Abstract
Background
Guided by the best practices adapted from national and international bodies including the World Health Organization (WHO), the Centers for Disease Control (CDC), and the UK Joint Biosecurity Centre (JBC), this paper aims to develop and provide an empirical risk stratification and assessment framework for advancing the safe resumption of global travel during the COVID-19 pandemic.
Method
Variables included in our model are categorized into four pillars: (i) incidence of cases, (ii) reliability of case data, (iii) vaccination, and (iv) variant surveillance. These measures are combined based on weights that reflect their corresponding importance in risk assessment within the context of the pandemic to calculate the risk score for each country. As a validation step, the outcome of the risk stratification from our model is compared against four countries.
Results
Our model is found to have good agreement with these benchmarked risk designations for 27 out of the top 30 countries with the strongest travel ties to Malaysia (90%). Each factor within this model signifies its importance and can be adapted by governing bodies to address the changing needs of border control policies for the recommencement of international travel.
Conclusion
In practice, the proposed model provides a turnkey solution for nations to manage transmission risk by enabling stakeholders to make informed, evidence-based decisions to minimize fluctuations of imported cases and serves as a structure to support the improvement, planning, and activation of public health control measures.
Keywords: SARS-CoV-2, COVID-19, Country risk stratification, International travel reopening, Weighted score, Malaysia
1. Introduction
International travel restrictions and border controls have been implemented across many countries in a global effort to contain the spread of the SARS-CoV-2 virus [[1], [2], [3]]. With much of the world dependent on global movements of people, goods and services, most travel bans and restrictions have had significant effects on local, regional, and global economies. Tourism is one of the key economic sectors that has been severely impacted; in Malaysia, for example, the industry accounts for 5.9% of the total gross domestic product and employs nearly a fourth of the nation's workforce [4]. Furthermore, border restrictions have had a significant impact on those who are seeking asylum, protection, and medical treatment [5], and those travelling for family, work, and education purposes.
As the pandemic evolves and as vaccination coverage widens, the easing of border control is progressively being rolled out worldwide at varying degrees of stringency and speed [6]. The reopening of international travel amid the pandemic, however, requires extensive and multi-factorial considerations and approaches. Harnessing these constructs contributes to data-driven insights for safe reopening during and beyond the outbreak, which can be used by policymakers and key stakeholders in formulating strategic policies in an effort to limit the number of imported cases and the transmissibility risk of new variants as one of the multi-pronged approaches in handling the COVID-19 crisis.
This paper aims to provide a risk stratification and assessment framework in supporting the safe reopening of international travel by evaluating four pillars of measures that have been identified as among the key drivers in building a comprehensive country risk profile during the pandemic: (i) incidence of cases, (ii) reliability of case data, (iii) vaccination, and (iv) variant surveillance. The proposed approach helps to weigh the relative importance of various measures in formulating a single holistic measure that can be used to assess the overall risk of individual countries. Travel policies, testing, and quarantine regimes for international arrivals can therefore be adapted to ensure adequate protection of travellers and the general population, and in guarding the home country's healthcare system from being overwhelmed.
2. Method
2.1. Overview of proposed model
We present here an empirical model for robust risk assessment and stratification that is based on a combination of best practices adopted from the World Health Organization (WHO) [2], the Centers for Disease Control (CDC) [3], and the UK Joint Biosecurity Centre (JBC) [7], in addition to our own selection of additional parameters and methodology. Parameters for the model calculation are categorized into four pillars: (i) incidence of cases, (ii) reliability of case data, (iii) vaccination, and (iv) variant surveillance. The list of parameters used and their definitions are shown in Table 1 . Weighted values for parameters within each pillar are combined, and the resulting score from each pillar is then weighted and summed across all four pillars. The resulting score will be used in the risk assessment and stratification for each country.
Table 1.
Parameters included in our risk assessment framework and their corresponding definitions, with comparisons to the indicators used in the frameworks employed by WHO, CDC, and JBC.
| Pillar | Parameter | Definition | WHO [2] | CDC [3] | JBC [7] |
|---|---|---|---|---|---|
| (1) Incidence of cases |
Cases per million population, 7-day average | New cases divided by population x 1 million, averaged over 7 days. | ✓ | ✓ | ✓ |
| Change in cases vs. cases in the preceding 14 days | Difference between cases per 1 million population (7-day average) on latest date and cases per 1 million population (7-day average) as of 14 days ago. Categorization format: 0 = Decreasing, 1 = Increasing at low rate (below 100), 2 = Increasing at high rate (above 100). | ✓ | |||
| (2) Reliability of case data |
Test positivity rate, 7-day average |
New cases divided by total daily tests conducted, averaged over 7 days [31] | ✓ | ✓ | |
| Tests per 100 population, 7-day average |
Number of tests done per 100 population | ✓ | ✓ | ||
| Trust in COVID-19 information from government (%) | Percentage of UMD Global CTIS survey respondents who declared their trust in COVID-19 information that came from government health departments [14]. | ||||
| (3) Vaccination |
Vaccinated population (%) | Percentage of total population that have completed full course of COVID-19 vaccination as prescribed by the protocol. | ✓ | ||
| Case fatality rate, 7-day average |
Ratio between the 7-day average of deaths and the 7-day average of cases 10 days earlier. | ||||
| (4) Variant surveillance |
Genome sequencing capability | Number of sequencing samples uploaded to GISAID over the past 2 weeks divided by total number of cases over 2 weeks prior to upload date x 100. Categorization format: 0 = Excellent (more than 1%), 1 = Moderate (less than 0.1%), 2 = None (no sequencing) | ✓ | ||
| Genome sequencing reporting delay | Categorization is based on the number of days since the last genomic sequencing data uploaded to GISAID [12]. Categorization format: 0 = Timely (less than 2 weeks), 1 = Late (more than 2 weeks), 2 = None (no sequencing done). | ||||
| Presence of very high priority variant of concern | Flags if a very high priority variant of concern is detected. Categorization format: 0 = Not present, 1 = Present. | ✓ |
Note: Definitions shown in Table 1 reflect the objectives of this paper and may not necessarily match the exact definitions used by WHO, CDC and JBC.
2.2. Parameters
Unless indicated otherwise, country-level data on epidemiological and vaccination parameters outlined in this section is sourced from Our World Data, a project of the Global Change Data Lab [8]. Also, due to variations in national reporting policies or data collection capacity, not all parameters required by the model is available for all countries and territories. To circumvent this limitation so that all countries and territories are compared on an equal footing, we used linear regression to produce estimates for these missing data points (the methodology is described in detail in the Supplementary Material).
2.2.1. Pillar 1: Incidence of cases
Pillar 1 is a measure of disease burden, which includes the number of daily COVID-19 cases per million population, as well as the change in this indicator over a 14-day period. The latter provides an assessment of near-future trends in the country's disease burden [9]. In this framework, we use a 7-day average as a more stable measure of incidence rates, given that there may be large fluctuations in the number of daily cases [10]. This pillar gives insight to the extent of disease transmission in a country, as well as the progress made by governments in managing the pandemic. Many countries have employed incidence rate systematic indicator monitoring to guide decision-making for COVID-19 reopening, mitigation, and response efforts such as the Indicator Monitoring Report (IMR) tool deployed in the United States [9]. The incidence rate is identified as one of the key metrics because it allows decision-makers to have a broad overview of a country's pandemic situation [11] as well as the rate at which new infections emerge.
2.2.2. Pillar 2: Reliability of case data
As the availability, quality, and completeness of data varies between countries due to factors such as testing resources and policies, we require supporting indicators to gauge the reliability of the official government case data presented in Pillar 1. The parameters included in Pillar 2 are the number of tests conducted per 100 population and the test positivity rate, both based on a 7-day average. The latter is defined as the number of daily cases divided by the number of tests conducted. The WHO recommends a test positivity rate of less than 5%, and a test positivity rate higher than this rate is indicative of insufficient population-based testing [11]. Moreover, the WHO recommends around 10 to 30 tests per confirmed case as a general benchmark for adequate testing [12]. By including testing rates, our model can help experts gauge if testing is done widely enough in the country of interest to capture most cases. Assessing the positivity rate is a critical step to help visualize the true distribution of cases, and if the spread of the virus in each country is under control.
Beyond testing, statistics on the level of public trust in COVID-19 information from their respective governments also act as an additional barometer on the reliability of official case and testing data and is an important predictor of public compliance to risk mitigation programmes [13]. Data for this variable is obtained from the daily survey results of the University of Maryland's Social Data Science Centre Global COVID-19 Trends and Impact Survey, in partnership with Facebook (UMD Global CTIS) [14].
2.2.3. Pillar 3: Vaccination
Pillar 3 encompasses vaccination coverage and the case fatality rate, which are critical components in estimating the risk of infection and deaths rates among infected populations within a geographic region. We describe vaccination coverage as the percentage of the population that has received the full course of COVID-19 vaccination as prescribed by the government or manufacturer protocol whereas the case fatality rate moving average helps to ascertain real-time vaccine effectiveness against mortality and better depicts the heterogeneity of recent cohorts.
High levels of vaccination have been shown to effectively reduce the risk and severity of infection [15,16]. With the E484K mutation seen in Beta, Gamma, Zeta, Eta, and Theta variants, a single dose of vaccine has an effectiveness of up to 70% against hospitalization and death [17]. Neutralizing antibodies against Omicron were identified in only 30–37% of those who received two vaccination doses [18]. Three doses of vaccine were found to be 94% and 90% effective in avoiding COVID-19-related hospitalizations throughout the Delta- and Omicron-predominant phases of the pandemic, respectively [19]. Therefore, countries with high vaccination coverage, such as the United Arab Emirates and Singapore, are deemed to be low risk. Furthermore, vaccine-acquired immunity has been associated with lower viral loads, thereby reducing the transmissibility of the virus [20]. According to the CDC, vaccinated individuals are five times less likely to be infected [21], thereby protecting local communities and reducing the likelihood of passing on COVID-19. With this backdrop, a vigilant approach towards vaccinated travellers is pivotal to prevent the resurgence of imported cases that could threaten to overwhelm the host country's healthcare system.
2.2.4. Pillar 4: Variant surveillance
With the recent emergence of variants of concern that may be more transmissible and evade vaccine-acquired immunity, there is a pressing need to consider individual country's capacity to conduct sufficient genomic sequencing and report the results in a timely manner [22,23]. In Pillar 4, we include measurements on the proportion of COVID-19 cases over the preceding 14 days that were sequenced as reported in GISAID via CoVariants.org [24], the number of days since the last sequencing data was uploaded to GISAID [24,25], and the presence of very high priority variants of concern, such as the Omicron variant which is found to be more transmissible than previously reported variants [24,25]. It is important to note that the availability of information about the presence of variants of concern hinges on a country's capacity to conduct genome sequencing, the lack of which could severely impact the pandemic, especially with increasing volume of international travel. Considering this factor also allows the host country to identify novel variants and trace their evolution in different countries, which is critical for revealing significant pathways of dissemination and supporting sentinel surveillance in travel medicine.
2.3. Country risk value calculation
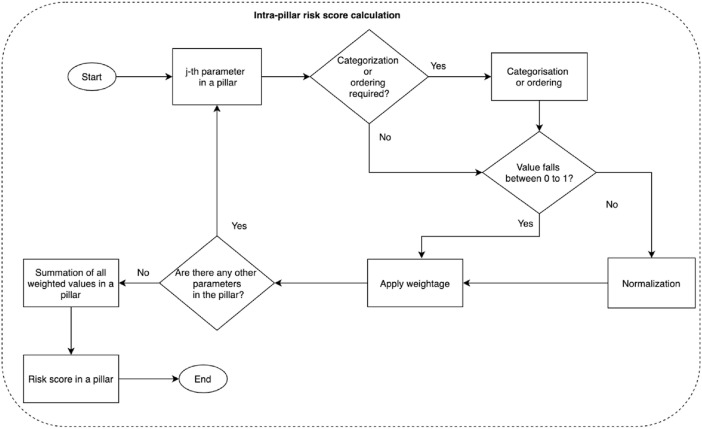
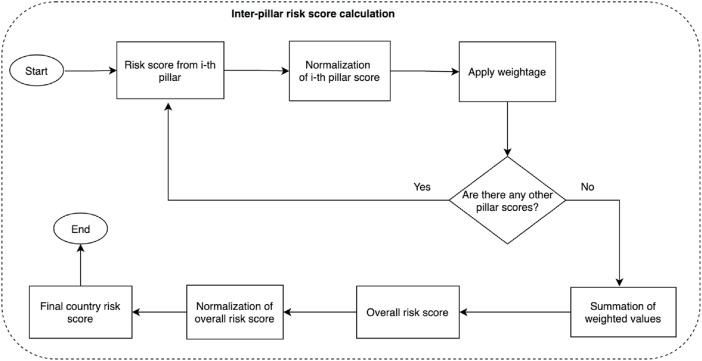
Measures for risk assessment are split into four pillars as described in Table 1, which are then combined to obtain the overall risk profile. This process is divided into two steps: (i) intra-pillar risk value calculation whereby parameters in each pillar are combined to obtain a risk score for a given pillar (Fig. 1 a), followed by (ii) inter-pillar risk score calculation whereby the output from each of four pillars are combined to obtain an overall country risk score (Fig. 1 b).
Fig. 1a.
Intra-pillar risk assessment score calculation flowchart.
Fig. 1b.
Inter-pillar risk assessment score calculation flowchart.
The weight for each parameter and pillar is determined based on the local and global landscape of the pandemic at the time the model is applied, in order to assign their relative order of importance. In deciding on the most appropriate weights to be used, we consider the priorities that are adopted by other countries such as the JBC in the UK [7], guidelines from the WHO [2], best practices and trends observed in the travel policies of other countries, and the expert opinions of our team of epidemiologists and public health specialists. In this model, we assign the highest weight to Pillar 3 (vaccination), followed by Pillar 4 (variant surveillance). We assign equal weights to Pillar 1 (incidence of cases) and Pillar 2 (reliability of case data) to balance the importance of the epidemiological data against the credibility of that data. The emphasis on both the incidence data and its reliability was also observed in the risk assessment framework by the CDC [3]. Aside from inter-pillar weights, the variables within each pillar are also assigned with weights based on their relative importance of each variable to the risk assessment. For simplicity and ease of interpretation, we have assigned the inter-pillar and intra-pillar weights with integer values between 1 and 5, with 5 reflecting the highest priority, as shown in Table 2 .
Table 2.
Weightage used in the model for intra-pillar and inter-pillar calculations.
| COVID-19 variable | Intra-pillar weight | Pillar | Inter-pillar weight |
|---|---|---|---|
| Cases per million population, 7-day average | 5 | (1) Incidence of cases |
1 |
| Change in cases per million population vs. preceding 14 days | 3 | ||
| Test positivity rate, 7-day average | 5 | ||
| Tests per 100 population, 7-day average | 3 | (2) Reliability of case data |
1 |
| Trust in COVID-19 information from the government % | 1 | ||
| Vaccinated population % | 5 | (3) Vaccination |
5 |
| Case fatality rate %, 7-day average | 2 | ||
| Genome sequencing capability | 3 | (4) Variant surveillance |
3 |
| Genome sequencing reporting delay | 2 | ||
| Presence of very high priority variant of concern | 5 |
Note: Weights shown are tailored to the situation of the pandemic situation as of October 6, 2021. As the situation continuously evolves, the weights should be adapted to the present-day priorities as outlined in the upcoming Section 4.
Normalized weighted values of all parameters within the same pillar are summed to obtain the combined risk score for that pillar as shown in Fig. 1a. The overall country risk score is then obtained through the summation of the normalized weighted score from each of the four pillars (Fig. 1b). The normalization method is based on the lowest and highest values drawn from a pool of all geographical entities included in the dataset; in this paper, it includes 224 countries and territories. Details on the normalization technique and other data pre-processing steps are available in the Supplementary Material.
The calculation of the overall country risk score from the parameter values can therefore be summarized in the formula below:
Let be the risk score for -th pillar where .
Let be the -th normalized parameter values in -th pillar.
Let be the weights assigned to the -th variable in -th pillar.
Let be the normalized risk score for -th pillar where .
Let be the weights assigned to each -th pillar.
Let be the overall risk score for a country before the final normalization.
So,
After the overall country risk score is obtained, we apply a final normalization so that all scores lie between 0 and 1. To stratify countries or territories by risk, the normalized overall country risk score is compared against a threshold value. If the resulting country score is below this threshold, the country is assigned to be low risk. Details on determining this threshold value will be covered in detail in Section 3.3.
3. Results
In the results reported below, we assume the position of the Malaysian authorities in assessing the risk profile for international arrivals from Australia, as an example, but the model can be adapted to any receiving or departing country of choice. We chose Australia as it is home to one of the largest Malaysian diaspora communities [26]. In addition, the volume of air traffic between Malaysia and Australia in 2020 was higher than that of other major global hubs such as the United Kingdom and the United Arab Emirates [27] despite less restrictive immigration and quarantine policies compared to Australia.
3.1. Calculation of risk assessment
Using parameter values that were sourced from Our World in Data, UMD Global CTIS, and GISAID via CoVariants.org (latest available data retrieved on October 6, 2021), the country risk score for Australia was derived based on the principles previously outlined in Section 2 and is summarized in Table 3 (detailed step-by-step calculations are shown in Supplementary Tables S1 and S2). The overall country risk score for Australia is 0.31.
Table 3.
Sample calculation of country risk score for Australia as of October 6, 2021.
| Value | Categorized | Normalized | Weight | Weighted | ||
|---|---|---|---|---|---|---|
| Pillar 1 | Cases per million population, 7-day average | 82.6 | 0.08 | 5 | 0.38 | |
| Change in cases per million population vs. past 14 days | 17.4 | 1 | 0.50 | 3 | 1.50 | |
| Weighted score: Incidence of cases | 1.88 | |||||
| Pillar 2 | Test positivity rate %, 7-day average | 1.10 | 0.02 | 5 | 0.11 | |
| Test per 100 population 7-day average | 0.77 | 0.23 | 3 | 0.69 | ||
| (Mis)trust in COVID-19 info from the govt. % | 55.8 | 0.47 | 1 | 0.47 | ||
| Weighted score: Reliability of case data | 1.28 | |||||
| Pillar 3 | Population not fully vaccinated % | 52.3 | 0.52 | 5 | 2.62 | |
| Case fatality rate %, 7-day average | 0.82 | 0.05 | 2 | 0.09 | ||
| Weighted score: Vaccination | 2.71 | |||||
| Pillar 4 | Genome sequence samples to 14-day cases ratio | 0.76 | 1 | 3 | 3.00 | |
| Genome sequence reporting delay in days | 0.00 | 0 | 2 | 0.00 | ||
| Presence of very high priority variant of concern | 0.00 | 0 | 5 | 0.00 | ||
| Weighted score: Variants of concern | 3.00 | |||||
| Overall | Pillar 1: Incidence of cases | 1.88 | 0.23 | 1 | 0.23 | |
| Pillar 2: Reliability of case data | 1.28 | 0.15 | 1 | 0.15 | ||
| Pillar 3: Vaccination | 2.71 | 0.39 | 5 | 1.94 | ||
| Pillar 4: Variant surveillance | 3.00 | 0.30 | 3 | 0.90 | ||
| Weighted overall score | 3.23 | |||||
| Overall country risk score | 3.23 | 0.31 |
3.2. Risk stratification
The calculation process in Section 3.1 above is repeated for all 224 countries and territories in our dataset. The spread of normalized score values for each of the pillar and for the overall normalized scores generated by our model are shown by percentiles (displayed at 10-percentage point intervals) in Table 4 .
Table 4.
Distribution of normalized risk score by percentile, by pillar and for the overall stratification as of October 6, 2021.
| Percentiles of weighted risk scores |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0% | 10% | 20% | 30% | 40% | 50% | 60% | 70% | 80% | 90% | 100% | |
| Pillar 1: Incidence of cases | 0.00 | 0.00 | 0.00 | 0.01 | 0.02 | 0.04 | 0.11 | 0.19 | 0.22 | 0.36 | 1.00 |
| Pillar 2: Reliability of case data | 0.00 | 0.25 | 0.35 | 0.39 | 0.45 | 0.46 | 0.49 | 0.50 | 0.51 | 0.59 | 1.00 |
| Pillar 3: Vaccination | 0.00 | 0.24 | 0.28 | 0.38 | 0.45 | 0.52 | 0.61 | 0.67 | 0.71 | 0.73 | 1.00 |
| Pillar 4: Variant surveillance | 0.00 | 0.20 | 0.30 | 0.30 | 0.50 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Normalized country risk score | 0.00 | 0.20 | 0.27 | 0.36 | 0.47 | 0.55 | 0.62 | 0.72 | 0.80 | 0.84 | 1.00 |
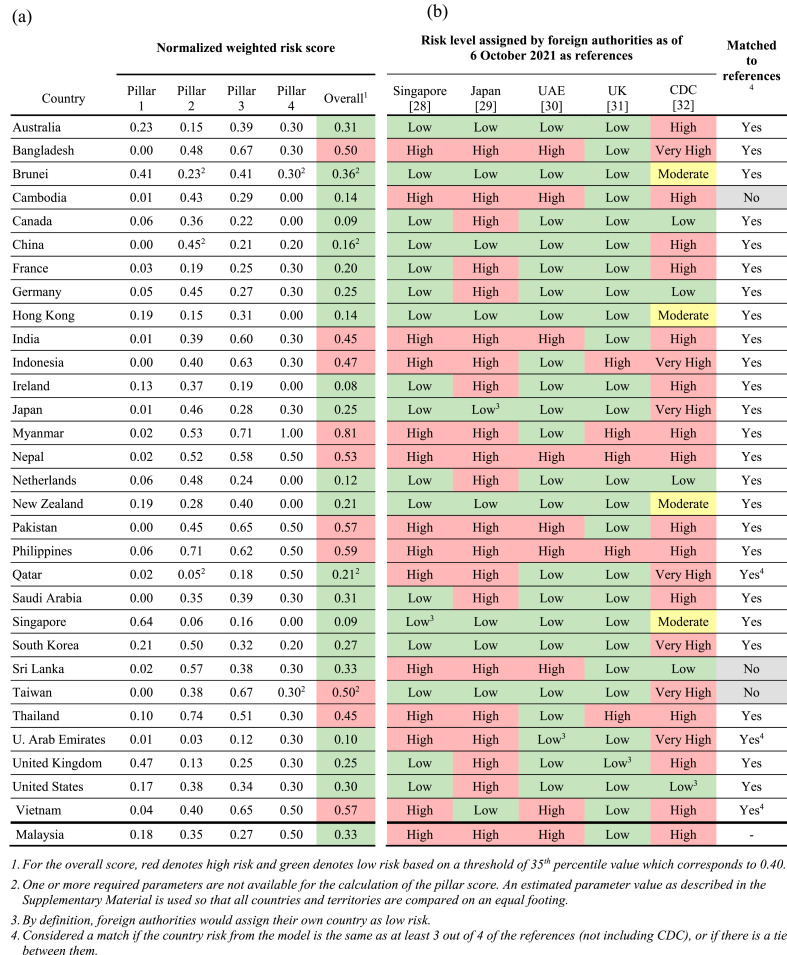
The normalized overall risk score for the top 30 countries that have the strongest travel ties to Malaysia is shown in Table 5 (a). In order to validate the result of our model, we compared our outcome with the risk status assigned by the authorities in Singapore, Japan, the Emirate of Abu Dhabi, and the United Kingdom. The level of risk designated by these foreign authorities as of October 6, 2021 are shown in Table 5(b). To streamline the definition of risk category across these multiple foreign designations, low risk for the context of this paper is taken to be Singapore's Categories I and II [28], countries that do not fall under the Denial of permission to entry category by Japan [29], the Emirate of Abu Dhabi's Green list [30], and countries that do not fall under the United Kingdom's Red list [31]. Risk level assigned by Centers for Disease Control and Prevention (CDC) is shown in Table 5(b) as a reference but is excluded from the comparison with the model output since CDC employs a four-category system (Low, Moderate, High, Very High) [32] that may not be objectively comparable to the two-category system employed by our model and the other reference countries.
Table 5.
(a) Result of normalized pillar-level and overall risk scores as calculated by our model for top 30 countries with the strongest travel ties to Malaysia and (b) Level of country risk as designated by other foreign authorities for references as of October 6, 2021.
In our model, a country is assigned to be either a low-risk or high-risk country if the normalized overall score is below or above a certain cut-off point. This threshold value is determined from the optimum percentile of the normalized overall scores drawn from all 224 countries and territories included in our dataset previously shown in Table 4. Based on the 35th percentile as the optimum threshold (the derivation of this optimal selection will be covered in the upcoming Section 3.3), the normalized overall score for each of the top 30 countries in Table 5(a) are assigned to be either low-risk (marked as green) or high-risk (marked as red).
Note that the cut-off score for a threshold of 35th percentile below which a country is designated as low risk in the example in Table 5(a) corresponds to 0.40 based on the methodology used to derive Table 4 (which lies between 30% and 40% under the overall risk factor). This cut-off score should not be incorrectly taken as 0.35 (the decimal representation of 35%) when dealing with the corresponding percentile values.
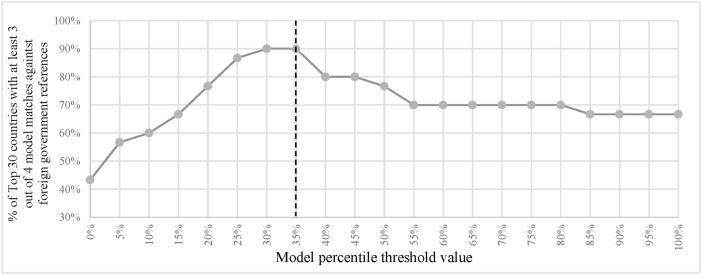
3.3. Threshold selection
We consider our results to be reliable if the outcome of the derived risk level for a given country is similar to those assigned by at least three out of the four benchmarked countries for risk stratification as shown in Table 5(b). In order to determine the optimum value of threshold that delivers the highest degree of accuracy based on this definition, we modulate the percentile threshold at 5-percentage point intervals from 0 to 100% and observe the resulting proportion of countries that are matched. For this validation stage, we evaluate the outcome from only the top 30 countries and territories listed in Table 5(a) as these are the priorities in the context of border reopening in Malaysia. As shown in Fig. 2 , the optimal percentile threshold for the dataset that we worked with is found to be 35th percentile, where the result of our risk stratification is in accordance with at least three out of the four benchmarked countries for 90% or 27 out of the top 30 countries.
Fig. 2.
Selection of the optimal threshold value for risk stratification.
3.4. Risk assignment
The overall normalized weighted score for Australia is 0.31, as shown in Table 3. Based on the spread of percentile values in Table 4, it can be read that 0.31 lies below the 35th percentile cut-off (which corresponds to a score threshold of 0.40), which indicates that Australia is a low-risk country.
While we have been solely discussing the overall risk thus far, the same principle also applies to the normalized score by pillar and their corresponding threshold value. For example, when looking at the risk profile of Australia from the point of Pillar 3 (vaccinations) only, it is also categorized as low risk as the pillar score of 0.39 also lies within the 35th percentile range of Pillar 3 (Table 4). In addition, although our model only refers to two risk categories (low and high), it can be adapted to include additional categories by adding the appropriate number of threshold values across the percentile distribution.
While the high or low risk assignment alone may be sufficient to gauge the level of risk of a given country, the overall normalized weighted score can also be used to compare the risk of travellers from the departing country (in this example, Australia at 0.31) against the receiving country (Malaysia at 0.33) following comparable principles advocated by WHO [2] to further assess the risk. In this example, it can be concluded that the arrivals from Australia would not exacerbate the prevailing COVID-19 situation in Malaysia given its lower risk score.
3.5. Extending the model over time
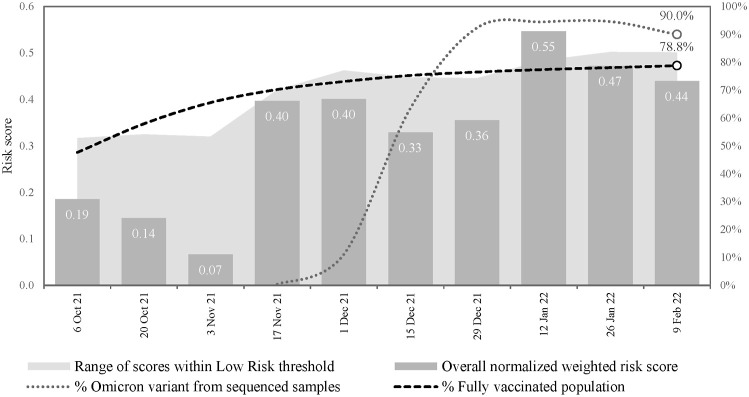
To demonstrate the agility of the model over time, we included data between October 6, 2021 and February 9, 2022 in two-week intervals. For simplicity, we maintained the same intra- and inter-pillar weights as the analysis in Table 3. The resulting normalized overall risk score and risk stratification for Australia as well as the low-risk threshold value is summarized in Fig. 3 . The proportion of fully vaccinated population and the prevalence of Omicron [25] as the new dominant strain are also shown to highlight the evolution of risk stratification against the evolving nature of the pandemic. Here, we show that Australia's risk remained low over time, except for the two-week interval beginning on January 12, 2022, when it surpasses the low-risk threshold value. This spike in the overall normalized weighted score is largely driven by the exceptionally high case positivity rate of over 40% during that brief period [8].
Fig. 3.
Risk score calculation for Australia between October 2021 and February 2022.
4. Discussion
As the pandemic prolongs into its third year, there is an urgent need to revive national and global economies which are heavily reliant on international trade and tourism [33,34]. Governments face the arduous task to balance the health of their people against the economic well-being of the country in a situation that is constantly evolving. We developed a data-driven model for COVID-19 risk assessment and stratification that can be adapted by governing bodies to address the changing needs of border control policies during the pandemic. To validate our model, we performed a side-by-side comparison with risk designations by the governments of Singapore, Japan, the Emirate of Abu Dhabi, and the United Kingdom, as well as an evaluation of how risk profiling changed over time as the pandemic evolved in Australia.
Early in the pandemic, statistical models that predicted spread of disease or the risk of importing the virus were used to define travel restrictions and border control [35]. However, given the current epidemiology of COVID-19 cases, such as the emergence of high priority variants of concern and with the introduction of population-based vaccinations, a more complex yet flexible model for risk assessment is required. Our model proposes to be a source of information that decision-makers can use to assess the risk of inbound and outbound travels during the pandemic. The model can help governments define and appropriately allocate resources for targeted public health control measures, such as improving capacity for testing and quarantine of travellers from high-risk countries [22]. Data-driven strategies, like our model, can also be used to inform on travel advisories and other preventative public health measures for outbound travel, to prevent the import of cases into the home country [35].
The proposed model discussed in this paper provides the flexibility to accommodate the dynamic situation and evolving national priorities. For example, with the emergence of the Omicron variant in late November 2021, governments may require a risk stratification approach that integrates critical information about the genome sequencing capacity in other countries in their travel risk assessment. In reference to our model, countries can adapt to the evolving nature of the pandemic with respect to variants of concern by increasing the weight for Pillar 4. Conversely, if a country is currently facing lower than desired vaccination rates, governments may choose to give equal priority to the burden of disease (Pillar 1) and the presence of variants of concern (Pillar 4) in their travel risk assessments to prevent a surge of cases in their home country. While we use a simple integer scale for weights in this paper, it can be revised for better accuracy and precision as more evidence is generated over time. Additionally, the optimal percentile threshold value for risk stratification can be adjusted based on current national priorities. The value can be lowered to reflect a more cautious approach to border control, such as when a country's healthcare system is stretched, or if there is a threat of a critical variant of concern.
The proposed model serves as a guidance and comes with its own set of limitations. Formulating and adapting national policies and plans require consideration of various factors, including political and economic implications, which are not captured in this model. For example, while the US and the UK government policies and messaging on immigration and public health are by and large guided by data and advice from CDC and JBC, respectively, it is the government that has the final say on policy. This likely explains some of the differences between expert recommendations and their resulting implementation. Furthermore, it is crucial to exercise caution in interpreting the results in light of other known factors that may not be directly considered in the model. Using recent data from Australia as an example, we show that our model captured the effect of very high test positivity rate during the peak spread of the Omicron variant, but it does not take into account the lower severity of Omicron [36,37] nor the fact that the government went ahead with significant relaxation of restrictions in January 2022 [38], which implies that the situation in Australia may not be as risky as what the figures alone may suggest. In conclusion, there may be situations in which the model's risk stratification should be overruled, even more so to prevent the spread of an emerging, critical variant of concern which may not necessarily be reflected in the guiding dataset.
Data used for the proposed model is based on publicly available sources, and therefore we rely on transparent and timely reporting by all countries to paint the true picture of the pandemic. Due to different national policies or capacity to collect and report COVID-19 data, some data points may be missing, which we circumvent by employing our best estimate. The assumptions made to generate these estimates may have led to some biases and misclassification of risk, especially since the missing data was likely not at random. However, as better data sharing practices become more commonplace, these biases could be overcome.
The proposed model of COVID-19 travel risk assessment and stratification can change across time and can be adapted to meet national priorities in managing the pandemic. A model such as ours could improve timely, data-driven, and transparent decision-making by governments, which are crucial components of effective pandemic management.
Funding source
This research did not receive any specific grant for funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Approval was not required.
CRediT authorship contribution statement
Khairul Omar: Writing – original draft, formulated the research questions, conceptualized and designed the study, created the model, and collect data, Writing – review & editing, the literature review, and the manuscript's organisation, Formal analysis, performed the modelling and analysis, Visualization, prepared the tables and figures, All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Dhesi Baha Raja: Writing – original draft, formulated the research questions, conceptualized and designed the study, Supervision, coordinated the execution of the study. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Nur Asheila Abdul Taib: Writing – drafted the first manuscript, Writing – review & editing, and the manuscript's organisation, Visualization, prepared the tables. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Nadia Rajaram: Writing – original draft, Writing – review & editing, the literature review, and the manuscript's organisation, Visualization, prepared the tables and figures. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Jinat Ahmed: Writing – original draft, Writing – review & editing, the literature review, and the manuscript's organisation, Visualization, prepared the tables and figures. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. H.S. Arvinder-Singh: Writing – original draft, designed the study, Writing – review & editing, All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Siti Aisah Mokhtar: Writing – review & editing, All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Alvin Kuo Jing Teo: Writing – original draft, designed the study, Writing – review & editing, All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Lidwina Edwin Amir: Writing – review & editing, Supervision, coordinated the execution of the study. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Michelle Chan: Writing – review & editing, Supervision, coordinated the execution of the study. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Quek Yee Theng: Writing – review & editing, Supervision, coordinated the execution of the study. All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript. Choo-Yee Ting: Writing – original draft, conceptualized and designed the study, Writing – review & editing, All authors critically reviewed the manuscript for relevant intellectual content. All authors have read and approved the final version of the manuscript.
Declaration of competing interest
Authors declare no conflicts of interest.
Acknowledgments
Thanks to Nicholas Tan for his support in the data collection as well as Yeong May Luu and Vivek Jason Jayaraj for their contribution in the study's conceptualization.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tmaid.2022.102318.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.European Commission A common approach to travel measures in the EU. https://ec.europa.eu/info/live-work-travel-eu/coronavirus-response/travel-during-coronavirus-pandemic/common-approach-travel-measures-eu_en Accessed 3 Nov 2021 from:
- 2.World Health Organization Risk assessment tool to inform mitigation measures for international travel in the context of COVID-19. Annex to: considerations for implementing a risk-based approach to international travel in the context of COVID-19. 2020. https://web.archive.org/web/20211110153117/https://www.who.int/publications/i/item/WHO-2019-nCoV-Risk-based_international_travel-Assessment_tool-2020.1 from.
- 3.Centers for Disease Control and Prevention How CDC determines the level for COVID-19 travel health notices. 11 Feb. 2020. www.cdc.gov/coronavirus/2019-ncov/travelers/how-level-is-determined.html from.
- 4.Hirschmann R. Travel and tourism in Malaysia - statistics & facts. Statista. 18 Aug. 2021 www.statista.com/topics/5741/travel-and-tourism-in-malaysia/#dossierKeyfigures Available: [Google Scholar]
- 5.Ikotun O., Akhigbe A., Okunade S. Sustainability of borders in a post-COVID-19 world. Politikon. 2021;48(2):297–311. https://www.tandfonline.com/doi/full/10.1080/02589346.2021.1913804 Available: [Google Scholar]
- 6.World Nomads Which countries are open for tourism during COVID-19? 23 June 2021. www.worldnomads.com/travel-safety/worldwide/worldwide-travel-alerts Accessed 3 Nov 2021 from:
- 7.UK Health Security Agency Guidance: risk assessment methodology to inform international travel traffic light system. 29 Oct 2021. https://www.gov.uk/government/publications/covid-19-risk-assessment-methodology-to-inform-international-travel-traffic-light-system/risk-assessment-methodology-to-inform-international-travel-traffic-light-system Accessed 30 Nov 2021 from:
- 8.Ritchie H., Mathieu E., Rodés-Guirao L., et al. OurWorldInData.org; 2020. Coronavirus pandemic (COVID-19)https://ourworldindata.org/coronavirus from. [Google Scholar]
- 9.Varela K., Scott B., Prather B.J., et al. Primary indicators to systematically monitor COVID-19 mitigation and response — Kentucky, May 19–July 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1173–1176. doi: 10.15585/mmwr.mm6934e3. Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D.W.S. Wong, Y. Li, “Spreading of COVID-19: Density matters,” PLoS One, vol. 15, no. 12, e0242398. Available: 10.1371/journal.pone.0242398. [DOI] [PMC free article] [PubMed]
- 11.World Health Organization Public health criteria to adjust public health and social measures in the context of COVID-19. Annex to: considerations in adjusting public health and social measures in the context of COVID-19. 2020. https://www.who.int/publications/i/item/considerations-in-adjusting-public-health-and-social-measures-in-the-context-of-covid-19-interim-guidance from.
- 12.World Health Organization COVID-19 - virtual press conference - 30 march 2020. 2020. https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-30mar2020.pdf?sfvrsn=6b68bc4a_2 Available:
- 13.Lazarus J.V., Ratzan S., Palayew A., et al. COVID-SCORE: a global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10) PLoS One. 2020;15(10):e0240011. doi: 10.1371/journal.pone.0240011. Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.University of Maryland The global COVID-19 trends and impact survey open data API. https://gisumd.github.io/COVID-19-API-Documentation/ from.
- 15.Hodgson S.H., Mansatta K., Mallett G., et al. What defines an efficacious COVID-19 vaccine? A review of the challenges assessing the clinical efficacy of vaccines against SARS-CoV-2. Lancet Infect Dis. 2020;21:26–35. doi: 10.1016/S1473-3099(20)30773-8. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30773-8/fulltext Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liang L.L., Kuo H.S., Ho H.J., Wu C.Y. COVID-19 vaccinations are associated with reduced fatality rates: evidence from cross-county quasi-experiments. J Glob Health. 2021;11 doi: 10.7189/jogh.11.05019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8285768/ Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung H., He S., Nasreen S., et al. Effectiveness of BNT162b2 and mRNA-1273 covid-19 vaccines against symptomatic SARS-CoV-2 infection and severe covid-19 outcomes in Ontario, Canada: test negative design study. BMJ. 2021;374(1943) doi: 10.1136/bmj.n1943. Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gruell H., Vanshylla K., Tober-Lau P., et al. mRNA booster immunization elicits potent neutralizing serum activity against the SARS-CoV-2 Omicron variant. Nat Med. 2022 doi: 10.1038/s41591-021-01676-0. Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thompson M.G., Natarajan K., Irving S.A., et al. Effectiveness of a third dose of mRNA vaccines against COVID-19–associated emergency department and urgent care encounters and hospitalizations among adults during periods of Delta and Omicron variant predominance—VISION Network, 10 States, August 2021–January 2022. MMWR Morb Mortal Wkly Rep. 2022;71 doi: 10.15585/mmwr.mm7104e3. https://stacks.cdc.gov/view/cdc/113718 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levine-Tiefenbrun M., Yelin I., Alapi H., et al. Viral loads of Delta-variant SARS-CoV-2 breakthrough infections after vaccination and booster with BNT162b2. Nat Med. 2021 doi: 10.1038/s41591-021-01575. Available: [DOI] [PubMed] [Google Scholar]
- 21.Bozio C.H., Grannis S.J., Naleway A.L., et al. Laboratory-confirmed COVID-19 among adults hospitalized with COVID-19–like illness with infection-induced or mRNA vaccine-induced SARS-CoV-2 immunity — nine States, january–september 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1539–1544. doi: 10.15585/mmwr.mm7044e1. Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization Technical considerations for implementing a risk-based approach to international travel in the context of COVID-19: interim guidance. Annex to: policy considerations for implementing a risk-based approach to international travel in the context of COVID-19. 2 Jul 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Risk-based-international-travel-2021.1 Accessed 30 Nov 2021 from:
- 23.Robishaw J.D., Alter S.M., Solano J.J., et al. Genomic surveillance to combat COVID-19: challenges and opportunities. Lancet Microbe. 2021;2(e481–84) doi: 10.1016/S2666-5247(21)00121-X. Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.GISAID Freunde von GISAID e.V., “GISAID - HCov19 Variants.”. https://www.gisaid.org/hcov19-variants/ from.
- 25.Hodcroft E. Overview of variants in countries. Covariants.Org, CoVariants (c) 2020–2021 https://covariants.org/per-country from. [Google Scholar]
- 26.Australian Bureau of Statistics Census QuickStats country of birth: people in Australia who were born in Malaysia. 2016. https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/5203_036 from.
- 27.Malaysian Airports Holding Berhad Emerging stronger together: airports statistics 2020. http://annualreport2020.malaysiaairports.com.my/wp-content/uploads/2021/04/airportstatistics2020.pdf Available:
- 28.Immigration and checkpoint Authority of Singapore, “SafeTravel: travel health control measures (category I,II,III,IV) https://web.archive.org/web/20211011033540/https://safetravel.ica.gov.sg/shn-and-swab-summary from.
- 29.Ministry of Foreign Affairs of Japan Border enforcement measures to prevent the spread of novel coronavirus (COVID-19): Denial of permission to entry. https://web.archive.org/web/20211008104333/https://www.mofa.go.jp/ca/fna/page4e_001053.html from.
- 30.Abu Dhabi Department of Culture & Tourism COVID-Safe Travel: the ‘green’ list. https://web.archive.org/web/20211011075926/https://visitabudhabi.ae/en/plan-your-trip/covid-safe-travel/permitted-countries from.
- 31.UK Department of Transport UK department of health and social care, “guidance: red list of countries and territories. https://web.archive.org/web/20211007055106/https://www.gov.uk/guidance/red-list-of-countries-and-territories from.
- 32.Centers for Disease Control and Prevention Covid-19 travel recommendations. https://web.archive.org/web/20211006101030/https://wwwnc.cdc.gov/travel/noticescovid19 Accessed 10 March 2022 from:
- 33.Söderlund B. 2020. The impact of travel restrictions on trade during the COVID-19 pandemic,” voxeu.org.https://voxeu.org/article/impact-travel-restrictions-trade-during-covid-19 from. [Google Scholar]
- 34.OECD . OECD.org; 2020. OECD policy responses to coronavirus (COVID-19): tourism policy responses to the coronavirus (COVID-19)https://www.oecd.org/coronavirus/policy-responses/tourism-policy-responses-to-the-coronavirus-covid-19-6466aa20/ from. [Google Scholar]
- 35.McBryde E.S., Meehan M.T., Adegboye O.A., et al. Role of modelling in COVID-19 policy development. Paediatr Respir Rev. 2020;35:57–60. doi: 10.1016/j.prrv.2020.06.013. Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wolter N., Jassat W., Walaza S., et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study. Lancet. 2022;399(10323):437–446. doi: 10.1016/S0140-6736(22)00017-4. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)00017-4/fulltext Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.UK Health Security Agency, “SARS-CoV-2 variants of concern and variants under investigation in England: technical briefing update on hospitalisation and vaccine effectiveness for Omicron VOC-21NOV-01 (B.1.1.529),” 2021. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1045619/Technical-Briefing-31-Dec-2021-Omicron_severity_update.pdf.
- 38.Reuters, “Australia to push ahead with reopening amid record COVID-19 cases,” Reuters.com, 2022. Accessed on 10 Mar 2022 from: https://www.reuters.com/business/healthcare-pharmaceuticals/australia-push-ahead-with-reopening-amid-record-covid-19-cases-2022-01-03/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.