Abstract
Objective
Anecdotal evidence suggests that the training of young surgeons in Upper GI is not homogeneous across the world. This survey aimed to investigate the different training programs and the level of satisfaction of young surgeons with their surgical and scientific education pathway.
Design
A multiple choice and single best answer format questionnaire was sent to 36 Upper GI chairs from international referral centres and then forwarded to young surgeons (attending physician less than 40 years old). The same questionnaire containing 5 main topics (demographics, residency, fellowship, academic research and activities, manual skill improvement) was posted online on a Surveymonkey website.
Setting
San Luigi University Hospital, Orbassano (Turin), Italy; Tertiary University Hospital
Results
Fourteen replies were received from colleagues in 36 referral centres (39% response rate) and 65 voluntary answers from the survey monkey platform. During residency training only 43% of residents had a specific training in upper GI tract surgery, which was characterized by a small number of interventions performed both with trainer scrubbed and unscrubbed. Fellowship programmes were undertaken by 49% of participants and 64% spent this training period abroad. Operative experience was reported by nearly all respondents with only 27% performing > 10 gastrectomies and only 11% performing > 10 oesophagectomies with the trainer scrubbed. The majority attended less than 10 meetings (58%), and 70% of them published less than 5 papers.
Conclusions
The present survey reveals that the young surgeons of the 21st century face many hurdles during their surgical training. Overall, the surgical education settings are limited for both practical and scientific training for upper GI trainees. As a result it is not possible to train in upper GI surgery to a level of competent independent practice.
Keywords: upper GI training, surgical education, scientific training, residency, fellowship
Introduction
Centralisation of specialist surgery has gradually evolved partly reflecting the view that the outcome of surgery is dependent on surgeon experience [1]. In complex upper gastrointestinal (GI) surgery the impact of centralisation on postoperative outcomes, especially mortality, has been reported extensively in the literature. In 2012 a summary [2] from the Netherlands included twelve systematic reviews and four meta-analyses, describing the effect of hospital and/or surgeon volume on mortality. The majority of these reviews (>90%) showed a lower mortality in high-volume hospitals. Surgeon expertise and skills, availability of critical care units, 24/7 availability of interventional radiology, effective prevention and managing of complications and adequate patient selection were reported to positively influence postoperative outcomes.
In 2011 the Association of Upper Gastrointestinal Surgeons in the UK published a document describing the provision of services required for patients with upper gastrointestinal surgical disease [3]. This was an update of the document originally published in 1999 and reflected the huge changes in the intervening 12 years of the nature of the diseases seen, the requirements for patients and the new surgical procedures available. Since 2011, there has been increasing centralization of specialized upper GI surgical services in the UK with an increasing emphasis on the quality of the services provided. The volume – outcome relationship, which drove the initial centralization of upper GI cancer services 10 – 15 years ago, has created a similar concentration of surgery for benign upper GI disease. As a consequence, there is the risk of potential dilution of upper GI surgical skills in hospitals without specialist Upper GI teams which also has implications for emergency surgical services. This must be taken into account when considering the optimum site for location of non-cancer Upper GI specialist surgical services.
A consequence of centralisation is the varying effect on the quality of training provided to young surgeons. In specialist centres trainees would be exposed to the full range of patients and their management. However, in smaller units opportunities in upper GI surgery may be reduced if patients are referred to specialist centres. Any surgical trainee wishing to pursue a career in upper GI surgery must have a broad experience in all aspects of general and visceral surgery. This should be complimented by working in a multidisciplinary environment so that the trainee can appreciate the contribution of medical and clinical oncology to treatment planning. In addition, trainees should develop a career long interest in the basic and applied science of upper GI cancer with a commitment to clinical audit, service improvement and research trials. Applying this experience is key to being able to take on the safe management of patients undergoing the full spectrum of complex treatments for oesophageal and gastric cancer.
Anecdotal evidence suggests that the training of young surgeons in Upper GI is not homogeneous across the world and that general surgery residency programs mostly from the west are deficient in delivering specialization pathways [4–12]. This survey aimed to investigate the different training programs and the level of satisfaction of young surgeons with their surgical and scientific education pathway.
Methods
Survey design.
We developed an international survey to investigate the training pathway of young surgeons (attending physician less than 40 years-old) in upper GI surgery around the world.
This survey was designed by a small focus group (one expert surgeon (MD) and one PhD student (RR)) and validated by a qualified upper GI surgical oncologist (WA) to assess its quality. Subsequently it has been shared with the Italian Group Research of Gastric Cancer (GIRCG). The basic instrument for the survey was a combined multiple choice and single best answer format questionnaire. Participation in this poll was voluntary and young surgeons were allowed to choose anonymity if they preferred. A completed response was considered as consent to participate.
In brief, the questionnaire included five topics:
Topic 1- Demographics of participants: name, nationality, age, gender and name of institution.
Topic 2- Residency period and institutional volume: This topic was dedicated to investigate the residency training program of each participant’s institution. The items were: residency period duration, upper GI disease volume/year of the centre, type of surgical approach performed in the centre (open/laparoscopic/robotic), number of gastrectomies, oesophagectomies and Upper GI functional procedures attended as an observer, assisted and performed both with trainer scrubbed and unscrubbed and finally grade of participant’s satisfaction related to residency training program.
Topic 3- Fellowship period and institutional volume: This topic investigated the fellowship/training program of each participant’s institution. The items requested included the same as in the residency survey but also recorded the country and institution where the fellowship was conducted.
Topic 4- Academic research and activities: This focused on the scientific/academic experience of each participant. This included the number of meetings and workshops attended, the number of oral and poster presentations, the number of publications produced as well as additional academic degrees obtained (Doctor of Philosophy, Postgraduate Masters and other courses).
Topic 5- Manual skill improvement: This topic evaluated the participants’ involvement in any surgical practical courses including the number of cadaver and/or simulation labs attended, the type of minimally invasive technique performed during the simulation labs and number of hours spent in those labs.
Survey dissemination:
The questionnaire was forwarded worldwide to young surgeons from 36 referral centres.
Furthermore, the same questionnaire was posted online on a survey monkey website.
Statistical analysis
Continuous variables were analysed using mean and standard deviations (SD), whereas categorical variables were analysed using frequencies and percentages.
Results
Between September 2018 and March 2019, 14 replies were received from colleagues in 36 referral centres following the initial circulation of the survey, a response rate of 39% (figure 1). Subsequently, 65 answers were received from 65 voluntary participants through an electronic application on the survey monkey platform between March 2019 and June 2020. Two thirds of the participants were from European Institutions with the remainder from Asia, South, Central and North America. The mean participants’ age was 35.1 years ± 4.92, with approximately 75% being male. The majority of trainees did their residency in mid to high volume upper GI institutions. (Table 1).
Figure 1.
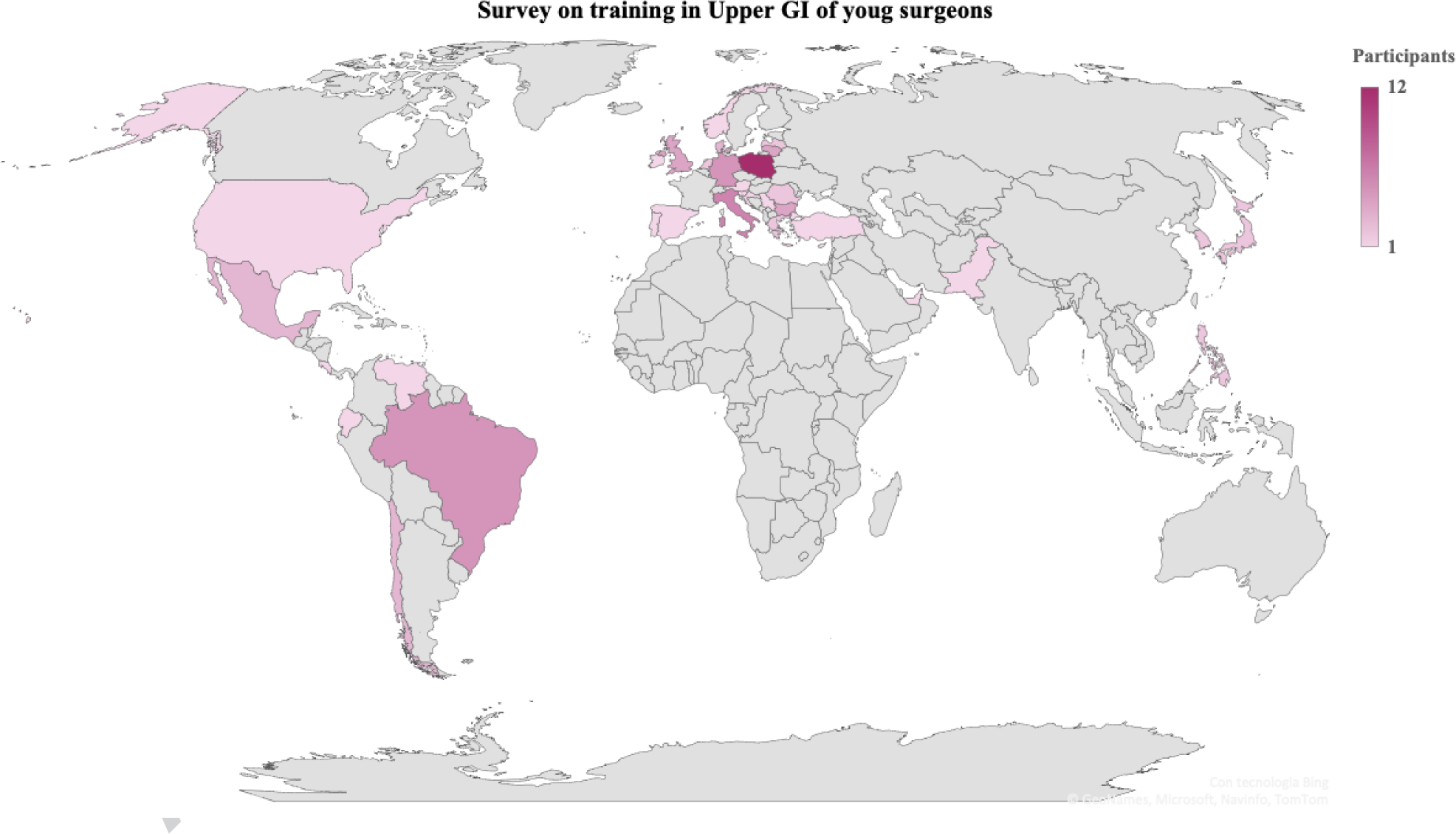
Survey on training in Upper GI of young surgeons: participants world map.
Table 1.
Demographics.
| PARTICIPANTS | nr | % |
|---|---|---|
| Age (years) | ||
| Mean ±SD | 35.15 ± 4.92 | |
| Median | 35.0 | |
| Gender | ||
| Male | 59 | 74.68 |
| Skipped answer | 1 | |
| COUNTRIES | ||
| Africa | 0 | 0 |
| Asia (Japan, South Korea, Emirates, Philippines, Pakistan) | 9 | 11.84 |
| North America (Canada, USA) | 3 | 3.95 |
| Central America (Ecuador, Mexico) | 3 | 3.95 |
| South America (Venezuela, Chile, Brazil) | 10 | 13.16 |
| Europe (Austria, United Kingdom, Bulgaria, Croatia, Germany, Greek, Ireland, Italy, Latvia, Lithuanian, Poland, Portugal, Romania, Turkey, Serbia, Slovenia, Spain) | 54 | 68.35 |
| Total | 79 | 100 |
Nr: Number; SD: Standard Deviation.
The duration of the residency period, the annual volume of upper GI disease at each centre, the type of surgical approach performed (open, laparoscopic and robotic) and the number of procedures attended as an observer or assisted during the residency programme are shown in Table 2 and Table 3. Almost all (95%) respondents received their training during a general surgery residency programme. During this training only 43% of residents had a specific training in upper GI tract surgery. The mean time of this specialized education period was 16.77 months ± 17.35.
Table 2.
Residency period’s characteristics
| Residency period duration | Nr years | |||
| Mean ±SD | 5.44 ± 1.64 | |||
| Median | 6 | |||
| General surgery residency | Nr trainees (%) | |||
| Yes | 75 (94.94) | |||
| Specific and official training period in upper GI | Nr trainees (%) | |||
| Yes | 34 (43,04) | |||
| Mean ±SD (months) | 16.77 ±17.35 | |||
| Type of approach in residency centers | Nr centers | |||
| Laparoscopic | 33 (41.77) | |||
| Robotic | 8 (10.12) | |||
| Open | 38 (48.10) | |||
| Level of Satisfaction | Nr trainees (%) | |||
| Negative | 28 (35.44) | |||
| Sufficient | 27 (34.17) | |||
| Good | 20 (25.31) | |||
| Optimal | 4 (5.06) | |||
| Centers volumes | Gastric resections performed N° (%) | Esophageal resections performed N° (%) | Functional interventions performed N° (%) | |
| Low Volumes (<20 patients treated/year) | 18 (22.78) | 44 (55.69) | 24 (30.37) | |
| Mid-High Volumes (21–100 patients treated/year) | 48 (60.75) | 32 (40.50) | 47 (59.49) | |
| Very High Volumes (>101 patients treated/year) | 13 (16.45) | 3 (3.79) | 8 (10.12) | |
Nr: Number; SD: Standard Deviation.
Table 3.
Number of interventions observed, assisted and performed during residency period.
| Gastric resections Nr trainees (%) | Esophageal resections Nr trainees (%) | Functional interventions Nr trainees (%) | ||||
|---|---|---|---|---|---|---|
| Nr of interventions observed | ||||||
| <20 | 34 (43.03) | 59 (74.68) | 41 (51.89) | |||
| >20 | 17 (21.51) | 16 (20.25) | 15 (18.98) | |||
| >50 | 17 (21.51) | 4 (5.06) | 18 (22.78) | |||
| >100 | 11 (13.92) | 0 | 5 (6.32) | |||
| Skipped answer | 0 | 0 | 0 | |||
| Nr of interventions assisted | ||||||
| <20 | 17 (21.79) | 49 (62.02) | 34 (43.03) | |||
| >20 | 24 (30.76) | 18 (22.78) | 17 (21.51) | |||
| >50 | 20 (25.64) | 8 (10.12) | 18 (22.78) | |||
| >100 | 17 (21.79) | 4 (5.06) | 10 (12.65) | |||
| Skipped answer | 1 | 0 | 0 | |||
| Performed with trainer scrubbed | Performed with trainer unscrubbed | Performed with trainer scrubbed | Performed with trainer unscrubbed | Performed with trainer scrubbed | Performed with trainer unscrubbed | |
| Nr of interventions performed | ||||||
| 0 | 21 (26.58) | 51 (68.92) | 52 (65.82) | 66 (88) | 34 (43.03) | 62 (82.67) |
| <5 | 23 (29.11) | 14 (18.92) | 18 (22.78) | 8 (10.67) | 22 (27.84) | 5 (6.67) |
| <10 | 14 (17.72) | 3 (4.05) | 2 (2.53) | 1 (1.33) | 6 (7.59) | 2 (2.67) |
| >10 | 7 (8.86) | 5 (6.76) | 4 (5.06) | 0 | 8 (10.12) | 3 (4) |
| >20 | 11 (13.92) | 0 | 0 | 0 | 3 (3.79) | 1 (1.33) |
| >50 | 3 (3.79) | 1 (1.35) | 3 (3.79) | 0 | 6 (7.59) | 2 (2.67) |
| Skipped answer | 0 | 5 | 0 | 4 | 0 | 4 |
Nr: Number
Overall, residency was characterized by a small number of interventions performed both with trainer scrubbed and unscrubbed; the majority of participants did less than five of all types of upper GI procedures. Experience of oesophageal surgery was limited with 75% observing < 20 procedures and 62% assisting in < 20 procedures. Rates for gastrectomy were better with 43% observing < 20 and 22% assisting in < 20 procedures. Almost half of surgeries performed were done with an open approach but the number of centres where laparoscopic and robotic approach was proposed is increasing. Only 30% of trainees described their residency training pathway as good or optimal. Analysis of overall satisfaction showed 35% were not satisfied with their training, and 34% described their education course as just sufficient.
During their residency, surgeons from Asia have observed and assisted more esophagectomies and gastrectomies with respect to their colleagues from Europe and America, while those from South America have performed more procedures, with or without a trainer scrubbed, with respect to the others.
For those undertaking specific fellowship programmes details of the duration, centre annual volume, type of surgical approach performed in the centre (open, laparoscopic and robotic), number of procedures attended as an observer or assisted and number of procedures performed with the trainer either scrubbed or unscrubbed are shown in Table 4 and Table 5.
Table 4.
Fellowship period’s characteristics
| Nr trainees (%) | |||
| Fellowship | |||
| Yes | 39 (49.36) | ||
| Abroad | 25 (64.10) | ||
| At home | 14 (35.89) | ||
| Countries | |||
| Belgium | 1 (4) | ||
| China | 1 (4) | ||
| Germany | 0 | ||
| Ireland | 1 (4) | ||
| Italy | 1 (4) | ||
| Japan | 1 | ||
| Saudi Arabia | 0 | ||
| Singapore | 1 (4) | ||
| South Korea | 7 (28) | ||
| Spain | 2 (8) | ||
| The Netherlands | 1 (4) | ||
| United Kingdom | 5 (20) | ||
| Duration | |||
| <1 month | 4 (10,81) | ||
| ≥ 1 month | 3 (8,11) | ||
| ≥ 3 months | 2 (5,41) | ||
| ≥ 6 months | 7 (18,92) | ||
| ≥ 1 year | 7 (18,92) | ||
| ≥ 2 years | 14 (37,84) | ||
| Skipped answer | 2 | ||
| Minimally invasive surgery performed | |||
| Laparoscopic | 14 (37,84) | ||
| Robotic | 15 (40,54) | ||
| Open | 8 (21,62) | ||
| Skipped answer | 2 | ||
| Level of Satisfaction | |||
| Negative | 7 (17,95) | ||
| Sufficient | 10 (25,64) | ||
| Good | 13 (33,33) | ||
| Optimal | 9 (23,08) | ||
| Centers volumes | Gastric resections performed Nr (%) | Esophageal resections performed Nr (%) | Functional interventions performed Nr (%) |
| Low Volumes (<20 patients treated/year) | 7 (17,95) | 15 (39,47) | 18 (48,65) |
| Mid-High Volumes (21–100 patients treated/year) | 16 (41.02) | 16 (42.10) | 11 (29.72) |
| Very High Volumes (>101 patients treated/year) | 16 (41,03) | 7 (18,42) | 8 (21,62) |
| Skipped answer | 0 | 1 | 2 |
Nr: Number
Table 5.
Number of interventions observed, assisted and performed during fellowship period.
| Gastric resections Nr (%) | Esophageal resections Nr (%) | Functional interventions Nr (%) | ||||
|---|---|---|---|---|---|---|
| Nr of interventions observed | ||||||
| <20 | 15 (38,46) | 30 (76,92) | 28 (71,79) | |||
| >20 | 8 (20,51) | 6 (15,38) | 4 (10,26) | |||
| >50 | 9 (23,08) | 3 (7,69) | 5 (12,82) | |||
| >100 | 7 (17,95) | 0 | 2 (5,13) | |||
| Nr of interventions assisted | ||||||
| <20 | 11 (28,21) | 26 (66,67) | 24 (63,16) | |||
| >20 | 10 (25,64) | 4 (10,26) | 4 (10,53) | |||
| >50 | 8 (20,51) | 5 (12,82) | 3 (7,89) | |||
| >100 | 10 (25,64) | 4 (10,26) | 7 (18,42) | |||
| Skipped answer | 0 | 0 | 1 | |||
| Performed with trainer scrubbed | Performed with trainer unscrubbed | Performed with trainer scrubbed | Performed with trainer unscrubbed | Performed with trainer scrubbed | Performed with trainer unscrubbed | |
| Nr of interventions performed | ||||||
| 0 | 11 (29,73) | 25 (65,79) | 23 (60,53) | 31 (81,58) | 20 (52,63) | 25 (65,79) |
| <5 | 11 (29,73) | 7 (18,42) | 10 (26,32) | 5 (13,16) | 9 (23,68) | 6 (15,79) |
| <10 | 5 (13,51) | 2 (5,26) | 1 (2,63) | 2 (5,26) | 2 (5,26) | 2 (5,26) |
| >10 | 5 (13,51) | 3 (7,89) | 3 (7,89) | 0 | 3 (7,89) | 3 (7,89) |
| >20 | 3 (8,11) | 1 (2,63) | 1 (2,63) | 0 | 2 (5,26) | 0 |
| >50 | 2 (5,41) | 0 | 0 | 0 | 2 (5,26) | 2 (5,26) |
| Skipped answer | 2 | 1 | 1 | 1 | 1 | 1 |
Nr: Number
Fellowship programmes were undertaken by 49% of participants and 64% spent this training period abroad. The top 3 countries where the fellowship training was done are South Korea, United Kingdom and Spain. The duration of the fellowship was ≥ 6 months for 19%, 1 year for 19% and ≥ 2 years for 38%. The response rate for observation and assisting during fellowships was only 50% of all respondents but of these 77% observed less than 20 oesophageal resections and 38% observed less than 20 gastrectomies. Operative experience was reported by nearly all respondents with 27% performing > 10 gastrectomies and 11% performing > 10 oesophagectomies with the trainer scrubbed. Experience in functional procedures was similar with 18% performing 10 or more under appropriate supervision.
The academic experience of the respondents including the number of meetings and/or workshops attended, oral and poster presentations and publications is shown in Table 6. The majority attended less than 10 meetings (58%), with 66% presenting less than 10 oral presentations and 65% presenting less than 10 posters. In addition, 70% of trainees published less than 5 papers.
Table 6.
Academic research and activities
| Meetings and workshops attended Nr trainees (%) | Oral presentations Nr trainees (%) | Poster Presentations Nr trainees (%) | Scientific publications produced Nr trainees (%) | |
|---|---|---|---|---|
| Nr of activities | ||||
| <5 | 22 (30,14) | 30 (39,47) | 32 (42,67) | 47 (70,15) |
| >5 | 20 (27,40) | 20 (26,32) | 17 (22,67) | 9 (13,43) |
| >10 | 8 (10,96) | 17 (22,37) | 18 (24,00) | 11 (16,42) |
| >20 | 23 (31,51) | 9 (11,84) | 8 (10,67) | |
| Skipped answer | 6 | 3 | 4 | 12 |
| Nr trainees (%) | ||||
| PhD | ||||
| Yes | 26 (35,14) | |||
| Skipped answer | 5 | |||
| Postgraduate master | ||||
| Yes | 20 (27,40) | |||
| Skipped answer | 6 | |||
| Other courses | ||||
| Yes | 33 (44,59) | |||
| Skipped answer | 5 | |||
Nr: Number
The participants’ involvement in any surgical practical courses (number of cadaver and/or simulation labs attended, type of minimally invasive technique performed during the simulation labs and number of hours spent in those labs) is shown in Table 7. Approximately 44% attended cadaveric labs and 58% simulation labs which were mainly laparoscopic courses.
Table 7.
Manual skill improvement
| Nr trainees (%) | |
| Cadaver lab | |
| Yes | 34 ( 44,16) |
| Skipped answer | 2 |
| Number of cadaver labs attended Mean ± SD |
2.7 ± 3.56 |
| Simulation lab | |
| Yes | 44 ( 57,89) |
| Missing | 3 |
| Laparoscopic simulation lab | 43 ( 91,49) |
| Robotic simulation lab | 4 ( 8,51) |
| Number of hours spent in simulation
labs Mean ± SD |
183.2 ±301.86 |
Nr: Number; SD: Standard Deviation.
There were no substantial differences between surgeons from referral centers and voluntary responders through survey monkey website with respect to their surgical training, while the first were more frequently involved in scientific activities.
Discussion
This survey describes the current experience of trainees in upper GI surgery across the World. The results have been analysed as a whole rather than by individual countries or continents because of the small sample size. However the overall experience seems to be very limited. More than half of participants performed less than 5 upper GI surgical procedures both in their residency and fellowship periods. Trainees spend much of their time observing or assisting particularly in oesophageal resection and this appears to be similar in residency and fellowship programmes. It is possible that experience in fellowship programmes is lower as 40% of the trainees spent up to 6 months in the programme and this was often abroad when they may not have operating licences for the country they were visiting. Overall academic exposure is limited with approximately 40% of trainees completing less than 5 posters and oral presentations and 70% of them less than 5 scientific papers. In addition, more than 30% of young surgeons participated in more than 20 meetings and workshops.
Surgical training has gained far more attention over recent years with the Basic Science Committee of the Society of University Surgeons in 2019 describing a strategy to become a capable and successful surgeon-scientist [13]. The committee defined the surgeon-scientist as “an essential component of the field of academic surgery, contributing to the fundamental understanding of disease and the discovery of innovative therapies”. In the strategy the first year is called “getting started” with the main goal to acquire the essential skills of the basic and clinical sciences. During this year trainees should participate in many conferences and workshops to learn specific topics, to meet potential collaborators, to hear and participate in discussions on scientific issues. The authors however fully recognise the need for the surgical trainee to develop their craft skills; “ Nobody would expect the talented athlete to win any games simply by understanding that hitting and catching are important; it is assumed that effective training in the art of baseball is required.”
Worldwide there is an increasing demand for specialized surgeons, which is related to the ongoing process of centralization of Upper GI major diseases in Tier 3 Hospitals ( typically Teaching Hospitals or large Regional Hospitals). In Europe, The Netherlands and the U.K. have already completed this process and in these countries the rate between upper GI and general surgeons is strongly increasing particularly in centralized unit serving populations from 1 to 2,5 million. This centralization process has been completed since many decades in Asia, where major upper GI diseases are routinely referred to teaching university hospitals or large Regional facilities and treated only by specialized doctors [3]. All fully recognise that the knowledge, clinical and technical skills to be a safe and successful upper GI surgeon are complex, demanding and take many years to perfect. It would seem from this study that we have a long way to go before we can put trainees on a trajectory that by the end of the initial postgraduate training they are in a position to practice independently with appropriate senior support and mentorship. It is probably not possible to develop a training programme that is universally applicable because of the different health systems across the World as well as the variation in oesophageal and gastric cancer incidence and presentation particularly between the West and the Far East. Residency programmes and training curricula are variable but it would seem that most trainees do need to take a fellowship on completion of their residency to gain the more complex skills of upper GI cancer surgery. In the USA there are specific Surgical Oncology fellowship programmes based at the major academic cancer institutions which are carefully monitored by the Accreditation Council for General Medical Education (ACGME). These are restricted to an annual intake of post residency surgeons to meet the service needs of the major centres [14]. In the UK trainees complete a General Surgery programme with the option of developing a special interest in upper GI surgery. However operative experience is similar to that reported in this survey with upper GI trainees performing under appropriate supervision a mean of 16 gastrectomies (IQR 3–32) and 25 oesophagectomies (IQR 4–50) before completion of their training [15].
It is clear from the evidence of this study that the clinical and technical experience of trainees is limited although they do seem to be accessing academic and scientific opportunities. The learning curve for competence in upper GI surgical procedures is steep. In 2016 Kim [16] investigated learning curves for open gastrectomy with D2 lymphadenectomy for gastric cancer. In a retrospectively collected series of 3284 patients submitted to gastric resection with extended lymphadenectomy by nine surgeons the analysis of surgical and oncological outcomes demonstrated that a surgeon must complete at least 100 operations to achieve his best oncological outcomes in each stage. The advent of minimally invasive surgery has introduced a new learning approach particularly for oesophago-gastric junctional and cardia cancer. A recent article [17] retrospectively analysed data of 646 patients who underwent minimally invasive Ivor Lewis oesophagectomy for oesophageal cancer in 4 referral hospitals. The authors reported that after 119 procedures the anastomotic leakage rate was lowest.
This study shows that such experience is currently beyond the expectation of most trainees particularly in the West. Practical workshops, cadaver and other simulation labs are important adjuncts to acquire manual skills and to overcome hurdles in practicing live surgery. In the present sample only 50% of trainees attended a simulation or a cadaver lab so it would seem appropriate to invest resources in such facilities and to ensure trainees have access to them [18].
There is no doubt that observation and assisting has its merits but this should not detract from hands-on operating experience. Consideration should be given to breaking procedures up into components according to the technical skill of the trainee. For example, mobilisation of the stomach could be the first step in which to achieve competence before moving on to lymphadenectomy and eventually anastomosis in a gastrectomy. This would ensure with the trainer scrubbed there is minimal safety risk to the patient.
This approach needs to be supplemented by appropriate reflection and coaching by the trainer to ensure the trainee develops confidence in their own ability. This of course must take place in an environment of trust and support which enhances a satisfactory experience for the trainee. Unfortunately there remain examples of limited support [19], which have been identified in this study with 35% dissatisfied with their training. The problem of training and job satisfaction of young surgeons is of such importance that a recent Comparative Study from US concluded that “ …the incorporation of wellness programs into surgical residencies is essential to the professional development of young surgeons to cultivate healthy lasting habits for a well-balanced career and life” [20]. The current generation of surgical trainees has a different outlook on their career progression to previous generations and this must be taken into consideration. The previous era of many long hours of training and service provision has passed and educators and trainers need to find new ways to positively develop the surgeon of the future. The move to competence based training and development needs to be embraced and to take over from the time based approach. Trainees do learn at different speeds and allowance needs to be made for this individual variation. However it is important to maintain the experiential side of training as this gives the trainee exposure to the many different presentations of clinical problems which are particularly common in upper GI surgery.
As in other areas of surgical practice it is essential that the trainee keeps up to date with developments in upper GI surgery and is able to contribute from their own experience particularly in the form of publications. Continuous updates on multidisciplinary guidelines and technical innovations, together with the awareness of the role of basic and applied research are essential for a young surgeon’s professional development. Data from our survey documented a high rate of trainees’ participation in meetings and workshops as observer. However their presentation and publication record was limited and they have very rarely acted as faculty in meetings or workshops. In some countries with limited academic facilities the scientific production and involvement in clinical and laboratory research is not considered as a means to evaluate candidates for a surgical service appointment. However departments where such contribution is encouraged are those to which trainees wish to go not only for their own domestic residency programme but also for an international visit for a fellowship. There is without doubt a responsibility for those leading academic units and clinical services to ensure they encourage their younger colleagues with advice and mentorship to develop professionally and enhance their job and training satisfaction.
This survey has some limitations. First of all, the examined sample size is small and some nations have a low or no response rate. Therefore, these results are not generalizable because the respondents differ significantly from the study population as a whole, although some studies supported the validity of low-response rate surveys [21]. Second, although we piloted the survey questions, the content and design may be sources of bias. A multiple-choice format with one best answer precluded feedback or expansion of young surgeons’ concerns outside the question topics.
Although the present survey permitted the responders to be anonymous, the majority of participants selected to disclose their identities and training programs. We understand that this could potentially result in trainees being less or more critical in their assessment, but we noticed that several participants chose anonymity especially in the first part of survey circulation where questionnaires were forwarded to trainees by their chief or senior colleagues.
Conclusions
The present survey reveals that the young surgeons of the 21st century face many hurdles during their surgical training. Overall, the surgical education settings are limited for both practical and scientific training for upper GI trainees. As a result it is not possible to train in upper GI surgery to a level of competent independent practice combining current residency and fellowship programmes. In addition, young surgeons are not satisfied with their experience. There is therefore a need to address the issues identified in this survey in order to ensure high-quality training in Upper GI surgery and to ensure the development of safe and competent surgeons for the future.
Highlights.
A multiple choice questionnaire was sent to young surgeons from 36 upper GI international centers
Demographics, residency, fellowship, academic research and manual skill were investigated
The survey reveals that upper GI young surgeons face many hurdles during their surgical training
Overall, the surgical education settings are limited for both practical and scientific training
Funding:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Declarations:
Conflicts of interest/Competing interests: The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Begg CB, Cramer LD, Hoskins WJ, Brennan MF (1998) Impact of hospital volume on operative mortality for major cancer surgery. JAMA 280:1747–51. 10.1001/jama.280.20.1747 [DOI] [PubMed] [Google Scholar]
- 2.Tol JAMG, Van Gulik TM, Busch ORC, Gouma DJ (2012) Centralization of Highly Complex Low-Volume Procedures in Upper Gastrointestinal Surgery. A Summary of Systematic Reviews and Meta-Analyses. Dig Surg 29:374–383. 10.1159/000343929 [DOI] [PubMed] [Google Scholar]
- 3.(2011) Abstracts of the Annual Scientific Meeting of the Association of Upper Gastrointestinal Surgeons for Great Britain and Ireland. September 15–16, 2011. Belfast, United Kingdom. Br J Surg 98 Suppl 7:1–55 [PubMed] [Google Scholar]
- 4.Montorsi M, De Manzini N (2019) The General Surgery Residency Program in Italy: a changing scenario. Updates Surg. 71:195–196 [DOI] [PubMed] [Google Scholar]
- 5.Cogbill TH, Klingensmith ME, Jones AT, et al. (2015) Resident Preparation for Careers in General Surgery: A Survey of Program Directors. In: Journal of Surgical Education. Elsevier Inc., pp e251–e257 [DOI] [PubMed] [Google Scholar]
- 6.Brochu A, Aggarwal R (2018) Research during general surgery residency: a Web-based review of opportunities, structure and outputs. J Surg Res 223:149–154. 10.1016/j.jss.2017.10.024 [DOI] [PubMed] [Google Scholar]
- 7.General Surgery Training Program | Surgery at Johns Hopkins Medicine. https://www.hopkinsmedicine.org/surgery/education/residency/general-surgery/. Accessed 5 Dec 2020
- 8.Surgical Residency Program. https://www.massgeneral.org/surgery/education-and-training/surgical-residency-program. Accessed 5 Dec 2020
- 9.Kim J-P (2004) Surgery in Korea. Arch Surg 139:336–340. 10.1001/archsurg.139.3.336 [DOI] [PubMed] [Google Scholar]
- 10.Poudel S, Hirano S, Kurashima Y, et al. (2019) A snapshot of surgical resident training in Japan: results of a national-level needs assessment survey. Surg Today 49:870–876. 10.1007/s00595-019-01819-4 [DOI] [PubMed] [Google Scholar]
- 11.Wijnhoven BPL (2019) Surgical training and research in the Netherlands. Keio J Med 68:68. 10.2302/kjm.68-005-ABST [DOI] [PubMed] [Google Scholar]
- 12.Greensmith M, Cho J, Hargest R (2016) Changes in surgical training opportunities in Britain and South Africa. Int. J. Surg 25:76–81 [DOI] [PubMed] [Google Scholar]
- 13.Goldstein AM, Blair AB, Keswani SG, et al. (2019) A Roadmap for Aspiring Surgeon-Scientists in Today’s Healthcare Environment. Ann. Surg. 269:66–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qadan M, Davies AR, Polk HC, et al. (2018) Cancer care in the developed world: A comparison of surgical oncology training programs. Am J Surg 215:1–7. 10.1016/j.amjsurg.2017.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allum W, Hornby S, Khera G, et al. (2013) General Surgery Logbook Survey. Bull R Coll Surg Engl 95:1–6. 10.1308/147363513x13500508920095 [DOI] [Google Scholar]
- 16.Kim CY, Nam BH, Cho GS, et al. (2016) Learning curve for gastric cancer surgery based on actual survival. Gastric Cancer 19:631–638. 10.1007/s10120-015-0477-0 [DOI] [PubMed] [Google Scholar]
- 17.Van Workum F, Stenstra MHBC, Berkelmans GHK, et al. (2019) Learning Curve and Associated Morbidity of Minimally Invasive Esophagectomy: A Retrospective Multicenter Study. Ann Surg 269:88–94. 10.1097/SLA.0000000000002469 [DOI] [PubMed] [Google Scholar]
- 18.Lee GI, Lee MR (2018) Can a virtual reality surgical simulation training provide a self-driven and mentor-free skills learning? Investigation of the practical influence of the performance metrics from the virtual reality robotic surgery simulator on the skill learning and associated cognitive workloads. Surg Endosc 32:62–72. 10.1007/s00464-017-5634-6 [DOI] [PubMed] [Google Scholar]
- 19.O’Sullivan KE, Byrne JS, Walsh TN (2013) Basic surgical training in Ireland: The impact of operative experience, training program allocation and mentorship on trainee satisfaction. Ir J Med Sci 182:687–692. 10.1007/s11845-013-0956-4 [DOI] [PubMed] [Google Scholar]
- 20.Trends in Surgeon Wellness (Take a Sad Song and Make It Better): A Comparison of Surgical Residents, Fellows, and Attendings - PubMed. https://pubmed-ncbi-nlm-nihgov.bibliopass.unito.it/31267897/. Accessed 26 Jun 2020 [PubMed]
- 21.Hikmet N, Chen SK (2003) An investigation into low mail survey response rates of information technology users in health care organizations. Int J Med Inform 72:29–34. 10.1016/j.ijmedinf.2003.09.002 [DOI] [PubMed] [Google Scholar]


