Abstract
Bilateral elbow dislocation associated with bilateral distal forearm fractures is extremely rare, therefore its optimal treatment, complications, and outcomes remain unclear. We present an illustrative case with a 2‐year follow up of a patient who sustained a complex injury of the upper extremity and underwent combined surgical and conservative treatment.
Keywords: bilateral elbow dislocation, bilateral radius and ulna fracture, ligament reconstruction, rehabilitation, treatment
Due to the limited information regarding complex bilateral injuries of the arm, its optimal therapy remains unclear. The major treatment goal should be a joint stabilization and early mobilization to optimize the chances of good functional recovery.

1. INTRODUCTION
The elbow is considered to be one of the most stable joints in the human body. Nevertheless, unilateral elbow dislocations are the second most common major joint dislocation, with a reported incidence of 5.21 dislocations per 100.000 people/year in the US population. 1 Contrarily, bilateral elbow dislocation (BED) is an extremely rare injury with only 20 reported cases. 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 The above‐mentioned includes 11 bilateral elbow dislocations associated with a skeletal injury, none of which describe associated bilateral fracture of the distal forearm. Complications after unilateral elbow dislocation are common and include residual pain, chronic stiffness, heterotopic ossifications, and functional instability, which can enhance early arthrosis and lead to permanent incapacity to work. 21 , 22 Due to the limited information regarding complex bilateral injuries of the upper extremity, its optimal therapy, complications, and outcomes remain unclear. We present an illustrative case of a patient who sustained BED associated with bilateral forearm fractures. After combined conservative and surgical treatment at 2‐year follow‐up, the patient has recovered uneventfully and fully returned to his working and recreational activities.
2. CASE PRESENTATION
A 39‐year‐old fit and otherwise healthy male soldier was admitted to the emergency department after a fall from a 3‐meter height, predominantly landing to the outstretched hands and lower back. Clinical examination revealed bilateral elbow and distal forearm deformity with a small wound (Gustilo‐Anderson type I) on the ulnar side of the right radiocarpal joint. The neurovascular status of both arms was unremarkable. Initial radiographs showed bilateral elbow dislocations with associated right lateral epicondyle avulsion fracture and bilateral impacted comminuted fractures of distal radius and ulna (Figure 1).
FIGURE 1.
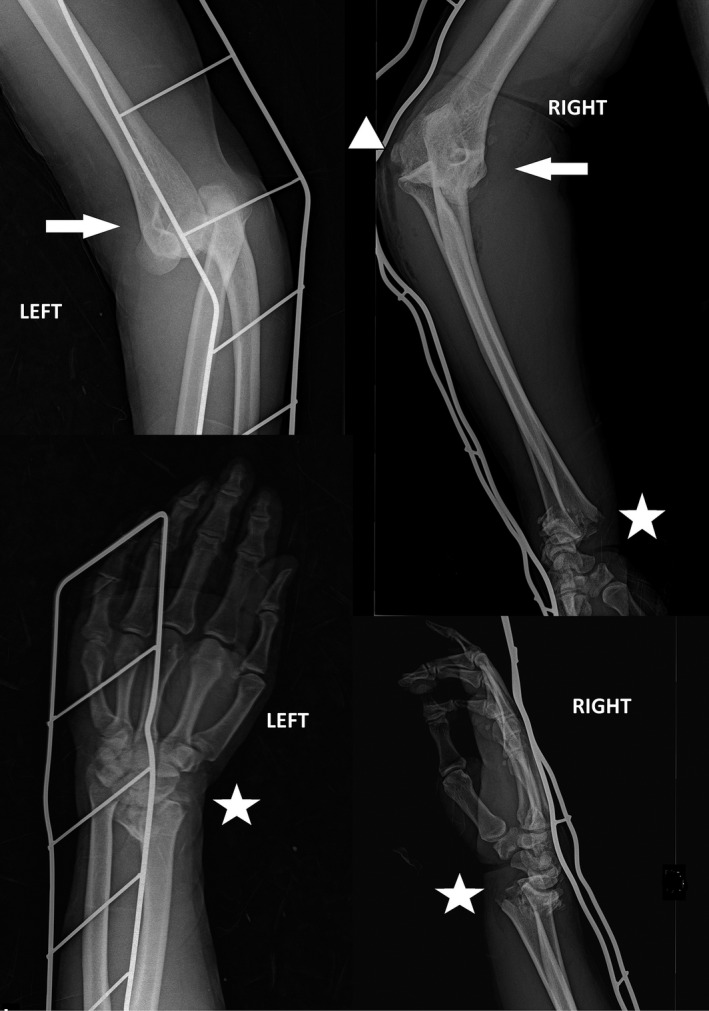
Initial radiographs in the atypical position taken at the emergency department showing bilateral elbow dislocations (white arrows) with associated right lateral epicondyle avulsion fracture (white triangle) and bilateral impacted comminuted fractures of distal radius and ulna (white stars)
The injuries were treated in two stages. In the first stage, under general anesthesia and using the image intensifier, a closed reduction of both elbows and distal forearms was performed, followed by proper wound care and antibiotic prophylaxis. The left elbow showed only valgus stress instability, so posterior elbow splint in 90° flexion with a forearm in the neutral rotation was applied. Contrarily, the right elbow showed multidirectional instability and its congruency was retained by temporarily ulnohumeral transfixation with a titanium Kirschner wire and the above‐elbow cast with a forearm in the neutral rotation. Proper bilateral post‐reduction position of both distal radius and ulna was retained with Kirschner wires and a cast with “window” at a wound location.
After closed reduction and immobilization of both elbows, the CT and MRI were obtained, which revealed further injuries. On the left elbow, an avulsion of the lateral epicondylar origin of the lateral collateral ligament (LCL) and a partially ruptured medial collateral ligament (MCL) were verified. On the right elbow, complete ruptures of both collateral ligaments and completely ruptured joint capsule were accompanied to a nondisplaced radial head fracture (Figures 2 and 3).
FIGURE 2.

Postreduction MSCT of the left elbow (A, B). The white arrow indicates an avulsion fracture of the lateral epicondyle in the coronal (A) and sagittal plane (B). Postreduction MSCT of the right elbow in atypical position (C). The white arrows indicate avulsion fractures of both epicondyles in the coronal plane (C). White star—lateral epicondyle
FIGURE 3.
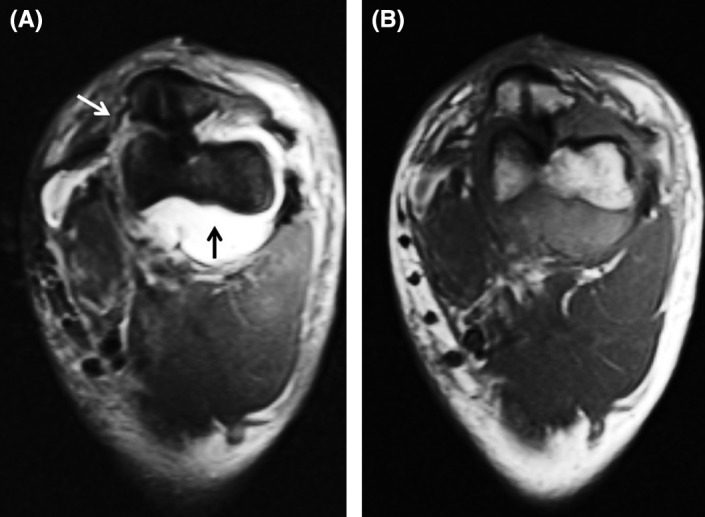
Postreduction MRI of the right elbow in atypical projections (because its congruency was retained temporarily by ulnohumeral transfixation due to its multidirectional instability). The fat‐suppressed proton‐density‐weighted TSE sequence. White arrow points to the medial collateral ligament rupture, and the black arrow points to the intraarticular effusion (A). T1 sequence of the same projection (B)
In the second stage, a day after the injury, a definitive surgical stabilization of multi‐directionally unstable right elbow was performed. Under general anesthesia, the right elbow was approached through Kocher interval. A complete rupture of the LCL complex and the rupture of the joint capsule was verified. A radial head was fractured on its lateral side in supination. The fragment was small (<25% of the radial head) and comminuted and therefore unable to fixate so it was evacuated. Ligamentous reconstruction was done using three 2.4 mm × 7.5 mm suture anchors (FASTak Arthrex) and non‐absorbable sutures. The humeral anchor was positioned on the lateral epicondyle to the “footprint” of the lateral ulnar collateral ligament (LUCL), while ulnar anchors were placed to the proximal part of the supinator crest (Figure 4). LUCL, which was avulsed at its proximal origin, was reconstructed and additionally sutured throughout its distal origin using ulnar anchors. The annular ligament and radial collateral ligament were reconstructed with non‐absorbable sutures. Lastly, the joint capsule was plicated. Intraoperatively, the elbow was congruent and stable throughout a full range of motion under the image intensifier. A posterior elbow splint in 90° flexion with a forearm in the neutral rotation was applied (Figure 5).
FIGURE 4.

Picture showing the intraoperative placement of the suture anchor in the ulna. The ruptured annular ligament is secured on the stay suture (ANL). Black star—lateral epicondyle, ANC, anconeus muscle; EDC, extensor digitorum communis muscle; EDU, extensor carpi ulnaris muscle
FIGURE 5.
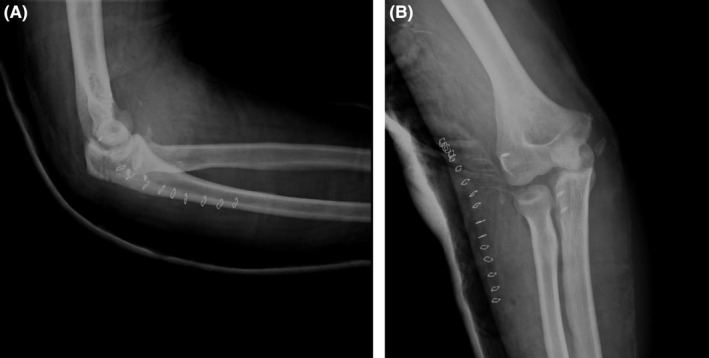
Lateral (A) and anteroposterior (B) postoperative radiographs of the right elbow showing concentric reduction with the surgical hardware in place
The patient was discharged a week postoperatively (post‐op) with the right elbow and radiocarpal joint immobilized with the above‐elbow cast in 90° flexion and forearm in neutral rotation.
The left elbow was in a hinged elbow brace which allowed a full range of motion, and the left radiocarpal joint was immobilized with below elbow cast. Indometacin (3 × 25 mg) with gastroprotection was recommended for 5 weeks as heterotopic ossification prevention. Two weeks post‐op, a hinged brace allowing full flexion and 60° extension was applied to the right elbow with radiocarpal joint immobilized with below elbow cast. Three‐week post‐op right elbow was allowed full extension, while the left elbow was allowed a full range of motion without any support. Also, Kirschner wires were removed. Five‐week post‐op right elbow orthosis and both below elbow casts were removed which was followed by a full range of motion and vigorous physiotherapy. The mainstay of the physical therapy program was elbow range of motion and strength exercises. At 2, 4, and 6 months follow‐up, the patient reported a painless range of motion and no instability problems. He also reported restriction of supination and palmar flexion on the right side, which improves with exercising.
Two years postoperatively, patient has bilateral painless 0°–140° flexion elbow range of motion with no restriction of pronation/supination on the left side and restriction of terminal supination on the right side. The bilateral wrist range of motion is also painless with 50° flexion and 75° extension on the right side and 65° flexion and 75° extension on the left side (Figure 6). Radiologically, there are initial signs of heterotopic ossifications, although its prophylaxis was carried out, but no signs of early arthrosis (Figure 7). The Disabilities of the Arm, Shoulder and Hand (DASH) score is 0.9 for the left and 1.7 for the right arm. The Mayo Elbow score is 100 bilaterally, and Mayo Wrist Score is 100 for the left and 90 for the right wrist. By the time of examination, 2 years post‐op, the patient is fully back to service and recreational activities without any limitation (Video S1).
FIGURE 6.

Patient at the 2‐year follow‐up showing a full bilateral range of elbow and radiocarpal motion with restriction of right supination and palmar flexion
FIGURE 7.

Two‐year follow‐up radiographs showing congruent elbow joints with surgical hardware in place (white arrows) and the presence of some ossific fragments (white stars) although prophylaxis of heterotopic ossifications was carried out. Distal radius bilaterally shows loss of alignment although the patient is functionally almost fully recovered
3. DISCUSSION
Bilateral elbow dislocation (BED) is a rare injury with only 20 reported cases to the present moment. That includes 9 isolated BED (7 adult and 2 pediatric) 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 and 10 BED associated with a skeletal injury (7 adult and 5 pediatric). 7 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 None of the cases sustained a BED associated with bilateral forearm fracture which makes the reported case unique. Elbow is one of the most stable joints, which at the same time allows a high range of forearm motion. With bony and capsuloligamentous structures as primary and joint‐crossing muscles as secondary stabilizing factors, a high force is necessary to dislocate the joint. 23 Biomechanical studies have shown that bony structures serve as the main stabilizers, limiting flexion/extension movements and stabilizing elbow in varus/valgus stress during rotational movements. In varus stress, stability mostly relies on bony structures, while valgus stability depends on ligaments as well as on bony structures. 24 , 25 Elbow dislocation requires prompt reduction followed by stability tests and neurovascular examination which would determine whether conservative treatment is sufficient or surgery is required. In doubtful cases, a CT or MRI can be done.
After the posterior dislocation, the elbow is usually more stable in flexion. For this reason, the elbow should be immobilized in at least 90° flexion. Moreover, biomechanical studies suggest that the LCL complex is torn in almost all elbow dislocations. For this reason, the elbow with sufficient MCL complex (and insufficient LCL) should be immobilized with the forearm in pronation which engages the lateral secondary elbow constraints, the wrist extensor origins and consequently provides more stability. When both LCL and MCL are torn, the forearm should be positioned in neutral to unload the both lateral and medial sides. In the situation when LCL is sufficient and MCL insufficient, the elbow should be immobilized in supination which would engage the medial secondary elbow constraints, the flexor‐pronator mass and therefore ensure more stability.
Surgical indications include complex dislocations with associated fractures, an osteochondral fragment, soft‐tissue entrapment which prevents concentric reduction, and open or neurovascular injury.
The primary objective of all therapeutic options is early mobilization. Interestingly, there is a lack of evidence that would specify the best time for mobilization after conservative or surgical treatment of elbow fractures in adults. 26 Elbows which are unstable after reduction due to torn capsuloligamentous structures need to be stabilized surgically. There is still debate among authors which intervention is optimal as some propose only ligament reconstruction 23 , 27 and other combination of ligament reconstruction and hinged fixator. 28 Furthermore, good outcomes are reported with hinged fixator only. 7 Our experience supports capsuloligamentous reconstruction followed by early mobilization as a reliable treatment for multidirectional elbow instability due to complex elbow dislocation. Complications after elbow injuries are common and difficult to treat. 29 Anakwe et al 21 showed that even simple elbow dislocations are not benign injuries with long‐term mean DASH score of 6,7 and high rate of residual pain and elbow stiffness. Also, the authors state that functional instability is not common and often does not limit activities which is supported by the presented case. Our patient reported no residual pain and stiffness bilaterally with a significantly lower DASH score, although he sustained a complex injury of the right elbow and additional bilateral complex forearm fractures.
Even isolated bilateral distal forearm fracture is a rare injury, with only a handful of case reports. 30 , 31 , 32 , 33 , 34 Whereas therapeutic options and outcomes of unilateral distal radius fracture (DRF) are well known, 35 due to limited information regarding bilateral DRF, its optimal therapy, complications, and outcomes remain unclear. The treatment goal is to retain optimal reduction and stability, which would allow early mobilization to achieve the best functional result. Depending on the fracture type and the associated injuries, distal forearm fractures can be treated conservatively with closed reduction and cast fixation or surgically using one of the available methods. Surgical treatment includes reduction in the fracture and fixation with the Kirschner wires or open reduction and internal fixation using plate and screws by the AO method. For the open or highly comminuted fractures, external fixation can be used. A recent retrospective study of 10 bilateral radius fractures treated with open reduction and internal fixation showed complications in one‐half of the patients after a mean 2.4‐year follow‐up. 36
As there are no standardized and evidence‐based protocols for the treatment of complex bilateral upper extremity injuries, a question remains whether something could have been done differently. Both distal radial fractures could have been treated with open reduction and internal fixation using plates and screws, but our idea was to use minimally invasive methods to yield the best result. So, the main goal was to reduce and stabilize all joints which would allow early rehabilitation. Our patient suffered no complications and recovered uneventfully which supports our treatment choice and rehabilitation protocol. Rare complex injuries such as BED associated with bilateral forearm fractures should not lessen the need for standardized treatment protocols, so patients could get the best possible care.
4. CONCLUSION
Due to the limited information regarding complex bilateral injuries of the upper extremity, its optimal therapy remains unclear. Treatment of bilateral complex elbow dislocation associated with bilateral distal forearm fractures should be focused on the unstable elbow. The treatment goal should be elbow stability and early mobilization. Other injuries should be treated with minimally invasive methods which would, together with the stabilized elbow, allow early and vigorous rehabilitation to yield the best possible functional upper extremity result.
CONFLICT OF INTEREST
The author(s) declare(s) that there is no conflict of interest.
AUTHOR CONTRIBUTION
Dino Bobovec, Daniel Rajačić, Tomislav Žigman, and Ivan Dobrić contributed to the design and implementation of the research, analysis of the results, and writing of the manuscript.
ETHICAL APPROVAL
1) This material is the authors' own original work, which has not been previously published elsewhere. 2) The paper is not currently being considered for publication elsewhere. 3) The paper reflects the authors' own research and analysis in a truthful and complete manner.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Supporting information
Video S1
ACKNOWLEDGEMENTS
None.
Bobovec D, Rajačić D, Žigman T, Dobrić I. Good functional recovery after bilateral elbow dislocation associated with bilateral distal radius and ulna fractures. Clin Case Rep. 2022;10:e05439. doi: 10.1002/ccr3.5439
Funding information
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article
DATA AVAILABILITY STATEMENT
Data available within the article or its supplementary materials.
REFERENCES
- 1. Stoneback JW, Owens BD, Sykes J, et al. Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am. 2012;94(3):240‐245. [DOI] [PubMed] [Google Scholar]
- 2. Schonbauer HR. Simultaneous, bilateral dislocation of the elbow. Monatsschr Unfallheilkd Versicherungsmed. 1957;60(4):119‐121. [PubMed] [Google Scholar]
- 3. Klever H. Congruent simultaneous dislocations of the elbow. Monatsschr Unfallheilkd Versicherungsmed. 1961;64:190‐192. [PubMed] [Google Scholar]
- 4. Oury JH, Roe RD, Laning RC. A case of bilateral anterior dislocations of the elbow. J Trauma. 1972;12(2):170‐173. [DOI] [PubMed] [Google Scholar]
- 5. Maitra AK. A rare case of bilateral simultaneous posterior dislocation of the elbow. Br J Clin Pract. 1979;33(8):233‐235. [PubMed] [Google Scholar]
- 6. Wilson A. Bilateral elbow dislocation. Aust N Z J Surg. 1990;60(7):553‐554. [DOI] [PubMed] [Google Scholar]
- 7. Koslowsky TC, Mader K, Siedek M, et al. Treatment of bilateral elbow dislocation using external fixation with motion capacity: a report of 2 cases. J Orthop Trauma. 2006;20(7):499‐502. [DOI] [PubMed] [Google Scholar]
- 8. Monka M, Ohoya Etsaka TO, Ngatse OKOA, et al. Bilateral traumatic dislocation of the elbow in a case and review of the literature. Int J Orthop Sci. 2018;4(4):762‐763. [Google Scholar]
- 9. Holloway NJ, Shanker H, Campbell AC. Bilateral posterior elbow dislocation with heterotopic ossification in a child. Injury Extra. 2006;37:56‐59. [Google Scholar]
- 10. Kovrizhnyĭ VG, Savvin EM. A case of simultaneous bilateral luxation in the elbow joint. Klin Khir. 1969;5:65. [PubMed] [Google Scholar]
- 11. Syed AA, O'Flanagan J. Simultaneous bilateral elbow dislocation in an international gymnast. Br J Sports Med. 1999;33(2):132‐133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Raman R, Srinivasan K, Matthews SJ, et al. Bilateral radial head fractures with elbow dislocation. Orthopedics. 2005;28(5):503‐505. [DOI] [PubMed] [Google Scholar]
- 13. Romero Pérez B, Marcos García A, Medina Henríquez JA, et al. Bilateral elbow dislocation related to essex‐lopresti injury. Rev Esp Cir OrtopTraumatol. 2012;56(1):59‐62. [DOI] [PubMed] [Google Scholar]
- 14. Reckers LJ, Raymundo JLP, Locks R. Elbow bilateral lateral dislocation. Acta Ortop Bras. 2006;14(1):42‐43. [Google Scholar]
- 15. Hui KS. Report of a pregnant lady with bilateral elbow dislocation caused by acute fall injury. J Acute Disease. 2015;4(2):155‐157. [Google Scholar]
- 16. Bauer S, Dunne B, Whitewood C. Simultaneous bilateral elbow dislocation with bilateral medial epicondyle fractures in a 13‐year‐old female gymnast with hyperlaxity. Case Rep. 2012;2012:bcr2012006972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jlalia Z, Abid H, Kamoun K, et al. Bilateral terrible triad of elbow: a pediatric case report. Ann Clin Case Rep. 2016;1:1191. [Google Scholar]
- 18. Sybert MW, Hennrikus WL. Bilateral medial epicondyle fractures with elbow dislocations in an adolescent female athlete. Trauma. 2017;19(2):142‐145. [Google Scholar]
- 19. Jensen UH, Rud B. Bilateral dislocation of the elbows. Ugeskr Laeg. 1983;145:1784. [PubMed] [Google Scholar]
- 20. Tayob AA, Shively RA. Bilateral elbow dislocations with intra‐articular displacement of the medial epicondyles. J Trauma. 1980;20(4):332‐335. [DOI] [PubMed] [Google Scholar]
- 21. Anakwe RE, Middleton SD, Jenkins PJ, et al. Patient‐reported outcomes after simple dislocation of the elbow. J Bone Joint Surg Am. 2011;93(13):1220‐1226. [DOI] [PubMed] [Google Scholar]
- 22. He SK, Yi M, Zhong G, et al. Appropriate excision time of heterotopic ossification in elbow caused by trauma. Acta Orthop Traumatol Turc. 2018;52(1):27‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. O’Driscoll SW, Jupiter JB, King GJ, et al. The unstable elbow. Instr Course Lect. 2001;50:89‐102. [PubMed] [Google Scholar]
- 24. Morrey BF, An K‐N. Stability of the elbow: osseous constraints. J Shoulder Elbow Surg. 2005;14(1):174‐178. [DOI] [PubMed] [Google Scholar]
- 25. Callaway GH, Field LD, Deng XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79(8):1223‐1231. [DOI] [PubMed] [Google Scholar]
- 26. Harding P, Rasekaba T, Smirneos L, et al. Early mobilisation for elbow fractures in adults. Cochrane Database Syst Rev. 2011;6:CD008130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mittlmeier T, Beck M. Luxation des ellenbogengelenks des erwachsenen [Dislocation of the adult elbow joint]. Der Unfallchirurg. 2009;112(5):487‐505. [DOI] [PubMed] [Google Scholar]
- 28. Duckworth AD, Ring D, Kulijdian A, et al. Unstable elbow dislocations. J Shoulder Elbow Surg. 2008;17(2):281‐286. [DOI] [PubMed] [Google Scholar]
- 29. Gundes H, Selek Ö, Gok U, et al. The relation between elbow range of motion and patient satisfaction after open release of stiff elbow. Acta Orthop Traumatol Turc. 2017;51(4):303‐307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gumbs VL, Segal D, Halligan JB, et al. Bilateral distal radius and ulnar fractures in adolescent weight lifters. Am J Sports Med. 1982;10(6):375‐379. [DOI] [PubMed] [Google Scholar]
- 31. Ozkan K, Ugutmen E, Unay K, et al. Fractures of the bilateral distal radius and scaphoid: a case report. J Med Case Reports. 2008;2:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bjørnsen LP. Bilateral combined fractures of the scaphoid and distal radius in a 13‐year‐old male. Acta Orthop Belg. 2008;74(6):856‐859. [PubMed] [Google Scholar]
- 33. Stone N III, Karamitopoulos M, Edelstein D, et al. Bilateral distal radius fractures in a 12‐year‐old boy after household electrical shock: case report and literature summary. Case Rep Med. 2014;2014:235756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ravikumar TV, Rahul P, Grover A, Samorekar B. Bilateral distal radius fracture in third trimester of pregnancy with accelerated union: a rare case report. J Clin Diagn Res. 2015;9(4):RD01‐RD02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wang J, Lu Y, Cui Y, et al. Is volar locking plate superior to external fixation for distal radius fractures? A comprehensive meta‐analysis. Acta Orthop Traumatol Turc. 2018;52(5):334‐342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Graham JG, Penna S, Fletcher D, et al. Outcomes of open reduction and internal fixation of bilateral fractures of the distal radius. J Hand Microsurg. 2019;11(2):117‐120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1
Data Availability Statement
Data available within the article or its supplementary materials.


