Abstract
The retinal world has been revolutionized by optical coherence tomography (OCT) and anti-vascular endothelial growth factor (VEGF) therapy. The numbers of intravitreal injections are on a constant rise and management in neovascular age-related macular degeneration (nAMD) is mainly driven by the qualitative assessment of macular fluid as detected on OCT scans. The presence of macular fluid, particularly subretinal fluid (SRF) and intraretinal fluid (IRF), has been used to trigger re-treatments in clinical trials and the real world. However, large discrepancies can be found between the evaluations of different readers or experts and especially small amounts of macular fluid might be missed during this process. Pixel-wise detection of macular fluid uses an entire OCT volume to calculate exact volumes of retinal fluid. While manual annotations of such pixel-wise fluid detection are unfeasible in a clinical setting, artificial intelligence (AI) is able to overcome this hurdle by providing real-time results of macular fluid in different retinal compartments. Quantitative fluid assessments have been used for various post hoc analyses of randomized controlled trials, providing novel insights into anti-VEGF treatment regimens. Nonetheless, the application of AI-algorithms in a prospective patient care setting is still limited. In this review, we discuss the use of quantitative fluid assessment in nAMD during anti-VEGF therapy and provide an outlook to novel forms of patient care with the support of AI quantifications.
Keywords: age-related macular degeneration, artificial intelligence, deep learning, intraretinal fluid, macular neovascularization, subretinal fluid
Introduction
Age-related macular degeneration (AMD) is the leading cause of blindness in Western countries in people over the age of 60 years. 1 In neovascular AMD (nAMD), macular neovascularization (MNV) causes specific patterns of fluid exudation. 2 This process of exudation leads to the pathological accumulation of fluid in different compartments of the retina, which can be separated into intraretinal fluid (IRF) inside the retina, subretinal fluid (SRF) beneath the neurosensory retina, and pigment epithelium detachment (PED) between the retinal pigment epithelium (RPE) and Bruch’s membrane (BM). 3 Optical coherence tomography (OCT) has been established as the primary imaging technique for the identification of pathological fluid. 4 It has been further established as the most important monitoring tool in retinal outpatient clinics. 4 The full potential of OCT imaging comes with its three-dimensional visualization of the retina and pathological processes. This potential supported the initial use of anti-vascular endothelial growth factor (VEGF) as the main agent to suppress excessive VEGF expression and related neovascularization. 5 Since then, anti-VEGF and OCT use has tremendously increased but has resulted in a relentless budget drain for health systems with new strategies and treatment regimens appearing to overcome the hurdle of real-world undertreatment or excessive over-monitoring. 6 The use of OCT significantly increased the effectiveness of patient care; however, correct decisions rely on correct interpretations of the entire OCT volume and considerable discrepancies can be found between professional reading centers and treating physicians. 7 The implementation of quantitative markers might render this conventional qualitative grading outdated.
Correct annotation of each pixel of the entire OCT volume requires an enormous amount of time and is practically unfeasible for real-time examinations. 8 Artificial intelligence (AI) was accepted as a tool to perform tasks originally accomplished by human experts. 9 The fast progress in AI-algorithm architectures, advances in computational power combined with the availability of data sets to train an AI-algorithm, has led to the rapid advances in this interdisciplinary field.9–11 This review aims to display recent efforts to establish quantitative markers in nAMD to improve the guidance of anti-VEGF therapy in clinical routine.
Optical coherence tomography and anti-VEGF treatment regimens
Introducing time-domain OCT imaging into clinical routine was a major milestone in ophthalmology. 12 The technical advances in OCT imaging were additionally reinforced by the introduction of anti-VEGF for the treatment of nAMD. 13 For the first time, exudation in nAMD could be seen in a three-dimensional manner and a treatment effect after anti-VEGF administration could be assessed on the OCT images. 4 The amount of excessive VEGF in nAMD was then related to the accumulation of macular fluid and OCT was branded to visualize VEGF over-expression as a ‘VEGF-meter’. 5 Technical advances from time-domain to Fourier-domain OCT technologies, including spectral-domain and swept-source technologies, greatly influenced the treatment strategies in the management of nAMD. 3 Due to these advances, scanning speed (A-Scan rate) has dramatically improved. This lead to the most commonly used OCT raster scanning the macula with increasing number of B-Scans, instead of six radial B-Scans from time-domain OCT ages that were difficult to interpolate to estimate the morphology between the radial scans. 4
After the realization of the advantage of intravitreal over intravenous application of anti-VEGF for retinal conditions, dosing and intervals for the continuous treatment had to be established. Fixed monthly treatments were associated with a high recovery in visual acuity. Soon afterwards, fixed bimonthly, or treatment as needed, pro re nata (PRN), were investigated and revealed similar success compared with monthly treatments.14,15 Individualized treatment was since then preferred although minor subclinical benefits were lost when allowing macular fluid to re-occur before treatment. 16 A PRN regimen still needed monthly appointments which resulted in a tremendous effort for health care systems. The treat-and-extend (T&E) regimen proactively counters the disadvantages of the PRN regimen: (1) Recurrence of macular fluid is not tolerated and (2) personalized intervals are possible even without monthly visits.17,18 This new regimen was quickly accepted as the preferred treatment regimen and visual acuity outcomes were comparable with others. 18
Each regimen has a unique presentation of macular fluid: Monthly fixed treatment has a minimum of residual fluid, whereas fixed bimonthly or fixed treatment at 12-week intervals allow more macular fluid to re-occur. The PRN regimen always requires macular fluid to re-occur to trigger re-treatment and results in the lowest number of injections for the patient. T&E, on the other hand, proactively clears the retina from pathological fluid; even if no fluid is present, re-treatment will be given. This ultimately results in more frequent injections while still keeping the personalized approach. Since the injection – and therefore also the control visit – are performed at different fluid accumulation stages, fluid measurements during therapy significantly differ between the regimens.
Qualitative fluid assessment
In clinical routine, macular fluid is often assessed by qualitative evaluation of the entire, or only a fraction of the, OCT volume. 19 IRF, SRF, and PED are then graded as either present or absent. Re-treatment is mainly triggered if either IRF or SRF is present. 3 More tolerant regimens, allowing SRF to a certain degree were proposed,20,21 with similar outcomes compared with more intolerant ones. 22 The main benefit in qualitative fluid assessment is the fast interpretation of the data. The drawbacks, on the other hand, are critical disagreements between investigators and inconclusive follow-up examinations. In the Comparison of Age-Related Macular Degeneration Treatments Trials (CATT), over 25% of the re-treatment decision disagreed with the reading center gradings. 7 Discrepancies were more frequent in cases with only IRF or small volumes of macular fluid where fluid was missed by the physicians. 7 Discrepancies in the detection of IRF between the investigators and the reading center was also seen in the FLUID study and confirmed in an independent cohort.22,23 These findings support the implementation of quantitative markers and even more preferred, an automated identification and standardized quantification of macular fluid using the entire OCT volume.
Fluid quantifications
Manual delineation of macular fluid
The precise assessment of every fluid pixel in an entire OCT volume is a time-consuming task. It might take up to 15 h for a single OCT volume, if performed manually. 8 It is therefore understandable that manual quantitative investigations are limited in sample size. In an early quantitative assessment of 14 eyes undergoing Ranibizumab treatment, a significant reduction in SRF, PED, and retinal volumes were noticeable 1 week after the initial injection. 24 One month after the initial injection, SRF further decreased and remained on a low lever after the second and third injections of a monthly loading dose comprising three injections. 24
In an ancillary study to the EXCITE trial, 25 27 eyes were manually graded and macular fluid quantified. After the first injections, the majority of IRF was cleared from the retina. In the monthly treatment cohort, IRF remained on a low level, whereas IRF in the quarterly treatment group showed considerable fluctuations. 26 A similar trend for residual SRF was seen in the monthly treatment cohort, whereas the quarterly treatment cohort showed great SRF fluctuations and more frequent re-occurring of SRF volumes. Sub-RPE fluid never completely resolved, but remained on lower levels in the more frequent treatment arm. 26 Keane et al. presented a study comprising 122 eyes that were graded for the neurosensory retina volume, SRF, PED, and subretinal tissue volume. 27 Compared with photodynamic therapy (PDT) using verteporfin, anti-VEGF greatly reduced the neurosensory retina volume. SRF reduction, on the other hand, was greater in the PDT treatment arm, but also decreased under anti-VEGF therapy. 27
Manual annotations in larger data sets are hard to acquire in a reasonable amount of time. Interreader agreement is good for SRF; however, IRF might be missed, especially in scans without abundant central IRF. 23 The main limitation for manual readings, however, is the constriction to smaller data sets due to the enormous time consumption when performing precise annotation. To guarantee precise and repeatable measurements in a feasible amount of time, automatic segmentation of macular fluid has to be implemented. The continuous progress of AI-algorithms is an optimal accompaniment for the demands of fluid quantifications.
Automated segmentation using artificial intelligence
Various AI-based algorithms have been presented to achieve a common goal: to measure macular fluid in a precise manner that is comparable with human error rates. 28 Automated algorithms can also be implemented by using graph-based methods, 29 which were built for retinal layer segmentations for their early OCT applications.30,31 Whereas humans show high sensitivity in detecting macular fluid, automated algorithms achieve higher specificity. 32 Quantification of fluid adds another dimension to detection in requiring the identification of fluid for each voxel in an entire OCT volume and rendering the individual voxels to total fluid compartments. Using AI-algorithms, real-time identification and measurement became available (Figures 1 and 2). 28 This led to re-assessments of well-conducted randomized controlled trials to (1) re-investigate and confirm the original results using fluid quantifications and (2) investigate fluid as a clinical parameter of disease activity in more detail.
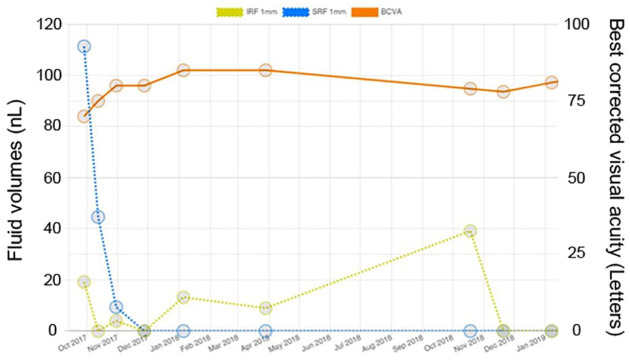
Figure 1.
Example of real-time quantification of macular fluid volumes (SRF = blue; IRF = yellow) for a patient with neovascular age-related macular degeneration following a treat-and-extend regimen using the Vienna Fluid Monitor. 33 The green lines mark the border of the central millimeter. (a) Baseline; (b) Month 1; (c) Month 2; (d) after the loading dose of 3 consecutive injections, the patient presents with a dry macula; (e and f) IRF remained on low level with some residual IRF; (g) after a missed visit, IRF volumes greatly increased; (h and i) after interval reduction, the macular remained without fluid. The quantitative measurements are shown in Figure 2.
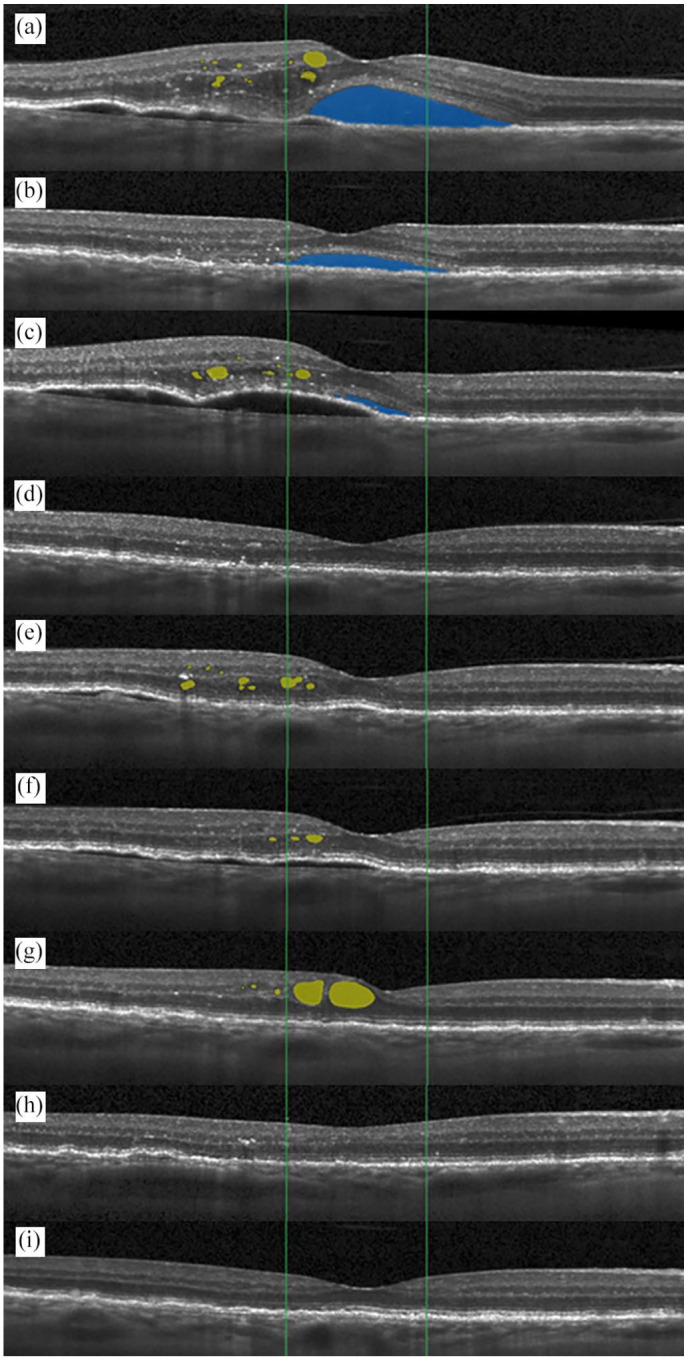
Figure 2.
Course of SRF (blue), IRF (yellow) within the central millimeter and best-corrected visual acuity (orange) of the patient presented in Figure 1 using the Vienna Fluid Monitor. 33 The patient was managed using a treat-and-extend regimen and anti-VEGF was administered at each visit. The increase of IRF after the sixth visit was caused by a missed visit and was accompanied by a decline of visual acuity. After full resolution of macular fluid, visual acuity was partly regained.
Fluid in nAMD follows specific topographic distributions. Whereas IRF and PED are usually located throughout the fovea, IRF is much more concentrated to the foveal center point. SRF, on the other hand, is more evenly distributed across the macular region with a high dominance in the parafoveal inferior section. 34 This gravitational effect is also seen in other diseases that present with SRF.35,36 An investigation of macular fluid in nAMD, diabetic macular edema (DME), and retinal vein occlusion (RVO) using data from large clinical trials identified nAMD to exhibit much less IRF compared with DME and RVO. 37 In contrast, SRF was present in large amounts in nAMD; however, its topographic location was mainly outside the foveal center and extended throughout the entire macular region. Response to anti-VEGF therapy in nAMD revealed a rapid decline in both SRF and IRF with 90% to 98% regression in each fluid compartment, respectively, after the first injection. 37 Over the first year of treatment, over 99% of SRF was cleared from the macula, whereas IRF declined approximately 93% compared with the baseline value. 37 Resistant fluid might be the result of two processes: (1) Re-emerging of fluid in non-proactive treatments (e.g. PRN) or due to missed or postponed visits in a proactive treatment, or (2) residual and/or resistant fluid which cannot be cleared from the retina. The higher amount of resistant fluid in the intraretinal compartment might be an indicator of degenerative processes leading to cystoid appearances on the OCT (Figure 3). The development of outer retinal tubulations (ORT) might also be mistaken for exudative fluid (Figure 4).38,39 Since their appearance is typically well distinguishable from IRF, the differentiation of ORT and IRF should be implemented in the training data of any algorithm. ORT annotated as false positive IRF might however influence the specificity of an algorithm and the amount of resistant fluid might be higher compared with expert gradings. This fact may also be true for degenerative cystoid spaces that do not respond anti-VEGF therapy.
Figure 3.
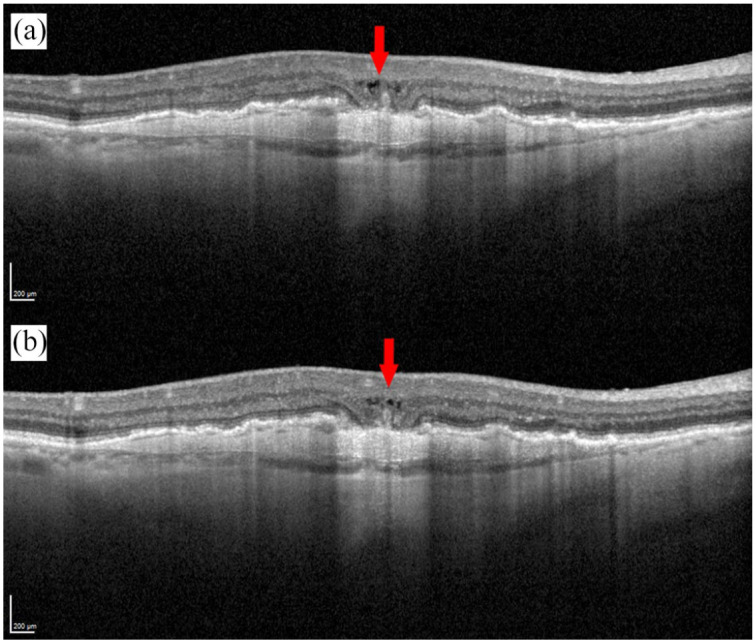
Degenerative cystoid fluid (red arrow) mimicking resistant intraretinal fluid (IRF) before (a) and after (b) anti-VEGF treatment.
Figure 4.
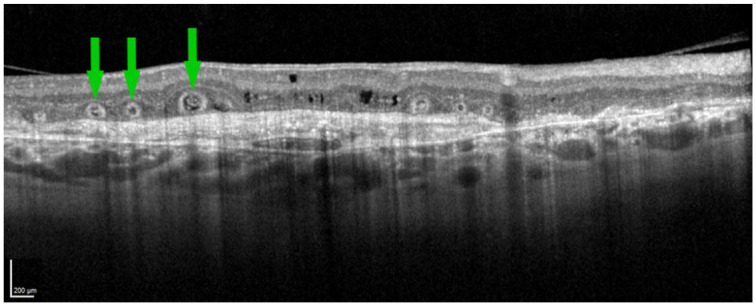
Outer retinal tubulations (ORT – exemplary ORTs: green arrows) imitating intraretinal fluid (IRF). A qualified reader is needed to distinguish ORT from IRF based on the characteristic appearance of ORT.
The first injection particularly clears the retina from exudative fluid in both subretinal and intraretinal compartments. PED volume does not respond to therapy the same as SRF or IRF. In the HARBOR study, SRF and IRF volumes were thoroughly resolved with a greater effect in the monthly dosing arm. PED, on the other hand, responds more reluctantly to anti-VEGF therapy and may never completely resolve, even under an intensive monthly treatment regimen. 40 In comparison to a monthly treatment regimen with very little amounts of fluid, a PRN regimen overall shows higher amounts of fluid.
In contrast, the FLUID study used a proactive T&E regimen. 20 However, in the experimental arm SRF was tolerated to a certain degree (200 µm height of SRF in the foveal center). No significant difference in best-corrected visual acuity (BCVA) between the treatment arms was found after the 24-month follow-up period. 22 In a post hoc AI-supported quantification of the FLUID study, our group could not find a significant difference in SRF or IRF volumes between the two treatment arms. 41 Furthermore, we also did not find a significant difference in the proportions of eyes with SRF or IRF, similar to the clinical investigators of the FLUID study.22,41 Interestingly, when originally assessed by the central reading center the proportion of eyes with IRF differed between the treatment arms. 22 This difference between reading center and investigator assessment highlights the importance of precise and objective quantifications of retinal biomarkers. In another post hoc analysis from the FLUID study, our group investigated eyes with residual SRF and visits in which the T&E interval was extended, although SRF was still present. 42 We were able to show a further increase in SRF volumes without the recurrence of IRF. In these visits with residual SRF and interval extension, BCVA significantly declined to the following visit. 42 This was, however, only measured as a short-term outcome. It has previously been shown that BCVA recovers with the resolution of SRF. 40 Therefore, this short-term effect of increasing SRF might be reversible in the longer term.
The amount of fluid significantly differs between first- and second-treated eyes. In a small real-world investigation, second-treated eyes had considerably less retinal fluid volume compared with first-treated eyes. 43 In another large-scale investigation, this was confirmed with larger volumes of most retinal compartments resulting in a more distinct impact on visual function. 44 Since patients are regularly followed for the first eye, it is of no surprise that second-treated eyes are diagnosed in an earlier stage of exudative processes and are treated at an earlier stage when the patient might still be asymptomatic.45,46 Subsequently, the visual gain is less pronounced in second-treated eyes with unchanging visual function over 3 years. 46 For 5-year visual acuity results, second-treated eyes have been described to have a worse outcome than first-treated eyes, receive less injections, and might therefore be prone to undertreatment. 47
However, final visual outcomes might not simply depend on the amount of retinal fluid at baseline. Fluctuations in retinal fluid volumes have been associated with worse visual outcomes. 48 Especially in the quartile with highest fluctuations of either SRF, IRF, or PED, each fluid compartment fluctuation was respectively associated with worse visual outcomes. For total fluid, a stepwise worsening was seen for increasing fluid fluctuations. 48 Similar findings were found when assessing central retinal thickness (CRT) in nAMD. 49 CRT has been widely used in studies investigating anti-VEGF in nAMD. However, due to the topographic distribution of retinal fluid and the abundance of SRF in nAMD, CRT might not be the most informative biomarker.19,28
Alternative indicators of macular fluid
Besides, SRF, IRF, and PED other retinal quantifications were previously used. In times of time-domain OCT devices, IRF was less distinguishable throughout the OCT volume. Therefore, the volume of the neurosensory retina was introduced as a separate fluid compartment and acted as a surrogate for the swelling of the retina during intraretinal exudation. 50 At the same time, SRF and PED were already introduced as their own fluid compartments. Further investigations on the neurosensory retinal volume revealed decreasing volumes under anti-VEGF therapy with a more pronounced effect of bevacizumab compared with photodynamic therapy or pegaptanib. 27 Similar results were found for SRF when comparing bevacizumab with photodynamic therapy or pegaptanib. 27 After switching from a suboptimal response to bevacizumab or ranibizumab to aflibercept a significant decrease in neurosensory retina volume was found with similar results for SRF and PED together with a significant increase in BCVA. 51
A simple way to estimate the amount of exudation in the retina is the measurement of central retinal thickness (CRT). 52 CRT became the most frequent way to measure structural outcomes in clinical studies and was available using the radial scans from time-domain OCT imaging. 28 Measurement of CRT can be extracted manually, but is often derived from automated layer segmentation using the internal limiting membrane as the inner border. There are some controversies, which OCT layer to use as the outer border: either Bruch’s membrane to include PED in the CRT measurement, or the RPE outer border to exclude PED.3,28 Due to the topographic distribution of macular fluid in nAMD, 34 CRT is mainly impacted by IRF but, depending on the definition of CRT, also by PED. The main exudative volume of pathological fluid in nAMD, however, is SRF and PED. 40 Nonetheless, CRT has been used as the main morphological treatment parameter in various studies.53,54 CRT might therefore not be the most informative parameter to measure disease activity. Fluid volumes, on the other hand, can now be assessed and correlated to the excessive amount of VEGF.5,13 In clinical evaluation, CRT does not correlate well with visual acuity.55,56 Fluid quantification might therefore be preferable when deciding on disease activity and re-treatments in nAMD.
More than fluid? OCT markers important for macular function
Clinical markers might be quickly assessed by a retinal expert. An overview of the presence of SRF, IRF, or PED can be quickly performed, whereas manual quantification is unfeasible in clinical routine.8,57 However, patient satisfaction and functional outcomes are not only based on the presence of fluid. The amount of fluid in the central millimeter is highly correlated with visual function,28,40 but subclinical markers might be as important as exudative fluid. Subretinal hyperreflective material (SHRM) can be quantified using high-resolution OCT imaging. 58 During anti-VEGF therapy, SHRM volume decreases and change of visual acuity is associated with the decrease of SHRM volumes.59,60 On the other hand, fibrosis as a result of retinal remodeling processes might not respond to anti-VEGF therapy.58,61 Fibrosis is furthermore associated with worse visual outcomes and overlaying photoreceptor degeneration. Fibrosis might therefore be as important as the development of macular atrophy as disease progresses, with photoreceptor degeneration as the common cause for vision loss. 62 It is therefore of great necessity to distinguish between SHRM and fibrosis, and combining both markers might be inadequate while sufficient OCT image resolution is present.27,50,63 Higher axial resolution of novel OCT devices might also allow the quantification of photoreceptor integrity directly.4,64 During anti-VEGF therapy, a morphological recovery of the foveal ellipsoid zone can be identified. Furthermore, ellipsoid zone integrity is associated with visual acuity. 64 Similar to pathological fluid quantifications, manual segmentation of photoreceptor layers is not feasible in a clinical setting. AI-algorithms for either the quantification of photoreceptor loss or preferably subclinical photoreceptor thinning might become important tools for the evaluation of treatment effects in various macular diseases.62,65,66
Discussion
Progress in computational power and imaging techniques comes with an overwhelming amount of information. A retinal expert or a general ophthalmologist, trained to evaluate disease-specific markers biomicroscopically, might be flooded with additional information provided by the new systems. Especially in times of rising numbers of intravitreal injections, 67 or during the COVID-19 pandemic, 68 a retinal outpatient clinic must strive for the best of care for the individual patient. Telemedicine and real-time evaluation of patients have therefore become even more important.69,70 The application of AI in retinal clinics has shown promising results in research and post hoc assessments of randomized controlled trials. 40 Solid evidence for the benefits an implementation of AI in the prospective management of patients in ophthalmology can bring, however, is still missing. This is because there is currently no Food and Drug Administration (FDA)-approved AI-algorithm available for fluid quantifications on OCT scans. Clinical trials are ongoing to evaluate the use of AI-supported fluid quantification in an outpatient clinic setting (NCT04662944, NCT05093374), but results are not yet available.
Reading centers might be useful for centralized assessments of OCT scans. However, strong discrepancies can be found when the same OCT volume is assessed by different qualified readers or retinal experts.7,22 These discrepancies exist for detecting the presence of fluid or a specific compartment of fluid. The discrepancies between readers and experts might be tremendously higher when total macular fluid is assessed and expert opinion might differ when annotating total volume scans. 57 Especially, IRF when present in only small amounts might be missed by the human investigator. 7 Nonetheless, IRF is associated with worse visual outcomes, whereas the decision to treat SRF in the long term is still not fully solved. There might be no exact conclusion, when macular fluid is only evaluated in a vague manner. It is therefore imperative to find a precise biomarker-focused approach when evaluating macular fluid during therapy. Artificial intelligence was established as a method to quantify macular fluid and support expert decisions by providing a repeatable output. 28 Although error rates are still present when using an AI-algorithm, they have been shown to be comparable with human decisions.71,72 This is understandable, as the AI will provide an output based on the training data and the labels given by a human grader. 9 When AI diagnoses were compared with those of retinal specialists and optometrists on OCT images alone, the AI outperformed half of the experts and all of the optometrists. Only with additional information, not available to the AI, were the experts and some of the optometrists able to perform on the same level. 71 The advantage of AI lies therefore in the time saved to perform such a task with the same efficiency and preciseness over multiple times. Furthermore, AI-algorithms might become able to annotate multiple biomarkers at the same time to put them together to perform an individual-based prediction of disease onset and progression.73,74 These superhuman tasks are already unachievable and new treatment regimens were developed to decrease the burden on clinicians.6,18,75
Intravitreal administration of anti-VEGF has been constantly rising. 67 Novel therapies for treating non-neovascular AMD might be approved in the following years,76–78 which would tremendously increase the number of treatments given by the clinical staff. Retinal experts need to efficiently plan their routine and support might be provided by automated quantification of OCT biomarkers. The first hurdles were already overcome by implementing AI-based quantification in a research setting and getting approval by the FDA for screening tools for diabetic retinopathy. 79 Further steps on this path will follow and ophthalmologists need to be mindful of them to provide adequate care for the growing amount of patients with retinal conditions. As OCT devices are capable of segmenting retinal layers and some are able to provide maps of drusen or different features, 80 future software updates might include the quantification of retinal fluid for neovascular AMD, diabetic macular edema, or retinal vein occlusion. Further research is needed to evaluate such algorithms in a prospective manner for real-world patient care.
Conclusion
Quantitative assessment of macular fluid in nAMD provided novel knowledge on the impact of fluid on visual outcomes. Artificial intelligence is well matched to overcome the hurdle of time-consuming annotations for the use of quantitative fluid measurements in the real world. Further research has to take other biomarkers into account, which also limit the visual outcome of patients. The algorithms’ capability to quantify macular fluid allows the physician to investigate the development of macular fibrosis and/or macular atrophy and might give the ophthalmologist a unique opportunity to improve patient care on an individual level. Prospective studies are needed to evaluate AI-algorithms in the real word. Continuous innovation will drive the field of ophthalmology, novel treatments might be approved for currently not-treatable diseases, and support is urgently needed to provide excellent and objective treatment to our patients in the years to come.
Acknowledgments
The authors thank Maximilian Lindell (Vienna Clinical Trial Center, Department of Ophthalmology and Optometry, Medical University of Vienna) for his assistance in medical writing assistance in the form of English editing.
Footnotes
Author contributions: Gregor S. Reiter: Conceptualization; Visualization; Writing – original draft; Writing – review & editing.
Ursula Schmidt-Erfurth: Funding acquisition; Methodology; Project administration; Resources; Writing – review & editing.
Conflict of interest statement: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: GSR: Research Funding: RetInSight; US-E: Research Funding: Genentech, Apellis, Kodiak; Consultancy: Heidelberg Engineering Novartis, Roche, RetInSight.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Gregor S. Reiter  https://orcid.org/0000-0001-7661-4015
https://orcid.org/0000-0001-7661-4015
Contributor Information
Gregor S. Reiter, Christian Doppler Laboratory for Ophthalmic Image Analysis, Department of Ophthalmology and Optometry, Medical University of Vienna, Währinger Gürtel 18-20, 1090 Vienna, Austria.
Ursula Schmidt-Erfurth, Christian Doppler Laboratory for Ophthalmic Image Analysis, Department of Ophthalmology and Optometry, Medical University of Vienna, Vienna, Austria.
References
- 1. Klein R, Klein BEK, Linton KLP. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 933–943. [DOI] [PubMed] [Google Scholar]
- 2. Spaide RF, Jaffe GJ, Sarraf D, et al. Consensus nomenclature for reporting neovascular age-related macular degeneration data: consensus on neovascular age-related macular degeneration nomenclature study group. Ophthalmology 2020; 127: 616–636. [DOI] [PubMed] [Google Scholar]
- 3. Schmidt-Erfurth U, Waldstein SM. A paradigm shift in imaging biomarkers in neovascular age-related macular degeneration. Prog Retin Eye Res 2016; 50: 1–24. [DOI] [PubMed] [Google Scholar]
- 4. Schmidt-Erfurth U, Klimscha S, Waldstein SM, et al. A view of the current and future role of optical coherence tomography in the management of age-related macular degeneration. Eye 2017; 31: 26–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rosenfeld PJ. Lessons learned from avastin and OCT – the great, the good, the bad, and the ugly: the LXXV Edward Jackson memorial lecture. Am J Ophthalmol 2019; 204: 26–45. [DOI] [PubMed] [Google Scholar]
- 6. Trivizki O, Karp MR, Chawla A, et al. Eliminating visual acuity and dilated fundus examinations improves cost efficiency of performing optical coherence tomography-guided intravitreal injections. Am J Ophthalmol 2020; 219: 222–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Toth CA, Decroos FC, Ying G-S, et al. Identification of fluid on optical coherence tomography by treating ophthalmologists versus a reading center in the comparison of age-related macular degeneration treatments trials. Retina 2015; 35: 1303–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Waldstein SM, Philip A-M, Leitner R, et al. Correlation of 3-dimensionally quantified intraretinal and subretinal fluid with visual acuity in neovascular age-related macular degeneration. JAMA Ophthalmol 2016; 134: 182–190. [DOI] [PubMed] [Google Scholar]
- 9. Schmidt-Erfurth U, Sadeghipour A, Gerendas BS, et al. Artificial intelligence in retina. Prog Retin Eye Res 2018; 67: 1–29. [DOI] [PubMed] [Google Scholar]
- 10. Ting DSW, Liu Y, Burlina P, et al. AI for medical imaging goes deep. Nat Med 2018; 24: 539–540. [DOI] [PubMed] [Google Scholar]
- 11. Ting DSW, Peng L, Varadarajan AV, et al. Deep learning in ophthalmology: the technical and clinical considerations. Prog Retin Eye Res 2019; 72: 100759. [DOI] [PubMed] [Google Scholar]
- 12. Fercher AF, Hitzenberger CK, Drexler W, et al. In vivo optical coherence tomography. Am J Ophthalmol 1993; 116: 113–114. [DOI] [PubMed] [Google Scholar]
- 13. Rosenfeld PJ. Optical coherence tomography and the development of antiangiogenic therapies in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2016; 57: OCT14–OCT26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fung AE, Lalwani GA, Rosenfeld PJ, et al. An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol 2007; 143: 566–583. [DOI] [PubMed] [Google Scholar]
- 15. Busbee BG, Ho AC, Brown DM, et al. Twelve-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology 2013; 120: 1046–1056. [DOI] [PubMed] [Google Scholar]
- 16. Schmucker CM, Rücker G, Sommer H, et al. Treatment as required versus regular monthly treatment in the management of neovascular age-related macular degeneration: a systematic review and meta-analysis. PLoS One 2015; 10: e0137866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Campochiaro PA, Akhlaq A. Sustained suppression of VEGF for treatment of retinal/choroidal vascular diseases. Prog Retin Eye Res 2021; 83: 100921. [DOI] [PubMed] [Google Scholar]
- 18. Freund KB, Korobelnik J-F, Devenyi R, et al. Treat-and-extend regimens with anti-VEGF agents in retinal diseases. Retina 2015; 35: 1489–1506. [DOI] [PubMed] [Google Scholar]
- 19. Schmidt-Erfurth U, Chong V, Loewenstein A, et al. Guidelines for the management of neovascular age-related macular degeneration by the European Society of Retina Specialists (EURETINA). Br J Ophthalmol 2014; 98: 1144–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arnold JJ, Markey CM, Kurstjens NP, et al. The role of sub-retinal fluid in determining treatment outcomes in patients with neovascular age-related macular degeneration – a phase IV randomised clinical trial with ranibizumab: the FLUID study. BMC Ophthalmol 2016; 16: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mitchell P, Holz FG, Hykin P, et al. Efficacy and safety of intravitreal aflibercept using a treat-and-extend regimen for neovascular age-related macular degeneration. Retina 2021; 41: 1911–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guymer RH, Markey CM, McAllister IL, et al. Tolerating subretinal fluid in neovascular age-related macular degeneration treated with ranibizumab using a treat-and-extend regimen. Ophthalmology 2019; 126: 723–734. [DOI] [PubMed] [Google Scholar]
- 23. Müller PL, Liefers B, Treis T, et al. Reliability of retinal pathology quantification in age-related macular degeneration: implications for clinical trials and machine learning applications. Transl Vis Sci Technol 2021; 10: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ahlers C, Golbaz I, Stock G, et al. Time course of morphologic effects on different retinal compartments after ranibizumab therapy in age-related macular degeneration. Ophthalmology 2008; 115: e39–e46. [DOI] [PubMed] [Google Scholar]
- 25. Schmidt-Erfurth U, Eldem B, Guymer R, et al. Efficacy and safety of monthly versus quarterly ranibizumab treatment in neovascular age-related macular degeneration: the EXCITE study. Ophthalmology 2011; 118: 831–839. [DOI] [PubMed] [Google Scholar]
- 26. Golbaz I, Ahlers C, Stock G, et al. Quantification of the therapeutic response of intraretinal, subretinal, and subpigment epithelial compartments in exudative AMD during anti-VEGF therapy. Invest Ophthalmol Vis Sci 2011; 52: 1599–1605. [DOI] [PubMed] [Google Scholar]
- 27. Keane PA, Heussen FM, Ouyang Y, et al. Assessment of differential pharmacodynamic effects using optical coherence tomography in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2012; 53: 1152–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schmidt-Erfurth U, Reiter GS, Riedl S, et al. AI-based monitoring of retinal fluid in disease activity and under therapy. Prog Retin Eye Res 2022; 86: 100972. [DOI] [PubMed] [Google Scholar]
- 29. Rashno A, Koozekanani DD, Drayna PM, et al. Fully automated segmentation of fluid/cyst regions in optical coherence tomography images with diabetic macular edema using neutrosophic sets and graph algorithms. IEEE Trans Biomed Eng 2018; 65: 989–1001. [DOI] [PubMed] [Google Scholar]
- 30. Garvin MK, Abràmoff MD, Wu X, et al. Automated 3-D intraretinal layer segmentation of macular spectral-domain optical coherence tomography images. IEEE Trans Med Imaging 2009; 28: 1436–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mishra Z, Ganegoda A, Selicha J, et al. Automated retinal layer segmentation using graph-based algorithm incorporating deep-learning-derived information. Sci Rep 2020; 10: 9541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Keenan TDL, Clemons TE, Domalpally A, et al. Retinal specialist versus artificial intelligence detection of retinal fluid from OCT. Ophthalmology 2021; 128: 100–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schlegl T, Waldstein SM, Bogunovic H, et al. Fully automated detection and quantification of macular fluid in OCT using deep learning. Ophthalmology 2018; 125: 549–558. [DOI] [PubMed] [Google Scholar]
- 34. Klimscha S, Waldstein SM, Schlegl T, et al. Spatial correspondence between intraretinal fluid, subretinal fluid, and pigment epithelial detachment in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2017; 58: 4039–4048. [DOI] [PubMed] [Google Scholar]
- 35. Ahn S-E, Oh J, Oh J-H, et al. Three-dimensional configuration of subretinal fluid in central serous chorioretinopathy. Invest Ophthalmol Vis Sci 2013; 54: 5944–5952. [DOI] [PubMed] [Google Scholar]
- 36. Kirkby GR, Chignell AH. Shifting subretinal fluid in rhegmatogenous retinal detachment. Br J Ophthalmol 1985; 69: 654–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Michl M, Fabianska M, Seeböck P, et al. Automated quantification of macular fluid in retinal diseases and their response to anti-VEGF therapy. Br J Ophthalmol 2022; 106: 113–120. [DOI] [PubMed] [Google Scholar]
- 38. Dolz-Marco R, Litts KM, Tan ACS, et al. The evolution of outer retinal tubulation, a neurodegeneration and gliosis prominent in macular diseases. Ophthalmology 2017; 124: 1353–1367. [DOI] [PubMed] [Google Scholar]
- 39. Preti RC, Govetto A, Filho RGA, et al. Optical coherence tomography analysis of outer retinal tubulations. Retina 2018; 38: 1518–1525. [DOI] [PubMed] [Google Scholar]
- 40. Schmidt-Erfurth UM, Vogl W, Jampol LM, et al. Application of automated quantification of fluid volumes to anti-VEGF therapy of neovascular age-related macular degeneration. Ophthalmology 2020; 127: 1211–1219. [DOI] [PubMed] [Google Scholar]
- 41. Reiter GS, Grechenig C, Vogl W-D, et al. Analysis of fluid volume and its impact on visual acuity in the fluid study as quantified with deep learning. Retina 2021; 41: 1318–1328. [DOI] [PubMed] [Google Scholar]
- 42. Grechenig C, Reiter GS, Riedl S, et al. Impact of residual subretinal fluid volumes on treatment outcomes in a subretinal fluid-tolerant treat-and-extend regimen. Retina 2021; 41: 2221–2228. [DOI] [PubMed] [Google Scholar]
- 43. Keenan TDL, Chakravarthy U, Loewenstein A, et al. Automated quantitative assessment of retinal fluid volumes as important biomarkers in neovascular age-related macular degeneration. Am J Ophthalmol 2021; 224: 267–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Moraes G, Fu DJ, Wilson M, et al. Quantitative analysis of OCT for neovascular age-related macular degeneration using deep learning. Ophthalmology 2021; 128: 693–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chew JK, Zhu M, Broadhead GK, et al. Bilateral neovascular age-related macular degeneration: comparisons between first and second eyes. Ophthalmologica 2017; 238: 23–30. [DOI] [PubMed] [Google Scholar]
- 46. Zarranz-Ventura J, Liew G, Johnston RL, et al. The neovascular age-related macular degeneration database: report 2: incidence, management, and visual outcomes of second treated eyes. Ophthalmology 2014; 121: 1966–1975. [DOI] [PubMed] [Google Scholar]
- 47. Cornish EE, Teo KY, Nguyen V, et al. Five-year incidence and visual acuity outcomes for intravitreal therapy in bilateral neovascular age-related macular degeneration. Retina 2021; 41: 118–124. [DOI] [PubMed] [Google Scholar]
- 48. Chakravarthy U, Havilio M, Syntosi A, et al. Impact of macular fluid volume fluctuations on visual acuity during anti-VEGF therapy in eyes with nAMD. Eye 2021; 35: 2983–2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Evans RN, Reeves BC, Maguire MG, et al. Associations of variation in retinal thickness with visual acuity and anatomic outcomes in eyes with neovascular age-related macular degeneration lesions treated with anti–vascular endothelial growth factor agents. JAMA Ophthalmol 2020; 138: 1043–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Keane PA, Liakopoulos S, Ongchin SC, et al. Quantitative subanalysis of optical coherence tomography after treatment with ranibizumab for neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2008; 49: 3115–3120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hariri A, Diniz B, Fou LV, et al. Quantitative OCT subanalysis of eyes with choroidal neovascularization switched from multiple injections of bevacizumab or ranibizumab to intravitreal aflibercept. Ophthalmic Surg Lasers Imaging Retina 2015; 46: 195–200. [DOI] [PubMed] [Google Scholar]
- 52. Hee MR, Puliafito CA, Wong C, et al. Quantitative assessment of macular edema with optical coherence tomography. Arch Ophthalmol 1995; 113: 1019–1029. [DOI] [PubMed] [Google Scholar]
- 53. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1419–1431. [DOI] [PubMed] [Google Scholar]
- 54. Dugel PU, Singh RP, Koh A, et al. HAWK and HARRIER: ninety-six-week outcomes from the phase 3 trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology 2021; 128: 89–99. [DOI] [PubMed] [Google Scholar]
- 55. Sharma S, Toth CA, Daniel E, et al. Macular morphology and visual acuity in the second year of the comparison of age-related macular degeneration treatments trials. Ophthalmology 2016; 123: 865–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Moutray T, Alarbi M, Mahon G, et al. Relationships between clinical measures of visual function, fluorescein angiographic and optical coherence tomography features in patients with subfoveal choroidal neovascularisation. Br J Ophthalmol 2008; 92: 361–364. [DOI] [PubMed] [Google Scholar]
- 57. Wilson M, Chopra R, Wilson MZ, et al. Validation and clinical applicability of whole-volume automated segmentation of optical coherence tomography in retinal disease using deep learning. JAMA Ophthalmol 2021; 139: 964–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Roberts PK, Zotter S, Montuoro A, et al. Identification and quantification of the angiofibrotic switch in neovascular AMD. Invest Ophthalmol Vis Sci 2019; 60: 304–311. [DOI] [PubMed] [Google Scholar]
- 59. Aslam TM, Mahmood S, Balaskas K, et al. Statistical modelling of the visual impact of subretinal fluid and associated features. Ophthalmol Ther 2021; 10: 127–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lee H, Jo A, Kim HC. Three-dimensional analysis of morphologic changes and visual outcomes in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2017; 58: 1337–1345. [DOI] [PubMed] [Google Scholar]
- 61. Llorente-González S, Hernandez M, González-Zamora J, et al. The role of retinal fluid location in atrophy and fibrosis evolution of patients with neovascular age-related macular degeneration long-term treated in real world. Acta Ophthalmol 2022; 100: e521–e531. [DOI] [PubMed] [Google Scholar]
- 62. Reiter GS, Told R, Schranz M, et al. Subretinal drusenoid deposits and photoreceptor loss detecting global and local progression of geographic atrophy by SD-OCT imaging. Invest Ophthalmol Vis Sci 2020; 61: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Keane PA, Patel PJ, Ouyang Y, et al. Effects of retinal morphology on contrast sensitivity and reading ability in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2010; 51: 5431–5437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Riedl S, Cooney L, Grechenig C, et al. Topographic analysis of photoreceptor loss correlated with disease morphology in neovascular age-related macular degeneration. Retina 2020; 40: 2148–2157. [DOI] [PubMed] [Google Scholar]
- 65. Orlando JI, Breger A, Bogunović H, et al. An amplified-target loss approach for photoreceptor layer segmentation in pathological OCT scans. In: Fu H, Garvin M, MacGillivray T, et al. (eds) Ophthalmic medical image analysis. OMIA 2019. Lecture notes in computer science. New York: Springer, 2019, pp. 26–34. [Google Scholar]
- 66. Orlando JI, Gerendas BS, Riedl S, et al. Automated quantification of photoreceptor alteration in macular disease using optical coherence tomography and deep learning. Sci Rep 2020; 10: 5619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Chopra R, Preston GC, Keenan TDL, et al. Intravitreal injections: past trends and future projections within a UK tertiary hospital. Eye. Epub ahead of print 25 June 2021. DOI: 10.1038/s41433-021-01646-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Schranz M, Georgopoulos M, Sacu S, et al. Incidence and surgical care of retinal detachment during the first SARS-CoV-2 lockdown period at a tertiary referral center in Austria. PLoS One 2021; 16: e0248010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Olivia Li J-P, Liu H, Ting DSJ, et al. Digital technology, tele-medicine and artificial intelligence in ophthalmology: a global perspective. Prog Retin Eye Res 2021; 82: 100900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Sim SS, Yip MY, Wang Z, et al. Digital technology for AMD management in the post-COVID-19 new normal. Asia Pac J Ophthalmol 2021; 10: 39–48. [DOI] [PubMed] [Google Scholar]
- 71. De Fauw J, Ledsam JR, Romera-Paredes B, et al. Clinically applicable deep learning for diagnosis and referral in retinal disease. Nat Med 2018; 24: 1342–1350. [DOI] [PubMed] [Google Scholar]
- 72. Kermany DS, Goldbaum M, Cai W, et al. Identifying medical diagnoses and treatable diseases by image-based deep learning. Cell 2018; 172: 1122–1131.e9. [DOI] [PubMed] [Google Scholar]
- 73. Schmidt-Erfurth U, Waldstein SM, Klimscha S, et al. Prediction of individual disease conversion in early AMD using artificial intelligence. Invest Ophthalmol Vis Sci 2018; 59: 3199–3208. [DOI] [PubMed] [Google Scholar]
- 74. Schmidt-Erfurth U, Bogunovic H, Grechenig C, et al. Role of deep learning–quantified hyperreflective foci for the prediction of geographic atrophy progression. Am J Ophthalmol 2020; 216: 257–270. [DOI] [PubMed] [Google Scholar]
- 75. Silva R, Berta A, Larsen M, et al. Treat-and-extend versus monthly regimen in neovascular age-related macular degeneration: results with ranibizumab from the TREND study. Ophthalmology 2018; 125: 57–65. [DOI] [PubMed] [Google Scholar]
- 76. Boyer DS, Schmidt-Erfurth U, Van Lookeren Campagne M, et al. The pathophysiology of geographic atrophy secondary to age-related macular degeneration and the complement pathway as a therapeutic target. Retina 2017; 37: 819–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Liao DS, Grossi FV, El Mehdi D, et al. Complement C3 inhibitor pegcetacoplan for geographic atrophy secondary to age-related macular degeneration: a randomized phase 2 trial. Ophthalmology 2020; 127: 186–195. [DOI] [PubMed] [Google Scholar]
- 78. Jaffe GJ, Westby K, Csaky KG, et al. C5 inhibitor avacincaptad pegol for geographic atrophy due to age-related macular degeneration: a randomized pivotal phase 2/3 trial. Ophthalmology 2021; 128: 576–586. [DOI] [PubMed] [Google Scholar]
- 79. Abràmoff MD, Lavin PT, Birch M, et al. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. npj Digit Med 2018; 1: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. De Sisternes L, Jonna G, Greven MA, et al. Individual drusen segmentation and repeatability and reproducibility of their automated quantification in optical coherence tomography images. Transl Vis Sci Technol 2017; 6: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]