Abstract
Homocysteine is a marker for derangements in one-carbon metabolism. Elevated homocysteine may represent a causal link between poor maternal nutrition and impaired embryonic and fetal development. We sought to investigate associations between reference range maternal homocysteine and embryonic and fetal growth. We enrolled 1060 singleton pregnancies (555 natural and 505 in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) pregnancies) from November 2010 to December 2020. Embryonic and fetal body and head growth was assessed throughout pregnancy using three-dimensional ultrasound scans and virtual reality techniques. Homocysteine was negatively associated with first trimester embryonic growth in the included population (crown-rump length B −0.023 mm, 95% CI −0.038,−0.007, p = 0.004, embryonic volume B −0.011 cm3, 95% CI −0.018,−0.004, p = 0.003). After stratification for conception mode, this association remained in IVF/ICSI pregnancies with frozen embryo transfer (crown-rump length B −0.051 mm, 95% CI −0.081,−0.023, p < 0.001, embryonic volume B −0.024 cm3, 95% CI −0.039,−0.009, p = 0.001), but not in IVF/ICSI pregnancies with fresh embryo transfer and natural pregnancies. Homocysteine was not associated with longitudinal measurements of head growth in first trimester, nor with second and third trimester fetal growth. Homocysteine in the highest quartile (7.3–14.9 µmol/L) as opposed to the lowest (2.5–5.2 µmol/L) was associated with reduced birth weight in natural pregnancies only (B −51.98 g, 95% CI −88.13,−15.84, p = 0.005). In conclusion, high maternal homocysteine within the reference range is negatively associated with first trimester embryonic growth and birth weight, and the effects of homocysteine are dependent on conception mode.
Keywords: embryo, fetus, homocysteine, growth, periconception, prenatal, birth, one carbon metabolism, ultrasound, virtual reality
1. Introduction
One-carbon metabolism plays an important role in fertility and pregnancy, being involved in developmental programming of cells and tissues, fetal growth and development [1]. Derangements in one-carbon metabolism are represented by elevated homocysteine levels, often in association with folate and vitamin B12 deficiency [1]. Such derangements represent one of the causal links between poor maternal nutrition and lifestyle, and the risk of impaired embryonic and fetal development, with implications for long-term postnatal health [2].
One-carbon metabolism is composed of the interlinked folate and methionine cycles, and the transsulfuration pathway, which support essential biological processes including cell multiplication, differentiation, and epigenetic programming [3]. Clinical applicable and usable biomarkers of one-carbon metabolism include homocysteine, folate, and vitamin B12. A high blood concentration of homocysteine is recognized as a sensitive marker for general folate deficiency [4,5].
Elevated homocysteine levels are known to impair female fertility and preimplantation embryo development. Studies report that elevated homocysteine impairs gamete quality, decreases fertilization success, and alters epigenetic processes in the preimplantation embryo [2,6]. It is also known that hyperhomocysteinemia in women is associated with pregnancy complications such as recurrent pregnancy loss and pregnancy hypertension disorders, and is negatively associated with birth outcomes such as low birth weight and preterm birth, although there are some inconsistencies in the literature in this regard [2,7,8,9].
Besides birth weight, only a few studies address the association between maternal homocysteine and prenatal development. Parisi et al. reported that high homocysteine levels are associated with delayed embryonic development (Carnegie stages) [10], together with reduced crown-rump length (CRL) and embryonic volume (EV) during the first trimester of pregnancy [11]. In addition, elevated maternal homocysteine represents a risk factor for postnatal neurological impairments in offspring [12]; but few studies investigated fetal brain development and head growth prior to birth [9,13]. Therefore, we hypothesized that maternal homocysteine may negatively influence embryonic and fetal growth throughout pregnancy, including head growth.
We were the first to hypothesize that maternal homocysteine is associated with neural tube defects [14,15] and continued this line of research in humans by revealing associations between maternal one-carbon metabolism and embryonic size and growth [16]. The current study is novel as we investigate associations between maternal homocysteine and serial prenatal size and growth parameters (i.e., embryonic, fetal, and neonatal parameters). Additionally, we limited our analyses of prenatal development to align with the reference range for homocysteine of the hospital laboratory, thereby excluding cases of hyperhomocysteinemia and several adverse pregnancy outcomes, as this has yet to be addressed.
2. Materials and Methods
This study is embedded in the Rotterdam Periconception Cohort (Predict Study), a prospective tertiary hospital-based birth cohort study at the Department of Obstetrics and Gynecology of the Erasmus MC, University Medical Center, Rotterdam, The Netherlands. This is an ongoing study initiated in 2009, with the aim of investigating the association between parental periconception health and its impact on reproduction, pregnancy, and neonatal outcomes [17]. The study was approved by the Central Committee on Research in The Hague and the local Medical Ethics Committee of the Erasmus MC (MEC-2004-227).
2.1. Study Population
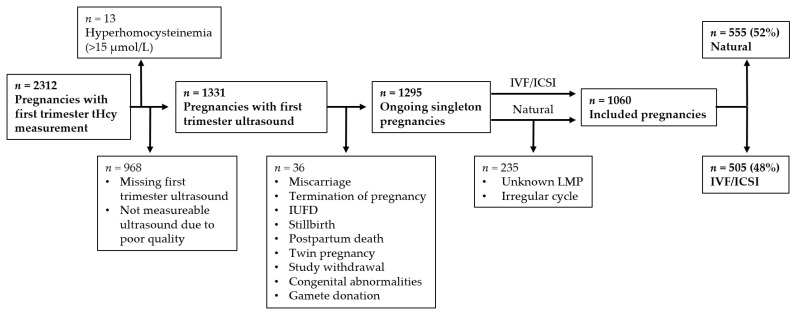
Between November 2010 and December 2020, pregnant women in early first-trimester (<11 weeks of gestation) were eligible for enrolment, provided they (and their partner) had at least reached the age of 18 years, and could read and speak the Dutch language. Figure 1 shows the criteria for inclusion and exclusion for the current study. Women were included if they had conceived naturally or following assisted reproduction (IVF/ICSI). In this study, natural pregnancies also included the use of ovulation induction and intrauterine insemination (IUI) to achieve a pregnancy, as fertilization is achieved via natural occurrence. In all analyses, cases of maternal hyperhomocysteinemia (homocysteine concentration ≥ 15 µmol/L) were excluded to obtain reference range homocysteine concentrations. This occurred in order to exclude any interference on prenatal development from the physiological condition that underlies hyperhomocysteinemia in pregnant women [18,19]. In addition, cases of hyperhomocysteinemia were too low to perform analyses. Exclusion criteria were cases of miscarriage, termination of pregnancy, intrauterine fetal death, stillbirth, postpartum death, twin pregnancy, study withdrawal, fetal congenital abnormalities, and gamete donation for IVF/ICSI pregnancies. All participants gave written informed consent before participation.
Figure 1.
Flowchart of included and excluded population (2010–2020) based on predefined criteria. Abbreviations: ICSI, intracytoplasmic sperm injection; IUFD, intrauterine fetal death; IVF, in vitro fertilization; LMP, last menstrual period; tHcy, total homocysteine.
2.2. Participant Measurements
In naturally conceived pregnancies, gestational age (GA) was calculated from the first day of the last menstrual period of a regular menstrual cycle. For IVF and ICSI pregnancies, GA was calculated from 14 days before the conception date for fresh embryo transfers and 14 days before the fictitious conception date for cryopreserved embryo transfers, adjusted for the age of the embryo at transfer. For pregnancies achieved via IUI, GA was calculated from 14 days before the insemination date. GA was considered unreliable in cases with an unknown last menstrual period or an irregular menstrual cycle (<21 or >35 days). Information on women and their partners was obtained via extensive self-reported questionnaires given at the time of enrolment (<11 weeks of gestation), covering details such as age, anthropometrics, family history, medical history, education, lifestyle behavior, and habits (from 4 weeks before to 8 weeks after conception). Based on Statistics Netherlands, education level was classified as ‘low’ for primary/lower vocational/intermediate secondary school, ‘intermediate’ for higher secondary/intermediate vocational school, and ‘high’ for higher vocational school/university [20]. The consumption of caffeine was defined as ‘none’ for 0 cups of coffee a day, ‘moderate’ for >0.1 and <2 cups of coffee a day, and ‘high’ for ≥2 cups of coffee a day, as 2 cups of coffee contain above the 200 mg/day recommended maximum dose of caffeine in pregnancy.
2.3. Laboratory Assays
At the time of enrolment (<11 weeks of gestation), one venous blood sample from both women and their partners was collected for the determination of biomarkers of one-carbon metabolism: serum homocysteine, folate, and vitamin B12. Homocysteine was measured until December 2020, whereas folate and vitamin B12 were measured until December 2016, due to a change in study protocol. In vitro quantitative determination of total L-homocysteine in human serum was performed using an HCYS assay with a Cobas 8000 system, and in vitro quantitative determination of human serum folate and vitamin B12 was performed using the Elecsys Folate III and Elecsys Vitamin B12 II assays with a Cobas 8000 system by Cobas® Roche Diagnostics. Protocols are publicly available online on www.diagnostics.roche.com (accessed on 20 December 2021).
2.4. Embryonic and Fetal Measurements
To measure embryonic and fetal growth parameters, ultrasound scans were obtained from all women in the first, second, and third trimesters of pregnancy, and neonatal birth weight was obtained from medical records.
2.4.1. First Trimester
Longitudinal transvaginal three-dimensional (3D) ultrasound scans were performed from enrolment to the end of the first trimester of pregnancy with a maximum of 6 scans per pregnancy. 3D ultrasound examinations were performed using a 6–12 MHz transvaginal probe of the Voluson E8 or E10 system (General Electric Medical Systems). 3D ultrasound images were stored as Cartesian volumes and analyzed by virtual reality (VR) systems and V-Scope software (the latter developed at the Erasmus MC in Rotterdam, The Netherlands). The VR systems used in the current study were the BARCO I-Space (until 2019) and Desktop VR system (since 2014), which all use the identical in-house developed software program V-Scope [21,22]. The VR system is a proven and reliable method to measure first trimester embryonic measurements in clinical practice [23]. Measurements of body size (CRL and EV) were performed from 6 + 0 to 13 + 6 weeks of gestation and measured with VR. In a subpopulation of the Predict Study (included population n = 118), measurements of head size (head volume (HV), biparietal diameter (BPD), occipitofrontal diameter (OFD), head circumference (HC), and cerebellar size (transcerebellar diameter (TCD)) were performed using an offline 3D software (4D view, GE Medical Systems) [17,24]. Such head and cerebellar measurements were performed at 9 and 11 weeks of gestation because the required reference points to perform such measurements were not visible earlier or only visible in a small proportion of the included population.
2.4.2. Second and Third Trimester
In a subpopulation of the Predict Study (included population n = 269) [25], longitudinal transabdominal 2D and 3D ultrasound scans were performed at 22, 26, and 32 weeks of gestation with a maximum of 3 scans per pregnancy. 3D ultrasound examinations were performed using a 4–8 MHz transducer of the Voluson E8 System (General Electric Medical Systems). During ultrasound examination, measurements of fetal biometry (BPD, HC, TCD, abdominal circumference (AC), femur length (FL), and estimated fetal weight (EFW)) were performed. EFW was calculated using the Hadlock formula [26]. Measurement protocols were extensively described in previously published articles from the Department of Obstetrics and Gynecology, Erasmus MC, University Medical Center, The Netherlands [11,21,27,28,29,30].
Additional second trimester measurements of fetal biometry were obtained from medical records and included a single time-point measure of BPD, HC, TCD, AC, FL, and EFW. These measurements were performed during the standard fetal anomaly scan, with a mean of 20 weeks of gestation, according to the ISUOG practice guidelines [31].
2.5. Additional Calculations
Birth at <37 weeks of gestation was defined as preterm birth, and neonatal birth weight of ≤2500 g as low birth weight. Hoftiezer percentiles were calculated according to the publication of Hoftiezer et al. [32]. Neonates were considered born small for gestational age (SGA) if Hoftiezer percentile was ≤0.1 and large for gestational age (LGA) if Hoftiezer percentile was ≥0.9. Hoftiezer percentiles represent reference curves from a healthy population.
2.6. Statistical Analyses
The Student’s t-test with unpaired samples was used to compare continuous variables, Fisher’s exact test for dichotomous categorical variables, and Chi-square test for polychotomous categorical variables. Non-parametric data were log10-transformed to obtain parametric data. Associations were performed with univariate linear regression for continuous exposure and outcome variables, and with binary logistic regression for continuous exposure variables and outcome dichotomous categorical variables.
In subanalyses, homocysteine was divided into categories, as the literature shows that the effect of homocysteine levels on neonatal birth weight is not linear. Homocysteine was divided into fourths with equal number of pregnancies per quartile: Q1 2.5–5.2 µmol/L, Q2 5.3–6.0 µmol/L, Q3 6.1–7.2 µmol/L, Q4 7.3–14.9 µmol/L, and Q1 was used as reference category.
Linear mixed models were used to analyze associations between longitudinal measurements and maternal homocysteine, adjusting for confounders and assuming the effect of homocysteine was constant over gestation. For all analyses, confounders were chosen based on the literature: (Model 1) adjustment for GA and (Model 2) adjustment for GA, conception mode, parity, folic acid supplement use, alcohol use, smoking, maternal BMI, maternal age, and fetal sex. All analyses were stratified by conception mode.
For all analyses, statistical significance was defined as p < 0.05. All analyses were executed in IBM SPSS Statistics for Windows (version 25), and R (version 4.1.1).
3. Results
3.1. Baseline Characteristics of the Study Population
A total of 1060 pregnancies were included in the study, of which 555 (52%) were natural pregnancies and 505 (48%) were conceived by IVF/ICSI, according to the inclusion and exclusion criteria described in Figure 1. The prevalence of hyperhomocysteinemia before the introduction of exclusion criteria was 0.56%. Participants with hyperhomocysteinemia had significantly lower serum folate concentrations when compared to the population with reference range homocysteine (Table S1). Maternal baseline characteristics of the included and excluded population are shown in Table S2. The included population was stratified by conception mode and maternal baseline characteristics were compared in Table 1. Women with pregnancies established by IVF/ICSI had lower homocysteine, were older, had a lower BMI, were less likely to drink alcohol and smoke, were 100% compliant with the use of folic acid supplementation and were more likely to be primiparous when compared to women with natural pregnancies. Additionally, serum folate of both the mother and the father were higher in IVF/ICSI pregnancies than in natural pregnancies.
Table 1.
Maternal baseline characteristics of natural and IVF/ICSI pregnancies of the included population.
| Characteristics |
Natural Pregnancies
(n = 555) |
IVF/ICSI Pregnancies
(n = 505) |
p-Value |
| Age a, mean ± SD | 31.8 ± 4.4 | 33.1 ± 4.3 | 0.000 |
| Ethnicity, n (%) | 0.553 | ||
| Dutch | 424 (80) | 390 (81) | |
| Western, other | 27 (5) | 31 (6) | |
| Non-western | 77 (15) | 63 (13) | |
| Education level, n (%) | 0.042 | ||
| Low | 46 (9) | 25 (5) | |
| Intermediate | 172 (33) | 181 (38) | |
| High | 309 (59) | 274 (57) | |
| BMI b, median (IQR) | 24.5 (22.2–28.5) | 24.4 (21.9–27.7) | 0.007 |
| Nulliparous, n (%) | 131 (25) | 249 (51) | 0.000 |
| Alcohol use, n (%) | 197 (37) | 110 (23) | 0.000 |
| Smoking, n (%) | 86 (16) | 57 (12) | 0.047 |
| Folic acid supplement use, n (%) | 520 (98) | 484 (100) | 0.002 |
| Caffeine use, n (%) | 0.285 | ||
| None | 231 (44) | 225 (46) | |
| Moderate | 223 (42) | 181 (37) | |
| High | 76 (14) | 79 (16) | |
| tHcy e, mean ± SD | 6.5 ± 1.7 | 6.3 ± 1.4 | 0.020 |
| Biomarkers * |
Natural Pregnancies
(n = 411) |
IVF/ICSI Pregnancies
(n = 271) |
p-Value |
| tHcy e, median (IQR) | 6.2 (5.3–7.2) | 6.0 (5.2–6.9) | 0.055 |
| Serum folate c, median (IQR) | 38.9 (31.9–44.7) | 41.0 (34.9–55.5) | 0.002 |
| Vitamin B12 d, median (IQR) | 316.5 (237.8–397.0) | 316.0 (256.0–404.0) | 0.238 |
| Paternal tHcy e, median (IQR) | 11.7 (10.0–13.8) | 11.3 (9.7–13.3) | 0.509 |
| Paternal serum folate c, median (IQR) | 17.5 (13.9–22.1) | 18.9 (15.0–24.2) | 0.005 |
| Paternal vitamin B12 d, median (IQR) | 344.0 (271.0–419.0) | 323.5 (260.0–416.0) | 0.426 |
a years, b kg/m2, c nmol/L, d pmol/L, e µmol/L. * Subgroup from November 2010 to December 2016. Alcohol use, smoking, folic acid supplementation and caffeine use were measured during the periconception period. Parametric data is represented as mean ± SD, whereas non-parametric data is represented as median (IQR). Abbreviations: BMI, body mass index; IUI, intrauterine insemination; IVF, in vitro fertilization; ICSI, intracytoplasmic sperm injection; SD, standard deviation; IQR, interquartile range. p-value < 0.05 represented in bold.
3.2. Maternal Homocysteine and Baseline Characteristics
In the included population, women conceiving naturally were more likely to have higher homocysteine levels than women pregnant after IVF/ICSI (OR 0.91 (95% CI 0.84,0.99), p = 0.02). Homocysteine was positively associated with maternal BMI (B 1.69 (95% CI 0.46,2.94), p = 0.01), with the odds of being a smoker (OR 0.89 (95% CI 0.82,0.97), p = 0.01), and with being nulliparous (OR 0.87 (95% CI 0.79,0.97), p = 0.01). Maternal homocysteine showed an inverse association with maternal and paternal vitamin B12 (B −0.23 (95% CI −0.27,−0.18), p < 0.01 and B −0.06 (95% CI −0.11,−0.01), p = 0.03 respectively), maternal and paternal serum folate (B −0.08 (95% CI −0.12,−0.04), p < 0.01 and B −0.06 (95% CI −0.12,0.00), p = 0.04 respectively), and there was a positive association with paternal homocysteine (B 0.09 (95% CI 0.03,0.15), p = 0.01).
3.3. First Trimester Embryonic Growth
In the included population, the mean GA for CRL and EV was 9 + 6 weeks (69 days). CRL and EV did not differ between natural and IVF/ICSI pregnancies. Linear mixed effect models showed that homocysteine was negatively associated with growth trajectories of CRL and EV in the included overall population (Table 2). The negative association persisted in IVF/ICSI pregnancies with frozen embryo transfer but not in IVF/ICSI pregnancies with fresh embryo transfer and natural pregnancies after stratification for conception mode (Table 2). In the included population, the same association was found if CRL and EV were analyzed at 7, 9, and 11 weeks of gestation individually (Table S3). At single time-point measurements, the negative association with CRL and EV was present for all modes of conception (Table S3).
Table 2.
Association between maternal homocysteine and longitudinal first trimester embryonic CRL and EV in the included population (n = 1060), natural pregnancies (n = 555) and IVF/ICSI pregnancies (n = 505).
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| CRL | ||||
| Beta (95% CI) √mm | p-value | Beta (95% CI) √mm | p-value | |
| Included population n = 919 |
−0.027 (−0.043, −0.012) | <0.001 | −0.023 (−0.038, −0.007) | 0.004 |
| Natural pregnancies n = 494 |
−0.027 (−0.052, −0.001) | 0.039 | −0.019 (−0.044, 0.006) | 0.141 |
| IVF/ICSI pregnancies, FrET n = 143 |
−0.051 (−0.080, −0.022) | <0.001 | −0.051 (−0.081, −0.023) | <0.001 |
| IVF/ICSI pregnancies, FET n = 282 |
−0.015 (−0.031, 0.001) | 0.061 | −0.013 (−0.029, 0.002) | 0.095 |
| EV | ||||
| Beta (95% CI) 3√cm | p-value | Beta (95% CI) 3√cm | p-value | |
| Included population n = 898 |
−0.013 (−0.021, −0.006) | <0.001 | −0.011 (−0.018, −0.004) | 0.003 |
| Natural pregnancies n = 482 |
−0.014 (−0.026, −0.002) | 0.022 | −0.011 (−0.022, 0.001) | 0.079 |
| IVF/ICSI pregnancies, FrET n = 144 |
−0.024 (−0.039, −0.009) | 0.001 | −0.024 (−0.039, −0.009) | 0.001 |
| IVF/ICSI pregnancies, FET n = 272 |
−0.005 (−0.013, 0.003) | 0.213 | −0.004 (−0.012, 0.003) | 0.305 |
CRL = crown-rump length, EV = embryonic volume, FET = fresh embryo transfer, FrET = frozen embryo transfer. Model 1: adjusted for GA, Model 2: adjusted for GA, conception mode (included population only), parity, smoking, folic acid supplement use, alcohol, BMI, age, and fetal sex. p-value < 0.05 represented in bold.
In the subpopulation including 118 pregnancies, embryonic BPD, OFD, HV, HC, and TCD at 9 and 11 weeks of gestation did not differ between natural and IVF/ICSI pregnancies. Linear mixed effect models showed that maternal homocysteine was not associated with longitudinal embryonic head growth (Table S4).
3.4. Second and Third Trimester Fetal Growth
Fetal BPD, TCD, AC, FL and EFW at a mean of 20 weeks of gestation did not differ between natural and IVF/ICSI pregnancies, but HC was significantly smaller in IVF/ICSI pregnancies when compared to natural pregnancies (mean 175.7 mm vs. 176.91 mm, p = 0.03). Linear regression showed that homocysteine was not associated with second trimester fetal growth (Table 3). Similarly, no association was found between second trimester fetal growth and quartiles of homocysteine.
Table 3.
Association between maternal homocysteine and fetal growth from the second trimester fetal anomaly scan in the included population (n = 1060), natural pregnancies (n = 555), and IVF/ICSI pregnancies (n = 505).
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| BPD | ||||
| Beta (95% CI) mm | p-value | Beta (95% CI) mm | p-value | |
| Included population n = 966 | −0.002 (−0.099, 0.095) | 0.966 | 0.009 (−0.092, 0.111) | 0.855 |
| Natural pregnancies n = 519 | 0.025 (0.704, −0.104) | 0.704 | 0.042 (−0.100, 0.183) | 0.563 |
| IVF/ICSI pregnancies n = 447 | −0.007 (−0.154, 0.140) | 0.925 | −0.004 (−0.149, 0.141) | 0.955 |
| HC | ||||
| Beta (95% CI) mm | p-value | Beta (95% CI) mm | p-value | |
| Included population n = 982 | −0.067 (−0.327, 0.193) | 0.613 | −0.035 (−0.304, 0.234) | 0.801 |
| Natural pregnancies n = 525 | −0.027 (−0.385, 0.330) | 0.881 | 0.003 (−0.381, 0.386) | 0.989 |
| IVF/ICSI pregnancies n = 457 | 0.009 (−0.351, 0.369) | 0.961 | 0.054 (−0.297, 0.406) | 0.762 |
| TCD | ||||
| Beta (95% CI) mm | p-value | Beta (95% CI) mm | p-value | |
| Included population n = 972 | −0.025 (−0.058, 0.008) | 0.137 | −0.023 (−0.057, 0.012) | 0.198 |
| Natural pregnancies n = 519 | −0.044 (−0.087, 0.000) | 0.051 | −0.040 (−0.088, 0.008) | 0.100 |
| IVF/ICSI pregnancies n = 453 | 0.027 (−0.020, 0.074) | 0.256 | 0.020 (−0.027, 0.067 | 0.409 |
| AC | ||||
| Beta (95% CI) mm | p-value | Beta (95% CI) mm | p-value | |
| Included population n = 980 | 0.011 (−0.276, 0.297) | 0.942 | 0.053 (−0.250, 0.357) | 0.731 |
| Natural pregnancies n = 524 | 0.136 (−0.240, 0.511) | 0.478 | 0.149 (−0.262, 0.561 | 0.477 |
| IVF/ICSI pregnancies n = 456 | −0.002 (−0.462, 0.423) | 0.994 | 0.048 (−0.386, 0.481) | 0.829 |
| FL | ||||
| Beta (95% CI) mm | p-value | Beta (95% CI) mm | p-value | |
| Included population n = 980 | −0.041 (−0.110, 0.027) | 0.235 | −0.036 (−0.112, 0.019) | 0.345 |
| Natural pregnancies n = 525 | −0.030 (−0.121, 0.061) | 0.521 | −0.018 (−0.121, 0.085) | 0.729 |
| IVF/ICSI pregnancies n = 455 | −0.018 (−0.119, 0.082) | 0.722 | −0.031 (−0.139, 0.077) | 0.569 |
| EFW | ||||
| Beta (95% CI) g | p-value | Beta (95% CI) g | p-value | |
| Included population n = 835 | −0.845 (−2.356, 0.665) | 0.272 | −0.614 (−2.249, 1.021) | 0.461 |
| Natural pregnancies n = 450 | −0.160 (−2.204, 1.883) | 0.878 | 0.099 (−2.215, 2.414) | 0.933 |
| IVF/ICSI pregnancies n = 385 | −0.666 (−2.715, 1.384) | 0.524 | −0.665 (−2.767, 1.455) | 0.541 |
AC = abdominal circumference, BPD = biparietal diameter, EFW = estimated fetal weight, FL = femur length, HC = head circumference, TCD = transcerebellar diameter. Fetal measurements were performed at a mean 20 weeks of gestation. Model 1: adjusted for GA, Model 2: adjusted for GA, conception mode (included population only), parity, smoking, folic acid supplement use, alcohol, BMI, age, and fetal sex.
In the subpopulation including 269 pregnancies, longitudinal fetal BPD, HC, TCD, AC, FL, and EFW measurements were obtained at a mean of 27 weeks of gestation (range 20–34 weeks of gestation). These measurements did not differ significantly between conception modes. Associations between homocysteine and longitudinal fetal BPD, HC, TCD, AC, and EFW were not significant, except for FL in IVF/ICSI pregnancies (Table S5).
3.5. Birth Weight
In the included population, the mean GA at birth was 39 + 1 weeks, and the average birth weight was 3286 g. Birth weight did not differ between natural and IVF/ICSI pregnancies. Linear regression showed that homocysteine was not associated with birth weight but was negatively associated with Hoftiezer percentiles in natural pregnancies (Table S6). The direction of association was opposite for mode of conception, as a positive association was found for IVF/ICSI pregnancies with fresh or frozen embryo transfer. We also found that homocysteine in the highest quartile, compared to the lowest quartile, was associated with reduced birth weight (Table 4) and Hoftiezer percentiles in natural pregnancies only (Table S7). Homocysteine did not influence the odds of having SGA and LGA neonates (Table S6), nor the odds of being born preterm or having a low birth weight.
Table 4.
Association between quartiles of homocysteine and birth weight in the included population (n = 983), natural pregnancies (n = 529), and IVF/ICSI pregnancies (n = 454).
| Model 1 | Model 2 | ||||
|---|---|---|---|---|---|
| Included population | |||||
| Beta (95% CI) g | p-value | Beta (95% CI) g | p-value | ||
| n = 229 | Q1 | Reference | Reference | ||
| n = 233 | Q2 | −83.97 (−161.0.7, −6.88) | 0.030 | −69.017 (−148.84, 10.81) | 0.090 |
| n = 297 | Q3 | −14.03 (−51.73, 23.68) | 0.465 | −12.27 (−50.09, 25.56) | 0.524 |
| n = 224 | Q4 | −13.02 (−40.44, 14.40) | 0.351 | −15.97 (−44.26, 12.29) | 0.267 |
| Natural pregnancies | |||||
| Beta (95% CI) g | p-value | Beta (95% CI) g | p-value | ||
| n = 127 | Q1 | Reference | Reference | ||
| n = 111 | Q2 | −62.38 (−171.91, 47.15) | 0.263 | −96.74 (−208.45, 14.96) | 0.090 |
| n = 155 | Q3 | −37.75 (−88.45, 12.95) | 0.144 | −50.29 (−103.09, 2.49) | 0.060 |
| n = 136 | Q4 | −33.62 (−68.39, 1.14) | 0.060 | −51.98 (−88.13, −15.84) | 0.005 |
| IVF/ICSI pregnancies | |||||
| Beta (95% CI) g | p-value | Beta (95% CI) g | p-value | ||
| n = 102 | Q1 | Reference | Reference | ||
| n = 122 | Q2 | −92.28 (−202.91, 18.36) | 0.102 | −42.04 (−160.02, 75.93) | 0.483 |
| n = 142 | Q3 | 14.33 (−42.72, 71.37) | 0.621 | 23.02 (−32.36, 78.39) | 0.414 |
| n = 88 | Q4 | 14.51 (−30.35, 59.36) | 0.524 | 28.44 (−17.81, 74.70) | 0.226 |
Model 1: adjusted for GA, Model 2: adjusted for GA, conception mode (included population only), parity, smoking, folic acid supplement use, alcohol, BMI, age, fetal sex. Quartiles of homocysteine are represented as Q1 2.5–5.2 µmol/L, Q2 5.3–6.0 µmol/L, Q3 6.1–7.2 µmol/L, Q4 7.3–14.9 µmol/L, and Q1 was used as reference category. p-value < 0.05 represented in bold.
4. Discussion
The present study sought to investigate the association between maternal first trimester homocysteine levels, within the standard reference range, and longitudinal embryonic and fetal growth from the sixth week of gestation until birth, based on mode of conception. We demonstrated that maternal homocysteine is negatively associated with embryonic growth (CRL, EV) during the first trimester, specifically in IVF/ICSI pregnancies with frozen embryo transfer. Embryonic head growth was not affected by maternal homocysteine levels. Homocysteine was not associated with second and third trimester fetal growth. Levels of homocysteine in the highest quartile were associated with reduced birth weight and Hoftiezer percentiles in natural pregnancies only.
Homocysteine is an important biological and clinical marker of one-carbon metabolism. It is well recognized that high homocysteine levels are indicative of folate and/or vitamin B12 deficiency [2,3], and this strong inverse association was consistent with our findings. In addition, the positive association we found between homocysteine, BMI, and smoking has been reported previously [33,34,35]. Women with a high BMI often follow a nutritiously poor diet and suffer from micronutrient deficiencies, explaining a higher risk of high homocysteine levels [34]. Smoking is associated with alterations of one-carbon metabolites within the liver, as well as the altered expression of enzymes involved in the one-carbon metabolism [36]. We report higher homocysteine levels and similar aforementioned associations in natural pregnancies, as opposed to IVF/ICSI pregnancies. Indeed, women undergoing ART treatment are most dedicated to pursue a healthy lifestyle, and their compliance to folic acid supplement may explain their lower homocysteine levels [37]. In line with this, we report that changes in homocysteine levels within our population are mostly a reflection of lifestyle and health-related habits, which is also confirmed by the positive association between maternal and paternal homocysteine.
Deficiencies of one-carbon substrates and co-factors during the periconceptional period are involved in alterations of the embryo’s genetic and epigenetic landscape, which negatively impact prenatal and early postnatal offspring growth [6]. Elevated maternal homocysteine is negatively associated with embryonic and fetal growth. Previous findings from our research group show that homocysteine is negatively associated with first trimester embryonic development according to the Carnegie stages in IVF/ICSI pregnancies only [10]. Here, we confirm results from our previous findings from Parisi et al., which was performed in a smaller study population [11]. However, we found that homocysteine was negatively associated with embryonic growth trajectories in IVF/ICSI pregnancies with frozen embryo transfer only. This is in agreement with studies which found that early embryonic growth patterns differ between frozen and fresh cycles [38], and children born from frozen embryos are at increased risk of being large for gestational age [39,40]. Potential epigenetic modifications during freezing and thawing may make embryos from frozen cycles more vulnerable to alterations of the maternal environment. In conclusion, first trimester embryonic growth in IVF/ICSI pregnancies may be most vulnerable to the effects of maternal homocysteine.
One-carbon metabolism is also involved in brain development and neural programming, and derangements of the pathway increase the short-term risk of embryonic neural tube-related defects and long-term childhood behavior, cognition, and autism spectrum disorders [41]. As reported in our recent review, elevated homocysteine is associated with adult cognitive impairment, but much less is known about its role in prenatal head growth and development [41]. Here, we show that homocysteine is not associated with head growth at any stage of pregnancy. These results are consistent with studies that found that homocysteine is not associated with neonatal HC [9,13,42,43]. However, we have included a small study group with restricted measurements of head and brain structures, so we cannot discount the possibility that homocysteine may have an effect on prenatal brain growth. Lastly, the postnatal effects that homocysteine may exert on brain activity may not be reflected by prenatal growth, or may develop postnatally only; this functional aspect requires further investigation.
First trimester embryonic growth is associated with second and third trimester fetal growth, and consequently with neonatal weight at birth [27]; therefore, it was unexpected to find no influence of homocysteine on fetal growth from the second trimester onwards. Previous studies reported that only homocysteine ≥ 8.31 µmol/L (compared to 5.81–6.60 µmol/L) was associated with reduced fetal FL and EFW during late pregnancy. However, it remains unclear whether these results would be consistent if homocysteine was analyzed continuously [44]. Our observations consider homocysteine as a continuous variable, but we also compared the effects of high versus low levels of homocysteine. With this approach, we show that the merits of homocysteine as a clinical biomarker on mid- and late pregnancy fetal growth may be limited. Fetal growth is dependent on placenta function, which plays a major role from mid-pregnancy. Placental function is disrupted by hyperhomocysteinemia [45], which generates reactive oxygen species such as hydrogen peroxide which lead to oxidative stress, endothelial dysfunction, and placenta-related clotting disorders; all of which can limit placental and fetal blood supply and, consequently, fetal growth [46,47]. As cases with hyperhomocysteinemia were excluded, the likelihood of finding any negative effects of homocysteine on placenta function and consequently fetal growth was small.
This study adds to the current debate on homocysteine and birth weight. Elevated homocysteine is associated with SGA neonates, preterm birth, and low neonatal birth weight [9,44,48,49,50]. However, the findings in these studies applied specifically to homocysteine levels in the highest category (usually >8 µmol/L, including cases of hyperhomocysteinemia) when compared to the lowest category (usually <3 µmol/L). These findings are in agreement with our results, in which homocysteine in the highest quartile (7.3–14.9 µmol/L) reduced birth weight and Hoftiezer percentiles in natural pregnancies only, although no cases of hyperhomocysteinemia were included. Instead, when homocysteine was analyzed as a continuous variable, no effect on birth weight was found. In secondary analyses, we included the three cases of hyperhomocysteinemia eligible after exclusion criteria (homocysteine 16.30–24.90 µmol/L) and found the same associations, with larger effect sizes for birth weight and Hoftiezer percentiles (data not shown). Homocysteine may serve as a clinical biomarker of impaired birth weight in natural pregnancies only. High levels of homocysteine within the reference range may still represent a risk factor for low birth weight.
Despite selecting women with a ‘healthy’ reference range of homocysteine, we found that there was still a negative association with embryonic growth during the first trimester. This observation may be due to epigenetic regulation of embryonic development; cell lineage specification and tissue patterning are predominant during the first trimester, under the influence of one-carbon metabolism [51]. Similarly, high levels of homocysteine within our reference range had a negative association with birth weight. This evidence suggests that high levels of homocysteine, even within the reference range, may represent a pregnancy risk factor.
Additionally, we confirm that conception mode is a strong determinant of the effects homocysteine exerts on first trimester embryonic growth and neonatal birth weight. Embryos from IVF/ICSI pregnancies with frozen embryo transfer appear to be most sensitive to the negative effects of homocysteine during the first trimester, whereas embryos from natural pregnancies were most vulnerable to negative effects at birth. This may suggest that ART treatment factors specific to the in vitro culture environment, and/or freezing/thawing procedures, may influence the way the embryo responds to the surrounding maternal environment during development. ART treatment may alter the embryo’s epigenome, which therefore responds differently to the influence of homocysteine during pregnancy.
This study is the first to analyze, longitudinally, embryonic, and fetal growth from the first trimester until birth. Detection of early pregnancy intrauterine growth is currently advantageous, as the majority of studies include birth as the earliest measurable time point. With this approach, we were able to keep track of offspring development throughout pregnancy, knowing that growth patterns are GA-dependent. All included longitudinal measurements have previously shown to have excellent inter- and intra-observer reproducibility [17]. The same fetal measurements at late gestation were analyzed both at single and multiple time points, using different measurement approaches, which reinforced the reliability of the results. Lastly, the VR approach to perform 3D embryonic measurements substantially improved the preciseness of measurements as opposed to 2D measurements.
The study design is a tertiary cohort, which includes a high-risk population that may introduce bias in the results and reduce external validity. A population-based cohort may avoid such interferences [52]. Moreover, we adjusted for confounders based on published knowledge and, as a result, residual confounding could be considered as analysis limitation. The sample size of the subpopulation was also a limitation. Growth measurements are a reflection of gross anatomy and have limited usefulness when trying to understand underlying molecular and biological processes. Animal studies would provide complementary insights in this regard [2,3,6].
Reduced embryonic and fetal growth is a sign of disturbed development and can lead to adverse postnatal growth patterns and development with long-lasting effects during the life course [53,54]. For this reason, reduced embryonic growth patterns in the first trimester and low birth weight, associated with elevated homocysteine exposure, may represent a risk factor for adverse postnatal effects. Here we confirm that homocysteine is a relevant biomarker for periconceptional health conditions in clinical practice. Caregivers should be aware that homocysteine is a sensitive marker for maternal health status, particularly with regards to nutrition (B vitamin deficiencies) and lifestyle [2]. We therefore recommend routine analysis of homocysteine levels in preconceptional and pregnant women and their partners, to treat such imbalances in a timely manner, as it also has been reported that high homocysteine levels in men affect sperm quality and DNA methylation [55,56]. If homocysteine is found to be elevated during pregnancy, extra fetal ultrasound examinations should be considered to aid decision making regarding obstetric surveillance (e.g., if growth restriction or changes in growth patterns are detected). Based on our findings, we recommend that special attention should be given to women who require ART treatment and who undergo a frozen cycle. Treatment could be postponed in cases of elevated maternal (and paternal) homocysteine levels. In combination with this, preconceptional and pregnant women should be encouraged to follow a healthy diet and lifestyle, to reduce the risks of elevated homocysteine levels during the periconception period and beyond. This can be achieved via tailored and ‘blended’ lifestyle care (e.g., smarterpregnancy.co.uk, accessed on 20-12-2021) [57,58,59,60,61,62].
Future research should investigate the role of homocysteine in women undergoing ART treatment to identify which factors related to fertility or the ART treatment itself influence the embryo’s response to maternal one-carbon metabolism. Lastly, during pregnancy, the reference range of homocysteine should be redefined or adapted, as high levels of homocysteine within the current reference range appear to negatively impact prenatal growth.
Acknowledgments
We would like to acknowledge all the researchers that have performed the ultrasound examinations and measured the embryos since the beginning of the study, and Anton Koning for converting the 3D ultrasounds into VR. Moreover, we would like to thank all women and their partners who participated in the Predict Study.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14061129/s1. Table S1: Comparison between cases of reference range homocysteine and hyperhomocysteinemia in the starting population, Table S2: Maternal baseline characteristics of the included and excluded population, Table S3: Association between maternal homocysteine, CRL and EV at 7, 9 and 11 weeks of gestation, Table S4: Association between maternal homocysteine and longitudinal first trimester embryonic head measurements in the included population (n = 118), natural pregnancies (n = 71) and IVF/ICSI pregnancies (n = 47), Table S5: Association between maternal homocysteine and longitudinal second and third trimester fetal growth in the included population (n= 269), natural pregnancies (n = 145) and IVF/ICSI pregnancies (n = 124), Table S6: Association between maternal homocysteine and neonatal birth weight in the included population (n = 1060), natural pregnancies (n = 555) and IVF/ICSI pregnancies (n = 505), Table S7: Association between quartiles of homocysteine and Hoftiezer percentiles in the included population (n = 983), natural pregnancies (n = 529) and IVF/ICSI pregnancies (n = 454).
Author Contributions
Conceptualization, E.R., M.R. and K.M.S.; formal analysis, E.R. and S.P.W.; writing—original draft preparation, E.R. and K.M.S.; writing—review and editing, K.M.S., S.S., K.D.S., M.R. and R.P.M.S.-T.; supervision, M.R., S.S. and R.P.M.S.-T.; project administration, R.P.M.S.-T. All authors have read and agreed to the published version of the manuscript.
Funding
This project has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement No. 812660. K.D.S. was in receipt of funding from the Biotechnology and Biological Sciences Research Council (BBSRC) (BB/K017810/1).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Central Committee on Research in The Hague and the local Medical Ethics Committee of the Erasmus MC (MEC-2004-227).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kalhan S.C. One carbon metabolism in pregnancy: Impact on maternal, fetal and neonatal health. Mol. Cell Endocrinol. 2016;435:48–60. doi: 10.1016/j.mce.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steegers-Theunissen R.P., Twigt J., Pestinger V., Sinclair K.D. The periconceptional period, reproduction and long-term health of offspring: The importance of one-carbon metabolism. Hum. Reprod. Update. 2013;19:640–655. doi: 10.1093/humupd/dmt041. [DOI] [PubMed] [Google Scholar]
- 3.Clare C.E., Brassington A.H., Kwong W.Y., Sinclair K.D. One-Carbon Metabolism: Linking Nutritional Biochemistry to Epigenetic Programming of Long-Term Development. Annu. Rev. Anim. Biosci. 2019;7:263–287. doi: 10.1146/annurev-animal-020518-115206. [DOI] [PubMed] [Google Scholar]
- 4.Ducker G.S., Rabinowitz J.D. One-Carbon Metabolism in Health and Disease. Cell Metab. 2017;25:27–42. doi: 10.1016/j.cmet.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medina M., Urdiales J.L., Amores-Sanchez M.I. Roles of homocysteine in cell metabolism: Old and new functions. Eur. J. Biochem. 2001;268:3871–3882. doi: 10.1046/j.1432-1327.2001.02278.x. [DOI] [PubMed] [Google Scholar]
- 6.Xu J., Sinclair K.D. One-carbon metabolism and epigenetic regulation of embryo development. Reprod. Fertil. Dev. 2015;27:667–676. doi: 10.1071/RD14377. [DOI] [PubMed] [Google Scholar]
- 7.Takimoto H., Mito N., Umegaki K., Ishiwaki A., Kusama K., Abe S., Yamawaki M., Fukuoka H., Ohta C., Yoshiike N. Relationship between dietary folate intakes, maternal plasma total homocysteine and B-vitamins during pregnancy and fetal growth in Japan. Eur. J. Nutr. 2007;46:300–306. doi: 10.1007/s00394-007-0667-6. [DOI] [PubMed] [Google Scholar]
- 8.Lindblad B., Zaman S., Malik A., Martin H., Ekstrom A.M., Amu S., Holmgren A., Norman M. Folate, vitamin B12, and homocysteine levels in South Asian women with growth-retarded fetuses. Acta Obstet. Gynecol. Scand. 2005;84:1055–1061. doi: 10.1111/j.0001-6349.2005.00876.x. [DOI] [PubMed] [Google Scholar]
- 9.Bergen N.E., Jaddoe V.W., Timmermans S., Hofman A., Lindemans J., Russcher H., Raat H., Steegers-Theunissen R.P., Steegers E.A. Homocysteine and folate concentrations in early pregnancy and the risk of adverse pregnancy outcomes: The Generation R Study. BJOG. 2012;119:739–751. doi: 10.1111/j.1471-0528.2012.03321.x. [DOI] [PubMed] [Google Scholar]
- 10.Parisi F., Rousian M., Koning A.H., Willemsen S.P., Cetin I., Steegers-Theunissen R.P. Periconceptional maternal one-carbon biomarkers are associated with embryonic development according to the Carnegie stages. Hum. Reprod. 2017;32:523–530. doi: 10.1093/humrep/dew349. [DOI] [PubMed] [Google Scholar]
- 11.Parisi F., Rousian M., Koning A.H., Willemsen S.P., Cetin I., Steegers E.A., Steegers-Theunissen R.P. Periconceptional maternal biomarkers of one-carbon metabolism and embryonic growth trajectories: The Rotterdam Periconceptional Cohort (Predict Study) Fertil Steril. 2017;107:691–698.e1. doi: 10.1016/j.fertnstert.2016.11.030. [DOI] [PubMed] [Google Scholar]
- 12.Ars C.L., Nijs I.M., Marroun H.E., Muetzel R., Schmidt M., Steenweg-de Graaff J., van der Lugt A., Jaddoe V.W., Hofman A., Steegers E.A., et al. Prenatal folate, homocysteine and vitamin B12 levels and child brain volumes, cognitive development and psychological functioning: The Generation R Study. Br. J. Nutr. 2019;122:S1–S9. doi: 10.1017/S0007114515002081. [DOI] [PubMed] [Google Scholar]
- 13.Tan A., Sinclair G., Mattman A., Vallance H.D., Lamers Y. Maternal vitamin B12 status in early pregnancy and its association with birth outcomes in Canadian mother-newborn Dyads. Br. J. Nutr. 2021;126:1823–1831. doi: 10.1017/S0007114521000581. [DOI] [PubMed] [Google Scholar]
- 14.Steegers-Theunissen R.P., Boers G.H., Blom H.J., Nijhuis J.G., Thomas C.M., Borm G.F., Eskes T.K. Neural tube defects and elevated homocysteine levels in amniotic fluid. Am. J. Obstet. Gynecol. 1995;172:1436–1441. doi: 10.1016/0002-9378(95)90474-3. [DOI] [PubMed] [Google Scholar]
- 15.Steegers-Theunissen R.P., Boers G.H., Trijbels F.J., Eskes T.K. Neural-tube defects and derangement of homocysteine metabolism. N. Engl. J. Med. 1991;324:199–200. doi: 10.1056/NEJM199101173240315. [DOI] [PubMed] [Google Scholar]
- 16.van Uitert E.M., van Ginkel S., Willemsen S.P., Lindemans J., Koning A.H., Eilers P.H., Exalto N., Laven J.S., Steegers E.A., Steegers-Theunissen R.P. An optimal periconception maternal folate status for embryonic size: The Rotterdam Predict study. BJOG. 2014;121:821–829. doi: 10.1111/1471-0528.12592. [DOI] [PubMed] [Google Scholar]
- 17.Rousian M., Schoenmakers S., Eggink A.J., Gootjes D.V., Koning A.H.J., Koster M.P.H., Mulders A., Baart E.B., Reiss I.K.M., Laven J.S.E., et al. Cohort Profile Update: The Rotterdam Periconceptional Cohort and embryonic and fetal measurements using 3D ultrasound and virtual reality techniques. Int. J. Epidemiol. 2021;50:6294444. doi: 10.1093/ije/dyab030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang S.S., Wong P.W., Malinow M.R. Hyperhomocyst(e)inemia as a risk factor for occlusive vascular disease. Annu. Rev. Nutr. 1992;12:279–298. doi: 10.1146/annurev.nu.12.070192.001431. [DOI] [PubMed] [Google Scholar]
- 19.Tinelli C., Di Pino A., Ficulle E., Marcelli S., Feligioni M. Hyperhomocysteinemia as a Risk Factor and Potential Nutraceutical Target for Certain Pathologies. Front. Nutr. 2019;6:49. doi: 10.3389/fnut.2019.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.CBS Opleidingsniveau. 2021. [(accessed on 20 December 2021)]. Available online: https://www.cbs.nl/nl-nl/nieuws/2019/33/verschil-levensverwachting-hoog-en-laagopgeleid-groeit/opleidingsniveau.
- 21.Rousian M., Koster M.P.H., Mulders A., Koning A.H.J., Steegers-Theunissen R.P.M., Steegers E.A.P. Virtual reality imaging techniques in the study of embryonic and early placental health. Placenta. 2018;64((Suppl. 1)):S29–S35. doi: 10.1016/j.placenta.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 22.Rousian M., Koning A.H., van der Spek P.J., Steegers E.A., Exalto N. Virtual reality for embryonic measurements requiring depth perception. Fertil. Steril. 2011;95:773–774. doi: 10.1016/j.fertnstert.2010.12.032. [DOI] [PubMed] [Google Scholar]
- 23.Baken L., van Gruting I.M., Steegers E.A., van der Spek P.J., Exalto N., Koning A.H. Design and validation of a 3D virtual reality desktop system for sonographic length and volume measurements in early pregnancy evaluation. J. Clin. Ultrasound. 2015;43:164–170. doi: 10.1002/jcu.22207. [DOI] [PubMed] [Google Scholar]
- 24.Husen S.C., Koning I.V., Go A., van Graafeiland A.W., Willemsen S.P., Groenenberg I.A.L., Steegers-Theunissen R.P.M. Three-dimensional ultrasound imaging of fetal brain fissures in the growth restricted fetus. PLoS ONE. 2019;14:e0217538. doi: 10.1371/journal.pone.0217538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Welling M.S., Husen S.C., Go A., Groenenberg I.A.L., Willemsen S.P., Bijma H.H., Steegers-Theunissen R.P.M. Growth trajectories of the human fetal brain in healthy and complicated pregnancies and associations with neurodevelopmental outcome in the early life course. Early Hum. Dev. 2020;151:105224. doi: 10.1016/j.earlhumdev.2020.105224. [DOI] [PubMed] [Google Scholar]
- 26.Hadlock F.P., Harrist R.B., Sharman R.S., Deter R.L., Park S.K. Estimation of fetal weight with the use of head, body, and femur measurement—A prospective study. Am. J. Obstet. Gynecol. 1985;151:333–337. doi: 10.1016/0002-9378(85)90298-4. [DOI] [PubMed] [Google Scholar]
- 27.van Uitert E.M., van der Elst-Otte N., Wilbers J.J., Exalto N., Willemsen S.P., Eilers P.H., Koning A.H., Steegers E.A., Steegers-Theunissen R.P. Periconception maternal characteristics and embryonic growth trajectories: The Rotterdam Predict study. Hum. Reprod. 2013;28:3188–3196. doi: 10.1093/humrep/det375. [DOI] [PubMed] [Google Scholar]
- 28.Koning I.V., Dudink J., Groenenberg I.A.L., Willemsen S.P., Reiss I.K.M., Steegers-Theunissen R.P.M. Prenatal cerebellar growth trajectories and the impact of periconceptional maternal and fetal factors. Hum. Reprod. 2017;32:1230–1237. doi: 10.1093/humrep/dex079. [DOI] [PubMed] [Google Scholar]
- 29.Parisi F., Rousian M., Koning A.H.J., Willemsen S.P., Steegers E.A.P., Steegers-Theunissen R.P.M. Effect of human embryonic morphological development on fetal growth parameters: The Rotterdam Periconceptional Cohort (Predict Study) Reprod. Biomed. Online. 2019;38:613–620. doi: 10.1016/j.rbmo.2018.12.016. [DOI] [PubMed] [Google Scholar]
- 30.Koning I.V., Baken L., Groenenberg I.A., Husen S.C., Dudink J., Willemsen S.P., Gijtenbeek M., Koning A.H., Reiss I.K., Steegers E.A., et al. Growth trajectories of the human embryonic head and periconceptional maternal conditions. Hum. Reprod. 2016;31:968–976. doi: 10.1093/humrep/dew043. [DOI] [PubMed] [Google Scholar]
- 31.Salomon L.J., Alfirevic Z., Da Silva Costa F., Deter R.L., Figueras F., Ghi T., Glanc P., Khalil A., Lee W., Napolitano R., et al. ISUOG Practice Guidelines: Ultrasound assessment of fetal biometry and growth. Ultrasound Obstet. Gynecol. 2019;53:715–723. doi: 10.1002/uog.20272. [DOI] [PubMed] [Google Scholar]
- 32.Hoftiezer L., Hof M.H.P., Dijs-Elsinga J., Hogeveen M., Hukkelhoven C., van Lingen R.A. From population reference to national standard: New and improved birthweight charts. Am. J. Obstet. Gynecol. 2019;220:383.e1–383.e17. doi: 10.1016/j.ajog.2018.12.023. [DOI] [PubMed] [Google Scholar]
- 33.Liu C., Luo D., Wang Q., Ma Y., Ping L., Wu T., Tang J., Peng D., Zhao P. Serum homocysteine and folate concentrations in early pregnancy and subsequent events of adverse pregnancy outcome: The Sichuan Homocysteine study. BMC Pregnancy Childbirth. 2020;20:176. doi: 10.1186/s12884-020-02860-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Bayyari N., Hamadneh J., Hailat R., Hamadneh S. Total homocysteine is positively correlated with body mass index, waist-to-hip ratio, and fat mass among overweight reproductive women: A cross-sectional study. Nutr. Res. 2017;48:9–15. doi: 10.1016/j.nutres.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 35.Tuenter A., Bautista Nino P.K., Vitezova A., Pantavos A., Bramer W.M., Franco O.H., Felix J.F. Folate, vitamin B12, and homocysteine in smoking-exposed pregnant women: A systematic review. Matern. Child. Nutr. 2019;15:e12675. doi: 10.1111/mcn.12675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Drake A.J., O’Shaughnessy P.J., Bhattacharya S., Monteiro A., Kerrigan D., Goetz S., Raab A., Rhind S.M., Sinclair K.D., Meharg A.A., et al. In utero exposure to cigarette chemicals induces sex-specific disruption of one-carbon metabolism and DNA methylation in the human fetal liver. BMC Med. 2015;13:18. doi: 10.1186/s12916-014-0251-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaye A.D., Jeha G.M., Pham A.D., Fuller M.C., Lerner Z.I., Sibley G.T., Cornett E.M., Urits I., Viswanath O., Kevil C.G. Folic Acid Supplementation in Patients with Elevated Homocysteine Levels. Adv. Ther. 2020;37:4149–4164. doi: 10.1007/s12325-020-01474-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spijkers S., Lens J.W., Schats R., Lambalk C.B. Fresh and Frozen-Thawed Embryo Transfer Compared to Natural Conception: Differences in Perinatal Outcome. Gynecol. Obstet. Investig. 2017;82:538–546. doi: 10.1159/000468935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Luke B., Brown M.B., Wantman E., Stern J.E., Toner J.P., Coddington C.C., 3rd Increased risk of large-for-gestational age birthweight in singleton siblings conceived with in vitro fertilization in frozen versus fresh cycles. J. Assist. Reprod. Genet. 2017;34:191–200. doi: 10.1007/s10815-016-0850-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Duijn L., Hoek J., Rousian M., Baart E.B., Willemsen S.P., Laven J.S.E., Steegers-Theunissen R.P.M., Schoenmakers S. Prenatal growth trajectories and birth outcomes after frozen-thawed extended culture embryo transfer and fresh embryo transfer: The Rotterdam Periconception Cohort. Reprod. Biomed. Online. 2021;43:279–287. doi: 10.1016/j.rbmo.2021.04.013. [DOI] [PubMed] [Google Scholar]
- 41.Rubini E., Baijens I.M.M., Horanszky A., Schoenmakers S., Sinclair K.D., Zana M., Dinnyes A., Steegers-Theunissen R.P.M., Rousian M. Maternal One-Carbon Metabolism during the Periconceptional Period and Human Foetal Brain Growth: A Systematic Review. Genes. 2021;12:1634. doi: 10.3390/genes12101634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nilsen R.M., Vollset S.E., Monsen A.L., Ulvik A., Haugen M., Meltzer H.M., Magnus P., Ueland P.M. Infant birth size is not associated with maternal intake and status of folate during the second trimester in Norwegian pregnant women. J. Nutr. 2010;140:572–579. doi: 10.3945/jn.109.118158. [DOI] [PubMed] [Google Scholar]
- 43.Takimoto H., Hayashi F., Kusama K., Kato N., Yoshiike N., Toba M., Ishibashi T., Miyasaka N., Kubota T. Elevated maternal serum folate in the third trimester and reduced fetal growth: A longitudinal study. J. Nutr. Sci. Vitaminol. 2011;57:130–137. doi: 10.3177/jnsv.57.130. [DOI] [PubMed] [Google Scholar]
- 44.Bergen N.E., Schalekamp-Timmermans S., Jaddoe V.W., Hofman A., Lindemans J., Russcher H., Tiemeier H., Steegers-Theunissen R.P., Steegers E.A. Maternal and Neonatal Markers of the Homocysteine Pathway and Fetal Growth: The Generation R Study. Paediatr. Perinat. Epidemiol. 2016;30:386–396. doi: 10.1111/ppe.12297. [DOI] [PubMed] [Google Scholar]
- 45.Hoek J., Schoenmakers S., Ringelberg B., Reijnders I.F., Willemsen S.P., De Rijke Y.B., Mulders A., Steegers-Theunissen R.P.M. Periconceptional maternal and paternal homocysteine levels and early utero-placental (vascular) growth trajectories: The Rotterdam periconception cohort. Placenta. 2021;115:45–52. doi: 10.1016/j.placenta.2021.09.012. [DOI] [PubMed] [Google Scholar]
- 46.Eskes T.K. Clotting disorders and placental abruption: Homocysteine—A new risk factor. Eur. J. Obstet. Gynecol. Reprod. Biol. 2001;95:206–212. doi: 10.1016/S0301-2115(00)00492-9. [DOI] [PubMed] [Google Scholar]
- 47.Chaudhry S.H., Taljaard M., MacFarlane A.J., Gaudet L.M., Smith G.N., Rodger M., Rennicks White R., Walker M.C., Wen S.W. The role of maternal homocysteine concentration in placenta-mediated complications: Findings from the Ottawa and Kingston birth cohort. BMC Pregnancy Childbirth. 2019;19:75. doi: 10.1186/s12884-019-2219-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hogeveen M., Blom H.J., den Heijer M. Maternal homocysteine and small-for-gestational-age offspring: Systematic review and meta-analysis. Am. J. Clin. Nutr. 2012;95:130–136. doi: 10.3945/ajcn.111.016212. [DOI] [PubMed] [Google Scholar]
- 49.Yajnik C.S., Chandak G.R., Joglekar C., Katre P., Bhat D.S., Singh S.N., Janipalli C.S., Refsum H., Krishnaveni G., Veena S., et al. Maternal homocysteine in pregnancy and offspring birthweight: Epidemiological associations and Mendelian randomization analysis. Int. J. Epidemiol. 2014;43:1487–1497. doi: 10.1093/ije/dyu132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Murphy M.M., Scott J.M., Arija V., Molloy A.M., Fernandez-Ballart J.D. Maternal homocysteine before conception and throughout pregnancy predicts fetal homocysteine and birth weight. Clin. Chem. 2004;50:1406–1412. doi: 10.1373/clinchem.2004.032904. [DOI] [PubMed] [Google Scholar]
- 51.Cai S., Quan S., Yang G., Ye Q., Chen M., Yu H., Wang G., Wang Y., Zeng X., Qiao S. One Carbon Metabolism and Mammalian Pregnancy Outcomes. Mol. Nutr. Food Res. 2021;65:e2000734. doi: 10.1002/mnfr.202000734. [DOI] [PubMed] [Google Scholar]
- 52.Kooijman M.N., Kruithof C.J., van Duijn C.M., Duijts L., Franco O.H., van Ijzendoorn M.H., de Jongste J.C., Klaver C.C., van der Lugt A., Mackenbach J.P., et al. The Generation R Study: Design and cohort update 2017. Eur. J. Epidemiol. 2016;31:1243–1264. doi: 10.1007/s10654-016-0224-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Henrichs J., Schenk J.J., Barendregt C.S., Schmidt H.G., Steegers E.A., Hofman A., Jaddoe V.W., Moll H.A., Verhulst F.C., Tiemeier H. Fetal growth from mid- to late pregnancy is associated with infant development: The Generation R Study. Dev. Med. Child Neurol. 2010;52:644–651. doi: 10.1111/j.1469-8749.2009.03513.x. [DOI] [PubMed] [Google Scholar]
- 54.Broere-Brown Z.A., Schalekamp-Timmermans S., Jaddoe V.W.V., Steegers E.A.P. Deceleration of fetal growth rate as alternative predictor for childhood outcomes: A birth cohort study. BMC Pregnancy Childbirth. 2019;19:216. doi: 10.1186/s12884-019-2358-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Forges T., Monnier-Barbarino P., Alberto J.M., Gueant-Rodriguez R.M., Daval J.L., Gueant J.L. Impact of folate and homocysteine metabolism on human reproductive health. Hum. Reprod. Update. 2007;13:225–238. doi: 10.1093/humupd/dml063. [DOI] [PubMed] [Google Scholar]
- 56.Yu Y., Jia C., Shi Q., Zhu Y., Liu Y. Hyperhomocysteinemia in men with a reproductive history of fetal neural tube defects: Three case reports and literature review. Medicine. 2019;98:e13998. doi: 10.1097/MD.0000000000013998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van der Windt M., Schoenmakers S., Willemsen S., van Rossem L., Steegers-Theunissen R. Optimizing the Periconception Lifestyle of Women With Overweight Using a Blended Personalized Care Intervention Combining eHealth and Face-to-face Counseling (eFUSE): Protocol for a Randomized Controlled Trial. JMIR Res. Protoc. 2021;10:e28600. doi: 10.2196/28600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.van der Windt M., van der Kleij R.M., Snoek K.M., Willemsen S.P., Dykgraaf R.H.M., Laven J.S.E., Schoenmakers S., Steegers-Theunissen R.P.M. Impact of a Blended Periconception Lifestyle Care Approach on Lifestyle Behaviors: Before-and-After Study. J. Med. Internet Res. 2020;22:e19378. doi: 10.2196/19378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Dijk M.R., Koster M.P.H., Oostingh E.C., Willemsen S.P., Steegers E.A.P., Steegers-Theunissen R.P.M. A Mobile App Lifestyle Intervention to Improve Healthy Nutrition in Women Before and During Early Pregnancy: Single-Center Randomized Controlled Trial. J. Med. Internet Res. 2020;22:e15773. doi: 10.2196/15773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.van Dijk M.R., Koster M.P.H., Willemsen S.P., Huijgen N.A., Laven J.S.E., Steegers-Theunissen R.P.M. Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod. Biomed. Online. 2017;35:453–460. doi: 10.1016/j.rbmo.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 61.Oostingh E.C., Koster M.P.H., van Dijk M.R., Willemsen S.P., Broekmans F.J.M., Hoek A., Goddijn M., Klijn N.F., van Santbrink E.J.P., Steegers E.A.P., et al. First effective mHealth nutrition and lifestyle coaching program for subfertile couples undergoing in vitro fertilization treatment: A single-blinded multicenter randomized controlled trial. Fertil. Steril. 2020;114:945–954. doi: 10.1016/j.fertnstert.2020.04.051. [DOI] [PubMed] [Google Scholar]
- 62.Oostingh E.C., Ophuis R.H., Koster M.P., Polinder S., Lingsma H.F., Laven J.S., Steegers-Theunissen R.P. Mobile Health Coaching on Nutrition and Lifestyle Behaviors for Subfertile Couples Using the Smarter Pregnancy Program: Model-Based Cost-Effectiveness Analysis. JMIR Mhealth Uhealth. 2019;7:e13935. doi: 10.2196/13935. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.