Abstract
One in three Americans report experiencing loneliness in everyday life, a number that has grown exponentially over the last few decades. As we respond to the SARS-COV2 pandemic with quarantine and social distancing, social isolation and feelings of loneliness are increasing among people of all ages. This presents as an opportune time to recognize the public health impact of these important psychosocial determinants. Loneliness and social isolation are associated with a higher incidence of CVD, higher healthcare utilization and worse outcomes even after controlling for conventional risk factors of CVD. In this review, we discuss loneliness and social isolation as determinants of cardiovascular outcomes, the pathophysiology of this association, and its implications in clinical practice. We discuss some of the shortcomings in the assessment of loneliness and social isolation while identifying the most commonly used rating scales for the same. Finally, we suggest modifications to interventions for loneliness and social isolation during the COVID-19 pandemic.
Keywords: Loneliness, social isolation, cardiovascular outcomes, psychosocial risk factors, COVID-19, pathophysiology
1. INTRODUCTION
Cardiovascular diseases (CVD) continue to be the leading cause of death in the United States, and mitigation of risk factors has been the mainstay in improving CVD outcomes. CVD cost about $351 billion in terms of healthcare expenditure annually and claim more than 650,000 lives [1]. Conventional risk factors such as dyslipidemia, high blood pressure, smoking, high fasting blood glucose, and high body mass index are the major contributors to the global CVD burden [2]. Intensive blood pressure control, tight control of low-density lipoprotein (LDL) level, and advocating smoking cessation are now considered the standard of care in the treatment as well as prevention of CVD [3, 4]. While the emphasis on the management of these conventional risk factors has led to a decline in the number of deaths from CVD by 12.5% over the last decade, this decline has plateaued, implying a limitation in predicting CVD outcomes based purely on the conventional risk factors [2, 5, 6]. Further, these risk factors do not explain the CVD risk in all patients. Thus, the search for other modifiable risk factors continues.
2. PSYCHOSOCIAL STRESS AND CVD
The next frontier for CVD risk factor reduction is focused on psychological health. Depression and anxiety play a critical role in the incidence and outcomes of CVD beyond that explained by conventional risk factors. One of the early studies found that the risk of incident coronary heart disease (CHD) was over 70% higher in depressed individuals relative to non-depressed individuals [7]. A number of meta-analyses reported that clinical depression or depressive symptoms increased the risk of CHD from 30% [8] to 60% [9-13]. The risk continued to be significant even after adjustment for other conventional risk factors, particularly cigarette smoking and physical inactivity [12], establishing depression as an independent risk factor for incident CHD as well as increased cardiovascular mortality [14, 15]. Furthermore, the increase in the risk of developing CVD is correlated with both the severity and recurrence of depression [16].
Similarly, anxiety disorders have been linked with higher incidence and poor outcomes of CVD, independent of conventional risk factors [17, 18]. Association between CVD and other psychosocial disorders, such as specific phobia, panic disorder, post-traumatic stress disorder and alcohol use disorder, unveil the breadth of psychopathology’s impact on CVD outcomes, prompting clinicians to explore other psychosocial risk factors [19]. Loneliness and social isolation are important determinants that have recently received growing attention as modifiable predictors of CVD risk.
3. LONELINESS AND SOCIAL ISOLATION: IMPACT ON HEALTH OUTCOMES
Loneliness and social isolation have reached epidemic proportions and are increasingly linked with poor health outcomes. Loneliness is a subjective feeling of unhappiness or dissatisfaction which stems from being alone. Social isolation is a complete or partial lack of contact between an individual and the society. While the two terms differ in definition, they are often used interchangeably in the literature. A significant association has been noticed between loneliness, social isolation and all-cause mortality [20-23]. A 2015 meta-analysis of 70 relevant studies found that social isolation, loneliness, and living alone corresponded to an average increase in mortality by 29%, 26%, and 32%, respectively [24]. When compared to conventional risk factors for mortality, this increased risk was greater than that from light smoking (less than 15 cigarettes per day), obesity, and physical inactivity [23]. On the other hand, strong social relationships can increase the likelihood of survival by as much as 50% [23]. In this review, we discuss the prevalence of social isolation and loneliness in the US and its impact specifically on the pathogenesis of CVD and its outcome.
4. LONELINESS AND SOCIAL ISOLATION: PREVALENCE BEFORE AND DURING COVID-19
The prevalence of loneliness amongst adults in the US is thought to have doubled over the last decade, and about a third of the population reports feeling lonely according to recent estimates [25, 26]. The prevalence is as high as 49% in some groups [27]. While conventionally thought an affliction of old-age, the prevalence is seen to be growing amongst the younger age groups. In a multi-state study in 2017, 33% of respondents aged <25 years reported loneliness compared to 11% of those aged >65 years [28].
The prevalence of loneliness and social isolation has more recently been impacted by the onslaught of the COVID-19 pandemic and the extensive changes in lifestyle brought about by social distancing and self-isolation measures. Observations from the SARS outbreak of 2003 predict an ominous trend of adverse mental health outcomes [29]. In a survey, all participants who were placed in quarantine in 2003 reported a sense of isolation, particularly due to lack of physical contact with family members, and long-term consequences included reduced direct contact with other people and avoidance of public places [30, 31]. In the current pandemic, with >90% of the population following “sheltering-in- place” orders, the rates of loneliness are as high as 43.8%, which is significantly higher than the previously reported prevalence of 38% [32]. Some populations are particularly hard hit by COVID-related loneliness and social isolation, such as college students and those residing in nursing homes [33]. In a survey of Chinese college students (N=992), COVID-related isolation worsened a myriad of psychological symptoms, including depression, fear, hypochondria, and obsessive-compulsive disorder [34]. Most nursing homes have essentially been on lockdown due to the increased risk of contagion during the current pandemic. There have been reports of many residents stopping to eat and giving up without family visits, making it imperative to focus on the consequences of this burning issue at hand.
5. LONELINESS AND SOCIAL ISOLATION: RELATIONSHIP WITH CVD
Loneliness is known to play an independent and critical role in the incidence, healthcare utilization, and outcomes of CVD.
5.1. Incidence
A meta-analysis investigating the incidence of CHD and stroke in high-income countries concluded that poor social relationships increased the risk of incident CHD by 29% and that of stroke by 32% [35]. Table 1 summarizes some representative studies investigating the incidence of CHD, MI, and death due to CHD in an otherwise healthy population [36-44].
Table 1.
Studies investigating the incidence of coronary heart disease (CHD) and myocardial infarction (MI) or death due to CHD in populations without a known history of CHD.
| Study (First Author, Year) | Study Focus | Sample Size (n) | Mean Age or Age Range (YYears)a | Genderb | Determinant Measured (Measure used)c | Prevalence of Determinantd |
|---|---|---|---|---|---|---|
| Hedblad, 1992 | Incidence | 394 | 68 | M | Lack of emotional support | - |
| Kawachi, 1996 | Outcome | 32,624 | 42-77 | M | Social isolation (Berkman-Syme SNI) |
5.8% (SNI I) |
| Eng, 2002 | Outcome | 28,369 | 55 | M | Social isolation (Berkman-Syme SNI) |
30% (SNI I & II) |
| Strodl, 2003 | Incidence | 10,432 | 70-75 | F | Low-fair social support (Duke Social Support Index | 15% |
| Rosengren, 2004 | Incidence | 741 | 50 | M | Low social integration and low emotional attachment | Low social integration 21.6% Low emotional attachment 23% |
| Barefoot, 2005 | Incidence | 9,573 | 57.5 | M & F (56% F) |
Social isolation (number and frequency of close contacts) | - |
| Lena André-Petersson, 2006 | Incidence | 414 | 68 | M | Unsatisfactory social support | 34.1% |
| Thurston, 2009 | Incidence | 2616 | 44 | M & F (56% F) |
Loneliness | - |
| Gafarov, 2013 | Incidence | 870 | 25-64 | F | Social isolation (Berkman-Syne ICC & SNI) |
57.1 (Low ICC) 77.1% (SNI I & II) |
Abbreviations: a: Age-range is provided if the mean population age was not measured.; b: Most studies either included males (M) or females (F). For studies that included both genders, the percentage of females has been noted; c: Determinant measured is the psychosocial factor studied. The measurement instrument used is mentioned for studies using a validated tool: Berkman-Syme Social Network Index (SNI) and Duke Social Support Index; d: Percentage of population that reported the presence of determinant; e: Relative risk (RR) along with the 95% confidence interval (CI).
5.2. Health-Care Utilization
Loneliness and social isolation also lead to greater health-care utilization amongst patients with cardiovascular disease. In a study of 1,681 respondents with heart failure, the group that experienced a higher degree of social isolation was reported to have 26% more out-patient and 57% more emergency room visits when compared to those with low levels of social isolation. The rate of hospitalization was 68% more in subjects with a high degree of social isolation than in those with a low degree of social isolation [45].
5.3. Outcomes
In addition to increased incidence and higher healthcare utilization, patients lacking social support have worse outcomes after cardiovascular events [46]. Berkman et al. observed that lack of emotional support after MI increased the odds of 6-month mortality by 2.9 times after controlling for severity of MI, comorbidities, risk factors such as smoking and hypertension, and sociodemographic factors [47]. In a study of 1,290 patients undergoing coronary artery bypass grafting, the ratings on the statement “I feel lonely” predicted survival at 30 days and 5 years after surgery, even after controlling for preoperative factors known to increase mortality [48].
6. GAPS IN LITERATURE
There are some limitations when considering loneliness and social isolation as risk factors for CVD. Most of the studies in the field are descriptive and observational analysis. While a significant association is seen between CVD and an umbrella of terms related to social support and social isolation, lack of a single validated measure is a major problem precluding a systematic analysis. Some studies have employed previously tested tools like the Berkman-Syme Social Network Index, which measures social integration, and Duke Social Support Index, which measures social interaction and subjective support [49, 50]. Similarly, several outcome measures are used for social isolation; the UCLA-Loneliness score has been used in multiple national and international reports [51]. However, most studies related to CVD outcomes have implemented independent questionnaires. The variability in determinants studied poses a problem in comparison and reproducibility of results, weakening the strength of association.
There has also been some concern of bias due to confounding of conventional risk factors, as the studies exploring the association of loneliness and social isolation with incident CHD have largely included unadjusted analysis. In a large cohort study from the UK, the risk of MI and stroke associated with social isolation was attenuated by 84% and 83%, respectively, when adjusted for other risk factors [46]. However, in more recent cohort studies, the association of loneliness with the difference in health determinants has been inconsistent [52, 53]. The effect of loneliness and social isolation on health behaviours and consequently worse health outcomes needs to be further explored with adequately powered studies before these can be ascertained to be independent CVD risk factors.
7. MECHANISMS LINKING LONELINESS AND SOCIAL ISOLATION WITH CVD
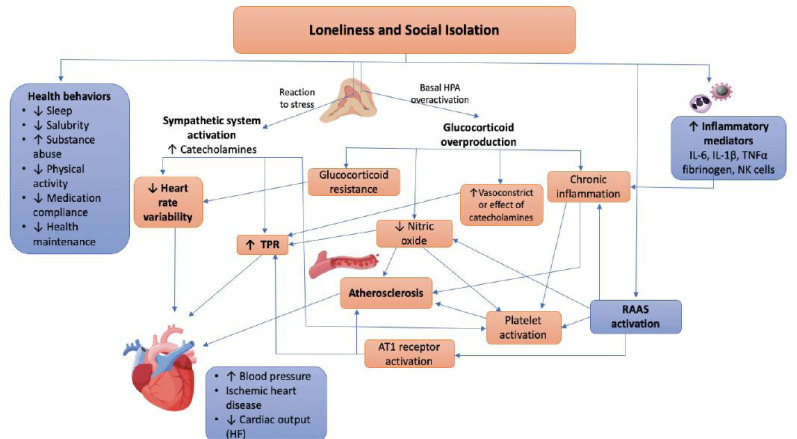
Several mechanisms have been proposed linking loneliness and social isolation to poor cardiovascular outcomes. Increased stress reactivity, autonomic dysregulation, and exaggerated inflammatory response have been implicated as important pathways [22, 52-54]. A pathophysiological model connecting loneliness and social isolation to atherogenesis and the development of CVD is summarized in (Fig. 1).
Fig. (1).
Hypothesized model of loneliness and social isolation affecting cardiovascular outcomes. Loneliness and social isolation can impact health-related behaviors. It also leads to an exaggerated autonomic response to stress and sympathetic nervous system hyperactivity. These conditions are associated with increased total peripheral resistance (TPR) and reduced heart rate variability (HRV), contributing to hypertension, ischemic heart disease and poor cardiac output. In animal models, social isolation has been associated with higher resting glucocorticoid levels from overactivation of the hypothalamic-pituitary-axis (HPA), leading to chronic inflammation and glucocorticoid resistance (receptor desensitization). It also increases the vasoconstrictive effects of catecholamines and decreases nitric oxide (NO) synthesis at the level of endothelial cells. There is evidence linking renin-angiotensin-aldosterone-system (RAAS) to social isolation, which in turn contributes to increased TPR, platelet activation and endothelial dysfunction. Loneliness has also been associated with increased circulating natural killer (NK) cells, fibrinogen and other inflammatory mediators, e.g. interleukin-6 (IL-6), IL-1β and tumor necrosis factor-alpha (TNF-alpha). This may be due to increased glucocorticoid levels or direct action on myelopoiesis. This state of chronic inflammation, along with endothelial dysfunction and platelet activation, leads to accelerated atherosclerosis. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
Lonely individuals are observed to have higher total peripheral resistance and these changes can be seen beginning early in life [52, 53]. A study by Cacioppo et al. comprising 89 undergraduate students with a mean age of 19.26 years, found that lonely young adults have higher total peripheral resistance in response to psychological stressors as compared to their non-lonely counterparts [53]. In the same study, non-lonely participants had a greater cardiac output than lonely participants. In the second part of the study, similar responses were observed in older adults (mean age 65 years) in addition to the observation that age-related increase in resting systolic blood pressure was higher in lonely adults as compared to non-lonely adults. A similar pattern was also seen in heart rate variability which is measured by the variation in beat-to-beat interval and is mediated by the autonomic nervous system. Low heart rate variability is associated with increased risk of CHD and cardiovascular mortality [55]. Lonely individuals tend to have lower heart rate variability in response to stress. Gouin et al. investigated the effect of social integration on heart rate in 60 students who were recruited to the study within 22 days of moving to a new country and found that lower levels of social integration at 5 months after recruitment were associated with higher resting heart rate and lower heart rate variability [56].
The role of hypothalamic-pituitary axis is somewhat more controversial. Persistent activation of the hypothalamic-pituitary axis was noted to be associated with loneliness in animal studies, leading to higher basal levels of corticosteroids and decreased glucocorticoid receptor sensitivity [22]. However, studies in humans do not show a significantly high cortisol level amongst lonely responders [53, 54]. Glucocorticoid resistance leading to chronic stress can mediate inflammation, which is an important part of the pathogenesis of atherosclerosis. Glucocorticoids also potentiate the vasoconstrictive effects of catecholamines [57]. In endothelial cells, glucocorticoids decrease nitric oxide (NO) through action on endothelial NO synthase [58]. More human studies with sufficient power are needed before we can accept or refute hypothalamic-pituitary axis overactivation as a plausible link between loneliness and CVD. There is evidence linking the renin-angiotensin-aldosterone system to social isolation, but further investigation is needed in the area as well [59]. In lonely individuals, levels of other inflammatory mediators including interleukin-6, tumor necrosis factor alpha, interleukin-1 beta, fibrinogen, and natural killer cell responses have also been reported to be exaggerated in response to stress [54, 60, 61].
Social isolation and stress have been shown to accelerate atherogenesis in cynomolgus monkeys independent of serum lipids or preponderance to atherosclerosis [62]. In Prairie Vole, social isolation may impair the normal release of protective anti-atherosclerotic factors like NO from the vascular endothelium [63]. In a study of 4,643 men and women stratified according to familial risk for CHD, a combination of low social support and high hostility significantly increased the odds of carotid artery lesions among high-risk women even after controlling for other risk factors. High-risk women showed significantly reduced odds of carotid artery lesions with high social support [64].
8. SCREENING FOR LONELINESS AND SOCIAL ISOLATION
As previously mentioned, multiple questionnaires have been used in literature to study the effects of loneliness. This poses a significant challenge to screening for loneliness in clinical practice. In an overview of 40 reviews of the public health impact of loneliness and social isolation, the authors came across 62 different self-reported questionnaires [65]. The R-UCLA-Loneliness Scale has been validated and deemed reliable [51]. The full version of the scale uses a 20-item questionnaire. An abbreviated 11-question scale has also demonstrated factorability and internal reliability on a two-factor model of “feeling isolated” and “available social connections” [66]. The UCLA 3-item scale is validated for telephone use, easy to administer, and it can be self-administered. It is a fast and easy questionnaire that can be helpful if incorporated into clinical practice and has gained a lot of popularity and is the most commonly used loneliness scale in the last decade [67]. However, the specific use of screening for loneliness with regards to CVD incidence and outcomes has not been studied. In present practice, screening for loneliness and social isolation continues to be reliant on a high index of suspicion amongst clinicians and self-reporting of patients.
9. POTENTIAL THERAPY OF LONELINESS AND SOCIAL ISOLATION WITH CVD
Multiple interventions have been studied at the individual and the community level to mitigate loneliness. Some models at the individual level include providing increased opportunities for social contact, enhanced social support, and behavioral interventions focused on social skills and addressing maladaptive social cognition. The latter has proven to be most effective in studies so far [68]. Home visitation and daily contact programs may be useful to address low social support amongst the elderly and people with disabilities [69]. Telephonic helplines have proven to be a useful tool that offers an opportunity to those suffering from loneliness to reach out to those willing to help. England’s Silver Line is one such example; lonely seniors can call to speak to an operator about any topic of their choice [70]. This center receives about 10,000 calls a week.
Some countries have attempted to intervene on a community level. The United Kingdom launched a “Campaign to end loneliness” in 2011, which included designating a Ministry of Loneliness and a £22 million program to reach out to 9 million citizens who admitted to being lonely. The measures under this campaign focus on reaching lonely individuals and supporting those in need through volunteer activities, neighborhood approaches, as well as policy changes across public departments like housing and transport [70].
At present, there are no approved pharmacological agents to reverse the pathological effects of loneliness. However, as more is learnt about the neurobiology of loneliness, pharmacological targets like selective serotonin reuptake inhibitors (SSRIs), allopregnanolone, and oxytocin emerge as important molecules to modify the downstream effects of loneliness [71, 72]. Most of the present studies in this arena are based on animal models which could offer promising targets in the management of adverse CVD outcomes of loneliness and social isolation in the future.
10. SUGGESTED MODIFICATIONS FOR LONELINESS AND SOCIAL ISOLATION INTERVENTIONS DURING COVID-19
Although face-to-face visits are the gold standard in combating loneliness and social isolation, several governmental agencies and researchers have implemented modifications to such contact to avoid the spread of COVID-19. The Centers for Medicare & Medicaid Services (CMS) have recommended outdoor family visits for nursing home residents while ensuring safe physical distancing and wearing a mask [73]. An emergency waiver suspending the requirement for complying with the Health Insurance Portability and Accountability Act (HIPAA) has increased the use of popular applications for video chats, such as Apple FaceTime and Facebook Messenger video chat for health care purposes [74]. Our team has found improvement in behavioral problems of nursing home residents with the use of Facetime with family members [75]. Others have used drive-through contacts with family members, parades, and therapeutic animal drop-ins through the interventions to curb loneliness and social isolation [33]. When family members are unavailable, researchers found telephone contact with medical students to be meaningful both for the students and geriatric patients [76]. Judicious use of antidepressants and anxiolytics is also needed for those that have new-onset or worsening of existing depression and anxiety.
CONCLUSION
Loneliness is a public health problem that is associated with an increased incidence of CVD incidence and poor outcomes. However, most of the studies in this field are observational. Loneliness, by the nature of its subjectivity and inter-person variability, is hard to identify and quantify, and we have identified some well-validated rating scales used in various studies. The impact of the current SARS-COV-2 pandemic, due to direct consequences of social distancing measures as well as its long-term implications from growing illness-anxiety and avoidance behavior, would be important for the epidemiological investigation of loneliness and social isolation. It is an opportunity to explore loneliness as an independent risk factor for CVD. While governmental agencies and researchers are modifying their approaches to combat loneliness in vulnerable populations, adequately powered studies are needed to factor for confounders like the difference in health-behavior and prevalence of conventional CVD risk factors. Clinically validated screening tools, along with greater awareness and social acceptability, are needed to better identify those at risk and mitigate cardiovascular risk. Future directions would then include studying the impact of treating loneliness in the prevention and outcomes of CVD.
ACKNOWLEDGEMENTS
Declared none.
LIST OF ABBREVIATIONS
- BMI
Body Mass Index
- CHD
Coronary Heart Disease
- CVD
Cardiovascular Disease
- MI
Myocardial Infarction
- NO
Nitric Oxide
AUTHORS' CONTRIBUTIONS
Dr. Sharma collected the data and wrote a preliminary draft of the paper. Dr Mehta conceived the idea of the paper. Dr. Mehta and Dr. Padala revised and prepared the final version of the paper.
CONSENT FOR PUBLICATION
My co-authors and I confirm our consent for the publication of the manuscript, Loneliness and social isolation: determinants of cardiovascular outcomes; Implications in COVID-19 era in Current Cardiology Reviews.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.Benjamin E.J., Muntner P., Alonso A., Bittencourt M.S., Callaway C.W., Carson A.P., Chamberlain A.M., Chang A.R., Cheng S., Das S.R., Delling F.N., Djousse L., Elkind M.S.V., Ferguson J.F., Fornage M., Jordan L.C., Khan S.S., Kissela B.M., Knutson K.L., Kwan T.W., Lackland D.T., Lewis T.T., Lichtman J.H., Longenecker C.T., Loop M.S., Lutsey P.L., Martin S.S., Matsushita K., Moran A.E., Mussolino M.E., O’Flaherty M., Pandey A., Perak A.M., Rosamond W.D., Roth G.A., Sampson U.K.A., Satou G.M., Schroeder E.B., Shah S.H., Spartano N.L., Stokes A., Tirschwell D.L., Tsao C.W., Turakhia M.P., VanWagner L.B., Wilkins J.T., Wong S.S., Virani S.S. Heart disease and stroke statistics-2019 update: A report from the american heart association. Circulation. 2019;139(10):e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Reddy K.S. Global burden of disease study 2015 provides GPS for global health 2030. Lancet. 2016;388(10053):1448–1449. doi: 10.1016/S0140-6736(16)31743-3. [DOI] [PubMed] [Google Scholar]
- 3.Wright J.T., Jr, Williamson J.D., Whelton P.K., Snyder J.K., Sink K.M., Rocco M.V., Reboussin D.M., Rahman M., Oparil S., Lewis C.E., Kimmel P.L., Johnson K.C., Goff D.C., Jr, Fine L.J., Cutler J.A., Cushman W.C., Cheung A.K., Ambrosius W.T. SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 2015;373(22):2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yusuf S., Bosch J., Dagenais G., Zhu J., Xavier D., Liu L., Pais P., López-Jaramillo P., Leiter L.A., Dans A., Avezum A., Piegas L.S., Parkhomenko A., Keltai K., Keltai M., Sliwa K., Peters R.J., Held C., Chazova I., Yusoff K., Lewis B.S., Jansky P., Khunti K., Toff W.D., Reid C.M., Varigos J., Sanchez-Vallejo G., McKelvie R., Pogue J., Jung H., Gao P., Diaz R., Lonn E. HOPE-3 Investigators. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N. Engl. J. Med. 2016;374(21):2021–2031. doi: 10.1056/NEJMoa1600176. [DOI] [PubMed] [Google Scholar]
- 5.Roth G.A., Johnson C., Abajobir A., Abd-Allah F., Abera S.F., Abyu G., Ahmed M., Aksut B., Alam T., Alam K., Alla F., Alvis-Guzman N., Amrock S., Ansari H., Ärnlöv J., Asayesh H., Atey T.M., Avila-Burgos L., Awasthi A., Banerjee A., Barac A., Bärnighausen T., Barregard L., Bedi N., Belay Ketema E., Bennett D., Berhe G., Bhutta Z., Bitew S., Carapetis J., Carrero J.J., Malta D.C., Castañeda-Orjuela C.A., Castillo-Rivas J., Catalá-López F., Choi J.Y., Christensen H., Cirillo M., Cooper L., Jr, Criqui M., Cundiff D., Damasceno A., Dandona L., Dandona R., Davletov K., Dharmaratne S., Dorairaj P., Dubey M., Ehrenkranz R., El Sayed Zaki M., Faraon E.J.A., Esteghamati A., Farid T., Farvid M., Feigin V., Ding E.L., Fowkes G., Gebrehiwot T., Gillum R., Gold A., Gona P., Gupta R., Habtewold T.D., Hafezi-Nejad N., Hailu T., Hailu G.B., Hankey G., Hassen H.Y., Abate K.H., Havmoeller R., Hay S.I., Horino M., Hotez P.J., Jacobsen K., James S., Javanbakht M., Jeemon P., John D., Jonas J., Kalkonde Y., Karimkhani C., Kasaeian A., Khader Y., Khan A., Khang Y.H., Khera S., Khoja A.T., Khubchandani J., Kim D., Kolte D., Kosen S., Krohn K.J., Kumar G.A., Kwan G.F., Lal D.K., Larsson A., Linn S., Lopez A., Lotufo P.A., El Razek H.M.A., Malekzadeh R., Mazidi M., Meier T., Meles K.G., Mensah G., Meretoja A., Mezgebe H., Miller T., Mirrakhimov E., Mohammed S., Moran A.E., Musa K.I., Narula J., Neal B., Ngalesoni F., Nguyen G., Obermeyer C.M., Owolabi M., Patton G., Pedro J., Qato D., Qorbani M., Rahimi K., Rai R.K., Rawaf S., Ribeiro A., Safiri S., Salomon J.A., Santos I., Santric Milicevic M., Sartorius B., Schutte A., Sepanlou S., Shaikh M.A., Shin M.J., Shishehbor M., Shore H., Silva D.A.S., Sobngwi E., Stranges S., Swaminathan S., Tabarés-Seisdedos R., Tadele Atnafu N., Tesfay F., Thakur J.S., Thrift A., Topor-Madry R., Truelsen T., Tyrovolas S., Ukwaja K.N., Uthman O., Vasankari T., Vlassov V., Vollset S.E., Wakayo T., Watkins D., Weintraub R., Werdecker A., Westerman R., Wiysonge C.S., Wolfe C., Workicho A., Xu G., Yano Y., Yip P., Yonemoto N., Younis M., Yu C., Vos T., Naghavi M., Murray C. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017;70(1):1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Norheim O.F., Jha P., Admasu K., Godal T., Hum R.J., Kruk M.E., Gómez-Dantés O., Mathers C.D., Pan H., Sepúlveda J., Suraweera W., Verguet S., Woldemariam A.T., Yamey G., Jamison D.T., Peto R. Avoiding 40% of the premature deaths in each country, 2010-30: review of national mortality trends to help quantify the UN sustainable development goal for health. Lancet. 2015;385(9964):239–252. doi: 10.1016/S0140-6736(14)61591-9. [DOI] [PubMed] [Google Scholar]
- 7.Ferketich A.K., Schwartzbaum J.A., Frid D.J., Moeschberger M.L. Depression as an antecedent to heart disease among women and men in the NHANES I study. National Health and Nutrition Examination Survey. Arch. Intern. Med. 2000;160(9):1261–1268. doi: 10.1001/archinte.160.9.1261. [DOI] [PubMed] [Google Scholar]
- 8.Gan Y., Gong Y., Tong X., Sun H., Cong Y., Dong X., Wang Y., Xu X., Yin X., Deng J., Li L., Cao S., Lu Z. Depression and the risk of coronary heart disease: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2014;14:371. doi: 10.1186/s12888-014-0371-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charlson F.J., Moran A.E., Freedman G., Norman R.E., Stapelberg N.J., Baxter A.J., Vos T., Whiteford H.A. The contribution of major depression to the global burden of ischemic heart disease: a comparative risk assessment. BMC Med. 2013;11:250. doi: 10.1186/1741-7015-11-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van der Kooy K., van Hout H., Marwijk H., Marten H., Stehouwer C., Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int. J. Geriatr. Psychiatry. 2007;22(7):613–626. doi: 10.1002/gps.1723. [DOI] [PubMed] [Google Scholar]
- 11.Wulsin L.R., Singal B.M. Do depressive symptoms increase the risk for the onset of coronary disease? A systematic quantitative review. Psychosom. Med. 2003;65(2):201–210. doi: 10.1097/01.PSY.0000058371.50240.E3. [DOI] [PubMed] [Google Scholar]
- 12.Nicholson A., Kuper H., Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur. Heart J. 2006;27(23):2763–2774. doi: 10.1093/eurheartj/ehl338. [DOI] [PubMed] [Google Scholar]
- 13.Rugulies R. Depression as a predictor for coronary heart disease. a review and meta-analysis. Am. J. Prev. Med. 2002;23(1):51–61. doi: 10.1016/S0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- 14.Holahan C.J., Pahl S.A., Cronkite R.C., Holahan C.K., North R.J., Moos R.H. Depression and vulnerability to incident physical illness across 10 years. J. Affect. Disord. 2010;123(1-3):222–229. doi: 10.1016/j.jad.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Surtees P.G., Wainwright N.W., Luben R.N., Wareham N.J., Bingham S.A., Khaw K.T. Depression and ischemic heart disease mortality: evidence from the EPIC-Norfolk United Kingdom prospective cohort study. Am. J. Psychiatry. 2008;165(4):515–523. doi: 10.1176/appi.ajp.2007.07061018. [DOI] [PubMed] [Google Scholar]
- 16.Kendler K.S., Gardner C.O., Fiske A., Gatz M. Major depression and coronary artery disease in the Swedish twin registry: phenotypic, genetic, and environmental sources of comorbidity. Arch. Gen. Psychiatry. 2009;66(8):857–863. doi: 10.1001/archgenpsychiatry.2009.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roest A.M., Martens E.J., de Jonge P., Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J. Am. Coll. Cardiol. 2010;56(1):38–46. doi: 10.1016/j.jacc.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 18.Batelaan N.M., Seldenrijk A., Bot M., van Balkom A.J., Penninx B.W. Anxiety and new onset of cardiovascular disease: critical review and meta-analysis. Br. J. Psychiatry. 2016;208(3):223–231. doi: 10.1192/bjp.bp.114.156554. [DOI] [PubMed] [Google Scholar]
- 19.Scott K.M., de Jonge P., Alonso J., Viana M.C., Liu Z., O’Neill S., Aguilar-Gaxiola S., Bruffaerts R., Caldas-de-Almeida J.M., Stein D.J., de Girolamo G., Florescu S.E., Hu C., Taib N.I., Lépine J.P., Levinson D., Matschinger H., Medina-Mora M.E., Piazza M., Posada-Villa J.A., Uda H., Wojtyniak B.J., Lim C.C., Kessler R.C. Associations between DSM-IV mental disorders and subsequent heart disease onset: beyond depression. Int. J. Cardiol. 2013;168(6):5293–5299. doi: 10.1016/j.ijcard.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawkley L.C., Cacioppo J.T. Loneliness and pathways to disease. Brain Behav. Immun. 2003;17(Suppl. 1):S98–S105. doi: 10.1016/S0889-1591(02)00073-9. [DOI] [PubMed] [Google Scholar]
- 21.Steptoe A., Shankar A., Demakakos P., Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. USA. 2013;110(15):5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xia N., Li H. Loneliness, Social Isolation, and Cardiovascular Health. Antioxid. Redox Signal. 2018;28(9):837–851. doi: 10.1089/ars.2017.7312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 25.Oscar Anderson G. Loneliness among older adults: A national survey of adults 45+. AARP Research. 2010. https://www.aarp.org/research/topics/life/info-2018/loneliness-social-connections.html
- 26.Edmondson B. All the lonely people. AARP Research. 2010. https://www.aarp.org/personal-growth/transitions/info-09-2010/all_the_lonely_people.html
- 27.Nyqvist F., Cattan M., Conradsson M., Näsman M., Gustafsson Y. Prevalence of loneliness over ten years among the oldest old. Scand. J. Public Health. 2017;45(4):411–418. doi: 10.1177/1403494817697511. [DOI] [PubMed] [Google Scholar]
- 28.Mullen R.A., Tong S., Sabo R.T., Liaw W.R., Marshall J., Nease D.E., Jr, Krist A.H., Frey J.J., III Loneliness in primary care patients: A prevalence study. Ann. Fam. Med. 2019;17(2):108–115. doi: 10.1370/afm.2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Usher K., Bhullar N., Jackson D. Life in the pandemic: Social isolation and mental health. J. Clin. Nurs. 2020;29(15-16):2756–2757. doi: 10.1111/jocn.15290. [DOI] [PubMed] [Google Scholar]
- 30.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marjanovic Z., Greenglass E.R., Coffey S. The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: an online questionnaire survey. Int. J. Nurs. Stud. 2007;44(6):991–998. doi: 10.1016/j.ijnurstu.2006.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290:113117. doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abbasi J. Social isolation-the other COVID-19 threat in nursing homes. JAMA. 2020 doi: 10.1001/jama.2020.13484. [DOI] [PubMed] [Google Scholar]
- 34.Chen B., Sun J., Feng Y. How have COVID-19 isolation policies affected young people’s mental health? - Evidence from chinese college students. Front. Psychol. 2020;11:1529. doi: 10.3389/fpsyg.2020.01529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valtorta N.K., Kanaan M., Gilbody S., Ronzi S., Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–1016. doi: 10.1136/heartjnl-2015-308790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hedblad B., Ostergren P.O., Hanson B.S., Janzon L., Johansson B.W., Juul-Möller S. Influence of social support on cardiac event rate in men with ischaemic type ST segment depression during ambulatory 24-h long-term ECG recording. The prospective population study ‘Men born in 1914’, Malmö, Sweden. Eur. Heart J. 1992;13(4):433–439. doi: 10.1093/oxfordjournals.eurheartj.a060193. [DOI] [PubMed] [Google Scholar]
- 37.Rosengren A., Wilhelmsen L., Orth-Gomér K. Coronary disease in relation to social support and social class in Swedish men. A 15 year follow-up in the study of men born in 1933. Eur. Heart J. 2004;25(1):56–63. doi: 10.1016/j.ehj.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 38.Barefoot J.C., Grønbaek M., Jensen G., Schnohr P., Prescott E. Social network diversity and risks of ischemic heart disease and total mortality: Findings from the Copenhagen City Heart Study. Am. J. Epidemiol. 2005;161(10):960–967. doi: 10.1093/aje/kwi128. [DOI] [PubMed] [Google Scholar]
- 39.André-Petersson L., Hedblad B., Janzon L., Ostergren P.O. Social support and behavior in a stressful situation in relation to myocardial infarction and mortality: Who is at risk? Results from prospective cohort study “Men born in 1914,” Malmö, Sweden. Int. J. Behav. Med. 2006;13(4):340–347. doi: 10.1207/s15327558ijbm1304_9. [DOI] [PubMed] [Google Scholar]
- 40.Gafarov V.V., Panov D.O., Gromova E.A., Gagulin I.V., Gafarova A.V. The influence of social support on risk of acute cardiovascular diseases in female population aged 25-64 in Russia. Int. J. Circumpolar Health. 2013;72:72. doi: 10.3402/ijch.v72i0.21210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kawachi I., Colditz G.A., Ascherio A., Rimm E.B., Giovannucci E., Stampfer M.J., Willett W.C. A prospective study of social networks in relation to total mortality and cardiovascular disease in men in the USA. J. Epidemiol. Community Health. 1996;50(3):245–251. doi: 10.1136/jech.50.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eng P.M., Rimm E.B., Fitzmaurice G., Kawachi I. Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. Am. J. Epidemiol. 2002;155(8):700–709. doi: 10.1093/aje/155.8.700. [DOI] [PubMed] [Google Scholar]
- 43.Strodl E., Kenardy J., Aroney C. Perceived stress as a predictor of the self-reported new diagnosis of symptomatic CHD in older women. Int. J. Behav. Med. 2003;10(3):205–220. doi: 10.1207/S15327558IJBM1003_02. [DOI] [PubMed] [Google Scholar]
- 44.Thurston R.C., Kubzansky L.D. Women, loneliness, and incident coronary heart disease. Psychosom. Med. 2009;71(8):836–842. doi: 10.1097/PSY.0b013e3181b40efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Manemann S.M., Chamberlain A.M., Roger V.L., Griffin J.M., Boyd C.M., Cudjoe T.K.M., Jensen D., Weston S.A., Fabbri M., Jiang R., Finney Rutten L.J. Perceived social isolation and outcomes in patients with heart failure. J. Am. Heart Assoc. 2018;7(11):e008069. doi: 10.1161/JAHA.117.008069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hakulinen C., Pulkki-Råback L., Virtanen M., Jokela M., Kivimäki M., Elovainio M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart. 2018;104(18):1536–1542. doi: 10.1136/heartjnl-2017-312663. [DOI] [PubMed] [Google Scholar]
- 47.Berkman L.F., Leo-Summers L., Horwitz R.I. Emotional support and survival after myocardial infarction. A prospective, population-based study of the elderly. Ann. Intern. Med. 1992;117(12):1003–1009. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- 48.Herlitz J., Wiklund I., Caidahl K., Hartford M., Haglid M., Karlsson B.W., Sjöland H., Karlsson T. The feeling of loneliness prior to coronary artery bypass grafting might be a predictor of short-and long-term postoperative mortality. Eur. J. Vasc. Endovasc. Surg. 1998;16(2):120–125. doi: 10.1016/S1078-5884(98)80152-4. [DOI] [PubMed] [Google Scholar]
- 49.Berkman L.F., Syme S.L. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am. J. Epidemiol. 1979;109(2):186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 50.Koenig H.G., Westlund R.E., George L.K., Hughes D.C., Blazer D.G., Hybels C. Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics. 1993;34(1):61–69. doi: 10.1016/S0033-3182(93)71928-3. [DOI] [PubMed] [Google Scholar]
- 51.Russell D.W. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 52.Hawkley L.C., Burleson M.H., Berntson G.G., Cacioppo J.T. Loneliness in everyday life: cardiovascular activity, psychosocial context, and health behaviors. J. Pers. Soc. Psychol. 2003;85(1):105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- 53.Cacioppo J.T., Hawkley L.C., Crawford L.E., Ernst J.M., Burleson M.H., Kowalewski R.B., Malarkey W.B., Van Cauter E., Berntson G.G. Loneliness and health: potential mechanisms. Psychosom. Med. 2002;64(3):407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 54.Steptoe A., Owen N., Kunz-Ebrecht S.R., Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29(5):593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- 55.Maheshwari A., Norby F.L., Soliman E.Z., Adabag S., Whitsel E.A., Alonso A., Chen L.Y. Low heart rate variability in a 2-minute electrocardiogram recording is associated with an increased risk of sudden cardiac death in the general population: The atherosclerosis risk in communities study. PLoS One. 2016;11(8):e0161648. doi: 10.1371/journal.pone.0161648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gouin J.P., Zhou B., Fitzpatrick S. Social integration prospectively predicts changes in heart rate variability among individuals undergoing migration stress. Ann. Behav. Med. 2015;49(2):230–238. doi: 10.1007/s12160-014-9650-7. [DOI] [PubMed] [Google Scholar]
- 57.Yang S., Zhang L. Glucocorticoids and vascular reactivity. Curr. Vasc. Pharmacol. 2004;2(1):1–12. doi: 10.2174/1570161043476483. [DOI] [PubMed] [Google Scholar]
- 58.Li H., Förstermann U. Nitric oxide in the pathogenesis of vascular disease. J. Pathol. 2000;190(3):244–254. doi: 10.1002/(SICI)1096-9896(200002)190:3<244::AID-PATH575>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 59.Häfner S., Baumert J., Emeny R.T., Lacruz M.E., Bidlingmaier M., Reincke M., Kuenzel H., Holle R., Rupprecht R., Ladwig K.H. MONICA/KORA Study Investigators. To live alone and to be depressed, an alarming combination for the renin-angiotensin-aldosterone-system (RAAS). Psychoneuroendocrinology. 2012;37(2):230–237. doi: 10.1016/j.psyneuen.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 60.Jaremka L.M., Fagundes C.P., Peng J., Bennett J.M., Glaser R., Malarkey W.B., Kiecolt-Glaser J.K. Loneliness promotes inflammation during acute stress. Psychol. Sci. 2013;24(7):1089–1097. doi: 10.1177/0956797612464059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hackett R.A., Hamer M., Endrighi R., Brydon L., Steptoe A. Loneliness and stress-related inflammatory and neuroendocrine responses in older men and women. Psychoneuroendocrinology. 2012;37(11):1801–1809. doi: 10.1016/j.psyneuen.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 62.Kaplan J.R., Manuck S.B., Clarkson T.B., Lusso F.M., Taub D.M., Miller E.W. Social stress and atherosclerosis in normocholesterolemic monkeys. Science. 1983;220(4598):733–735. doi: 10.1126/science.6836311. [DOI] [PubMed] [Google Scholar]
- 63.Peuler J.D., Scotti M.A., Phelps L.E., McNeal N., Grippo A.J. Chronic social isolation in the prairie vole induces endothelial dysfunction: implications for depression and cardiovascular disease. Physiol. Behav. 2012;106(4):476–484. doi: 10.1016/j.physbeh.2012.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Knox S.S., Adelman A., Ellison R.C., Arnett D.K., Siegmund K., Weidner G., Province M.A. Hostility, social support, and carotid artery atherosclerosis in the National Heart, Lung, and Blood Institute Family Heart Study. Am. J. Cardiol. 2000;86(10):1086–1089. doi: 10.1016/S0002-9149(00)01164-4. [DOI] [PubMed] [Google Scholar]
- 65.Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 66.Lee J., Cagle J.G. Validating the 11-item revised university of california los angeles scale to assess loneliness among older adults: An evaluation of factor structure and other measurement properties. Am. J. Geriatr. Psychiatry. 2017;25(11):1173–1183. doi: 10.1016/j.jagp.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 67.Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res. Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Masi C.M., Chen H.Y., Hawkley L.C., Cacioppo J.T. A meta-analysis of interventions to reduce loneliness. Pers. Soc. Psychol. Rev. 2011;15(3):219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jeste D.V., Lee E.E., Cacioppo S. Battling the modern behavioral epidemic of loneliness: Suggestions for research and interventions. JAMA Psychiatry. 2020;77(6):553–554. doi: 10.1001/jamapsychiatry.2020.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.The website for campaign to end loneliness. https://www.campaigntoendloneliness.org
- 71.Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: Clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238–49. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Norman G.J., Cacioppo J.T., Morris J.S., Malarkey W.B., Berntson G.G., Devries A.C. Oxytocin increases autonomic cardiac control: Moderation by loneliness. Biol. Psychol. 2011;86(3):174–180. doi: 10.1016/j.biopsycho.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 73.Center for clinical standards and quality/ quality, safety and oversight group, center for medicare and medicaid services. Nursing home re-opening recommendations for state and local officials. https://www.cms.gov/files/document/qso-20-30-nh.pdf-0
- 74.Wright J.H., Caudill R. Remote treatment delivery in response to the COVID-19 pandemic. Psychother. Psychosom. 2020;89(3):130–132. doi: 10.1159/000507376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Padala S.P., Jendro A.M., Orr L.C. Facetime to reduce behavioral problems in a nursing home resident with Alzheimer’s dementia during COVID-19. Psychiatry Res. 2020;288:113028. doi: 10.1016/j.psychres.2020.113028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Office E.E., Rodenstein M.S., Merchant T.S., Pendergrast T.R., Lindquist L.A. Reducing social isolation of seniors during COVID-19 through medical student telephone contact. J. Am. Med. Dir. Assoc. 2020;21(7):948–950. doi: 10.1016/j.jamda.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]