Abstract
Background and aims
South Asian (SA) ethnicity is associated with an increased risk of atherosclerotic cardiovascular disease (ASCVD). However, the implications of considering SA ethnicity as a “risk-enhancing factor” per recent American College of Cardiology/American Heart Association guidelines are not fully understood.
Methods
We used data from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study, a community-based cohort study of individuals of SA ancestry living in the US. The Pooled Cohort Equations were used to estimate 10-year ASCVD risk. Metabolic risk factors and coronary artery calcium (CAC) scores were assessed.
Results
Among 1,114 MASALA participants included (median age 56 years, 48% women), 28% were already using a statin at baseline, 25% had prevalent diabetes, and 59% qualified for 10-year ASCVD risk assessment for statin allocation purposes. The prevalence of low, borderline, intermediate, and high estimated ASCVD risk was 65%, 11%, 20% and 5%, respectively. Among participants at intermediate risk, 30% had CAC=0 and 37% had CAC>100, while among participants at borderline risk, 54% had CAC=0 and 13% had CAC>100. Systematic consideration of intermediate and, particularly, of borderline risk individuals as statin candidates would enrich the statin-consideration group with CAC=0 participants up to 35%. Prediabetes and abdominal obesity were highly prevalent across all estimated risk strata, including among those with CAC=0.
Conclusions
Our findings suggest that systematic consideration of borderline-risk SAs as statin candidates might result in considerable overtreatment, and further risk assessment with CAC may help better personalize statin allocation in these individuals. Early, aggressive lifestyle interventions aimed at reducing the risk of incident diabetes should be strongly recommended in US SAs, particularly among those considered candidates for statin therapy for primary prevention. Longitudinal studies are needed to confirm the favorable prognosis of CAC=0 in SAs.
Keywords: atherosclerosis, cardiovascular disease, coronary artery calcium, diabetes, guidelines, prediabetes, risk assessment, statins, South Asian
1. Introduction
South Asian (SA) ethnicity is associated with an increased risk of atherosclerotic cardiovascular disease (ASCVD) events, particularly ischemic coronary heart disease, compared to most other racial/ethnic groups. This has been consistently reported in studies conducted in the SA subcontinent,1 multinational comparative analyses,2 and epidemiological studies in countries with large SA immigrant populations.3-8
In a commendable attempt to improve the prevention of ASCVD in the large, rapidly growing SA population living in the US,9,10 the 2018 and 2019 American College of Cardiology/American Heart Association (ACC/AHA) Cholesterol and Primary Prevention Guidelines included SA ethnicity among their “risk enhancing factors”.11,12 These are features associated with increased average ASCVD risk that may be used to enrich clinician-patient discussions of individuals considered borderline or intermediate risk after clinical risk estimation. Typically, presence of risk-enhancing factors will result in a stronger consideration for statin therapy initiation.11,12
Recent studies have shown, however, that there is marked risk heterogeneity among individuals at intermediate risk and with up to three risk enhancing factors (other than SA ethnicity). Specifically, a coronary artery calcium (CAC) score of zero is highly prevalent in these individuals, and is associated with low ASCVD event rates.13,14 These findings suggest that even among individuals with prevalent risk enhancing features there is room for further risk assessment, potentially with tools such as CAC, for a more personalized allocation of chronic preventive statin therapy.15 In this context, whether this may also apply to SA ethnicity has not yet been assessed in the context of the 2018/2019 ACC/AHA guideline recommendations.
We therefore sought to describe, in the largest-to-date US cohort study of SA individuals free of clinical ASCVD at baseline, the implications of implementing the 2018/2019 ACC/AHA recommendations for ASCVD risk assessment in SAs and of considering SA ethnicity as a risk-enhancing feature. The burden of coronary atherosclerosis was assessed using the CAC score, which has been shown to be a robust predictor of ASCVD events in 4 US racial-ethnic groups16 and is a guideline-recommended aid for further risk assessment in borderline/intermediate risk individuals.11,12 We also described the burden of cardiovascular risk factors with special attention to characteristics associated with increased risk of incident diabetes, such as pre-diabetes and abdominal obesity.17-20 We hypothesized that a non-negligible proportion of SAs considered statin candidates under the risk enhancer approach would be at low absolute ASCVD risk, while at high risk of developing diabetes.
2. Patients and methods
2.1. The Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study
MASALA is an NIH/NHLBI-funded, community-based, observational, prospective cohort study of individuals of SA ancestry recruited from the greater San Francisco Bay (CA) and Chicago (IL) areas.21,22 The first baseline study visit (Visit 1) took place between October 2010 and March 2013 and recruited most participants (78%). A second baseline visit (Visit 1A) took place between March 2017 and March 2018 (22% participants), aimed at enriching the study population with people of lower income and from SA countries other than India; as well as at increasing overall sample size and statistical power. All MASALA participants were expected to be free from clinically overt ASCVD at study entry, although very few prevalent cases of ASCVD were detected during the baseline study examinations (all excluded from the present analysis). MASALA participants are currently being followed for incident ASCVD events, with longitudinal data expected to become available in the coming years.
The study protocol was approved by the Institutional Review Boards of Northwestern University, Chicago (IL) and the University of California, San Francisco (CA), and written informed consent was obtained from all participants before study entry. Further details on the MASALA study have been published elsewhere,21,22 and are available on the study website (https://www.masalastudy.org/).
2.2. Study design and population
We conducted a cross-sectional analysis pooling data from both MASALA baseline visits (1 and 1A). We excluded individuals with missing CAC scores, participants younger than 40 or older than 75 years of age (the Pooled Cohort Equations [PCE] are recommended for 10-year ASCVD risk estimation in individuals ages 40 to 75 years11,12), participants with missing data on any of the variables used by the PCE, and individuals with prevalent ASCVD (Figure 1).
Figure 1.
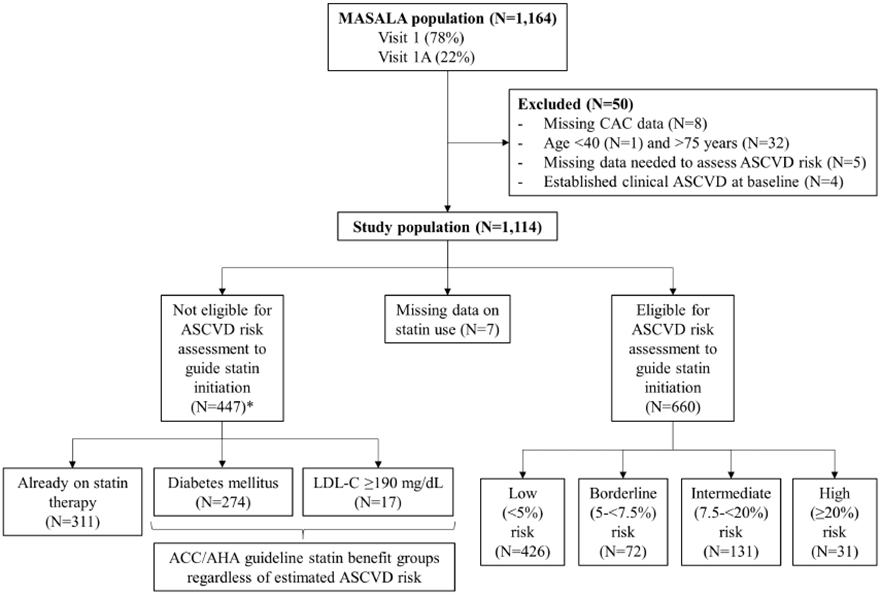
Flow of the population included in the study.
Categories are not mutually exclusive. 10-year ASCVD risk was estimated using the Pooled Cohort Equations for non-Hispanic Whites. Estimated risk categories were defined using the 2018/2019 ACC/AHA guideline thresholds: low (<5%), borderline (5 – <7.5%), intermediate (7.5% – <20%) and high (≥20%) risk. ACC/AHA = American College of Cardiology/American Heart Association; ACC/AHA = American College of Cardiology/American Heart Association; ASCVD = atherosclerotic cardiovascular disease events; CAC = coronary artery calcium; LDL-C = low-density lipoprotein cholesterol; MASALA = Mediators of Atherosclerosis in South Asians Living in America; N = number.
For analyses on the interplay between ASCVD risk estimations, statin consideration groups, CAC burden, and clinical ASCVD risk factors, we also excluded individuals already using a statin, and those with diabetes or low-density lipoprotein (LDL) cholesterol levels ≥190 mg/dL. The latter two groups are considered to benefit from statins regardless of their estimated ASCVD risk in current ACC/AHA Cholesterol and Primary Prevention Guidelines.11,12
2.3. Estimation of ASCVD risk
Ten-year risk of ASCVD events was estimated in all participants qualifying for ASCVD risk estimation for statin initiation purposes using the PCE. In the absence of SA-specific equations, the equations for non-Hispanic white men and women were used per ACC/AHA guideline recommendations.11,12 Based on these estimations, participants were classified as having low (<5%), borderline (5 to <7.5%), intermediate (7.5 to <20%) or high (≥20%) 10-year ASCVD risk.
2.4. Measurement and quantification of CAC
CAC was measured at both baseline visits following a common computed tomography protocol, adapted to both electron-beam and multi-detector scans.21 CAC was quantified using the Agatston score.23 For the present analyses, CAC was categorized as 0, 1-100, and >100.
2.5. Other variables and definitions
Baseline information on sociodemographic characteristics and cardiovascular risk factors was collected in both MASALA baseline visits using standardized procedures.21,22 A questionnaire was administered to capture information on age, sex, country of birth, highest educational attainment, family income, tobacco use, and medical conditions. Use of medications and supplements was identified using inventories for each study participant. Blood pressure was measured thrice in the seated resting position, with the mean of the last 2 readings used for analyses. Waist circumference was measured by trained study personnel using a flexible tape measure at the site of maximum circumference, halfway between the lower ribs and the anterior superior iliac spine. The average of two consecutive measures was used. Nurses or certified phlebotomists performed phlebotomy to obtain nearly 100 mL of blood from individuals while fasting, and levels of total and high density lipoprotein cholesterol, triglycerides, glucose and glycosylated hemoglobin (HbA1c) were measured in a central laboratory using standard procedures.21
For the present analysis, participants were considered to have diabetes if they met any of the following criteria:24 1) fasting blood glucose ≥126 mg/dL, 2) HbA1c >6.5%, or 3) medication use for diabetes. Prediabetes was defined as either 1) glucose levels 100 – 125 mg/dL or 2) HbA1c ≥5.7% and <6.5%. Although it has been proposed that HbA1c may overestimate the prevalence of diabetes and pre-diabetes in SAs,25 it was included in our definitions following current American Diabetes Association recommendations.24 Abdominal obesity was defined using the World Health Organization’s cut-points for SAs, i.e., a waist circumference >80 cm for women, and a waist circumference >90 cm for men.26 Consistent with prior analyses in the MASALA population, a yearly family income >75,000 USD was used to define high family income.21,27
2.6. Statistical analyses
We calculated the number and proportion of MASALA participants who were already taking a statin at baseline, the prevalence of diabetes, and the prevalence of LDL cholesterol levels ≥190 mg/dl.
For participants qualifying for ASCVD risk estimation for statin initiation purposes (i.e., with none of those three characteristics), we described their baseline characteristics, overall and by estimated ASCVD risk, including sociodemographic features, clinical cardiovascular risk factors, and CAC burden. Categorical variables were summarized using absolute count and percentage, and continuous variables were summarized using mean and standard deviation or median and interquartile range. For statistical comparisons across estimated ASCVD risk categories, we used chi-squared tests for categorical variables, and ANOVA and Kruskal-Wallis tests for continuous variables, as appropriate.
We then described the frequency of statin consideration and its interplay with CAC after considering SA ethnicity as a risk enhancing factor in borderline and intermediate risk individuals. To model this analysis, we considered 3 scenarios: a) assuming that only participants with high estimated ASCVD risk would be considered for statin therapy, b) assuming that all intermediate estimated risk individuals would also be considered for statin therapy, and c) also considering all borderline risk participants as statin candidates. In each of those scenarios, we described the distribution of CAC categories in the resulting “statin-recommended” group.
We also calculated the number and proportion of MASALA participants qualifying for ASCVD risk assessment with CAC=0, CAC 1-100 and CAC>100, respectively, who would be considered statin-recommended in each of those three scenarios. Finally, we described the risk factor profile of those individuals.
All analyses were conducted using Stata software, version 15.28 A p value of <0.05 was used as threshold to define statistical significance.
3. Results
3.1. Study participants
Of the 1,164 participants from MASALA, 50 were excluded from the present analysis (Figure 1). This defined a study population of 1,114 SAs free of established ASCVD, with a median age of 56 years (interquartile range 49 – 63) and 48% of whom were women.
3.2. Eligibility for 10-year ASCVD risk estimation for statin initiation purposes
Overall, 28% participants were already taking a statin, 25% had prevalent diabetes, and 1.5% had LDL cholesterol levels ≥190 mg/dL. This defined a total of 447 study participants (41%) who were either prevalent statin users or would be considered to benefit from statins regardless of their estimated ASCVD risk. Also, a total of 7 participants had missing data on statin use. The remaining 660 (59%) participants would qualify for 10-year ASCVD risk assessment for statin allocation purposes according to current ACC/AHA Guidelines.
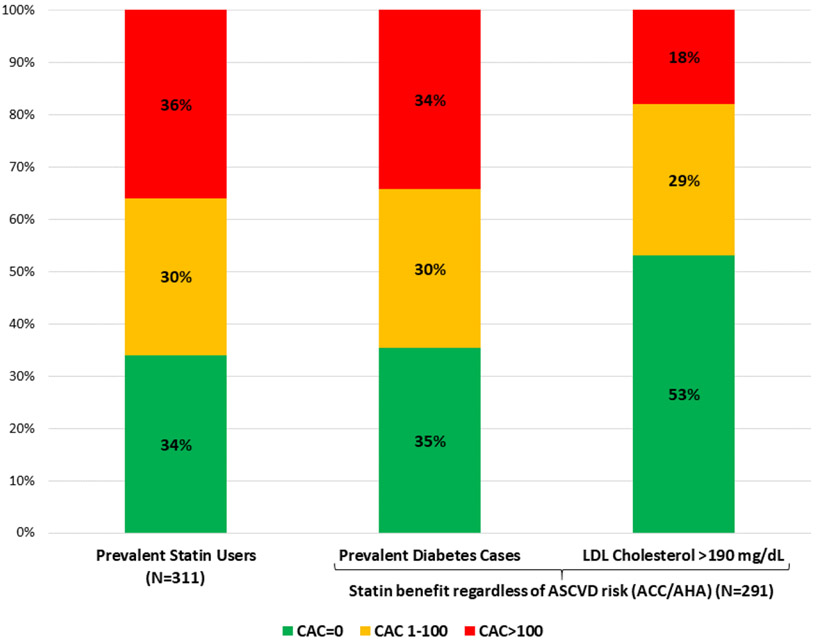
3.3. Characteristics of participants already taking a statin or considered to benefit from statins regardless of ASCVD risk
Figure 2A displays the baseline CAC burden of these individuals (N=447). The prevalence of CAC>100 ranged from 18% in participants with LDL cholesterol ≥190 mg/dL to 35% in those with diabetes. The prevalence of CAC=0 was similar to that of CAC>100 in individuals using a statin as well as in those with diabetes, while it was almost 3-fold higher than CAC>100 in participants with LDL cholesterol >190 mg/dL.
Figure 2.
(A) Burden of CAC among MASALA participants either taking statins at baseline or considered to benefit from statins regardless of ASCVD risk according to current ACC/AHA guidelines.
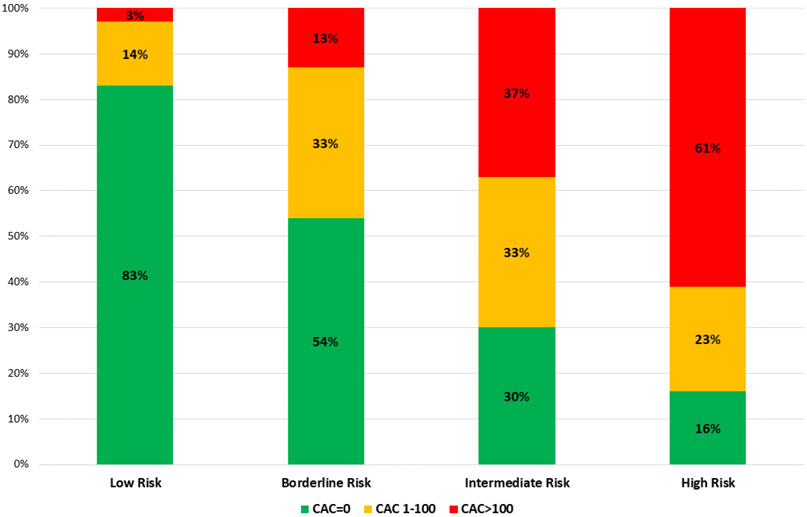
Categories are not mutually exclusive. ACC/AHA = American College of Cardiology/American Heart Association; ASCVD = atherosclerotic cardiovascular disease events; CAC = coronary artery calcium; LDL = low-density lipoprotein; MASALA = Mediators of Atherosclerosis in South Asians Living in America. (B) Burden of CAC among MASALA participants qualifying for ASCVD risk assessment for statin initiation purposes, by estimated ASCVD risk categories. 10-year ASCVD risk was estimated using the Pooled Cohort Equations for non-Hispanic Whites. Estimated risk categories were defined using the 2018/2019 ACC/AHA guideline thresholds: low (<5%), borderline (5 – <7.5%), intermediate (7.5% – <20%) and high (≥20%) risk. ACC/AHA = American College of Cardiology / American Heart Association; ASCVD = atherosclerotic cardiovascular disease events; CAC = coronary artery calcium; MASALA = Mediators of Atherosclerosis in South Asians Living in America
3.4. Characteristics of participants qualifying for ASCVD risk assessment for statin allocation
Overall, the median age of these individuals (N=660) was 54 years, and 55% were women (Table 1). High educational level and high family income were both very frequent. The prevalence of current tobacco use was very low (3%) and 19% used medications for hypertension. Of note, 61% had prediabetes (median HbA1c 5.7%), and almost 4 out of 5 had abdominal obesity (79%).
Table 1.
Characteristics of MASALA participants qualifying for 10-year ASCVD risk assessment for statin allocation purposes.
| Overall | 10-year estimated ASCVD risk* |
|||||
|---|---|---|---|---|---|---|
| Low (<5%) |
Borderline (5-7.5%) |
Intermediate (7.5-20%) |
High (≥20%) |
p value | ||
| Number (%) | 660 (100) | 426 (64.6) | 72 (10.9) | 131 (19.9) | 31 (4.7) | |
| Age, years | 54 (48, 61) | 50 (45, 54) | 56 (53, 61) | 63 (60, 67) | 71 (68, 74) | <0.001 |
| Women | 360 (54.5) | 308 (72.3) | 18 (25.0) | 30 (22.9) | 4 (12.9) | <0.001 |
| Education ≥ Bachelor’s | 578 (87.6) | 371 (87.1) | 61 (84.7) | 119 (90.8) | 27 (87.1) | 0.589 |
| High family income* | 412 (64.5) | 288 (69.7) | 42 (60.0) | 69 (54.8) | 13 (43.3) | 0.006 |
| Abdominal obesity† | 523 (79.2) | 337 (79.1) | 58 (80.6) | 106 (80.9) | 22 (71.0) | 0.661 |
| Fasting glucose, mg/dL | 92 (86, 98) | 90 (85, 96) | 94 (89, 102) | 93 (89, 100) | 98 (90, 107) | <0.001 |
| HbA1c, % | 5.7 (5.5, 5.9) | 5.7 (5.5, 5.9) | 5.8 (5.5, 6.0) | 5.7 (5.5, 5.9) | 5.7 (5.5, 6.0) | 0.108 |
| Prediabetes‡ | 401 (60.8) | 241 (56.6) | 53 (73.6) | 82 (62.6) | 25 (80.7) | 0.004 |
| Total cholesterol, mg/dL | 196 (31) | 196 (30) | 196 (32) | 194 (32) | 197 (37) | 0.928 |
| HDL cholesterol, mg/dL | 49 (41, 59) | 52 (44, 62) | 43 (36, 50) | 44 (39, 54) | 45 (37, 55) | <0.001 |
| Triglycerides, mg/dL | 114 (87, 151) | 110 (83, 144) | 137 (102, 173) | 119 (89, 158) | 114 (83, 155) | <0.001 |
| Systolic blood pressure, mmHg | 124 (16) | 120 (14) | 126 (14) | 133 (16) | 142 (16) | <0.001 |
| Diastolic blood pressure, mmHg | 74 (10) | 72 (10) | 76 (11) | 78 (10) | 79 (11) | <0.001 |
| Hypertension medication use | 125 (18.9) | 44 (10.3) | 13 (18.1) | 49 (37.4) | 19 (61.3) | <0.001 |
| Current smoker | 21 (3.2) | 3 (0.7) | 5 (6.9) | 10 (7.6) | 3 (9.7) | <0.001 |
| Estimated 10-year ASCVD risk§ | 3.0 (1.3, 7.1) | 1.6 (1.0, 2.9) | 6.0 (5.4, 6.6) | 11.0 (9.0, 14.0) | 23.8 (21.1, 26.0) | <0.001 |
Family income ≥ 75,000 USD per year.
Waist circumference >80 cm for women or >90 cm for men.
Glucose levels 100 – 125 mg/dL or HbA1c ≥5.7% and <6.5%.
Estimated using the Pooled Cohort Equations for non-Hispanic Whites.
Categorical variables are presented as number (%), and continuous variables are presented as mean (standard deviation) or median (interquartile range).
ASCVD = atherosclerotic cardiovascular disease events; HbA1c = glycosylated hemoglobin; HDL = high-density lipoprotein; MASALA = Mediators of Atherosclerosis in South Asians Living in America
The most frequent estimated 10-year ASCVD risk stratum was low (65% prevalence), followed by intermediate risk (20%), and 72 (11%) participants were classified as having borderline estimated ASCVD risk. Conversely, the high-risk stratum was the least frequent (5% prevalence). The higher the estimated ASCVD risk, the older the age, the more frequent the male sex, the lower the family income, and the worse the profile for most traditional risk factors (Table 1).
Overall, 435 of these participants (66%) had CAC=0, 135 (20%) had CAC 1-100, and 90 (14%) had CAC>100. The higher the estimated ASCVD risk the higher the CAC burden, with a highest prevalence of CAC>100 observed in those at high estimated ASCVD risk (61%) and a highest prevalence of CAC=0 observed among low risk participants (83%) (Figure 2B). Among participants considered at intermediate risk, 30% had CAC=0 while 37% had CAC>100, and among participants at borderline risk, 54% had CAC=0 while 13% had CAC>100.
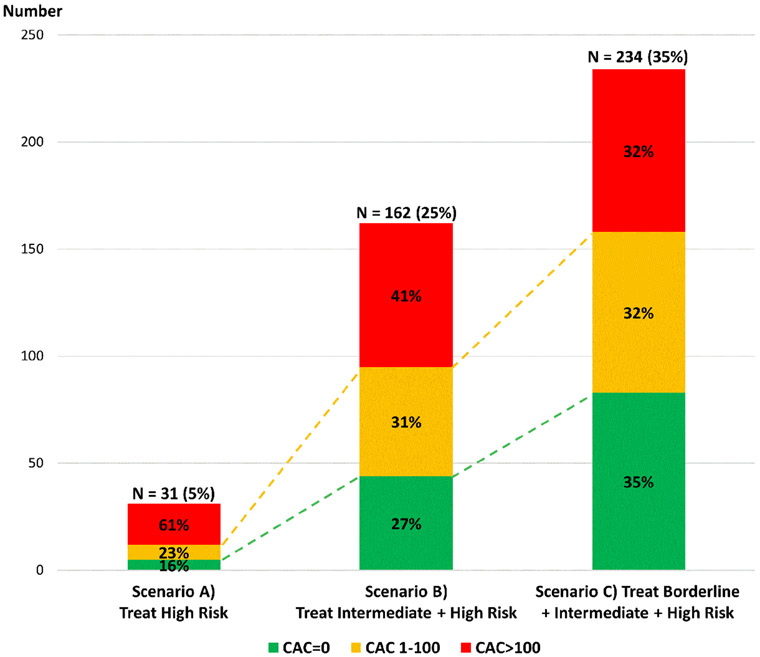
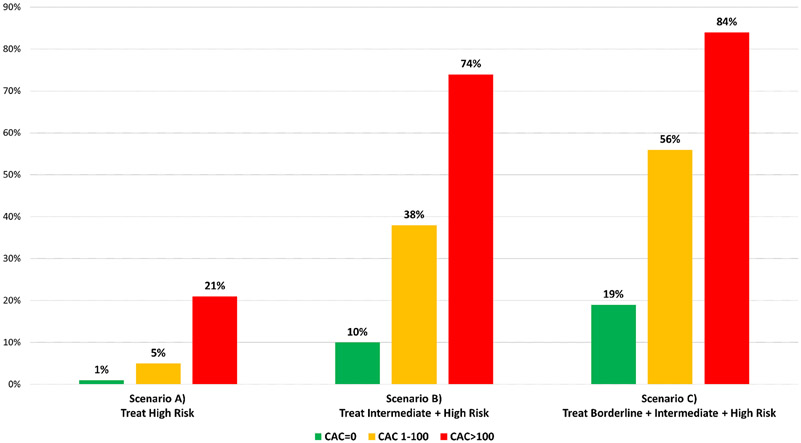
3.5. Implications of using SA ethnicity as a risk-enhancing factor in participants at intermediate estimated risk
If all participants at intermediate and high estimated 10-year ASCVD risk were considered candidates for statin therapy, a total of 162 (25%) participants qualifying for ASCVD risk assessment would be considered statin-recommended. The prevalence of CAC>100 in this group was 41%, while 27% had CAC=0 (Figure 3A). Compared to only considering individuals at high risk, consideration for statin therapy also of those at intermediate risk would increase the absolute number of CAC>100 participants who would be treated with statins from 19 (21% of all with CAC>100) to 67 (74% of all with CAC>100) (Figures 3A and B). The number of individuals with CAC=0 who would be treated with statins would increase from 5 (1% of all participants with CAC=0) to 44 (10% of participants with CAC=0).
Figure 3.
Distribution of CAC scores among participants who would be considered statin-recommended using SA ethnicity as a risk enhancing factor (A), and proportion of participants qualifying for ASCVD risk assessment who would be considered statin-recommended using SA ethnicity as a risk enhancing factor, by CAC score (B).
10-year ASCVD risk was estimated using the Pooled Cohort Equations for non-Hispanic Whites. Estimated risk categories were defined using the 2018/2019 ACC/AHA guideline thresholds: borderline (5 – <7.5%), intermediate (7.5% – <20%) and high (≥20%) risk. ACC/AHA = American College of Cardiology / American Heart Association; ASCVD = atherosclerotic cardiovascular disease events; CAC = coronary artery calcium; MASALA = Mediators of Atherosclerosis in South Asians Living in America
3.6. Implications of using SA ethnicity as a risk-enhancing factor in participants at borderline estimated risk
If the 72 participants at borderline estimated risk were also considered candidates for statin therapy, this would define a total of 234 (35%) participants qualifying for ASCVD risk assessment who would be considered statin-recommended. Of these, 32% had CAC>100, while 35% had CAC=0 (Figure 3A). This approach increased the absolute number of CAC>100 participants who would be treated with statins from 67 to 76 (84% of all participants with CAC>100), while the number of individuals with CAC=0 who would be treated with statins would increase from 44 to 83 (19% of participants with CAC=0) (Figures 3A and B).
3.7. Risk factors for incident diabetes among statin candidates with CAC=0
The prevalence of prediabetes in the intermediate + high estimated risk group was 66% overall (59% in the CAC=0 subgroup) and the median HbA1c was 5.7% (Table 2). The prevalence of abdominal obesity was also very high in these individuals (79% and 81.8%, respectively). The prevalence of prediabetes and abdominal obesity was also high in the borderline + intermediate + high estimated risk group, as well as specifically among those with CAC=0.
Table 2.
Distribution of key cardiovascular risk factors among MASALA participants who would be considered statin-recommended using SA ethnicity as a risk enhancing factor.
| Intermediate + high | Borderline + intermediate + high | |||
|---|---|---|---|---|
| estimated ASCVD risk* | estimated ASCVD risk* | |||
| Overall | CAC=0 | Overall | CAC=0 | |
| Number (%) | 162 (100) | 44 (27.2) | 234 (100) | 83 (35.4) |
| Age, years | 65 (61, 69) | 63 (59, 68) | 62 (57, 67) | 60 (54, 66) |
| Women | 34 (21.0) | 12 (27.3) | 52 (22.2) | 21 (25.3) |
| Abdominal obesity† | 128 (79.0) | 36 (81.8) | 186 (79.5) | 65 (78.3) |
| Fasting glucose, mg/dL | 94 (89, 101) | 93 (88, 98) | 94 (89, 101) | 92 (87, 99) |
| HbA1c, % | 5.7 (5.5, 5.9) | 5.7 (5.5, 5.9) | 5.7 (5.5, 5.9) | 5.7 (5.5, 5.9) |
| Prediabetes‡ | 107 (66.1) | 25 (59.1) | 160 (68.4) | 57 (68.8) |
| Total cholesterol, mg/dL | 195 (33) | 189 (26) | 195 (32) | 192 (27) |
| HDL cholesterol, mg/dL | 45 (39, 54) | 43 (40, 53) | 44 (37, 53) | 43 (38, 51) |
| Triglycerides, mg/dL | 118 (88, 157) | 142 (98, 168) | 123 (91, 164) | 135 (97, 172) |
| Hypertension medication use | 68 (42.0) | 16 (36.4) | 81 (34.6) | 22 (26.5) |
Estimated using the Pooled Cohort Equations for non-Hispanic Whites.
Waist circumference >80 cm for women or >90 cm for men.
Glucose levels 100 – 125 mg/dL or HbA1c ≥5.7% and <6.5%.
Categorical variables are presented as number (%), and continuous variables are presented as mean (standard deviation) or median (interquartile range). ASCVD = atherosclerotic cardiovascular disease events; HbA1c = glycosylated hemoglobin; HDL = high-density lipoprotein; MASALA = Mediators of Atherosclerosis in South Asians Living in America
4. Discussion
In the largest-to-date community-based US cohort of SA adults 40 years of age or older and free of clinical ASCVD, 28% were already using a statin at baseline, 25% had prevalent diabetes, and only 59% would qualify for 10-year ASCVD risk assessment for statin initiation purposes. Using the PCE in the latter individuals, participants with a low (<5%) estimated ASCVD risk were the majority (65%) and had a very high prevalence of CAC=0, while there were few with high-risk estimations (5%), most of whom had CAC>100. CAC=0 was present in 30% participants with intermediate estimated risk, and in 54% of those at borderline risk. Systematic consideration for preventive statin therapy of all SAs at intermediate and particularly at borderline estimated risk would significantly enrich the statin-consideration group with individuals with CAC=0 (35%). In parallel, the prevalence of features associated with a high risk of incident diabetes, such as prediabetes and abdominal obesity, was very high across all estimated risk strata, including among participants at borderline/intermediate estimated ASCVD risk with CAC=0. These findings have implications for risk assessment strategies, guideline recommendations, and public heath interventions aimed at improving the prevention of ASCVD in SA men and women living in the US.
The high prevalence of CAC>100 (37%) and particularly of CAC>0 (70%) observed among participants at intermediate risk, together with the marked increase in the absolute number of CAC>100 participants who would be treated (as compared to treating only those at high estimated risk), provides further support to considering statin therapy for primary prevention purposes in these individuals. Nevertheless, it must also be noted that 30% of them had CAC=0. Although data on incident events are still not available in MASALA, prior analyses of Multi-Ethnic Study of Atherosclerosis (MESA) participants at intermediate risk and with up to three risk enhancing features reported low ASCVD event rates if CAC=0.13,14 Moreover, analyses in MESA and other cohorts with low baseline statin use have reported low 10-year event rates also among individuals with CAC=0 and prediabetes/metabolic syndrome, which are frequent risk factors in non-diabetic SAs.29,30 Therefore, should the “power of zero” be confirmed also in US SAs,31,32 rather than a systematic recommendation to consider statins in all SAs at intermediate risk, use of additional risk stratification tools such as the CAC score could aid in a more personalized allocation of preventive medications, also in this group.
Among participants at borderline estimated risk, the frequency of CAC=0 was 4-fold that of CAC>100. This is the group in which consideration of SA ethnicity as a risk enhancing factor is likely to make the greatest difference in terms of changing risk management, resulting in a statin recommendation. Again, because the prevalence of non-calcified plaque and its importance in the genesis of ASCVD events in SA individuals are currently unknown, longitudinal analyses are needed to better understand the prognostic implications of CAC=0 in this ethnic group. For now, our findings suggest that systematic use of statins in US SA individuals at borderline estimated risk might lead to considerable overtreatment.
Potential explanations to the high burden of CAC=0 in this SA study population, including among those at borderline/estimated risk and those already treated with statins, stem from the characteristics of the SA population in the US as well as of those of the MASALA study. US SAs represent on average a highly educated and high-income SA subgroup.33,34 Moreover, the majority are of Indian origin, and international studies suggest that Indians comprise a lower-risk SA subgroup compared to people from Pakistan and Bangladesh.35-37 Consistent with these trends, the population included in the initial MASALA study also comprised a wealthy, highly educated, mostly Indian SA cohort.21,22 In the coming years, MASALA will be expanded to include additional 1,150 participants from Pakistan and Bangladesh, both of which are rapidly growing groups in the US believed to shoulder a higher burden of coronary heart disease. In addition, exclusion of individuals with established clinical ASCVD after age 40 years further selected a relatively healthy SA subpopulation in MASALA. Finally, it must be noted that a 30-40% prevalence of CAC=0 has been reported even in middle-aged populations with diabetes or severe hypercholesterolemia.38
Of note, we also observed a very high prevalence of risk factors predisposing to the development of diabetes among borderline and intermediate risk SAs, particularly abdominal obesity and prediabetes. Because statins slightly accelerate the development of diabetes in predisposed persons,11,12 our findings suggest that statin-based preventive interventions in SAs should be coupled with aggressive lifestyle interventions, aimed at increasing physical activity, reducing abdominal fat, and reducing the intake of simple carbohydrates, as means to reduce cardiovascular risk and the odds of developing diabetes in subsequent years. Potentially, these lifestyle improvements could be the central focus of the preventive intervention among borderline/intermediate SAs with CAC=0, while statin therapy could perhaps be reassessed later. More generally, the concerningly high prevalence of prediabetes and of abdominal obesity observed in the overall MASALA population further stresses the need for early, aggressive primordial interventions aimed at preventing the development of these risk factors, as crucial steps towards curtailing the pandemic of ASCVD in US SAs.
4.1. Study limitations
Some limitations of the present study are worth discussing. First, as described above, the current lack of incident ASCVD data in MASALA mandates caution when extrapolating the protective prognosis associated with CAC=0 to SA populations. Nonetheless, the favorable prognosis associated with CAC=0 in MESA participants with other risk enhancing factors is reassuring.13,14 Moreover, the favorable prognosis of CAC=0 has also been confirmed in multiple other populations, including those considered at increased ASCVD risk.38
Second, we used the PCE equations for non-Hispanic Whites to estimate ASCVD risk in SAs. Although this is the approach recommended by the ACC/AHA until SA-specific equations are developed in the US, the resulting risk estimates should be interpreted cautiously.11,12 Still, it must be noted that 83% of MASALA participants with low estimated risk had CAC=0, and 61% with high estimated risk had CAC>100. This suggests a reasonably good performance of the PCE in these two groups at the extremes of risk, although formal validation analyses are needed to confirm these findings. On the other hand, the results in the borderline/intermediate risk strata suggest marked risk heterogeneity within those groups, with significant room for further risk stratification.
Finally, because we excluded prevalent statin users from the analyses of participants qualifying for ASCVD risk estimation, it could be argued that we might have underestimated the proportion of individuals with a high CAC burden who would be considered statin-recommended according to current guideline recommendations. Nevertheless, the distribution of CAC burden observed among prevalent statin users was almost identical to that observed when borderline, intermediate and high-risk individuals were combined. Consequently, inclusion of such individuals in the analyses would not have altered our estimates. Moreover, by excluding those individuals, our analysis was able to resemble the real-life scenario in which the new 2019 ACC/AHA guideline recommendations for SA individuals would be implemented.
4.2. Conclusions
Systematic consideration of intermediate- and particularly of borderline-risk SAs as statin candidates (as per a SA ethnicity as a risk enhancer approach) markedly increases the number of CAC=0 individuals who would be treated with statins, potentially resulting in overtreatment. Although longitudinal studies are needed to better understand the prognostic implications of CAC=0 in SAs, further risk assessment with CAC may help better personalize statin allocation also in this large, rapidly growing ethnic group in the US. Aggressive lifestyle interventions aimed at reducing the risk of incident diabetes should be strongly recommended in US SAs, particularly among those considered for statin therapy for primary ASCVD prevention.
HIGHLIGHTS.
The prevalence of CAC=0 was high (54%) among US SAs at borderline risk
Treatment of all borderline-risk SAs with statins might lead to overtreatment
Longitudinal studies are needed in SAs to confirm the favorable prognosis of CAC=0
Abdominal obesity (81%) and prediabetes (74%) are highly frequent in this group
Preventive interventions in borderline-risk SAs should aim at reducing diabetes risk
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
We further confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
We understand that the Corresponding Author is the sole contact for the Editorial process (including Editorial Manager and direct communications with the office). He is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs. We confirm that we have provided a current, correct email address which is accessible by the Corresponding Author: mcainzosachirica@houstonmethodist.org
REFERENCES
- 1.Goyal A, Yusuf S. The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res. 2006;124:235–244. [PubMed] [Google Scholar]
- 2.Yusuf S, Hawken S, Ounpuu S, on behalf of the INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 3.Hajra A, Li Y, Siu S, Udaltsova N, Armstrong MA, Friedman GD, Klatsky AL. Risk of coronary disease in the South Asian American population. J Am Coll Cardiol. 2013;62:644–645. [DOI] [PubMed] [Google Scholar]
- 4.Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo KK, Montague PA, Kelemen L, Yi C, Lonn E, Gerstein H, Hegele RA, McQueen M. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet. 2000;356:279–284. [DOI] [PubMed] [Google Scholar]
- 5.Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ. 2017;357:j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cainzos-Achirica M, Vela E, Cleries M, Bilal U, Mauri J, Pueyo MJ, Rosas A, Enjuanes C, Blaha MJ, Kanaya AM, Comin-Colet J. Cardiovascular risk factors and disease among non-European immigrants living in Catalonia. Heart. 2019;105:1168–1174. [DOI] [PubMed] [Google Scholar]
- 7.Fedeli U, Avossa F, Ferroni E, Schievano E, Bilato C, Modesti PA, Corti MC. Diverging patterns of cardiovascular diseases across immigrant groups in Northern Italy. Int J Cardiol. 2018;254:362–367. [DOI] [PubMed] [Google Scholar]
- 8.Rabanal KS, Selmer RM, Igland J, Tell GS, Meyer HE. Ethnic inequalities in acute myocardial infarction and stroke rates in Norway 1994-2009: a nationwide cohort study (CVDNOR). BMC Public Health. 2015;15:1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United States Census Bureau. The Asian Population 2010. Available online at: https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf (Accessed 15 July 2021)
- 10.Volgman AS, Palaniappan LS, Aggarwal NT, Gupta M, Khandelwal A, Krishnan AV, Lichtman JH, Mehta LS, Patel HN, Shah KS, Shah SH, Watson KE; American Heart Association Council on Epidemiology and Prevention; Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; and Stroke Council. Atherosclerotic Cardiovascular Disease in South Asians in the United States: Epidemiology, Risk Factors, and Treatments: A Scientific Statement From the American Heart Association. Circulation. 2018;138:e1–e34. [DOI] [PubMed] [Google Scholar]
- 11.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–e1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel J, Al Rifai M, Blaha MJ, Budoff MJ, Post WS, Polak JF, Bluemke DA, Scheuner MT, Kronmal RA, Blumenthal RS, Nasir K, McEvoy JW. Coronary Artery Calcium Improves Risk Assessment in Adults With a Family History of Premature Coronary Heart Disease: Results From Multiethnic Study of Atherosclerosis. Circ Cardiovasc Imaging. 2015;8:e003186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel J, Pallazola VA, Dudum R, Greenland P, McEvoy JW, Blumenthal RS, Virani SS, Miedema MD, Shea S, Yeboah J, Abbate A, Hundley WG, Karger AB, Tsai MY, Sathiyakumar V, Ogunmoroti O, Cushman M, Savji N, Liu K, Nasir K, Blaha MJ, Martin SS, Al Rifai M. Assessment of Coronary Artery Calcium Scoring to Guide Statin Therapy Allocation According to Risk-Enhancing Factors: The Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol. 2021. Jul 14 doi: 10.1001/jamacardio.2021.2321. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dzaye O, Dudum R, Reiter-Brennan C, Kianoush S, Tota-Maharaj R, Cainzos-Achirica M, Blaha MJ. Coronary artery calcium scoring for individualized cardiovascular risk estimation in important patient subpopulations after the 2019 AHA/ACC primary prevention guidelines. Prog Cardiovasc Dis. 2019;62:423–430. [DOI] [PubMed] [Google Scholar]
- 16.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O'Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. [DOI] [PubMed] [Google Scholar]
- 17.Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weir GC, Bonner-Weir S. Five stages of evolving beta-cell dysfunction during progression to diabetes. Diabetes. 2004. Dec;53 Suppl 3:S16–S21. [DOI] [PubMed] [Google Scholar]
- 19.Stevens J, Couper D, Pankow J, Folsom AR, Duncan BB, Nieto FJ, Jones D, Tyroler HA. Sensitivity and specificity of anthropometries for the prediction of diabetes in a biracial cohort. Obes Res. 2001;9:696–705. [DOI] [PubMed] [Google Scholar]
- 20.Freemantle N, Holmes J, Hockey A, Kumar S. How strong is the association between abdominal obesity and the incidence of type 2 diabetes? Int J Clin Pract. 2008;62:1391–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanaya AM, Kandula N, Herrington D, Budoff MJ, Hulley S, Vittinghoff E, Liu K. Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study: Objectives, Methods, and Cohort Description. Clin Cardiol. 2013;36:713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanaya AM, Chang A, Schembri M, Puri-Taneja A, Srivastava S, Dave SS, Vijayakumar EN, Qamar Z, Naik HD, Siddiqui F, Kandula NR. Recruitment and retention of US South Asians for an epidemiologic cohort: Experience from the MASALA study. J Clin Transl Sci. 2019;3:97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42:S13–S28. [DOI] [PubMed] [Google Scholar]
- 25.Gujral UP, Prabhakaran D, Pradeepa R, Kandula NR, Kondal D, Deepa M, Zakai NA, Anjana RM, Rautela G, Mohan V, Narayan KMV, Tandon N, Kanaya AM. Isolated HbA1c identifies a different subgroup of individuals with type 2 diabetes compared to fasting or post-challenge glucose in Asian Indians: The CARRS and MASALA studies. Diabetes Res Clin Pract. 2019;153:93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Health Organization. Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation. Geneva, 8–11 December 2008. Available online at: https://apps.who.int/iris/bitstream/handle/10665/44583/9789241501491_eng.pdf;isessionid=902FE633966D44CFBE47D30A3BB41F86?seciuence=1 (Accessed 15 July 2021) [Google Scholar]
- 27.Kanaya AM, Kandula NR, Ewing SK, Herrington D, Liu K, Blaha MJ, Srivastava S, Dave SS, Budoff MJ. Comparing coronary artery calcium among U.S. South Asians with four racial/ethnic groups: the MASALA and MESA studies. Atherosclerosis. 2014;234:102–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. [Google Scholar]
- 29.Malik S, Zhao Y, Budoff M, Nasir K, Blumenthal RS, Bertoni AG, Wong N. Coronary Artery Calcium Score for Long-term Risk Classification in Individuals With Type 2 Diabetes and Metabolic Syndrome From the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol. 2017;2:1332–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Malik S, Budoff MJ, Katz R, Blumenthal RS, Bertoni AG, Nasir K, Szklo M, Barr RG, Wong ND. Impact of subclinical atherosclerosis on cardiovascular disease events in individuals with metabolic syndrome and diabetes: the multi-ethnic study of atherosclerosis. Diabetes Care. 2011;34:2285–2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nasir K, Bittencourt MS, Blaha MJ, Blankstein R, Agatson AS, Rivera JJ, Miedema MD, Sibley CT, Shaw LJ, Blumenthal RS, Budoff MJ, Krumholz HM. Implications of Coronary Artery Calcium Testing Among Statin Candidates According to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2015;66:1657–1668. [DOI] [PubMed] [Google Scholar]
- 32.Nasir K Message for 2018 Cholesterol Management Guidelines Update: Time to Accept the Power of Zero. J Am Coll Cardiol. 2018;72:3243–3245. [DOI] [PubMed] [Google Scholar]
- 33.Pew Research Center. 5 facts about Indian Americans. Available online at: http://www.pewresearch.org/fact-tank/2014/09/30/5-facts-about-indian-americans/ (Accessed 15 July 2021)
- 34.United States Census Bureau. American Community Survery. 2017. American Community Survey 1-Year Estimates. Available online at: https://factfinder.census.gov/faces/tableservices/isf/pages/productview.xhtml?src=bkmk (Accessed 15 July 2021)
- 35.Satish P, Vela E, Bilal U, Cleries M, Kanaya AM, Kandula N, Virani SS, Islam N, Valero-Elizondo J, Yahya T, Comin-Colet J, Nasir K, Mauri J, Cainzos-Achirica M. Burden of cardiovascular risk factors and disease in five Asian groups in Catalonia: a disaggregated, population-based analysis of 121 000 first-generation Asian immigrants. Eur J Prev Cardiol. 2021. May 10:zwab074. doi: 10.1093/eurjpc/zwab074. Epub ahead of print. PMID: 33969397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patel AP, Wang M, Kartoun U, Ng K, Khera AV. Quantifying and Understanding the Higher Risk of Atherosclerotic Cardiovascular Disease Among South Asian Individuals: Results From the UK Biobank Prospective Cohort Study. Circulation. 2021. Jul 12. doi: 10.1161/CIRCULATIONAHA.120.052430. Epub ahead of print. PMID: 34247495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, Pandey MR, Haque S, Mendis S, Rangarajan S, Yusuf S. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–94. [DOI] [PubMed] [Google Scholar]
- 38.Nasir K, Cainzos-Achirica M. Role of coronary artery calcium score in the primary prevention of cardiovascular disease. BMJ. 2021;373:n776. [DOI] [PubMed] [Google Scholar]