Abstract
Background:
Corneal collagen cross-linking (CXL) is considered an effective procedure for slowing down or eliminating the progression of keratoconus. New techniques, in combination with CXL, have been proposed to stop the evolution of keratoconus and improve the visual function.
Objective:
To evaluate the effectiveness of combined photorefractive keratectomy (PRK) with mitomycin-C (MMC) application and CXL in the management of grade 1–2 keratoconus over a 2-year follow-up.
Methods:
Fifteen eyes underwent topography-guided PRK with 0.02% MMC application immediately followed by standard CXL.
Results:
Best corrected visual acuity improved from 0.15 ± 0.11 logMAR to 0.08 ± 0.09 logMAR at 24 months (p < 0.0001) in treated eyes. Mean steepest meridian keratometry reduced from 48.79 ± 3.22 D at baseline to 46.16 ± 3.11 D at 24 months (p < 0.0001). Mean flattest meridian keratometry reduced from 45.18 ± 2.17 D preoperatively to 44.35 ± 2.19 D at 24 months (p < 0.0001).
Conclusion:
Simultaneous topography-guided PRK with MMC 0.02% application and standard CXL is a safe, promising and effective procedure in the treatment of mild and moderate keratoconus.
Keywords: corneal collagen crosslinking, keratoconus, mitomycin C, photorefractive keratectomy, refractive surgery
Introduction
Keratoconus is a slow, chronic, non-inflammatory, ectatic corneal disorder characterized by changes in corneal collagen structure and organization, with progressive corneal thinning, leading to distorted vision, irregular astigmatism and myopia. 1
In recent years, the corneal collagen cross-linking (CXL) procedure has found a broad international application for slowing down or eliminating the progression of keratoconus.2–6
The treatment of irregular astigmatism and ametropia due to keratoconus with topography-guided photorefractive keratectomy (PRK) has been used for about 10 years with good results.7–9 This technique is based on corneal tissue ablation fitted on an ideal corneal shape (usually a sphere) under the topography map guidance. Topography-guided PRK flattens not only some of the cone peaks but also an arcuate broader area of the cornea away from the cone, usually in the superior nasal periphery; this ablation pattern, like a hyperopic treatment, causes some amount of steepening, or elevation adjacent to the cone, effectively normalizing and smoothing the cornea. 10 However, this technique can cause long-term complications including keratoconus worsening with progressive corneal thinning and apical opacity up to corneal perforation.
New techniques, in combination with CXL, have been proposed to stop the evolution of keratoconus with improved functional vision, including intra-corneal rings and phakic intraocular lenses.11,12 Kanellopoulos and Binder were the first to treat patients affected by keratoconus with combined CXL and topography-guided PRK. The procedure was in two steps with 1-year interval: first CXL and then PRK technique. 2
Since then, other studies analysed the simultaneous use of topography-guided PRK followed immediately by CXL in progressive keratoconus. 13
However, there are some limitations related to the combined procedures risks. In fact, cross-linked corneas may have a different ablation rate compared with normal corneas, which could lead to unpredictable refractive PRK results. Moreover, the PRK technique could remove the cross-linked corneal tissue, therefore decreasing the stiffening effects of the CXL treatment. In addition, there is an increased risk of haze formation after PRK. 3
Majmudar et al. 14 first reported the use of mitomycin C (MMC) in humans as a modulator of wound-healing after refractive surgery. In addition, several studies reported a decrease of haze incidence after PRK surgery using MMC and showed a lower onset of other complications such as refractive regression.15,16 MMC, in fact, can block keratocyte activation, proliferation and myofibroblast differentiation that can lead to haze formation. 17
Therefore, the aim of this study was to evaluate the clinical outcome, effectiveness and the safety of simultaneous topography-guided PRK with 0.02% MMC application and CXL combined in patients affected by mild or moderate keratoconus over a long-term follow-up.
Material and methods
Population and baseline examination
This retrospective interventional study analysed patients with a diagnosis of mild or moderate keratoconus treated with combined PRK and CXL.
The inclusion criteria were stage 1 or 2 keratoconus (Amsler–Krumeich classification) documented by topography in the previous 12 months of observation, with a corneal thickness ⩾ 450 µm. The parameters defined to evaluate keratoconus progression were: worsening of uncorrected visual acuity (UCVA) and/or best corrected visual acuity (BCVA) of more than one Snellen line, an increase in central corneal astigmatism of at least 1.00 D, an increase in the maximum cone apex curvature of at least 1.00 D, and a reduction of at least 10 µm or more in the thinnest point. Progression was established as changes in all the above-indicated parameters.
Exclusion criteria were: patients below 18 years of age, loss to follow-up prior to the 2 years postoperative visit, advanced keratoconus (stage 3 or 4 Amsler–Krumeich classification), central corneal opacities, previous refractive surgery, history of herpetic keratitis, and pregnancy.
Baseline examination included UCVA and BCVA, slit-lamp examination, intraocular pressure (IOP) measurement, manifest and cycloplegic refraction, corneal topography and fundus examination. Hard contact lenses and soft contact lenses were stopped 4 weeks and 2 weeks before topography, respectively.
UCVA and BCVA were recorded using Early Treatment Diabetic Retinopathy Study (ETDRS) chart and converted in logMAR for analysis purpose. Corneal topography was performed using Tomey TMS 5 (TOMEY GmbH, Nuremberg, Germany). Measurements were repeated at least 3 times, and the best image was chosen for the final analysis. The baseline and postoperative data included corneal astigmatism (CA), flattest meridian keratometry (Kf), steepest meridian keratometry (Ks) and mean keratometry (Km). Central corneal thickness (CCT) was measured at least 5 times (DGH 550 Pachette 2 Pachymeter, DGH Technology, Exton, PA, USA), and the lower value was chosen. The excimer laser used for PRK treatment was the WaveLight® ALLEGRETTO WAVE® Eye-Q (ALCON, Fort Worth, TX, USA).
Surgical technique
All patients underwent the following two-step procedure:
Step 1 (topography-guided PRK): after topical anaesthesia, the epithelium was gently removed within a 9-mm diameter using a hockey knife. Topography-guided PRK was performed with the aim to reduce irregular astigmatism and also part of the refractive error. The optical zone diameter was limited to 6 mm with a transition zone of 2 mm. Maximal ablation depth limit was 50 µm. In this context a correction up to 70% of the cylinder and up to 40% of the spherical component was attempted. After photoablation, 0.02% MMC was applied for 30 s, followed by copious irrigation with balanced salt solution.
Step 2 (standard CXL): riboflavin (0.1% in 20% dextran solution; Ricrolin, SOOFT, Italy) was administered topically every 2 min for 30 min and was continued every 2 min during UVA exposure. The cornea was exposed to UVA 370 nm light (UV-X System; Peschke Meditrade GmbH, Hünenberg, Switzerland) for 30 min with an irradiance of 3.0 mW/cm2.
After treatment, ofloxacin and dexamethasone phosphate 0.1% eye drops were administered, and therapeutic contact lens (etafilcon A contact lenses; ACUVUE, Jacksonville, FL, USA) were applied. Tobramycin drops 4 times a day for 1 week, dexamethasone phosphate 0.1% 4 times a day for 2 weeks and then tapered for other 2 weeks were prescribed. Orally Aminoacids (Aminoftal, SOOFT, Italy) were administered for 2 weeks. Topic hyaluronic acid drops 3 times a day were administered for 3 months. The contact lens was removed after 5 days when the re-epithelialization was completed.
Patients were assessed at 3, 6, 12 and 24 months after surgery. On each visit, the patients underwent UCVA and BCVA measurement. The presence of haze was evaluated using slit lamp according to the staging described by Fantes et al. 18 Corneal topography was performed at each visit.
Statistical analysis
Data were reported as mean values ± standard deviation (SD). The differences between data at baseline and at following time points were evaluated with paired t-test. A p-value < .05 was considered statistically significant.
Results
Fifteen eyes of 15 patients were included in the study: 8 males (53.34%) and 7 females (46.66%). The age of the patients ranged from 21 to 40 years, with a mean of 28.27 ± 9.21 years.
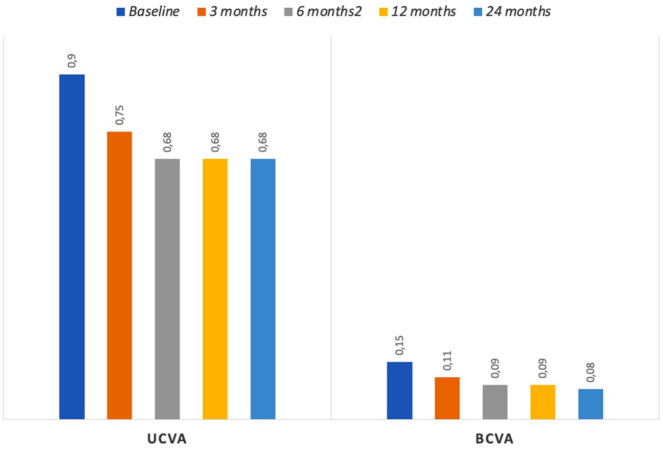
The cohort of patients showed an improvement of UCVA and BCVA during the follow-up that was statistically significant (Table 1 and Figure 1). In particular, there was a statistically significant difference between the mean preoperative (0.9 ± 0.19 logMAR) and 6-month postoperative UCVA (0.68 ± 0.26 logMAR) (p = 0.0001). Besides, UCVA improved progressively until the end of the 24-month follow- up period (0.68 ± 0.27 logMAR) (p = 0.0002). The baseline mean BCVA (0.15 ± 0.11 logMAR) showed a significant change to 0.09 ± 0.09 logMAR at 6 months (p = 0.0004), improving progressively until 0.08 ± 0.09 logMAR at 24 months (p < 0.0001) (Figure 2). In particular, 11 eyes gained one ETDRS line in BCVA and 4 patients gained two lines. No patient lost any ETDRS line over the 24-month-long follow-up.
Table 1.
Preoperative and postoperative data for: UCVA (uncorrected visual acuity) and BCVA (best corrected visual acuity) in logMAR; refractive outcomes in diopters (D) for mean sphere, mean cylinder and mean spherical equivalent (SE); topographic data in D for steepest keratometry (Ks), flattest keratometry (Kf), mean keratometry (Km) and corneal astigmatism (CA).
| Baseline | 3 months |
p value (versus baseline) |
6 months |
p value (versus baseline) |
12 months |
p value (versus baseline) |
24 months |
p value (versus baseline) |
|
|---|---|---|---|---|---|---|---|---|---|
| UCVA | 0.9 ± 0.19 | 0.75 ± 0.29 | 0.008 | 0.68 ± 0.26 | 0.0001 | 0.68 ± 0.27 | 0.0002 | 0.68 ± 0.27 | 0.0002 |
| BCVA | 0.15 ± 0.11 | 0.11 ± 0.12 | 0.0004 | 0.09 ± 0.09 | <0.0001 | 0.09 ± 0.09 | <0.0001 | 0.08 ± 0.09 | <0.0001 |
| Sphere | 3.65 ± 2.01 | 3.03 ± 1.93 | <0.0001 | 2.93 ± 1.93 | <0.0001 | 2.83 ± 1.89 | <0.0001 | 2.83 ± 1.89 | <0.0001 |
| Cylinder | 3.63 ± 1.67 | 2.1 ± 1.54 | <0.0001 | 1.97 ± 1.52 | <0.0001 | 1.93 ± 1.49 | <0.0001 | 2.04 ± 1.46 | <0.0001 |
| SE | 5.49 ± 2.26 | 4.07 ± 2.21 | <0.0001 | 3.9 ± 2.17 | <0.0001 | 3.8 ± 2.11 | <0.0001 | 3.8 ± 2.13 | <0.0001 |
| Ks | 48.79 ± 3.22 | 46.47 ± 3.17 | <0.0001 | 46.25 ± 3.16 | <0.0001 | 46.22 ± 3.16 | <0.0001 | 46.16 ± 3.11 | <0.0001 |
| Kf | 45.18 ± 2.17 | 44.46 ± 2.21 | <0.0001 | 44.40 ± 2.21 | <0.0001 | 44.37 ± 2.19 | <0.0001 | 44.35 ± 2.19 | <0.0001 |
| Km | 46.98 ± 2.62 | 45.42 ± 2.65 | <0.0001 | 45.32 ± 2.61 | <0.0001 | 45.3 ± 2.6 | <0.0001 | 45.26 ± 2.57 | <0.0001 |
| CA | 3.62 ± 1.71 | 2.1 ± 1.52 | <0.0001 | 1.98 ± 1.51 | <0.0001 | 1.94 ± 1.49 | <0.0001 | 1.90 ± 1.47 | <0.0001 |
Figure 1.
Preoperative and postoperative uncorrected distance visual acuity (UCVA) and best corrected distance visual acuity (BCVA) in logMAR.
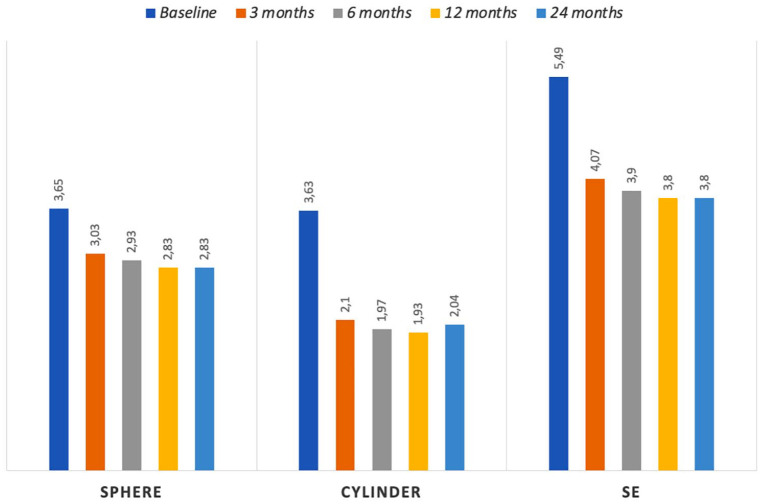
Figure 2.
Refractive outcomes in diopters (D) at baseline and during the follow-up period for mean sphere, mean cylinder and mean spherical equivalent (SE).
The baseline and postoperative refraction data are shown in Table 1 and Figure 2. The mean target spherical correction was 0.85 ± 0.8 D (range 0.5–1.25 D) and the mean cylindrical correction was 1.74 ± 0.93 D (range 0.5–2.25 D). The baseline sphere correction was 3.65 ± 2.01 D and significantly decreased to 2.93 ± 1.93 D (p < 0.0001) at 6 months. This still significantly improved at month 24 (2.83 ± 1.89 D, p < 0.0001). A statistically significant difference was also recorded in the measurements of mean cylinder. The mean baseline cylinder decreased from 3.63 ± 1.67 D to 1.97 ± 1.52 D at 6 months (p < 0.0001), and to 2.04 ± 1.46 D at 24 months (p < 0.0001). Our data also showed a statistically significant difference between the mean preoperative spherical equivalent (SE) (5.49 ± 2.26 D) and the 6-month postoperative value (3.9 ± 2.17 D, p < 0.0001). Moreover, SE improved until the end of the 24-month follow-up period to 3.8 ± 2.13 D (p < 0.0001).
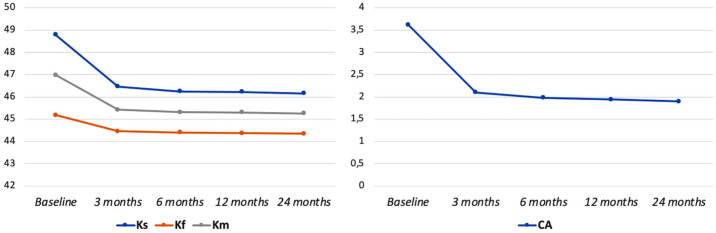
The topographic corneal outcomes measured during the follow-up are shown in Table 1 and Figure 3. In particular, we found that the average keratometry readings progressively improved until the final check at 24 months. All the patients showed a corneal flattening with statistically significant reduction of steepest (Ks) and flattest meridian keratometry (Kf). In fact, the mean Ks value reduce from 48.8 ± 3.22 D to 46.16 ± 3.11 D after 2 years of follow-up (p < 0.0001). In the same way, mean Kf decrease from 45.18 ± 2.17 D to 44.35 ± 2.18 D at 24 months (p < 0.0001). Consequently, the mean keratometry (Km) and the corneal astigmatism (CA) showed significant improvement over the follow-up.
Figure 3.
Topographic corneal outcomes in diopters (D) at baseline and during the postoperative follow-up for steepest keratometry (Ks), flattest keratometry (Kf), mean keratometry (Km) and corneal astigmatism (CA).
The mean ablation depth was 34.8 ± 10.07 µm (range = 24–40 µm). No serious complications were recorded during the follow-up period.
Discussion
The long-term effectiveness of topography-guided PRK followed by MMC 0.02% topical application and corneal CXL in the treatment of mild or moderate keratoconus has been analysed in this study. Kannellopoulos and Binder introduced subsequential CXL and topography-guided PRK 1 year apart to address the refractive aspect of keratoconus using PRK and to improve the corneal biomechanics using CXL. 2 In addition, other several following studies reported the simultaneous use of topography-guided PRK and CXL techniques showing good results for UCVA, BCVA, keratometry reduction and haze development.3,19 In particular, Iqbal et al. described the use of simultaneous PRK with accelerated CXL finding similar outcomes to standard CXL alone at 24 months. However, CXL alone was associated with a late myopic component reduction; instead, combined PRK–CXL showed early effect on both the myopic and the astigmatic components. 20
In this study, topography-guided excimer laser treatment was used in highly irregular corneas that are beyond the limits of wavefront measuring devices, making this approach more efficient in treating highly irregular astigmatism, such as in keratoconus, as its measurements are based solely on the cornea surface reflection. 10 A statistically significant improvement in visual acuity, refraction and average keratometry readings over a 2-year-long follow-up has been found, which is consistent with previous studies.21,22
While Sherif et al. 23 performed topography-guided PRK in post-CXL keratoconus eyes, our study evaluated the outcomes of combined PRK with CXL in mild or moderate keratoconus eyes. In accordance with our results, they documented statistically significant improvement in mean cylinder, visual acuity and keratometry at 6 months postoperative in keratoconus eyes undergoing topography-guided PRK. This validated the potential of the PRK to provide enhanced visual function. In addition, we found a stabilization or an improvement of all parameters after 2 years, in line with previous study by Kontadakis et al. 24 Our data showed a progressive improvement of BCVA and UCVA, means Ks, Km and Kf, SE and mean cylinder in the first year; then, the parameters remained stable over time, documenting the long-term efficacy and safety of the procedure. In fact, no patient suffered a worsening over time.
Our results showed a significant improvement of the mean UCVA over the first sixth month after the procedure. These results are comparable with Alessio et al.’s previous study. 14 The improvement continued during the follow-up time. Also, the observed BCVA gradual improvement was statistically significant over the 24 months period considered. In particular, 73.34% of eyes gained one line (Snellen chart lines) in BCVA and 26.66% gained two lines. These results are comparable with those reported in other previous studies.3,25,26 In addition, no loss of BCVA lines has been reported in accordance with other studies.13,27 Moreover, our patients had a reduction in mean Ks of 2.64 D, in mean Kf of 0.83 D and in mean Km of 1.72 D.
Our outcomes confirmed that simultaneous PRK with MMC and CXL may produce better outcomes than the corresponding sequential technique because of a minimization effect of potential superficial scarring associated with PRK and a wound-healing modulator effect of the MMC.
In particular, although MMC augments keratocyte apoptosis in the anterior corneal stroma, it has been described to inhibit mitosis of myofibroblast precursor cells in ablation procedures such as PRK. 28 These can lead to a reduction haze formation as previously documented by Kanellopoulos et al.2,3 However, a significant increase in corneal haze incidence has been reported by Awwad et al. 29 following MMC application in CXL procedure.
In our study, only two eyes presented a grade 1 haze at the third month check, which resolved with adequate local steroid therapy. All eyes had no haze at the end of the 24-month follow-up.19,26
The potential disadvantage of simultaneous procedures could be a hyperopic shift due to CXL-associated flattening of the cornea. This disadvantage can be overcome by customizing the treatment on an individualized basis. In fact, in our study, no patient showed a hyperopic shift.
Other previous studies positively evaluated the simultaneous topography-guided PRK and CXL in the treatment of keratoconus.3,13,19,23–26,30 In patients with early, progressive keratoconus with a clear central cornea, CXL can reduce the risk of progression.4–6 However, if the patient is contact-lens intolerant, CXL alone may not address the problem. For such cases, customized topography-guided PRK with adjunctive CXL can be considered.
Iqbal et al. retrospectively studied the effectiveness and safety of combined PRK with CXL (“CXL plus”) in 79 keratoconus eyes. They concluded that “CXL plus” technique improved the refractive status in keratoconus patients during the 18-month follow-up. However, they described early postoperative complications such as delayed epithelial healing and corneal haze. 31
This study demonstrated that this therapeutic approach is effective and safe with 24-month refractive stability. The results of simultaneous customized topography-guided PRK with MMC and CXL in mild or moderate keratoconus eyes are promising and provide surgeons with another tool in the armamentarium to improve vision with a high degree of refractive predictability.
The limits of this research are the small number of treated eyes and the 24-month follow-up period. Further studies with a larger number of participants and a longer follow-up are necessary to confirm the positive results of this technique.
Footnotes
Author contributions: Giuseppe De Rosa: Conceptualization; Data curation; Formal analysis; Methodology; Resources; Supervision; Validation; Writing – original draft; Writing – review & editing.
Settimio Rossi: Conceptualization; Data curation; Formal analysis; Methodology; Resources; Supervision; Validation; Writing – original draft; Writing – review & editing.
Carmine Santamaria: Conceptualization; Data curation; Formal analysis; Methodology; Resources; Supervision; Validation; Writing – original draft; Writing – review & editing.
Rosa Boccia: Conceptualization; Data curation; Formal analysis; Methodology; Resources; Supervision; Validation; Writing – original draft; Writing – review & editing.
Luigi De Rosa: Conceptualization; Data curation; Formal analysis; Methodology; Resources; Supervision; Validation; Writing – original draft; Writing – review & editing.
Francesco Maria D’Alterio: Conceptualization; Data curation; Formal analysis; Methodology; Resources; Supervision; Validation; Writing – original draft; Writing – review & editing.
Francesca Simonelli: Conceptualization; Data curation; Formal analysis; Methodology; Resources; Supervision; Validation; Writing – original draft; Writing – review & editing.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethicals statement: The study was conducted within the tenets of the Declaration of Helsinki. The study was evaluated by the Local Institutional Review Board at Comitato di Ricerca Dipartimentale - Napoli which concluded that the study did not require ethics approval given its retrospective nature.
ORCID iD: Francesco Maria D’Alterio  https://orcid.org/0000-0003-4248-4376
https://orcid.org/0000-0003-4248-4376
Contributor Information
Giuseppe De Rosa, Eye Clinic, Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania ‘Luigi Vanvitelli’, Naples, Italy.
Settimio Rossi, Eye Clinic, Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania ‘Luigi Vanvitelli’, Naples, Italy.
Carmine Santamaria, Eye Clinic, Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania ‘Luigi Vanvitelli’, Naples, Italy.
Rosa Boccia, Eye Clinic, Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania ‘Luigi Vanvitelli’, Naples, Italy.
Luigi De Rosa, Eye Clinic, Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania ‘Luigi Vanvitelli’, Naples, Italy.
Francesco Maria D’Alterio, Eye Clinic, Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania ‘Luigi Vanvitelli’, Via Sergio Pansini 5, 80131 Naples, Italy.
Francesca Simonelli, Eye Clinic, Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania ‘Luigi Vanvitelli’, Naples, Italy.
References
- 1. Mas Tur V, MacGregor C, Jayaswal R, et al. A review of keratoconus: diagnosis, pathophysiology, and genetics. Surv Ophthalmol 2017; 62: 770–783. [DOI] [PubMed] [Google Scholar]
- 2. Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea 2007; 26: 891–895. [DOI] [PubMed] [Google Scholar]
- 3. Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg 2009; 25: S812–S818. [DOI] [PubMed] [Google Scholar]
- 4. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A- induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 2003; 135: 620–627. [DOI] [PubMed] [Google Scholar]
- 5. Woo JH, Iyer JV, Lim L, et al. Conventional versus accelerated collagen cross-linking for keratoconus: a comparison of visual, refractive, topographic and biomechanical outcomes. Open Ophthalmol J 2017; 11: 262–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rossi S, Santamaria C, Boccia R, et al. Standard, transepithelial and iontophoresis corneal cross-linking: clinical analysis of three surgical techniques. Int Ophthalmol 2018; 38: 2585–2592. [DOI] [PubMed] [Google Scholar]
- 7. Alio JL, Belda JI, Osman AA, et al. Topography-guided laser in situ keratomileusis (TOPOLINK) to correct irregular astigmatism after previous refractive surgery. J Refract Surg 2003; 19: 516–527. [DOI] [PubMed] [Google Scholar]
- 8. De Rosa G, Boccia R, Santamaria C, et al. Customized photorefractive keratectomy to correct high ametropia after penetrating keratoplasty: a pilot study. J Optom 2015; 8: 174–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shetty R, D’Souza S, Srivastava S, et al. Topography-guided custom ablation treatment for treatment of keratoconus. Indian J Ophthalmol 2013; 61: 445–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lin DTC, Holland S, Tan JCH, et al. Clinical results of topography-based customized ablations in highly aberrated eyes and keratoconus/ectasia with cross-linking. J Refract Surg 2012; 28(Suppl. 11): S841–S848. [DOI] [PubMed] [Google Scholar]
- 11. Chan CCK, Sharma M, Wachler BSB. Effect of inferior-segment Intacs with and without C3-R on keratoconus. J Cataract Refract Surg 2007; 33: 75–80. [DOI] [PubMed] [Google Scholar]
- 12. Izquierdo L, Jr, Henriquez MA, McCarthy M. Artiflex phakic intraocular lens implantation after corneal collagen cross-linking in keratoconic eyes. J Refract Surg 2011; 27: 482–487. [DOI] [PubMed] [Google Scholar]
- 13. Alessio G, L’abbate M, Sborgia C, et al. Photorefractive keratectomy followed by cross-linking versus cross-linking alone for management of progressive keratoconus: two-year follow-up. Am J Ophthalmol 2013; 155: 54–65. [DOI] [PubMed] [Google Scholar]
- 14. Majmudar PA, Forstot SL, Dennis RF, et al. Topical mitomycin-C for subepithelial fibrosis after refractive corneal surgery. Ophthalmology 2000; 107: 89–94. [DOI] [PubMed] [Google Scholar]
- 15. Hashemi H, Salimi Y, Pir P, et al. Photorefractive keratectomy with mitomycin-C for high myopia: three year follow-up results. Acta Med Iran 2017; 55: 42–48. [PubMed] [Google Scholar]
- 16. Kanellopoulos AJ. Management of progressive keratoconus with partial topography-guided PRK combined with refractive, customized CXL – a novel technique: the enhanced Athens protocol. Clin Ophthalmol 2019; 13: 581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Santhiago MR, Netto MV, Wilson SE. Mitomycin C: biological effects and use in refractive surgery. Cornea 2012; 31: 311–321. [DOI] [PubMed] [Google Scholar]
- 18. Fantes FE, Hanna KD, Waring GO, 3rd, et al. Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol 1990; 108: 665–675. [DOI] [PubMed] [Google Scholar]
- 19. Kymionis GD, Kontadakis GA, Kounis GA, et al. Simultaneous topography-guided PRK followed by corneal collagen cross-linking for keratoconus. J Refract Surg 2009; 25: S807–S811. [DOI] [PubMed] [Google Scholar]
- 20. Iqbal M, Elmassry A, Tawfik A, et al. Standard cross-linking versus photorefractive keratectomy combined with accelerated cross-linking for keratoconus management: a comparative study. Acta Ophthalmol 2019; 97: e623–e631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tamayo GE, Castell C, Vargas P, et al. High-resolution wavefront-guided surface ablation with corneal cross-linking in ectatic corneas: a pilot study. Clin Ophthalmol 2017; 11: 1777–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhu W, Han Y, Cui C, et al. Corneal collagen crosslinking combined with phototherapeutic keratectomy and photorefractive keratectomy for corneal ectasia after laser in situ keratomileusis. Ophthalmic Res 2018; 59: 135–141. [DOI] [PubMed] [Google Scholar]
- 23. Sherif AM, Ammar MA, Mostafa YS, et al. One-year results of simultaneous topography-guided photorefractive keratectomy and corneal collagen cross-linking in keratoconus utilizing a modern ablation software. J Ophthalmol 2015; 2015: 321953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kontadakis GA, Kankariya VP, Tsoulnaras K, et al. Long-term comparison of simultaneous topography-guided photorefractive keratectomy followed by corneal cross-linking versus corneal cross-linking alone. Ophthalmology 2016; 123: 974–983. [DOI] [PubMed] [Google Scholar]
- 25. Stojanovic A, Zhang J, Chen X, et al. Topography-guided transepithelial surface ablation followed by corneal collagen cross-linking performed in a single combined procedure for the treatment of keratoconus and pellucid marginal degeneration. J Refract Surg 2010; 26: 145–152. [DOI] [PubMed] [Google Scholar]
- 26. Kymionis GD, Portaliou DM, Kounis GA, et al. A. Simultaneous topography-guided photorefractive keratectomy followed by corneal collagen cross-linking for keratoconus. Am J Ophthalmol 2011; 152: 748–755. [DOI] [PubMed] [Google Scholar]
- 27. Mukherjee AN, Selimis V, Aslanides I. Transepithelial photorefractive keratectomy with crosslinking for keratoconus. Open Ophthalmol J 2013; 7: 63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carlos de Oliveira R, Wilson SE. Biological effects of mitomycin C on late corneal haze stromal fibrosis following PRK. Exp Eye Res 2020; 200: 108218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Awwad ST, Chacra LM, Helwe C, et al. Mitomycin C application after corneal cross-linking for keratoconus increases stromal haze. J Refract Surg 2021; 37: 83–90. [DOI] [PubMed] [Google Scholar]
- 30. Sakla H, Altroudi W, Munoz G, et al. Simultaneous topography-guided partial photorefractive keratectomy and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg 2014; 40: 1430–1438. [DOI] [PubMed] [Google Scholar]
- 31. Iqbal M, Elmassry A, Tawfik A, et al. Evaluation of the effectiveness of cross-linking combined with photorefractive keratectomy for treatment of keratoconus. Cornea 2018; 37: 1143–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]