Abstract
Methionine restriction (MR) extends lifespan and improves several markers of health in rodents. However, the proximate mechanisms of MR on these physiological benefits have not been fully elucidated. The essential amino acid methionine plays numerous biological roles and limiting its availability in the diet directly modulates methionine metabolism. There is growing evidence that redox regulation of methionine has regulatory control on some aspects of cellular function but interactions with MR remain largely unexplored. We tested the functional role of the ubiquitously expressed methionine repair enzyme methionine sulfoxide reductase A (MsrA) on the metabolic benefits of MR in mice. MsrA catalytically reduces both free and protein-bound oxidized methionine, thus playing a key role in its redox state. We tested the extent to which MsrA is required for metabolic effects of MR in adult mice using mice lacking MsrA. As expected, MR in control mice reduced body weight, altered body composition, and improved glucose metabolism. Interestingly, lack of MsrA did not impair the metabolic effects of MR on these outcomes. Moreover, females had blunted MR responses regardless of MsrA status compared to males. Overall, our data suggests that MsrA is not required for the metabolic benefits of MR in adult mice.
Subject terms: Molecular medicine, Chemical modification, Ageing, Metabolism, Homeostasis
Introduction
Restriction of dietary intake of the amino acid methionine, even in the absence of restriction of calories, has been shown to consistently extend lifespan and improve metabolic health in rodents. Previous studies have shown that dietary methionine restriction (MR) in rodents can extend lifespan up to 42% compared to rodents fed diets replete with methionine1–3. Moreover, MR has strong effects on metabolic function and has been shown to improve glucose homeostasis4–9, decrease oxidative stress2,10–15, and promote adipose tissue browning16–22. These findings are consistent with the idea that dietary intervention by restricting methionine improves health in addition to extending longevity. Understanding the molecular mechanisms responsible for the physiological effects of MR could then have significant impact as potential targets to improve human health throughout life.
While pro-longevity dietary interventions affect many molecular pathways consistent with the pillars of aging, it seems likely that the effects of MR may strongly affect methionine-dependent pathways. Methionine metabolism has multiple roles in regulating physiological function. Methionine is the initiating amino acid in protein translation, and restriction of this amino acid in the diet has been shown to reduce protein synthesis23–27. MR has also been shown to increase activity of pathways involved in protein degradation and recycling including the ubiquitin proteasome system and autophagy consistent with enhanced proteostasis28. Methionine plays a significant role in the generation of hydrogen sulfide via conversion to cysteine through the transsulfuration pathway. Hydrogen sulfide and its generation has been shown to play a central role in the effects of dietary restriction including calorie restriction (CR) and MR29. Methionine is also used in the generation of S-adenosyl methionine (SAM) which is the primary methyl group donor for methyltransferases. The effects of MR on this metabolite are complex with levels being decreased in some cases30–32 while having no impact in others31,33, and with MR either increasing global DNA methylation30 or having no effect12,30. There is also evidence that other interventions that extend lifespan significantly alter methionine metabolism. For example, Ames dwarf mice, which live more than 40% longer than their controls due to a mutation in Prop1, have also been shown to have altered sulfur metabolism and higher SAM turnover34,35. Interestingly, Ames dwarf mice show no impact of MR on glucose metabolism36 or longevity34 suggesting perhaps overlap in pro-longevity mechanisms of these interventions.
The potential role of methionine reduction–oxidation (redox) regulation in the mechanism of MR has been relatively unexplored. Methionine itself is extremely susceptible to oxidation due to the sulfur atom that makes up its amino acid side chain. Under oxidizing conditions, the pro-chiral sulfur of methionine’s thioether can be oxidized to yield two epimers of L-methionine sulfoxide37. Methionine sulfoxide reductases (Msr) have evolved to catalytically reduce methionine sulfoxide to methionine. This is an important oxidative damage repair mechanism as methionine and methionine sulfoxide differ in structure and polarity. In addition, there is growing evidence that redox regulation of methionine residues may also act as functional regulators of proteins38–42. At least four forms of Msr have evolved in mammals: MsrA which reduces the chiral (S) epimer of methionine sulfoxide and MsrB1-3 which reduce the (R) epimer. Of these, MsrA is the most ubiquitously distributed among mammalian tissues and the most well-studied Msr. The lack of MsrA does increase sensitivity to oxidative challenge and results in increased oxidation of methionine residues43. Interestingly, MsrA has also been reported to play a role in the regulation of glucose and insulin signaling under metabolic challenge. The lack of MsrA in mice exacerbates insulin resistance caused by high fat feeding in part by failing to prevent oxidative damage to key insulin signaling proteins44. Conversely, overexpression of MsrA preserves insulin sensitivity in mice fed a high fat diet45.
Relatively little is known regarding the potential role of methionine redox metabolism or Msr activity in the outcomes of MR. MR in mice reduces plasma methionine and methionine sulfoxide levels to approximately the same degree31. It has also been shown that the lack of both MsrA and MsrB1, but not either independently, can hinder growth rate of weaned mice under MR33, suggesting an important role of Msr enzymes in preserving methionine during restriction. Here, we directly tested the functional requirement for MsrA on the metabolic outcomes of MR in mice. Using mice lacking MsrA expression (MsrA KO), we find that MsrA is not required to reduce body weight or composition under MR. Moreover MsrA KO mice responded as well, or better, to MR in terms of improvement in glucose metabolism and respiration. Together, our studies suggest that functional MsrA is not required for the metabolic benefits of MR.
Results
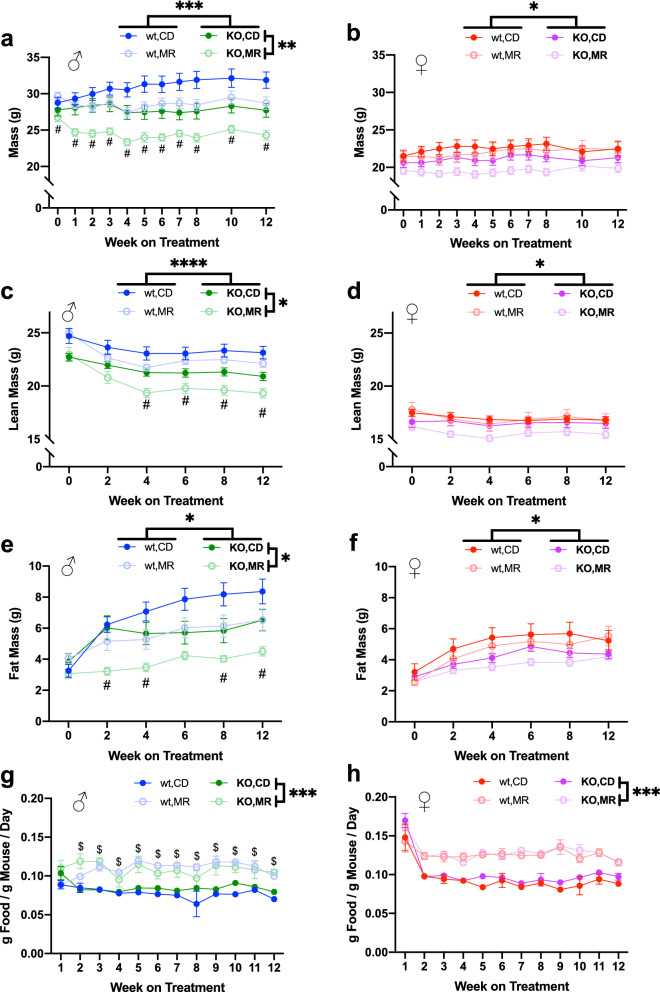
In this study, we used adult mice to potentially differentiate the effects of MR on metabolic function from those of MR-mediated delays in development2. At an average 7.5 months of age, fully grown mice began dietary interventions of either MR (0.15% methionine as proportion of protein) or composition equivalent control diet (CD) which was replete with levels of methionine (0.86% methionine as proportion of protein) approximately equivalent to that found in normal chow. During the study, diets were provided ad libitum and food consumption was monitored throughout. Prior to intervention with each diet, both male and female MsrA KO mice were lower in body weight than their wild type counterparts (Fig. 1a, b). In wild type males, MR reduced body weight and fat mass compared to CD, consistent with previous reports1,5,6,17,18,21,22,30. In addition, MR caused a small change in lean mass compared to CD. Surprisingly, MR induced reduction of male body weight, fat mass, and lean mass in MsrA KO to a greater extent than in wild type mice—the percentage change in these outcomes was larger in MsrA KO males compared to wild type males (Fig. 1a, c, e). MR did not result in significant changes body weight, fat mass, or lean mass regardless of genotype during the 3 months of treatment in females (Fig. 1d, f).
Figure 1.
MR has sex-specific effects on physiological measures. Body weight (a), (b) and normalized food consumption (g), (h) measured weekly while on MR diet. Body composition data for fat mass (c), (d), lean mass (e), (f) measured every two weeks. Sexes analyzed separately with Repeated Measures, 3-Way ANOVA. Main effects for diet and MsrA KO genotype indicated by significance bars by legends (right side and above, respectively). Post-hoc diet specific effect within a genotype was analyzed with Repeated Measures, 2-Way ANOVA Multiple Comparisons with False Discovery Rate correction, Q = 0.05. Means at specific time points being significantly different (p < 0.05) between diets for wild type denoted by dollar sign ($) and for MsrA KO denoted by a pound sign (#). Graphs represent means ± s.e.m, and all groups were 8–10 mice. (*p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001).
Despite the reported body weight reduction in the MR groups, we also found that MR increased food consumption in all MR groups compared to their sex- or genotype-equivalent CD groups (Fig. 1g, h). This increase in food consumption when normalized to body weight was stable throughout the three months the mice were on the diet. While MR significantly increased food consumption compared to CD, post-hoc analysis of these data indicated that only the wild type males had a significant difference between the MR and CD. These results are similar to others reported in regards to body composition and food consumption under MR1,5,6,17,18,21,22,24,30.
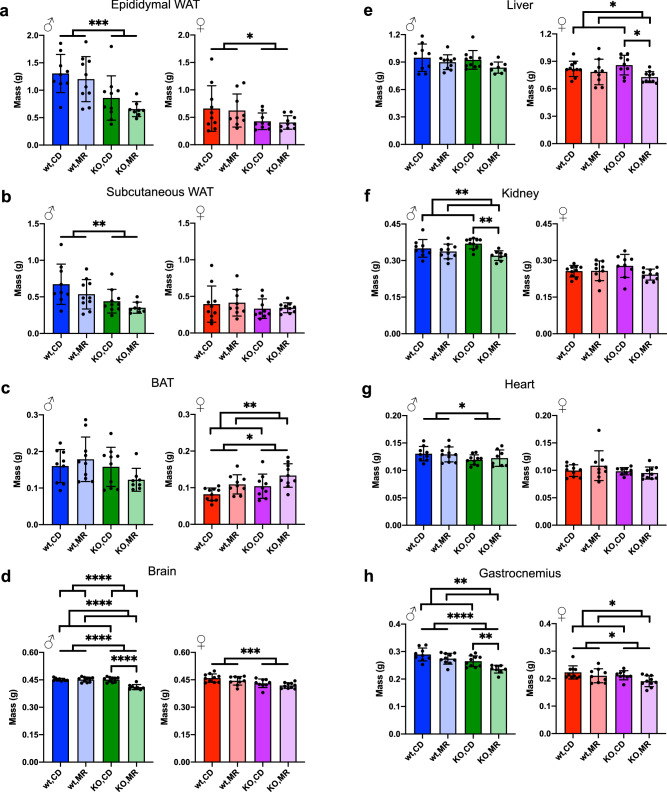
The post-mortem tissue masses reflected the decreased fat mass observed with QMR (Fig. 1e, f) with epididymal and subcutaneous white adipose tissue (WAT) being lower for the MsrA KO males, but with only a small difference observed in the MsrA KO female subcutaneous WAT (Fig. 2a, b). Brown adipose tissue (BAT) was significantly increased in females by MR (Fig. 2c) but not males; previous studies have been equivocal in reporting this the response of BAT to MR4,16,46. Surprisingly, MR resulted in a dramatic decrease in brain mass for the male MsrA KO mice, but the reason for this is unclear (Fig. 2d). MR also resulted in sex-specific decreases in liver and kidney mass—a decrease in liver mass in the females and a decrease in kidney mass in the males (Fig. 2e, f). The change in heart mass and gastrocnemius mass (Fig. 2g, h) was consistent with the lean mass decrease observed with QMR (Fig. 1c, d).
Figure 2.
MR has sex-specific effects on tissue masses. Tissue masses for Epididymal WAT (a), Subcutaneous WAT (b), BAT (c), Brain (d), Liver (e), Kidney (f), Heart (g), and Gastrocnemius (h) were measured at time of collection. Analysis was within each sex via Two-Way ANOVA for main effects. Post-hoc analysis was performed with Sidac multiple comparisons correction to assess the diet effect within each genotype. Graphs represent means ± s.d. and all groups were 8–10 mice. (*p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001).
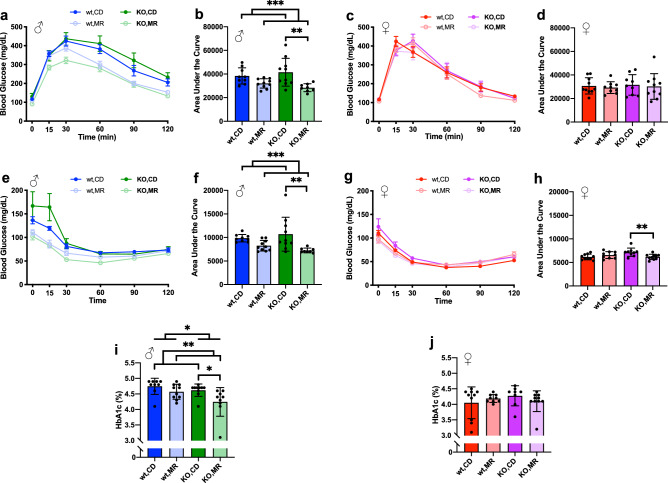
Similar to previously reports, glucose metabolism was improved by MR even when started in non-obese adult animals4–6,9,22. In males, glucose tolerance tested (GTT) after 9 weeks of intervention was improved when MR groups were analyzed as a whole (Fig. 3a, b). Post-hoc analysis of the within-sex, two-way ANOVA showed a significant effect of MR in MsrA KO (p = 0.0047) though not in wild type mice (p = 0.1545) (Fig. 3b). MR also improved insulin sensitivity in males as measured by insulin tolerance test (ITT) following 11 weeks of dietary intervention (Fig. 3e, f). Similar to GTT results, there was a significant post-hoc effect of MR on MsrA KO mice (p = 0.0012) though not in wild type mice (Fig. 3f). In contrast to results in males, MR had no significant main effect on GTT or ITT in female mice for either wild type or MsrA KO mice (Fig. 3c, d, g, h). To assess for potential differences in the molecular pathways regulating insulin sensitivity, we also measured phosphorylation of Akt. Western blots were performed to assess Akt phosphorylation, and we found no effect of MsrA on possible molecular mechanisms of insulin sensitivity. Phosphorylation of Akt in fasted animals was unaffected by either diet or genotype in males; in females, phosphorylation was increased in MsrA KO compared to wild type (Supplemental Fig. S4a). In skeletal muscle, we found no significant change in either males or females, in line with our glucose metabolism results (Supplemental Fig. S5a). We also measured glycated hemoglobin A1c (HbA1c) as an additional marker of glucose metabolic function, and found HbA1c significantly lower in male mice on MR compared to CD (Fig. 3i) but there was no effect of diet in females (Fig. 3j). Interestingly, MsrA KO males had lower HbA1c than their wild type male counterparts overall, although there was no difference between MsrA KO and wild type females.
Figure 3.
Males have greater glucose metabolism response to MR than females. Glucose Tolerance Test curves (a), (c) and Area Under the Curve (AUC) for their respective curves (b), (d) for both sexes. Insulin Tolerance Test curves (e), (g) and AUC for their respective curves (f), (h). AUC calculated by the trapezoid method and analyzed within each sex via Two-Way ANOVA for main effects. Post-hoc analysis was performed with Sidac multiple comparisons correction to assess the diet effect within each genotype. HbA1c was analyzed similarly (i), (j). Line graphs represent means ± s.e.m., bar graphs represent means ± s.d.. Groups were 8–10 mice. (*p < 0.05; **p < 0.01; ***p < 0.001).
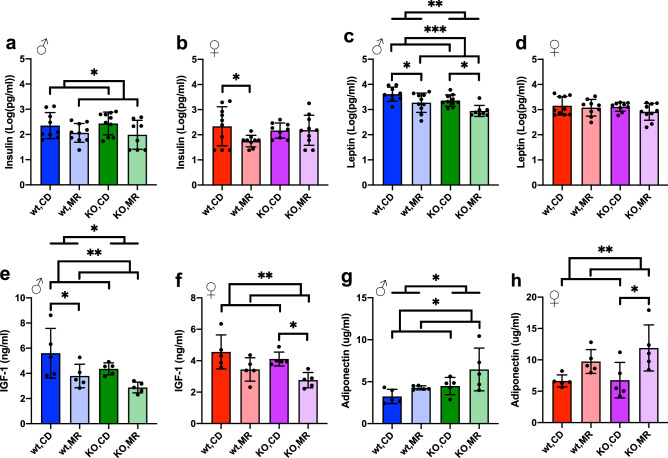
After 12 weeks of MR, plasma was collected after overnight fast to assess endocrinological effects of MR in wild type and MsrA KO mice. MR significantly reduced insulin concentrations in males compared to CD (Fig. 4a). In females, MR reduced insulin concentration in wild type females but not MsrA KO (Fig. 4b). These results are generally in line with the idea that MR improves glucose metabolic function in vivo4–6,9,22. Leptin, a peptide secreted from adipose tissue and involved in satiety, was lower in the MR males compared to CD males, but unchanged by diet in females (Fig. 4c, d). Serum concentrations of IGF-1 were decreased with MR in both sexes as has been shown in other studies2,8,46–49 and is associated with increased lifespan34,49, however there was only a significant genotype effect of the MsrA KO in the males (Fig. 4e, f). Adiponectin was increased with MR in both sexes as has been shown in other studies8,18,46, with a genotype effect observed in the males with the MsrA KO having higher concentrations of adiponectin compared to wild type (Fig. 4g, h). The effect of MR on other endocrine factors associate with metabolic function were largely unchanged in with diet or genotype in male mice. However, MR did affect these outcomes in female mice with both genotype and diet dependent effects (Supplemental Fig. S1).
Figure 4.
MR alters metabolic markers more in males. MilliPlex of serum from mice overnight fasted at time of sacrifice. Selected panel results of Insulin (a), (b) and Leptin (c), (d) measured by MilliPlex. Data was log transformed before analysis to preserve normality. Data points at lower end of detection were included as lowest value given by the assay’s internal standard curve. IGF-1 (e), (f) and Adiponectin (g), (h) measured in plasma by ELISA. Analysis was within each sex via Two-Way ANOVA for main effects. Post-hoc analysis was performed with Sidac multiple comparisons correction to assess the diet effect within each genotype. Graphs represent means ± s.d. and all groups were 8–10 mice for MilliPlex, and 5 mice per group for IGF-1 ELISA. (*p < 0.05; **p < 0.01; ***p < 0.001).
MR has been shown to decrease oxidative stress in numerous studies 2,10–15. Given the role of MsrA in repairing/regulating oxidative damage to methionine, we tested whether the lack of MsrA altered the effect of MR on such outcomes (Supplemental Figs. S4, S5). We found no effect of MR or lack of MsrA on the content of GPX1 or SOD2 expression in liver (Supplemental Fig. S4b, e). In line with reducing oxidative stress, we found MR decreased GPX4 expression in males, but not females (Supplemental Fig. S4c). As a measure of oxidative damage, we measured 4-hydoxynonal (HNE; Supplemental Fig. S4d) adducts, the result of lipid oxidation. We found an interaction effect detected in males between diet and genotype though no effect of either alone. This suggests some possible benefit of MsrA KO, but more studies would be required to determine this. In muscle, we found no effect of diet or genotype on HNE (Supplemental Fig. S5b), but did indicate that MsrA KO had decreased SOD2 expression in males only (Supplemental Fig. S5c). Together these results suggest the main effects reported are not due to dramatic changes in oxidative stress or damage.
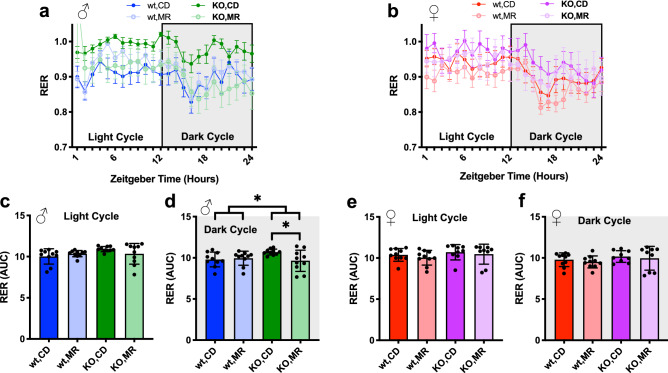
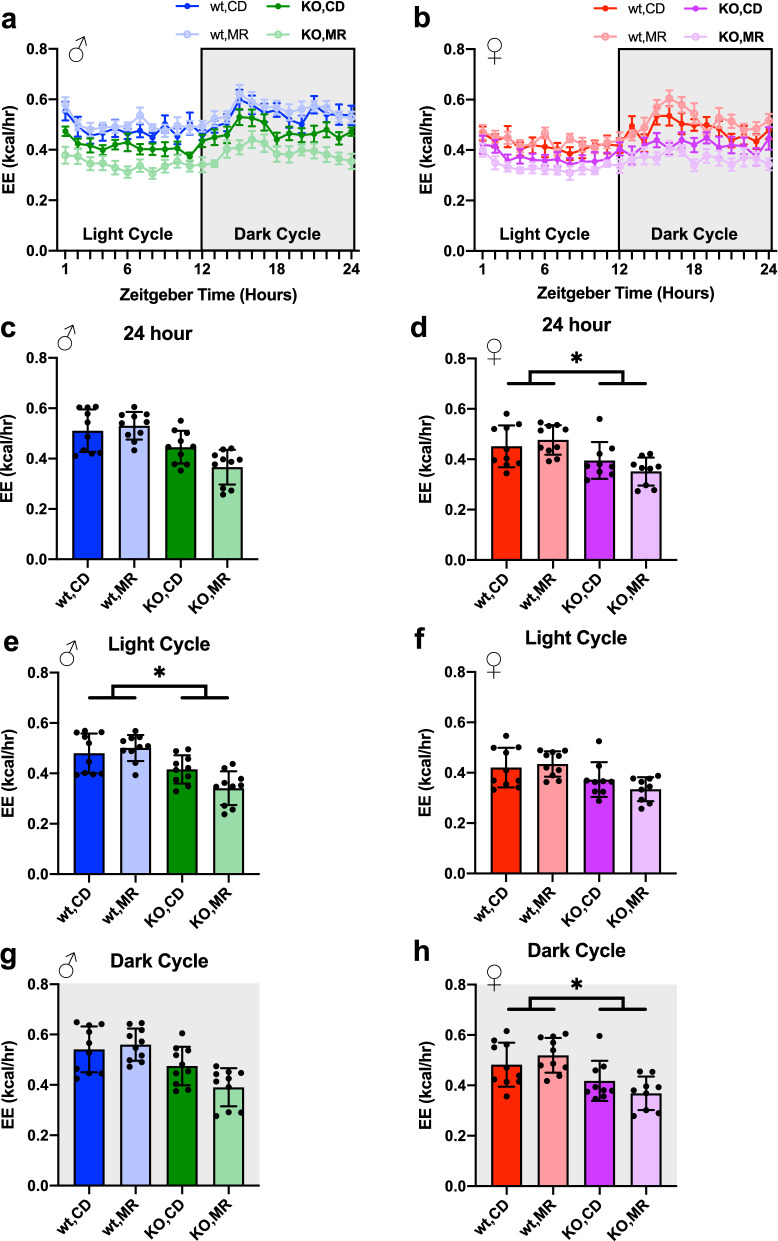
We also addressed the effect of MR and lack of MsrA on whole animal metabolism as an additional assessment of metabolic function. Using an independent cohort of mice treated identically, we measured respiration of animals following 8 months of MR. Overall, MR did not affect respiratory exchange ratio (RER) compared to CD (Fig. 5) with the exception of a decrease in dark cycle RER in MsrA KO males on MR (Fig. 5d). Oxygen consumption (VO2) and carbon dioxide production (VCO2) were also analyzed normalized to body weight (Supplemental Fig. S2) and lean mass (Supplemental Fig. S3), with only lean mass normalization showing significant effect of genotype but not diet. Energy expenditure (EE) was calculated from this data and averaged over 24 h, as well as broken into the light and dark cycle averages (Fig. 6). ANCOVA analysis controlling for lean body mass yielded a main effect of the MsrA KO for light cycle EE (Fig. 6e), but had a nearly significant genotype effect for overall 24 h average EE. Females had a similar outcome with a main effect of MsrA KO for the dark cycle and overall 24 h average EE (Fig. 6d, h). Taken together these results indicate that MR did not significantly alter EE, while MsrA KO had a more profound effect when controlled for lean body mass (Fig. 6).
Figure 5.
MR had minimal impact on RER. Respiratory Exchange Ratio (RER) for 24 h period (a), (b), analyzed via 3-Way ANOVA for light and dark cycle independently. Graphs represent mean ± s.e.m. Male light cycle (c) and dark cycle (d) AUC, and Female light cycle (e) and dark cycle (f) analyzed within each sex via Two-Way ANOVA for main effects on Area Under the Curve (AUC) for RER. Post-hoc analysis was performed with Sidac multiple comparisons correction to assess the diet effect within each genotype. Line graphs represent means ± s.e.m., bar graphs represent means ± s.d., and all groups were 9–10 mice on diet for ~ 8 months. (*p < 0.05).
Figure 6.
Energy Expenditure was not impacted by MR. Energy Expenditure (EE) for 24 h period based on VO2 not normalized to mass for mice from Cohort 2 (a), (b). Data averaged over the 24 h test period (c), (d), and for the light (e), (f) and dark (g), (h) cycle separately. Analyzed with ANCOVA using lean mass as a control variable for AUC graphs of EE for full 24 h as well as light and dark cycles. Line graph represents mean ± s.e.m., bar graphs represent mean ± s.d. Groups were 9–10 mice. (*p < 0.05).
Discussion
Insight regarding the molecular underpinnings of MR have the potential to significantly advance our understanding of the physiological benefits of this intervention including those on longevity and metabolic function. Here we tested whether the methionine sulfoxide reducing enzyme MsrA impacts the effect of MR on metabolism in mice. Overall, we found that mice lacking MsrA have normal, or potentially even greater, response to MR compared to wild type mice in terms of weight loss, glucose and insulin response, and respiration. One interpretation of these outcomes could be that MsrA is dispensable for the effects of MR on glucose metabolism in vivo, or that the impact of MsrA modulation by MR is on functions that do not directly affect glucose metabolism. In regards to the potential lack of requirement of this enzyme, Zhao et al. showed previously that lack of MsrA did not significantly impact growth from weaning under methionine restricted conditions, a classical bioassay for growth33. This report showed also that the lack of MsrB1 alone had no effect in this assay, but that the lack of both MsrA and MsrB1 delayed growth under methionine restriction from weaning. Together, these data suggest a functional requirement for Msr in general under conditions of limiting methionine, and also that there may be compensatory mechanisms for this process among Msr enzymes. Data from MsrB1 KO mice showed that other Msr enzymes are upregulated in a tissue specific manner50. More work in this area would be of benefit to understanding the role of Msr and methionine metabolism in general in MR.
Among potential mechanisms by which MR alters physiological function are reported improvements in resistance and response to oxidative stress induced by MR2,10,11,15,43. While not a primary antioxidant, MsrA has been shown to play an important role in the resistance to oxidative stress and the lack of MsrA reduces resistance to oxidant challenge in mice43,44. Studies have shown that loss of any of these Msr enzymes under normal diet conditions is survivable, but can make the organism more sensitive to oxidative stress. Counterintuitively, knockout of the four Msr enzymes, MsrA and MsrB1-3, has been shown to increase oxidative stress resistance, presumably through compensatory mechanisms among the antioxidant defense system51. In addition to repairing oxidized methionine, Msr have been proposed to act more generally in oxidant defense as part of a methionine redox system52. In this scenario, methionine acts as a “free-radical sink” taking on oxidative damage to protect other macromolecules in the cell. These methionine residues can then be recycled (reduced) by Msr to further defend the cell from oxidant damage. Under this paradigm, it is conceivable that restriction of methionine then increases the importance of functional Msr to prevent oxidative damage. While we did not address this here, it would be of interest to assess the interplay of MR and MsrA under such oxidant challenges.
While our results in general suggest MsrA is not required for the effects of MR on metabolism, some of our results do suggest potential roles in mediating other functions affected by MR. For example, MR in wild type mice did not significantly affect lean mass throughout our study. On the other hand, MsrA KO mice lost a significantly quantity of lean mass under MR that did not return to normal levels through the duration of study (Fig. 1c). Generally, loss of lean mass might be associated with declines in muscle mass, function, etc. We did observe a decrease in gastrocnemius mass at time of tissue collection in both sexes with MR which was significant in MsrA KO post-hoc testing (Fig. 2h). A similar decrease in mass has been reported in other MR studies4,7,47. Further examination of muscle function and structure will be necessary to delineate this potential novel relationship between methionine metabolism and muscle. In particular, assessment of late-life muscle function and the effect of MR with Rota-Rod and grip strength would expand on our understanding of whether this intervention improves overall healthy aging. Fat mass was also shown to decreased by MR (Fig. 1e, f) as measured by QMR. However, the individual tissue masses did not corroborate this (Fig. 2a–c). This could have been the result of how the tissue was collected as well as that the QMR fat signal measured the entire organism. Contributions from other tissues or fat depots not collected could have resulted in this discrepancy. In addition, it will be of interest to determine whether the MR-mediated declines in kidney, liver, and brain mass of MsrA KO mice have significant impact on the function of these organs in vivo.
MR has been shown to mediate many of its functional benefits through modulation of endocrine regulation. For example, MR has been shown to increase circulating concentrations of adiponectin8,18,46; this adipokine then can directly improve glucose metabolism. MR has also been shown to reduce IGF12,8,46,47, likely through down-regulation of growth hormone signaling pathways. While IGF1 is more directly associated with improved glucose metabolism, the relationship between low IGF1 and improved glucose metabolism shown with MR likely reflects reduced concentrations of the pro-diabetogenic growth hormone. More generally, our results show a varied, and sex-dependent, response to MR in terms of most endocrine outcomes measured in our comprehensive endocrinological assays.
In this study, the response to MR on physical and functional outcomes was more pronounced in male mice compared to female mice regardless of genotype. Some evidence of this can be seen in a recent study by Forney et al. which also tested the response to MR in both sexes17. Similar to our results, this previous study showed that MR has significantly different functional impact on each sex and in general that males respond more robustly to MR than do females. This suggests a significant interaction between these factors and the animal’s sex, but it remains an open question if this is driven by sex hormones or sex chromosomes. The lack of MsrA had no effect on these sex-differences, suggesting that this enzyme does not affect the central mediators of this MR and genetic sex relationship. Further experiments would be required to better understand the interactions of methionine sulfoxide reductases and sex with the effects of MR. Some possible areas of interest could be gleaned from studies on how MsrA mutations impact human health. We have previously shown that MsrA plays a role in the metabolic response to diet-induced obesity in mice44,45. Decreases in MsrA have been associated with pathologies of the eye lens and have been implicated in Alzheimer’s Disease53–55. GWAS have also implicated MsrA mutants in rheumatoid arthritis56. These studies provide possible areas of investigation to better understand the interactions with MR.
Overall, our results indicate that (1) MsrA is not functionally required for the effects of MR on metabolic function and its loss may enhance certain effects, (2) MR can significantly improve body composition and metabolic function even when administered to normal adult rodents, (3) in general, males respond to a greater degree to MR than do females in terms of metabolic function. While our studies investigated these interactions and effects in adult mice, it remains an open question as to their long-term effects on longevity and health span. While previous studies have indicated that lack of MsrA does not negatively impact lifespan, its interaction with MR is uncertain.
Methods
Animal usage and ethical procedures
All animal experiments were approved by the Institutional Animal Care and Use Committees and UTHSA (Animal Protocol 20170190AR), and have been reported following ARRIVE guidelines. All methods were conducted in accordance with international ethical standards and guidelines.
Animal experiments
Cohort 1
Genetic mutant mice with homozygous deletion of MsrA were maintained on C57Bl/6 J background as previously reported44. For this study, both male and female mice were used, with wild-type C57Bl/6 J as controls. All mice were confirmed for genotype by PCR analysis of tail-derived genomic DNA. Animal studies were performed in a specific pathogen-free vivarium maintained at 25 °C with a 12 h:12 h light:dark cycle. Mice were maintained in ventilator cages at density of 3–4 (male) or 5 (female) mice per cage, and provided food and water ad libitum throughout study except prior to metabolic assessment. Mice were maintained on standard chow (NIA-31 equivalent) until an age of approximately 7.5 months post-weaning until cages were assigned to either control diet (CD) (0.86% Met, TestDiet 578F w/0.86% MET—5SFD) or MR (0.15% Met, 0% Cys, Test Diet 96D2, modified TestDiet 58B0) diet for the duration of the study. 9–10 mice were assigned to each group combination of sex, genotype, and diet, resulting in 8 groups of 9–10 mice. Cages were assigned non-randomly to have approximately equal starting weights between diet groups within each genotype. Body weight and composition (by quantitative magnetic resonance, Echo MRI, Houston TX) were performed prior to initiation of dietary intervention. During the study, mice were weighed weekly, food consumption was measured weekly, and body composition was measured bi-weekly. Tissues were collected after euthanasia via CO2 asphyxiation, and measured for mass before being snap frozen in liquid nitrogen for storage. During the course of the study one male mouse suffered from rectal prolapse and subsequent weight loss. Data collected from this mouse was censored from the study.
Cohort 2
An identical cohort of mice was started at the same time using the same experimental paradigm. These mice were used for measurement of oxygen consumption after being treated with MR or CD for approximately 8 months. Body weight and food consumption were measured in these mice on the same schedule as the first group. Body composition was measured monthly.
Glucose tolerance (GTT) and insulin tolerance tests (ITT)
Following an overnight (16 h) fast, fasting blood glucose concentrations were measured by tail bleed using an AimStrip Plus digital glucose meter. For GTT mice injected intraperitoneally with 1.5 mg/g body weight glucose in PBS. Blood glucose was measured by tail bleed at 15, 30, 60, 90, and 120 min post injection. Area Under the Curve (AUC) was calculated via the trapezoid method. ITT were performed similarly with intraperitoneal injection of 0.75U Insulin/g body weight in PBS and measurement of blood glucose by tail bleed following 15, 30, 60, 90, and 120 min. GTT were performed two weeks prior to ITT in the same animals.
Hemoglobin A1c
At the completion of study, mice were fasted overnight and tail bleed was performed to collect whole blood in EDTA washed tubes and temporarily stored on ice. Collected blood was allowed to warm to room temperature before HbA1c was measured on a Siemens Vantage DCA Analyzer (Siemens AG, Munich, Germany).
MilliPlex metabolic panel
At the completion of study, mice were fasted overnight. Blood was collected and centrifuged in EDTA-coated tubes then flash frozen. Plasma was then tested in the MilliPlex MMHMAG-44 K MILLIPLEX MAP Mouse Metabolic Hormone Panel (EMD Millipore). Data was log transformed to preserve normality prior to analysis.
ELISA
IGF1 ELISA (Abcam, ab100695) and Adiponectin ELISA (Abcam, ab108785) were performed as per manufacturer’s instructions.
Oxygen consumption
Oxygen consumption was performed on mice after eight months on diet. Oxygen consumption and carbon dioxide generation was measured via the CLAMS system (Columbus Instruments). Mice were individually housed during testing and were housed for 24 h before measurement was started. Oxygen and carbon dioxide volume were measured for the next 24 h after acclimatization. Measurements were based on 1 h bins.
Energy expenditure
Energy expenditure was calculated based on lean mass from QMR and VO2 following equations provided by the CLAMS system. Briefly, EE was calculated based as 3.815 + 1.232 * RER * VO2, with VO2 not normalized to mass.
Western blot
Samples were prepared by homogenizing ~ 50 mg of tissue in ~ 550ul (11ul:1 mg) RIPA for skeletal muscle and ~ 500ul (10ug:1 mg) RIPA for liver. RIPA contained protease and phosphatase inhibitor cocktail (Pierce). Tissue samples homogenized using a TissueLyserII (Qiagen) for 2 min at 30 Hz for skeletal muscle and 1 min at 30 Hz for liver. Supernatant after centrifugation was collected and protein measured using Pierce BCA assay (Bio-Rad).
Blotting was performed with Criterion TGX gels (Bio-Rad). Gels were transferred to PVDF membranes (Bio-Rad) and total protein measured with Ponceau S (Sigma) staining imaged with a Perfection V39 flatbed scanner (Epson). Membranes were blocked with 10% non-fat dry milk or 2% BSA in TBST. Membranes were incubated with primary antibody overnight at 4 °C with agitation: Akt (Cell Signaling, 9272), SOD2 (AbCam, ab13533), GPX4 (Santa Cruz Biotechnology, sc-27529), pAkt(S473) (Cell Signaing, 9271), GPX1 (AbCam, ab22604), HNE (Alpha Diagnostic, HNE11-S). Membranes were washed with TBST and incubated with HRP secondary (Santa Cruz Biotechnology) for 1 h at room temperature. Membranes were then washed and developed with Pierce ECL Plus Western Blotting Substrate (ThermoFisher). Membranes were imaged on a Typhoon FLA 7000 (Amersham). All quantifications were performed in ImageStudioLite (LI-Cor).
Statistics
Statistics were completed using Prism 8. Physiological measures of body weight/composition and food consumption were measured within sex via a Repeated Measures, 3-Way ANOVA with post-hoc multiple comparisons performed with the False Discovery Rate set Q = 0.05. All other tests were performed using 2-Way ANOVA within each sex with post hoc tests to assess diet effect within genotype, Sidac corrected. Energy Expenditure was analyzed with the “car” package in R to perform an ANCOVA controlling for lean body weight as a covariate.
Supplementary Information
Acknowledgements
We would also like to acknowledge the experimental assistance of Yuhong Liu and Jodie Cropper throughout this study, and Dr. Jonathan Dorigatti for experimental assistance and helpful discussions. Milliplex analyte panels were performed by Bioanalytics and Single-Cell (BASiC) Core at UT-Health San Antonio. Metabolic cage assessments were performed by the Integrated Physiology of Aging Core at the San Antonio Nathan Shock Center (P30 AG013319). This research was funded in part by R01 AG050797, R01 AG057431, T32 AG021890 and the San Antonio Area Foundation. ABS is partially supported by the Geriatric Research, Education and Clinical Center of the South Texas Veterans Health Care System. This material is the result of work supported with resources and the use of facilities at South Texas Veterans Health Care System, San Antonio, Texas. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Author contributions
Study was formulated by A.B.S. and K.M.T. Data was collected and analyzed by K.M.T. Figures and manuscript drafts were prepared by K.M.T. A.B.S. and K.M.T. reviewed, edited, and approved the manuscript.
Data availability
The data presented in the work are available from the corresponding author upon request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-08978-4.
References
- 1.Richie JP, Jr, et al. Methionine restriction increases blood glutathione and longevity in F344 rats. FASEB. 1994;8:1302–1307. doi: 10.1096/fasebj.8.15.8001743. [DOI] [PubMed] [Google Scholar]
- 2.Miller RA, et al. Methionine-deficient diet extends mouse lifespan, slows immune and lens aging, alters glucose, T4, IGF-I and insulin levels, and increases hepatocyte MIF levels and stress resistance. Aging Cell. 2005;4:119–125. doi: 10.1111/j.1474-9726.2005.00152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun L, Akha AAS, Miller RA, Harper JM. Life-span extension in mice by preweaning food restriction and by methionine restriction in middle age. J. Gerontol. A. Biol. Sci. Med. Sci. 2009;64A:711–722. doi: 10.1093/gerona/glp051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guerra BA, et al. Dietary sulfur amino acid restriction upregulates DICER to confer beneficial effects. Mol. Metab. 2019;29:124–135. doi: 10.1016/j.molmet.2019.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grant L, et al. Methionine restriction improves renal insulin signalling in aged kidneys. Mech. Aging Dev. 2016;157:35–43. doi: 10.1016/j.mad.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Lees EK, et al. Methionine restriction restores a younger metabolic phenotype in adult mice with alterations in fibroblast growth factor 21. Aging Cell. 2014;13:817–827. doi: 10.1111/acel.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swaminathan A, Fokin A, Venckūnas T, Degens H. Methionine restriction plus overload improves skeletal muscle and metabolic health in old mice on a high fat diet. Sci. Rep. 2021;11:1260. doi: 10.1038/s41598-021-81037-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ables GP, Perrone CE, Orentreich D, Orentreich N. Methionine-restricted C57BL/6J mice are resistant to diet-induced obesity and insulin resistance but have low bone density. PLoS ONE. 2012;7:e51357. doi: 10.1371/journal.pone.0051357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stone KP, Wanders D, Orgeron M, Cortez CC, Gettys TW. Mechanisms of increased in vivo insulin sensitivity by dietary methionine restriction in mice. Diabetes. 2014;63:3721–3733. doi: 10.2337/db14-0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gomez A, et al. Cysteine dietary supplementation reverses the decrease in mitochondrial ROS production at complex I induced by methionine restriction. J. Bioenerg. Biomembr. 2015;47:199–208. doi: 10.1007/s10863-015-9608-x. [DOI] [PubMed] [Google Scholar]
- 11.Ying Y, et al. Dietary l-methionine restriction decreases oxidative stress in porcine liver mitochondria. Exp. Gerontol. 2015;65:35–41. doi: 10.1016/j.exger.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Sanchez-Roman I, et al. Effects of aging and methionine restriction applied at old age on ROS generation and oxidative damage in rat liver mitochondria. Biogerontology. 2012;13:399–411. doi: 10.1007/s10522-012-9384-5. [DOI] [PubMed] [Google Scholar]
- 13.Caro P, et al. Forty percent and eighty percent methionine restriction decrease mitochondrial ROS generation and oxidative stress in rat liver. Biogerontology. 2008;9:183–196. doi: 10.1007/s10522-008-9130-1. [DOI] [PubMed] [Google Scholar]
- 14.Sanchez-Roman I, et al. Forty percent methionine restriction lowers DNA methylation, complex I ROS generation, and oxidative damage to mtDNA and mitochondrial proteins in rat heart. J. Bioenerg. Biomembr. 2011;43:699–708. doi: 10.1007/s10863-011-9389-9. [DOI] [PubMed] [Google Scholar]
- 15.Sanz A, et al. Methionine restriction decreases mitochondrial oxygen radical generation and leak as well as oxidative damage to mitochondrial DNA and proteins. FASEB J. 2006;20:1064–1073. doi: 10.1096/fj.05-5568com. [DOI] [PubMed] [Google Scholar]
- 16.Patil YN, Dille KN, Burk DH, Cortez CC, Gettys TW. Cellular and molecular remodeling of inguinal adipose tissue mitochondria by dietary methionine restriction. J. Nutr. Biochem. 2015;26:1235–1247. doi: 10.1016/j.jnutbio.2015.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forney LA, et al. Sexually dimorphic effects of dietary methionine restriction are dependent on age when the diet is introduced. Obesity. 2020;28:581–589. doi: 10.1002/oby.22721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hasek BE, et al. Dietary methionine restriction enhances metabolic flexibility and increases uncoupled respiration in both fed and fasted states. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;299:R728–R739. doi: 10.1152/ajpregu.00837.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wanders D, et al. FGF21 Mediates the Thermogenic and Insulin-Sensitizing Effects of Dietary Methionine Restriction but Not Its Effects on Hepatic Lipid Metabolism. Diabetes. 2017;66:858–867. doi: 10.2337/db16-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wanders D, et al. Role of GCN2-independent signaling through a noncanonical PERK/NRF2 pathway in the physiological responses to dietary methionine restriction. Diabetes. 2016;65:1499–1510. doi: 10.2337/db15-1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plaisance EP, et al. Role of β-adrenergic receptors in the hyperphagic and hypermetabolic responses to dietary methionine restriction. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2010;299:R740–R750. doi: 10.1152/ajpregu.00838.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forney LA, Wanders D, Stone KP, Pierse A, Gettys TW. Concentration-dependent linkage of dietary methionine restriction to the components of its metabolic phenotype: concentration dependence of methionine restriction. Obesity. 2017;25:730–738. doi: 10.1002/oby.21806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kozieł R, et al. Methionine restriction slows down senescence in human diploid fibroblasts. Aging Cell. 2014;13:1038–1048. doi: 10.1111/acel.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pettit AP, et al. Dietary methionine restriction regulates liver protein synthesis and gene expression independently of eukaryotic initiation factor 2 phosphorylation in mice. J. Nutr. 2017;147:1031–1040. doi: 10.3945/jn.116.246710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sikalidis AK, Mazor KM, Kang M, Liu H, Stipanuk MH. Total 4EBP1 Is elevated in liver of rats in response to low sulfur amino acid intake. J. Amino Acids. 2013;2013:1–11. doi: 10.1155/2013/864757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nichenametla SN, Mattocks DAL, Malloy VL, Pinto JT. Sulfur amino acid restriction-induced changes in redox-sensitive proteins are associated with slow protein synthesis rates: glutathione redox status and protein synthesis rates. Ann. N. Y. Acad. Sci. 2018;1418:80–94. doi: 10.1111/nyas.13556. [DOI] [PubMed] [Google Scholar]
- 27.Jonsson WO, et al. Physiologic responses to dietary sulfur amino acid restriction in mice are influenced by Atf4 status and biological sex. J. Nutr. 2021;151:785–799. doi: 10.1093/jn/nxaa396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruckenstuhl C, et al. Lifespan extension by methionine restriction requires autophagy-dependent vacuolar acidification. PLoS Genet. 2014;10:e1004347. doi: 10.1371/journal.pgen.1004347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hine C, et al. Endogenous hydrogen sulfide production is essential for dietary restriction benefits. Cell. 2015;160:132–144. doi: 10.1016/j.cell.2014.11.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mattocks DAL, et al. Short term methionine restriction increases hepatic global DNA methylation in adult but not young male C57BL/6J mice. Exp. Gerontol. 2016;88:1–8. doi: 10.1016/j.exger.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gao X, et al. Dietary methionine influences therapy in mouse cancer models and alters human metabolism. Nature. 2019;572:397–401. doi: 10.1038/s41586-019-1437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tamanna N, Mayengbam S, House JD, Treberg JR. Methionine restriction leads to hyperhomocysteinemia and alters hepatic H2S production capacity in Fischer-344 rats. Mech. Ageing Dev. 2018;176:9–18. doi: 10.1016/j.mad.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 33.Zhao H, Kim G, Levine RL. Methionine sulfoxide reductase contributes to meeting dietary methionine requirements. Arch. Biochem. Biophys. 2012;522:37–43. doi: 10.1016/j.abb.2012.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown-Borg HM, et al. Growth hormone signaling is necessary for lifespan extension by dietary methionine. Aging Cell. 2014;13:1019–1027. doi: 10.1111/acel.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uthus EO, Brown-Borg HM. Methionine flux to transsulfuration is enhanced in the long living Ames dwarf mouse. Mech. Aging Dev. 2006;127:444–450. doi: 10.1016/j.mad.2006.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown-Borg HM, Rakoczy S, Wonderlich JA, Armstrong V, Rojanathammanee L. Altered dietary methionine differentially impacts glutathione and methionine metabolism in long-living growth hormone-deficient Ames dwarf and wild-type mice. Longev. Heal. 2014;3:10. doi: 10.1186/2046-2395-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bentley R. Methionine and derivatives: exploring chirality at sulfur. Biochem. Mol. Biol. Educ. 2005;33:274–276. doi: 10.1002/bmb.2005.49403304274. [DOI] [Google Scholar]
- 38.Ciorba MA, Heinemann SH, Weissbach H, Brot N, Hoshi T. Modulation of potassium channel function by methionine oxidation and reduction. Proc. Natl. Acad. Sci. 1997;94:9932–9937. doi: 10.1073/pnas.94.18.9932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gao J, et al. Loss of conformational stability in calmodulin upon methionine oxidation. Biophys. J. 1998;74:1115–1134. doi: 10.1016/S0006-3495(98)77830-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ciorba MA, Heinemann SH, Weissbach H, Brot N, Hoshi T. Regulation of voltage-dependent K + channels by methionine oxidation: effect of nitric oxide and vitamin C. FEBS Lett. 1999;442:48–52. doi: 10.1016/S0014-5793(98)01616-0. [DOI] [PubMed] [Google Scholar]
- 41.Dow LK, Changela A, Hefner HE, Churchill MEA. Oxidation of a critical methionine modulates DNA binding of the Drosophila melanogaster high mobility group protein HMG-D. FEBS Lett. 1997;414:514–520. doi: 10.1016/S0014-5793(97)01059-4. [DOI] [PubMed] [Google Scholar]
- 42.Fricke TC, et al. Oxidation of methionine residues activates the high-threshold heat-sensitive ion channel TRPV2. Proc. Natl. Acad. Sci. 2019;116:24359–24365. doi: 10.1073/pnas.1904332116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Salmon AB, et al. Lack of methionine sulfoxide reductase A in mice increases sensitivity to oxidative stress but does not diminish life span. FASEB J. 2009;23:3601–3608. doi: 10.1096/fj.08-127415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Styskal J, et al. Methionine sulfoxide reductase A affects insulin resistance by protecting insulin receptor function. Free Radic. Biol. Med. 2013;56:123–132. doi: 10.1016/j.freeradbiomed.2012.10.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hunnicut J, Liu Y, Richardson A, Salmon AB. MsrA overexpression targeted to the mitochondria, but not cytosol, preserves insulin sensitivity in diet-induced obese mice. PLoS ONE. 2015;10:e0139844. doi: 10.1371/journal.pone.0139844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Elshorbagy AK, et al. Cysteine supplementation reverses methionine restriction effects on rat adiposity: signifi cance of stearoyl-coenzyme A desaturase. J. Lipid Res. 2011;52:104–112. doi: 10.1194/jlr.M010215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hens JR, et al. Methionine-restricted diet inhibits growth of MCF10AT1-derived mammary tumors by increasing cell cycle inhibitors in athymic nude mice. BMC Cancer. 2016;16(1):1–13. doi: 10.1186/s12885-016-2367-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Malloy VL, et al. Methionine restriction decreases visceral fat mass and preserves insulin action in aging male Fischer 344 rats independent of energy restriction. Aging Cell. 2006;5:305–314. doi: 10.1111/j.1474-9726.2006.00220.x. [DOI] [PubMed] [Google Scholar]
- 49.Nichenametla SN, Mattocks DAL, Malloy VL. Age-at-onset-dependent effects of sulfur amino acid restriction on markers of growth and stress in male F344 rats. Aging Cell. 2020;19(7):e13177. doi: 10.1111/acel.13177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fomenko DE, et al. MsrB1 (Methionine-R-sulfoxide Reductase 1) knock-out mice: roles OF MsrB1 in redox regulation and identification of a novel selenoprotein form. J. Biol. Chem. 2009;284:5986–5993. doi: 10.1074/jbc.M805770200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lai L, et al. Loss of methionine sulfoxide reductases increases resistance to oxidative stress. Free Radic. Biol. Med. 2019;145:374–384. doi: 10.1016/j.freeradbiomed.2019.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kumar RA, Koc A, Cerny RL, Gladyshev VN. Reaction mechanism, evolutionary analysis, and role of zinc in drosophila methionine-R-sulfoxide reductase. J. Biol. Chem. 2002;277:37527–37535. doi: 10.1074/jbc.M203496200. [DOI] [PubMed] [Google Scholar]
- 53.Sreekumar PG. Methionine sulfoxide reductase A: Structure, function and role in ocular pathology. World J. Biol. Chem. 2011;2:184. doi: 10.4331/wjbc.v2.i8.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brennan LA, Lee W, Giblin FJ, David LL, Kantorow M. Methionine sulfoxide reductase A (MsrA) restores α-crystallin chaperone activity lost upon methionine oxidation. Biochim. Biophys. Acta BBA Gen. Subj. 2009;1790:1665–1672. doi: 10.1016/j.bbagen.2009.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gabbita SP, Aksenov MY, Lovell MA, Markesbery WR. Decrease in peptide methionine sulfoxide reductase in Alzheimer’s disease brain. J. Neurochem. 2002;73:1660–1666. doi: 10.1046/j.1471-4159.1999.0731660.x. [DOI] [PubMed] [Google Scholar]
- 56.Martín J-E, et al. Identification of the oxidative stress-related gene MSRA as a rheumatoid arthritis susceptibility locus by genome-wide pathway analysis. Arthritis Rheum. 2010;62:3183–3190. doi: 10.1002/art.27648. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in the work are available from the corresponding author upon request.