Abstract
The emergence of SARS-CoV-2 in the human population and the resulting COVID-19 pandemic have led to the development of various diagnostic tests. The OraSure InteliSwab™ COVID-19 Rapid Test is a recently developed and FDA emergency use-authorized rapid antigen-detecting test that functions as a lateral flow device targeting the nucleocapsid protein. Due to SARS-CoV-2 evolution, there is a need to evaluate the sensitivity of rapid antigen-detecting tests for new variants, especially variants of concern such as Omicron. In this study, the sensitivity of the OraSure InteliSwab™ Test was investigated using cultured strains of the known variants of concern (VOCs, Alpha, Beta, Gamma, Delta, and Omicron) and the ancestral lineage (lineage A). Based on dilution series in cell culture medium, an approximate limit of detection for each variant was determined. The OraSure InteliSwab™ Test showed an overall comparable performance using recombinant nucleocapsid protein and different cultured variants, with recorded limits of detection ranging between 3.77 × 105 and 9.13 × 105 RNA copies/mL. Finally, the sensitivity was evaluated using oropharyngeal swabs from Syrian golden hamsters inoculated with the six VOCs. Ultimately, the OraSure InteliSwab™ COVID-19 Rapid Test showed no decrease in sensitivity between the ancestral SARS-CoV-2 strain and any VOCs including Omicron.
Keywords: SARS-CoV-2, COVID-19, rapid antigen-detecting test, variants of concern, Delta, Omicron
1. Introduction
Since the emergence of SARS-CoV-2, a wide variety of diagnostic assays have been developed. These assays primarily use quantitative real-time reverse transcription polymerase chain reactions (qRT-PCRs) which detect viral RNA. Due to their high sensitivity and specificity, qRT-PCRs function as the gold standard for COVID-19 diagnostics [1]. However, qRT-PCR-based diagnostics require advanced laboratory infrastructure and trained personnel. Furthermore, the relatively long time to receive results could hamper direct decision making.
Another diagnostic assay is the rapid antigen-detecting test (RDT). RDTs can be performed at home, produce results within hours [2,3,4,5], and complement qRT-PCR-based diagnostics [6]. As the name suggests, RDTs are based on the detection of antigen presence.
The emergence of new variants of concern (VOCs) highlights the need to continuously validate current diagnostic assays. Here, we assess the sensitivity of the OraSure InteliSwab™ using all currently identified VOCs (Alpha, Beta, Gamma, Delta, and Omicron [7]) compared to the ancestral lineage (lineage A) of SARS-CoV-2. In addition, we employ the Syrian hamster COVID-19 model to determine the InteliSwab™ performance in a controlled infection environment.
2. Materials and Methods
2.1. Recombinant Nucleocapsid Protein Assay
SARS-CoV-2 nucleocapsid proteins (NPs) of described variants were expressed with an N-terminus poly-histidine tag in BL21(DE3) cells. Affinity capture of the protein was performed using nickel sepharose HP, followed by a buffer exchange into Tris/NaCl using a GE HiTrap 26/10 desalting column. The lineage A variant was expressed using reference sequence QHD43423.2, amino acids 1–419. Subsequent SARS-CoV-2 variant mutations were cloned via mutagenesis and sequenced confirmed. All recombinant NPs used for device testing were of >95% purity. Expression levels of purified NP were 80–150 mg/L depending on the variant. To load the sample on the test device, 50 µL of sample was introduced at the center of the flat pad. With the developer solution vials resting in the test stand’s slots, the loaded test devices were placed in separate vials containing the developer solution. Each test device was left in the developer solution for 30 min, after which the result was read. A positive result was a red line at the test and control zones.
2.2. Cells and Viruses
The SARS-CoV-2 isolates used in this study are summarized in Table S1. Virus propagation was performed in VeroE6 cells in DMEM supplemented with 2% fetal bovine serum, 1 mM L-glutamine, 50 U/mL penicillin, and 50 μg/mL streptomycin (DMEM2). VeroE6 cells were maintained in DMEM supplemented with 10% fetal bovine serum, 1 mM L-glutamine, 50 U/mL penicillin, and 50 μg/mL streptomycin. At regular intervals, mycoplasma testing was performed. No mycoplasma and no contaminants were detected. Sequencing from viral stocks included libraries prepared from Stranded Total RNA Prep Ligation with Ribo-Zero Plus kit per the manufacturer’s protocol (Illumina, San Diego, CA, USA) and sequenced on an Illumina MiSeq at 2 × 150 base pair reads. No nucleotide change was found >5%.
2.3. InteliSwab™ Assay on SARS-CoV-2 Isolates
Prior to dilutions and tests, each SARS-CoV-2 stock variant was inactivated using irradiation with 2 Mrad. To evaluate the effect of the irradiation process on the InteliSwab™ results, the test was performed on irradiated and unirradiated 10-fold serially diluted Delta variant stocks. The results showed that the sensitivity of OraSure InteliSwab™ COVID-19 Rapid Test was the same for both the irradiated and the unirradiated stocks (Figure S1).
Then, 10-fold serial dilutions of irradiated SARS-CoV-2 variants were performed with 1× Dulbecco’s phosphate-buffered saline (PBS). Three OraSure InteliSwab™ COVID-19 Rapid Tests were used to test each dilution, making a total of 15 test devices per variant. The test procedure was carried out as above. More precise limits of detection (LODs) for the test were determined by performing 2-fold serial dilutions in 3 replicates for each variant beginning at the 10-fold dilution LOD. Three test devices were used for each dilution. The same procedures for loading samples and analyzing test results were followed for the 10-fold serial dilutions. The final LOD for each variant was determined to be the minimum concentration (dilution) for which all 9 test devices were positive.
2.4. Ethics Statement
Animal experiments were conducted in an AAALAC International-accredited facility and approved by the Rocky Mountain Laboratories Institutional Care and Use Committee following the guidelines put forth in the Guide for the Care and Use of Laboratory Animals 8th edition, the Animal Welfare Act, United States Department of Agriculture and the United States Public Health Service Policy on the Humane Care and Use of Laboratory Animals.
The Institutional Biosafety Committee (IBC) approved work with SARS-CoV-2 strains under BSL3 conditions. Virus inactivation of all samples was performed according to IBC-approved standard operating procedures for the removal of specimens from high containment areas.
2.5. Animal Experiment
Four six-week-old Syrian golden hamsters (N = 6 per group, Envigo Indianapolis) were challenged intranasally with 40 µL of 1 × 103 Median Tissue Culture Infectious Dose (TCID50)/mL virus in sterile DMEM. All virus stocks were full genome sequenced, and no SNPs >10% in spike or nucleoprotein were detected. Weights were recorded daily. Oropharyngeal swabs were collected in 1 mL of DMEM2 on day post infection (DPI) 1–7. A volume of 50 µL of medium was pipetted onto the absorbent pad of the InteliSwab™ as outlined in the instructions for use, described previously.
2.6. RNA Extraction and qRT-PCR
RNA was extracted from 140 µL of sample for each dilution with the Qiagen QIAamp Viral RNA Kit according to the manufacturer’s instructions with an elution volume of 60 µL. Following the extraction, copies of genomic RNA were determined by qRT-PCR with the TaqMan™ Fast Virus One-Step Master Mix and QuantStudio 6 Flex Real-Time PCR System from Applied Biosystems according to the manufacturer’s instructions. The qRT-PCR applied targets the E gene of SARS-CoV-2 [8]. Ten-fold dilutions of SARS-CoV-2 standards with known copy numbers were used to construct a standard curve and calculate copies/mL.
3. Results
Through the use of monoclonal antibodies, the OraSure InteliSwab™ COVID-19 Rapid Test detects the conserved SARS-CoV-2 nucleocapsid protein (NP). To assess the performance of the InteliSwab™ for different VOCs, we first generated recombinant NP for the identified SARS-CoV-2 VOCs and the ancestral lineage A (Table 1). Sample dilutions were prepared in phosphate-buffered saline (PBS) and 50 µL of the dilution was used on each RDT. In order to determine the limit of detection (LOD), the assay was performed for each of the variant NPs with N = 20 tests. Limited variation was observed between the different NPs; the NP LOD was either 0.313 ng/mL for Alpha and Gamma or 0.469 ng/mL for lineage A, Beta, Delta, and Omicron (Table 2).
Table 1.
Nucleocapsid protein mutations of the SARS-CoV-2 variants.
| Variant | Nucleocapsid Mutations by Relative Position | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Alpha | D3L | R203K | G204R | S235F | |||||
| Beta | T205I | ||||||||
| Gamma | P80R | R203K | G204R | ||||||
| Delta | D63G | R203M | D377Y | ||||||
| Omicron | P13L | R203M | |||||||
Table 2.
InteliSwab™ limits of detection for SARS-CoV-2 variants.
| Variant | Recombinant Nucleocapsid Protein (ng/mL) | TCID50/mL | Genome Copies/mL | Ct-Value |
|---|---|---|---|---|
| Lineage A | 0.469 | 2.5 × 102 | 5.61 × 105 | 24.85 |
| Alpha | 0.313 | 2.5 × 102 | 6.06 × 105 | 25.16 |
| Beta | 0.469 | 5.0 × 102 | 3.77 × 105 | 25.41 |
| Gamma | 0.313 | 2.5 × 103 | 4.30 × 105 | 25.03 |
| Delta | 0.469 | 5.0 × 102 | 9.13 × 105 | 24.36 |
| Omicron | 0.469 | 5.0 × 102 | 4.51 × 105 | 25.04 |
The sensitivity of the RDT was also evaluated using SARS-CoV-2 virus isolates. Virus stocks were serially diluted 10-fold, starting at 1 × 105 median tissue culture infectious dose (TCID50)/mL, and SARS-CoV-2 genome copy number and cycle-threshold value (Ct value) were determined. Next, 50 µL of each dilution was tested in triplicate. The lowest virus concentration at which all 3 RDTs were positive was 1 × 103 TCID50/mL for all variants except Gamma, which was 1 × 104 TCID50/mL. These lowest virus dilutions with 3 positive RDTs represented Ct values between 21 and 23 and corresponded to genome copy numbers between 7.72 × 106 and 1.59 × 106 copies/mL.
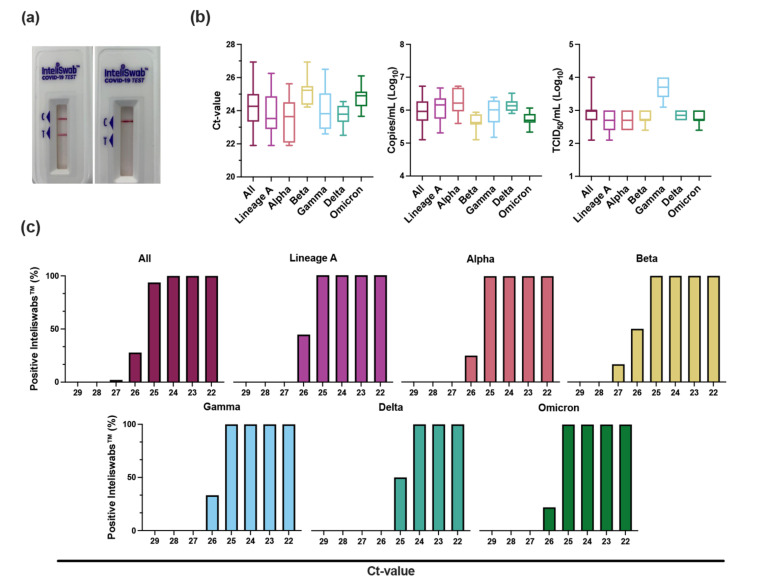
To differentiate further, 2-fold dilutions were performed in triplicate, beginning at the lowest virus concentration with 3 positive RDTs from the 10-fold dilutions described above. Each of these dilutions was then evaluated in triplicate using 50 µL on the RDT. The LOD was defined as the lowest virus concentration with all 9 positive RDTs. The LODs based on TCID50/mL were 2.50 × 102 for both lineage A and Alpha, 5.00 × 102 for Beta, Delta, and Omicron, and 2.50 × 103 for Gamma (Table 2, Figure 1b). For Ct values, the LODs were 24.85 for lineage A, 25.16 for Alpha, 25.41 for Beta, 25.03 for Gamma, 24.36 for Delta, and 25.04 for Omicron (Figure 1c and Figure S2). These values corresponded to genome copies/mL of 5.61 × 105, 6.06 × 105, 3.77 × 105, 4.30 × 105, 9.13 × 105, and 4.51 × 105, respectively.
Figure 1.
InteliSwab™ Test detection ability for SARS-CoV-2 variants. Cell culture stocks of the variants were serially diluted, and viral load was measured by gRNA qRT-PCR. (a) Comparison of a positive InteliSwab™ Test (left) and a negative InteliSwab™ Test (right). (b) Box plots displaying the distribution of positive InteliSwab™ Tests across the 6 variants compared to the Ct values, RNA copies/mL, and TCID50/mL. The positive InteliSwabs™ are from the 2-fold dilution series for each variant (from left to right, N = 145, 31, 27, 19, 30, 18, and 20). Shown is the median, minimum, and maximum. (c) Bar charts representing the percentage of positive InteliSwab™ Tests compared to Ct values. Initial Ct values were rounded to the nearest whole number.
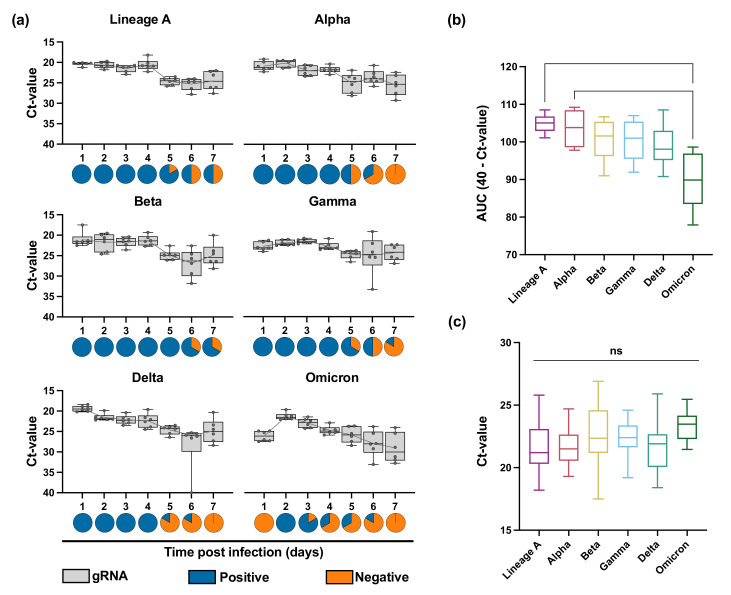
To determine the performance of the RDT in a controlled infection environment, we used the SARS-CoV-2 Syrian hamster model. Six 4–6-week-old male and female Syrian golden hamsters were intranasally inoculated with 1 × 103 TCID50/mL for each variant. Oropharyngeal swabs were collected daily in 1 mL DMEM containing 2% FBS, 2 mM L-glutamine, and 100 units/mL penicillin/streptomycin. Swabs were analyzed by qRT-PCR and tested on the InteliSwab™ (1 RDT per hamster per day, 50 µL). On average, all 6 animals were positive for 4 consecutive days, starting at 1 day post infection (DPI), for lineage A, Alpha, Beta, Gamma, and Delta. For Omicron, however, the RDTs were positive 6/6 on 2 DPI, 5/6 on 3 DPI, and 3/6 on 3 and 4 DPI. At 6 and 7 DPI, the tests were all negative (Figure 2a). This was explained by decreased shedding after Omicron infection as compared to the other variants, and not by decreased test sensitivity (Figure 2b). The overall Ct values of positive RDTs were comparable between the different viruses and were at most 24–26 (Figure 2c). Combined with the reduction in shedding in this animal model, this suggests that the functioning of the RDT is directly related to the infection kinetics within the host.
Figure 2.
InteliSwab™ results for SARS-CoV-2 variants in Syrian golden hamsters. For each variant, animals (N = 6) were inoculated with 1 × 103 TCID50/mL. Oropharyngeal swabs were taken for 7 days. (a) Box plots depicting viral load (gRNA) in swabs across the 7 days; box and whiskers represent the median, minimum, maximum, and individual Ct values. Gray lines represent the mean Ct value of oropharyngeal swabs for each day. Pie charts show results of oropharyngeal swabs tested by InteliSwab™; blue = positive; orange = negative. For b and c, statistical significance was measured by the Kruskal–Wallis test. (b) Box plots showing cumulative (area under the curve (AUC) analysis) respiratory shedding of SARS-CoV-2 variants viral load in oropharyngeal swabs measured by gRNA. Box and whiskers represent the median, minimum, and maximum cumulative respiratory shedding. For lineage A and Omicron, p = 0.0083. For Alpha and Omicron, p = 0.0385. (c) Box plots representing the positive OraSure InteliSwabs™ from all oropharyngeal swabs measured across the 7 days. Box and whiskers represent the median, minimum, and maximum Ct values (from left to right, N = 35, 28, 38, 32, 26, and 10), ns = not significant.
4. Discussion
As SARS-CoV-2 continues to evolve in the human population, there is a concern that diagnostic assays originally designed using the ancestral lineage A strain will not be able to detect new variants. Previous studies have demonstrated no variation in sensitivity for some of the RDT tests between the variants Alpha, Beta, Gamma, Delta, and the ancestral strain [9,10,11,12]. However, only a few studies have included Omicron [13]. Because such a pan-variant of concern antigen test is crucial for public health, there is a need to evaluate RDTs on the current VOCs.
Using recombinant protein and cell-cultured SARS-CoV-2 variants, we observed only minor differences in the sensitivity of the InteliSwab™ for Alpha, Beta, Gamma, Delta, and Omicron compared to the initial lineage A variant. Thus, we conclude that the mutations present in the NPs for the current VOCs do not affect the detection ability of this RDT. In addition, based on Ct values, no difference in sensitivity was observed when using the InteliSwab™ on Syrian golden hamsters experimentally infected with the different VOCs.
When compared to other manufactured RDTs, the InteliSwab™ demonstrated similar sensitivity for lineage A and the VOCs. For example, the commonly used Abbott BinaxNOW™ COVID-19 Antigen Self-Test was initially reported to have a LOD between 8 × 105–2 × 106 genome copies/mL, while the Quidel QuickVue® At-Home OTC COVID-19 Test was determined to have a LOD of 2 × 104 TCID50/mL for lineage A [14,15]. Additionally, when evaluating the sensitivity of 4 other rapid tests, a study found all tests to have a general LOD between 2 × 106–5 × 106 genome copies/mL for lineage A, Alpha, Beta, Gamma, and Delta [9]. Ten rapid tests were also previously shown to be capable of detecting the Omicron variant at 2 × 106 copies/mL [13].
Based on our results, recombinant NP can act as a valuable analytical tool for rapid screening the function of RDTs. Differences in post-translational modification in E. coli expressed NP appear not to impact monoclonal antibodies cross recognition of the de facto proteins clinically. This suggests that recombinant NP could be used as a surrogate to live viral testing and would enable easy routine monitoring of emerging VOCs.
It is worth noting that peak shedding of lineage A, Alpha, Beta, Gamma, and Delta variants, as determined by the lowest Ct value, was observed at 1 DPI, while peak shedding of Omicron was observed at 2 DPI. In addition, shedding with Omicron in the hamster model trailed off faster as compared to the other VOCs. Therefore, the delay in the detection ability of this RDT in the samples obtained from Syrian golden hamsters inoculated with Omicron suggests that the overall temporal dynamics in viral shedding might have an impact on the RDT’s ability to detect infection. Preliminary human data suggest a shift towards a delay in the peak of viral shedding in humans with Omicron, similar to what is shown here in the hamster model [16,17]. This shedding delay could result in an inability for the RDTs to detect a SARS-CoV-2 infection in its early stages.
SARS-CoV-2 has previously shown to have Ct values ranging between 18.77–40 in human oropharyngeal/nasal swabs [18]. While our study is limited by not evaluating the LOD of the InteliSwab™ for human samples, our results support the current rapid antigen testing guidelines made by the Centers for Disease Control and Prevention: a negative result should not be used as a confirmatory result [19].
To conclude, the OraSure InteliSwab™ Test showed comparable sensitivity between the ancestral SARS-CoV-2 strain and all the VOCs including Omicron. Our data would suggest that the InteliSwab™ Test is not affected by the current mutations in the NP; however, it is not clear if future mutations may affect the RDT’s sensitivity. Therefore, there is a need to continuously evaluate existing diagnostic tests. With the potential changes in the temporal dynamics of viral shedding in humans, this should also include the real-world performance of RDTs.
Acknowledgments
We would like to thank Myndi Holbrook, Emmie de Wit, Brandi Williamson, Meaghan Flagg, Kyle Rosenke, Matthew Lewis, Katie Willebrand, Natalie Thornburg, Bin Zhou, Sue Tong, Sujatha Rashid, Ranjan Mukul, Kimberly Stemple, Craig Martens, Kent Barbian, Stacey Ricklefs, Sarah Anzick, and Keith Kardos for critical review and the animal care takers for their assistance during the study. The following reagent was obtained through: CDC, hu/USA/CA_CDC_5574/2020, WA1, BEI Resources, NIAID, NIH: SARS-Related Coronavirus 2, Isolate hCoV-19/England/204820464/2020, NR282 54000, contributed by CDC. Severe Acute Respiratory Syndrome-Related Coronavirus 2, Isolate hCoV-19/England/204820464/20200, NR-54000, contributed by Bassam Hallis. B.1.351 (beta variant) Isolate Name: hCoV-19/USA/MD-HP01542/2021 contributed by John Hopkins Bloomberg School of Public Health: Andrew Pekosz. Omicron Isolate name hCoV-19/USA/WI-WSLH-221686/2021 contributed by University of Wisconsin-Madison: Pete Halfman and Yoshihiro Kawaoka.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/v14030543/s1, Table S1: SARS-CoV-2 isolates used in this study; Figure S1: Evaluation of the effects of irradiation on OraSure InteliSwab™ results; Figure S2: Distribution of all OraSure InteliSwab™ results tested on irradiated sample compared to the RNA copies/mL.
Author Contributions
Conceptualization, J.D.B. and V.J.M.; methodology, N.v.D., J.D.B., V.J.M. and C.K.Y.; formal analysis, Z.A.W., J.C.R., T.A.S. and C.K.Y.; investigation, Z.A.W., J.Y., M.F., R.J.F., I.O.D., J.E.S., J.R.P., N.v.D., J.D.B., V.J.M. and C.K.Y.; writing—original draft preparation, Z.A.W. and C.K.Y.; writing—review and editing, all authors; visualization, Z.A.W., J.C.R., T.A.S. and C.K.Y.; supervision, J.D.B., V.J.M. and C.K.Y.; funding acquisition, J.D.B. and V.J.M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH). The OraSure part of the project has been funded in whole or part with Federal funds from the Department of Health and Human Services; Office of the Assistant Secretary for Preparedness and Response; Biomedical Advanced Research and Development Authority, under contracts No. 75A50120C00061 and 75A50121C00078.
Institutional Review Board Statement
Animal experiments were conducted in an AAALAC International-accredited facility and were approved by the Rocky Mountain Laboratories Institutional Care and Use Committee following the guidelines put forth in the Guide for the Care and Use of Laboratory Animals 8th edition, the Animal Welfare Act, United States Department of Agriculture and the United States Public Health Service Policy on the Humane Care and Use of Laboratory Animals. The Institutional Biosafety Committee (IBC) approved work with infectious SARS-CoV-2 virus strains under BSL3 conditions. Virus inactivation of all samples was performed according to IBC-approved standard operating procedures for the removal of specimens from high containment areas.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data have been deposited in Figshare with https://www.doi.org/10.6084/m9.figshare.19224939.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Boger B., Fachi M.M., Vilhena R.O., Cobre A.F., Tonin F.S., Pontarolo R. Systematic review with meta-analysis of the accuracy of diagnostic tests for COVID-19. Am. J. Infect. Control. 2021;49:21–29. doi: 10.1016/j.ajic.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheng M.P., Papenburg J., Desjardins M., Kanjilal S., Quach C., Libman M., Dittrich S., Yansouni C.P. Diagnostic Testing for Severe Acute Respiratory Syndrome-Related Coronavirus 2: A Narrative Review. Ann. Intern. Med. 2020;172:726–734. doi: 10.7326/M20-1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rezaei M., Razavi Bazaz S., Zhand S., Sayyadi N., Jin D., Stewart M.P., Ebrahimi Warkiani M. Point of Care Diagnostics in the Age of COVID-19. Diagnostics. 2020;11:9. doi: 10.3390/diagnostics11010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song Q., Sun X., Dai Z., Gao Y., Gong X., Zhou B., Wu J., Wen W. Point-of-care testing detection methods for COVID-19. Lab Chip. 2021;21:1634–1660. doi: 10.1039/D0LC01156H. [DOI] [PubMed] [Google Scholar]
- 5.Suleman S., Shukla S.K., Malhotra N., Bukkitgar S.D., Shetti N.P., Pilloton R., Narang J., Nee Tan Y., Aminabhavi T.M. Point of care detection of COVID-19: Advancement in biosensing and diagnostic methods. Chem. Eng. J. 2021;414:128759. doi: 10.1016/j.cej.2021.128759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsiao W.W., Le T.N., Pham D.M., Ko H.H., Chang H.C., Lee C.C., Sharma N., Lee C.K., Chiang W.H. Recent Advances in Novel Lateral Flow Technologies for Detection of COVID-19. Biosensors. 2021;11:295. doi: 10.3390/bios11090295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tracking SARS-CoV-2 Variants. [(accessed on 24 January 2022)]. Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
- 8.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K., Bleicker T., Brunink S., Schneider J., Schmidt M.L., et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro. Surveill. 2020;25:2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jungnick S., Hobmaier B., Mautner L., Hoyos M., Haase M., Baiker A., Lahne H., Eberle U., Wimmer C., Hepner S., et al. In Vitro Rapid Antigen Test Performance with the SARS-CoV-2 Variants of Concern, B.1.1.7 (Alpha), B.1.351 (Beta), P.1 (Gamma), and B.1.617.2 (Delta) Microorganisms. 2021;9:1967. doi: 10.3390/microorganisms9091967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kontogianni K., Cubas-Atienzar A.I., Wooding D., Buist K., Thompson C.R., Williams C.T., Baldwin L., Escadafal C., Sacks J.A., Adams E.R., et al. Lateral flow antigen tests can sensitively detect live cultured virus of the SARS-CoV-2 B1.1.7 lineage. J. Infect. 2021;83:e1–e4. doi: 10.1016/j.jinf.2021.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Osterman A., Iglhaut M., Lehner A., Spath P., Stern M., Autenrieth H., Muenchhoff M., Graf A., Krebs S., Blum H., et al. Comparison of four commercial, automated antigen tests to detect SARS-CoV-2 variants of concern. Med. Microbiol. Immunol. 2021;210:263–275. doi: 10.1007/s00430-021-00719-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pickering S., Batra R., Merrick B., Snell L.B., Nebbia G., Douthwaite S., Reid F., Patel A., Kia Ik M.T., Patel B., et al. Comparative performance of SARS-CoV-2 lateral flow antigen tests and association with detection of infectious virus in clinical specimens: A single-centre laboratory evaluation study. Lancet Microbe. 2021;2:e461–e471. doi: 10.1016/S2666-5247(21)00143-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deerain J., Druce J., Tran T., Batty M., Yoga Y., Fennell M., Dwyer D.E., Kok J., Williamson D.A. Assessment of the analytical sensitivity of ten lateral flow devices against the SARS-CoV-2 omicron variant. J. Clin. Microbiol. 2021;60:jcm0247921. doi: 10.1128/jcm.02479-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perchetti G.A., Huang M.L., Mills M.G., Jerome K.R., Greninger A.L. Analytical Sensitivity of the Abbott BinaxNOW COVID-19 Ag Card. J. Clin. Microbiol. 2021;59:e02880-20. doi: 10.1128/JCM.02880-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.In Vitro Diagnostics EUAs–Antigen Diagnostic Tests for SARS-CoV-2. [(accessed on 8 February 2022)]; Available online: https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/in-vitro-diagnostics-euas-antigen-diagnostic-tests-sars-cov-2.
- 16.National Institute of Infectious Diseases Disease Control. Prevention Center NCfGHaM Active Epidemiological Investigation on SARS-CoV-2 Infection Caused by Omicron Variant (Pango Lineage B.1.1.529) in Japan: Preliminary Report on Infectious Period; Japan. 2022. [(accessed on 8 February 2022)]. Available online: https://www.niid.go.jp/niid/en/2019-ncov-e/10884-covid19-66-en.html.
- 17.He X., Lau E.H.Y., Wu P., Deng X., Wang J., Hao X., Lau Y.C., Wong J.Y., Guan Y., Tan X., et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- 18.Toptan T., Eckermann L., Pfeiffer A.E., Hoehl S., Ciesek S., Drosten C., Corman V.M. Evaluation of a SARS-CoV-2 rapid antigen test: Potential to help reduce community spread? J. Clin. Virol. 2021;135:104713. doi: 10.1016/j.jcv.2020.104713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Interim Guidance for Antigen Testing for SARS-CoV-2. [(accessed on 8 February 2022)]; Available online: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html#anchor_1631295114633.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data have been deposited in Figshare with https://www.doi.org/10.6084/m9.figshare.19224939.