Abstract
An association has been found between cannabis use disorder (CUD) and violence in several clinical populations, including veterans with posttraumatic stress disorder (PTSD), and there is evidence that CUD has been increasing among veterans since September 11, 2001. There is also evidence that some veterans may be attempting to self-medicate psychological problems including PTSD and aggression with cannabis, despite the lack of safety and efficacy data supporting this use. To date, however, the association between CUD and aggression has yet to be examined in a large, non-clinic sample of veterans. The present study examined the association between cannabis use disorder, anger, aggressive urges, and difficulty controlling violence in a large sample of Iraq/Afghanistan-era veterans (N = 3,028). Results of multivariate logistic regressions indicated that current CUD was significantly positively associated with difficulty managing anger (OR = 2.93, p < 0.05), aggressive impulses/urges (OR = 2.74, p < 0.05), and problems controlling violence in past 30 days (OR = 2.71, p < 0.05) even accounting for demographic variables, comorbid symptoms of depression and PTSD, and co-morbid alcohol and substance use disorders. Lifetime CUD was also uniquely associated with problems controlling violence in the past 30 days (OR = 1.64, p < 0.05), but was not significantly associated with difficulty managing anger or aggressive impulses/urges. Findings indicated that the association between CUD and aggression needs to be considered in treatment planning for both CUD and problems managing anger and aggressive urges, and point to a critical need to disentangle the mechanism of the association between CUD and violence in veterans.
Keywords: cannabis use disorder, anger, aggression, violence, veterans
Since cannabis emerged as a recreational drug in the United States in the 1930s, the national narrative around the drug has swung dramatically from its vilification as a “killer weed” that incites violence, to a drug that leads to the chronic passivity of an “amotivational syndrome” (Himmelstein, 1983), to a potential therapeutic agent for a range of conditions including posttraumatic stress disorder (PTSD; Orsolini et al., 2019). As we enter the third decade of the 21st century, the stakes have never been higher for an accurate understanding of the relationship between cannabis use on health and psychological functioning, particularly in military veterans. Rates of cannabis use disorders (CUD) in veterans receiving medical care through the Veterans Affairs Health Care System (VA) have increased by more than 50% between 2002 and 2009 (Bonn-Miller et al., 2012). Recent research has found that cannabis use is associated with increased aggression in clinical populations (Dugré et al., 2017; Kolla & Mishra, 2018; Moore & Stuart, 2005), including veterans receiving treatment for PTSD (Wilkinson et al, 2015).
Controlling anger and aggressive urges is among the most prevalent post-deployment concerns reported by Iraq and Afghanistan-era combat veterans (Sayer et al., 2010; Sippel et al., 2016), and anger and aggression have consistently been identified as critical concerns for those with PTSD (Novaco & Chemtob, 2015; Orth & Wieland, 2006; Van Voorhees et al., 2018; Van Voorhees et al., 2016). Not surprisingly, there is evidence that veterans with PTSD and others who struggle with aggression may use cannabis to self-medicate their symptoms, despite the lack of evidence of its safety or efficacy for this purpose (Orsolini et al., 2019; Steenkamp et al., 2017; Wilkinson et al., 2016). Specifically, at least one study has found support that individuals with CUD reported using the drug to “decrease aggression” (Arendt et al., 2007), and a recent study of 147 veterans who had been deployed post September 11, 2001 found that PTSD was among the most commonly reported problems for which veterans were likely to endorse medicinal cannabis use. In fact, among these veterans, those who said they use cannabis for medicinal purposes were three times more likely to have a diagnosis of PTSD than were those who reported using the drug recreationally (Metrik et al., 2018). Evidence suggests, however, that cannabis use after PTSD treatment may actually worsen PTSD symptoms and aggression. For example, Wilkinson and colleagues (2015) found that among veterans who received intensive PTSD treatment, new initiation of cannabis use post-treatment was associated with increased PTSD symptoms and higher levels of violence compared to those who never used or stopped cannabis use after PTSD treatment.
Taken together, studies suggest that cannabis use is on the rise among veterans (Bonn-Miller et al., 2012), and that at least some veterans may be using cannabis to self-medicate psychological symptoms including PTSD (Metrik et al., 2018) and aggression (Arendt et al., 2007). Although there is evidence of a relationship between cannabis use and aggression in clinical populations (Dugré et al., 2017; Kolla & Mishra, 2018; Moore & Stuart, 2005) and in veterans being treated for PTSD (Wilkinson et al, 2015), the link between CUD and a more general sample of current-era military veterans has not yet been examined. The current study sought to examine the associations between CUD and anger, aggressive urges, and difficulty controlling violence in a large sample of Iraq/Afghanistan-era veterans. Based on prior research linking cannabis use and violence in clinical populations (Dugré et al., 2017; Moore & Stuart, 2005; Kolla & Mishra, 2018; Wilkinson et al, 2015), and the high rates of both in the Iraq/Afghanistan-era veteran population (Bonn-Miller et al., 2012; Hoge et al., 2004; Sundin et al., 2014), we predicted that CUD would be associated with anger, aggressive urges, and violence, even after accounting for demographic variables, combat exposure, history of incarceration, other substance use disorders, and comorbid psychopathology.
Methods
Participants and procedures
Participants included 3,028 Iraq/Afghanistan-era veterans who participated between 2005 and 2015 in a multi-site study of Post-Deployment Mental Health led by the Department of Veterans Affairs’ (VA) Mid-Atlantic Mental Illness, Research, Education, and Clinical Center (MIRECC). Study procedures have been described elsewhere (Brancu et al., 2017; Kimbrel et al., 2014). To be eligible, participants must have served in the U.S. military after September 11, 2001. Veterans were recruited through targeted mailings, advertisements, and clinician referrals. The local institutional review boards at each participating site approved the study protocol. All participants provided written informed consent prior to enrollment. Study procedures consisted of a diagnostic clinical interview and completion of a battery of self-report questionnaires.
Measures
Demographic variables including age, sex, race, level of education (coded as either “high school or less” or “more than high school”), and marital status (coded as “married/living as married” or “divorced/never married/other”) were collected. Highest military rank (coded as “enlisted” or “officer”) and history of incarceration (“yes” or “no”) were also reported.
The Structured Clinical Interview for DSM-IV-TR (SCID; First et al., 1994) was used to diagnose current and lifetime psychiatric disorders, based DSM-IV-TR criteria. Clinical interviewers completed a SCID training program and received ongoing supervision from experienced clinicians. Rater observations were conducted throughout the study to evaluate and correct any rater drift. Interviewers demonstrated excellent reliability (Fleiss’ kappa = 0.94) when scoring a series of seven training videos. Substance dependence and abuse diagnoses were combined into a single substance use disorder variable for each substance. For example, participants who met criteria for either cannabis dependence or cannabis abuse were coded as having cannabis use disorder. The same was done for alcohol use disorder and other substance use disorders.
The Symptom Checklist-90-R (SCL-90-R; Derogatis, 1994) was used to assess difficulty managing anger and aggressive impulses. Prior research has found that the six-item hostility subscale of the SCL-90-R taps two dissociable constructs reflecting “difficulty managing anger” and “aggressive impulses and urges” (Elbogen et al., 2010). Difficulty managing anger includes 4 items: “feeling easily annoyed or irritated;” “temper outbursts that you could not control;” “getting into frequent arguments;” and “shouting or throwing things.” Aggressive impulses and urges includes 2 items: “having urges to break or smash things;” “having urges to beat, injure, or harm someone.” Participants rated how distressing each item had been over the past weeks on a 5-point Likert scale (0 = “not at all”; 1 = “a little bit”; 2 = “moderately”; 3 = “quite a bit”; 4 = “extremely”). Mean scores were calculated. In order to be able to make comparisons between participants with moderate to severe difficulties versus those with little or none, participants were divided into dichotomous groups for each construct (0 = not at all/a little bit; 1 = moderately/quite a bit/extremely).
Difficulty controlling violence was assessed with the question, “During the past 30 days, have you had trouble controlling violent behavior (that is, hitting someone)?” (0 = no; 1 = yes). This item has been used in prior research with veterans (Crawford et al., 2007; Elbogen et al, 2010).
The Beck Depression Inventory-II (BDI-II; Beck et al., 1996) was used to assess the severity of depressive symptoms during the past two weeks. The BDI-II consists of 21 items that are rated from 0 to 3, with higher scores indicating greater severity.
The Davidson Trauma Scale (DTS; Davidson et al., 1997) was used to assess PTSD symptom severity. The DTS assesses the 17 symptoms of PTSD, based on the DSM-IV criteria. Participants rate the frequency and severity of each item on a 0 to 4 scale based on how they felt during the past week regarding their most bothersome traumatic event.
The Combat Exposure Scale (CES; Keane et al., 1989) was used to assess combat exposure. The CES consists of 7 self-report items that are rated on a 5-point scale to reflect the frequency, duration, or percentage of combat exposure.
Data analysis plan
All analyses were conducted using SAS 9.4. Descriptive statistics were calculated to characterize demographic, substance use, and psychological characteristics of participants. Chi-square and t-tests were used to compare demographic, substance use, and psychological characteristics of individuals with lifetime CUD and those without. Bivariate logistic regressions were conducted to examine the relationship between the three anger/aggression variables (difficulty managing anger, aggressive impulses/urges, and problems controlling violence in the past 30 days), CUD, and demographics, military rank, combat exposure, history of incarceration, clinical covariates (PTSD and depression severity), alcohol use disorder, and other drug use disorder. Next, multivariate logistic regression models predicting each anger/aggression variable were conducted. Continuous measures of depression (BDI-II) and PTSD (DTS) were used to examine the impact of symptom severity on these variables rather than the presence of diagnosis.
Results
Descriptive statistics are presented in Table 1. Demographic associations with lifetime CUD included younger age, male sex, lower education, unmarried marital status, and enlisted rank. Persons with lifetime CUD were also more likely to report a history of incarceration, meet criteria for current alcohol use disorder (AUD), and have more severe depression and PTSD symptoms.
Table 1.
Demographic, Substance Use, and Clinical Characteristics by Lifetime CUD Status
| Full Sample (n=3028) | No Cannabis Use Disorder (n=2705) | Cannabis Use Disorder (n=323) | p | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Characteristic | N | (%) | N | (%) | N | (%) | |
| Race | n.s. | ||||||
| Caucasian | 1447 | (47.8%) | 1296 | (47.9%) | 151 | (46.8%) | |
| African-American | 1451 | (47.9%) | 1289 | (47.7%) | 162 | (50.2%) | |
| Other | 130 | (4.3%) | 120 | (4.4%) | 10 | (3.1%) | |
| Sex | .0001 | ||||||
| Male | 2406 | (79.5%) | 2122 | (78.5%) | 284 | (87.9%) | |
| Female | 622 | (20.5%) | 583 | (21.6%) | 39 | (12.07%) | |
| Education | .0061 | ||||||
| High School or less | 1220 | (40.3%) | 1067 | (39.5%) | 153 | (47.4%) | |
| More than high school | 1808 | (59.7%) | 1638 | (60.6%) | 150 | (52.6%) | |
| Marital Status | .016 | ||||||
| Divorced/Never Married/Other | 1411 | (46.6%) | 1240 | (45.8%) | 171 | (52.9%) | |
| Married/Living as married | 1617 | (53.4%) | 1465 | (54.2%) | 152 | (47.1%) | |
| Highest Military Rank | .0001 | ||||||
| Enlisted | 2791 | (92.2%) | 2475 | (91.5%) | 316 | (97.8%) | |
| Officer | 237 | (7.8%) | 230 | (8.5%) | 7 | (2.2%) | |
| History of incarceration | 680 | (22.5%) | 530 | (19.6%) | 150 | (46%) | .0001 |
| Current Depression | 603 | (19.9%) | 534 | (19.7%) | 69 | (21.4%) | n.s. |
| Current PTSD | 926 | (30.6%) | 821 | (30.4%) | 105 | (32.5%) | n.s. |
| Current Alcohol Use Disorder | 189 | (6.2%) | 144 | (5.3%) | 45 | (13.9%) | .0001 |
| Current Other Drug Use Disorder | 17 | (0.6%) | 13 | (0.5%) | 4 | (1.2%) | n.s. |
| Characteristic | M | (sd) | M | (sd) | M | (sd) | |
|
| |||||||
| Age | 37.45 | (10.26) | 37.91 | (10.25) | 33.63 | (9.52) | .0001 |
| Combat Exposure - CES | 11.05 | (10.54) | 11.00 | (10.51) | 11.52 | (10.90) | n.s. |
| Depression Severity -BDI | 14.05 | (12.63) | 13.84 | (12.63) | 15.80 | (12.55) | .0085 |
| PTSD Severity - DTS | 39.12 | (39.49) | 38.37 | (39.37) | 45.40 | (40.00) | .0026 |
Note. CES=Combat Exposure Scale; BDI = Beck Depression Inventory; DTS=Davidson Trauma Scale
Difficulty with controlling violence in the past 30 days was present among eight percent (n = 255) of the sample. Moderate or greater difficulties managing anger were endorsed by 33.3% (n = 1,007) and moderate or greater aggressive impulses/urges were endorsed by 17.6% (n = 533) of the sample. Difficulty controlling violence in the past 30 days was related to SCL-90 scores assessing difficulty managing anger (r = .44, p < .0001) and aggressive urges/impulses (r = .47, p < .0001). In bivariate analyses, both lifetime CUD [OR = 1.56 (95% CI 1.05-2.29)] and current CUD [OR = 4.2 (95% CI 2.19-8.05)] were significantly related to difficulty controlling violence in the past 30 days (see Figure 1). Current [OR = 3.74 (95% CI 2.06-6.80)] but not lifetime CUD [OR=1.12 (95% CI 0.87-1.46)] was associated with odds of reporting difficulty managing anger. Similarly, current CUD [OR = 4.09 (2.30-7.27)] but not lifetime CUD [OR = 1.22 (95% CI 0.90-1.66)] was associated with odds of reporting increased aggressive impulses and urges.
Figure 1.
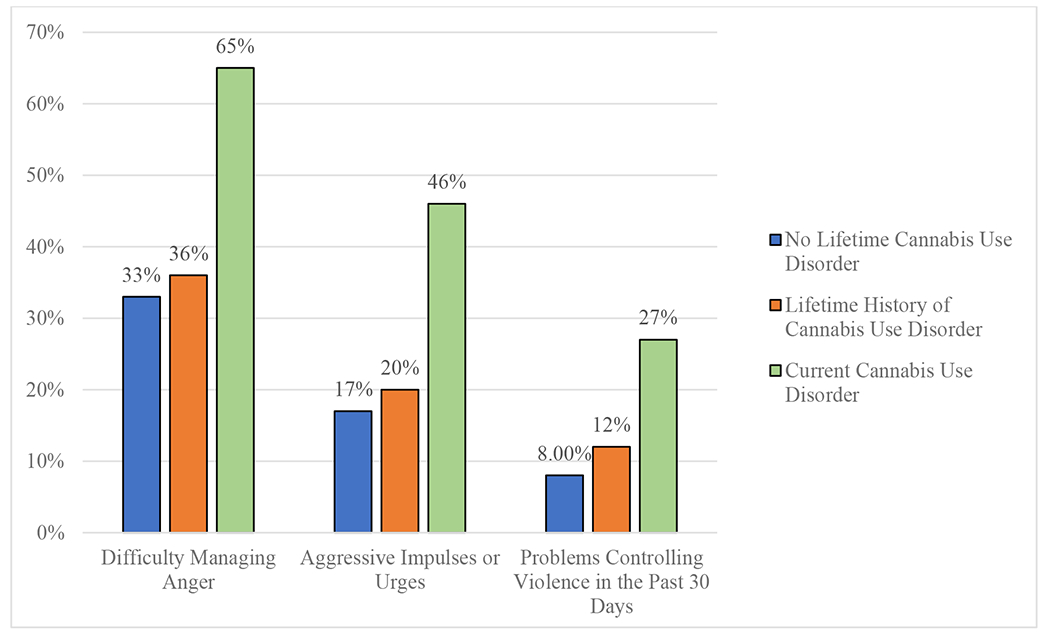
Association between Cannabis Use Disorder and Anger, Aggressive Impulses, and Problems Controlling Violence in the Past 30 Days among Iraq/Afghanistan-era Veterans (N=3031)
Results from the bivariate and multivariate logistic regressions predicting each anger/aggression outcome are presented in Table 2. Current CUD remained significantly positively associated with all three outcomes (difficulty managing anger, aggressive impulses/urges, and problems controlling violence in past 30 days), even accounting for demographic/history variables, combat exposure, depressive symptoms, PTSD symptom severity, current alcohol use disorder, and presence of other drug use disorders. Lifetime CUD was also uniquely associated with problems controlling violence in the past 30 days, but was not significantly associated with difficulty managing anger or aggressive impulses/urges.
Table 2.
Summary of Bivariate and Multivariate Logistic Regression Models examining Anger, Aggressive Impulses, and Problems Controlling Violence in the Past 30 Days
| Difficulty Managing Anger | Aggressive Impulses or Urges | Problems Controlling Violence in the Past 30 Days | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | OR (95% CI) |
AOR (95% CI) |
OR (95% CI) |
AOR (95% CI) |
OR (95% CI) |
AOR (95% CI) |
|||
| Age | 0.98*** (0.97-0.98) |
0.98** (0.97-1.00) |
0.97*** (0.96-0.98) |
0.98** (0.97-0.99) |
0.99 (0.98-1.00) |
1.01 (1.00-1.03) |
|||
| Race (White) | 1.07 (0.92-1.24) |
1.08 (0.85-1.38) |
1.22* (1.01-1.47) |
1.19 (0.93-1.53) |
0.93 (0.72-1.20) |
0.99 (0.72-1.34) |
|||
| Female Sex | 0.98 (0.82-1.19) |
1.02 (0.74-1.40) |
0.65*** (0.50-0.84) |
0.52*** (0.37-0.74) |
0.91 (0.66-1.26) |
0.94 (0.62-1.41) |
|||
| Education (> high school) |
0.64*** (0.55-0.75) |
0.94 (0.74-1.20) |
0.60*** (0.50-0.73) |
0.93 (0.73-1.19) |
0.60*** (0.47-0.78) |
0.88 (0.65-1.19) |
|||
| Currently Married | 1.05 (0.90-1.22) |
1.73*** (1.35-2.21) |
0.99 (0.82-1.20) |
1.18 (0.92-1.52) |
1.00 (0.77-1.29) |
1.12 (0.82-1.53) |
|||
| History of incarceration | 2.05*** (1.72-2.44) |
1.45** (1.10-1.89) |
2.05*** (1.67-2.52) |
1.16 (1.89-1.51) |
2.05*** (1.57-2.70) |
1.18 (0.86-1.63) |
|||
| Highest Military Rank (Officer) | 0.36*** (0.25-0.51) |
0.72 (0.43-1.20) |
0.36*** (0.22-0.59) |
0.78 (0.43-1.42) |
0.13*** (0.04-0.41) |
0.22** (0.07-0.71) |
|||
| Combat Exposure - CES | 1.07*** (1.06-1.08) |
1.01* (1.00-1.03) |
1.07*** (1.06-1.08) |
1.01 (1.00-1.02) |
1.06*** (1.05-1.07) |
1.01 (1.00-1.03) |
|||
| Depression Severity - BDI | 1.18*** (1.17-1.20) |
1.11*** (1.10-1.13) |
1.11*** (1.10-1.12) |
1.06*** (1.04-1.07) |
1.09*** (1.08-1.10) |
1.05*** (1.03-1.07) |
|||
| PTSD Severity - DTS | 1.05*** (1.05-1.05) |
1.03*** (1.02-1.03) |
1.04*** (1.03-1.04) |
1.02*** (1.02-1.03) |
1.03*** (1.03-1.04) |
1.02*** (1.01-1.02) |
|||
| Current Alcohol Use Disorder | 2.62*** (1.95-3.53) |
1.16 (0.74-1.80) |
2.80*** (2.04-3.83) |
1.28 (0.86-1.91) |
2.71*** (1.83-4.01) |
1.21 (0.75-1.94) |
|||
| Other Drug Use Disorder | 2.88* (1.09-7.60) |
0.73 (0.19-2.82) |
4.21** (1.62-10.96) |
1.46 (0.43-4.89) |
4.60** (1.61-13.17) |
1.91 (0.52-6.98) |
|||
| Cannabis Use Disorder | |||||||||
| Lifetime | 1.12 (0.87-1.46) |
0.92 (0.63-1.34) |
1.22 (0.90-1.66) |
1.07 (0.73-1.58) |
1.56* (1.05-2.29) |
1.64* (1.05-2.56) |
|||
| Current | 3.74*** (2.06-6.80) |
2.93* (1.24-6.92) |
4.09*** (2.30-7.27) |
2.74* (1.26-5.98) |
4.20*** (2.19-8.05) |
2.71* (1.18-6.23) |
|||
Note.
p<.05;
p<.01;
p<.001;
OR = Odds Ratio; AOR = Adjusted Odds Ratios; Adjusted Odds Ratios reflect adjustment for all the other variables in the model.
Discussion
The current study sought to examine the associations between CUD, anger and aggression in a large and diverse sample of Iraq/Afghanistan-era veterans. We found that current CUD was significantly associated with increased odds of self-reported problems managing anger, aggressive impulses/urges, and problems controlling violence in the past 30 days. The prevalence of difficulty controlling violence in the past 30 days among those with current CUD (27%) was more than twice as high as those with lifetime CUD (12%) and more than three times as high as those without lifetime CUD (8%). Similar patterns were found for aggressive impulses urges and problems managing anger (see Figure 1). Even in the multivariate models, adjusting for demographics, military rank, combat exposure, history of incarceration, clinical covariates (PTSD and depression severity), alcohol use disorder, and other drug use disorder, current CUD was significantly associated with all three anger/aggression variables. Lifetime CUD remained significantly associated with difficulty controlling violence in the past 30 days. Together, these findings suggest a robust, unique association between CUD and difficulties with anger and aggression in veterans.
While the current study cannot address the direction of the relationship between CUD and violence, the statistically significant association between these variables in veterans, across different dimensions of anger management problems and violent impulses, indicates that this is an area of critical importance for future research. To date, several mechanisms for the relationship between cannabis use and violence/aggression have been proposed. First, some researchers have suggested that cannabis use may cause increased aggression (Moore & Stuart, 2005). Not only is cannabis withdrawal often characterized by irritability and anger, but its psychopharmacological effects can also include confusion, paranoia, suspiciousness, and panic attacks, which may increase the propensity to respond to others with violence. Second, the cognitive impairments caused by cannabis use may also decrease the ability to appropriately attend to interpersonal conflict and inhibit inappropriate responses (Moore & Stuart, 2005). Third, individuals who use cannabis may have problems controlling aggression independent of their use of cannabis, and they may use the drug as a method of self-medication. At least one study has found evidence to support this hypothesis in a non-veteran clinical sample (Arendt et al., 2007), and this explanation for the link aligns with reports by veterans that they use cannabis to manage psychological problems including PTSD symptoms (Metrik et al., 2018).
With respect to immediate clinical implications, our findings suggest that it may be important for therapists to ask veterans with CUD specifically about their problems with anger and aggression, and that anger management strategies may be a useful addition to substance use treatment particularly for this disorder. Conversely, it may also be important for clinicians to ask veterans with anger problems or aggression about their use of cannabis, so that they can better evaluate whether substance abuse treatment may be warranted.
Additional research to disentangle the potential mechanisms of the association between CUD and violence is needed. If CUD contributes to violence, then preventing and treating CUD will be particularly critical among veterans who struggle with aggressive urges, including those with PTSD. If, on the other hand, veterans are using cannabis to manage aggressive urges, the safety and effectiveness of its use for this purpose should be a high research priority among researchers. Finally, it is important to note that these two mechanisms are not necessarily mutually exclusive: It is possible that veterans may attempt to manage aggressive urges through cannabis use, but that heavy use may also exacerbate the very symptoms users are attempting to alleviate.
Results of this study should be considered in light of several limitations. First, the sample consisted of participants who self-selected to participate in this research and may not be representative of all Iraq/Afghanistan-era veterans. Second, the use of self-report measures of anger and aggression may have resulted in an underestimate of these constructs, as participants may be reluctant to disclose violent urges. Response biases may have similarly affected the disclosure of CUD, which could have inflated the estimated associations between these constructs. Finally, although this study assessed anger, aggressive urges, and perceived problems controlling violence, it did not include a measure of violent acts; hence, it is unknown whether CUD is associated with actual violence.
In summary, the findings from the current study suggest that CUD may be uniquely associated with problems managing anger, aggressive impulses/urges, and problems controlling violence in veterans, even after accounting for a wide array of relevant covariates. This finding is particularly important given the high rate of anger difficulties and aggressive behavior among veterans as well as the increasing rate of CUD among veterans in recent years. Additional research aimed at understanding the complex relationship between CUD and anger/aggression is warranted.
Acknowledgements
This work was supported by the Mid-Atlantic Mental Illness Research, Education, and Clinical Center (MIRECC). Dr. Dillon was supported by a Career Development Award (IK2RX002965) from the Rehabilitation Research and Development Service of the Department of Veterans Affairs Office of Research and Development (VA ORD). Dr. Beckham was supported by a Senior Research Career Scientist award (1K6BX003777) and Dr. Szabo was supported by a Career Development Award (1IK2CX001397) from the Clinical Science Research and Development of VA ORD. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government or any of the institutions with which the authors are affiliated.
References
- Arendt M, Rosenberg R, Fjordback L, Brandholdt J, Foldager L, Sher L, & Munk-Jørgensen P (2007). Testing the self-medication hypothesis of depression and aggression in cannabis-dependent subjects. Psychological Medicine, 37, 935–945. DOI: 10.1017/S0033291706009688 [DOI] [PubMed] [Google Scholar]
- Beck AT, & Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory—II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bonn-Miller MO, Harris AH, & Trafton JA (2012). Prevalence of cannabis use disorder diagnoses among veterans in 2002, 2008, and 2009. Psychological Services, 9, 404–416. DOI: 10.1037/a0027622 [DOI] [PubMed] [Google Scholar]
- Brancu M, Wagner HR, Morey RA, Beckham JC, Calhoun PS, Tupler LA, & McDonald SD (2017). The Post-Deployment Mental Health (PDMH) study and repository: A multi-site study of US Afghanistan and Iraq era veterans. International Journal of Methods in Psychiatric Research, 26, e1570. 10.1002/mpr.1570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford EF, Calhoun PS, Braxton LE, & Beckham JC (2007). Validity of the personality assessment inventory aggression scales and violence potential index in veterans with PTSD. Journal of Personality Assessment, 88, 90–98. DOI: 10.1080/00223890709336839 [DOI] [PubMed] [Google Scholar]
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, … & Davison RM (1997). Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine, 27, 153–160. DOI: 10.1017/S0033291796004229 [DOI] [PubMed] [Google Scholar]
- Derogatis LR (1994). SCL-90-R: Administration, scoring and procedures manual (3rd ed.). Minneapolis, MN: Nation Computer Systems. [Google Scholar]
- Dugré JR, Dellazizzo L, Giguère C-E, Potvin S, & Dumais A (2017). Persistency of cannabis use predicts violence following acute psychiatric discharge. Frontiers in Psychiatry, 8, 1–8. DOI: 10.3389/fpsyt.2017.00176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbogen EB, Wagner HR, Fuller SR, Calhoun PS, Kinneer PM, Mid-Atlantic Mental Illness Research, Education, and Clinical Center Workgroup, & Beckham JC (2010). Correlates of anger and hostility in Iraq and Afghanistan war veterans. American Journal of Psychiatry, 167, 1051–1058. DOI: 10.1176/appi.ajp.2010.09050739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, and Williams JBW (1994) Structural Clinical Interview for Axis I DSM-IV Disorders, second ed. Biometrics Research Department, New York, NY. [Google Scholar]
- Himmelstein JL (1983). From killer weed to drop-out drug: the changing ideology of marihuana. Contemporary Crisis, 7, 13–38. [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351, 13–22. DOI: 10.1056/NEJMoa040603 [DOI] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, & Mora CA (1989). Clinical evaluation of a measure to assess combat exposure. Psychological Assessment, 1, 53–55. DOI: 10.1037/1040-3590.1.1.53 [DOI] [Google Scholar]
- Kimbrel NA, Calhoun PS, Elbogen EB, Brancu M, Beckham JC, V. A. Mid-Atlantic MIRECC Registry Workgroup. (2014). The factor structure of psychiatric comorbidity among Iraq/Afghanistan-era veterans and its relationship to violence, incarceration, suicide attempts, and suicidality. Psychiatry Research, 220, 397–403. 10.1016/j.psychres.2014.07.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolla NJ, & Mishra A (2018). The endocannabinoid system, aggression, and the violence of synthetic cannabinoid use, borderline personality disorder, antisocial personality disorder, and other psychiatric disorders. Frontiers in Behavioral Neuroscience, 12, 41. DOI: 10.3389/fnbeh.2018.00041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Bassett SS, Aston ER, Jackson KM, & Borsari B (2018). Medicinal versus recreational cannabis use among returning veterans. Translational Issues in Psychological Science, 4, 6–20. DOI: 10.1037/tps0000133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore TM & Stuart GL (2005). A review of the literature on marijuana and interpersonal violence. Aggression and Violent Behavior, 10, 171–192. DOI: 10.1016/j.avb.2003.10.002 [DOI] [Google Scholar]
- Novaco RW, & Chemtob CM (2015). Violence Associated With Combat-Related Posttraumatic Stress Disorder: The Importance of Anger. Psychological Trauma: Theory, Research, Practice and Policy. DOI: 10.1037/tra0000067 [DOI] [PubMed] [Google Scholar]
- Orsolini L, Chiappini S, Volpe U, De Berardis D, Latini R, Papanti GD, & Corkery JM (2019). Use of medicinal cannabis and synthetic cannabinoids in post-traumatic stress disorder (PTSD): a systematic review. Medicina, 55, 525. DOI: 10.3390/medicina55090525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orth U, & Wieland E (2006). Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: a meta-analysis. Journal of Consulting and Clinical Psychology, 74(4), 698–706. doi: 10.1037/0022-006X.74.4.698 [DOI] [PubMed] [Google Scholar]
- Sayer NA, Noorbaloochi S, Frazier P, Carlson K, Gravely A, & Murdoch M (2010). Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatric Services, 61, 589–597. DOI: 10.1176/appi.ps.61.6.589 [DOI] [PubMed] [Google Scholar]
- Sippel LM, Mota NP, Kachadourian LK, Krystal JH, Southwick SM, Harpaz-Rotem I, & Pietrzak RH (2016). The burden of hostility in US Veterans: results from the National Health and Resilience in Veterans Study. Psychiatry Research, 243, 421–430. DOI: 10.1016/j.psychres.2016.06.040 [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Blessing EM, Galatzer-Levy IR, Hollahan LC, & Anderson WT (2017). Marijuana and other cannabinoids as a treatment for posttraumatic stress disorder: a literature review. Depression and Anxiety, 34, 207–216. DOI: 10.1002/da.22596 [DOI] [PubMed] [Google Scholar]
- Sundin J, Herrell RK, Hoge CW, Fear NT, Adler AB, Greenberg N, … Bliese PD (2014). Mental health outcomes in US and UK military personnel returning from Iraq. The British Journal of Psychiatry, 204, 200–207. doi: 10.1192/bjp.bp.113.129569 [DOI] [PubMed] [Google Scholar]
- Van Voorhees EE, Dennis PA, Elbogen EB, Fuemmeler B, Neal LC, Calhoun PS, & Beckham JC (2018). Characterizing anger-related affect in individuals with posttraumatic stress disorder using ecological momentary assessment. Psychiatry Research, 261, 274–280. DOI: 10.1016/j.psychres.2017.12.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees EE, Dennis PA, Neal LC, Hicks TA, Calhoun PS, Beckham JC, & Elbogen EB (2016). Posttraumatic Stress Disorder, Hostile Cognitions, and Aggression in Iraq/Afghanistan Era Veterans. Psychiatry, 79, 70–84. doi: 10.1080/00332747.2015.1123593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson ST, Radhakrishnan R, & D’Souza DC (2016). A systematic review of the evidence for medical marijuana in psychiatric indications. Journal of Clinical Psychiatry, 77, 1050–1064. DOI: 10.4088/JCP.15r10036 [DOI] [PubMed] [Google Scholar]
- Wilkinson ST, Stefanovics E, & Rosenheck RA (2015). Marijuana use is associated with worse outcomes in symptom severity and violent behavior in patients with PTSD. Journal of Clinical Psychiatry, 76, 1174–1180. DOI: 10.4088/JCP.14m09475 [DOI] [PMC free article] [PubMed] [Google Scholar]


