Abstract
Introduction: Low serum vitamin D has been shown to be a risk factor for Coronavirus 2019 (COVID-19). The aim of this study was to assess the effects of high dose vitamin D supplementation on hs-CRP, ESR and clinical outcomes, including duration of hospitalization, quality of life and New York Heart Association (NYHA) Functional Classification, in adults with COVID-19. Methods: This double-blind, randomized control trial will be conducted on patients with RT-PCR and/or chest CT scan diagnosis of COVID-19 admitted in Imam Reza Hospital, Mashhad, Iran. Participants will be randomized into control and intervention groups based on randomization sampling. The intervention group will receive soft gel containing 50,000 IU vitamin D on the first day followed by 10,000 IU/day through a supplement drop daily for 29 days. The control group will receive 1000 IU vitamin D daily through supplement drop and a placebo soft gel. All participants will undergo laboratory assessment including inflammatory markers, serum 25)OH)D, complete blood count (CBC), liver and renal profile, lipid profile and erythrocyte sedimentation rate (ESR) at baseline and at day 30. The mortality rate will be recorded in both groups. Results: Data will be presented using descriptive statistics. Comparison of changes in study parameters over the study period will be performed using analysis of covariance adjusting for possible confounders. Conclusions: The findings of this will provide evidence on the effects of high dose vitamin D supplementation on inflammatory markers in hospitalized COVID-19 patients.
Keywords: COVID-19, vitamin d, inflammation
Introduction
Since the novel coronavirus disease (COVID-19) has become pandemic, several strategies for the prevention and treatment of this fatal disease have been proposed. These strategies have become more important by the emergence of new variants of this virus, such as the delta variant. Nutritional supplementations such as vitamin D have been considered as a potentially effective method, along with antiviral agents, in treatment and reducing the severity of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection.
SARS-CoV-2 enters respiratory cells through angiotensin-converting enzyme 2 (ACE2) receptor. The hypothesis for the importance of treating hypovitaminosis D in COVID-19 patients has been originated from the observations that vitamin D down-regulated ACE-2 receptors (Arboleda and Urcuqui-Inchima, 2020; Hoffmann et al., 2020). From the clinical point of view, hypovitaminosis D is related to the poor prognosis in COVID-19 patients (Munshi et al., 2021). Observational studies have shown a greater risk of mortality due to COVID-19 in vitamin D deficient patients (Baktash et al., 2021; Mariani et al., 2021; Radujkovic et al., 2020).
Although studies have shown the effectiveness of vitamin D supplementation on COVID-19 outcomes, results from randomized clinical trials are inconsistent. A recent meta-analysis on the randomized controlled trials revealed that there might be an association between vitamin D supplementation and improvement of clinical outcomes such as hospital length of stay and mortality. However there is a lack of evidence regarding the optimal dose and duration of vitamin D supplementation, particularly in hospitalized patients (Pal et al., 2021).
The inconsistent results of existing studies justify the need for a well-designed intervention where factors such as the duration of treatment, dosage and delivery of vitamin D, as well as biomarkers and clinical outcomes are chosen and measured in the light of recent findings. Hence, we aimed to design and perform a randomized clinical trial to evaluate the effect of high dose vitamin D supplementation on selected biomarkers and clinical outcomes of patients infected with COVID-19.
Methods/design
Trial design
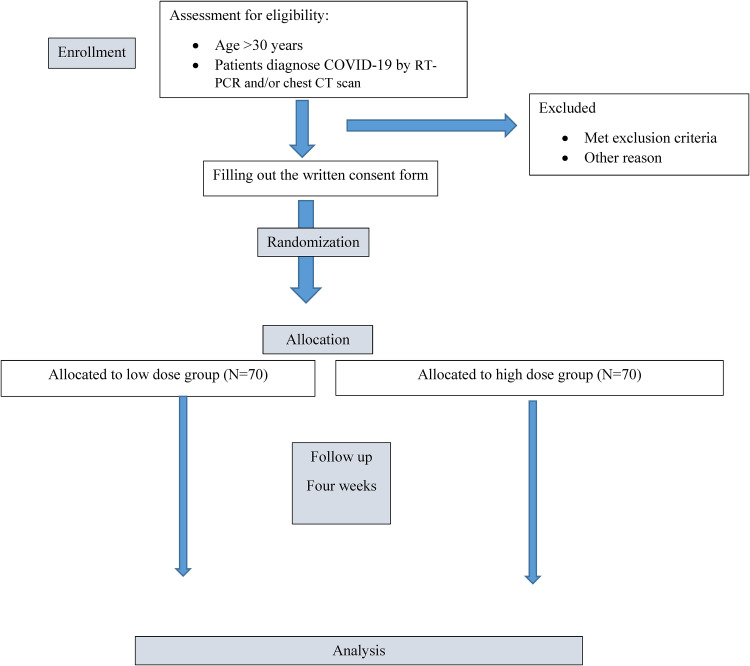
This RCT protocol was written according to the CONSORT SPIRIT 2013 guidelines. In the present double-blind, randomized, placebo-controlled parallel single center, intent-to-treat clinical trial study we will include 140 patients with the diagnosis of COVID-19. Figure 1https://link.springer.com/article/10.1186/s13063-020-04928-5 - Figure 1 shows the trial design. Participants will be selected from patients with the diagnosis of COVID-19 admitted in Imam Reza hospital related to Mashhad University of Medical Sciences (MUMS) from January 2021.
Figure 1.
Study flow chart.
Eligibility criteria
Eligibility criteria for covid-19 patients will be done as follows. Individuals will be allocated into two groups by block randomization.
Inclusion criteria
Hospitalized patients are eligible to participate if they are at least 30 years old, have a confirmed SARS-CoV-2 infection by RT-PCR and/or chest CT scan within the preceding three days, and willingness to participate in the study by signing an informed consent form (or informed consent form obtained from the trusted person, or emergency inclusion procedure in the context of lockdown, as appropriate).
Exclusion criteria
The following exclusion criteria are considered: Cancer, renal failure, history of calcium lithiasis, contraindications for consumption of vitamin D supplements, including active granulomatosis (sarcoidosis, tuberculosis, lymphoma), receiving treatment with vitamin D or vitamin D supplementation during the preceding month (with the exception of supplements providing 800 IU or less vitamin D per day), known hypervitaminosis D or hypercalcemia, known intolerance to vitamin D, enrolment in another clinical trial simultaneously.
Baseline assessment
Summarizes the study timeline is presented in Table 1. The baseline assessment related clinical status (severity of disease) will be performed by internist, then the research dietitian, who will collect demographic details, medical history, New York Heart Association (NYHA) functional class and short-form 36 Health Status Questionnaire (SF-36).
Table 1.
Timeline and applied tests.
| Time Point | weeks | ||
|---|---|---|---|
| 0 | 2 | 4 | |
| Enrolment | ✓ | ||
| Eligibility screening | ✓ | ||
| Informed consent | ✓ | ||
| Randomization | ✓ | ||
| Allocation | ✓ | ||
| Intervention Treatment: 50.000 IU soft gel (single dose) and 10.000 IU daily drop daily | ✓ | ||

|
|||
| Control: placebo soft gel (single dose) + 1000 IU drop daily |

|
||
| Compliance and side effect |

|
||
| Laboratory assessment | ✓ | ✓ | |
| Inflammatory markers (hs-CRP, ESR, RDW, NLR, PLR) | ✓ | ✓ | |
| Renal function tests (Cr, Urea) | ✓ | ✓ | |
| Liver function tests (LDH,AST,ALT,GGT) | ✓ | ✓ | |
| Lipid profile (LDL-c, HDL-c,TG, Total cholesterol) | ✓ | ✓ | |
| Fasting blood glucose | ✓ | ✓ | |
| Ca, P, Albumin, 25(OH)D | ✓ | ✓ | |
| SF-36 and NYHA questionnaire | ✓ | ✓ | |
Fasting blood glucose (FBG), alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), Lactate Dehydrogenase (LDH), Creatinine (Cr), calcium (Ca), phosphate (P), High sensitive C-Reactive Protein (hs-CRP), Erythrocyte sedimentation rate (ESR), Red Cell Distribution Width (RDW), Neutrophil-to-lymphocyte ratio (NLR), Platelet-to-lymphocyte ratio (PLR), Low-density lipoprotein cholestrol (LDL-c), High-density lipoprotein cholesterol (HDL-c), Triglycerides (TG).
Randomization and interventions
Eligibility of patients will be determined at the first screening visit. Block randomization method will be used for this trial study. Participants will be allocated randomly (1:1) to control and intervention groups based on random block procedure consisting of two subjects per block. Blocking will be complemented according to patient's baseline characteristics such as severity of disease (mild or moderate) and type of intervention.
The intervention group will receive high-dose vitamin D3 supplement in a single bolus dose of 50,000 IU as a soft gel (ZAHRAVI, Iran) on the day of inclusion followed by a daily dose of 10,000 IU for 29 days in the form of oral drop (Prepared in the Department of Pharmacology, Mashhad University of Medical Sciences) from the second day of admission. Cholecalciferol is packaged in a drop containing 10,000 IU/mL. Thus, participants in the intervention group take 1 mL of vitamin D drop daily. The control group will receive gelatin soft gels as placebo, along with 1000 IU vitamin D3 supplement in the form of oral drop (one mL of oral drops containing 1000 IU) daily for 30 days from the day of inclusion Soft gel and supplement drops are prepared in the Department of Pharmacology, Mashhad University of Medical Sciences.
Ethics approval
The study has been approved by the ethics committee of Mashhad university of Medical Sciences (Ethic number: IR.MUMS.REC.1399.237) and was registered in the Iranian Registry of Clinical Trials website (IRCT ID: IRCT20110726007117N11).
Safety consideration
The intervention will be stopped in cases such as any intervention-related side effects and upon the request of participants due to deterioration in their disease condition. Also Follow up will be done one month after the end of the study to evaluate complications. Also study participants will be asked to contact the investigators regarding observation of toxicity symptoms within 2 years of the study. In order to prevent matrix calcification, we will consider vitamin K2 100 microgram/day (RDA dose of vitamin K). The Ethics committee of Mashhad University of Medical Sciences (MUMS) will decide for the referred cases. All subjects will be informed of their laboratory test results as the study will be completed.
Power calculation and sample size estimates
The sample size was calculated with respect to the desired power (80%) and effect size (0.52) for this study (Munro, 2005). Considering a potential dropout rate of 10%, the sample size was calculated as 140 participants (70 participants in each group).
Blinding
This study is double-blind and both the investigators and the participants will be blinded regarding the supplementation dose. Both drops (High dose and low dose vitamin D) will be labelled as A and B by the Department of Pharmacology, respectively. In addition, both drops will be similar in taste, colour, size and identical manufacturing department (Department of Pharmacology, Mashhad University of Medical Sciences, Mashhad, Iran).
Applied tests during the study
Clinical outcome measurement
We will assess clinical outcome indicators such as quality of life (SF-36 questionnaire) and the New York Heart Association (NYHA) functional classification (Eskandari et al., 2015; Montazeri et al., 2005) at baseline and after one month of intervention. Moreover duration of hospital stay were recorded.
Laboratory assessment
Primary outcome tests such as Hs-CRP and ESR will be measured Pars Azmun test kits in BT-3000 auto-analyzer Biotechnical, Rome, Italy and Westergren method respectively.
All blood samples will be taken in the morning and after 12 h of midnight fasting by taking 10 mL of intravenous blood, which will be stored in two tubes, including a tube containing EDTA for complete blood count (CBC) test and a gel tube for biochemical and hormonal tests. The samples will then be centrifuged at 3500 rpm for 15 min at 4 °C to separate serum and aliquots of serum and will then be stored at − 80 °C for analysis. A sample will be analysed for CBC, and the rest of the samples will be stored immediately at − 80 °C.
Hematologic measurements include CBC using blood control (R&D SYSTEMS, Minnesota, USA) in Sysmex KX21 (Sysmex, Japan). Biochemical measurements include fasting blood glucose (FBG), alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), Lactate Dehydrogenase (LDH), urea, creatinine, calcium, phosphate, and albumin. For FBG, ALT, AST, ALP, GGT, Creatinine, and BUN, LDL-c, HDL-c, Triglycerides (TG), total cholesterol (Pars Azmun test kits in BT-3000 auto-analyzer Biotechnical, Rome, Italy).
Serum 25(OH)D concentrations will be measured using commercial ELISA kits (Pishgaman Sanjesh- Iran), using an Awareness/Stat Fax 2100 analyzer.
Statistical methods
All analyses will be based on the intention-to-treat (ITT) approach. Data will be analyzed by using the SPSS software, version 16 (IBM Inc, Chicago, IL, USA). Continuous and categorical data will be demonstrated as mean ± standard deviation (SD), frequency of distribution in different categories (%), respectively. The normality of data will be assessed by Kolmogorov-Smirnov test Comparison of continuous data between intervention and control groups at baseline will be performed using the independent t-test or Mann-Whitney test Paired t-test or Wilcoxon test will be conducted for before and after intervention comparisons. Comparison of the distribution pattern of categorical data will be performed using the chi-square or Fisher exact tests. The mixed model analysis will be applied to identify any differences between two treatment groups after adjusting for confounding variables considering the random effects of confounders. In addition, the chi-square test or exact Fischer test will be performed to compare mortality rates between study groups. In this study the considered value of alpha will less than 0.05.
Outcome measures
The primary objective is to compare the effect of high dose consists of a bolus initial dose and a continuous dose oral vitamin D3 administration on hs-CRP, ESR and clinical outcomes, including duration of hospital stay, quality of life (SF-36 questionnaire) and the New York Heart Association (NYHA) Functional Classification, in hospitalized adults infected with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2).
Secondary outcomes include
To compare the effect of high dose with low dose oral vitamin D3 administration on
Inflammatory markers, including NLR, PLR, RDW.
Renal function tests, including creatinine and urea.
Liver function tests, including AST, ALT, ALP, LDH and GGT.
Lipid profile, including low density lipoprotein-cholesterol (LDL-c), high density lipoprotein-cholesterol (HDL-c), Triglyceride, total cholesterol, and fasting plasma glucose.
To compare the effect of high dose with low dose oral vitamin D3 administration on 28-day all-cause mortality rate in hospitalized adults infected with SARS-CoV-2.
Discussion
The emerging rapid dissemination and increasing mortality of COVID-19 have resulted in the administration of various empirical medications and supplements without solid evidence for their effectiveness (Huttner et al., 2020; Shin, 2020; Vijayvargiya et al., 2020). However, considerable numbers of the studied medications were not effective against COVID-19 till preparing this protocol. Theoretically, an agent that has the potential to prevent virus replication and cytokine storm at the same time can be considered as the most effective treatment in this disease (Clark, 2020; Hirawat et al., 2021). Based on previous studies, vitamin D has the potential to be effective in both pathways (Arboleda and Urcuqui-Inchima, 2020; Farid et al., 2021; Gilani et al., 2021; Jakovac, 2020; Khan et al., 2021). Furthermore, vitamin D has immunomodulatory effects that can hypothetically prevent or reduce the cytokine storm in the process of COVID-19 through augmentation of the innate immune response and reducing the acquired immune system response to COVID-19 (Gasmi et al., 2020; TurrubIATes-HernánDez et al., 2021; Yaqinuddin et al., 2021). Cross-sectional studies showed a relationship between serum vitamin D levels and COVID-19 severity and outcome (Katz et al., 2021; Kazemi et al., 2021; Luo et al., 2021; Yadav et al., 2021). Therefore, vitamin D administration was considered in some COVID-19 treatment protocols without confirmed evidence. On the other hand, the findings of currently published RCTs on the effects of vitamin D administration on severity and disease outcome in COVID-19 patients are controversial (Butler-Laporte et al., 2021; Murai et al., 2021; Shah et al., 2021). The dose of vitamin D required to protect our body against COVID-19 infections still not clear. Following medical evidence, serum vitamin D concentrations of 50 to 60 ng /mL seem to be suitable (Chakhtoura et al., 2020). In this respect, the first stage consists of a high initial dose followed by a lower maintenance dose. Studies reported that to attain the above serum concentration needed 4000 IU vitamin D/day (for over 12 weeks) or 11,000 IU /day (for 4 weeks) in vitamin D deficient people. Recently, a study recommended that doses ranging from 4000 IU to 10,000 IU (for bone action and non-calcemic effects, respectively) are effective and safe to attain the beneficial effects of vitamin D (Ferder et al., 2020).
The findings of this RCT might provide evidence about accepting or rejecting the hypothesis that daily dose of 10,000 IU vitamin D in the form of drop for 29 days administered to COVID-19 patients is effective in reducing admission duration, disease severity and mortality. Due to the adequate sample size, this RCT can produce reliable findings that will help clinicians and researchers in decision making to whether include vitamin D administration in the treatment protocol of COVID-19 patients or perform the administration with caution till further studies provide more evidence in this regard.
Conclusion
We describe the protocol for a clinical trial design investigating the effects of high dose vitamin D supplementation as a nutritional intervention strategy on biochemical and inflammatory factors in adults with COVID-19. Our hypothesis is that oral supplementation of 10,000 IU of vitamin D for one month, will decrease the inflammation and improve clinical outcomes in the covid-19 patients. Finding of the current study, negative or positive, could provide a step change in the evidence guiding current and future policies regarding the validity, dosage and duration of vitamin D administration as complementary treatment in COVID-19 patients.
Acknowledgements
We sincerely thank all patients participating in this study in advance, because this study would not be possible without their cooperation. We also express our appreciation to those who helped us in in this study.
This study is funded by Mashhad University of Medical Sciences (grant nu: 981873).
Abbreviation
- Hs-CRP
High sensitive C - reactive protein
- NLR
Neutrophil-to-lymphocyte ratio
- ALP
Alkaline phosphatase
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- Ca
calcium
- Cr
Creatinine
- ESR
Erythrocyte sedimentation rate
- FBG
Fasting blood glucose
- GGT
Gamma-glutamyl transferase
- HDL-c
High-density lipoprotein cholesterol
- LDH
Lactate Dehydrogenase
- LDL-c
Low-density lipoprotein cholesterol
- P
Phosphate
- PLR
Platelet-to-lymphocyte ratio
- RDW
Red Cell Distribution Width
- TG
Triglycerides
Footnotes
Availability of data and materials: The datasets collected and/or analyzed during the present study are not publicly accessible due to ethical concerns but corresponding author may provide datasets upon reasonable request.
Authors’ contributions: MGH, HV, RR, ZL, NM, MM initially conceptualized and designed the study. PSH, ZKH and AJ upgraded the protocol design. MGH contributed to obtaining the initial funding. The manuscript was written by ZKH, PSH and AJ and was reviewed by all members. AJ was responsible for the design optimizing and statistical analysis. EH, MSH, OA and RE contribute sampling. GF performed English editing. All authors read and approved the final manuscript.
Consent for publication and ethical approval to the paper: Ethical approval was obtained from ethics committee of MUMS. The ethical approval code is IR.MUMS.REC.1399.237. The informed consent will be obtained from all study participants or their legal guardian.
ORCID iDs: Reza Rezvani https://orcid.org/0000-0003-3585-9854
Hasan Vatanparast https://orcid.org/0000-0003-2621-8385
Majid Ghayour Mobarhan https://orcid.org/0000-0002-1081-6754
Trial registration: This trial is registered at clinicaltrials.gov (ID: IRCT20110726007117N11) on July 6, 2020.
Trial status: The trial enrollment started on 22 January 2021 and currently is collecting data. Collection labour data of patients expected to take about 4 months.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Mashhad University of Medical Sciences, (grant number 981873).
Supplemental Material: Supplemental material for this article is available online.
References
- Arboleda JF, Urcuqui-Inchima S. (2020) Vitamin D supplementation: A potential approach for coronavirus/COVID-19 therapeutics? Frontiers in Immunology 11: 1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baktash V, Hosack T, Patel N, et al. (2021) Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgraduate Medical Journal 97: 442–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler-Laporte G, Nakanishi T, Mooser V, et al. (2021) Small increases in vitamin D are not predicted to decrease in COVID-19 (Mendelian randomization)–June 2021. PLoS Medicine 18: e1003605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakhtoura M, Napoli N, Fuleihan GEH. (2020) Commentary: Myths and facts on vitamin D amidst the COVID-19 pandemic. Metabolism: Clinical and Experimental 109: 154276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark IA. (2020) Background to new treatments for COVID-19, including its chronicity, through altering elements of the cytokine storm. Reviews in Medical Virology 31: e2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eskandari S, Heravi KM, Rejeh N, et al. (2015) Translation and validation study of the Iranian version of Minnesota living with heart failure questionnaire.
- Farid N, Rola N, Koch EA, et al. (2021) Active vitamin D supplementation and COVID-19 infections. Irish Journal of Medical Science 190: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferder L, Martín Giménez VM, Inserra F, et al. (2020) Vitamin D supplementation as a rational pharmacological approach in the COVID-19 pandemic. American Journal of Physiology-Lung Cellular and Molecular Physiology 319: L941–L948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasmi A, Tippairote T, Mujawdiya PK, et al. (2020) Micronutrients as immunomodulatory tools for COVID-19 management. Clinical Immunology 220: 108545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilani SJ, Bin-Jumah M, Nadeem MS, et al. (2021) Vitamin D attenuates COVID-19 complications via modulation of proinflammatory cytokines, antiviral proteins, and autophagy. Expert Review of Anti-Infective Therapy 20: 231–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirawat R, Saifi MA, Godugu C. (2021) Targeting inflammatory cytokine storm to fight against COVID-19 associated severe complications. Life Sciences 267: 118923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M, Kleine-Weber H, Schroeder S, et al. (2020) H., Nitsche A., Müller MA, Drosten C., Pöhlmann S. Cell 181: 271.
- Huttner B, Catho G, Pano-Pardo J, et al. (2020) COVID-19: Don’t neglect antimicrobial stewardship principles!. Clinical Microbiology and Infection 26: 808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakovac H. (2020) COVID-19 and vitamin D—Is there a link and an opportunity for intervention? American Journal of Physiology-Endocrinology and Metabolism 318: E589–E589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J, Yue S, Xue W. (2021) Increased risk for COVID-19 in patients with vitamin D deficiency. Nutrition (Burbank, Los Angeles County, Calif.) 84: 111106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemi A, Mohammadi V, Aghababaee SK, et al. (2021) Association of vitamin D status with SARS-CoV-2 infection or COVID-19 severity: A systematic review and meta-analysis. Advances in Nutrition 12: 1636–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan AH, Nasir N, Nasir N, et al. (2021) Vitamin D and COVID-19: Is there a role? Journal of Diabetes & Metabolic Disorders 20: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo X, Liao Q, Shen Y, et al. (2021) Vitamin D deficiency is associated with COVID-19 incidence and disease severity in Chinese people. The Journal of Nutrition 151: 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani J, Giménez VMM, Bergam I, et al. (2021) Association between vitamin D deficiency and COVID-19 incidence, complications, and mortality in 46 countries: An ecological study. Health Security 19: 302–308. [DOI] [PubMed] [Google Scholar]
- Montazeri A, Goshtasebi A, Vahdaninia M, et al. (2005) The short form health survey (SF-36): Translation and validation study of the Iranian version. Quality of Life Research 14: 875–882. [DOI] [PubMed] [Google Scholar]
- Munro BH. (2005) Statistical Methods for Health Care Research. Philadelphia, PA, USA: Lippincott Williams & Wilkins. [Google Scholar]
- Munshi R, Hussein MH, Toraih EA, et al. (2021) Vitamin D insufficiency as a potential culprit in critical COVID-19 patients. Journal of Medical Virology 93: 733–740. [DOI] [PubMed] [Google Scholar]
- Murai IH, Fernandes AL, Sales LP, et al. (2021) Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial. JAMA 325: 1053–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal R, Banerjee M, Bhadada S, et al. (2021) Vitamin D supplementation and clinical outcomes in COVID-19: A systematic review and meta-analysis. Journal of Endocrinological Investigation 45: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radujkovic A, Hippchen T, Tiwari-Heckler S, et al. (2020) Vitamin D deficiency and outcome of COVID-19 patients. Nutrients 12: 2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah K, Saxena D, Mavalankar D. (2021) Vitamin D supplementation, COVID-19 and disease severity: A meta-analysis. QJM: An International Journal of Medicine 114: 175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin H-S. (2020) Empirical treatment and prevention of COVID-19. Infection & Chemotherapy 52: 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TurrubIATes-HernánDez FJ, Sánchez-Zuno GA, GOnzáLez-esTeVez G, et al. (2021) Potential immunomodulatory effects of vitamin D in the prevention of severe coronavirus disease 2019: An ally for Latin America. International Journal of Molecular Medicine 47: 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayvargiya P, Garrigos ZE, Almeida NEC, et al. (2020) Treatment considerations for COVID-19: A critical review of the evidence (or lack thereof). Mayo Clinic Proceedings 95: 1454–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav D, Birdi A, Tomo S, et al. (2021) Association of vitamin D status with COVID-19 infection and mortality in the Asia Pacific region: A cross-sectional study. Indian Journal of Clinical Biochemistry 36: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaqinuddin A, Ambia AR, Alaujan RA. (2021) Immunomodulatory effects of vitamin D and vitamin C to improve immunity in COVID-19 patients. Journal of Health and Allied Sciences NU 12: 1–6. [Google Scholar]