Abstract
Purpose
The purpose of this study is to report a single center experience with portable digital radiographically (DR) guided bedside IVC filters placed in intensive care unit (ICU) patients with high ICP and elevated head of bed (HOB).
Materials and methods
A retrospective chart review was conducted on all bedside IVC filters placed from January 1, 2010 to September 16, 2020. Patients with high ICP and elevated head of bed requirements were included. Charts were reviewed for filter type, common femoral vein (CFV) access, filter location, pre procedure imaging, pre and post filter ICPs, glascow coma scale, number of radiographs taken, and filter removal. ICPs were obtained 1 h prior to procedure and 2 h post procedure and analyzed with a paired T test.
Filters were placed by reviewing prior CT scan for IVC size, caval variants, renal and iliac veins and vertebral body landmarks. Then, CFV access was obtained and a Bentson wire was advanced 30–40 cm. A radiograph was used to confirm adequate position of the of the wire. The filter sheath was advanced and serial radiographs were used to position the filter sheath at the final predetermined position below the renal veins and above the iliac bifurcation. The filter was deployed, and a radiograph was obtained to confirm filter positioning.
Results
A total of 9 DR guided bedside IVC filters were placed (4 Denali, 3 Option Elite, 2 Celect). Indications included prophylactic placement (n = 8) and acute DVT (n = 1). The average patient age was 35.8 years (range: 18–56 years) CT abdomen and pelvis was used to assess for the level of renal veins in all patients (n = 9). No caval variants were encountered on pre-procedural planning. The average pre, intraprocedural, and post procedure intracranial pressure was 16 mmHg, 13 mmHg, and 16 mmHg, respectively. Confirmation of placement after final placement was available in 7 patients (4 DR, 2 CT and one fluoroscopic examination). Two non-procedural related deaths occurred.
Technical success, defined as successful placement of IVC filter at the predetermined level, was achieved in 100% of patients (n = 9). The right CFV was used in most patients (n = 7). The left CFV was used for access in two patients due to right CFV thrombus (n = 1) and existing right femoral venous central line (n = 1). The average number of radiographs taken was 5.8 (range 4–9). In all cases, filters were placed below the level of the lowest renal vein (n = 9). A comparison of pre, during and post intervention ICP pressures is shown in table, 2. No differences between pre and post filter ICP was noted (p = 0.77). Three filters were later removed. One minor complication was reported, which was filter tilt (23%) in an Option filter.
Conclusion
Bedside IVC filters can be safely placed in patients with head trauma and high ICP who are unable to lay supine using portable DR guidance with a high rate of technical success and minimal complications.
Keywords: IVC, Filter, Prophylactic, Inferior Vena Cava, Thrombus
1. Introduction
Critically ill patients are at elevated risk of deep vein thrombosis (DVT).1 Many patients are not candidates for anticoagulation and as a result, inferior vena cava (IVC) filters are frequently requested to prevent pulmonary embolus (PE). Head trauma presents an additional challenge as many of these patients are unable to lay supine for the procedure due to high intracranial pressures (ICP) and ICP monitoring (ICPM). This necessitates filters be placed at bedside, ideally with the head of the bed elevated. Prior reports on bedside filter placement have been in supine patients using either mobile fluoroscopy or intravascular ultrasound (IVUS), which is not always feasible.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16
The purpose of this study is to report a single center experience with portable DR guided bedside IVC filters placed in intensive care unit (ICU) patients with high ICP and elevated head of bed (HOB).
2. Materials and Methods
Local IRB approval was obtained. A retrospective chart review was conducted on all bedside IVC filters placed using DR guidance from January 1, 2010 to September 16, 2020. Only patients with ICPM and elevated HOB requirements were included. Patient selection methodology is depicted in chart 1. Filter type, common femoral vein (CFV) access site, filter location, pre procedure imaging, pre- and post-filter ICPs, Glascow coma scale (GCS), number of radiographs taken, filter position and filter removal were recorded. ICPs were obtained 1 h prior to procedure and 2 h post procedure and analyzed with a paired T test.
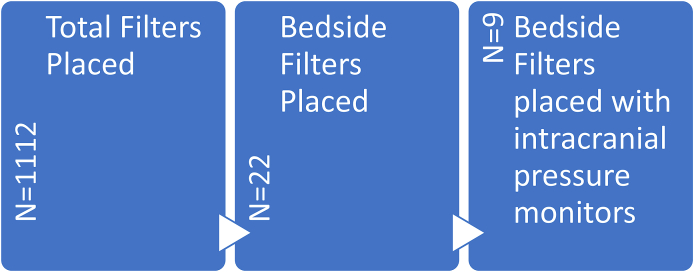
Chart 1.
Patient Selection. Total Filters represents the number of total filters placed from January 1st 2010 to September 16th 2020.
Filters were placed after reviewing prior contrast enhanced CT scans of the abdomen and pelvis for IVC size, caval variants, and renal and iliac vein anatomy and determining appropriate vertebral body landmarks. Then, CFV access was obtained under US guidance using a micropuncture set and a Bentson wire was advanced approximately 30 cm into the IVC (Fig. 1A). A DR was used to confirm the adequate position of the wire to the right of the vertebral bodies. The filter sheath was advanced over the wire and serial digital radiographs were used to position the filter sheath at the final predetermined position at the level of the vertebral bodies, below the renal veins and above the iliac bifurcation (Fig. 1B). The filter was deployed blindly by keeping the filter pusher stationary while the sheath was pulled back completely. A final DR was obtained to confirm filter positioning (Fig. 1D). Manual compression was then applied at the access site. The HOB elevation was maintained during the procedure and ICPs were monitored in the ICU.
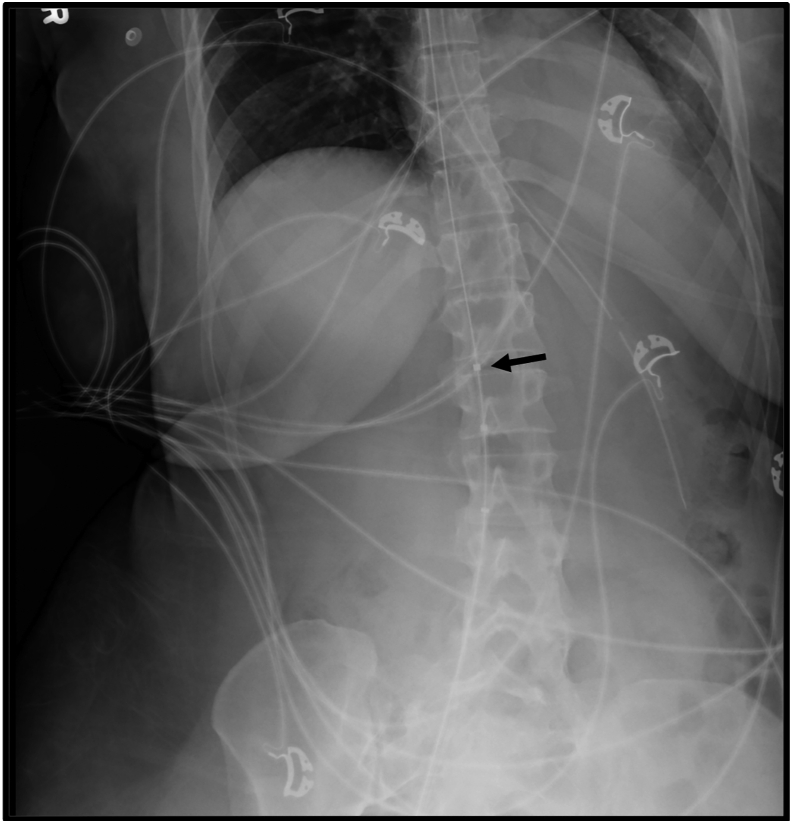
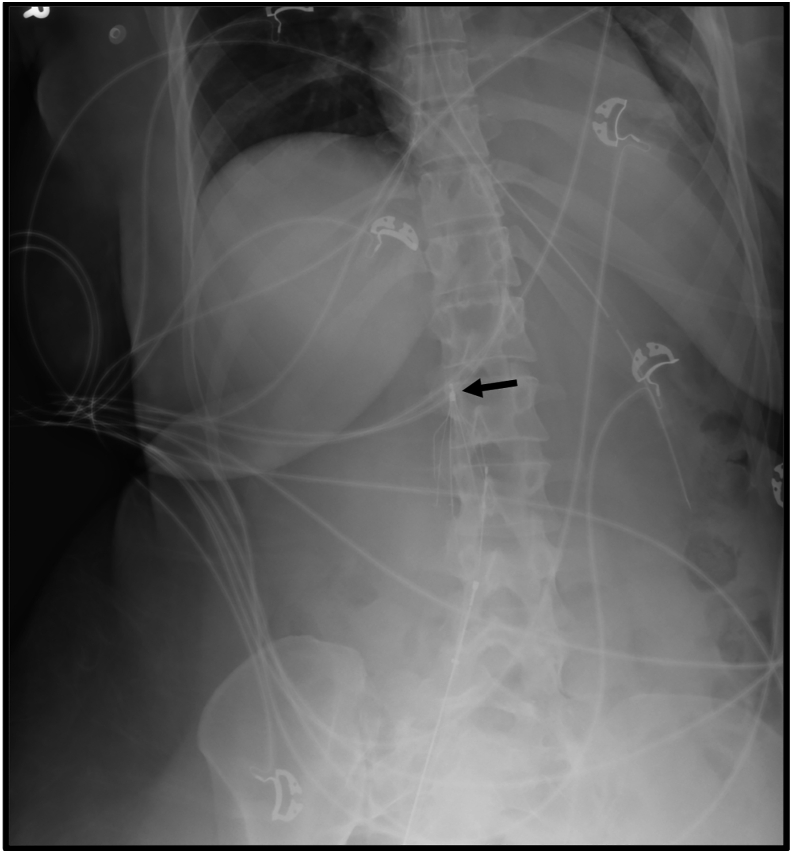
Fig. 1C.
The filter is advanced through the sheath and partially exposed to confirm adequate placement prior to complete deployment. The hook of the filter (Denali) is shown at the level of L2 (arrow).
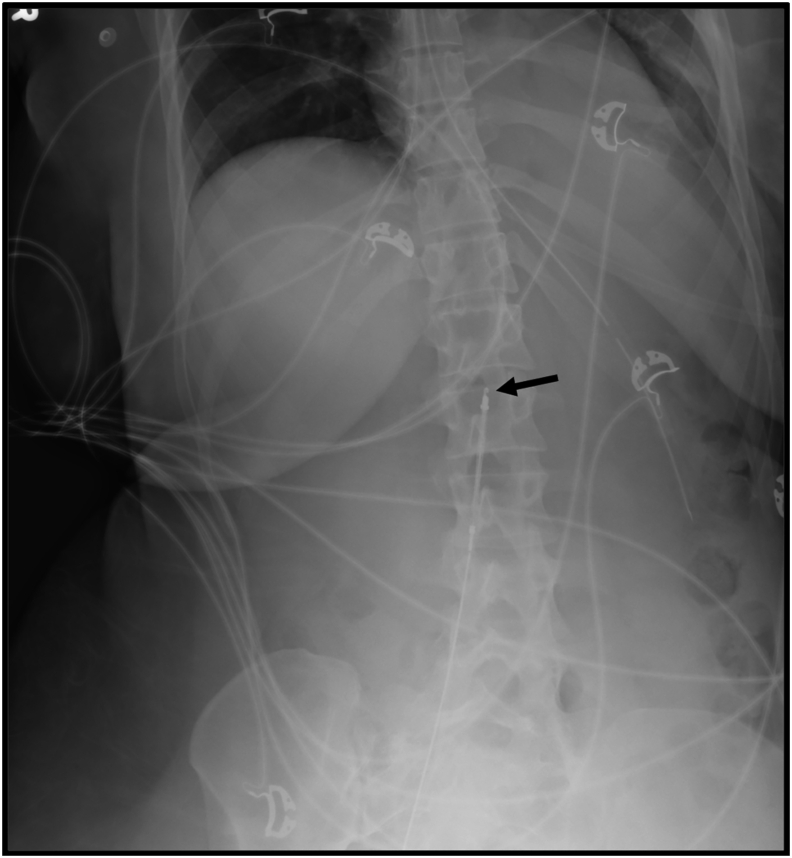
Fig. 1A.
After obtaining right CFV access, a bentson wire is advanced approximately 30 cm, shown here in the inferior vena cava (arrow).
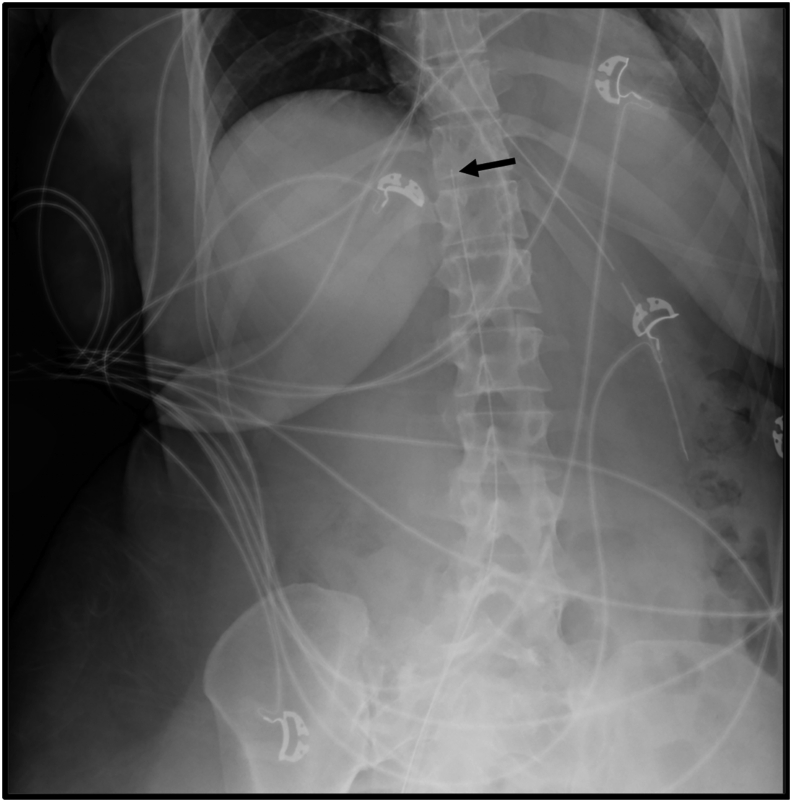
Fig. 1B.
The Bentson wire was further advanced, and the filter sheath advanced to the superior endplate of L2, the level of the renal veins on comparison CT scan (arrow).
Fig. 1D.
Final deployment demonstrates appropriate IVC filter position, with the hook of the filter at the level of L2 (arrow).
3. Results
The average patient age was 35.8 years (range: 18–56 years). Additional patient characteristics and procedural details are listed in Table 1.
Table 1.
Summary of patients.
| Age | Sex | Initial GCS | Indication | Pre-procedure Planning |
Access Site | Level | Filter type | Radiographs Taken |
Post Filter Imaging | Removal | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 37 | M | 7 | Prophylaxis | CT A/P | R CFV | L3-L4 | Option Elite | 6 | None | Nb |
| 2 | 18 | M | 3T | Prophylaxis | CT A/P | R CFV | L1 | Cook Celect | 5 | None | Na |
| 3 | 47 | M | 3T | Prophylaxis | CT A/P | R CFV | L2 | Option Elite | 7 | CTA A/P | Na |
| 4 | 56 | M | 3T | Prophylaxis | CT A/P | L CFV | L2 | Cook Celect | 6 | KUB | Nb |
| 5 | 51 | M | 3T | Existing R CFV thrombus | CT A/P | L CFV | L2 | Denali | 5 | Removal | Y |
| 6 | 35 | M | 5 | Prophylaxis | CT A/P | R CFV | L2 | Option Elite | 5 | KUB | Nb |
| 7 | 35 | F | 6T | Prophylaxis | CT A/P | R CFV | L2 | Denali | 4 | CT A/P | Y |
| 8 | 18 | M | 3T | Prophylaxis | CT A/P | R CFV | L1 | Denali | 6 | KUB | Y |
| 9 | 26 | F | 4T | Prophylaxis | CT A/P | R CFV | L2 | Denali | 9 | KUB | Nb |
Filter not removed due to patient death during hospitalization.
Filter not removed due to loss to follow-up.
A total of 9 DR guided bedside IVC filters were placed (4 Denali, 3 Option Elite, 2 Celect). Indications included prophylactic placement (n = 8) and acute DVT (n = 1). CT abdomen and pelvis was used to assess for the level of renal veins in all patients (n = 9). No caval variants were encountered on pre-procedural planning.
Intracranial pressure measurements are detailed in Table 2. The average pre, intraprocedural, and post procedure intracranial pressure was 16.1 mmHg, 13.2 mmHg, and 15.5 mmHg, respectively. There was no statistically significant difference between pre and post intracranial pressures (p = 0.77).
Table 2.
Comparison of intracranial pressures.
| Patient | ICP Pre (mmHg) | ICP During (mmHg) | ICP Post (mmHg) | Change in ICP (mmHg) |
|---|---|---|---|---|
| 1 | 13 | 11 | 11 | −2 |
| 2 | 28 | 26 | 29 | 1 |
| 3 | 15 | 5 | 5 | −10 |
| 4 | 19 | 20 | 17 | −2 |
| 5 | 13 | 15 | 14 | 1 |
| 6 | 8 | 9 | 14 | 6 |
| 7 | 15 | 11 | 17 | 2 |
| 8 | 16 | 7 | 23 | 7 |
| 9 | 18 | 15 | 10 | −8 |
| Mean | 16.1 | 13.2 | 15.6 | −0.56 |
| Median | 15 | 11 | 14 | 1 |
Technical success, defined as successful placement of IVC filter at the predetermined level, was achieved in 100% of patients (n = 9). The right CFV was used in most patients (n = 7). The left CFV was used for access in two patients due to right CFV thrombus (n = 1) and existing right femoral venous central line (n = 1). The average number of radiographs taken was 5.8 (range 4–9). In all cases, filters were placed below the level of the lowest renal vein (n = 9). A comparison of pre, during and post intervention ICP pressures is shown in Table 2. No differences between pre and post filter ICP was noted (p = 0.77). Three filters were later removed. One minor complication was reported, which was filter tilt (23%) in an Option filter.
4. Discussion
The use of IVC in high-risk patients for PE without DVT is highly controversial. Although recent consensus guidelines recommend against prophylactic filters in the trauma patient without documented lower extremity DVT, prophylactic IVC filters are still requested in high-risk patients.
The current standard method of bedside IVC filter placement utilizes either mobile C arm, trans-abdominal ultrasound (US) or IVUS in supine patients. Technical success has been reported up to 97% for transabdominal US guided filter placement, however careful patient selection needs to be implemented as patient body habitus, position, bowel gas, all contribute to necessary visibility for proper filter deployment.18 One study demonstrated nearly 12% of patients were not candidates for safe transabdominal US guided filter placement, and in these patients IVUS is frequently the next option if available.18 Technical success rates for IVUS deployed filters depends on the operators experience and has been reported at high as 99%.3 Data comparing these methods is limited, however it has been suggested that filter malposition and filter tilt are higher in IVUS guided placement compared to conventional fluoroscopy.17
Patient positioning for filter deployment can present an additional challenge. Both standard filter placement and transabdominal US guided filter placements prefer the patient in a supine position. In this study, patients were unable to lay supine due to ICP requirements and had the head of bed elevated to a minimum of 30°. In these patients, DR bedside guidance was successful in accurately deploying filters with minimal complications.
When assessing for placement of bedside filters under DR guidance, as a standard catheter venography is not performed, the interventionalist needs to carefully review recent CT scans of the abdomen with contrast to identify the level of the renal veins and the caval bifurcation, rule out DVT and identify potential anatomic caval variants. In contrast to transabdominal US or IVUS, renal veins are not visualized at the time of placement, and thus a vertebral body is selected to mark the level of the lowest renal vein prior to the procedure.
Potential pitfalls of placing bedside filters with DR include IVC filter tilt, malposition or IVC perforation. These complications can be pinpointed to a few key steps. Pulling the sheath back too low commonly results in malposition. If the sheath is advanced with the filter in place, or if the filter is simultaneously advanced while the sheath is pulled back, the filter may be placed either too high, or may result in IVC perforation.
The main limitations of this study are the retrospective nature of the study and limited sample size.
5. Conclusion
Bedside IVC filters can be safely placed in patients with head trauma and high ICP who are unable to lay supine using portable DR guidance with a high rate of technical success and minimal complications.
Ethical approval
The study was approved by the ethics committee of UT Health San Antonio. All clinical practices and observations were conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from each patient before the study was conducted.
Patient consent
Written informed consent was obtained from patients for publication of these case reports and any accompanying images.
Declaration of competing interest
The authors declare no conflicts of interest.
References
- 1.Toker S., Hak D.J., Morgan S.J. Deep vein thrombosis prophylaxis in trauma patients. Thrombosis. 2011;2011:505373. doi: 10.1155/2011/505373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matusov Y., Weinberg A.S., Liang R., et al. Use of the bedside-placed angel catheter IVC filter for venous thromboembolic disease in critically ill medical patients. J Intensive Care Med. 2020;35:225–232. doi: 10.1177/0885066619874692. [DOI] [PubMed] [Google Scholar]
- 3.Glocker R.J., Awonuga O., Novak Z., et al. Bedside inferior vena cava filter placement by intravascular ultrasound in critically ill patients is safe and effective for an extended time. J Vasc Surg Venous Lymphat Disord. 2014;2:377–382. doi: 10.1016/j.jvsv.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 4.Killingsworth C.D., Taylor S.M., Patterson M.A., et al. Prospective implementation of an algorithm for bedside intravascular ultrasound-guided filter placement in critically ill patients. J Vasc Surg. 2010;51:1215–1221. doi: 10.1016/j.jvs.2009.12.041. [DOI] [PubMed] [Google Scholar]
- 5.Qin X., Lu C., Ren P., et al. New method for ultrasound-guided inferior vena cava filter placement. J Vasc Surg Venous Lymphat Disord. 2018;6:450–456. doi: 10.1016/j.jvsv.2017.12.057. [DOI] [PubMed] [Google Scholar]
- 6.Ebaugh J.L., Chiou A.C., Morasch M.D., et al. Bedside vena cava filter placement guided with intravascular ultrasound. J Vasc Surg. 2001;34:21–26. doi: 10.1067/mva.2001.115599. [DOI] [PubMed] [Google Scholar]
- 7.Tola J.C., Holtzman R., Lottenberg L. Bedside placement of inferior vena cava filters in the intensive care unit. Am Surg. 1999;65:833–837. discussion 837-838. [PubMed] [Google Scholar]
- 8.Patel N., Saucedo J. Bedside placement of a retrievable inferior vena cava filter in a morbidly obese patient guided by modified IVUS approach. J Invasive Cardiol. 2012;24:E311–E313. [PubMed] [Google Scholar]
- 9.Aidinian G., Fox C.J., White P.W., et al. Intravascular ultrasound--guided inferior vena cava filter placement in the military multitrauma patients: a single-center experience. Vasc Endovasc Surg. 2009;43:497–501. doi: 10.1177/1538574409334824. [DOI] [PubMed] [Google Scholar]
- 10.Vesco P.A., Falimirski M.E., Williams H.K., et al. Abdominal computed tomography and the placement of inferior vena caval filters. J Trauma. 2006;60:1197–1201. doi: 10.1097/01.ta.0000218062.19676.9a. discussion 1202-1203. [DOI] [PubMed] [Google Scholar]
- 11.Conners M.S., 3rd, Becker S., Guzman R.J., et al. Duplex scan-directed placement of inferior vena cava filters: a five-year institutional experience. J Vasc Surg. 2002;35:286–291. doi: 10.1067/mva.2002.120372. [DOI] [PubMed] [Google Scholar]
- 12.Chiou A.C. Intravascular ultrasound-guided bedside placement of inferior vena cava filters. Semin Vasc Surg. 2006;19:150–154. doi: 10.1053/j.semvascsurg.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Wellons E.D., Rosenthal D., Shuler F.W., et al. Real-time intravascular ultrasound-guided placement of a removable inferior vena cava filter. J Trauma. 2004;57:20–23. doi: 10.1097/01.ta.0000135500.64630.93. discussion 23-25. [DOI] [PubMed] [Google Scholar]
- 14.Nunn C.R., Neuzil D., Naslund T., et al. Cost-effective method for bedside insertion of vena caval filters in trauma patients. J Trauma. 1997;43:752–758. doi: 10.1097/00005373-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Hislop S., Fanciullo D., Doyle A., et al. Correlation of intravascular ultrasound and computed tomography scan measurements for placement of intravascular ultrasound-guided inferior vena cava filters. J Vasc Surg. 2014;59:1066–1072. doi: 10.1016/j.jvs.2013.10.071. [DOI] [PubMed] [Google Scholar]
- 16.Kaufman JA, Barnes GD, Chaer RA, et al. Society of Interventional Radiology Clinical Practice Guideline for Inferior Vena Cava Filters in the Treatment of Patients with Venous Thromboembolic Disease: Developed in collaboration with the American College of Cardiology, American College of Chest Physicians, American College of Surgeons Committee on Trauma, American Heart Association, Society for Vascular Surgery, and Society for Vascular Medicine. J Vasc Interv Radiol. 2020;31:1529–1544. doi: 10.1016/j.jvir.2020.06.014. [DOI] [PubMed] [Google Scholar]
- 17.Ganguli S., Hawkins B.M., Abtahian F., et al. Comparison of inferior vena cava filters placed at the bedside via intravenous ultrasound guidance versus fluoroscopic guidance. Ann Vasc Surg. 2017;39:250–255. doi: 10.1016/j.avsg.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 18.Passman M.A., Dattilo J.B., Guzman R.J., et al. Bedside placement of inferior vena cava filters by using transabdominal duplex ultrasonography and intravascular ultrasound imaging. J Vasc Surg. 2005;42:1027–1032. doi: 10.1016/j.jvs.2005.06.027. [DOI] [PubMed] [Google Scholar]