Abstract
We conducted a meta-analysis to evaluate the efficacy of low-intensity extracorporeal shock wave therapy (LI-ESWT) in the treatment of erectile dysfunction (ED). From July 2011 to June 2021, we finally selected 16 randomized controlled trials (RCTs) including 1,064 participants to evaluate the efficacy of LI-ESWT in the treatment of ED from PubMed, EMBASE, and Cochrane databases. The data are analyzed by Review Manager Version 5.4. Fifteen articles mentioned International Index of Erectile Function (IIEF), in the follow-up of 1 month (mean difference [MD] = 3.18, 95% confidence interval [CI] = [1.38, 4.98], p = .0005), 3 months (MD = 3.01, 95% CI = [2.04, 3.98], p < .00001), and 6 months (MD = 3.20, 95% CI = [2.49, 3.92], p < .00001). After treatment, the improvement of IIEF in the LI-ESWT group was better than that in the control group. Besides, eight of the 16 trials provided data on the proportion of patients with baseline Erectile Hardness Score (EHS) ≤ 2 improved to EHS ≥ 3. The LI-ESWT group was also significantly better than the placebo group (odds ratio [OR] = 5.07, 95% CI = [1.78, 14.44], p = .002). The positive response rate of Questions 2 and 3 of the Sexual Encounter Profile (SEP) was not statistically significant (SEP2: OR = 1.27, 95% CI = [0.70, 2.30], p = .43; SEP3: OR = 4.24, 95% CI = [0.67, 26.83], p = .13). The results of this meta-analysis suggest that treatment plans with an energy density of 0.09 mJ/mm2 and pulses number of 1,500 to 2,000 are more beneficial to IIEF in ED patients. In addition, IIEF improvement was more pronounced in patients with moderate ED after extracorporeal shockwave therapy.
Keywords: low-intensity extracorporeal shockwave therapy, erectile dysfunction, randomized controlled trials, meta-analysis, International Index of Erectile Function, Erectile Hardness Score
Introduction
Erectile dysfunction (ED) refers to the inability of the penis to continuously achieve or maintain sufficient erection to meet a satisfactory sexual life (Burnett et al., 2018). The incidence rate of ED is increasing and the prevalence of ED is 30% to 65% among men aged 40 to 80 years (Ayta et al., 1999; Corona et al., 2010). The most common clinical treatment for ED is oral phosphodiesterase 5 inhibitor (PDE5I; Hatzimouratidis et al., 2010). However, some literatures reported that when PDE5I is used to treat ED patients, some patients say it is ineffective, and some patients will have various side effects, such as flushing and headache (Hatzimouratidis et al., 2010; Washington & Shindel, 2010).
Extracorporeal shock wave (ESW) is a two-way sound wave carrying energy. According to the different energy density levels of ESW, ESW has different functions in clinical application (Rassweiler et al., 2011). High energy density ESW has focused on mechanical damage characteristics, so it is often used in the treatment of stones. Medium energy density ESW has anti-inflammatory function and it is often used in surgery, such as synovial bursitis and nonbinding fracture. Low energy density ESW can promote angiogenesis and improve its blood supply and it is often used in chronic injury, musculoskeletal recovery, and cardiovascular disease (Nishida et al., 2004; Vardi et al., 2010; Wang et al., 2002). Studies have reported that the important mechanism of ED is vascular endothelial function injury or disorder (Gandaglia et al., 2014; Shindel et al., 2008) and low-intensity extracorporeal shock wave therapy (LI-ESWT) can stimulate the expression of angiogenesis-related factors, such as vascular endothelial growth factor (VEGF), so as to promote vascular regeneration (Cooper & Bachoo, 2018; Klomjit et al., 2020; Sundaram et al., 2018). As a result, LI-ESWT has been widely used in clinical treatment of ED (Rizk et al., 2018).
We carried out a meta-analysis of randomized controlled trials (RCTs) to systematically evaluate the efficacy of LI-ESWT in the treatment of ED.
Materials and Methods
Search Strategy
Under the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA; Moher et al., 2009), we searched three databases, namely, PubMed, Embase, and Cochrane, by computer and the retrieval time was limited from July 2011 to June 2021. The retrieval strategy is to search for the following Medical Subject Headings (MeSH) terms: shock wave, erectile dysfunction, the international index of erectile function, and the erection hardness scores. In addition, the researcher also traced all references involved in the included literature to supplement and obtain relevant literature. This study only included published articles and had no restrictions on the language of the articles. All articles were read independently by two researchers. In case of disagreement, an agreement will be reached through discussion or inviting the assistance of a third researcher.
Inclusion Criteria and Article Selection
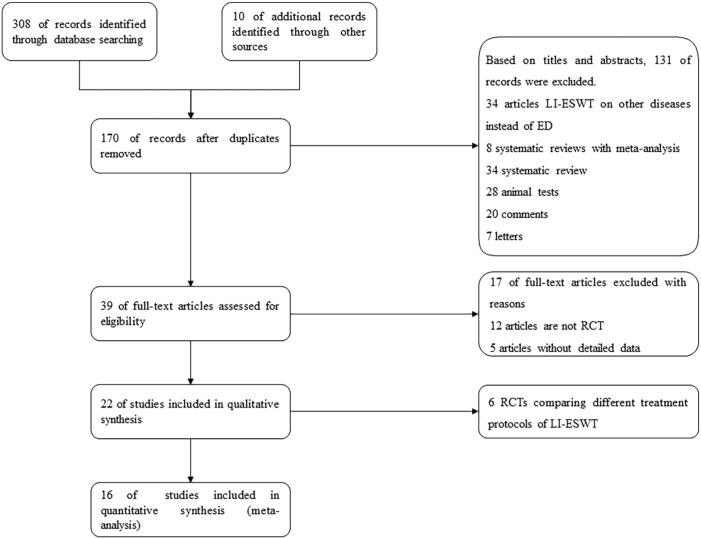
Included articles should meet the following inclusion criteria: (a) all RCTs describing LI-ESWT treatment for ED; (b) the content and data of any article are available; (c) all the data in the paper are true and valid; (d) no matter whether the test adopts blind method and allocation concealment or not; (e) no matter whether the patients are complicated with other complications; and (f) the severity of ED patients is not limited. Case reports, review articles, conference reports and abstracts, and some studies with incomplete data were excluded. The PRISMA flowchart of literature screening is presented in Figure 1.
Figure 1.
Flowchart of Selection PRISMA
Note. RCTs = randomized controlled trials; LI-ESWT = low-intensity extracorporeal shock wave therapy; ED = erectile dysfunction.
Quality Assessment
We mainly used Cochrane bias risk assessment tool to evaluate all randomized controlled studies, supplemented by Jadad scale for reference (Cumpston et al., 2019; Moher et al., 1996). Each article was evaluated according to the following three quality evaluation criteria: (+) bias is low, (?) not mentioned or no sufficient information to judge bias, and (−) bias is high. All authors independently participated in the evaluation of each RCT and exchanged results. If there is any objection, it will be resolved through discussion and negotiation until all the results are consistent.
Data Extraction
The two authors extracted data from the included studies according to the predetermined criteria independently, and recorded the data on the premade data extraction table. The extracted data include (a) author’s name (publication time), (b) country, (c) number of participants, (d) age, (e) PDE5I response or not, (f) treatment setup, (g) control group setup, (h) follow-up time, and (i) outcome indicators. This study does not need ethical approval because it is a retrospective analysis of existing studies.
Statistical Analyses
This study uses Review Manager Version 5.4 (Cochrane Collaboration, London, UK) for data analysis. We use fixed effect model or random effect model for analysis. The dichotomous data are expressed in odds ratios (ORs) and 95% confidence interval (CIs), whereas the continuous outcomes are expressed in mean difference (MD) and 95% CI. We usually used I-square (I2) to assess the heterogeneity of the study. If the p value is greater than .05 in the Q-value statistic test and the I2 value is less than 50%, we believe that the study is homogeneous and can be analyzed by the fixed effect model. While the results with I2 test value are greater than 50% and significant heterogeneity, the random effect model is used for analysis. Results of this meta-analysis are presented in forest plots and the data with p < .05 were considered statistically significant.
Results
Study Selection, Search Results, and Characteristics of the Trials
We searched according to the above search strategy and finally retrieve 318 articles. A total of 279 articles were excluded by deleting duplicate literature and screening abstracts and titles. Of the remaining 39 articles, 23 articles were excluded because they are not RCT or lack of effective data. Finally, the remaining 16 articles were included in the study to evaluate the effectiveness of LI-ESWT in the treatment of ED (Baccaglini et al., 2020; Fojecki et al., 2017; Kalyvianakis & Hatzichristou, 2017; Kim et al., 2020; Kitrey et al., 2016; Ladegaard et al., 2021; Olsen et al., 2015; Ortac et al., 2021; Shendy et al., 2021; Sramkova et al., 2020; Srini et al., 2015; Vardi et al., 2012; Vinay et al., 2021; Yamaçake et al., 2019; Yee et al., 2014; Zewin et al., 2018). The details of each study are presented in Table 1. There was no significant difference in mean age and severity of ED between the LI-ESWT group and the placebo group.
Table 1.
The details of each study.
| Authors’ name | Year | Country | No. of participants | Age | PDE5I-response or not | LI-ESWT setup | Control setup | Methodology | Follow-up time | Outcome indicators |
|---|---|---|---|---|---|---|---|---|---|---|
| Baccaglini et al. | 2019 | Brazil | 77 | 64.6 ± 5.3 | NA | • Energy density: 0.09 mJ/mm2
• Frequency: 5 Hz • Pulse: 600 pulses/treatment • RENOVA® electromagnetic device |
NA | • One treatment/week • 8 weeks treatment |
• 1 month | • IIEF variation scores |
| Fojecki et al. | 2016 | Denmark | 118 | 64.4 ± 8.4 | Yes | • Energy density: 0.09 mJ/mm2
• Frequency: 5 Hz • Pulse: 600 pulses/treatment • FBL10, Richard-Wolf GmbH |
With a gel pad that prevent the passage of energy | • One treatment/week • 5 weeks treatment |
• 1 month | • EHS response rate • IIEF variation scores |
| Kalyvianakis et al. | 2017 | Greece | 46 | 54 (31–72) | Yes | • Energy density: 0.09 mJ/mm2
• Frequency: 2 Hz • Pulse: 1,500 pulses/treatment • Omnispec ED1000 |
With an element that block delivery of shockwaves | • Two treatments/week • 3 weeks treatment • 3 weeks no treatment • 3 weeks treatment |
• 1 month • 3 months • 6 months |
• IIEF variation scores |
| Kim et al. | 2019 | Korea | 81 | 64.2 ± 6.6 | NA | • Energy density: 20 mJ/mm2
• 15 mJ/mm2 • 12 mJ/mm2 • Frequency: 5 Hz • Pulse: 3000 pulses/treatment • MT 2000H |
Sham treatment without delivering any energy | • Two treatments/week • 3 weeks treatment • 3 weeks no treatment • 3 weeks treatment |
• 1 month • 2 months |
• EHS response rate • IIEF variation scores |
| Kitrey et al. | 2015 | Israel | 55 | 62 (28–81) | No | • Energy density: 0.09 mJ/mm2
• Frequency: 2 Hz • Pulse: 1,500 pulses/treatment • Omnispec ED1000 |
Sham treatment without delivering any energy | • Two treatments/week • 3 weeks treatment • 3 weeks no treatment • 3 weeks treatment |
• 1 month | • EHS response rate • IIEF variation scores |
| Ladegaard et al. | 2021 | Denmark | 38 | 62.5 ± 5.8 | Yes | • Energy density: 0.15 mJ/mm2
• Frequency: 5 Hz • Pulse: 4000 pulses/treatment • Duolith SD1 |
With a sham pad that prevent shockwaves | • One treatment/week • 5 weeks treatment |
• 1 month • 3 months |
• IIEF variation scores |
| Olsen et al. | 2015 | Denmark | 105 | 60 (37–80) | Yes | • Energy density: 0.15 mJ/mm2
• Frequency: 5 Hz • Pulse: 3,000 pulses/treatment • Duolith SD1 |
With a cap used to prevent LI-ESWT | • One treatment/week • 5 weeks treatment |
• 1 month • 3 months • 6 months |
• EHS response rate |
| Ortac et al. | 2021 | Turkey | 66 | 41 ± 10.7 | NA | • Energy density: 0.2 mJ/mm2
• Frequency: 5 Hz • Pulse: 3,000 pulses/treatment • Duolith SD1 |
With a shock wave absorbent material | • One treatment/week • 4 weeks treatment |
• 3 months • 6 months |
• IIEF variation scores • SEP2 response rate • SEP3 response rate |
| Shendy et al. | 2021 | Egypt | 42 | 48 ± 5.6 | Yes | • Energy density: 0.09 mJ/mm2
• Pulse: 3,000 pulses/treatment • Duolith SD1 |
With an element that blocked the delivery of shock waves | • Two treatments/week • 3 weeks treatment • 3 weeks no treatment • 3 weeks treatment |
• 3 months | • IIEF variation scores |
| Sramkova et al. | 2019 | Czech | 60 | 54.3 ± 9.2 | Yes | • Energy density: 0.16 mJ/mm2
• Richard Wolf GmbH |
With a gel head that blocked shockwaves | • Two treatments/week • 4 weeks treatment |
• 1 month • 3 months |
• IIEF variation scores • SEP2 response rate • SEP3 response rate |
| Srini et al. | 2015 | India | 77 | Not mentioned | Yes | • Energy density: 0.09 mJ/mm2
• Frequency: 2 Hz • Pulse: 1,500 pulses/treatment • Omnispec ED1000 |
With a metal plate to block the transmission of the shockwave energy | • Two treatments/week • 3 weeks treatment • 3 weeks no treatment • 3 weeks treatment |
• 1 month • 3 months • 6 months • 9 month • 12 months |
• EHS response rate • IIEF variation scores |
| Vardi et al. | 2012 | Israel | 60 | 57 (27–77) | Yes | • Energy density: 0.09 mJ/mm2
• Frequency: 5 Hz • Pulse: 1,500 pulses/treatment • Omnispec ED1000 |
With a metal plate that prevented the shock wave energy | • Two treatments/week • 3 weeks treatment • 3 weeks no treatment • 3 weeks treatment |
• 1 month | • EHS response rate • IIEF variation scores |
| Vinay et al. | 2020 | Spain | 76 | 60 (53–66) | No | • Energy density: 0.09 mJ/mm2
• Frequency: 2 Hz • Pulse: 5,000 pulses/treatment • RENOVA® electromagnetic device |
With a probe that did not generate shockwaves | • One treatment/week • 4 weeks treatment |
• 1 month • 3 months • 6 months |
• EHS response rate • IIEF variation scores • SEP2 response rate • SEP3 response rate |
| Yamaçake et al. | 2018 | Brazil | 20 | 54 (46–61) | NA | • Energy density: 0.09 mJ/mm2
• Pulse: 2,000 pulses/treatment • Swiss Dolorclast |
With a probe that emitted 0 energy | • Two treatments/week • 3 weeks treatment |
• 1 month • 3 months |
• IIEF variation scores |
| Yee et al. | 2014 | China | 58 | 61.0 ± 7.3 | Yes | • Energy density: 0.09 mJ/mm2
• Frequency: 2 Hz • Pulse: 1,500 pulses/treatment • Omnispec ED1000 |
The energy setting was 0 during each treatment | • Two treatments/week • 3 weeks treatment • 3 weeks no treatment • 3 weeks treatment |
• 1 month | • IIEF variation scores |
| Zewin et al. | 2018 | Egypt | 85 | 52.1 ± 6.8 | NA | • Energy density: 0.09 mJ/mm2
• Frequency: 2 Hz • Pulse: 1,500 pulses/treatment • Dornier Aries device |
Without any therapy | • Two treatments/week • 3 weeks treatment • 3 weeks no treatment • 3 weeks treatment |
• 3 months • 6 months |
• EHS response rate • IIEF variation scores |
Note. PDE5I = phosphodiesterase 5 inhibitor; LI-ESWT = low-intensity extracorporeal shock wave therapy; NA = not available; IIEF = International Index of Erectile Function; EHS = Erectile Hardness Score.
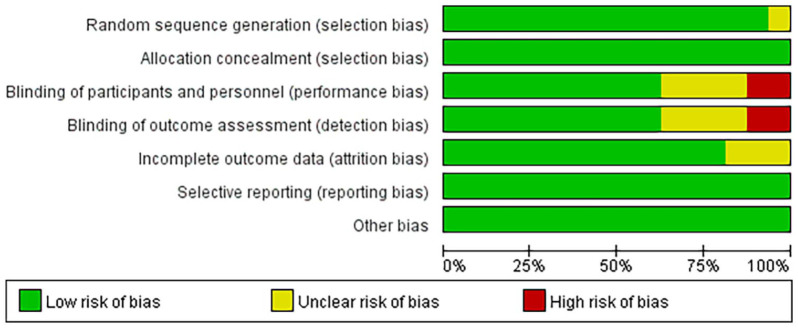
Risk of Bias
All included studies in meta-analysis were RCTs. The summary and graph of bias risk are presented in Figure 2 and Supplemental Figure S1.
Figure 2.
The Risk of Bias Graph.
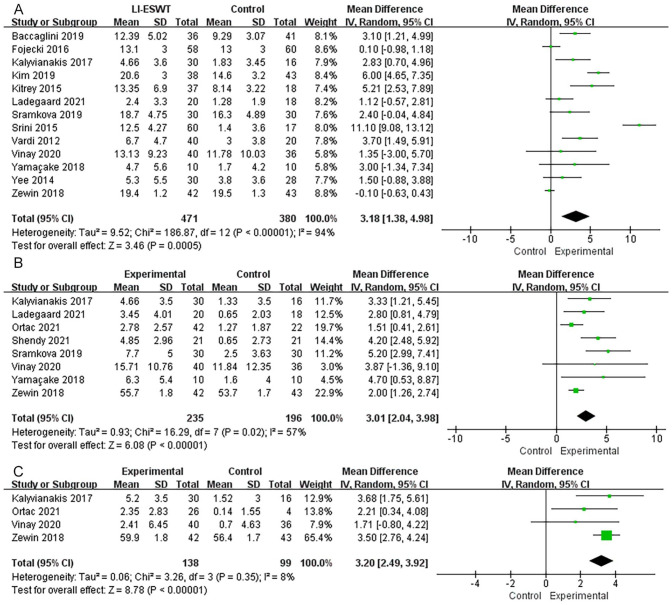
International Index of Erectile Function (IIEF)
Among the 16 included studies, 12 articles provided IIEF data at 1 month follow-up after treatment, eight provided data at 3 months follow-up, and four provided data at 6 months follow-up. Heterogeneity test proved that there was statistical heterogeneity among trials in each group, so random effect model was used for meta-analysis. The results reported that after 1 month (MD = 3.18, 95% CI = [1.38, 4.98], p = .0005), 3 months (MD = 3.01, 95% CI = [2.04, 3.98], p < .00001), and 6 months follow-up (MD = 3.20, 95% CI = [2.49, 3.92], p < .00001), the treatment group can significantly increase the IIEF of ED patients compared with the control group, and the results are statistically significant (Figure 3). The IIEF data analyzed are all variation values and some data with negative change values are replaced by their final values.
Figure 3.
Forest Plots Showing the Improvement of IIEF by LI-ESWT at Different Follow-Up Times After Treatment: (A) 1 Month Follow-Up; (B) 3 Months Follow-Up; (C) 6 Months Follow-Up
Note. LI-ESWT = low-intensity extracorporeal shock wave therapy; IIEF = International Index of Erectile Function; SD = standard deviation; IV = inverse variance; CI = confidence interval; df = degrees of freedom.
Erection Hardness Scores
Overall, eight of the 16 articles provided data on the improvement of patients with baseline Erectile Hardness Score (EHS) ≤ 2 to EHS ≥ 3 after treatment. The random effect model was used for the meta-analysis. The results identified that there was a significant difference in the number of people of EHS improvement between the treatment group and the control group (OR = 5.07, 95% CI = [1.78, 14.44], p = .002), indicating that the treatment group can significantly improve the EHS of patients compared with the control group (Supplemental Figure S2).
Sexual Encounter Profile (SEP)
Questions 2 and 3 of the SEP are usually used as another evaluation criterion. These two questions were mentioned in three studies. The results identified that compared with the control group, the “yes” response rate of the LI-ESWT group was not statistically significant (SEP2: OR = 1.27, 95% CI = [0.70, 2.30], p = .43; SEP3: OR = 4.24, 95% CI = [0.67, 26.83], p = .13; Supplemental Figure S3).
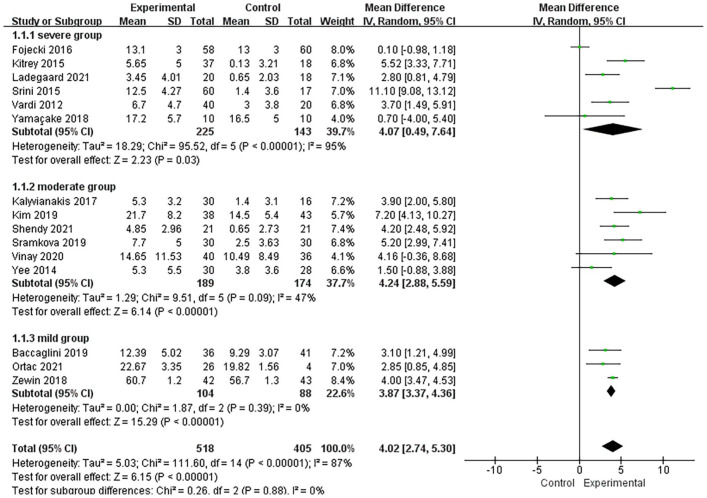
Subgroup Analysis
IIEF Baseline
According to the IIEF baseline value, the articles were divided into severe group (IIEF baseline value < 12), moderate group (IIEF baseline value 12–17), and mild group (IIEF baseline value > 17). We use the existing data to analysis and found that no matter in which subgroup, the improvement of IIEF in the treatment group was higher than that in the control group (severe: MD = 4.07, 95% CI = [0.49, 7.64], p = .03; moderate: MD = 4.24, 95% CI = [2.88, 5.59], p < .00001; mild: MD = 3.87, 95% CI = [3.37, 4.36], p < .00001; Figure 4).
Figure 4.
Forest Plots Showing the Subgroup Analysis of Different IIEF Baselines
Note. IIEF = International Index of Erectile Function; SD = standard deviation; IV = inverse variance; CI = confidence interval; df = degrees of freedom.
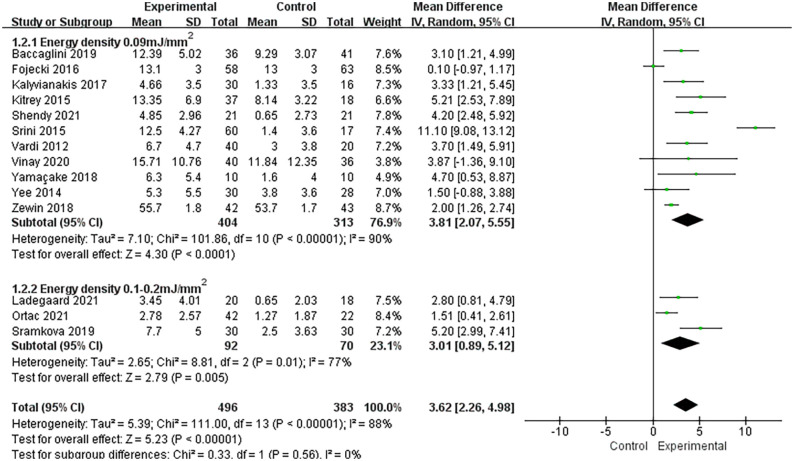
Energy Density
Because two of the 16 RCTs did not mention specific energy density or IIEF index, only the remaining 14 experiments were analyzed. According to the set energy density, it is divided into two groups: the energy density is equal to 0.09 mJ/mm2 and the energy density is between 0.1 and 0.2 mJ/mm2. The results suggested that in the two subgroups, the treatment group could significantly increase the IIEF of patients compared with the control group (0.09 mJ/mm2: MD = 3.81, 95% CI = [2.07, 5.55], p < .0001; 0.1–0.2 mJ/mm2: MD = 3.01, 95% CI = [0.89, 5.12], p = .005; Figure 5).
Figure 5.
Forest Plots Showing the Subgroup Analysis of Different Energy Density Treatments
Note. SD = standard deviation; IV = inverse variance; CI = confidence interval; df = degrees of freedom.
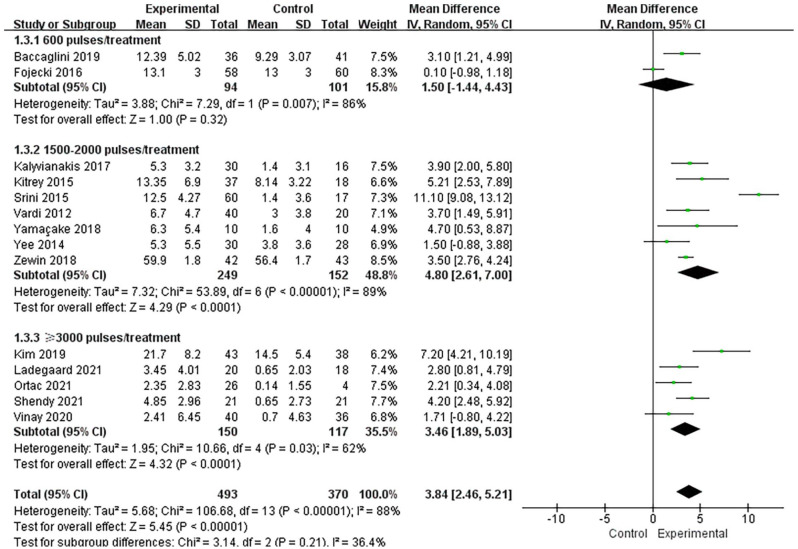
Pulses
We divided 14 RCTs into three groups according to the number of pulses per treatment: the number of pulses is equal to 600, the number of pulses is between 1,500 and 2,000, and the number of pulses is greater than 3,000. The results of the 600 pulses group reported that the treatment group could increase the IIEF of patients compared with the control group, but the difference was not statistically significant (MD = 1.50, 95% CI = [−1.44, 4.43], p = .32). The results of the group with pulse number between 1,500 and 2,000 suggested that the treatment group could significantly increase the IIEF of patients (MD = 4.80, 95% CI = [2.61, 7.00], p < .0001). In the group with pulse number greater than 3,000, compared with the control group, the treatment group can also significantly increase the IIEF of patients and the difference is statistically significant (MD = 3.46, 95% CI = [1.89, 5.03], p < .0001; Figure 6).
Figure 6.
Forest Plots Showing the Subgroup Analysis of Treatment With Different Pulse Numbers
Note. SD = standard deviation; IV = inverse variance; CI = confidence interval; df = degrees of freedom.
Discussion
We conducted a meta-analysis of 16 studies including 1,064 participants to compare the efficacy of LI-ESWT and placebo in the treatment of ED. It was found that the improvement of IIEF and EHS after LI-ESWT treatment was greater than that of placebo group, but there was no significant difference in SEP2 and SEP3. These results suggest that LI-ESWT is more effective than placebo in improving the symptoms of ED patients.
At present, the clinical treatment methods of ED include oral PDE5I, injection of vasodilator into corpus cavernosum of penis, transurethral administration of prostaglandin E, penile prosthesis implantation, and vacuum assisted erection device (Salonia et al., 2021). One of the most commonly used regimes is PDE5I drug treatment, but this plan cannot correct the potential pathophysiological mechanism of the penis, and many patients are insensitive or even ineffective to it. LI-ESWT is noninvasive and rehabilitative compared with the second-line or third-line treatment of ED, and patients who are ineffective in PDE5I treatment can also benefit from LI-ESWT treatment (Chung & Cartmill, 2015; Gruenwald et al., 2012; Kitrey et al., 2016).
The mechanism of LI-ESWT improving IIEF in the treatment of ED is not clear. In recent years, it has been identified that ESW can produce “cavitation effect,” open up physiologically closed micro vessels, and accelerate capillary microcirculation (Maisonhaute et al., 2002). ESW can also promote neovascularization and the expression of angiogenic markers, so as to promote tissue remodeling (Holfeld et al., 2016; Young Academic Urologists Men’s Health Group et al., 2017). However, there is controversy about whether LI-ESWT is associated with neuronal nitric oxide synthase (nNOS) synthesis. Studies have identified that LI-ESWT can promote the regeneration of in endothelial, smooth muscle, and neural expression of nNOS (Liu et al., 2013; Qiu et al., 2013), but there are also studies reported that LI-ESWT does not rely on nitric oxide and cyclic guanosine monophosphate to improve erectile function (Assaly-Kaddoum et al., 2016). One study described that LI-ESWT can also reduce the activity of sympathetic nervous system (Sokolakis et al., 2019). Most studies only report preliminary results, but there is no clear answer to the actual mechanism of LI-ESWT.
By analyzing our results, we found that LI-ESWT had different effects on erectile function with different energy density or pulses. When the energy density is 0.09 mJ/mm2, the improvement of IIEF is better than that in the energy density between 0.1 and 0.2 mJ/mm2. And 1,500 or 2,000 pulses per treatment bring more improvement than 600 or 3,000 pulses. The improvement of IIEF in patients with different severity of ED after LI-ESWT treatment is also different. Through our meta-analysis, we found that the improvement was more obvious in patients with moderate ED than in patients with mild or severe ED. In addition, the improvement of IIEF is different under different follow-up times. The improvement after 6 months follow-up is better than that after 1 month and 3 months. However, because only one RCT mentioned the follow-up results after 12 months, the long-term effect of LI-ESWT still needs further follow-up investigation.
In the process of data extraction, some reports reported neither IIEF final average data and standard deviation nor IIEF change data. Instead, they provide data such as interquartile range (IQR), sample median, and sample size. For the consistency and comparability of statistical data, the sample mean and standard deviation were estimated using the methods provided by the researchers (Luo et al., 2018; Wan et al., 2014).
The minimum clinically important difference (MCID) is considered to be an ideal method to evaluate the real clinical efficacy of interventions. It has been determined that the MCID in IIEF score is 4 points, indicating a 4 points difference may be clinically significant to patients (Rosen et al., 2011). For the trials included in this study, the comprehensive improvement of IIEF score in some groups after LI-ESWT treatment is less than 4 points, which may not have clinical value. With the publication of more and more RCTs, MCID is very important as an evaluation standard. Therefore, it is recommended to use MCID as an accurate and meaningful tool for evaluating LI-ESWT treatment in the future.
Compared with previous meta-analyses, our study excluded studies with high heterogeneity and included many latest studies, which is more convincing. Although the articles included in this meta-analysis are high-quality RCTs, there are still some limitations as follows: (a) Some experiments did not use double-blind research in the research process, and some patients withdrew from the research because they could not tolerate the intervention measures. These bias factors will affect our final research results. (b) Some experimental data only provide median and IQR, so we must use formulas to convert them into mean and standard deviation, and there may be some errors in this process. (c) Because most study endpoints were evaluated only 1 to 6 months after treatment, we could not infer the long-term efficacy of LI-ESWT treatment. (d) Our study did not report other indicators to evaluate ED, such as quality of sexual life, peak whole-body velocity, and resistance index because only one or two RCTs reported these indicators, and the results were not convincing. Therefore, further research and relevant data are needed to help us demonstrate the impact of LI-ESWT treatment on these indicators. (e) We did not assess the potential impact of age, hypertension, diabetes, hyperlipidemia, and coronary artery disease on IIEF.
Conclusion
This meta-analysis that contains 16 RCTs identified that LI-ESWT could significantly increase IIEF and EHS in ED patients, especially in moderate ED group, but had no significant improvement in positive response rate of SEP2 and SEP3. In general, LI-ESWT has become a popular choice for the treatment of ED because of its effectiveness and low risk, but more clinical experiments, longer follow-up, and more detailed data are still needed to support this conclusion.
Supplemental Material
Supplemental material, sj-tif-1-jmh-10.1177_15579883221087532 for Systematic Review and Meta-Analysis of 16 Randomized Controlled Trials of Clinical Outcomes of Low-Intensity Extracorporeal Shock Wave Therapy in Treating Erectile Dysfunction by Huibao Yao, Xiaofeng Wang, Hongquan Liu, Fengze Sun, Gonglin Tang, Xingjun Bao, Jitao Wu, Zhongbao Zhou and Jian Ma in American Journal of Men’s Health
Supplemental material, sj-tif-2-jmh-10.1177_15579883221087532 for Systematic Review and Meta-Analysis of 16 Randomized Controlled Trials of Clinical Outcomes of Low-Intensity Extracorporeal Shock Wave Therapy in Treating Erectile Dysfunction by Huibao Yao, Xiaofeng Wang, Hongquan Liu, Fengze Sun, Gonglin Tang, Xingjun Bao, Jitao Wu, Zhongbao Zhou and Jian Ma in American Journal of Men’s Health
Supplemental material, sj-tif-3-jmh-10.1177_15579883221087532 for Systematic Review and Meta-Analysis of 16 Randomized Controlled Trials of Clinical Outcomes of Low-Intensity Extracorporeal Shock Wave Therapy in Treating Erectile Dysfunction by Huibao Yao, Xiaofeng Wang, Hongquan Liu, Fengze Sun, Gonglin Tang, Xingjun Bao, Jitao Wu, Zhongbao Zhou and Jian Ma in American Journal of Men’s Health
Footnotes
Author contributions: J.M. and Z.Z. contributed to conceptualization; H.Y., H.L., F.S., and X.B. contributed to data curation; H.Y., X.W., G.T., and X.B. contributed to formal analysis. J.W. and J.M. contributed to funding acquisition. H.Y., X.W., H.L., and F.S. contributed to investigation. H.Y., X.W., H.L., F.S., and G.T. contributed to methodology. Z.Z. and J.M. contributed to project administration. F.S., G.T., and X.B. contributed to resources. H.Y. and X.W. contributed to software. G.T., X.B., and J.W. contributed to supervision. H.Y., X.W., and H.L. contributed to writing—original draft. Z.Z. and J.M. contributed to writing—review & editing.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants from the National Nature Science Foundation of China (Nos. 81870525 and 81572835) and Taishan Scholars Program of Shandong Province (No. tsqn201909199).
ORCID iD: Huibao Yao  https://orcid.org/0000-0002-5484-6904
https://orcid.org/0000-0002-5484-6904
Supplemental Material: Supplemental material for this article is available online.
References
- Assaly-Kaddoum R., Giuliano F., Laurin M., Gorny D., Kergoat M., Bernabé J., Vardi Y., Alexandre L., Behr-Roussel D. (2016). Low intensity extracorporeal shock wave therapy improves erectile function in a model of type II diabetes independently of NO/cGMP pathway. The Journal of Urology, 196(3), 950–956. 10.1016/j.juro.2016.03.147 [DOI] [PubMed] [Google Scholar]
- Ayta I. A., McKinlay J. B., Krane R. J. (1999). The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU International, 84(1), 50–56. 10.1046/j.1464-410x.1999.00142.x [DOI] [PubMed] [Google Scholar]
- Baccaglini W., Pazeto C. L., Corrêa Barros E. A., Timóteo F., Monteiro L., Saad Rached R. Y., Navas A., Glina S. (2020). The role of the low-intensity extracorporeal shockwave therapy on penile rehabilitation after radical prostatectomy: A randomized clinical trial. The Journal of Sexual Medicine, 17(4), 688–694. 10.1016/j.jsxm.2019.12.024 [DOI] [PubMed] [Google Scholar]
- Burnett A. L., Nehra A., Breau R. H., Culkin D. J., Faraday M. M., Hakim L. S., Heidelbaugh J., Khera M., McVary K. T., Miner M. M., Nelson C. J., Sadeghi-Nejad H., Seftel A. D., Shindel A. W. (2018). Erectile dysfunction: AUA guideline. The Journal of Urology, 200(3), 633–641. 10.1016/j.juro.2018.05.004 [DOI] [PubMed] [Google Scholar]
- Chung E., Cartmill R. (2015). Evaluation of clinical efficacy, safety and patient satisfaction rate after low-intensity extracorporeal shockwave therapy for the treatment of male erectile dysfunction: An Australian first open-label single-arm prospective clinical trial. BJU International, 115(Suppl. 5), 46–49. 10.1111/bju.13035 [DOI] [PubMed] [Google Scholar]
- Cooper B., Bachoo P. (2018). Extracorporeal shock wave therapy for the healing and management of venous leg ulcers. The Cochrane Database of Systematic Reviews, 6, CD011842. 10.1002/14651858.CD011842.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corona G., Lee D. M., Forti G., O’Connor D. B., Maggi M., O’Neill T. W., Pendleton N., Bartfai G., Boonen S., Casanueva F. F., Finn J. D., Giwercman A., Han T. S., Huhtaniemi I. T., Kula K., Lean M. E. J., Punab M., Silman A. J., Vanderschueren D., . . . EMAS Study Group. (2010). Age-related changes in general and sexual health in middle-aged and older men: Results from the European Male Ageing Study (EMAS). The Journal of Sexual Medicine, 7(4 Pt 1), 1362–1380. 10.1111/j.1743-6109.2009.01601.x [DOI] [PubMed] [Google Scholar]
- Cumpston M., Li T., Page M. J., Chandler J., Welch V. A., Higgins J. P., Thomas J. (2019). Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Database of Systematic Reviews, 10, ED000142. 10.1002/14651858.ED000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fojecki G. L., Tiessen S., Osther P. J. S. (2017). Effect of low-energy linear shockwave therapy on erectile dysfunction—A double-blinded, sham-controlled, randomized clinical trial. The Journal of Sexual Medicine, 14(1), 106–112. 10.1016/j.jsxm.2016.11.307 [DOI] [PubMed] [Google Scholar]
- Gandaglia G., Briganti A., Jackson G., Kloner R. A., Montorsi F., Montorsi P., Vlachopoulos C. (2014). A systematic review of the association between erectile dysfunction and cardiovascular disease. European Urology, 65(5), 968–978. 10.1016/j.eururo.2013.08.023 [DOI] [PubMed] [Google Scholar]
- Gruenwald I., Appel B., Vardi Y. (2012). Low-intensity extracorporeal shock wave therapy—A novel effective treatment for erectile dysfunction in severe ED patients who respond poorly to PDE5 inhibitor therapy. The Journal of Sexual Medicine, 9(1), 259–264. 10.1111/j.1743-6109.2011.02498.x [DOI] [PubMed] [Google Scholar]
- Hatzimouratidis K., Amar E., Eardley I., Giuliano F., Hatzichristou D., Montorsi F., Vardi Y., Wespes E., & European Association of Urology. (2010). Guidelines on male sexual dysfunction: Erectile dysfunction and premature ejaculation. European Urology, 57(5), 804–814. 10.1016/j.eururo.2010.02.020 [DOI] [PubMed] [Google Scholar]
- Holfeld J., Zimpfer D., Albrecht-Schgoer K., Stojadinovic A., Paulus P., Dumfarth J., Thomas A., Lobenwein D., Tepeköylü C., Rosenhek R., Schaden W., Kirchmair R., Aharinejad S., Grimm M. (2016). Epicardial shock-wave therapy improves ventricular function in a porcine model of ischaemic heart disease. Journal of Tissue Engineering and Regenerative Medicine, 10(12), 1057–1064. 10.1002/term.1890 [DOI] [PubMed] [Google Scholar]
- Kalyvianakis D., Hatzichristou D. (2017). Low-intensity shockwave therapy improves hemodynamic parameters in patients with vasculogenic erectile dysfunction: A triplex ultrasonography-based sham-controlled trial. The Journal of Sexual Medicine, 14(7), 891–897. 10.1016/j.jsxm.2017.05.012 [DOI] [PubMed] [Google Scholar]
- Kim K. S., Jeong H. C., Choi S. W., Choi Y. S., Cho H. J., Ha U.-S., Hong S.-H., Lee J. Y., Lee S. W., Ahn S. T., Moon D. G., Bae W. J., Kim S. W. (2020). Electromagnetic low-intensity extracorporeal shock wave therapy in patients with erectile dysfunction: A sham-controlled, double-blind, randomized prospective study. The World Journal of Men’s Health, 38(2), 236–242. 10.5534/wjmh.190130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitrey N. D., Gruenwald I., Appel B., Shechter A., Massarwa O., Vardi Y. (2016). Penile low intensity shock wave treatment is able to shift PDE5i nonresponders to responders: A double-blind, sham controlled study. Journal of Urology, 195(5), 1550–1555. 10.1016/j.juro.2015.12.049 [DOI] [PubMed] [Google Scholar]
- Klomjit N., Lerman A., Lerman L. O. (2020). It comes as a shock: Kidney repair using shockwave therapy. Hypertension (Dallas, Tex.: 1979), 76(6), 1696–1703. 10.1161/HYPERTENSIONAHA.120.14595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladegaard P. B. J., Mortensen J., Skov-Jeppesen S. M., Lund L. (2021). Erectile dysfunction a prospective randomized placebo-controlled study evaluating the effect of Low-Intensity Extracorporeal Shockwave Therapy (LI-ESWT) in men with erectile dysfunction following radical prostatectomy. Sexual Medicine, 9(3), 100338. 10.1016/j.esxm.2021.100338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou F., Li G.-Y., Wang L., Li H.-X., Bai G.-Y., Guan R.-L., Xu Y.-D., Gao Z.-Z., Tian W.-J., Xin Z.-C. (2013). Evaluation of the effect of different doses of low energy shock wave therapy on the erectile function of streptozotocin (STZ)-induced diabetic rats. International Journal of Molecular Sciences, 14(5), 10661–10673. 10.3390/ijms140510661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo D., Wan X., Liu J., Tong T. (2018). Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Statistical Methods in Medical Research, 27(6), 1785–1805. 10.1177/0962280216669183 [DOI] [PubMed] [Google Scholar]
- Maisonhaute E., Prado C., White P. C., Compton R. G. (2002). Surface acoustic cavitation understood via nanosecond electrochemistry. Part III: Shear stress in ultrasonic cleaning. Ultrasonics Sonochemistry, 9(6), 297–303. 10.1016/s1350-4177(02)00089-5 [DOI] [PubMed] [Google Scholar]
- Moher D., Fortin P., Jadad A. R., Jüni P., Klassen T., Le Lorier J., Liberati A., Linde K., Penna A. (1996). Completeness of reporting of trials published in languages other than English: Implications for conduct and reporting of systematic reviews. Lancet (London, England), 347(8998), 363–366. 10.1016/s0140-6736(96)90538-3 [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., & PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. British Medical Journal (Clinical Research Ed.), 339, b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishida T., Shimokawa H., Oi K., Tatewaki H., Uwatoku T., Abe K., Matsumoto Y., Kajihara N., Eto M., Matsuda T., Yasui H., Takeshita A., Sunagawa K. (2004). Extracorporeal cardiac shock wave therapy markedly ameliorates ischemia-induced myocardial dysfunction in pigs in vivo. Circulation, 110(19), 3055–3061. 10.1161/01.CIR.0000148849.51177.97 [DOI] [PubMed] [Google Scholar]
- Olsen A. B., Persiani M., Boie S., Hanna M., Lund L. (2015). Can low-intensity extracorporeal shockwave therapy improve erectile dysfunction? A prospective, randomized, double-blind, placebo-controlled study. Scandinavian Journal of Urology, 49(4), 329–333. 10.3109/21681805.2014.984326 [DOI] [PubMed] [Google Scholar]
- Ortac M., Özmez A., Cilesiz N. C., Demirelli E., Kadıoğlu A. (2021). The impact of extracorporeal shock wave therapy for the treatment of young patients with vasculogenic mild erectile dysfunction: A prospective randomized single-blind, sham controlled study. Andrology, 9(5), 1571–1578. 10.1111/andr.13007 [DOI] [PubMed] [Google Scholar]
- Qiu X., Lin G., Xin Z., Ferretti L., Zhang H., Lue T. F., Lin C.-S. (2013). Effects of low-energy shockwave therapy on the erectile function and tissue of a diabetic rat model. The Journal of Sexual Medicine, 10(3), 738–746. 10.1111/jsm.12024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rassweiler J. J., Knoll T., Köhrmann K.-U., McAteer J. A., Lingeman J. E., Cleveland R. O., Bailey M. R., Chaussy C. (2011). Shock wave technology and application: An update. European Urology, 59(5), 784–796. 10.1016/j.eururo.2011.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizk P. J., Krieger J. R., Kohn T. P., Pastuszak A. W. (2018). Low-intensity shockwave therapy for erectile dysfunction. Sexual Medicine Reviews, 6(4), 624–630. 10.1016/j.sxmr.2018.01.002 [DOI] [PubMed] [Google Scholar]
- Rosen R. C., Allen K. R., Ni X., Araujo A. B. (2011). Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function scale. European Urology, 60(5), 1010–1016. 10.1016/j.eururo.2011.07.053 [DOI] [PubMed] [Google Scholar]
- Salonia A., Bettocchi C., Boeri L., Capogrosso P., Carvalho J., Cilesiz N. C., Cocci A., Corona G., Dimitropoulos K., Gül M., Hatzichristodoulou G., Jones T. H., Kadioglu A., Martínez Salamanca J. I., Milenkovic U., Modgil V., Russo G. I., Serefoglu E. C., Tharakan T., . . . EAU Working Group on Male Sexual and Reproductive Health. (2021). European association of urology guidelines on sexual and reproductive health-2021 update: Male sexual dysfunction. European Urology, 80(3), 333–357. 10.1016/j.eururo.2021.06.007 [DOI] [PubMed] [Google Scholar]
- Shendy W. S., Elsoghier O. M., El Semary M. M., Ahmed A. A., Ali A. F., Saber-Khalaf M. (2021). Effect of low-intensity extracorporeal shock wave therapy on diabetic erectile dysfunction: Randomised control trial. Andrologia, 53(4), Article e13997. 10.1111/and.13997 [DOI] [PubMed] [Google Scholar]
- Shindel A. W., Kishore S., Lue T. F. (2008). Drugs designed to improve endothelial function: Effects on erectile dysfunction. Current Pharmaceutical Design, 14(35), 3758–3767. 10.2174/138161208786898752 [DOI] [PubMed] [Google Scholar]
- Sokolakis I., Dimitriadis F., Psalla D., Karakiulakis G., Kalyvianakis D., Hatzichristou D. (2019). Effects of low-intensity shock wave therapy (LiST) on the erectile tissue of naturally aged rats. International Journal of Impotence Research, 31(3), 162–169. 10.1038/s41443-018-0064-0 [DOI] [PubMed] [Google Scholar]
- Sramkova T., Motil I., Jarkovsky J., Sramkova K. (2020). Erectile dysfunction treatment using focused linear low-intensity extracorporeal shockwaves: Single-blind, sham-controlled, randomized clinical trial. Urologia Internationalis, 104(5–6), 417–424. 10.1159/000504788 [DOI] [PubMed] [Google Scholar]
- Srini V. S., Reddy R. K., Shultz T., Denes B. (2015). Low intensity extracorporeal shockwave therapy for erectile dysfunction: A study in an Indian population. The Canadian Journal of Urology, 22(1), 7614–7622. [PubMed] [Google Scholar]
- Sundaram S., Sellamuthu K., Nagavelu K., Suma H. R., Das A., Narayan R., Chakravortty D., Gopalan J., Eswarappa S. M. (2018). Stimulation of angiogenesis using single-pulse low-pressure shock wave treatment. Journal of Molecular Medicine (Berlin, Germany), 96(11), 1177–1187. 10.1007/s00109-018-1690-1 [DOI] [PubMed] [Google Scholar]
- Vardi Y., Appel B., Jacob G., Massarwi O., Gruenwald I. (2010). Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. European Urology, 58(2), 243–248. 10.1016/j.eururo.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Vardi Y., Appel B., Kilchevsky A., Gruenwald I. (2012). Does low intensity extracorporeal shock wave therapy have a physiological effect on erectile function? Short-term results of a randomized, double-blind, sham controlled study. Journal of Urology, 187(5), 1769–1775. 10.1016/j.juro.2011.12.117 [DOI] [PubMed] [Google Scholar]
- Vinay J., Moreno D., Rajmil O., Ruiz-Castañe E., Sanchez-Curbelo J. (2021). Penile low intensity shock wave treatment for PDE5I refractory erectile dysfunction: A randomized double-blind sham-controlled clinical trial. World Journal of Urology, 39(6), 2217–2222. 10.1007/s00345-020-03373-y [DOI] [PubMed] [Google Scholar]
- Wan X., Wang W., Liu J., Tong T. (2014). Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology, 14(1), Article 135. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C.-J., Huang H.-Y., Pai C.-H. (2002). Shock wave-enhanced neovascularization at the tendon-bone junction: An experiment in dogs. The Journal of Foot and Ankle Surgery: Official Publication of the American College of Foot and Ankle Surgeons, 41(1), 16–22. 10.1016/s1067-2516(02)80005-9 [DOI] [PubMed] [Google Scholar]
- Washington S. L., Shindel A. W. (2010). A once-daily dose of tadalafil for erectile dysfunction: Compliance and efficacy. Drug Design, Development and Therapy, 4, 159–171. 10.2147/dddt.s9067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaçake K. G. R., Carneiro F., Cury J., Lourenço R., Françolin P. C., Piovesan A. C., Srougi M., Nahas W. C., Antonopoulos I. M. (2019). Low-intensity shockwave therapy for erectile dysfunction in kidney transplant recipients. A prospective, randomized, double blinded, sham-controlled study with evaluation by penile Doppler ultrasonography. International Journal of Impotence Research, 31(3), 195–203. 10.1038/s41443-018-0062-2 [DOI] [PubMed] [Google Scholar]
- Yee C.-H., Chan E. S., Hou S. S.-M., Ng C.-F. (2014). Extracorporeal shockwave therapy in the treatment of erectile dysfunction: A prospective, randomized, double-blinded, placebo controlled study: Therapy for ED. International Journal of Urology, 21(10), 1041–1045. 10.1111/iju.12506 [DOI] [PubMed] [Google Scholar]
- Young Academic Urologists Men’s Health Group, Fode M., Hatzichristodoulou G., Serefoglu E. C., Verze P., Albersen M. (2017). Low-intensity shockwave therapy for erectile dysfunction: Is the evidence strong enough? Nature Reviews Urology, 14(10), 593–606. 10.1038/nrurol.2017.119 [DOI] [PubMed] [Google Scholar]
- Zewin T. S., El-Assmy A., Harraz A. M., Bazeed M., Shokeir A. A., Sheir K., Mosbah A. (2018). Efficacy and safety of low-intensity shock wave therapy in penile rehabilitation post nerve-sparing radical cystoprostatectomy: A randomized controlled trial. International Urology and Nephrology, 50(11), 2007–2014. 10.1007/s11255-018-1987-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-tif-1-jmh-10.1177_15579883221087532 for Systematic Review and Meta-Analysis of 16 Randomized Controlled Trials of Clinical Outcomes of Low-Intensity Extracorporeal Shock Wave Therapy in Treating Erectile Dysfunction by Huibao Yao, Xiaofeng Wang, Hongquan Liu, Fengze Sun, Gonglin Tang, Xingjun Bao, Jitao Wu, Zhongbao Zhou and Jian Ma in American Journal of Men’s Health
Supplemental material, sj-tif-2-jmh-10.1177_15579883221087532 for Systematic Review and Meta-Analysis of 16 Randomized Controlled Trials of Clinical Outcomes of Low-Intensity Extracorporeal Shock Wave Therapy in Treating Erectile Dysfunction by Huibao Yao, Xiaofeng Wang, Hongquan Liu, Fengze Sun, Gonglin Tang, Xingjun Bao, Jitao Wu, Zhongbao Zhou and Jian Ma in American Journal of Men’s Health
Supplemental material, sj-tif-3-jmh-10.1177_15579883221087532 for Systematic Review and Meta-Analysis of 16 Randomized Controlled Trials of Clinical Outcomes of Low-Intensity Extracorporeal Shock Wave Therapy in Treating Erectile Dysfunction by Huibao Yao, Xiaofeng Wang, Hongquan Liu, Fengze Sun, Gonglin Tang, Xingjun Bao, Jitao Wu, Zhongbao Zhou and Jian Ma in American Journal of Men’s Health