of the human subjects cannot readily be ascertained directly or through identifiers linked to the subjects, the investigator does not contact the subjects, and the investigator will not re-identify subjects.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not Applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Lola Al-Uqdah, Email: Lola.al-uqdah@phila.gov, Email: laluqdah67@gmail.com.
F. Abron Franklin, Email: Frank.Franklin@phila.gov.
Chu-Chuan Chiu, Email: Chu-Chuan.Chiu@phila.gov.
Brianna N. Boyd, Email: brianna.boyd@phila.gov
References
- 1.Ciardi F, Menon V, Jensen JL, et al. Knowledge, attitudes and perceptions of COVID-19 vaccination among healthcare workers of an inner-city hospital in New York. Vaccines. 2021;9(7):713. doi: 10.3390/vaccines9050516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. The Lancet Regional Health-Europe. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Office of the Assistant Secretary for Planning and Evaluation . COVID-19 vaccine hesitancy: Demographic factors, geographic patterns, and changes over time. U.S. Department of Health and Human Services; 2021. [Google Scholar]
- 4.MacDonald NE, SAGE Working Group on Vaccine Hesitancy Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Soares P, Rocha JV, Moniz M, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021;9(3):300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thaker J, Subramanian A. Exposure to COVID-19 vaccine hesitancy is as impactful as Vaccine misinformation in inducing a decline in vaccination intentions in New Zealand: Results from pre-post between-groups randomized block experiment. Frontiers in Communication. 2021 doi: 10.3389/fcomm.2021.721982. [DOI] [Google Scholar]
- 7.Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bogart LM, Ojikutu BO, Tyagi K, et al. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among Black Americans living with HIV. Journal of Acquired Immune Deficiency Syndromes. 2021;86(2):200. doi: 10.1097/QAI.0000000000002570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schuster M, Eskola J, Duclos P, SAGE Working Group on Vaccine Hesitancy Review of vaccine hesitancy: Rationale, remit, and methods. Vaccine. 2015;33(34):4157–4160. doi: 10.1016/j.vaccine.2015.04.035. [DOI] [PubMed] [Google Scholar]
- 10.Verger P, Fressard L, Collange F, et al. Vaccine hesitancy among general practitioners and its determinants during controversies: A national cross-sectional survey in France. eBioMedicine. 2015;2(8):891–897. doi: 10.1016/j.ebiom.2015.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Human Vaccines and Immunotherapeutics. 2020;16(11):2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dube E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy. Human Vaccines and Immunotherapeutics. 2013;9(8):1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auxier, B., & Anderson, M. (2021). Social media use in 2021. The Pew Research Center. Retrieved from https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/.
- 14.Gupta S, Bashir L. Social networking usage questionnaire: Development and validation in an Indian higher education context. Turkish Online Journal of Distance Education. 2018;19(4):214–227. doi: 10.17718/tojde.471918. [DOI] [Google Scholar]
- 15.Qualtrics software, Version December 2021 of Qualtrics. Copyright © 2021 Qualtrics. Qualtrics and all other Qualtrics product or service names are registered trademarks or trademarks of Qualtrics. Retrieved from https://www.qualtrics.com.
- 16.United States Census Bureau. (2019). QuickFacts. Retrieved from https://www.census.gov/quickfacts/philadelphiacitypennsylvania.
- 17.Kim H. Statistical notes for clinical researchers: Chi-squared test and Fisher's exact test. Restorative Dentistry Endodontics. 2017;42(2):152. doi: 10.5395/rde.2017.42.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Statistical Methodology) 1995;57(1):289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 19.Cramér, H. (1946). Mathematical methods of statistics. Princeton University Press 282. ISBN 0-691-08004-6.
- 20.Basch CH, Meleo-Erwin Z, Fera J, Jaime C, Basch CE. A global pandemic in the time of viral memes: COVID-19 vaccine misinformation and disinformation on TikTok. Human Vaccines & Immunotherapeutics. 2021;17(8):2373–2377. doi: 10.1080/21645515.2021.1894896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blankenship EB, Goff ME, Yin J, et al. Sentiment, contents, and retweets: A study of two vaccine-related Twitter datasets. The Permanente Journal. 2018;22:17–138. doi: 10.7812/TPP/17-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griffith J, Marani H, Monkman H. COVID-19 vaccine hesitancy in Canada: Content analysis of tweets using the Theoretical Domains Framework. Journal of medical Internet research. 2021;23(4):e26874. doi: 10.2196/26874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamel, L., Lopes, L., & Sparks, G. (2021). Kaiser Family Foundation COVID-19 vaccine monitor: October 2021. Kaiser Family Foundation. Retrieved from https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-october-2021/.
- 24.Martinez SM, Arredondo EM, Roesch S. Physical activity promotion among churchgoing Latinas in San Diego, California: Does neighborhood cohesion matter? Journal of Health Psychology. 2012;18(10):1319–1329. doi: 10.1177/1359105312462433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Debnam K, Holt CL, Clark EM, Roth DL, Southward P. Relationship between religious social support and general social support with health behaviors in a national sample of African Americans. Journal of Behavioral Medicine. 2012;35(2):179–189. doi: 10.1007/s10865-011-9338-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krause N. Church-based social relationships and change in self - esteem over time. Journal for the Scientific Study of Religion. 2009;48(4):756–773. doi: 10.1111/j.1468-5906.2009.01477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whitney E. Culturally tailoring a patient empowerment and diabetes education curriculum for the African American church. The Diabetes Educator. 2017;43(5):441–448. doi: 10.1177/0145721717725280. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from [The Philadelphia Department of Public Health] but restrictions apply to the availability of these data and are not publicly available. Data are however available from the authors upon reasonable request and with permission of [The Philadelphia Department of Public Health].
Not Applicable.