Abstract
Oromandibular dystonia (OMD) is a clinical problem which is commonly encountered in the practice of movement disorders. OMD results from a variety of genetic and acquired etiologies and can occur as an isolated manifestation, or as part of an isolated generalized or a combined dystonia syndrome. There are only very few systematic reviews on this condition which often causes significant disability. We review here the etiology, clinical features, diagnostic approach and management of OMD.
Keywords: Approach, etiology, oromandibular dystonia
INTRODUCTION
Cranial dystonia may involve the upper face or the lower face, jaw, tongue and pharynx.[1] Cranial dystonia involving the upper part of face includes blepharospasm, oculogyric crisis, and frontalis dystonia. The term oromandibular dystonia (OMD) is used to denote lower cranial dystonia, involving the muscles of the lower face, jaw, tongue and pharynx.[2] OMD commonly occurs together with blepharospasm, and the combination is generally called Meige syndrome.[3] OMD can be seen in a variety of scenarios, either in isolation, as part of a more widespread dystonia, or as a part of a combined dystonia syndrome with a broader clinical presentation. Identification of lower cranial dystonia in isolated generalized and combined dystonia syndromes guides etiological diagnosis, because of its association with specific etiologies. In this review, we will discuss the clinical features, etiology, and approach to diagnosis and management of oromandibular dystonia.
SEARCH STRATEGY
Relevant studies on OMD were reviewed using PubMed search. The key words “oromandibular dystonia”, “lower cranial dystonia,” “facial dystonia,” “orofacial dystonia,” “mandibular dystonia,” and “lingual dystonia” were used and articles published till 5th October 2020 were considered. A total of 65 articles on “lower cranial dystonia,” 1142 articles on “facial dystonia” (122 on “lower facial dystonia”), 175 articles on “orofacial dystonia,” 147 articles on “mandibular dystonia,” 405 articles on “oromandibular dystonia,” and 287 articles on “lingual dystonia,” were found. The abstracts were reviewed by the authors and articles relevant for this review were selected.
EPIDEMIOLOGY AND DEMOGRAPHIC FEATURES
The prevalence of OMD is estimated to be 68.9 cases/million.[4] The onset of OMD peaks in the sixth decade of life.[5] Women are almost twice as frequently affected as men. Hormonal factors probably play a role in this; an interesting, 12-year follow up of a patient with OMD highlighted the influence of hormonal factors on OMD, with severity of symptoms varying in different phases of menstrual cycle.[6]
ETIOLOGICAL FACTORS
Most cases of OMD occur in combination with blepharospasm or dystonia in other body parts, manifesting as an isolated phenomenon only in 2–23% of the cases.[7] In the largest study on OMD till date, only 34.2% of patients had focal OMD whereas 54.6% had OMD as part of segmental dystonia and 11.3% presented with generalized dystonia.[5]
”Primary” (Dystonia presenting and remaining as an isolated phenomenon, without evidence of neurodegeneration, structural brain damage or other detectable non-genetic etiology) or idiopathic dystonia due to a genetic or presumed genetic cause is the commonest etiology sub-type of OMD, accounting for >60% of cases.[8] Tardive dystonia (drug-induced) is the most common cause of secondary OMD, reported in 22.8% of the cases. Other described causes are peripheral-induced OMD (related to orofacial trauma) in 9.3% of the cases, post-anoxic states in 2.5%, neurodegenerative disorders in 1.8%, and head injury-associated OMD in 0.9%.[8] However, in a large series of lingual dystonia, 41% of cases were reported to be secondary to medications, 18% were associated with heredodegenerative conditions and post-encephalitic state, 12% occurred as part of isolated generalized dystonia and 29% were focal and presumed to be “primary.”[9]
CLINICAL FEATURES
Dystonia is defined as a movement disorder characterized by sustained or intermittent muscle contractions causing abnormal, often repetitive, movements, postures, or both. Dystonic movements are typically patterned, twisting, and may be tremulous, are often initiated or worsened by voluntary action and are associated with overflow muscle activation. Dystonia is classified along two axes: clinical characteristics and etiology.[10] Clinically, dystonia may be either isolated (Dystonia, with or without dystonic tremor, being the only abnormality on neurological examination) or combined (Dystonia with other movement disorders, neurological examination abnormalities or evidence of systemic involvement). A careful clinical examination and confirmation of clinical phenomenology of dystonia and associated neurological and systemic features help to arrive at a syndromic diagnosis, narrow down the etiological possibilities and guide diagnostic investigations.
Oromandibular dystonia has to be differentiated from chorea involving the lower facial muscles. Cranial dystonia usually consists of prolonged movements and postures, which are distressing to the patient, and cause functional disability. On the contrary, orofacial chorea consists of brief and non-patterned movements, which may not be distressing to the patient and does not cause functional disability.[11] Similar to OMD, facial dystonic tics are often patterned, but associated sensory phenomena, urge to perform the movements and relief after performing the movements will help to make the correct phenomenological diagnosis.
OMD consists of sustained or intermittent involuntary, repetitive, patterned muscle contractions affecting the lower part of the face, mouth, jaw, tongue, and pharynx. It can be associated with difficulties in speaking, chewing, swallowing, and even breathing. Usual triggers include stress, speaking and swallowing.[12] The first symptom is usually precipitated by specific movements or actions (action dystonia), later on progressing to involve additional actions and then occurring at rest and the spasms becoming more intense. Morning benefit (milder symptoms during morning) and overflow phenomenon (activation of muscles which are not otherwise involved, during certain tasks) are relatively common. OMD can be subdivided into different subtypes: jaw-opening dystonia, jaw-closing dystonia, jaw-deviating dystonia, perioral dystonia, and/or lingual dystonia.[13] Jaw opening dystonia is caused by sustained contractions of the lateral pterygoid muscles presenting as involuntary opening and/or inability to close the mouth. Prolonged jaw opening results in difficulty with mastication, swallowing and causes drooling. Patients have difficulty articulating and may have unintelligible speech.[14] Jaw closing dystonia can occur alone, or in association with jaw opening dystonia. Sustained contractions of the masseter and/or temporalis muscles result in trismus and jaw clenching. Forced jaw closure may damage the lips, gums, tongue and buccal mucosa. Teeth may be cracked, and it may be impossible to maintain dentures in place. Temporomandibular joint pain may occur, along with recurrent jaw dislocation. Jaw closing dystonia has been described in musicians who play wind instruments and develop task-specific dystonia in response to attempting to play their instrument.[15]
Isolated OMD is often misdiagnosed as dental problems, bruxism or temporomandibular joint disorders. The association of OMD with temporomandibular joint disorders is also known. Occasionally, OMD may be asymmetrical or even unilateral, thus mimicking hemifacial spasm or hemi-masticatory spasm.[16,17]
OMD could lead to secondary complications and these should be looked for while examining the patient. It can cause dysphagia, speech disorders, subluxation of the temporomandibular joint, deviation of the mandible, and soft-tissue trauma intraorally. Occlusal relationship may change and significant weight loss can occur due to poor oral intake.
Muscles of the pharynx and larynx may also be involved in patients with OMD; larynx is considered as a separate body region and not part of cranial dystonia in the current classification of dystonia.[10] When larynx is involved, the voice may become harsh, hoarse and strained, a condition termed spasmodic dysphonia. Cervical dystonia is also a common accompaniment of OMD; less often distal muscles, such as those of the upper limbs may also be affected. The upper limb dystonia may manifest as dystonic tremor alone and posturing may not be evident. Careful examination for additional neurological examination abnormalities like parkinsonism, pyramidal signs, ataxia and polyneuropathy should be done in all patients as these are often seen in patients with OMD resulting from conditions causing progressive neurodegeneration or structural damage.
CLUES TO ETIOLOGICAL DIAGNOSIS
The conditions which cause OMD, either as an isolated phenomenon, part of a generalized dystonia syndrome, or as part of more diffuse neurological involvement, are listed in Tables 1 and 2. Though the list is long, careful analysis of the clinical characteristics (e.g., age at onset, temporal course, additional body regions affected and additional neurologic and systemic features) help to narrow down the differentials and tailor the battery of diagnostic investigations for the individual patient.
Table 1.
Acquired causes of OMD
| Drugs & toxins |
| Neuroleptics-typical and atypical (Acute and Tardive) |
| Antidepressants[18] (Sertraline, Citalopram, Venlafaxine, Fluoxetine, |
| Paroxetine, Amoxapine) |
| Anticonvulsants (Phenytoin, Sodium Valproate, Carbamazepine, |
| Lamotrigine) |
| Anti-emetics (Metoclopramide, Sulpiride, Domperidone, Cisapride) |
| Antibiotics (Cefixime,[19] Levofloxacin[20]) |
| Cetirizine,[21] Betahistine,[22] Promethazine,[23] Prochlorperazine, |
| Dextromethorphan[24] |
| Anaesthetic agents (Propofol, Sevoflurane, Fentanyl, Nitrous oxide[25]) |
| Capecitabine[26] |
| L-dopa, Methylphenidate,[27] Lithium |
| Alcohol, manganese, mercury, Carbon monoxide poisoning, glue sniffing |
| Metabolic/Endocrine |
| Kernicterus[28] |
| Hypoparathyroidism |
| Extrapontine myelinolysis[29] |
| Uremia,[30] acquired hepatocerebral degeneration[31] |
| Cerebral Palsy/Post hypoxic encephalopathy[32] |
| Autoimmune/paraneoplastic |
| SLE, APLA syndrome, Sjogren syndrome, Behcet syndrome,[33] |
| Coeliac disease |
| Anti- NMDA, LGI-1, CASPR2 encephalitis |
| anti-Hu, anti-Ri,[34] anti- Yo, IgLON5 |
| Satoyoshi syndrome[35] |
| Infections |
| HIV encephalitis,[36] CNS toxoplasmosis |
| Tuberculosis[37] |
| SSPE,[38] variant CJD |
| Mycoplasma,[39] West Nile Virus, Varicella Zoster,[40] Mumps, Japanese |
| Encephalitis[41] |
| Structural |
| Vascular (ischemic or hemorrhagic stroke) – Basal |
| ganglia/cerebellum/thalamus[42] |
| Brainstem neoplasm |
| Brainstem demyelination |
| Others |
| Traumatic brain injury |
| Radiation therapy[43] |
| Facial trauma |
| Functional |
APLA: Antiphospholipid antibody, CASPR2: Contactin-associated protein-like 2, CJD: Creutzfeldt-Jakob disease, HIV: Human Immunodeficiency virus, IgLON5: immunoglobulin-like cell adhesion molecule 5, LGI1: Leucine-rich, glioma inactivated 1, NMDA: N-methyl-D-aspartate, SSPE: Subacute sclerosing panencephalitis, SLE: Systemic lupus erythematosus
Table 2.
Genetic causes of OMD
| Autosomal dominant |
| DYT-THAP1, DYT-TAF1, DYT-ATP1A3, DYT-KMT2B, |
| DYT-PRKRA, DYT-TOR1A* |
| DYT-CIZ1, DYT-ANO3, DYT-GNAL |
| Spinocerebellar ataxia 1,2,3,8,12,36 |
| Neuroferritinopathy |
| Autosomal recessive |
| Pantothenate kinase associated neurodegeneration |
| Wilson’s disease |
| Chorea-acanthocytosis |
| Aceruloplasminemia |
| Niemann-Pick C |
| Gaucher disease |
| GM2 gangliosidosis |
| Type II GM1 gangliosidosis |
| Tay-Sachs disease |
| Friedreich’s ataxia[44] |
| Ataxia telangiectasia |
| Cerebrotendinous xanthomatosis |
| Methylmalonic aciduria[45] |
| Glutaric aciduria type 1 |
| Dopa-responsive dystonia |
| Dopamine transporter deficiency syndrome[46] |
| Hypermanganesemia with dystonia-1[47] |
| Fahr’s disease |
| DYT-COL6A3, DYT-HPCA, DYT-VPS16 |
| Woodhouse Sakati syndrome |
| COASY protein–associated neurodegeneration |
| Mitochondrial membrane protein–associated neurodegeneration |
| X-linked |
| Lesch Nyhan syndrome |
| McLeod syndrome[48] |
| Mitochondrial |
| Leigh syndrome |
| Deafness-dystonia syndrome[49] |
* Prominent OMD is unusual but could be seen in some patients with more severe manifestations
Isolated OMD in adulthood with or without spread to cranio-cervical region suggests a genetic etiology, without neurodegeneration or structural brain damage (”primary” dystonia). Cranial dystonia with onset in childhood and adolescence, even if isolated at onset, generally evolves into combined dystonia syndromes, and degenerative/heredo-degenerative etiologies are more likely.[50]
Tongue bite is encountered in tardive and idiopathic OMD and OMD associated with neurodegenerative etiologies like neuro-acanthocytosis, but not associated with the movement pattern in edentulous dyskinesia.[51] In a study comparing tardive with idiopathic OMD, oro-facial-lingual stereotypic movements were significantly more frequent in the tardive group. Presence of stereotypic movements in the limbs, akathisia, and respiratory dyskinesias in patients with OMD further suggests tardive etiology. Dystonia in tardive OMD was more likely to be restricted to the oromandibular region, whereas in patients with idiopathic OMD, there was often coexistent cervical dystonia.[8] This corroborates with finding of spread in isolated focal dystonia in a prospective cohort.[52] Dystonic tremor of the jaw and lips is described in embouchure dystonia and posttraumatic oromandibular dystonia, in addition to primary OMD.[53]
Geste antagoniste (sensory tricks) are usually observed in “primary dystonia,”[54] but have also been described rarely in some heredodegenerative conditions and dystonia associated with structural brain damage.[55] In patients with Pantothenate kinase-associated neurodegeneration (PKAN), a characteristic geste antagoniste for oromandibular (jaw opening) dystonia – touching chin with both hands – has been proposed as “mantis sign”.[56] Sensory tricks are also described in post-traumatic OMD.[57]
Singers have been described with spasmodic dysphonia but task-specific oromandibular dystonia are less common. Reported task-specific oromandibular dystonia include embouchure dystonia,[58] chewing-induced,[59] auctioneer's jaw[60] and prayer-induced dystonia.[61]
ACQUIRED DISORDERS
Drug-induced OMD is the commonest acquired cause, with dopamine receptor blocking agents the commonest drug group implicated. Other drugs precipitating OMD are listed in Table 1. Brainstem lesions due to demyelination or tumor, and ischemic and hemorrhagic stroke involving basal ganglia, thalamus or cerebellum, can cause OMD.[62]
Autoimmune encephalitis should be considered in the appropriate clinical scenario as it is imminently treatable. Anti-NMDA, anti-LGI1 and anti-Ri have been classically associated with oromandibular dystonia, but it has also been described in anti-Ma2[63] and anti-IgLON5.[64] Other immune disorders like Celiac disease,[65] Sjogren's syndrome[66] and lupus[67] presenting with OMD have also been described. The infections which are reported to present with OMD include CNS toxoplasmosis and Japanese encephalitis, which have a predilection to involve basal ganglia. Oromandibular-facial trauma, dental procedures and parotid gland surgery have been reported to precipitate and exacerbate OMD.[68,69] This has been termed as peripherally induced OMD, although the physiological and biochemical mechanisms are not well understood.[57] OMD can occur as sequelae of traumatic brain injury and hypoxic injury; OMD can be a prominent feature in children with dystonic cerebral palsy (CP), though isolated OMD as a manifestation of perinatal hypoxia is rare.
GENETIC CAUSES
Table 2 lists the genetic disorders which have OMD as part of clinical spectrum. Among the genetic causes presenting and remaining as isolated dystonia (erstwhile “primary dystonia”), involvement of lower cranial musculature helps in narrowing differential diagnosis. Genetic OMDs with onset in childhood-adolescence are likely to become generalized. These include DYT-THAP1, DYT-TAF1, DYT-ATP1A3, DYT-KMT2B and rarely DYT-TOR1A. Other OMDs with onset in adulthood remain focal or segmental (cranio-cervical). These include DYT-CIZ1, DYT-ANO3 and DYT-GNAL. DYT-COL6A3, DYT-HPCA and DYT-VPS16 are recessively inherited isolated dystonia, with symptom onset from childhood to adulthood, and dystonia distribution from focal to generalized.
Jaw dystonia is a prominent feature in Lesch-Nyhan syndrome, associated classically with self-injurious behavior and cognitive and behavioral disturbances. However, attenuated variants presenting with predominant dystonia have been reported.[70] Neurodegeneration with brain iron accumulation (NBIA) syndromes should be considered in patients with childhood or early adulthood onset cranio-cervical dystonia.[71] Associated features like Parkinsonism and pyramidal signs and radiological findings will point to the diagnosis. Jaw opening dystonia and facial dystonia have been described in type III GM1 gangliosidosis, observed in >80% of patients.[72,73,74] These are also seen in Niemann-Pick disease type C,[75] GM2 gangliosidosis,[76] Cerebrotendinous xanthomatosis,[77] Tay-Sachs disease[78] and Ataxia telangiectasia.[79,80]
Dopa responsive dystonia due to GTP-CH1 deficiency classically presents in childhood with lower limb dystonia, but progression to generalized dystonia is commonly described and cranial-cervical involvement was found in 68% of patients in one study.[81] Rare cases with isolated oromandibular dystonia have also been described.[82] Other pediatric neurotransmitter disorders with dopa-responsive dystonia phenotype have oculogyric crisis as a classical clinical feature,[83] but lower cranial dystonia is also reported. These should be considered in the appropriate age group because of the excellent treatment response. Dopamine transporter deficiency syndrome also has oromandibular dystonia as a prominent feature.[84]
OMD has been described in various Spinocerebellar ataxias including SCA1,[85] SCA2,[86] SCA3,[87] SCA8,[88] SCA12[89] and SCA36.[90] OMD may occur during the course of the illness, or rarely, can be the presenting feature. Dystonia was present in 14% of SCA2 patients in a cohort and was found to be associated with larger repeats.[91]
Mitochondrial disorders can present with hypokinetic and hyperkinetic movement disorders. Dystonia is the commonest hyperkinetic movement disorder observed and is usually generalized or multifocal, although focal dystonia involving the cranial musculature has also been described. Patients with mitochondrial disorders presenting with dystonia are more likely to harbor mtDNA mutations.[92]
FUNCTIONAL OMD
Involvement of the face represents 16.3% of all functional movement disorders (FMD) in a large series of patients.[93] Facial involvement is generally characterized by an episodic onset, highly variable course, inconsistency of presentation over time, higher prevalence in women (9:1) and young-adult population, and association with other conditions like atypical facial pain and migraine and other functional neurological symptoms like speech disturbances and weakness ipsilateral to the most affected side of face. The most common pattern of facial FMDs consists of tonic, sustained, lateral, and/or downward protrusion of one side of the lower lip with ipsilateral jaw deviation, as found in 84.3% of the largest series published so far.[93]
Unlike organic OMD, most subjects have asymmetric facial involvement and absence of geste antagoniste. FMDs are usually present at rest right from the beginning, in contrast to the task-specific/action induced dystonia occurring in OMD.[94] FMDs involving the face can often be triggered by examination of eye movements or by asking the patients to sustain muscular contraction of the face.
OMD should be differentiated from local/mechanical disorders of the mandible or temporomandibular joint. The occurrence of local pain and a careful observation of the nature of functional impairment (e.g. chewing difficulty) helps in the differential diagnosis.
DIAGNOSTIC EVALUATION
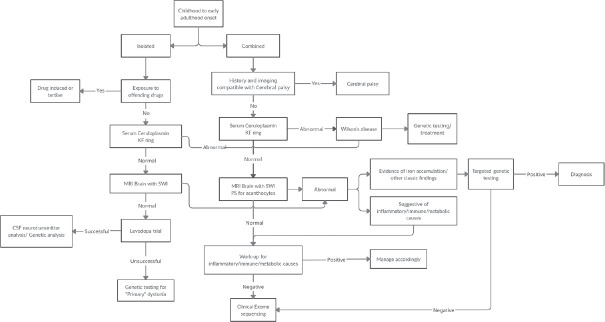
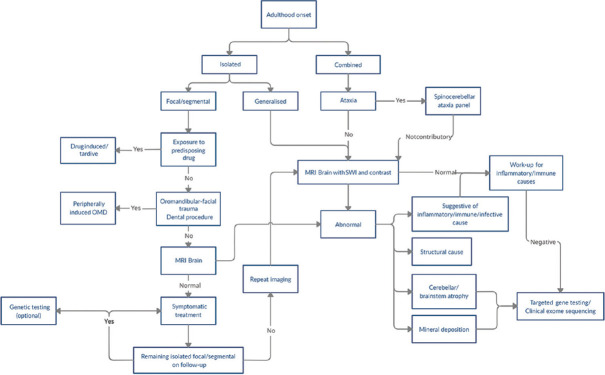
A detailed clinical history including drug history and the temporal evolution of dystonic and associated symptoms is key for evaluation of OMD as this provides useful information to tailor the investigations for the individual patient. Detailed physical examination to look for subtle dystonia elsewhere and for additional neurological signs should be done. Serum ceruloplasmin level and slit lamp exam to rule out Wilson's disease should be performed for all patients who present in childhood, adolescence or early adulthood. MRI Brain is necessary in all cases, unless a clear drug history suggesting tardive dystonia is present. MRI should include SWI sequences to look for evidence of iron accumulation. Specific investigations, including genetic studies, can be further performed based on the clinical phenotype and radiological findings. The diagnostic approach depends on the age of the patient as the possible etiologies vary depending on age of onset. In the absence of history suggestive of tardive dystonia, heredo-degenerative conditions or conditions with structural brain damage are more likely in children and young adults even if the OMD is isolated at the time of presentation. Figures 1 and 2 show simplified diagnostic algorithms which can be followed in children and adults respectively, who present with OMD. Certain clinicoradiological clues can guide the differential diagnosis [Table 3] and should not be missed.
Figure 1.
Approach to oromandibular dystonia with onset in childhood to early adulthood
Figure 2.
Approach to oromandibular dystonia with onset in adulthood
Table 3.
Clinicoradiological clues for specific etiology
| Clinicoradiological clue | Disease |
|---|---|
| Optic atrophy | Leigh syndrome |
| Methylmalonic aciduria | |
| Friedreich’s ataxia | |
| PLA2G6 associated neurodegeneration | |
| Pantothenate kinase associated neurodegeneration | |
| Mitochondrial membrane protein–associated neurodegeneration | |
| Cataract | Wilson’s disease |
| Cerebrotendinous xanthomatosis | |
| Oculogyric crisis | Tyrosine hydroxylase deficiency |
| Sepiapterin reductase deficiency | |
| 6-pyruvolyltetrahydropterin synthase deficiency | |
| Aromatic L-amino acid decarboxylase deficiency | |
| Drug induced | |
| Deafness | Leigh syndrome |
| Dystonia-deafness syndrome | |
| Woodhouse-Sakati Syndrome | |
| Cerebrotendinous xanthomatosis | |
| Self-injurious behavior[95] | Lesch-Nyhan syndrome |
| Pantothenate kinase associated neurodegeneration Chorea-acanthocytosis | |
| Wilson’s disease | |
| 6-pyruvolyltetrahydropterin synthase deficiency | |
| Anti-NMDA encephalitis | |
| Ataxia | Friedreich’s ataxia |
| Ataxia telangiectasia | |
| Cerebrotendinous xanthomatosis | |
| Niemann-Pick type-C | |
| Aceruloplasminemia | |
| PLA2G6 associated neurodegeneration | |
| Pantothenate kinase associated neurodegeneration | |
| Wilson’s disease | |
| Spinocerebellar ataxias | |
| Peripheral neuropathy | Spinocerebellar ataxias – SCA 2, 3 |
| Friedreich’s ataxia | |
| Niemann-Pick type-C | |
| Cerebrotendinous xanthomatosis | |
| GM2 gangliosidosis | |
| PLA2G6 associated neurodegeneration | |
| Mitochondrial membrane protein–associated neurodegeneration | |
| COASY protein–associated neurodegeneration | |
| Hypogonadism | Woodhouse Sakati syndrome |
| Ataxia telangiectasia | |
| Hepatic involvement | Wilson’s disease |
| Aceruloplasminemia | |
| Ataxia telangiectasia | |
| Niemann-Pick type-C | |
| Gaucher disease | |
| GM1 gangliosidosis | |
| McLeod syndrome | |
| Acquired hepatocerebral degeneration | |
| Coeliac disease | |
| Renal dysfunction | Leigh syndrome |
| Methylmalonic aciduria | |
| Lesch Nyhan syndrome | |
| Wilson’s disease | |
| Glutaric aciduria type 1 | |
| Systemic lupus erythematosus | |
| Brain iron accumulation on MRI | Pantothenate kinase associated neurodegeneration |
| PLA2G6 associated neurodegeneration | |
| Aceruloplasminemia | |
| Neuroferritinopathy | |
| Woodhouse Sakati syndrome | |
| COASY protein–associated neurodegeneration | |
| GM1 gangliosidosis | |
| T2 hyperintensities in Globus pallidus on MRI | Wilson’s disease |
| Methylmalonic aciduria | |
| Leigh syndrome | |
| Extrapontine myelinolysis | |
| Japanese encephalitis | |
| Kernicterus | |
| Behcet syndrome | |
| Acquired hepatocerebral degeneration | |
| Carbon monoxide poisoning |
PATHOGENESIS
Physiological studies of the somatotopic organization of the basal ganglia suggest that the lateral portion of the substantia nigra and the caudo-ventral portion of putamen and pallidum are primarily concerned with orolingual and head movement, and that the basal ganglia in one cerebral hemisphere play a role in bilateral orofacial-lingual motor control.[96] Curra et al.,[97] using Transcranial Magnetic Stimulation (TMS) based studies, found that the cortical silent period from perioral muscles in patients with OMD is significantly shortened, compared to healthy volunteers. This indicates that reduced excitability of cortical inhibitory interneurons or reduced facilitation of inhibitory interneurons from subcortical or other cortical structures plays a role in the pathogenesis.
TREATMENT
OMD can significantly affect communication and swallowing function and it is important to address the social, emotional and nutritional impact of the disorder. A multidisciplinary approach combining medical treatment with speech therapy and nutrition management is important in addressing the needs of patients. Proper dental and oral evaluation is needed to assess orofacial and oropharyngeal function.[98] Triggers (especially relevant to sensory tricks) and the subtype of OMD should be carefully identified.
Sensory tricks (geste antagoniste) do not seem to provide adequate long-term relief and mostly requires actions that interfere with normal functional activities. Sensory tricks like pressing the teeth or lips with the fingers, placing objects in the mouth, singing, or humming may be helpful in few patients. Oral appliances have also shown to be useful,[99] especially when they mimic the patient's sensory tricks. Sensory tricks may work better for jaw-opening dystonia rather than jaw-closing dystonia.[100]
Pharmacological treatment of OMD is mostly based on empirical experience rather than supported by rational scientific evidence.[101] Oral medications are seldom beneficial in improving dystonic symptoms. The oral medications which can be tried include anticholinergic drugs, baclofen, dopaminergic drugs, and benzodiazepines. Tetrabenazine is reported to be useful in 26–60% of OMD patients but is associated with side effects like parkinsonism, depression and suicidal ideation.[102]
Chemodenervation with botulinum toxin (BTX) is considered by most to be the first line of treatment. However, there are no supporting high-level clinical trials, and the evidence is mainly based on small series of cases. Abobotulinumtoxin A and onabotulinumtoxin A have level C evidence according to the American Academy of Neurology Classification for the Quality of Evidence; for incobotulinumtoxin A and rimabotulinumtoxin B, it is level U (inadequate data/still unproven).[103] Empirical experience over past 20 years has shown BTX to be an effective and safe approach in the treatment of OMD.[104] Jaw closure dystonia tends to respond better to BTX than jaw-opening or mixed dystonia.[2] BTX has been found to be equally effective in tardive as well as idiopathic OMD.
For OMD refractory to medical management, Deep brain stimulation targeting the globus pallidus internus has been shown to be effective in case series, but the evidence is still preliminary.[105,106]
CONCLUSIONS
Oromandibular dystonia is a rather common movement disorder and causes significant interference with functioning because of its impact on speech and swallowing functions. Genetic and presumed genetic (idiopathic), and tardive etiologies account for the majority of isolated OMD in adulthood. In an isolated generalized dystonia or a combined dystonia syndrome, presence of prominent oro-mandibular involvement often helps to narrow down the list of differentials. Management of OMD may need a multidisciplinary approach. BTX provides relief in the majority of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Termsarasab P, Tanenbaum DR, Frucht SJ. The phenomenology and natural history of idiopathic lower cranial dystonia. J Clin Mov Disord. 2014;1:3. doi: 10.1186/2054-7072-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan EK, Jankovic J. Botulinum toxin A in patients with oromandibular dystonia: Long-term follow-up. Neurology. 1999;53:2102–7. doi: 10.1212/wnl.53.9.2102. [DOI] [PubMed] [Google Scholar]
- 3.Pandey S, Sharma S. Meige's syndrome: History, epidemiology, clinical features, pathogenesis and treatment. J Neurol Sci. 2017;372:162–70. doi: 10.1016/j.jns.2016.11.053. [DOI] [PubMed] [Google Scholar]
- 4.Nutt JG, Muenter MD, Aronson A, Kurland LT, Melton LJ., 3rd Epidemiology of focal and generalized dystonia in Rochester, Minnesota. Mov Disord. 1988;3:188–94. doi: 10.1002/mds.870030302. [DOI] [PubMed] [Google Scholar]
- 5.Slaim L, Cohen M, Klap P, Vidailhet M, Perrin A, Brasnu D, et al. Oromandibular dystonia: Demographics and clinical data from 240 patients. J Mov Disord. 2018;11:78–81. doi: 10.14802/jmd.17065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sex-related influences on the frequency and age of onset of primary dystonia, Epidemiologic Study of Dystonia in Europe (ESDE) Collaborative Group. Neurology. 1999;53:1871–3. doi: 10.1212/wnl.53.8.1871. [DOI] [PubMed] [Google Scholar]
- 7.Tolosa E, Marti MJ. Blepharospasm-oromandibular dystonia syndrome (Meige's syndrome): Clinical aspects. Adv Neurol. 1988;49:73–84. [PubMed] [Google Scholar]
- 8.Tan EK, Jankovic J. Tardive and idiopathic oromandibular dystonia: A clinical comparison. J Neurol Neurosurg Psychiatry. 2000;68:186–90. doi: 10.1136/jnnp.68.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Esper CD, Freeman A, Factor SA. Lingual protrusion dystonia: Frequency, etiology and botulinum toxin therapy. Parkinsonism Relat Disord. 2010;16:438–41. doi: 10.1016/j.parkreldis.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 10.Albanese A, Bhatia K, Bressman SB, Delong MR, Fahn S, Fung VS, et al. Phenomenology and classification of dystonia: A consensus update. Mov Disord. 2013;28:863–73. doi: 10.1002/mds.25475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donaldson I, Marsden CD, Schneider SA, Bhatia KP. Oxford University Press; 2012. Marsden's Book of Movement Disorders. Idiopathic (primary) cranial dystonias. [Google Scholar]
- 12.Gonzalez-Alegre P, Schneider RL, Hoffman H. Clinical, etiological, and therapeutic features of jaw-opening and jaw-closing oromandibular dystonias: A decade of experience at a single treatment center. Tremor Other Hyperkinet Mov (N Y) 2014;4:231. doi: 10.7916/D8TH8JSM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clark GT, Ram S. Orofacial movement disorders. Oral Maxillofac Surg Clin North Am. 2016;28:397–407. doi: 10.1016/j.coms.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Skármeta NP, Espinoza-Mellado P, Chana P. Orofacial dystonia and other oromandibular movement disorders. In: Rizk TMG, editor. Dystonia. Rijeka: IntechOpen; 2018. [Google Scholar]
- 15.Frucht SJ, Fahn S, Greene PE, O'Brien C, Gelb M, Truong DD, et al. The natural history of embouchure dystonia. Mov Disord. 2001;16:899–906. doi: 10.1002/mds.1167. [DOI] [PubMed] [Google Scholar]
- 16.Yaltho TC, Jankovic J. The many faces of hemifacial spasm: Differential diagnosis of unilateral facial spasms. Mov Disord. 2011;26:1582–92. doi: 10.1002/mds.23692. [DOI] [PubMed] [Google Scholar]
- 17.Thompson PD, Obeso JA, Delgado G, Gallego J, Marsden CD. Focal dystonia of the jaw and the differential diagnosis of unilateral jaw and masticatory spasm. J Neurol Neurosurg Psychiatry. 1986;49:651–6. doi: 10.1136/jnnp.49.6.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uvais NA, Sreeraj VS, Sathish Kumar SV. Sertraline induced mandibular dystonia and bruxism. J Family Med Prim Care. 2016;5:882–4. doi: 10.4103/2249-4863.201168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mondet L, Radoube F, Gras V, Masmoudi K. Cefixime-induced oromandibular dystonia in an adult: A case report. Curr Drug Saf. 2017 doi: 10.2174/1574886312666170310095320. doi: 10.2174/1574886312666170310095320. [DOI] [PubMed] [Google Scholar]
- 20.Lizarraga KJ, Lopez MR, Singer C. Reversible craniocervical dystonia associated with levofloxacin. J Clin Mov Disord. 2015;2:10. doi: 10.1186/s40734-015-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Esen I, Demirpence S, Yis U, Kurul S. Cetirizine-induced dystonic reaction in a 6-year-old boy. Pediatr Emerg Care. 2008;24:627–8. doi: 10.1097/PEC.0b013e3181850c35. [DOI] [PubMed] [Google Scholar]
- 22.De Riu G, Sanna MP, De Riu PL. An elderly female patient with tardive oromandibular dystonia after prolonged use of the histamine analog betahistine. J Clin Neurosci. 2010;17:1330–1. doi: 10.1016/j.jocn.2010.01.034. [DOI] [PubMed] [Google Scholar]
- 23.Zhang R, Lai J, Huang J. Acute onset of orofacial dystonia from promethazine treatment: A case report. Medicine (Baltimore) 2019;98:e17675. doi: 10.1097/MD.0000000000017675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kimber TE, Thompson PD. Segmental dystonia in the context of dextromethorphan abuse: A new cause of delayed onset drug-induced dystonia? Mov Disord Clin Pract. 2015;2:299–300. doi: 10.1002/mdc3.12148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jitprapaikulsan J, Srivanitchapoom P. Acute dystonic reaction following general anesthetic agent use. Tremor Other Hyperkinet Mov (N Y) 2017;7:514. doi: 10.7916/D8862V0P. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cengiz A, Aybay MN, Sarici SF, Oner V, Arslan FZ, Cengiz A. Capecitabine-related neurotoxicity presenting as oromandibular dystonia. J Oncol Pract. 2018;14:202–4. doi: 10.1200/JOP.2017.021543. [DOI] [PubMed] [Google Scholar]
- 27.Uzun ME, Korkmaz MF, Ekici A, Kaymaz N. Methylphenidate induced acute dystonic reaction. Indian J Pediatr. 2018;85:577. doi: 10.1007/s12098-018-2711-3. [DOI] [PubMed] [Google Scholar]
- 28.Das S, van Landeghem FKH. Clinicopathological spectrum of bilirubin encephalopathy/kernicterus. Diagnostics (Basel) 2019;9:24. doi: 10.3390/diagnostics9010024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seiser A, Schwarz S, Aichinger-Steiner MM, Funk G, Schnider P, Brainin M. Parkinsonism and dystonia in central pontine and extrapontine myelinolysis. J Neurol Neurosurg Psychiatry. 1998;65:119–21. doi: 10.1136/jnnp.65.1.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang HC, Cheng SJ. The syndrome of acute bilateral basal ganglia lesions in diabetic uremic patients. J Neurol. 2003;250:948–55. doi: 10.1007/s00415-003-1122-0. [DOI] [PubMed] [Google Scholar]
- 31.Ferrara J, Jankovic J. Acquired hepatocerebral degeneration. J Neurol. 2009;256:320–32. doi: 10.1007/s00415-009-0144-7. [DOI] [PubMed] [Google Scholar]
- 32.Hannawi Y, Abers MS, Geocadin RG, Mirski MA. Abnormal movements in critical care patients with brain injury: A diagnostic approach. Crit Care. 2016;20:60. doi: 10.1186/s13054-016-1236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Revilla FJ, Racette BA, Perlmutter JS. Chorea and jaw-opening dystonia as a manifestation of NeuroBehcet's syndrome. Mov Disord. 2000;15:741–4. doi: 10.1002/1531-8257(200007)15:4<741::aid-mds1025>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 34.Pittock SJ, Parisi JE, McKeon A, Roemer SF, Lucchinetti CF, Tan KM, et al. Paraneoplastic jaw dystonia and laryngospasm with antineuronal nuclear autoantibody type 2 (anti-Ri) Arch Neurol. 2010;67:1109–15. doi: 10.1001/archneurol.2010.209. [DOI] [PubMed] [Google Scholar]
- 35.Ashalatha R, Kishore A, Sarada C, Nair MD. Satoyoshi syndrome. Neurol India. 2004;52:94–5. [PubMed] [Google Scholar]
- 36.Wicki J, Germanier Y, Sztajzel R, Burkhard PR. Brueghel syndrome as a new manifestation of HIV encephalopathy. Eur Neurol. 2008;60:107–8. doi: 10.1159/000138963. [DOI] [PubMed] [Google Scholar]
- 37.Alarcon F, Duenas G, Cevallos N, Lees AJ. Movement disorders in 30 patients with tuberculous meningitis. Mov Disord. 2000;15:561–9. doi: 10.1002/1531-8257(200005)15:3<561::AID-MDS1021>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 38.Singer C, Lang AE, Suchowersky O. Adult-onset subacute sclerosing panencephalitis: Case reports and review of the literature. Mov Disord. 1997;12:342–53. doi: 10.1002/mds.870120313. [DOI] [PubMed] [Google Scholar]
- 39.Brandel JP, Vidailhet M, Noseda G, Harpey JP, Agid Y. Mycoplasma pneumoniae postinfectious encephalomyelitis with bilateral striatal necrosis. Mov Disord. 1996;11:333–6. doi: 10.1002/mds.870110322. [DOI] [PubMed] [Google Scholar]
- 40.Gollomp SM, Fahn S. Transient dystonia as a complication of varicella. J Neurol Neurosurg Psychiatry. 1987;50:1228–9. doi: 10.1136/jnnp.50.9.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kalita J, Misra UK, Pradhan PK. Oromandibular dystonia in encephalitis. J Neurol Sci. 2011;304:107–10. doi: 10.1016/j.jns.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 42.Kim HJ, Lee MC, Kim JS, Chung SJ, Kim HJ, Kwon M, et al. Lingual dystonia as a manifestation of thalamic infarction. Mov Disord. 2009;24:1703–4. doi: 10.1002/mds.22657. [DOI] [PubMed] [Google Scholar]
- 43.Salazar G, Español G, Fragoso M, Rey A, Escalante S, Zegarra J. Oromandibular dystonia secondary to radiotherapy. Peripheral injuries triggering thalamic disruption?: A case report. Basal Ganglia. 2011;1:235–6. [Google Scholar]
- 44.Jankovic J. Friedreich's ataxia presenting with childhood onset progressive dystonia and spasticity. In: Fernandez HH, Merello M, editors. Movement Disorders: Unforgettable Cases and Lessons from the Bedside. New York: Springer Publishing Company; 2012. pp. 191–3. [Google Scholar]
- 45.Tan AH, Mah JSY, Thong MK, Lim S-Y. Methylmalonic aciduria: A treatable disorder of which adult neurologists need to be aware. Mov Disord Clin Pract. 2016;3:104–5. doi: 10.1002/mdc3.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ng J, Zhen J, Meyer E, Erreger K, Li Y, Kakar N, et al. Dopamine transporter deficiency syndrome: Phenotypic spectrum from infancy to adulthood. Brain. 2014;137:1107–19. doi: 10.1093/brain/awu022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yapici Z, Tuschl K, Eraksoy M. Hypermanganesemia with dystonia 1: A novel mutation and response to iron supplementation. Mov Disord Clin Pract. 2020;7:94–6. doi: 10.1002/mdc3.12861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gantenbein AR, Damon-Perriere N, Bohlender JE, Chauveau M, Latxague C, Miranda M, et al. Feeding dystonia in McLeod syndrome. Mov Disord. 2011;26:2123–6. doi: 10.1002/mds.23843. [DOI] [PubMed] [Google Scholar]
- 49.Kojovic M, Pareés I, Lampreia T, Pienczk-Reclawowicz K, Xiromerisiou G, Rubio-Agusti I, et al. The syndrome of deafness-dystonia: Clinical and genetic heterogeneity. Mov Disord. 2013;28:795–803. doi: 10.1002/mds.25394. [DOI] [PubMed] [Google Scholar]
- 50.Schneider SA, Bhatia KP. Secondary dystonia-clinical clues and syndromic associations. J Mov Disord. 2009;2:58–63. doi: 10.14802/jmd.09016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blanchet PJ, Popovici R, Guitard F, Rompre PH, Lamarche C, Lavigne GJ. Pain and denture condition in edentulous orodyskinesia: Comparisons with tardive dyskinesia and control subjects. Mov Disord. 2008;23:1837–42. doi: 10.1002/mds.22102. [DOI] [PubMed] [Google Scholar]
- 52.Berman BD, Groth CL, Sillau SH, Pirio Richardson S, Norris SA, Junker J, et al. Risk of spread in adult-onset isolated focal dystonia: A prospective international cohort study. J Neurol Neurosurg Psychiatry. 2020;91:314–20. doi: 10.1136/jnnp-2019-321794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Silverdale MA, Schneider SA, Bhatia KP, Lang AE. The spectrum of orolingual tremor--a proposed classification system. Mov Disord. 2008;23:159–67. doi: 10.1002/mds.21776. [DOI] [PubMed] [Google Scholar]
- 54.Martino D, Liuzzi D, Macerollo A, Aniello MS, Livrea P, Defazio G. The phenomenology of the geste antagoniste in primary blepharospasm and cervical dystonia. Mov Disord. 2010;25:407–12. doi: 10.1002/mds.23011. [DOI] [PubMed] [Google Scholar]
- 55.Molho ES, Feustel PJ, Factor SA. Clinical comparison of tardive and idiopathic cervical dystonia. Mov Disord. 1998;13:486–9. doi: 10.1002/mds.870130319. [DOI] [PubMed] [Google Scholar]
- 56.Petrovic IN, Kresojevic N, Ganos C, Svetel M, Dragasevic N, Bhatia KP, et al. Characteristic “Forcible” geste antagoniste in oromandibular dystonia resulting from pantothenate kinase-associated neurodegeneration. Mov Disord Clin Pract. 2014;1:112–4. doi: 10.1002/mdc3.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sankhla C, Lai EC, Jankovic J. Peripherally induced oromandibular dystonia. J Neurol Neurosurg Psychiatry. 1998;65:722–8. doi: 10.1136/jnnp.65.5.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Frucht SJ. Embouchure dystonia--Portrait of a task-specific cranial dystonia. Mov Disord. 2009;24:1752–62. doi: 10.1002/mds.22550. [DOI] [PubMed] [Google Scholar]
- 59.Sharma C, Kumawat BL, Garg A, Kumar Rana K. Chewing-induced facial dystonia: A rare presentation of task-specific dystonia. BMJ Case Rep 2017. 2017 doi: 10.1136/bcr-2016-218956. doi: 10.1136/bcr-2016-218956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Scolding NJ, Smith SM, Sturman S, Brookes GB, Lees AJ. Auctioneer's jaw: A case of occupational oromandibular hemidystonia. Mov Disord. 1995;10:508–9. doi: 10.1002/mds.870100418. [DOI] [PubMed] [Google Scholar]
- 61.Ilic TV, Pötter M, Holler I, Deuschl G, Volkmann J. Praying-induced oromandibular dystonia. Mov Disord. 2005;20:385–6. doi: 10.1002/mds.20353. [DOI] [PubMed] [Google Scholar]
- 62.Dietrichs E, Heier MS, Nakstad PH. Jaw-opening dystonia presumably caused by a pontine lesion. Mov Disord. 2000;15:1026–8. doi: 10.1002/1531-8257(200009)15:5<1026::aid-mds1046>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 63.Dalmau J, Graus F, Villarejo A, Posner JB, Blumenthal D, Thiessen B, et al. Clinical analysis of anti-Ma2-associated encephalitis. Brain. 2004;127:1831–44. doi: 10.1093/brain/awh203. [DOI] [PubMed] [Google Scholar]
- 64.Honorat JA, Komorowski L, Josephs KA, Fechner K, St Louis EK, Hinson SR, et al. IgLON5 antibody: Neurological accompaniments and outcomes in 20 patients. Neurol Neuroimmunol Neuroinflamm. 2017;4:e385. doi: 10.1212/NXI.0000000000000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tarabzouni S, AlKhairallah T. Isolated neurological manifestation in silent celiac disease. J Mov Disord. 2017;10:105–7. doi: 10.14802/jmd.16063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Papageorgiou SG, Kontaxis T, Bonakis A, Kalfakis N. Orofacial dystonia related to Sjogren's syndrome. Clin Rheumatol. 2007;26:1779–81. doi: 10.1007/s10067-006-0519-4. [DOI] [PubMed] [Google Scholar]
- 67.Wu K, Christodoulou L, Siddiqui A, D'Cruz D, Andrews T. Bilateral reversible basal ganglia changes associated with dystonia and hemifacial spasms in central nervous system lupus. Quant Imaging Med Surg. 2015;5:928–9. doi: 10.3978/j.issn.2223-4292.2015.03.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Raoofi S, Khorshidi H, Najafi M. Etiology, diagnosis and management of oromandibular dystonia: An update for stomatologists. J Dent (Shiraz) 2017;18:73–81. [PMC free article] [PubMed] [Google Scholar]
- 69.Schrag A, Bhatia KP, Quinn NP, Marsden CD. Atypical and typical cranial dystonia following dental procedures. Mov Disord. 1999;14:492–6. doi: 10.1002/1531-8257(199905)14:3<492::aid-mds1018>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 70.Jinnah HA, Ceballos-Picot I, Torres RJ, Visser JE, Schretlen DJ, Verdu A, et al. Attenuated variants of Lesch-Nyhan disease. Brain. 2010;133:671–89. doi: 10.1093/brain/awq013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brugger F, Kagi G, Pandolfo M, Mencacci NE, Batla A, Wiethoff S, et al. Neurodegeneration with brain iron accumulation (NBIA) syndromes presenting with late-onset craniocervical dystonia: An illustrative case series. Mov Disord Clin Pract. 2017;4:254–7. doi: 10.1002/mdc3.12393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hirayama M, Kitagawa Y, Yamamoto S, Tokuda A, Mutoh T, Hamano T, et al. GM1 gangliosidosis type 3 with severe jaw-closing impairment. J Neurol Sci. 1997;152:99–101. doi: 10.1016/s0022-510x(97)00139-1. [DOI] [PubMed] [Google Scholar]
- 73.Roze E, Paschke E, Lopez N, Eck T, Yoshida K, Maurel-Ollivier A, et al. Dystonia and parkinsonism in GM1 type 3 gangliosidosis. Mov Disord. 2005;20:1366–9. doi: 10.1002/mds.20593. [DOI] [PubMed] [Google Scholar]
- 74.Muthane U, Chickabasaviah Y, Kaneski C, Shankar SK, Narayanappa G, Christopher R, et al. Clinical features of adult GM1 gangliosidosis: Report of three Indian patients and review of 40 cases. Mov Disord. 2004;19:1334–41. doi: 10.1002/mds.20193. [DOI] [PubMed] [Google Scholar]
- 75.Koens LH, Kuiper A, Coenen MA, Elting JWJ, de Vries JJ, Engelen M, et al. Ataxia, dystonia and myoclonus in adult patients with Niemann-Pick type C. Orphanet J Rare Dis. 2016;11:121. doi: 10.1186/s13023-016-0502-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nardocci N, Bertagnolio B, Rumi V, Angelini L. Progressive dystonia symptomatic of juvenile GM2 gangliosidosis. Mov Disord. 1992;7:64–7. doi: 10.1002/mds.870070113. [DOI] [PubMed] [Google Scholar]
- 77.Alcalay R, Wu S, Patel S, Frucht S. Oromandibular dystonia as a complication of cerebrotendinous xanthomatosis. Mov Disord. 2009;24:1397–9. doi: 10.1002/mds.22585. [DOI] [PubMed] [Google Scholar]
- 78.Grim KK, Phillips GD, Renner DR. Dysarthria and stutter as presenting symptoms of late-onset tay-sachs disease in three siblings. Mov Disord Clin Pract. 2015;2:289–90. doi: 10.1002/mdc3.12194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carrillo F, Schneider SA, Taylor AM, Srinivasan V, Kapoor R, Bhatia KP. Prominent oromandibular dystonia and pharyngeal telangiectasia in atypical ataxia telangiectasia. Cerebellum. 2009;8:22–7. doi: 10.1007/s12311-008-0055-7. [DOI] [PubMed] [Google Scholar]
- 80.Vidailhet M, Anheim M, Hubsch C. Dysarthria, dystonia, and cerebellar ataxia: The tale of four sisters. In: Fernandez HH, Merello M, editors. Movement Disorders: Unforgettable Cases and Lessons from the Bedside. New York: Springer Publishing Company; 2012. pp. 194–5. [Google Scholar]
- 81.Trender-Gerhard I, Sweeney MG, Schwingenschuh P, Mir P, Edwards MJ, Gerhard A, et al. Autosomal-dominant GTPCH1-deficient DRD: Clinical characteristics and long-term outcome of 34 patients. J Neurol Neurosurg Psychiatry. 2009;80:839–45. doi: 10.1136/jnnp.2008.155861. [DOI] [PubMed] [Google Scholar]
- 82.Steinberger D, Topka H, Fischer D, Muller U. GCH1 mutation in a patient with adult-onset oromandibular dystonia. Neurology. 1999;52:877–9. doi: 10.1212/wnl.52.4.877. [DOI] [PubMed] [Google Scholar]
- 83.Wijemanne S, Jankovic J. Dopa-responsive dystonia--clinical and genetic heterogeneity. Nat Rev Neurol. 2015;11:414–24. doi: 10.1038/nrneurol.2015.86. [DOI] [PubMed] [Google Scholar]
- 84.Kurian MA, Li Y, Zhen J, Meyer E, Hai N, Christen HJ, et al. Clinical and molecular characterisation of hereditary dopamine transporter deficiency syndrome: An observational cohort and experimental study. Lancet Neurol. 2011;10:54–62. doi: 10.1016/S1474-4422(10)70269-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wu YR, Lee-Chen GJ, Lang AE, Chen CM, Lin HY, Chen ST. Dystonia as a presenting sign of spinocerebellar ataxia type 1. Mov Disord. 2004;19:586–7. doi: 10.1002/mds.10708. [DOI] [PubMed] [Google Scholar]
- 86.Antenora A, Peluso S, Sacca F, De Michele G, Filla A. Jaw-opening oromandibular dystonia associated with spinocerebellar ataxia type 2. Mov Disord Clin Pract. 2014;1:121–2. doi: 10.1002/mdc3.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Catai LMP, Camargo CHF, Moro A, Ribas G, Raskin S, Teive HAG. Dystonia in patients with spinocerebellar ataxia 3-Machado-Joseph disease: An underestimated diagnosis. Open Neurol J? 2018;12:41–9. doi: 10.2174/1874205X01812010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ushe M, Perlmutter JS. Oromandibular and lingual dystonia associated with spinocerebellar ataxia type 8. Mov Disord. 2012;27:1741–2. doi: 10.1002/mds.25295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ganos C, Saifee TA, Kassavetis P, Erro R, Batla A, Cordivari C, et al. Dystonic tremor and spasmodic dysphonia in spinocerebellar ataxia type 12. Mov Disord Clin Pract. 2014;1:79–81. doi: 10.1002/mdc3.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Miyashiro A, Sugihara K, Kawarai T, Miyamoto R, Izumi Y, Morino H, et al. Oromandibular dystonia associated with SCA36. Mov Disord. 2013;28:558–9. doi: 10.1002/mds.25304. [DOI] [PubMed] [Google Scholar]
- 91.Avan Gaalen J, Giunti P, van de Warrenburg BP. Movement disorders in spinocerebellar ataxias. Mov Disord. 2011;26:792–800. doi: 10.1002/mds.23584. [DOI] [PubMed] [Google Scholar]
- 92.Martikainen MH, Ng YS, Gorman GS, Alston CL, Blakely EL, Schaefer AM, et al. Clinical, genetic, and radiological features of extrapyramidal movement disorders in mitochondrial disease. JAMA Neurol. 2016;73:668–74. doi: 10.1001/jamaneurol.2016.0355. [DOI] [PubMed] [Google Scholar]
- 93.Fasano A, Valadas A, Bhatia KP, Prashanth LK, Lang AE, Munhoz RP, et al. Psychogenic facial movement disorders: Clinical features and associated conditions. Mov Disord. 2012;27:1544–51. doi: 10.1002/mds.25190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fasano A, Tinazzi M. Functional facial and tongue movement disorders. Handb Clin Neurol. 2016;139:353–65. doi: 10.1016/B978-0-12-801772-2.00031-X. [DOI] [PubMed] [Google Scholar]
- 95.Fischer JF, Mainka T, Worbe Y, Pringsheim T, Bhatia K, Ganos C. Self-injurious behaviour in movement disorders: Systematic review. J Neurol Neurosurg Psychiatry. 2020;91:712–9. doi: 10.1136/jnnp-2019-322569. [DOI] [PubMed] [Google Scholar]
- 96.Jankovic J. Cranial-cervical dyskinesias: An overview. Adv Neurol. 1988;49:1–13. [PubMed] [Google Scholar]
- 97.Curra A, Romaniello A, Berardelli A, Cruccu G, Manfredi M. Shortened cortical silent period in facial muscles of patients with cranial dystonia. Neurology. 2000;54:130–5. doi: 10.1212/wnl.54.1.130. [DOI] [PubMed] [Google Scholar]
- 98.Karp BI, Alter K. Botulinum toxin treatment of blepharospasm, orofacial/oromandibular dystonia, and hemifacial spasm. Semin Neurol. 2016;36:84–91. doi: 10.1055/s-0036-1571952. [DOI] [PubMed] [Google Scholar]
- 99.Lo SE, Gelb M, Frucht SJ. Geste antagonistes in idiopathic lower cranial dystonia. Mov Disord. 2007;22:1012–7. doi: 10.1002/mds.21149. [DOI] [PubMed] [Google Scholar]
- 100.Singer C, Papapetropoulos S. A comparison of jaw-closing and jaw-opening idiopathic oromandibular dystonia. Parkinsonism Relat Disord. 2006;12:115–8. doi: 10.1016/j.parkreldis.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 101.Jankovic J. Medical treatment of dystonia. Mov Disord. 2013;28:1001–12. doi: 10.1002/mds.25552. [DOI] [PubMed] [Google Scholar]
- 102.Jankovic J, Beach J. Long-term effects of tetrabenazine in hyperkinetic movement disorders. Neurology. 1997;48:358–62. doi: 10.1212/wnl.48.2.358. [DOI] [PubMed] [Google Scholar]
- 103.Simpson DM, Hallett M, Ashman EJ, Comella CL, Green MW, Gronseth GS, et al. Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2016;86:1818–26. doi: 10.1212/WNL.0000000000002560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ramirez-Castaneda J, Jankovic J. Long-term efficacy, safety, and side effect profile of botulinum toxin in dystonia: A 20-year follow-up. Toxicon. 2014;90:344–8. doi: 10.1016/j.toxicon.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 105.Sako W, Morigaki R, Mizobuchi Y, Tsuzuki T, Ima H, Ushio Y, et al. Bilateral pallidal deep brain stimulation in primary Meige syndrome. Parkinsonism Relat Disord. 2011;17:123–5. doi: 10.1016/j.parkreldis.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 106.Inoue N, Nagahiro S, Kaji R, Goto S. Long-term suppression of Meige syndrome after pallidal stimulation: A 10-year follow-up study. Mov Disord. 2010;25:1756–8. doi: 10.1002/mds.23166. [DOI] [PubMed] [Google Scholar]