Abstract
The NOTCH gene was identified approximately 110 years ago. Classical studies have revealed that NOTCH signaling is an evolutionarily conserved pathway. NOTCH receptors undergo three cleavages and translocate into the nucleus to regulate the transcription of target genes. NOTCH signaling deeply participates in the development and homeostasis of multiple tissues and organs, the aberration of which results in cancerous and noncancerous diseases. However, recent studies indicate that the outcomes of NOTCH signaling are changeable and highly dependent on context. In terms of cancers, NOTCH signaling can both promote and inhibit tumor development in various types of cancer. The overall performance of NOTCH-targeted therapies in clinical trials has failed to meet expectations. Additionally, NOTCH mutation has been proposed as a predictive biomarker for immune checkpoint blockade therapy in many cancers. Collectively, the NOTCH pathway needs to be integrally assessed with new perspectives to inspire discoveries and applications. In this review, we focus on both classical and the latest findings related to NOTCH signaling to illustrate the history, architecture, regulatory mechanisms, contributions to physiological development, related diseases, and therapeutic applications of the NOTCH pathway. The contributions of NOTCH signaling to the tumor immune microenvironment and cancer immunotherapy are also highlighted. We hope this review will help not only beginners but also experts to systematically and thoroughly understand the NOTCH signaling pathway.
Subject terms: Drug development, Target identification, Cancer microenvironment, Differentiation, Neurogenesis
Introduction
The NOTCH gene was first named in studies of Drosophila melanogaster with notched wings in the 1910s1–3. Homologs of NOTCH were then identified in multiple metazoans, and all these NOTCH homologs shared similar structures and signaling components4–7. NOTCH variants were also found in ancient humans and were found to be involved in brain size control8. Generally, NOTCH is considered an ancient and highly conserved signaling pathway. NOTCH signaling participates in various biological processes across species, such as organ formation, tissue function, and tissue repair; thus, aberrant NOTCH signaling may cause pathological consequences.
In the past two decades, various drugs targeting NOTCH signaling have been tested in preclinical and clinical settings, yet no drug has been approved. Recent studies indicate that the NOTCH pathway is far more extensive and complicated than previously believed. As immunotherapy has revolutionized cancer treatment, NOTCH signaling and its relation with antitumor immunity have attracted the attention of scientists.
This review aims to illustrate the history, architecture, regulatory mechanisms, relation to health and diseases, and therapeutic applications of the NOTCH signaling pathway. In regard to specific behaviors of the NOTCH signaling pathway, we tried to focus on studies of mammals rather than those of other animals. We hope this review will help not only beginners but also experts to systematically and thoroughly understand the NOTCH signaling pathway.
A brief history of notch signaling
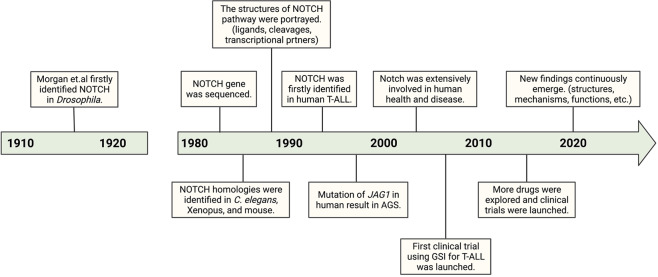
The NOTCH gene was first described in a study of D. melanogaster mutants with notched wings in the 1910s1,3,4. Haploinsufficiency of NOTCH caused D. melanogaster to have notches at the end of their wings, while complete insufficiency was lethal. The discovery of this phenotype inspired the later proposed nomenclature. The D. melanogaster NOTCH gene was then isolated9 and sequenced10 in the 1980s, and the putative NOTCH protein was found to span the membrane and contain many epidermal growth factor (EGF)-like repeats11. Studies of NOTCH signaling in D. melanogaster then increased12–18, drawing attention to the whole signaling pathway. In 1988 and 1989, LIN-12 and GLP-1 were identified as NOTCH homologs in Caenorhabditis elegans4,5, seemingly associated with C. elegans development5,19,20. In 1990, XOTCH (a homolog of D. melanogaster NOTCH) was identified in Xenopus6, and the cDNA of the mammalian NOTCH gene was cloned7. Since then, research on NOTCH in other animals has gained popularity. More details of NOTCH signaling have been clarified, and as such, NOTCH has been recognized as an ancient and highly conserved signaling pathway across metazoans21–26.
In 1991, the NOTCH gene was first linked to human T cell acute lymphoblastic leukemia (T-ALL). In 1997, Alagille syndrome (AGS) was found to be caused by the mutation of JAG1, which encodes a ligand of NOTCH127,28. AGS is a noncancerous autosomal dominant disorder characterized by the abnormal development of multiple organs. Since these discoveries, the relationship of NOTCH with human health and diseases has been extensively studied. In addition, translational studies have been performed. The first clinical trial involving NOTCH signaling was launched in 2006, using a γ-secretase inhibitor to treat patients with T-ALL or other leukemias29,30. It was halted due to severe diarrhea, yet the results largely promoted the therapeutic targeting of NOTCH signaling. Various drugs and antibodies targeting other components of NOTCH signaling have been explored in preclinical and clinical settings, although none has yet been approved. In recent years, many new studies have been appearing, such as detailed structural analyses31–33, analyses of complicated regulatory mechanisms34,35, and analyses of diversified functions in health and diseases36–38, highlighting some unexplored areas of NOTCH signaling. A brief history of NOTCH signaling is shown in Fig. 1. A strong understanding of NOTCH signaling is required; thus, more efforts are needed.
Fig. 1.
A brief history of the NOTCH signaling pathway. T-ALL, T cell acute lymphoblastic leukemia; AGS, Alagille syndrome; GSI, γ-secretase inhibitor
The architecture of notch signaling
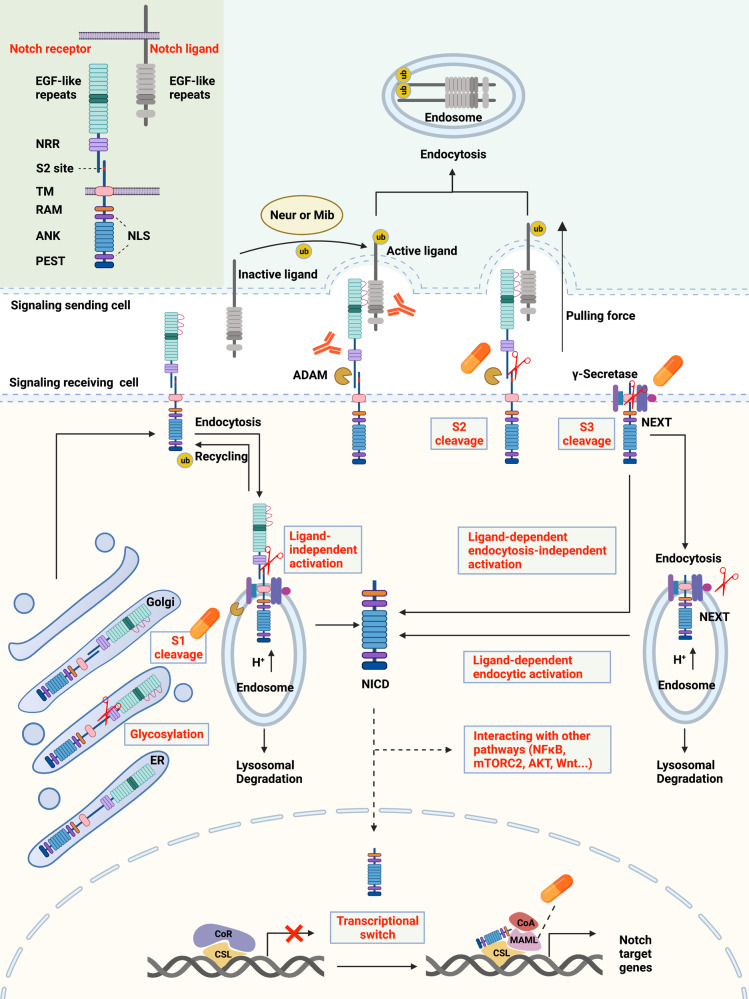
The NOTCH signaling pathway has certain characteristics. Classical signaling pathways, mediated by G protein-coupled receptors (GPCRs)39 and enzyme-linked receptors40, have multiple intermediates between the membranous receptors and nuclear effectors. However, the canonical NOTCH signaling pathway has no intermediate, with receptors directly translocated into the nucleus after three cleavages21,41,42 (Fig. 2). In addition, S2 cleavage of NOTCH receptors is triggered by interactions with ligands expressed on adjacent cells, indicating a rather narrow range of NOTCH signaling. NOTCH signaling is involved in multiple aspects of metazoans’ life42, including cell fate decisions, embryo and tissue development, tissue functions and repair, as well as noncancerous and cancerous diseases. Thus, understanding of the architecture of the NOTCH signaling pathway is necessary.
Fig. 2.
Overview of the NOTCH signaling pathway and therapeutic targets. In signal-receiving cells, NOTCH receptors are first generated in the ER and then trafficked to the Golgi apparatus. During trafficking, NOTCH receptors are glycosylated at the EGF-like repeat domain (red curves). Then, in the Golgi apparatus, NOTCH receptors are cleaved into heterodimers (S1 cleavage) and transported to the cell membrane. With the help of ubiquitin ligases, some of the NOTCH receptors on the cell membrane are endocytosed into endosomes. Endosomes contain an acidic environment with ADAMs and γ-secretase. The NOTCH receptors in endosomes can be recycled to the cell membrane, cleaved into NICD, or transported into lysosomes for degradation. In signal-sending cells, NOTCH ligands are distributed on the cell membrane and can bind to NOTCH receptors on signal-receiving cells. However, the ligands are inactive before ubiquitylation by Neur or Mib. After ubiquitylation, ligands can be endocytosed, thus producing a pulling force for the binding receptors. Without the pulling force, the S2 site (red marks) of NOTCH receptors is hidden by the NRR domain, and thus, the NOTCH receptors are resistant to cleavage by ADAMs. With the pulling force, the NRR domain is extended, therefore exposing the S2 site for cleavage. ADAMs and the pulling force are both necessary for S2 cleavage. After S2 cleavage, the remaining part of the NOTCH receptor is called NEXT. NEXT can be further cleaved on the cell membrane by γ-secretase or endocytosed into endosomes. In the former mode, NICD is released on the cell membrane. In the latter mode, NEXT can be cleaved into NICD or transported into lysosomes for degradation. In total, there are three approaches to generate NICD, classified as ligand-independent activation, ligand-dependent endocytosis-independent activation, and ligand-dependent endocytic activation. NICD can be translocated into the nucleus or remain in the cytoplasm to crosstalk with other signaling pathways, such as NFκB, mTORC2, AKT, and Wnt. The classical model proposes that, in the absence of NICD, CSL binds with corepressors to inhibit the transcription of target genes. Once NICD enters the nucleus, it can bind with CSL and recruit MAMLs, releasing corepressors, recruiting coactivators, and thus promoting the transcription of NOTCH target genes. There are two main approaches to inhibit NOTCH signaling for therapy. One is designing inhibitors of the key components of the pathways, including the enzymes that participate in S1 cleavage, ADAMs, γ-secretase, and MAML. The other one is producing antibody-drug conjugates against NOTCH receptors and ligands. The protein structures of NOTCH ligands and receptors are shown in the top left corner. NICD, NOTCH intracellular domain; ADAM, a disintegrin and metalloproteinase domain-containing protein; Neur, Neuralized; Mib, Mindbomb; NRR, negative regulatory region; NEXT, NOTCH extracellular truncation; CSL, CBF-1/suppressor of hairless/Lag1; MAMLs, Mastermind-like proteins; TM, transmembrane domain; RAM, RBPJ association module; ANK, ankyrin repeats; PEST, proline/glutamic acid/serine/threonine-rich motifs; NLS, nuclear localization sequence; CoR, corepressor; CoA, coactivator; ub, ubiquitin
The receptors and ligands of NOTCH signaling
D. melanogaster has only one NOTCH receptor9. C. elegans has two redundant NOTCH receptors, LIN-12 and GLP-14. Mammals have four NOTCH paralogs, NOTCH1, NOTCH2, NOTCH3, and NOTCH421, showing both redundant and unique functions. In humans, NOTCH1, NOTCH2, NOTCH3, and NOTCH4 are located on chromosomes 9, 1, 19, and 6, respectively. After transcription and translation, NOTCH precursors are generated in the endoplasmic reticulum (ER) and then translocated into the Golgi apparatus. In the ER, the NOTCH precursors are initially glycosylated at the EGF-like repeat domain. Glycosylations include O-fucosylation, O-glucosylation, and O-GlcNAcylation, which are catalyzed by the enzymes POFUT1, POGLUT1, and EOGT1, respectively43. Subsequently, in the Golgi apparatus, O-fucose is extended by the Fringe family of GlcNAc transferases, while O-glucose is extended by the xylosyltransferases GXYLT1/2 and XXYLT144–46. The glycosylation of NOTCH is vital to its stability and function. Alteration of core glycosylation enzymes severely inhibits the activity of NOTCH signaling47–51, making these enzymes vital for further research.
The glycosylated NOTCH precursors undergo S1 cleavage in the Golgi apparatus before being transported to the cell membrane. The cleavage always occurs at a conserved site (heterodimerization domain) and is catalyzed by a furin-like protease, cutting NOTCH into a heterodimer (mature form). Here, we take mouse NOTCH1 as an example to illustrate the structure of mature NOTCH on the cell membrane.
The extracellular domain (N-terminal) contains 36 EGF-like repeats and a negative regulatory region (NRR)43. The 11th and 12th EGF-like repeats usually interact with ligands43, although a new study found that many more motifs of the extracellular domain are involved in ligand binding52. The NRR domain is composed of three cysteine-rich Lin12-NOTCH repeats (LNRs) and a heterodimerization region critical for S2 cleavage. Located after the membrane-spanning region, the intracellular RBPJ association module (RAM) domain is responsible for interacting with transcription factors in the nucleus, and seven ankyrin repeat (ANK) domains are observed in the RAM domain. Nuclear localization sequences are located on both sides of the ANK domains. At the end of the intracellular domain (C-terminus), there are conserved proline/glutamic acid/serine/threonine-rich motifs (PEST domains) that contain degradation signals and are thus critical for the stability of the NOTCH intracellular domain (NICD). Mammalian NOTCH2-4 have similar structures to NOTCH1, diverging mainly in the number of EGF-like repeats, the glycosylation level of the EGF-like repeats, and the length of the PEST domains. The level of NOTCH receptors on the cell membrane is controlled by constitutive endocytosis, which is promoted by ubiquitin ligases. An appreciable amount of NOTCH receptors are ubiquitinated and degraded in the proteosome, while the rest are expressed on the cell membrane to transmit signals.
Humans and mice have five acknowledged NOTCH ligands21,53,54: delta-like ligand 1 (DLL1), delta-like ligand 3 (DLL3), delta-like ligand 4 (DLL4), Jagged-1 (JAG1), and Jagged-2 (JAG2), all of which present redundant and unique functions. For instance, DLL1 governs cell differentiation and cell-to-cell communication54, DLL3 suppresses cell growth by inducing apoptosis55, DLL4 activates NF-κΒ signaling to enhance vascular endothelial factor (VEGF) secretion and tumor metastasis56, JAG1 enhances angiogenesis54, and JAG2 promotes cell survival and proliferation54.
The structures of the NOTCH ligands are partially similar to those of the receptors. The ligands are also transmembrane proteins, and the extracellular domains contain multiple EGF-like repeats, which determine the crosstalk with corresponding receptors. The levels and functions of the ligands are also controlled by ubiquitylation and endocytosis (discussed in the section “Ligand ubiquitylation”).
The canonical NOTCH signaling pathway
The mature NOTCH receptors on the cell membrane are heterodimers, with the heterodimerization domain being cleaved in the Golgi apparatus (S1 cleavage). Generally, binding to extracellular domains of NOTCH receptors allows ligands to initiate endocytosis. Such endocytosis induces receptors to change their conformation, exposing the enzymatic site for S2 cleavage57. Receptors then experience S3 cleavage, changing into the effector form: NOTCH intracellular domain (NICD). NICD is degraded in the cytoplasm or transported into the nucleus to regulate the transcription of target genes (Fig. 2).
S2 cleavage is the only ligand-binding step and is thus vital for signal initiation. The structural basis of S2 cleavage is illustrated in Fig. 2. The S2 site (metalloprotease site) is hidden by the LNR domain in the silent phase, referred to as the “autoinhibited conformation”58. Once bound with ligands, the receptor extends the LNR domain and exposes the S2 site for cleavage59–61. The core enzymes for S2 cleavage include a disintegrin and metalloprotease 10 (ADAM 10) and its isoforms ADAM 17 and ADAMTS162–64, which are popular targets for drug discovery. The product of S2 cleavage (larger part) is composed of the transmembrane domain and the intracellular domain, which is also called NOTCH extracellular truncation (NEXT)65.
NEXT is further cleaved at the S3 site, releasing NICD, which can be translocated into the nucleus and function as a transcription factor. The enzyme responsible for S3 cleavage is γ-secretase, which contains the catalytic subunits presenilin1 or presenilin2 (PS1 or PS2)66,67, APH-1, PEN-2, and nicastrin (NCT)68. However, the classical substrates for γ-secretase contain NOTCH receptors and amyloid precursor protein (APP), the successive cleavage of which is related to Alzheimer’s disease69–72. The structural basis for γ-secretase to recognize NOTCH or APP had remained unclear until recently, when Yigong Shi’s team elucidated the structural basis31,32. In short, the transmembrane helix of NOTCH or APP closely interacts with the surrounding transmembrane helix of PS1 (the catalytic subunit of γ-secretase); thus, the hybrid β-sheet promotes substrate cleavages, although some differences exist between NOTCH and APP73. Structural information would accelerate the discovery of substrate-specific inhibitors of NOTCH and APP. Additionally, S3 cleavage can occur both on the cell membrane and in the endosome after NEXT is endocytosed, termed the endocytosis-independent model and endocytic-activation model, respectively74.
After release from the cell membrane, NICD is translocated into the nucleus to regulate gene transcription, the mechanism of which may be related to the nuclear localization sequences of NICD and importins alpha 3, 4, and 775. However, the details of this translocation remain unclear. CBF-1/suppressor of hairless/Lag1 (CSL, also called recombination signal binding protein-J, RBPJ) is a ubiquitous transcription factor (TF) that recruits other co-TFs to regulate gene expression76,77. The target genes of NOTCH signaling are largely determined by the Su (H) motif of CSL, which is responsible for DNA binding21. The canonical NOTCH target gene families are Hairy/Enhancer of Split (HES) and Hairy/Enhancer of Split related to YRPW motif (HEY)21.
In the traditional model of NICD regulating gene transcription21,42,78,79, CSL recruits corepressor proteins and histone deacetylases (HDACs) to repress the transcription of target genes without NICD binding. NICD binding can change the conformation of the CSL-repressing complex, dissociating repressive proteins and recruiting activating partners to promote the transcription of target genes. The transcriptional coactivator Mastermind-like protein (MAML) is one of the core activating partners that can recognize the NICD/CSL interface, after which it recruits other activating partners. Drugs targeting MAML are under study.
Recently, Kimble et al. used single-molecule fluorescence in situ hybridization to study the NOTCH transcriptional program in germline stem cells of C. elegans and found that NICD dictated the probability of transcriptional firing and thus the number of nascent transcripts80. However, NICD did not orchestrate a synchronous transcriptional response in the nucleus, in contrast to that seen in the classical model. Gomez-Lamarca et al. found similar results in D. melanogaster81. NICD promoted the opening of chromatin and enhanced the recruitment of both the NICD-containing activating CSL complex and the NICD-free repressive CSL complex. Bray et al. proposed a new model to interpret their findings. In the NOTCH-off state, chromatin is compact, and only the NICD-free (repressing) CSL complex regulates transcription. In the NOTCH-on state, chromatin is loosened and bound to both NICD-containing (activating) and NICD-free (repressive) CSL complexes. Because the number of activating complexes is greater than that of repressive complexes after NICD enters the nucleus, NICD promotes the transcription of target genes. Bray et al. further reported that nucleosome turnover occurred frequently at NOTCH-responsive regions and depended on the Brahma SWI/SNF chromatin remodeling complex82. Consistently, Kimble et al. found that NOTCH signaling regulated the duration of the transcriptional burst but not the intensity of signaling or the time between bursts83. Oncogenic NOTCH is also considered to enhance repositioning to promote the transcription of genes, such as MYC84. In general, the new model from Bray et al. helps explain the flexibility of NOTCH signaling, although the details still require further elucidation.
The noncanonical NOTCH signaling pathway
Pathways other than canonical signaling pathway are also able to initiate signaling, classified as noncanonical NOTCH signaling pathways. Although the mature NOTCH receptors on the cell membrane are capable of ligand binding, some are endocytosed for renewal. Endocytosed NOTCH receptors can return to the cell membrane, be degraded in lysosomes or activated in endosomes (ligand-independent activation)74,85. Interestingly, endosome trafficking can also be regulated by NOTCH signaling86. Endosomes have been proven to contain ADAM and γ-secretase87. Ligand-independent activation of NOTCH signaling is vital to T cell development88. One example of ligand-independent activation is T cell receptor (TCR)-mediated self-amplification87. The activated TCR/CD3 complex can activate the signaling axis of LCK-ZAP70-PLCγ-PKC. PKC then activates ADAM and γ-secretase on the endosome to initiate S2 and S3 cleavage and thus NOTCH signaling. Activated NOTCH signaling can further upregulate immune-related genes to amplify the immune response.
Independent of CSL, NICD can interact with the NF-κB, mTORC, PTEN, AKT, Wnt, Hippo, or TGF-β pathways at the cytoplasmic and/or nuclear level to regulate the transcription of target genes34,89–96. The crosstalk between NICD and NF-κB affects the malignant properties of cervical cancer89, colorectal cancer97, breast cancer98, and small-cell lung cancer cells99. Targeting the NF-κB pathway could be an effective way to block noncanonical NOTCH signaling.
In addition to those mentioned above, there is a newly identified mechanism of noncanonical activation. In the classical model, S3 cleavage is necessary for NOTCH receptors to release NICD and thus regulate the transcription of target genes. However, membrane-tethered NOTCH may activate the PI3K-AKT pathway, promoting the transcription of interleukin-10 and interleukin-12100. In blood flow-mediated NOTCH signaling, the transmembrane domain instead of NICD recruits other partners to promote the formation of an endothelial barrier35. NOTCH3 itself can promote the apoptosis of tumor endothelial cells, independent of cleavage and transcription regulation101. The JAG1 intracellular domain can promote tumor growth and epithelial–mesenchymal transition (EMT) without binding to NOTCH receptors102. These noncanonical mechanisms provide this ancient signaling pathway with more unique functions while massively increasing its complexity.
The mechanisms regulating NOTCH signaling
Glycosylation
The glycosylation of NOTCH receptors on specific EGF-like repeats is crucial for the maturation of receptors, which also affects signaling output. First, O-fucosylation catalyzes the enzyme Pofut1 to affect ligand binding. Elimination of Pofut1 greatly influences the ligand binding of NOTCH signaling in embryonic stem cells, lymphoid cells, and angiogenic cells of mice103–105. The aberration of fringe family proteins, which catalyzes the elongation of O-fucose, can also affect ligand binding106–109. Second, O-glucose of NOTCH receptors is involved in S2 cleavage. Alteration of O-glucosylation damages the proteolysis of NOTCH receptors after ligand binding110,111. Third, the sites of O-glycosylation, such as EGF 12, are important regions for ligand binding, the loss of which decreases NOTCH signaling in T cells112. Furthermore, EGF 28 might contribute to DLL1-mediated NOTCH1 signaling113. Targeting glycosylation is also thought to effectively inhibit NOTCH signaling114.
Receptor trafficking
After S1 cleavage, most mature NOTCH proteins are transported to the cell membrane. However, reaching the membrane does not guarantee stability. NOTCH receptors are constitutively endocytosed through a process modulated by ubiquitin ligases such as FBXW, NUMB, ASB, DTX1, NEDD4, ITCH, and CBL74,115–118. Endocytosed NOTCH can be recycled to the cell membrane or trapped in the cytoplasm74; thus, receptor trafficking can directly affect the level of NOTCH receptors on the cell membrane. Furthermore, the endocytosed NOTCH receptors in the cytoplasm can be degraded or activated. Degradation is usually initiated by the endosomal sorting complex required for transport (ESCRT) system119–122, the failure of which also lays the foundation for receptor activation. However, the mechanism of ligand-independent activation remains clear123–125. The balance between degradation and activation after endocytosis is closely related to downstream signaling79. The specific distribution of receptors and ligands on the cell membrane can also influence the regional intensity of NOTCH signaling79.
Ligand ubiquitylation
Unlike the ubiquitylation of NOTCH receptors, ubiquitylation of ligands (usually catalyzed by Neuralized (Neur) and Mindbomb (Mib)) in signal-sending cells is necessary for signaling activation. Without Neur or Mib, NOTCH signaling decreases significantly126–128. One explanation is that the endocytosis of ligands promotes exposure of the NRR domain of the receptor for S2 cleavage129,130.
Cis-inhibition
Receptors and ligands expressed on different cells can initiate signal transduction. However, receptors and ligands expressed on the same cell both inhibit and activate the whole signaling pathway, termed cis-inhibition and cis-activation79,131. DLL3 seems to operate only in cis-inhibition132,133. The loss of DLL3 increases NOTCH activity during T cell development in vivo133. DLL1-NOTCH1 can function in both cis- and trans-activation131. Thus, the balance between cis- and trans-interactions can be vital to signaling output.
Other regulatory mechanisms
Various signals regulate the transcription of NOTCH receptors and thus the whole signaling pathway, such as AKT, RUNX1, SIRT6, CBFB, and DEC1134–138. Many noncoding RNAs regulate the level of NOTCH receptors, such as microRNA-26a, microRNA-26b, microRNA-153, microRNA-182, and microRNA-34a139–142. Nitric oxide regulates the activity of ADAM17 and USP9X and ultimately NOTCH signaling143,144. Calzado et al. found that dual-specificity tyrosine-regulated kinase 2 (DYRK2) phosphorylated the NOTCH1 intracellular domain to promote its degradation by FBXW7145. In the classical model, NOTCH signaling is prompted through the interaction between receptors and ligands in extracellular domains. However Suckling et al. found that the interaction between the C2 domain of NOTCH ligands and the phospholipid membrane of receptor-containing cells modulated NOTCH signaling.146 This finding provides a possible explanation for the diversified consequences of NOTCH signaling mediated by different ligand–receptor interactions.
Notch signaling in organ development and repair
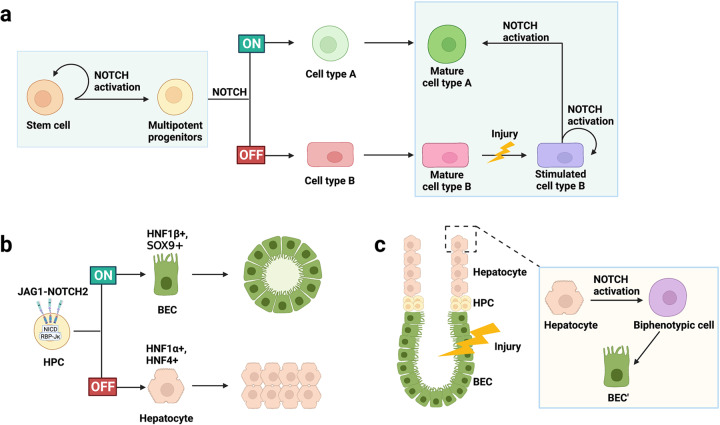
As a highly conserved signaling pathway, NOTCH deficiency leads to serious embryonic lethality. NOTCH signaling is active in the early stage of embryonic development but is maintained at a low level in the mature stage of body development. It also increases rapidly under conditions of injury or stress and is indispensable for development and injury repair (Fig. 3). First, NOTCH signaling promotes the self-renewal and dedifferentiation of stem and progenitor cells, thus maintains progenitor stemness and the stem cell pool. Among these cells, neural stem cells147–149 and multipotent progenitor cells (MPCs)150,151 are classic representatives. Different combinations of NOTCH ligands and receptors promote stem cell proliferation and inhibit terminal differentiation. Second, NOTCH signaling is involved in the selection of cell fate. Based on temporal and spatial expression of NOTCH ligands, receptors, and cell-enriched transcription factors, NOTCH signaling induces fixed differentiation of progenitor cells, such as differentiation of cardiac progenitor cells into endocardial cells and hepatoblasts into bile duct lineage cells152,153. Furthermore, NOTCH signaling is vital to maintaining the homeostasis of the body in normal regeneration and damage repair. NOTCH signaling can rapidly regulate the dynamic transformation of cells to maintain physiological homeostasis, such as stem cells and tail cells in angiogenesis, through lateral inhibition154–157. It also induces the differentiation and transformation of mature cells to promote damage repair, for example, in liver regeneration158. Last, numerous ligands and receptors are involved in NOTCH signaling and have specified temporal and spatial expression in various organs and tissues, although the consequences are similar.
Fig. 3.
The role of NOTCH signaling in body development and damage repair. NOTCH signaling is involved in regulating the differentiation and function of stem cells, affecting organ production and damage repair. a NOTCH signaling promotes the self-renewal of stem cells, induces multipotent progenitors for lineage selection, and generates different terminal cells; when the organ is damaged, cell type A is damaged and destroyed, and the stimulated cell type B rapidly upregulates the expression of NOTCH signaling to promote their own proliferation, and is partially redifferentiated into cell type A. b Highly activated NOTCH induces the expression of bile duct cell-enriched transcription factors and promotes the differentiation of multipotent hepatocyte progenitors into bile duct epithelial cells. c In liver injury, BEC are damaged and destroyed. NOTCH signaling is highly expressed in hepatocytes, which are further transformed into biphenotypic cells, which manifests the biliary tract morphology, and finally generate new BEC (BEC’) to form small tubular structures. HPC, hematopoietic progenitor cell; BEC, bile duct epithelial cell; SOX9, SRY-related high-mobility group box 9; HNF, hepatocyte nuclear factor
NOTCH and somitogenesis
The somitogenesis of vertebrates occurs in a strict order and is regulated by the segmentation clock. It is closely related to the expression of oscillating genes regulated by NOTCH, Wnt and FGF signaling159–162. NOTCH signaling triggers an excitatory signal, causing presomitic mesoderm (PSM) to transition into a self-sustaining cyclic oscillation state163,164. The gene oscillation period is consistent with the half-life of HES7165 and induces lunatic fringe (Lfng) transcription. LFNG, as a glycosyl transferase that can modify the extracellular domain of NOTCH after translation and periodically blocks the cleavage of NOTCH receptors, causes the formation of cyclic NICD166–168. PSM is a group of self-sustaining oscillating cells, but the synchronous oscillation between depends on the transmission of NOTCH signaling169–171. LFNG inhibits the activation of NOTCH signaling in neighboring cells by regulating the function of DLL1164,172,173. In Lfng-knockout mice, PMS oscillation fails to synchronize, but PMS oscillation amplitude and period remain unaffected170. This finding further demonstrates that LFNG is a key coupling factor for synchronous oscillations between cells.
NOTCH and skeleton
In the growth and development of MPC, NOTCH signaling regulates and inhibits the production of osteoblasts151, chondrocytes174–178, and osteoclasts179,180 through different ligands and receptors (NOTCH1, NOTCH2, JAG1, DLL1) as well as the downstream target gene (SRY-related high-mobility group box 9, SOX9). In addition, the latest research shows that inhibiting glucose metabolism can guide NOTCH to regulate MPC150, proving the complex role of NOTCH signaling in the skeletal microenvironment. In the mouse model, the absence of NOTCH signaling leads to depletion of MPC and nonunion of fractures181, consistent with the finding that activated JAG1-NOTCH signaling reduces MPC senescence and cell cycle arrest. Interestingly, using γ-secretase inhibitors intermittently and temporarily for fractures significantly promotes cartilage and bone callus formation, as well as superior strength182. This indicates that NOTCH signaling exerts its function in a temporally and spatially dependent manner.
NOTCH and cardiomyogenesis
During heart wall formation, NOTCH signaling regulates the ratio of cardiomyocytes to noncardiomyocytes by inhibiting myogenesis, further promoting atrioventricular canal remodeling and maturation, EMT development and heart valve formation183–185. In the endocardium layer, the DLL4-NOTCH1-mediated Hey1/2-Bmp2-Tbx2 signaling axis is a complex negative feedback regulation loop, where overexpressed Tbx2 can in turn inhibit upstream Hey expression186–189. In embryos lacking key NOTCH signaling molecules such as Notch1, Rbpj, Hey1/Heyl, or Hey2, EMT development is hindered, and endocardial cells are activated but fail to scatter and invade heart glia190. NOTCH signaling affects the expression of the cadherin 5190 and the TGF-β family member bone morphogenetic protein 2 (BMP2)186,189. In addition, by downregulating VEGFR2, a key negative regulator of EMT within atrioventricular canals (AVCs), NOTCH signaling further induces EMT. Studies have found that active NOTCH1 is most highly expressed in endocardial cells at the base of the trabecular membrane. Bone morphogenetic protein 10 (BMP10)191 and Neuregulin 1 (NRG1)192 are key molecules of NOTCH signaling that regulate the proliferation, differentiation, and correct folding of cardiomyocytes during trabecular development.
NOTCH and the vasculature
NOTCH4 and DLL4 are specifically expressed on vascular endothelial cells (ECs)184,193. Deficiencies in NOTCH signaling result in serious defects in the vasculature of the embryo and yolk sac during embryonic development194 as well as abnormal development of multiple organs, such as the retinal vasculature195,196 and uterine blood vessels197 in rats. At the cellular level, the vascular system mainly includes ECs, pericytes and vascular smooth muscle cells (VSMCs). Under stressors such as hypoxia, resting ECs quickly transform into a state of active growth and high plasticity and then dynamically transform between tip cells (TCs) and stalk cells (SCs) through lateral inhibition rather than direct lineage changes154,155. This cascade reaction between DLL4-mediated NOTCH signaling and VEGFA-VEGFR2 signaling induces ECs near dominant TCs to maintain a high level of NOTCH signaling, inhibiting their differentiation into TCs198,199. NOTCH signaling activates the Wnt pathway through feedback regulation to maintain the connection between ECs, promoting vascular stability200. In addition, DLL4-NOTCH can maintain arterial blood–retinal barrier homeostasis by inhibiting transcytosis201. NOTCH signaling is also important for the development of VSMCs202,203. Blocking Notch signaling in neural crest cells, especially NOTCH2 and NOTCH3, results in vascular dysplasia, aortic defects, and even bleeding202,204–206. The regulation of the downstream transcription factors PAX1, SCX, and SOX9 by NOTCH signaling is vital for regulating the differentiation of progenitor cells in the sclera toward VSMCs207.
NOTCH signaling acts decisively in the arteriovenous differentiation of endothelial cells208,209. NOTCH signaling induces the expression of the arterial marker ephrin B2 and inhibits that of the venous marker EphB4, thereby regulating the number and diameter of arteriovenous vessels210,211. In mice with dysfunctional mutations of NOTCH signaling molecules such as Notch1, Dll4, Hey1, or Hey2, the arterial subregion is defective, while venous differentiation is hyperactive, leading to unexpected bleeding210,212,213. Before blood perfusion, active NOTCH signaling on the arterial side can be detected. High levels of VEGF, ERK/MAP kinase and Wnt pathway components increase DLL4 expression214,215, and the transcription factors Fox1C and Fox2C promote DLL4 activation216. Interestingly, ECs can sense and respond to laminar flow through NOTCH1, similar to the shear stress response, transforming the hemodynamic mechanical force into an intracellular signal, which is necessary for vascular balance217,218.
NOTCH and the hemopoietic system
NOTCH signaling is important in the differentiation, development, and function of hematopoietic system cells, both lymphocytes and myeloid cells. In early embryonic development, the hematopoietic endothelium forms hematopoietic stem cells through NOTCH-dependent endothelial-to-hematopoietic transition219. NOTCH signaling is fundamental in maintaining the number and stemness of hematopoietic stem cells220. In lymphocyte development, the absence of NOTCH1 or CSL in early hematopoietic progenitor cells (HPCs) leads to thymic T cell development retardation and B cell accumulation, with HES1 being the key mediator221. Naïve thymocytes highly express NOTCH and immediately downregulate NOTCH1 expression once they successfully pass β-selection. Some scholars propose that NOTCH-mediated T cell development is initiated in the prethymic niche222,223. For example, bone mesenchymal cells outside the thymus can cross-link with HPCs through NOTCH ligands on the surface to promote the generation of T cell lineages224,225. Shreya S et al. induced the production of HSPC-derived CD7+ progenitor T cells with DLL4 and VCAM-1 in vitro engineering, and these cells further differentiated into mature T cells after thymus transplantation226. Regarding B cells, the development of splenic marginal zone B (MZB) cells depends on DLL1-NOTCH2 signaling227,228. In addition, it was found that active NOTCH2 signaling can mediate the lineage conversion of follicular B cells into MZB cells so that mature B cell subpopulations can quickly and dynamically transform based on the needs of the immune system229,230. The development of innate lymphoid cells (ILCs) was recently found to be NOTCH-dependent231–233, and the response of different subtypes of ILCs to NOTCH signaling is heterogeneous234,235. It is interesting that ILCs can activate MZB cells through DLL1 to enhance antibody production236. Regarding myeloid cells, NOTCH signaling is significant in the development of macrophages237,238, dendritic cells239,240, granulocytes241, etc.
NOTCH and the liver
NOTCH signaling plays a key role in determining the fate of biliary tract cells and directing the correct morphogenesis of the biliary tree. Active NOTCH signaling, especially mediated by NOTCH2 and JAG1, promotes the expression of transcription factors enriched in bile duct cells, induces the differentiation of hepatocytes toward bile duct cells, and promotes the formation of the bile duct plates152,153. The expression of SOX9, a downstream molecule of NOTCH signaling, is synchronized with the asymmetric development of the bile duct152,242, with a mouse model of liver-specific deletion of Sox9 echoing this finding. Interestingly, delayed biliary tract development caused by liver-specific deletion of Sox9 eventually resolves in a spontaneous manner, proving that SOX9 plays a major role in timing regulation through the development of the biliary tract243.
The liver has a strong compensatory regeneration ability, where NOTCH signaling responds quickly with significant upregulation, and the transformation of hepatocytes into bile duct-like cells can be observed (Fig. 3c). Similarly, high levels of dual-phenotype hepatocytes can also be observed in liver slices of patients with early liver diseases. Additionally, in a mouse orthotopic liver transplantation model, a high level of NOTCH1 (NICD and HES1) signaling was found to have a protective effect on hepatocytes during ischemia–reperfusion injury, regulating macrophage immunity244. In incomplete liver injury, NOTCH signaling mediates the proliferation and differentiation of facultative progenitor cells, thereby promoting biliary tract repair. Such damage repair can be induced mainly by NOTCH2245,246, consistent with the discovery of the role of NOTCH2 signaling in the differentiation and selection of liver progenitor cells during liver development.
NOTCH and the gastrointestinal tract
Studies have shown that NOTCH signaling prevents embryonic epithelial cells from differentiating into secretory lineages247, with Hes1 being the main negative regulator248. Highly activated NOTCH signaling promotes the differentiation of intestinal stem cells toward intestinal epithelial cells249. Inhibiting NOTCH signaling increases the differentiation of secretory goblet cells250. Additionally, the lateral inhibition of NOTCH/DLL1 and the synergy of the Wnt signaling pathway250 drive Paneth cell differentiation and subsequent crypt formation251. NOTCH signaling is also essential in the lineage selection of gastric stem cells252 and necessary to maintain the homeostasis of gastric antral stem cells253. Activated NOTCH signaling in differentiated mature gastric epithelial cells induces their dedifferentiation254. NOTCH signaling is also vital to the proliferation of pancreatic progenitor cells and their correct differentiation into mature pancreatic cells255,256. DLL1 and DLL4 are specifically expressed in β cells, while JAG1 is expressed in α cells257. The DLL1-NOTCH-HES1 signaling axis promotes the growth and fate selection of multipotent pancreatic progenitor cells, while JAG1 competes with DLL1 to induce opposite effects258.
NOTCH and the nervous system
NOTCH signaling negatively regulates neurogenic phenotypes259–262. Its absence induces differentiation of neural stem cells toward neurons at the cost of glial cell production, in both D. melanogaster and vertebrates263–266. There are two mainstream models: the classic lateral inhibition model that is similar to vascular development267 and the model involving oscillatory expression of HES1, NEUROG2 and DLL1268. In addition, NOTCH signaling promotes the differentiation of most glial cell subtypes, except for oligodendrocytes. In the peripheral nervous system, the interaction between NOTCH signaling and Hairy2 is vital for the development of neural crest cells, although the specific regulatory mechanism remains unclear269. Active NOTCH signaling blocks the occurrence and stratification of the trigeminal nerve, leading to disorders of brain development. Furthermore, NOTCH signaling drives intestinal neural crest cells to develop into precocious glial cells in Hirschsprung disease270,271. These results indicate that NOTCH signaling participates in neural crest differentiation, but further exploration is required272.
NOTCH and other organs or systems
NOTCH signaling functions throughout lung development and the damage repair process273. Components of NOTCH signaling are highly expressed in various cells and tissues during lung development. Inhibition of NOTCH signaling or RBPJ deficiency causes defects in proximal airway differentiation, club-cell secretion inhibition, and excessive proliferation of ciliated cells and neuroendocrine cells. NOTCH2 is the main factor activating alveolar morphogenesis and maintaining airway epithelial integrity274. NOTCH signaling mediates the balance between the proliferation and differentiation of basal cells275. In damage repair, NOTCH2 in basal cells is activated, promoting the separation of cell lineages and producing secretory cells276.
NOTCH signaling is important in cell lineage selection, epidermal homeostasis and skin function277. NOTCH signaling in the skin promotes cell differentiation278, while NOTCH in hair follicles inhibits cell differentiation, promotes proliferation and maintains stemness. Notch signaling is also closely related to cilia cell proliferation, differentiation and morphogenesis and may be involved in asymmetric cell division in the embryonic epidermis279,280. NOTCH signaling regulates sebaceous gland stem cells directly and indirectly. In Rbpj-deficient mice, the differentiation of sebaceous stem cells is inhibited, and the number of sebaceous glands (SGs) is reduced, with compensatory, enlarged SGs still existing281. Many skin diseases have been found to have NOTCH signaling changes, such as hidradenitis suppurativa, psoriasis, and atopic dermatitis282,283.
Notch signaling in noncancerous diseases
As mentioned above, NOTCH signaling is essential for body development and homeostasis, indicating that NOTCH signaling is vital for the occurrence and development of diseases. Most genetic diseases caused by NOTCH mutations have a low incidence and lack effective treatment. For example, the first discovered related disorder, Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), has no effective treatment other than supportive treatment. The prognosis of only a few patients with AGS can be improved through liver transplantation, suggesting that further research is necessary. Most of the diseases caused by nonmutant NOTCH signaling abnormalities present corresponding developmental characteristics. New and interesting findings have appeared recently. For example, NOTCH signaling may be related to alcohol-associated preference, playing an important role in nonalcoholic fatty liver disease. We will now focus on the manifestations of NOTCH signaling abnormalities in diseases caused by congenital or nongenetic mutations (Table 1).
Table 1.
NOTCH Signaling in Noncancerous diseases
| Disease type | Key NOTCH components | Affected organs/tissue | Main manifestations | Ref. |
|---|---|---|---|---|
| Diseases related to abnormal expression of NOTCH signaling factors caused by gene mutation | ||||
| CADASIL | NOTCH3 | Arterioles of the brain | Particulate osmophilic substances are deposited near VSMCs; arterial damage and brain damage | 285,286,291,636 |
| Alagille syndrome | NOTCH2, JAG1 | Multiple organs and systems | Absence of bile ducts, cholestasis; peripheral arterial stenosis; specific facial features | 28,293,301 |
| Spondylocostal dysostosis | DLL3, MESP2, HES7 | Vertebral column | Malformed ribs, asymmetrical rib cage, short trunk | 306,637 |
| Hajdu-Cheney disease | NOTCH2 | Skeletal tissue | Truncated NOTCH2 proteins escape ubiquitylation and degradation, mediating active NOTCH2 signaling; osteoporosis, craniofacial anomalies | 638–640 |
| Left ventricle cardiomyopathy | MIB1 | Heart | Promotes the engulfment of NOTCH ligands, inhibits NOTCH signal transduction; hinders ventricular myocardium development | 641,642 |
| Adams-Oliver syndrome | NOTCH1, RBPJ, DLL4 | Skin, limbs | Scalp hypoplasia, terminal transverse limb defects | 643,644 |
| Bicuspid aortic valve disease | NOTCH1, RBPJ, JAG1 | Cardiac valves | Related to valvular disorders of EMT and valve calcification | 645–647 |
| Schizophrenia | NOTCH4 | Brain | One of the strongest candidate susceptibility genes for schizophrenia | 648,649 |
| Diseases related to abnormal expression of NOTCH signaling factors caused by factors other than gene mutation | ||||
| Pulmonary arterial hypertension | NOTCH1, NOTCH3 | Pulmonary vasculature | ECs and VSMCs hyperproliferation and activation; vascular remodeling, pulmonary artery obstruction | 331,332,650,651 |
| Nonalcoholic steatohepatitis | NOTCH1, JAG1 | Liver | Abnormal NOTCH signaling activation in liver cells promotes osteopontin expression and secretion | 315,316,318 |
| Osteoarthritis | RBPJ, JAG1, HES1 | Articular cartilage | Abnormally high expression of NOTCH factors in OA; NOTCH signaling plays a dual regulatory role, participating in both damage repair and progression of disease, with temporal and spatial specificity | 320–323 |
| Graft versus host disease | NOTCH1, NOTCH2, JAG1, DLL1, DLL4 | Immune system | Activation and promotion the differentiation and function of T cells; increases the BCR responsiveness of patient B cells | 337,339,340,652 |
| Pancreatitis | NOTCH1, JAG1, HES1 | Pancreas | Associated with tissue regeneration and renewal after pancreatitis; contributes to the differentiation and proliferation of acinar cells | 653–655 |
| Multiple sclerosis | JAG1 | Myelin sheath | Inhibition of oligodendrocyte maturation and differentiation and formation of the myelin sheath | 656–658 |
| Duchenne muscular dystrophy | JAG1 | Skeletal muscle | Associated with the depletion and senescence of MPCs | 659,660 |
| Klippel-Feil syndrome | RIPPLY2 | Vertebra | Regulates the asymmetric development of embryos | 661,662 |
| Alcohol associative preference | NOTCH/Su(H) | Neurons | Affects alcohol-related neuroplasticity in adults | 663 |
CADASIL Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, VSMCs vascular smooth muscle cells, MESP2 mesoderm posterior 2, MIB1 mindbomb homolog 1, RBPJ recombination signal binding protein-J, EMT epithelial–mesenchymal transition, ECs endothelial cells, OA osteoarthritis, BCR B-cell receptor, MPCs multipotent progenitor cells, RIPPLY2 ripply transcriptional repressor 2, Su(H) suppressor of hairless
Diseases associated with abnormal expression of NOTCH signaling related to mutations
CADASIL
CADASIL syndrome, an arteriolar vascular disease mediated by dominant mutations in the NOTCH3 gene, is the most common hereditary cause of stroke and vascular dementia in adults284,285. NOTCH3 is mainly expressed in VSMCs and pericytes, especially arterioles. In a study of 50 unrelated CADASIL patients, 45 with NOTCH3 pathogenic mutations286 presented abnormal folding of NOTCH3 and deposition of osmophilic particles near VSMCs287,288, and cerebral arteries showed reduced lumen diameter unassociated with chronic hypertension289. Notch3-knockout mice show obvious structural abnormalities of arterioles and loss of vascular smooth muscle, simulating some CADASIL vascular changes, but are insufficient to constitute a complete CADASIL pathological model290. Attempts have been made to simulate the main pathological features of CADASIL regarding vascular damage and unique brain damage291, such as introducing Notch3 pathogenic point mutations into large P1-derived artificial chromosomes (PACs) to construct transgenic mouse models with large genome fragments of Nothc3 pathogenic mutations292 and using patient-derived induced pluripotent stem cell modeling. Evidently, NOTCH3 is pathogenic when mutated, although its underlying mechanism remains unclear.
Alagille syndrome
AGS is an autosomal dominant genetic disease caused by abnormal NOTCH signaling, with JAG1 mutations being predominant (greater than 90%) and NOTCH2 mutations being second most common (5%)27,28,293. AGS affects multiple organs throughout the body, inducing, for example, abnormal development of the liver, heart, vasculature, bones, eyes, and maxillofacial dysplasia. Liver damage is the most prominent and is characterized by a lack of interlobular bile ducts and varying degrees of cholestasis, jaundice, and itching. AGS is one of the most important causes of chronic cholestasis in children. Symptoms ameliorate with age, yet there is still no effective treatment other than liver transplantation294,295. These findings are consistent with the roles of JAG1 and NOTCH2 in bile duct development and morphological maintenance mentioned above. Interestingly, according to statistics, JAG1 has more than 430 mutation sites outside of mutation hotspots. Similarly, its phenotype is highly variable, and a correlation between genotype and phenotype has not yet been found296–299. Thus, it remains a mystery how changes in different NOTCH receptors and ligands affect the occurrence and development of AGS. There was no research model with the characteristics of AGS until the structural defect model of the biliary tree using biopsies from AGS patients was developed, and experiments have indicated that AGS liver organoids may be a good human 3D model of AGS300. JAG1 homozygous mutations often lead to embryonic lethality in mice. Andersson et al. successfully constructed mice homozygous for a missense mutation (H268Q) in Jag1 (Jag1Ndr/Ndr), and these mice showed a decreased rate of embryonic lethality and recapitulation of all AGS features. Surviving mice presented with the classic absence of bile ducts and other features of AGS, including defects of the heart, vasculature, and eyes301,302. In the pathological tissues of patients and mouse models, Joshua et al. found that the expression level of SOX9 was negatively correlated with the severity of AGS liver damage, and overexpression of SOX9 could rescue bile duct loss in Jag1+/– mouse models. One explanation is that overexpressed SOX9 can be recruited to the NOTCH2 promoter to upregulate the expression of NOTCH2 in the liver, thereby compensating for the decreased expression of the JAG1 ligand303. These new research models and related experimental data have promoted and informed further research on AGS.
Congenital scoliosis
Sporadic and familial congenital scoliosis (CS) refers to the lateral curvature of at least one spine segment caused by fetal spinal dysplasia. Studies have shown that CS is closely related to genetic factors, environmental factors, developmental abnormalities, and NOTCH signaling304. Several key NOTCH genes involved in the segmentation clock mechanism may explain the features of a genetic model of a rare syndrome characterized mainly by CS-spondylocostal dysostosis (SCD)305,306.
When analyzing genes in the families of SCD patients, multiple mutation sites in DLL3 are found, and the phenotype of pyramidal dysplasia in Dll3-free mice is similar to that of SCD patients307. The genetic correlation between DLL3 mutation and spinal rib dysplasia has been reported308, and DLL3 deletion alone is unable to induce a complete SCD phenotype. In addition, Mesp2 is a downstream gene of NOTCH in somite differentiation, and abnormal expression of its 4 pairs of base repeats are closely related to SCD. Mesp2-knockout mice have spinal chondrodysplasia and serve as the current main research model309,310. In mice, inactivation of Lfng or Hes7 can distort the development of the spine and ribs, with corresponding mutations also found in patients311,312. Furthermore, environmental damage to genetically susceptible mice affects the penetrance and severity of the CS phenotype, especially under hypoxic conditions, providing an explanation for the family phenotypic variation of SCD313.
Diseases associated with abnormal expression of NOTCH signaling not related to mutations
Nonalcoholic steatohepatitis
There is almost no NOTCH activity in hepatocytes of healthy adults, while NOTCH activity is slightly elevated in hepatocytes of people with simple steatosis and highly elevated in the hepatocytes of nonalcoholic steatohepatitis (NASH)/fibrosis patients; NOTCH activity is positively correlated with the severity of the disease. In NASH patients or high-fat diet-induced NASH mouse models, the expression of NOTCH1, NOTCH2, and HES1 is highly elevated, which activates neoadipogenesis and increases liver steatosis314–316. Such abnormal NOTCH activation may mainly be induced by JAG1/NOTCH signaling triggered by intercellular TLR4317. NOTCH-active hepatocytes can upregulate the expression of SPP1 through the downstream transcription factor SOX9, promoting secretion of osteopontin (OPN) by hepatocytes and activating hepatic stellate cells (HSCs) to induce liver fibrosis318.
Osteoarthritis
The expression level of NOTCH signaling components is low in the articular cartilage of healthy adults but higher in osteoarthritis (OA) biopsies319,320. After trauma, NOTCH signaling is abnormally activated in joint tissues, and its continuous activation can cause early and progressive OA-like lesions. However, transient NOTCH signaling activation helps synthesize cartilage matrix and promotes joint repair321. Inhibition of NOTCH signaling was found to significantly reduce the proliferation of OA chondrocytes. However, the specific inhibition of cartilage NOTCH signaling and the decrease in MMP13 abundance in the joint can delay cartilage degeneration322. Eventually, long-term loss of NOTCH signaling will cause cartilage homeostasis imbalance and bone destruction. The findings above suggest that Rbpj and Hes1 play a major mediating role323. In summary, NOTCH signaling presents duality when regulating the physiology and pathology of articular cartilage, and its effects are depending on temporal and spatial factors.
Lung-related diseases
Allergic asthma is mainly driven by the Th2 immune response, where NOTCH signaling activates the expression of the key transcription factor Gata3324,325. Preclinical studies of γ-secretase inhibitor (GSI) have also proven that inhibiting NOTCH signaling reduces the asthma phenotype326,327. NOTCH signaling plays an important role in promoting Th2 cell lymph node regression and lung migration328. NOTCH4 has been further proven to be vital in the occurrence of asthma. Repeated exposure to allergens can induce regulatory T cells (Tregs) to upregulate the expression of NOTCH4, dampening their immunoregulatory function and activating downstream Wnt and Hippo pathways. These factors turn Tregs into Th2 and Th17 cells, maintaining persistent allergic asthma95,329. In addition, upregulation of JAG1 expression is found in lung tissues of patients with interstitial pulmonary fibrosis. In chronic lung injury, repeated injury promotes continuous upregulation of JAG1 by inhibiting CXCR7, leading to the continuous activation of NOTCH in surrounding fibroblasts and inducing profibrotic responses330. NOTCH3 is an important mediator of pulmonary artery remodeling in pulmonary arterial hypertension (PAH) that mediates the excessive proliferation and dedifferentiation of VSMCs329. In addition, the regulation of NOTCH1 in endothelial cells also promotes the progression of PAH331,332. Chronic obstructive pulmonary disease (COPD) is a common lung disease associated with smoking. Studies have shown that smoking and PM2.5 exposure promote the activation of NOTCH signaling, leading to the imbalance of T cell subsets and immune disorders, thus aggravating COPD333–335.
Other diseases
NOTCH signaling is a regulator of the CD4+ T cells that cause graft versus host disease (GVHD)336. Inhibition of NOTCH signaling reduces target organ injury and germinal center formation, significantly reducing the severity and mortality of GVHD337,338. Activated NOTCH signaling can directly activate reactive T cells and promote their function339. The responsiveness of patients’ B cell receptors is also significantly enhanced by activated NOTCH signaling340. NOTCH signaling is also involved in regulating the glomerular filtration barrier. Abnormal activation of NOTCH1 signaling in the glomerular endothelium inhibits the expression of VE-cadherin and induces albuminuria through the transcription factors Snai1 and Erg36. In adult pancreatic β cells, the abnormal activation of NOTCH signaling, especially DLL1 and DLL4, can promote β cell proliferation. A large number of naïve, dysfunctional β-cells, which proliferate but are unable to secrete insulin normally, causes glucose intolerance257,341.
Notch signaling in cancers
NOTCH as an oncogene in cancers
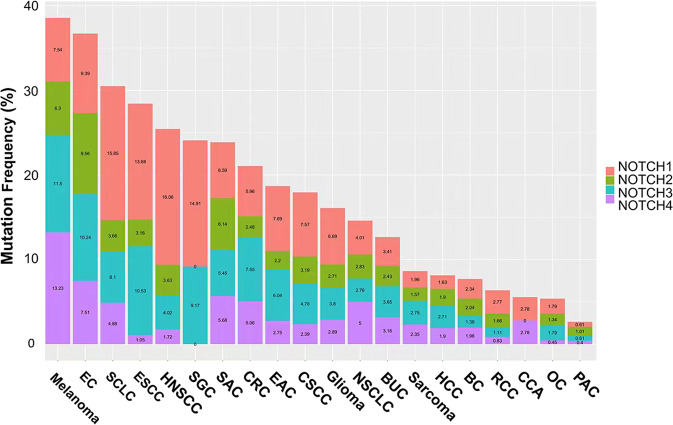
NOTCH was first identified as an oncogene in T-ALL342,343. Subsequently, the alteration of NOTCH receptors was discovered in various cancers (Fig. 4). The activation of NOTCH in breast cancer, lung adenocarcinoma, hepatocellular cancer, ovarian cancer and colorectal cancer was determined to be oncogenic78 (Table 2). The pattern of NOTCH activation varies; for example, NOTCH can be activated by upstream signals or by structural alteration resulting from its internal mutations. Potential mechanisms of tumorigenesis include controlling the tumor-initiating cell phenotype, regulating known upstream or downstream tumor-associated signaling factors, such as MYC or P53, facilitating angiogenesis or tumor invasion, regulating the cell cycle, etc. These mechanisms will now be discussed based on cancer type.
Fig. 4.
Mutation frequencies of NOTCH receptors in different cancers. Data are obtained from cBioPortal (http://cbioportal.org). We included data from two studies: MSK-IMPACT Clinical Sequencing and TCGA PanCancer Atlas Studies, with a total of 21289 patients. And we only used samples with mutation information, including missense, truncating, inframe, splice, and structural variation/fusion. This figure shows the mutation frequency of the four receptors of NOTCH in different cancer types. EC, endometrial carcinoma; SCLC, small-cell lung cancer; ESCC, esophageal squamous cell carcinoma; HNSCC, head, and neck squamous cell carcinoma; SGC, salivary gland cancer; SAC, stomach adenocarcinoma; CRC, colorectal cancer; EAC, esophagogastric adenocarcinoma; CSCC, cervical squamous cell carcinoma; NSCLC, non-small-cell lung cancer; BUC, bladder urothelial carcinoma; HCC, hepatocellular carcinoma; BC, breast cancer; RCC, renal cell carcinoma; CCA, cholangiocarcinoma; OC, ovarian cancer; PAC, prostate adenocarcinoma
Table 2.
NOTCH Signaling in Cancers
| Cancer type | Involved NOTCH components | Relevant evidence | Ref. |
|---|---|---|---|
| NOTCH signaling pathway plays an oncogenic role | |||
| T-cell acute lymphoblastic leukemia | NOTCH1, NOTCH3 |
More than 50% of T-ALL patients have NOTCH1 somatic activating mutations; Transplanted hematopoietic progenitor cells with activation of Notch1 signaling in murine models can develop T-ALL; Activating mutations of NOTCH3 without NOTCH1 has also been found in several T-ALLs. |
344,345,350 |
| Splenic marginal zone lymphoma | NOTCH1, NOTCH2 | Activating mutations of NOTCH signaling appeared in 58% of SMZLs, related to inferior survival. | 351 |
| B-chronic lymphocytic leukemia | NOTCH1-2, JAG1-2 |
Constitutively expression of NOTCH1, NOTCH2 proteins and their ligands JAG1 and JAG2 were detected in B-CLL; Dysfunction of NOTCH signaling reduces the morbidity of B-CLL, while activation of NOTCH signaling increases its survival. |
352,664 |
| Lung adenocarcinoma | NOTCH1, NOTCH3 |
NOTCH1 and NOTCH3 were detected highly expressed, suggesting poor prognosis and intensive invasion; Notch1-3 were confirmed contributing to the initiation and progression of LUAD in vivo and in vitro. |
355,356,358 |
| Breast cancer | NOTCH1, NOTCH4, JAG1 |
Upregulation of non-mutated NOTCH1 and JAG1 is associated with poor prognosis of BC; The mutations of Notch1 and Notch4 mediated by the mouse mammary tumor virus can promote epithelial mammary tumorigenesis; BC cell lines with functionally recurrent rearrangements of NOTCH genes are sensitive to NOTCH inhibitors. |
379,380,382 |
| Colorectal cancer | NOTCH1 |
Upregulation of NOTCH ligands (DLL1, DLL3, DLL4, JAG1 and JAG2) and aberrant activation of NOTCH1 were detected; Active Notch1 signaling induces the proliferation and activation of colon cancer hepatocytes, promoting cell invasion and metastasis. |
365,367 |
| Ovarian cancer | NOTCH1, NOTCH3 |
Ntch1 and Notch3 promote the occurrence and development of ovarian cancer; Overexpression of Notch3 is related to cell hyperproliferation and anti-apoptosis. |
389–393 |
| Adenoid cystic carcinoma | NOTCH1-2 |
Activated mutations of NOTCH1 and NOTCH2 were frequently detected in ACC; NOTCH1 inhibitors have significant antitumor efficacy in both ACC patients and PDX models. |
415–420 |
| Clear cell renal cell carcinoma | NOTCH1 | Overexpression of NOTCH ligands and receptors were observed in CCRCC tissues, and activated NOTCH1 led to dysplastic hyperproliferation of tubular epithelial cells. | 422 |
| Hepatocellular carcinoma* | NOTCH1 |
Approximately 30% of human HCC samples have activated NOTCH signaling, promoting the formation of liver tumors in mice; NOTCH activation facilitates EMT progression and metastasis in HCC; Mutations in the NOTCH target gene HES5 in HCC samples can present both protumorigenic and antitumorigenic functions. |
400,402,404 |
| Glioma* | NOTCH1-2 |
Inhibiting NOTCH signaling with a γ-secretase inhibitor in glioma constrains tumor growth both in vivo and in vitro. NOTCH1 has oncogenic potential in the brain associating other oncogenic hotspots, such as p53 loss. Positive feedback of NOTCH1-SOX2 enhances glioma stem cell invasion along white matter tracts. Inactivation of Rbpj, Notch1 or Notch2 accelerates tumor growth in a mouse model. |
407–410 |
| NOTCH signaling pathway palys a tumor suppressing role | |||
| Squamous cell cancers | NOTCH1-3 |
Inactivated NOTCH1-3 were detected in SCC specimens; The genomic aberrations in NOTCH1 induced by mutagenic agent could cause an increasing tumor burden in SCCs; DNMAML1, an inhibitor to canonical NOTCH transcription, promotes de novo SCC formation. |
438–440,449,451 |
| Neuroendocrine tumors | NOTCH1, DLL3 |
Nearly 25% of human SCLC cases present inactivation of NOTCH target genes; DLL3, an inhibitory NOTCH signaling components, was detected highly expressed in SCLC and lung carcinoid tumors; Gastroenteropancreatic and lung neuroendocrine tumors exhibit decreased NOTCH expression and mutated NOTCH components; Activating NOTCH1 could inhibit the growth of thyroid neuroendocrine cancer cells in vitro. |
425,426,431,432 |
| Pancreatic ductal adenocarcinomaa | NOTCH1 |
Notch1 could inhibit the formation of pancreatic intraepithelial neoplasia in a PDAC mouse model; Notch1 loss is required for progression in a Kras-induced PDAC model. |
454–456 |
T-ALL T-cell acute lymphoblastic leukemia, SMZL splenic marginal zone lymphoma, B-CLL B-cell chronic lymphocytic leukemia, LUAD lung adenocarcinoma, BC breast cancer, ACC adenoid cystic carcinoma, PDX patient-derived xenograft; CCRCC clear cell renal cell carcinoma, HCC hepatocellular carcinoma, EMT epithelial–mesenchymal transition, SCC, squamous cell cancer; SCLC small-cell lung cancer, DANMAML1 Dominant-Negative Mastermind Like1, PDAC pancreatic ductal adenocarcinoma
aNOTCH might act as a tumor suppressor in oncogenic-oriented HCC405 and GBM413, while as an oncogene in tumorsuppressive-oriented PDAC454–456
Hematological malignancies
The oncogenic effects of NOTCH were first identified with the chromosome t (7;9) translocation of the NOTCH1 gene in T-ALL342,343. More than 50% of T-ALL patients have NOTCH1 somatic activating mutations344. Transplanted hematopoietic progenitor cells with constitutive activation of NOTCH1 signaling in murine models can lead to the development of T-ALL345. Mechanistically, NOTCH1 activation in T-ALL might involve the extracellular heterodimerization domain (HD) and/or the C-terminal PEST domain344. Mutations destabilizing the HD of NOTCH1 could facilitate ligand-independent pathway activation. Furthermore, mutations disrupting the intracellular PEST domain could increase the half-life of NICD1. Many studies suggest that NOTCH1 may induce the expression of MYC by regulating its enhancer N-Me and play a key role in the initiation and maintenance of T-ALL346. The interaction of NOTCH1 and PTEN promotes anabolic pathways in T-ALL347. In addition to these synergistic effects, NOTCH1 can directly regulate the expression of specific lncRNAs, such as LUNAR1, which is essential for the malignant proliferation of T-ALL cells348. Additionally, NOTCH signaling regulates the progression of the T-ALL cell cycle via the expression of the G(1) phase proteins cyclin D3, CDK4, and CDK6349. In recent years, activating mutations of NOTCH3 independent of NOTCH1 mutations have also been found in several cases350, providing novel insights into NOTCH mutations in T-ALL.
In addition, activating mutations in NOTCH have been identified in other hematological malignancies. Approximately 58% of splenic marginal zone lymphoma cases have activating NOTCH mutations, termed NNK-SMZLs, and such cases are related to inferior survival351. In a B cell chronic lymphocytic leukemia (B-CLL) murine model, dysfunction of NOTCH signaling reduces morbidity, while activation of NOTCH signaling increases the survival and apoptosis resistance of B-CLL cells352. In diffuse large B-cell lymphoma (DLBCL), NOTCH also participates in the tumor growth through the FBXW7-NOTCH-CCL2/CSF1 axis353. Although NOTCH plays an oncogenic role in most hematological malignancies, it inhibits the growth and survival of acute myeloid leukemia (AML), and consistent activation of NOTCH1-4 leads to AML growth arrest and caspase-dependent apoptosis354.
Lung adenocarcinoma
In lung adenocarcinoma (LUAD) patients, high expression of NOTCH1 and NOTCH3 has been detected355,356. This alteration involves loss of NUMB expression, which increases NOTCH activity, and gain-of-function mutations of the NOTCH1 gene357. In vivo and in vitro studies confirmed that NOTCH1-3 contributes to the initiation and progression of LUAD358–360, indicating that NOTCH acts as an oncogene in LUAD. The tumorigenesis effect might involve activating mutations of downstream genes regulating the tumor-initiating cell phenotype. First, NOTCH3 is a key driver gene in KRAS-mediated LUAD that activates PKCι-ELF3-NOTCH3 signaling to regulate asymmetric cell division in tumor initiation and maintenance processes361. Second, coactivation of NOTCH1 and MYC increases the frequency of NICD1-induced adenoma formation and enables tumor progression and metastases in a mouse model360. In addition, NOTCH1 activation in KRAS-induced LUAD suppresses p53-mediated apoptosis358. However, NOTCH mutations have opposite effects in LUAD and squamous cell carcinoma (SCC) according to recent studies362. Since most studies of NOTCH are conducted in undistinguished non-small-cell lung cancer (NSCLC) patients, the specific effect of NOTCH in LUAD needs further research.
Colorectal cancer
Physiologically, NOTCH signaling is essential for the development and homeostasis of normal intestinal epithelia; for example, NOTCH signaling regulates the differentiation of colonic goblet cells and stem cells363,364. In human colorectal cancer (CRC) tissues, significant upregulation of NOTCH ligands (DLL1, DLL3, DLL4, JAG1, and JAG2) and aberrant activation of the NOTCH receptor (NOTCH1) are found365,366. Such abnormal NOTCH activation is associated with poorer prognosis and metastasis of CRC367. Inhibiting NOTCH by miR-34a and Numb suppresses the proliferation and differentiation of colon cancer stem cells368, indicating that NOTCH activation is a trigger of colon cancer development. Abnormal NOTCH signaling promotes the invasion and metastasis of CRC cells, possibly through the NOTCH-DAB1-ABL-TRIO pathway, EMT and TGF-β-dependent neutrophil effects369. On the one hand, NOTCH promotes CRC invasion by inducing ABL tyrosine kinase activation and phosphorylation of the RHOGEF protein TRIO370. On the other hand, active NOTCH signaling promotes the occurrence of metastasis by reshaping the tumor microenvironment and regulating EMT-associated transcription factors such as SLUG and SNAIL367,371,372. In conclusion, the NOTCH pathway induces EMT in colon cancer with TP53 deletion370,373,374.
Breast cancer
Studies of NOTCH signaling in epithelial tumors were first performed in breast cancer375–378. Upregulation of non-mutated NOTCH signaling-related proteins, such as NOTCH1 and JAG1, is associated with poor prognosis in breast cancer379. In mouse models, mutations in Notch1 and Notch4 mediated by mouse mammary tumor viruses can promote epithelial mammary tumorigenesis380,381. Moreover, functionally recurrent rearrangements of NOTCH gene families are found in breast cancer, of which cell lines are sensitive to NOTCH inhibitors382. In HER2-expressing breast cancer cells, NOTCH activation seems to be associated with cytotoxic chemotherapy resistance383. Such an abnormal increase in NOTCH signaling expression is believed to be related to a lack of NUMB expression384, and its promoting effect on breast cancer tumorigenesis might be exerted from multiple aspects. First, NOTCH signaling maintains the stemness of breast cancer cells and promotes initiation385,386. Second, NOTCH signaling shapes elements of the breast cancer microenvironment, especially tumor-associated macrophages (TAMs), which is related to the innate immune phenotype387. In addition, NOTCH can be activated by the ASPH-Notch axis, providing materials for the synthesis/release of prometastatic exosomes in breast cancer388.
Ovarian cancer
In ovarian cancer, approximately 23% of patients have NOTCH signaling alterations389. NOTCH1 and NOTCH3 have been discovered to directly promote the occurrence and development of ovarian cancer389–392. Overexpression of NOTCH3 is related to cell hyperproliferation and apoptosis inhibition, as well as tumor metastasis and recurrence393,394. As NOTCH3 is positively correlated with JAG1 and JAG2 expression in ovarian cancer, the carcinogenic function of NOTCH3 is potentially mediated by JAG1-NOTCH3 activation395, and dynamin-dependent endocytosis is required. Notch2/Notch3 and other NOTCH signaling molecules have achieved certain effects by inhibiting Jag1 in a mouse ovarian cancer model396,397. In addition, through methylation of the VEGFR2 promoter, NOTCH signaling facilitates angiogenesis in ovarian cancer mediated by VEGFR2 negative feedback398.
Hepatocellular carcinoma
NOTCH signaling is a pathogenic factor in NASH, yet its role in hepatocellular carcinoma (HCC) is less well defined399. Approximately 30% of human HCC samples have activated NOTCH signaling, which in mice promotes the formation of liver tumors400. Recently, NOTCH activation was found in some HCC subtypes with unique molecular and clinicopathologic features and was found to be associated with poor prognosis399. NOTCH activation is also related to the activation of insulin-like growth factor 2, which contributes to hepatocarcinogenesis401. Furthermore, NOTCH activation facilitates EMT progression and metastasis in HCC402. On the other hand, NOTCH activation slows HCC growth and can predict HCC patient prognosis403. Mutations in the NOTCH target gene HES5 in HCC samples can present both protumorigenic and antitumorigenic functions404. A close relationship between the function of NOTCH1 and the P53 mutation state has been reported, in which NOTCH1 activation increases the invasiveness of P53 WT HCC cells while decreasing that of P53-mutated HCC cells405. Although showing contradictory functions in HCC, NOTCH is still mainly considered an oncogenic factor.
Glioma
NOTCH signaling used to be considered oncogenic in glioma, in which it maintains brain cancer stem cells406. Knockdown of NOTCH ligands in human brain microvascular endothelial cells (hBMECs) or inhibition of NOTCH signaling with a γ-secretase inhibitor in glioma constrains tumor growth both in vitro and in vivo407,408. Notch1 has potentially oncogenic effects in the brain in association with other oncogenic hits, such as p53 loss in a medulloblastoma mouse model409. Positive feedback of NOTCH1-SOX2 enhances glioma stem cell invasion along white matter tracts410. NOTCH also induces the expression of lncRNA and TUG1 to maintain the stemness of glioma stem cells and suppress differentiation411. Moreover, NOTCH1 signaling promotes the invasion and growth of glioma-initiating cells by modulating the CXCL12/CXCR4 chemokine system412. However, NOTCH suppresses forebrain tumor subtypes. Inactivation of Rbpj, Notch1, or Notch2 receptors accelerates tumor growth in a mouse model413. Such a subtype-specific effect of NOTCH in glioma might be related to cooperation with P53. Overall, NOTCH signaling acts either as an oncogenic factor or a tumor suppressor in different glioma subtypes, and the mechanisms need further exploration414.
Other cancers
Adenoid cystic carcinoma (ACC), commonly found in the salivary gland, frequently features activating NOTCH1 and NOTCH2 mutations415–418. NOTCH1 inhibitors have significant antitumor efficacy in both ACC patients and patient-derived xenograft (PDX) models419,420. Upregulation of MYB signaling through NOTCH mutation and amplification might also be a potential driving mechanism of ACC421. Activated NOTCH1 also produces CD133(+) ACC cells, regarded as cancer stem-like cells in ACC. In clear cell renal cell carcinoma (CCRCC), the overexpression of NOTCH ligands and receptors is observed in tumor tissues. Activated NOTCH1 leads to dysplastic hyperproliferation of tubular epithelial cells, and treatment involving a γ-secretase inhibitor leads to CCRCC cell inhibition both in vitro and in vivo422.
NOTCH as a tumor suppressor in cancers
NOTCH may be involved in many cancers as a protumor effector, but it can also act as a tumor suppressor in others, such as squamous cell carcinoma (SCC) and neuroendocrine tumors423 (Fig. 4, Table 2). Antitumor mechanisms include regulating transcription factors with malignant effects, activating downstream suppressive genes, inhibiting the cell cycle, etc. In light of studies regarding its antitumor effects, the traditional opinion of NOTCH as an oncogene has been challenged414.
Neuroendocrine tumors
NOTCH is now believed to act as a suppressor in neuroendocrine tumors (NETs), including tumors derived from the thyroid, neuroendocrine cells of the gut, the pancreas, and the respiratory system424. Small-cell lung cancer (SCLC) is the most common type of pulmonary NET, with nearly 25% of human SCLC cases presenting inactivation of NOTCH target genes in one comprehensive genomic profiling analysis425. A recent study used a multiomics approach to analyze the dynamic changes during transdifferentiation from NSCLC to SCLC426, which is a special feature of acquired resistance to EGFR-TKIs in LUAD. This study found that the downregulation of NOTCH signaling was essential for the initial cell state switch of LUAD cells426, indicating that NOTCH plays a tumor-suppressive role in SCLC. Furthermore, high DLL3 expression is frequently detected in SCLC and lung carcinoid tumors55,426–428, which downregulates NOTCH signaling via cis-inhibition. In an SCLC mouse model, activation of Notch1 or Notch2 reduces the expression of synaptophysin and Ascl1, inhibiting the cell cycle process429,430. Likewise, in human medullary thyroid cancer (MTC) tumor samples, NOTCH1 protein is undetectable, while the expression of NICD1 inhibits MTC cell proliferation431. In an analysis of gastroenteropancreatic NET tumor specimens, reduced NOTCH expression and mutated components were found432,433. Mechanistically, some studies consider that such an antitumorigenesis effect might be mediated by the NOTCH-ASCL1-RB-P53 tumor suppression pathway434,435, while others hold that activated NOTCH could inhibit cell growth via cell cycle arrest associated with upregulated P21431,436. NOTCH could also mark and initiate deprogramming in rare pulmonary NET cells that serve as stem cells in SCLC437. Considering the suppressor effect of NOTCH in NETs, drugs targeting DLL3 have been tested in SCLC, with promising results witnessed in preclinical trials (discussed in detail in the following sections).
Squamous cell cancers
In SCC specimens, inactivated NOTCH1-3 has been detected438–440. 40% of head and neck squamous cell cancer (HNSCC) cases are found to have inactivated NOTCH1441,442. In cutaneous squamous cell cancer (cSCC) and its adjacent normal tissue, NOTCH receptors are also frequently found mutated, resulting in loss of function or downregulation443. Similarly, malfunction of NOTCH1 and NOTCH2 was found in lung squamous cell carcinoma (LUSC) patients444. This negative relation between NOTCH and carcinogenesis was also found in bladder445, esophageal446,447, and cervical SCC448. In an SCC mouse model, genomic aberrations in NOTCH1 induced by mutagenic agents result in an increased tumor burden449,450. Dominant-negative Mastermind-like 1 (DNMAML1), an inhibitor of canonical NOTCH transcription, promotes de novo SCC formation451. Moreover, a study of γ-secretase inhibitors in Alzheimer’s disease (AD) patients showed that inhibiting S3 cleavage in NOTCH might increase the risk of nonmelanoma skin cancer452. Most studies of the mutated form of NOTCH in SCCs show that NOTCH function relies deeply on context; for example, NOTCH function can be affected by factors such as the P53 pathway and the intrinsic transcription-repressive protein RBP-Jκ440. The detailed regulatory mechanism is unclear, although some studies believe that NOTCH signaling maintains the CD133 phenotype in stem cells of SCCs453. Furthermore, decreased NOTCH1 expression also dysregulates cell cycle-associated genes in SCCs such as LUSC362.
Pancreatic ductal carcinoma
NOTCH mutation is common in PDAC454. NOTCH1 can inhibit the formation of pancreatic intraepithelial neoplasia (PanIN) in a PDAC mouse model455. Additionally, Notch1 loss is required progression in a Kras-induced PDAC mouse model456, suggesting its role as a tumor suppressor gene. However, previous studies suggest that NOTCH plays an oncogenic role in the occurrence and development of PDAC457–459. NOTCH signaling has been found to be activated in PDAC, which causes the growth of premalignant PDAC cells457.
NOTCH signaling in the tumor microenvironment
The tumor microenvironment (TME) refers to the factors surrounding tumor cells during their generation and development, including various immune cells, fibroblasts, extracellular matrix (ECM) components, and vasculature460,461. NOTCH signaling is deeply involved in regulating the diversified components of the TME462 (Fig. 5).
Fig. 5.
NOTCH signaling pathway in antitumor immunity. NOTCH signaling plays important roles in both tumor-suppressive and tumor-promoting immune cells. NOTCH signaling promotes the differentiation of many immune cells. DLL and JAG mediate both similar and distinct effects. DC, dendritic cell; CD8T, CD8+ T cell; MDSC, myeloid-derived suppressor cell; CD4T, CD4+ T cell; Th1, type1 T helper cell; Th2, type2 T helper cell; Treg, regulatory T cell; TAM, tumor-associated macrophage; TAN, tumor-associated neutrophil; PD-1, programmed death-1; EOMES, eomesodermin; GZMB, granzyme B; DLL, delta-like ligand; CCL2, C-C motif chemokine ligand 2
NOTCH signaling in immune cells
Generally, immune cells in the TME can be classified into two clusters, inflammatory (tumor-suppressive) immune cells and immune-suppressive (tumor-promoting) immune cells463, and NOTCH signaling plays important roles in both cell types. NOTCH signaling not only determines the differentiation of immune cells but also regulates their functional states.
Dendritic cells
In a mouse model with CD11c lineage-specific deletion of Dll1, CD8+ T cells are decreased, while regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs) are increased, leading to faster tumor growth464. Administration of a DLL1 analog can reverse Dll1 deficiency-induced immunosuppression464. However, mice with CD11c lineage-specific deletion of JAG2 do not show this phenotype, and administration of a JAG1-competitive antagonist reduces Tregs, improving antitumor immunity464. In the colitis-associated colorectal cancer (CRC) model, Notch2 deficiency in the CD11c lineage impairs dendritic cell (DC) differentiation, reduces DC migration, and suppresses antigen-presenting capacity465, mirroring those conditions found in a pioneering study in nontumoral conditions240. In conclusion, both NOTCH ligands (DLL1) and receptors (NOTCH2) play positive roles in DC function, while JAG2 on DCs plays negative roles. As NOTCH signaling is crucial for DC differentiation and maturation, two research groups developed a method to increase the yield of cDC1s from mouse and human hematopoietic progenitor cells by employing DLL1-expressing stroma466,467, which might be applicable for autologous DC-based vaccination468.
CD8+ T cells
First, the DLL1-NOTCH1/2 axis is necessary for naïve CD8+ T cells to differentiate into effector T cells because it regulates the expression of the transcription factor eomesodermin (EOMES) and effector molecules (granzyme B and perforin)469–472. Selective activation of DLL1/4-NOTCH inhibits tumor growth473. In addition, NOTCH signaling is involved in the TCR-mediated self-amplification of T cells (section “The noncanonical NOTCH signaling pathway”). The activated TCR/CD3 complex can directly promote the cleavage of NOTCH receptors on endosomes, initiating the response of CD8+ T cells independent of NOTCH ligands87. As adenosine A2A receptor (A2AR) stimulation decreases TCR-mediated NOTCH activity474, inhibiting A2AR might help boost the CD8+ T cell response41. Second, NOTCH signaling is essential for the persistence and function of human lung tissue-resident memory T cells (TRM cells)475, thus assisting long tumor control476–478. Third, NOTCH signaling is also reported to have a negative impact on CD8+ T cells. NOTCH signaling upregulates the PD-1 expression of CD8+ T cells, thus promoting their exhaustion479. Inhibition of the NOTCH signaling pathway decreases the PD-1 level of CD8+ T cells and promotes the cytotoxicity of tumor-infiltrating CD8+ T cells in CRC patients480. Collectively, NOTCH receptors on CD8+ T cells play positive roles in antitumor immunity, paving the way for displaying NOTCH receptors on T cells for autologous T cell transfer therapy. One challenge in current chimeric antigen receptor-T (CAR-T) cell therapy is the exhaustion of transferred CAR-T cells. In light of this challenge, researchers designed new CAR-T cells with a synthetic NOTCH (synNOTCH) receptor loaded on the cell membrane481,482. These synNOTCH CAR-T cells not only promote the immune response but also maintain a higher fraction of effector T cells in the memory state481,482, which suggests the utility of such a strategy for next-generation CAR-T cell engineering483,484.
CD4+ T cells, B cells, and NK cells
Different ligand-mediated NOTCH signaling pathways also induce further differentiation and functions of CD4+ T cells485. DLL-mediated NOTCH signaling promotes type1 T helper cell (Th1) differentiation, while JAG1/2-mediated NOTCH signaling induces the differentiation of Th2 and Tregs485–487. Blocking NOTCH signaling with a GSI deeply impaired the generation and immunosuppressive function of Tregs488. However, Charbonnier et al. found that deletion of NOTCH components enhanced the immune-suppressive functions of Tregs, while transgenic overexpression of the NOTCH1 intracellular domain impaired Treg fitness489. As NOTCH signaling plays diversified roles in the generation and function of Tregs, distinguishing different signal-sending cells, ligands and receptors might be of much significance. DLL1-NOTCH2 signaling also mediates the development of splenic MZB cells. NK cells isolated from cancer patients show lower expression levels of NOTCH receptors than those of healthy donors490.
Tumor-associated macrophages
First, NOTCH signaling is necessary for the terminal differentiation of tumor-associated marcrophages (TAMs)491. The deletion of CSL in monocyte lineages abrogates TAM differentiation and functions491. A recent study found that inhibition of NOTCH signaling indeed impeded the differentiation of monocyte-derived TAMs while increasing the differentiation of Kupffer cell-like TAMs (kclTAMs) by upregulating Wnt/β-catenin signaling492. Second, NOTCH signaling participates in the recruitment of TAMs in basal-like breast cancer (BLBC)387. JAG1-NOTCH1/2/3 signaling in BLBC cells promotes the secretion of IL-1β and CCL2, recruiting TAMs into the TME. Simultaneously, the TAMs secrete transforming growth factor-β (TGF-β) to induce JAG1 expression in BLBC cells via the TGFβR1-SMAD2/3 pathway. This paracrine loop contributes to the suppressive immune microenvironment of BLBC and also indicates therapeutic opportunities. Third, NOTCH signaling regulates the polarization of TAMs between M1-like (tumor-suppressive) and M2-like (tumor-promoting) phenotypes. JAG1-NOTCH signaling between endocrine-resistant breast cancer cells and TAMs results in the differentiation of TAMs toward an M2-like phenotype, contributing to resistance to endocrine therapy493. NOTCH signaling mediates M2 polarization of TAMs in diffuse large B cell lymphoma (DLBCL) through the CREBBP/EP300-FBXW7-NOTCH-CCL2/CSF1 pathway353. However, NOTCH signaling is also reported to promote the M1 polarization of macrophages in anti-infection immunity494,495 and anticancer immunity496,497. In terms of transplanted tumors, macrophages with insufficient NOTCH signaling exhibit M2 phenotypes, while macrophages with forced activation of NOTCH signaling show M1 phenotypes and promote tumor shrinkage496,497.
Myeloid-derived suppressor cells
Similar to its role in TAMs, NOTCH signaling also participates in the differentiation498–500, chemotaxis501, and function of MDSCs. Regarding functional regulation, tumor-derived factors upregulate JAG1/2 on MDSCs through NFkB-p65 signaling, forming a suppressive immune microenvironment502. Anti-JAG1/2 antibodies decrease the accumulation and tolerogenic activity of MDSCs and inhibit the expression of the immunosuppressive factors arginase I and iNOS, thus restoring defective antitumor immunity502. In addition to its immune-regulatory functions, NOTCH signaling also participates in the MDSC-mediated regulation of tumor cell behaviors. Bone marrow-derived CD11b+JAG2+ cells infiltrate primary colorectal tumors and initiate the EMT program of tumor cells, thus promoting tumor metastasis503. Polymorphonuclear-MDSCs (PMN-MDSCs) interact with circulating tumor cells (CTCs) through NOTCH signaling, enhancing CTC dissemination and metastatic potency504. MDSCs activate NOTCH signaling in tumor cells to endow them with stem cell-like qualities in breast cancer505,506. In summary, NOTCH signaling mainly promotes the immune-suppressive and tumor-promoting functions of MDSCs; thus, targeting JAG1/2 might be a promising strategy.
Tumor-associated neutrophils
Jackstadt et al. reported that NOTCH1 signaling in CRC cells could promote the secretion of CXCL5 and TGF-β, recruiting tumor-associated neutrophils (TANs) to drive metastasis367. Additionally, JAG2-expressing TANs impair the cytotoxicity of CD8+ T cells via NOTCH signaling507.
NOTCH signaling in cancer-associated fibroblasts and the extracellular matrix
On the one hand, NOTCH signaling participates in the differentiation of cancer-associated fibroblasts (CAFs). In keratinocyte tumors, loss of NOTCH signaling promotes CAF differentiation and further tumor initiation508–510. However, in colon and prostate cancer, CAF differentiation is initiated by elevated NOTCH signaling511,512. In addition, CAFs activate NOTCH signaling in cancer cells to promote various malignant behaviors, including the cancer stem cell phenotype513–515, chemotherapy resistance516, metastasis517,518, and disease recurrence519. ECM components, such as fibulin-1520, fibulin-3521, microfibril-associated glycoprotein 2 (MAGP2)522, and laminin α5 (LAMA5)523, can also regulate the intensity of NOTCH signaling in cancer cells. Furthermore, activated NOTCH signaling in PDAC cells is reported to reshape the ECM through exosomes, thus promoting lung metastasis524.
NOTCH signaling in the tumor vasculature
The balance of DLL4 and JAG1 endothelial expression is important for tumor vasculature generation. When DLL4 is inhibited, small blood vessel branches sprout, tumor vascular density increases, vascular function remains poor, overall tumor perfusion decreases, and tumor growth is inhibited. Such effects on the tumor vasculature thus could be employed for antitumor therapy525,526. After binding to NOTCH receptors, JAG1 promotes angiogenesis by competing with DLL4. In breast cancer, JAG1 has been confirmed to induce tumor angiogenesis and tumor growth527,528. Additionally, NOTCH activation in ECs promotes lung metastasis, while endothelial NOTCH1 activation in the liver reduces intercellular adhesion molecule-1 expression and endothelial tumor cell adhesion and retention, thereby reducing liver metastasis528,529. During radiotherapy, endothelial NOTCH1 activation protects tumor vessels from radiotherapy-induced damage and regulates endothelial-mesenchymal transition530. Surprisingly, NOTCH3 acts as a receptor-dependent receptor in the endothelium to induce endothelial cell apoptosis and can be blocked by JAG1526. Furthermore, NOTCH blockade in VSMC-DA suppresses the contractile phenotype and promotes the secretory phenotype of VSMC-DA cells, thereby enhancing tumor cell invasion and proliferation526.
Notch-targeted therapies
As a classical and fundamental signaling pathway in humans, NOTCH is crucial for the development and homeostasis of most tissues. Deregulated NOTCH signaling leads to various diseases, as presented above. For decades, NOTCH-targeting therapeutic strategies have been searched, with many drugs being studied in the preclinical stage or tested in clinical trials. NOTCH signaling has been investigated as a therapeutic target for the treatment of cancer, most recently in the fields of immunity and inflammatory disorders. In the following chapter, research on ongoing or completed NOTCH-targeted therapeutics will be presented according to the employed mechanism (Table 3).
Table 3.
Drugs targeting the NOTCH signaling pathway assessed in clinical trials
| Type | Drugs | NCT/Ref. | Year | Phase | Status | Cancer type and patients | Results |
|---|---|---|---|---|---|---|---|
| GSI | PF-03084014 | NCT00878189560 | 2009 | I | Completed | Solid malignancies, N = 64 |
ORR: 13%; 1 CR observed in patients with advanced thyroid cancer, and 5 PRs in patients with desmoid tumors; All-grade AEs: 84.4%, grade ≥ 3 AEs: 35.9%. |
| NCT00878189665 | 2009 | I | Completed | T-ALL and T-LBL, N = 8 | 1 CR in a T-ALL patient with NOTCH1 mutation. | ||
| NCT02299635 | 2015 | II | Terminated | TNBC, N = 19 |
SAEs: 6/19; study terminated prematurely based on project reprioritization by the sponsor. |
||
| NCT01981551571 | 2013 | II | Active | Desmoid tumors (aggressive fibromatosis), N = 17 | 5 (29%) patients experienced a PR for more than 2 years with tolerable toxicity. | ||
| NCT04195399 | 2020 | II | Recruiting | Progressive, surgically unresectable desmoid tumors, N = 35 | - | ||
| RO4929097 | NCT00532090561 | 2007 | I | Completed | Platinum-resistant ovarian cancer, N = 110 |
1 PR in patients with colorectal adenocarcinoma with neuroendocrine features; 1 nearly complete FDG-PET response in a patient with melanoma. |
|
| NCT01119599562 | 2010 | 0/I | Completed | Glioma, N = 21 |
No dose-limiting toxicities were observed in combination with temozolomide; decreased expression of NICD in tumor cells and blood vessels. |
||
| NCT01175343569 | 2010 | II | Completed | Platinum-resistant ovarian cancer, N = 45 | No objective responses were observed. | ||
| NCT01122901666 | 2010 | II | Completed | GBM, N = 47 | Inactive in recurrent GBM patients. | ||
| NCT01120275568 | 2016 | II | Completed | Metastatic melanoma, n = 32 | Tolerated but did not achieve NOTCH target inhibition. | ||
| NCT01116687570 | 2010 | II | Completed | Metastatic colorectal cancer, N = 37 | No radiographic responses were seen, and time to progression was short. | ||
| MK-0752 | NCT00100152 | 2005 | I | Terminated | T-ALL, N = 50 |
1/6 patients showed 45% reduction in mediastinal mass; study was halted for severe diarrhea. |
|
| NCT00106145667 | 2005 | I | Completed | Solid tumors, N = 103 |
1 objective response and 10 cases of SD were observed in patients with high-grade gliomas; weekly dosing was generally well tolerated. |
||
| NCT00572182566 | 2008 | I | Terminated | Brain and central nervous system tumors, N = 33 |
No objective responses were reported in 23 pediatric patients; study terminated by sponsor. |
||
| NCT00645333668 | 2008 | I/II | Completed | Breast cancer, N = 30 | Enhanced the efficacy of docetaxel with manageable toxicity. | ||
| NCT00756717 | 2008 | IV | Completed | Breast cancer, N = 20 |
No serious adverse events; No available efficacy data.. |
||
| LY3039478 | NCT01695005565,669,670 | 2012 | I | Completed | Solid cancers, N = 237 |
Prednisone might reduce gastrointestinal toxicities; PR was observed in 1 patient with breast cancer, 1 patient with leiomyosarcoma and 1 patient with angiosarcoma. |
|
| NCT02518113671 | 2015 | I | Completed | T- ALL/T-LBL, N = 36 |
6 patients (16.7%) experienced DLTs; 1 patient (2.8%) had a confirmed response that lasted 10.51 months. |
||
| NCT02784795672 | 2016 | Ib | Completed | Solid cancer, N = 94 | Combination with other anticancer agents produced disappointing results. | ||
| LY900009 | NCT01158404564 | 2010 | I | Completed | Solid cancer, N = 35 |
No objective response; 5/35 patients had a SD. |
|
| AL101 | NCT04461600 | 2020 | II | recruiting | NOTCH-activated TNBC, N = 67 | - | |
| NCT04973683 | 2021 | I | recruiting | NOTCH-activated ACC, N = 12 | - | ||
| DLL3 | Rovalpituzumab tesirine (Rova-T) | NCT01901653673 | 2013 | I | Completed | SCLC, N = 74 |
11 (18%) patients had an objective response, ten of whom had high DLL3 expression; 28 (38%) suffered serious drug-related adverse events. |
| NCT02819999579 | 2016 | I | Terminated | SCLC, N = 26 | There was no clear efficacy benefit of combining Rova-T with platinum-based chemotherapy. | ||
| NCT03026166589 | 2017 | I/II | Terminated | SCLC, N = 42 |
ORR was 30% in patients treated with combination therapy with Rova-T and ICIs; however, the toxicity was high, suggesting that the combination was not well tolerated; enrollment was stopped because of the DLT. |
||
| NCT02674568586 | 2016 | II | Completed | SCLC, N = 339 |
Median OS was 5.6 months; grade 3-5 AEs were seen in 213 (63%) patients; Demonstrated modest clinical activity in 3L+ SCLC, with associated toxicities. |
||
| NCT03033511587 | 2017 | III | Terminated | SCLC, N = 748 |
Lack of survival benefit of maintenance therapy with rovalpituzumab tesirine after first-line platinum-based chemotherapy; the study did not meet its primary end point and was terminated early. |
||
| NCT03061812588 | 2017 | III | Completed | SCLC, N = 444 | Compared with topotecan, Rova-T exhibited an inferior OS and higher rates of serosal effusions, photosensitivity reactions, and peripheral edema. | ||
| SC-002 | NCT02500914591 | 2015 | I | Terminated | SCLC, N = 35 |
5 (14%) patients achieved a PR; 37% of patients had serious AEs considered to be related to SC-002; no further development is planned because of the systemic toxicity and limited efficacy. |
|
| AM757 | NCT03319940 | 2017 | I | Recruiting | SCLC, N = 332 | - | |
| HPN328 | NCT04471727 | 2020 | I | Recruiting | SCLC, N = 67 | - | |
| DLL4 | Enoticumab (REGN421) | NCT00187159594 | 2015 | I | Completed | Solid tumors, N = 53 |
2 PRs were observed in patients with NSCLC and ovarian cancer; MTD was not reached. |
| Demcizumab (OMP-21M18) | NCT00744563595 | 2014 | I | Completed | Solid tumors, N = 55 | Demonstrated antitumor activity with a low dose. | |
| NCT01189968674 | 2010 | I | Completed | Metastatic nonsquamous NSCLC, N = 40 |
Modulated the expression of genes regulating NOTCH signaling and angiogenesis; increased the risk of cardiovascular disease when combined with pemetrexed and carboplatin. |
||
| NCT01952249596 | 2013 | Ib/II | Phase Ib, completed; phase II, terminated | Platinum-resistant ovarian, primary peritoneal, and fallopian tube cancer, N = 19 |
Researchers are no longer pursuing ovarian cancer as an indication; the phase II portion of the study was terminated. |
||
| NOTCH1 | Brontictuzumab (OMP-52M51) | NCT01778439420 | 2013 | I | Completed | Selected refractory solid tumors, N = 48 |
2 patients achieved PR and 4 patients achieved ≥ 6 months of SD in ACC with NOTCH1 activation; DLTs included diarrhea and fatigue. |
| NOTCH2/3 | Tarextumab (OMP-59R5) | NCT01277146616 | 2011 | I | Completed | Solid tumors, N = 42 |
9 subjects had SD; Lower doses were tolerated. |
| NCT01647828615 | 2012 | II | Completed | Untreated metastatic pancreatic cancer, N = 177 | There were no OS, PFS, or ORR benefits with the addition of tarextumab to nab-paclitaxel and gemcitabine in first-line metastatic PDAC. | ||
| NCT01859741 | 2019 | I/II | Terminated | SCLC, N = 172 | Terminated for unimproved PFS in combination with etoposide and platinum therapy. | ||
| NOTCH3 | PF-06650808 | NCT02129205617 | 2014 | I | Terminated | Breast cancer and other advanced solid tumors, N = 40 |
5 PRs were observed with manageable safety; all of responders had positive NOTCH3 expression; the study was terminated due to a change in sponsor prioritization. |
T-ALL T cell acute lymphoblastic leukemia, T-LBL T cell lymphoblastic lymphoma, TNBC triple-negative breast cancer, SCLC small-cell lung cancer, NSCLC non-small-cell lung cancer, PDAC pancreatic ductal adenocarcinoma, GBM glioblastoma, ORR objective response rate, CR complete response, PR partial response, SD stable disease, PFS progression-free survival, OS overall survival, AE adverse event, SAE serious adverse event, ACC adenoid cystic carcinoma, FDG-PET [18F]-2-fluoro-2-deoxy-D-glucose-positron emission tomography, DLT dose-limiting toxicity, NICD NOTCH intracellular domain, 3L+ more than 3 lines of therapy, MTD maximum tolerated dose
Cleavage inhibitors
S1 cleavage
Precursors of NOTCH receptors require S1 cleavage in the Golgi before integration with their ligands. Sarcoendoplasmic reticulum Ca2+-ATPase (SERCA) is an important accessory factor in this process that modulates ATP-dependent calcium pumps531. Malfunction of SERCAs impairs NOTCH signaling, especially that of mutant NOTCH1532. Mutant NOTCH1 protein acts as an oncogene in T-ALL as well as other malignant tumors533, making SERCAs potential therapeutic targets534. Thapsigargin, a guaianolide compound of plant origin that inhibits SERCAs in mammalian cells, has been tested in breast cancer and leukemia at the preclinical stage535–537. CPA534, CAD204520538 and other small molecular inhibitors of SERCA with lower off-target toxicity have been investigated in the laboratory, yet no surprising results have been reported to encourage further clinical trials.
S2 cleavage
S2 cleavage occurs in the ligand–receptor binding domain, mediating ectodomain shedding and regulating the transmission speed of NOTCH signaling539,540. A disintegrin and metalloproteinase domain-containing protein 10 (ADAM10) or ADAM17 (also called tumor necrosis factor-alpha convertase, TACE) can be exploited to prevent S2 cleavage and NOTCH signaling transmission, as they are key enzymes of S2 cleavage62,541–543. Similar to SERCA inhibitors, ADAM inhibitors target the entire NOTCH pathway. Small molecule drugs targeting ADAMs have been studied in non-small-cell lung cancer544, hepatocellular carcinoma545, renal carcinoma546, breast cancer547, and systemic sclerosis548. Some of these inhibitors have shown anti-NOTCH activities in vitro and in animal experiments, yet no clinical trial has been initiated.
S3 cleavage
The canonical signal transmission of NOTCH signaling from outisde the cell to inside the cell relies heavily on S3 cleavage mediated by the γ-secretase complex549,550, suggesting that it is promising to modulate the function of γ-secretase for treatment.
γ-Secretase inhibitors
γ-Secretase inhibitors (GSIs) were first tested as a treatment for Alzheimer’s disease (AD) in clinical trials because γ-secretase contributes to catalyzing the production of β-amyloid peptide. Unfortunately, the study was terminated shortly after it began because of serious NOTCH-associated adverse events such as gastrointestinal symptoms, infections, and nonmelanoma skin cancers551. Since then, researchers have attempted to treat cancer with GSIs to disrupt NOTCH signaling. In preclinical studies, GSIs are widely studied as a treatment for cancer, showing antitumor activity in diverse tumor types, such as breast cancer552,553, hepatocellular carcinoma554,555, non-small-cell lung cancer556, colorectal cancer557, prostate cancer558, and gliomas559. Cancer patients were first documented to receive GSI treatment in 2006, with one of six patients with T-ALL or acute myeloid leukemia receiving MK-0752 in a phase I clinical trial; the trial showed a promising 45% reduction in mediastinal mass after 28 days, although the treatment was paused because of severe diarrhea (NCT00100152). Other drugs, including PF-03084014560, RO4929097561,562, BMS-986115563, LY900009564, LY3039478565, and MK-0752566,567, have emerged in phase I trials, all of which have shown antitumor efficacy. However, most have presented dose-limiting toxicities. To date, only RO4929097 and PF-03084014 have entered phase II trials. Unfortunately, although the adverse events (AEs) were well tolerated, only 1 patient among 32 patients with metastatic melanoma treated with RO4929097 achieved a partial response568. Similar outcomes occurred in platinum-resistant epithelial ovarian cancer and colorectal cancer, with no objective response among valid participants569,570; thus, few agents have entered phase III/IV clinical trials. PF-03084014, also called nirogacestat, achieved more promising outcomes in patients with desmoid tumors (aggressive fibromatosis) than RO4929097, as 29% of the 15 patients experienced a confirmed partial response that was maintained for more than 2 years571. A phase III clinical trial for nirogacestat has already been registered, although the trial has yet to begin (NCT03785964).
In addition to cancer, because NOTCH plays a critical role in the differentiation of Th cells, GSIs have also been studied in allergic diseases such as asthma572. NOTCH signaling regulates Th1 and Th2 responses in allergic pulmonary inflammation, indicating its promising targetability in immune disease.
γ-Secretase modulators
γ-Secretase modulators (GSMs) were originally studied in AD573. As a superior option to GSIs, GSMs aim to modify the catalytic activity of γ-secretase rather than to nonselectively inhibit it, enabling partial NOTCH signaling function to be maintained and thus theoretically ameliorating adverse events574. The selective inhibitor MRK-560 targeting PSEN1, an important catalytic subclass of γ-secretase complexes, has been proven to effectively decrease mutant NOTCH1 processing and cause cell cycle arrest in T-ALL without associated gut toxicity575. GSMs are only applied in AD as drugs that are designed to modulate amyloid-β (Aβ) peptide generation without impacting the function of NOTCH576,577.
Antibody-drug conjugates
Given the severe adverse events of inhibiting the overall NOTCH pathway, antibodies targeting different receptors and ligands have been explored to achieve precise targeting of NOTCH signaling578,579. There are five ligands and four receptors in the NOTCH signaling pathway21. Although the roles of each component are not completely clear, functions related to specific diseases have been confirmed, making them potential targets41.
Antibodies against ligands
JAG1
As reported previously, the upregulated expression of JAG1 enhances proliferation and angiogenesis in various malignant tumors, including adrenocortical carcinoma580, breast cancer379, and prostate cancer581. These pathological mechanisms make JAG1 a promising target, and monoclonal antibodies against JAG1 have been studied in breast cancer582, ovarian cancer396, and other malignant tumors582. 15D11, one of the most promising fully human monoclonal antibodies against JAG1, has been studied at the preclinical stage; 15D11 increases chemotherapy sensitivity, reduces neoplastic growth in bone metastases, and, most importantly, causes minor adverse effects583.
DLL3
DLL3 is an inhibitory ligand of NOTCH signaling that is highly upregulated and aberrantly expressed on the cell surface of small-cell lung cancer (SCLC) and other high-grade neuroendocrine tumors as a key driving gene55,584,585. DLL3-directed antibody-drug conjugates (ADCs) induce durable and safe responses in SCLC and large-cell neuroendocrine cancer (LCNEC) PDX tumor models427. Positive results inspired further clinical trials. In 2017, Charles M Rudin et al. first reported their encouraging results of rovalpituzumab tesirine (Rova-T); 11 of 60 assessable patients with SCLC or LCNEC had confirmed objective responses, and the objective response rate (ORR) was relatively higher in patients with high DLL3 expression. Although 38% of 74 patients suffered severe drug-related AEs, the AEs could be controlled579. Unfortunately, further phase II and III studies failed to achieve their efficacy end points. Relapsed/refractory SCLC patients receiving Rova-T after at least two lines of therapy achieved a median overall survival (mOS) time of only 5.6 months, and the ORR was 12.4%586. A study of Rova-T as a maintenance therapy after first-line platinum-based chemotherapy was terminated shortly after it began due to a lack of survival benefit587. Compared with concurrent standard second-line chemotherapy, Rova-T showed shorter OS and lower safety588. Attempts to combine chemotherapy and immune checkpoint inhibitors also failed, with extra toxicities and moderate efficacy579,589. Although the abovementioned studies failed to meet their expected end points, complete responses appeared in nearly every study, indicating that this therapeutic strategy has good prospects. However, strategies to stratify patients and appropriate biomarkers should be explored. Researchers have also attempted to explore further indications and novel drugs related to DLL3-targeting antibodies. IDH-mutant gliomas show selective and homogeneous expression of DLL3, and researchers found that patient-derived IDH-mutant glioma tumorspheres were sensitive to Rova-T in vitro590. Another DLL3 ADC, SC-002, presented an ORR of 14% and a severe AE rate of 37% in a phase I clinical trial in SCLC591. Furthermore, some novel drugs targeting DLL3 are in trials actively recruiting patients, such as AM757 (a bispecific antibody targeting DLL3 and CD3, NCT04702737) and HPN328 (a trispecific antibody, NCT04471727).
DLL4
DLL4 is an important regulator of tumor angiogenesis and cancer stem cells and is activated in a wide range of human cancers592. The combination of specific DLL4 blockade and ionizing radiation impairs tumor growth by promoting nonfunctional tumor angiogenesis and extensive tumor necrosis593. When combined with VEGF blockade, REGN421, a monoclonal antibody targeting DLL4, presented antitumor effects in ovarian cancer525. A phase I clinical trial of REGN421, also called enoticumab, was conducted in patients with advanced solid tumors. Of the 32 treated patients in whom toxicity was tolerable, 2 patients had partial response, and 16 patients had stable disease594. Demcizumab, another anti-DLL4 antibody, showed antitumor activity at the minimum dose and with shorter exposure in a phase I clinical study of solid tumors but presented a significant risk of cardiac toxicity595. After dose optimization, combining demcizumab with paclitaxel achieved an ORR of 21% in platinum-resistant ovarian cancer patients without dose-limiting toxicity596. Strategies employing dual variable domain immunoglobulin (DVD-Ig) molecules targeting DLL4 and VEGF have been studied, such as ABT-165, which showed superior efficacy and safety in preclinical models597, and navicixizumab (OMP-305B83), which presented modest antitumor potency and toxicity in a phase Ib clinical trial of solid tumors598.
JAG2/DLL1
JAG2, believed to promote cell survival and proliferation, interacts with NOTCH2, the nucleus pulposus (NP)599, and hematopoietic stem and progenitor cells (HSPCs)600. Additionally, high expression of JAG2 facilitates the development of cancers, such as lung adenocarcinoma601 and bladder cancer602. DLL1 is essential for the development and differentiation of B lymphocytes227,603. These two ligands might be promising targets, although drugs targeting these ligands have yet to be reported.
Antibodies against receptors
NOTCH1
Mutant NOTCH1 induces the occurrence of T-ALL and T-ALL cell proliferation344,604. It can also act as an oncogene in colorectal carcinoma605, glioma606 and other malignant tumors607, making it a possible antitumor target. In phase I clinical trials, a monoclonal antibody targeting NOTCH1 called brontictuzumab was tested in patients with solid tumors (NCT03031691 and NCT01778439) and lymphoid malignancies (NCT01703572). A clinical benefit was achieved in 6 of 12 ACC patients with tolerable toxicity420. In addition to tumor activation, NOTCH1 also promotes the immune response depending on Tregs. In preclinical trials, drugs selectively inhibiting NOTCH1 have been shown to strengthen the function of Tregs to suppress the progression of inflammatory arthritis608 and modulate the immune response in transplantation609.
NOTCH2/NOTCH3
Dysregulated NOTCH2 is vital for the development of cancers such as some B cell leukemias610, pancreatic ductal adenocarcinoma (PDAC)611, and malignant melanoma612. Similarly, NOTCH3 acts as a facilitating factor in various tumors, such as lung cancer613, ERBB2-negative breast cancer614, and ovarian cancer391. OMP-59R5 (tarextumab), which blocks both NOTCH2 and NOTCH3, is effective in treating a variety of tumors397 and has been tested as a treatment for PDAC615, SCLC (NCT01859741), and other solid tumors616 in clinical trials. However, OMP-59R5 in combination with chemotherapy did not produce a superior outcome in PDAC or SCLC patients, and neither drug achieved a better objective response in other solid tumors. PF-06650808, a novel anti-NOTCH3 ADC, achieved 5 partial responses among 40 patients with breast cancer or other solid tumors, with a manageable safety profile and positive NOTCH3 expression detected in all responders617.
NOTCH4
The functions of NOTCH4 differ in different types of cancer. The overexpression of NOTCH4 is regarded as a poor prognosis marker in some scenarios618, while in others, it is considered a favorable marker619. There are no mature drugs targeting NOTCH4.
Transcription blockers
Activating the transcription of target genes is the last step of NOTCH signaling. Therapies targeting downstream mediators of NOTCH signaling remain unexplored. NOTCH transcription depends on the NOTCH ternary complex (NTC), which contains the DNA-binding protein CSL (also called CBF-1/RBPJ, Su (H), or Lag-1), NICD and MAML1620,621. RIN1, a small molecule inhibitor of RBPJ, causes proliferation of hematologic cancer cell lines in vitro622. IMR-1, a small molecule inhibitor of MAML1, inhibits the growth of NOTCH-dependent cell lines in vitro623. CB-103, an orally active small molecule altering NTC function, produces loss-of-function NOTCH phenotypes and inhibits the growth of human breast cancer and leukemia xenografts, notably without causing the dose-limiting intestinal toxicity of other NOTCH inhibitors624. Such novel drugs may represent new agents for NOTCH-based diseases.
NOTCH signaling agonists
NOTCH signaling can both accelerate and suppress the development of diseases, which unsurprisingly applies in cancers625,626. That is, enhancing NOTCH signaling can be a targeted therapy strategy. Some chrysin and hesperetin compounds have been used to activate NOTCH signaling in anaplastic thyroid cancer with NOTCH1 deficiency627,628. Inhibitory effects on established tumor cell lines were found, although the underlying mechanism remains unclear. The negative regulatory region (NRR) can autoinhibit the metalloprotease cleavage of NOTCH to enhance its signaling. Some activating antibodies of NOTCH receptors induce conformational changes in the NRR, making it accessible to ADAM metalloproteinases, thus facilitating activation of NOTCH signaling629.
Summary of clinical trials
Several NOTCH-targeted therapies have been evaluated in clinical trials; specifically, these therapies have been tested in cancers41. Among cleavage inhibitors, drugs targeting S1-S2 cleavage are still within preclinical stages. Drugs targeting S3 cleavage (GSIs and GSMs) have made their way into further clinical research; research of GSIs has been restrained due to severe toxicities, though GSMs are being continuously explored. Among the antibodies against ligands, drugs targeting JAG1, DLL3 and DLL4 have shown promising results in preclinical studies. Drugs targeting DLL3 and DLL4 have been studied in early clinical trials, with only those targeting DLL3 performing well. Unfortunately, further studies of agents targeting DLL3 failed to meet expectations. Drugs targeting JAG2/DLL1 have shown great potential, but no drug has reached mature development. Among the antibodies against receptors, the majority have achieved mediocre results. Of the transcription blockers and signal agonists, the blockers have only been studied in the preclinical stage, while agonists remain only theoretical. Of the abovementioned agents, those targeting DLL3 and GSIs are the most popular because they have shown potential.
However, neither of these agents can be applied clinically considering safety and efficacy. On the one hand, most pan-NOTCH inhibitors exhibit dose-limiting gastrointestinal toxicities mediated by hyperplasia of intestinal goblet cells, including diarrhea and vomiting, which often lead to suspension of further investigations253,630. Regarding GSIs, attempts have been made to improve tolerance, such as combining GSIs with glucocorticoids631, using intermittent dosing regimens632, and applying drugs that inhibit disease-specific subunits of the γ-secretase complex633. On the other hand, the majority of ADCs have failed to reach the expected efficacy in cancer studies, although they have performed well in some individuals. Cell heterogeneity might be an explanation for such findings. Taking SCLC as an example, researchers found that a minority of nonneuroendocrine SCLC cells with NOTCH activation could sustain the growth of neuroendocrine SCLC cells without NOTCH activation and exhibit cancer stem cell-like properties634, resulting in primary resistance to anti-DLL3 drugs. Insufficient affinity of ADCs might be another reasonable explanation. Additionally, the complexity of NOTCH signaling and bypass signaling might circumvent NOTCH-targeted therapies. In the future, exploring predictive biomarkers, reducing drug toxicities, and exploiting multitargeted drugs might overcome the challenges of NOTCH-targeted therapies.
Concluding remarks and future perspectives
It has been approximately 110 years since the NOTCH gene was first identified in D. melanogaster. We summarized both classical and cutting-edge findings of NOTCH signaling in this review, illustrating the history, architecture, regulatory mechanism, physiology, and pathology of NOTCH signaling as well as therapeutics targeting NOTCH signaling. We identified certain areas of basic research and clinical applications of NOTCH signaling as worthy of further exploration.
One of the most interesting things regarding NOTCH signaling is the dual role it plays in different conditions, particularly in cancers. First, the functions of NOTCH signaling are different within the same tissues, and this is possibly caused by the utilization of different ligands; for example, DLL4/JAG1 regulates tumor vasculature, and DLL1/JAG2 regulate DC functions. Second, the functions of NOTCH signaling vary in different tissues. For instance, NOTCH acts as an oncogene in some tumors and as a tumor suppressor gene in others. Several mechanisms might explain this phenomenon: (a) Different tissues have different expression patterns of NOTCH signaling components, and thus, the outcomes of NOTCH signaling are tissue-specific; for example, DLL3 has tissue-specific effects in SCLC, and NOTCH1 has tissue-specific effects in T-ALL. (b) NOTCH signaling effects occur over a small range, while the cell morphology and intercellular distance are diverse in different tissues. (c) NOTCH signaling activates the transcription of a series of genes containing both positive and negative regulators of biological events. As these downstream genes are also regulated by other driver genes, such as Myc and P53, the mutational status of these driver genes also affects the outcome of NOTCH signaling. Third, tumors are massive complexes containing different clones of cancer cells and multiple types of noncancerous cells, making the overall effect of NOTCH signaling complicated and unpredictable.
Several strategies can be employed to clarify the mechanisms of NOTCH signaling. First, deciphering the subtle differences between different ligand–receptor interactions is essential. Second, spatially resolved transcriptomic analyses635, which dissect the embedded tissues into very small pieces and acquire their expression profiles, can be used to explore the impact of spatial characteristics on the outcome of NOTCH signaling. Third, comprehensive analysis of NOTCH target genes is needed because there may be more target genes than are currently known81, and epigenetic and transcriptomic analyses might help.
NOTCH-targeted therapy has been studied for decades but has failed to meet expectations. The reasons for these shortcomings might be the cytotoxicity induced by pan-NOTCH inhibitors, the low affinity of current ADCs, and the upregulation of bypass pathways. Novel drugs such as isoform-specific drugs and high-affinity ADCs may be a solution, as they might have increased efficacy and lower cytotoxicity. In addition, protein refolding is an attractive mode of action to employ to restore the functions of inactivated NOTCH signaling. Another strategy is to develop novel treatment strategies, such as DC-pulsed vaccine therapy and synNOTCH CAR-T cell therapy. Complementary combination therapies, such as combination of inhibitors of other pathways, chemotherapy, radiation therapy, and immunotherapy, are also promising. Among these potential combinations, combinations with immunotherapy are expected to be the most useful.
Much work remains to be accomplished for combining NOTCH-targeted therapy with immunotherapy, and the following strategies might help. First, functional studies are needed to comprehensively delineate the consequences of different NOTCH mutations and their effects on the immune microenvironment. NOTCH plays a complex role in tumor immunity, and its overall impact on tumors remains unclear. Second, clinical applications targeting different stages and types of cancer should be considered separately. Canonical NOTCH signaling is widely activated among cells to mediate adjacent intercellular interactions, yet its effects are highly dependent on context and/or cancer type. Third, appropriate ligands and/or receptors should be well chosen because they may have contradictory biological effects. For example, DLL1-NOTCH mainly functions as an immune-activating signal in DCs and CD8+ T cells. However, JAG1/2-NOTCH mainly functions as an immunosuppressive signal, inhibiting DCs and CD8+ T cells while activating many immunosuppressive cells. It is evident that drugs selectively enhancing DLL1-NOTCH signaling while inhibiting JAG1/2-NOTCH signaling can outperform pan-NOTCH-targeting drugs in actual practice. Fourth, conditions triggering the anti-immune or proimmune effects of NOTCH signaling in tumor cells should be considered. It has been acknowledged that NOTCH signaling may be immunosuppressive or tumor suppressive, yet the conditions or triggering factors leading to certain effects remain unknown. Thus, the effect of NOTCH signaling under different microenvironments should be investigated to generate better and more predictable medical applications. Fifth, cytotoxicity should be considered, including the toxicity of the drug itself and the toxicities induced by combination therapies. Sixth, predictive biomarkers should be explored to bolster NOTCH-targeting monotherapy and/or ICI therapy should be combined with NOTCH-targeting monotherapy to achieve maximum efficacy.
In summary, NOTCH factors present complicated and highly changeable functions, suggesting that elaboration of the general mechanism is required. Novel drugs with higher efficacy and lower cytotoxicity are worth investigating, as are new therapeutic strategies. Once a complete understanding of NOTCH signaling is achieved, it can be applied in actual medical practice, fulfilling the long-overdue mission of benefiting patients.
Supplementary information
Supplementary Table1. The role of NOTCH signaling in developmental processes
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 62131009, 82072597, 81874120, and 82073370).
Author contributions
Q.C. conceptualized this review. B.Z. and W.L. primarily searched for the papers and made the outline. B.Z., W.L., and Y.L. drafted the manuscript and drew the figures. Y.Y. edited the language. H.Z. helped with paper searching. Q.C. and K.W. provided helpful suggestions on the structure and content of this review. All authors revised the manuscript. All authors have read and approved the article.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Figures were created with biorender.com.
Footnotes
These authors contributed equally: Binghan Zhou, Wanling Lin, Yaling Long
Supplementary information
The online version contains supplementary material available at 10.1038/s41392-022-00934-y.
References
- 1.Metz CW, Bridges CB. Incompatibility of mutant races in Drosophila. Proc. Natl Acad. Sci. USA. 1917;3:673–678. doi: 10.1073/pnas.3.12.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohr OL. Character changes caused by mutation of an entire region of a chromosome in Drosophila. Genetics. 1919;4:275–282. doi: 10.1093/genetics/4.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bridges CB. Non-disjunction as proof of the chromosome theory of heredity (concluded) Genetics. 1916;1:107–163. doi: 10.1093/genetics/1.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yochem J, Weston K, Greenwald I. The Caenorhabditis elegans lin-12 gene encodes a transmembrane protein with overall similarity to Drosophila Notch. Nature. 1988;335:547–550. doi: 10.1038/335547a0. [DOI] [PubMed] [Google Scholar]
- 5.Austin J, Kimble J. Transcript analysis of glp-1 and lin-12, homologous genes required for cell interactions during development of C. elegans. Cell. 1989;58:565–571. doi: 10.1016/0092-8674(89)90437-6. [DOI] [PubMed] [Google Scholar]
- 6.Coffman C, Harris W, Kintner C. Xotch, the Xenopus homolog of Drosophila notch. Science. 1990;249:1438–1441. doi: 10.1126/science.2402639. [DOI] [PubMed] [Google Scholar]
- 7.Stubbs JD, et al. cDNA cloning of a mouse mammary epithelial cell surface protein reveals the existence of epidermal growth factor-like domains linked to factor VIII-like sequences. Proc. Natl Acad. Sci. USA. 1990;87:8417–8421. doi: 10.1073/pnas.87.21.8417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lodewijk GA, Fernandes DP, Vretzakis I, Savage JE, Jacobs FMJ. Evolution of human brain size-associated NOTCH2NL genes proceeds toward reduced protein levels. Mol. Biol. Evol. 2020;37:2531–2548. doi: 10.1093/molbev/msaa104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Artavanis-Tsakonas S, Muskavitch MA, Yedvobnick B. Molecular cloning of Notch, a locus affecting neurogenesis in Drosophila melanogaster. Proc. Natl Acad. Sci. USA. 1983;80:1977–1981. doi: 10.1073/pnas.80.7.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wharton KA, Johansen KM, Xu T, Artavanis-Tsakonas S. Nucleotide sequence from the neurogenic locus notch implies a gene product that shares homology with proteins containing EGF-like repeats. Cell. 1985;43:567–581. doi: 10.1016/0092-8674(85)90229-6. [DOI] [PubMed] [Google Scholar]
- 11.Kidd S, Kelley MR, Young MW. Sequence of the notch locus of Drosophila melanogaster: relationship of the encoded protein to mammalian clotting and growth factors. Mol. Cell Biol. 1986;6:3094–3108. doi: 10.1128/mcb.6.9.3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johansen KM, Fehon RG, Artavanis-Tsakonas S. The notch gene product is a glycoprotein expressed on the cell surface of both epidermal and neuronal precursor cells during Drosophila development. J. Cell Biol. 1989;109:2427–2440. doi: 10.1083/jcb.109.5.2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rykowski MC, Parmelee SJ, Agard DA, Sedat JW. Precise determination of the molecular limits of a polytene chromosome band: regulatory sequences for the Notch gene are in the interband. Cell. 1988;54:461–472. doi: 10.1016/0092-8674(88)90067-0. [DOI] [PubMed] [Google Scholar]
- 14.Cagan RL, Ready DF. Notch is required for successive cell decisions in the developing Drosophila retina. Genes Dev. 1989;3:1099–1112. doi: 10.1101/gad.3.8.1099. [DOI] [PubMed] [Google Scholar]
- 15.Xu T, Rebay I, Fleming RJ, Scottgale TN, Artavanis-Tsakonas S. The Notch locus and the genetic circuitry involved in early Drosophila neurogenesis. Genes Dev. 1990;4:464–475. doi: 10.1101/gad.4.3.464. [DOI] [PubMed] [Google Scholar]
- 16.Hartley DA, Xu TA, Artavanis-Tsakonas S. The embryonic expression of the Notch locus of Drosophila melanogaster and the implications of point mutations in the extracellular EGF-like domain of the predicted protein. EMBO J. 1987;6:3407–3417. doi: 10.1002/j.1460-2075.1987.tb02664.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Breeden L, Nasmyth K. Similarity between cell-cycle genes of budding yeast and fission yeast and the Notch gene of Drosophila. Nature. 1987;329:651–654. doi: 10.1038/329651a0. [DOI] [PubMed] [Google Scholar]
- 18.Kidd S, Young MW. Transposon-dependent mutant phenotypes at the Notch locus of Drosophila. Nature. 1986;323:89–91. doi: 10.1038/323089a0. [DOI] [PubMed] [Google Scholar]
- 19.Austin J, Kimble J. glp-1 is required in the germ line for regulation of the decision between mitosis and meiosis in C. elegans. Cell. 1987;51:589–599. doi: 10.1016/0092-8674(87)90128-0. [DOI] [PubMed] [Google Scholar]
- 20.Greenwald IS, Sternberg PW, Horvitz HR. The lin-12 locus specifies cell fates in Caenorhabditis elegans. Cell. 1983;34:435–444. doi: 10.1016/0092-8674(83)90377-x. [DOI] [PubMed] [Google Scholar]
- 21.Kopan R, Ilagan MX. The canonical Notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137:216–233. doi: 10.1016/j.cell.2009.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gazave E, et al. Origin and evolution of the notch signalling pathway: an overview from eukaryotic genomes. BMC Evol. Biol. 2009;9:249. doi: 10.1186/1471-2148-9-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Käsbauer T, et al. The Notch signaling pathway in the cnidarian Hydra. Dev. Biol. 2007;303:376–390. doi: 10.1016/j.ydbio.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 24.Artavanis-Tsakonas S, Rand MD, Lake RJ. Notch signaling: cell fate control and signal integration in development. Science. 1999;284:770–776. doi: 10.1126/science.284.5415.770. [DOI] [PubMed] [Google Scholar]
- 25.Fernández R, Gabaldón T. Gene gain and loss across the metazoan tree of life. Nat. Ecol. Evol. 2020;4:524–533. doi: 10.1038/s41559-019-1069-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cary GA, et al. Systematic comparison of sea urchin and sea star developmental gene regulatory networks explains how novelty is incorporated in early development. Nat. Commun. 2020;11:6235. doi: 10.1038/s41467-020-20023-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li L, et al. Alagille syndrome is caused by mutations in human Jagged1, which encodes a ligand for Notch1. Nat. Genet. 1997;16:243–251. doi: 10.1038/ng0797-243. [DOI] [PubMed] [Google Scholar]
- 28.Oda T, et al. Mutations in the human Jagged1 gene are responsible for Alagille syndrome. Nat. Genet. 1997;16:235–242. doi: 10.1038/ng0797-235. [DOI] [PubMed] [Google Scholar]
- 29.Deangelo DJ, et al. A phase I clinical trial of the notch inhibitor MK-0752 in patients with T-cell acute lymphoblastic leukemia/lymphoma (T-ALL) and other leukemias. J. Clin. Oncol. 2006;24:6585–6585. [Google Scholar]
- 30.Andersson ER, Lendahl U. Therapeutic modulation of Notch signalling-are we there yet? Nat. Rev. Drug Discov. 2014;13:357–378. doi: 10.1038/nrd4252. [DOI] [PubMed] [Google Scholar]
- 31.Yang G, et al. Structural basis of Notch recognition by human γ-secretase. Nature. 2019;565:192–197. doi: 10.1038/s41586-018-0813-8. [DOI] [PubMed] [Google Scholar]
- 32.Zhou, R. et al. Recognition of the amyloid precursor protein by human γ-secretase. Science363, eaaw0930 (2019). [DOI] [PubMed]
- 33.Yang G, et al. Structural basis of γ-secretase inhibition and modulation by small molecule drugs. Cell. 2021;184:521–533.e514. doi: 10.1016/j.cell.2020.11.049. [DOI] [PubMed] [Google Scholar]
- 34.Sarin A, Marcel N. The NOTCH1-autophagy interaction: regulating self-eating for survival. Autophagy. 2017;13:446–447. doi: 10.1080/15548627.2016.1268303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Polacheck WJ, et al. A non-canonical Notch complex regulates adherens junctions and vascular barrier function. Nature. 2017;552:258–262. doi: 10.1038/nature24998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li L, et al. Aberrant activation of notch1 signaling in glomerular endothelium induces albuminuria. Circ. Res. 2021;128:602–618. doi: 10.1161/CIRCRESAHA.120.316970. [DOI] [PubMed] [Google Scholar]
- 37.Horita N, et al. Delta-like 1-expressing cells at the gland base promote proliferation of gastric antral stem cells in mouse. Cell Mol. Gastroenterol. Hepatol. 2021;13:275–287. doi: 10.1016/j.jcmgh.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang D, Shain AH. The landscape of driver mutations in cutaneous squamous cell carcinoma. NPJ Genom. Med. 2021;6:61. doi: 10.1038/s41525-021-00226-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dorsam RT, Gutkind JS. G-protein-coupled receptors and cancer. Nat. Rev. Cancer. 2007;7:79–94. doi: 10.1038/nrc2069. [DOI] [PubMed] [Google Scholar]
- 40.Lemmon MA, Schlessinger J. Cell signaling by receptor tyrosine kinases. Cell. 2010;141:1117–1134. doi: 10.1016/j.cell.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Majumder S, et al. Targeting Notch in oncology: the path forward. Nat. Rev. Drug Discov. 2021;20:125–144. doi: 10.1038/s41573-020-00091-3. [DOI] [PubMed] [Google Scholar]
- 42.Siebel C, Lendahl U. Notch signaling in development, tissue homeostasis, and disease. Physiol. Rev. 2017;97:1235–1294. doi: 10.1152/physrev.00005.2017. [DOI] [PubMed] [Google Scholar]
- 43.Kovall RA, Gebelein B, Sprinzak D, Kopan R. The canonical notch signaling pathway: structural and biochemical insights into shape, sugar, and force. Dev. Cell. 2017;41:228–241. doi: 10.1016/j.devcel.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee TV, et al. Negative regulation of notch signaling by xylose. PLoS Genet. 2013;9:e1003547. doi: 10.1371/journal.pgen.1003547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sethi MK, et al. Identification of glycosyltransferase 8 family members as xylosyltransferases acting on O-glucosylated notch epidermal growth factor repeats. J. Biol. Chem. 2010;285:1582–1586. doi: 10.1074/jbc.C109.065409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sethi MK, et al. Molecular cloning of a xylosyltransferase that transfers the second xylose to O-glucosylated epidermal growth factor repeats of notch. J. Biol. Chem. 2012;287:2739–2748. doi: 10.1074/jbc.M111.302406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shi S, Stanley P. Protein O-fucosyltransferase 1 is an essential component of Notch signaling pathways. Proc. Natl Acad. Sci. USA. 2003;100:5234–5239. doi: 10.1073/pnas.0831126100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sasamura T, et al. neurotic, a novel maternal neurogenic gene, encodes an O-fucosyltransferase that is essential for Notch-Delta interactions. Development. 2003;130:4785–4795. doi: 10.1242/dev.00679. [DOI] [PubMed] [Google Scholar]
- 49.Moloney DJ, et al. Fringe is a glycosyltransferase that modifies Notch. Nature. 2000;406:369–375. doi: 10.1038/35019000. [DOI] [PubMed] [Google Scholar]
- 50.Wang Y, et al. Fucosylation deficiency in mice leads to colitis and adenocarcinoma. Gastroenterology. 2017;152:193–205.e10. doi: 10.1053/j.gastro.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Servián-Morilla E, et al. POGLUT1 biallelic mutations cause myopathy with reduced satellite cells, α-dystroglycan hypoglycosylation and a distinctive radiological pattern. Acta Neuropathol. 2020;139:565–582. doi: 10.1007/s00401-019-02117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zeronian, M. R. et al. Notch-Jagged signaling complex defined by an interaction mosaic. Proc Natl Acad Sci USA118, e2102502118 (2021). [DOI] [PMC free article] [PubMed]
- 53.Yuan X, et al. Notch signaling: an emerging therapeutic target for cancer treatment. Cancer Lett. 2015;369:20–27. doi: 10.1016/j.canlet.2015.07.048. [DOI] [PubMed] [Google Scholar]
- 54.Capaccione KM, Pine SR. The Notch signaling pathway as a mediator of tumor survival. Carcinogenesis. 2013;34:1420–1430. doi: 10.1093/carcin/bgt127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Owen DH, et al. DLL3: an emerging target in small cell lung cancer. J. Hematol. Oncol. 2019;12:61. doi: 10.1186/s13045-019-0745-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pitulescu ME, et al. Dll4 and Notch signalling couples sprouting angiogenesis and artery formation. Nat. Cell Biol. 2017;19:915–927. doi: 10.1038/ncb3555. [DOI] [PubMed] [Google Scholar]
- 57.Langridge PD, Struhl G. Epsin-dependent ligand endocytosis activates notch by force. Cell. 2017;171:1383–1396.E12. doi: 10.1016/j.cell.2017.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gordon WR, et al. Structural basis for autoinhibition of Notch. Nat. Struct. Mol. Biol. 2007;14:295–300. doi: 10.1038/nsmb1227. [DOI] [PubMed] [Google Scholar]
- 59.Stephenson NL, Avis JM. Direct observation of proteolytic cleavage at the S2 site upon forced unfolding of the Notch negative regulatory region. Proc. Natl Acad. Sci. USA. 2012;109:E2757–2765. doi: 10.1073/pnas.1205788109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gordon WR, et al. Mechanical allostery: evidence for a force requirement in the proteolytic activation of notch. Dev. Cell. 2015;33:729–736. doi: 10.1016/j.devcel.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Xu X, et al. Insights into autoregulation of Notch3 from structural and functional studies of its negative regulatory region. Structure. 2015;23:1227–1235. doi: 10.1016/j.str.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Seegar TCM, et al. Structural basis for regulated proteolysis by the α-secretase ADAM10. Cell. 2017;171:1638–1648.e1637. doi: 10.1016/j.cell.2017.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lambrecht BN, Vanderkerken M, Hammad H. The emerging role of ADAM metalloproteinases in immunity. Nat. Rev. Immunol. 2018;18:745–758. doi: 10.1038/s41577-018-0068-5. [DOI] [PubMed] [Google Scholar]
- 64.Du H, et al. Macrophage-released ADAMTS1 promotes muscle stem cell activation. Nat. Commun. 2017;8:669. doi: 10.1038/s41467-017-00522-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Groot AJ, Vooijs MA. The role of Adams in Notch signaling. Adv. Exp. Med. Biol. 2012;727:15–36. doi: 10.1007/978-1-4614-0899-4_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li YM, et al. Photoactivated gamma-secretase inhibitors directed to the active site covalently label presenilin 1. Nature. 2000;405:689–694. doi: 10.1038/35015085. [DOI] [PubMed] [Google Scholar]
- 67.Li YM, et al. Presenilin 1 is linked with gamma-secretase activity in the detergent solubilized state. Proc. Natl Acad. Sci. USA. 2000;97:6138–6143. doi: 10.1073/pnas.110126897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kimberly WT, et al. Gamma-secretase is a membrane protein complex comprised of presenilin, nicastrin, Aph-1, and Pen-2. Proc. Natl Acad. Sci. USA. 2003;100:6382–6387. doi: 10.1073/pnas.1037392100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Golde TE, Estus S, Younkin LH, Selkoe DJ, Younkin SG. Processing of the amyloid protein precursor to potentially amyloidogenic derivatives. Science. 1992;255:728–730. doi: 10.1126/science.1738847. [DOI] [PubMed] [Google Scholar]
- 70.Takami M, et al. gamma-Secretase: successive tripeptide and tetrapeptide release from the transmembrane domain of beta-carboxyl terminal fragment. J. Neurosci. 2009;29:13042–13052. doi: 10.1523/JNEUROSCI.2362-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Suzuki N, et al. An increased percentage of long amyloid beta protein secreted by familial amyloid beta protein precursor (beta APP717) mutants. Science. 1994;264:1336–1340. doi: 10.1126/science.8191290. [DOI] [PubMed] [Google Scholar]
- 72.Hardy JA, Higgins GA. Alzheimer’s disease: the amyloid cascade hypothesis. Science. 1992;256:184–185. doi: 10.1126/science.1566067. [DOI] [PubMed] [Google Scholar]
- 73.Deatherage CL, et al. Structural and biochemical differences between the Notch and the amyloid precursor protein transmembrane domains. Sci. Adv. 2017;3:e1602794. doi: 10.1126/sciadv.1602794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Conner SD. Regulation of notch signaling through intracellular transport. Int Rev. Cell Mol. Biol. 2016;323:107–127. doi: 10.1016/bs.ircmb.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 75.Huenniger K, et al. Notch1 signaling is mediated by importins alpha 3, 4, and 7. Cell Mol. Life Sci. 2010;67:3187–3196. doi: 10.1007/s00018-010-0378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bottoni G, et al. CSL controls telomere maintenance and genome stability in human dermal fibroblasts. Nat. Commun. 2019;10:3884. doi: 10.1038/s41467-019-11785-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dreval K, Lake RJ, Fan H-Y. HDAC1 negatively regulates selective mitotic chromatin binding of the Notch effector RBPJ in a KDM5A-dependent manner. Nucleic Acids Res. 2019;47:4521–4538. doi: 10.1093/nar/gkz178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Aster JC, Pear WS, Blacklow SC. The varied roles of notch in cancer. Annu Rev. Pathol. 2017;12:245–275. doi: 10.1146/annurev-pathol-052016-100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bray SJ. Notch signalling in context. Nat. Rev. Mol. Cell Biol. 2016;17:722–735. doi: 10.1038/nrm.2016.94. [DOI] [PubMed] [Google Scholar]
- 80.Lee, C., Sorensen, E. B., Lynch, T. R. & Kimble, J. C. elegans GLP-1/Notch activates transcription in a probability gradient across the germline stem cell pool. Elife5, e18370 (2016). [DOI] [PMC free article] [PubMed]
- 81.Gomez-Lamarca MJ, et al. Activation of the notch signaling pathway in vivo elicits changes in CSL nuclear dynamics. Dev. Cell. 2018;44:611–623.e617. doi: 10.1016/j.devcel.2018.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pillidge, Z. & Bray, S. J. SWI/SNF chromatin remodeling controls Notch-responsive enhancer accessibility. EMBO Rep.20, e46944 (2019). [DOI] [PMC free article] [PubMed]
- 83.Lee C, Shin H, Kimble J. Dynamics of notch-dependent transcriptional bursting in its native context. Dev. Cell. 2019;50:426–435.e4. doi: 10.1016/j.devcel.2019.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Petrovic J, et al. Oncogenic notch promotes long-range regulatory interactions within hyperconnected 3D cliques. Mol. Cell. 2019;73:1174–1190. doi: 10.1016/j.molcel.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pamarthy S, Kulshrestha A, Katara GK, Beaman KD. The curious case of vacuolar ATPase: regulation of signaling pathways. Mol. Cancer. 2018;17:41. doi: 10.1186/s12943-018-0811-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jin, K. et al. NOTCH-induced rerouting of endosomal trafficking disables regulatory T cells in vasculitis. J. Clin. Invest.131, e136042 (2021). [DOI] [PMC free article] [PubMed]
- 87.Steinbuck MP, Arakcheeva K, Winandy S. Novel TCR-mediated mechanisms of notch activation and signaling. J. Immunol. 2018;200:997–1007. doi: 10.4049/jimmunol.1700070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Radtke F, MacDonald HR, Tacchini-Cottier F. Regulation of innate and adaptive immunity by Notch. Nat. Rev. Immunol. 2013;13:427–437. doi: 10.1038/nri3445. [DOI] [PubMed] [Google Scholar]
- 89.Song LL, et al. Notch-1 associates with IKKalpha and regulates IKK activity in cervical cancer cells. Oncogene. 2008;27:5833–5844. doi: 10.1038/onc.2008.190. [DOI] [PubMed] [Google Scholar]
- 90.Yue F, et al. Pten is necessary for the quiescence and maintenance of adult muscle stem cells. Nat. Commun. 2017;8:14328. doi: 10.1038/ncomms14328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen, L.-J. et al. Gm364 coordinates MIB2/DLL3/Notch2 to regulate female fertility through AKT activation. Cell Death Differ (2021). [DOI] [PMC free article] [PubMed]
- 92.Li H, et al. NCSTN promotes hepatocellular carcinoma cell growth and metastasis via β-catenin activation in a Notch1/AKT dependent manner. J. Exp. Clin. Cancer Res. 2020;39:128. doi: 10.1186/s13046-020-01638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mangolini M, et al. Notch2 controls non-autonomous Wnt-signalling in chronic lymphocytic leukaemia. Nat. Commun. 2018;9:3839. doi: 10.1038/s41467-018-06069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rajakulendran N, et al. Wnt and Notch signaling govern self-renewal and differentiation in a subset of human glioblastoma stem cells. Genes Dev. 2019;33:498–510. doi: 10.1101/gad.321968.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hammad H, Lambrecht BN. Wnt and Hippo pathways in regulatory T cells: a NOTCH above in asthma. Nat. Immunol. 2020;21:1313–1314. doi: 10.1038/s41590-020-0797-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Luo, K. Signaling cross talk between TGF-β/Smad and other signaling pathways. Cold Spring Harb. Perspect. Biol.9, a022137 (2017). [DOI] [PMC free article] [PubMed]
- 97.Fernández-Majada V, et al. Nuclear IKK activity leads to dysregulated notch-dependent gene expression in colorectal cancer. Proc. Natl Acad. Sci. USA. 2007;104:276–281. doi: 10.1073/pnas.0606476104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hossain F, et al. Notch signaling regulates mitochondrial metabolism and NF-κB Activity in triple-negative breast cancer cells via IKKα-dependent non-canonical pathways. Front. Oncol. 2018;8:575. doi: 10.3389/fonc.2018.00575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kuramoto T, et al. Dll4-Fc, an inhibitor of Dll4-notch signaling, suppresses liver metastasis of small cell lung cancer cells through the downregulation of the NF-κB activity. Mol. Cancer Ther. 2012;11:2578–2587. doi: 10.1158/1535-7163.MCT-12-0640. [DOI] [PubMed] [Google Scholar]
- 100.Gentle ME, Rose A, Bugeon L, Dallman MJ. Noncanonical Notch signaling modulates cytokine responses of dendritic cells to inflammatory stimuli. J. Immunol. 2012;189:1274–1284. doi: 10.4049/jimmunol.1103102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lin S, et al. Non-canonical NOTCH3 signalling limits tumour angiogenesis. Nat. Commun. 2017;8:16074. doi: 10.1038/ncomms16074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pelullo M, et al. Kras/ADAM17-dependent Jag1-ICD reverse signaling sustains colorectal cancer progression and chemoresistance. Cancer Res. 2019;79:5575–5586. doi: 10.1158/0008-5472.CAN-19-0145. [DOI] [PubMed] [Google Scholar]
- 103.Stahl M, et al. Roles of Pofut1 and O-fucose in mammalian Notch signaling. J. Biol. Chem. 2008;283:13638–13651. doi: 10.1074/jbc.M802027200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yao D, et al. Protein O-fucosyltransferase 1 (Pofut1) regulates lymphoid and myeloid homeostasis through modulation of Notch receptor ligand interactions. Blood. 2011;117:5652–5662. doi: 10.1182/blood-2010-12-326074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wang Y, et al. Uncontrolled angiogenic precursor expansion causes coronary artery anomalies in mice lacking Pofut1. Nat. Commun. 2017;8:578. doi: 10.1038/s41467-017-00654-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jafar-Nejad H, Leonardi J, Fernandez-Valdivia R. Role of glycans and glycosyltransferases in the regulation of Notch signaling. Glycobiology. 2010;20:931–949. doi: 10.1093/glycob/cwq053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Takeuchi H, Haltiwanger RS. Role of glycosylation of Notch in development. Semin. Cell Dev. Biol. 2010;21:638–645. doi: 10.1016/j.semcdb.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Luther KB, Haltiwanger RS. Role of unusual O-glycans in intercellular signaling. Int. J. Biochem. Cell Biol. 2009;41:1011–1024. doi: 10.1016/j.biocel.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Stanley P, Okajima T. Roles of glycosylation in Notch signaling. Curr. Top. Dev. Biol. 2010;92:131–164. doi: 10.1016/S0070-2153(10)92004-8. [DOI] [PubMed] [Google Scholar]
- 110.Acar M, et al. Rumi is a CAP10 domain glycosyltransferase that modifies Notch and is required for Notch signaling. Cell. 2008;132:247–258. doi: 10.1016/j.cell.2007.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fernandez-Valdivia R, et al. Regulation of mammalian Notch signaling and embryonic development by the protein O-glucosyltransferase Rumi. Development. 2011;138:1925–1934. doi: 10.1242/dev.060020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ge C, Stanley P. The O-fucose glycan in the ligand-binding domain of Notch1 regulates embryogenesis and T cell development. Proc. Natl Acad. Sci. USA. 2008;105:1539–1544. doi: 10.1073/pnas.0702846105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rana NA, et al. O-glucose trisaccharide is present at high but variable stoichiometry at multiple sites on mouse Notch1. J. Biol. Chem. 2011;286:31623–31637. doi: 10.1074/jbc.M111.268243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bousseau S, et al. Glycosylation as new pharmacological strategies for diseases associated with excessive angiogenesis. Pharm. Ther. 2018;191:92–122. doi: 10.1016/j.pharmthera.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 115.Yeh C-H, Bellon M, Nicot C. FBXW7: a critical tumor suppressor of human cancers. Mol. Cancer. 2018;17:115. doi: 10.1186/s12943-018-0857-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ye L, et al. NUMB maintains bone mass by promoting degradation of PTEN and GLI1 via ubiquitination in osteoblasts. Bone Res. 2018;6:32. doi: 10.1038/s41413-018-0030-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Guo Y, et al. Numb enriches a castration-resistant prostate cancer cell subpopulation associated with enhanced notch and hedgehog signaling. Clin. Cancer Res. 2017;23:6744–6756. doi: 10.1158/1078-0432.CCR-17-0913. [DOI] [PubMed] [Google Scholar]
- 118.Liu P, Verhaar AP, Peppelenbosch MP. Signaling size: ankyrin and SOCS box-containing ASB E3 ligases in action. Trends Biochem. Sci. 2019;44:64–74. doi: 10.1016/j.tibs.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 119.Giebel B, Wodarz A. Tumor suppressors: control of signaling by endocytosis. Curr. Biol. 2006;16:R91–92. doi: 10.1016/j.cub.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 120.Thompson BJ, et al. Tumor suppressor properties of the ESCRT-II complex component Vps25 in Drosophila. Dev. Cell. 2005;9:711–720. doi: 10.1016/j.devcel.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 121.Troost T, Jaeckel S, Ohlenhard N, Klein T. The tumour suppressor Lethal (2) giant discs is required for the function of the ESCRT-III component Shrub/CHMP4. J. Cell Sci. 2012;125:763–776. doi: 10.1242/jcs.097261. [DOI] [PubMed] [Google Scholar]
- 122.Vaccari T, Bilder D. The Drosophila tumor suppressor vps25 prevents nonautonomous overproliferation by regulating notch trafficking. Dev. Cell. 2005;9:687–698. doi: 10.1016/j.devcel.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 123.Chastagner P, Israël A, Brou C. Itch/AIP4 mediates Deltex degradation through the formation of K29-linked polyubiquitin chains. EMBO Rep. 2006;7:1147–1153. doi: 10.1038/sj.embor.7400822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hori K, Sen A, Kirchhausen T, Artavanis-Tsakonas S. Synergy between the ESCRT-III complex and Deltex defines a ligand-independent Notch signal. J. Cell Biol. 2011;195:1005–1015. doi: 10.1083/jcb.201104146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Shimizu H, et al. Compensatory flux changes within an endocytic trafficking network maintain thermal robustness of Notch signaling. Cell. 2014;157:1160–1174. doi: 10.1016/j.cell.2014.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wang W, Struhl G. Distinct roles for Mind bomb, Neuralized and Epsin in mediating DSL endocytosis and signaling in Drosophila. Development. 2005;132:2883–2894. doi: 10.1242/dev.01860. [DOI] [PubMed] [Google Scholar]
- 127.Overstreet E, Fitch E, Fischer JA. Fat facets and Liquid facets promote Delta endocytosis and Delta signaling in the signaling cells. Development. 2004;131:5355–5366. doi: 10.1242/dev.01434. [DOI] [PubMed] [Google Scholar]
- 128.Daskalaki A, et al. Distinct intracellular motifs of Delta mediate its ubiquitylation and activation by Mindbomb1 and Neuralized. J. Cell Biol. 2011;195:1017–1031. doi: 10.1083/jcb.201105166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Le Borgne R, Remaud S, Hamel S, Schweisguth F. Two distinct E3 ubiquitin ligases have complementary functions in the regulation of delta and serrate signaling in Drosophila. PLoS Biol. 2005;3:e96. doi: 10.1371/journal.pbio.0030096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Fontana JR, Posakony JW. Both inhibition and activation of Notch signaling rely on a conserved Neuralized-binding motif in Bearded proteins and the Notch ligand Delta. Dev. Biol. 2009;333:373–385. doi: 10.1016/j.ydbio.2009.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nandagopal, N., Santat, L. A. & Elowitz, M. B. activation in the Notch signaling pathway. eLife8, e37880 (2019). [DOI] [PMC free article] [PubMed]
- 132.Chapman G, Sparrow DB, Kremmer E, Dunwoodie SL. Notch inhibition by the ligand DELTA-LIKE 3 defines the mechanism of abnormal vertebral segmentation in spondylocostal dysostosis. Hum. Mol. Genet. 2011;20:905–916. doi: 10.1093/hmg/ddq529. [DOI] [PubMed] [Google Scholar]
- 133.Hoyne GF, Chapman G, Sontani Y, Pursglove SE, Dunwoodie SL. A cell autonomous role for the Notch ligand Delta-like 3 in αβ T-cell development. Immunol. Cell Biol. 2011;89:696–705. doi: 10.1038/icb.2010.154. [DOI] [PubMed] [Google Scholar]
- 134.Kohlhaas V, et al. Active Akt signaling triggers CLL toward Richter transformation via overactivation of Notch1. Blood. 2021;137:646–660. doi: 10.1182/blood.2020005734. [DOI] [PubMed] [Google Scholar]
- 135.Li Y, et al. Human NOTCH4 is a key target of RUNX1 in megakaryocytic differentiation. Blood. 2018;131:191–201. doi: 10.1182/blood-2017-04-780379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Liu M, et al. Sirt6 deficiency exacerbates podocyte injury and proteinuria through targeting Notch signaling. Nat. Commun. 2017;8:413. doi: 10.1038/s41467-017-00498-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Malik N, et al. The transcription factor CBFB suppresses breast cancer through orchestrating translation and transcription. Nat. Commun. 2019;10:2071. doi: 10.1038/s41467-019-10102-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Gallo C, et al. The bHLH transcription factor DEC1 promotes thyroid cancer aggressiveness by the interplay with NOTCH1. Cell Death Dis. 2018;9:871. doi: 10.1038/s41419-018-0933-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chen X, et al. MicroRNA-26a and −26b inhibit lens fibrosis and cataract by negatively regulating Jagged-1/Notch signaling pathway. Cell Death Differ. 2017;24:1990. doi: 10.1038/cdd.2017.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Qiao J, et al. MicroRNA-153 improves the neurogenesis of neural stem cells and enhances the cognitive ability of aged mice through the notch signaling pathway. Cell Death Differ. 2020;27:808–825. doi: 10.1038/s41418-019-0388-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Spitschak A, Meier C, Kowtharapu B, Engelmann D, Pützer BM. MiR-182 promotes cancer invasion by linking RET oncogene activated NF-κB to loss of the HES1/Notch1 regulatory circuit. Mol. Cancer. 2017;16:24. doi: 10.1186/s12943-016-0563-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wasson CW, et al. Long non-coding RNA HOTAIR drives EZH2-dependent myofibroblast activation in systemic sclerosis through miRNA 34a-dependent activation of NOTCH. Ann. Rheum. Dis. 2020;79:507–517. doi: 10.1136/annrheumdis-2019-216542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Wang R, et al. iNOS promotes CD24CD133 liver cancer stem cell phenotype through a TACE/ADAM17-dependent Notch signaling pathway. Proc. Natl Acad. Sci. USA. 2018;115:E10127–E10136. doi: 10.1073/pnas.1722100115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Majumdar, U. et al. Nitric oxide prevents aortic valve calcification by S-nitrosylation of USP9X to activate NOTCH signaling. Sci. Adv.7, eabe3706 (2021). [DOI] [PMC free article] [PubMed]
- 145.Morrugares R, et al. Phosphorylation-dependent regulation of the NOTCH1 intracellular domain by dual-specificity tyrosine-regulated kinase 2. Cell Mol. Life Sci. 2020;77:2621–2639. doi: 10.1007/s00018-019-03309-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Suckling RJ, et al. Structural and functional dissection of the interplay between lipid and Notch binding by human Notch ligands. EMBO J. 2017;36:2204–2215. doi: 10.15252/embj.201796632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Baonza A, Garcia-Bellido A. Notch signaling directly controls cell proliferation in the Drosophila wing disc. Proc. Natl Acad. Sci. USA. 2000;97:2609–2614. doi: 10.1073/pnas.040576497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Knust E, Campos-Ortega JA. The molecular genetics of early neurogenesis in Drosophila melanogaster. Bioessays. 1989;11:95–100. doi: 10.1002/bies.950110405. [DOI] [PubMed] [Google Scholar]
- 149.Dray N, et al. Dynamic spatiotemporal coordination of neural stem cell fate decisions occurs through local feedback in the adult vertebrate brain. Cell Stem Cell. 2021;28:1457–1472.e1412. doi: 10.1016/j.stem.2021.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hilton MJ, et al. Notch signaling maintains bone marrow mesenchymal progenitors by suppressing osteoblast differentiation. Nat. Med. 2008;14:306–314. doi: 10.1038/nm1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Dong Y, et al. RBPjkappa-dependent Notch signaling regulates mesenchymal progenitor cell proliferation and differentiation during skeletal development. Development. 2010;137:1461–1471. doi: 10.1242/dev.042911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zong Y, et al. Notch signaling controls liver development by regulating biliary differentiation. Development. 2009;136:1727–1739. doi: 10.1242/dev.029140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Sparks EE, Huppert KA, Brown MA, Washington MK, Huppert SS. Notch signaling regulates formation of the three-dimensional architecture of intrahepatic bile ducts in mice. Hepatology. 2010;51:1391–1400. doi: 10.1002/hep.23431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Alabi RO, Farber G, Blobel CP. Intriguing roles for endothelial ADAM10/Notch signaling in the development of organ-specific vascular beds. Physiol. Rev. 2018;98:2025–2061. doi: 10.1152/physrev.00029.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Herbert SP, Stainier DY. Molecular control of endothelial cell behaviour during blood vessel morphogenesis. Nat. Rev. Mol. Cell Biol. 2011;12:551–564. doi: 10.1038/nrm3176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hellström M, et al. Dll4 signalling through Notch1 regulates formation of tip cells during angiogenesis. Nature. 2007;445:776–780. doi: 10.1038/nature05571. [DOI] [PubMed] [Google Scholar]
- 157.Jakobsson L, et al. Endothelial cells dynamically compete for the tip cell position during angiogenic sprouting. Nat. Cell Biol. 2010;12:943–953. doi: 10.1038/ncb2103. [DOI] [PubMed] [Google Scholar]
- 158.Minnis-Lyons, S. E. et al. Notch-IGF1 signaling during liver regeneration drives biliary epithelial cell expansion and inhibits hepatocyte differentiation. Sci. Signal14, eabe3706 (2021). [DOI] [PubMed]
- 159.Peel AD, Chipman AD, Akam M. Arthropod segmentation: beyond the Drosophila paradigm. Nat. Rev. Genet. 2005;6:905–916. doi: 10.1038/nrg1724. [DOI] [PubMed] [Google Scholar]
- 160.Dequéant ML, et al. A complex oscillating network of signaling genes underlies the mouse segmentation clock. Science. 2006;314:1595–1598. doi: 10.1126/science.1133141. [DOI] [PubMed] [Google Scholar]
- 161.Diaz-Cuadros M, et al. In vitro characterization of the human segmentation clock. Nature. 2020;580:113–118. doi: 10.1038/s41586-019-1885-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Sonnen, K. F. et al. Modulation of phase shift between Wnt and Notch signaling oscillations controls mesoderm segmentation. Cell172, (2018). [DOI] [PMC free article] [PubMed]
- 163.Lewis J. Autoinhibition with transcriptional delay: a simple mechanism for the zebrafish somitogenesis oscillator. Curr. Biol. 2003;13:1398–1408. doi: 10.1016/s0960-9822(03)00534-7. [DOI] [PubMed] [Google Scholar]
- 164.Hubaud A, Regev I, Mahadevan L, Pourquié O. Excitable dynamics and yap-dependent mechanical cues drive the segmentation clock. Cell. 2017;171:668–682.e611. doi: 10.1016/j.cell.2017.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Pourquié O. Vertebrate somitogenesis. Annu. Rev. Cell Dev. Biol. 2001;17:311–350. doi: 10.1146/annurev.cellbio.17.1.311. [DOI] [PubMed] [Google Scholar]
- 166.Bessho Y, Hirata H, Masamizu Y, Kageyama R. Periodic repression by the bHLH factor Hes7 is an essential mechanism for the somite segmentation clock. Genes Dev. 2003;17:1451–1456. doi: 10.1101/gad.1092303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Dale JK, et al. Periodic notch inhibition by lunatic fringe underlies the chick segmentation clock. Nature. 2003;421:275–278. doi: 10.1038/nature01244. [DOI] [PubMed] [Google Scholar]
- 168.Cole SE, Levorse JM, Tilghman SM, Vogt TF. Clock regulatory elements control cyclic expression of Lunatic fringe during somitogenesis. Dev. Cell. 2002;3:75–84. doi: 10.1016/s1534-5807(02)00212-5. [DOI] [PubMed] [Google Scholar]
- 169.Hubaud A, Pourquié O. Signalling dynamics in vertebrate segmentation. Nat. Rev. Mol. Cell Biol. 2014;15:709–721. doi: 10.1038/nrm3891. [DOI] [PubMed] [Google Scholar]
- 170.Yoshioka-Kobayashi K, et al. Coupling delay controls synchronized oscillation in the segmentation clock. Nature. 2020;580:119–123. doi: 10.1038/s41586-019-1882-z. [DOI] [PubMed] [Google Scholar]
- 171.Jiang YJ, et al. Notch signalling and the synchronization of the somite segmentation clock. Nature. 2000;408:475–479. doi: 10.1038/35044091. [DOI] [PubMed] [Google Scholar]
- 172.Zhang N, Gridley T. Defects in somite formation in lunatic fringe-deficient mice. Nature. 1998;394:374–377. doi: 10.1038/28625. [DOI] [PubMed] [Google Scholar]
- 173.Okubo Y, et al. Lfng regulates the synchronized oscillation of the mouse segmentation clock via trans-repression of Notch signalling. Nat. Commun. 2012;3:1141. doi: 10.1038/ncomms2133. [DOI] [PubMed] [Google Scholar]
- 174.Mead TJ, Yutzey KE. Notch pathway regulation of chondrocyte differentiation and proliferation during appendicular and axial skeleton development. Proc. Natl Acad. Sci. USA. 2009;106:14420–14425. doi: 10.1073/pnas.0902306106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Akiyama H, Chaboissier MC, Martin JF, Schedl A, de Crombrugghe B. The transcription factor Sox9 has essential roles in successive steps of the chondrocyte differentiation pathway and is required for expression of Sox5 and Sox6. Genes Dev. 2002;16:2813–2828. doi: 10.1101/gad.1017802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Tsingas M, et al. Sox9 deletion causes severe intervertebral disc degeneration characterized by apoptosis, matrix remodeling, and compartment-specific transcriptomic changes. Matrix Biol. 2020;94:110–133. doi: 10.1016/j.matbio.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Long F, Ornitz DM. Development of the endochondral skeleton. Cold Spring Harb. Perspect. Biol. 2013;5:a008334. doi: 10.1101/cshperspect.a008334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Liu CF, Samsa WE, Zhou G, Lefebvre V. Transcriptional control of chondrocyte specification and differentiation. Semin. Cell Dev. Biol. 2017;62:34–49. doi: 10.1016/j.semcdb.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Luo Z, et al. Notch signaling in osteogenesis, osteoclastogenesis, and angiogenesis. Am. J. Pathol. 2019;189:1495–1500. doi: 10.1016/j.ajpath.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Yu J, Canalis E. Notch and the regulation of osteoclast differentiation and function. Bone. 2020;138:115474. doi: 10.1016/j.bone.2020.115474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Hankenson KD, Gagne K, Shaughnessy M. Extracellular signaling molecules to promote fracture healing and bone regeneration. Adv. Drug Deliv. Rev. 2015;94:3–12. doi: 10.1016/j.addr.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 182.Wang C, et al. Transient gamma-secretase inhibition accelerates and enhances fracture repair likely via Notch signaling modulation. Bone. 2015;73:77–89. doi: 10.1016/j.bone.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.High FA, Epstein JA. The multifaceted role of Notch in cardiac development and disease. Nat. Rev. Genet. 2008;9:49–61. doi: 10.1038/nrg2279. [DOI] [PubMed] [Google Scholar]
- 184.Niessen K, Karsan A. Notch signaling in cardiac development. Circ. Res. 2008;102:1169–1181. doi: 10.1161/CIRCRESAHA.108.174318. [DOI] [PubMed] [Google Scholar]
- 185.Luxán G, D’Amato G, MacGrogan D, de la Pompa JL. Endocardial Notch signaling in cardiac development and disease. Circ. Res. 2016;118:e1–e18. doi: 10.1161/CIRCRESAHA.115.305350. [DOI] [PubMed] [Google Scholar]
- 186.de la Pompa JL, Epstein JA. Coordinating tissue interactions: Notch signaling in cardiac development and disease. Dev. Cell. 2012;22:244–254. doi: 10.1016/j.devcel.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Rutenberg JB, et al. Developmental patterning of the cardiac atrioventricular canal by Notch and Hairy-related transcription factors. Development. 2006;133:4381–4390. doi: 10.1242/dev.02607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Papoutsi, T., Luna-Zurita, L., Prados, B., Zaffran, S. & de la Pompa, J. L. Bmp2 and Notch cooperate to pattern the embryonic endocardium. Development145 (2018). [DOI] [PubMed]
- 189.Luna-Zurita L, et al. Integration of a Notch-dependent mesenchymal gene program and Bmp2-driven cell invasiveness regulates murine cardiac valve formation. J. Clin. Invest. 2010;120:3493–3507. doi: 10.1172/JCI42666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Timmerman LA, et al. Notch promotes epithelial-mesenchymal transition during cardiac development and oncogenic transformation. Genes Dev. 2004;18:99–115. doi: 10.1101/gad.276304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Chen H, et al. BMP10 is essential for maintaining cardiac growth during murine cardiogenesis. Development. 2004;131:2219–2231. doi: 10.1242/dev.01094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Grego-Bessa J, et al. Notch signaling is essential for ventricular chamber development. Dev. Cell. 2007;12:415–429. doi: 10.1016/j.devcel.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Holderfield MT, Hughes CC. Crosstalk between vascular endothelial growth factor, notch, and transforming growth factor-beta in vascular morphogenesis. Circ. Res. 2008;102:637–652. doi: 10.1161/CIRCRESAHA.107.167171. [DOI] [PubMed] [Google Scholar]
- 194.Krebs LT, et al. Notch signaling is essential for vascular morphogenesis in mice. Genes Dev. 2000;14:1343–1352. [PMC free article] [PubMed] [Google Scholar]
- 195.Lobov IB, et al. Delta-like ligand 4 (Dll4) is induced by VEGF as a negative regulator of angiogenic sprouting. Proc. Natl Acad. Sci. USA. 2007;104:3219–3224. doi: 10.1073/pnas.0611206104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Suchting S, et al. The Notch ligand Delta-like 4 negatively regulates endothelial tip cell formation and vessel branching. Proc. Natl Acad. Sci. USA. 2007;104:3225–3230. doi: 10.1073/pnas.0611177104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Moldovan GE, Miele L, Fazleabas AT. Notch signaling in reproduction. Trends Endocrinol. Metab. 2021;32:1044–1057. doi: 10.1016/j.tem.2021.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zarkada G, Heinolainen K, Makinen T, Kubota Y, Alitalo K. VEGFR3 does not sustain retinal angiogenesis without VEGFR2. Proc. Natl Acad. Sci. USA. 2015;112:761–766. doi: 10.1073/pnas.1423278112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Hultgren NW, et al. Slug regulates the Dll4-Notch-VEGFR2 axis to control endothelial cell activation and angiogenesis. Nat. Commun. 2020;11:5400. doi: 10.1038/s41467-020-18633-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Phng LK, et al. Nrarp coordinates endothelial Notch and Wnt signaling to control vessel density in angiogenesis. Dev. Cell. 2009;16:70–82. doi: 10.1016/j.devcel.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Yang JM, et al. Dll4 suppresses transcytosis for arterial blood-retinal barrier homeostasis. Circ. Res. 2020;126:767–783. doi: 10.1161/CIRCRESAHA.119.316476. [DOI] [PubMed] [Google Scholar]
- 202.High FA, et al. An essential role for Notch in neural crest during cardiovascular development and smooth muscle differentiation. J. Clin. Invest. 2007;117:353–363. doi: 10.1172/JCI30070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.High FA, et al. Endothelial expression of the Notch ligand Jagged1 is required for vascular smooth muscle development. Proc. Natl Acad. Sci. USA. 2008;105:1955–1959. doi: 10.1073/pnas.0709663105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Boucher JM, Harrington A, Rostama B, Lindner V, Liaw L. A receptor-specific function for Notch2 in mediating vascular smooth muscle cell growth arrest through cyclin-dependent kinase inhibitor 1B. Circ. Res. 2013;113:975–985. doi: 10.1161/CIRCRESAHA.113.301272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Campos AH, Wang W, Pollman MJ, Gibbons GH. Determinants of Notch-3 receptor expression and signaling in vascular smooth muscle cells: implications in cell-cycle regulation. Circ. Res. 2002;91:999–1006. doi: 10.1161/01.res.0000044944.99984.25. [DOI] [PubMed] [Google Scholar]
- 206.Baeten JT, Lilly B. Differential Regulation of NOTCH2 and NOTCH3 Contribute to Their Unique Functions in Vascular Smooth Muscle Cells. J. Biol. Chem. 2015;290:16226–16237. doi: 10.1074/jbc.M115.655548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Briot A, et al. Repression of Sox9 by Jag1 is continuously required to suppress the default chondrogenic fate of vascular smooth muscle cells. Dev. Cell. 2014;31:707–721. doi: 10.1016/j.devcel.2014.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Hasan SS, et al. Endothelial Notch signalling limits angiogenesis via control of artery formation. Nat. Cell Biol. 2017;19:928–940. doi: 10.1038/ncb3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Luo W, et al. Arterialization requires the timely suppression of cell growth. Nature. 2021;589:437–441. doi: 10.1038/s41586-020-3018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.You LR, et al. Suppression of Notch signalling by the COUP-TFII transcription factor regulates vein identity. Nature. 2005;435:98–104. doi: 10.1038/nature03511. [DOI] [PubMed] [Google Scholar]
- 211.Hainaud P, et al. The role of the vascular endothelial growth factor-Delta-like 4 ligand/Notch4-ephrin B2 cascade in tumor vessel remodeling and endothelial cell functions. Cancer Res. 2006;66:8501–8510. doi: 10.1158/0008-5472.CAN-05-4226. [DOI] [PubMed] [Google Scholar]
- 212.Fischer A, Schumacher N, Maier M, Sendtner M, Gessler M. The Notch target genes Hey1 and Hey2 are required for embryonic vascular development. Genes Dev. 2004;18:901–911. doi: 10.1101/gad.291004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Pereira FA, Qiu Y, Zhou G, Tsai MJ, Tsai SY. The orphan nuclear receptor COUP-TFII is required for angiogenesis and heart development. Genes Dev. 1999;13:1037–1049. doi: 10.1101/gad.13.8.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Corada M, Morini MF, Dejana E. Signaling pathways in the specification of arteries and veins. Arterioscler Thromb. Vasc. Biol. 2014;34:2372–2377. doi: 10.1161/ATVBAHA.114.303218. [DOI] [PubMed] [Google Scholar]
- 215.Trindade A, et al. Overexpression of delta-like 4 induces arterialization and attenuates vessel formation in developing mouse embryos. Blood. 2008;112:1720–1729. doi: 10.1182/blood-2007-09-112748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Kume T, Jiang H, Topczewska JM, Hogan BL. The murine winged helix transcription factors, Foxc1 and Foxc2, are both required for cardiovascular development and somitogenesis. Genes Dev. 2001;15:2470–2482. doi: 10.1101/gad.907301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Mack JJ, et al. NOTCH1 is a mechanosensor in adult arteries. Nat. Commun. 2017;8:1620. doi: 10.1038/s41467-017-01741-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Weijts B, et al. Blood flow-induced Notch activation and endothelial migration enable vascular remodeling in zebrafish embryos. Nat. Commun. 2018;9:5314. doi: 10.1038/s41467-018-07732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Ditadi A, et al. Human definitive haemogenic endothelium and arterial vascular endothelium represent distinct lineages. Nat. Cell Biol. 2015;17:580–591. doi: 10.1038/ncb3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Butler JM, et al. Endothelial cells are essential for the self-renewal and repopulation of Notch-dependent hematopoietic stem cells. Cell Stem Cell. 2010;6:251–264. doi: 10.1016/j.stem.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Wendorff AA, et al. Hes1 is a critical but context-dependent mediator of canonical Notch signaling in lymphocyte development and transformation. Immunity. 2010;33:671–684. doi: 10.1016/j.immuni.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 222.Chen ELY, Thompson PK, Zúñiga-Pflücker JC. RBPJ-dependent Notch signaling initiates the T cell program in a subset of thymus-seeding progenitors. Nat. Immunol. 2019;20:1456–1468. doi: 10.1038/s41590-019-0518-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Jenkinson EJ, Jenkinson WE, Rossi SW, Anderson G. The thymus and T-cell commitment: the right niche for Notch? Nat. Rev. Immunol. 2006;6:551–555. doi: 10.1038/nri1883. [DOI] [PubMed] [Google Scholar]
- 224.Yu VWC, et al. Specific bone cells produce DLL4 to generate thymus-seeding progenitors from bone marrow. J. Exp. Med. 2015;212:759–774. doi: 10.1084/jem.20141843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Shah NJ, et al. An injectable bone marrow-like scaffold enhances T cell immunity after hematopoietic stem cell transplantation. Nat. Biotechnol. 2019;37:293–302. doi: 10.1038/s41587-019-0017-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Shukla S, et al. Progenitor T-cell differentiation from hematopoietic stem cells using Delta-like-4 and VCAM-1. Nat. Methods. 2017;14:531–538. doi: 10.1038/nmeth.4258. [DOI] [PubMed] [Google Scholar]
- 227.Hozumi K, et al. Delta-like 1 is necessary for the generation of marginal zone B cells but not T cells in vivo. Nat. Immunol. 2004;5:638–644. doi: 10.1038/ni1075. [DOI] [PubMed] [Google Scholar]
- 228.Descatoire, M. et al. Identification of a human splenic marginal zone B cell precursor with NOTCH2-dependent differentiation properties. J. Exp. Med.211, (2014). [DOI] [PMC free article] [PubMed]
- 229.Lechner M, et al. Notch2-mediated plasticity between marginal zone and follicular B cells. Nat. Commun. 2021;12:1111. doi: 10.1038/s41467-021-21359-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Graf R, et al. BCR-dependent lineage plasticity in mature B cells. Science. 2019;363:748–753. doi: 10.1126/science.aau8475. [DOI] [PubMed] [Google Scholar]
- 231.Hernández DC, et al. An in vitro platform supports generation of human innate lymphoid cells from CD34(+) hematopoietic progenitors that recapitulate ex vivo identity. Immunity. 2021;54:2417–2432.e2415. doi: 10.1016/j.immuni.2021.07.019. [DOI] [PubMed] [Google Scholar]
- 232.De Obaldia ME, Bhandoola A. Transcriptional regulation of innate and adaptive lymphocyte lineages. Annu. Rev. Immunol. 2015;33:607–642. doi: 10.1146/annurev-immunol-032414-112032. [DOI] [PubMed] [Google Scholar]
- 233.Yang Q, et al. T cell factor 1 is required for group 2 innate lymphoid cell generation. Immunity. 2013;38:694–704. doi: 10.1016/j.immuni.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Chea S, et al. Single-cell gene expression analyses reveal heterogeneous responsiveness of fetal innate lymphoid progenitors to notch signaling. Cell Rep. 2016;14:1500–1516. doi: 10.1016/j.celrep.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 235.Perchet T, et al. The notch signaling pathway is balancing type 1 innate lymphoid cell immune functions. Front. Immunol. 2018;9:1252. doi: 10.3389/fimmu.2018.01252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Magri G, et al. Innate lymphoid cells integrate stromal and immunological signals to enhance antibody production by splenic marginal zone B cells. Nat. Immunol. 2014;15:354–364. doi: 10.1038/ni.2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Foldi J, Shang Y, Zhao B, Ivashkiv LB, Hu X. RBP-J is required for M2 macrophage polarization in response to chitin and mediates expression of a subset of M2 genes. Protein Cell. 2016;7:201–209. doi: 10.1007/s13238-016-0248-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.López-López S, et al. NOTCH4 exhibits anti-inflammatory activity in activated macrophages by interfering with interferon-γ and TLR4 signaling. Front Immunol. 2021;12:734966. doi: 10.3389/fimmu.2021.734966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Zhou J, Cheng P, Youn JI, Cotter MJ, Gabrilovich DI. Notch and wingless signaling cooperate in regulation of dendritic cell differentiation. Immunity. 2009;30:845–859. doi: 10.1016/j.immuni.2009.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Lewis KL, et al. Notch2 receptor signaling controls functional differentiation of dendritic cells in the spleen and intestine. Immunity. 2011;35:780–791. doi: 10.1016/j.immuni.2011.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Radke AL, et al. Mature human eosinophils express functional Notch ligands mediating eosinophil autocrine regulation. Blood. 2009;113:3092–3101. doi: 10.1182/blood-2008-05-155937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Hofmann JJ, et al. Jagged1 in the portal vein mesenchyme regulates intrahepatic bile duct development: insights into Alagille syndrome. Development. 2010;137:4061–4072. doi: 10.1242/dev.052118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Antoniou A, et al. Intrahepatic bile ducts develop according to a new mode of tubulogenesis regulated by the transcription factor SOX9. Gastroenterology. 2009;136:2325–2333. doi: 10.1053/j.gastro.2009.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Kageyama S, Nakamura K, Ke B, Busuttil RW, Kupiec-Weglinski JW. Serelaxin induces Notch1 signaling and alleviates hepatocellular damage in orthotopic liver transplantation. Am. J. Transpl. 2018;18:1755–1763. doi: 10.1111/ajt.14706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Fiorotto R, et al. Notch signaling regulates tubular morphogenesis during repair from biliary damage in mice. J. Hepatol. 2013;59:124–130. doi: 10.1016/j.jhep.2013.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Cordero-Espinoza L, et al. Dynamic cell contacts between periportal mesenchyme and ductal epithelium act as a rheostat for liver cell proliferation. Cell Stem Cell. 2021;28:1907–1921. doi: 10.1016/j.stem.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Sayols, S. et al. Signalling codes for the maintenance and lineage commitment of embryonic gastric epithelial progenitors. Development147, dev188839 (2020). [DOI] [PubMed]
- 248.Jensen J, et al. Control of endodermal endocrine development by Hes-1. Nat. Genet. 2000;24:36–44. doi: 10.1038/71657. [DOI] [PubMed] [Google Scholar]
- 249.Sallé J, et al. Intrinsic regulation of enteroendocrine fate by Numb. EMBO J. 2017;36:1928–1945. doi: 10.15252/embj.201695622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Yin X, et al. Niche-independent high-purity cultures of Lgr5+ intestinal stem cells and their progeny. Nat. Methods. 2014;11:106–112. doi: 10.1038/nmeth.2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Serra D, et al. Self-organization and symmetry breaking in intestinal organoid development. Nature. 2019;569:66–72. doi: 10.1038/s41586-019-1146-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Demitrack ES, et al. Notch signaling regulates gastric antral LGR5 stem cell function. EMBO J. 2015;34:2522–2536. doi: 10.15252/embj.201490583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Gifford GB, et al. Notch1 and Notch2 receptors regulate mouse and human gastric antral epithelial cell homoeostasis. Gut. 2017;66:1001–1011. doi: 10.1136/gutjnl-2015-310811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Kim T-H, Shivdasani RA. Notch signaling in stomach epithelial stem cell homeostasis. J. Exp. Med. 2011;208:677–688. doi: 10.1084/jem.20101737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Apelqvist A, et al. Notch signalling controls pancreatic cell differentiation. Nature. 1999;400:877–881. doi: 10.1038/23716. [DOI] [PubMed] [Google Scholar]
- 256.Fujikura J, et al. Notch/Rbp-j signaling prevents premature endocrine and ductal cell differentiation in the pancreas. Cell Metab. 2006;3:59–65. doi: 10.1016/j.cmet.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 257.Rubey M, et al. DLL1- and DLL4-mediated notch signaling is essential for adult pancreatic islet homeostasis. Diabetes. 2020;69:915–926. doi: 10.2337/db19-0795. [DOI] [PubMed] [Google Scholar]
- 258.Seymour PA, et al. Jag1 modulates an oscillatory Dll1-Notch-Hes1 signaling module to coordinate growth and fate of pancreatic progenitors. Dev. Cell. 2020;52:731–747. doi: 10.1016/j.devcel.2020.01.015. [DOI] [PubMed] [Google Scholar]
- 259.Louvi A, Artavanis-Tsakonas S. Notch signalling in vertebrate neural development. Nat. Rev. Neurosci. 2006;7:93–102. doi: 10.1038/nrn1847. [DOI] [PubMed] [Google Scholar]
- 260.Portin P, Rantanen M. Interaction of master mind, big brain, neuralized and Notch genes of Drosophila melanogaster as expressed in adult morphology. Hereditas. 1991;114:197–200. doi: 10.1111/j.1601-5223.1991.tb00324.x. [DOI] [PubMed] [Google Scholar]
- 261.Kelley MR, Kidd S, Deutsch WA, Young MW. Mutations altering the structure of epidermal growth factor-like coding sequences at the Drosophila Notch locus. Cell. 1987;51:539–548. doi: 10.1016/0092-8674(87)90123-1. [DOI] [PubMed] [Google Scholar]
- 262.Ye Y, Lukinova N, Fortini ME. Neurogenic phenotypes and altered Notch processing in Drosophila Presenilin mutants. Nature. 1999;398:525–529. doi: 10.1038/19096. [DOI] [PubMed] [Google Scholar]
- 263.Zamboni M, Llorens-Bobadilla E, Magnusson JP, Frisén J. A widespread neurogenic potential of neocortical astrocytes is induced by injury. Cell Stem Cell. 2020;27:605–617.e605. doi: 10.1016/j.stem.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Gao F, et al. Transcription factor RBP-J-mediated signaling represses the differentiation of neural stem cells into intermediate neural progenitors. Mol. Cell Neurosci. 2009;40:442–450. doi: 10.1016/j.mcn.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 265.Chi Z, et al. Botch promotes neurogenesis by antagonizing Notch. Dev. Cell. 2012;22:707–720. doi: 10.1016/j.devcel.2012.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Mall M, et al. Myt1l safeguards neuronal identity by actively repressing many non-neuronal fates. Nature. 2017;544:245–249. doi: 10.1038/nature21722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Cárdenas A, et al. Evolution of cortical neurogenesis in amniotes controlled by Robo signaling levels. Cell. 2018;174:590–606.e521. doi: 10.1016/j.cell.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Lui JH, Hansen DV, Kriegstein AR. Development and evolution of the human neocortex. Cell. 2011;146:18–36. doi: 10.1016/j.cell.2011.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Nichane M, Ren X, Souopgui J, Bellefroid EJ. Hairy2 functions through both DNA-binding and non DNA-binding mechanisms at the neural plate border in Xenopus. Dev. Biol. 2008;322:368–380. doi: 10.1016/j.ydbio.2008.07.026. [DOI] [PubMed] [Google Scholar]
- 270.Ngan ES, et al. Hedgehog/Notch-induced premature gliogenesis represents a new disease mechanism for Hirschsprung disease in mice and humans. J. Clin. Invest. 2011;121:3467–3478. doi: 10.1172/JCI43737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Tang W, et al. Exome-wide association study identified new risk loci for Hirschsprung’s disease. Mol. Neurobiol. 2017;54:1777–1785. doi: 10.1007/s12035-016-9752-2. [DOI] [PubMed] [Google Scholar]
- 272.Harima Y, Takashima Y, Ueda Y, Ohtsuka T, Kageyama R. Accelerating the tempo of the segmentation clock by reducing the number of introns in the Hes7 gene. Cell Rep. 2013;3:1–7. doi: 10.1016/j.celrep.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 273.Hussain M, et al. Notch signaling: linking embryonic lung development and asthmatic airway remodeling. Mol. Pharm. 2017;92:676–693. doi: 10.1124/mol.117.110254. [DOI] [PubMed] [Google Scholar]
- 274.Tsao P-N, et al. Epithelial Notch signaling regulates lung alveolar morphogenesis and airway epithelial integrity. Proc. Natl Acad. Sci. USA. 2016;113:8242–8247. doi: 10.1073/pnas.1511236113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Rock JR, et al. Notch-dependent differentiation of adult airway basal stem cells. Cell Stem Cell. 2011;8:639–648. doi: 10.1016/j.stem.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Pardo-Saganta A, et al. Injury induces direct lineage segregation of functionally distinct airway basal stem/progenitor cell subpopulations. Cell Stem Cell. 2015;16:184–197. doi: 10.1016/j.stem.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Singh K, et al. JunB defines functional and structural integrity of the epidermo-pilosebaceous unit in the skin. Nat. Commun. 2018;9:3425. doi: 10.1038/s41467-018-05726-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Nguyen B-C, et al. Cross-regulation between Notch and p63 in keratinocyte commitment to differentiation. Genes Dev. 2006;20:1028–1042. doi: 10.1101/gad.1406006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Ezratty EJ, et al. A role for the primary cilium in Notch signaling and epidermal differentiation during skin development. Cell. 2011;145:1129–1141. doi: 10.1016/j.cell.2011.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Williams SE, Beronja S, Pasolli HA, Fuchs E. Asymmetric cell divisions promote Notch-dependent epidermal differentiation. Nature. 2011;470:353–358. doi: 10.1038/nature09793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Veniaminova NA, et al. Niche-Specific Factors Dynamically Regulate Sebaceous Gland Stem Cells in the Skin. Dev. Cell. 2019;51:326–340.e4. doi: 10.1016/j.devcel.2019.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Gratton, R. et al. Pleiotropic role of notch signaling in human skin diseases. Int. J. Mol. Sci.21, 4214 (2020). [DOI] [PMC free article] [PubMed]
- 283.Wang B, et al. Gamma-secretase gene mutations in familial acne inversa. Science. 2010;330:1065. doi: 10.1126/science.1196284. [DOI] [PubMed] [Google Scholar]
- 284.Baudrimont M, Dubas F, Joutel A, Tournier-Lasserve E, Bousser MG. Autosomal dominant leukoencephalopathy and subcortical ischemic stroke. A clinicopathological study. Stroke. 1993;24:122–125. doi: 10.1161/01.str.24.1.122. [DOI] [PubMed] [Google Scholar]
- 285.Joutel A, et al. Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature. 1996;383:707–710. doi: 10.1038/383707a0. [DOI] [PubMed] [Google Scholar]
- 286.Joutel A, et al. Strong clustering and stereotyped nature of Notch3 mutations in CADASIL patients. Lancet. 1997;350:1511–1515. doi: 10.1016/S0140-6736(97)08083-5. [DOI] [PubMed] [Google Scholar]
- 287.Monet-Leprêtre M, et al. Abnormal recruitment of extracellular matrix proteins by excess Notch3 ECD: a new pathomechanism in CADASIL. Brain. 2013;136:1830–1845. doi: 10.1093/brain/awt092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Okeda R, Arima K, Kawai M. Arterial changes in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) in relation to pathogenesis of diffuse myelin loss of cerebral white matter: examination of cerebral medullary arteries by reconstruction of serial sections of an autopsy case. Stroke. 2002;33:2565–2569. doi: 10.1161/01.str.0000032620.91848.1c. [DOI] [PubMed] [Google Scholar]
- 289.Baron-Menguy C, Domenga-Denier V, Ghezali L, Faraci FM, Joutel A. Increased Notch3 activity mediates pathological changes in structure of cerebral arteries. Hypertension. 2017;69:60–70. doi: 10.1161/HYPERTENSIONAHA.116.08015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Dubroca C, et al. Impaired vascular mechanotransduction in a transgenic mouse model of CADASIL arteriopathy. Stroke. 2005;36:113–117. doi: 10.1161/01.STR.0000149949.92854.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Ling C, et al. Modeling CADASIL vascular pathologies with patient-derived induced pluripotent stem cells. Protein Cell. 2019;10:249–271. doi: 10.1007/s13238-019-0608-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Joutel A, et al. Cerebrovascular dysfunction and microcirculation rarefaction precede white matter lesions in a mouse genetic model of cerebral ischemic small vessel disease. J. Clin. Invest. 2010;120:433–445. doi: 10.1172/JCI39733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.McDaniell R, et al. NOTCH2 mutations cause Alagille syndrome, a heterogeneous disorder of the notch signaling pathway. Am. J. Hum. Genet. 2006;79:169–173. doi: 10.1086/505332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Lykavieris P, Hadchouel M, Chardot C, Bernard O. Outcome of liver disease in children with Alagille syndrome: a study of 163 patients. Gut. 2001;49:431–435. doi: 10.1136/gut.49.3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Fabris L, et al. Pathobiology of inherited biliary diseases: a roadmap to understand acquired liver diseases. Nat. Rev. Gastroenterol. Hepatol. 2019;16:497–511. doi: 10.1038/s41575-019-0156-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Colliton RP, et al. Mutation analysis of Jagged1 (JAG1) in Alagille syndrome patients. Hum. Mutat. 2001;17:151–152. doi: 10.1002/1098-1004(200102)17:2<151::AID-HUMU8>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 297.Warthen DM, et al. Jagged1 (JAG1) mutations in Alagille syndrome: increasing the mutation detection rate. Hum. Mutat. 2006;27:436–443. doi: 10.1002/humu.20310. [DOI] [PubMed] [Google Scholar]
- 298.Suskind DL, Murray KF. Increasing the mutation rate for Jagged1 mutations in patients with Alagille syndrome. Hepatology. 2007;46:598–599. doi: 10.1002/hep.21860. [DOI] [PubMed] [Google Scholar]
- 299.Kamath BM, Spinner NB, Rosenblum ND. Renal involvement and the role of Notch signalling in Alagille syndrome. Nat. Rev. Nephrol. 2013;9:409–418. doi: 10.1038/nrneph.2013.102. [DOI] [PubMed] [Google Scholar]
- 300.Huch M, et al. Long-term culture of genome-stable bipotent stem cells from adult human liver. Cell. 2015;160:299–312. doi: 10.1016/j.cell.2014.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Andersson ER, et al. Mouse model of alagille syndrome and mechanisms of Jagged1 Missense mutations. Gastroenterology. 2018;154:1080–1095. doi: 10.1053/j.gastro.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Adams JM, Jafar-Nejad H. A new model of alagille syndrome with broad phenotypic representation. Gastroenterology. 2018;154:803–806. doi: 10.1053/j.gastro.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 303.Adams JM, et al. Sox9 is a modifier of the liver disease severity in a mouse model of alagille syndrome. Hepatology. 2020;71:1331–1349. doi: 10.1002/hep.30912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Pourquié O. Vertebrate segmentation: from cyclic gene networks to scoliosis. Cell. 2011;145:650–663. doi: 10.1016/j.cell.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Lefebvre M, et al. Diagnostic strategy in segmentation defect of the vertebrae: a retrospective study of 73 patients. J. Med. Genet. 2018;55:422–429. doi: 10.1136/jmedgenet-2017-104939. [DOI] [PubMed] [Google Scholar]
- 306.Dunwoodie SL. The role of Notch in patterning the human vertebral column. Curr. Opin. Genet. Dev. 2009;19:329–337. doi: 10.1016/j.gde.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 307.Kusumi K, et al. The mouse pudgy mutation disrupts Delta homologue Dll3 and initiation of early somite boundaries. Nat. Genet. 1998;19:274–278. doi: 10.1038/961. [DOI] [PubMed] [Google Scholar]
- 308.Bulman MP, et al. Mutations in the human delta homologue, DLL3, cause axial skeletal defects in spondylocostal dysostosis. Nat. Genet. 2000;24:438–441. doi: 10.1038/74307. [DOI] [PubMed] [Google Scholar]
- 309.Whittock NV, et al. Mutated MESP2 causes spondylocostal dysostosis in humans. Am. J. Hum. Genet. 2004;74:1249–1254. doi: 10.1086/421053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Makino Y, et al. Spatiotemporal disorder in the axial skeleton development of the Mesp2-null mouse: a model of spondylocostal dysostosis and spondylothoracic dysostosis. Bone. 2013;53:248–258. doi: 10.1016/j.bone.2012.11.033. [DOI] [PubMed] [Google Scholar]
- 311.Sparrow DB, Sillence D, Wouters MA, Turnpenny PD, Dunwoodie SL. Two novel missense mutations in HAIRY-AND-ENHANCER-OF-SPLIT-7 in a family with spondylocostal dysostosis. Eur. J. Hum. Genet. 2010;18:674–679. doi: 10.1038/ejhg.2009.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Sparrow DB, et al. Mutation of the LUNATIC FRINGE gene in humans causes spondylocostal dysostosis with a severe vertebral phenotype. Am. J. Hum. Genet. 2006;78:28–37. doi: 10.1086/498879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Sparrow DB, et al. A mechanism for gene-environment interaction in the etiology of congenital scoliosis. Cell. 2012;149:295–306. doi: 10.1016/j.cell.2012.02.054. [DOI] [PubMed] [Google Scholar]
- 314.Valenti L, et al. Hepatic notch signaling correlates with insulin resistance and nonalcoholic fatty liver disease. Diabetes. 2013;62:4052–4062. doi: 10.2337/db13-0769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Zhu C, Tabas I, Schwabe RF, Pajvani UB. Maladaptive regeneration—the reawakening of developmental pathways in NASH and fibrosis. Nat. Rev. Gastroenterol. Hepatol. 2021;18:131–142. doi: 10.1038/s41575-020-00365-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Romeo SNotch. and Nonalcoholic Fatty Liver and Fibrosis. N. Engl. J. Med. 2019;380:681–683. doi: 10.1056/NEJMcibr1815636. [DOI] [PubMed] [Google Scholar]
- 317.Yu, J. et al. Hepatocyte TLR4 triggers inter-hepatocyte Jagged1/Notch signaling to determine NASH-induced fibrosis. Sci. Transl. Med.13, eabe1692 (2021). [DOI] [PMC free article] [PubMed]
- 318.Zhu, C. et al. Hepatocyte Notch activation induces liver fibrosis in nonalcoholic steatohepatitis. Sci. Transl. Med.10, eaat0344 (2018). [DOI] [PMC free article] [PubMed]
- 319.Sassi N, et al. The role of the Notch pathway in healthy and osteoarthritic articular cartilage: from experimental models to ex vivo studies. Arthritis Res. Ther. 2011;13:208. doi: 10.1186/ar3255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Monteagudo S, Lories RJ. A Notch in the joint that exacerbates osteoarthritis. Nat. Rev. Rheumatol. 2018;14:563–564. doi: 10.1038/s41584-018-0076-7. [DOI] [PubMed] [Google Scholar]
- 321.Liu Z, et al. A dual role for NOTCH signaling in joint cartilage maintenance and osteoarthritis. Sci. Signal. 2015;8:ra71. doi: 10.1126/scisignal.aaa3792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Sun J, et al. Notch ligand Jagged1 promotes mesenchymal stromal cell-based cartilage repair. Exp. Mol. Med. 2018;50:1–10. doi: 10.1038/s12276-018-0151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Hosaka Y, et al. Notch signaling in chondrocytes modulates endochondral ossification and osteoarthritis development. Proc. Natl Acad. Sci. USA. 2013;110:1875–1880. doi: 10.1073/pnas.1207458110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Tindemans I, et al. Increased surface expression of NOTCH on memory T cells in peripheral blood from patients with asthma. J. Allergy Clin. Immunol. 2019;143:769–771.e3. doi: 10.1016/j.jaci.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 325.Tindemans I, et al. Notch signaling in T cells is essential for allergic airway inflammation, but expression of the Notch ligands Jagged 1 and Jagged 2 on dendritic cells is dispensable. J. Allergy Clin. Immunol. 2017;140:1079–1089. doi: 10.1016/j.jaci.2016.11.046. [DOI] [PubMed] [Google Scholar]
- 326.Huang, M.-T., Chiu, C.-J. & Chiang, B.-L. Multi-faceted notch in allergic airway inflammation. Int. J. Mol. Sci.20, 3508 (2019). [DOI] [PMC free article] [PubMed]
- 327.KleinJan A, et al. The Notch pathway inhibitor stapled α-helical peptide derived from mastermind-like 1 (SAHM1) abrogates the hallmarks of allergic asthma. J. Allergy Clin. Immunol. 2018;142:76–85.e8. doi: 10.1016/j.jaci.2017.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Tindemans I, et al. Notch signaling licenses allergic airway inflammation by promoting Th2 cell lymph node egress. J. Clin. Investig. 2020;130:3576–3591. doi: 10.1172/JCI128310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Harb H, et al. A regulatory T cell Notch4-GDF15 axis licenses tissue inflammation in asthma. Nat. Immunol. 2020;21:1359–1370. doi: 10.1038/s41590-020-0777-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Cao Z, et al. Targeting of the pulmonary capillary vascular niche promotes lung alveolar repair and ameliorates fibrosis. Nat. Med. 2016;22:154–162. doi: 10.1038/nm.4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Steffes LC, et al. A Notch3-marked subpopulation of vascular smooth muscle cells is the cell of origin for occlusive pulmonary vascular lesions. Circulation. 2020;142:1545–1561. doi: 10.1161/CIRCULATIONAHA.120.045750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Dabral S, et al. Notch1 signalling regulates endothelial proliferation and apoptosis in pulmonary arterial hypertension. Eur. Respir. J. 2016;48:1137–1149. doi: 10.1183/13993003.00773-2015. [DOI] [PubMed] [Google Scholar]
- 333.Gu X-Y, Chu X, Zeng X-L, Bao H-R, Liu X-J. Effects of PM2.5 exposure on the Notch signaling pathway and immune imbalance in chronic obstructive pulmonary disease. Environ. Pollut. 2017;226:163–173. doi: 10.1016/j.envpol.2017.03.070. [DOI] [PubMed] [Google Scholar]
- 334.Bodas M, et al. Cigarette smoke activates NOTCH3 to promote goblet cell differentiation in human airway epithelial cells. Am. J. Respir. Cell Mol. Biol. 2021;64:426–440. doi: 10.1165/rcmb.2020-0302OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Ballester-López C, et al. The Notch ligand DNER regulates macrophage IFNγ release in chronic obstructive pulmonary disease. EBioMedicine. 2019;43:562–575. doi: 10.1016/j.ebiom.2019.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Di Ianni M, et al. NOTCH and graft-versus-host disease. Front. Immunol. 2018;9:1825. doi: 10.3389/fimmu.2018.01825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Radojcic V, et al. Notch signaling mediated by Delta-like ligands 1 and 4 controls the pathogenesis of chronic GVHD in mice. Blood. 2018;132:2188–2200. doi: 10.1182/blood-2018-03-841155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Yvon ES, et al. Overexpression of the Notch ligand, Jagged-1, induces alloantigen-specific human regulatory T cells. Blood. 2003;102:3815–3821. doi: 10.1182/blood-2002-12-3826. [DOI] [PubMed] [Google Scholar]
- 339.Amsen D. T cells take directions from supporting cast in graft-versus-host disease. J. Clin. Investig. 2017;127:1215–1217. doi: 10.1172/JCI93552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Poe JC, et al. An aberrant NOTCH2-BCR signaling axis in B cells from patients with chronic GVHD. Blood. 2017;130:2131–2145. doi: 10.1182/blood-2017-05-782466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Bartolome A, Zhu C, Sussel L, Pajvani UB. Notch signaling dynamically regulates adult β cell proliferation and maturity. J. Clin. Invest. 2019;129:268–280. doi: 10.1172/JCI98098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Reynolds TC, Smith SD, Sklar J. Analysis of DNA surrounding the breakpoints of chromosomal translocations involving the beta T cell receptor gene in human lymphoblastic neoplasms. Cell. 1987;50:107–117. doi: 10.1016/0092-8674(87)90667-2. [DOI] [PubMed] [Google Scholar]
- 343.Ellisen LW, et al. TAN-1, the human homolog of the Drosophila notch gene, is broken by chromosomal translocations in T lymphoblastic neoplasms. Cell. 1991;66:649–661. doi: 10.1016/0092-8674(91)90111-b. [DOI] [PubMed] [Google Scholar]
- 344.Weng AP, et al. Activating mutations of NOTCH1 in human T cell acute lymphoblastic leukemia. Science. 2004;306:269–271. doi: 10.1126/science.1102160. [DOI] [PubMed] [Google Scholar]
- 345.Pear WS, et al. Exclusive development of T cell neoplasms in mice transplanted with bone marrow expressing activated Notch alleles. J. Exp. Med. 1996;183:2283–2291. doi: 10.1084/jem.183.5.2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Herranz D, et al. A NOTCH1-driven MYC enhancer promotes T cell development, transformation and acute lymphoblastic leukemia. Nat. Med. 2014;20:1130–1137. doi: 10.1038/nm.3665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Herranz D, et al. Metabolic reprogramming induces resistance to anti-NOTCH1 therapies in T cell acute lymphoblastic leukemia. Nat. Med. 2015;21:1182–1189. doi: 10.1038/nm.3955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Trimarchi T, et al. Genome-wide mapping and characterization of Notch-regulated long noncoding RNAs in acute leukemia. Cell. 2014;158:593–606. doi: 10.1016/j.cell.2014.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Joshi I, et al. Notch signaling mediates G1/S cell-cycle progression in T cells via cyclin D3 and its dependent kinases. Blood. 2009;113:1689–1698. doi: 10.1182/blood-2008-03-147967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Bernasconi-Elias P, et al. Characterization of activating mutations of NOTCH3 in T-cell acute lymphoblastic leukemia and anti-leukemic activity of NOTCH3 inhibitory antibodies. Oncogene. 2016;35:6077–6086. doi: 10.1038/onc.2016.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Bonfiglio F, et al. Genetic and phenotypic attributes of splenic marginal zone lymphoma. Blood. 2021;139:732–747. doi: 10.1182/blood.2021012386. [DOI] [PubMed] [Google Scholar]
- 352.Tardivon D, et al. Notch signaling promotes disease initiation and progression in murine chronic lymphocytic leukemia. Blood. 2021;137:3079–3092. doi: 10.1182/blood.2020006701. [DOI] [PubMed] [Google Scholar]
- 353.Huang Y-H, et al. CREBBP/EP300 mutations promoted tumor progression in diffuse large B-cell lymphoma through altering tumor-associated macrophage polarization via FBXW7-NOTCH-CCL2/CSF1 axis. Signal Transduct. Target Ther. 2021;6:10. doi: 10.1038/s41392-020-00437-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Kannan S, et al. Notch activation inhibits AML growth and survival: a potential therapeutic approach. J. Exp. Med. 2013;210:321–337. doi: 10.1084/jem.20121527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Yuan X, et al. Meta-analysis reveals the correlation of Notch signaling with non-small cell lung cancer progression and prognosis. Sci. Rep. 2015;5:10338. doi: 10.1038/srep10338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Liu L, et al. An RFC4/Notch1 signaling feedback loop promotes NSCLC metastasis and stemness. Nat. Commun. 2021;12:2693. doi: 10.1038/s41467-021-22971-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Westhoff B, et al. Alterations of the Notch pathway in lung cancer. Proc. Natl Acad. Sci. USA. 2009;106:22293–22298. doi: 10.1073/pnas.0907781106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Licciulli S, et al. Notch1 is required for Kras-induced lung adenocarcinoma and controls tumor cell survival via p53. Cancer Res. 2013;73:5974–5984. doi: 10.1158/0008-5472.CAN-13-1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Xu X, et al. The cell of origin and subtype of K-Ras-induced lung tumors are modified by Notch and Sox2. Genes Dev. 2014;28:1929–1939. doi: 10.1101/gad.243717.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Allen TD, Rodriguez EM, Jones KD, Bishop JM. Activated Notch1 induces lung adenomas in mice and cooperates with Myc in the generation of lung adenocarcinoma. Cancer Res. 2011;71:6010–6018. doi: 10.1158/0008-5472.CAN-11-0595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Ali SA, Justilien V, Jamieson L, Murray NR, Fields AP. Protein kinase Cι drives a NOTCH3-dependent Stem-like phenotype in mutant KRAS lung adenocarcinoma. Cancer Cell. 2016;29:367–378. doi: 10.1016/j.ccell.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Sinicropi-Yao SL, et al. Co-expression analysis reveals mechanisms underlying the varied roles of NOTCH1 in NSCLC. J. Thorac. Oncol. 2019;14:223–236. doi: 10.1016/j.jtho.2018.10.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Qiao L, Wong BC. Role of Notch signaling in colorectal cancer. Carcinogenesis. 2009;30:1979–1986. doi: 10.1093/carcin/bgp236. [DOI] [PubMed] [Google Scholar]
- 364.Tyagi, A., Sharma, A. K. & Damodaran, C. A review on Notch signaling and colorectal cancer. Cells9, 1549 (2020). [DOI] [PMC free article] [PubMed]
- 365.Fre S, et al. Notch and Wnt signals cooperatively control cell proliferation and tumorigenesis in the intestine. Proc. Natl Acad. Sci. USA. 2009;106:6309–6314. doi: 10.1073/pnas.0900427106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Hayakawa Y, et al. BHLHA15-positive secretory precursor cells can give rise to tumors in intestine and colon in mice. Gastroenterology. 2019;156:1066–1081.e1016. doi: 10.1053/j.gastro.2018.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Jackstadt R, et al. Epithelial NOTCH signaling rewires the tumor microenvironment of colorectal cancer to drive poor-prognosis subtypes and metastasis. Cancer Cell. 2019;36:319–336.e317. doi: 10.1016/j.ccell.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Bu P, et al. A miR-34a-numb feedforward loop triggered by inflammation regulates asymmetric stem cell division in intestine and colon cancer. Cell Stem Cell. 2016;18:189–202. doi: 10.1016/j.stem.2016.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Ruland J. Colon cancer: epithelial notch signaling recruits neutrophils to drive metastasis. Cancer Cell. 2019;36:213–214. doi: 10.1016/j.ccell.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 370.Sonoshita M, et al. Promotion of colorectal cancer invasion and metastasis through activation of NOTCH-DAB1-ABL-RHOGEF protein TRIO. Cancer Discov. 2015;5:198–211. doi: 10.1158/2159-8290.CD-14-0595. [DOI] [PubMed] [Google Scholar]
- 371.Jackstadt R, Sansom OJ. Mouse models of intestinal cancer. J. Pathol. 2016;238:141–151. doi: 10.1002/path.4645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Kranenburg OPrometastatic. NOTCH signaling in colon cancer. Cancer Discov. 2015;5:115–117. doi: 10.1158/2159-8290.CD-14-1456. [DOI] [PubMed] [Google Scholar]
- 373.Chanrion M, et al. Concomitant Notch activation and p53 deletion trigger epithelial-to-mesenchymal transition and metastasis in mouse gut. Nat. Commun. 2014;5:5005. doi: 10.1038/ncomms6005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Sonoshita M, et al. Suppression of colon cancer metastasis by Aes through inhibition of Notch signaling. Cancer Cell. 2011;19:125–137. doi: 10.1016/j.ccr.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 375.Parida S, et al. A procarcinogenic colon microbe promotes breast tumorigenesis and metastatic progression and concomitantly activates Notch and β-Catenin Axes. Cancer Discov. 2021;11:1138–1157. doi: 10.1158/2159-8290.CD-20-0537. [DOI] [PubMed] [Google Scholar]
- 376.Nabet BY, et al. Exosome RNA unshielding couples stromal activation to pattern recognition receptor signaling in cancer. Cell. 2017;170:352–366.e313. doi: 10.1016/j.cell.2017.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Krishna BM, et al. Notch signaling in breast cancer: from pathway analysis to therapy. Cancer Lett. 2019;461:123–131. doi: 10.1016/j.canlet.2019.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Gallahan D, Kozak C, Callahan R. A new common integration region (int-3) for mouse mammary tumor virus on mouse chromosome 17. J. Virol. 1987;61:218–220. doi: 10.1128/jvi.61.1.218-220.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Reedijk M, et al. High-level coexpression of JAG1 and NOTCH1 is observed in human breast cancer and is associated with poor overall survival. Cancer Res. 2005;65:8530–8537. doi: 10.1158/0008-5472.CAN-05-1069. [DOI] [PubMed] [Google Scholar]
- 380.Callahan R, Smith GH. MMTV-induced mammary tumorigenesis: gene discovery, progression to malignancy and cellular pathways. Oncogene. 2000;19:992–1001. doi: 10.1038/sj.onc.1203276. [DOI] [PubMed] [Google Scholar]
- 381.Theodorou V, et al. MMTV insertional mutagenesis identifies genes, gene families and pathways involved in mammary cancer. Nat. Genet. 2007;39:759–769. doi: 10.1038/ng2034. [DOI] [PubMed] [Google Scholar]
- 382.Robinson DR, et al. Functionally recurrent rearrangements of the MAST kinase and Notch gene families in breast cancer. Nat. Med. 2011;17:1646–1651. doi: 10.1038/nm.2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Jordan NV, et al. HER2 expression identifies dynamic functional states within circulating breast cancer cells. Nature. 2016;537:102–106. doi: 10.1038/nature19328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Colaluca IN, et al. NUMB controls p53 tumour suppressor activity. Nature. 2008;451:76–80. doi: 10.1038/nature06412. [DOI] [PubMed] [Google Scholar]
- 385.Dittmer J. Breast cancer stem cells: features, key drivers and treatment options. Semin. Cancer Biol. 2018;53:59–74. doi: 10.1016/j.semcancer.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 386.Ibrahim SA, et al. Syndecan-1 is a novel molecular marker for triple negative inflammatory breast cancer and modulates the cancer stem cell phenotype via the IL-6/STAT3, Notch and EGFR signaling pathways. Mol. Cancer. 2017;16:57. doi: 10.1186/s12943-017-0621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Shen Q, et al. Notch shapes the innate immunophenotype in breast cancer. Cancer Discov. 2017;7:1320–1335. doi: 10.1158/2159-8290.CD-17-0037. [DOI] [PubMed] [Google Scholar]
- 388.Lin Q, et al. ASPH-notch axis guided exosomal delivery of prometastatic secretome renders breast cancer multi-organ metastasis. Mol. Cancer. 2019;18:156. doi: 10.1186/s12943-019-1077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.The Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature474, 609–615 (2011). [DOI] [PMC free article] [PubMed]
- 390.Lu KH, et al. Selection of potential markers for epithelial ovarian cancer with gene expression arrays and recursive descent partition analysis. Clin. Cancer Res. 2004;10:3291–3300. doi: 10.1158/1078-0432.CCR-03-0409. [DOI] [PubMed] [Google Scholar]
- 391.Park JT, et al. Notch3 gene amplification in ovarian cancer. Cancer Res. 2006;66:6312–6318. doi: 10.1158/0008-5472.CAN-05-3610. [DOI] [PubMed] [Google Scholar]
- 392.Hopfer O, Zwahlen D, Fey MF, Aebi S. The Notch pathway in ovarian carcinomas and adenomas. Br. J. Cancer. 2005;93:709–718. doi: 10.1038/sj.bjc.6602719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Groeneweg JW, Foster R, Growdon WB, Verheijen RH, Rueda BR. Notch signaling in serous ovarian cancer. J. Ovarian Res. 2014;7:95. doi: 10.1186/s13048-014-0095-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Park JT, et al. Notch3 overexpression is related to the recurrence of ovarian cancer and confers resistance to carboplatin. Am. J. Pathol. 2010;177:1087–1094. doi: 10.2353/ajpath.2010.100316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Choi JH, et al. Jagged-1 and Notch3 juxtacrine loop regulates ovarian tumor growth and adhesion. Cancer Res. 2008;68:5716–5723. doi: 10.1158/0008-5472.CAN-08-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Steg AD, et al. Targeting the notch ligand JAGGED1 in both tumor cells and stroma in ovarian cancer. Clin. Cancer Res. 2011;17:5674–5685. doi: 10.1158/1078-0432.CCR-11-0432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Yen WC, et al. Targeting Notch signaling with a Notch2/Notch3 antagonist (tarextumab) inhibits tumor growth and decreases tumor-initiating cell frequency. Clin. Cancer Res. 2015;21:2084–2095. doi: 10.1158/1078-0432.CCR-14-2808. [DOI] [PubMed] [Google Scholar]
- 398.Hu W, et al. Biological roles of the Delta family Notch ligand Dll4 in tumor and endothelial cells in ovarian cancer. Cancer Res. 2011;71:6030–6039. doi: 10.1158/0008-5472.CAN-10-2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Zhu C, et al. Notch activity characterizes a common hepatocellular carcinoma subtype with unique molecular and clinicopathologic features. J. Hepatol. 2021;74:613–626. doi: 10.1016/j.jhep.2020.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Razumilava N, Gores GJ. Notch-driven carcinogenesis: the merging of hepatocellular cancer and cholangiocarcinoma into a common molecular liver cancer subtype. J. Hepatol. 2013;58:1244–1245. doi: 10.1016/j.jhep.2013.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Villanueva A, et al. Notch signaling is activated in human hepatocellular carcinoma and induces tumor formation in mice. Gastroenterology. 2012;143:1660–1669.e1667. doi: 10.1053/j.gastro.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Zhang L, et al. An essential role of RNF187 in Notch1 mediated metastasis of hepatocellular carcinoma. J. Exp. Clin. Cancer Res. 2019;38:384. doi: 10.1186/s13046-019-1382-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Viatour P, et al. Notch signaling inhibits hepatocellular carcinoma following inactivation of the RB pathway. J. Exp. Med. 2011;208:1963–1976. doi: 10.1084/jem.20110198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Luiken S, et al. NOTCH target gene HES5 mediates oncogenic and tumor suppressive functions in hepatocarcinogenesis. Oncogene. 2020;39:3128–3144. doi: 10.1038/s41388-020-1198-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Lim SO, et al. Notch1 differentially regulates oncogenesis by wildtype p53 overexpression and p53 mutation in grade III hepatocellular carcinoma. Hepatology. 2011;53:1352–1362. doi: 10.1002/hep.24208. [DOI] [PubMed] [Google Scholar]
- 406.Hu YY, et al. Notch signaling contributes to the maintenance of both normal neural stem cells and patient-derived glioma stem cells. BMC Cancer. 2011;11:82. doi: 10.1186/1471-2407-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Zhu TS, et al. Endothelial cells create a stem cell niche in glioblastoma by providing NOTCH ligands that nurture self-renewal of cancer stem-like cells. Cancer Res. 2011;71:6061–6072. doi: 10.1158/0008-5472.CAN-10-4269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Chu Q, Orr BA, Semenkow S, Bar EE, Eberhart CG. Prolonged inhibition of glioblastoma xenograft initiation and clonogenic growth following in vivo Notch blockade. Clin. Cancer Res. 2013;19:3224–3233. doi: 10.1158/1078-0432.CCR-12-2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Natarajan S, et al. Notch1-induced brain tumor models the sonic hedgehog subgroup of human medulloblastoma. Cancer Res. 2013;73:5381–5390. doi: 10.1158/0008-5472.CAN-13-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Wang J, et al. Invasion of white matter tracts by glioma stem cells is regulated by a NOTCH1-SOX2 positive-feedback loop. Nat. Neurosci. 2019;22:91–105. doi: 10.1038/s41593-018-0285-z. [DOI] [PubMed] [Google Scholar]
- 411.Katsushima K, et al. Targeting the Notch-regulated non-coding RNA TUG1 for glioma treatment. Nat. Commun. 2016;7:13616. doi: 10.1038/ncomms13616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Yi L, et al. Notch1 signaling pathway promotes invasion, self-renewal and growth of glioma initiating cells via modulating chemokine system CXCL12/CXCR4. J. Exp. Clin. Cancer Res. 2019;38:339. doi: 10.1186/s13046-019-1319-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Giachino C, et al. A tumor suppressor function for notch signaling in forebrain tumor subtypes. Cancer Cell. 2015;28:730–742. doi: 10.1016/j.ccell.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 414.Parmigiani, E., Taylor, V. & Giachino, C. Oncogenic and tumor-suppressive functions of NOTCH signaling in glioma. Cells9 (2020). [DOI] [PMC free article] [PubMed]
- 415.Stephens PJ, et al. Whole exome sequencing of adenoid cystic carcinoma. J. Clin. Invest. 2013;123:2965–2968. doi: 10.1172/JCI67201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Ho AS, et al. The mutational landscape of adenoid cystic carcinoma. Nat. Genet. 2013;45:791–798. doi: 10.1038/ng.2643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Drier Y, et al. An oncogenic MYB feedback loop drives alternate cell fates in adenoid cystic carcinoma. Nat. Genet. 2016;48:265–272. doi: 10.1038/ng.3502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Karpinets TV, et al. Whole-genome sequencing of common salivary gland carcinomas: subtype-restricted and shared genetic alterations. Clin. Cancer Res. 2021;27:3960–3969. doi: 10.1158/1078-0432.CCR-20-4071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Xie M, et al. Alterations of Notch pathway in patients with adenoid cystic carcinoma of the trachea and its impact on survival. Lung Cancer. 2018;121:41–47. doi: 10.1016/j.lungcan.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 420.Ferrarotto R, et al. A phase I dose-escalation and dose-expansion study of brontictuzumab in subjects with selected solid tumors. Ann. Oncol. 2018;29:1561–1568. doi: 10.1093/annonc/mdy171. [DOI] [PubMed] [Google Scholar]
- 421.Ferrarotto R, et al. Proteogenomic analysis of salivary adenoid cystic carcinomas defines molecular subtypes and identifies therapeutic targets. Clin. Cancer Res. 2021;27:852–864. doi: 10.1158/1078-0432.CCR-20-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Bhagat TD, et al. Notch pathway is activated via genetic and epigenetic alterations and is a therapeutic target in clear cell renal cancer. J. Biol. Chem. 2017;292:837–846. doi: 10.1074/jbc.M116.745208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Nowell CS, Radtke F. Notch as a tumour suppressor. Nat. Rev. Cancer. 2017;17:145–159. doi: 10.1038/nrc.2016.145. [DOI] [PubMed] [Google Scholar]
- 424.Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing But NET: a review of neuroendocrine tumors and carcinomas. Neoplasia. 2017;19:991–1002. doi: 10.1016/j.neo.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Hu J, et al. Comprehensive genomic profiling of small cell lung cancer in Chinese patients and the implications for therapeutic potential. Cancer Med. 2019;8:4338–4347. doi: 10.1002/cam4.2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Quintanal-Villalonga A, et al. Multi-omic analysis of lung tumors defines pathways activated in neuroendocrine transformation. Cancer Discov. 2021;11:3028–3047. doi: 10.1158/2159-8290.CD-20-1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Saunders LR, et al. A DLL3-targeted antibody-drug conjugate eradicates high-grade pulmonary neuroendocrine tumor-initiating cells in vivo. Sci. Transl. Med. 2015;7:302ra136. doi: 10.1126/scitranslmed.aac9459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Xie H, et al. Expression of delta-like protein 3 is reproducibly present in a subset of small cell lung carcinomas and pulmonary carcinoid tumors. Lung Cancer. 2019;135:73–79. doi: 10.1016/j.lungcan.2019.07.016. [DOI] [PubMed] [Google Scholar]
- 429.Gazdar AF, Bunn PA, Minna JD. Small-cell lung cancer: what we know, what we need to know and the path forward. Nat. Rev. Cancer. 2017;17:725–737. doi: 10.1038/nrc.2017.87. [DOI] [PubMed] [Google Scholar]
- 430.George J, et al. Comprehensive genomic profiles of small cell lung cancer. Nature. 2015;524:47–53. doi: 10.1038/nature14664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Kunnimalaiyaan M, Vaccaro AM, Ndiaye MA, Chen H. Overexpression of the NOTCH1 intracellular domain inhibits cell proliferation and alters the neuroendocrine phenotype of medullary thyroid cancer cells. J. Biol. Chem. 2006;281:39819–39830. doi: 10.1074/jbc.M603578200. [DOI] [PubMed] [Google Scholar]
- 432.Wang H, Chen Y, Fernandez-Del Castillo C, Yilmaz O, Deshpande V. Heterogeneity in signaling pathways of gastroenteropancreatic neuroendocrine tumors: a critical look at notch signaling pathway. Mod. Pathol. 2013;26:139–147. doi: 10.1038/modpathol.2012.143. [DOI] [PubMed] [Google Scholar]
- 433.Rekhtman N, et al. Next-generation sequencing of pulmonary large cell neuroendocrine carcinoma reveals small cell carcinoma-like and non-small cell carcinoma-like subsets. Clin. Cancer Res. 2016;22:3618–3629. doi: 10.1158/1078-0432.CCR-15-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Borromeo MD, et al. ASCL1 and NEUROD1 reveal heterogeneity in pulmonary neuroendocrine tumors and regulate distinct genetic programs. Cell Rep. 2016;16:1259–1272. doi: 10.1016/j.celrep.2016.06.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Meder L, et al. NOTCH, ASCL1, p53 and RB alterations define an alternative pathway driving neuroendocrine and small cell lung carcinomas. Int. J. Cancer. 2016;138:927–938. doi: 10.1002/ijc.29835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Wyche TP, et al. Thiocoraline activates the Notch pathway in carcinoids and reduces tumor progression in vivo. Cancer Gene Ther. 2014;21:518–525. doi: 10.1038/cgt.2014.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Ouadah Y, et al. Rare pulmonary neuroendocrine cells are stem cells regulated by Rb, p53, and Notch. Cell. 2019;179:403–416.e23. doi: 10.1016/j.cell.2019.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Stransky N, et al. The mutational landscape of head and neck squamous cell carcinoma. Science. 2011;333:1157–1160. doi: 10.1126/science.1208130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Natsuizaka M, et al. Interplay between Notch1 and Notch3 promotes EMT and tumor initiation in squamous cell carcinoma. Nat. Commun. 2017;8:1758. doi: 10.1038/s41467-017-01500-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Al Labban D, et al. Notch-effector CSL promotes squamous cell carcinoma by repressing histone demethylase KDM6B. J. Clin. Investig. 2018;128:2581–2599. doi: 10.1172/JCI96915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Agrawal N, et al. Exome sequencing of head and neck squamous cell carcinoma reveals inactivating mutations in NOTCH1. Science. 2011;333:1154–1157. doi: 10.1126/science.1206923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Fukusumi T, Califano JA. The NOTCH pathway in head and neck squamous cell carcinoma. J. Dent. Res. 2018;97:645–653. doi: 10.1177/0022034518760297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.South AP, et al. NOTCH1 mutations occur early during cutaneous squamous cell carcinogenesis. J. Invest. Dermatol. 2014;134:2630–2638. doi: 10.1038/jid.2014.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Wang NJ, et al. Loss-of-function mutations in Notch receptors in cutaneous and lung squamous cell carcinoma. Proc. Natl Acad. Sci. USA. 2011;108:17761–17766. doi: 10.1073/pnas.1114669108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Rampias T, et al. A new tumor suppressor role for the Notch pathway in bladder cancer. Nat. Med. 2014;20:1199–1205. doi: 10.1038/nm.3678. [DOI] [PubMed] [Google Scholar]
- 446.Gao YB, et al. Genetic landscape of esophageal squamous cell carcinoma. Nat. Genet. 2014;46:1097–1102. doi: 10.1038/ng.3076. [DOI] [PubMed] [Google Scholar]
- 447.Agrawal N, et al. Comparative genomic analysis of esophageal adenocarcinoma and squamous cell carcinoma. Cancer Discov. 2012;2:899–905. doi: 10.1158/2159-8290.CD-12-0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.Khelil M, et al. Delta-like ligand-Notch1 signaling is selectively modulated by HPV16 E6 to promote squamous cell proliferation and correlates with cervical cancer prognosis. Cancer Res. 2021;81:1909–1921. doi: 10.1158/0008-5472.CAN-20-1996. [DOI] [PubMed] [Google Scholar]
- 449.Nassar D, Latil M, Boeckx B, Lambrechts D, Blanpain C. Genomic landscape of carcinogen-induced and genetically induced mouse skin squamous cell carcinoma. Nat. Med. 2015;21:946–954. doi: 10.1038/nm.3878. [DOI] [PubMed] [Google Scholar]
- 450.Nicolas M, et al. Notch1 functions as a tumor suppressor in mouse skin. Nat. Genet. 2003;33:416–421. doi: 10.1038/ng1099. [DOI] [PubMed] [Google Scholar]
- 451.Proweller A, et al. Impaired notch signaling promotes de novo squamous cell carcinoma formation. Cancer Res. 2006;66:7438–7444. doi: 10.1158/0008-5472.CAN-06-0793. [DOI] [PubMed] [Google Scholar]
- 452.Extance A. Alzheimer’s failure raises questions about disease-modifying strategies. Nat. Rev. Drug Discov. 2010;9:749–751. doi: 10.1038/nrd3288. [DOI] [PubMed] [Google Scholar]
- 453.Quan XX, et al. Targeting Notch1 and IKKα enhanced NF-κB activation in CD133(+) skin cancer stem cells. Mol. Cancer Ther. 2018;17:2034–2048. doi: 10.1158/1535-7163.MCT-17-0421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Bailey P, et al. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature. 2016;531:47–52. doi: 10.1038/nature16965. [DOI] [PubMed] [Google Scholar]
- 455.Avila JL, Kissil JL. Notch signaling in pancreatic cancer: oncogene or tumor suppressor? Trends Mol. Med. 2013;19:320–327. doi: 10.1016/j.molmed.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Hanlon L, et al. Notch1 functions as a tumor suppressor in a model of K-ras-induced pancreatic ductal adenocarcinoma. Cancer Res. 2010;70:4280–4286. doi: 10.1158/0008-5472.CAN-09-4645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Plentz R, et al. Inhibition of gamma-secretase activity inhibits tumor progression in a mouse model of pancreatic ductal adenocarcinoma. Gastroenterology. 2009;136:1741–1749.e1746. doi: 10.1053/j.gastro.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Maniati E, et al. Crosstalk between the canonical NF-κB and Notch signaling pathways inhibits Pparγ expression and promotes pancreatic cancer progression in mice. J. Clin. Invest. 2011;121:4685–4699. doi: 10.1172/JCI45797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Cook N, et al. Gamma secretase inhibition promotes hypoxic necrosis in mouse pancreatic ductal adenocarcinoma. J. Exp. Med. 2012;209:437–444. doi: 10.1084/jem.20111923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Anderson NM, Simon MC. The tumor microenvironment. Curr. Biol. 2020;30:R921–r925. doi: 10.1016/j.cub.2020.06.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Bejarano L, Jordāo MJC, Joyce JA. Therapeutic targeting of the tumor microenvironment. Cancer Disco. 2021;11:933–959. doi: 10.1158/2159-8290.CD-20-1808. [DOI] [PubMed] [Google Scholar]
- 462.Meurette O, Mehlen P. Notch signaling in the tumor microenvironment. Cancer Cell. 2018;34:536–548. doi: 10.1016/j.ccell.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 463.Hinshaw DC, Shevde LA. The tumor microenvironment innately modulates cancer progression. Cancer Res. 2019;79:4557–4566. doi: 10.1158/0008-5472.CAN-18-3962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464.Tchekneva EE, et al. Determinant roles of dendritic cell-expressed Notch Delta-like and Jagged ligands on anti-tumor T cell immunity. J. Immunother. Cancer. 2019;7:95. doi: 10.1186/s40425-019-0566-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Wang L, et al. Notch-regulated dendritic cells restrain inflammation-associated colorectal carcinogenesis. Cancer Immunol. Res. 2021;9:348–361. doi: 10.1158/2326-6066.CIR-20-0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 466.Kirkling ME, et al. Notch signaling facilitates in vitro generation of cross-presenting classical dendritic cells. Cell Rep. 2018;23:3658–3672.e3656. doi: 10.1016/j.celrep.2018.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Balan S, et al. Large-scale human dendritic cell differentiation revealing notch-dependent lineage bifurcation and heterogeneity. Cell Rep. 2018;24:1902–1915.e1906. doi: 10.1016/j.celrep.2018.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Guilliams M, Scott CL. ‘NOTCHing up’ the in vitro production of dendritic cells. Trends Immunol. 2018;39:765–767. doi: 10.1016/j.it.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 469.Cho OH, et al. Notch regulates cytolytic effector function in CD8+ T cells. J. Immunol. 2009;182:3380–3389. doi: 10.4049/jimmunol.0802598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Maekawa Y, et al. Notch2 integrates signaling by the transcription factors RBP-J and CREB1 to promote T cell cytotoxicity. Nat. Immunol. 2008;9:1140–1147. doi: 10.1038/ni.1649. [DOI] [PubMed] [Google Scholar]
- 471.Backer RA, et al. A central role for Notch in effector CD8(+) T cell differentiation. Nat. Immunol. 2014;15:1143–1151. doi: 10.1038/ni.3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Kuijk LM, et al. Notch controls generation and function of human effector CD8+ T cells. Blood. 2013;121:2638–2646. doi: 10.1182/blood-2012-07-442962. [DOI] [PubMed] [Google Scholar]
- 473.Huang Y, et al. Resuscitating cancer immunosurveillance: selective stimulation of DLL1-Notch signaling in T cells rescues T-cell function and inhibits tumor growth. Cancer Res. 2011;71:6122–6131. doi: 10.1158/0008-5472.CAN-10-4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Sorrentino C, et al. Adenosine A2A receptor stimulation inhibits tcr-induced Notch1 activation in CD8+T-cells. Front. Immunol. 2019;10:162. doi: 10.3389/fimmu.2019.00162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Hombrink P, et al. Programs for the persistence, vigilance and control of human CD8(+) lung-resident memory T cells. Nat. Immunol. 2016;17:1467–1478. doi: 10.1038/ni.3589. [DOI] [PubMed] [Google Scholar]
- 476.Savas P, et al. Single-cell profiling of breast cancer T cells reveals a tissue-resident memory subset associated with improved prognosis. Nat. Med. 2018;24:986–993. doi: 10.1038/s41591-018-0078-7. [DOI] [PubMed] [Google Scholar]
- 477.Cho JW, et al. Dysregulation of T(FH)-B-T(RM) lymphocyte cooperation is associated with unfavorable anti-PD-1 responses in EGFR-mutant lung cancer. Nat. Commun. 2021;12:6068. doi: 10.1038/s41467-021-26362-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Mami-Chouaib F, et al. Resident memory T cells, critical components in tumor immunology. J. Immunother. Cancer. 2018;6:87. doi: 10.1186/s40425-018-0399-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 479.Mathieu M, Cotta-Grand N, Daudelin JF, Thébault P, Labrecque N. Notch signaling regulates PD-1 expression during CD8(+) T-cell activation. Immunol. Cell Biol. 2013;91:82–88. doi: 10.1038/icb.2012.53. [DOI] [PubMed] [Google Scholar]
- 480.Yu W, Wang Y, Guo P. Notch signaling pathway dampens tumor-infiltrating CD8(+) T cells activity in patients with colorectal carcinoma. Biomed. Pharmacother. 2018;97:535–542. doi: 10.1016/j.biopha.2017.10.143. [DOI] [PubMed] [Google Scholar]
- 481.Choe, J. H. et al. SynNotch-CAR T cells overcome challenges of specificity, heterogeneity, and persistence in treating glioblastoma. Sci. Transl. Med.13, eabe7378 (2021). [DOI] [PMC free article] [PubMed]
- 482.Roybal KT, et al. Precision tumor recognition by T cells with combinatorial antigen-sensing circuits. Cell. 2016;164:770–779. doi: 10.1016/j.cell.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 483.Yu S, Yi M, Qin S, Wu K. Next generation chimeric antigen receptor T cells: safety strategies to overcome toxicity. Mol. Cancer. 2019;18:125. doi: 10.1186/s12943-019-1057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 484.Hyrenius-Wittsten, A. et al. SynNotch CAR circuits enhance solid tumor recognition and promote persistent antitumor activity in mouse models. Sci. Transl. Med.13, eabd8836 (2021). [DOI] [PMC free article] [PubMed]
- 485.Amsen D, Antov A, Flavell RA. The different faces of Notch in T-helper-cell differentiation. Nat. Rev. Immunol. 2009;9:116–124. doi: 10.1038/nri2488. [DOI] [PubMed] [Google Scholar]
- 486.Kared H, et al. Jagged2-expressing hematopoietic progenitors promote regulatory T cell expansion in the periphery through notch signaling. Immunity. 2006;25:823–834. doi: 10.1016/j.immuni.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 487.Cahill EF, Tobin LM, Carty F, Mahon BP, English K. Jagged-1 is required for the expansion of CD4+ CD25+ FoxP3+ regulatory T cells and tolerogenic dendritic cells by murine mesenchymal stromal cells. Stem Cell Res. Ther. 2015;6:19. doi: 10.1186/s13287-015-0021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 488.Samon JB, et al. Notch1 and TGFbeta1 cooperatively regulate Foxp3 expression and the maintenance of peripheral regulatory T cells. Blood. 2008;112:1813–1821. doi: 10.1182/blood-2008-03-144980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Charbonnier LM, Wang S, Georgiev P, Sefik E, Chatila TA. Control of peripheral tolerance by regulatory T cell-intrinsic Notch signaling. Nat. Immunol. 2015;16:1162–1173. doi: 10.1038/ni.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 490.Zakiryanova GK, et al. Notch signaling defects in NK cells in patients with cancer. Cancer Immunol. Immunother. 2021;70:981–988. doi: 10.1007/s00262-020-02763-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 491.Franklin RA, et al. The cellular and molecular origin of tumor-associated macrophages. Science. 2014;344:921–925. doi: 10.1126/science.1252510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 492.Ye YC, et al. NOTCH Signaling via WNT regulates the proliferation of alternative, CCR2-independent tumor-associated macrophages in hepatocellular carcinoma. Cancer Res. 2019;79:4160–4172. doi: 10.1158/0008-5472.CAN-18-1691. [DOI] [PubMed] [Google Scholar]
- 493.Liu H, et al. Jagged1 promotes aromatase inhibitor resistance by modulating tumor-associated macrophage differentiation in breast cancer patients. Breast Cancer Res. Treat. 2017;166:95–107. doi: 10.1007/s10549-017-4394-2. [DOI] [PubMed] [Google Scholar]
- 494.Palaga T, et al. Notch signaling is activated by TLR stimulation and regulates macrophage functions. Eur. J. Immunol. 2008;38:174–183. doi: 10.1002/eji.200636999. [DOI] [PubMed] [Google Scholar]
- 495.Boonyatecha N, Sangphech N, Wongchana W, Kueanjinda P, Palaga T. Involvement of Notch signaling pathway in regulating IL-12 expression via c-Rel in activated macrophages. Mol. Immunol. 2012;51:255–262. doi: 10.1016/j.molimm.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 496.Wang YC, et al. Notch signaling determines the M1 versus M2 polarization of macrophages in antitumor immune responses. Cancer Res. 2010;70:4840–4849. doi: 10.1158/0008-5472.CAN-10-0269. [DOI] [PubMed] [Google Scholar]
- 497.Zhao JL, et al. Forced activation of notch in macrophages represses tumor growth by upregulating miR-125a and disabling tumor-associated macrophages. Cancer Res. 2016;76:1403–1415. doi: 10.1158/0008-5472.CAN-15-2019. [DOI] [PubMed] [Google Scholar]
- 498.Saleem SJ, Conrad DH. Hematopoietic cytokine-induced transcriptional regulation and Notch signaling as modulators of MDSC expansion. Int Immunopharmacol. 2011;11:808–815. doi: 10.1016/j.intimp.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 499.Wang SH, et al. The blockage of Notch signalling promoted the generation of polymorphonuclear myeloid-derived suppressor cells with lower immunosuppression. Eur. J. Cancer. 2016;68:90–105. doi: 10.1016/j.ejca.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 500.Jiang H, et al. Reduction of myeloid derived suppressor cells by inhibiting Notch pathway prevents the progression of endometriosis in mice model. Int. Immunopharmacol. 2020;82:106352. doi: 10.1016/j.intimp.2020.106352. [DOI] [PubMed] [Google Scholar]
- 501.Yang Z, et al. Notch1 signaling in melanoma cells promoted tumor-induced immunosuppression via upregulation of TGF-β1. J. Exp. Clin. Cancer Res. 2018;37:1. doi: 10.1186/s13046-017-0664-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 502.Sierra RA, et al. Anti-jagged immunotherapy inhibits MDSCs and overcomes tumor-induced tolerance. Cancer Res. 2017;77:5628–5638. doi: 10.1158/0008-5472.CAN-17-0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 503.Caiado F, et al. Bone marrow-derived CD11b+Jagged2+ cells promote epithelial-to-mesenchymal transition and metastasization in colorectal cancer. Cancer Res. 2013;73:4233–4246. doi: 10.1158/0008-5472.CAN-13-0085. [DOI] [PubMed] [Google Scholar]
- 504.Sprouse, M. L. et al. PMN-MDSCs enhance CTC metastatic properties through reciprocal interactions via ROS/notch/nodal signaling. Int. J. Mol. Sci.20, (2019). [DOI] [PMC free article] [PubMed]
- 505.Peng D, et al. Myeloid-derived suppressor cells endow stem-like qualities to breast cancer cells through IL6/STAT3 and NO/NOTCH cross-talk signaling. Cancer Res. 2016;76:3156–3165. doi: 10.1158/0008-5472.CAN-15-2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 506.Welte T, et al. Oncogenic mTOR signalling recruits myeloid-derived suppressor cells to promote tumour initiation. Nat. Cell Biol. 2016;18:632–644. doi: 10.1038/ncb3355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 507.Yang M, et al. Tumour-associated neutrophils orchestrate intratumoural IL-8-driven immune evasion through Jagged2 activation in ovarian cancer. Br. J. Cancer. 2020;123:1404–1416. doi: 10.1038/s41416-020-1026-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 508.Hu B, et al. Multifocal epithelial tumors and field cancerization from loss of mesenchymal CSL signaling. Cell. 2012;149:1207–1220. doi: 10.1016/j.cell.2012.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 509.Procopio MG, et al. Combined CSL and p53 downregulation promotes cancer-associated fibroblast activation. Nat. Cell Biol. 2015;17:1193–1204. doi: 10.1038/ncb3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 510.Demehri S, Turkoz A, Kopan R. Epidermal Notch1 loss promotes skin tumorigenesis by impacting the stromal microenvironment. Cancer Cell. 2009;16:55–66. doi: 10.1016/j.ccr.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Peng Y, et al. Direct contacts with colon cancer cells regulate the differentiation of bone marrow mesenchymal stem cells into tumor associated fibroblasts. Biochem. Biophys. Res. Commun. 2014;451:68–73. doi: 10.1016/j.bbrc.2014.07.074. [DOI] [PubMed] [Google Scholar]
- 512.Su Q, et al. Jagged1 upregulation in prostate epithelial cells promotes formation of reactive stroma in the Pten null mouse model for prostate cancer. Oncogene. 2017;36:618–627. doi: 10.1038/onc.2016.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 513.Tsuyada A, et al. CCL2 mediates cross-talk between cancer cells and stromal fibroblasts that regulates breast cancer stem cells. Cancer Res. 2012;72:2768–2779. doi: 10.1158/0008-5472.CAN-11-3567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 514.Liu C, et al. LSD1 stimulates cancer-associated fibroblasts to drive Notch3-dependent self-renewal of liver cancer stem-like cells. Cancer Res. 2018;78:938–949. doi: 10.1158/0008-5472.CAN-17-1236. [DOI] [PubMed] [Google Scholar]
- 515.Du Y, et al. Intracellular Notch1 signaling in cancer-associated fibroblasts dictates the plasticity and stemness of melanoma stem/initiating cells. Stem Cells. 2019;37:865–875. doi: 10.1002/stem.3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 516.Boelens MC, et al. Exosome transfer from stromal to breast cancer cells regulates therapy resistance pathways. Cell. 2014;159:499–513. doi: 10.1016/j.cell.2014.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 517.Pelon F, et al. Cancer-associated fibroblast heterogeneity in axillary lymph nodes drives metastases in breast cancer through complementary mechanisms. Nat. Commun. 2020;11:404. doi: 10.1038/s41467-019-14134-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 518.Liubomirski Y, et al. Notch-mediated tumor-stroma-inflammation networks promote invasive properties and CXCL8 expression in triple-negative breast cancer. Front Immunol. 2019;10:804. doi: 10.3389/fimmu.2019.00804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Strell C, et al. Impact of epithelial-stromal interactions on peritumoral fibroblasts in ductal carcinoma in situ. J. Natl Cancer Inst. 2019;111:983–995. doi: 10.1093/jnci/djy234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 520.Gong J, et al. Increased expression of Fibulin-1 is associated with hepatocellular carcinoma progression by regulating the notch signaling pathway. Front Cell Dev. Biol. 2020;8:478. doi: 10.3389/fcell.2020.00478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 521.Nandhu MS, et al. Development of a function-blocking antibody against Fibulin-3 as a targeted reagent for glioblastoma. Clin. Cancer Res. 2018;24:821–833. doi: 10.1158/1078-0432.CCR-17-1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 522.Donovan LJ, Cha SE, Yale AR, Dreikorn S, Miyamoto A. Identification of a functional proprotein convertase cleavage site in microfibril-associated glycoprotein 2. Matrix Biol. 2013;32:117–122. doi: 10.1016/j.matbio.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 523.Gordon-Weeks, A. et al. Tumour-derived laminin α5 (LAMA5) promotes colorectal liver metastasis growth, branching angiogenesis and notch pathway inhibition. Cancers (Basel)11, 630 (2019). [DOI] [PMC free article] [PubMed]
- 524.Ogawa K, et al. Prometastatic secretome trafficking via exosomes initiates pancreatic cancer pulmonary metastasis. Cancer Lett. 2020;481:63–75. doi: 10.1016/j.canlet.2020.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 525.Kuhnert F, et al. Dll4 blockade in stromal cells mediates antitumor effects in preclinical models of ovarian cancer. Cancer Res. 2015;75:4086–4096. doi: 10.1158/0008-5472.CAN-14-3773. [DOI] [PubMed] [Google Scholar]
- 526.Xu Z, et al. MMGZ01, an anti-DLL4 monoclonal antibody, promotes nonfunctional vessels and inhibits breast tumor growth. Cancer Lett. 2016;372:118–127. doi: 10.1016/j.canlet.2015.12.025. [DOI] [PubMed] [Google Scholar]
- 527.Funahashi Y, et al. A notch1 ectodomain construct inhibits endothelial notch signaling, tumor growth, and angiogenesis. Cancer Res. 2008;68:4727–4735. doi: 10.1158/0008-5472.CAN-07-6499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 528.Boareto M, Jolly MK, Ben-Jacob E, Onuchic JN. Jagged mediates differences in normal and tumor angiogenesis by affecting tip-stalk fate decision. Proc. Natl Acad. Sci. USA. 2015;112:E3836–3844. doi: 10.1073/pnas.1511814112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 529.Banerjee D, et al. Notch suppresses angiogenesis and progression of hepatic metastases. Cancer Res. 2015;75:1592–1602. doi: 10.1158/0008-5472.CAN-14-1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 530.Banerjee D, et al. High-dose radiation increases Notch1 in tumor vasculature. Int J. Radiat. Oncol. Biol. Phys. 2020;106:857–866. doi: 10.1016/j.ijrobp.2019.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 531.Periz G, Fortini ME. Ca(2+)-ATPase function is required for intracellular trafficking of the Notch receptor in Drosophila. EMBO J. 1999;18:5983–5993. doi: 10.1093/emboj/18.21.5983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 532.Pagliaro L, Marchesini M, Roti G. Targeting oncogenic Notch signaling with SERCA inhibitors. J. Hematol. Oncol. 2021;14:8. doi: 10.1186/s13045-020-01015-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 533.Malecki MJ, et al. Leukemia-associated mutations within the NOTCH1 heterodimerization domain fall into at least two distinct mechanistic classes. Mol. Cell Biol. 2006;26:4642–4651. doi: 10.1128/MCB.01655-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 534.Roti G, et al. Complementary genomic screens identify SERCA as a therapeutic target in NOTCH1 mutated cancer. Cancer Cell. 2013;23:390–405. doi: 10.1016/j.ccr.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 535.Roti G, et al. Leukemia-specific delivery of mutant NOTCH1 targeted therapy. J. Exp. Med. 2018;215:197–216. doi: 10.1084/jem.20151778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 536.Treiman M, Caspersen C, Christensen SB. A tool coming of age: thapsigargin as an inhibitor of sarco-endoplasmic reticulum Ca(2+)-ATPases. Trends Pharm. Sci. 1998;19:131–135. doi: 10.1016/s0165-6147(98)01184-5. [DOI] [PubMed] [Google Scholar]
- 537.Jackisch C, et al. Delayed micromolar elevation in intracellular calcium precedes induction of apoptosis in thapsigargin-treated breast cancer cells. Clin. Cancer Res. 2000;6:2844–2850. [PubMed] [Google Scholar]
- 538.Marchesini M, et al. Blockade of oncogenic NOTCH1 with the SERCA inhibitor CAD204520 in T cell acute lymphoblastic leukemia. Cell Chem. Biol. 2020;27:678–697.e613. doi: 10.1016/j.chembiol.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 539.Mumm JS, et al. A ligand-induced extracellular cleavage regulates gamma-secretase-like proteolytic activation of Notch1. Mol. Cell. 2000;5:197–206. doi: 10.1016/s1097-2765(00)80416-5. [DOI] [PubMed] [Google Scholar]
- 540.Cousin H, Abbruzzese G, Kerdavid E, Gaultier A, Alfandari D. Translocation of the cytoplasmic domain of ADAM13 to the nucleus is essential for Calpain8-a expression and cranial neural crest cell migration. Dev. Cell. 2011;20:256–263. doi: 10.1016/j.devcel.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 541.Saha N, Robev D, Himanen JP, Nikolov DB. ADAM proteases: emerging role and targeting of the non-catalytic domains. Cancer Lett. 2019;467:50–57. doi: 10.1016/j.canlet.2019.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 542.Murthy A, et al. Notch activation by the metalloproteinase ADAM17 regulates myeloproliferation and atopic barrier immunity by suppressing epithelial cytokine synthesis. Immunity. 2012;36:105–119. doi: 10.1016/j.immuni.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 543.Edwards DR, Handsley MM, Pennington CJ. The ADAM metalloproteinases. Mol. Asp. Med. 2008;29:258–289. doi: 10.1016/j.mam.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 544.Lu HY, et al. Novel ADAM-17 inhibitor ZLDI-8 inhibits the proliferation and metastasis of chemo-resistant non-small-cell lung cancer by reversing Notch and epithelial mesenchymal transition in vitro and in vivo. Pharm. Res. 2019;148:104406. doi: 10.1016/j.phrs.2019.104406. [DOI] [PubMed] [Google Scholar]
- 545.Yang B, et al. MicroRNA-3163 targets ADAM-17 and enhances the sensitivity of hepatocellular carcinoma cells to molecular targeted agents. Cell Death Dis. 2019;10:784. doi: 10.1038/s41419-019-2023-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 546.Guo Z, Jin X, Jia H. Inhibition of ADAM-17 more effectively down-regulates the Notch pathway than that of γ-secretase in renal carcinoma. J. Exp. Clin. Cancer Res. 2013;32:26. doi: 10.1186/1756-9966-32-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 547.Mullooly M, et al. ADAM10: a new player in breast cancer progression? Br. J. Cancer. 2015;113:945–951. doi: 10.1038/bjc.2015.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 548.Kavian N, et al. Targeting ADAM-17/notch signaling abrogates the development of systemic sclerosis in a murine model. Arthritis Rheum. 2010;62:3477–3487. doi: 10.1002/art.27626. [DOI] [PubMed] [Google Scholar]
- 549.Fortini ME. Gamma-secretase-mediated proteolysis in cell-surface-receptor signalling. Nat. Rev. Mol. Cell Biol. 2002;3:673–684. doi: 10.1038/nrm910. [DOI] [PubMed] [Google Scholar]
- 550.Mumm JS, Kopan R. Notch signaling: from the outside. Dev. Biol. 2000;228:151–165. doi: 10.1006/dbio.2000.9960. [DOI] [PubMed] [Google Scholar]
- 551.Doody RS, et al. A phase 3 trial of semagacestat for treatment of Alzheimer’s disease. N. Engl. J. Med. 2013;369:341–350. doi: 10.1056/NEJMoa1210951. [DOI] [PubMed] [Google Scholar]
- 552.Das A, et al. A novel triazole, NMK-T-057, induces autophagic cell death in breast cancer cells by inhibiting γ-secretase-mediated activation of Notch signaling. J. Biol. Chem. 2019;294:6733–6750. doi: 10.1074/jbc.RA119.007671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 553.Sardesai S, et al. A phase I study of an oral selective gamma secretase (GS) inhibitor RO4929097 in combination with neoadjuvant paclitaxel and carboplatin in triple negative breast cancer. Invest N. Drugs. 2020;38:1400–1410. doi: 10.1007/s10637-020-00895-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 554.Han B, et al. Notch1 downregulation combined with interleukin-24 inhibits invasion and migration of hepatocellular carcinoma cells. World J. Gastroenterol. 2015;21:9727–9735. doi: 10.3748/wjg.v21.i33.9727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 555.Yong YL, et al. Gamma-secretase complex-dependent intramembrane proteolysis of CD147 regulates the Notch1 signaling pathway in hepatocellular carcinoma. J. Pathol. 2019;249:255–267. doi: 10.1002/path.5316. [DOI] [PubMed] [Google Scholar]
- 556.Pine SR. Rethinking gamma-secretase inhibitors for treatment of non-small-cell lung cancer: is notch the target? Clin. Cancer Res. 2018;24:6136–6141. doi: 10.1158/1078-0432.CCR-18-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 557.Akiyoshi T, et al. Gamma-secretase inhibitors enhance taxane-induced mitotic arrest and apoptosis in colon cancer cells. Gastroenterology. 2008;134:131–144. doi: 10.1053/j.gastro.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 558.Cui D, et al. Notch pathway inhibition using PF-03084014, a γ-secretase inhibitor (GSI), enhances the antitumor effect of docetaxel in prostate cancer. Clin. Cancer Res. 2015;21:4619–4629. doi: 10.1158/1078-0432.CCR-15-0242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 559.Gilbert CA, Daou MC, Moser RP, Ross AH. Gamma-secretase inhibitors enhance temozolomide treatment of human gliomas by inhibiting neurosphere repopulation and xenograft recurrence. Cancer Res. 2010;70:6870–6879. doi: 10.1158/0008-5472.CAN-10-1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 560.Messersmith WA, et al. A Phase I, dose-finding study in patients with advanced solid malignancies of the oral γ-secretase inhibitor PF-03084014. Clin. Cancer Res. 2015;21:60–67. doi: 10.1158/1078-0432.CCR-14-0607. [DOI] [PubMed] [Google Scholar]
- 561.Tolcher AW, et al. Phase I study of RO4929097, a gamma secretase inhibitor of Notch signaling, in patients with refractory metastatic or locally advanced solid tumors. J. Clin. Oncol. 2012;30:2348–2353. doi: 10.1200/JCO.2011.36.8282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 562.Xu R, et al. Molecular and clinical effects of notch inhibition in glioma patients: a phase 0/i trial. Clin. Cancer Res. 2016;22:4786–4796. doi: 10.1158/1078-0432.CCR-16-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 563.Aung KL, et al. A multi-arm phase I dose escalating study of an oral NOTCH inhibitor BMS-986115 in patients with advanced solid tumours. Invest N. Drugs. 2018;36:1026–1036. doi: 10.1007/s10637-018-0597-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 564.Pant S, et al. A first-in-human phase I study of the oral Notch inhibitor, LY900009, in patients with advanced cancer. Eur. J. Cancer. 2016;56:1–9. doi: 10.1016/j.ejca.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 565.Massard C, et al. First-in-human study of LY3039478, an oral Notch signaling inhibitor in advanced or metastatic cancer. Ann. Oncol. 2018;29:1911–1917. doi: 10.1093/annonc/mdy244. [DOI] [PubMed] [Google Scholar]
- 566.Fouladi M, et al. Phase I trial of MK-0752 in children with refractory CNS malignancies: a pediatric brain tumor consortium study. J. Clin. Oncol. 2011;29:3529–3534. doi: 10.1200/JCO.2011.35.7806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 567.Cook N, et al. A phase I trial of the γ-secretase inhibitor MK-0752 in combination with gemcitabine in patients with pancreatic ductal adenocarcinoma. Br. J. Cancer. 2018;118:793–801. doi: 10.1038/bjc.2017.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 568.Lee SM, et al. Phase 2 study of RO4929097, a gamma-secretase inhibitor, in metastatic melanoma: SWOG 0933. Cancer. 2015;121:432–440. doi: 10.1002/cncr.29055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 569.Diaz-Padilla I, et al. A phase II study of single-agent RO4929097, a gamma-secretase inhibitor of Notch signaling, in patients with recurrent platinum-resistant epithelial ovarian cancer: a study of the Princess Margaret, Chicago and California phase II consortia. Gynecol. Oncol. 2015;137:216–222. doi: 10.1016/j.ygyno.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 570.Strosberg, J. R. et al. A phase II study of RO4929097 in metastatic colorectal cancer. Eur. J. Cancer48, 997–1003 (2012). [DOI] [PMC free article] [PubMed]
- 571.Kummar S, et al. Clinical activity of the γ-secretase inhibitor PF-03084014 in adults with desmoid tumors (aggressive fibromatosis) J. Clin. Oncol. 2017;35:1561–1569. doi: 10.1200/JCO.2016.71.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 572.Kang JH, et al. Gamma-secretase inhibitor reduces allergic pulmonary inflammation by modulating Th1 and Th2 responses. Am. J. Respir. Crit. Care Med. 2009;179:875–882. doi: 10.1164/rccm.200806-893OC. [DOI] [PubMed] [Google Scholar]
- 573.Kukar TL, et al. Substrate-targeting gamma-secretase modulators. Nature. 2008;453:925–929. doi: 10.1038/nature07055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 574.Golde TE, Koo EH, Felsenstein KM, Osborne BA, Miele L. γ-Secretase inhibitors and modulators. Biochim. Biophys. Acta. 2013;1828:2898–2907. doi: 10.1016/j.bbamem.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 575.Habets, R. A. et al. Safe targeting of T cell acute lymphoblastic leukemia by pathology-specific NOTCH inhibition. Sci. Transl. Med.11, eaau6246 (2019). [DOI] [PubMed]
- 576.Zhang S, et al. A presenilin-1 mutation causes Alzheimer disease without affecting Notch signaling. Mol. Psychiatry. 2020;25:603–613. doi: 10.1038/s41380-018-0101-x. [DOI] [PubMed] [Google Scholar]
- 577.Soares HD, et al. The γ-secretase modulator, BMS-932481, modulates Aβ peptides in the plasma and cerebrospinal fluid of healthy volunteers. J. Pharm. Exp. Ther. 2016;358:138–150. doi: 10.1124/jpet.116.232256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 578.Murciano-Goroff YR, Taylor BS, Hyman DM, Schram AM. Toward a more precise future for oncology. Cancer Cell. 2020;37:431–442. doi: 10.1016/j.ccell.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 579.Hann CL, et al. A phase 1 study evaluating rovalpituzumab tesirine in frontline treatment of patients with extensive-stage SCLC. J. Thorac. Oncol. 2021;16:1582–1588. doi: 10.1016/j.jtho.2021.06.022. [DOI] [PubMed] [Google Scholar]
- 580.Simon DP, Giordano TJ, Hammer GD. Upregulated JAG1 enhances cell proliferation in adrenocortical carcinoma. Clin. Cancer Res. 2012;18:2452–2464. doi: 10.1158/1078-0432.CCR-11-2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 581.Santagata S, et al. JAGGED1 expression is associated with prostate cancer metastasis and recurrence. Cancer Res. 2004;64:6854–6857. doi: 10.1158/0008-5472.CAN-04-2500. [DOI] [PubMed] [Google Scholar]
- 582.Masiero M, et al. Development of therapeutic anti-JAGGED1 antibodies for cancer therapy. Mol. Cancer Ther. 2019;18:2030–2042. doi: 10.1158/1535-7163.MCT-18-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 583.Zheng H, et al. Therapeutic antibody targeting tumor- and osteoblastic niche-derived Jagged1 sensitizes bone metastasis to chemotherapy. Cancer Cell. 2017;32:731–747.e736. doi: 10.1016/j.ccell.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 584.Sabari JK, Lok BH, Laird JH, Poirier JT, Rudin CM. Unravelling the biology of SCLC: implications for therapy. Nat. Rev. Clin. Oncol. 2017;14:549–561. doi: 10.1038/nrclinonc.2017.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 585.Puca, L. et al. Delta-like protein 3 expression and therapeutic targeting in neuroendocrine prostate cancer. Sci. Transl. Med.11, eaav0891 (2019). [DOI] [PMC free article] [PubMed]
- 586.Morgensztern D, et al. Efficacy and safety of rovalpituzumab tesirine in third-line and beyond patients with DLL3-expressing, relapsed/refractory small-cell lung cancer: results from the phase II TRINITY study. Clin. Cancer Res. 2019;25:6958–6966. doi: 10.1158/1078-0432.CCR-19-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 587.Johnson ML, et al. Rovalpituzumab tesirine as a maintenance therapy after first-line platinum-based chemotherapy in patients with extensive-stage-SCLC: results from the phase 3 MERU study. J. Thorac. Oncol. 2021;16:1570–1581. doi: 10.1016/j.jtho.2021.03.012. [DOI] [PubMed] [Google Scholar]
- 588.Blackhall F, et al. Efficacy and safety of rovalpituzumab tesirine compared with topotecan as second-line therapy in DLL3-High SCLC: results from the phase 3 TAHOE study. J. Thorac. Oncol. 2021;16:1547–1558. doi: 10.1016/j.jtho.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 589.Malhotra J, et al. A phase 1-2 study of rovalpituzumab tesirine in combination with nivolumab plus or minus ipilimumab in patients with previously treated extensive-stage SCLC. J. Thorac. Oncol. 2021;16:1559–1569. doi: 10.1016/j.jtho.2021.02.022. [DOI] [PubMed] [Google Scholar]
- 590.Spino M, et al. Cell surface Notch ligand DLL3 is a therapeutic target in isocitrate dehydrogenase-mutant glioma. Clin. Cancer Res. 2019;25:1261–1271. doi: 10.1158/1078-0432.CCR-18-2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 591.Morgensztern D, et al. SC-002 in patients with relapsed or refractory small cell lung cancer and large cell neuroendocrine carcinoma: Phase 1 study. Lung Cancer. 2020;145:126–131. doi: 10.1016/j.lungcan.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 592.Ridgway J, et al. Inhibition of Dll4 signalling inhibits tumour growth by deregulating angiogenesis. Nature. 2006;444:1083–1087. doi: 10.1038/nature05313. [DOI] [PubMed] [Google Scholar]
- 593.Liu SK, et al. Delta-like ligand 4-notch blockade and tumor radiation response. J. Natl Cancer Inst. 2011;103:1778–1798. doi: 10.1093/jnci/djr419. [DOI] [PubMed] [Google Scholar]
- 594.Chiorean EG, et al. A phase i first-in-human study of enoticumab (REGN421), a fully human delta-like ligand 4 (Dll4) monoclonal antibody in patients with advanced solid tumors. Clin. Cancer Res. 2015;21:2695–2703. doi: 10.1158/1078-0432.CCR-14-2797. [DOI] [PubMed] [Google Scholar]
- 595.Smith DC, et al. A phase I dose escalation and expansion study of the anticancer stem cell agent demcizumab (anti-DLL4) in patients with previously treated solid tumors. Clin. Cancer Res. 2014;20:6295–6303. doi: 10.1158/1078-0432.CCR-14-1373. [DOI] [PubMed] [Google Scholar]
- 596.Coleman RL, et al. Demcizumab combined with paclitaxel for platinum-resistant ovarian, primary peritoneal, and fallopian tube cancer: The SIERRA open-label phase Ib trial. Gynecol. Oncol. 2020;157:386–391. doi: 10.1016/j.ygyno.2020.01.042. [DOI] [PubMed] [Google Scholar]
- 597.Li Y, et al. ABT-165, a dual variable domain immunoglobulin (DVD-Ig) targeting DLL4 and VEGF, demonstrates superior efficacy and favorable safety profiles in preclinical models. Mol. Cancer Ther. 2018;17:1039–1050. doi: 10.1158/1535-7163.MCT-17-0800. [DOI] [PubMed] [Google Scholar]
- 598.Jimeno A, et al. A first-in-human phase 1a study of the bispecific anti-DLL4/anti-VEGF antibody navicixizumab (OMP-305B83) in patients with previously treated solid tumors. Invest N. Drugs. 2019;37:461–472. doi: 10.1007/s10637-018-0665-y. [DOI] [PubMed] [Google Scholar]
- 599.Long J, et al. JAG2/Notch2 inhibits intervertebral disc degeneration by modulating cell proliferation, apoptosis, and extracellular matrix. Arthritis Res. Ther. 2019;21:213. doi: 10.1186/s13075-019-1990-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 600.Guo P, et al. Endothelial jagged-2 sustains hematopoietic stem and progenitor reconstitution after myelosuppression. J. Clin. Invest. 2017;127:4242–4256. doi: 10.1172/JCI92309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 601.Yang Y, et al. The Notch ligand Jagged2 promotes lung adenocarcinoma metastasis through a miR-200-dependent pathway in mice. J. Clin. Invest. 2011;121:1373–1385. doi: 10.1172/JCI42579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 602.Chen YT, et al. Jagged2 progressively increased expression from Stage I to III of Bladder Cancer and Melatonin-mediated downregulation of Notch/Jagged2 suppresses the Bladder Tumorigenesis via inhibiting PI3K/AKT/mTOR/MMPs signaling. Int J. Biol. Sci. 2020;16:2648–2662. doi: 10.7150/ijbs.48358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 603.Santos MA, et al. Notch1 engagement by Delta-like-1 promotes differentiation of B lymphocytes to antibody-secreting cells. Proc. Natl Acad. Sci. USA. 2007;104:15454–15459. doi: 10.1073/pnas.0702891104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 604.Grabher C, von Boehmer H, Look AT. Notch 1 activation in the molecular pathogenesis of T-cell acute lymphoblastic leukaemia. Nat. Rev. Cancer. 2006;6:347–359. doi: 10.1038/nrc1880. [DOI] [PubMed] [Google Scholar]
- 605.Liao W, et al. Antitumor activity of Notch‑1 inhibition in human colorectal carcinoma cells. Oncol. Rep. 2018;39:1063–1071. doi: 10.3892/or.2017.6176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 606.Purow BW, et al. Expression of Notch-1 and its ligands, Delta-like-1 and Jagged-1, is critical for glioma cell survival and proliferation. Cancer Res. 2005;65:2353–2363. doi: 10.1158/0008-5472.CAN-04-1890. [DOI] [PubMed] [Google Scholar]
- 607.Ferrarotto R, et al. Activating NOTCH1 mutations define a distinct subgroup of patients with adenoid cystic carcinoma who have poor prognosis, propensity to bone and liver metastasis, and potential responsiveness to Notch1 inhibitors. J. Clin. Oncol. 2017;35:352–360. doi: 10.1200/JCO.2016.67.5264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 608.Choi BY, et al. Inhibition of Notch1 induces population and suppressive activity of regulatory T cell in inflammatory arthritis. Theranostics. 2018;8:4795–4804. doi: 10.7150/thno.26093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 609.Magee CN, et al. Notch-1 inhibition promotes immune regulation in transplantation via regulatory T cell-dependent mechanisms. Circulation. 2019;140:846–863. doi: 10.1161/CIRCULATIONAHA.119.040563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 610.Lee SY, et al. Gain-of-function mutations and copy number increases of Notch2 in diffuse large B-cell lymphoma. Cancer Sci. 2009;100:920–926. doi: 10.1111/j.1349-7006.2009.01130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 611.Mazur PK, et al. Notch2 is required for progression of pancreatic intraepithelial neoplasia and development of pancreatic ductal adenocarcinoma. Proc. Natl Acad. Sci. USA. 2010;107:13438–13443. doi: 10.1073/pnas.1002423107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 612.Massi D, et al. Evidence for differential expression of Notch receptors and their ligands in melanocytic nevi and cutaneous malignant melanoma. Mod. Pathol. 2006;19:246–254. doi: 10.1038/modpathol.3800526. [DOI] [PubMed] [Google Scholar]
- 613.Lin L, et al. Targeting specific regions of the Notch3 ligand-binding domain induces apoptosis and inhibits tumor growth in lung cancer. Cancer Res. 2010;70:632–638. doi: 10.1158/0008-5472.CAN-09-3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 614.Yamaguchi N, et al. NOTCH3 signaling pathway plays crucial roles in the proliferation of ErbB2-negative human breast cancer cells. Cancer Res. 2008;68:1881–1888. doi: 10.1158/0008-5472.CAN-07-1597. [DOI] [PubMed] [Google Scholar]
- 615.Hu ZI, et al. A randomized phase II trial of nab-paclitaxel and gemcitabine with tarextumab or placebo in patients with untreated metastatic pancreatic cancer. Cancer Med. 2019;8:5148–5157. doi: 10.1002/cam4.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 616.Smith DC, et al. A phase 1 dose escalation and expansion study of Tarextumab (OMP-59R5) in patients with solid tumors. Invest N. Drugs. 2019;37:722–730. doi: 10.1007/s10637-018-0714-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 617.Rosen LS, et al. A phase I, dose-escalation study of PF-06650808, an anti-Notch3 antibody-drug conjugate, in patients with breast cancer and other advanced solid tumors. Invest N. Drugs. 2020;38:120–130. doi: 10.1007/s10637-019-00754-y. [DOI] [PubMed] [Google Scholar]
- 618.Harrison H, et al. Regulation of breast cancer stem cell activity by signaling through the Notch4 receptor. Cancer Res. 2010;70:709–718. doi: 10.1158/0008-5472.CAN-09-1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 619.Xiu M, et al. Targeting Notch4 in cancer: molecular mechanisms and therapeutic perspectives. Cancer Manag. Res. 2021;13:7033–7045. doi: 10.2147/CMAR.S315511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 620.Nam Y, Sliz P, Song L, Aster JC, Blacklow SC. Structural basis for cooperativity in recruitment of MAML coactivators to Notch transcription complexes. Cell. 2006;124:973–983. doi: 10.1016/j.cell.2005.12.037. [DOI] [PubMed] [Google Scholar]
- 621.Tamura K, et al. Physical interaction between a novel domain of the receptor Notch and the transcription factor RBP-J kappa/Su(H) Curr. Biol. 1995;5:1416–1423. doi: 10.1016/s0960-9822(95)00279-x. [DOI] [PubMed] [Google Scholar]
- 622.Hurtado C, et al. Disruption of NOTCH signaling by a small molecule inhibitor of the transcription factor RBPJ. Sci. Rep. 2019;9:10811. doi: 10.1038/s41598-019-46948-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 623.Astudillo L, et al. The small molecule IMR-1 inhibits the notch transcriptional activation complex to suppress tumorigenesis. Cancer Res. 2016;76:3593–3603. doi: 10.1158/0008-5472.CAN-16-0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 624.Lehal R, et al. Pharmacological disruption of the Notch transcription factor complex. Proc. Natl Acad. Sci. USA. 2020;117:16292–16301. doi: 10.1073/pnas.1922606117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 625.Koch U, Radtke F. Notch and cancer: a double-edged sword. Cell Mol. Life Sci. 2007;64:2746–2762. doi: 10.1007/s00018-007-7164-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 626.Zage PE, et al. Notch pathway activation induces neuroblastoma tumor cell growth arrest. Pediatr. Blood Cancer. 2012;58:682–689. doi: 10.1002/pbc.23202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 627.Yu XM, Phan T, Patel PN, Jaskula-Sztul R, Chen H. Chrysin activates Notch1 signaling and suppresses tumor growth of anaplastic thyroid carcinoma in vitro and in vivo. Cancer. 2013;119:774–781. doi: 10.1002/cncr.27742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 628.Patel PN, Yu XM, Jaskula-Sztul R, Chen H. Hesperetin activates the Notch1 signaling cascade, causes apoptosis, and induces cellular differentiation in anaplastic thyroid cancer. Ann. Surg. Oncol. 2014;21:S497–504. doi: 10.1245/s10434-013-3459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 629.Li K, et al. Modulation of Notch signaling by antibodies specific for the extracellular negative regulatory region of NOTCH3. J. Biol. Chem. 2008;283:8046–8054. doi: 10.1074/jbc.M800170200. [DOI] [PubMed] [Google Scholar]
- 630.Demitrack ES, Samuelson LC. Notch as a Driver of Gastric Epithelial Cell Proliferation. Cell Mol. Gastroenterol. Hepatol. 2017;3:323–330. doi: 10.1016/j.jcmgh.2017.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 631.Real PJ, et al. Gamma-secretase inhibitors reverse glucocorticoid resistance in T cell acute lymphoblastic leukemia. Nat. Med. 2009;15:50–58. doi: 10.1038/nm.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 632.Luistro L, et al. Preclinical profile of a potent gamma-secretase inhibitor targeting notch signaling with in vivo efficacy and pharmacodynamic properties. Cancer Res. 2009;69:7672–7680. doi: 10.1158/0008-5472.CAN-09-1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 633.Govaerts I, et al. PSEN1-selective gamma-secretase inhibition in combination with kinase or XPO-1 inhibitors effectively targets T cell acute lymphoblastic leukemia. J. Hematol. Oncol. 2021;14:97. doi: 10.1186/s13045-021-01114-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 634.Ito T. Intratumoral heterogeneity of Notch1 expression in small cell lung cancer. J. Thorac. Dis. 2018;10:1272–1275. doi: 10.21037/jtd.2018.03.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 635.Marx V. Method of the Year: spatially resolved transcriptomics. Nat. Methods. 2021;18:9–14. doi: 10.1038/s41592-020-01033-y. [DOI] [PubMed] [Google Scholar]
- 636.Joutel A. Prospects for diminishing the impact of nonamyloid small-vessel diseases of the brain. Annu. Rev. Pharm. Toxicol. 2020;60:437–456. doi: 10.1146/annurev-pharmtox-010818-021712. [DOI] [PubMed] [Google Scholar]
- 637.Matsuda M, et al. Recapitulating the human segmentation clock with pluripotent stem cells. Nature. 2020;580:124–129. doi: 10.1038/s41586-020-2144-9. [DOI] [PubMed] [Google Scholar]
- 638.Simpson MA, et al. Mutations in NOTCH2 cause Hajdu-Cheney syndrome, a disorder of severe and progressive bone loss. Nat. Genet. 2011;43:303–305. doi: 10.1038/ng.779. [DOI] [PubMed] [Google Scholar]
- 639.Isidor B, et al. Truncating mutations in the last exon of NOTCH2 cause a rare skeletal disorder with osteoporosis. Nat. Genet. 2011;43:306–308. doi: 10.1038/ng.778. [DOI] [PubMed] [Google Scholar]
- 640.Fukushima H, et al. NOTCH2 Hajdu-Cheney Mutations Escape SCF-Dependent Proteolysis to Promote Osteoporosis. Mol. Cell. 2017;68:645–658.e5. doi: 10.1016/j.molcel.2017.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 641.Luxán G, et al. Mutations in the NOTCH pathway regulator MIB1 cause left ventricular noncompaction cardiomyopathy. Nat. Med. 2013;19:193–201. doi: 10.1038/nm.3046. [DOI] [PubMed] [Google Scholar]
- 642.Towbin JA, Lorts A, Jefferies JL. Left ventricular non-compaction cardiomyopathy. Lancet. 2015;386:813–825. doi: 10.1016/S0140-6736(14)61282-4. [DOI] [PubMed] [Google Scholar]
- 643.Stittrich A-B, et al. Mutations in NOTCH1 cause Adams-Oliver syndrome. Am. J. Hum. Genet. 2014;95:275–284. doi: 10.1016/j.ajhg.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 644.Hassed SJ, et al. RBPJ mutations identified in two families affected by Adams-Oliver syndrome. Am. J. Hum. Genet. 2012;91:391–395. doi: 10.1016/j.ajhg.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 645.Nus M, et al. Diet-induced aortic valve disease in mice haploinsufficient for the Notch pathway effector RBPJK/CSL. Arterioscler Thromb. Vasc. Biol. 2011;31:1580–1588. doi: 10.1161/ATVBAHA.111.227561. [DOI] [PubMed] [Google Scholar]
- 646.MacGrogan D, et al. Sequential ligand-dependent notch signaling activation regulates valve primordium formation and morphogenesis. Circ. Res. 2016;118:1480–1497. doi: 10.1161/CIRCRESAHA.115.308077. [DOI] [PubMed] [Google Scholar]
- 647.Wang Y, et al. Notch-Tnf signalling is required for development and homeostasis of arterial valves. Eur. Heart J. 2017;38:675–686. doi: 10.1093/eurheartj/ehv520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 648.Ikeda M, et al. Genetic evidence for association between NOTCH4 and schizophrenia supported by a GWAS follow-up study in a Japanese population. Mol. Psychiatry. 2013;18:636–638. doi: 10.1038/mp.2012.74. [DOI] [PubMed] [Google Scholar]
- 649.Zhang Y, et al. Convergent lines of evidence support as a schizophrenia risk gene. J. Med. Genet. 2021;58:666–678. doi: 10.1136/jmedgenet-2020-106830. [DOI] [PubMed] [Google Scholar]
- 650.Morris HE, Neves KB, Montezano AC, MacLean MR, Touyz RM. Notch3 signalling and vascular remodelling in pulmonary arterial hypertension. Clin. Sci. 2019;133:2481–2498. doi: 10.1042/CS20190835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 651.Li X, et al. Notch3 signaling promotes the development of pulmonary arterial hypertension. Nat. Med. 2009;15:1289–1297. doi: 10.1038/nm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 652.Zhang Y, et al. Notch signaling is a critical regulator of allogeneic CD4+ T-cell responses mediating graft-versus-host disease. Blood. 2011;117:299–308. doi: 10.1182/blood-2010-03-271940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 653.Siveke JT, et al. Notch signaling is required for exocrine regeneration after acute pancreatitis. Gastroenterology. 2008;134:544–555. doi: 10.1053/j.gastro.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 654.Golson ML, Loomes KM, Oakey R, Kaestner KH. Ductal malformation and pancreatitis in mice caused by conditional Jag1 deletion. Gastroenterology. 2009;136:1761–1771.e1. doi: 10.1053/j.gastro.2009.01.040. [DOI] [PubMed] [Google Scholar]
- 655.Zhang X, et al. Inhibition of Notch activity promotes pancreatic cytokeratin 5-positive cell differentiation to beta cells and improves glucose homeostasis following acute pancreatitis. Cell Death Dis. 2021;12:867. doi: 10.1038/s41419-021-04160-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 656.John GR, et al. Multiple sclerosis: re-expression of a developmental pathway that restricts oligodendrocyte maturation. Nat. Med. 2002;8:1115–1121. doi: 10.1038/nm781. [DOI] [PubMed] [Google Scholar]
- 657.Seifert T, Bauer J, Weissert R, Fazekas F, Storch MK. Notch1 and its ligand Jagged1 are present in remyelination in a T-cell- and antibody-mediated model of inflammatory demyelination. Acta Neuropathol. 2007;113:195–203. doi: 10.1007/s00401-006-0170-9. [DOI] [PubMed] [Google Scholar]
- 658.Zhang Y, et al. Notch1 signaling plays a role in regulating precursor differentiation during CNS remyelination. Proc. Natl Acad. Sci. USA. 2009;106:19162–19167. doi: 10.1073/pnas.0902834106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 659.Mu X, et al. The role of Notch signaling in muscle progenitor cell depletion and the rapid onset of histopathology in muscular dystrophy. Hum. Mol. Genet. 2015;24:2923–2937. doi: 10.1093/hmg/ddv055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 660.Vieira NM, et al. Jagged 1 rescues the Duchenne muscular dystrophy phenotype. Cell. 2015;163:1204–1213. doi: 10.1016/j.cell.2015.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 661.Tracy MR, Dormans JP, Kusumi K. Klippel-Feil syndrome: clinical features and current understanding of etiology. Clin. Orthop. Relat. Res. 2004;424:183–190. [PubMed] [Google Scholar]
- 662.Karaca E, et al. Rare variants in the notch signaling pathway describe a novel type of autosomal recessive Klippel-Feil syndrome. Am. J. Med. Genet. A. 2015;167A:2795–2799. doi: 10.1002/ajmg.a.37263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 663.Petruccelli E, et al. Alcohol activates Scabrous-notch to influence associated memories. Neuron. 2018;100:1209–1223. doi: 10.1016/j.neuron.2018.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 664.Rosati E, et al. Constitutively activated Notch signaling is involved in survival and apoptosis resistance of B-CLL cells. Blood. 2009;113:856–865. doi: 10.1182/blood-2008-02-139725. [DOI] [PubMed] [Google Scholar]
- 665.Papayannidis C, et al. A Phase 1 study of the novel gamma-secretase inhibitor PF-03084014 in patients with T-cell acute lymphoblastic leukemia and T-cell lymphoblastic lymphoma. Blood Cancer J. 2015;5:e350. doi: 10.1038/bcj.2015.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 666.Peereboom DM, et al. A phase II and pharmacodynamic Trial of RO4929097 for patients with recurrent/progressive glioblastoma. Neurosurgery. 2021;88:246–251. doi: 10.1093/neuros/nyaa412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 667.Krop I, et al. Phase I pharmacologic and pharmacodynamic study of the gamma secretase (Notch) inhibitor MK-0752 in adult patients with advanced solid tumors. J. Clin. Oncol. 2012;30:2307–2313. doi: 10.1200/JCO.2011.39.1540. [DOI] [PubMed] [Google Scholar]
- 668.Schott AF, et al. Preclinical and clinical studies of gamma secretase inhibitors with docetaxel on human breast tumors. Clin. Cancer Res. 2013;19:1512–1524. doi: 10.1158/1078-0432.CCR-11-3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 669.Mir O, et al. Notch pathway inhibition with LY3039478 in soft tissue sarcoma and gastrointestinal stromal tumours. Eur. J. Cancer. 2018;103:88–97. doi: 10.1016/j.ejca.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 670.Azaro A, et al. Phase 1 study of 2 high dose intensity schedules of the pan-Notch inhibitor crenigacestat (LY3039478) in combination with prednisone in patients with advanced or metastatic cancer. Invest N. Drugs. 2021;39:193–201. doi: 10.1007/s10637-020-00944-z. [DOI] [PubMed] [Google Scholar]
- 671.Borthakur G, et al. Phase 1 study to evaluate Crenigacestat (LY3039478) in combination with dexamethasone in patients with T-cell acute lymphoblastic leukemia and lymphoma. Cancer. 2021;127:372–380. doi: 10.1002/cncr.33188. [DOI] [PubMed] [Google Scholar]
- 672.Azaro A, et al. A phase 1b study of the Notch inhibitor crenigacestat (LY3039478) in combination with other anticancer target agents (taladegib, LY3023414, or abemaciclib) in patients with advanced or metastatic solid tumors. Invest N. Drugs. 2021;39:1089–1098. doi: 10.1007/s10637-021-01094-6. [DOI] [PubMed] [Google Scholar]
- 673.Rudin CM, et al. Rovalpituzumab tesirine, a DLL3-targeted antibody-drug conjugate, in recurrent small-cell lung cancer: a first-in-human, first-in-class, open-label, phase 1 study. Lancet Oncol. 2017;18:42–51. doi: 10.1016/S1470-2045(16)30565-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 674.McKeage MJ, et al. Phase IB trial of the anti-cancer stem cell DLL4-binding agent demcizumab with pemetrexed and carboplatin as first-line treatment of metastatic non-squamous NSCLC. Target Oncol. 2018;13:89–98. doi: 10.1007/s11523-017-0543-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table1. The role of NOTCH signaling in developmental processes