Abstract
Background: Inspired by intense challenges encountered by patients and clinicians, we examined the experiences of living with sarcoidosis in three of the hardest impacted English-speaking cities during the early COVID-19 pandemic: London, New Orleans, and New York. Methods: A multi-disciplinary, multi-national research team including 6 patient leaders conducted qualitative investigations with analyses rooted in grounded theory. Recruitment occurred by self-referral through patient advocacy groups. Results: A total of 28 people living with sarcoidosis participated. The majority of patients had multi-system and severe sarcoidosis. Dominant themes were consistent across groups with differences expressed in spirituality and government and health systems. Racial, gender, and able-bodied inequity were voiced regarding healthcare access and intervention, societal interactions, and COVID-19 exposure and contraction. Agreement regarding extreme disruption in care and communication created concern for disability and survival. Concerns of COVID-19 exposure triggering new sarcoidosis cases or exacerbating established sarcoidosis were expressed. Pre-COVID-19 impediments in sarcoidosis healthcare delivery, medical knowledge, and societal burdens were intensified during the pandemic. Conversely, living with sarcoidosis cultivated personal and operational preparedness for navigating the practicalities and uncertainties of the pandemic. Optimism prevailed that knowledge of sarcoidosis, respiratory, and multi-organ diseases could provide pathways for COVID-19-related therapy and support; however, remorse was expressed regarding pandemic circumstances to draw long-awaited attention to multi-organ system and respiratory conditions. Conclusion: Participants expressed concepts warranting infrastructural and scientific attention. This framework reflects pre- and intra-pandemic voiced needs in sarcoidosis and may be an agent of sensitization and strategy for other serious health conditions. A global query into sarcoidosis will be undertaken.
Keywords: sarcoidosis, patient-centered, multi-system, multi-organ, quality of life, chronic, disparities, COVID
KUDOS Statement
During the COVID-19 pandemic, both patients and clinicians experienced extreme challenges in providing and receiving sarcoidosis care. Further, patients with sarcoidosis had a unique experience of living in the COVID-19 pandemic as a vulnerable population.
In order to better understand and improve the quality of healthcare delivery and living, we convened a multi-national research team consisting of patient leaders, physicians, nurses, and therapists. We interviewed 28 patients recruited through sarcoidosis patient organizations in the 3 hardest impacted English-speaking cities during the early COVID-19 pandemic: London, New Orleans, and New York. The majority of participants had a multi-organ systems and severe sarcoidosis.
A great deal was learned to guide future healthcare delivery, disease management, and education. Among the many concepts expressed by the participants, there was great similarity across the 3 groups. The differences between the groups were in an expression of spirituality as well as in details of government and health systems.
Race, gender, and disability (including people with sarcoidosis) were voiced as inequities in healthcare access and intervention, societal respect, as well as disproportional COVID-19 exposure and contraction, with the expressed concern that these groups were at higher risk during the pandemic. There was clear agreement among all groups that there was an extreme disruption in care and communication and great concern that their diagnosis created survival disadvantage because of the disease biology and because they are less likely to receive life-saving treatment. These were thought to be true pre-COVID-19 but became overt during the pandemic.
The participants noted many crossover concepts between sarcoidosis and COVID-19. Some concepts related to whether COVID-19 infection could increase sarcoidosis disease activity or trigger new sarcoidosis cases, other concepts related to the biologic similarity of both being systemic multi-organ diseases mostly recognized for lung involvement. Many participants expressed struggles related to future health uncertainty, and lack of health professional knowledge.
Another similarity was that having sarcoidosis before the COVID-19 pandemic provided patients with experience to cope with the pandemic better than the general public. Many thought that the experience of people with sarcoidosis could help those living with multi-systemic effects of COVID-19.
Take-Home Message
People with sarcoidosis expressed infrastructural and scientific concepts that warrant close attention. There is perceived disparity in pre- and intra-pandemic of equity in healthcare access and in chance for survival. The pre- and intra-pandemic expressed needs of sarcoidosis patients may provide similar agency for other serious health conditions.
Introduction
Sarcoidosis is a systemic disease of granulomatous formation and aggregation in single or multiple organs, conferring a wide spectrum of multiple and diverse manifestations, symptoms, and severity. Disease burden is driven by inflammation which, if not self-limited or pharmacologically quelled, results in progressive, life-threatening damage, and fibrosis. The destructive capacity of sarcoidosis varies depending on the volume of granulomatous burden, organ/s involved, and location. For example, moderate granulomatous burden in cardiac muscle may be “clinically silent,” whereas miniscule aggregates crossing conduction pathways can cause fatal arrhythmias. Pulmonary, cutaneous, and ocular involvement are commonly recognized; while cardiac, neurological, gastrointestinal, and osseous manifestations are likely under-reported.
Several antigenic triggers are associated with sarcoidosis including mold, infectious and chemical exposures, with yet unknown influence on phenotype, genotypic interactions, or prognosis (1). The systemic inflammatory nature of active sarcoidosis can cause fever, fatigue/malaise, arthralgia/arthritis, atypical cutaneous, and other diffuse nonspecific manifestations challenging the ability to distinguish between active sarcoidosis and other concomitant diseases. Disease burden, immunosuppressive treatment, infection, and poor access to care worsen health outcomes.
COVID-19 is a mild to severe respiratory and multi-system illness transmitted chiefly by infectious respiratory droplets. COVID-19 is commonly characterized by fever, cough, and shortness of breath potentially progressing to respiratory failure. However, both in COVID-19's acute and chronic forms, multiple organ systems may be involved resulting in cutaneous, articular, neurological, cardiac, gastrointestinal, and hematological manifestations. The chronic form may be related to immune activation, long recovery, persistent residual damage to organ tissue as with sarcoidosis.
At the time of this publication, the literature lacks an investigation of sarcoidosis as experienced by patients in the COVID-19 pandemic. The stark initial challenges encountered by patients and clinicians in the early COVID-19 pandemic predominantly expressed through international, national, and local online support groups inspired this study. This study examines the experience of living with sarcoidosis in three of the hardest impacted regions during the early COVID-19 pandemic: London, New Orleans, and New York.
Methods
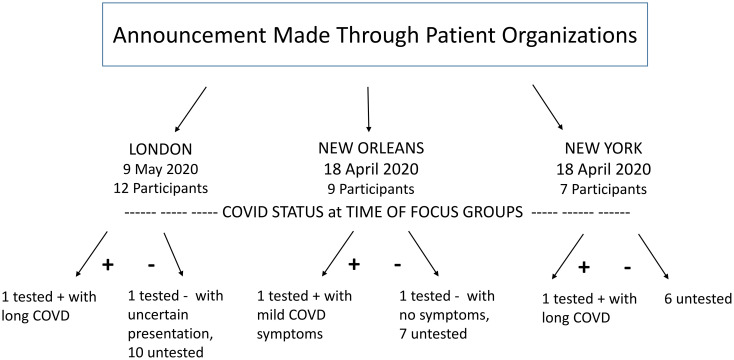
The impact of the COVID-19 pandemic on people living with sarcoidosis was examined in three global English-speaking areas with the highest COVID-19 incidence and death per capita during April 2020: London, UK; New Orleans, USA; New York City, USA (2,3). Three geographically distinct focus groups (FGs) with an a priori decision of 5 to 12 attendees per group based on the response, were conducted in April/May 2020 (Figures 1 and 2). The study protocol was approved, implemented, and with all participants consented according to Institutional Review Board #743566. Potential participants self-referred to the project after viewing sarcoidosis support group email or social media announcements, and were accepted on a first-come basis.
Figure 1.
Process diagram.
Figure 2.
CONSORT diagram of enrollment.
Face-to-face FG interviews via Zoom.us were closed to nonparticipants, planned for 90 to 120 min, led by AMR and LAS with an open interview framework relying upon patient-driven discussion for the content of COVID-19 related topics. FGs began with interviewer and participant introductions. Participants were invited to state their first name, the duration, degree of organ involvement, and treatment of sarcoidosis, along with a history of COVID-19 exposure or infection. Two questions drove the FG discussions: (1) “Thinking back to just before COVID-19 emerged, and then thinking about now, how has COVID-19 impacted your life as a person living with sarcoidosis?” (2) “Thinking back to prior to COVID-19 and then now, how has your health-related to sarcoidosis changed since COVID-19 emergence?.” During the discussion, intuitive interviewer probes delved for further detail or to check for a collective agreement. FGs were audio-recorded with concomitant field notes and transcribed verbatim. Participants were aware of the interviewers’ backgrounds and openly informed of the project's goals and motivations.
The study team consisted of 4 experienced qualitative researchers (AMR, DN, KJ, LAS) an RN/PhD and psychometrician, an MSc/PhD and 2 MD/MPHs, and 6 patient research partners (PRPs), a male and female from each geographic area, nationally recognized peer leaders with prior exposure to collaborative research (4). This resulted in 10 coders for each transcript. PRPs were trained on practical aspects of grounded theory (5,6) which guided transcript analyses, concept generation, triangulation, theme emergence, and framework production.
PRPs’ individual and group analyses provided the initial concept generation for each transcript, which was then merged with the iterative in-depth manual and Nvivo10 software-generated analyses by the professional researchers. A sequential nominal group approach facilitated all collective concept generation, agreement, and framework production (7,8). PRPs were restricted to observing the initial consensus exercises of their own FG's transcript but responsible for review and feedback on the team's analysis.
Results
A total of 28 interviewees (Table 1) participated without attrition. The median FG duration of 2.83 h and was driven by patient contributions and enthusiasm. Each FG member received their group's transcript for feedback, without further commentary.
Table 1.
Patients and Characteristics.
| Patient | Age/gender | Race/ethnicity | Diagnosis | Involvement as stated by participant | Biopsy | Oxygen use | Medication stated by participant | COVID-19 tested ± |
|---|---|---|---|---|---|---|---|---|
| New York City Focus Group | ||||||||
| NYC-1 | 50 y/F | W | ns/2015 | Pulmonary, articular | Y | GC | N/N | |
| NYC-2 | 57 y/F | B | ns/2013 | Cardiac, pulmonary, articular | Y | NS | N/N | |
| NYC-3 | 56 y/F | B | ns/2011 | CNS, ocular, lacrimal, pulmonary, cutaneous: LP, osseous | Y | IFX | N/N | |
| NYC-4 | 63 y/F | B | 2010/2010 | Cardiac, pulmonary, GI, PNS, cutaneous | Y | No meds | N/N | |
| NYC-5 | 52 y/M | H | 2004/2011 | CNS, ocular, cardiac, pulmonary, GI, cutaneous, osseous | Y | Y | NS | Y/Y+ Home recovery. Long COVID pulmonary, cutaneous blistering rash, arthritis. |
| NYC-6 | 55 y/F | W | ns/2009 | Cardiac, pulmonary, GI, PNS (autonomic), cutaneous, osseous | Y | NS | N/N | |
| NYC-7 | 50 y/F | W | 2005/2016 | CNS, lacrimal, cardiac, cutaneous | Y | IFX, MTX | N/N | |
| New Orleans Focus Group | ||||||||
| NO-1 | 64 y/M | B | 1997/2000 | Pulmonary | Y | IFX, GC | N/Y− | |
| NO-2 | 57 y/F | W | ns/2013 | Cardiac, pulmonary, cutaneous EN, articular | Y | GC, MTX,ADL | N/N | |
| NO-3 | 55 y/M | B | ns/2014 | CNS, pulmonary | Y | NS | N/N | |
| NO-4 | 53 y/F | B | ns/2018 | Pulmonary | ns | NS | N/N | |
| NO-5 | ns/F | B | ns/2017 | CNS, ocular, pulmonary, cutaneous | Y | IFX, MTX | N/N | |
| NO-6 | ns/F | B | ns/2016 | Pulmonary, joint | ns | NS | N/N | |
| NO-7 | 58 y/F | B | ns/1994 | Pulmonary, cutaneous: LP, articular | Y | IFX, MTX, HXQ | Y/Y+ mildly symptomatic | |
| NO-8 | 70 y/F | B | ns/1981 | Pulmonary, skin | Y | MTX | N/N | |
| NO-9 | 52 y/F | B | 2004/2006 | CNS, ocular, pulmonary, PH, PNS, cutaneous: LP | Y | Y | MMF, MTX, HXQ, PAH meds | N/N |
| London Focus Group | ||||||||
| UK-1 | 64 y/M | W | ns/2016 | Tonsillar, cardiac, pulmonary | Y | GC | N/N | |
| UK-2 | 57 y/F | W | 2017/2019 | Cardiac, pulmonary, glandular, articular | Y | GC | N/N | |
| UK-3 | 43 y/F | W | 2010/2019 | Ocular, Pulmonary, cutaneous | Y | HXQ, MTX, GC | N/N | |
| UK-4 | 48 y/F | W | ns/2014 | Pulmonary, cutaneous, EN, articular | Y | HXQ, GC | N/N | |
| UK-5 | 51 y/M | W | ns/2014 | Cardiac, renal, cutaneous | Y | NS | N/N | |
| UK-6 | 60 y/F | W | ns/2019 | Pulmonary, gastric, bone, joint, lymph nodes | Y | GC | N/N | |
| UK-7 | 60 y/F | W | ns/2020 | Pulmonary, lymph nodes, | Y | NS | N/N | |
| UK-8 | 64 y/F | W | ns/1974 | Ocular, CNS, PNS, cardiac, pulmonary, cutaneous | Y | MTX | N/Y- | |
| UK-9 | 50 y/M | W | ns/2018 | Cardiac, pulmonary | Y | GC | N/N | |
| UK-10 | 55 y/M | W | 2004/2014 | Cardiac, pulmonary, lymph node | Y | MTX | N/N | |
| UK-11 | 46 y/F | W | ns/2017 | Cardiac, pulmonary | Y | GC | N/N | |
| UK-12 | 64 y/M | W | ns/2011 | Pulmonary, cutaneous | Y | HXQ | Y/Y+ Pulmonary, cutaneous, prolonged recovery with sequelae of blistering rash, arthritis, | |
Abbreviations: ADL, adalimumab; B, Black race; CNS, central nervous system; EN, erythema nodosum; F, female; GC, glucocorticoids, HXQ, hydroxychloroquine, IFX, infliximab, LP, Lupus pernio, M, male; MMF, mycophenolate mofetil; MTX, methotrexate; NS, not stated; PAH, pulmonary arterial hypertension; PNS, peripheral nervous system; W, White race.
Data saturation for each focus group was cross-checked by concept occurrences in the other 2, concept consistency prevailed between groups except in areas of spirituality and regional particulars. No repeat interviews or follow-up questions occurred.
Overarching Themes (OTs)
Three overarching themes ( bold-type ) shelter all concept items (Box 1). Major themes (see Supplemental Material), though predominately under one OT, may overlap with another OT. Major themes are described below with selected quotes (Box 2). Divergent themes are addressed under relevant OTs.
Box 1.
Overarching Themes.
“ Sarcoidosis Survival Ecology ” (OT1): defined by its main themes, “Interconnections” and “Personal Evolution and Emergence”
“ COVID-19—Sarcoidosis Interactions and Similarities ” (OT2): addresses the overlap and interconnections between sarcoidosis and of COVID-19
“ Environmental/Societal External Needs and Influences ” (OT3): predominantly fixed factors influencing participants’ circumstances
BOX 2.
Selected Quotes From Online Supplemental Material.
| Subject | Quote |
| Over-Arching Theme 1 (OT1): “Sarcoidosis Survival Ecology” | |
| UK-1 | “I started shielding in February. I bought my first mask in January. I was in hospital between operations. But it was just my personal previous life experience … I saw it coming.” |
| NYC-3 | “My son is 15 and he's, being homeschooled again. I did like the fact that he would get up in the morning and go to school every day that would give me time if things really did hurt … as you know, we don't fake being sick we fake being well … so it bothers me that when I’m in a flare he can't be sheltered as much as he normally is.” |
| NYC-4 | Anyhow, so I try to keep things in perspective. So yes, I’m very afraid that if I get it I might not survive it. But by the same token, I’ve survived sarcoidosis and those very same things (strategies) helped me survive. |
| NO-8 | So finally I went online praising God asking him to please send me (help), (while) sitting on the side of the bed before I went to church. Mr R's (peer) name came up for sarcoidosis. So I called him and he told me about a good doctor |
| NYC-3 | “C” (peer) brings the light. When you’re amongst your sarky family—it infuses you, it gives you like the “purple power” I call it. You feel uplifted and you feel golden, you know. We can all laugh together, all cry together … but we’re all unified in that we share those things—where we might look fine on the outside. |
| UK-2 | This group has been incredibly constructive … I’ll probably sleep better tonight than I have done for an awful long time, just because I’ve met all these people who’ve got the same thing as I have—who know what's it like. …—if there could be some way of working with charities to do focus groups, just to give us a chance to meet each other—which has been great—and talk and vent, I think that might go a long way to help with some of the mental health problems that people are experiencing at moment. |
| UK-3 | “We’re so scared, scared, scared. We can't breathe because we’re in an anxious state … because you can't have fear and anxiety and scaremongering [whilst] being isolated like in a prison. You’ll go mad and how I do it, is to do with self-control … Yeah, switch off that news. You’ve got to live your life, right?” |
| NYC-6 | But, F … (a peer), it's not for nothing. At least we know that somebody has had it (COVID-19) and has survived it. You know, and that's what gives me hope. |
| Over-Arching Theme 2 (OTC2): “COVID-19—Sarcoidosis Interactions and Similarities” | |
| UK-8 | But I was told I had to go into the COVID unit here because no other ward could take me because it could be COVID-19, even though I’ve been isolated for four weeks. So I was in the unit (put) at risk … for two days. Two tests came back negative. But they still couldn't believe it because it was so like COVID-19. |
| UK-12 | I still suffer from fatigue. And when I had COVID-19, it was just like being under a sarcoidosis attack, like the night fevers, the temperature, a bit of trouble breathing, but it wasn't alarming because already lived through it with sarcoidosis. |
| UK-8 | —they’ve never compared the two. If people with sarcoid get it, are they then not at risk of having a double dose of something because sarcoid can be triggered by infection? |
| UK-3 | “… there's no supply of it. I found out about eight, nine chemists with no supply of hydroxychloroquine. (01:46:28) And then finally, there's one chemist, but they didn't deliver. Oh, this is just a headache. It's one thing after another thing. I finally got chemist who said that we’re going to deliver it to me. But then I had to go 15minutes down the road to collect it off a bench. Yep.” |
| UK-3 | I left a lot of messages with Dr B's secretary. No one's got back to me. It's been (ongoing) for 2 months. So with the sarcoid, I don't know how I’m treating it; if I’m treating it the right way or the wrong way, because no one's done a consultation (ie, follow-up) |
| UK-2 | Having to tell my doctor why I have to go to tele appointments for two years they (finally) managed to implement it in the space of 2 weeks when C19 came in and it's just so great. It saves me 2 and half hours on the train. It saves me being surrounded by lots of people who are very, very ill. |
| UK-8 | But from a sarcoidosis point of view, we find this all the time (lack of disease knowledge) when we see doctors that don't understand sarcoid. |
| NYC-3 | So I’m hoping that one of the things that come out of this (COVID-19) is that we bring more awareness to the systemic aspect of sarcoidosis |
| Over-Arching Theme 3 (OTC3): “Environmental/Societal External Needs and Influences” | |
| NYC-1 | And I’ve been typing in these comments saying “sarcoidosis” because you know, it is it is a race issue … a lot of African Americans have this disease (sarcoidosis). And I feel like from working in the city … and we were we’re all living and functioning within the schools and these buildings that have very poor air quality … |
| UK-3 | I took him (her son) out of school probably around the 16th of March. I did not listen to the government. I have an autoimmune disease … |
| NYC-1 | I live in an apartment building—a two-floor apartment building. People in my apartment building are going in and out. And I’m terrified to even walk out the front door to check the mail |
| NO-4 | last week or so. I had just came from my infusion and stopped at a store and … coughed in the store. When I left … a lady, actually walked up to my car as I was getting in … and she actually sprayed me down with lysol and ran back to her car. Now I’m kind of paranoid because when I go out … although I don't go out much … I’m scared to … cough. |
| NO-1 | Disproportionately it's blacks and women on the “frontline” … nurses, hospital workers, grocery check-out is a big one … the people that society relies upon are those types of jobs and … they are at risk for us … |
| NYC-5 | In terms of protection and protecting others—historically black lives are less valued in society and health wise … now with this pandemic … |
| UK-2 | … the effect it has on families. And that's a two way thing. what we ask from our children and our spouses is extreme because they can't shield with us. it's all going to be down to personal trade-offs over … keeping ourselves safe, keeping our families safe—sending their children to school and so on, but also the trade-off of how we maintain the economic viability of our family units. And all of these are mutually incompatible. |
| NYC-4 | I have an elderly father. He's 94 and I’m power of attorney for him and I was trying to do some business for him. I couldn't do it online. And I had to go out on Thursday, and it was so overwhelming. I didn't realize maybe because I’ve been inside so long. |
| UK-1 | But if it was a case of a triage, then … I wouldn't be very high on the list (due to cardiac sarcoidosis). Which is which is fine, it's available resources. |
| UK-2 | if I get COVID-19 and have to go to ITU … they’re going to say “she's not gonna survive, so she's not going to get an ITU (ICU) bed.” |
Sarcoidosis Survival Ecology (OT1)
“Sarcoidosis Survival Ecology” (OT1)
defined by its main themes, “Interconnections” and “Personal Evolution and Emergence,” reflect themes of multi-faceted, iterative, interdependent actions, and experiential personal growth while living with sarcoidosis describing identity, knowledge, and learned-COVID-19/crisis preparedness.
Networks, Activism, and Healing
A clear distinction was made between support groups and focus groups. Both created a sense of “belonging,” “support,” and “validation,” but support groups facilitated bi-directional knowledge sharing, peer mentorship in navigating healthcare, resources, and expectations. Focus groups stimulated pragmatism, relating to research, education, and health systems policy needs for standardized information.
Divergence
All participants of the New Orleans group were strongly and normatively declarative in spirituality and faith, which did not occur in other groups.
Self-Advocacy and Growth
Participants unanimously confirmed a trajectory of being initially devastated by a sarcoidosis diagnosis and the multi-relational experience of uncertainty and the subsequent gathering of motivation to become knowledgeable about the disease, health systems, and coping. Beyond the fear and dread of COVID-19, there was agreement that wisdom gained from living with sarcoidosis put them in a place of preparedness to protect against COVID-19, such as the early self-imposed implementation of family/self-isolation, and coping with the complex uncertainties associated with COVID-19.
Self-advocacy and self-protection were perceived as sometimes creating a hardship on personal and professional relationships during COVID-19. It placed additional work or restrictive burdens on others; including forcing patients to share the seriousness of their health status with others when they would have otherwise elected not to, e.g. employers, visitors, etc.
Credible Information
Participants initially were heavily involved with COVID-19-related news several hours daily, and subsequently restricted their exposure to less than an hour to protect psychological and emotional well-being, productivity, and engagement in more fulfilling life activities.
Discussions persisted around the credibility of COVID-19 information. Most participants distilled information from several sources; with reliance on scientists from governmental or international organizations such as Centers for Disease Control (CDC) or World Health Organization (WHO) or National Health Service (NHS). Widely expressed was that the presentation of information was misused and misrepresented for political, self-interested gain and by the media for “shock value.”
COVID-19—Sarcoidosis Interactions and Similarities (OT2)
“COVID-19—Sarcoidosis Interactions and Similarities” (OT2)
addresses the repeated voicings related to the myriad colliding facets between the respiratory and multi-organ system nature of sarcoidosis and of COVID-19; as well as questions regarding the viral triggering of inflammatory diseases.
Disease Behaviors
Clinical guidance was confused by similar symptomatology and manifestations between sarcoidosis flaring and COVID-19, i.e. sarcoidosis activity versus COVID-19 infection versus both occuring simultaneously; and made more complicated by COVID-19 testing/re-testing's questionable utility and reliability. Participants reported having to rely upon clinicians without experience in sarcoidosis to answer complex questions. This included addressing sarcoidosis flares, whether to continue sarcoidosis treatment and confusion over sarcoidosis versus COVID-19 symptoms. Further, in the United Kingdom, this became especially problematic when relying upon GP diagnosis for the attainment of COVID-19 protective status for vulnerable people (9,10).
These uncertainties led to a lack of confidence in COVID-19 screening, as well as diagnostic interpretations and treatment plans. Additionally confounding was the potential of immune-modulating sarcoidosis medications to increase vulnerability to infection, potentially conferr a protective effect or even be effectice in the treatment of COVID-19. Concern over the potential of potential pathogenic interactions between COVID-19 and sarcoidosis disease behavior, were diffuse in all groups, and notably in those with cardiac sarcoidosis. Despite, interest in sarcoidosis therapies potentially attenuating COVID-19 virility, participants’ fear of their immunosuppressed status drove compliance with the new/alternate sarcoidosis treatment strategies in response to the pandemic.
Shared and Intersecting Patterns
Evolving knowledge of research, diagnosis, natural history, and disease phenotypes, prognostic factors, and management as well as patient, general population, and clinician education were voiced as sharing similar trajectories in COVID-19 in the general population and the pre-COVID-19 sarcoidosis experience. The groups expressed that respiratory and multi-organ system conditions, like sarcoidosis, historically received limited public awareness, research attention, and funding; and that the COVID-19 pandemic may lead to a greater appreciation of and knowledge in respiratory and multi-organ system diseases. Further expressed was the hope that knowledge gained in sarcoidosis (1,11–16) might be useful in understanding the quality-of-life and therapeutic realms of COVID-19 treatment and recovery.
Participants had proactive self-determination strategies distilled to minimizing risk, vigilance in detection, paying attention to distinctive features of otherwise non-specific symptoms, for example, fever-type, and pattern, and self-reliance in deciding when and how to seek medical treatment. Though sarcoidosis was perceived as an experience which cultivated skills that facilitated greater ease in coping with and responding to the threat of exposure and to the uncertain medical knowledge during COVID-19; a sarcoidosis diagnosis was perceived as creating disparities when compared with the healthy population impacting “eligibility selection” for life-saving COVID-19 interventions such as mechanical ventilation and ICU admission. Many perceived COVID-19 infection as inexorably linked to death, in sarcoidosis; therefore each group's COVID-19 survivors were important catalysts for expressed new perspectives, relief yet sustained vigilance.
Healthcare Logistics
COVID-19-related disruption on all aspects of routine and emergent sarcoidosis-care was diffusely reported in relation to essential and critical diagnostics, infusions, medication assessment/tapering, attainment of refills and communication lines to specialists. Participants expressed a sense of health system abandonment during the pandemic, apprehension was particularly voiced regarding follow-up care by those with cardiac and ocular sarcoidosis and those midstream of a new sarcoidosis diagnositic work-up. These strains led to worry and greater uncertainty for sarcoidosis-related survival. Related to this, participants voiced a sense of guilt in having a health condition that required significant attention and resources, while in the midst of a pandemic.
The abrupt discontinuation or prolonged unchecked administration of glucocorticoids, were voiced experiences. Participants reported difficulties with hydroxychloroquine attainment as a result of depleted supplies as well as roadblocks by insurance in the United States.
Environmental/Societal External Needs and Influences (OT3)
“Environmental/Societal External Needs and Influences” (OT3)
captures predominantly fixed situational factors that patients perceive require patient effort to navigate and influences patient behavior and outcomes. It characterizes factors which are predominantly unidirectional pressures. This is different from the bi-directional inter-relational growth experiences of “Sarcoidosis Survival Ecology” (OT1). These external constructs include healthcare system access, de-prioritization of COVID-19 treatment for pre-existing conditions, race, gender and socio-economic status* (SES) (17) as well as having a disability, work options, positive and negative community influences, and one's physical environment. Under these confines managing COVID-19 exposure, caring for other vulnerable people, and relationships are described as operative themes.
Race, Gender, Socio-Economic, and Disability Inequity
“Discrimination” and “Healthcare Disparities” were pervasive themes relational to recurrent sub-themes including a disproportion of essential workforce thus increasing COVID-19 exposure and contraction, financial hardship pressuring work and caring for vulnerable others. Also, many sub-themes of deficiency in access to education, computers, technology as well as being pre-disposed to disrespectful social interactions (18).
While racial, gender, and SES health disparities such as COVID-19 testing and insurance coverage were less prominently voiced in the UK group, health disparities related to geographic location and preferential medical resource allocation to the able-bodied without underlying health conditions, such as access to critical care beds or mechanical ventilation, was strongly voiced by all groups.
Managing Exposure
Having sarcoidosis, immunosuppression, and prior non-COVID-19 infection experiences drove sub-themes of early self-imposed isolation, moving from city dwellings, and combining or splitting households to reduce location-based risk. Household decision-making regarding decontamination rituals, obtaining and handling of essential supplies, and risk reduction strategies between household members were motivated by the immunosuppressed vulnerability.
Social Factors
Positive and negative social factors were voiced. Participants noted that local communities rallied to assist and protect those more vulnerable, but alternatively participants reported feeling increasingly vulnerable due to self-interested individualistic attitudes toward protecting others and because of “guidance” from unreliable sources. Participants also experienced negative attitudes in pre-COVID-19 times for sarcoidosis symptoms such as coughing in public—now markedly exacerbated.
In the UK, a “shielding letter” for high or moderate risk groups was necessary for priority food and pharmacy deliveries and to access special protected shopping hours (9,10). However, sarcoidosis was not specifically listed (10,19) with patients frustrated and reliant on the local physician/GP for issuance. The practical value of the letter was perceived to have both negative (potentially being denied ventilator support) and positive (priority access to medications and groceries) implications.
Work and Family
Patients reported myriad layers of complexity dictated by circumstance influencing work and home relations with resultant physical, financial, logistical, and psychological implications. A number of participants were primary caregivers which had further implications for self-exposure as well as protecting and providing for the vulnerable family member. Configuration of physical space impacted exposure risk, personal relationships, and well-being. The UK organized specialty provisions for childcare and eldercare for essential workers as well as work accommodations for vulnerable employees or employees with vulnerable family members at home.
Discussion
In the best of times, it is challenging for clinicians and patients to address healthcare needs related to complex multi-organ system diseases such as sarcoidosis. As researchers, investigating sarcoidosis experiences of the COVID-19 pandemic, the purview of the sarcoidosis experience before the COVID-19 pandemic provided an essential relational platform. The COVID-19 pandemic has amplified and disclosed underlying infrastructural vulnerabilities that had routinely impacted this population, but it also appears to have underscored strengths often cultivated by living with a serious health condition.
This research exemplifies the extent to which patient expertise has the potential to drive research and health system priorities. As a result of living through the COVID-19 pandemic, people with complex health conditions can provide guidance on both how navigate the extreme times precipitated by a pandemic as well as how this experience can influence routine healthcare delivery in the future. We anticipate these pre- and intra-pandemic findings are unlikely to be unique to sarcoidosis (19) and ardently hope that this dense, intense base of information will inform investigational off-shoots into psychological, systems management, and quality-of-life research in sarcoidosis and other multi-system diseases—including “post-COVID-19 syndrome.”
The framework is intricate and more extensive than could have been anticipated, but it captures the necessary detail reflective of a complicated multi-system disease (sarcoidosis) experienced with in the context of another biologically and socially complex disease (COVID-19). In this regard, the framework is an agent of sensitization and strategy that can be tested and applied beyond sarcoidosis. In regard to sarcoidosis, the framework discloses unstable underpinnings to healthcare system structure, education, communication, and service industries that required the push of a crisis for overt revelation. The crisis also illuminated pre-existing education and knowledge gaps, and the need to be better equipped to support those living with precarious multi-system diseases in a crisis. Importantly, the pandemic heightened participants’ pre-existing sensibilities and frustrations regarding inequities of disability and race, and healthcare structure and society interactions as a subclass, particularly in relation to research funding, allocation of healthcare resources, knowledge, and clear communication.
The strengths of the design harnessed the perspectives, priorities, and concerns of participants residing in global English-speaking areas with the highest incidence and mortality during the time of data collection. Thus, we anticipate that the broadest and most intense experiences of the COVID-19 outbreak as experienced by people living with sarcoidosis are captured here. The collection time-period occurred after the initial few weeks of isolation measures, therefore, allowing for valuable assimilation perspectives and experiences to augment relevant concept collection.
In this study, patient participants, PRPs, and researchers developed an authentic collaboration at the onset, in question framing, research design and conduct, and subsequent dissemination strategies. Power-sharing served to reduce inequalities and enabled honest and transparent discussions.
Pervasive in all groups was the need for improved access to specialist physicians and nurses for a deeper lever of individualized support and care. The authors draw attention to the lack of any patient and caregiver inclusion on COVID-19 related research published to date. These frustrations were recently expressed by the physician–patients with COVID-19 (20) and echo throughout our findings with relevance to the COVID-19 or sarcoidosis disease experience or both combined. These physician–patients urge the formation of “one-stop” clinics as hubs of care, pattern-recognition and sentinel expertise to identify and manage COVID-19 sequelae in order to expeditiously augment and propel the acquisition and dissemination of medical knowledge. Sarcoidosis centers of excellence still appear to have a sequestered recognition and treatment knowledge not yet deployed in general pulmonary, rheumatology, or other sub-specialty clinics, as reflected in the framework. However, the framework also states that the global experience of COVID-19 may yet influence the frontiers of knowledge dissemination in these rarer complex multi-system diseases.
Whether underlying inflammatory diseases are pathogenically triggered or worsened by the contraction of COVID-19 was presented in this data months before such suppositions were published in the literature (21,22). This speaks to seasoned patients’ instinctual inclination related to sarcoidosis natural history, susceptibility according to the degree of immunosuppression, and conceivable synergistic and potentiating pathogenicity. Similarly, astute speculations regarding vaccine availability, effect, and management—as well as discriminatory implications of COVID-19—again, seemed driven by patients’ expertise acquired by experiential sensitization to pathogenicity and medical knowledge exposure.
Regarding study limitations, the hope for survival appears to drive content, however, defeat, a fairly common concept expressed on patient social media, is absent in our study. Selection bias with participant self-referral via patient associations may have attracted participants: (a) with higher levels of self-efficacy skills, (b) “seasoned” with longer disease durations and possibly “upskilled” in coping, and (c) less likely hampered by psychological demotivation. Outreach strategies designed specifically to support those newly diagnosed and experiencing mental hardship could be warranted.
We regret that access to linguistic resources impeded the ability to investigate non-English speaking, high COVID-19 endemic areas. We also recognize that representation was heavily weighted by participants with more severe disease. However, a bias toward disease severity likely intensifies and broadens the conceptual spectrum that might be experienced across sarcoidosis severity and phenotypical differences. We will further examine these differences in the global open-query phase of this project.
The conclusions reached in this study promise helpful and generalizable insights; despite constantly evolving information and issues of the COVID-19 pandemic. Data collection was completed prior to the current global concerns of schooling during the pandemic, however the six PRP authors as international leaders advocate this to be a serious situation and best left to parental households to decide on an individual family basis.
Future directions are currently querying these results in the global sarcoidosis patient community to assess generalizability and deficits of these findings.
Supplemental Material
Supplemental material, sj-docx-1-jpx-10.1177_23743735221075556 for Sarcoidosis Illuminations on Living During COVID-19: Patient Experiences of Diagnosis, Management, and Survival Before and During the Pandemic* by Lesley Ann Saketkoo LA, MD, MPH, Kelly Jensen, MD, MPH, Dimitra Nikoletou, PhD, MSc, Jacqui J. Newton, Frank J. Rivera, BA, Mike Howie, Rodney K. Reese, Melanie Goodman, BS, Patricia B. Hart, MBA, Whitney Bembry, MD, Adam Russell, BA, Isabelle Lian, MS, Matthew R. Lammi, MD, MSCR, Mary Beth Scholand MB, MD, and Anne-Marie Russell AM, PhD, APRN, ATSF in Journal of Patient Experience
Acknowledgments
Sarcoidosis UK, Sarcoidosis Awareness Foundation of Louisiana, National Sarcoidosis Support Network, New Orleans Sarcoidosis Support Group. AMR is a National Institute for Health Research (NIHR) Senior Nurse and Midwife Research Leader. The views expressed in this article are those of the author(s) and not necessarily those of the NIHR, or the Department of Health and Social Care.
Author Biographies
Lesley Ann Saketkoo is the director and founder of New Orleans Scleroderma and Sarcoidosis Patient Care and Research Center. Her clinical research work in clinical trial design, in identifying patients' priorities in life-threatening autoimmune illness including pulmonary hypertension and pulmonary fibrosis and developing research tools with patients including targeting self-management strategies with yoga, dance and singing for lung health rehabilitation as well as mindfulness practices. She is currently co-director/co-founder of UMC Comprehensive Pulmonary Hypertension Center and Interstitial Lung Disease Clinic Programs with Louisiana State University and Tulane University Schools of Medicine. Saketkoo's interest in sarcoidosis began in the second year of medical school encountering neurosarcoidosis, which was meant to be a 'rare disease' and at that time the standard treatment was only prednisone. The condition itself was fascinating but importantly demanded comprehensive set of skills and attention in order to appropriately care for patients. She found that caring for people living with inflammatory and fibrosing multi-organ system diseases was her 'calling'.
Kelly Jensen attended medical school at Tulane University during which she spent a year conducting public health research in Peru and residency at Oregon Health and Science University. She started working on a project examining the impact of diet on symptom burden in patients living with systemic sclerosis during medical school. She has since been involved in projects examining experiences of patients living with sarcoidosis during the COVID pandemic and factors affecting health-related quality of life in patients with sarcoidosis and systemic sclerosis. She is interested in clinical outcomes research especially related to CTD-ILD.
Dimitra Nikoletou leads the department of Rehabilitation Sciences and postgraduate research degrees for the Joint Faculty of Health, Social Care and Education, Kingston University and St George's University of London. Previously having as a research physiotherapist in NHS hospitals in Scotland and England and King's College London. She co-leads the Inclusive Health and Wellbeing Research group , a multidisciplinary group of 23 allied health academics and NHS researchers that focuses on research in rare diseases, global health and hard-to-reach. She co-founded St George's Interstitial Lung Disease (ILD) Support Group . Her research specializes in clinical exercise physiology and exercise prescription with a particular focus on rare diseases.
Jacqui J. Newton was diagnosed with sarcoidosis in 1974, gradually affecting lungs, eyes, skin, joints, spinal cord and CNS. She reports having had ‘a really good education on sarcoidosis from my first consultant’, which helped her navigate disease course and be able to be a support for others. Since then, flares have been misdiagnosed by others and undiagnosed often, until 2013 when she was found the neurosarcoidosis expert in the UK, Dr Desmond Kidd. She has been SarcoidosisUK (https://www.sarcoidosisuk.org/) Patient Ambassador since 2015 whereby she helps moderate support groups across the UK and develop educational programming. Her voluntary work with SarcoidosisUK and sarcoidosis-related projects is flexible and gives her a great sense of purpose. She is a committed patient research partner in the hopes of supporting improved health outcomes in sarcoidosis.
Frank J. Rivera was diagnosed with multi-system sarcoidosis in 2011. Frank founded Sarcoidosis of Long Island in 2012 and is an advocate for sarcoidosis and social justice in the realms of policy-making, research and education. He has represented sarcoidosis communities as a speaker at two Congressional briefings and appeared on NBC Nightly News in 2018 to discuss ‘Right to Try' legislation. He is the author of two books, ‘ Walking in Silent Pain ’ and ‘ I Have Sarcoidosis But It Doesn’t Have Me ’. Frank is a National Advocate for Foundation for Sarcoidosis Research. He was named Rare Undiagnosed Genetic Disease Ambassador for Illumina and is an ambassador for the Foundation for Sarcoidosis Research and ‘Person of the Year’ in Brookhaven Town. In 2020, Frank started Stronger Than Sarcoidosis a nonprofit made by patients for patients. He is heartened that patient voice and expertise is increasingly recognized as integral to science and policy-making.
Mike Howie, an information security geek from Fife, Scotland, got lost in Berkshire, England, many years ago. Professionally he is a Certified Information Security Manager with previous certifications as a Prince Practitioner, ISO27001 and ISO20000 Lead Auditor and Cyber Essentials Plus accreditor. Outside of work he's chaired his local Surgery Patient Participation Group for 6 years and previously led the Central London Sarcoidosis UK Support Group. Following a sarcoidosis diagnosis in 2014 affecting his cardiac and renal organs, these voluntary leadership roles allow Mike to give back by helping augment the presence of patient expertise in advocacy, research, education and policy-making.
Rodney K. Reese lived, thrived and truly embodied the title of ‘warrior’. Rodney was a firefighter in Baton Rouge, Louisiana, and throughout his life mentored young people throughout his community. Aside from his everyday valour, Rodney was a tremendous presence in the sarcoidosis community, always finding ways to support others as a friend and mentor. He was one of the original patient ambassadors with the Foundation for Sarcoidosis Research (FSR) , he founded his own organization, The Sarcoidosis Awareness Foundation of Louisiana and he partnered with the Bernie Mac Foundation and Stronger Than Sarcoidosis on several projects. Beyond his involvement in these organizations, Rodney was there for anyone living with a complex disease. Rodney made sure everyone he met felt welcome, cared for and not alone.
Melanie Goodman is a New Orleans native. She has a BS in biology and works full time as a senior project manager. She began researching publications and other information on sarcoidosis in 2013, when she was first diagnosed with multisystem sarcoidosis at 50. This was motivated by curiosity and necessity because the multitude of physicians that she had experienced significant delay in the sarcoidosis diagnosis, and these physicians who first treated her had no experience diagnosing and treating sarcoidosis. She eventually found and received medical care by sarcoidosis specialists in Chicago, New Orleans, and Boston. Goodman recognized a need and started the New Orleans Sarcoidosis Support Group in 2015. Goodman has lent herself to helping newly diagnosed sarcoidosis patients navigate the healthcare system and obtain specialty care. Goodman has been a Patient Expert and Advisor and a Patient Research Partner on various Sarcoidosis research efforts between 2015 and 2020.
Patricia B. Hart graduated from Andrews University in Michigan with a bachelor's degree in English and Communications. While working and raising a family, Pat earned an MBA from Long Island University. She retired from a 35-year career in human resources, in part as a result of her diagnosis with sarcoidosis. Not one to remain idle, Pat became active in the sarcoidosis community, managing an online support group to help those newly diagnosed learn about the disease and navigate through their medical options. Pat is a certified health and wellness coach and advocates for a more holistic approach to treatment.
Whitney Bembry, MD, MPH, is a second-year adult and pediatric rheumatology fellow at Saint Louis University School of Medicine. Bembry received her residency training in Internal Medicine and Pediatrics at Tulane University School of Medicine, where she served as both Med-Peds Chief Resident and Pediatric Chief Resident during an additional academic year. She received her medical degree and MPH from Mercer University School of Medicine. She has a passion for improving transitions of care in the fields of pediatric and adult rheumatology and is looking to develop curricula and a systematic approach to transitions.
Adam Russell supports clinical research on patient experiences of interstitial lung diseases through audio transcription, proof reading, and editing. Adam is primarily a graphic designer, illustrator, and photographer working on a range of eco and ethical projects. Commissioned work includes producing graphics for health-related projects, advertising for vegan products, print and pattern designs, and photographic cataloguing of artistic images and products.
Isabelle Lian recently graduated from Tulane University with a Bachelor of Science in Neuroscience and is preparing to enter medical school this summer. Her prior research explored the potential to foster resilient physicians through Compassion Cultivation Training and other mindfulness techniques. In her other patient-centered projects, Lian has a special interest in the areas of COVID-19, diet, and exercise. She is examining the impact of these on the patient experience in conditions such as sarcoidosis, scleroderma, and myositis.
Matthew R. Lammi is a pulmonary and critical care physician-researcher who focuses on patients with pulmonary hypertension, connective tissue disease-related pulmonary complications, and sarcoidosis. He is the Director of the Comprehensive Pulmonary Hypertension Center-University Medical Center and a member of the New Orleans Scleroderma and Sarcoidosis Patient Care and Research Center. His research is focused on early identification of pulmonary hypertension and predictive modeling.
Mary B. Scholand is an Associate Professor of Medicine at the University of Utah and is the Director of the Interstitial Lung Disease Program. She has focused her practice on improving the care and quality of life for patients with all interstitial lung diseases including sarcoidosis. She is active in many multicenter clinical networks. Her research includes characterizing ILD phenotypes, conducting therapeutic clinical trials and patient-reported disease characterization.
Anne-Marie Russell is a senior lecturer and research lead in the College of Medicine and Health, University of Exeter. She maintains clinical activities through honorary appointments with Royal Devon and Exeter and Imperial College Healthcare NHS Trusts. Anne-Marie's research is focused on patient reported measures including experience, engagement and health outcomes employing mixed methods and patient-centred approaches. Anne-Marie collaborates on studies relating to interstitial lung disease (ILD) and palliative care. She is the author/co-author of numerous peer-reviewed publications and regularly conducts peer review. Anne-Marie works collaboratively with ILD and sarcoidosis charities in the UK, US and Europe.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Sarcoidosis Awareness Foundation of Louisiana (grant number L30 HL129466, unknown). Charles and Elizabeth Wetmore Foundation (LAS), Sarcoidosis Awareness Foundation of Louisiana (LAS), National Institutes of Health (US) NIH/NHLBI L30 HL129466 (MRL). National Institute of Health Research UK (AMR).
Ethics Statement on Human and Animal Research: The study protocol was approved, implemented, and with all participants providing consent according to Institutional Review Board #743566 and the World Medical Association Declaration of Helsinki. This study did not involve animals.
ORCID iD: Lesley Ann Saketkoo https://orcid.org/0000-0002-1878-8591
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Grunewald J, Grutters JC, Arkema EV, Saketkoo LA, Moller DR, Müller-Quernheim J. Sarcoidosis. Nat Rev Dis Primers. 2019;5(1):45. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Centers for Disease Control. Interactive map by date. Last Accessed 13 October, 2020. https://covid.cdc.gov/covid-data-tracker/#county-map.
- 3.Coronavirus (COVID) in the UK. Last Accessed 13 October, 2020. https://coronavirus.data.gov.uk/.
- 4.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-57. [DOI] [PubMed] [Google Scholar]
- 5.Strauss A, Corbin J. Grounded theory methodology: an overview. In: Denzin N, Lincoln Y, eds. Handbook of Qualitative Research. 1st ed. Thousand Oaks, CA: SAGE Publications; 1994:273-84. [Google Scholar]
- 6.Saketkoo LA, Pauling JD. Qualitative methods to advance care, diagnosis, and therapy in rheumatic diseases. Rheum Dis Clin North Am. 2018;44(2):267-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rand Organization. Multiple articles and chapters in PDF format by the RAND Organization. Accessed 3 February 2020. http://www.rand.org/international_programs/pardee/pubs/futures_method/delphi.html.
- 8.VandeVen AH, Delbecq AL. The effectiveness of nominal, Delphi, and interacting group decision making processes. Acad Manage J. 1974;17(4):605-21. [Google Scholar]
- 9.Accessed 27 September 2020. https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19.
- 10.Accessed 27 September 2020. https://www.nhs.uk/conditions/coronavirus-covid-19/people-at-higher-risk/whos-at-higher-risk-from-coronavirus/.
- 11.Voortman M, Stern BJ, Saketkoo LA, Drent M. The burden of neurosarcoidosis: essential approaches to early diagnosis and treatment. Semin Respir Crit Care Med. 2020;41(5):641-51. [DOI] [PubMed] [Google Scholar]
- 12.Saketkoo LA, Karpinski A, Young J, Adell R, Walker M, Hennebury Tet al. et al. Feasibility, utility and symptom impact of modified mindfulness training in sarcoidosis. ERJ Open Res. 2018;4(2):00085-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hendriks CMR, Saketkoo LA, Elfferich MDP, De Vries J, Wijnen PAHM, Drent M. Sarcoidosis and work participation: the need to develop a disease-specific core set for assessment of work ability. Lung. 2019;197(4):407-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Kofahi K, Korsten P, Ascoli C, Virupannavar S, Mirsaeidi M, Chang Iet al. et al. Management of extrapulmonary sarcoidosis: challenges and solutions. Ther Clin Risk Manag. 2016;12:1623-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baughman RP, Scholand MB, Rahaghi FF. Clinical phenotyping: role in treatment decisions in sarcoidosis. Eur Respir Rev. 2020;29(155):190145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strookappe B, Saketkoo LA, Elfferich M, Holland A, De Vries J, Knevel Tet al. et al. Physical activity and training in sarcoidosis: review and experience-based recommendations. Expert Rev Respir Med. 2016;10(10):1057-68. [DOI] [PubMed] [Google Scholar]
- 17.APA website. Accessed 3 August, 2020. https://www.apa.org/topics/socioeconomic-status.
- 18.Wilkerson I. Caste: The Origins of Our Discontents. New York, NY: Random House; 2020. [Google Scholar]
- 19.Michaud K, Wipfler K, Shaw Y, Simon TA, Cornish A, England BRet al. et al. Experiences of patients With rheumatic diseases in the United States during early days of the COVID-19 pandemic. ACR Open Rheumatol. 2020;2(6):335-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alwan NA, Attree E, Blair JM, et al. From doctors as patients: a manifesto for tackling persisting symptoms of COVID-19. BMJ. 2020;370:m3565. [DOI] [PubMed] [Google Scholar]
- 21.Fonseca M, Summer R, Roman J. Acute exacerbation of interstitial lung disease as a sequela of COVID-19 pneumonia. Am J Med Sci. 2021;361(1):126-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Southern BD. Patients with interstitial lung disease and pulmonary sarcoidosis are at high risk for severe illness related to COVID-19. Cleve Clin J Med. 2020. 10.3949/ccjm.87a.ccc026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpx-10.1177_23743735221075556 for Sarcoidosis Illuminations on Living During COVID-19: Patient Experiences of Diagnosis, Management, and Survival Before and During the Pandemic* by Lesley Ann Saketkoo LA, MD, MPH, Kelly Jensen, MD, MPH, Dimitra Nikoletou, PhD, MSc, Jacqui J. Newton, Frank J. Rivera, BA, Mike Howie, Rodney K. Reese, Melanie Goodman, BS, Patricia B. Hart, MBA, Whitney Bembry, MD, Adam Russell, BA, Isabelle Lian, MS, Matthew R. Lammi, MD, MSCR, Mary Beth Scholand MB, MD, and Anne-Marie Russell AM, PhD, APRN, ATSF in Journal of Patient Experience