The COVID-19 pandemic has affected countries differently depending on the resilience of the healthcare system in each country. The pandemic also revealed a lack of health emergency preparedness caused by inadequate healthcare system capacity in many low- and middle-income countries. Likewise, the COVID-19 pandemic revealed the frailty of the healthcare system in Mongolia.
Mongolia's capacity to detect, respond to and recover from emergency health threats remains underdeveloped, and is faced with a COVID-19 pandemic with no functional emergency response structure. Without a National Health Protection Agency backed by the legal framework to support and enable response to public health emergencies – organisations outside of health sector with distinct functions to respond to incidents of natural disasters and accidents led the pandemic response. Hence, Mongolia's response has been marred with problems of improper coordination between relevant ministries, inefficient resource allocation, poor use of human and other resources and a duplication of functions. Accordingly, the pandemic revealed Mongolia's need for a Centre for Disease Control and Prevention, or National Health Protection Agency. Such agencies are essential for building the foundation towards developing a system for health security and public health emergency management.
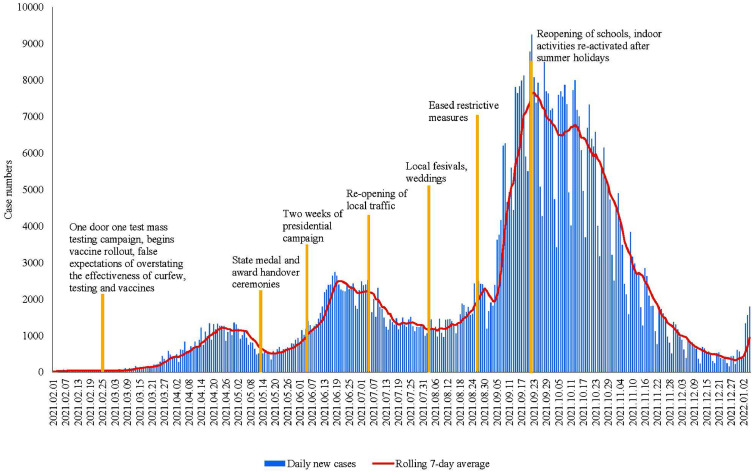
Regardless, the COVID-19 pandemic improved the country's supply of medical equipment and infrastructure substantially. As of November 2021, there was a 2 – 4-fold increase in the number of PCR machines, X-ray devices, and oxygen beds nationwide, compared to a year before. Similarly, Mongolia quickly enhanced international cooperation in the wake of the pandemic and received significant support from the World Bank, UNICEF, and Governments of Japan and United States to expand vaccination capacity against COVID-19 in the country. As of Jan 24, 2022, 71·8% of Mongolian population have been double vaccinated while 31% have received a booster dose helping reduce hospitalisations and deaths associated with the pandemic.1 The remarkably high vaccination rate was achieved through extensive vaccination campaigns and community engagement,2 providing infection updates initially through daily press briefings from the Ministry of Health, and currently, via an online portal with daily updates.3 A further incentive that gave impetus to the vaccination drive was the government initiative involving cash handout to every citizen who received a full dose of the COVID-19 vaccine.4 However, the high vaccination rate did not curb infection spread,5 and pandemic waves are seen to coincide with major policy shifts, political events and national celebrations (Figure 1).
Figure 1.
Daily new confirmed cases of COVID-19 in Mongolia.
With no operative integrated risk management plan in Mongolia, a combination of poorly structured authoritative bodies; decisions inconsistent with public health science; and community engagement approaches that treated the population as passive recipients rather than active participants of health response efforts increased the rates of burnout among healthcare workers, prompting a lack of public trust in the government's ability to handle the pandemic. While it seems compelling that the primary healthcare service and the National Centre for Communicable Diseases provide support for health surveillance, testing and contact tracing, community outreach and vaccine coverage in response to the pandemic; physicians are overburdened and unable to provide essential healthcare. Consequently, healthcare workers are often victims of social attacks and criticisms as a result of public distrust in the healthcare system. Notwithstanding, healthcare workers are forced to work with inadequate remuneration and uncertain legal protections.6 Although the government has repeatedly provided one-time benefits, a legislative act indicating a threefold increase in base salary for healthcare workers during a pandemic is not enforced. Therefore, it is necessary to establish and implement a comprehensive legal framework for working conditions of healthcare workers during outbreaks, and make provisions to improve their remuneration and capacity to respond during the current pandemic and in future health emergencies.
The most vital component for health emergency response in Mongolia remains increasing government expenditure on health, and prioritising government spending for maintaining real-time data-driven health emergency management systems. Currently, an electronic health surveillance monitor registers and reports confirmed cases and close contacts as soon as they are identified. However, the health surveillance databases are fragmented, thus precluding their use for urgent decision-making. Besides, creating sufficient contingency fund for health emergencies will prevent funds from being diverted from other government programs. As the healthcare system is underfinanced and unable to fully serve COVID-19 patients, government spending on diagnosis and treatment during the COVID-19 pandemic have been covered by the Health Insurance Fund, posing serious risks of disrupting essential health services.
Overall, the COVID-19 pandemic presented the most pressing needs for public health emergencies in the country. A policy shift towards those meaningful initiatives will help Mongolia better prepare the health security system, public health emergency preparedness, and response capacities in the country.
Author Contributions
AD conceived of the presented idea; BJ, TB, and BL co-developed the ideas for the paper; AD wrote the first draft in consultation with OB, TB, BJ, and BL; AD, BJ, OB reviewed and edited the draft; all authors read and approved the final draft.
Declaration of interests
We declare no competing interests.
Acknowledgments/funding
Authors wrote in their personal capacity; the views expressed in this paper are the authors' and not those of the Government of Mongolia. The authors received no financial support for the paper.
References
- 1.Dambadarjaa D., Altankhuyag G.E., Chandaga U., et al. Factors associated with COVID-19 vaccine hesitancy in Mongolia: a web-based cross-sectional survey. Int J Environ Res Public Health. 2021;18(24):12903. doi: 10.3390/ijerph182412903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bayasgalan T., Anuurad E., Byambaa E. COVID-19 and public health efforts in Mongolia: a lesson maybe learned? J Clin Transl Sci. 2020;5:e18. 1–2. [Google Scholar]
- 3.Ministry of Health. COVID-19 situation report. 2021. https://covid19.mohs.mn/p/cat/post/57/. Accessed 27 January, 2022.
- 4.Ministry of Finance. A decision has been made to reward citizens who receive two doses of the vaccine with 50,000MNT. 2021. https://ikon.mn/n/27ky. Accessed 27 January, 2021.
- 5.Chimeddorj B., Mandakh U., Le L.V., et al. SARS-CoV-2 seroprevalence in Mongolia: Results from a national population survey. Lancet Reg Health Western Pac. 2021;17 doi: 10.1016/j.lanwpc.2021.100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nyamsuren T.S., Jargalsaikhan T., Bayarmaa V., et al. Public perception and behavioural response during COVID-19 pandemic. Coronavirus Infection Research. 2021:49–57. [Google Scholar]