Abstract
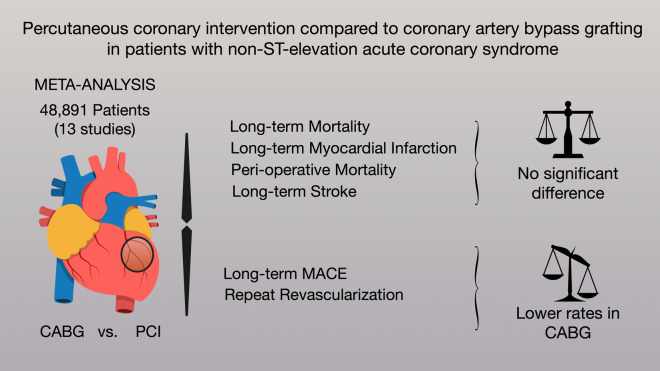
Non-ST-elevation acute coronary syndrome (NSTE-ACS) affects millions of patients. Although an invasive strategy can improve survival, the optimal treatment [i.e., percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG)] is not clear. We performed a meta-analysis of studies reporting outcomes between PCI and CABG in patients with NSTE-ACS. MEDLINE, EMBASE and Cochrane Library were assessed. The primary outcome was long-term mortality. Inverse variance method and random model were performed. We identified 13 observational studies (48,891 patients). No significant difference was found in the primary endpoint [CABG vs. PCI, incidence rate ratio (IRR) 0.93, 95% confidence interval (CI) 0.70; 1.23]. CABG was associated with lower long-term major adverse cardiovascular events (MACE) (IRR 0.64, 95% CI 0.54; 0.76) and lower long-term re-revascularization (IRR 0.37, 95% CI 0.30; 0.47). There was no significant difference in long-term myocardial infarction (CABG vs. PCI, IRR 0.96, 95% CI 0.50; 1.84) and peri-operative mortality (CABG vs. PCI, odds ratio 1.36, 95% CI 0.94; 1.95). For the treatment of NSTE-ACS, CABG and PCI are associated with similar rates of long-term mortality and myocardial infarction. CABG is associated with lower rates of long-term MACE and re-revascularization. Randomized comparisons in this setting are necessary.
Subject terms: Cardiovascular biology, Interventional cardiology
Introduction
Non-ST-elevation acute coronary syndrome (NSTE-ACS) represents a large proportion of patients with acute coronary syndromes (ACS) impacting millions of patients worldwide1,2. Recently, the percentage of patients presenting with non-ST-elevation myocardial infarction (NSTEMI) has increased in both Europe and United States1,2. Although a routine invasive strategy in NSTE-ACS may improve long-term survival and reduce late myocardial infarction3, the optimal treatment method remains controversial. Specifically, it remains unclear as to whether percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) provide better long-term outcomes4. A possible difference in treatment outcomes might be plausible, as recent publications have shown that PCI and CABG mechanisms differ5,6. Although both stents and bypass grafts provide revascularization to vascular territories affected by flow-limiting stenoses, only CABG also provides protection against vessel occlusions from non–flow-limiting stenoses, because the majority of bypass graft insertions are performed distal to plaque location5,6.
To date, there is no randomized comparison of PCI vs. CABG surgery in the specific setting of NSTE-ACS. While there have been a number of non-randomized studies published, their results have been inconclusive. Additionally, no systematic review and meta-analysis addressing this topic exists in the literature.
In this analysis we set out to systematically review the literature on the impact of the treatment modality on clinical outcome in NSTE-ACS.
Methods
This analysis was prospectively registered on the International Prospective Register of Systematic Reviews in Health and Social Care (PROSPERO, ID number CRD42020214423). Ethical and internal review board approval was not required for this analysis as no human or animal subjects were involved.
Search strategy
A medical librarian (MD) performed a comprehensive literature search to identify contemporary studies comparing outcomes in patients with NSTE-ACS (unstable angina pectoris [UAP] and non-ST-elevation myocardial infarction [NSTEMI]) who underwent either PCI or CABG. Searches were run on October 19, 2020 in the following databases: Ovid MEDLINE® (ALL; 2008 to present); Ovid EMBASE (1974 to present); and The Cochrane Library (Wiley). The search strategy for Ovid MEDLINE is available in Supplementary Table 1.
Study selection and eligibility criteria
The study selection followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) strategy7. After de-duplication, records were screened by two independent reviewers (TC and HK). Any discrepancies and disagreements were resolved by a third author (TD). All titles and abstracts were reviewed against pre-defined inclusion and exclusion criteria. Studies were considered for inclusion if they were written in English, reported direct comparison between PCI patients and CABG patients and had at least 1 outcome of interest reported. Studies evaluating refractory angina, chronic coronary disease, conference abstracts, proceedings and case reports were excluded. The safety of the comparability of CABG and PCI in a setting of patients with acute ischemic injury and even heart failure has been previously demonstrated8.
Following the first round of screening, full text was pulled for selected studies for a second round of eligibility screening. Reference lists for articles in these selected studies were also searched for any relevant articles not captured by the original search strategy.
Data abstraction and quality assessment
The data extraction and the quality assessment were performed independently by two different investigators (TC and HK) and verified by a third investigator (TD) for accuracy. The following variables were extracted: age, sex, left ventricular ejection fraction, hypertension, diabetes, smoking status, prior cerebrovascular accident, prior myocardial infarction, prior percutaneous coronary intervention, number of vessels addressed (1, 2 or 3), use of drug eluting stents, left main disease and discharge with ASA and/or ADP-inhibitor. Risk of bias was assessed based on Newcastle–Ottawa assessment scale (Supplementary Table 2)9.
Outcomes and effect summary
The primary outcome was long-term mortality (> 6 months). Mean follow up by study is summarized in Table 1. Secondary outcomes were long-term major adverse cardiovascular events (defined in Supplementary Table 3), long-term re-revascularization, long-term myocardial infarction, peri-operative mortality (in-hospital and 30-day events) and long-term stroke. For the primary outcome, a sensitivity analysis comparing adjusted and low risk of bias studies vs. unadjusted studies was also performed.
Table 1.
Studies included in the meta-analysis.
| Study | Study design | Demographics comparability | Country | Patients syndrom included | No patients | Endpoints included | Mean follow-up (Y) |
|---|---|---|---|---|---|---|---|
| De Feyter10 | Prespecified analysis—arts trial | Unadjusted | Netherlands | Unstable angina | 450 | MORTl, MACE, MI, RR | 1 |
| Chew11 | Post-hoc analysis—synergy trial | Unadjusted | Australia | Unstable angina and NSTEMI | 9902 | MORTl, MI | 0.5 |
| Hochholzer12 | Prospective cohort study | Multivariable regression | Germany | Unstable angina and NSTEMI | 1024 | MORTl, MI | 1.3 |
| Alhabib13 | Prospective study—gulf race-2 registry | Unadjusted | Saudi Arabia | Unstable angina and NSTEMI | 802 | MORTp, MORTl | 1 |
| Roe14 | Retrospective—crusade registry | Unadjusted | United States | NSTEMI | 15,281 | MORTl, MACE, RR | 3.2 |
| Buszman15 | Prospective study—milestone registry | Propensity score matching | Poland | Unstable angina and NSTEMI | 4566 | MORTp, MORTl | 3 |
| Ben-Gal16 | Post-hoc analysis—acuity trial | Propensity score matching | Israel | Unstable angina and NSTEMI | 1772 | MORTp, MORTl, MACE, MI, RR | 1 |
| Kurlansky17 | Retrospective—care registry | Propensity score matching | United States | NSTEMI | 3228 | MACE | 5.6 (CABG) AND 5.1 (PCI) |
| Chang18 | Patient level data—best/precombat/syntax | Unadjusted | South Korea | Unstable angina and NSTEMI | 1246 | MORTl, MACE, MI, RR | 5 |
| Freitas19 | Prospective observational study | Multivariable regression | Portugal | NSTEMI | 688 | MORTl | 4.8 |
| Huckaby20 | Retrospective | Multivariable regression | United States | NSTEMI | 2001 | MORTl, MACE, MI, RR | 3.6 |
| Jia21 | Prospective observational study | Multivariable regression | China | Unstable angina and NSTEMI | 2819 | MORTl, MACE, MI, RR | 7.5 |
| Ram22 | Prospective study –acsis registry | Multivariable regression | Israel | Unstable angina and NSTEMI | 5112 | MORTp, MORTl | 3 |
CABG coronary artery bypass grafting, MACE major adverse cardiovascular events, MI myocardial infarction, MORTl long-term mortality, MORTp peri-operative mortality, NSTEMI non-ST-elevation myocardial infarction, PCI percutaneous coronary intervention, RR re-revascularization.
Data analysis
Peri-operative binary outcomes were reported as odds ratios (OR) while long-term outcomes, were reported as incidence rate ratio (IRR); for both estimates the generic inverse variance method was used and 95% confidence intervals (CIs) were also presented.
Random effect meta-analysis was performed using “metafor” and “meta” package23,24. CABG was the reference for all pairwise comparisons. Heterogeneity was reported as low (I2 = 0–25%), moderate (I2 = 26–50%), or high (I2 > 50%)25. Leave-one-out analysis for the primary outcome was performed to assess the robustness of the obtained estimate. Meta-regression was used to explore the effects of: year of publication, mean follow-up time, age, sex, left ventricular ejection fraction, hypertension, diabetes, smoking status, prior cerebrovascular accident, prior myocardial infarction, prior percutaneous coronary intervention, number of vessels addressed (1, 2 or 3), use of drug eluting stents, left main disease and discharge with ASA and/or ADP-inhibitor on the IRR of the primary outcome.
Statistical significance was set at the 2-tailed 0.05 level, without multiplicity adjustments. All statistical analyses were performed using R (version 3.3.3, R Project for Statistical Computing) within RStudio.
Ethic declaration
Ethical and internal review board approval was not required for this analysis as no human or animal subjects were involved.
Results
Description of included studies
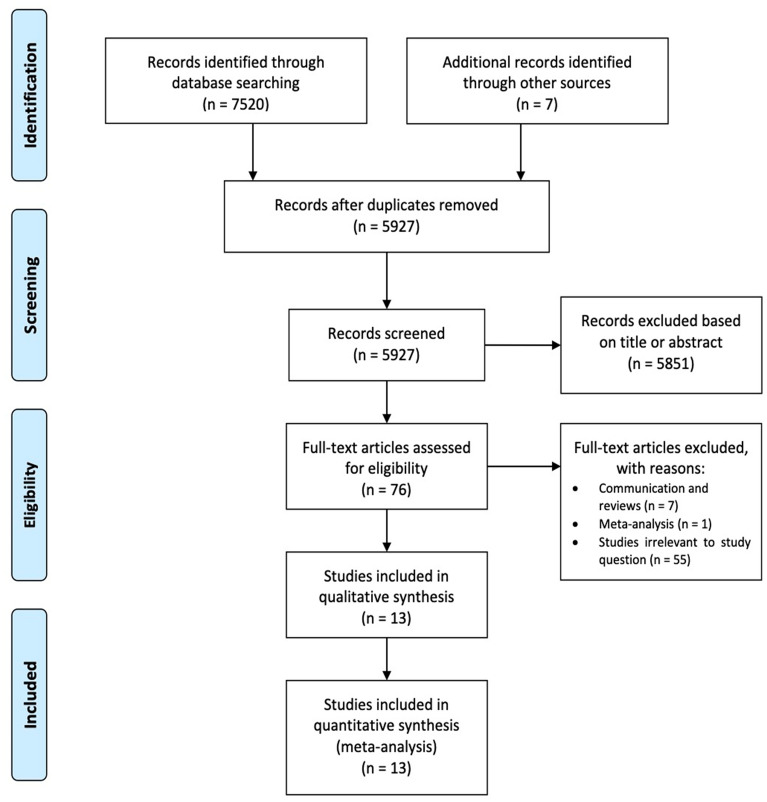
A total of 7520 records were identified through database searching. After duplicate records were removed, 5927 citations were retrieved and their titles and abstracts were screened; 13 studies were included in the final analysis, with a total of 48,891 patients. The full PRISMA flow diagram outlining the study selection process is available in Fig. 17,26,27. A complete list of studies included in the final analysis is presented in Table 1.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses flow diagram.
All studies were observational: 5 of them were unadjusted and 8 adjusted (adjustment details are shown in Table 1). Ten studies were multicenter; 3 originated from the United States, 2 from Israel, 1 each from Netherlands, Australia, Germany, Saudi Arabia, Poland, South Korea, Portugal and China.
The number of patients in each study ranged from 450 to 15,281. The mean age ranged from 56.1 to 75 years. The percentage of female sex in each study ranged from 18.0 to 43.5%. The prevalence of hypertension ranged from 43.0 to 87.3%, diabetes from 22.0 to 100.0%, smoking from 5.0 to 74.0%, prior cerebrovascular accident from 2.1 to 11.9% and prior myocardial infarction from 21.3 to 100.0%. The percentage of 1-vessel disease ranged from 0.0 to 47.2%, 2-vessels from 9.3 to 67.0% and 3-vesels from 16.3 to 100.0% (Supplementary Table 4).
Primary outcome
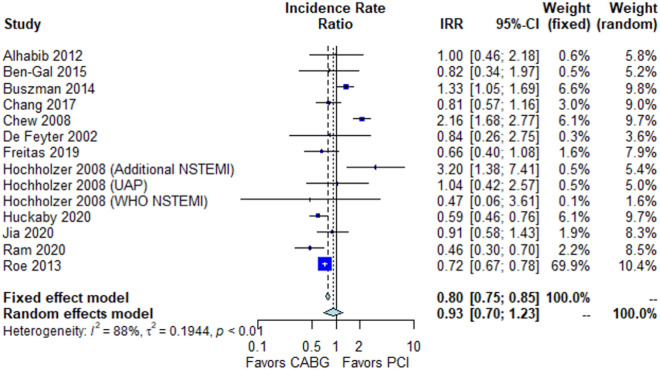
Detailed results of the meta-analysis are outlined in Fig. 2 and summarized in Table 2.
Figure 2.
Outcomes of CABG compared with PCI in non-ST-elevation acute coronary syndrome.
Table 2.
Outcomes summary.
| Outcome | Studies no. | Patients no. | Random effect estimate (95% CI), p-value | Fixed effect estimate (95% CI), p-value | Heterogeneity (I2, p-value) |
|---|---|---|---|---|---|
| Long-term mortality | 12 | 26,725 | IRR 0.93 [0.70; 1.23], p = 0.61 | IRR 0.80 [0.75; 0.85], p < 0.001 | 88.1%, p < 0.001 |
| Long-term MACE | 8 | 24,519 | IRR 0.64 [0.54; 0.76], p < 0.001 | IRR 0.69 [0.65; 0.73], p < 0.001 | 77.4%, p < 0.001 |
| Long-term re-revascularization | 6 | 22,573 | IRR 0.37 [0.30; 0.47], p < 0.001 | IRR 0.37 [0.30; 0.47], p < 0.001 | 42.7%, p = 0.11 |
| Long-term myocardial infarction | 7 | 7572 | IRR 0.96 [0.50; 1.84], p = 0.61 | IRR 1.56 [1.41; 1.74], p < 0.001 | 93.0%, p < 0.001 |
| Peri-operative mortality | 5 | 4334 | OR 1.36 [0.94; 1.95], p = 0.10 | OR 1.36 [0.94; 1.95], p = 0.10 | 60.0%, p = 0.83 |
| Long-term stroke | 6 | 13,197 | IRR 0.96 [0.72; 1.28], p = 0.81 | IRR 0.96 [0.72; 1.28], p = 0.81 | 0.0%, p = 0.497 |
| Late MACE plus stroke | 5 | 6842 | IRR 0.67 [0.50; 0.90], p = 0.007 | IRR 0.72 [0.66; 0.79], p < 0.001 | 86.9%, p < 0.001 |
CI confidence interval, IRR incidence rate ratio, MACE major adverse cardiovascular events, No number, OR odds ratios.
No significant difference between the groups was found in long-term mortality (IRR 0.93, 95% CI 0.70; 1.23, p = 0.83, Fig. 3). This finding was confirmed in the sensitivity analysis comparing adjusted and low risk of bias studies vs. unadjusted studies (p-interaction = 0.58, Supplementary Fig. 1).
Figure 3.
Forest plot showing pooled rates of long-term mortality in patients with non-ST-elevation acute coronary syndrome (NSTE-ACS) treated with coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI). Abbreviations: CABG coronary artery bypass grafting, CI confidence interval, IRR incidence rate ratio, NSTEMI non-ST-elevation myocardial infarction, PCI percutaneous coronary intervention, UAP unstable angina pectoris, WHO world health organization.
Leave-one-out analysis confirmed the solidity of the pooled estimate (Supplementary Fig. 2). Funnel plot did not demonstrate evidence of publication bias (Supplementary Fig. 3).
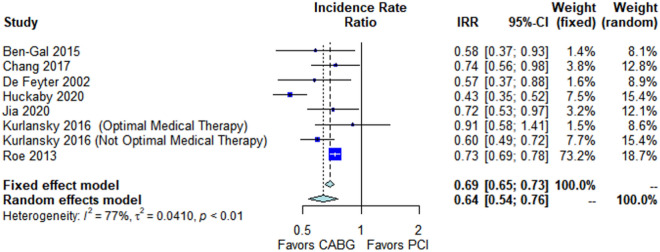
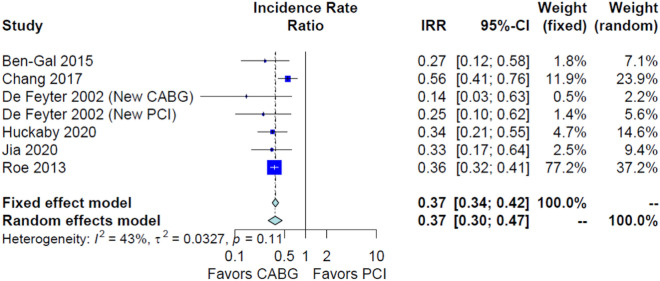
Secondary outcomes
CABG was associated with lower long-term major adverse cardiovascular events (IRR 0.64, 95% CI 0.54; 0.76, p < 0.001, Fig. 4) and long-term re-revascularization (IRR 0.37, 95% CI 0.30; 0.47, p < 0.001, Fig. 5). No significant difference was found in long-term myocardial infarction (IRR 0.96, 95% CI 0.50; 1.84, p = 0.61, Supplementary Fig. 4), peri-operative mortality (OR 1.36, 95% CI 0.94; 1.95, p = 0.10 Supplementary Fig. 5) and long-term stroke (IRR 0.96, 95% CI 0.72; 1.28, p = 0.81 Supplementary Fig. 6).
Figure 4.
Forest plot showing pooled rates of long-term major adverse cardiovascular events (MACE) in patients with non-ST-elevation acute coronary syndrome (NSTE-ACS) treated with coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI). Abbreviations: CABG coronary artery bypass grafting, CI confidence interval, IRR incidence rate ratio, PCI percutaneous coronary intervention.
Figure 5.
Forest plot showing pooled rates of long-term re-revascularization in patients with non-ST-elevation acute coronary syndrome (NSTE-ACS) treated with coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI). Abbreviations: CABG coronary artery bypass grafting, CI confidence interval, IRR incidence rate ratio, PCI percutaneous coronary intervention.
Meta-regression
At meta-regression, the year of publication, the proportion of patients with prior PCI and the left main disease were inversely associated with the IRR for the primary outcome (beta = − 0.07, p = 0.01; beta = − 0.05, p = 0.004; and beta = 0.004 respectively). The proportion of 1-vessel disease was associated with the IRR for the primary outcome (beta = 0.01, p = 0.04, Supplementary Table 5). That means that recent studies, studies with higher percentage of patients with prior PCI and left main disease reported lower long-term mortality in the CABG group; and studies with higher percentage of patients with 1-vessel disease reported lower long-term mortality in the PCI group.
Discussion
Our analysis suggests that for the treatment of NSTE-ACS, CABG and PCI are similar with respect to long-term mortality and myocardial infarction rates. The analysis further suggests that CABG is associated with decreased rates of long-term MACE and re-revascularization.
This is the first meta-analysis to address this important topic; our results are relevant as a substantial number of patients worldwide present with NSTE-ACS every year; in Germany over a period of 10 years 2.77 million cases of NSTE-ACS were recorded1. In the United States there are more than 1 million hospitalizations per year due to acute coronary syndrome28, with the proportion of patients with non-ST-elevation myocardial infarction being over 50% of all infarctions and increasing over time2. In other studies the annual incidence of NSTE-ACS has been reported with 88 per 100,000 inhabitants29.
Previous studies have suggested that an invasive strategy might be superior to a conservative one3,30, but have not summarized a recommendation for a specific invasive therapy (PCI or CABG). Currently, only 4–10% of the patients with NSTE-ACS receive CABG and 30–40% of them PCI1,31.
Our findings support the current guidelines, where no clear recommendation for PCI or CABG is given and a suggestion that the criteria applied for patients with stable coronary artery disease should be applied to stabilized patients with NSTE-ACS is made4. Both American and European guidelines recommend a heart-team approach to revascularization decisions in NSTE-ACS4,32 and that, factors such as extent and complexity of the coronary artery disease, as well as other factors should be considered.
It has been proposed that the survival benefit of PCI or CABG may be primarily due to an infarct-preventing mechanism rather than to revascularization per se5,33. This theory might provide a mechanistical explanation of our results, showing no mortality difference in 2 invasive treatments treating the same acute events. This line of argumentation finds supports in a meta-analysis we performed demonstrating an association of a survival advantage of CABG over PCI only in cases when there was also a difference in the rate of myocardial infarction34. This also highlights the importance of focusing on anatomically defined coronary artery disease, as recently published randomized data demonstrates that in patients with three-vessel coronary artery disease, the incidence of death, myocardial infarction, or stroke at one year was significantly lower for CABG compared to fractional flow reserve guided PCI35.
This argumentation is also supported by the results of the meta-regression we performed, showing that the recent studies and studies with higher percentage of patients with prior PCI reported lower long-term mortality in the CABG group; and studies with higher percentage of patients with 1-vessel disease reported lower long-term mortality in the PCI group. This seems to explain also the apparent similarity in effect estimates stemming from unadjusted and adjusted studies, with older studies being often unadjusted and the recent ones adjusted.
If we further explore the apparent discrepancies in adjusted effect estimates from some specific studies, older studies (e.g., Hochholzer et al., 2008) showed a survival advantage for PCI, while newer ones (e.g., Ram et al., 2020) showed a survival advantage for CABG. However, the percentage of the patients who received optimal medical therapy (antiplatelet, diuretic and statin therapy) was massively lower in for the CABG group in the cohort analyzed by Hochholzer (e.g., 90% vs. 2.9% for dual antiplatelet therapy), potentially providing an explanation for the observed differences.
Study strength and limitations
This is the first meta-analysis to address this important topic. Moreover, we analyzed 5 different outcomes and performed different subgroup analyses and a meta-regression of 14 different pre-operative factors. However, this work has the intrinsic limitations of observational series, including the risk of methodological heterogeneity of the included studies, residual confounders and ecological fallacy of meta-regression. In addition, treatment allocation bias is likely present in all observational series comparing two interventions with different operative risk and invasiveness.
Conclusion
Our analysis suggests that for the treatment of NSTE-ACS, CABG and PCI are similar with respect to long-term mortality and myocardial infarction rates. The analysis further suggests that CABG is associated with decreased rates of long-term MACE and re-revascularization. Randomized comparisons in this specific setting are necessary.
Supplementary Information
Acknowledgements
We thank Mr. Benjamin May for editorial assistance.
Abbreviations
- CABG
Coronary artery bypass grafting
- CAD
Coronary artery disease
- MACE
Major cardiovascular adverse events
- MI
Myocardial infarction
- NSTE-ACS
Non-ST-elevation acute coronary syndrome
- NSTEMI
Non-ST-elevation myocardial infarction
- PCI
Percutaneous coronary intervention
- UAP
Unstable angina pectoris
Author contributions
H.K., T.C., M.G. and T.D. designed the study. M.D. performed the literature review in the three different libraries. H.K. and T.C. selected the studies, qualified the studies according to the risk of bias, performed the data abstraction, built the tables and organized the results. M.R. and N.B.R. performed the statistical analyses. P.W.S., G.B.Z., M.G. and T.D. analyzed the data. H.K., T.C., N.B.R., M.G. and T.D. wrote the manuscript. All the authors read and approved the final version of manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Data availability
The datasets generated analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hristo Kirov and Tulio Caldonazo.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-09158-0.
References
- 1.Neumann JT, et al. Temporal trends in incidence and outcome of acute coronary syndrome. Clin. Res. Cardiol. 2020;109:1–7. doi: 10.1007/s00392-020-01612-1. [DOI] [PubMed] [Google Scholar]
- 2.Khera S, et al. Non-ST-elevation myocardial infarction in the United States: Contemporary trends in incidence, utilization of the early invasive strategy, and in-hospital outcomes. J. Am. Heart Assoc. 2014;3(4):e000995. doi: 10.1161/JAHA.114.000995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bavry AA, et al. Benefit of early invasive therapy in acute coronary syndromes: A meta-analysis of contemporary randomized clinical trials. J. Am. Coll. Cardiol. 2006;48(7):1319–1325. doi: 10.1016/j.jacc.2006.06.050. [DOI] [PubMed] [Google Scholar]
- 4.Neumann F-J, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019;40(2):87–165. doi: 10.1093/eurheartj/ehy394. [DOI] [PubMed] [Google Scholar]
- 5.Doenst T, et al. PCI and CABG for treating stable coronary artery disease: JACC review topic of the week. J. Am. Coll. Cardiol. 2019;73(8):964–976. doi: 10.1016/j.jacc.2018.11.053. [DOI] [PubMed] [Google Scholar]
- 6.Doenst T, et al. Improving terminology to describe coronary artery procedures: JACC review topic of the week. J. Am. Coll. Cardiol. 2021;78(2):180–188. doi: 10.1016/j.jacc.2021.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Page MJ, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sá M, et al. Coronary artery bypass graft surgery improves survival without increasing the risk of stroke in patients with ischemic heart failure in comparison to percutaneous coronary intervention: A meta-analysis with 54,173 patients. Braz. J. Cardiovasc. Surg. 2019;34(4):396–405. doi: 10.21470/1678-9741-2019-0170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells, G., The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis.http://www.ohri.ca/programs/clinical_epidemiology.oxford.htm, 2004.
- 10.de Feyter PJ, et al. Bypass surgery versus stenting for the treatment of multivessel disease in patients with unstable angina compared with stable angina. Circulation. 2002;105(20):2367–2372. doi: 10.1161/01.cir.0000016643.34907.17. [DOI] [PubMed] [Google Scholar]
- 11.Chew DP, et al. Patients with non-ST-elevation acute coronary syndromes undergoing coronary artery bypass grafting in the modern era of antithrombotic therapy. Am. Heart J. 2008;155(2):239–244. doi: 10.1016/j.ahj.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Hochholzer W, et al. Percutaneous coronary intervention versus coronary artery bypass grafting as primary revascularization in patients with acute coronary syndrome. Am. J. Cardiol. 2008;102(2):173–179. doi: 10.1016/j.amjcard.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 13.AlHabib KF, et al. Prevalence, predictors, and outcomes of conservative medical management in non-ST-segment elevation acute coronary syndromes in Gulf RACE-2. Angiology. 2012;63(2):109–118. doi: 10.1177/0003319711409200. [DOI] [PubMed] [Google Scholar]
- 14.Roe MT, et al. Long-term outcomes after invasive management for older patients with non-ST-segment elevation myocardial infarction. Circ. Cardiovasc. Qual. Outcomes. 2013;6(3):323–332. doi: 10.1161/CIRCOUTCOMES.113.000120. [DOI] [PubMed] [Google Scholar]
- 15.Buszman PE, et al. Comparison of stenting and surgical revascularization strategy in non-ST elevation acute coronary syndromes and complex coronary artery disease (from the milestone registry) Am. J. Cardiol. 2014;114(7):979–987. doi: 10.1016/j.amjcard.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Ben-Gal Y, et al. Surgical versus percutaneous coronary revascularization for multivessel disease in diabetic patients with non-ST-segment-elevation acute coronary syndrome: Analysis from the Acute Catheterization and Early Intervention Triage Strategy trial. Circ. Cardiovasc. Interv. 2015;8(6):e002032. doi: 10.1161/CIRCINTERVENTIONS.114.002032. [DOI] [PubMed] [Google Scholar]
- 17.Kurlansky P, et al. Coronary artery bypass graft versus percutaneous coronary intervention. Circulation. 2016;134(17):1238–1246. doi: 10.1161/CIRCULATIONAHA.115.021183. [DOI] [PubMed] [Google Scholar]
- 18.Chang M, et al. Comparison of outcome of coronary artery bypass grafting versus drug-eluting stent implantation for non–ST-elevation acute coronary syndrome. Am. J. Cardiol. 2017;120(3):380–386. doi: 10.1016/j.amjcard.2017.04.038. [DOI] [PubMed] [Google Scholar]
- 19.Freitas P, et al. Coronary artery bypass grafting versus percutaneous coronary intervention in patients with non–ST-Elevation myocardial infarction and left main or multivessel coronary disease. Am. J. Cardiol. 2019;123(5):717–724. doi: 10.1016/j.amjcard.2018.11.052. [DOI] [PubMed] [Google Scholar]
- 20.Huckaby LV, et al. Revascularization following non-ST elevation myocardial infarction in multivessel coronary disease. J. Card. Surg. 2020;35(6):1195–1201. doi: 10.1111/jocs.14539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jia S, et al. Comparison of percutaneous coronary intervention, coronary artery bypass grafting and medical therapy in non-ST elevation acute coronary syndrome patients with 3-vessel disease. Circ. J. 2020;84(10):1718–1727. doi: 10.1253/circj.CJ-20-0300. [DOI] [PubMed] [Google Scholar]
- 22.Ram E, et al. Outcomes of different revascularization strategies among patients presenting with acute coronary syndromes without ST elevation. J. Thorac. Cardiovasc. Surg. 2020;160(4):926–935.e6. doi: 10.1016/j.jtcvs.2019.08.130. [DOI] [PubMed] [Google Scholar]
- 23.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010;36(3):1–48. [Google Scholar]
- 24.Schwarzer G, Carpenter JR, Rücker G. Meta-analysis with R. Springer; 2015. [Google Scholar]
- 25.Higgins JP, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 27.Hutton B, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015;162(11):777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 28.Virani SS, et al. Heart disease and stroke statistics—2020 update: A report from the American Heart Association. Circulation. 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 29.Antoniades L, et al. Epidemiology of acute coronary syndromes in the Mediterranean island of Cyprus (CYPACS study, Cyprus study of acute coronary syndromes) Hellenic J. Cardiol. 2014;55(55):139–149. [PubMed] [Google Scholar]
- 30.Reaño JDP, et al. A systematic review and meta-analysis on the effectiveness of an invasive strategy compared to a conservative approach in patients> 65 years old with non-ST elevation acute coronary syndrome. PLoS ONE. 2020;15(2):e0229491. doi: 10.1371/journal.pone.0229491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ranasinghe I, et al. Risk stratification in the setting of non-ST elevation acute coronary syndromes 1999–2007. Am. J. Cardiol. 2011;108(5):617–624. doi: 10.1016/j.amjcard.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Amsterdam EA, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014;64(24):e139–e228. doi: 10.1016/j.jacc.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 33.Doenst T, Sigusch H. Surgical collateralization: The hidden mechanism for improving prognosis in chronic coronary syndromes. J. Thor. Cardiovasc. Surg. 2020;163:703–708. doi: 10.1016/j.jtcvs.2020.10.121. [DOI] [PubMed] [Google Scholar]
- 34.Gaudino, M., et al., Difference in spontaneous myocardial infarction and mortality in percutaneous versus surgical revascularization trials: A systematic review and meta-analysis. J. Thor. Cardiovasc. Surg. (2021). [DOI] [PMC free article] [PubMed]
- 35.Fearon WF, et al. Fractional flow reserve-guided pci as compared with coronary bypass surgery. New Engl. J. Med. 2021;386:128–137. doi: 10.1056/NEJMoa2112299. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated analyzed during the current study are available from the corresponding author on reasonable request.