Abstract
Psoriasis is one of the most widespread chronic inflammatory skin diseases, affecting about 2%–3% of the worldwide adult population. The pathogenesis of this disease is quite complex, but an interaction between genetic and environmental factors has been recognized with an essential modulation of inflammatory and immune responses in affected patients. Psoriatic plaques generally represent the clinical psoriatic feature resulting from an abnormal proliferation and differentiation of keratinocytes, which cause dermal hyperplasia, skin infiltration of immune cells, and increased capillarity. Some scientific pieces of evidence have reported that psychological stress may play a key role in psoriasis, and the disease itself may cause stress conditions in patients, thus reproducing a vicious cycle. The present review aims at examining immune cell involvement in psoriasis and the relationship of depression and stress in its pathogenesis and development. In addition, this review contains a focus on the possible use of natural products, thus pointing out their mechanism of action in order to counteract clinical and psychological symptoms.
Keywords: psoriasis, immune system, immune cells, depression, stress, natural products
1. Introduction
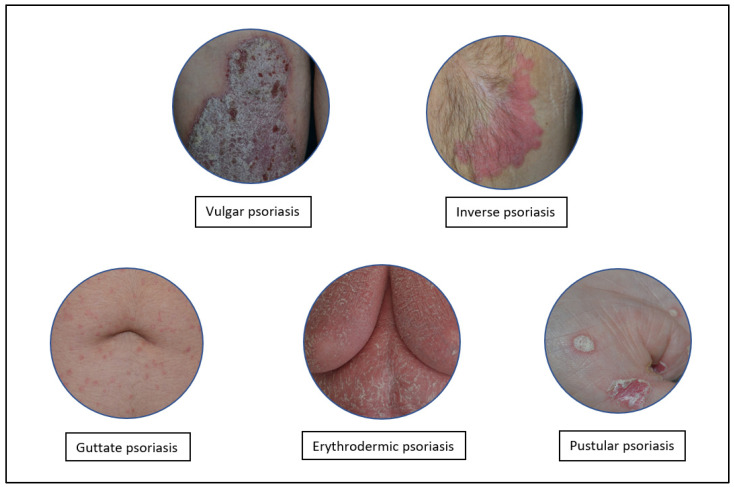
Psoriasis is one of the most common chronic inflammatory skin diseases that affects about ~2%–3% of the worldwide adult population [1,2]. Psoriasis affects both males and females, without prevalence of gender [3], and its clinical lesions start to appear between 20 and 30 years of age, although children and adolescents may also be affected [4]. This pathology can be classified into several forms: Psoriasis vulgaris, P. guttata, P. pustolosa, P. erythrodermica, and P. inversa [5] (Figure 1).
Figure 1.
Different types of psoriasis.
The pathogenesis of the disease is quite complex, but an interaction between genetic and environmental factors has been recognized [6,7,8]. Psoriasis is characterized by skin lesions that appear as erythematous and reddened plaques with silvery lamelliform scales, sometimes painful and itchy [9], especially in the elbows, knees, and scalp [10]. These plaques are often the result of an abnormal proliferation and differentiation of keratinocytes, thus resulting in dermal hyperplasia [11], immune cell infiltration, and increased capillarity [12]. Because of the significant role of immune cells in the pathogenesis of psoriasis, this disease is also classified as an autoimmune disease. In fact, different studies have already shown that the activation of T helper (Th)1 lymphocytes leads to an increase in interferon (IFN)-γ and tumor necrosis factor (TNF)-α levels [13]. CD4+ T cells also produce interleukin (IL)-17, which is responsible for the abnormal cell proliferation and stimulation of keratinocytes, thus leading to cytokine release [14,15]. In this context, the IL-23/IL-17 axis would play a crucial role in psoriatic lesion formation [16,17]. These cytokines, with particular reference to IL-17, are also produced by other immune cells, such as γδ T cells, natural killer (NK) cells, NKT cells, and innate lymphoid cells (ILCs) [18], which are involved in the pathogenesis of psoriasis [19]. Psoriasis also affects the psychological plane, reducing the quality of life of patients [20,21]: the appearance of skin lesions can cause discomfort in patients and may increase layoff and unemployment rates and depressive states up to suicide rates [22,23]. Not only the affected patients are stressed out, but also stressful conditions may represent contributing causes of psoriasis [24]. In fact, stress can activate an inadequate response of the hypothalamic–pituitary–adrenal (HPA) axis, thus stimulating corticotropin-releasing hormone (CRH) and vasopressin release in the hypothalamus with the consequent adrenocorticotropic hormone (ACTH) increase [25]. ACTH regulates glucocorticoid secretion [25], but psoriatic patients are extremely reactive to stress and show reduced cortisol levels, resulting in immune system hyperactivity and increased inflammation [25,26,27]. As of today, the therapeutic approaches used for the treatment of psoriasis mainly act by reducing its severity or even suppressing symptoms, but no therapy is currently 100% effective. The most used treatments are monoclonal antibodies against TNF-α, IL-17, and IL-23 and topical cortisone-based ointments that contribute to the disappearance of plaques [28,29]. However, as mentioned, these approaches are not definitively curative and are long-term therapies, thus causing a weakening of the immune system [30]. For this reason, a growing interest is aimed at alternative treatments based on natural product use, such as some nutraceuticals and polyphenols whose mechanism of action is mainly antioxidant and that are recognized to be safe [31,32,33,34,35,36].
In this review, immune cell involvement in psoriasis pathogenesis and the psychological consequences of psoriatic patients are reported. In addition, an overview of some natural products that might be used to manage this complex disease is designed.
2. Cell Types Involved in the Pathogenesis of Psoriasis
2.1. Keratinocytes
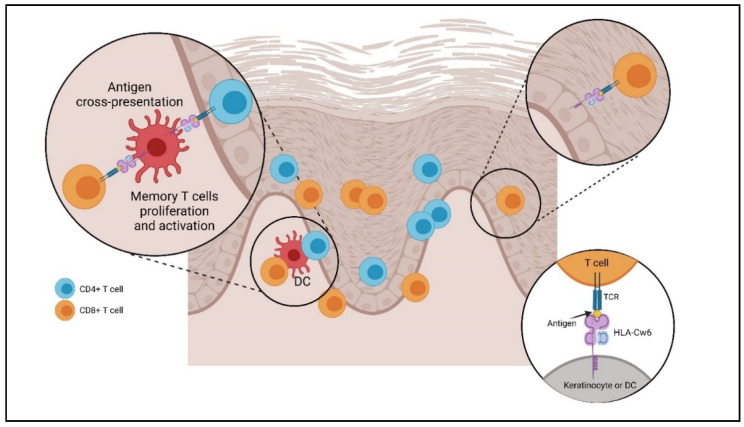
Keratinocytes are the most distributed cells in the skin characterized by a turnover that occurs in about 50 days under physiological conditions and in 5 days only during psoriasis, demonstrating an increased cell turnover and in particular of keratinocytes [37,38,39]. These cells play a key role in maintaining the inflammatory balance [40]: any mechanism that can alter this balance can lead to the development and evolution of chronic skin diseases, including psoriasis [41]. Activated keratinocytes may contribute to the release of chemokines, which are able to attract different defense cells to the site of phlogosis [42]. In particular, keratinocytes regulate the expression of the antimicrobial peptide cathelicidin LL-37 [43] and produce chemokine ligand (CXCL)8, also known as keratinocyte-derived chemokine 8 (KC8), which is responsible for neutrophil infiltration [44]; CXCL10; and chemokine receptor (CXCR) 3, which activate monocytes and Th1 cells [45]. Furthermore, chemokine ligand (CCL) 20 and IL-18 are implicated in the enrolment of Langerhans cells (LCs), dendritic cells (DCs), and cutaneous lymphocyte-associated antigen (CLA) T cells [46,47]. In addition, keratinocytes play the role of antigen-presenting cells, expressing the human leucocyte antigen (HLA) or major histocompatibility complex (MHC) [48]. HLA-Cw6 is a valid candidate for functional involvement in psoriasis. HLA-Cw6 participates in the cross-presentation of the antigen on a DC surface, resulting in the activation of CD8+ antigen-specific T cells. Cross-priming depends on the help of CD4+ T cells in the presentation of intracellular antigens in the dermis (activation of resident memory T cells) and lymph nodes (activation of naive T cells). Activated CD8+ T cells can migrate into the epidermis by binding to HLA-Cw6 keratinocytes, triggering the release of cytokines, chemokines, and proinflammatory mediators. This process increases inflammation and induces the proliferation of keratinocytes. The cyclical mechanism triggered in this way causes the psoriatic injury (Figure 2) [49,50]. Among the receptors expressed by keratinocytes and immune cells, the most important group is represented by the Toll-like receptors (TLRs), a class of phylogenetically conserved proteins [51,52,53,54], both in physiological and pathological conditions [55]. A reduced and increased expression was found in keratinocytes obtained from psoriatic plaques of TLR-5 and TLR-1, respectively [56,57]. Furthermore, keratinocytes’ structural integrity is maintained by keratins (KRTs), which play an important role in the pathogenesis of psoriasis [58]. In stress conditions, keratinocytes release damage-associated molecular patterns (DAMPs), which activate different molecular pathways, including the mitogen-activated protein kinase pathway (MAPK) and the transcription factors nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB) and nuclear factor erythroid 2-related factor 2 (NRF-2), which in turn mediate KRT6, KRT16, and KRT17 transcription. A high proliferative stage under pathological conditions is indicated by the increased expression of KRT16/17–KRT6; in particular, KRT17 expression is negligible in normal epidermis but is overexpressed in hyperproliferative diseases, such as psoriasis. KRT17 activates cell proliferation through the mTOR–AKT signaling, an important intracellular pathway involved in the regulation of the cell cycle. KRT17 may also act as an autoantigen, thus activating DCs and triggering the cytokine cascade, which in turn acts on keratinocytes by activating extracellular signal-regulated kinases (ERK)1/2 and signal transducers and activators of transcription (STAT)1/3. This activation further increases keratin gene expression, creating a loop that contributes to psoriasis appearance [59]. All these reported pieces of evidence highlight the important role played by keratinocytes in the formation and development of this chronic inflammatory disease.
Figure 2.
Role of HLA-Cw6 in psoriasis pathogenesis. Created with BioRender.com (accessed on 18 February 2022).
2.2. Dendritic Cells
Different types of dendritic cells can be detected in the skin under both physiological and pathological conditions [60,61]. These cells can act as antigen-presenting cells (APCs), but also as an important source of chemical mediators of inflammation, such as TNF-α and IL-23 [62].
2.2.1. Plasmacytoid Dendritic Cells (pDCs)
Plasmacytoid dendritic cells (pDCs) are a cell population present in the blood and secondary lymphoid organs [63]. They are involved in the antiviral immune response and can secrete large amounts of IFN-α [64]. Once stimulated by the viral antigen, these cells can differentiate into DCs [65] or dendritic myeloid cells (mDCs), which can modulate the inflammatory response by Th1 lymphocytes [66]. pDCs may accumulate in peripheral tissues during noninfectious phlogosis states, such as psoriasis [67]. pDCs have also been found in inflamed tissues of psoriasis-like diseases, such as systemic lupus erythematosus [68] and rheumatoid arthritis [69]. The activation of pDCs occurs by TLR-7 and TLR-9 [70,71]. This activation would therefore represent the trigger point of the pathogenesis of psoriasis, leading to a mechanism that contributes to the appearance of the psoriatic phenotype. Several studies, including murine models, have shown that an increase in IFN-α produced by pDCs can be found in the skin damaged with psoriatic plaques [67,72]. In addition to viral antigens, their recruitment and activation can also be induced by keratinocyte-released chemokines, such as CXCR4, CXCR3, and CCR5 [73,74]. The monoclonal antibody antiblood DC antigen 2 (BDCA2) is able to inhibit the development of psoriatic lesions, blocking the activation of pDCs [72]. Further studies using imiquimod [75], a synthetic imidazoquinolinone recognized by TLR-7 [76], have demonstrated the induction and activation of pDCs with IFN-α release [77].
2.2.2. Myeloid Dendritic Cells (mDCs)
Myeloid dendritic cells (mDCs) are highly represented in psoriatic skin lesions [62] and may be recognized as CD11c + CD1c (phenotypically immature cells) and CD11c + DC-LAMP + DEC-205/CD205 + BDCA-1+ (phenotypically mature cells). CD11c + CD1c cells are responsible for the production and release of TNF-α, IL-6, IL-20, IL-23, and IL-12 and produce inducible nitric oxide synthase (iNOS) [78]. Thus, these cells are particularly involved in the formation of psoriatic lesions [79,80,81,82], acting as mediators of inflammation and playing a key role in the pathogenesis of this chronic disease [60]. Although these cells are capable of releasing a large number of chemical mediators of inflammation, they primarily secrete IL-23, which interacts with the IL-17-mediated immune response [80,82]. Several studies have also shown that the presence of mDCs in psoriatic skin is 30 times higher than in healthy skin [78]. The CD11 + Dc-LAMP + DEC-205/CD205 + BDCA-1+ mDCs may be considered APCs, and their number does not appear to increase in psoriasis-injured skin compared with that in healthy skin [81]. The mDCs can also be activated and recruited by keratinocytes releasing CCL20 and promoting a recall of the Th17 lymphocytes to the phlogosis site [12,83]. The data collected clearly show not only the involvement of mDCs in the pathogenesis of psoriasis but also the crucial role that these cells play in the development of the disease.
2.2.3. Langerhans Cells (LCs)
Langerhans cells (LCs) are specialized dendritic cells with a defense role through antigen recognition and phagocytosis and are characterized by the presence of Birbeck granules in their cytoplasm, which are involved in endocytosis processes [84]. Studies on murine models have shown that LCs can play a role in acute psoriasis [85], increasing in number, and then decreasing after administration of an anti-IL-β antibody [86], which is responsible for the migratory deficiency and inhibition of LCs [87]. LCs appear to be involved in perpetuating psoriatic inflammation. LCs release different inflammatory chemokines [88], including IL-23 [89,90]. Further studies have shown that DCs can secrete TNF-α and iNOS [79,82] and can activate allogeneic T cells and induce the release of IL-17, IL-22, and IFN-γ [17], such as LCs in psoriatic skin [88,90]. Other studies have described a protective and a modulating role in situ played by LCs through IL-10 release [91] and neutrophil recruitment [92], respectively. LCs’ role is not fully understood, but these cells appear to be involved in perpetuating inflammation and psoriatic injury.
2.3. Innate Lymphoid Cells (ILCs)
Innate lymphoid cells (ILCs) are heterogeneous immune cells involved in the formation of lymph nodes during fetal life and the remodeling of organs and tissues [93]. ILC2s produce type 2 cytokines (e.g., IL-4, IL-5, IL-9, IL-13) that are implicated in the immune response to allergens, helminths, cancer, and viruses [94]. ILC2s have also been identified in greater levels in tissues with allergy symptoms, such as nasal polyps in patients with chronic rhinosinusitis and the skin of individuals with atopic dermatitis [95]. Elevated concentrations of ILC2s in the blood are linked to atopic dermatitis, while high concentrations of ILC3 are linked to psoriasis [96]. ILC3 releases IL-17 and IL-22 and expresses NKp44, a natural cytotoxic receptor (NKR) involved in viral antigen recognition and interactions with other immune cells [97,98,99]. The presence of these cells in psoriasis-injured skin is higher than in noninjured skin [98].
Natural Killer Cells (NKs)
Natural killer cells (NKs) belong to the ILC family. They maintain the state of health of the body and show cytotoxic and effector activity [97]. The cytotoxic effect is explained by the release of substances that induce cell lysis, such as granzyme, perforin, and granulysin (GNLY) [19], up to apoptosis induction [100,101]. NKs are found in excess in psoriatic lesions [102]; NKs represent about 8% of the entire cell population infiltrated into the lesion and express cytokines involved in psoriatic processes, such as IL-2, TNF-α, and IFN-γ as well as IL-17 and IL-22 [103,104]. Furthermore, they stimulate chemokine release by keratinocytes, useful for the in situ recall of other immune cells, implementing the inflammatory state [105]. NKs can express membrane NK receptors, such as killer immunoglobulin-like receptor (KIR) [106]. HLA-G is a ligand of KIR-2DL4 [107].
2.4. T Cells (Lymphocyte T Helper, T Cytotoxin γδ T, Natural Killer T Cells)
T cells are responsible for innate immunity, acting as sentinels and intervening in counteracting pathogenic antigens. They express TCRs (T cell receptors) consisting of an α chain and a β chain; however, T cells γδ T express receptors consisting of a γ chain and a δ chain [108]. T lymphocytes are widely represented in psoriasis-induced skin lesions [109] and are responsible for the release of IFN-γ, TNF-α, and IL-17 [109]. They also act in concert with keratinocytes, inducing the expression of HLA and IL-6 [109,110]. Specifically, Th, CD4+, and cytotoxic T lymphocytes (CD8+) are involved in the development of the disease [17,111]. Studies in immunodeficient mice have shown that CD4+ is among the first promoters of psoriasis [112]. In addition, CD4+ cell activation causes in situ recall and CD8+ cell stimulation, which are also involved in the pathogenesis of psoriasis [113]. The early infiltration of cytotoxic T lymphocytes, and not of Th lymphocytes, induces the phlogistic state typical of psoriasis [114,115]. In addition, keratinocytes express HLA-C*0602, which has antigens typical of TCD8+ cells and not CD4+ cells [49]. The efficacy of treatment with cyclosporin A [116,117] correlated with T lymphocyte inhibition and IL-2 reduction [116] has highlighted the significant role played by these cells in the pathogenesis of the disease. CD4+ Th17 can release IL-17, IL-23 [118], IL-22 [119], IFN-γ, and TNF-α. Th22 cells together with NK cells contribute to IL-22 release [119]. Some studies have shown that the γδ T cells are the T cells most involved in the release of IL-17 [17,120] and express different chemokines, such as CCR6, thus implementing the inflammatory state [120]. Natural killer T cells (NKTs) are a subpopulation of T cells that secrete IL-4 and IFN-γ and also represent a link between the adaptive and the innate immune system. Additionally, NKTs release cytokines (TNF-α, IFN-γ, IL-17, IL-22) and chemokines (CCR5, CCR6, CXCR3), thus stimulating the infiltration of other immune cells [121,122,123]. In fact, NKs and NKTs may contribute to the induction and maintenance of the inflammatory state, as also observed in a murine model of psoriasis [122,123]. These cells recognize the antigen presented by the surface receptor CD1d [124] and are highly represented in psoriatic skin, suggesting their involvement in the pathogenesis of the disease [103].
2.5. Neutrophils
Neutrophils are the cells most involved in the innate immunity; in fact, these cells play an important defense role through a respiratory burst, resulting in the release of reactive oxygen radicals (ROS) and degranulation and formation of neutrophil extracellular traps (NETs) [125]. Their activity is also related to the interaction and communication with APC cells and lymphocytes [126,127]. In psoriatic plaque-injured skin, neutrophils work by increasing respiratory bursts and releasing proteases, such as neutrophil elastase (NE), cathepsin g, myeloperoxidase (MPO), and proteinase 3. These mechanisms contribute to the increase in oxidative stress processes with consequent employment of the chemical mediators of phlogosis and the formation of autoantigen, typical of the psoriatic lesion [128,129]. However, the abundant presence of neutrophils is considered a typical histopathological sign of psoriasis; in fact, the neutrophil/lymphocyte ratio (NLR) is significantly increased in psoriatic patients [130,131]. The role played by NETs in the pathogenesis of psoriasis appears crucial: increased levels have been observed in lesions and plaques of psoriatic skin. A consequence of this numerical overload is the augmented release of IL-17 due to a stronger cellular stimulation, with the further secretion of chemical mediators, which again leads to a self-amplification of the number of neutrophils [128].
2.6. Mast Cells
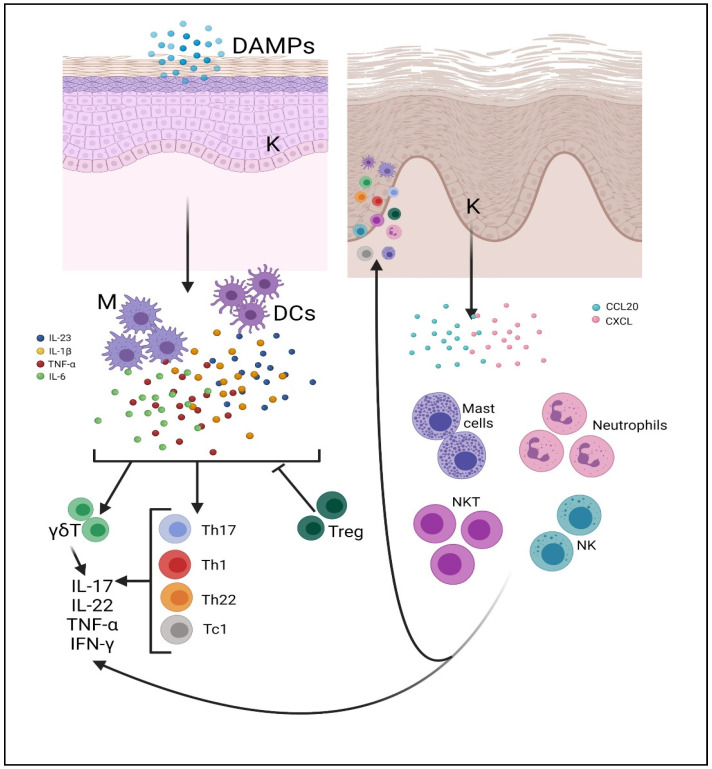
Mast cells are related to innate immunity and primarily responsible for acute inflammatory processes [132]. Once activated, these cells secrete several substances contained in the cytoplasmic granules such as heparin and histamine, nitric oxide (NO), leukotrienes, and interleukins such as IL-8, IL-17, and IL-22 [133,134]. Moreover, mast cells are active in skin lesions, contributing to the formation of psoriatic plaque [134]. The role of mast cells in psoriasis is mainly related to IL-22 production, whereas their role in IL-17 secretion is still unclear. IL-17 appears to be produced mainly by T cells and only to a small extent by mast cells [134], although other studies support the hypothesis that mast cells are involved in IL-17 production in both healthy and psoriatic skin [62]. The pathogenetic mechanism of immune cells in psoriasis in summarized in Figure 3.
Figure 3.
The pathogenetic mechanism of psoriasis. DAMPs activate DCs and macrophages by inducing the secretion of IL-23, IL-1β, IL-6, and TNF-α. They stimulate the TCD4+ (Th1, Th17, Th22) and CD8+ (Tc1)-mediated immune response. Mast cells, neutrophils, NK and NKT cells, and other immune cells infiltrate the site of phlogosis in the skin, contributing to disease progression by releasing IL-17 and antimicrobial peptides. Treg cells lose their suppressive activity and, in some cases, convert to Th17 cells, further increasing the local inflammatory reaction. Cytokines and chemokines act on keratinocytes, inducing their hyperproliferation. Activated keratinocytes produce CCL20 and CXCL1, 3, 8, 11, increasing cell infiltration. This creates an amplified continuous cycle that leads to injury. Abbreviations: M, macrophages; K, keratinocytes. Created with BioRender.com (accessed on 18 February 2022).
3. Psoriasis-Related Psychological Alterations
A peculiar psychological and personality profile can be outlined in patients with psoriasis. Some studies have shown that patients with this disease generally have a type D (D for “distressed”) personality, with high levels of social inhibition (SI) and negative affectivity (NA) [135]. This means that these patients experience strong negative emotions, but they avoid expressing them because of their fear of being disapproved [136]. In addition, they are more likely to manifest early maladaptive patterns, including emotional deprivation and vulnerability to harm [137], which are significant predictors of psychological distress, leading to difficulties in communicating their needs and emotions [138]. Several studies show that the quality of life of these patients is much lower than that of healthy patients, and that its impact is similar to that of other major chronic diseases [139]. Psoriasis and mental disorders could also be considered in a syndemic context since they influence each other on both a physiological and social level, which may suggest that they may become acute or alleviate at the same time [140]. Therefore, according to this perspective, a psychological intervention could be effective in alleviating both psoriasis and mental disorders [141]. Cognitive behavioral psychotherapy (CBT) is effective in treating psoriasis, especially in patients with moderate or severe forms, in terms of both area of reduction and severity of the disease [142], as well as being useful in treating feelings of hopelessness and other related comorbidities [142].
3.1. Psoriasis and Depression
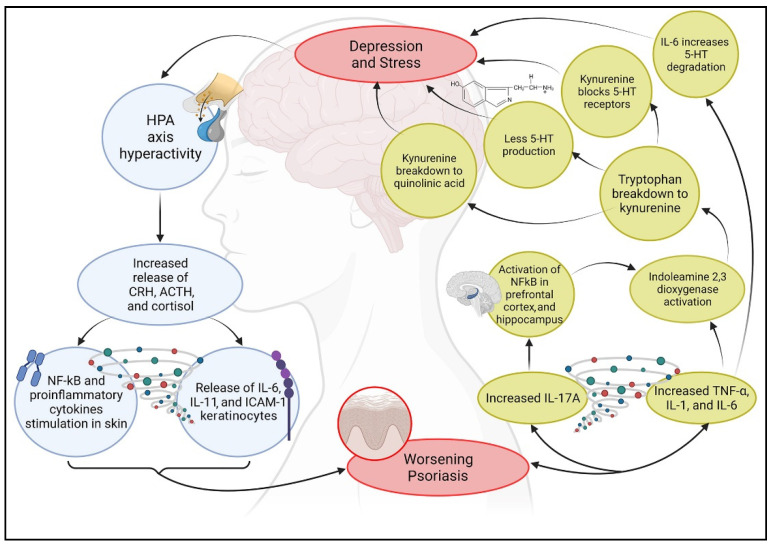
Several studies have demonstrated a correlation between psoriasis and depression [143]. Kurd et al. (2010) examined the clinical reports of almost 1 million subjects, aimed to determine the incidence of levels of anxiety, suicide risk, and depression in both patients with psoriasis and the rest of the population [144]. The results suggest that psoriatic patients have a higher risk of developing depression [145] and anxiety and are at a higher risk of committing suicide, especially young and male patients, as well as having greater comorbidities with other psychiatric disorders [144]. Furthermore, several studies suggest that depressed patients show a 30% higher production of proinflammatory cytokines, such as IL-1β, TNF-α, and C-reactive protein (CRP) [146,147], which affect the metabolism of some neurotransmitters (such as dopamine, serotonin, and glutamate), neuroendocrine function, and even neuroplasticity, resulting in neurotoxicity and neuronal apoptosis [148,149]. This production of cytokines can play an important role in both the aggravation of psoriasis and depression, confirming the link between the immune and neuroendocrine system and human behavior, which is altered in these cases [146,150,151]. A mechanism that elicits the onset of depression and at the same time chronic inflammation in patients with psoriasis is the hyperactivity of the HPA axis, resulting in the release of increased levels of CRH, ACTH, and cortisol and in a stimulation of the transcription factor NF-kB and of the proinflammatory cytokines in the skin [152]. CRH stimulates the proinflammatory cytokines IL-6 and IL-11 as well as the expression of the intracellular adhesion molecule-1 (ICAM-1) of keratinocytes, which promotes the migration of immune cells and facilitates cell-mediated immune responses [153]. In addition, dysfunction of cortisol receptors (mineralocorticoids and glucocorticoids) downstream from the HPA axis reduces the sensitivity of the anti-inflammatory effects of cortisol since the body is unable to skillfully regulate corticosteroid levels (Figure 4) [154]. Recently, the role of Th17 cells in depression has been investigated [155]. Several studies found that these cells were augmented in the blood of depressed patients [156]. Patients with psoriasis who show high levels of cytokines, Th17 cells and IL-17A, are more subjected to develop depression and anxiety disorders [144]. These data suggest a strong correlation between depression and the immune system; therefore, a relationship between depression and psoriasis may be hypothesized [157]: depression improvement might be observed following treatment of psoriasis, and conversely, depression treatment might improve psoriasis symptoms [157].
Figure 4.
Interactive relationship between psoriasis, depression, and stress. This graphic scheme summarizes the biological cyclic mechanism discussed in this review. Created with BioRender.com (accessed on 14 March 2022).
3.2. Psoriasis and Stress
Stress influences the activity of the immune response by increasing the cascade of proinflammatory cytokines [158]. Two neurotransmitters are generally associated with stress and psoriasis: serotonin (5-HT) and dopamine (DOPA). Serotonin is a potent neurotransmitter involved in nervous, immune, and endocrine systems [159,160,161,162,163,164]. Low levels of 5-HT increase the production of some inflammatory mediators, such as TNF-α and IL-1β, which induces the activation and deterioration of keratinocytes via NF-kB, which is activated by IL-17A in the prefrontal cortex and in the hippocampus, thus worsening the symptoms of psoriasis [165,166]. Inflammation can also activate indoleamine 2,3-dioxygenase, which induces tryptophan, a precursor of 5-HT, to break down into kynurenine [167], an antagonist of serotonin receptors, thus inducing depressive symptoms despite 5-HT availability. Moreover, kynurenine can break down into quinolinic acid, a neurotoxin that accumulates in the anterior cingulate gyrus of depressed patients [168]. This whole process is also adjuvated by IL-6, which increases the degradation of serotonin in the brain [169]. The psoriatic inflammatory process can simultaneously decrease the production of serotonin and may inhibit 5-HT receptors, thus contributing to its reduction (Figure 4).
DOPA can regulate mast cell degranulation and consequently stimulates the release of proinflammatory cytokines [170]; therefore, dopamine might be considered a risk factor for psoriasis [171]. Both innate and adaptive immune systems are involved in the stress response. Similar to what happens in the skin, damage-associated molecular patterns stimulate innate immune cells [172] to produce different interleukins and TNF-α [173] and to recruit an increasing number of monocytes that begin to circulate in the blood [174]. This unresolved inflammatory state can lead to chronic psychological stress [175]. The adaptive immune system can activate T cells in response to stress, thus stimulating cytokine release and NK cell and DC recruitment [176]. Consequent to stress, the sympathetic nervous system can endorse amine secretion, thus provoking the proliferation of myeloid cells (such as monocytes). These pieces of evidence suggest a link between stress and etiology of psoriasis.
4. Natural Compounds as an Alternative Treatment for Psoriasis
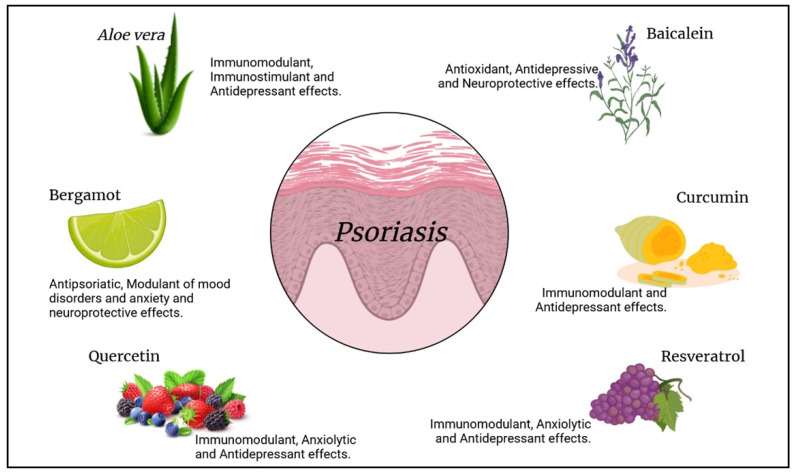
No definitive treatment is currently available to treat psoriasis; however, some biological therapies have shown encouraging results [177,178,179]. In particular, treatment with monoclonal antibodies, such as infliximab, ixekizumab, risankizumab, bimekizumab, guselkumab, secukinumab, and brodalumab, determined excellent outcomes in patients with moderate to severe psoriasis [180]. These drugs are mainly anti-TNF-α, anti-IL12/23, anti-IL-17, and anti-IL-23 antibodies and demonstrate the significant involvement of these patterns in exacerbating psoriasis and the therapeutic significance of using them as targets [180]. However, the long-term administration of these drug is often related to the appearance of different side effects [180,181]; for this reason, other therapeutic approaches and natural medicine have recently gained much attention from the scientific world. Natural products are potentially rich in bioactive compounds; in fact, different studies have already shown that some of these natural extracts may play anti-inflammatory, antioxidant, and antiproliferative effects [182,183]. These pieces of evidence demonstrate their possible use for the treatment of different diseases and also of psoriasis even thanks to their safety and the possible better compliance of patients [184,185,186]. In the following section, some of the best-known natural compounds with antipsoriatic properties are reported (Figure 5).
Figure 5.
Natural compounds and their effects on psoriasis. Created with BioRender.com (accessed on 14 March 2022).
4.1. Aloe vera L.
Aloe vera L., a plant belonging to the Liliaceae family, contains polysaccharides, salicylic acid, and vitamins that have anti-inflammatory and antipruritic properties [187]. Aloe vera possesses an immunomodulating effect, stimulating macrophages and lymphocytes to release NO and cytokines and activating the maturation of undeveloped dendritic cells [187]. A study conducted by Leng et al. (2018) showed that Aloe vera can inhibit overexpression of keratinocytes and overregulation of the NF-κB signaling pathway [188]. Clinical and preclinical studies demonstrated that ethanolic extract of Aloe vera exerts a positive activity on psoriatic lesions, similar to traditional drugs [189]. In addition, Aloe vera may have a significant antidepressant effect. The intake of at least 500 mg of Aloe vera capsules reduced depressive state in patients after 8 weeks of treatment [190]. The concomitant use of fluoxetine, a selective serotonin reuptake inhibitor (SSRI), reduces depressant symptoms in a mouse model [191].
4.2. Bergamot Essential Oil
Bergamot is the common name for Citrus bergamia, a plant belonging to the Rutaceae family [192]. Bergamot essential oil is one of the herbal preparations derived from C. bergamia, and it exerts antibacterial properties [193] and can help in the moderation of mood disorders and stress-induced anxiety, as well as sleep induction, and neuroprotection [194]. A study by Valkova et al. (2007) showed that the combination of bergamot essential oil and UVB rays significantly reduced the symptoms of psoriatic lesion [195]. This is probably due to the action of 5-methoxypsoralen (5-MOP), the major constituent of bergamot essential oil, mainly used in cosmetics and medicine. The application of this molecule in herbal medicine is useful, in fact, to combat skin damage, such as psoriasis-induced skin lesions and vitiligo [196]. Moreover, bergamot essential oil has been shown to be useful in neuroprotection (even during experimental brain ischemia), chronic pain control, and the management of stress, anxiety, and anxiety-related conditions in neuropharmacological research [197].
4.3. Quercetin
Quercetin, well known for its antioxidant and anti-inflammatory activity [198], can induce apoptosis through ROS generation [199] and can support keratinocyte-growth inhibition induced by arsenic trioxide [200]. A study by Mestry et al. (2020) evaluated the beneficial effect of a gel based on quercetin combined with Commiphora mukul in the treatment of psoriasis [201]. Moreover, on the one hand, quercetin decreased TNF-α, IL-6, and IL-17 levels, modulating the inflammatory state in psoriasis [202], and on the other hand, it is also involved in the management of cholinergic and serotonergic functions, producing an anxiolytic and antidepressant effect and enhancing memory performance [203]. A recent study has confirmed that quercetin significantly reduces anxiety behaviors in mice subjected to mild traumatic brain injury and regulates ACTH and corticosterone levels in the HPA axis, enhancing depressive states [204].
4.4. Baicalein
Baicalein, a traditional Chinese drug with anti-inflammatory and antiviral effects [205], can regulate keratinocyte proliferation and differentiation [206]. It can decrease the severity of chronic inflammations by improving the antioxidant status and reducing the oxidative stress, regulating the secretion of cytokines and chemokines (IL-6 and TNF-α reduction) [207,208], inhibiting Th17 activation, and blocking the IL-17-induced inflammatory cascade. Furthermore, baicalein can improve depressive symptoms, preventing the loss of dopamine and brain-derived neurotrophic factor (BDNF) [183,209]. In particular, a study on a murine model highlighted that baicalein treatment can alleviate depression-like symptoms [210].
4.5. Curcumin
Curcumin can be used for the treatment of psoriasis. In fact, the active constituent of Curcuma longa [211] shows an antiproliferative effect on keratinocytes [181]. Moreover, curcumin may have significant anti-inflammatory effects by decreasing cytokine levels, such as IL-1β, IL-6, IL-22, and TNF-α, suggesting new perspectives for its therapeutic use [212]. Furthermore, curcumin inhibits phosphorylase kinases, which are increased in patients with psoriasis [213]. Curcumin also showed a strong antidepressant effect [214] thanks to its modulation of neurotransmitters, such as noradrenaline, dopamine, serotonin, and monoamine, and through moderation of excessive corticosterone secretion, which causes dysfunction in the HPA axis [215].
4.6. Resveratrol
Resveratrol is a polyphenol with anti-inflammatory and antioxidant properties contained in several foods, especially red wine, which is a key element in the Mediterranean food tradition [216,217,218,219]. Resveratrol acts by reducing the secretion of inflammatory cytokines and inducing apoptosis in keratinocytes via silent mating type information regulation 2 homolog (SIRT1). Resveratrol may act by inhibiting the release of IL-17 [220]. In addition, a study by Khurana et al. (2020) proved that resveratrol-loaded polymeric micelles act on psoriatic lesions with positive dermatological results [221]. A recent study showed that resveratrol also plays a critical role in neuroprotection, inhibiting the expression of phosphodiesterase 4D (PDE4D), an enzyme that catalyzes the hydrolysis of cyclic adenosine monophosphate (cAMP). PDE4D regulates cAMP expression at the intracellular level, reducing the depressant- and anxious-like states of corticosterone induced by cell lesion on a mouse model [222].
In summary, natural products analyzed here show antipsoriatic, antidepressant, and anxiolytic activities.
The biological effects of natural compounds are summarized in Table 1.
Table 1.
Biological effects of natural compounds on psoriasis.
| Natural Compounds | Biological Effects | References |
|---|---|---|
| Aloe vera L. | Immunomodulant and stimulant effect on macrophages, lymphocytes, and dendritic cells. | [187] |
| Antidepressant effect. | [190,191] | |
| Bergamot essential oil | Antibacterial and anti-psoriatic properties. | [193,195] |
| Moderation of mood disorders and stress-induced anxiety. Neuroprotective and sleep-inducing effect. | [194] | |
| Quercetin | Decrease in TNF-α, IL-6, and IL-17 levels. | [202] |
| Regulation of cholinergic and sero-tonergic functions, anxiolytic and anti-depressant effects, enhances memory performance. | [203,204] | |
| Baicalein | Antioxidant effect, inhibits the release of IL-17 and the expression of IL-6 and TNF-α. | [207,208] |
| Antidepressive and neuroprotective effect. | [183,209] | |
| Curcumin | Decrease in IL-1β, IL-6, IL-22, and TNF-α levels. | [212] |
| Modulates serotonin, monoamine, noradrenaline, and dopamine. Regu-lates the function of the HPA axis. | [214,215] | |
| Resveratrol | Reduces the secretion of inflammatory cytokines and induces apoptosis in keratinocytes. Inhibits the release of IL-17. | [220] |
| Anxiolytic and antidepressant effect by inhibiting the expression of PDE4D, which regulates cAMP expression at the intracellular level. | [222] |
5. Conclusions
Psoriasis is the most common chronic autoimmune skin disease that seems to arise from the interaction between external and internal factors, as well as vitiligo. High stressogenic conditions and alterations in the psychological picture seem to play a key role in the development of these diseases. It results from a chronic inflammatory state orchestrated by cells of the immune system, such as lymphocytes, mast cells, dendritic cells, and NK cells, which interact with keratinocytes. Since not all pathogenetic mechanisms related to these cells have been clarified, this review aims to evaluate the state of the art on the etiology of psoriasis and to offer further reflection points. In addition, no definitive treatment for psoriasis is available until now: commercial drugs cannot be administered for long times, so the use of alternative treatments can improve the clinical, physical, and psychological features of patients suffering from this disease. Further clinical and preclinical studies should be conducted to adopt natural compound therapy as an adjunct to traditional medicines, as these compounds act on the immune system, the skin, and the central nervous system. In conclusion, since the inflammatory psoriatic state results from uncontrolled activation of immune system cells, further studies on natural bioactive compounds that inhibit or suppress these hyperactivations could be suggested.
Acknowledgments
The authors are thankful to all the scientists cited below and their valuable works.
Author Contributions
Conceptualization, A.A.; investigation, A.A., A.F., N.I., E.M. and M.V.; data curation, A.A., E.R.L., A.F., N.I., E.M., M.V., S.G., A.S., N.C. and S.P.; writing—original draft preparation, A.A. and A.F.; writing—review and editing, A.A., E.R.L., N.I., M.V., S.G., A.S., N.C. and S.P.; visualization, A.F.; supervision, S.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Not available.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pergolizzi S., Vaccaro M., Magaudda L., Mondello M.R., Arco A., Bramanti P., Cannavo S.P., Guarneri B. Immunohistochemical study of epidermal nerve fibres in involved and uninvolved psoriatic skin using confocal laser scanning microscopy. Arch. Dermatol. Res. 1998;290:483–489. doi: 10.1007/s004030050340. [DOI] [PubMed] [Google Scholar]
- 2.Vaccaro M., Pergolizzi S., Mondello M.R., Santoro G., Cannavo S.P., Guarneri B., Magaudda L. The dermoepidermal junction in psoriatic skin as revealed by scanning electron microscopy. Arch. Dermatol. Res. 1999;291:396–399. doi: 10.1007/s004030050428. [DOI] [PubMed] [Google Scholar]
- 3.Iskandar I.Y.K., Parisi R., Griffiths C.E.M., Ashcroft D.M. Systematic review examining changes over time and variation in the incidence and prevalence of psoriasis by age and gender. Br. J. Dermatol. 2020;184:243–258. doi: 10.1111/bjd.19169. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong A.W. Psoriasis. JAMA Dermatol. 2017;153:956. doi: 10.1001/jamadermatol.2017.2103. [DOI] [PubMed] [Google Scholar]
- 5.Raychaudhuri S.K., Maverakis E., Raychaudhuri S.P. Diagnosis and classification of psoriasis. Autoimmun. Rev. 2014;13:490–495. doi: 10.1016/j.autrev.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Dika E., Bardazzi F., Balestri R., Maibach H.I. Environmental Factors and Psoriasis1. In Environmental Factors in Skin Diseases. Curr. Probl. Dermatol. 2007;35:118–135. doi: 10.1159/000106419. [DOI] [PubMed] [Google Scholar]
- 7.Chandra A., Ray A., Senapati S., Chatterjee R. Genetic and epigenetic basis of psoriasis pathogenesis. Mol. Immunol. 2015;64:313–323. doi: 10.1016/j.molimm.2014.12.014. [DOI] [PubMed] [Google Scholar]
- 8.Fernandes A.R., Martins-Gomes C., Santini A., Silva A.M., Souto E.B. Design of Nanostructures for Versatile Therapeutic Applications. Elsevier; Amsterdam, The Netherlands: 2018. Psoriasis vulgaris—Pathophysiology of the disease and its classical treatment versus new drug delivery systems; pp. 379–406. [Google Scholar]
- 9.Nestle F.O., Kaplan D.H., Barker J. Psoriasis. N. Engl. J. Med. 2009;361:496–509. doi: 10.1056/NEJMra0804595. [DOI] [PubMed] [Google Scholar]
- 10.Bhosle M.J., Kulkarni A., Feldman S.R., Balkrishnan R. Quality of life in patients with psoriasis. Health Qual. Life Outcomes. 2006;4:35. doi: 10.1186/1477-7525-4-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heng M.C., Kloss S.G., Kuehn C.S., Chase D.G. The sequence of events in psoriatic plaque formation after tape-stripping. Br. J. Dermatol. 1985;112:517–532. doi: 10.1111/j.1365-2133.1985.tb15259.x. [DOI] [PubMed] [Google Scholar]
- 12.Benhadou F., Mintoff D., Del Marmol V. Psoriasis: Keratinocytes or Immune Cells—Which Is the Trigger? Dermatology. 2019;235:91–100. doi: 10.1159/000495291. [DOI] [PubMed] [Google Scholar]
- 13.Nestle F.O., Turka L.A., Nickoloff B.J. Characterization of dermal dendritic cells in psoriasis. Autostimulation of T lymphocytes and induction of Th1 type cytokines. J. Clin. Investig. 1994;94:202–209. doi: 10.1172/JCI117308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iwakura Y., Ishigame H., Saijo S., Nakae S. Functional specialization of interleukin-17 family members. Immunity. 2011;34:149–162. doi: 10.1016/j.immuni.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Di Cesare A., Di Meglio P., Nestle F.O. The IL-23/Th17 axis in the immunopathogenesis of psoriasis. J. Investig. Dermatol. 2009;129:1339–1350. doi: 10.1038/jid.2009.59. [DOI] [PubMed] [Google Scholar]
- 16.Kastelein R.A., Hunter C.A., Cua D.J. Discovery and biology of IL-23 and IL-27: Related but functionally distinct regulators of inflammation. Annu. Rev. Immunol. 2007;25:221–242. doi: 10.1146/annurev.immunol.22.012703.104758. [DOI] [PubMed] [Google Scholar]
- 17.Lowes M.A., Kikuchi T., Fuentes-Duculan J., Cardinale I., Zaba L.C., Haider A.S., Bowman E.P., Krueger J.G. Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. J. Investig. Dermatol. 2008;128:1207–1211. doi: 10.1038/sj.jid.5701213. [DOI] [PubMed] [Google Scholar]
- 18.Amin M., Darji K., No D.J., Wu J.J. Review of phase III trial data on IL-23 inhibitors tildrakizumab and guselkumab for psoriasis. J. Eur. Acad. Dermatol. Venereol. 2017;31:1627–1632. doi: 10.1111/jdv.14451. [DOI] [PubMed] [Google Scholar]
- 19.Sato Y., Ogawa E., Okuyama R. Role of Innate Immune Cells in Psoriasis. Int. J. Mol. Sci. 2020;21:6604. doi: 10.3390/ijms21186604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vanderpuye-Orgle J., Zhao Y., Lu J., Shrestha A., Sexton A., Seabury S., Lebwohl M. Evaluating the economic burden of psoriasis in the United States. J. Am. Acad. Dermatol. 2015;72:961–967.e965. doi: 10.1016/j.jaad.2015.02.1099. [DOI] [PubMed] [Google Scholar]
- 21.Brezinski E.A., Dhillon J.S., Armstrong A.W. Economic Burden of Psoriasis in the United States: A Systematic Review. JAMA Dermatol. 2015;151:651–658. doi: 10.1001/jamadermatol.2014.3593. [DOI] [PubMed] [Google Scholar]
- 22.Hawro T., Zalewska A., Hawro M., Kaszuba A., Krolikowska M., Maurer M. Impact of psoriasis severity on family income and quality of life. J. Eur. Acad. Dermatol. Venereol. 2015;29:438–443. doi: 10.1111/jdv.12572. [DOI] [PubMed] [Google Scholar]
- 23.Singh S., Taylor C., Kornmehl H., Armstrong A.W. Psoriasis and suicidality: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2017;77:425–440.e422. doi: 10.1016/j.jaad.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 24.Ferreira B.I., Abreu J.L., Reis J.P., Figueiredo A.M. Psoriasis and Associated Psychiatric Disorders: A Systematic Review on Etiopathogenesis and Clinical Correlation. J. Clin. Aesthet. Dermatol. 2016;9:36–43. [PMC free article] [PubMed] [Google Scholar]
- 25.Hall J.M., Cruser D., Podawiltz A., Mummert D.I., Jones H., Mummert M.E. Psychological Stress and the Cutaneous Immune Response: Roles of the HPA Axis and the Sympathetic Nervous System in Atopic Dermatitis and Psoriasis. Dermatol. Res. Pract. 2012;2012:403908. doi: 10.1155/2012/403908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Connor C.J., Liu V., Fiedorowicz J.G. Exploring the Physiological Link between Psoriasis and Mood Disorders. Dermatol. Res. Pract. 2015;2015:409637. doi: 10.1155/2015/409637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Snast I., Reiter O., Atzmony L., Leshem Y.A., Hodak E., Mimouni D., Pavlovsky L. Psychological stress and psoriasis: A systematic review and meta-analysis. Br. J. Dermatol. 2018;178:1044–1055. doi: 10.1111/bjd.16116. [DOI] [PubMed] [Google Scholar]
- 28.Takeshita J., Grewal S., Langan S.M., Mehta N.N., Ogdie A., Van Voorhees A.S., Gelfand J.M. Psoriasis and comorbid diseases: Epidemiology. J. Am. Acad. Dermatol. 2017;76:377–390. doi: 10.1016/j.jaad.2016.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Conrad C., Gilliet M. Psoriasis: From Pathogenesis to Targeted Therapies. Clin. Rev. Allergy Immunol. 2018;54:102–113. doi: 10.1007/s12016-018-8668-1. [DOI] [PubMed] [Google Scholar]
- 30.Cho J.S., Pietras E.M., Garcia N.C., Ramos R.I., Farzam D.M., Monroe H.R., Magorien J.E., Blauvelt A., Kolls J.K., Cheung A.L., et al. IL-17 is essential for host defense against cutaneous Staphylococcus aureus infection in mice. J. Clin. Investig. 2010;120:1762–1773. doi: 10.1172/JCI40891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alesci A., Cicero N., Salvo A., Palombieri D., Zaccone D., Dugo G., Bruno M., Vadala R., Lauriano E.R., Pergolizzi S. Extracts deriving from olive mill waste water and their effects on the liver of the goldfish Carassius auratus fed with hypercholesterolemic diet. Nat. Prod. Res. 2014;28:1343–1349. doi: 10.1080/14786419.2014.903479. [DOI] [PubMed] [Google Scholar]
- 32.Pergolizzi S., D’Angelo V., Aragona M., Dugo P., Cacciola F., Capillo G., Dugo G., Lauriano E.R. Evaluation of antioxidant and anti-inflammatory activity of green coffee beans methanolic extract in rat skin. Nat. Prod. Res. 2018;34:1535–1541. doi: 10.1080/14786419.2018.1523161. [DOI] [PubMed] [Google Scholar]
- 33.Alesci A., Miller A., Tardugno R., Pergolizzi S. Chemical analysis, biological and therapeutic activities of Olea europaea L. Nat. Prod. Res. 2021 doi: 10.1080/14786419.2021.1922404. [DOI] [PubMed] [Google Scholar]
- 34.Gervasi T., Pellizzeri V., Benameur Q., Gervasi C., Santini A., Cicero N., Dugo G. Valorization of raw materials from agricultural industry for astaxanthin and beta-carotene production by Xanthophyllomyces dendrorhous. Nat. Prod. Res. 2018;32:1554–1561. doi: 10.1080/14786419.2017.1385024. [DOI] [PubMed] [Google Scholar]
- 35.Naviglio D., Pizzolongo F., Ferrara L., Aragòn A., Santini A. Extraction of pure lycopene from industrial tomato by-products in water using a new high-pressure process. J. Sci. Food Agric. 2008;88:2414–2420. doi: 10.1002/jsfa.3334. [DOI] [Google Scholar]
- 36.Durazzo A., Lucarini M., Camilli E., Marconi S., Gabrielli P., Lisciani S., Gambelli L., Aguzzi A., Novellino E., Santini A., et al. Dietary Lignans: Definition, Description and Research Trends in Databases Development. Molecules. 2018;23:3251. doi: 10.3390/molecules23123251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li J., Li X., Hou R., Liu R., Zhao X., Dong F., Wang C., Yin G., Zhang K. Psoriatic T cells reduce epidermal turnover time and affect cell proliferation contributed from differential gene expression. J. Dermatol. 2015;42:874–880. doi: 10.1111/1346-8138.12961. [DOI] [PubMed] [Google Scholar]
- 38.Mondello M.R., Magaudda L., Pergolizzi S., Santoro A., Vaccaro M., Califano L., Cannavo S.P., Guarneri B. Behaviour of laminin 1 and type IV collagen in uninvolved psoriatic skin. Immunohistochemical study using confocal laser scanning microscopy. Arch. Dermatol. Res. 1996;288:527–531. doi: 10.1007/BF02505249. [DOI] [PubMed] [Google Scholar]
- 39.Magaudda L., Mondello M.R., Vaccaro M., Pergolizzi S., Cannavo S.P., Guarneri B., Santoro A. Changes in the distribution of actin-associated proteins in psoriatic keratinocytes. Immunohistochemical study using confocal laser scanning microscopy. Arch. Dermatol. Res. 1997;289:378–383. doi: 10.1007/s004030050208. [DOI] [PubMed] [Google Scholar]
- 40.Salmon J.K., Armstrong C.A., Ansel J.C. The skin as an immune organ. West. J. Med. 1994;160:146–152. [PMC free article] [PubMed] [Google Scholar]
- 41.Albanesi C., De Pita O., Girolomoni G. Resident skin cells in psoriasis: A special look at the pathogenetic functions of keratinocytes. Clin. Dermatol. 2007;25:581–588. doi: 10.1016/j.clindermatol.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 42.Lowes M.A., Suarez-Farinas M., Krueger J.G. Immunology of psoriasis. Annu. Rev. Immunol. 2014;32:227–255. doi: 10.1146/annurev-immunol-032713-120225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lande R., Botti E., Jandus C., Dojcinovic D., Fanelli G., Conrad C., Chamilos G., Feldmeyer L., Marinari B., Chon S., et al. The antimicrobial peptide LL37 is a T-cell autoantigen in psoriasis. Nat. Commun. 2014;5:5621. doi: 10.1038/ncomms6621. [DOI] [PubMed] [Google Scholar]
- 44.Nickoloff B.J., Turka L.A. Immunological functions of non-professional antigen-presenting cells: New insights from studies of T-cell interactions with keratinocytes. Immunol. Today. 1994;15:464–469. doi: 10.1016/0167-5699(94)90190-2. [DOI] [PubMed] [Google Scholar]
- 45.Gillitzer R., Wolff K., Tong D., Muller C., Yoshimura T., Hartmann A.A., Stingl G., Berger R. MCP-1 mRNA expression in basal keratinocytes of psoriatic lesions. J. Investig. Dermatol. 1993;101:127–131. doi: 10.1111/1523-1747.ep12363613. [DOI] [PubMed] [Google Scholar]
- 46.Homey B., Wang W., Soto H., Buchanan M.E., Wiesenborn A., Catron D., Muller A., McClanahan T.K., Dieu-Nosjean M.C., Orozco R., et al. Cutting edge: The orphan chemokine receptor G protein-coupled receptor-2 (GPR-2, CCR10) binds the skin-associated chemokine CCL27 (CTACK/ALP/ILC) J. Immunol. 2000;164:3465–3470. doi: 10.4049/jimmunol.164.7.3465. [DOI] [PubMed] [Google Scholar]
- 47.Gangemi S., Merendino R.A., Guarneri F., Minciullo P.L., DiLorenzo G., Pacor M., Cannavo S.P. Serum levels of interleukin-18 and s-ICAM-1 in patients affected by psoriasis: Preliminary considerations. J. Eur. Acad. Dermatol. Venereol. 2003;17:42–46. doi: 10.1046/j.1468-3083.2003.00647.x. [DOI] [PubMed] [Google Scholar]
- 48.Sugita K., Kabashima K., Atarashi K., Shimauchi T., Kobayashi M., Tokura Y. Innate immunity mediated by epidermal keratinocytes promotes acquired immunity involving Langerhans cells and T cells in the skin. Clin. Exp. Immunol. 2007;147:176–183. doi: 10.1111/j.1365-2249.2006.03258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nair R.P., Stuart P.E., Nistor I., Hiremagalore R., Chia N.V.C., Jenisch S., Weichenthal M., Abecasis G.R., Lim H.W., Christophers E., et al. Sequence and haplotype analysis supports HLA-C as the psoriasis susceptibility 1 gene. Am. J. Hum. Genet. 2006;78:827–851. doi: 10.1086/503821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Prinz J.C. Autoimmune aspects of psoriasis: Heritability and autoantigens. Autoimmun. Rev. 2017;16:970–979. doi: 10.1016/j.autrev.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 51.Lauriano E.R., Pergolizzi S., Capillo G., Kuciel M., Alesci A., Faggio C. Immunohistochemical characterization of Toll-like receptor 2 in gut epithelial cells and macrophages of goldfish Carassius auratus fed with a high-cholesterol diet. Fish. Shellfish Immunol. 2016;59:250–255. doi: 10.1016/j.fsi.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 52.Lauriano E.R., Silvestri G., Kuciel M., Zuwala K., Zaccone D., Palombieri D., Alesci A., Pergolizzi S. Immunohistochemical localization of Toll-like receptor 2 in skin Langerhans’ cells of striped dolphin (Stenella coeruleoalba) Tissue Cell. 2014;46:113–121. doi: 10.1016/j.tice.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 53.Lauriano E.R., Aragona M., Alesci A., Lo Cascio P., Pergolizzi S. Toll-like receptor 2 and alpha-Smooth Muscle Actin expressed in the tunica of a urochordate, Styela plicata. Tissue Cell. 2021;71:101584. doi: 10.1016/j.tice.2021.101584. [DOI] [PubMed] [Google Scholar]
- 54.Alesci A., Pergolizzi S., Lo Cascio P., Fumia A., Lauriano E.R. Neuronal Regeneration: Vertebrates comparative overview and new perspectives for Neurodegenerative diseases. Acta Zool. 2021 doi: 10.1111/azo.12397. [DOI] [Google Scholar]
- 55.McInturff J.E., Modlin R.L., Kim J. The role of toll-like receptors in the pathogenesis and treatment of dermatological disease. J. Investig. Dermatol. 2005;125:1–8. doi: 10.1111/j.0022-202X.2004.23459.x. [DOI] [PubMed] [Google Scholar]
- 56.Miller L.S., Sorensen O.E., Liu P.T., Jalian H.R., Eshtiaghpour D., Behmanesh B.E., Chung W., Starner T.D., Kim J., Sieling P.A., et al. TGF-alpha regulates TLR expression and function on epidermal keratinocytes. J. Immunol. 2005;174:6137–6143. doi: 10.4049/jimmunol.174.10.6137. [DOI] [PubMed] [Google Scholar]
- 57.Curry J.L., Qin J.Z., Bonish B., Carrick R., Bacon P., Panella J., Robinson J., Nickoloff B.J. Innate immune-related receptors in normal and psoriatic skin. Arch. Pathol Lab. Med. 2003;127:178–186. doi: 10.5858/2003-127-178-IIRRIN. [DOI] [PubMed] [Google Scholar]
- 58.Xiao C.Y., Zhu Z.L., Zhang C., Fu M., Qiao H.J., Wang G., Dang E.L. Small interfering RNA targeting of keratin 17 reduces inflammation in imiquimod-induced psoriasis-like dermatitis. Chin. Med. J. 2020;133:2910–2918. doi: 10.1097/CM9.0000000000001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang X., Yin M., Zhang L.J. Keratin 6, 16 and 17-Critical Barrier Alarmin Molecules in Skin Wounds and Psoriasis. Cells. 2019;8:807. doi: 10.3390/cells8080807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zaba L.C., Krueger J.G., Lowes M.A. Resident and “inflammatory” dendritic cells in human skin. J. Investig. Dermatol. 2009;129:302–308. doi: 10.1038/jid.2008.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pergolizzi S., Rizzo G., Favaloro A., Alesci A., Pallio S., Melita G., Cutroneo G., Lauriano E.R. Expression of VAChT and 5-HT in Ulcerative Colitis dendritic cells. Acta Histochem. 2021;123:151715. doi: 10.1016/j.acthis.2021.151715. [DOI] [PubMed] [Google Scholar]
- 62.Chiricozzi A., Romanelli P., Volpe E., Borsellino G., Romanelli M. Scanning the Immunopathogenesis of Psoriasis. Int. J. Mol. Sci. 2018;19:179. doi: 10.3390/ijms19010179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu Y.J. IPC: Professional type 1 interferon-producing cells and plasmacytoid dendritic cell precursors. Annu. Rev. Immunol. 2005;23:275–306. doi: 10.1146/annurev.immunol.23.021704.115633. [DOI] [PubMed] [Google Scholar]
- 64.Cella M., Jarrossay D., Facchetti F., Alebardi O., Nakajima H., Lanzavecchia A., Colonna M. Plasmacytoid monocytes migrate to inflamed lymph nodes and produce large amounts of type I interferon. Nat. Med. 1999;5:919–923. doi: 10.1038/11360. [DOI] [PubMed] [Google Scholar]
- 65.Fonteneau J.F., Gilliet M., Larsson M., Dasilva I., Munz C., Liu Y.J., Bhardwaj N. Activation of influenza virus-specific CD4+ and CD8+ T cells: A new role for plasmacytoid dendritic cells in adaptive immunity. Blood. 2003;101:3520–3526. doi: 10.1182/blood-2002-10-3063. [DOI] [PubMed] [Google Scholar]
- 66.Blanco P., Palucka A.K., Gill M., Pascual V., Banchereau J. Induction of dendritic cell differentiation by IFN-alpha in systemic lupus erythematosus. Science. 2001;294:1540–1543. doi: 10.1126/science.1064890. [DOI] [PubMed] [Google Scholar]
- 67.Gilliet M., Conrad C., Geiges M., Cozzio A., Thurlimann W., Burg G., Nestle F.O., Dummer R. Psoriasis triggered by toll-like receptor 7 agonist imiquimod in the presence of dermal plasmacytoid dendritic cell precursors. Arch. Dermatol. 2004;140:1490–1495. doi: 10.1001/archderm.140.12.1490. [DOI] [PubMed] [Google Scholar]
- 68.Farkas L., Beiske K., Lund-Johansen F., Brandtzaeg P., Jahnsen F.L. Plasmacytoid dendritic cells (natural interferon- alpha/beta-producing cells) accumulate in cutaneous lupus erythematosus lesions. Am. J. Pathol. 2001;159:237–243. doi: 10.1016/S0002-9440(10)61689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Van Krinks C.H., Matyszak M.K., Gaston J.S. Characterization of plasmacytoid dendritic cells in inflammatory arthritis synovial fluid. Rheumatology. 2004;43:453–460. doi: 10.1093/rheumatology/keh115. [DOI] [PubMed] [Google Scholar]
- 70.Kadowaki N., Ho S., Antonenko S., Malefyt R.W., Kastelein R.A., Bazan F., Liu Y.J. Subsets of human dendritic cell precursors express different toll-like receptors and respond to different microbial antigens. J. Exp. Med. 2001;194:863–869. doi: 10.1084/jem.194.6.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ito T., Amakawa R., Inaba M., Hori T., Ota M., Nakamura K., Takebayashi M., Miyaji M., Yoshimura T., Inaba K., et al. Plasmacytoid dendritic cells regulate Th cell responses through OX40 ligand and type I IFNs. J. Immunol. 2004;172:4253–4259. doi: 10.4049/jimmunol.172.7.4253. [DOI] [PubMed] [Google Scholar]
- 72.Nestle F.O., Conrad C., Tun-Kyi A., Homey B., Gombert M., Boyman O., Burg G., Liu Y.J., Gilliet M. Plasmacytoid predendritic cells initiate psoriasis through interferon-alpha production. J. Exp. Med. 2005;202:135–143. doi: 10.1084/jem.20050500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Randolph G.J., Ochando J., Partida-Sanchez S. Migration of dendritic cell subsets and their precursors. Annu. Rev. Immunol. 2008;26:293–316. doi: 10.1146/annurev.immunol.26.021607.090254. [DOI] [PubMed] [Google Scholar]
- 74.Sozzani S. Dendritic cell trafficking: More than just chemokines. Cytokine Growth Factor Rev. 2005;16:581–592. doi: 10.1016/j.cytogfr.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 75.Vinter H., Iversen L., Steiniche T., Kragballe K., Johansen C. Aldara(R)-induced skin inflammation: Studies of patients with psoriasis. Br. J. Dermatol. 2015;172:345–353. doi: 10.1111/bjd.13236. [DOI] [PubMed] [Google Scholar]
- 76.Takeda K., Kaisho T., Akira S. Toll-like receptors. Annu. Rev. Immunol. 2003;21:335–376. doi: 10.1146/annurev.immunol.21.120601.141126. [DOI] [PubMed] [Google Scholar]
- 77.Honda K., Ohba Y., Yanai H., Negishi H., Mizutani T., Takaoka A., Taya C., Taniguchi T. Spatiotemporal regulation of MyD88-IRF-7 signalling for robust type-I interferon induction. Nature. 2005;434:1035–1040. doi: 10.1038/nature03547. [DOI] [PubMed] [Google Scholar]
- 78.Lowes M.A., Turton J.A., Krueger J.G., Barnetson R.S. Psoriasis vulgaris flare during efalizumab therapy does not preclude future use: A case series. BMC Dermatol. 2005;5:9. doi: 10.1186/1471-5945-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zaba L.C., Fuentes-Duculan J., Eungdamrong N.J., Abello M.V., Novitskaya I., Pierson K.C., Gonzalez J., Krueger J.G., Lowes M.A. Psoriasis is characterized by accumulation of immunostimulatory and Th1/Th17 cell-polarizing myeloid dendritic cells. J. Investig. Dermatol. 2009;129:79–88. doi: 10.1038/jid.2008.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Johnson-Huang L.M., McNutt N.S., Krueger J.G., Lowes M.A. Cytokine-producing dendritic cells in the pathogenesis of inflammatory skin diseases. J. Clin. Immunol. 2009;29:247–256. doi: 10.1007/s10875-009-9278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chu C.C., Di Meglio P., Nestle F.O. Harnessing dendritic cells in inflammatory skin diseases. Semin. Immunol. 2011;23:28–41. doi: 10.1016/j.smim.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lowes M.A., Chamian F., Abello M.V., Fuentes-Duculan J., Lin S.L., Nussbaum R., Novitskaya I., Carbonaro H., Cardinale I., Kikuchi T., et al. Increase in TNF-alpha and inducible nitric oxide synthase-expressing dendritic cells in psoriasis and reduction with efalizumab (anti-CD11a) Proc. Natl. Acad. Sci. USA. 2005;102:19057–19062. doi: 10.1073/pnas.0509736102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kim T.G., Jee H., Fuentes-Duculan J., Wu W.H., Byamba D., Kim D.S., Kim D.Y., Lew D.H., Yang W.I., Krueger J.G., et al. Dermal clusters of mature dendritic cells and T cells are associated with the CCL20/CCR6 chemokine system in chronic psoriasis. J. Investig. Dermatol. 2014;134:1462–1465. doi: 10.1038/jid.2013.534. [DOI] [PubMed] [Google Scholar]
- 84.Alesci A., Lauriano E.R., Aragona M., Capillo G., Pergolizzi S. Marking vertebrates langerhans cells, from fish to mammals. Acta Histochem. 2020;122:151622. doi: 10.1016/j.acthis.2020.151622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sundberg J.P., Boggess D., Sundberg B.A., Beamer W.G., Shultz L.D. Epidermal dendritic cell populations in the flaky skin mutant mouse. Immunol. Investig. 1993;22:389–401. doi: 10.3109/08820139309063417. [DOI] [PubMed] [Google Scholar]
- 86.Schon M., Behmenburg C., Denzer D., Schon M.P. Pathogenic function of IL-1 beta in psoriasiform skin lesions of flaky skin (fsn/fsn) mice. Clin. Exp. Immunol. 2001;123:505–510. doi: 10.1046/j.1365-2249.2001.01421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cumberbatch M., Singh M., Dearman R.J., Young H.S., Kimber I., Griffiths C.E. Impaired Langerhans cell migration in psoriasis. J. Exp. Med. 2006;203:953–960. doi: 10.1084/jem.20052367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fujita H., Shemer A., Suarez-Farinas M., Johnson-Huang L.M., Tintle S., Cardinale I., Fuentes-Duculan J., Novitskaya I., Carucci J.A., Krueger J.G., et al. Lesional dendritic cells in patients with chronic atopic dermatitis and psoriasis exhibit parallel ability to activate T-cell subsets. J. Allergy Clin. Immunol. 2011;128:574–582.e12. doi: 10.1016/j.jaci.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 89.Martini E., Wiken M., Cheuk S., Gallais Serezal I., Baharom F., Stahle M., Smed-Sorensen A., Eidsmo L. Dynamic Changes in Resident and Infiltrating Epidermal Dendritic Cells in Active and Resolved Psoriasis. J. Investig. Dermatol. 2017;137:865–873. doi: 10.1016/j.jid.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 90.Eidsmo L., Martini E. Human Langerhans Cells with Pro-inflammatory Features Relocate within Psoriasis Lesions. Front. Immunol. 2018;9:300. doi: 10.3389/fimmu.2018.00300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bos J.D., Hulsebosch H.J., Krieg S.R., Bakker P.M., Cormane R.H. Immunocompetent cells in psoriasis. In situ immunophenotyping by monoclonal antibodies. Arch. Dermatol. Res. 1983;275:181–189. doi: 10.1007/BF00510050. [DOI] [PubMed] [Google Scholar]
- 92.Terhorst D., Chelbi R., Wohn C., Malosse C., Tamoutounour S., Jorquera A., Bajenoff M., Dalod M., Malissen B., Henri S. Dynamics and Transcriptomics of Skin Dendritic Cells and Macrophages in an Imiquimod-Induced, Biphasic Mouse Model of Psoriasis. J. Immunol. 2015;195:4953–4961. doi: 10.4049/jimmunol.1500551. [DOI] [PubMed] [Google Scholar]
- 93.Cupedo T., Crellin N.K., Papazian N., Rombouts E.J., Weijer K., Grogan J.L., Fibbe W.E., Cornelissen J.J., Spits H. Human fetal lymphoid tissue-inducer cells are interleukin 17-producing precursors to RORC+ CD127+ natural killer-like cells. Nat. Immunol. 2009;10:66–74. doi: 10.1038/ni.1668. [DOI] [PubMed] [Google Scholar]
- 94.Lo Presti E.L., De Gaetano A.D., Pioggia G., Gangemi S. Comprehensive Analysis of the ILCs and Unconventional T Cells in Virus Infection: Profiling and Dynamics Associated with COVID-19 Disease for a Future Monitoring System and Therapeutic Opportunities. Cells. 2022;11:542. doi: 10.3390/cells11030542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mashiko S., Mehta H., Bissonnette R., Sarfati M. Increased frequencies of basophils, type 2 innate lymphoid cells and Th2 cells in skin of patients with atopic dermatitis but not psoriasis. J. Dermatol. Sci. 2017;88:167–174. doi: 10.1016/j.jdermsci.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 96.Mjosberg J., Eidsmo L. Update on innate lymphoid cells in atopic and non-atopic inflammation in the airways and skin. Clin. Exp. Allergy. 2014;44:1033–1043. doi: 10.1111/cea.12353. [DOI] [PubMed] [Google Scholar]
- 97.Parodi M., Favoreel H., Candiano G., Gaggero S., Sivori S., Mingari M.C., Moretta L., Vitale M., Cantoni C. NKp44-NKp44 Ligand Interactions in the Regulation of Natural Killer Cells and Other Innate Lymphoid Cells in Humans. Front. Immunol. 2019;10:719. doi: 10.3389/fimmu.2019.00719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Teunissen M.B.M., Munneke J.M., Bernink J.H., Spuls P.I., Res P.C.M., Te Velde A., Cheuk S., Brouwer M.W.D., Menting S.P., Eidsmo L., et al. Composition of innate lymphoid cell subsets in the human skin: Enrichment of NCR(+) ILC3 in lesional skin and blood of psoriasis patients. J. Investig. Dermatol. 2014;134:2351–2360. doi: 10.1038/jid.2014.146. [DOI] [PubMed] [Google Scholar]
- 99.Villanova F., Flutter B., Tosi I., Grys K., Sreeneebus H., Perera G.K., Chapman A., Smith C.H., Di Meglio P., Nestle F.O. Characterization of innate lymphoid cells in human skin and blood demonstrates increase of NKp44+ ILC3 in psoriasis. J. Investig. Dermatol. 2014;134:984–991. doi: 10.1038/jid.2013.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Moretta L., Bottino C., Pende D., Mingari M.C., Biassoni R., Moretta A. Human natural killer cells: Their origin, receptors and function. Eur J. Immunol. 2002;32:1205–1211. doi: 10.1002/1521-4141(200205)32:5<1205::AID-IMMU1205>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 101.Belizario J.E., Neyra J.M., Setubal Destro Rodrigues M.F. When and how NK cell-induced programmed cell death benefits immunological protection against intracellular pathogen infection. Innate Immun. 2018;24:452–465. doi: 10.1177/1753425918800200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vissers W.H., Arndtz C.H., Muys L., Van Erp P.E., de Jong E.M., van de Kerkhof P.C. Memory effector (CD45RO+) and cytotoxic (CD8+) T cells appear early in the margin zone of spreading psoriatic lesions in contrast to cells expressing natural killer receptors, which appear late. Br. J. Dermatol. 2004;150:852–859. doi: 10.1111/j.1365-2133.2004.05863.x. [DOI] [PubMed] [Google Scholar]
- 103.Ottaviani C., Nasorri F., Bedini C., de Pita O., Girolomoni G., Cavani A. CD56brightCD16(-) NK cells accumulate in psoriatic skin in response to CXCL10 and CCL5 and exacerbate skin inflammation. Eur. J. Immunol. 2006;36:118–128. doi: 10.1002/eji.200535243. [DOI] [PubMed] [Google Scholar]
- 104.Chowdhury A.C., Chaurasia S., Mishra S.K., Aggarwal A., Misra R. IL-17 and IFN-gamma producing NK and gammadelta-T cells are preferentially expanded in synovial fluid of patients with reactive arthritis and undifferentiated spondyloarthritis. Clin. Immunol. 2017;183:207–212. doi: 10.1016/j.clim.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 105.Peng H., Tian Z. Diversity of tissue-resident NK cells. Semin Immunol. 2017;31:3–10. doi: 10.1016/j.smim.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 106.Barten R., Torkar M., Haude A., Trowsdale J., Wilson M.J. Divergent and convergent evolution of NK-cell receptors. Trends Immunol. 2001;22:52–57. doi: 10.1016/S1471-4906(00)01802-0. [DOI] [PubMed] [Google Scholar]
- 107.Rajagopalan S., Long E.O. KIR2DL4 (CD158d): An activation receptor for HLA-G. Front. Immunol. 2012;3:258. doi: 10.3389/fimmu.2012.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Girardi M. Immunosurveillance and immunoregulation by gammadelta T cells. J. Investig. Dermatol. 2006;126:25–31. doi: 10.1038/sj.jid.5700003. [DOI] [PubMed] [Google Scholar]
- 109.Laggner U., Di Meglio P., Perera G.K., Hundhausen C., Lacy K.E., Ali N., Smith C.H., Hayday A.C., Nickoloff B.J., Nestle F.O. Identification of a novel proinflammatory human skin-homing Vgamma9Vdelta2 T cell subset with a potential role in psoriasis. J. Immunol. 2011;187:2783–2793. doi: 10.4049/jimmunol.1100804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cai Y., Xue F., Quan C., Qu M., Liu N., Zhang Y., Fleming C., Hu X., Zhang H.G., Weichselbaum R., et al. A Critical Role of the IL-1beta-IL-1R Signaling Pathway in Skin Inflammation and Psoriasis Pathogenesis. J. Investig. Dermatol. 2019;139:146–156. doi: 10.1016/j.jid.2018.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hijnen D., Knol E.F., Gent Y.Y., Giovannone B., Beijn S.J., Kupper T.S., Bruijnzeel-Koomen C.A., Clark R.A. CD8(+) T cells in the lesional skin of atopic dermatitis and psoriasis patients are an important source of IFN-gamma, IL-13, IL-17, and IL-22. J. Investig. Dermatol. 2013;133:973–979. doi: 10.1038/jid.2012.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Nickoloff B.J., Wrone-Smith T. Injection of pre-psoriatic skin with CD4+ T cells induces psoriasis. Am. J. Pathol. 1999;155:145–158. doi: 10.1016/S0002-9440(10)65109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gunderson A.J., Mohammed J., Horvath F.J., Podolsky M.A., Anderson C.R., Glick A.B. CD8(+) T cells mediate RAS-induced psoriasis-like skin inflammation through IFN-gamma. J. Investig. Dermatol. 2013;133:955–963. doi: 10.1038/jid.2012.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Conrad C., Boyman O., Tonel G., Tun-Kyi A., Laggner U., de Fougerolles A., Kotelianski V., Gardner H., Nestle F.O. Alpha1beta1 integrin is crucial for accumulation of epidermal T cells and the development of psoriasis. Nat. Med. 2007;13:836–842. doi: 10.1038/nm1605. [DOI] [PubMed] [Google Scholar]
- 115.Di Meglio P., Villanova F., Navarini A.A., Mylonas A., Tosi I., Nestle F.O., Conrad C. Targeting CD8(+) T cells prevents psoriasis development. J. Allergy Clin. Immunol. 2016;138:274–276.e276. doi: 10.1016/j.jaci.2015.10.046. [DOI] [PubMed] [Google Scholar]
- 116.Rebora A. Cyclosporine A in psoriasis. Clin. Dermatol. 1991;9:515–522. doi: 10.1016/0738-081X(91)90081-U. [DOI] [PubMed] [Google Scholar]
- 117.Mondello M.R., Califano L., Cannavo S.P., Di Mauro D., Guarneri B., Magaudda L., Pergolizzi S., Santoro G., Vaccaro M. Psoriasis and cyclosporin: Immunohistochemical aspects of the basement membrane. Acta Derm. Venereol. Suppl. 1994;186:96–98. [PubMed] [Google Scholar]
- 118.Volpe E., Servant N., Zollinger R., Bogiatzi S.I., Hupe P., Barillot E., Soumelis V. A critical function for transforming growth factor-beta, interleukin 23 and proinflammatory cytokines in driving and modulating human T(H)-17 responses. Nat. Immunol. 2008;9:650–657. doi: 10.1038/ni.1613. [DOI] [PubMed] [Google Scholar]
- 119.Duhen T., Geiger R., Jarrossay D., Lanzavecchia A., Sallusto F. Production of interleukin 22 but not interleukin 17 by a subset of human skin-homing memory T cells. Nat. Immunol. 2009;10:857–863. doi: 10.1038/ni.1767. [DOI] [PubMed] [Google Scholar]
- 120.Sumaria N., Roediger B., Ng L.G., Qin J., Pinto R., Cavanagh L.L., Shklovskaya E., Fazekas de St Groth B., Triccas J.A., Weninger W. Cutaneous immunosurveillance by self-renewing dermal gammadelta T cells. J. Exp. Med. 2011;208:505–518. doi: 10.1084/jem.20101824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cosmi L., De Palma R., Santarlasci V., Maggi L., Capone M., Frosali F., Rodolico G., Querci V., Abbate G., Angeli R., et al. Human interleukin 17-producing cells originate from a CD161+CD4+ T cell precursor. J. Exp. Med. 2008;205:1903–1916. doi: 10.1084/jem.20080397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Nickoloff B.J., Bonish B., Huang B.B., Porcelli S.A. Characterization of a T cell line bearing natural killer receptors and capable of creating psoriasis in a SCID mouse model system. J. Dermatol. Sci. 2000;24:212–225. doi: 10.1016/S0923-1811(00)00120-1. [DOI] [PubMed] [Google Scholar]
- 123.Nickoloff B.J., Wrone-Smith T., Bonish B., Porcelli S.A. Response of murine and normal human skin to injection of allogeneic blood-derived psoriatic immunocytes: Detection of T cells expressing receptors typically present on natural killer cells, including CD94, CD158, and CD161. Arch. Dermatol. 1999;135:546–552. doi: 10.1001/archderm.135.5.546. [DOI] [PubMed] [Google Scholar]
- 124.Kriegsmann K., Kriegsmann M., von Bergwelt-Baildon M., Cremer M., Witzens-Harig M. NKT cells—New players in CAR cell immunotherapy? Eur. J. Haematol. 2018;101:750–757. doi: 10.1111/ejh.13170. [DOI] [PubMed] [Google Scholar]
- 125.Tecchio C., Cassatella M.A. Neutrophil-derived chemokines on the road to immunity. Semin. Immunol. 2016;28:119–128. doi: 10.1016/j.smim.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Leliefeld P.H., Koenderman L., Pillay J. How Neutrophils Shape Adaptive Immune Responses. Front. Immunol. 2015;6:471. doi: 10.3389/fimmu.2015.00471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rosales C., Lowell C.A., Schnoor M., Uribe-Querol E. Neutrophils: Their Role in Innate and Adaptive Immunity 2017. J. Immunol. Res. 2017;2017:9748345. doi: 10.1155/2017/9748345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Chiang C.C., Cheng W.J., Korinek M., Lin C.Y., Hwang T.L. Neutrophils in Psoriasis. Front. Immunol. 2019;10:2376. doi: 10.3389/fimmu.2019.02376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cannavo S.P., Riso G., Casciaro M., Di Salvo E., Gangemi S. Oxidative stress involvement in psoriasis: A systematic review. Free Radic. Res. 2019;53:829–840. doi: 10.1080/10715762.2019.1648800. [DOI] [PubMed] [Google Scholar]
- 130.Polat M., Bugdayci G., Kaya H., Oguzman H. Evaluation of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in Turkish patients with chronic plaque psoriasis. Acta. Dermatovenerol. Alp. Pannonica Adriat. 2017;26:97–100. doi: 10.15570/actaapa.2017.28. [DOI] [PubMed] [Google Scholar]
- 131.Mrowietz U. Neutrophils’ sexiness is independent of trendy fashion. Exp. Dermatol. 2017;26:312–313. doi: 10.1111/exd.13102. [DOI] [PubMed] [Google Scholar]
- 132.Alesci A., Pergolizzi S., Fumia A., Calabrò C., Lo Cascio P., Lauriano E.R. Mast cells in goldfish (Carassius auratus) gut: Immunohistochemical characterization. Acta Zool. 2022;114:166–171. doi: 10.1111/azo.12417. [DOI] [Google Scholar]
- 133.Lauriano E.R., Calo M., Silvestri G., Zaccone D., Pergolizzi S., Lo Cascio P. Mast cells in the intestine and gills of the sea bream, Sparus aurata, exposed to a polychlorinated biphenyl, PCB 126. Acta Histochem. 2012;114:166–171. doi: 10.1016/j.acthis.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 134.Mashiko S., Bouguermouh S., Rubio M., Baba N., Bissonnette R., Sarfati M. Human mast cells are major IL-22 producers in patients with psoriasis and atopic dermatitis. J. Allergy Clin. Immunol. 2015;136:351–359.e351. doi: 10.1016/j.jaci.2015.01.033. [DOI] [PubMed] [Google Scholar]
- 135.Lim D.S., Bewley A., Oon H.H. Psychological Profile of Patients with Psoriasis. Ann. Acad. Med. Singap. 2018;47:516–522. [PubMed] [Google Scholar]
- 136.Emons W.H., Meijer R.R., Denollet J. Negative affectivity and social inhibition in cardiovascular disease: Evaluating type-D personality and its assessment using item response theory. J. Psychosom. Res. 2007;63:27–39. doi: 10.1016/j.jpsychores.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 137.Mizara A., Papadopoulos L., McBride S.R. Core beliefs and psychological distress in patients with psoriasis and atopic eczema attending secondary care: The role of schemas in chronic skin disease. Br. J. Dermatol. 2012;166:986–993. doi: 10.1111/j.1365-2133.2011.10799.x. [DOI] [PubMed] [Google Scholar]
- 138.Dehghani F., Dehghani F., Kafaie P., Taghizadeh M.R. Alexithymia in different dermatologic patients. Asian J. Psychiatr. 2017;25:42–45. doi: 10.1016/j.ajp.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 139.DiBonaventura M., Carvalho A.V.E.d., Souza C.d.S., Squiassi H.B., Ferreira C.N. The association between psoriasis and health-related quality of life, work productivity, and healthcare resource use in Brazil. An. Bras. Dermatol. 2018;93:197–204. doi: 10.1590/abd1806-4841.20186069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Singer M., Bulled N., Ostrach B., Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389:941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- 141.Larsen M.H., Krogstad A.L., Aas E., Moum T., Wahl A.K. A telephone-based motivational interviewing intervention has positive effects on psoriasis severity and self-management: A randomized controlled trial. Br. J. Dermatol. 2014;171:1458–1469. doi: 10.1111/bjd.13363. [DOI] [PubMed] [Google Scholar]
- 142.Xiao Y., Zhang X., Luo D., Kuang Y., Zhu W., Chen X., Shen M. The efficacy of psychological interventions on psoriasis treatment: A systematic review and meta-analysis of randomized controlled trials. Psychol. Res. Behav. Manag. 2019;12:97–106. doi: 10.2147/PRBM.S195181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Esposito M., Saraceno R., Giunta A., Maccarone M., Chimenti S. An Italian study on psoriasis and depression. Dermatology. 2006;212:123–127. doi: 10.1159/000090652. [DOI] [PubMed] [Google Scholar]
- 144.Kurd S.K., Troxel A.B., Crits-Christoph P., Gelfand J.M. The risk of depression, anxiety, and suicidality in patients with psoriasis: A population-based cohort study. Arch. Dermatol. 2010;146:891–895. doi: 10.1001/archdermatol.2010.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Pancar Yuksel E., Durmus D., Sarisoy G. Perceived stress, life events, fatigue and temperament in patients with psoriasis. J. Int. Med. Res. 2019;47:4284–4291. doi: 10.1177/0300060519862658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Dowlati Y., Herrmann N., Swardfager W., Liu H., Sham L., Reim E.K., Lanctot K.L. A meta-analysis of cytokines in major depression. Biol. Psychiatry. 2010;67:446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 147.Jokela M., Virtanen M., Batty G.D., Kivimaki M. Inflammation and Specific Symptoms of Depression. JAMA Psychiatry. 2016;73:87–88. doi: 10.1001/jamapsychiatry.2015.1977. [DOI] [PubMed] [Google Scholar]
- 148.Catena-Dell’Osso M., Bellantuono C., Consoli G., Baroni S., Rotella F., Marazziti D. Inflammatory and neurodegenerative pathways in depression: A new avenue for antidepressant development? Curr. Med. Chem. 2011;18:245–255. doi: 10.2174/092986711794088353. [DOI] [PubMed] [Google Scholar]
- 149.Capuron L., Miller A.H. Immune system to brain signaling: Neuropsychopharmacological implications. Pharmacol. Ther. 2011;130:226–238. doi: 10.1016/j.pharmthera.2011.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Bortolato B., Carvalho A.F., Soczynska J.K., Perini G.I., McIntyre R.S. The Involvement of TNF-alpha in Cognitive Dysfunction Associated with Major Depressive Disorder: An Opportunity for Domain Specific Treatments. Curr. Neuropharmacol. 2015;13:558–576. doi: 10.2174/1570159X13666150630171433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gonzalez-Parra S., Dauden E. Psoriasis and Depression: The Role of Inflammation. Actas Dermosifiliogr. 2019;110:12–19. doi: 10.1016/j.ad.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 152.Arborelius L., Owens M.J., Plotsky P.M., Nemeroff C.B. The role of corticotropin-releasing factor in depression and anxiety disorders. J. Endocrinol. 1999;160:1–12. doi: 10.1677/joe.0.1600001. [DOI] [PubMed] [Google Scholar]
- 153.Quevedo M.E., Slominski A., Pinto W., Wei E., Wortsman J. Pleiotropic effects of corticotropin releasing hormone on normal human skin keratinocytes. In Vitro Cell Dev. Biol. Anim. 2001;37:50–54. doi: 10.1290/1071-2690(2001)037<0050:PEOCRH>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 154.Jacobson L., Sapolsky R. The role of the hippocampus in feedback regulation of the hypothalamic-pituitary-adrenocortical axis. Endocr. Rev. 1991;12:118–134. doi: 10.1210/edrv-12-2-118. [DOI] [PubMed] [Google Scholar]
- 155.Beurel E., Lowell J.A. Th17 cells in depression. Brain. Behav. Immun. 2018;69:28–34. doi: 10.1016/j.bbi.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Davami M.H., Baharlou R., Ahmadi Vasmehjani A., Ghanizadeh A., Keshtkar M., Dezhkam I., Atashzar M.R. Elevated IL-17 and TGF-beta Serum Levels: A Positive Correlation between T-helper 17 Cell-Related Pro-Inflammatory Responses with Major Depressive Disorder. Basic Clin. Neurosci. 2016;7:137–142. doi: 10.15412/J.BCN.03070207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sahi F.M., Masood A., Danawar N.A., Mekaiel A., Malik B.H. Association Between Psoriasis and Depression: A Traditional Review. Cureus. 2020;12:e9708. doi: 10.7759/cureus.9708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Moynihan J., Rieder E., Tausk F. Psychoneuroimmunology: The example of psoriasis. G Ital. Dermatol. Venereol. 2010;145:221–228. [PMC free article] [PubMed] [Google Scholar]
- 159.Zaccone G., Lauriano E.R., Silvestri G., Kenaley C., Icardo J.M., Pergolizzi S., Alesci A., Sengar M., Kuciel M., Gopesh A. Comparative neurochemical features of the innervation patterns of the gut of the basal actinopterygian, Lepisosteus oculatus, and the euteleost, Clarias batrachus. Acta Zool. 2015;96:127–139. doi: 10.1111/azo.12059. [DOI] [Google Scholar]
- 160.Lauriano E.R., Żuwała K., Kuciel M., Budzik K.A., Capillo G., Alesci A., Pergolizzi S., Dugo G., Zaccone G. Confocal immunohistochemistry of the dermal glands and evolutionary considerations in the caecilian, Typhlonectes natans(Amphibia: Gymnophiona) Acta Zool. 2016;97:154–164. doi: 10.1111/azo.12112. [DOI] [Google Scholar]
- 161.Lauriano E.R., Icardo J.M., Zaccone D., Kuciel M., Satora L., Alesci A., Alfa M., Zaccone G. Expression patterns and quantitative assessment of neurochemical markers in the lung of the gray bichir, Polypterus senegalus (Cuvier, 1829) Acta Histochem. 2015;117:738–746. doi: 10.1016/j.acthis.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 162.Zaccone D., Icardo J.M., Kuciel M., Alesci A., Pergolizzi S., Satora L., Lauriano E.R., Zaccone G. Polymorphous granular cells in the lung of the primitive fish, the bichir Polypterus senegalus. Acta Zool. 2017;98:13–19. doi: 10.1111/azo.12145. [DOI] [Google Scholar]
- 163.Zaccone G., Lauriano E.R., Kuciel M., Capillo G., Pergolizzi S., Alesci A., Ishimatsu A., Ip Y.K., Icardo J.M. Identification and distribution of neuronal nitric oxide synthase and neurochemical markers in the neuroepithelial cells of the gill and the skin in the giant mudskipper, Periophthalmodon schlosseri. Zoology. 2017;125:41–52. doi: 10.1016/j.zool.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 164.Maina J.N., Icardo J.M., Zaccone G., Aragona M., Lauriano E.R., Alesci A., Albano M., Guerrera M.C., Germana A., Fernandes J.M.O., et al. Immunohistochemical and ultrastructural study of the immune cell system and epithelial surfaces of the respiratory organs in the bimodally-breathing African sharptooth catfish (Clarias gariepinus Burchell, 1822) Anat. Rec. 2022 doi: 10.1002/ar.24896. [DOI] [PubMed] [Google Scholar]
- 165.Chalinee R., Tewin T. Psoriasis: A review of the role of serotonergic system. Afr. J. Biotechnol. 2010;9:1528–1534. doi: 10.5897/AJB10.020. [DOI] [Google Scholar]
- 166.Shajib M.S., Khan W.I. The role of serotonin and its receptors in activation of immune responses and inflammation. Acta Physiol. 2015;213:561–574. doi: 10.1111/apha.12430. [DOI] [PubMed] [Google Scholar]
- 167.Capuron L., Neurauter G., Musselman D.L., Lawson D.H., Nemeroff C.B., Fuchs D., Miller A.H. Interferon-alpha-induced changes in tryptophan metabolism. relationship to depression and paroxetine treatment. Biol. Psychiatry. 2003;54:906–914. doi: 10.1016/S0006-3223(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 168.Muller N., Schwarz M.J. The immune-mediated alteration of serotonin and glutamate: Towards an integrated view of depression. Mol. Psychiatry. 2007;12:988–1000. doi: 10.1038/sj.mp.4002006. [DOI] [PubMed] [Google Scholar]
- 169.Wang J., Dunn A.J. Mouse interleukin-6 stimulates the HPA axis and increases brain tryptophan and serotonin metabolism. Neurochem. Int. 1998;33:143–154. doi: 10.1016/S0197-0186(98)00016-3. [DOI] [PubMed] [Google Scholar]
- 170.Mori T., Kabashima K., Fukamachi S., Kuroda E., Sakabe J., Kobayashi M., Nakajima S., Nakano K., Tanaka Y., Matsushita S., et al. D1-like dopamine receptors antagonist inhibits cutaneous immune reactions mediated by Th2 and mast cells. J. Dermatol. Sci. 2013;71:37–44. doi: 10.1016/j.jdermsci.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 171.Wardhana M., Windari M., Puspasari N., Suryawati N. Role of Serotonin and Dopamine in Psoriasis: A Case-Control Study. Open Access Maced. J. Med. Sci. 2019;7:1138–1142. doi: 10.3889/oamjms.2019.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Portou M.J., Baker D., Abraham D., Tsui J. The innate immune system, toll-like receptors and dermal wound healing: A review. Vascul. Pharmacol. 2015;71:31–36. doi: 10.1016/j.vph.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 173.Rosenblat J.D., Cha D.S., Mansur R.B., McIntyre R.S. Inflamed moods: A review of the interactions between inflammation and mood disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2014;53:23–34. doi: 10.1016/j.pnpbp.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 174.Ginhoux F., Jung S. Monocytes and macrophages: Developmental pathways and tissue homeostasis. Nat. Rev. Immunol. 2014;14:392–404. doi: 10.1038/nri3671. [DOI] [PubMed] [Google Scholar]
- 175.Maes M., Van der Planken M., Stevens W.J., Peeters D., DeClerck L.S., Bridts C.H., Schotte C., Cosyns P. Leukocytosis, monocytosis and neutrophilia: Hallmarks of severe depression. J. Psychiatr. Res. 1992;26:125–134. doi: 10.1016/0022-3956(92)90004-8. [DOI] [PubMed] [Google Scholar]
- 176.Mueller S.N., Mackay L.K. Tissue-resident memory T cells: Local specialists in immune defence. Nat. Rev. Immunol. 2016;16:79–89. doi: 10.1038/nri.2015.3. [DOI] [PubMed] [Google Scholar]
- 177.Talamonti M., Galluzzo M., Chiricozzi A., Quaglino P., Fabbrocini G., Gisondi P., Marzano A.V., Potenza C., Conti A., Parodi A., et al. Management of biological therapies for chronic plaque psoriasis during COVID-19 emergency in Italy. J. Eur. Acad. Dermatol. Venereol. 2020;34:e770–e772. doi: 10.1111/jdv.16841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Geng W., Zhao J., Fu J., Zhang H., Qiao S. Efficacy of several biological therapies for treating moderate to severe psoriasis: A network meta-analysis. Exp. Ther. Med. 2018;16:5085–5095. doi: 10.3892/etm.2018.6859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ronholt K., Iversen L. Old and New Biological Therapies for Psoriasis. Int. J. Mol. Sci. 2017;18:2297. doi: 10.3390/ijms18112297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sbidian E., Chaimani A., Afach S., Doney L., Dressler C., Hua C., Mazaud C., Phan C., Hughes C., Riddle D., et al. Systemic pharmacological treatments for chronic plaque psoriasis: A network meta-analysis. Cochrane Database Syst. Rev. 2020;1:CD011535. doi: 10.1002/14651858.CD011535.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Huang T.H., Lin C.F., Alalaiwe A., Yang S.C., Fang J.Y. Apoptotic or Antiproliferative Activity of Natural Products against Keratinocytes for the Treatment of Psoriasis. Int. J. Mol. Sci. 2019;20:2558. doi: 10.3390/ijms20102558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Fumia A., Cicero N., Gitto M., Nicosia N., Alesci A. Role of nutraceuticals on neurodegenerative diseases: Neuroprotective and immunomodulant activity. Nat. Prod. Res. 2021:1–18. doi: 10.1080/14786419.2021.2020265. [DOI] [PubMed] [Google Scholar]
- 183.Alesci A., Fumia A., Lo Cascio P., Miller A., Cicero N. Immunostimulant and Antidepressant Effect of Natural Compounds in the Management of COVID-19 Symptoms. J. Am. Coll. Nutr. 2021:1–15. doi: 10.1080/07315724.2021.1965503. [DOI] [PubMed] [Google Scholar]
- 184.Bonesi M., Loizzo M.R., Provenzano E., Menichini F., Tundis R. Anti-Psoriasis Agents from Natural Plant Sources. Curr Med. Chem. 2016;23:1250–1267. doi: 10.2174/0929867323666160321121819. [DOI] [PubMed] [Google Scholar]
- 185.Alessio A., Pergolizzi S., Gervasi T., Aragona M., Lo Cascio P., Cicero N., Lauriano E.R. Biological effect of astaxanthin on alcohol-induced gut damage in Carassius auratus used as experimental model. Nat. Prod. Res. 2020;35:5737–5743. doi: 10.1080/14786419.2020.1830396. [DOI] [PubMed] [Google Scholar]
- 186.Alesci A., Salvo A., Lauriano E.R., Gervasi T., Palombieri D., Bruno M., Pergolizzi S., Cicero N. Production and extraction of astaxanthin from Phaffia rhodozyma and its biological effect on alcohol-induced renal hypoxia in Carassius auratus. Nat. Prod. Res. 2015;29:1122–1126. doi: 10.1080/14786419.2014.979417. [DOI] [PubMed] [Google Scholar]
- 187.Miroddi M., Navarra M., Calapai F., Mancari F., Giofre S.V., Gangemi S., Calapai G. Review of Clinical Pharmacology of Aloe vera L. in the Treatment of Psoriasis. Phytother Res. 2015;29:648–655. doi: 10.1002/ptr.5316. [DOI] [PubMed] [Google Scholar]
- 188.Leng H., Pu L., Xu L., Shi X., Ji J., Chen K. Effects of aloe polysaccharide, a polysaccharide extracted from Aloe vera, on TNFalphainduced HaCaT cell proliferation and the underlying mechanism in psoriasis. Mol. Med. Rep. 2018;18:3537–3543. doi: 10.3892/mmr.2018.9319. [DOI] [PubMed] [Google Scholar]
- 189.Niculet E., Radaschin D.S., Nastase F., Draganescu M., Baroiu L., Miulescu M., Arbune M., Tatu A.L. Influence of phytochemicals in induced psoriasis (Review) Exp. Ther. Med. 2020;20:3421–3424. doi: 10.3892/etm.2020.9013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Foadoddini M., Alinejad Mofrad S. Effect of Aloe vera Extract on Depression in People with Prediabetes. Modern Care J. 2020;17:e100927. doi: 10.5812/modernc.100927. [DOI] [Google Scholar]
- 191.Maurya A.K., Amrita B.Y., Pandey D.K. To examine antidepressant impact of Aloe Vera and Fluoxetine in Mice. Eur. J. Mol. Clin. Med. 2021;8:3612–3619. [Google Scholar]
- 192.Chen J., Wu G., Zhu C., Wu Y., Wei R., Ma Q. Structurally Diverse Flavonoids from Citrus medica L. Var. sarcodactylis Swingle and Their Multiple Bioactivities: A Review. J. Food Nutr. Res. 2022;10:81–87. doi: 10.12691/jfnr-10-2-1. [DOI] [Google Scholar]
- 193.Cirmi S., Bisignano C., Mandalari G., Navarra M. Anti-infective potential of Citrus bergamia Risso et Poiteau (bergamot) derivatives: A systematic review. Phytother. Res. 2016;30:1404–1411. doi: 10.1002/ptr.5646. [DOI] [PubMed] [Google Scholar]
- 194.Mannucci C., Navarra M., Calapai F., Squeri R., Gangemi S., Calapai G. Clinical Pharmacology of Citrus bergamia: A Systematic Review. Phytother. Res. 2017;31:27–39. doi: 10.1002/ptr.5734. [DOI] [PubMed] [Google Scholar]
- 195.Valkova S. UVB phototherapeutic modalities. Comparison of two treatments for chronic plaque psoriasis. Acta Dermatovenerol. Alp. Pannonica Adriat. 2007;16:26–30. [PubMed] [Google Scholar]
- 196.Forlot P., Pevet P. Bergamot (Citrus bergamia Risso et Poiteau) essential oil: Biological properties, cosmetic and medical use. A review. J. Essent. Oil Res. 2012;24:195–201. doi: 10.1080/10412905.2012.659527. [DOI] [Google Scholar]
- 197.Valussi M., Donelli D., Firenzuoli F., Antonelli M. Bergamot Oil: Botany, Production, Pharmacology. Encyclopedia. 2021;1:152–176. doi: 10.3390/encyclopedia1010016. [DOI] [Google Scholar]
- 198.Alesci A., Aragona M., Cicero N., Lauriano E.R. Can neutraceuticals assist treatment and improve COVID-19 symptoms? Nat. Prod. Res. 2021 doi: 10.1080/14786419.2021.1914032. [DOI] [PubMed] [Google Scholar]
- 199.Lee Y.K., Hwang J.T., Kwon D.Y., Surh Y.J., Park O.J. Induction of apoptosis by quercetin is mediated through AMPKalpha1/ASK1/p38 pathway. Cancer Lett. 2010;292:228–236. doi: 10.1016/j.canlet.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 200.Shen S.C., Lee W.R., Yang L.Y., Tsai H.H., Yang L.L., Chen Y.C. Quercetin enhancement of arsenic-induced apoptosis via stimulating ROS-dependent p53 protein ubiquitination in human HaCaT keratinocytes. Exp. Dermatol. 2012;21:370–375. doi: 10.1111/j.1600-0625.2012.01479.x. [DOI] [PubMed] [Google Scholar]
- 201.Mestry M., Rane M., Bajaj A. Commiphora mukul and Quercetin Loaded Liposphere Gel: Potential Treatment for Psoriasis. Indian J. Pharm. Educ. Res. 2020;54:654–667. doi: 10.5530/ijper.54.3.115. [DOI] [Google Scholar]
- 202.Chen H., Lu C., Liu H., Wang M., Zhao H., Yan Y., Han L. Quercetin ameliorates imiquimod-induced psoriasis-like skin inflammation in mice via the NF-kappaB pathway. Int. Immunopharmacol. 2017;48:110–117. doi: 10.1016/j.intimp.2017.04.022. [DOI] [PubMed] [Google Scholar]
- 203.Samad N., Saleem A., Yasmin F., Shehzad M.A. Quercetin protects against stress-induced anxiety- and depression-like behavior and improves memory in male mice. Physiol. Res. 2018;67:795–808. doi: 10.33549/physiolres.933776. [DOI] [PubMed] [Google Scholar]
- 204.Kosari-Nasab M., Shokouhi G., Ghorbanihaghjo A., Mesgari-Abbasi M., Salari A.A. Quercetin mitigates anxiety-like behavior and normalizes hypothalamus-pituitary-adrenal axis function in a mouse model of mild traumatic brain injury. Behav. Pharmacol. 2019;30:282–289. doi: 10.1097/FBP.0000000000000480. [DOI] [PubMed] [Google Scholar]
- 205.Zhao Q., Chen X.Y., Martin C. Scutellaria baicalensis, the golden herb from the garden of Chinese medicinal plants. Sci. Bull. 2016;61:1391–1398. doi: 10.1007/s11434-016-1136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Huang K.F., Ma K.H., Liu P.S., Chen B.W., Chueh S.H. Baicalein increases keratin 1 and 10 expression in HaCaT keratinocytes via TRPV4 receptor activation. Exp. Dermatol. 2016;25:623–629. doi: 10.1111/exd.13024. [DOI] [PubMed] [Google Scholar]
- 207.Yan W.J., Ma X.C., Gao X.Y., Xue X.H., Zhang S.Q. Latest research progress in the correlation between baicalein and breast cancer invasion and metastasis. Mol. Clin. Oncol. 2016;4:472–476. doi: 10.3892/mco.2016.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Dinda B., Dinda S., DasSharma S., Banik R., Chakraborty A., Dinda M. Therapeutic potentials of baicalin and its aglycone, baicalein against inflammatory disorders. Eur. J. Med. Chem. 2017;131:68–80. doi: 10.1016/j.ejmech.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 209.Lee B., Sur B., Park J., Kim S.H., Kwon S., Yeom M., Shim I., Lee H., Hahm D.H. Chronic administration of baicalein decreases depression-like behavior induced by repeated restraint stress in rats. Korean J. Physiol. Pharmacol. 2013;17:393–403. doi: 10.4196/kjpp.2013.17.5.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zhao X., Kong D., Zhou Q., Wei G., Song J., Liang Y., Du G. Baicalein alleviates depression-like behavior in rotenone- induced Parkinson’s disease model in mice through activating the BDNF/TrkB/CREB pathway. Biomed. Pharmacother. 2021;140:111556. doi: 10.1016/j.biopha.2021.111556. [DOI] [PubMed] [Google Scholar]
- 211.Zielinska A., Alves H., Marques V., Durazzo A., Lucarini M., Alves T.F., Morsink M., Willemen N., Eder P., Chaud M.V., et al. Properties, Extraction Methods, and Delivery Systems for Curcumin as a Natural Source of Beneficial Health Effects. Medicina. 2020;56:336. doi: 10.3390/medicina56070336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Sun J., Zhao Y., Hu J. Curcumin inhibits imiquimod-induced psoriasis-like inflammation by inhibiting IL-1beta and IL-6 production in mice. PLoS ONE. 2013;8:e67078. doi: 10.1371/journal.pone.0067078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Nardo V.D., Gianfaldoni S., Tchernev G., Wollina U., Barygina V., Lotti J., Daaboul F., Lotti T. Use of Curcumin in Psoriasis. Open Access Maced. J. Med. Sci. 2018;6:218–220. doi: 10.3889/oamjms.2018.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Tizabi Y., Hurley L.L., Qualls Z., Akinfiresoye L. Relevance of the anti-inflammatory properties of curcumin in neurodegenerative diseases and depression. Molecules. 2014;19:20864–20879. doi: 10.3390/molecules191220864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Polese B., Zhang H., Thurairajah B., King I.L. Innate Lymphocytes in Psoriasis. Front. Immunol. 2020;11:242. doi: 10.3389/fimmu.2020.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Alesci A., Nicosia N., Fumia A., Giorgianni F., Santini A., Cicero N. Resveratrol and Immune Cells: A Link to Improve Human Health. Molecules. 2022;27:424. doi: 10.3390/molecules27020424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Di Stefano V., Avellone G., Pitonzo R., Capocchiano V.G., Mazza A., Cicero N., Dugo G. Natural co-occurrence of ochratoxin A, ochratoxin B and aflatoxins in Sicilian red wines. Food Addit. Contam. Part A Chem. Anal. Control Expo. Risk Assess. 2015;32:1343–1351. doi: 10.1080/19440049.2015.1055521. [DOI] [PubMed] [Google Scholar]
- 218.Rigon R.B., Fachinetti N., Severino P., Durazzo A., Lucarini M., Atanasov A.G., El Mamouni S., Chorilli M., Santini A., Souto E.B. Quantification of Trans-Resveratrol-Loaded Solid Lipid Nanoparticles by a Validated Reverse-Phase HPLC Photodiode Array. Appl. Sci. 2019;9:4961. doi: 10.3390/app9224961. [DOI] [Google Scholar]
- 219.Yeung A.W.K., Aggarwal B.B., Orhan I.E., Barreca D., Battino M., Belwal T., Bishayee A., Daglia M., Devkota H.P., Echeverria J., et al. Resveratrol, a popular dietary supplement for human and animal health: Quantitative research literature analysis-a review. Anim. Sci. Pap. Rep. 2019;37:103–118. [Google Scholar]
- 220.Oliveira A.L.B., Monteiro V.V.S., Navegantes-Lima K.C., Reis J.F., Gomes R.S., Rodrigues D.V.S., Gaspar S.L.F., Monteiro M.C. Resveratrol Role in Autoimmune Disease-A Mini-Review. Nutrients. 2017;9:1306. doi: 10.3390/nu9121306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Khurana B., Arora D., Narang R.K. QbD based exploration of resveratrol loaded polymeric micelles based carbomer gel for topical treatment of plaque psoriasis: In vitro, ex vivo and in vivo studies. J. Drug Deliv. Sci. Technol. 2020;59:101901. doi: 10.1016/j.jddst.2020.101901. [DOI] [Google Scholar]
- 222.Zhu X., Li W., Li Y., Xu W., Yuan Y., Zheng V., Zhang H., O’Donnell J.M., Xu Y., Yin X. The antidepressant- and anxiolytic-like effects of resveratrol: Involvement of phosphodiesterase-4D inhibition. Neuropharmacology. 2019;153:20–31. doi: 10.1016/j.neuropharm.2019.04.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.