Abstract
Background
Globally, dyslipidemia has been shown to be an independent predictor of many cardiovascular and cerebrovascular events, which led to recent advocacy towards dyslipidemia prevention and control as a key risk factor and its prognostic significance to reduce the burden of stroke and myocardial infarction (MI).
Aims
This study aimed to evaluate hyperlipidemia as a risk factor connected with stroke and CVD. Moreover, having identified this risk factor, the study evaluates how hyperlipidemia has been examined earlier and what can be done in the future.
Methods
All prospective studies concerning hyperlipidemia as risk factors for stroke and CVD were identified by a search of PubMed/MEDLINE and EMBASE databases with keywords hyperlipidemia, risk factors, stroke, and cardiovascular disease.
Results
The constant positive association between the incidence of coronary heart disease and cholesterol concentration of LDL is apparent in observational studies in different populations. Thus, the reduction of LDL cholesterol in those populations, particularly with regard to initial cholesterol concentrations, can reduce the risk of vascular diseases. However, the impact of using lipid-lowering drugs, such as statins, has been demonstrated in several studies as an important factor in decreasing the mortality and morbidity rates of patients with stroke and CVD.
Conclusion
After reviewing all the research mentioned in this review, most studies confirmed that hyperlipidemia is a risk factor for stroke and correlated in patients with CVD.
Keywords: Hyperlipidemia, stroke, cardiovascular disease, risk factors, dyslipidemia, cardiovascular and cerebrovascular events
1. INTRODUCTION
Dyslipidemia is defined as the abnormal levels of lipids and lipoproteins in the blood. It is manifested as an elevation in total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), and reduced high-density lipoprotein cholesterol (HDL-C). Globally, it has been shown to be an independent predictor of many cardiovascular and cerebrovascular events, which led to recent advocacy towards dyslipidemia prevention and control as a key risk factor and its prognostic significance to reduce the burden of stroke and myocardial infarction (MI) [1, 2].
Myocardial infarction is the most common form of chronic heart disease (CHD) and is the leading cause of death, with over 15% deaths each year, and mainly prevalent in males of all age groups than females. In 2015, approximately 7.4 million deaths were caused by CHD, and by the year 2030, it is estimated that 23.6 million people will die due to CHD. The age spectrum prevalence of MI extends from 0.06% in men younger than 45 years of age to 2.46% in those older than 75 years [3].
Stroke is the second leading cause of mortality and a major cause of permanent disability, with 11.13% of total deaths attributed to it. Its incidence weighs up to 0.2% of the population yearly, with the death of one in six sufferers within the first month of ischemic stroke and almost half the survivors' being dependent on others due to disability [4, 5].
A pivotal mechanism of hyperlipidemia is atherosclerosis; this term encompasses both inflammatory and immunological responses. Early stages include endothelial dysfunction resulting from oxidative stress-driven by hyperlipidemia, smoking, diabetes mellitus, or hypertension, followed by vascular oxidization of LDL, which accumulates and activates scavenger receptors on macrophages resulting in both their activation and ox-LDL uptake.
Although about 90% of the risk factors are modifiable, including dyslipidemia, diabetes mellitus, obesity, smoking, psychosocial factors, hypertension, alcohol consumption, sedentary lifestyle, and a diet low in fruits and vegetables, increments are evident in MI cases within developing countries in contrast to the declining rates of MI in industrialized countries [3].
1.1. Aims
This study aimed to evaluate hyperlipidemia as a risk factor that is connected with stroke and CVD. Moreover, having identified this risk factor, the study evaluates how hyperlipidemia has been examined earlier and what can be done in the future.
2. METHODS
2.1. Design and Strategy
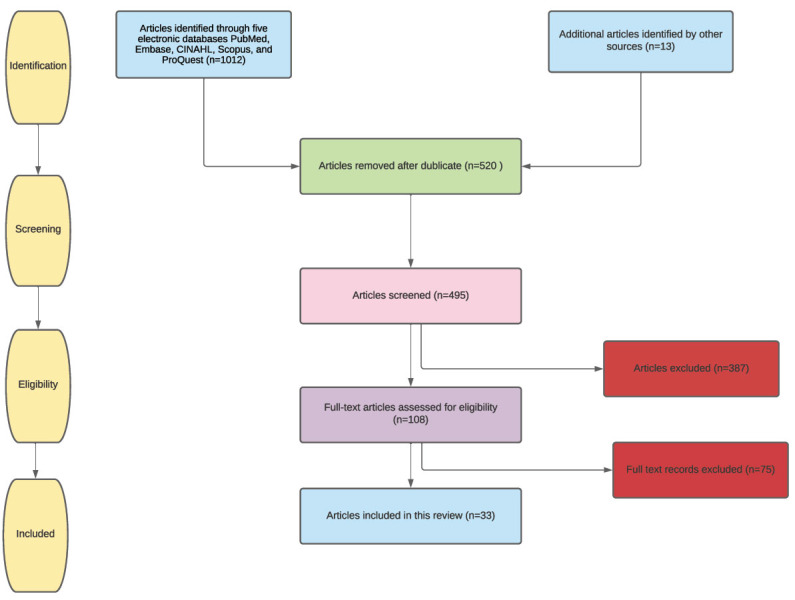
This review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [6]. A three-step method was applied to classify the included studies: (1) a systematic search of electronic databases, (2) a manual search of journal references, and (3) meetings and discussions with content experts. Five electronic databases (PubMed, Embase, CINAHL, Scopus, and ProQuest) were chosen and systematically searched for relevant, full-text availability, and English-only studies from each database's point of inception until December 18, 2019.
An initial search was carried on PubMed using three main concepts derived from the aim: (“hyperlipidemia” OR “stroke” OR “cardiovascular disease”) and (“hyperlipidemia” AND “risk factor”) and (“hyperlipidemia” AND “risk factor” AND “stroke” OR “cardiovascular disease). Booleans and truncation symbols were utilized and filters such as “English” and “full-text” were applied. Using the eligibility criteria, the titles and abstracts of the studies were screened for relevance before full-text screening by two reviewers. Existing reviews were scanned for relevant studies that may have been missed during the search. Any discrepancies that arose were evaluated and discussed between the two reviewers until a consensus was reached (Fig. 1).
Fig. (1).
Prisma flow chart (A higher resolution / colour version of this figure is available in the electronic copy of the article).
All randomized clinical trials concerning hyperlipidemia as risk factors for stroke and CVD were identified by a search of PubMed/MEDLINE and EMBASE databases with keywords hyperlipidemia, risk factors, stroke, and cardiovascular disease. The results included all prospective studies involving patients with stroke and CVD risk factors and lipid profile. Randomized controlled trials of CVD and stroke risk factors published from 1995 to 2020 qualified for inclusion criteria. The method of randomized distribution of participants to CVD or stroke risk factors or placebo was eligible. Studies were included if they were published between 1995 and 2020, and if they afforded information on inclusion criteria, the number of randomization methods, trial endpoints, duration of follow-up, trial interventions, and methods of analyses. Findings were independently derived and reviewed. Nonetheless, no additional analyses were conducted.
2.2. Data Extraction
With reference to the PRISMA checklist, the data of the involved studies were extracted in two steps. Firstly, publication details (author's name, year of publication), country of publication, study aim, methodology (sample characteristics, study design, method of data collection), method of data analysis, and findings were extracted. Secondly, discrepancies that arose between the two reviewers were discussed until a consensus was reached.
2.3. Critical Appraisal
The ten-item Critical Appraisal Skills Program (CASP) tool [7] was used to appraise the involved studies that fulfilled the eligibility criteria. The aspects evaluated included (1) suitability and appropriateness of the study's objective and aims, (2) rigor of the methodology, (3) appropriateness of the study design, (4) sampling method, (5) data collection, (6) reflexivity of the researchers, (7) ethical concerns and measures, (8) data analysis, (9) rigor of the findings, and (10) research significance and implications.
These aspects of the involved studies were rated (“Yes” = three points, “Can't tell” = two points, or “No” = one point), and each study was scored out of the maximum score of 30. The included studies had an average score of 28.6, with scores ranging from 26 to 30, and interrater reliability of 97%. The included studies were of good quality and all the studies were included regardless of their quality of appraisal because the authors believe that a critical appraisal is to improve the rigor of the synthesis and not to select rigorous studies.
2.4. Ethical Considerations
This study was deemed IRB-exempt according to the Human Subjects Protection guidelines since data were openly accessible and individual patients were not identifiable. The review was based on ethical guidelines for carrying out research studies. The references used in the research are well cited and referenced to avoid plagiarism. The sources were summarized to assure that the study is not just a duplicate of the previous studies. Also, there were no incidences where individual ideas that may be biased were involved in the study as for facts. This assures that the review is reliable, therefore, crucial to the many targeted users.
3. RESULTS
In our review of the literature, we identified 20 studies showing a relationship between dyslipidemia and cardiovascular disease and stroke, while, in contrast, 13 studies showed no relationship among them. The characteristics of patients, number of risk factors, and findings are summarized in Tables (1 and 2).
Table 1.
Summary of the included studies showing no relation between lipid and MI and stroke.
| Author, Year | Name of the Study | Participants | Number of Risk Factors | Findings |
|---|---|---|---|---|
| Jia Zheng, Zhaoqing Sun, Xingang Zhang, Zhao Li, Xiaofan Guo, Yanxia Xie, Yingxian Sun & Liqiang Zheng, 2019 | Non-traditional lipid profiles associated with ischemic stroke not hemorrhagic stroke in hypertensive patients: Results from an 8.4 years follow-up study | 5099 hypertensive patients, aged 35 or older and without cardiovascular disease, were selected for the prospective cohort study. | Age, sex, ethnicity, BMI, current smoking, current drinking, diabetes mellitus, SBP, DBP, and anti-hypertensive medications | The study concluded that HDL had no association with ischemic stroke and all lipid parameters were not associated with hemorrhagic stroke incidence. In addition to this, LDL/HDL was the best predictor of IS; hence it may help improve the efficacy of the individualized patient stroke risk assessment, diagnosis, and guide clinical decisions. |
| Hindy, G., Engström, G., Larsson, S. C., Traylor, M., Markus, H. S., Melander, O., & Orho-Melander, M. (2018) |
Role of Blood Lipids in the Development of Ischemic Stroke and its Subtypes Mendelian randomization (MR) | 185 genome-wide lipids- SNPs | High LDL, High Triglyceride, Low HDL | LDL cholesterol lowering is likely to prevent large artery atherosclerosis but may not prevent small artery occlusion nor cardioembolic strokes. High-density lipoprotein cholesterol elevation may lead to benefits in small artery disease prevention. Finally, triglyceride-lowering may not yield benefits in ischemic stroke and its subtypes. |
| Mukesh Gupta (2018) |
Assessment of Lipid Profile of Patients with Acute Myocardial Infarction: A Comparative Study | 20 AMI patients and 20 normal | Patients with acute myocardial infarction and who gave written consent for participating in the study. 2. Chest pain lasting more than 20 minutes 3. Diagnostic ECG changes with characteristic ECG alterations consisting of (in Absence of LVH and LBBB) a. ST-elevation: i. New ST elevation at J point in two contiguous leads with the cut-points. ii. ≥0.1mV in all leads other than leads V2–V3 where the following cut points apply. ≥0.2 mV in men ≥40 years; ≥0.25 mV in men | Risk of AMI is not prevented by a reduction in the mean serum cholesterol levels. |
| Ravnskov, U., Diamond, D. M., Hama, R., Hamazaki, T., Hammarskjöld, B., Hynes, N., ... & McCully, K. S. (2016) |
Lack of association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: A systematic review | 68094 elderly people | Low-density lipoprotein cholesterol (LDL-C) as a risk factor for mortality in elderly people | High LDL-C is inversely associated with mortality in most people over 60 years of age. This study provides the rationale for a re-evaluation of guidelines recommending pharmacological reduction of LDL-C in the elderly as a component of cardiovascular disease prevention strategies. |
| Domma, A. M., & Gamal, M. A. (2015) | Association between Acute Myocardial Infarction, Lipid Profile and Smoking Habit | 125 males and 49 females their ages ranged from 30-90 years old. | Smoking, increased total blood cholesterol and triglycerides concentration. | No clear evidence that increased total blood cholesterol and triglycerides concentration play an important role in the development of myocardial infarction in those patients included in this study. |
| Philip-Ephraim, E. E., Charidimou, A., & Kajogbola, G. A. (2015) | Quadriparesis due to simultaneous occurrence of hemorrhagic and ischemic stroke | 100 patients with an age range of 32 to 88 years. | There were 100 patients, comprising 50 acute ischemic stroke patients and 50 non-stroke patients (controls) who had diseases other than stroke, including peptic ulcer disease, bronchial asthma, uncontrolled hypertension, and diabetes mellitus. | The predictive role of lipid profile as a stroke risk factor remains controversial as our study failed to demonstrate the association between lipid profile and stroke. |
| Lauren C Blekkenhorst Richard L Prince Jonathan M Hodgson Wai H Lim Kun ZhuAmanda Devine Peter L Thompson Joshua R Lewis (2015) |
Dietary saturated fat intake and atherosclerotic vascular disease mortality in older women: A prospective cohort study | 1469 women with a mean ± SD age of 75.2 ± 2.7 y | Outcome data were serum lipids at baseline and ASVD deaths over 10 y (13,649 person-years of follow-up). Other risk factors for ASVD were assessed and adjusted for in multivariable analyses. | LDL cholesterol was not associated with ASVD mortality in this cohort. |
| Bianca Nogrady Medicine Today (2015) |
Does lipid-lowering reduce stroke risk in the elderly? The nine-year French observational study. |
7484 men and women, with a mean age of 73.9 years | Age, sex, body mass index, hypertension, systolic blood pressure, and high lipid. | The study found no association between lipid lowering drug use and reductions in the risk of coronary heart disease, even after accounting for age, sex, body mass index, hypertension, systolic blood pressure, and other factors. Commenting on the study, Professor Mark Nelson said that although the finding was interesting, the lack of effect of lipid lowering on coronary artery disease suggested the outcomes were compromised by treatment allocation bias. |
| Lise Bathum, René Depont Christensen, Lars Engers Pedersen, Palle Lyngsie Pedersen, John Larsen &Jørgen Nexøe (2013) |
Association of lipoprotein levels with mortality in subjects aged 50 + without previous diabetes or cardiovascular disease: A population-based register study | 118160 subjects aged 50 + | Compared with subjects with TC < 5 mmol/L, adjusted hazard ratios for the group aged 60–70 years ranged from 0.68 (95% confidence interval (CI) 0.61–0.77) for TC 5–5.99 mmol/L to 0.67 (95% CI 0.59–0.75) for TC 6–7.99 mmol/L and 1.02 (95% CI 0.68–1.53) for TC ≥ 8 mmol/L in males and from 0.57 (95% CI 0.48–0.67) to 0.59 (95% CI 0.50–0.68) and 1.02 (95% CI: 0.77–1.37) in females. |
These associations indicate that high lipoprotein levels do not seem to be harmful in the general population. |
| Khan, H. A., Alhomida, A. S., & Sobki, S. H. (2013) |
Lipid profile of patients with acute myocardial infarction and its correlation with systemic inflammation. |
67 AMI patients and 25 patients with chest pain | ST-elevated myocardial infarction, non-ST-elevated myocardial infarction, chest pain. | The findings suggest that reduction in serum cholesterol does not prevent the risk of AMI. |
| Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group, 2010 | Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: A double-blind randomised trial. | 12,064 men and women aged 18–80 years with a history of myocardial infarction. | Men and women aged 18–80 years with a history of previous myocardial infarction were eligible provided they match the following inclusion criteria: either current statin use or clear indication for this treatment (and no clear indication for folic acid); total cholesterol of at least 3·5 mmol/L if already on a statin or 4·5 mmol/L if not; and no clear contraindications to the study treatments.11 Individuals with other predominant medical problems that could reduce compliance with long-term study treatment were also excluded. |
Participants assigned to 80mg simvastatin vs. 20 mg results showed no apparent differences in numbers of hemorrhagic strokes or deaths attributed to vascular or non- causes despite the reduction in LDL. |
| Willey, J. Z., Xu, Q., Boden-Albala, B., Paik, M. C., Moon, Y. P., Sacco, R. L., & Elkind, M. S. (2009) | Lipid Profile Components and Risk of Ischemic Stroke The Northern Manhattan Study (NOMAS) Population-based prospective cohort study. |
2940 patients | Stroke-free community residents. | Baseline lipid panel components were not associated with increased stroke risk in this cohort. |
| Prospective Studies Collaboration, 1995. | Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts | 450,000 individuals | Sex, diastolic blood pressure, history of coronary disease, or ethnicity (Asian or non-Asian). | Did not find an association between total cholesterol levels and stroke after standardization forage except, perhaps, in those under 45 years of age when screened. |
Table 2.
Summary of the included studies showing a relation between lipid and MI and stroke.
| Author, Year | Name of the Study | Participant | Number of Risk Factors | Findings |
|---|---|---|---|---|
| Heart Protection Study Collaborative Group, 2002 | Heart Protection Study | 20536 Age 40-80 years |
Those without the diagnosed coronary disease who had cerebrovascular disease, or had peripheral artery disease, or had diabetes; men and, separately, women; those aged either under or over 70 years at entry. | Allocation to 40 mg simvastatin daily reduced the rates of myocardial infarction, stroke, and revascularization by about one-quarter. |
| Sever et al., 2003 | Anglo Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA) Double-blind placebo-controlled trial |
19342 hypertensive patients (aged 40-79 years | All coronary events, all cardiovascular events, fatal and non-fatal stroke, development of chronic stable angina, heart failure, and peripheral arterial disease. | The reductions in major cardiovascular events with atorvastatin are large, given the short follow-up time. |
| Scandinavian Simvastatin Survival Study Group, 1994 | Scandinavian Simvastatin Survival Study (4S) Randomized double-blind trial |
4444 patients | Effect of cholesterol-lowering with simvastatin on mortality and morbidity in patients with coronary heart disease (CHD). | Long-term treatment with simvastatin is safe and improves survival in CHD patients. |
| Tonkin, Simes, Sharpe, & Thomson, 1998 | The Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) Randomized double-blind trial |
9014 patients who were 31 to 75 years of age | The patients had a history of myocardial infarction or hospitalization for unstable angina and initial plasma total cholesterol levels of 155 to 271 mg per deciliter. Compared the effects of pravastatin (40 mg daily) with those of a placebo. |
Pravastatin therapy reduced mortality from coronary heart disease and overall mortality, as compared with the rates in the placebo group, as well as the incidence of all pre-specified cardiovascular events in patients with a history of myocardial infarction or unstable angina who had a broad range of initial cholesterol levels. |
| Sacks et al., 1996 | The Cholesterol and Recurrent Events (CARE) trial | 4159 men and women aged 21 to 75 enrolled in 80 centers around the US and Canada |
Secondary prevention of CHD 3 to 20 months post-MI Total-C < 240; LDL-C between 115 and 174; Triglycerides < 350 mg/dL 5 years Treatment with Pravastatin 40 mg vs. placebo |
The benefit of cholesterol-lowering therapy extends to most patients with coronary disease who have average cholesterol levels |
| SPARCL Investigators, 2006. | Stroke Prevention by Aggressive Reduction in Cholesterol Levels Study (SPARCL) | 4,731 participants, 40% female Mean age 63 years |
For subjects randomized to atorvastatin 80 mg/d or placebo stroke or TIA without known coronary heart disease |
Atorvastatin 80 mg/d is similarly efficacious in preventing strokes and other cardiovascular events, irrespective of baseline ischemic stroke subtype. |
| Mitchell Elkind et al., 1990 | Northern Manhattan Study (NOMAS) | Over 4,400 people from the community were enrolled | Stroke and stroke risk factors in the Northern Manhattan community in whites, blacks, and Hispanics living in the same community. A population-based incidence and case-control study. |
The study has already made great advances in the understanding, prevention, and treatment of stroke. Caribbean Hispanics from the Northern Manhattan community had strokes at a younger age than blacks and whites. There was also a higher rate of stroke-related death in Caribbean Hispanic and black patients than in white patients. |
| Blackburn, Keys, Simonson, et al. 1984 | Lipid Research Clinics Coronary Primary Prevention Trial (LRC-CPPT): A multicenter, randomized, double-blind study |
3,806 asymptomatic middle-aged men were enrolled with primary hypercholesterolemia | Tested the efficacy of cholesterol lowering in reducing the risk of coronary heart disease (CHD) | Reducing total cholesterol by lowering LDL-C levels can diminish the incidence of CHD morbidity and mortality in men at high risk for CHD because of raised LDL-C levels. |
| Hennekens, Sacks, Tonkin, et al., 2004 | Additive Benefits of Pravastatin and Aspirin to Decrease Risks of Cardiovascular Disease Randomized and Observational Comparisons of Secondary Prevention Trials and Their Meta-analyses | 73 900 patient-years of observation | Secondary prevention with pravastatin sodium and aspirin (40 mg/d) decreases cardiovascular disease risks | More widespread and appropriate combined use of statins and aspirin in secondary prevention of cardiovascular disease will avoid large numbers of premature deaths. |
| Prospective Studies Collaboration, 1995 | Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts | Review of 45 prospective observational cohorts involving 450,000 individuals with 5-30 years of follow-up | The relations of blood cholesterol and diastolic blood pressure with subsequent stroke rates were examined. | After standardization for age, there was no association between blood cholesterol and stroke except, perhaps, in those under 45 years of age when screened. However, because the types of strokes were not centrally available, lack of any overall relation might conceal a positive association with ischemic stroke together with a negative association with hemorrhagic stroke. |
| Zinat Nadia Hatmi, Nasrin Jalilian, and Ali Pakravan, 2019 | The Relationship Between Premature Myocardial Infarction with TC/HDL-C Ratio Subgroups in a Multiple Risk Factor Model | 1222 MI cases of both women and men. Cases included 523 newly diagnosed MI patients under 55 years. Whereas controls included 699 newly diagnosed cases of MI whose ages were above 55 years | CAD risk factors of cases and controls included: smoking, family history of premature CAD, fasting blood sugar, cholesterol and Triglyceride, HDL, LDL, and hypertension. | The study concluded that reduction of the level of TC/HDL-C ratio from low risk to a very low risk category, will diminish the risk of MI by about 8% in patients under 55 years of age. Therefore, the study suggests that aggressive treatment interventions aiming towards lowering TC/HDL-C ratio could be a crucial clinical implication |
| Amit V. Khera, Olga V. Demler, Steven J. Adelman, Heidi L. Collins, Robert J. Glynn, Paul M Ridker, Daniel J. Rader, and Samia Mora, 2018. | Cholesterol Efflux Capacity, HDL Particle Number, and Incident Cardiovascular Events | 17,802 asymptomatic individuals with normal LDL cholesterol but increased C-reactive protein levels, 314 cases of CVD were compared to age and sex matched controls | Risk factors include age, race, treatment group (placebo or rosuvastatin), systolic blood pressure, smoking status, body-mass index, fasting glucose, log-transformed triglycerides, LDL cholesterol level, and family history of premature CAD. | For both baseline and on statin analyses, HDL particle number was the strongest inverse predictor among four HDL-related biomarkers, whereas cholesterol efflux capacity was associated with CVD in individuals on potent statin therapy but not at baseline. |
| Michael V. Holmes, Iona Y. Millwood, Christiana Kartsonaki, Michael R. Hill, Derrick A. Bennett, Ruth Boxall, Yu Guo, Xin Xu, Zheng Bian, Ruying Hu, Robin G. Walters, Junshi Chen, Mika Ala-Korpela, Sarah Parish, Robert J. Clarke, Richard Peto, Rory Collins, Liming Li, Zhengming Chen and on behalf of the China Kadoorie Biobank Collaborative Group, 2018. |
Lipids, Lipoproteins, and Metabolites and Risk of Myocardial Infarction and Stroke | 4,662 common control subjects aged between 30 to 79. | Age, sex, smoking, SBP, BMI, type 2 diabetes, and total cholesterol/HDL-C ratio. | Positive association between MI, IS, and Very low-, intermediate-, and low-density lipoprotein particles were concluded. High-density lipoprotein (HDL) particles were found to be inversely associated with MI. |
| Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Yong- Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee, 2017. | Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: A nationwide population-based study | Study population consisted of 3,656,648 subjects with no history of MI or stroke | BMI, smoking, alcohol consumption, DM, Blood pressure, regular exercise, dyslipidemia | Cholesterol variability is an important risk factor and predictor for MI and stroke. |
| Emanuele Di Angelantonio, Pei Gao, Lisa Pennells,, Stephen Kaptoge, Muriel Caslake, Alexander Thompson, Adam S. Butterworth, Nadeem Sarwar, David Wormser, and Danish Saleheen, Christie M. Ballantyne, Bruce M. Psaty, Johan Sundström, Paul M Ridker, Dorothea Nagel, Richard F. Gillum,Ian Ford, Pierre Ducimetiere, Stefan Kiechl, Wolfgang Koenig, Robin P. F. Dullaart, Gerd Assmann, Ralph B. D'Agostino Sr, Gilles R. Dagenais, Jackie A. Cooper, Daan Kromhout, Altan Onat, Robert W. Tipping, Agustín Gómez-de-la-Cámara, Annika Rosengren, Susan E. Sutherland, John Gallacher, F. Gerry R. Fowkes,Edoardo Casiglia, Albert Hofman, Veikko Salomaa, Elizabeth Barrett-Connor, Robert Clarke, Eric Brunner, J. Wouter Jukema, Leon A. Simons, Manjinder Sandhu, Nicholas J. Wareham, Kay-Tee Khaw, Jussi Kauhanen, Jukka T. Salonen, William J. Howard, Børge G. Nordestgaard, Angela M. Wood, Simon G. Thompson, S. Matthijs Boekholdt, Naveed Sattar, Chris Packard, Vilmundur Gudnason, and John Danesh, 2012 |
Lipid-Related Markers and Cardiovascular Disease Prediction |
165,544 participants without baseline CVD in 37 prospective cohorts |
Age, sex, smoking status, history of diabetes, and systolic blood pressure, total cholesterol, HDL-C, assayed triglyceride, apolipoprotein B and A-I, lipoprotein(a), or lipoprotein-associated phospholipase A2 |
In a study of individuals without known CVD, the enrollment of lipid related markers information such as apolipoprotein B and A-I, lipoprotein(a), or lipoproteinassociated phospholipase A2 mass to risk scores containing conventional lipid markers of total cholesterol and HDL-C, led to a slight improvement in CVD prediction |
| Canouï-Poitrine F, Luc G, Bard J.-M, Ferrieres J, Yarnell J., Arveiler D., Morange P. Kee F., Evans A., Amouyel P., Ducimetiere P., Empana J.-P. | Relative Contribution of Lipids and Apolipoprotein to Incident Coronary Heart Disease and Ischemic Stroke: The PRIME Study | 9,711 men aged 50–59 years, free of CHD and stroke at baseline | Age, systolic blood pressure, antihypertensive treatment, current smoking status, body mass index and diabetes | Total-C, HDL-C, LDL-C, non-HDL-C, Triglycerides, Apo A1 and Apo B100, their ratios and Lp(a) are significantly predictive of future CHD, weak predictors, if anything, of ischemic stroke over 10 year period. |
| Salim Yusuf,, D.Phil., Eva Lonn, Prem Pais, Jackie Bosch, Patricio López-Jaramillo, Jun Zhu, Denis Xavier, Alvaro Avezum, Lawrence A. Leiter, Leopoldo S. Piegas, Alexander Parkhomenko, Matyas Keltai, 2016. | Blood-Pressure and Cholesterol Lowering in Persons without Cardiovascular Disease | 12,705 participants at intermediate risk who did not have cardiovascular disease. The study included men 55 years of age or older and women 65 years of age or older | The trial included age with at least one additional risk factor besides it, female sex, smoking, BMI, waist to hip ratio, low HDL, impaired glucose tolerance, early DM, family history of coronary heart disease, early renal dysfunction, family history of premature CHD, BP, race or ethnic group and medication used. | The combination of rosuvastatin (10 mg per day), candesartan (16 mg per day), and hydrochlorothiazide (12.5 mg per day) produced greater LDL reduction and was found to be associated with a significantly lower rate of cardiovascular events than dual placebo among individuals at intermediate risk who did not have cardiovascular disease. |
| Raffaele De Caterina, Marco Scarano, RosaMaria Marfisi, Giuseppe Lucisano, Francesco Palma, Alfonso Tatasciore and Roberto Marchioli, 2010. | Cholesterol-Lowering Interventions and Stroke Insights From a Meta-Analysis of Randomized Controlled Trials |
266,973 patients, with a cumulative exposure of 946,582 person-years, with the total number of trials testing the effectiveness of cholesterol lowering interventions and stroke being 82 . | Age, patient history of MI, inclusion of patients with diabetes mellitus, heart failure, and baseline levels of TC, triglycerides, and HDL-C. | Cholesterol lowering therapy is found to be linked with a significant reduction of stroke (total and non-fatal strokes), whereas no intervention was associated with a reduction of fatal stroke. This appears to be true for both statin and non-statin cholesterol-lowering interventions, with statins being the most effective, there appears to be a proportionality between the reduction of cholesterol (mostly LDL-C) and the reduction of total stroke, with an approximation of 0.8% reduction in TC for a 1.0% reduction of the relative risk of stroke. |
| Heart Protection Study Collaborative Group, 2016 | Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20,536 high-risk individuals: a randomised controlled trial | 20 536 men and women aged about 40–80 years at high risk of vascular and non-vascular outcomes | The group assigned 20mg simvastatin achieved an average LDL reduction by 1.0 mmol/L, which was proportional to a 23% reduction in cardiovascular events with significant divergence each year, prolonged LDL-lowering statin treatment results in a significant reduction in vascular events and benefit persists for at least 5 years wich support prompt initiation and long term statin treatment. |
|
| Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group, 2010 | Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: A double-blind randomised trial. | 12,064 men and women aged 18–80 years with a history of myocardial infarction. | Men and women aged 18–80 years with a history of previous myocardial infarction were eligible provided they match the following inclusion criteria: either current statin use or clear indication for this treatment (and no clear indication for folic acid); total cholesterol of at least 3·5 mmol/L if already on a statin or 4·5 mmol/L if not; and no clear contraindications to the study treatments.11 individuals with other predominant medical problems that could reduce compliance with long-term study treatment were also excluded. |
Participants assigned 80mg simvastatin had a 6% (SE 3·5%) reduction in major vascular events with a further 0·35 mmol/L reduction in LDL cholesterol compared to those allocated to 20mg |
| Jeffrey S. Berger, Aileen P. McGinn, Barbara V. Howard, Lewis Kuller, JoAnn E. Manson, Jim Otvos, J. David Curb, Charles B. Eaton, Robert C. Kaplan, John K. Lynch, Daniel M. Rosenbaum, and Sylvia Wassertheil-Smoller, 2012 | Lipid and Lipoprotein Biomarkers and the Risk of Ischemic Stroke in Postmenopausal Women. | 82,591 postmenopausal women aged between 50-79 years. | Women who made the inclusion criteria provided informed consent to be a part of the study and were 50–79 years of age at baseline, postmenopausal, had no medical conditions associated with a predicted survival of <3 years |
The study concluded that IDL,VLDL and triglyceride were associated with ischemic stroke. These results support the AHA guidelines that state triglycerides as stroke risk factors. |
| Xiaojuan Liu, Ling Yan, Fuzhong Xue, 2018. | The associations of lipids and lipid ratios with stroke: A prospective cohort study | 42 005 participants (25 989 men and 16 016 women) were enrolled aged between 20-80 years. | Three lipid ratios were computed: TC/HDL-C, TG/HDL-C, and LDL-C/HDL-C, all of which have at least once been reported as a predictor of cardiovascular risk in the literature, Systolic blood pressure (SBP) and diastolic blood pressure (DBP), BMI, history or current cigarette smoking, alcohol consumption status, family history of CVD, history of hypertension, Type 2 diabetes mellitus and information on the use of lipid-lowering drugs. | In men,TC/HDL-C was the most important predictor of ischemic and total stroke, whereas TG was the most reliable in predicting ischemic and total stroke in women. These two lipid indexes may serve as potential targets for stroke prevention and are of important prognostic value. |
3.1. Total Cholesterol
A positive relationship between a high level of total cholesterol and the development of stroke and CVD has been demonstrated in several studies [8-13] Table (2). The Heart Protection Study [8] showed that lowering cholesterol, using daily 40 mg simvastatin, reduced the rates of myocardial infarction, stroke, and revascularization by about one-quarter among 20,536 UK adults (aged 40–80 years). Similarly, the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT-LLA) reported the outcome of the lipid-lowering atorvastatin (10 mg). Significant and important proportional decreases in cardiovascular events were observed in a group of hypertensive patients who were, on average, at only mild cardiovascular risk, given certain risk factors and who would not have been considered conventionally dyslipidemic [9].
The Scandinavian Simvastatin Survival Study showed that long-term simvastatin therapy was also effective and increased the survival of CHD patients in 4444 cases [10], while a long-term intervention with pravastatin in ischemic disease (LIPID) study group found that drug treatment decreased mortality from coronary heart disease and overall mortality of patients with a history of myocardial infarcts or unstable angina. Patients had a wide range of initial cholesterol levels, compared with outcomes of the placebo group, and also the frequency of all pre-specified cardiovascular events [13].
For patients with average cholesterol levels, the Cholesterol and Recurrent Events (CARE) Trial conducted a study of 4159 patients with myocardial infarcts, who had plasma total cholesterol levels below 240 mg per deciliter (mean, 209) and low-density lipoprotein (LDL) cholesterol levels of 115 to 174 mg per deciliter (mean, 139) [11]. A 40 mg dose of pravastatin per day or placebo was administered to those patients, and the results showed that the benefit of cholesterol-lowering therapy was extended to the majority of patients with coronary artery disease who had average cholesterol levels [11].
The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) program investigators identified evidence that in patients with previous stroke or transient ischemic attack (TIA), and without established coronary heart disease, 80 mg of atorvastatin per day reduced the overall occurrence of strokes and cardiovascular events, with only a slight increase in the rate of hemorrhagic stroke [12].
Some observational studies have found no association between lower TC levels and increased risk of hemorrhagic stroke and myocardial infarction Table (1). Similarly, no correlation was identified between total cholesterol and stroke, following standardization forage, except perhaps, for those under 45 years of age who were screened [14]. In a comparison of the mean TC levels and HDL levels in 20 patients of an AMI group and 20 patients in a control group, a reduction in the mean serum cholesterol levels did not prevent the incidence of AMI, although serum HDL and elevated HS-CRP were highly predisposed to an AMI for high-risk individuals [15].
3.2. Low-density Lipoprotein (LDL)
In the identified studies, 20 provided detailed results for LDL cholesterol [8-14, 16-28]. In most observational studies (but not all), there was an association between reduced LDL- C levels and decreased ischemic stroke and CVD risk [8-13, 23-28]. The Lipid Research Clinics Coronary Primary Prevention Trial (LRC-CPPT) demonstrated that reducing total cholesterol by lowering LDL-C levels decreased CHD morbidity and mortality in people who were highly vulnerable to CHD because of rising LDL-C rates [23].
A systematic review and meta-analysis of all randomized trials that tested statin drugs (published before August 2003) were performed [29]. Each 10% reduction in LDL-C was estimated to reduce the risk of all strokes by 15.6% and carotid IMT by 0.73% per year [29].
In the Heart Protection Study (HPS), the long-term efficacy and safety of lowering LDL cholesterol with statins were assessed. The study found that a more extended LDL-lowering statin therapy produced a larger total decrease in vascular accidents, even after research therapy with HPS ended; the results remained unchanged for at least five years, without any proof of emerging hazards. Such results provide further evidence for the timely initiation and long-term continuity of statin therapy. The 20 mg simvastatin community achieved an average LDL reduction of 1.0 mmol/L, which is equivalent to a 23% decrease in cardiovascular events with significant differences each year, and extended LDL-lowering statin therapy resulted in a significant decline in cardiac accidents and ongoing gain for at least five years, with timely initiation and long-term statin therapy [28]. Furthermore, a meta-analysis was performed, which included 81,700 patients, among which 41,979 were treated with PSCK9 inhibitors. A total of 1319 cases of myocardial infarctions were registered in the treatment group as compared to 1608 in controls, resulting in a reduction of the incidence of myocardial infarction by 19% and stroke by 25%, by using PCSK9 inhibitors [30].
3.3. High-density Lipoprotein (HDL)
An analysis from the JUPITER trial (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) with 17,802 asymptomatic patients was linked to controls (balanced in age and sex), with an average LDL cholesterol, and with elevated C-reactive protein rates, for 314 CVD cases. The results showed that for both baseline and statin studies, the HDL particle number was the best reverse indicator of four HDL biomarkers, relative to cholesterol efflux capability in CVD in people undergoing efficient, but not baseline, statin therapy [31].
The Framingham Heart Study identified an inverse relationship between high-density lipoprotein cholesterol (HDL-C) levels and the incidence of CVD [32], while in a systematic review and meta-analysis of 119 clinical trials that included 35,760 participants, 17 trials reported that the use of niacin as a monotherapy was associated with a reduction in some cardiovascular events [33].
3.4. Triglycerides
In a systematic review and meta-regression analysis of 40 randomized controlled trials (RCTs) of lipid- modifying drugs, with cardiovascular events as an outcome, and with a total enrollment of 200,593 patients, it was found that changes in triglyceride levels indicate cardiovascular events in RCTs. In primary prevention populations, this relationship was significant, but not in secondary prevention populations [34]. Triglyceride was the most reliable in predicting ischemic and total stroke in women according to a prospective cohort study on a total of 42,005 participants [35].
In a second study, the lipid and lipoprotein biomarkers were investigated as predictors of ischemic stroke among 82,591 postmenopausal women aged between 50–79 years. The ischemic stroke event was significantly associated with postmenopausal women with a profile of lipid and lipoprotein biomarkers: baseline, triglycerides, VLDL, and IDL particle amount [36].
Patients with type 2 diabetes were at higher risk of cardiovascular disease (CVD), in part, owing to hypertriglyceridemia and low high-density lipoprotein cholesterol. It is unknown whether
adding the triglyceride-lowering treatment fenofibrate therapy to statins reduces the risk of cardiovascular disease (CVD) in study participants with dyslipidemia (defined as triglyceride levels greater than 204 mg/dL and high-density lipoprotein cholesterol levels less than 34 mg/Dl) [37]. It has been found that the combination of fenofibrate and omega-3 fatty acids significantly decreased triglycerides by 41% in patients with hypertriglyceridemia [38]. The synergetic effect between fenofibrate and simvastatin is effective, and well-tolerated therapies improve the TG and HDLC profile in high-risk patients with mixed dyslipidemia [39].
3.5. Non-traditional Lipid (TC/HDL-C, Very Low-Density Lipoprotein, Intermediate Density Lipoprotein)
In some studies, after adjusting for confounders, the TC/HDL-C ratio showed a significant association with the risk of ischemic and total stroke and MI [35, 40]. A study of 1222 MI cases of both women and men, including 523 newly diagnosed MI patients under 55 years, and 699 newly diagnosed cases of MI whose age was above 55 years as control, concluded that a change in the TC/HDL-C ratio from low risk to very low risk would reduce the risk of MI by around 8% in patients under 55 years of age. This study thus indicated that aggressive treatment strategies targeted at reducing the TC/HDL-C ratio could be crucial to physician participation [40].
4. DISCUSSION
This study aimed to evaluate hyperlipidemia as a cardiovascular and stroke risk factor. Dyslipidemias is characterized by lipid circulatory disorders, including high levels of low-density lipoprotein cholesterol (LDL-C), elevated triglycerides, high levels of total cholesterol (TC), and low levels of high-density lipoprotein cholesterol (HDL-C) [41]. Dyslipidemia is conventionally considered to play an essential role in the pathogenesis of cardiovascular diseases and stroke [42-44]. The plasma levels of total cholesterol and low-density lipoprotein (LDL) cholesterol are important risk factors for coronary heart disease [45].
LDL carries about 60–70% serum cholesterol [46] and transports the liver's cholesterol to the peripheral tissues. A high level of LDL-C is harmful because it can build up to initiate the formation of atherosclerotic plaques on the arterial walls [47]. Large randomized trials have shown that lowering LDL cholesterol with 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors (“statins”) reduces coronary mortality and morbidity in some high-risk patients.
The Scandinavian Simvastatin Survival Study and other randomized trials of cholesterol-lowering therapy involved people with pre-existing cardiac disease and excluded older people, so that they mainly involved middle-aged men and excluded women because women tend to develop cardiovascular diseases at an older age than men.
The results of the Heart Protection Study showed that lowering LDL cholesterol with statins produced a significant reduction in the incidence of major vascular events among a much wider range of high-risk individuals than had previously been shown to benefit from such treatment. In particular, it demonstrated significant benefits not only for those who were already known to have coronary artery disease but also for those who had not been diagnosed with coronary artery disease, peripheral artery disease, or diabetes (for which there has previously been little direct evidence of benefit), irrespective of the concentration of lipids in the blood when treatment was started [8].
Since hypertension makes an important contribution to the general cardiovascular risk, the use of statins in hypertensive patients should be considered. The lipid-lowering arm of ASCOT's findings showed that in hypertensive patients, who on average were at moderate risk of developing cardiovascular events, cholesterol-lowering with atorvastatin 10 mg conferred a 36% reduction in fatal CHD and non-fatal myocardial infarction compared with the placebo [9]. This study showed the benefits of statin treatment in addition to those of good blood-pressure control.
Although total cholesterol is a significant risk factor for coronary heart disease, the relationship between plasma cholesterol and coronary events appears to be stronger if levels are elevated rather than at average values [45]. However, the CARE trial showed that the benefit achieved by lowering the LDL cholesterol levels of patients who have hypercholesterolemia could be extended to the more typical patients with coronary disease, who have an average LDL cholesterol level [11].
Treatment with 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins) decreases the risk of stroke among patients with a history of stroke or TIA. The effect of intensive lipid-lowering therapy with atorvastatin compared with placebo among patients with prior stroke or transient ischemic attack (TIA) was evaluated by the SPARCL trial. Treatment with 80 mg of atorvastatin per day decreased the risk of stroke, major coronary events, and revascularization in patients with a recent stroke or TIA [12]. These results by the SPARCL trial were consistent with the hypothesis that reduction in LDL cholesterol levels reduces the risk of recurrent stroke. The results of the SPARCL study contrasted with those of the Heart Protection Study (HPS), which found no reduction in the risk of stroke among patients with prior cerebrovascular disease, due to a greater reduction in LDL cholesterol in the SPARCL study than in the HPS study (56 mg per deciliter (1.4 mmol per liter) vs. 39 mg per deciliter (1.0 mmol per liter)) [8, 12].
The results of several studies have been consistent with the idea that increased LDL cholesterol is an important factor in the pathogenesis of CHD [10, 48]. These studies provided evidence for a beneficial effect of statin-forms, such as simvastatin, on fatal plus non-fatal cerebrovascular events [10]. In addition, the risk of myocardial infarction or stroke is significantly reduced by lowering cholesterol levels with pravastatin in patients with a broad range of initial cholesterol levels, and a history of myocardial infarction or unstable angina reduces the risk of death from CHD, cardiovascular disease, and all causes combined [13].
The results of the LIPID study extended the findings of the Scandinavian Simvastatin Survival Study, which showed that treatment benefited from CHD mortality and overall mortality among patients with CHD, who had a mean cholesterol level of 261 mg per deciliter (6.7 mmol per liter) at study entry [10]. In contrast, the LIPID results show similar benefits in patients with a mean cholesterol level of about 44 mg per deciliter (1.1 mmol per liter), which is lower than that reported in the Scandinavian study [13].
Most of the studies reviewed did not record non-fatal strokes. All the findings relate mainly to stroke mortality; thus, the results for less severe strokes may have been different. Although some studies included patients with previous strokes, the numbers affected would be small, particularly in the middle ages [14]. The LRC-CPPT demonstrated that treatment of asymptomatic middle-aged men with primary hypercholesterolemia with cholestyramine resin reduces the incidence of CHD. This result is in line with those of previous cholesterol-lowering clinical trials, which showed a general trend of efficacy for selected endpoints of CHD [23]. The Heart Protection Study (HPS) assessed the long-term efficacy and safety of lowering LDL cholesterol with statins and reported cause-specific mortality and major morbidity during in-trial and post-trial periods [28].
Proprotein Convertase Subtilisin/Kexin 9 (PCSK9) is a circulating protease that binds to the low-density lipoprotein (LDL) receptor, resulting in intracellular degradation that reduces receptor activity and promotes higher levels of serum LDLc [30, 49]. Clinical trials have shown that PCSK9 inhibitors reduce the incidence of myocardial infarction and stroke, which is in agreement with the effect of this new drug [30, 50-54].
A combined analysis of prospective observational studies of cholesterol, blood pressure, and stroke showed no independent association between baseline blood total cholesterol and stroke risk across the entire range of total cholesterol values studied [14]. HDL may have several potentially important antiatherosclerotic, anti-inflammatory, antithrombotic, and endothelial protective effects [47, 55]. HDL-C hypotheses, related to their functions and role, led to a growing interest in drugs that increase HDL-C levels, like niacin, as potential interventions to reduce the risk of CVD [47]. HDL particle number is the strongest HDL-related biomarker of residual risk in participants treated with potent statin therapy [31]. In addition to effectively reducing LDL-C, statins are also able to increase HDL-C by 6-14.7% [56].
Although more effective cholesterol-lowering drugs achieved large reductions in blood cholesterol and in CHD, no significant difference in stroke mortality was observed in some studies. This can be explained by the substantial heterogeneity of the study population, design, endpoint definition, or maybe due to missing data on type-specific strokes, insufficient adjustment for potential medical confounders, and different stroke subtypes being differently related to total cholesterol [14, 35]. Hence, a positive association with occlusive stroke might be offset by a negative association with hemorrhagic stroke. There is some evidence for this hypothesis [10, 18, 57]; although the total cholesterol levels required for any substantial increase in hemorrhagic stroke may be very low, there is a negative association [14].
The inflammatory process is a vital component of cardiovascular disease pathogenesis; therefore, the risk of such diseases can not be prevented by lowering the level of cholesterol and lipoprotein in the exclusion of other inflammatory markers, such as c-reactive protein [15]. Accordingly, we could explain the results in some studies by the absence of association between the lipid profile and the development of stroke and MI [58, 59].
Recently, new research has expanded our understanding of the role of inflammation in myocardial infarction (MI), ischemic stroke (IS), and intracerebral hemorrhage (ICH) [60]. Therefore, several studies have looked at the associations between inflammatory marker levels and their predictive ability for cardiovascular diseases and stroke [61, 62]. By providing a full analysis of lipoprotein, lipid and several circulating metabolites with the interactions of MI, IS, and ICH events may add a useful predictive risk factor value for these diseases. The research study [24] found a positive association between MI, IS, and Very low-, intermediate-, and low-density lipoprotein particles, whereas high-density lipoprotein (HDL) particles were found to be inversely associated with MI.
High triglyceride levels are also associated with the risk of cardiovascular disease and were predictive of cardiovascular events in randomized controlled trials (RCTs) of lipid- modifying drugs [34]. The findings from large cohort studies have added to the growing evidence that serum lipid and lipid ratio parameters are associated with the risk of stroke. When estimated as continuous variables, higher levels of TG, TC/HDL-C, and TG/HDL-C in men and TG in women were associated with an increased risk of ischemic and total stroke [35].
Non-traditional lipids abnormalities may play a larger role in the risk of ischemic stroke than traditional lipids. In a prospective evaluation of lipid and lipoprotein biomarkers associated with incident ischemic stroke, baseline levels of triglycerides were a significant biomarker among postmenopausal women. Other biomarkers at baseline, including VLDL triglyceride, VLDL particle number, VLDL size, LDL particle number, IDL particle number, HDL cholesterol, HDL size, and the total cholesterol/HDL-C ratio, were also associated with future ischemic stroke [36].
The TC/HDL-C ratio has been identified as one of the most feasible and robust predictors of future cardiovascular events [63-65]. Hypertriglyceridemia has recently emerged as one of the most effective therapeutic targets [66]. Fibrates are TG lowering drugs, reducing the risk of major cardiovascular events predominantly by the prevention of coronary events; they also might have a role in individuals at high risk of cardiovascular events and those with combined dyslipidemia [67]. A synergic effect of fibrates, such as omega-3 fatty acids combined with fenofibrate, in patients with hypertriglyceridemia had a positive impact on decreasing triglyceride levels in addition to non-traditional lipids, such as the triglycerides/HDL cholesterol ratio [38].
In statin therapy, even high doses could not adequately correct elevated triglycerides (TG) and low high-density lipoprotein-cholesterol (HDL-C) levels; the association of the two commonly called atherogenic dyslipidemia still conferred patients with a residual CVD risk [39]. Adding a triglyceride-lowering treatment to statins reduces the risk of cardiovascular disease (CVD). The extended follow-up of ACCORD-lipid participants confirmed the original neutral effect of fenofibrate in the overall study cohort; continued observation of heterogeneity of baseline lipids therapy suggests that fenofibrate therapy may reduce CVD in patients with hypertriglyceridemia diabetes and low-density lipoprotein cholesterol [37, 68]. Besides, coadministration of fenofibrate and simvastatin is an effective and well-tolerated therapy to improve the TG and HDLC profiles in high-risk patients with mixed dyslipidemia [39].
CONCLUSION
A solid link of hyperlipidemia, especially LDL-C with CVD and stroke, indicating the importance of lowering LDL-C in patients that are considered intermediate to high risk for CVD with statin and a combination of therapeutic medications, has been shown. Moreover, identifying which factors are most important to residual risk to develop stroke and CVD is essential to reduce the mortality and morbidity among populations. The current review revealed some areas that need additional studies and generated several queries that need further analysis. In particular, the results from the current review recommend conducting a meta-analysis for randomized clinical trials.
ACKNOWLEDGEMENTS
Declared none.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was deemed IRB-exempt according to the Human Subjects Protection guidelines since data were openly accessible and individual patients were not identifiable.
HUMAN AND ANIMAL RIGHTS
The review was based on ethical guidelines for carrying out research studies. There are also no incidences where individual ideas that may be biased are involved in the study as for facts.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.Kim M.K., Han K., Kim H-S., Park Y-M., Kwon H-S., Yoon K-H., Lee S.H. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur. Heart J. 2017;38(48):3560–3566. doi: 10.1093/eurheartj/ehx585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olamoyegun M.A., Akinlade A.T., Fawale M.B., Ogbera A.O. Dyslipidaemia as a risk factor in the occurrence of stroke in Nigeria: prevalence and patterns. Pan Afr. Med. J. 2016;25:72. doi: 10.11604/pamj.2016.25.72.6496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jayaraj JC, Davatyan K, Subramanian S, Priya J. Epidemiology of Myocardial Infarction. Myocardial Infarction: IntechOpen. 2018 [Google Scholar]
- 4.Habibi-Koolaee M., Shahmoradi L., Niakan Kalhori S.R., Ghannadan H., Younesi E. Prevalence of stroke risk factors and their distribution based on stroke subtypes in gorgan: a retrospective hospital-based study-2015-2016. Neurol. Res. Int. 2018;2018 doi: 10.1155/2018/2709654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klijn C.J., Hankey G.J. American Stroke Association and European Stroke Initiative. Management of acute ischaemic stroke: new guidelines from the American Stroke Association and European Stroke Initiative. Lancet Neurol. 2003;2(11):698–701. doi: 10.1016/S1474-4422(03)00558-1. [DOI] [PubMed] [Google Scholar]
- 6.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. PRISMA Group. Preferred reporting items for systematic reviews and meta- analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Critical Appraisal Skills Program. CASP Checklist. 2018. https://casp-uk.net/casp-tools-checklists/
- 8.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360(9326):7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 9.Sever P.S., Dahlöf B., Poulter N.R., Wedel H., Beevers G., Caulfield M., Collins R., Kjeldsen S.E., Kristinsson A., McInnes G.T., Mehlsen J., Nieminen M., O’Brien E., Ostergren J. ASCOT investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361(9364):1149–1158. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 10.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344(8934):1383–1389. [PubMed] [Google Scholar]
- 11.Sacks F.M., Pfeffer M.A., Moye L.A., Rouleau J.L., Rutherford J.D., Cole T.G., Brown L., Warnica J.W., Arnold J.M., Wun C.C., Davis B.R., Braunwald E. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N. Engl. J. Med. 1996;335(14):1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 12.Amarenco P., Bogousslavsky J., Callahan A., III, Goldstein L.B., Hennerici M., Rudolph A.E., Sillesen H., Simunovic L., Szarek M., Welch K.M., Zivin J.A. Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N. Engl. J. Med. 2006;355(6):549–559. doi: 10.1056/NEJMoa061894. [DOI] [PubMed] [Google Scholar]
- 13.Tonkin A., Simes R., Sharpe N., Thomson A. Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N. Engl. J. Med. 1998;339(19):1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 14.Collaboration P.S. Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts. Prospective studies collaboration. Lancet. 1995;346(8991-8992):1647–1653. doi: 10.1016/S0140-6736(95)92836-7. [DOI] [PubMed] [Google Scholar]
- 15.Gupta M. Assessment of Lipid Profile of Patients with Acute Myocardial Infarction: A Comparative Study. Journal of Medical Science And clinical Research. 2018;06:483–6. doi: 10.18535/jmscr/v6i3.81. [DOI] [Google Scholar]
- 16.Hindy G., Engström G., Larsson S.C., Traylor M., Markus H.S., Melander O., Orho-Melander M. Stroke Genetics Network (SiGN) Role of Blood Lipids in the Development of Ischemic Stroke and its Subtypes: A Mendelian Randomization Study. Stroke. 2018;49(4):820–827. doi: 10.1161/STROKEAHA.117.019653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ravnskov U., Diamond D.M., Hama R., Hamazaki T., Hammarskjöld B., Hynes N., Kendrick M., Langsjoen P.H., Malhotra A., Mascitelli L., McCully K.S., Ogushi Y., Okuyama H., Rosch P.J., Schersten T., Sultan S., Sundberg R. Lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: a systematic review. BMJ Open. 2016;6(6):e010401. doi: 10.1136/bmjopen-2015-010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Philip-Ephraim EE, Charidimou A, Kajogbola GA. Quadriparesis due to simultaneous occurrence of hemorrhagic and ischemic stroke. International journal of stroke : official journal of the International Stroke Society. 2015;10(2):E11. doi: 10.1111/ijs.12404. [DOI] [PubMed] [Google Scholar]
- 19.Blekkenhorst L.C., Prince R.L., Hodgson J.M., Lim W.H., Zhu K., Devine A., Thompson P.L., Lewis J.R. Dietary saturated fat intake and atherosclerotic vascular disease mortality in elderly women: a prospective cohort study. Am. J. Clin. Nutr. 2015;101(6):1263–1268. doi: 10.3945/ajcn.114.102392. [DOI] [PubMed] [Google Scholar]
- 20.Alpérovitch A., Kurth T., Bertrand M., Ancelin M-L., Helmer C., Debette S., Tzourio C. Primary prevention with lipid lowering drugs and long term risk of vascular events in older people: population based cohort study. BMJ. 2015;350:h2335. doi: 10.1136/bmj.h2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bathum L., Depont Christensen R., Engers Pedersen L., Lyngsie Pedersen P., Larsen J., Nexøe J. Association of lipoprotein levels with mortality in subjects aged 50 + without previous diabetes or cardiovascular disease: a population-based register study. Scand. J. Prim. Health Care. 2013;31(3):172–180. doi: 10.3109/02813432.2013.824157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Armitage J., Bowman L., Wallendszus K., Bulbulia R., Rahimi K., Haynes R., Parish S., Peto R., Collins R. Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group. Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: a double-blind randomised trial. Lancet. 2010;376(9753):1658–1669. doi: 10.1016/S0140-6736(10)60310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Lipid Research Clinics Coronary Primary Prevention Trial results. I. Reduction in incidence of coronary heart disease. JAMA. 1984;251(3):351–364. doi: 10.1001/jama.1984.03340270029025. [DOI] [PubMed] [Google Scholar]
- 24.Holmes M.V., Millwood I.Y., Kartsonaki C., Hill M.R., Bennett D.A., Boxall R., Guo Y., Xu X., Bian Z., Hu R., Walters R.G., Chen J., Ala-Korpela M., Parish S., Clarke R.J., Peto R., Collins R., Li L., Chen Z. China kadoorie biobank collaborative group. Lipids, lipoproteins, and metabolites and risk of myocardial infarction and stroke. J. Am. Coll. Cardiol. 2018;71(6):620–632. doi: 10.1016/j.jacc.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canouï-Poitrine F., Luc G., Bard J.M., Ferrieres J., Yarnell J., Arveiler D., Morange P., Kee F., Evans A., Amouyel P., Ducimetiere P., Empana J.P. PRIME Study Group. Relative contribution of lipids and apolipoproteins to incident coronary heart disease and ischemic stroke: the PRIME Study. Cerebrovasc. Dis. 2010;30(3):252–259. doi: 10.1159/000319067. [DOI] [PubMed] [Google Scholar]
- 26.Yusuf S., Lonn E., Pais P., Bosch J., López-Jaramillo P., Zhu J., Xavier D., Avezum A., Leiter L.A., Piegas L.S., Parkhomenko A., Keltai M., Keltai K., Sliwa K., Chazova I., Peters R.J., Held C., Yusoff K., Lewis B.S., Jansky P., Khunti K., Toff W.D., Reid C.M., Varigos J., Accini J.L., McKelvie R., Pogue J., Jung H., Liu L., Diaz R., Dans A., Dagenais G. HOPE-3 investigators. blood-pressure and cholesterol lowering in persons without cardiovascular disease. N. Engl. J. Med. 2016;374(21):2032–2043. doi: 10.1056/NEJMoa1600177. [DOI] [PubMed] [Google Scholar]
- 27.De Caterina R., Scarano M., Marfisi R., Lucisano G., Palma F., Tatasciore A., Marchioli R. Cholesterol-lowering interventions and stroke: insights from a meta-analysis of randomized controlled trials. J. Am. Coll. Cardiol. 2010;55(3):198–211. doi: 10.1016/j.jacc.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 28.Heart Protection Study Collaborative Group. Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20,536 high-risk individuals: a randomised controlled trial. Lancet. 2011;378(9808):2013–2020. doi: 10.1016/S0140-6736(11)61125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amarenco P., Labreuche J., Lavallée P., Touboul P-J. Statins in stroke prevention and carotid atherosclerosis: systematic review and up-to-date meta-analysis. Stroke. 2004;35(12):2902–2909. doi: 10.1161/01.STR.0000147965.52712.fa. [DOI] [PubMed] [Google Scholar]
- 30.Cordero A, Rodríguez-Mañero M, Fácila L, Fernández-Olmo MR, Gómez-Martínez MJ, Valle A, et al. Prevention of myocardial infarction and stroke with pcsk9 inhibitors treatment: a metanalysis of recent randomized clinical trials. 2020 doi: 10.1007/s40200-020-00557-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khera A.V., Demler O.V., Adelman S.J., Collins H.L., Glynn R.J., Ridker P.M., Rader D.J., Mora S. Cholesterol Efflux Capacity, High-Density Lipoprotein Particle Number, and Incident Cardiovascular Events: An Analysis From the JUPITER Trial (Justification for the Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin). Circulation. 2017;135(25):2494–2504. doi: 10.1161/CIRCULATIONAHA.116.025678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gordon T., Castelli W.P., Hjortland M.C., Kannel W.B., Dawber T.R. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am. J. Med. 1977;62(5):707–714. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 33.D’Andrea E, Hey SP, Ramirez CL, Kesselheim AS. Assessment of the role of niacin in managing cardiovascular disease outcomes: a systematic review and meta-analysis. JAMA network open. 2019;2(4):e192224-e. doi: 10.1001/jamanetworkopen.2019.2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stauffer M.E., Weisenfluh L., Morrison A. Association between triglycerides and cardiovascular events in primary populations: a meta-regression analysis and synthesis of evidence. Vasc. Health Risk Manag. 2013;9:671–680. doi: 10.2147/VHRM.S52713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu X., Yan L., Xue F. The associations of lipids and lipid ratios with stroke: A prospective cohort study. J. Clin. Hypertens. (Greenwich) 2019;21(1):127–135. doi: 10.1111/jch.13441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berger J.S., McGinn A.P., Howard B.V., Kuller L., Manson J.E., Otvos J., Curb J.D., Eaton C.B., Kaplan R.C., Lynch J.K., Rosenbaum D.M., Wassertheil-Smoller S. Lipid and lipoprotein biomarkers and the risk of ischemic stroke in postmenopausal women. Stroke. 2012;43(4):958–966. doi: 10.1161/STROKEAHA.111.641324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elam M.B., Ginsberg H.N., Lovato L.C., Corson M., Largay J., Leiter L.A., Lopez C., O’Connor P.J., Sweeney M.E., Weiss D., Friedewald W.T., Buse J.B., Gerstein H.C., Probstfield J., Grimm R., Ismail-Beigi F., Goff D.C., Jr, Fleg J.L., Rosenberg Y., Byington R.P. ACCORDION Study Investigators. Association of fenofibrate therapy with long-term cardiovascular risk in statin-treated patients with type 2 diabetes. JAMA Cardiol. 2017;2(4):370–380. doi: 10.1001/jamacardio.2016.4828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koh K.K., Oh P.C., Sakuma I., Lee Y., Han S.H., Shin E.K. Vascular and metabolic effects of omega-3 fatty acids combined with fenofibrate in patients with hypertriglyceridemia. Int. J. Cardiol. 2016;221:342–346. doi: 10.1016/j.ijcard.2016.07.038. [DOI] [PubMed] [Google Scholar]
- 39.Foucher C., Aubonnet P., Reichert P., Berli M., Schaeffer A., Calvo Vargas C.G., Lochocka A., Belenky D., Koch H.F. Cholib study Investigators. New Fixed-Dose Combinations of Fenofibrate/Simvastatin Therapy Significantly Improve the Lipid Profile of High-Risk Patients with Mixed Dyslipidemia Versus Monotherapies. Cardiovasc. Ther. 2015;33(6):329–337. doi: 10.1111/1755-5922.12148. [DOI] [PubMed] [Google Scholar]
- 40.Hatmi ZN, Jalilian N, Pakravan A. The Relationship Between Premature Myocardial Infarction with TC/HDL-C Ratio Subgroups in a Multiple Risk Factor Model. Advanced journal of emergency medicine. 2019;3(3) doi: 10.22114/ajem.v0i0.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kopin L., Lowenstein C. Dyslipidemia. Ann. Intern. Med. 2017;167(11):ITC81–ITC96. doi: 10.7326/AITC201712050. [DOI] [PubMed] [Google Scholar]
- 42.Wengrofsky P, Lee J, Makaryus AN. Dyslipidemia and its role in the pathogenesis of atherosclerotic cardiovascular disease: implications for evaluation and targets for treatment of dyslipidemia based on recent guidelines. . Dyslipidemia: IntechOpen. 2019 [Google Scholar]
- 43.Upadhyay R.K. Emerging risk biomarkers in cardiovascular diseases and disorders. J. Lipids. 2015;2015 doi: 10.1155/2015/971453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tziomalos K., Athyros V.G., Karagiannis A., Mikhailidis D.P. Dyslipidemia as a risk factor for ischemic stroke. Curr. Top. Med. Chem. 2009;9(14):1291–1297. doi: 10.2174/156802609789869628. [DOI] [PubMed] [Google Scholar]
- 45.Kannel W.B. Range of serum cholesterol values in the population developing coronary artery disease. Am. J. Cardiol. 1995;76(9):69C–77C. doi: 10.1016/S0002-9149(99)80474-3. [DOI] [PubMed] [Google Scholar]
- 46.Dipiro J.T., Talbert R.L., Yee G.C., Matzke G.R., Wells B.G., Posey L.M. In: Pharmacotherapy: a pathophysiologic approach. McGraw-Hill M., editor. New York: 2014. [Google Scholar]
- 47.Elshourbagy N.A., Meyers H.V., Abdel-Meguid S.S. Cholesterol: the good, the bad, and the ugly - therapeutic targets for the treatment of dyslipidemia. Med. Princ. Pract. 2014;23(2):99–111. doi: 10.1159/000356856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Furberg C.D., Adams H.P., Jr, Applegate W.B., Byington R.P., Espeland M.A., Hartwell T., Hunninghake D.B., Lefkowitz D.S., Probstfield J., Riley W.A., et al. Asymptomatic Carotid Artery Progression Study (ACAPS) Research Group. Effect of lovastatin on early carotid atherosclerosis and cardiovascular events. Circulation. 1994;90(4):1679–1687. doi: 10.1161/01.CIR.90.4.1679. [DOI] [PubMed] [Google Scholar]
- 49.Mach F., Baigent C., Catapano A.L., Koskinas K.C., Casula M., Badimon L., Chapman M.J., De Backer G.G., Delgado V., Ference B.A., Graham I.M., Halliday A., Landmesser U., Mihaylova B., Pedersen T.R., Riccardi G., Richter D.J., Sabatine M.S., Taskinen M.R., Tokgozoglu L., Wiklund O. ESC Scientific Document Group. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020;41(1):111–188. doi: 10.1093/eurheartj/ehz455. [DOI] [PubMed] [Google Scholar]
- 50.Mourikis P., Zako S., Dannenberg L., Nia A.M., Heinen Y., Busch L., Richter H., Hohlfeld T., Zeus T., Kelm M., Polzin A. Lipid lowering therapy in cardiovascular disease: From myth to molecular reality. Pharmacol. Ther. 2020;213:107592. doi: 10.1016/j.pharmthera.2020.107592. [DOI] [PubMed] [Google Scholar]
- 51.AlTurki A., Marafi M., Dawas A., Dube M-P., Vieira L., Sherman M.H., Gregoire J., Thanassoulis G., Tardif J.C., Huynh T. Meta-analysis of Randomized Controlled Trials Assessing the Impact of Proprotein Convertase Subtilisin/Kexin Type 9 Antibodies on Mortality and Cardiovascular Outcomes. Am. J. Cardiol. 2019;124(12):1869–1875. doi: 10.1016/j.amjcard.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 52.Jalloh M.A., Doroudgar S., Ip E.J. What is the impact of the 2017 cochrane systematic review and meta-analysis that evaluated the use of PCSK9 inhibitors for lowering cardiovascular disease and mortality? Expert Opin. Pharmacother. 2018;19(7):739–741. doi: 10.1080/14656566.2018.1464558. [DOI] [PubMed] [Google Scholar]
- 53.Karatasakis A., Danek B.A., Karacsonyi J., Rangan B.V., Roesle M.K., Knickelbine T., Miedema M.D., Khalili H., Ahmad Z., Abdullah S., Banerjee S., Brilakis E.S. Effect of PCSK9 inhibitors on clinical outcomes in patients with hypercholesterolemia: a meta-analysis of 35 randomized controlled trials. J. Am. Heart Assoc. 2017;6(12) doi: 10.1161/JAHA.117.006910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Turgeon R.D., Tsuyuki R.T., Gyenes G.T., Pearson G.J. Cardiovascular efficacy and safety of PCSK9 inhibitors: systematic review and meta-analysis including the ODYSSEY OUTCOMES trial. Can. J. Cardiol. 2018;34(12):1600–1605. doi: 10.1016/j.cjca.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 55.Nofer J-R., Kehrel B., Fobker M., Levkau B., Assmann G., von Eckardstein A. HDL and arteriosclerosis: beyond reverse cholesterol transport. Atherosclerosis. 2002;161(1):1–16. doi: 10.1016/S0021-9150(01)00651-7. [DOI] [PubMed] [Google Scholar]
- 56.Downs J.R., Clearfield M., Weis S., Whitney E., Shapiro D.R., Beere P.A., Langendorfer A., Stein E.A., Kruyer W., Gotto A.M., Jr Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279(20):1615–1622. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 57.Law M.R., Thompson S.G., Wald N.J. Assessing possible hazards of reducing serum cholesterol. BMJ. 1994;308(6925):373–379. doi: 10.1136/bmj.308.6925.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Domma A., Gamal M. Association between acute myocardial infaraction, lipid profile and smoking habbits. IOSR-JDMS. 2015;14:6. [Google Scholar]
- 59.Khan H.A., Alhomida A.S., Sobki S.H. Lipid profile of patients with acute myocardial infarction and its correlation with systemic inflammation. Biomark. Insights. 2013;8:1–7. doi: 10.4137/BMI.S11015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maas M.B., Furie K.L. Molecular biomarkers in stroke diagnosis and prognosis. Biomarkers Med. 2009;3(4):363–383. doi: 10.2217/bmm.09.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zakynthinos E., Pappa N. Inflammatory biomarkers in coronary artery disease. J. Cardiol. 2009;53(3):317–333. doi: 10.1016/j.jjcc.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 62.Kettunen J., Ritchie S.C., Anufrieva O., Lyytikäinen L-P., Hernesniemi J., Karhunen P.J., Kuukasjärvi P., Laurikka J., Kähönen M., Lehtimäki T., Havulinna A.S., Salomaa V., Männistö S., Ala-Korpela M., Perola M., Inouye M., Würtz P. Biomarker glycoprotein acetyls is associated with the risk of a wide spectrum of incident diseases and stratifies mortality risk in angiography patients. Circulation. Circ Genom Precis Med. 2018;11(11) doi: 10.1161/CIRCGEN.118.002234. [DOI] [PubMed] [Google Scholar]
- 63.Ingelsson E., Schaefer E.J., Contois J.H., McNamara J.R., Sullivan L., Keyes M.J., Pencina M.J., Schoonmaker C., Wilson P.W., D’Agostino R.B., Vasan R.S. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA. 2007;298(7):776–785. doi: 10.1001/jama.298.7.776. [DOI] [PubMed] [Google Scholar]
- 64.Ridker P.M., Rifai N., Cook N.R., Bradwin G., Buring J.E. Non-HDL cholesterol, apolipoproteins A-I and B100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. JAMA. 2005;294(3):326–333. doi: 10.1001/jama.294.3.326. [DOI] [PubMed] [Google Scholar]
- 65.Bairey Merz C.N., Ramineni T., Leong D. Sex-specific risk factors for cardiovascular disease in women-making cardiovascular disease real. Curr. Opin. Cardiol. 2018;33(5):500–505. doi: 10.1097/HCO.0000000000000543. [DOI] [PubMed] [Google Scholar]
- 66.Han S.H., Nicholls S.J., Sakuma I., Zhao D., Koh K.K. Hypertriglyceridemia and cardiovascular diseases: revisited. Korean Circ. J. 2016;46(2):135–144. doi: 10.4070/kcj.2016.46.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jun M., Foote C., Lv J., Neal B., Patel A., Nicholls S.J., Grobbee D.E., Cass A., Chalmers J., Perkovic V. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. 2010;375(9729):1875–1884. doi: 10.1016/S0140-6736(10)60656-3. [DOI] [PubMed] [Google Scholar]
- 68.Ginsberg H.N., Elam M.B., Lovato L.C., Crouse J.R., III, Leiter L.A., Linz P., Friedewald W.T., Buse J.B., Gerstein H.C., Probstfield J., Grimm R.H., Ismail-Beigi F., Bigger J.T., Goff D.C., Jr, Cushman W.C., Simons-Morton D.G., Byington R.P. ACCORD Study Group. Effects of combination lipid therapy in type 2 diabetes mellitus. N. Engl. J. Med. 2010;362(17):1563–1574. doi: 10.1056/NEJMoa1001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.