Abstract
Background
COVID-19 vaccine uptake by healthcare workers (HCWs) is critical to protect HCWs, the patients they care for, and the healthcare infrastructure. Our study aims to examine the actual COVID-19 vaccination rate among HCWs and identify risk factors associated with vaccine nonacceptance.
Study Design and Methods
A retrospective analysis of COVID-19 vaccinations for HCWs at a large multi-site US academic medical center from 12/18/2020 through 05/04/2021. Comparisons between groups were performed using unpaired student t-test for continuous variables and the chi-square test for categorical variables. A logistic regression analysis was used to assess the associations between vaccine uptake and risk factor(s).
Results
Of the 65,270 HCWs included in our analysis, the overall vaccination rate was 78.6%. Male gender, older age, White and Asian race, and direct patient care were associated with higher vaccination rates (P <.0001). Significant differences were observed between different job categories. Physicians and advanced practice staff, and healthcare professionals were more likely to be vaccinated than nurses and support staff.
Conclusions
Our data demonstrated higher initial vaccination rates among HCWs than the general population national average during the study period. We observed significant disparities among different high-risk HCWs groups, especially among different job categories, black HCWs and younger HCWs despite their high risk of contracting the infection. Interventions to address lower vaccination rate and vaccine hesitancy should be built with these disparities and differences in mind to create more targeted interventions.
Keywords: COVID-19, Vaccination, Healthcare workers, Vaccine uptake
Abbreviations: AZ, Arizona; COVID-19, Coronavirus Disease 2019; Fl, Florida; HCW, Health care workers; IRB, Institutional Review Board; LPN, Licensed Practical Nurse; MN, Minnesota; OHS, Occupational Health Service; OR, Odd Ratio; US, United States; RN, Registered Nurse; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2; WI, Wisconsin
1. Background
The emergence and spread of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing over 434 million confirmed Coronavirus Disease 2019 (COVID-19) cases and 5.9 million deaths, has resulted in extraordinary public health and economic burden across the globe [1]. The United States (US) was one of the most affected countries with the highest number of confirmed cases and per capita mortality compared to the other high-income countries [2]. Over the last two years, several public health interventions were placed to address this burden, including the rapid development of several COVID-19 vaccines [1], [3], [4]. Since the rollout of the COVID-19 vaccines in December of 2020, vaccination campaigns in the US and across the globe have been met with vaccine hesitancy among the general population [5], [6], [7], [8], [9], [10], which threatens the likelihood of attaining herd immunity. Additionally, the disproportionate COVID-19 burden among high risk groups adds another layer of complexity in vaccine hesitancy [5]. Health care workers (HCW) are not immune to vaccine hesitancy. When vaccines first became available, over one fifth of HCWs globally reported being hesitant to take the COVID-19 vaccine [11]. In March 2021, the reported COVID-19 vaccination rate among HCWs in long term care facilities varied between 45 and 75% depending upon role [12].
Vaccine hesitancy or slow vaccine uptake among HCWs raised concern given their increased risk of contracting and transmitting the infection and their significant role in influencing patients’ vaccination decisions [13], [14]. While COVID-19 vaccine hesitancy and vaccination uptake in the general population have been studied [5], [6], [7], [8], [9], the literature regarding vaccine hesitancy and uptake among HCWs is limited. A systematic review summarizing the evidence of 34 studies assessing 76,471 participants suggests vaccine hesitancy among HCWs is attributed to several factors, including safety and efficacy concerns, and potential side effects. In contrast, male gender, older age, doctoral degree, higher perceived risk, direct care job, and history of influenza vaccination were associated with higher probability of accepting COVID-19 vaccination [12]. Data regarding vaccination rates was limited to two studies from the United States (US) reporting a vaccination rate of 56.8% among Long-Term Care Facilities (LTCF) HCWs [11] and 57.9% in a single center study [15] with substantial disparities in uptake by race/ethnicity and occupational category, and one additional study from the United Kingdom also demonstrating a significant difference in vaccination rates between age groups, ethnic origins, and job roles [16].
On September 9, 2021, the Centers for Medicare & Medicaid Services (CMS) announced plans to require vaccination of all staff working in participating healthcare facilities. The interim Omnibus COVID-19 Health Care Staff Vaccination Interim Final Rule was published on November 5, 2021 and went into effect January 20, 2022. Understanding HCWs’ voluntary vaccine uptake prior to an occupational requirement is warranted, given their crucial role in influencing COVID-19 acceptance among the general population.
We conducted a multicenter retrospective cohort study to examine COVID-19 vaccination rates among HCWs and identify risk factors associated with vaccine nonacceptance, to enrich the body of evidence in this area.
2. Methods
This study is a retrospective analysis of vaccinations for HCWs documented in the occupational health service (OHS) COVID-19 database from 12/18/2020 through 05/04/2021 at a large multi-site US academic medical center employing approximately 76,000 HCWs. Mayo Clinic consists of main campuses in Minnesota, Florida, and Arizona and a healthcare system including hospitals and clinics across southern Minnesota and western Wisconsin. We included all actively employed HCWs with a hire date before April 1st, 2021, who were eligible for the COVID-19 vaccine during the study period. Data analyzed from the OHS database includes HCW demographic information, vaccination status, and history of previous COVID-19 infection data. This study was determined to be exempt by the Mayo Clinic Institutional Review Board (IRB application #20–007051].
2.1. Vaccination program
The voluntary COVID-19 vaccination program was launched in December 2020 in a staged fashion prioritizing the vaccination of HCWs by occupational risk in a process described previously [17]. By March 31st, 2021, all HCWs eligible for vaccination under their respective state’s public health guidelines had been offered vaccination. Throughout this period, no institutional requirement existed for COVID-19 vaccination.
2.2. Data collection
The OHS COVID-19 database was used to collect vaccine data. This database also provided demographic and occupational data, including age, gender, location, employment duration, job, and most recent positive SARS-CoV-2 molecular assay results and dates as applicable.
HCW jobs were divided into nine categories: Administrative Staff, Advanced Practice, Clinical Support Staff including support staff in direct patient care environments, Healthcare Professional including licensed health staff such as physical and occupational therapists, Nonclinical Support Staff including support staff in patient care environments with no direct patient care duties such as custodial staff, Nurses, Physicians, Research, and Student Workers (Table 1 ).
Table 1.
List of included variables.
| Included Variable | Categories | Examples |
|---|---|---|
| Age | <25, 25–34, 35–44, 45–54, 55–64, and >=65 | |
| Duration of hire | Employment duration in months | |
| Job duties | Administrative Staff | administrator, administrative assistant, communication and media, coders, customer service and marketing, engineers, finance, human resources personal, information systems personnel, legal staff, management and planning staff, safety and training |
| Advanced Practice | advanced practice nurses and physician assistants | |
| Clinical Support Staff | support staff in direct patient care environments (desk support, patient care technician) | |
| Healthcare Professional | allied health staff (audiologists, chiropractors, dietitians, physical and occupational therapists, optometrists, paramedics, pharmacists, physiotherapists, podiatrists, radiology assistants, social workers and therapists) | |
| Nonclinical Support Staff | support staff in patient care environments with no direct patient care duties (bio-tech, clerks, custodial, food service, general service, patient transport, maintenance and powerplant, security, surgical recorder and warehouse and distribution) | |
| Nurses | RN and LPN | |
| Physicians | residents, fellows and attending physicians | |
| Research | Research staff | |
| Student Workers | Students from the school of health sciences with an active paid job | |
| Race and ethnicity | Non-Hispanic White, Black or African American, Hispanic, Asian, and Other (American Indian or Alaska Native, Native Hawaiian and Other Pacific Islander, and HCWs reporting two or more race categories) | |
| Job location | Arizona, Florida, and Midwest region (main campus in Rochester MN and health system sites in southern MN and western WI) | |
| Patient Care | Direct Care | |
| No direct Care | ||
| Positive SARS-CoV-2 molecular assay | Positive SARS-CoV-2 result and duration between a positive test result and vaccine acceptance |
Age data were classified into six categories (<25, 25–34, 35–44, 45–54, 55–64, and >=65). Race and ethnicity were reflected in a single demographic variable within the OHS and Human Resources databases. Options were Non-Hispanic White, Black or African American, Hispanic, Asian, and Other (American Indian or Alaska Native, Native Hawaiian and Other Pacific Islander, and HCWs reporting two or more race categories). Job location was categorized into Arizona, Florida, and Midwest region (including the main Rochester MN campus and health system sites across southern MN and western WI) (Table 1).
SARS-CoV-2 test results were available for HCWs who had testing at any Mayo facility per established processes, or who submitted documentation of an externally obtained test to OHS. Data regarding the most recent positive SARS-CoV-2 molecular assay results and the test dates were collected from the OHS records. Prior positive test was defined as a test that was positive prior to the availability of vaccines on 12/18/2020 for both vaccinated and unvaccinated groups. The duration between a positive test result and vaccination was categorized into 90 days or less and greater than 90 days to assess the association of prior infection with vaccine uptake. Vaccination status was defined as vaccinated if the HCW received at least one dose of an approved vaccine and unvaccinated if no vaccination dose was received during the study period. During most of the study period, HCWs who primarily teleworked were not eligible for vaccination in the state of Minnesota; these HCWs were excluded from analysis. All records were deidentified before analysis.
2.3. Statistical analysis
Data were summarized as median and interquartile range for continuous variables and absolute and relative frequencies (%) for categorical variables. Comparisons between groups on vaccination status were performed using nonparametric Wilcoxon rank-sum test for continuous variables and the chi-square test for categorical variables.
A logistic regression analysis with robust standard errors was used to assess the associations Odds Ratios (OR) between COVID-19 vaccine uptake and risk factors, including job duty category, demographics (age categories, gender), practice location, and history of previous COVID-19 infection. We adjusted for job category (nonclinical support staff vs. other job categories), race (White vs. others race groups), age (<25 vs. other age categories), gender, and history of previous COVID-19 infection. To account for variation in vaccination acceptance among US communities, we also adjusted for location (Midwest, AZ, FL). All statistical analyses were performed using a standard software package (Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC.). Two tailed P < 0.05 was considered as statistically significant.
3. Results
During the study period, 65,270 out of the 77,592 HCWs included in the database met the inclusion criteria. Seventy-one percent of HCWs were female, with an average age of 40 years (IQR: 16 to 100) and an average duration since hire of 71.6 months (IQR: 1 to 775.5), the majority were Non-Hispanic White and from a midwest practice site. Nursing staff and non-clinical support staff accounted for 45.4% of the HCWs assessed, followed by physicians and administrative staff. More than half of the HCWs work in a direct patient care environment and 4386 (6.7%) HCWs had at least one previous positive SARS-CoV-2 molecular assay result recorded before COVID-19 vaccines became available.
The overall vaccination rate was 78.6% (51,320 HCWs received at least one dose of their COVID-19 vaccine) during the study period. The following factors were significantly associated with higher vaccination rates: male gender, older age, Non-Hispanic White and Asian racial groups, longer duration since hire and direct patient care (P <.0001) (Table 2 ).
Table 2.
Demographic Characteristics of the participants and SARS-CoV-2 vaccination.
| Variables |
Vaccinated N:51,320 (78.6%) |
Unvaccinated N:13,950(21.4%) |
P value** |
|---|---|---|---|
| Age Groups, years | <0.0001 | ||
| <25 | 2314(65.3%) | 1228(34.7%) | |
| 25–34 | 13,230(72.5%) | 5022(27.5%) | |
| 35–44 | 13,188(78.3%) | 3648(21.7%) | |
| 45–54 | 10,224(82.2%) | 2215(17.8%) | |
| 55–65 | 9949(86.2%) | 1590(13.8%) | |
| >=65 | 2412(90.7%) | 246(9.3%) | |
| Gender | <0.0001 | ||
| Male | 15,516(81.9%) | 3433(18.12%) | |
| Female | 35,796(77.3%) | 10,509(22.7%) | |
| Race/Ethnicity | <0.0001 | ||
| Non-Hispanic White | 41,230(80.3%) | 10,125(19.7%) | |
| Black | 1575(61.5%) | 988(38.5%) | |
| Hispanic | 2153(75.3%) | 706(24.7%) | |
| Asian | 3824(87.9%) | 524(12.1%) | |
| Other | 928(73.3%) | 338(26.7%) | |
| Job location | <0.0001 | ||
| Midwest region | 39,040(81.1%) | 9111(18.9%) | |
| Arizona | 6471(74.2%) | 2246(25.8%) | |
| Florida | 5590 (70.3%) | 2364(29.7%) | |
| Job category | <0.0001 | ||
| Administrative Staff | 5735(82.5%) | 1216(17.5%) | |
| Physician | 6351(95.8%) | 277(4.2%) | |
| Advanced Practice | 3858(89%) | 477(11%) | |
| Nurse | 12,644(78.9%) | 3386(21.1%) | |
| Healthcare Professional | 3111(83.6%) | 611(16.4%) | |
| Clinical Support Staff | 4351(70.6%) | 1815(29.4%) | |
| Research | 4438(75.3%) | 1454(24.7%) | |
| Student Worker | 1097(82.5%) | 232(17.5%) | |
| Nonclinical Support Staff | 9,038(68.9%) | 4,074(31.1%) | |
| Patient Care Role | <0.0001 | ||
| Direct Care | 29,970(82.4%) | 6,414 (17.6%) | |
| No Direct Care | 20,653(74.3%) | 7,128(25.7%) | |
| Duration of hire, months Median (IQR) | 80.8(0-775.5) | 46.5(0-626.8) | <0.0001 |
| Prior positive SARS-CoV-2 molecular assay*** | 3,018(68.8%) | 1,368(31.2%) | <0.0001 |
SARS-CoV-2: severe acute respiratory syndrome coronavirus 2.
*Missing variables for age, gender, race, patient care, job category and location were excluded from the analysis.
** Nonparametric Wilcoxon rank-sum test for continuous variables and the chi-square test for categorical variables.
***Includes positive tests prior to vaccine availability on 12/18/2020 for both groups.
While direct patient care status was a predictive factor for vaccination among HCWs, significant differences were observed between job categories. Physicians, advanced practice staff, and healthcare professionals were more likely to be vaccinated than nurses and both clinical and non-clinical support staff (P <.0001) (Table 2).
In contrast, a history of previous positive SARS-CoV-2 molecular assay was associated with a lower vaccination rate (OR, 0.55; 95% CI, 0.51–0.58, P <.0001) (Table 2). Approximately half of those who accepted vaccination after a positive SARS-CoV-2 molecular assay did so within 90 days after their test result.
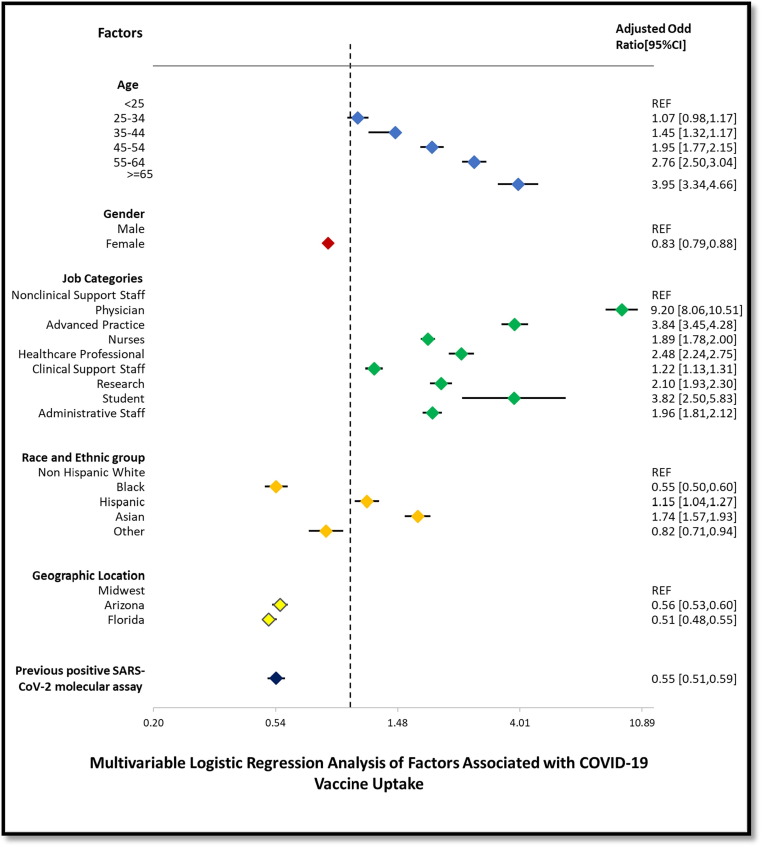
The multivariable analysis (Fig. 1 ) again demonstrated the differences observed between the different job categories, gender, age groups, location, and previous positive SARS-CoV-2 molecular assay, with physicians and advanced practice staff having the highest odds of being vaccinated (OR, 9.2; 95% CI, 8.1–10.5and OR, 3.8; 95% CI, 3.4–4.3 respectively) compared to non-clinical support staff. The odds of being vaccinated increased with increasing age, with the highest odds of vaccination among HCWs older than 65 years (OR, 3.95; 95% CI, 3. 3–4.7). The differences in vaccination rate by race and ethnicity were redemonstrated in the multivariable analysis, with Asian HCWs having the highest rate of vaccination followed by Hispanic HCWs ((OR, 1.7; 95% CI, 1.6–1.9) and (OR, 1.2; 95% CI, 1.04–1.3) respectively). The vaccination rate among Black or African American HCWs remained the lowest even after adjusting for other factors (OR, 0.55; 95% CI, 0.50–0.60). Female HCWs and HCWs located in Florida and Arizona showed decreased odds of being vaccinated. Additionally, a history of previous positive SARS-Cov-2 molecular assay showed a lower odd of being vaccinated.
Fig. 1.
Multivariable Logistic Regression Analysis of Factors Associated with COVID-19 Vaccine Uptake.
4. Discussion
In the cohort assessed, the majority of HCWs (78.6%) opted to take COVID-19 vaccine during the first four months of the vaccine campaign roll out. While HCWs vaccination rate was higher than that predicted by initial surveys (33%-77%)[18], [19], [20], [21], [22], [23] and the reported actual uptake of 56.8% among LTCF HCWs [11] and 57.9% in a single center study [15], important difference were observed among subgroups [13], [14]. Even though most HCWs in the US are now subject to occupational vaccination requirements, understanding the patterns and disparities associated with voluntary COVID-19 vaccination acceptance in HCWs is still important. Public perception of HCW vaccine hesitancy can influence vaccine uptake by the general public. We demonstrated that physicians and advance practice providers in particular had little hesitancy and high vaccination rates prior to vaccine requirements in healthcare. This information is also helpful to support community and occupational vaccination campaign teams and public health officials so they can allocate resources and target interventions especially for vulnerable groups of workers least likely to seek vaccination.
While multiple studies [12], [24] including our cohort have demonstrated that working in a patient care environment is associated with vaccine uptake, the disparity in vaccination rates among job categories within patient care environments is concerning given the higher risk of infection and mortality among these HCWs [25]. Our study results aligned with previously observed and predicted variation in vaccination among age groups with increased vaccine uptake in older age groups, both in HCWs and the general population [5], [12], [15], [24], [26]. These trends may reflect higher perceived vulnerability to COVID-19 among the older population [27]. We also found disparities in COVID-19 vaccination among racial and ethnic groups, similar to the general population and other HCWs [15], [28]. After adjusting for geographic location and other factors, vaccination rates were higher in Hispanic and Asian HCWs, and lower in Black or African American HCWs, compared to Non-Hispanic White HCWs. Racial disparities persisted within job groups but were strongly influenced by job category and geographic location, highlighting the complexity of addressing vaccine hesitancy within racial and ethnic groups.
In contrast to vaccine acceptance surveys [21], [29] showing no association between intent to receive vaccine and previous COVID-19 infection, our study found a lower vaccination rate among HCWs who were previously infected with COVID-19. This is similar to data reported by Thornton et al. and colleagues in their single center vaccine uptake study [15]. This finding may be attributable to the demographics of the population, level of vaccine hesitancy in the general population and perceived immunity from an infection.
Overall our results showed a higher vaccination rate than the reported rates by Lee et al. [11] and Thornton et al. [15], and demonstrated a similar disparity in vaccination uptake among different job categories, with the highest vaccination rates observed in physicians and advanced practice providers, while nurses and support staff had the lowest vaccination rates [11], [15]. In comparison to previously published studies [11], [15] the strengths of our study included the large sample size [n = 65,270] and use of an integrated occupational health database across all clinic and hospital sites.. Utilizing the OHS database where vaccination records and all employee occupational health data is stored allowed assessment of variation in vaccination by geographic region and decreased the risk of ascertainment bias in vaccination status and prior COVID-19 infection. In addition, the vaccination campaign was aimed to reduce barriers to vaccination among HCWs by providing frequent reminders and offering flexible scheduling options [17].
As is common in retrospective observational studies, one of our study's limitations was the utilization of Human Resources demographic data which can include omissions. Despite this, <3% of demographic information was missing, and this did not impact the overall analysis. The study design could not assess other factors such as vaccine beliefs, perceived risk, personal health status, socioeconomic factors, or political views. Additionally, while our study includes a large cohort of HCWs, it may not be fully representative of all HCWs across the US, although the inclusion of 3 different regions mitigates this limitation somewhat.
Given the complexity and the importance of vaccination, further efforts are needed to increase vaccine uptake among HCWs and the general population to combat the COVID-19 pandemic and attain herd immunity. Our study adds to the limited available data regarding COVID-19 vaccine uptake among HCWs, which will provide health care systems and public health officials with a better understanding of patterns associated with voluntary vaccine uptake among HCWs, to inform more tailored and targeted interventions to address these issues as booster doses of COVID-19 vaccine are recommended but may not be required.
5. Conclusion
Our data demonstrated higher initial vaccination rates among health care workers than the general population national average during the study period. We observed significant disparities among high-risk HCWs groups, especially among different job categories. The highest vaccination rates were observed among physicians and advanced practice providers, while nonclinical support staff had the lowest vaccination rates despite their high risk of contracting the infection. Black or African American HCWs had lower vaccination rates even after controlling for other occupational and demographic factors, which is alarming given the excess COVID-19 related morbidity and mortality affecting minority communities in the US. Younger HCW and those with prior COVID-19 infection were also less likely to accept vaccination. Interventions to address lower vaccination rate and vaccine hesitancy should be built with these disparities and differences in mind to create more targeted interventions for ongoing booster vaccination campaigns.
Funding
This work was supported by the Division of Public Health, Infectious Diseases and Occupational Medicine at Mayo Clinic, Rochester.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We would like to acknowledge the Mayo Clinic Occupational Health Service for providing access to deidentified data.
References
- 1.Organization WH. WHO coronavirus disease (COVID-19) dashboard Geneva: World Health Organization; 2022. Available from: https://covid19.who.int/.
- 2.Engineering CfSSa. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU): Johns Hopkins University; 2022. Available from: https://coronavirus.jhu.edu/map.html.
- 3.Baden L.R., El Sahly H.M., Essink B., Kotloff K., Frey S., Novak R., et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2020;384(5):403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murthy B.P., Sterrett N., Weller D., Zell E., Reynolds L., Toblin R.L., et al. Disparities in COVID-19 vaccination coverage between urban and rural counties—United States, December 14, 2020–April 10, 2021. Morb Mortal Wkly Rep. 2021;70(20):759. doi: 10.15585/mmwr.mm7020e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Troiano G., Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solís Arce J.S., Warren S.S., Meriggi N.F., Scacco A., McMurry N., Voors M., et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021 doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee J.T. Disparities in COVID-19 vaccination coverage among health care personnel working in long-term care facilities, by job category, national healthcare safety network—United States, March 2021. MMWR Morb Mortal Wkly Rep. 2021;70 doi: 10.15585/mmwr.mm7030a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biswas N., Mustapha T., Khubchandani J., Price J.H. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021 doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nguyen LH, Drew DA, Joshi AD, Guo C-G, Ma W, Mehta RS, et al. Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study. medRxiv: Preprint Server Health Sci 2020:2020.04.29.20084111.
- 14.Paterson P., Meurice F., Stanberry L.R., Glismann S., Rosenthal S.L., Larson H.J. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 15.Thornton J.D., Dixon-Williams S., Huml A., Perzynski A., Gunzler D., Einstadter D. A cross-sectional study of SARS-CoV-2 vaccination among employees of an urban safety-net health care system. Ann Intern Med. 2021 doi: 10.7326/M21-1513. M21-1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azamgarhi T., Hodgkinson M., Shah A., Skinner J.A., Hauptmannova I., Briggs T.W.R., et al. BNT162b2 vaccine uptake and effectiveness in UK healthcare workers - a single centre cohort study. Nat Commun. 2021;12(1):3698. doi: 10.1038/s41467-021-23927-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swift M.D., Sampathkumar P., Breeher L.E., Ting H.H., Virk A. Mayo clinic’s multidisciplinary approach to Covid-19 vaccine allocation and distribution. NEJM Catal Innovations Care Deliv. 2021;2(1) [Google Scholar]
- 18.Lucia V.C., Kelekar A., Afonso N.M. COVID-19 vaccine hesitancy among medical students. J Public Health (Oxf) 2020 doi: 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaw J., Stewart T., Anderson K.B., Hanley S., Thomas S.J., Salmon D.A., et al. Assessment of U.S. health care personnel (HCP) attitudes towards COVID-19 vaccination in a large university health care system. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shekhar R., Sheikh A.B., Upadhyay S., Singh M., Kottewar S., Mir H., et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021;9(2):119. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unroe K.T., Evans R., Weaver L., Rusyniak D., Blackburn J. Willingness of long-term care staff to receive a COVID-19 vaccine: a single state survey. J Am Geriatr Soc. 2021;69(3):593–599. doi: 10.1111/jgs.17022. [DOI] [PubMed] [Google Scholar]
- 22.Manning M.L., Gerolamo A.M., Marino M.A., Hanson-Zalot M.E., Pogorzelska-Maziarz M. COVID-19 vaccination readiness among nurse faculty and student nurses. Nurs Outlook. 2021;S0029–6554(21):00023–33. doi: 10.1016/j.outlook.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gadoth A., Halbrook M., Martin-Blais R., Gray A., Tobin N.H., Ferbas K.G., et al. Cross-sectional assessment of COVID-19 vaccine acceptance among health care workers in Los Angeles. Ann Intern Med. 2021;174(6):882–885. doi: 10.7326/M20-7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li M., Luo Y., Watson R., Zheng Y., Ren J., Tang J., et al. Healthcare workers' (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J. 2021 doi: 10.1136/postgradmedj-2021-140195. [DOI] [PubMed] [Google Scholar]
- 25.Bandyopadhyay S., Baticulon R.E., Kadhum M., Alser M., Ojuka D.K., Badereddin Y., et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob Health. 2020;5(12) doi: 10.1136/bmjgh-2020-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Diesel J., Sterrett N., Dasgupta S., Kriss J.L., Barry V., Esschert K.V., et al. COVID-19 vaccination coverage among adults—United States, December 14, 2020–May 22, 2021. Morb Mortal Wkly Rep. 2021;70(25):922. doi: 10.15585/mmwr.mm7025e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gerussi V., Peghin M., Palese A., Bressan V., Visintini E., Bontempo G., et al. Vaccine hesitancy among Italian patients recovered from COVID-19 infection towards influenza and Sars-Cov-2 vaccination. Vaccines. 2021;9(2):172. doi: 10.3390/vaccines9020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ndugga N., Pham O., Hill L., Artiga S., Mengistu S. Latest data on COVID-19 vaccinations race/ethnicity. Kais Family Found. 2021 [Google Scholar]
- 29.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]